Abstract
Background
Failure of implantation and conception may result from inability of the blastocyst to escape from its outer coat, which is known as the zona pellucida. Artificial disruption of this coat is known as assisted hatching and has been proposed as a method for improving the success of assisted conception by facilitating embryo implantation.
Objectives
To determine effects of assisted hatching (AH) of embryos derived from assisted conception on live birth and multiple pregnancy rates.
Search methods
We searched the following databases (from their inception to 27 May 2020), with no language or date restriction: Cochrane Gynaecology and Fertility Group (CGFG) specialised register, CENTRAL, MEDLINE, Embase and PsycINFO. We checked reference lists of relevant studies and searched the trial registers.
Selection criteria
Two review authors identified and independently screened trials. We included randomised controlled trials (RCTs) of AH (mechanical, chemical, or laser disruption of the zona pellucida before embryo replacement) versus no AH that reported live birth or clinical pregnancy data.
Data collection and analysis
We used standard methodological procedures recommended by Cochrane. Two review authors independently performed quality assessments and data extraction.
Main results
We included 39 RCTs (7249 women). All reported clinical pregnancy data, including 2486 clinical pregnancies. Only 14 studies reported live birth data, with 834 live birth events. The quality of evidence ranged from very low to low. The main limitations were serious risk of bias associated with poor reporting of study methods, inconsistency, imprecision, and publication bias. Five trials are currently ongoing.
We are uncertain whether assisted hatching improved live birth rates compared to no assisted hatching (odds ratio (OR) 1.09, 95% confidence interval (CI) 0.92 to 1.29; 14 RCTs, N = 2849; I² = 20%; low‐quality evidence). This analysis suggests that if the live birth rate in women not using assisted hatching is about 28%, the rate in those using assisted hatching will be between 27% and 34%.
Analysis of multiple pregnancy rates per woman showed that in women who were randomised to AH compared with women randomised to no AH, there may have been a slight increase in multiple pregnancy rates (OR 1.38, 95% CI 1.13 to 1.68; 18 RCTs, N = 4308; I² = 48%; low‐quality evidence). This suggests that if the multiple pregnancy rate in women not using assisted hatching is about 9%, the rate in those using assisted hatching will be between 10% and 14%.
When all of the included studies (39) are pooled, the clinical pregnancy rate in women who underwent AH may improve slightly in comparison to no AH (OR 1.20, 95% CI 1.09 to 1.33; 39 RCTs, N = 7249; I² = 55%; low‐quality evidence). However, when a random‐effects model is used due to high heterogeneity, there may be little to no difference in clinical pregnancy rate (P = 0.04).
All 14 RCTs that reported live birth rates also reported clinical pregnancy rates, and analysis of these studies illustrates that AH may make little to no difference in clinical pregnancy rates when compared to no AH (OR 1.07, 95% CI 0.92 to 1.25; 14 RCTs, N = 2848; I² = 45%).
We are uncertain about whether AH affects miscarriage rates due to the quality of the evidence (OR 1.13, 95% CI 0.82 to 1.56; 17 RCTs, N = 2810; I² = 0%; very low‐quality evidence).
Authors' conclusions
This update suggests that we are uncertain of the effects of assisted hatching (AH) on live birth rates. AH may lead to increased risk of multiple pregnancy. The risks of complications associated with multiple pregnancy may be increased without evidence to demonstrate an increase in live birth rate, warranting careful consideration of the routine use of AH for couples undergoing in vitro fertilisation (IVF) or intracytoplasmic sperm injection (ICSI).
AH may offer a slightly increased chance of achieving a clinical pregnancy, but data quality was of low grade. We are uncertain about whether AH influences miscarriage rates.
Plain language summary
Assisted hatching of fertilised eggs in assisted conception (IVF and ICSI)
Review question
Does assisted hatching (help to hatch human embryos in the laboratory) during assisted reproduction improve the chance of achieving pregnancy and live birth, and does it affect the risk of multiple pregnancy?
Background
Assisted hatching is a technique that is sometimes used in assisted reproduction for in vitro fertilisation (IVF) and intracytoplasmic sperm injection (ICSI). It involves thinning the coat surrounding the fertilised egg or making a hole in it. It is suggested that this may improve the chance of the embryo attaching to the lining of the womb, so that pregnancy can begin.
Study characteristics
Cochrane Review authors included 39 randomised controlled trials (RCTs) of 7249 women. All studies reported clinical pregnancy, but only 14 studies reported live birth, and only 18 reported multiple pregnancy. The evidence is current to May 2020.
Key results
This review of RCTs demonstrates that we are uncertain of the effects of assisted hatching on live birth rate when compared to no assisted hatching. Assisted hatching may increase slightly multiple pregnancy rates when compared to no AH. Assisted hatching may improve slightly the chances of clinical pregnancy in women. We are uncertain about the effects of AH on miscarriage.
Only studies that report live birth and multiple pregnancy as their primary outcome measures should be performed and funded in the future.
Quality of the evidence
The quality of the evidence is low to very low. The main limitations are serious risk of bias associated with poor reporting of study methods, inconsistency, imprecision, and publication bias.
Summary of findings
Summary of findings 1. Assisted hatching compared to no assisted hatching for women undergoing assisted conception.
| Assisted hatching compared to no assisted hatching for women undergoing assisted conception | ||||||
|
Patient or population: women undergoing assisted conception Setting: clinic Intervention: assisted hatching Comparison: no assisted hatching | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | №. of participants (studies) | Quality of evidence (GRADE) | Comments | |
| Risk with no assisted hatching | Risk with assisted hatching | |||||
| Live births per woman randomised | 283 per 1000 | 301 per 1000 (267 to 338) | OR 1.09 (0.92 to 1.29) | 2849 (14 RCTs) | ⊕⊕⊝⊝ LOWa | |
| Multiple pregnancy rate per woman randomised | 91 per 1000 | 121 per 1000 (102 to 144) | OR 1.38 (1.13 to 1.68) | 4308 (18 RCTs) | ⊕⊕⊝⊝ LOWb | |
| Clinical pregnancy rate per woman randomised | 322 per 1000 | 363 per 1000 (341 to 387) | OR 1.20 (1.09 to 1.33) | 7249 (39 RCTs) | ⊕⊕⊝⊝ LOWb | |
| Miscarriage rate per woman randomised | 53 per 1000 | 60 per 1000 (44 to 81) | OR 1.13 (0.82 to 1.56) | 2810 (17 RCTs) | ⊕⊝⊝⊝ VERY LOWc | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; OR: odds ratio; RCT: randomised controlled trial. | ||||||
| GRADE Working Group grades of evidence. High quality: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low quality: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded two levels for serious risk of bias and publication bias: in many studies, the method was unclear and information was incomplete. The main limitation was serious risk of bias associated with poor reporting of study methods.
bDowngraded two levels for serious risk of bias and for serious inconsistency.
cDowngraded three levels for serious risk of bias, serious inconsistency, and serious imprecision (only 158 events).
Background
Description of the condition
The World Health Organization estimates that one in four couples in developing countries have been found to be affected by infertility (Mascarenhas 2012). Increasing numbers of couples require treatment by the assisted conception (AC) procedures of in vitro fertilisation (IVF) and intracytoplasmic sperm injection (ICSI) ‐ types of assisted reproductive technology (ART). In the UK in 2018, 54,000 women had 68,727 fresh and frozen IVF cycles at Human Fertilisation and Embryology Authority (HFEA)‐licensed fertility clinics (HFEA 2020). In 2016, across 40 European countries, a total of 156,002 cycles of IVF and 407,222 cycles of ICSI were performed, with ART infants contributing to 2.9% of all births. Following IVF and ICSI, clinical pregnancy rates per transfer were 34.8% and 33.2%, respectively (ESHRE‐ European IVF monitoring consortium 2020).
The European Society of Human Reproduction and Embryology (ESHRE) reported that the most important indicator of success of ART treatment is the birth of a single healthy child (Land 2003). Following this, the Harbin Consensus Conference Workshop Group developed a modified Consolidated Standards of Reporting Trials (CONSORT) statement for infertility trials and recommended that the preferred primary outcome of all infertility trials is live birth (defined as any delivery of a live infant at ≥ 20 weeks' gestation) (Harbin Consensus Conference Workshop Group 2014).
Numerous innovations have improved assisted reproduction outcomes; these include laboratory technologies to improve fertilisation, cryopreservation techniques, blastocyst transfers to improve success (Glujovsky 2016), pre‐genetic testing (Sengupta 2012), and time lapse embryo imaging, which provides a better selection of embryos for transfer (Freour 2012).
To improve ART outcomes, a receptive endometrium in the presence of a good quality embryo is important for achieving a successful pregnancy. The quality of the transferred embryos may be affected by genetic disorders, issues with hatching (zona pellucida harding), and poor laboratory cultural conditions.
The human oocyte and early embryo is surrounded by a 13‐ to 15‐μm‐thick acellular matrix, the zona pellucida (ZP) (Bleil 1980), which is composed of glycoproteins, carbohydrates, and zona pellucida‐specific proteins (ZP1, ZP2, ZP3, ZP4) (Lefievre 2004). The zona pellucida is bi‐layered; the outer layer is thick, whereas the inner layer is thin but resilient. It is involved in sperm binding and induction of the acrosome reaction, and it promotes oocyte fusion (Gupta 2015). Following fertilisation, the zona pellucida blocks polyspermy, prevents blastomere dispersal, and helps in oviductal transport. It avoids contact with other cells (epithelial lining of the reproductive tract, leucocytes, spermatozoa, and other cells of the embryo). It is essential for maintaining the integrity of the pre‐compacted embryo. Compaction is the formation of structural junctions between blastomeres. Once compaction occurs, the zona pellucida is no longer essential (Hammadeh 2011). Zona hardening occurs naturally after fertilisation to ensure this threefold function. A combination of lysins produced by the cleaving embryo or the uterus and physical expansion then reduces the zona thickness in preparation for hatching. Zona hardening, although not readily quantifiable, may also be induced by in vitro culture and by in vivo aging (De Vos 2000).
After fertilisation, the zona maintains the three‐dimensional integrity of the uncompacted embryo for up to six days in early development, facilitates free passage of the compacted embryo through the fallopian tube into the uterus, and protects the embryo from micro‐organisms and immune cells (Bronson 1970). During embryonic development, fluid starts to accumulate between cells at the morulae stage. As the volume of fluid increases, a cavity gradually appears, forming the blastocoele. This normally happens between Days 4 and 5 in human embryos in vitro and is known as the blastocyst stage. Concurrently with the increase in fluid inside the blastocyst, the number of cells increases. This combination causes progressive enlargement of the blastocyst and its cavity, leading to progressive thinning of the ZP. Finally, the blastocyst breaks free of the ZP through a process called hatching (Hardarson 2012). This process occurs before implantation.
Human embryos resulting from controlled ovarian hyperstimulation develop more slowly in vitro compared to embryos in vivo. These embryos manifest a relatively high degree of cytogenetic abnormalities and cellular fragmentation and a reduced rate of blastocyst development, although maternal age and treatment protocols may influence rates (Hsu 1999). Cultured embryos also hatch and implant at lower rates than occurs naturally (Harlow 1982; Mercader 2001). It is unclear whether this is due to 'hardening' of the zona pellucida as a result of cross‐linking of its constituent ZP glycoproteins in an in vitro environment (Cohen 1991). With IVF and ICSI treatment, the possible combination of delayed embryo hatching and advanced endometrial development may present an unfavourable environment for implantation (Check 1999; Hsu 1999).
Description of the intervention
Artificial disruption of the zona pellucida is known as assisted hatching (AH) and was first suggested in the 1980s. It was subsequently observed in women undergoing embryo biopsy for pre‐implantation genetic diagnosis (Fehilly 1985). AH is a complementary technique to conventional ART and involves thinning or completely diminishing a small fraction of the outer coat of a fertilised egg or early embryo to encourage hatching and implantation in the receptive endometrium.
A variety of techniques have since been employed to assist embryo hatching, including chemical drilling of the ZP with acidic Tyrode’s medium, ZP thinning using acidic Tyrode’s, mechanical piercing of the ZP with a microneedle, known also as partial zona dissection (PZD), and mechanical expansion of the ZP via injected hydrostatic pressure, carving a hole in ZP via piezoelectric pulses and laser‐assisted zona drilling (Avella 2019). Regardless of the AH technique employed, it is important to distinguish whether the zona has remained unbreached (as in thinning), has been fully breached (when a hole is made chemically), or has been completely removed. This distinction may have implications for whether an embryo is able to undergo normal zona expansion and escape following AH (Blake 2001), as well as for subsequent monozygotic twinning (da Costa 2001; Menezo 2003; Schieve 2000). At present, laser AH is the most popular complementary ART technique (Hammadeh 2011)
How the intervention might work
Zona thickness appears to be influenced by a variety of factors including the woman's age (Balakier 2012), hormone profile, smoking, and cause of infertility. Increased ZP thickness correlates negatively with embryo implantation rates (Avella 2019, Loret de Mola 1997). Implantation of the embryo into the endometrium is initiated by hatching of the embryo from the surrounding ZP (Hardarson 2012). Failure of the embryonic zona pellucida to rupture following blastocyst expansion has been suggested as a possible contributing factor to failure of embryo implantation. To help embryos escape from their zona during blastocyst expansion, different types of assisted hatching have been proposed (De Vos 2000).
Many mechanisms by which AH could improve embryo implantation have been postulated. One of these mechanisms is AH overcoming the zona pellucida hardening caused by IVF and cell culture or cryopreservation. Additionally, some evidence indicates that embryos that have undergone zona manipulation for AH tend to implant one day earlier than unhatched embryos (Rink 1995). Finally, as suggested by Cohen 1992, artificial opening could enhance hormonal and metabolite exchange, as well as messaging between the embryo and the endometrium.
Why it is important to do this review
Zona manipulation of some form has been offered to women of advanced age and to those with high follicle‐stimulating hormone (FSH) levels, with high risk of zona hardening (as with in vitro oocyte maturation), and status post repeated implantation failure (Al‐Nuaim 2002). However, considerable uncertainty remains over whether AH significantly improves IVF and ICSI clinical outcomes and embryo implantation rates, or whether it is associated with negative consequences for embryo development and viability. Previous updates showed that AH results in an increase in clinical pregnancy rates when compared with no AH, but AH has failed to result in a statistically significant increase in live birth rates. However, few trials have reported on live birth rates. We hope that updating this review and incorporating more studies will provide more conclusive evidence of effects of AH on live birth rate particularly rather than only on clinical pregnancy rates, as well as its effects on other outcomes such as miscarriage and multiple pregnancy rates.
Objectives
To determine effects of assisted hatching (AH) of embryos derived from assisted conception on live birth and multiple pregnancy rates.
Methods
Criteria for considering studies for this review
Types of studies
Published and unpublished randomised controlled trials (RCTs) were eligible for inclusion. We excluded non‐randomised studies (e.g. studies with evidence of inadequate sequence generation such as alternate days and patient numbers), as they are associated with high risk of bias. Trials were eligible for inclusion only if data could be extracted per woman and not per cycle. We excluded trials that presented results as per cycle rather than as per woman (unless it was clear in the text that per cycle and per woman were used interchangeably). We excluded cross‐over trials, as the design is not valid in this context.
Types of participants
Eligible participants were women of all nationalities and reproductive ages undergoing assisted conception by IVF or ICSI, using their own gametes and consenting to participation in a trial of AH after fertilisation.
In the subgroup analysis, poor prognosis referred to women with increased age, previous IVF failure, high FSH, or use of frozen embryos, or it was used when the primary study protocol referred to women with a poor prognosis.
Types of interventions
Trials that investigated any known method of AH after fertilisation were included. Techniques used to disrupt the zona pellucida before embryo replacement were of the following forms.
Mechanical.
Chemical.
Laser.
Trials in which assisted hatching took place to the following extent were eligible.
Breaching the zona pellucida by a hole (by laser, chemical, or mechanical means).
Thinning the zona pellucida (with no actual hole created).
Removing the entire zona pellucida.
Trials were eligible when AH was performed on fresh embryos and cryopreserved embryos following thawing and before embryo transfer, as well as on vitrified‐warmed embryos that were transferred at the cleavage stage. The effects of these interventions were compared to those of a control by which AH was not performed.
Trials directly comparing different AH methods (without including a control group with no assisted hatching performed) were excluded because the objective of this review was to determine the overall effectiveness of the technique of AH.
We excluded biopsied embryos for purposes of pre‐genetic screening (PGS)/pre‐genetic diagnosis (PGD) during assisted reproduction because this approach aims towards embryo selection ‐ not towards increased possibility of implantation per se. As assisted hatching has been proposed to improve implantation, leading to improved clinical pregnancy and live birth rates, biopsied embryos for PGS and PGD were excluded.
Types of outcome measures
Primary outcomes
Live birth rate per woman
Multiple pregnancy rate per woman
Secondary outcomes
Clinical pregnancy rate per woman (defined as pregnancy diagnosed by ultrasonographic visualisation of one or more gestational sacs, or definitive clinical signs of pregnancy)
Miscarriage rate per woman (loss of pregnancy up to 20 weeks' gestation per woman)
Monozygotic twinning per woman
Ectopic pregnancy rate per woman
Congenital or chromosomal abnormalities per woman
Only trials that reported at least clinical pregnancy rate per woman were included. The first version of the review included trials with implantation as an outcome; however for this update, we have removed implantation rate as an outcome. It is not possible to pool implantation, as the data are reported per embryo. We recorded live birth as an event per woman and not by the number of infants delivered because of the large number of multiple births.
Search methods for identification of studies
We searched for all published and unpublished RCTs of AH versus no AH, without language restrictions, from inception of the databases until 27 May 2020, in consultation with the Gynaecology and Fertility Group Information Specialist.
Electronic searches
We searched the following electronic databases, trial registers, and websites:
Cochrane Gynaecology and Fertility (CGF) Group Specialised Register of Controlled Trials, ProCite platform, searched 27 May 2020, (Appendix 1);
CENTRAL, via the Cochrane Register of Studies Online (CRSO), Web platform, searched 27 May 2020, (Appendix 2);
MEDLINE, Ovid platform, searched from 1946 to 27 May 2020, (Appendix 3);
Embase, Ovid platform, searched from 1980 to 27 May 2020, (Appendix 4);
PsycINFO, Ovid platform, searched from 1806 to 27 May 2020,(Appendix 5).
Searching other resources
International trial registers: the ClinicalTrials database, a service of the US National Institutes of Health (clinicaltrials.gov/ct2/home) and the World Health Organization International Trials Registry Platform search portal (www.who.int/trialsearch/Default.aspx);
We also handsearched the reference lists of relevant articles retrieved by the search.
Data collection and analysis
We conducted data collection and analysis in accordance with the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2019).
Selection of studies
Two review authors (LL and SH) scanned titles and abstracts from the first searches; the same methods were adopted by another review author for the second searches. Trials that appeared relevant were selected and formally assessed for inclusion independently by three review authors using an inclusion and exclusion form. We resolved disagreements through discussion. Multiple reports of the same study were collated under a single reference. We corresponded with study investigators as required to clarify study eligibility. Trials excluded at this stage are detailed in the table Characteristics of excluded studies table. We have documented the selection process with a PRISMA flow chart (Figure 1).
1.
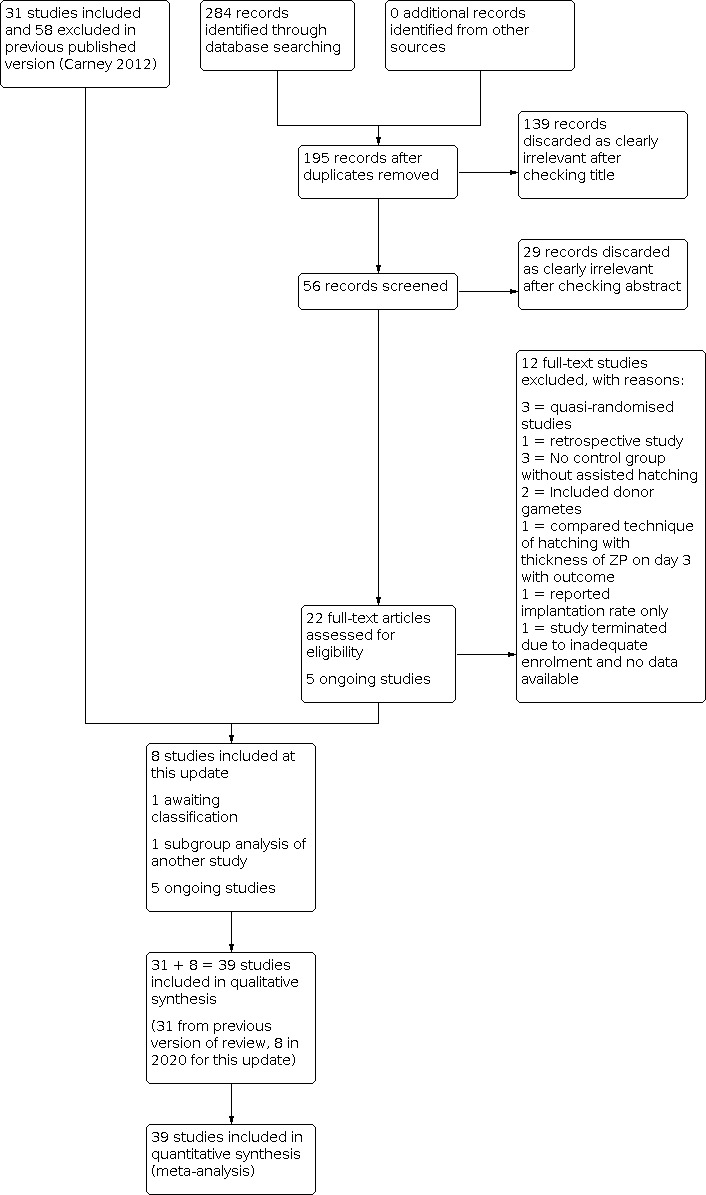
Study flow diagram.
Data extraction and management
Two review authors (LL and MAA) independently extracted data from eligible studies using the Cochrane data collection form for Intervention reviews (RCTs only) (Figure 2; Figure 3). Discrepancies in data extraction were resolved by consensus during discussions with another review author (MWS or SF).
2.

Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
3.

Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
Assessment of risk of bias in included studies
Two review authors (LL and MAA) independently assessed the included studies for risk of bias using the Cochrane risk of bias assessment tool to assess allocation (random sequence generation and allocation concealment), blinding of participants and personnel, blinding of outcome assessors, incomplete outcome data, selective reporting, and other bias (http://handbook.cochrane.org). Disagreements were resolved by discussion or by a third review author (MWS or SF).
For each trial, it was determined whether adequate allocation concealment was described, and the trial was classed as being at low risk of bias if this was the case. If it was not the case, or if it was unclear how allocation concealment was achieved, the trial was classed as being at high risk or unclear risk, respectively. For each trial, we determined whether an acceptable method of sequence generation was described within the text (e.g. by stating that a computer‐generated randomisation list had been used). If this was the case, again the trial was classed as being at low risk in this respect. Similarly, if this was unclear, the trial was classed as having unclear risk of bias. We determined who was blinded in each trial. If participants and medical staff in the trial were blinded to allocation, the trial was at low risk. If this was not stated or if it was clear that this was not the case, the trial was again classed as having unclear risk or high risk of bias, respectively. Finally, selective reporting is an important issue in this review and is an important contributor to reporting bias, with only a minority of trials reporting on the primary outcome of live birth. Each trial that reported live birth was classed as low risk unless it did not report clinical pregnancy; in that case, it was reported as high risk. Each trial that did not report live birth was classed as high risk. Study authors were contacted if risks of bias were unclear to support the assessment
Measures of treatment effect
All outcomes were dichotomous, and results were expressed for each trial as an odds ratio (OR) with 95% confidence interval (CI); P values were calculated.
Unit of analysis issues
The primary analysis was per woman randomised. Data that did not allow valid analysis (e.g. 'per cycle' data) were not pooled. Multiple live births (e.g. twins, triplets) were counted as one live birth event.
Dealing with missing data
Attempts were made to obtain additional information on trial methods, actual original trial data, or both, by contacting the principal authors of the trials. Reminders were sent (when necessary) to study authors if no reply had been received four weeks after the initial request. Only available data were analysed, and no imputation of data was undertaken.
Assessment of heterogeneity
Consideration of the clinical and methodological characteristics of included studies was undertaken to ascertain if they were sufficiently similar for meta‐analysis to provide a clinically meaningful result. Heterogeneity between the results of different trials was examined using the I² statistic. Statistical heterogeneity was deemed significant if the P value was ≤ 0.1, that is, an indication of greater variation than would be expected by chance. I² values were also examined, and higher values (> 40%) were taken to indicate high heterogeneity (Higgins 2019).
Assessment of reporting biases
In view of the difficulty of detecting and correcting for publication bias and other reporting biases, review authors aimed to minimise their potential impact by ensuring a comprehensive search for eligible studies, and by staying alert for duplication of data. If 10 or more studies were included in an analysis, we planned to use a funnel plot to explore the possibility of small‐study effects (a tendency for estimates of the intervention effect to be more beneficial in smaller studies). Asymmetry can be found in funnel plots, especially when high heterogeneity is noted. Asymmetry detected in a funnel plot would probably be due to true heterogeneity (Stuck 1998).
Data synthesis
Studies were combined via meta‐analysis using a fixed‐effect model for AH versus no AH with RevMan 5.4 software (RevMan 2020). An increase in the odds of a particular outcome was displayed graphically in the meta‐analyses to the right of the centre‐line, and a decrease in the odds of an outcome was displayed to the left of the centre‐line.
Subgroup analysis and investigation of heterogeneity
The following subgroup analyses were undertaken for the 2012 and 2020 updates.
Number of attempts: first or repeat attempt at assisted conception.
Mode of assisted conception: IVF or ICSI.
Method of assisted hatching: chemical, laser, or mechanical.
Prognosis of woman: good or poor.
Extent of AH: thinning, breaching, complete removal of zona pellucida.
Type of embryo: fresh or frozen embryo transfer (frozen embryo transfer included thawed cryopreserved and vitrified‐warm embryo).
Sensitivity analysis
We performed sensitivity analysis to examine the stability of results for our primary outcomes and for clinical pregnancy, in relation to:
adequacy of allocation concealment, by removing trials with unclear or inadequate allocation concealment; and
adequacy of the randomisation process, by removing trials for which the method of randomisation was unclear.
Summary of findings and assessment of the certainty of the evidence
We prepared a Summary of findings table using GRADEpro and Cochrane methods (Higgins 2011; GRADEpro GDT 2015).This table evaluated the overall quality of the body of evidence for the main review outcomes (live birth, multiple pregnancy, clinical pregnancy and miscarriage) for the main review comparison (assisted hatching versus no assisted hatching). We assessed the quality of the evidence using GRADE criteria: risk of bias, consistency of effect, imprecision, indirectness and publication bias). Judgements about evidence quality (high, moderate, low or very low) were be made by two review authors working independently (LL and MAA), with disagreements resolved by discussion. Judgements were justified, documented, and incorporated into reporting of results for each outcome. We planned to extract study data, format our comparisons in data tables and prepare a summary of findings table before writing the results and conclusions of our review.
Results
Description of studies
Results of the search
In our updated search in 2020, we identified 284 discrete records, of which 22 were examined in full text as they were potentially eligible. Twelve were excluded in 2020 as they did not meet our inclusion criteria, one was identified as a subgroup analysis of an included study (Desai 2013; Hagemann 2010), and one is awaiting classification (Elnahas A 2018); therefore eight were eligible for inclusion. The previous version of the review included 31 studies and excluded 58 studies, so altogether there are now 39 included studies and 70 excluded studies (Figure 1). Five ongoing trials are registered at http://www.clinicaltrials.gov (a service of the US National Institutes of Health) and at http://www.who.int/trialsearch/Default.aspx (The World Health Organization International Trials Registry Platform search portal) (see Characteristics of ongoing studies).
All included trials were described in published reports (full papers or abstracts). One included study was published in Spanish (González‐Ortega 2015), and one excluded study was published in Chinese (Lu 2016). In total, the studies included in our review recruited a total of 7249 women undergoing IVF or ICSI: 3688 women in the assisted hatching groups and 3561 women in the control groups.
Included studies
Study design and setting
We included a total of 39 studies, including eight new studies for this update (Abulsoud 2019; Elnahas 2017; González‐Ortega 2015; Nada 2018; Razi 2013; Safari 2017; Shi 2016; Wan 2014) (Figure 1).
The trials were carried out in 17 different countries: USA (Carter 2003; Cohen 1992; Hagemann 2010; Hurst 1998; Laffoon 1999; Lanzendorf 1998; Sagoskin 2007; Tucker 1993; Tucker 1996), Italy (Antinori 1999; Nagy 1999), Belgium (Hellebaut 1996), Turkey (Balaban 2006; Ciray 2005; Isik 2000; Isiklar 1999; Kutlu 2010), Brazil (Baruffi 2000; Petersen 2005), Australia (Ryan 1997), Germany (Jelinkova 2002), China (Fang 2010; Ge 2008; Ng 2005; Shi 2016; Wan 2014), Japan (Utsunomiya 1998), Israel (Rufas‐Sapir 2004; Stein 1995), Iran (Razi 2013; Safari 2017; Valojerdi 2010), Canada (Balakier 2009), Egypt (Abulsoud 2019; Elhelw 2005; Elnahas 2017; Nada 2018), and Mexico (González‐Ortega 2015). One European multi‐centre study involved women at IVF centres in Switzerland, France, Germany, and Spain (Germond 2004).
Participants
The age of participants ranged from 27 to 42 years (when reported). Some trials had subgroup data within them (e.g. Elnahas 2017; Ge 2008; Germond 2004; Kutlu 2010; Rufas‐Sapir 2004; Shi 2016; Stein 1995; and Tucker 1996 presented pregnancy for different age groups), whilst other studies included only women 35 years of age and older (e.g. González‐Ortega 2015; Lanzendorf 1998) or younger than 35 years old (Antinori 1999; Hurst 1998). Other studies included women of other specific age groups, for example, 38 years of age or younger (Balakier 2009; Hagemann 2010). Subgroup analysis based on age of the women has not been achievable, as studies did not categorise age groups in a universal way.
Fourteen trials included women with a poor prognosis (Abulsoud 2019; Antinori 1999; Cohen 1992; Elhelw 2005; Ge 2008; Germond 2004; González‐Ortega 2015; Jelinkova 2002; Kutlu 2010; Lanzendorf 1998; Petersen 2005; Rufas‐Sapir 2004; Stein 1995; Utsunomiya 1998). Fourteen trials included women with a good prognosis (Antinori 1999; Balakier 2009; Carter 2003; Ciray 2005; Cohen 1992; Elnahas 2017; Ge 2008; Hellebaut 1996; Hurst 1998; Kutlu 2010; Laffoon 1999; Nada 2018; Sagoskin 2007; Tucker 1993), and the remaining studies did not provide information.
Interventions
Twelve trials were repeat cycles, and eight included women undergoing their first assisted reproductive technology (ART) cycle; 19 trials did not report whether the treatment cycle was a first or repeat cycle or were mixed cycles. A total of 12 trials included women undergoing ICSI alone, 15 were IVF only, and the rest were unstated or included mixed ICSI and IVF cycles. Twenty‐eight trials involved transfer of fresh embryos exclusively, nine involved frozen or vitrified‐warmed embryos only, two used fresh and frozen embryos (Germond 2004; Ge 2008), and one study used a combination of fresh and frozen embryos (Ryan 1997).
Eleven trials employed chemical means for assisted hatching, five employed mechanical means, and 23 employed laser.
Seventeen trials utilised a breach of the zona pellucida with a hole (Antinori 1999; Cohen 1992; Germond 2004; Hagemann 2010; Hellebaut 1996; Hurst 1998; Isiklar 1999; Laffoon 1999; Lanzendorf 1998; Nagy 1999; Razi 2013; Rufas‐Sapir 2004; Ryan 1997; Sagoskin 2007; Stein 1995; Tucker 1996; Wan 2014), a further 17 utilised non‐breach thinning (Abulsoud 2019; Balaban 2006; Balakier 2009; Baruffi 2000; Ciray 2005; Elhelw 2005; Elnahas 2017; Ge 2008; Kutlu 2010; Nada 2018; Ng 2005; Petersen 2005; Safari 2017; Shi 2016; Tucker 1996; Utsunomiya 1998; Valojerdi 2010), and two performed complete zona removal (Isik 2000; Jelinkova 2002). For two studies, this was unknown (Carter 2003; González‐Ortega 2015), whilst another study used a new method of AH whereby the zona pellucida was expanding mechanically (Fang 2010). Three trials reported the thickness of the zona pellucida (in each case, choosing zona thickness > 12 µm as an inclusion criterion).
Twenty‐five trials reported the interval between AH and embryo transfer (20 trials reported less than four hours; three trials, four to eight hours; and two, longer than eight hours).
Blastocyst transfer occurred in four trials (Isik 2000; Isiklar 1999; Laffoon 1999; Wan 2014), one of which involved complete zona removal (Isik 2000).
Outcomes
Outcome measures utilised for this review were reported by varying numbers of trials.
14 trials reported live birth rate.
18 trials reported multiple pregnancy rate.
39 trials reported clinical pregnancy rate.
17 trials reported miscarriages.
6 trials reported monozygotic twinning.
5 trials reported ectopic pregnancy.
3 trials reported congenital or chromosomal abnormalities, or both.
3 trials reported embryo damage.
No trials reported in vitro blastocyst development post AH.
Further details about the included trials are provided in the Characteristics of included studies table and in Table 2 and Table 3.
1. Mean age of participants in assisted hatching and control groups.
| Study | AH n, mean age (SD) | Control n, mean age (SD) | OR for clinical pregnancy |
| Abulsoud 2019 | 65, 39.2 (1.2) | 65, 39.5 (1.2) | 2.50 (1.14 to 5.49) |
| Antinori 1999: first IVF | 73, 37.5 | 69, 36.0 | 1.27 (0.70 to 2.32) |
| Antinori 1999: repeat IVF | 96, 27.5 | 103, 27 | 1.86 (0.81 to 4.25) |
| Balaban 2006 | 183, 32.4 (3.3) | 183, 32.7 (3.1) | 1.85 (1.19 to 2.86) |
| Balakier 2009 | 45, 32.5 (3.8) | 39, 33.8 (3.2) | 0.64 (0.27 to 1.55) |
| Baruffi 2000 | 51, 31.8 (3.6) | 52, 31.4 (3.6) | 0.74 (0.33 to 1.65) |
| Carter 2003 | 121, 34 (3.3) | 82, 34 (3.2) | 0.95 (0.54 to 1.67) |
| Ciray 2005 | 60, 33.1 (4.2) | 30, 34.0 (3.7) | 0.62 (0.26 to 1.49) |
| Cohen 1992: FSH < 15 | 69, 36.50 (3.30) | 68, 36.70 (3.70) | 2.11 (1.18 to 3.77) |
| Cohen 1992: poor prognosis | 80, 36.7 (4.3) | 83, 35.3 (4.2) | 1.30 (0.66 to 2.55) |
| Cohen 1992: FSH > 15 | not stated | not stated | 1.30 (0.66 to 2.55) |
| Elhelw 2005 | not stated | not stated | 1.77 (0.52 to 6.01) |
| Elnahas 2017 | 80, 31.0 (4.7) | 80, 31.7 (4.9) | 1.58 (0.81 to 3.08) |
| Fang 2010 | 61, 32.3 (3.4) | 64, 32.1 (3.6) | 2.37 (1.07 to 5.28) |
| Ge 2008: fresh embryo | 387, 31.08 (4.68) | 373, 30.44 (4.15) | 0.99 (0.74 to 1.32) |
| Ge 2008: frozen embryo | 100, 31.84 (3.85) | 100, 30.66 (4.42) | 2.05 (0.99 to 4.22) |
| Germond 2004: first cycle of frozen‐thawed embryos | 62, 32.8 (4.2) | 53, 32.6 (3.8) | 0.09 (0.01 to 0.76) |
| Germond 2004: poor prognosis, first cycle of fresh embryos | 22, 39.3 (2.9) | 21, 38.3 (3.4) | 0.51 (0.10 to 2.45) |
| González‐Ortega 2015 | 154, 38.5 (2.8) | 149, 37.3 (4.2) | 2.71 (1.62 to 4.56) |
| Hagemann 2010 | 59, 32.1 (3.0) | 62, 31.2 (3.5) | 0.81 (0.37 to 1.76) |
| Hellebaut 1996 | 60, 30.9 (4.3) | 60, 30.8 (3.9) | 1.15 (0.55 to 2.43) |
| Hurst 1998 | 13, 30.0 (0.9) | 7, 30.0 (0.8) | 0.40 (0.06 to 2.89) |
| Isik 2000 | 24, 30.5 (5.2) | 22, 29.1 (3.6) | 2.0 (0.62 to 6.49) |
| Isiklar 1999 | not stated | not stated | 3.20 (0.91 to 11.27) |
| Jelinkova 2002 | 128, 32.3 (4.24) | 129, 32.1 (3.16) | 1.86 (1.12 to 3.10) |
| Kutlu 2010: good prognosis | 73, 29.9 (2.9) | 66, 28.9 (3.4) | 1.06 (0.54 to 2.08) |
| Kutlu 2010: poor prognosis | 58, 38.0 (2.3) | 55, 37.4 (2.4) | 1.23 (0.58 to 2.60) |
| Laffoon 1999 | not stated | not stated | 0.85 (0.28 to 2.58) |
| Lanzendorf 1998 | 41, 38.30 (0.31) | 48, 38.50 (0.26) | 0.90 (0.38 to 2.10) |
| Nada 2018 | 158, 31.3 (4.1) | 150, 32.6 (2.4) | 1.79 (1.05 to 3.07) |
| Nagy 1999 | 20, 32.0 (4.0) | 20, 31.4 (3.7) | 8.0 (1.44 to 44.3) |
| Ng 2005 | 80, 34.0 (range 25 to 40) | 80, 34.0 (range 26 to 40) | 0.81 (0.33 to 2.00) |
| Petersen 2005: 1 previous implantation failure | 35, 34.6 (4.6) | 35, 34.1 (5.3) | 1.15 (0.41 to 3.19) |
| Petersen 2005: several previous implantation failures | 40, 35.7 (3.8) | 40, 35.3 (5.1) | 4.11 (1.04 to 16.29) |
| Razi 2013 | 90, 32.9 (0.5) | 92, 31.6 (0.4) | 0.7 (0.3 to 1.6) |
| Rufas‐Sapir 2004 | not stated | not stated | 0.72 (0.38 to 1.36) |
| Ryan 1997 | not stated | not stated | 0.74 (0.35 to 1.59) |
| Safari 2017 | 30, 30.6 (5.6) | 32, 29.2 (5.3) | 0.58 (0.19 to 1.78) |
| Sagoskin 2007 | 118, 34.0 (3.3) | 81, 34.0 (3.2) | 0.94 (0.53 to1.65) |
| Shi 2016 | 82, 37.2 (2.22) | 96, 36.97 (1.96) | 0.65 (0.36 to 1.18) |
| Stein 1995 | not stated | not stated | 1.54 (0.67 to 3.54) |
| Tucker 1993 | 110, 34.1 (4.8) | 108, 34.2 (4.1) | 1.37 (0.79 to 2.35) |
| Tucker 1996 | 50, 35.3 (4.2) | 50, 33.5 (4.3) | 0.74 (0.35 to 1.59) |
| Utsunomiya 1998 | not stated | not stated | 1.36 (0.32 to 5.73) |
| Valojerdi 2010 | 200, 30.86 (5.82) | 200, 29.85 (5.14) | 0.53 (0.35 to 0.80) |
| Wan 2014 | 96, 33.1 (3.7) | 102, 32.6 (3.4) | 1.91 (1.08 to 3.38) |
2. Prognostic factors in included trials.
| Study ID | Balanced age between groups | Balances no. of embryos transferred | Prognosis: poor/good | FSH levels | Blastocyst transfer | Complete/partial AH | Frozen cycles |
| Abulsoud 2019 | Yes | Yes | Poor | No data | No | Thinning | Fresh |
| Antinori 1999 | AH mean 1.5 years older | Yes | Good and poor subgroups | No data | No | Complete hole | Not stated |
| Balaban 2006 | Yes | Yes | Unselected | < 10 | No | Thinning | Frozen |
| Balakier 2009 | AH mean 1.3 years older | Yes | Good | < 10 | No | Thinning | Fresh |
| Baruffi 2000 | Yes | Yes | Good | No data | No | Thinning | Fresh |
| Carter 2003 | Yes | Yes | Good | < 10 | No | Not stated | Fresh |
| Ciray 2005 | Yes | Yes | Good | < 15 | No | Thinning | Fresh |
| Cohen 1992 | Yes | Yes | Unstated | ≤ 15 and > 15 subgroups | No | Complete hole | Fresh |
| Elhelw 2005 | Yes | No data | Poor | No data | No | Thinning | Frozen |
| Elnahas 2017 | Yes | No data | Good | No data | No | Thinning | Frozen |
| Fang 2010 | Yes | Yes | Not stated | No data | No | Mechanical expansion | Frozen thawed |
| Ge 2008 | Yes | Yes | Mixed | No data | No | Thinning | Fresh and frozen subgroups |
| Germond 2004 | Yes | Yes | Mixed, in subgroups | Between 3 and 12 | No | Complete hole | Fresh and frozen subgroups |
| González‐Ortega 2015 | Yes | Yes | Poor | > 12 | No | Partial | Fresh |
| Hagemann 2010 | Mean age data given only for combined cycles 1 and 2 | Yes | Under 38 years, > 2 previously failed cycles, ZP thickness > 13 micrometers | No data | No | 20 micrometer diameter opening | Fresh |
| Hellebaut 1996 | Yes | Yes | Good | No data | No | Complete hole | Fresh |
| Hurst 1998 | Yes | Yes | Good | < 10 | No | Complete hole | Fresh |
| Isik 2000 | AH mean 1.4 years older | Yes | Unstated | < 10 | Yes | Removal complete | Fresh |
| Isiklar 1999 | No data | Yes | Unstated | No data | Yes | Complete hole | Fresh |
| Jelinkova 2002 | Yes | Yes | Poor | No data | Yes | Removal complete | Fresh |
| Kutlu 2010 | Yes | Yes | Good and poor subgroups | No data | No | Complete hole | Fresh |
| Laffoon 1999 | No data | No data | Good | No data | No | Complete hole | Fresh |
| Lanzendorf 1998 | No | Yes | Poor | No data | No | Complete hole | Fresh |
| Nada 2018 | Yes | Yes | Good | AH 5.4 ± 1.3 No AH 6.0 ± 1.1 | No | Thinning | Fresh |
| Nagy 1999 | Yes | Yes | Unstated | No data | No | Thinning | Frozen‐thaw cycle |
| Ng 2005 | Yes | Higher proportion of controls received 3 embryos | Unstated | < 11 | No | Thinning | Frozen‐thaw cycle |
| Petersen 2005 | Yes | Yes | Poor | No data | No | Thinning | Fresh |
| Razi 2013 | Yes | Yes | Unstated | No data | No | Partial | Fresh |
| Rufas‐Sapir 2004 | No data | Yes | Poor | No data | No | Complete hole | Fresh |
| Ryan 1997 | No data | No data | Unstated | No data | No | Complete hole | Both |
| Safari 2017 | Yes | Yes | Unstated | AH 6.4 ± 2.3 No AH 5.6 ± 2.1 |
No | Thinning | Frozen |
| Sagoskin 2007 | Yes | Yes | Good | < 10 | No | Hole | Fresh |
| Shi 2016 | Yes | Yes | Advanced maternal age | < 10 | No | Zona Thinning | Fresh |
| Stein 1995 | No data | No data | Poor | No data | No | Complete hole | Fresh |
| Tucker 1993 | Yes | Yes | Good | < 15 | No | Thinning | Fresh |
| Tucker 1996 | AH mean 1.8 years older | Yes | Not stated | No data | No | Complete hole | Fresh |
| Utsunomiya 1998 | No data | No data | Poor | No data | No | Thinning | Fresh |
| Valojerdi 2010 | Yes | Yes | Not stated | No data | No | Partially thinned | Vitrified‐warmed embryo |
| Wan 2014 | Yes | Yes | Previously unsuccessful 1 fresh cycle | No data | Yes | Partial | Vitrified‐warmed embryo |
AH: assisted hatching. ET: embryo transfer. FSH: follicle‐stimulating hormone.
Excluded studies
We excluded 72 studies from the review (see Characteristics of excluded studies). Reasons for exclusion included inadequate method of randomisation, no per woman data, inadequate reporting of clinical pregnancy, no control group, inclusion of women with donor gametes, and, in the remainder, studies were not randomised and two studies were found to be retrospective studies on close examination of the text. Conference abstracts were excluded only when further details were asked from study authors and no response was provided, and we could not utilise available data.
Risk of bias in included studies
The overall methodological quality of the included trials was considered sub‐optimal, largely due to risk of bias in the included studies. Further details of the trials' risk of bias can be found in the Characteristics of included studies table. Summaries of risk of bias for all included studies are presented in Figure 2 and Figure 3.
Allocation
Random sequence generation
All 39 trials stated that randomisation had occurred. Regarding random sequence generation, 23 studies were at low risk of this bias, 15 had unclear risk, and one was at high risk (Hagemann 2010).
Allocation concealment
Three studies were at low risk of selection bias related to allocation concealment (Abulsoud 2019; Elnahas 2017; González‐Ortega 2015), and 36 studies had unclear risk.
Blinding
Although blinding was unlikely to influence findings for the primary review outcome (live birth), eight trials employed double blinding with both the woman and the outcome assessor unaware of the allocation (Balakier 2009; Cohen 1992; Ge 2008; González‐Ortega 2015; Hagemann 2010; Lanzendorf 1998; Ng 2005; Razi 2013). In 28 studies, it is unclear if blinding was used or who was blinded (participant or assessor), and in the remaining three studies, no blinding was reported (Ciray 2005; Hellebaut 1996; Shi 2016).
Incomplete outcome data
Ideally, studies should randomise women on the day of assessment of embryos for suitability for embryo transfer. Two studies we assessed as high risk related to incomplete outcome data (Nada 2018; Safari 2017). One excluded participants after randomisation due to cycle cancellation but gave no reason for why cycles were cancelled, and one randomised 32 participants into each trial arm but reported outcomes for only 30 participants. A total of 16 studies were at low risk of bias related to incomplete outcome data, and 21 studies had unclear risk.
Selective reporting
All pre‐specified outcomes were reported within the outcomes of all studies. Many studies did not report live birth, multiple pregnancy, or miscarriage outcomes.
Other potential sources of bias
Age groups were matched in trials with similar means in the AH and control groups.
Thirty‐two trials were reported as full published papers. Seven trials were published in conference abstract form only (Antinori 1999; Carter 2003; Elhelw 2005; Laffoon 1999; Rufas‐Sapir 2004; Ryan 1997; Utsunomiya 1998).
No funding bias or any other conflicts of interests were noted in the included studies.
Effects of interventions
See: Table 1
Assisted hatching compared to no assisted hatching
Primary outcomes
Live birth per woman
Only 14 of the 39 trials reported live birth rate. We are uncertain of the effect of AH on live birth rate when compared to no AH (odds ratio (OR) 1.09, 95% confidence interval (CI) 0.92 to 1.29; 14 RCTs, N = 2849; I² = 20%; low‐quality evidence; Analysis 1.1; Figure 4).
1.1. Analysis.

Comparison 1: Live birth: assisted hatching compared with no assisted hatching, Outcome 1: Live birth per woman randomised
4.

Forest plot of comparison: 1 Live birth rate, outcome: 1.1 Live birth per woman randomised.
Subgroup analysis
Number of attempts ‐ first or repeat attempt at ART: no evidence indicates that the effect of assisted hatching differed between those undergoing their first or subsequent attempts (P = 0.23). We are uncertain of the effect of AH on the live birth rate in women in their first attempt at ART (OR 0.78, 95% CI 0.48 to 1.28; 3 RCTs, n = 380; I² = 15%) or in subsequent attempts at ART (OR 1.40, 95% CI 0.62 to 3.13; 1 RCT only) when compared to no AH (Analysis 1.2)
Mode of conception ‐ assisted conception procedure (IVF/ICSI): no evidence shows that the effect of assisted hatching differed between those undergoing IVF and those undergoing ICSI (P = 0.20). For couples undergoing ICSI, AH may improve slightly the live birth rate when compared to no AH (OR 1.54, 95% CI 1.02 to 2.33; 3 RCTs, n = 640; I² = 0%). For couples undergoing IVF, there may be little to no difference in live birth rate with AH compared to no AH (OR 1.00, 95% CI 0.60 to 1.68; 3 RCTs, n = 241; I² = 58%) (Analysis 1.3)
Method of assisted hatching: no evidence suggests that the effect of assisted hatching differed between chemical and laser methods (P = 0.80). We are uncertain of the effect of chemical AH or laser AH on live birth rate when compared to no AH (OR 1.13, 95% CI 0.74 to 1.74; 4 RCTs, n = 366; I² = 5%; and OR 1.07, 95% CI 0.89 to 1.28; 10 RCTs, n = 2473; I² = 24%, respectively). None of the trials that employed mechanical forms of AH reported on live births (Analysis 1.4)
Prognosis: no evidence shows that the effect of assisted hatching differed between women in poor prognosis groups and women in good prognosis groups (P = 0.12). We are uncertain of the effect of AH on live birth rate in women with a good prognosis compared with no AH (OR 1.03, 95% CI 0.83 to 1.28; 6 RCTs, n = 1495; I² = 23%) and in women with a poor prognosis who underwent AH compared to no AH (OR 1.46, 95% CI 0.99 to 2.15; 4 RCTs, n = 576; I² = 0%) (Analysis 1.5)
Extent of zona manipulation: no evidence indicates that the effect of assisted hatching differed between thinning of zona and breaching the zona with a hole (P = 0.64). We are uncertain of the effect of AH with thinning of the zona pellucida on live birth rate compared with no AH and AH with breech of the zona pellucida on live birth rate compared with no AH (OR 1.06, 95% CI 0.86 to 1.30; 6 RCTs; I² = 31%; and OR 1.15, 95% CI 0.87 to 1.51; 8 RCTs, n = 1107; I² = 21%, respectively) (Analysis 1.6)
Type of embryo ‐ fresh or frozen embryo: no evidence shows that the effect of assisted hatching differed between fresh and frozen embryos (P = 0.35). We are uncertain of the effect of AH on live birth rate in women who had fresh embryo transfer compared with the no AH group (OR 1.16, 95% CI 0.94 to 1.44; 11 RCTs, N = 1669; I² = 16%). Only one study reported use of frozen embryos (Safari 2017), and two studies reported use of fresh and frozen embryos (Ge 2008; Germond 2004)
1.2. Analysis.

Comparison 1: Live birth: assisted hatching compared with no assisted hatching, Outcome 2: First or repeat attempt
1.3. Analysis.

Comparison 1: Live birth: assisted hatching compared with no assisted hatching, Outcome 3: Conception mode
1.4. Analysis.

Comparison 1: Live birth: assisted hatching compared with no assisted hatching, Outcome 4: Hatching method
1.5. Analysis.

Comparison 1: Live birth: assisted hatching compared with no assisted hatching, Outcome 5: Prognosis
1.6. Analysis.

Comparison 1: Live birth: assisted hatching compared with no assisted hatching, Outcome 6: Live birth rate by extent of assisted hatching
Sensitivity analysis
Allocation concealment: no trials were assessed as low risk
Method of randomisation: 11 trials stated the method of randomisation (Balakier 2009; Cohen 1992; Ge 2008; Germond 2004; Hellebaut 1996; Hurst 1998; Lanzendorf 1998; Nada 2018; Petersen 2005; Razi 2013; Sagoskin 2007). Analysis of the data from these trials suggests that there was no improvement in live birth rate between AH groups and control groups (OR 1.10, 95% CI 0.92 to 1.32; n = 2411; I² = 11%)
Other analyses
We used a funnel plot to assess publication bias and small‐study effects. The funnel plot shows only some mild asymmetry (Figure 5). The funnel plot is likely to be detecting small‐study effects.
5.

Funnel plot of comparison: 1 Live birth: assisted hatching compared with no assisted hatching, outcome: 1.1 Live birth per woman randomised.
Multiple pregnancy per woman
Eighteen of the 39 trials reported on multiple pregnancy. AH may lead to a higher multiple pregnancy rate compared to no AH (OR 1.38, 95% CI 1.13 to 1.68; 18 RCTs, n = 4308; I² = 48%; low‐quality evidence; Analysis 2.1; Figure 6).
2.1. Analysis.

Comparison 2: Multiple pregnancy: assisted hatching compared with no assisted hatching, Outcome 1: Multiple pregnancy rate per woman randomised
6.

Forest plot of comparison: 4 Multiple pregnancy rate, outcome: 4.1 Multiple pregnancy rate per woman randomised.
Subgroup analysis
Number of attempts ‐ first attempt or repeat attempt at ART: no evidence indicates that the effect of AH differed between those undergoing their first attempt and those undergoing subsequent attempts (P = 0.28). We are uncertain of the effect of AH on the multiple pregnancy rate in women who underwent AH compared with no AH in their first attempt at ART (OR 0.73, 95% CI 0.31 to 1.72; 4 RCTs, n = 654; I² = 0%) or in subsequent attempts at ART (OR 1.25, 95% CI 0.80 to 1.94; 5 RCTs, n = 1068; I² = 25%) (Analysis 2.2)
Mode of conception‐ assisted conception procedure (IVF/ICSI): no evidence shows that the effect of AH differed between those undergoing IVF and those undergoing ICSI treatment (P = 0.21). For couples undergoing ICSI, AH may lead to slightly higher multiple pregnancy rates when compared to no AH (OR 3.09, 95% CI 1.57 to 6.08; 3 RCTs, n = 573; I² = 52%). For couples undergoing IVF, AH may lead to slightly higher multiple pregnancy rates when compared to no AH (OR 1.87, 95% CI 1.28 to 2.72; 6 RCTs, n = 1126; I² = 36%) (Analysis 2.3)
Method of assisted hatching: evidence suggests that the effect of AH differed between chemical, laser, and mechanical methods (P = 0.08). We are uncertain of the effect of chemical AH on the multiple pregnancy rate when compared to no AH (OR 1.55, 95% CI 0.98 to 2.47; 4 RCTs, n = 534; I² = 10%). Both laser and mechanical AH may lead to a slightly higher multiple pregnancy rate when compared to no AH (OR 1.29, 95% CI 1.03 to 1.61; 4 RCTs, n = 534; I² = 50%; and OR 8.33, 95% CI 1.56‐44.64; 1 RCT only, n = 44, respectively) (Analysis 2.4)
Prognosis: some evidence suggests that the effect of AH differed between women in poor prognosis groups and women in good prognosis groups (P = 0.02). We are uncertain of the effect of AH on the multiple pregnancy rate in women with a good prognosis compared with no AH (OR 1.08, 95% CI 0.81 to 1.44; 6 RCTs, n = 1569; I² = 0%). In women with a poor prognosis, AH may lead to a slightly higher multiple pregnancy rate when compared to no AH (OR 1.95, 95% CI 1.27 to 3.00; 6 RCTs, n = 1186; I² = 0%) (Analysis 2.5)
Extent of zona manipulation: no evidence indicates that the effect of AH differed between thinning of zona and breaching of zona with a hole (P = 0.65). AH may lead to a slightly higher multiple pregnancy rate in women who had assisted hatching with thinning of the zona pellucida compared with no AH (OR 1.34, 95% CI 1.02 to 1.76; 6 RCTs, n = 2148; I² = 71%) and assisted hatching with breech of the zona pellucida by a hole only compared with no AH (OR 1.51, 95% CI 1.08 to 2.11; 9 RCTs, n = 1629; I² = 35%). Only one study reported complete removal of the zona pellucida (Isik 2000) (Analysis 2.6)
Type of embryo ‐ fresh or frozen embryo: no evidence suggests that the effect of assisted hatching differed between fresh and frozen embryos (P = 0.46). We are uncertain of the affect of AH on the multiple pregnancy rate in women who had fresh embryo transfer compared with no AH (OR 1.30, 95% CI 0.98 to 1.73; 13 RCTs, n = 2264; I² = 0%) and in women who had frozen embryo transfer compared with no AH (OR 1.60, 95% CI 1.00 to 2.55; 3 RCTs, n = 926; I² = 88%) (Analysis 2.7)
Multiple pregnancy per pregnancy: overall, AH may lead to a higher multiple pregnancy rate compared to control (OR 1.37, 95% CI 1.09 to 1.72; 17 trials, n = 1598; I² = 25%) (Analysis 2.8)
2.2. Analysis.

Comparison 2: Multiple pregnancy: assisted hatching compared with no assisted hatching, Outcome 2: First or repeat attempt
2.3. Analysis.

Comparison 2: Multiple pregnancy: assisted hatching compared with no assisted hatching, Outcome 3: Conception mode
2.4. Analysis.

Comparison 2: Multiple pregnancy: assisted hatching compared with no assisted hatching, Outcome 4: Hatching method
2.5. Analysis.

Comparison 2: Multiple pregnancy: assisted hatching compared with no assisted hatching, Outcome 5: Prognosis
2.6. Analysis.

Comparison 2: Multiple pregnancy: assisted hatching compared with no assisted hatching, Outcome 6: Multiple pregnancy rate per woman grouped by extent of assisted hatching
2.7. Analysis.

Comparison 2: Multiple pregnancy: assisted hatching compared with no assisted hatching, Outcome 7: Fresh or frozen embryo transfer
2.8. Analysis.

Comparison 2: Multiple pregnancy: assisted hatching compared with no assisted hatching, Outcome 8: Multiple pregnancy per pregnancy
Sensitivity analysis
Allocation concealment: only one trial was assessed as low risk (González‐Ortega 2015)
Method of randomisation: 15 trials stated the method of randomisation (Balaban 2006; Balakier 2009; Carter 2003; Cohen 1992; Ge 2008; Germond 2004; González‐Ortega 2015; Hellebaut 1996; Isik 2000; Isiklar 1999; Lanzendorf 1998; Ng 2005; Razi 2013; Sagoskin 2007; Valojerdi 2010). Analysis of the data from these trials suggests that AH may lead to a high multiple pregnancy rate when compared to no AH (OR 1.37, 95% CI 1.11 to 1.69; n = 3597; I² = 53%)
Secondary outcomes
Clinical pregnancy rate per woman
Thirty‐nine trials reported clinical pregnancy data. AH may improve slightly the clinical pregnancy rate compared to no AH (OR 1.20, 95% CI 1.09 to 1.33; I² = 55%; low‐quality evidence; Analysis 3.1; Figure 7). Furthemore, the forest plots show high heterogeneity. When a random‐effects model is used, there may be little to no difference in clinical pregnancy rate among women who underwent AH compared with those given control (P = 0.04).
3.1. Analysis.

Comparison 3: Clinical pregnancy: assisted hatching compared with no assisted hatching, Outcome 1: Clinical pregnancy rate per woman randomised
7.

Forest plot of comparison: 2 Clinical pregnancy, outcome: 2.1 Clinical pregnancy rate per woman randomised.
Among the 14 trials reporting both clinical pregnancy and live births, analysis demonstrated that we are uncertain of the effect of AH on clinical pregnancy rate in women who underwent AH compared with those given the control (OR 1.07, 95% CI 0.92 to 1.25; I² = 45%) (Analysis 4.1).
4.1. Analysis.

Comparison 4: Clinical pregnancies in trials that reported live births: assisted hatching compared with no assisted hatching, Outcome 1: Clinical pregnancies in trials reporting live births
Subgroup analysis
Number of attempts ‐ first or repeat attempt at ART: some evidence suggests that the effect of AH differed between those undergoing their first attempt and those undergoing subsequent attempts (P < 0.00001; fixed model). When the random‐effects model is used, the effect is less pronounced (P = 0.0002). With the fixed‐effect model, there may be a slight decrease in the clinical pregnancy rate among women who underwent AH compared with no AH in their first attempt at ART (OR 0.74, 95% CI 0.56 to 0.98; 8 RCTs, n = 1010 women; I² = 9%). There may be slight improvement in clinical pregnancy rate among women who underwent AH compared to no AH in women undergoing repeat attempts at ART (OR 1.65, 95% CI 1.34 to 2.04; 11 RCTs, n = 1798; I² = 38%) (Analysis 3.2)
Mode of conception ‐ assisted conception procedure (IVF/ICSI): no evidence shows that the effect of AH differed between those undergoing IVF and those undergoing ICSI treatment (P = 0.62). For couples undergoing ICSI, AH may improve slightly the clinical pregnancy rate when compared to no AH (OR 1.40, 95% CI 1.14 to 1.71; 11 RCTs; n = 1825; I² = 30%). For couples undergoing IVF, AH may improve slightly the clinical pregnancy rate when compared to no AH (OR 1.31, 95% CI 1.10 to 1.55; 15 RCTs, n = 2460; I² = 28%) (Analysis 3.3)
Method of assisted hatching: no evidence indicates that the effect of AH differed between laser, chemical, and mechanical methods (P = 0.48) (Analysis 3.4). Chemical AH may improve slightly the clinical pregnancy rate when compared to no AH (OR 1.33, 95% CI 1.08 to 1.64; 11 RCTs, n = 1536; I² = 0%). Laser AH may improve slightly the clinical pregnancy rate when compared to no AH (OR 1.15, 95% CI 1.03 to 1.30; 23 RCTs, n = 5127; I² = 67%). We are uncertain of the effect of mechanical AH on the clinical pregnancy rate when compared to control (OR 1.30, 95% CI 0.89 to 1.88; 5 RCTs, n = 586; I² = 51%)
Prognosis: some evidence suggests that the effect of AH differed between women in poor prognosis groups and women in good prognosis groups (P = 0.0009; fixed‐effect model). When a random‐effects model is used, the effect is less pronounced (P = 0.005) than with the fixed‐effect model. In women with a good prognosis, we are uncertain of the effect of AH on the clinical pregnancy rate when compared with no AH (OR 1.10, 95% CI 0.94 to 1.29; 14 RCTs, n = 2721; I² = 0%). In women with a poor prognosis, AH may improve slightly the clinical pregnancy rate when compared with no AH (OR 1.68, 95% CI 1.38 to 2.04; 14 RCTs, n = 2108; I² = 25%) (Analysis 3.5)
Extent of zona manipulation: some evidence shows that the effect of AH differed depending upon the extent of assisted hatching (P = 0.04). In women who had AH with thinning of the zona pellucida, we are uncertain of the effect on the clinical pregnancy rate when compared to no AH (OR 1.10, 95% CI 0.96 to 1.26; 17 RCTs, n = 3774; I² = 57%). In women who had AH with breech of the zona pellucida by a hole only, we are uncertain of the effect of AH on clinical pregnancy rate when compared with control (OR 1.17, 95% CI 0.98 to 1.39; 17 RCTs, n = 2543; I² = 46%). Only two studies used AH with complete removal of the zona pellucida (Isik 2000; Jelinkova 2002), and only one study used AH with expansion of the zona pellucida (Fang 2010) (Analysis 3.6)
Type of embryos ‐ fresh or frozen embryo: in fresh embryo groups: no evidence indicates that the effect of AH differed between fresh and frozen embryos (P = 0.58). AH may improve slightly the clinical pregnancy rate in women who had fresh embryo transfer when compared with no AH (OR 1.23, 95% CI 1.10 to 1.38; 30 RCTs, n = 5349; I² = 41%). We are uncertain of the effect of AH on the clinical pregnancy rate in women who had frozen embryo transfer when compared to no AH (OR 1.15, 95% CI 0.93 to 1.42; 10 RCTs, n = 1700; I² = 76%) (Analysis 3.7)
3.2. Analysis.

Comparison 3: Clinical pregnancy: assisted hatching compared with no assisted hatching, Outcome 2: First or repeat attempt
3.3. Analysis.

Comparison 3: Clinical pregnancy: assisted hatching compared with no assisted hatching, Outcome 3: Conception mode
3.4. Analysis.

Comparison 3: Clinical pregnancy: assisted hatching compared with no assisted hatching, Outcome 4: Hatching method
3.5. Analysis.

Comparison 3: Clinical pregnancy: assisted hatching compared with no assisted hatching, Outcome 5: Prognosis
3.6. Analysis.

Comparison 3: Clinical pregnancy: assisted hatching compared with no assisted hatching, Outcome 6: Extent of assisted hatching
3.7. Analysis.

Comparison 3: Clinical pregnancy: assisted hatching compared with no assisted hatching, Outcome 7: Fresh and frozen embryo transfer
Sensitivity analysis
Allocation concealment: limiting the analysis to trials that reported allocation concealment left only three trials (Abulsoud 2019; Elnahas 2017; González‐Ortega 2015). Analysis of the data from these trials suggests that there was improvement in the clinical pregnancy rate in the AH group when compared to the no AH group (OR 2.28, 95% CI 1.59 to 3.27; n = 593; I² = 0%)
Method of randomisation: 23 trials stated an acceptable method of randomisation. Analysis of the data from these trials suggests that there was improvement in the clinical pregnancy rate in the AH group compared to the no AH group (OR 1.16, 95% CI 1.03 to 1.30; n = 5050; I² = 63%)
Other analyses
We used a funnel plot to assess publication bias and small‐study effects. The funnel plots are symmetrical (Figure 8Figure 9).
8.

Funnel plot of comparison: 3 Clinical pregnancy: assisted hatching compared with no assisted hatching, outcome: 3.1 Clinical pregnancy rate per woman randomised.
9.

Funnel plot of comparison: 4 Clinical pregnancies in trials that reported live births: assisted hatching compared with no assisted hatching, outcome: 4.1 Clinical pregnancies in trials reporting live births.
Miscarriage per woman
Seventeen (17) trials reported miscarriage rates, accounting for 2810 women. Due to the quality of the evidence, we are uncertain about the difference in miscarriage rate among women who underwent AH compared with those who underwent no AH (OR 1.13, 95% CI 0.82 to 1.56; 17 RCTs, n = 2810; I² = 0%; very low‐quality evidence; Figure 10; Analysis 5.1).
10.

Forest plot of comparison: 3 Miscarriage rate, outcome: 3.1 Miscarriage per woman randomised.
5.1. Analysis.

Comparison 5: Miscarriage: assisted hatching compared with no assisted hatching, Outcome 1: Miscarriage per woman randomised
Subgroup analysis
Number of attempts ‐ first or repeat attempt at ART: no evidence indicates that the effect of AH differed between those undergoing their first or subsequent attempts (P = 0.18) (Analysis 5.2)
Mode of conception ‐ assisted conception procedure (IVF/ICSI): no evidence shows that the effect of AH differed between those undergoing IVF and those undergoing ICSI treatment (P = 0.90) (Analysis 5.3)
Method of assisted hatching: no evidence suggests that the effect of AH differed between methods of AH (P = 1.00) (Analysis 5.4)
Prognosis: no evidence indicates that the effect of AH differed between women in poor prognosis groups and women in good prognosis groups (P = 0.73) (Analysis 5.5)
5.2. Analysis.

Comparison 5: Miscarriage: assisted hatching compared with no assisted hatching, Outcome 2: First or repeat attempt
5.3. Analysis.

Comparison 5: Miscarriage: assisted hatching compared with no assisted hatching, Outcome 3: Conception mode
5.4. Analysis.

Comparison 5: Miscarriage: assisted hatching compared with no assisted hatching, Outcome 4: Hatching method
5.5. Analysis.

Comparison 5: Miscarriage: assisted hatching compared with no assisted hatching, Outcome 5: Prognosis
Monozygotic twinning
Six trials reported data on monozygotic twinning (Figure 11). Hurst 1998 reported two monozygotic twins from three pregnancies in the AH group and none in the control group (0 from three pregnancies). Hagemann 2010 reported one case of monozygotic twins in the AH group also. Balakier 2009, Isik 2000, Jelinkova 2002, Lanzendorf 1998, and Ng 2005 reported absence of monozygotic twins in either group. There was an overall rate of 0.8% for the AH group and 0% for the control group (Analysis 6.1).
11.

Forest plot of comparison: 5 Monozygotic twinning rate, outcome: 5.1 Monozygotic twinning per woman randomised.
6.1. Analysis.

Comparison 6: Monozygotic twinning: assisted hatching compared with no assisted hatching, Outcome 1: Monozygotic twinning per woman randomised
Ectopic pregnancy
Five trials reported ectopic pregnancy data. Lanzendorf 1998 reported one ectopic pregnancy in the control group and none in the AH group. Hagemann 2010, Hellebaut 1996, and Hurst 1998 reported absence of ectopic pregnancies. Shi 2016 reported one ectopic pregnancy each in the AH and control groups.
Congenital or chromosomal abnormalities
Two trials reported absence of congenital or chromosomal abnormalities (Hurst 1998; Lanzendorf 1998), and two trials reported fetal abnormalities in both AH and control groups (Hagemann 2010; Razi 2013).
Failure to transfer any embryos per woman
No trials reported data on this outcome.
Embryo damage
Three trials reported absence of embryo damage (Hurst 1998; Lanzendorf 1998; Stein 1995).
In vitro blastocyst development
No trials reported data on in vitro blastocyst development.
No further analyses were performed because of the paucity of data on these secondary outcomes.
Assessment of reporting bias
We produced funnel plots for the outcomes of live birth (Figure 5) and clinical pregnancy (Figure 8; Figure 9), and we did not find any strong suggestion of publication bias.
Discussion
Summary of main results
Live birth
For this update, the primary outcome remained live birth rate. However only 14 of the 39 studies reported this outcome, representing 39% of all women randomised in the studies.
We are uncertain of the effects of assisted hatching (AH) on live birth rates when compared to no AH (Table 1). It is disappointing that the conclusions of this review are still limited by the paucity of available data since publication of the first Cochrane Review on this topic. Researchers still are not publishing the most important and sought after statistic on the impact of AH on assisted conception, namely, the 'live birth (take home baby rate)'. This reflects the gap that continues to exist between the practice of assisted conception and clinical obstetrics, with the absence of a central database of patient records that would facilitate follow‐up of these women by authorised agencies. Moving forward, we hope that with publication of the modified CONSORT statement to improve reporting of fertility trials, the primary outcome measure of all fertility trials in the future will be live birth (Harbin Consensus Conference Workshop Group 2014). Reported live birth data in one‐third of all studies suggest haste on the part of study authors to disseminate data limited to short‐term outcomes, and for all intents and purposes, these data are incomplete.
Multiple pregnancy
AH may lead to a higher multiple pregnancy rate compared to no AH; furthermore, an increase in multiple pregnancies per clinical pregnancy has been noted (37% increase in odds ratio (OR)). Given this significance in combination with uncertainty about any evidence of an increase in success at achieving live birth with AH, we may need to consider the overall risks versus benefits of this technique.
Only half of the studies that report multiple pregnancy rates also report live birth data. This is unfortunate as it limits interpretation of results, given this high multiple pregnancy rate, because as many as 5% of multiple pregnancies are lost at between 20 and 40 weeks' gestation. In addition, many studies were transferring two to four embryos, although the numbers transferred were balanced between groups. The increase in multiple pregnancies can be attributed to an increase in implantation rates resulting in higher pregnancy rates or monozygotic twinning, or both, with AH. This must be taken into consideration in planning this procedure.
It is likely that reducing to one the number of embryos transferred will not completely eliminate monozygotic twinning. Implantation rate was not considered as an outcome in this update for two reasons. Pooling of embryo implantation data for meta‐analysis is statistically problematic. Implantation is traditionally expressed 'per embryo transferred', without regard for the number of women. However, more than one embryo is normally transferred per woman, resulting in an embryo clustering effect and necessitating more advanced analysis to render the results meaningful. A statistically valid and easier approach is to express implantation 'per woman randomised'. This also confers the advantage of being more useful in aiding understanding of resulting live births. This approach requires, however, that the number of women with at least one gestation sac is reported, which is not the case in practice.
Clinical pregnancy
All 39 included trials reported on clinical pregnancy. Similar to the previous update (in 2012), this update suggests that overall, AH may slightly improve the chance of achieving a clinical pregnancy, but these results are less reliable because of high risk of bias and dependence upon the statistical model. Subgroup analysis supports these results.
When analysis of clinical pregnancy rate was restricted to those trials that went on to report live birth, the clinical pregnancy result showed little to no difference in effect between AH and control groups.
Miscarriage
We are uncertain of the effect of AH on miscarriage rates when compared to controls.
Other outcomes
The impact of AH on ectopic pregnancy, congenital and chromosomal abnormalities, blastocyst formation, and embryo damage could unfortunately not be determined by this review because of the paucity of available data. This is disappointing as it leaves many unanswered questions about perceived risks of the procedure, from embryo damage to chromosomal and congenital abnormalities.
Overall completeness and applicability of evidence
A large number of trials were incorporated into this review, involving a large sample size. The results of 7249 women in 39 trials are included in this review, leading to a low to very low level of evidence. Failure of many trials to report on primary outcomes (live birth, multiple pregnancy) and variable levels of reporting on other outcomes allow potential bias to be introduced into the analysis. This calls for standardised outcome reporting for future assisted conception trials as discussed.
Quality of the evidence
The quality of the evidence is low to very low. The main limitations are serious risk of bias associated with poor reporting of study methods, inconsistency, imprecision, and publication bias (Table 1).
Potential biases in the review process
Three review authors (LL, SH, and MAA) with varying levels of expertise undertook the search process several times to minimise the risk of bias introduced by review authors; they had no conflicts of interest.
We were unable to get responses from authors of various studies when abstracts were published and we had requested relevant or additional data. These studies could potentially have been included in the review.
Agreements and disagreements with other studies or reviews
Overall, the addition of eight new trials to this update has not changed the findings regarding live birth that were reported in previous reviews, namely, that no current evidence suggests that AH increases the chances of a live birth.
Clinical pregnancy rate may improve slightly in women undergoing AH, but these results are not reliable and robust.
Three recent non‐Cochrane systematic reviews have been published (He 2018; Li 2016; Zeng 2018). Li 2016 used random‐effects models for their meta‐analysis. They suggested that there is an increase in clinical pregnancy and multiple pregnancy rates with AH when compared to control. We agree with these findings generally, but Li 2016 did not present clear assessment of the quality and robustness of evidence related to these outcome improvements. Review authors suggested there was no improvement in live birth rates and no difference in miscarriage rates between AH and control groups. Li 2016 reported clinical pregnancy in 36 RCTs; however, this present Cochrane Review included 39 RCTs reporting clinical pregnancy (some different from the studies included by Li 2016), One RCT ‐ Urman 2002 ‐ which is reported in Li 2016 ‐ was excluded from the previous published Cochrane Review due to inadequate methods of allocation. He 2018 published a systematic review about AH that focused on a population of women older than 35 years of age. These review authors similarly demonstrated no increase in live birth rate or miscarriage rate with AH compared to control. Conversely, they demonstrated no increase in multiple pregnancy and no improvement in clinical pregnancy rate with AH compared to control. Our Cochrane Review did not specifically look at this subgroup, but this population was incorporated into our poor prognosis subgroup. Our data for the poor prognosis subgroup suggest that AH may improve slightly clinical pregnancy and may increase multiple pregnancy when compared to control. Zeng 2018 examined laser AH only in cryopreserved embryos. Their analysis led to the conclusions that AH improved clinical pregnancy rates and increased multiple pregnancy rates when compared to control but led to no difference in live birth rate and miscarriage rate. Our subgroup analysis of cryopreserved embryos includes all methods of AH. Our results suggest that AH makes little to no difference in live birth, clinical pregnancy, or multiple pregnancy when compared to control in this subgroup. Zeng 2018 included studies that reported data outcomes per embryo transfer rather than per woman; this could explain in part the differences in results.
Authors' conclusions
Implications for practice.
This update suggests that we are uncertain of the effect of assisted hatching (AH) on improving live birth rate, but it may slightly improve the chance of achieving a clinical pregnancy. However this result is not robust. The increase in clinical pregnancy rate is slightly higher in women with poor prognosis including those with previously failed in vitro fertilisation (IVF)/intracytoplasmic sperm injection (ICSI). Most trials still fail to report on live birth rates. Low‐quality evidence suggests increased risk of multiple pregnancy with assisted hatching, and very low‐quality evidence suggests that AH does not increase the miscarriage rate.
Implications for research.
This review once again highlights a wide range of currently unresolved issues that provide potential avenues for future research, including the need for high‐quality trials that report live births, clinical pregnancies, and adverse events (including multiple pregnancies, miscarriages, and long‐term adverse outcomes) and are powered to investigate effects in clinical subgroups.
The potential of assisted hatching in assisted conception makes it imperative that studies of high methodological quality (preferably multi‐centre trials of appropriate design, adequate power, and appropriate duration of follow‐up) are undertaken to provide these urgently needed answers; such studies should be funded only if they report the important primary outcome measures of live birth and multiple pregnancy.
What's new
| Date | Event | Description |
|---|---|---|
| 7 April 2021 | Amended | Searching sections corrected in methods and appendices |
History
Protocol first published: Issue 1, 2000 Review first published: Issue 4, 2003
| Date | Event | Description |
|---|---|---|
| 5 October 2020 | New search has been performed | Review authors have updated the Cochrane Review |
| 5 October 2020 | New citation required but conclusions have not changed | The addition of 8 trials has not led to a change in Review conclusions (Abulsoud 2019; Elnahas 2017; González‐Ortega 2015; Nada 2018; Razi 2013; Safari 2017; Shi 2016; Wan 2014) |
| 30 May 2013 | Amended | Minor correction to review title (format only) |
| 8 August 2012 | New citation required but conclusions have not changed | Seven new studies added; no change to conclusions |
| 8 August 2012 | New search has been performed | Review updated August 2012. Seven new studies in this update (Balakier 2009; Fang 2010; Ge 2008; Germond 2004; Hagemann 2010; Kutlu 2010; Valojerdi 2010) |
| 17 June 2008 | New search has been performed | New search identified 4 new randomised controlled trials, which have been added. Conclusions have not changed |
| 15 May 2008 | Amended | Converted to new review format |
| 18 September 2007 | New citation required and conclusions have changed | Substantive amendments made |
Acknowledgements
We wish to thank Helen Nagels and Marian Showell of the Cochrane Gynaecology and Fertility Group for help with literature searches and professional support that was invaluable to this update.
The authors of the 2020 update thank Dr. Debbie Blake and Dr. Kenneth Ma for contributions to early drafts of this update. They also thank Dr Paraskevi Vogiatzi, Dr Annika Strandell and Professor Andy Vail for providing referee comment on the updated review.
We wish to thank Dr. Demián Glujovsky for translating González‐Ortega et al., 2015 (published in Spanish) and for extracting data from the paper for the purposes of this review.
We wish to thank Dr. Jasmine Lee for translating Lu et al., 2016 (published in Chinese) and for extracting data for the purposes of this review.
We wish to thank Dr. Claudia González Ortega and Dr. Iman Halvaei for their correspondence to support the risk of bias assessments for their studies, González‐Ortega 2015 and Razi 2013, respectively.
We acknowledge the editorial board of the Cochrane Gynaecology and Fertility Group for support and advice provided.
We acknowledge the significant contributions of others to the original review and the updates that followed, including previous review authors, S Dias and Prof C Farquhar.
Edmond Edi‐Osagie contributed to the designing and worked on the original review.
Lee Hooper developed the second search strategy, undertook the February 2002 searches, and screened these search results, the late Phil McGinlay contributed to designing the original review, and we acknowledge the contributions of Sarah‐Kate Carney and Linsey Nelson.
Appendices
Appendix 1. Cochrane Gynaecology and Fertility (CGF) specialised register search strategy
PROCITE platform
Searched 27 May 2020
Keywords CONTAINS "IVF" or "in vitro fertilization" or "in‐vitro fertilisation" or "ICSI" or "intracytoplasmic sperm injection" or "Embryo" or "in‐vitro fertilization" or "Embryo Transfer" or "ET" or "Blastocyst" or "implantation" or "poor implantation" or "poor prognostic patients" or "recurrent implantation failure" or "repeated implantation failure" or Title CONTAINS"IVF" or "in vitro fertilization" or "in‐vitro fertilisation" or "ICSI" or "intracytoplasmic sperm injection" or "Embryo" or "in‐vitro fertilization" or "Embryo Transfer" or "ET" or "Blastocyst" or "implantation" or "poor implantation" or "poor prognostic patients" or "recurrent implantation failure" or "repeated implantation failure"
AND
Keywords CONTAINS "assisted hatching" or "assisted hatching techniques" or "assisted zona hatching" or "zona drilling" or "zona free" or "zona laser" or "zona pellucida dissection" or "zona pellucida removal techniques" or "zona thinning" or "mechanical assisted hatching" or "Chemical hatching" or "Chemically activated" or "laser‐assisted hatching" or "laser assisted" or "laser drilling" or "Laser hatching" or "Tyrodes" or "thinning" or Title CONTAINS "assisted hatching" or "assisted hatching techniques" or "assisted zona hatching" or "zona drilling" or "zona free" or "zona laser" or "zona pellucida dissection" or "zona pellucida removal techniques" or "zona thinning" or "mechanical assisted hatching" or "Chemical hatching" or "Chemically activated" or "laser‐assisted hatching" or "laser assisted" or "laser drilling" or "Laser hatching" or "Tyrodes" or "thinning"
(184 records)
Appendix 2. CENTRAL via the Cochrane Register of Studies Online (CRSO) search strategy
Web platform
Searched 27 May 2020
#1 MESH DESCRIPTOR Embryo Transfer EXPLODE ALL TREES 1076
#2 MESH DESCRIPTOR Fertilization in Vitro EXPLODE ALL TREES 2028
#3 MESH DESCRIPTOR Sperm Injections, Intracytoplasmic EXPLODE ALL TREES 530
#4 (vitro fertili?ation):TI,AB,KY 3336
#5 ivf:TI,AB,KY 5516
#6 icsi:TI,AB,KY 2661
#7 (intracytoplasmic sperm injection*):TI,AB,KY 1859
#8 (embryo* or blastocyst*):TI,AB,KY 7494
#9 implantation*:TI,AB,KY 17443
#10 (assisted reproducti*):TI,AB,KY 1375
#11 (poor prognos*):TI,AB,KY 3520
#12 (recur* adj3 implant* ):TI,AB,KY 190
#13 #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 29082
#14 (zona* adj5 (dissect* or tyrode* or proteinase* or piezon* or krypton* or yag*)):TI,AB,KY 30
#15 (zona* adj5 (pellucid* or manipulate* or disrupt* or thin* or drill*)):TI,AB,KY 226
#16 (mechanical adj5 zona*):TI,AB,KY 3
#17 (chemical adj5 zona*):TI,AB,KY 4
#18 (laser adj5 zona*):TI,AB,KY 47
#19 hatch*:TI,AB,KY 391
#20 pzd:TI,AB,KY 6
#21 microfertili?ation:TI,AB,KY 5
#22 (micro fertili?ation):TI,AB,KY 1
#23 #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 523
#24 #13 AND #23 347
Appendix 3. MEDLINE search strategy
Ovid platform
Searched from 1946 to 27 May 2020
1 exp embryo transfer/ or exp fertilization in vitro/ or exp sperm injections, intracytoplasmic/ (41278) 2 in vitro fertili?ation.tw. (23107) 3 ivf‐et.tw. (2311) 4 icsi.tw. (8369) 5 intracytoplasmic sperm injection$.tw. (7167) 6 (embryo$ or blastocyst$).tw. (355005) 7 implantation$.tw. (166687) 8 ART.tw. (101884) 9 assisted reproducti$.tw. (14867) 10 (ivf or et).tw. (286418) 11 or/1‐10 (887220) 12 (assist$ adj5 hatch$).tw. (397) 13 (zona$ adj5 (dissect$ or tyrode$ or proteinase$ or piezon$ or krypton$ or yag$)).ti,ab,sh. (183) 14 (zona$ adj5 (pellucid$ or manipulat$ or disrupt$ or thin$ or drill$)).ti,ab,sh. (5425) 15 (mechanical adj5 zona$).tw. (60) 16 (chemical$ adj5 zona$).tw. (53) 17 (laser adj5 zona$).tw. (137) 18 pzd.tw. (72) 19 or/12‐18 (5815) 20 11 and 19 (2897) 21 randomized controlled trial.pt. (506126) 22 controlled clinical trial.pt. (93684) 23 randomized.ab. (480049) 24 placebo.tw. (213550) 25 clinical trials as topic.sh. (191286) 26 randomly.ab. (333535) 27 trial.ti. (218599) 28 (crossover or cross‐over or cross over).tw. (84663) 29 or/21‐28 (1319801) 30 exp animals/ not humans.sh. (4700877) 31 29 not 30 (1213169) 32 20 and 31 (159)
Appendix 4. Embase search strategy
Ovid platform
Searched from 1980 to 27 May 2020
1 (assist$ adj5 hatch$).tw. (696) 2 (zona$ adj5 (dissect$ or tyrode$ or proteinase$ or piezon$ or krypton$ or yag$)).ti,ab,sh. (356) 3 (zona$ adj5 (pellucid$ or manipulat$ or disrupt$ or thin$ or drill$)).ti,ab,sh. (6079) 4 (mechanical adj5 zona$).tw. (74) 5 (chemical$ adj5 zona$).tw. (52) 6 (laser adj5 zona$).tw. (226) 7 pzd.tw. (94) 8 or/1‐7 (6757) 9 exp embryo transfer/ or exp fertilization in vitro/ or exp intracytoplasmic sperm injection/ (68949) 10 in vitro fertili?ation.tw. (30147) 11 ivf‐et.tw. (3196) 12 icsi.tw. (15993) 13 intracytoplasmic sperm injection$.tw. (9566) 14 (ivf or et).tw. (690080) 15 (embryo$ or blastocyst$).tw. (392034) 16 implantation$.tw. (238479) 17 ART.tw. (127295) 18 assisted reproducti$.tw. (22584) 19 or/9‐18 (1398644) 20 8 and 19 (3633) 21 Clinical Trial/ (963034) 22 Randomized Controlled Trial/ (598954) 23 exp randomization/ (86801) 24 Single Blind Procedure/ (38819) 25 Double Blind Procedure/ (169202) 26 Crossover Procedure/ (62950) 27 Placebo/ (335995) 28 Randomi?ed controlled trial$.tw. (227639) 29 Rct.tw. (36951) 30 random allocation.tw. (1997) 31 randomly allocated.tw. (34904) 32 allocated randomly.tw. (2533) 33 (allocated adj2 random).tw. (812) 34 Single blind$.tw. (24525) 35 Double blind$.tw. (201612) 36 ((treble or triple) adj blind$).tw. (1133) 37 placebo$.tw. (301171) 38 prospective study/ (598878) 39 or/21‐38 (2176633) 40 case study/ (68827) 41 case report.tw. (400435) 42 abstract report/ or letter/ (1092786) 43 or/40‐42 (1551618) 44 39 not 43 (2123502) 45 20 and 44 (312)
Appendix 5. PsycINFO search strategy
Ovid platform
Searched from 1806 to 27 May 2020
1 exp Embryo/ or exp Reproductive Technology/ or exp Infertility/ (5151) 2 in vitro fertili?ation.tw. (744) 3 ivf‐et.tw. (19) 4 icsi.tw. (72) 5 intracytoplasmic sperm injection$.tw. (56) 6 (embryo$ or blastocyst$).tw. (11093) 7 implantation$.tw. (4383) 8 ART.tw. (44913) 9 assisted reproducti$.tw. (968) 10 (ivf or et).tw. (140592) 11 or/1‐10 (202023) 12 (assist$ adj5 hatch$).tw. (5) 13 (zona$ adj5 (pellucid$ or manipulat$ or disrupt$ or thin$ or drill$)).ti,ab,sh. (23) 14 pzd.tw. (5) 15 12 or 13 or 14 (33) 16 11 and 15 (8)
Data and analyses
Comparison 1. Live birth: assisted hatching compared with no assisted hatching.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Live birth per woman randomised | 14 | 2849 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.92, 1.29] |
| 1.2 First or repeat attempt | 4 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.2.1 First attempt at IVF or ICSI | 3 | 380 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.48, 1.28] |
| 1.2.2 Repeat attempt at IVF or ICSI | 1 | 150 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.40 [0.62, 3.13] |
| 1.3 Conception mode | 6 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.3.1 ICSI only | 3 | 640 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.54 [1.02, 2.33] |
| 1.3.2 IVF only | 3 | 241 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.60, 1.68] |
| 1.4 Hatching method | 14 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.4.1 Chemical | 4 | 366 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.74, 1.74] |
| 1.4.2 Laser | 10 | 2473 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.89, 1.28] |
| 1.5 Prognosis | 9 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.5.1 Poor prognosis | 4 | 576 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.46 [0.99, 2.15] |
| 1.5.2 Good prognosis | 6 | 1495 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.83, 1.28] |
| 1.6 Live birth rate by extent of assisted hatching | 14 | 2849 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.92, 1.29] |
| 1.6.1 Thinning only | 6 | 1742 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.86, 1.30] |
| 1.6.2 Breach by hole only | 8 | 1107 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.87, 1.51] |
| 1.7 Fresh or frozen embryo transfer | 12 | 1731 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.14 [0.92, 1.41] |
| 1.7.1 Fresh | 11 | 1669 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.94, 1.44] |
| 1.7.2 Frozen | 1 | 62 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.22, 2.07] |
1.7. Analysis.

Comparison 1: Live birth: assisted hatching compared with no assisted hatching, Outcome 7: Fresh or frozen embryo transfer
Comparison 2. Multiple pregnancy: assisted hatching compared with no assisted hatching.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Multiple pregnancy rate per woman randomised | 18 | 4308 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.38 [1.13, 1.68] |
| 2.2 First or repeat attempt | 8 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.2.1 First attempt at IVF or ICSI | 4 | 654 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.31, 1.72] |
| 2.2.2 Repeat attempt at IVF or ICSI | 5 | 1068 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.25 [0.80, 1.94] |
| 2.3 Conception mode | 9 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.3.1 ICSI only | 3 | 573 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.09 [1.57, 6.08] |
| 2.3.2 IVF only | 6 | 1126 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.87 [1.28, 2.72] |
| 2.4 Hatching method | 18 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.4.1 Chemical | 4 | 534 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.55 [0.98, 2.47] |
| 2.4.2 Laser | 13 | 3730 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.29 [1.03, 1.61] |
| 2.4.3 Mechanical | 1 | 44 | Odds Ratio (M‐H, Fixed, 95% CI) | 8.33 [1.56, 44.64] |
| 2.5 Prognosis | 10 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.5.1 Poor prognosis | 6 | 1186 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.95 [1.27, 3.00] |
| 2.5.2 Good prognosis | 6 | 1569 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.81, 1.44] |
| 2.6 Multiple pregnancy rate per woman grouped by extent of assisted hatching | 16 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.6.1 Thinning only | 6 | 2148 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.34 [1.02, 1.76] |
| 2.6.2 Breach by hole | 9 | 1629 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.51 [1.08, 2.11] |
| 2.6.3 Complete removal of zona | 1 | 25 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.07, 5.28] |
| 2.7 Fresh or frozen embryo transfer | 16 | 3190 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.38 [1.08, 1.75] |
| 2.7.1 Fresh | 13 | 2264 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.30 [0.98, 1.73] |
| 2.7.2 Frozen | 3 | 926 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.60 [1.00, 2.55] |
| 2.8 Multiple pregnancy per pregnancy | 17 | 1598 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.37 [1.09, 1.72] |
Comparison 3. Clinical pregnancy: assisted hatching compared with no assisted hatching.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Clinical pregnancy rate per woman randomised | 39 | 7249 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.20 [1.09, 1.33] |
| 3.2 First or repeat attempt | 18 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.2.1 First attempt at IVF or ICSI | 8 | 1010 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.56, 0.98] |
| 3.2.2 Repeat attempt at IVF or ICSI | 11 | 1798 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.65 [1.34, 2.04] |
| 3.3 Conception mode | 26 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.3.1 ICSI only | 11 | 1825 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.40 [1.14, 1.71] |
| 3.3.2 IVF only | 15 | 2460 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.31 [1.10, 1.55] |
| 3.4 Hatching method | 39 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.4.1 Chemical | 11 | 1536 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.33 [1.08, 1.64] |
| 3.4.2 Laser | 23 | 5127 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.15 [1.03, 1.30] |
| 3.4.3 Mechanical | 5 | 586 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.30 [0.89, 1.88] |
| 3.5 Prognosis | 24 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.5.1 Poor prognosis | 14 | 2108 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.68 [1.38, 2.04] |
| 3.5.2 Good prognosis | 14 | 2721 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.94, 1.29] |
| 3.6 Extent of assisted hatching | 37 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.6.1 Thinning only | 17 | 3774 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.96, 1.26] |
| 3.6.2 Breach by hole only | 17 | 2543 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.98, 1.39] |
| 3.6.3 Complete removal of zona | 2 | 301 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.93 [1.21, 3.09] |
| 3.6.4 Expansion of zona pellucida | 1 | 125 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.37 [1.07, 5.28] |
| 3.7 Fresh and frozen embryo transfer | 38 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.7.1 Fresh embryo transfer | 30 | 5349 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.23 [1.10, 1.38] |
| 3.7.2 Frozen embryo transfer only | 10 | 1700 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.93, 1.42] |
Comparison 4. Clinical pregnancies in trials that reported live births: assisted hatching compared with no assisted hatching.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Clinical pregnancies in trials reporting live births | 14 | 2849 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.92, 1.25] |
Comparison 5. Miscarriage: assisted hatching compared with no assisted hatching.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Miscarriage per woman randomised | 17 | 2810 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.82, 1.56] |
| 5.2 First or repeat attempt | 8 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.2.1 First attempt at IVF or ICSI | 4 | 442 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.51, 1.89] |
| 5.2.2 Repeat attempt at IVF or ICSI | 5 | 966 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.96 [0.90, 4.28] |
| 5.3 Conception mode | 10 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.3.1 ICSI only | 4 | 665 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.20 [0.58, 2.47] |
| 5.3.2 IVF only | 6 | 896 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.28 [0.65, 2.52] |
| 5.4 Hatching method | 17 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.4.1 Chemical | 5 | 412 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.56, 2.21] |
| 5.4.2 Laser | 11 | 2244 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.78, 1.64] |
| 5.4.3 Mechanical | 1 | 154 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.14 [0.07, 18.58] |
| 5.5 Prognosis | 11 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.5.1 Poor prognosis | 7 | 1133 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.21 [0.70, 2.08] |
| 5.5.2 Good prognosis | 5 | 626 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.50, 2.14] |
| 5.6 Miscarriage per clinical pregnancy | 15 | 777 | Odds Ratio (M‐H, Random, 95% CI) | 0.94 [0.62, 1.43] |
5.6. Analysis.

Comparison 5: Miscarriage: assisted hatching compared with no assisted hatching, Outcome 6: Miscarriage per clinical pregnancy
Comparison 6. Monozygotic twinning: assisted hatching compared with no assisted hatching.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 6.1 Monozygotic twinning per woman randomised | 6 | 729 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.23 [0.34, 31.03] |
Comparison 7. Robust studies (randomisation method and allocation concealment stated and live birth reported): assisted hatching compared with no assisted hatching.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 7.1 Live births | 1 | 960 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.82, 1.41] |
| 7.2 Clinical pregnancies | 1 | 960 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.85, 1.43] |
7.1. Analysis.

Comparison 7: Robust studies (randomisation method and allocation concealment stated and live birth reported): assisted hatching compared with no assisted hatching, Outcome 1: Live births
7.2. Analysis.

Comparison 7: Robust studies (randomisation method and allocation concealment stated and live birth reported): assisted hatching compared with no assisted hatching, Outcome 2: Clinical pregnancies
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Abulsoud 2019.
| Study characteristics | ||
| Methods | Randomised into 2 groups using sealed envelopes but no further details No information on random sequence generation Single centre Unclear if participants were blinded Unclear if outcome assessor was blinded No power calculation was documented Published full paper |
|
| Participants | 130 patients attending a private IVF centre in Cairo, Egypt, undergoing fresh ICSI using Day 3 embryos. Age ≥ 38 years, requiring ≥ 375 IU of gonadotrophin per day, with previously failed ICSI Mean age: control group 39.5, AH group 39.2 |
|
| Interventions | LAH 3 hours before embryo transfer, thinning of zona pellucida until 25% irradiated Control – 65 women LAH – 65 women |
|
| Outcomes | Chemical pregnancy (defined as bhCG > 25 on blood 14 days after ET) Clinical pregnancy (defined as presence of FH 7 weeks after ET) |
|
| Notes | Mean number of embryos transferred: control 2.5, LAH 2.7 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes used |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information given about whether participants or outcome assessors were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients had outcomes reported |
| Selective reporting (reporting bias) | High risk | No reporting of miscarriage, multiple pregnancy, or live birth |
| Other bias | Unclear risk | No information |
Antinori 1999.
| Study characteristics | ||
| Methods | Randomisation stated but method unclear Allocation concealment unclear Unclear if single centre/multi‐centre Unclear whether participants and assessors were blinded Unclear whether power calculation performed ITT analysis unclear Published as abstract | |
| Participants | 341 women from Italy undergoing IVF. Subgrouped by previous IVF experience: (a) without previous IVF experience (n = 199) or (b) with more than 6 previous IVF failures (n = 142) Mean age: control group 27.0, AH group 27.5 years | |
| Interventions | AH (laser; complete zona breach; unclear how long from egg retrieval to AH; unclear how long from AH to transfer) ‐ 169 women randomised, 221 embryos transferred (estimated) vs Control ‐ no AH ‐ 172 women randomised, 247 embryos transferred (estimated) |
|
| Outcomes | Clinical pregnancy, miscarriage, multiple pregnancy | |
| Notes | No reply No. of embryos transferred: AH 2.3, control 2.4 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation stated but method unclear |
| Allocation concealment (selection bias) | Unclear risk | Unclear; no details provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Unclear whether participants and assessors were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No evidence of post‐randomisation exclusions but timing of allocation unclear |
| Selective reporting (reporting bias) | Unclear risk | Protocol not viewed. Not sure if these are all planned outcomes |
| Other bias | Unclear risk | Conference abstract |
Balaban 2006.
| Study characteristics | ||
| Methods | Randomisation by computer‐generated numbers | |
| Participants | 366 women from Turkey undergoing ICSI treatment only Exclusion: women undergoing IVF |
|
| Interventions | AH (laser thinning) (n = 183) vs No AH (laser thinning) (n = 183) Unclear on how long before transfer, frozen‐thawed embryos only |
|
| Outcomes | Primary: implantation rate Secondary: clinical pregnancy, miscarriage, multiple pregnancy rate |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation by computer‐generated numbers |
| Allocation concealment (selection bias) | Unclear risk | No details in text |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No details on blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No losses to follow‐up and all women analysed |
| Selective reporting (reporting bias) | Low risk | All outcomes listed in the methods section reported |
| Other bias | Low risk | None identified |
Balakier 2009.
| Study characteristics | ||
| Methods | Single centre Unclear whether power calculation performed ITT analysis unclear Published as full paper | |
| Participants | 84 women from Canada with no more than 1 unsuccessful previous IVF attempt, ≤ 37 years of age, Day 3 FSH ≤ 10 mIU/mL
Mean age: control: 33.8 ± 3.2; AH: 32.5 ± 3.8 54 women underwent their first IVF cycle; the other 30 (13 AH) their second cycle |
|
| Interventions | Laser‐assisted thinning (n = 45): total length of laser cut was approximately 30 to 40 μm, and about 60% to 80% of the outer layer of the zona pellucida was thinned without complete breaching, applying 2 ms laser beams vs Control (n = 39) |
|
| Outcomes | Clinical pregnancy; multiple pregnancies; spontaneous miscarriage; live birth | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation list |
| Allocation concealment (selection bias) | Unclear risk | No details in text |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Study was double‐blinded to patients and medical personnel |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No losses to follow‐up and all women analysed |
| Selective reporting (reporting bias) | Low risk | Live birth reported |
| Other bias | Low risk | None identified |
Baruffi 2000.
| Study characteristics | ||
| Methods | Single centre Unclear whether power calculation performed ITT analysis unclear Published as full paper | |
| Participants | 103 women from Brazil aged 37 years or younger, undergoing ICSI for the first time. Mean zona thickness: control group 17.1 μm (SD 1.7); AH 16.6 μm (SD 2.2). Mean age: control group 31.4 (3.6); AH group 31.8 (3.6) | |
| Interventions | AH (laser; thinning partial; 48 hour egg retrieval to AH; 0 hour AH to transfer), 51 women randomised, 141 embryos transferred vs No AH, 52 women randomised, 149 embryos transferred |
|
| Outcomes | Implantation, clinical pregnancy, miscarriage | |
| Notes | No reply No. of embryos transferred: AH 2.76; control 2.87 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Women were selected at random via a randomisation table |
| Allocation concealment (selection bias) | Unclear risk | No information in the text |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information in the text |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No losses to follow‐up and all women analysed |
| Selective reporting (reporting bias) | Unclear risk | Original protocol not viewed. Live birth not reported, so not sure it was planned |
| Other bias | Unclear risk | No reply from authors ‐ see notes |
Carter 2003.
| Study characteristics | ||
| Methods | Single centre Unclear whether power calculation performed Published as abstract; study authors provided additional information | |
| Participants | 203 women from fertility clinic in USA Age < 40 years FSH < 10, ovulatory menstrual cycles, day 3 ET with good embryo quality Women with more than 1 failed IVF cycle excluded | |
| Interventions | Laser hatching (n = 121) vs No hatching (n = 82) |
|
| Outcomes | Clinical pregnancy rate, multiple pregnancy rate | |
| Notes | Additional information provided by study authors
Dropouts included for the denominator in this review No. of embryos: AH 2.2; control 2.1 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised by computer generation on Day 3 |
| Allocation concealment (selection bias) | Unclear risk | Unclear; no details provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Participants not blinded or unclear Assessor not blinded or unclear |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated but included dropouts |
| Selective reporting (reporting bias) | High risk | This was a conference abstract only and was not published as a full paper, although study authors did provide additional information. Live birth was not reported |
| Other bias | Unclear risk | Conference abstract |
Ciray 2005.
| Study characteristics | ||
| Methods | Single centre Power calculation not reported ITT analysis not stated Published as full paper | |
| Participants | 114 women from Turkey undergoing ART for ASRM grade 3 to 4 endometriosis only (poor prognosis) Age < 40 years; AH group 33.1 (4.2); control group 34.0 (3.7) Basal FSH: AH group 7.4 (3.5); control group 9.0 (5.1) | |
| Interventions | Laser hatching (thinning to a quarter), 76 women randomised, 146 embryos transferred (16 cancelled) vs No hatching, only fresh embryo transfer cycles, 38 women randomised, 72 embryos transferred (8 cancelled) |
|
| Outcomes | Clinical pregnancy rate, implantation rate | |
| Notes | No. of embryos: AH 2.4; control 2.4 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised method stated 2:1 date, with the aid of computer programme |
| Allocation concealment (selection bias) | Unclear risk | Unclear; no details |
| Blinding (performance bias and detection bias) All outcomes | High risk | No evidence of blinding of participants or assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All women appear to have been analysed |
| Selective reporting (reporting bias) | Unclear risk | All outcomes reported but original protocol not viewed; live birth not reported |
| Other bias | Low risk | None identified |
Cohen 1992.
| Study characteristics | ||
| Methods | Single centre Unclear whether power calculation performed ITT analysis unclear Published as full paper | |
| Participants | 330 women from North America undergoing IVF Mean age: control group 36.7 (3.7); AH group 36.5 (3.3) | |
| Interventions | AH by acid Tyrode's (chemical; complete zona breach hole; 68 to 72 hour egg retrieval to AH; 4 to 8 hours AH to transfer), 69 women with FSH < 15 (trial 1), 80 women with poor prognosis (trial 2, thick zona pellucida, low developmental rate, excessive fragmentation), 15 women with FSH > 15 (trial 3) No AH, 68 women with FSH < 15 (trial 1), 83 women with poor prognosis (trial 2, thick zona pellucida, low developmental rate, excessive fragmentation), 15 women with FSH > 15 (trial 3) |
|
| Outcomes | Implantation, clinical pregnancy (rates given for trials 1, 2, and 3), live births (rates given for women in trial 1 only), multiple pregnancy (rates given for women in trials 1 and 2 only) | |
| Notes | Attempted to contact author about this study. Reply received, but no additional information offered No. of embryos: AH 3.5; control 3.4 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Pre‐printed randomisation list |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants blinded Assessor blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No evidence of post‐randomisation exclusions, but timing of allocation unclear |
| Selective reporting (reporting bias) | Low risk | Original protocol not viewed. Live birth reported |
| Other bias | Low risk | None identified |
Elhelw 2005.
| Study characteristics | ||
| Methods | Power calculation not reported ITT not stated Published as abstract only | |
| Participants | 74 women from Egypt undergoing ICSI only Poor prognosis Previous 2 implantation failures Cryo‐thaw cycles only | |
| Interventions | Laser hatching (thinning to quarter) vs no hatching. AH done 1 hour before embryo transfer AH: 37 women randomised, 121 embryos transferred Control: 37 women randomised, 130 embryos transferred | |
| Outcomes | Implantation rate, clinical pregnancy rate | |
| Notes | No author contact as all details in the article No data on no. of embryos transferred |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated; no details |
| Allocation concealment (selection bias) | Unclear risk | Not clear |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Participant blinding unclear Assessor blinding unclear |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No details |
| Selective reporting (reporting bias) | High risk | Conference abstract only. No evidence of a full paper. Live birth not reported |
| Other bias | Unclear risk | Conference abstract |
Elnahas 2017.
| Study characteristics | ||
| Methods | Randomised into 2 groups on day of ET using sealed envelope but no further details No information on random sequence generation No information about centres Unclear whether participants were blinded Unclear whether outcome assessor blinded No power calculation documented Published full paper |
|
| Participants | 160 patients undergoing frozen ET after IVF using Day 3 embryos. Age 18 to 40 years, following first IVF pregnancy, following 1 implantation failure, or following postponement of transfer to avoid sequelae of OHSS Only included excellent (≥ 8 cells and fragmentation < 10%) or good (≥ 8 cells and fragmentation between 10% and 20%) quality Day 3 embryos Mean age: control group 31.7, AH group 31.0 |
|
| Interventions | LAH 1 hour before embryo transfer, thinning of zona pellucida at only one‐eighth of its surface (no breaching) Control – 80 women LAH – 80 women |
|
| Outcomes | Clinical pregnancy (defined by transvaginal ultrasound scan on fourth and sixth weeks to detect IU GS and fetal pulsations) | |
| Notes | Mean age: LAH group 31.02, non‐LAH group 31.71 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information given |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes used |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information about clinician or participant blinding nor blinding of outcome assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcomes reported for all patients |
| Selective reporting (reporting bias) | High risk | No multiple pregnancy, miscarriage, or live birth data given. Implantation rates given as percentages only |
Fang 2010.
| Study characteristics | ||
| Methods | Single‐centre randomised controlled trial | |
| Participants | 125 women in China who had their first IVF/ICSI cycles between 2006 and 2008, with fresh IVF‐ET failures or without fresh embryo transfers Mean age: 32.3 in AH group, 32.1 in control group Setting: fertility centre, China (2006 to 2008) |
|
| Interventions | Mechanical assisted hatching: expanding/stretching zona pellucida via injected hydrostatic pressure AH: 61 women, 178 embryos Control: 64 women, 190 embryos |
|
| Outcomes | Clinical pregnancy, implantation rates | |
| Notes | Unclear whether power calculation performed ITT analysis unclear Published as full paper | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Unclear whether participants were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unclear |
| Selective reporting (reporting bias) | Unclear risk | Original protocol not viewed. Live birth not reported, so not sure it was planned |
| Other bias | Low risk | None identified |
Ge 2008.
| Study characteristics | ||
| Methods | Randomised controlled trial | |
| Participants | 760 women from China having IVF with fewer than 5 failed cycles of ART with normal baseline FSH concentration. Those participants with uterine abnormality or low fertilisation capacity (rate of fertilisation < 20% and late ICSI following fertilisation failure of IVF) were excluded Mean age: fresh, 31.08 AH, 30.44 control; frozen, 31.84 AH, 30.66 control |
|
| Interventions | Laser thinning to about 50% of initial ZP thickness AH: 387 women with fresh embryos, 100 women with frozen‐thawed embryos Control: 373 women with fresh embryos, 100 women with frozen‐thawed embryos |
|
| Outcomes | Implantation rate, pregnancy rate, live birth | |
| Notes | Unclear whether power calculation performed ITT not stated Published as full paper | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Women were randomised according to a randomisation list based on sequential numbers in sealed envelopes |
| Allocation concealment (selection bias) | Unclear risk | Unclear allocation |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Blinded both clinicians and patient |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Fresh embryo transfer cycles: total of 831 IVF/ICSI cycles were performed during the study period. Of these, 772 met the inclusion criteria, but 12 participants abandoned embryo transfer for various reasons such as avoiding potential risks of ovarian hyperstimulation syndrome Frozen‐thawed embryo transfer: total of 245 frozen‐thawed cycles were also performed, of which 45 were excluded because they did not meet the criteria of the study or because embryo transfer was abandoned |
| Selective reporting (reporting bias) | Low risk | Original protocol not viewed. Live birth reported |
| Other bias | Low risk | None identified |
Germond 2004.
| Study characteristics | ||
| Methods | Multi‐centre RCT | |
| Participants | 153 women in 4 European IVF centres between 20 and 45 years old, with ≥ 1 functional ovary, normal FSH and prolactin levels, no clinically significant findings within 6 months before starting treatment, and normal uterine cavity | |
| Interventions | Laser assisted hatching using diode laser AH: 56 women undergoing first cycle of frozen‐thawed embryos, 23 women who had a poor prognosis using fresh embryos Control: 53 women undergoing first cycle of frozen‐thawed embryos, 21 women who had a poor prognosis using fresh embryos |
|
| Outcomes | Clinical pregnancies, live births, miscarriages, multiple pregnancies | |
| Notes | Power calculation performed
ITT not stated Published as full paper |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Women were randomised according to a randomisation list |
| Allocation concealment (selection bias) | Unclear risk | Not stated in the text |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated in the text |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No evidence of attrition bias |
| Selective reporting (reporting bias) | Low risk | Live birth reported |
| Other bias | Low risk | None identified |
González‐Ortega 2015.
| Study characteristics | ||
| Methods | Prospective randomised study IVF and ICSI Repeat cycle January 2008 till June 2010 |
|
| Participants | Inclusion criteria: ≥ 38 years old, basal FSH ≥ 12.0 mUI/mL, ≥ 2 failed IVF‐ICSI cycles with ≥ 6 good quality embryos already transferred, with adequate endometrial receptiveness, with atraumatic embryo transfers Exclusion criteria: frozen‐thawed embryo transfers, egg donation cycles, fewer than 2 growing follicles, bad quality embryos, non‐receptive endometrium, traumatic embryo transfer |
|
| Interventions | Timing of assisted hatching: ≥ 1 hour before embryo transfer (on Days 2 and 3) Method of assisted hatching: laser |
|
| Outcomes | Clinical pregnancy rate, multiple pregnancy rate, miscarriage rate | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Correspondence from study author ‐ computer‐generated randomisation |
| Allocation concealment (selection bias) | Low risk | Correspondence from study author ‐ sealed envelopes |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Correspondence from study author ‐ clinicians and patients blinded to allocation |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No losses reported |
| Selective reporting (reporting bias) | Unclear risk | Original protocol not viewed. Live birth not reported, so not sure it was planned |
| Other bias | Unclear risk | Not enough information provided |
Hagemann 2010.
| Study characteristics | ||
| Methods | Randomised single‐centre cross‐over trial | |
| Participants | 103 women in the United States younger than 38 years of age with any embryo with zona pellucida thickness > 13 μm and more than 2 previously failed IVF cycles Mean age: 32.1 years in hatched group, 31.2 in unhatched group | |
| Interventions | AH performed by acidic Tyrode's solution AH: 49 women Control: 54 women |
|
| Outcomes | Clinical intrauterine pregnancy rate, implantation rate, spontaneous pregnancy loss, live birth rate | |
| Notes | Power calculation: study states it has inadequate power. Study as ultimately performed had sufficient statistical power to identify only a 30% absolute effect size with alpha = 0.05 and beta = 0.80
ITT analysis unclear Published as full paper |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomisation was performed by IVF lab staff by drawing 1 of 200 opaque envelopes from a box |
| Allocation concealment (selection bias) | Unclear risk | Opaque envelopes drawn but not numbered |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Study arm to which participants belonged was blinded to caregivers, with the exception of IVF embryologists, as well as to participants |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unclear |
| Selective reporting (reporting bias) | High risk | Live birth reported (but results not included in this study, as results were given only for both cycles combined, not for just the first cycle; these are the data we are using). No other evidence of reporting bias |
| Other bias | Low risk | None identified |
Hellebaut 1996.
| Study characteristics | ||
| Methods | Randomised single‐centre trial | |
| Participants | 120 women from Belgium undergoing IVF or ICSI Mean age: control group 30.8 (3.9); AH group 30.9 (4.3) years | |
| Interventions | AH (mechanical; complete zona breach hole; 48 hour egg retrieval to AH; 0.2 hour AH to transfer) vs no AH AH: 60 women randomised, 168 embryos transferred Control: 60 women randomised, 162 embryos transferred | |
| Outcomes | Implantation, clinical pregnancy, live birth, miscarriage, ectopic pregnancy | |
| Notes | Attempted to contact author about this study. A reply including much useful additional information was received
No. of embryos transferred: AH 2.8 (0.6); control 2.7 (0.6) Unclear whether power calculation performed ITT analysis unclear Published as full paper |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | By computer on day of transfer |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment unclear |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants not blinded Assessor not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | ITT analysis unclear |
| Selective reporting (reporting bias) | Low risk | Live birth reported. Study authors responded to requests for details. No other evidence of bias; all outcomes stated were reported |
| Other bias | Low risk | None identified |
Hurst 1998.
| Study characteristics | ||
| Methods | Single‐centre randomised trial | |
| Participants | 20 women from North America undergoing IVF with no prior IVF (30 years or less, FSH < 10 IU/L, normal endometrium and sperm) or with prior IVF (35 years or less, 6 embryos, 50% fertilisation, normal endometrium). Mean age: control group 30 (0.8); AH group 30 (0.9) | |
| Interventions | AH by acid Tyrode's (chemical; complete zona breach hole; ? hour egg retrieval to AH; ? hour AH to transfer) vs no AH AH: 13 women randomised, 52 embryos transferred Control: 7 women randomised, 28 embryos transferred | |
| Outcomes | Implantation, clinical pregnancy, live births | |
| Notes | Attempted to contact author about this study. A reply including much useful additional information was received No of embryos transferred: AH 4.0; control 4.0 Unclear whether power calculation performed ITT analysis unclear Published as full paper |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐randomised |
| Allocation concealment (selection bias) | Unclear risk | Unclear; no details |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Participants not blinded or unclear Assessor not blinded or unclear |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | ITT analysis unclear |
| Selective reporting (reporting bias) | Low risk | Protocol not viewed but outcomes reported including live birth |
| Other bias | Low risk | None identified |
Isik 2000.
| Study characteristics | ||
| Methods | Single‐centre randomised trial | |
| Participants | 46 women from Turkey with > 5 Day 3 cleavage stage embryos (FSH at Day 3: control 6.1 (3.0); AH 5.5 (1.4) IU/L) undergoing ICSI Mean duration of infertility: 6.7 years Mean age: control group 29.1 (3.6); AH group 30.5 (5.2) years | |
| Interventions | AH enzymatic (chemical; complete and total zona breach; 120 to 144 hour egg retrieval to AH; 0.5 to 1 hour AH to transfer) vs no AH AH: 24 women randomised, 71 embryos transferred Control: 22 women randomised, 63 embryos transferred | |
| Outcomes | Implantation | |
| Notes | Study author response No. of embryos transferred, blastocyst transfer: AH 2.95 (0.9); control 2.86 (0.8) Unclear whether power calculation performed ITT analysis unclear Published as full paper |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table used on Day 3 |
| Allocation concealment (selection bias) | Unclear risk | Allocation unclear |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Participants not blinded or unclear Assessor not blinded or unclear |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated |
| Selective reporting (reporting bias) | Unclear risk | Protocol not viewed; however live birth not reported |
| Other bias | Low risk | None identified |
Isiklar 1999.
| Study characteristics | ||
| Methods | Single‐centre randomised trial | |
| Participants | 44 women from Turkey undergoing IVF Mean age not stated | |
| Interventions | AH (mechanical; complete zona breach; ? hour egg retrieval to AH; ? hour AH to transfer) vs no AH AH: 22 women randomised, 83 embryos transferred Control: 22 women randomised, 78 embryos transferred | |
| Outcomes | Implantation, clinical pregnancy, multiple pregnancy | |
| Notes | Attempted to contact author about this study No. of embryos transferred: AH 3.7; control 3.5 Unclear whether power calculation performed ITT analysis unclear Published as abstract |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment unclear |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Unclear whether participants and assessor were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | ITT analysis unclear |
| Selective reporting (reporting bias) | Unclear risk | This publication was in abstract form only, no full paper publication was identified. Study authors do not report on live birth |
| Other bias | Unclear risk | Conference abstract |
Jelinkova 2002.
| Study characteristics | ||
| Methods | Single‐centre randomised trial | |
| Participants | 255 IVF participants only; at least 2 previous failures
Age: AH 32.3 (4.24), control 32.1 (3.16) Germany |
|
| Interventions | AH (chemical removal by acid; complete zona breach) AH: 128 women Control: 127 women |
|
| Outcomes | Clinical pregnancy rate, implantation rate | |
| Notes | Attempted to contact author about this study No. of embryos transferred: AH 2.2; control 2.2 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation stated |
| Allocation concealment (selection bias) | Unclear risk | Unclear; no details |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Unclear whether participants were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated |
| Selective reporting (reporting bias) | Unclear risk | Original protocol not viewed. Live birth not reported, so not sure if it was planned |
| Other bias | Low risk | None identified |
Kutlu 2010.
| Study characteristics | ||
| Methods | Single‐centre randomised trial | |
| Participants | 252 infertile couples receiving ART treatment at Medicana Camlica Hospital, Istanbul, Turkey. Subgrouped by prognosis: poor (n = 113) or good (n = 139) | |
| Interventions | AH was performed by laser method AH: 73 women younger than 35 years, 58 women aged 35 or over Control: 66 women younger than 35 years, 55 women aged 35 or over |
|
| Outcomes | Clinical pregnancy rate, implantation rate | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was performed in a computerised manner |
| Allocation concealment (selection bias) | Unclear risk | Not stated within the text |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated within the text |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | ITT analysis unclear |
| Selective reporting (reporting bias) | Unclear risk | Original protocol not viewed. Live birth not reported, so not sure if it was planned |
| Other bias | Low risk | None identified |
Laffoon 1999.
| Study characteristics | ||
| Methods | Single‐centre randomised trial | |
| Participants | 56 women from North America younger than 40 years undergoing IVF. Mean age not stated | |
| Interventions | AH (mechanical; complete zona breach; ? hour egg retrieval to AH; ? hour AH to transfer) vs no AH AH: 28 women randomised, embryos transferred not stated Control: 28 women randomised, embryos transferred not stated | |
| Outcomes | Clinical pregnancy | |
| Notes | Attempted to contact author about this study No. of embryos transferred not stated Unclear whether power calculation performed ITT analysis unclear Published as abstract |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Timing and method not stated |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment unclear |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Participants not blinded or unclear Assessor not blinded or unclear |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | ITT analysis unclear |
| Selective reporting (reporting bias) | High risk | Published as a conference abstract. Unable to find a full paper publication. Live birth not reported |
| Other bias | Unclear risk | Conference abstract |
Lanzendorf 1998.
| Study characteristics | ||
| Methods | Single‐centre randomised trial | |
| Participants | 94 women from North America 36 years of age or older (mean basal FSH: control 7.6 IU/L (SD 2.0); AH 7.9 IU/L (SD 2.5)), undergoing IVF (some with ICSI), half previously treated with IVF Mean age: control 38.5 (0.26); AH 38.3 (0.31) | |
| Interventions | AH by acid Tyrode's (chemical; complete zona breach; 55 hour egg retrieval to AH; ? hour AH to transfer) vs no AH AH: 42 women randomised, 180 embryos transferred Control: 52 women randomised, 212 embryos transferred | |
| Outcomes | Implantation, clinical pregnancy, multiple pregnancy, live births | |
| Notes | Attempted to contact author about this study. A reply including much useful additional information was received No. of embryos stated: AH 4.4; control 4.4 Unclear whether power calculation performed ITT analysis performed |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised; method stated |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment via sealed envelopes on day of aspiration |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants blinded Assessor blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | ITT analysis performed |
| Selective reporting (reporting bias) | Unclear risk | No evidence of selective reporting, although original protocol not viewed. Study authors did report on live birth |
| Other bias | Low risk | None identified |
Nada 2018.
| Study characteristics | ||
| Methods | Randomisation – computer‐generated list of random numbers but block randomisation with block size of 4 – allocation concealment unclear Participant blinding unclear Conducted at 2 private centres in Cairo and Beni Suif Participants not blinded or unclear Full article |
|
| Participants | 326 women Only high‐quality Day 3 embryos were used (defined as 8 to 10 cells on Day 3, < 15% fragmentation, absence of multi‐nucleation, symmetrical blastomeres, absence of ZP dysmorphism, absence of perivitelline space granularity, colourless cytoplasm with moderate granulation, no inclusions) |
|
| Interventions | LAH to dissolve 25% to 30% of ZP with 3 adjacent pulses of the laser LAH – 163 patients (5 with cycle cancellation) – 158 remaining No LAH – 163 patients (13 with cycle cancellation) remaining LAH just before transfer (no further information given) |
|
| Outcomes | Live birth rate Clinical pregnancy (defined as serum hCG > 20 IU/L and TVS confirming GS with pulsating fetal pole 4 weeks post transfer or 6 weeks post menstrual) Implantation rate (per embryo transferred, defined as number of GS present on TV USS 4 weeks after transfer/number of embryos transferred) |
|
| Notes | 2 to 3 embryos transferred per cycle Sample size calculation performed (presumed pregnancy rate of 57% and 40% in control) ITT analysis Mean age: LAH 31.27, control 32.64 Study registered on Pan African Clinical Trials Registry: PACTR201602001467322 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated list of random numbers |
| Allocation concealment (selection bias) | Unclear risk | Block randomisation with block size of 4 with 1:1 ratio of LAH vs control but no further information |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Assessor blinded to allocation No information about participants or other personnel |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 18 participants excluded after randomisation due to cycle cancellation – no reasons for cancellation given |
| Selective reporting (reporting bias) | High risk | Multiple pregnancy rate given with denominator per embryo transferred |
| Other bias | Unclear risk | No information Although registered on Pan African Clinical Trials Registry, no primary or secondary outcomes stated in trial information |
Nagy 1999.
| Study characteristics | ||
| Methods | Single‐centre randomised trial | |
| Participants | 38 women from Italy with cryopreserved embryos undergoing IVF and ICSI Mean age: control group 31.4 (3.7); AH group 32.0 (4.0) | |
| Interventions | AH (laser; complete zona breach; ? hour egg retrieval to AH; ? hour AH to transfer) with concomitant removal of damaged blastomeres vs no AH and no damaged blastomere removal AH: 20 women randomised, 65 embryos transferred Control: 18 women randomised, 52 embryos transferred | |
| Outcomes | Clinical pregnancy | |
| Notes | Attempted to contact author about this study. Reply received No. of embryos: AH: 2.9, control: 3.2 Unclear whether power calculation performed ITT analysis unclear |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation stated but method unclear or incorrect |
| Allocation concealment (selection bias) | Unclear risk | Unclear; no details |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Participants not blinded or unclear Assessor not blinded or unclear |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | ITT analysis unclear |
| Selective reporting (reporting bias) | High risk | Published as a conference abstract only. No evidence of a full paper publication. Study authors did not report on live birth |
| Other bias | Low risk | None identified |
Ng 2005.
| Study characteristics | ||
| Methods | Randomised trial | |
| Participants | 160 women from Hong Kong with frozen embryo transfer Mean age: 34.0 years | |
| Interventions | Laser‐assisted thinning 1/4 with frozen embryos compared to frozen embryos AH: 80 women Control: 80 women |
|
| Outcomes | Clinical pregnancy, miscarriage, multiple pregnancy rates | |
| Notes | No study author contact as all details clearly stated in article No. of embryos stated: AH, transferred 2 in 52.5% and 3 in 41.3%; control, transferred 2 in 36.2% and 3 in 61.3% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation |
| Allocation concealment (selection bias) | Unclear risk | 'Sealed envelopes' used but unclear if these were opaque and how they were numbered |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blinding until completion of the study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No evidence of attrition bias |
| Selective reporting (reporting bias) | Unclear risk | Original protocol not viewed. Study authors did not report on live birth |
| Other bias | Low risk | None identified |
Petersen 2005.
| Study characteristics | ||
| Methods | Randomised trial | |
| Participants | 150 women from Brazil undergoing ART cycles All participants had 1 failed treatment cycle Mean age: 34 years | |
| Interventions | ICSI cycles only
AH quarter‐laser thinning vs control AH: 35 women with 1 previous implantation failure, 40 women with repeated implantation failures Control: 35 women with 1 previous implantation failure, 40 women with repeated implantation failures |
|
| Outcomes | Live birth, clinical pregnancy, miscarriage, multiple pregnancy | |
| Notes | Study author response No. of ET: mean 2.7 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers table |
| Allocation concealment (selection bias) | Unclear risk | Unclear ‐ code ID to mask identity of participants but not clear how or who generated this |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All women randomised appear to have been analysed |
| Selective reporting (reporting bias) | Low risk | Original protocol not viewed but study authors did report on live birth |
| Other bias | Low risk | None identified |
Razi 2013.
| Study characteristics | ||
| Methods | Prospective randomised First ICSI cycle March 2009 to April 2010 Fresh ET on Day 2 |
|
| Participants | 182 infertile couples with male factor | |
| Interventions | LAH on the morning of fresh ET (Day 2 embryos) Experimental group had LAH (n = 90) Control group had no LAH (n = 92) |
|
| Outcomes | Live birth rate, multiple pregnancy rate, clinical pregnancy rate, congenital anomaly rate | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated number |
| Allocation concealment (selection bias) | Unclear risk | No information provided in article or by correspondence |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Correspondence with study author ‐ both clinicians and patients blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Appears complete |
| Selective reporting (reporting bias) | Low risk | Appears complete |
| Other bias | Low risk | None identified |
Rufas‐Sapir 2004.
| Study characteristics | ||
| Methods | Unknown randomisation method and allocation concealment. Occurred on day of embryo transfer | |
| Participants | 207 women 3 consecutive failed IVF cycles All ages Undergoing IVF only |
|
| Interventions | Mechanical partial zonal dissection: complete breach technique vs control AH ‐ 104 women Control ‐ 103 women |
|
| Outcomes | Clinical pregnancy, miscarriage | |
| Notes | Study author response AH 3.4; ET control 3.7 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unknown randomisation method |
| Allocation concealment (selection bias) | Unclear risk | Unknown allocation concealment |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Unclear |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data appear complete |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Other bias | Unclear risk | Conference abstract |
Ryan 1997.
| Study characteristics | ||
| Methods | Single‐centre randomised trial | |
| Participants | 200 women from Sydney, Australia, undergoing ART cycles | |
| Interventions | AH: Tyrode's complete breach ‐ hole chemical means on both fresh and frozen‐thawed embryos: 100 women Control: 100 women |
|
| Outcomes | Clinical pregnancy | |
| Notes | Additional information received from first author regarding definition of pregnancy. No further publication planned Mean: ET 2.17 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers table |
| Allocation concealment (selection bias) | Unclear risk | Unclear whether allocation concealed |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Unclear whether blinding took place |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All women randomised appear to have been analysed |
| Selective reporting (reporting bias) | Unclear risk | Original protocol not viewed. Study authors did not report on live birth |
| Other bias | Unclear risk | Conference abstract |
Safari 2017.
| Study characteristics | ||
| Methods | Randomised study – block randomisation – selection of blocks conducted by simple random method but no further information about allocation sequence generation of blocks Allocation concealment – block randomisation used with block size of 6 but unclear about whether there was allocation concealment from the methods described Participant blinding unclear Assessor blinding unclear No power calculation Full article Conducted at single centre in Yazd, Iran |
|
| Participants | 96 patients Previously underwent IVF or ICSI with embryo cryopreservation Day 2 or 3 vitrified‐warmed embryos at 4 to 8 cells with grade B or C (B defined as a little inequality in the size of blastomeres, < 10% cytoplasmic fragments; C defined as unequal blastomeres with < 50% fragmentation) |
|
| Interventions | Randomised into 3 arms 32 randomised to cosmetic micromanipulation and LAH (excluded from this review) 32 randomised to sham/LAH 32 randomised to control (no LAH or CM) |
|
| Outcomes | Live birth rate (unclear about what difference is in delivery rate) Delivery rate Clinical pregnancy Chemical pregnancy |
|
| Notes | Mean female age: sham/LAH 30.6, control/no LAH 29.23 Mean no. of embryos transferred: sham/LAH 2, control/no LAH 2 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Stated simple random method used for block randomisation but no details |
| Allocation concealment (selection bias) | Unclear risk | Block randomisation used with block size of 6 but unclear about whether there was allocation concealment from the methods described |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information about whether participants or outcome assessors were blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 32 randomised in Sham/LAH group; results reported only for 30 participants with no explanation given |
| Selective reporting (reporting bias) | High risk | Separate data not given for IVF and ICSI. Another cosmetic micromanipulation group also involved, which we have not used in our data |
| Other bias | High risk | Clinical pregnancy in LAH group: 7/30; live birth: 8/30; delivery rate: 7/30 |
Sagoskin 2007.
| Study characteristics | ||
| Methods | Randomised trial | |
| Participants | 199 women from USA undergoing IVF or ICSI Good prognosis group with only 1 previous implantation failure Fresh embryo transfer cycles only | |
| Interventions | Laser hatching (breach with hole) AH: 121 randomised, 118 analysed, 254 embryos; control: 82 randomised, 81 analysed, 170 embryos | |
| Outcomes | Live birth, clinical pregnancy, miscarriage, multiple pregnancy rates | |
| Notes | No study author contacted as all details clearly stated in article ET: AH 2.2 (0.4); control 2.1 (0.3) Power calculation not reported Published as a full paper |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Treatment assignments were determined by a computer‐generated randomised series at a 3:2 ratio of treatments to controls |
| Allocation concealment (selection bias) | Unclear risk | Not stated within text |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated within text |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | ITT unclear |
| Selective reporting (reporting bias) | Low risk | Live birth reported |
| Other bias | Low risk | None identified |
Shi 2016.
| Study characteristics | ||
| Methods | Prospective randomised study in China IVF and ICSI Time period of study not known Fresh ET on Day 3 |
|
| Participants | 178 patients aged 35 to < 42 years | |
| Interventions | LAH on Day 3 embryos Laser thinning of zona Experimental group had LAH (n = 82) (53 IVF and 29 ICSI) Control group had no LAH (n = 96) (70 IVF and 26 ICSI) |
|
| Outcomes | Live birth, clinical pregnancy, miscarriage, multiple pregnancy rates | |
| Notes | No loss to follow‐up in both groups Study registered on clinical trial registry at clinicaltrial.gov: NCT01765322 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | States only that patients were randomly allocated to AH group and control group but provides no details |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open‐label study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No losses to follow‐up; outcomes reported for all |
| Selective reporting (reporting bias) | Unclear risk | No information about monozygotic twins provided even though multiple pregnancy rates provided. Results for IVF/ICSI not provided separately |
| Other bias | Low risk | None identified Study reported primary and secondary outcomes as stated on clinical trials registry |
Stein 1995.
| Study characteristics | ||
| Methods | Single‐centre randomised trial | |
| Participants | 154 women from Israel with repeated implantation failure (> 3 attempts) undergoing IVF Mean age not stated | |
| Interventions | AH (mechanical; complete zona breach; ? hour egg retrieval to AH; 1.5 hour AH to transfer) vs no AH AH: 72 women randomised, 230 embryos transferred Control: 82 women randomised, 295 embryos transferred | |
| Outcomes | Clinical pregnancy, miscarriage | |
| Notes | Attempted to contact author about this study; no reply received Unclear whether power calculation performed ITT analysis unclear Published as full paper |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation stated but method unclear or incorrect |
| Allocation concealment (selection bias) | Unclear risk | Unclear; no details |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Participants not blinded or unclear Assessor not blinded or unclear |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | ITT analysis unclear |
| Selective reporting (reporting bias) | High risk | Original protocol not viewed but study authors did not report on live birth |
| Other bias | Low risk | None identified |
Tucker 1993.
| Study characteristics | ||
| Methods | Single‐centre randomised trial | |
| Participants | 218 women from North America undergoing IVF (mean basal FSH: control group 9.0 (5.3); AH group 8.8 (3.7) IU/L) Mean age: control group 34.2 (4.1); AH group 34.1 (4.8) | |
| Interventions | AH with acid Tyrode's thinning to 1/4; 72 hour egg retrieval to AH; 1 to 3 hour AH to transfer) vs no AH AH: 110 women randomised, 333 embryos transferred Control: 108 women randomised, 312 embryos transferred | |
| Outcomes | Implantation, clinical pregnancy | |
| Notes | Attempted to contact author about this study; no reply received ET: AH 2.9, control 3.0 Unclear whether power calculation performed ITT analysis unclear Published as full paper |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation stated but method unclear or incorrect |
| Allocation concealment (selection bias) | Unclear risk | Unclear; no details |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Participants not blinded or unclear Assessor not blinded or unclear |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | ITT analysis unclear |
| Selective reporting (reporting bias) | High risk | Original protocol not viewed but study authors did not report on live birth |
| Other bias | Low risk | None identified |
Tucker 1996.
| Study characteristics | ||
| Methods | Single‐centre randomised trial | |
| Participants | 100 women from North America undergoing ICSI Mean age: control group 33.5 (4.3); AH group 35.3 (4.2) | |
| Interventions | AH with acid Tyrode's (chemical; complete zona breach; 72 hour egg retrieval to AH; 4 hour AH to transfer) vs no AH AH: 50 women randomised, 189 embryos transferred Control: 50 women randomised, 184 embryos transferred | |
| Outcomes | Implantation, clinical pregnancy | |
| Notes | Attempted to contact author about this study; no reply received ET: AH 3.7, control 3.8 Unclear whether power calculation performed ITT analysis unclear |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation stated but method unclear or incorrect |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment unclear |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Participants not blinded or unclear Assessor not blinded or unclear |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Women randomised appear to be analysed |
| Selective reporting (reporting bias) | Unclear risk | Original protocol not viewed but study authors did not report on live birth |
| Other bias | Low risk | None identified |
Utsunomiya 1998.
| Study characteristics | ||
| Methods | Single‐centre randomised trial | |
| Participants | 55 women from Japan undergoing either ICSI or IVF No data provided on age | |
| Interventions | AH with acid (chemical): 27 women
No other details about the day of treatment provided Control: 28 women |
|
| Outcomes | Clinical pregnancy rate only (gestation sac on ultrasound) | |
| Notes | No attempt to contact study author No. of ETs not stated Unclear whether power calculation performed ITT analysis unclear Published as abstract only |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation stated but method unclear or incorrect |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment unclear |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Participants not blinded or unclear Assessor not blinded or unclear |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | ITT analysis unclear |
| Selective reporting (reporting bias) | High risk | Published as a conference abstract only and did not report on live births |
| Other bias | Unclear risk | Conference abstract |
Valojerdi 2010.
| Study characteristics | ||
| Methods | Single‐centre randomised trial | |
| Participants | 400 women in Iran undergoing first treatment cycle and women with previous failed cycles Mean age: control group 29.85 (5.14); AH group 30.86 (5.82) |
|
| Interventions | Partially thinned by laser AH: 200 women randomised Control: 200 women randomised |
|
| Outcomes | Clinical pregnancy, implantation rates | |
| Notes | Power calculation not reported ITT analysis unclear |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation list participants |
| Allocation concealment (selection bias) | Unclear risk | Methodological or linguistic confusion in description of allocation in the study. Sequential numbers in sealed envelopes (200 participants in each group) |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Blinding of clinician but not patient |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated |
| Selective reporting (reporting bias) | Unclear risk | Original protocol not viewed but study authors did not report on live birth |
| Other bias | Low risk | None identified |
Wan 2014.
| Study characteristics | ||
| Methods | Prospective randomised Not known whether participant had first or previous treatment IVF or ICSI June 2010 to August 2011 Fresh ET done with cleavage stage ‐ no result provided Blastocysts vitrified and randomised in 2 groups, then FET after warming |
|
| Participants | 203 infertile couples | |
| Interventions | Control group ‐ no LAH (n = 102) Experimental group ‐ had LAH (n = 101) (2 blastocysts did not survive after warming, 3 were lost to follow‐up), so total results n = 96 2 embryos (blastocysts) transferred in both groups after warming |
|
| Outcomes | Live birth rate, multiple pregnancy rate, clinical pregnancy rate, miscarriage rate | |
| Notes | Study author contacted but no response received Figure 2 and tables are contradictory due to number of participants in each group as stated in the paper; we accepted the data as described in the text and presumed that there was an error in Figure 2 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "during the study period, 203 patients who met the inclusion criteria were enrolled and randomly divided into two groups" |
| Allocation concealment (selection bias) | Unclear risk | Paper states patients "were randomly divided into two groups" but no further information provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 5 patients in the QLAH group who met the exclusion criteria were excluded from analyses (2 patients had no surviving blastocysts for transfer after warming) but 3 patients were lost to follow‐up. No patients in the control group were lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | No response from study author on further details. Live birth rate reported |
| Other bias | Unclear risk | Description of population ‐ unclear whether they had first or previous treatment |
AH: assisted hatching. ART: assisted reproductive technology. ASRM: American Society for Reproductive Medicine. CM: cosmetic micromanipulation ET: embryo transfer. FET: fresh embryo transfer. FSH: follicle‐stimulating hormone. GS: gestation sac hCG: human chorionic gonadotropin. ICSI: intracytoplasmic sperm injection. ITT: intention‐to‐treat. IVF: in vitro fertilisation. LAH: laser‐assisted hatching. QLAH: quarter laser‐assisted hatching. TV: transvaginal. TVS: transvaginal sonography. USS: ultrasound scan. ZP: zona pellucida. Mean age given in years (standard deviation). Note: only arms where all or no embryos transferred and were treated with AH were accepted for data extraction.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Abdelmassih 2002 | Pooled oocytes, then randomised; no per woman data provided |
| Amorocho 2012 | Compares technique of hatching with thickness of ZP on Day 3 of embryo development. Further details asked for but no response from study authors |
| Antinori 1996a | Not a randomised controlled trial Mentions randomly selected, not randomly allocated |
| Antinori 1996b | No randomised comparison between control and assisted hatching groups |
| Balaban 2002 | Not randomised No appropriate controls |
| Bider 1997 | Not randomised |
| Blake 2001 | Not randomised No embryo transfer occurred, so no review outcomes could be measured |
| Carter 2003a | No per woman data |
| Chao 1997 | Assessment of pregnancy was by hCG only 14 days after embryo transfer |
| Check 1996 | Not randomised Benefits of AH confounded by concurrent assessment of 2 different culture media |
| Chen 1999 | Not randomised Benefits of assisted hatching confounded by concurrent assessment of 2 different culture media |
| Chimote 2013 | Compared techniques of hatching. No information regarding randomisation method; does not suggest it is a randomised study |
| Cieslak 1999 | Comparison of 2 types of assisted hatching; no 'no assisted hatching' control group was used More than 1 cycle per woman |
| Cohen 1990 | Not randomised |
| Debrock 2011 | Primary outcome was implantation; results per embryo transfer, not per woman |
| De Croo 2013 | Implantation rate per woman reported in the abstract. Contacted for full data; no response from study authors, so excluded |
| Demirol 2003 | No pregnancy data provided |
| Dirnfeld 2003 | No hatching |
| Dokras 1994 | No appropriate outcome measure |
| Domitrz 2000 | No clear information about randomisation and allocation |
| Ebner 2002 | No per woman data |
| Edirisinghe 1999 | Not randomised |
| Feng 2009 | Not a prospective study ‐ a retrospective study |
| Figueira 2012 | Implantation and pregnancy rates provided in percentages. Date per embryo transfer. Not enough data to utilise study. Study population egg donation cryobank programme, which was not the reason for exclusion |
| Frydman 2006 | No per woman data |
| Gabrielsen 2004 | Pseudo‐randomised (alternate days) |
| Grace 2007 | No control. Comparing assisted hatching in good embryos with assisted hatching in poor embryos |
| Hershlag 1999 | Not randomised Control group from the period 1990 to 1993; assisted hatching group from 1994 to 1996 (historical controls) |
| Hiraoka 2009 | No control. Comparing half thinning vs quarter thinning |
| Hur 2011 | Not clear whether randomised; results appear to be per embryo transfer rather than per woman |
| Huttelova 1999 | Not randomised Benefits of AH confounded by concurrent assessment of 2 different culture media |
| Kanyo 2016 | Quasi‐randomisation. Randomised based on last number/digit of registration number given by administrator at the reception desk at first visit to the centre; study authors contacted but no further details obtained; therefore decision to exclude |
| Kirienko 2019 | Included cycles with donor oocytes; contacted to see whether could provide separate data for donor/autologous cycles – no reply |
| Komarovsky 2002 | No per woman data |
| Komarovsky 2003 | No per woman data |
| Le 2018 | No control arm; this is an RCT of thinning assisted hatching vs drilling assisted hatching of ZP before FET |
| Lee 1999 | Not randomised |
| Levron 2003 | No per woman data |
| Lu 2016 | Quasi‐randomised study |
| Lu 2019 | Full article demonstrated this was a retrospective study ‐ not an RCT |
| Ma 2007 | No per woman data |
| Magli 1998 | No per woman data |
| Mahadevan 1998 | Not randomised No concurrent controls |
| Mansour 2000 | Randomisation by alternate day ‐ inadequate allocation |
| Meldrum 1998 | Not randomised No concurrent controls |
| Montag 1999 | Not randomised No concurrent controls |
| Nadir 2005 | Alternate randomisation. |
| Nagy 2003 | No per woman data |
| Nakayama 1998 | No appropriate outcome measure |
| Nakayama 1999 | No per woman data |
| NCT02124291 | Study terminated for insufficient enrolment, (only 18 patients enrolled); no data available |
| Ng 2008 | No control. Compared 2 methods of laser |
| Obradors 2012 | Vitrified embryos from oocyte donation programme |
| Obruca 1994 | Not randomised No concurrent controls |
| Olivennes 1997 | No per woman data |
| Peterson 2006 | Results per embryo transfer only No per woman data |
| Ren 2013 | Study looked at effects of the site of assisted hatching on embryo comparing performing AH at the site near inner cell mass (ICM) vs performing AH at the site opposite to the ICM; there was no control group with no AH |
| Rienzi 2002 | Assisted hatching was part of the ICSI method |
| Ringler 1999 | Not clear how many women were included in the study or for how many cycles (only cycles were mentioned); mixture of participants and donated eggs was used for the study |
| Schoolcraft 1994 | Not randomised Control and intervention groups recruited at different times |
| Shahin 2003 | No per woman data |
| Sifer 2005 | Per cycle data only No per woman data |
| Szell 1998 | Not randomised Benefits of assisted hatching confounded by concurrent assessment of 2 different culture media |
| Tao 1997 | Not randomised Some of the women in the assisted hatching group were randomised but most were allocated to assisted hatching routinely, with no control option |
| Tucker 1991 | Not randomised |
| Urman 2002 | Inadequate method of allocation |
| Valojerdi 2008 | Inadequate method of allocation |
| Yano 2007 | No per woman data, only per cycle data |
| Zech 1998 | Numbers in tables do not add up correctly and text and tables are contradictory on age groups used in the prospective part of the study. Asked for clarification from authors ‐ no response |
| Zhang 2009 | Not a prospective study ‐ retrospective study |
AH: assisted hatching. FET: fresh embryo transfer. hCG: human chorionic gonadotropin. ICM: inner cell mass. ICSI: intracytoplasmic sperm injection. RCT: randomised controlled trial. ZP: zona pellucida.
Characteristics of studies awaiting classification [ordered by study ID]
Elnahas A 2018.
| Methods | Prospective randomised study |
| Participants | 120 women undergoing fresh embryo transfer and 120 women undergoing frozen embryo transfer |
| Interventions | Laser‐assisted hatching with infrared diode laser to induce zonal microdissection 60 women from fresh ET group randomised to LAH; unclear number of women in frozen ET group randomised to LAH |
| Outcomes | Clinical pregnancy rate Implantation rate |
| Notes | Study authors contacted but no reply at present |
ET: embryo transfer. LAH: laser‐assisted hatching.
Characteristics of ongoing studies [ordered by study ID]
NCT02752568.
| Study name | Assisted hatching vs endometrial scratch in recurrent Implantation failure |
| Methods | Allocation: randomised Intervention model: factorial assignment Masking: open‐label Primary purpose: treatment |
| Participants | 18 to 40 years Inclusion criteria: recurrent implantation failure, normal uterine cavity by transvaginal ultrasound |
| Interventions | Laser‐assisted hatching vs endometrial scratch vs no intervention Group 1 consists of 100 patients who will undergo endometrial scratch followed by controlled ovarian hyperstimulation; Group 2 consists of 100 patients who will undergo controlled ovarian hyperstimulation and assisted hatching; Group 3 consists of 100 patients who will undergo controlled ovarian hyperstimulation |
| Outcomes | Primary outcome measure: number of patients with positive pregnancy test |
| Starting date | April 2016 |
| Contact information | Suzy Abdelaziz; mailto:suzyabdelaziz92%40gmail.com?subject=NCT02752568, ivfobgyn, Assisted Hatching Versus Endometrial Scratch in Recurrent Implantation Failure |
| Notes |
http://apps.who.int/trialsearch/Trial2.aspx?TrialID=NCT02752568 Not yet recruiting Date first received 27 April 2016 |
NCT03623659.
| Study name | Does partial zona pellucida removal from vitrified‐warmed human blastocysts improve delivery rate in IVF? A multicentric RCT on laser assisted hatching |
| Methods | Randomised Parallel assignment Masking ‐ triple (participant, care provider, and outcome assessor) |
| Participants | 700 participants 18 to 40 years old Female Inclusion criteria: single‐embryo transfer of vitrified/warmed blastocyst (SET); first or second frozen IVF (with or without intracytoplasmic sperm injection) cycle of blastocysts; first or second oocyte retrieval Exclusion criteria: pre‐implantation genetic testing (PGT) cycle; BMI > 35 kg/m²; severe male factor; abnormal uterine cavity |
| Interventions | Active comparator: AH group Subjects whose vitrified/warmed blastocysts will be subjected to treatment of laser‐assisted hatching Procedure: laser‐assisted hatching After warming, blastocysts are subjected to laser‐assisted hatching (LAH) following standard procedure. LAH procedure lasts 1 minute per blastocyst No intervention: control group Subjects whose vitrified/warmed blastocysts will be subjected to the same procedures except for treatment of laser‐assisted hatching |
| Outcomes |
Primary outcome measures Delivery rate [time frame: 38 weeks after embryo transfer] Number of deliveries that result in a live birth per transferred blastocyst Secondary outcome measures Implantation rate [time frame: 6 to 7 weeks after transfer] • Number of gestational sacs observed at echographic screening at 6 weeks of pregnancy divided by the number of transferred embryos Clinical pregnancy rate [time frame: 4 weeks after transfer] • Ultrasonographic demonstration of an intrauterine gestational sac divided by the number of included women Biochemical pregnancy rate [time frame: 4 weeks after transfer] • Pregnancies failing to progress to the point of ultrasound confirmation divided by the number of women with a positive pregnancy test on blood Ongoing pregnancy rate [time frame: 20 weeks after transfer] • Ultrasonographic demonstration of an intrauterine gestational sac with fetal hearth divided by the number of included women Multiple pregnancy rate [time frame: 4 weeks after transfer] • Pregnancy in which more than 1 fetus develops in the uterus at the same time divided by the number of women with a clinical pregnancy Obstetrical and neonatal complication rates [time frame: after birth; 9 to 10 months after transfer] • Condition that adversely affects women and their fetal health during delivery Congenital anomalies rate [time frame: after birth, 9 to 10 months after transfer] • Birth defects, congenital disorders, congenital malformations, and congenital abnormalities are conditions of prenatal origin that are present at birth, potentially impacting an infant's health, development, and/or survival divided by the number of live births |
| Starting date | 5 September 2018 |
| Contact information | Alessandra Alteri; alteri.alessandra@hsr.it Paola Vigano; vigano.paola@hsr.it |
| Notes | ClinicalTrials.gov Identifier: NCT03623659 https://clinicaltrials.gov/ct2/show/NCT03623659?cond=assisted+hatching&draw=2&rank=4 Date first received 9 August 2018 |
NCT03810157.
| Study name | Does laser‐assisted hatching (LAH) improve the pregnancy outcomes in humans? |
| Methods | Randomised Parallel assignment |
| Participants | 1200 participants 22 to 45 years Female Inclusion criteria: patients undergoing IVF/ICSI‐ET cycle; zona pellucida of cleavage‐stage embryo thicker than 8 μm Exclusion criteria: number of embryos transferred per cycle > 2; transferred embryos including fresh and frozen cycle in the same cycle; embryos developed from frozen‐thawed oocytes |
| Interventions | Experimental: laser‐assisted hatching system Embryos were exposed to a dose of laser energy focused outside the zona pellucida by laser‐assisted hatching system Device: laser‐assisted hatching system ZP was thinned or drilled with the laser‐assisted hatching system. Laser pulse was 0.296 ms. Laser aperture was 8 μm No intervention: control group Nothing is done |
| Outcomes |
Primary outcome measure Efficacy of LAH in ART [time frame: 6 months] • Clinical pregnancy assessed Secondary outcome measure Feasibility of LAH in ART [time frame: 1 year] • Incidence of LAH adverse events assessed by miscarriage rate and multiple gestation rate |
| Starting date | 26 December 2018 |
| Contact information | Ming Wang; wangmingbio@snnu.edu.cn Tangdu Hospital, Xi'an, Shaanxi, China 710038 |
| Notes | ClinicalTrials.gov Identifier: NCT038101 https://clinicaltrials.gov/ct2/show/NCT03810157?cond=assisted+hatching&draw=2&rank=8 Other study ID number: 1215 Date first received 14 January 2019 |
NCT03833869.
| Study name | The effect of assisted hatching on implantation rate in frozen blastocyst transfer ‐ a prospective randomized controlled study |
| Methods | Current study aims to assess effects of assisted hatching on implantation rate of frozen blastocysts Randomised, parallel assignment, open‐label |
| Participants | 84 participants 18 to 39 years Female Inclusion criteria: in vitro fertilisation patients at investigators' institution intended to undergo transfer of frozen 5‐day embryo (blastocyst); 18 to 39 years old; first to third treatment cycle; previously had maximum of 4 embryos transferred Exclusion criteria: over 40 years old; congenital or acquired uterine malformations; hydrosalpinx; chronic autoimmune disease; embryo intended to undergo pre‐implantation genetic diagnosis |
| Interventions | Experimental: assisted hatching 5‐Day frozen embryos will undergo assisted hatching before embryo transfer No intervention: control 5‐Day frozen embryos will not undergo any additional procedures before embryo transfer Procedure: assisted hatching Controlled hatching of zona pellucida in the laboratory before embryo transfer |
| Outcomes |
Primary outcome measure Implantation rate [time frame: 5 to 6 weeks following embryo transfer] • Number of gestational sacs demonstrated on ultrasound divided by number of embryos transferred (expressed as percentage) Secondary outcome measures Chemical pregnancy [time frame: 5 to 6 weeks following embryo transfer] • Increase and subsequent decrease in beta hCG levels with no evidence of gestational sac on ultrasound Early spontaneous abortion [time frame: up to 15 weeks from embryo transfer] • Spontaneous abortion of pregnancy during first trimester of pregnancy |
| Starting date | 1 March 2019 |
| Contact information | Hadas Ganer Herman, MD; hadassganer@yahoo.com Edith Wolfson Medical Center, H̱olon, Israel |
| Notes | Clinicaltrials.gov identifier: NCT03833869 https://clinicaltrials.gov/ct2/show/NCT03833869 Other study ID number: 0020‐19‐WOMC Date first received 7 February 2019 |
NTR3387.
| Study name | A multicentre randomized controlled trial on the efficacy of laser assisted hatching in poor prognosis patients undergoing IVF or ICSI: the AHA trial |
| Methods | Randomised, double‐blinded |
| Participants | Repeated implantation failure |
| Interventions | In the intervention group, embryos to be transferred will undergo laser‐assisted hatching. One‐eighth of the ZP will be completely breached using the laser. Laser pulse duration should not exceed 400 µs per pulse at maximum power of 100%, corresponding to 285 mW output peak power in clinical mode. If isotherm rings are used, the rings corresponding to 60°C and higher should not contact adjacent blastomeres. Preferably, part of the ZP is selected with underneath a large area of perivitelline space or in the vicinity of an area with extensive fragmentation |
| Outcomes | Primary outcome: live birth rate Secondary outcomes: pregnancy rate, ongoing pregnancy rate, implantation rate, multiple pregnancy rate, monozygotic twinning rate, percentage of major and minor malformations in children born (assessed at birth) |
| Starting date | 2012 |
| Contact information | MHJM Curfs Fertility Centre Isala, Isala Klinieken P.O. Box 10400, Netherlands m.h.j.m.curfs@isala.nl |
| Notes |
http://apps.who.int/trialsearch/Trial2.aspx?TrialID=NTR3387 Study completed but not yet published Date first received 6 April 2012 |
AH: assisted hatching. ART: assisted reproductive technologies. ASRM: American Society of Reproductive Medicine. CM: cosmetic micromanipulation ET: embryo transfer. FET: fresh embryo transfer. FSH: follicle‐stimulating hormone. GS: gestation sac hCG: human chorionic gonadotropin. ICSI: intracytoplasmic sperm injection. ITT: intention‐to‐treat. IVF: in vitro fertilisation. LAH: laser‐assisted hatching. QLAH: quarter laser‐assisted hatching. TV: transvaginal. TVS: transvaginal sonography. USS: ultrasound scan. ZP: zona pellucida.
Differences between protocol and review
For the 2005 update, we investigated the following subgroups.
Age (when reported in the studies) ≥ 35 years.
First cycle versus previous failed cycles of IVF, ICSI, or both.
ICSI only cycles.
Chemical versus laser versus mechanical.
Thinning versus breach with hole versus complete removal.
For the 2007 update, the subgroup of poor prognosis women (age ≥ 35, poor ovulation induction, previous failed cycles, or referred to as poor prognosis women in the protocol) and new subgroups of fresh and frozen embryo transfer cycles were added.
No new subgroups were added to the 2020 update.
For the 2020 update, the review was reformatted in line with current recommended Cochrane guidance for reporting outcomes.
For the 2020 update, we added exclusion criterion: biopsied embryos were excluded (for purposes of PGS/PGD) during assisted reproduction because essentially they have largely been affected by assisted hatched with a hole made in them routinely at Day 3.
For the 2020 update, we specified which specific outcomes would be subject to sensitivity analysis. Sensitivity analysis was conducted for our primary outcomes and for clinical pregnancy, as those are the most important clinical outcomes.
Contributions of authors
Mourad Seif contributed to conceiving the review, designing the review, publishing the protocol, co‐ordinating the review, collecting data for the review, developing a search strategy, undertaking searches, screening search results, organising retrieval of papers, screening retrieved papers against inclusion criteria, arbitrating on quality and data extraction, interpreting data, providing a methodological perspective, providing a clinical perspective, providing a policy perspective, editing the review, providing general advice on the review, and performing previous work that was the foundation of the review.
Muhammad A Akhtar updated this review by extracting data, conducting analysis, and editing the review in detail.
Lauren Lacey updated this review by completing new searches, retrieving papers, screening retrieved papers against inclusion criteria, extracting data, conducting analysis, and editing the review in detail.
Sibte Hassan updated this review by completing new searches, retrieving papers, and screening retrieved papers against inclusion criteria.
Sebastian Franik updated this review by providing support in analysis and editing the review.
Sources of support
Internal sources
Central Manchester and Manchester Children's University Trust, UK
University of Manchester, UK
University of Auckland, New Zealand
External sources
Ministry of Health, New Zealand
-
Dr. Demián Glujovsky, Editor, Cochrane, Other
Translated González‐Ortega et al., 2015 (published in Spanish) and extracted data from the paper for the purposes of this review.
-
Dr. Jasmine Lee, Other
Translated Lu et al., 2016 (published in Chinese) and extracted data for the purposes of this review.
Declarations of interest
MAA, SF, SH and LL have no interests to declare. MS has received travel and accommodation support for conferences unrelated to the topic of this review.
Edited (no change to conclusions)
References
References to studies included in this review
Abulsoud 2019 {published data only}
- Abulsoud M, El-Ghareeb A, Abdel Rahman H, Al Ahwany A, Ebrahim L, Wael Ragab M. The effect of quarter laser assisted hatching of human embryos on pregnancy rates after intracytoplasmic sperm injection. International Journal of Pharmaceutical Sciences Review and Research May/June 2019;56(1):112-6. [Google Scholar]
Antinori 1999 {published data only}
- Antinori S, Versaci C, Dani L, Barbaro E, Antinori M, Cerusico C, et al. Laser assisted hatching at the extremes of the IVF spectrum: first cycle and after 6 cycles. A randomized prospective trial [abstract]. Fertility and Sterility 1999;72(3 Suppl 1):S111. [Google Scholar]
Balaban 2006 {published data only}
- Balaban B, Urman B, Yakin K, Isiklar A. Laser assisted hatching increases pregnancy and implantation rates in cryopreserved embryos that were allowed to cleave in-vitro after thawing: a prospective randomised study. Human Reproduction 2006;21(8):2136-40. [DOI] [PubMed] [Google Scholar]
Balakier 2009 {published data only}
- Balakier H, Mandel R, Sojecki A, Motamedi G, Zaver S, Librach C. Laser zona thinning in women aged < or = 37 years: a randomized study. Fertility and Sterility 2009;91(4 Suppl):1479-82. [PMID: ] [DOI] [PubMed] [Google Scholar]
Baruffi 2000 {published data only}
- Baruffi RL, Mauri AL, Petersen CG, Ferreira RC, Coelho J, Franco JG. Zona thinning with noncontact diode laser in patients aged < or = 37 years with no previous failure of implantation: a prospective randomized study. Journal of Assisted Reproduction and Genetics 2000;17(10):557-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carter 2003 {published and unpublished data}
- Carter J, Graham J, Han T, Davis A, Richter K, Widra E. Preliminary results of a prospective randomized study to assess the value of laser assisted hatching before cleavage stage embryo transfer among good-prognosis in vitro fertilization (IVF) patients. Fertility and Sterility 2003;80 Suppl 3:S94. [Google Scholar]
Ciray 2005 {published data only}
- Ciray HN, Bener F, Karagenc L, Ulug U, Bahceci M. Impact of assisted hatching on ART outcome in women with endometriosis. Human Reproduction 2005;20(9):2546-9. [DOI] [PubMed] [Google Scholar]
Cohen 1992 {published data only}
- Cohen J, Alikani M, Trowbridge J, Rosenwaks Z. Implantation enhancement by selective assisted hatching using zona drilling of human embryos with poor prognosis. Human Reproduction 1992;7(5):685-91. [DOI] [PubMed] [Google Scholar]
- Liu H-C, Alikani M, Cohen J, Rosenwaks Z. Assisted hatching facilitates earlier implantation after IVF-ET. In: Fertility and Sterility Abstracts. Vol. 58. 1992:61 (O-136). [PubMed]
- Liu H-C, Cohen J, Alikani M, Noyes N, Rosenwaks Z. Assisted hatching facilitates earlier implantation. Fertility and Sterility 1993;60(5):871-5. [PubMed] [Google Scholar]
Elhelw 2005 {published data only}
- Elhelw B, El Sadek MM, Al Nomrosy KM. Laser assisted hatching may enhance implantation and pregnancy rates on cryopreserved-thawed embryos in patients with repeated implantation failures. A prospective randomised study. In: ESHRE Copenhagen - poster abstract. 2005.
Elnahas 2017 {published data only}
- Elnahas T, Tawab N, Azmy O, Elnoury A, El-Faissal Y, Fouad T, et al. Prospective randomized trial on the use of laser assisted hatching for transfer of frozen/thawed embryos in human intracytoplasmic sperm injection. Middle East Fertility Society Journal 2017;22(4):309–12. [Google Scholar]
Fang 2010 {published data only}
- Fang C, Li T, Miao BY, Zhuang GL, Zhou C. Mechanically expanding the zona pellucida of human frozen thawed embryos: a new method of assisted hatching. Fertility and Sterility 2010;94(4):1302-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Ge 2008 {published data only}
- Ge HS, Zhou W, Zhang W, Lin JJ. Impact of assisted hatching on fresh and frozen-thawed embryo transfer cycles: a prospective, randomized study. Reproductive Biomedicine Online 2008;16(4):589-96. [PMID: ] [DOI] [PubMed] [Google Scholar]
Germond 2004 {published data only}
- Primi M-P, Senn A, Montag M, Van der Ven H, Mandelbaum J, Veiga A, et al. A European multicentre prospective randomized study to assess the use of assisted hatching with a diode laser and the benefit of immunosuppressive/antibiotic treatment in different patient populations. Human Reproduction 2004;19(10):2325-33. [DOI] [PubMed] [Google Scholar]
González‐Ortega 2015 {published data only}
- González-Ortega C, Cancino-Villarreall P, Anaya-Torres FJ, Pérez-Peña E, Gutiérrez-Gutiérrez AM. Impact of laser-assisted hatching (quarter technique) in poor prognosis patients. Ginecologia y Obstetricia de Mexico 2015;83(11):670-9. [PubMed] [Google Scholar]
Hagemann 2010 {published data only}
- Desai SG, Cooper AR, Hagemann AR, Odem RR, Ratts VS, Jungheim ES. Assisted hatching may benefit young women with a poor ovarian response. Fertility & Sterility 2013;100(3 Suppl):S506. [Google Scholar]
- Hagemann AR, Lanzendorf SE, Jungheim ES, Chang AS, Ratts VS, Odem RR. A prospective, randomized, double-blinded study of assisted hatching in women younger than 38 years undergoing in vitro fertilization. Fertility & Sterility 2010;93(2):586-91. [PMID: ] [DOI] [PubMed] [Google Scholar]
Hellebaut 1996 {published and unpublished data}
- Hellebaut S, De Sutter P, Dozortsev D, Onghena A, Qian C, Dhont M. Does assisted hatching improve implantation rates after in vitro fertilization or intracytoplasmic sperm injection in all patients? A prospective randomized study. Journal of Assisted Reproduction and Genetics 1996;13(1):19-22. [DOI] [PubMed] [Google Scholar]
Hurst 1998 {published and unpublished data}
- Hurst BS, Tucker KE, Awoniyi CA, Schlaff WD. Assisted hatching does not enhance IVF success in good-prognosis patients. Journal of Assisted Reproduction and Genetics 1998;15(2):62-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Isik 2000 {published data only}
- Isik AZ, Vicdan K, Kaba A, Dagli G. Comparison of zona manipulated and zona intact blastocyst transfers: a prospective randomized trial. Journal of Assisted Reproduction and Genetics 2000;17(3):135-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Isiklar 1999 {published data only}
- Isiklar A, Balaban B, Aksoy S, Alatas C, Mercan R, Nuhoglu A, et al. The effect of mechanical assisted hatching on progression of cleavage stage embryos to the blastocyst stage [abstract]. Fertility & Sterility 1999;72(3 Suppl 1):S162. [Google Scholar]
Jelinkova 2002 {published data only}
- Jelinkova L, Pavelkova J, Reeka N, Paulus W, Zivny J, Sterzik K. Chemical removal of the zona pellucida improves implantation. Human Reproduction 2002;17:131. [DOI] [PubMed] [Google Scholar]
- Jelinkova L, Pavelkova J, Strehler E, Paulus W, Zivny J, Sterzik K. Improved implantation rate after chemical removal of the zona pellucida. Fertility & Sterility 2003;79 Suppl 6:1299-303. [DOI] [PubMed] [Google Scholar]
Kutlu 2010 {published data only}
- Kutlu P, Atwar O, Vanlioglu OF. Laser assisted zona thinning technique has no beneficial effect on the ART outcomes of two different maternal age groups. Journal of Assisted Reproduction and Genetics 2010;27(8):457-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
Laffoon 1999 {published data only}
- Laffoon IS, Sokoloski JE, Volk EA, Hughes L, Krivinko DM, Sanfilippo JS, et al. The effect of assisted hatching on the outcome of assisted reproductive technology cycles in women under 39 years of age [abstract]. Fertility & Sterility 1999;72(3 Suppl 1):S243. [Google Scholar]
Lanzendorf 1998 {published and unpublished data}
- Lanzendorf SE, Nehchiri F, Mayer JF, Oehninger S, Muasher SJ. A prospective, randomized, double-blind study for the evaluation of assisted hatching in patients with advanced maternal age. Human Reproduction 1998;13(2):409-13. [DOI] [PubMed] [Google Scholar]
Nada 2018 {published data only}
- Nada M, El‐Noury A, Al‐Inany H, Bibars M, Taha T, Salama S, et al. Effect of laser‐assisted zona thinning, during assisted reproduction, on pregnancy outcome in women with endometriosis: randomized controlled trial. Archives of Gynecology and Obstetrics 2018;297(2):521–8. [DOI] [PubMed] [Google Scholar]
Nagy 1999 {published data only}
- Nagy ZP, Rienzi L, Iacobelli M, Morgia F, Ubaldi F, Schimberni M, et al. Laser-assisted hatching and removal of degenerated blastomere(s) of frozen-thawed embryos improves pregnancy rate [abstract]. Fertility & Sterility 1999;72(3 Suppl 1):S4. [Google Scholar]
Ng 2005 {published data only}
- Ng EHY, Naveed F, Lau EYL, Yeung WSB, Chan CCWC, Tang OS, et al. A randomized double-blind controlled study of the efficacy of laser-assisted hatching on implantation and pregnancy rates of frozen-thawed embryo transfer at the cleavage stage. Human Reproduction 2005;20:979-85. [DOI] [PubMed] [Google Scholar]
Petersen 2005 {published data only}
- Petersen CG, Mauri AL, Baruffi RL, Oliveira JBA, Massaro FC, Elder K, et al. Implantation failures: success of assisted hatching with quarter-laser zona thinning. Reproductive Biomedicine Online 2005;10 Suppl 2:224-9. [DOI] [PubMed] [Google Scholar]
Razi 2013 {published data only}
- Razi MH, Halvaei I, Razi Y. Laser assisted zona hatching does not improve live birth rate in patients undergoing their first ICSI cycles. Iranian Journal of Reproductive Medicine 2013;11(12):1021-6. [PMC free article] [PubMed] [Google Scholar]
Rufas‐Sapir 2004 {published data only}
- Rufas-Sapir O, Stein A, Orvieto R, Avrech OM, Kotler N, Pinkas H, et al. Is assisted hatching beneficial in patients with recurrent implantation failures. Clinical & Experimental Obstetrics & Gynecology 2004;31 Suppl 2:110-2. [PubMed] [Google Scholar]
Ryan 1997 {published data only}
- Ryan JP, Pike IL, Catt JW, Porter RN, Saunders DM. Failure of assisted hatching to increase pregnancy rates following the transfer of fresh or frozen-thawed day 2 human embryos. In: Human Reproduction Abstracts of 13th Annual Meeting of the ESHRE. 1997:188.
Safari 2017 {published data only}
- Safari S, Khalili M, Barekati Z, Halvaei I, Anvari M, Nottola S. Cosmetic micromanipulation of vitrified-warmed cleavage stage embryos does not improve ART outcomes: an ultrastructural study of fragments. Reproductive Biology 2017;17:210–7. [DOI] [PubMed] [Google Scholar]
Sagoskin 2007 {published data only}
- Sagoskin AW, Levy MJ, Tucker MJ, Richter KS, Widra EA. Laser assisted hatching in good prognosis patients undergoing in vitro fertilisation embryo transfer: a randomised controlled trial. Fertility & Sterility 2007;87(2):283-7. [DOI] [PubMed] [Google Scholar]
Shi 2016 {published data only}
- Shi W, Hongwei T, Zhang W, Li N, Li M, Li W, et al. A prospective randomized controlled study of laser-assisted hatching on the outcome of first fresh IVF-ET cycle in advanced age women. Reproductive Sciences 2016;23(10):1397-401. [DOI] [PubMed] [Google Scholar]
Stein 1995 {published data only}
- Stein A, Rufas O, Amit S, Avrech O, Pinkas H, Ovadia J, et al. Assisted hatching by partial zona dissection of human pre-embryos in patients with recurrent implantation failure after in vitro fertilization. Fertility & Sterility 1995;63(4):838-41. [DOI] [PubMed] [Google Scholar]
Tucker 1993 {published data only}
- Tucker MJ, Luecke NM, Wiker SR, Wright G. Chemical removal of the outside of the zona pellucida of day 3 human embryos has no impact on implantation rate. Journal of Assisted Reproduction and Genetics 1993;10(3):187-91. [DOI] [PubMed] [Google Scholar]
Tucker 1996 {published data only}
- Tucker MJ, Morton PC, Wright G, Ingargiola PE, Sweitzer CL, Elsner CW, et al. Enhancement of outcome from intracytoplasmic sperm injection: does co-culture or assisted hatching improve implantation rates? Human Reproduction 1996;11(11):2434-7. [DOI] [PubMed] [Google Scholar]
Utsunomiya 1998 {published data only}
- Utsunomiya T, Sato M, Hirotsuru K. Assisted hatching by zona thinning to multiple-failure in vitro fertilization patients [abstract]. Fertility & Sterility 1998;70(3 Suppl 1):S328. [Google Scholar]
Valojerdi 2010 {published data only}
- Valojerdi MR, Eftekhari-Yazdi P, Karimian L, Hassani F, Movaghar B. Effect of laser zona thinning on vitrified-warmed embryo transfer at the cleavage stage: a prospective, randomized study. Reproductive Biomedicine Online 2010;20(2):234-42. [PMID: ] [DOI] [PubMed] [Google Scholar]
Wan 2014 {published data only}
- Wan C-Y, Song C, Diao L-H, Li G-G, Bao Z-J, Hu X-D, et al. Laser-assisted hatching improves clinical outcomes of vitrified-warmed blastocysts developed from low-grade cleavage-stage embryos: a prospective randomized study. Reproductive Biomedicine Online 2014;28(5):582-9. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Abdelmassih 2002 {published data only}
- Abdelmassih S, Cardoso J, Abdelmassih V, Dias JA, Abdelmassih R, Nagy ZP. Laser-assisted ICSI: a novel approach to obtain higher oocyte survival and embryo quality rates. Human Reproduction 2002;17 Suppl 10:2694-7. [DOI] [PubMed] [Google Scholar]
Amorocho 2012 {published data only}
- Amorocho B, Calderon G, Gumbao D, Sanchez A, Molla M, Landeras JTI. The effect of the thickness of the zona pellucida using LAH (laser assisted hatching) or not in IVF/ICSI cycles for two age groups. Fertility & Sterility 2012;98 Suppl 1(3):S257. [Conference abstract] [Google Scholar]
Antinori 1996a {published data only}
- Antinori S, Selman HA, Caffa B, Panci C, Dani G, Versaci C. Zona opening of human embryos using a non-contact UV laser for assisted hatching in patients with poor prognosis of pregnancy. Human Reproduction 1996;11:2488-92. [DOI] [PubMed] [Google Scholar]
Antinori 1996b {published data only}
- Antinori S, Panci C, Selman HA, Caffa B, Dani G, Versaci C. Zona thinning with the use of laser: a new approach to assisted hatching in humans. Human Reproduction 1996;11:590-4. [DOI] [PubMed] [Google Scholar]
Balaban 2002 {published data only}
- Balaban B, Urman B, Alatas C, Mercan R, Mumcu A, Isiklar A. A comparison of four different techniques of assisted hatching. Human Reproduction 2002;17:1239-43. [DOI] [PubMed] [Google Scholar]
Bider 1997 {published data only}
- Bider D, Livshits A, Yonish M, Yemini Z, Mashiach S, Dor J. Assisted hatching by zona drilling of human embryos in women of advanced age. Human Reproduction 1997;12:317-20. [DOI] [PubMed] [Google Scholar]
Blake 2001 {published data only}
- Blake CA, Forsberg AS, Johansson BR, Wikland M. Laser zona pellucida thinning - an alternative approach to assisted hatching. Human Reproduction 2001;16(9):1959-64. [DOI] [PubMed] [Google Scholar]
Carter 2003a {published data only}
- Carter J, Graham J, Han T, Davis A, Richter K, Widra E. Preliminary results of a prospective randomized study to assess the value of laser assisted hatching before cleavage stage embryo transfer among good-prognosis in vitro fertilization (IVF) patients. Fertility & Sterility 2003;80 Suppl 3:S94. [Google Scholar]
Chao 1997 {published data only}
- Chao KH, Chen SU, Chen HF, Wu MY, Yang YS, Ho HN. Assisted hatching increases the implantation and pregnancy rate of in vitro fertilization (IVF)-embryo transfer (ET), but not that of IVF-tubal ET in patients with repeated IVF failures. Fertility & Sterility 1997;67:904-8. [DOI] [PubMed] [Google Scholar]
Check 1996 {published data only}
- Check JH, Hoover L, Nazari A, O'Shaughnessy A, Summers D. The effect of assisted hatching on pregnancy rates after frozen embryo transfer. Fertility & Sterility 1996;65:254-7. [DOI] [PubMed] [Google Scholar]
Chen 1999 {published data only}
- Chen C, Kattera S, Lim MN. Improved pregnancy rates in assisted reproduction using assisted hatching and delayed embryo transfer. In: Proceedings of the 11th World Congress on In Vitro Fertilization and Human Reproductive Genetics, Bologna, Italy. Monduzzi, 1999:169-72.
Chimote 2013 {published data only}
- Chimote NM, Chimote NN, Nath NM, Mehta BN. Transfer of spontaneously hatching or hatched blastocyst yields better pregnancy rates than expanded blastocyst transfer. Journal of Human Reproductive Sciences 2013;6(3):183-218. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cieslak 1999 {published data only}
- Cieslak J, Ivakhnenko V, Wolf G, Sheleg S, Verlinsky Y. Three-dimensional partial zona dissection for preimplantation genetic diagnosis and assisted hatching. Fertility & Sterility 1999;71(2):308-13. [DOI] [PubMed] [Google Scholar]
Cohen 1990 {published data only}
- Cohen J, Elsner C, Kort H, Malter H, Massey J, Mayer MP, et al. Impairment of the hatching process following IVF in the human and improvement of implantation by assisting hatching using micromanipulation. Human Reproduction 1990;5(1):7-13. [DOI] [PubMed] [Google Scholar]
Debrock 2011 {published data only}
- Debrock D, Peeraer K, Spiessens C, Willeman D, De Loecker P, D'Hooghe TM. The effect of modified quarter laser-assisted zona hardening on the implantation rate per embryo in frozen/vitrified-thawed/warmed embryo transfer cycles: a prospective randomized controlled trial. Human Reproduction 2011;26:1997-2007. [DOI] [PubMed] [Google Scholar]
De Croo 2013 {published data only}
- De Croo I, Vanden Meerschaut F, Van Steelandt S, Van den Abbeel E, De Sutter P. Prospective, randomized trial on the effect of laser assisted hatching on frozen-thawed embryo transfer cycles. Fertility & Sterility 2013;100 Suppl(3):S16. [conference abstract] [Google Scholar]
Demirol 2003 {published data only}
- Demirol A, Sari T, Gurgan T. Comparison of the laser-assisted ICSI and conventional ICSI results in recurrent ICSI failure patients with few oocytes. Human Reproduction 2003;18 Suppl 1:61. [Google Scholar]
Dirnfeld 2003 {published data only}
- Dirnfeld M, Shiloh H, Bider D, Harari E, Koifman M, Lahav Baratz S, et al. A prospective randomized controlled study of the effect of short coincubation of gametes during insemination on zona pellucida thickness. Gynecological Endocrinology 2003;17:397-403. [DOI] [PubMed] [Google Scholar]
Dokras 1994 {published data only}
- Dokras A, Ross C, Gosden B, Sargent IL, Barlow DH. Micromanipulation of human embryos to assist hatching. Fertility & Sterility 1994;61:514-20. [DOI] [PubMed] [Google Scholar]
Domitrz 2000 {published data only}
- Domitrz J, Wolczynski S, Syrewicz M, Kuczynski W, Szamatowicz J, Grochowski D, et al. Enzymatic assisted hatching in the infertile couple after failed attempts IVF ET. Ginekologia Polska 2000;71:1047-52. [PubMed] [Google Scholar]
Ebner 2002 {published data only}
- Ebner T, Moser M, Yaman C, Sommergruber M, Hartl J, Jesacher K, et al. Prospective hatching of embryos developed from oocytes exhibiting difficult oolemma penetration during ICSI. Human Reproduction 2002;17:1317-20. [DOI] [PubMed] [Google Scholar]
Edirisinghe 1999 {published data only}
- Edirisinghe WR, Ahnonkitpanit V, Promviengchai S, Suwajanakorn S, Pruksananonda K, Chinpilas V, et al. A study failing to determine significant benefits from assisted hatching: patients selected for advanced age, zonal thickness of embryos, and previous failed attempts. Journal of Assisted Reproduction and Genetics 1999;16:294-301. [DOI] [PMC free article] [PubMed] [Google Scholar]
Feng 2009 {published data only}
- Feng HL, Hershlag A, Scholl GM, Cohen MA. A retro-prospective study comparing three different assisted hatching techniques. Fertility & Sterility 2009;91(4 Suppl):1323-5. [PMID: ] [DOI] [PubMed] [Google Scholar]
Figueira 2012 {published data only}
- Braga DPAF, Figueira RCS, Setti AS, Colturato SS, Iaconelli A Jr, Borges E Jr. Relevância do assited hatching com laser em um programa de ovo-doação utilizando banco de óvulos criopreservados: um estudo prospectivo randomizado. Jornal Brasileiro de Reproducao Assistida 2011;15(3):34-7. [Google Scholar]
- Figueira R, Paes D, Setti A, Iaconelli A, Borges E. Relevance of assisted hatching in an oocyte donation programme using egg cryobanking: a prospective randomised study. European Journal of Obstetrics & Gynecology and Reproductive Biology 2012;164(1):48-51. [DOI] [PubMed] [Google Scholar]
Frydman 2006 {published data only}
- Frydman N, Madoux S, Hesters L, Duvernoy C, Feyereisen E, Le Du A, et al. A randomised double-blind controlled study on the efficacy of laser zona pellucida thinning on live birth rates in cases of advanced female age. Human Reproduction 2006;21(8):2131-5. [DOI] [PubMed] [Google Scholar]
Gabrielsen 2004 {published data only}
- Gabrielsen A, Agerholm I, Toft B, Hald F, Petersen K, Aagaard J, et al. Assisted hatching improves implantation rates on cryopreserved-thawed embryos: a randomized prospective study. Human Reproduction 2004;19:2258-62. [DOI] [PubMed] [Google Scholar]
Grace 2007 {published data only}
- Grace J, Bolton V, Braude P, Khalaf Y. Assisted hatching is more effective when embryo quality was optimal in previous failed IVF/ICSI cycles. Journal of Obstetrics and Gynaecology 2007;27(1):56-60. [PMID: ] [DOI] [PubMed] [Google Scholar]
Hershlag 1999 {published data only}
- Hershlag A, Paine T, Cooper GW, Scholl GM, Rawlinson K, Kvapil G. Monozygotic twinning associated with mechanical assisted hatching. Fertility & Sterility 1999;71(1):144-6. [DOI] [PubMed] [Google Scholar]
Hiraoka 2009 {published data only}
- Hiraoka K, Hiraoka K, Horiuchi T, Kusuda T, Okano S, Kinutani M, et al. Impact of the size of zona pellucida thinning area on vitrified-warmed cleavage-stage embryo transfers: a prospective, randomized study. Journal of Assisted Reproduction and Genetics 2009;26(9-10):515-21. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hur 2011 {published data only}
- Hur YS, Park JH, Ryu EY, Yoon HJ, Yoon SH, Hur CY, et al. Effect of artificial shrinkage on outcome in fresh blastocyst transfer cycles. Clinical and Experimental Reproductive Medicine 2011;38(2):87-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
Huttelova 1999 {published data only}
- Huttelova R, Becvarova V, Mardesic T, Muller P, Hulvert J, Voboril J. Assisted hatching combined with long-term culture. In: Proceedings of the 11th World Congress on In Vitro Fertilization & Human Reproductive Genetics, Bologna, Italy. Monduzzi, 1999:169-72.
Kanyo 2016 {published data only}
- Kanyo K, Zeke J, Kriston, R, Szücs Z, Cseh S, Somoskoi B, Konc J. The impact of laser-assisted hatching on the outcome of frozen human embryo transfer cycles. Zygote 2016;24(5):742-7. [DOI] [PubMed] [Google Scholar]
Kirienko 2019 {published data only}
- Kirienko K, Apryshko V, Naumova A, Kharitonova M, Klepukov A, Bolt A, et al. Mechanical zona pellucida removal of vitrified-warmed human blastocysts does not affect the clinical outcome. RBMO 2019;39(5):745-9. [DOI] [PubMed] [Google Scholar]
Komarovsky 2002 {published data only}
- Komarovsky D, Strassburger D, Raziel A, Kasterstein E, Schachter M, Friedler S, et al. A prospective randomized trial of assisted hatching in cryopreserved embryo transfer. Human Reproduction 2002;17:76. [Google Scholar]
Komarovsky 2003 {published data only}
- Komarovsky D, Bern O, Kasterstein E, Strassburger D, Raziel A, Friedler S, et al. A prospective randomized comparison between laser and chemically-assisted hatching in thawed embryo transfers. Human Reproduction 2003;18 Suppl 1:77. [Google Scholar]
Le 2018 {published data only}
- Le MT, Nguyen TTA, Nguyen TTT, Nguyen VT, Le DD, Nguyen VQH, et al. Thinning and drilling laser-assisted hatching in thawed embryo transfer: a randomized controlled trial. Clinical and Experimental Reproductive Medicine 2018;45(3):129-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lee 1999 {published data only}
- Lee JE, Lee DR, Paik HR, Shim HN, Cho JH, Roh SI, et al. Biochemical assisted hatching (BAH) increased the implantation and pregnancy rate in human cryopreserved embryo transfer [abstract]. Fertility & Sterility 1999;72(3 Suppl 1):S4-S5. [Google Scholar]
Levron 2003 {published data only}
- Levron J, Ferber Meiri B, Bider D, Shulman A, Levin T, Shporn E. A prospective randomized study comparing laser and tyrode's medicated methods of assisted hatching. Fertility & Sterility 2003;80 Suppl 3:S202. [Google Scholar]
Lu 2016 {published data only}
- Lu X-M, Xu C, Wang L, Sun N-X, Zhang Q, Guan P-F, et al. Effect of laser-assisted hatching on outcome of frozen-thawed embryo transfer for patients with previous repeated implantation failure. Academic Journal of Second Military Medical University 2016;37(1):106-10. [Google Scholar]
Lu 2019 {published data only}
- Lu X, Liu Y, Cao X, Liu S, Dong X. Laser-assisted hatching and clinical outcomes in frozen-thawed cleavage-embryo transfers of patients with previous repeated failure. Lasers in Medical Science 2019;34:1137-45. [DOI] [PubMed] [Google Scholar]
Ma 2007 {published data only}
- Ma S, Rowe T, Ho Yuen B. Impact of assisted hatching on the outcome of intracytoplasmic sperm injection: a prospective, randomized clinical trial and pregnancy follow-up. Fertility & Sterility 2006;85(4):895-900. [DOI] [PubMed] [Google Scholar]
Magli 1998 {published and unpublished data}
- Magli MC, Gianaroli L, Ferraretti AP, Fortini D, Aicardi G, Montanaro N. Rescue of implantation potential in embryos with poor prognosis by assisted zona hatching. Human Reproduction 1998;13(5):1331-5. [DOI] [PubMed] [Google Scholar]
Mahadevan 1998 {published data only}
- Mahadevan MM, Miller MM, Maris MO, Moutos D. Assisted hatching of embryos by micromanipulation for human in vitro fertilization: UAMS experience. Journal of the Arkansas Medical Society 1998;94:529-31. [PubMed] [Google Scholar]
Mansour 2000 {published data only}
- Mansour RT, Rhodes CA, Aboulghar MA, Serour GI, Kamal A. Transfer of zona-free embryos improves outcomes in poor prognosis patients: a prospective randomised controlled study. Human Reproduction 2000;15:1061-4. [DOI] [PubMed] [Google Scholar]
Meldrum 1998 {published data only}
- Meldrum DR, Wisot A, Yee B, Garzo G, Yeo L, Hamilton F. Assisted hatching reduces the age-related decline in IVF outcome in women younger than age 43 without increasing miscarriage or monozygotic twinning. Journal of Assisted Reproduction and Genetics 1998;15:418-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Montag 1999 {published data only}
- Montag M, Ven H. Laser-assisted hatching in assisted reproduction. Croatian Medical Journal 1999;40:398-403. [PubMed] [Google Scholar]
Nadir 2005 {published data only}
- Nadir Ciray H, Bener F, Karagenç L, Ulug U, Bahçeci M. Impact of assisted hatching on ART outcome in women with endometriosis. Human Reproduction 2005;20(9):2546-9. [DOI] [PubMed] [Google Scholar]
Nagy 2003 {published data only}
- Nagy ZP, Toledo A, Mitchell Leef D, Elsner C, Massey J, Kort H. A prospective randomized study to evaluate the effect of laser micro-hole drilling of zona pellucida prior to ICSI on implantation and pregnancy results. Human Reproduction 2003;18 Suppl 1:60-1. [Google Scholar]
Nakayama 1998 {published data only}
- Nakayama T, Fujiwara H, Tastumi K, Fujita K, Higuchi T, Mori T. A new assisted hatching technique using a piezo-micromanipulator. Fertility & Sterility 1998;69(4):784-8. [DOI] [PubMed] [Google Scholar]
Nakayama 1999 {published data only}
- Nakayama T, Fujiwara H, Yamada S, Tastumi K, Honda T, Fujii S. Clinical application of a new assisted hatching method using piezo-micromanipulator for morphologically low-quality embryos in poor-prognosis infertile patients. Fertility & Sterility 1999;71(6):1014-8. [DOI] [PubMed] [Google Scholar]
NCT02124291 {unpublished data only}
- NCT02124291. Effect of assisted hatching on vitrified embryo transfer clinical outcome (VitHatSZMC). http://apps.who.int/trialsearch/Trial2.aspx?TrialID=NCT02124291 (registered 23 April 2014).
Ng 2008 {published data only}
- Ng EH, Lau EY, Yeung WS, Cheung TM, Tang OS, Ho PC. Randomized double-blind comparison of laser zona pellucida thinning and breaching in frozen-thawed embryo transfer at the cleavage stage. Fertility & Sterility 2008;89(5):1147-53. [PMID: ] [DOI] [PubMed] [Google Scholar]
Obradors 2012 {published data only}
- Obradors A, Durban M, Pujol A, Vassena R, Coll O, Vernaeve V. Assisted hatching does not improve implantation rates when key factors are controlled for: time to stop using it? Fertility & Sterility 2013;98(3 Suppl 1):S57. [conference abstract] [Google Scholar]
Obruca 1994 {published data only}
- Obruca A, Strohmer H, Sakkas D, Menezo Y, Kogosowski A, Barak Y. Use of lasers in assisted fertilization and hatching. Human Reproduction 1994;9:1723-6. [DOI] [PubMed] [Google Scholar]
Olivennes 1997 {published data only}
- Olivennes F, Hazout AD. A prospective randomized study of the use of assisted hatching in IVF-ET patients with high day-3 FSH. Increased clinical pregnancy rate with assisted hatching but high rate of miscarriages. In: Fertility and Sterility. Abstracts of the Meeting of the American Society for Reproductive Medicine. 1997:S227.
Peterson 2006 {published data only}
- Peterson C, Mauri A, Baruffi R, Oliveira J, Felipe V, Massaro F, et al. Laser-assisted hatching of cryopreserved-thawed embryos by thinning one quarter of the zona. Reproductive BioMedicine Online 2006;13(5):668-75. [DOI] [PubMed] [Google Scholar]
Ren 2013 {published data only}
- Ren X, Liu Q, Chen W, Zhu G, Zhang H. Effect of the site of assisted hatching on vitrified-warmed blastocyst transfer cycles: a prospective randomized study. Journal of Assisted Reproduction and Genetics 2013;30(5):691-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rienzi 2002 {published data only}
- Rienzi L, Ubaldi F, Iacobelli M, Martinez F, Ferrero S, Greco E. Controlled comparison of ICSI and laser-assisted ICSI in low responder patients. Human Reproduction 2002;17:36. [Google Scholar]
Ringler 1999 {published data only}
- Ringler GE, Marrs RP, Stein AL, Varygas JM, Schiewe MC. Improved pregnancy rates using assisted hatching on day 3 frozen-thawed embryos [abstract]. Fertility & Sterility 1999;72(3 Suppl 1):S86. [Google Scholar]
Schoolcraft 1994 {published data only}
- Schoolcraft WB, Schlenker T, Gee M, Jones GS, Jones HW. Assisted hatching in the treatment of poor prognosis in vitro fertilization candidates. Fertility & Sterility 1994;62(3):551-4. [DOI] [PubMed] [Google Scholar]
Shahin 2003 {published data only}
- Shahin A, Krussel JS, Sayed EH, Ahmed AG, Al Hussaini TK, Hirchenhain J. A prospective randomized study on laser assisted hatching in good prognosis patients. Human Reproduction 2003;18 Suppl 1:53. [Google Scholar]
Sifer 2005 {unpublished data only}
- Sifer C, Sellami A, Martin-Pont B, Bottero J, Porcher R, Poncelet C, et al. A prospective randomised study to assess the benefit of zona pellucida partial digestion prior to frozen-thawed embryo transfers. In: ESHRE Copenhagen - oral abstract. 2005. [DOI] [PubMed]
- Sifer C, Sellami A, Poncelot C, Kulski P, Martin-Pont B, Bottero J, et al. A prospective randomised study to assess the benefit of zona pellucida partial digestion prior to frozen-thawed embryo transfers. In: ESHRE Copenhagen - oral abstract, 2005. Human Reproduction 2006;21(9):2384-9. [DOI] [PubMed] [Google Scholar]
Szell 1998 {published data only}
- Szell AZ, Antaran JM, Chetkowski RJ. Pregnancy and implantation rates from the transfer of human embryos cultured in P1 or human tubal fluid medium and transferred with or without assisted hatching. Fertility & Sterility 1998;70:S495. [Google Scholar]
Tao 1997 {published data only}
- Tao J, Tamis R. Application of assisted hatching for 2-day-old, frozen-thawed embryo transfer in a poor prognosis population. Journal of Assisted Reproduction and Genetics 1997;14(2):128-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tucker 1991 {published data only}
- Tucker MJ, Cohen J, Massey JB, Mayer MP, Wiker SR, Wright G. Partial dissection of the zona pellucida of frozen-thawed human embryos may enhance blastocyst hatching, implantation and pregnancy rates. American Journal of Obstetrics and Gynecology 1991;165(2):342-5. [DOI] [PubMed] [Google Scholar]
Urman 2002 {published data only}
- Urman B, Balaban B, Alatas C, Aksoy S, Mumcu A, Isiklas A. Zona-intact versus zona-free blastocyst transfer: a prospective randomised study. Fertility & Sterility 2002;70(3 Suppl 1):S238. [DOI] [PubMed] [Google Scholar]
Valojerdi 2008 {published data only}
- Valojerdi MR, Eftekhari-Yazdi P, Karimian L, Ashtiani SK. Effect on laser zona pellucida opening on clinical outcome of assisted reproduction technology in patients with advanced female age, recurrent implantation failure, or frozen-thawed embryos. Fertility & Sterility 2008;90(1):84-91. [DOI] [PubMed] [Google Scholar]
Yano 2007 {published data only}
- Yano K, Yano C, Kubo T, Ohashi I, Maeda N, Fukaya T. Chemical zona pellucida thinning with acidified Tyrode's solution: comparison between partial and circumferential techniques. Journal of Assisted Reproduction and Genetics 2007;24(10):471-5. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Zech 1998 {published data only}
- Zech H, Stecher A, Vanderzwalmen P, Murach KF. Investigation of the usefulness of laser-assisted hatching for women of ages above and below forty years [abstract]. Fertility & Sterility 1998;70(3 Suppl 1):S428. [Google Scholar]
Zhang 2009 {published data only}
- Zhang XJ, Yang YZ, Lv Q, Min LH, Li XL, Bai P. Effect of the size of zona pellucida thinning by laser assisted hatching on clinical outcome of human frozen-thawed embryo transfers. Cryo Letters 2009;30(6):455-61. [PMID: ] [PubMed] [Google Scholar]
References to studies awaiting assessment
Elnahas A 2018 {published data only (unpublished sought but not used)}
- Elnahas A, Elnahas T, Azmy O, Elnoury A, Abdelhalim A, Aboelghar M, et al. The use of laser assisted hatching of frozen/ thawed embryos versus laser assisted hatching of fresh embryos in human intracytoplasmic sperm injection. Journal of Obstetrics and Gynaecology 2018;38(5):729. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
NCT02752568 {unpublished data only}
- NCT02752568. Assisted hatching versus endometrial scratch in recurrent Implantation failure. http://apps.who.int/trialsearch/Trial2.aspx?TrialID=NCT02752568 (fist received 27 April 2016).
NCT03623659 {unpublished data only}
- NCT03623659. Does partial zona pellucida removal from vitrified-warmed human blastocysts improve delivery rate in IVF? A multicentric RCT on laser assisted hatching. clinicaltrials.gov/ct2/show/NCT03623659 (first received 9 August 2018).
NCT03810157 {unpublished data only}
- NCT03810157. Does laser-assisted hatching (LAH) improve the pregnancy outcomes in humans? clinicaltrials.gov/ct2/show/NCT03810157 (first received 18 January 2019).
NCT03833869 {unpublished data only}
- NCT03833869. The effect of assisted hatching on implantation rate in frozen blastocyst transfer - a prospective randomized controlled study. clinicaltrials.gov/ct2/show/NCT03833869 (first received 7 February 2019).
NTR3387 {unpublished data only}
- NTR3387. A multicentre randomized controlled trial on the efficacy of laser assisted hatching in poor prognosis patients undergoing IVF or ICSI: the AHA trial. http://apps.who.int/trialsearch/Trial2.aspx?TrialID=NTR3387 (registered 6 April 2012).
Additional references
Al‐Nuaim 2002
- Al-Nuaim LA, Jenkins JM. Assisted hatching in assisted reproduction. British Journal of Obstetrics and Gynaecology 2002;109:856-62. [DOI] [PubMed] [Google Scholar]
Avella 2019
- Avella MA, Milne KA, Dawood S, Dawood A, Tucker MJ. Assisted hatching of human embryos for successful implantation. In: Nagy Z, Varghese A, Agrawal A (eds). In Vitro Fertilisation. Springer, Cham, 2019. [Google Scholar]
Balakier 2012
- Balakier H, Sojecki A, Motamedi G, Bashar S, Mandel R, Librach C. Is the zona pellucida thickness of human embryos influenced by women's age and hormonal levels? Fertility & Sterility 2012;98(1):77-83. [DOI] [PubMed] [Google Scholar]
Bleil 1980
- Bleil JD, Wasserman PM. Structure and function of the zona pellucida: identification and characterisation of the proteins of the mouse oocyte zona pellucida. Developmental Biology 1980;76:185-202. [DOI] [PubMed] [Google Scholar]
Bronson 1970
- Bronson RA, McLaren A. Transfer to mouse oviduct of eggs with and without the zona pellucida. Journal of Reproductive Fertility 1970;22:129-36. [DOI] [PubMed] [Google Scholar]
Check 1999
- Check JH, Choe JK, Katsoff D, Summers-Chase D, Wilson C. Controlled ovarian hyperstimulation adversely affects implantation following in vitro fertilization-embryo transfer. Journal of Assisted Reproduction and Genetics 1999;16(8):416-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cohen 1991
- Cohen J. Assisted hatching of human embryos. Journal of In Vitro Fertilization and Embryo Transfer 1991;8(4):179-90. [DOI] [PubMed] [Google Scholar]
da Costa 2001
- da Costa ALE, Abdelmassih S, Oliveira FG, Abdelmassih V, Abdelmassih R, Nagy ZP, et al. Monozygotic twins and transfer at the blastocyst stage after ICSI. Human Reproduction 2001;16(2):333-6. [DOI] [PubMed] [Google Scholar]
Desai 2013
- Desai SG, Cooper AR, Hagemann AR, Odem RR, Ratts VS, Jungheim ES. Assisted hatching may benefit young women with poor ovarian response. Fertility & Sterility 2013;100(3 Supplement):S506. [Google Scholar]
De Vos 2000
- De Vos A, Van Steirteghem A. Zona hardening, zona drilling and assisted hatching: new achievements in assisted reproduction. Cells Tissues Organs 2000;166(2):220-7. [DOI] [PubMed] [Google Scholar]
ESHRE‐ European IVF monitoring consortium 2020
- Wyns C, Bergh C, Calhaz-Jorge C, De Geyter Ch, Kupka MS, Motrenko T, et al. ART in Europe, 2016: results generated from European registries by ESHRE. Human Reproduction Open 2020;2020(3):1-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fehilly 1985
- Fehilly CB, Cohen J, Simons RF, Fishel SB, Edwards RG. Cryopreservation of cleaving embryos and expanded blastocysts in the human: a comparative study. Fertility & Sterility 1985;44:638-44. [DOI] [PubMed] [Google Scholar]
Freour 2012
- Freour T, Lammers J, Splingart C, Jean M, Barriere P. Time lapse embryoscope as a routine technique in the IVF laboratory: a useful tool for better embryo selection? Gynécologie Obstétrique & Fertilité 2012;40(9):476-80. [DOI] [PubMed] [Google Scholar]
Glujovsky 2016
- Glujovsky D, Farquhar C, Quinteiro Retamar AM, Alvarez Sedo CR, Blake D. Cleavage stage versus blastocyst stage embryo transfer in assisted reproductive technology. Cochrane Database of Systematic Reviews 2016, Issue 6. Art. No: CD002118. [DOI: 10.1002/14651858.CD002118.pub5] [DOI] [PubMed] [Google Scholar]
GRADEpro GDT 2015 [Computer program]
- GRADE Working Group, McMaster University GRADEpro GDT. Hamilton (ON): GRADE Working Group, McMaster University, accessed 19 September 2020. Available at gdt.gradepro.org.
Gupta 2015
- Gupta SK. Role of zona pellucida during fertilisation in humans. Journal of Reproductive Immunology 2015;108:90-7. [DOI] [PubMed] [Google Scholar]
Hammadeh 2011
- Hammadeh ME, Fischer-Hammadeh C, Ali KR. Assisted hatching in assisted reproduction: a state of the art. Journal of Assisted Reproduction and Genetics 2011;28(2):119-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
Harbin Consensus Conference Workshop Group 2014
- Barnhart KT, Farquhar C, Fauser BCJM, Mol B, Legro RS, Wu X, et al. Improving the reporting of clinical trials of infertility treatments (IMPRINT): modifying the CONSORT statement. Human Reproduction 2014;29(10):2075-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hardarson 2012
- Hardarson T, Van Landuyt L, Jones G. The blastocyst. Human Reproduction 27;Suppl 1:i72-91. [DOI] [PubMed] [Google Scholar]
Harlow 1982
- Harlow GM, Quinn P. Development of pre-implantation mouse embryos in vitro and in vivo. Australian Journal of Biology and Science 1982;35:187-93. [DOI] [PubMed] [Google Scholar]
He 2018
- He F, Zhang CY, Wang LS, Li SL, Hu LN. Assisted hatching in couples with advanced maternal age: a systematic review and meta-analysis. Current Medical Science 2018;38(3):552-7. [DOI] [PubMed] [Google Scholar]
HFEA 2020
- Human Fertilisation & Embryology Authority. Fertility treatment 2018: trends and figures: UK statistics for IVF and DI treatment, storage, and donation. https://www.hfea.gov.uk/media/3158/fertility-treatment-2018-trends-and-figures.pdf (accessed 30 June 2020).
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). London: The Cochrane Collaboration, 2011. www.cochrane-handbook.org. [Google Scholar]
Higgins 2019
- Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane Handbook for Systematic Reviews of Interventions Version 6.0 (updated August 2019). London: The Cochrane Collaboration, 2019. www.cochrane-handbook.org. [Google Scholar]
Hsu 1999
- Hsu MI, Mayer J, Aronshon M, Lazendorf S, Muasher S, Kolm P, et al. Embryo implantation in in vitro fertilization and intracytoplasmic sperm injection: impact of cleavage status, morphology grade, and number of embryos transferred. Fertility & Sterility 1999;72(4):679-85. [DOI] [PubMed] [Google Scholar]
Land 2003
- Land J, Evers J. Risks and complications in assisted reproduction techniques: report of an ESHRE consensus meeting. Human Reproduction 2003;18:455-7. [DOI] [PubMed] [Google Scholar]
Lefievre 2004
- Lefievre L, Conner SJ, Salpekar A, Olufowobi O, Ashton P, Pavlovic B, et al. Four zona pellucida glycoproteins are expressed in the human. Human Reproduction 2004;19:1580-6. [DOI] [PubMed] [Google Scholar]
Li 2016
- Li D, Yang DL, An J, Jiao J, Zhou YM, Wu QJ, et al. Effect of assisted hatching on pregnancy outcomes: a systematic review and meta-analysis of randomized controlled trials. Nature Scientific Reports 2016 Aug 9 [Epub ahead of print];6:1-9. [DOI: 10.1038/srep31228] [DOI] [PMC free article] [PubMed] [Google Scholar]
Loret de Mola 1997
- Loret De Mola JR, Garside WT, Bucci J, Tureck RW, Heyner S. Analysis of the human zona pellucida during culture: correlation with diagnosis and the preovulatory hormonal environment. Journal of Assisted Reproduction and Genetics 1997;14:332-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mascarenhas 2012
- Mascarenhas MN, Flaxman SR, Boerna T, Vanderpoel S, Stevens GA. National, regional, and global trends in infertility prevalence since 1990: a systematic analysis of 277 health surveys. PLoS Medicine 2012;9(12):e1001356.. [DOI] [PMC free article] [PubMed] [Google Scholar]
Menezo 2003
- Menezo Y, Cassuto G, Chavrier M. Culture conditions and not prolonged culture time are responsible for monozygotic twinning in human in vitro fertilization. Fertility & Sterility 2003;80(2):462-3. [DOI] [PubMed] [Google Scholar]
Mercader 2001
- Mercader A, Simon C, Galan A, Herrer R, Albert C, Remohi J, et al. An analysis of spontaneous hatching in a human endometrial epithelial coculture system: is assisted hatching justified? Journal of Assisted Reproduction and Genetics 2001;18(6):315-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
RevMan 2020 [Computer program]
- The Cochrane Collaboration Review Manager (RevMan). Version 5.4. Copenhagen: The Cochrane Collaboration, 2020.
Rink 1995
- Rink K, Descloux L, Delacretaz G, Senn A, Nocera D, Germond M. Zona pellucida drilling by a 1.48um laser: influence on the biomechanics of the hatching process [abstract]. In: SPIE - The International Society for Optical Engineering Proceedings, Barcelona. 1995:2624.
Schieve 2000
- Schieve LA, Meikle SF, Peterson HB, Jen G, Burnett NM, Wilcox LS. Does assisted hatching pose a risk for monozygotic twinning in pregnancies conceived through in vitro fertilization. Fertility & Sterility 2000;74:288-94. [DOI] [PubMed] [Google Scholar]
Sengupta 2012
- Sengupta SB, Delhanty JD. Preimplantation genetic diagnosis: recent triumphs and remaining challenges. Expert Review of Molecular Diagnostics 2012;12(6):585-92. [DOI] [PubMed] [Google Scholar]
Stuck 1998
- Stuck AE, Rubenstein LZ, Wieland D. Bias in meta-analysis detected by a simple, graphical test. Asymmetry detected in funnel plot was probably due to true heterogeneity. British Medical Journal 1998;316(7129):469-71. [PMC free article] [PubMed] [Google Scholar]
Zeng 2018
- Zeng MF, Su SQ, Li LM. The effect of laser-assisted hatching on pregnancy outcomes of cryopreserved-thawed embryo transfer: a meta-analysis of randomized controlled trials. Lasers in Medical Science 2018;33:655–66. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Carney 2012
- Carney SK, Das S, Blake D, Farquhar C, Seif MM, Nelson L. Assisted hatching on assisted conception (in vitro fertilisation (IVF) and intracytoplasmic sperm injection (ICSI)). Cochrane Database of Systematic Reviews 2012, Issue 12. Art. No: CD001894. [DOI: 10.1002/14651858.CD001894.pub5] [DOI] [PMC free article] [PubMed] [Google Scholar]
Edi‐Osagie 2003
- Edi Osagie E, Hooper L, Seif MW. The impact of assisted hatching on live birth rates and outcomes of assisted conception: a systematic review. Human Reproduction 2003;18(9):1828-35. [DOI] [PubMed] [Google Scholar]


