Abstract
Background
Pelvic inflammatory disease (PID) affects 4% to 12% of women of reproductive age. The main intervention for acute PID is broad‐spectrum antibiotics administered intravenously, intramuscularly or orally. We assessed the optimal treatment regimen for PID.
Objectives
To assess the effectiveness and safety of antibiotic regimens to treat PID.
Search methods
In January 2020, we searched the Cochrane Sexually Transmitted Infections Review Group's Specialized Register, which included randomized controlled trials (RCTs) from 1944 to 2020, located through hand and electronic searching; CENTRAL; MEDLINE; Embase; four other databases; and abstracts in selected publications.
Selection criteria
We included RCTs comparing antibiotics with placebo or other antibiotics for the treatment of PID in women of reproductive age, either as inpatient or outpatient treatment. We limited our review to a comparison of drugs in current use that are recommended by the 2015 US Centers for Disease Control and Prevention guidelines for treatment of PID.
Data collection and analysis
We used standard methodological procedures expected by Cochrane. Two authors independently extracted data, assessed risk of bias and conducted GRADE assessments of the quality of evidence.
Main results
We included 39 RCTs (6894 women) in this review, adding two new RCTs at this update. The quality of the evidence ranged from very low to high, the main limitations being serious risk of bias (due to poor reporting of study methods and lack of blinding), serious inconsistency, and serious imprecision.
None of the studies reported quinolones and cephalosporins, or the outcomes laparoscopic evidence of resolution of PID based on physician opinion or fertility outcomes. Length of stay results were insufficiently reported for analysis.
Regimens containing azithromycin versus regimens containing doxycycline
We are uncertain whether there was a clinically relevant difference between azithromycin and doxycycline in rates of cure for mild‐moderate PID (RR 1.18, 95% CI 0.89 to 1.55; 2 RCTs, 243 women; I2 = 72%; very low‐quality evidence). The analyses may result in little or no difference between azithromycin and doxycycline in rates of severe PID (RR 1.00, 95% CI 0.96 to 1.05; 1 RCT, 309 women; low‐quality evidence), or adverse effects leading to discontinuation of treatment (RR 0.71, 95% CI 0.38 to 1.34; 3 RCTs, 552 women; I2 = 0%; low‐quality evidence). In a sensitivity analysis limited to a single study at low risk of bias, azithromycin probably improves the rates of cure in mild‐moderate PID (RR 1.35, 95% CI 1.10 to 1.67; 133 women; moderate‐quality evidence), compared to doxycycline.
Regimens containing quinolone versus regimens containing cephalosporin
The analysis shows there may be little or no clinically relevant difference between quinolones and cephalosporins in rates of cure for mild‐moderate PID (RR 1.05, 95% CI 0.98 to 1.14; 4 RCTs, 772 women; I2 = 15%; low‐quality evidence), or severe PID (RR 1.06, 95% CI 0.91 to 1.23; 2 RCTs, 313 women; I2 = 7%; low‐quality evidence). We are uncertain whether there was a difference between quinolones and cephalosporins in adverse effects leading to discontinuation of treatment (RR 2.24, 95% CI 0.52 to 9.72; 6 RCTs, 1085 women; I2 = 0%; very low‐quality evidence).
Regimens with nitroimidazole versus regimens without nitroimidazole
There was probably little or no difference between regimens with or without nitroimidazoles (metronidazole) in rates of cure for mild‐moderate PID (RR 1.02, 95% CI 0.95 to 1.09; 6 RCTs, 2660 women; I2 = 50%; moderate‐quality evidence), or severe PID (RR 0.96, 95% CI 0.92 to 1.01; 11 RCTs, 1383 women; I2 = 0%; moderate‐quality evidence). The evidence suggests that there was little to no difference in in adverse effects leading to discontinuation of treatment (RR 1.05, 95% CI 0.69 to 1.61; 17 studies, 4021 women; I2 = 0%; low‐quality evidence). . In a sensitivity analysis limited to studies at low risk of bias, there was little or no difference for rates of cure in mild‐moderate PID (RR 1.05, 95% CI 1.00 to 1.12; 3 RCTs, 1434 women; I2 = 0%; high‐quality evidence).
Regimens containing clindamycin plus aminoglycoside versus quinolone
We are uncertain whether quinolone have little to no effect in rates of cure for mild‐moderate PID compared to clindamycin plus aminoglycoside (RR 0.88, 95% CI 0.69 to 1.13; 1 RCT, 25 women; very low‐quality evidence). The analysis may result in little or no difference between quinolone vs. clindamycin plus aminoglycoside in severe PID (RR 1.02, 95% CI 0.87 to 1.19; 2 studies, 151 women; I2 = 0%; low‐quality evidence). We are uncertain whether quinolone reduces adverse effects leading to discontinuation of treatment (RR 0.21, 95% CI 0.02 to 1.72; 3 RCTs, 163 women; I2 = 0%; very low‐quality evidence).
Regimens containing clindamycin plus aminoglycoside versus regimens containing cephalosporin
We are uncertain whether clindamycin plus aminoglycoside improves the rates of cure for mild‐moderate PID compared to cephalosporin (RR 1.02, 95% CI 0.95 to 1.09; 2 RCTs, 150 women; I2 = 0%; low‐quality evidence). There was probably little or no difference in rates of cure in severe PID with clindamycin plus aminoglycoside compared to cephalosporin (RR 1.00, 95% CI 0.95 to 1.06; 10 RCTs, 959 women; I2= 21%; moderate‐quality evidence). We are uncertain whether clindamycin plus aminoglycoside reduces adverse effects leading to discontinuation of treatment compared to cephalosporin (RR 0.78, 95% CI 0.18 to 3.42; 10 RCTs, 1172 women; I2 = 0%; very low‐quality evidence).
Authors' conclusions
We are uncertain whether one treatment was safer or more effective than any other for the cure of mild‐moderate or severe PID
Based on a single study at a low risk of bias, a macrolide (azithromycin) probably improves the rates of cure of mild‐moderate PID, compared to tetracycline (doxycycline).
Plain language summary
Treatment for pelvic inflammatory disease
Review question
We assessed the effectiveness and safety of different treatments for pelvic inflammatory disease (PID) that are recommended by current clinical guidelines for treatment of PID (the 2015 US Centers for Disease Control and Prevention guidelines for treatment of PID).
Background
PID is an infection of the upper part of the woman's reproductive system (the womb, the tubes that connect the womb and ovaries, where the egg travels along), the ovaries (which make eggs), and inside the pelvis). It is a common condition affecting women of childbearing age. Symptoms of PID range from none to severe. If effective treatment is not started promptly, the consequences can be infertility (unable to have children), pregnancies outside the womb, and chronic pelvic pain (pain in the lower tummy). There is a wide range of treatment options. The choice is based on severity of symptoms, experience of the doctor, national/international guidelines, and rate of side effects. We wanted to learn if there is a preferable antibiotic (used to treat bacterial infections) therapy with high rates of cure and few side effects to treat PID.
Studies characteristics
We searched the available literature up to 10 January 2020 and included 39 studies with 6894 women with an average of 14 days of treatment and follow‐up (monitoring after treatment). These trials included women of childbearing age with mild to severe PID. Trials mostly used a single or a combination of antibiotics with different administration routes: intravenous (into a blood vessel), intramuscular (into the muscle), and oral (as a tablet). In mild‐moderate cases, intramuscular and oral treatments were prescribed, and in moderate‐severe cases, treatments were usually started in hospital and were completed at home.
Key results
We are uncertain whether one treatment was safer or more effective than any other for the cure of PID. From a single study, at low risk of bias, the use of a macrolide probably improves the rates of cure in mild‐moderate PID.
Apart from one high quality result in one comparison, the quality of the evidence ranged from very low to moderate, the main problems being serious risk of bias (poor reporting of study methods; doctors and women may have known which medicine was given), and results differed across studies.
Summary of findings
Background
Description of the condition
Pelvic inflammatory disease (PID) in women describes inflammation of the upper genital tract and surrounding structures as a result of ascending infection from the lower genital tract – bacteria spread directly from the cervix to the endometrium and on to the upper genital tract (Soper 2010). The signs and symptoms of PID are not specific and may range from asymptomatic to serious illness. PID can produce endometritis, parametritis (infection of the structures near the uterus), salpingitis (infection of the fallopian tubes), oophoritis (infection of the ovary), and tubo‐ovarian abscess (Workowski 2015). Peritonitis (infection inside the peritoneum, the thin layer of tissue lining the abdomen) and perihepatitis (infection around the liver) can also occur. Peritonitis, tubo‐ovarian abscess, and severe systemic illness (e.g. fever and malaise) are considered severe forms of PID; the other forms of presentation are considered mild or moderate according to the subjective opinion of the examining doctor or nurse (Soper 2010).
The most common complaint of PID is lower abdominal pain, with or without vaginal discharge. Specific grading of the clinical presentation using symptom scores has been described (e.g. McCormack 1977; Hager 1989), but has not been validated, and use of these scores is inconsistent. PID does not have a diagnostic gold standard. The most commonly used diagnostic criteria are based on those from the Centers for Disease Control and Prevention (CDC) (Workowski 2015), namely sexually active young women and other women at risk for sexually transmitted disease (STD) who are experiencing recent pelvic or lower abdominal pain where no cause other than PID can be identified, and one or more of the following minimum criteria are present on pelvic examination: cervical motion tenderness, uterine tenderness, or adnexal tenderness. The requirement for all three minimum criteria to be present increases the specificity of the diagnosis but reduces sensitivity.
Two sexually transmitted infections (Chlamydia trachomatis and Neisseria gonorrhoeae) have been strongly implicated in the aetiology of PID (Newman 2015); however, based on the pattern of organisms isolated from the upper genital tract, the infection may often be polymicrobial (caused by more than one type of bacteria) (Eschenbach 1975; Arredondo 1997; Baveja 2001; Haggerty 2006). This suggests that initial damage produced by C trachomatis or N gonorrhoeae may permit the opportunistic entry of other bacteria, including anaerobes (bacteria that do not need oxygen to grow) (Ross 2014a). However, in many cases, no infection is found in the lower genital tract (Goller 2016).
The public health importance of PID can be estimated from the frequency of chlamydial and gonococcal infections. In 2012, among women aged 15 to 49 years, the estimated global prevalence of chlamydia was 3.4% (95% confidence interval (CI) 2.5% to 4.5%), gonorrhoea was 2% (95% CI 1.4% to 2.8%), and trichomoniasis was 4.0% (95% CI 2.7% to 5.8%) (Rowley 2019). In one prospective study of 1170 women with elevated risk for having chlamydial cervicitis, 8.6% developed PID within three years; among women with chlamydia, the risk ratio (RR) for developing PID was 2.5 (95% CI 1.5 to 4.0) (Ness 2006). In the UK, the prevalence of PID is about 2% among women between 16 and 46 years old (Simms 1999; Datta 2012; Ross 2014a). However, in some other countries, the rates of chlamydia infection are lower, for example, in Jordan it is 0.6% in symptomatic women and 0.5% in asymptomatic women (Mahafzah 2008). Among women with PID, 10% to 20% may become infertile, 40% will develop chronic pelvic pain, and 10% of those who conceive will have an ectopic pregnancy (Blanchard 1998; Ness 2002; Ness 2005; Mahafzah 2008).
The morbidity associated with PID relates to the acute inflammatory process, which can cause abdominal pain, vaginal discharge, dyspareunia (pain during sexual intercourse), and abnormal menstrual bleeding. In addition, long‐term complications secondary to tubal damage occur and include chronic pelvic pain, ectopic pregnancy, and infertility (Workowski 2015). PID has a prevalence of between 2% and 12%, and it cannot be diagnosed reliably from clinical symptoms and signs, which have a positive predictive value for salpingitis of only 65% to 90% compared with laparoscopy (Workowski 2015; CDC 2018). Direct visualization of the fallopian tubes via laparoscopy has a higher sensitivity, but there is considerable inter‐ and intra‐observer reproducibility (Molander 2003). Endometrial biopsy may have some utility (Ross 2004), but is not performed routinely and is of uncertain diagnostic and prognostic value, since endometritis (infection of the inner mucosal lining of the uterus) can persist despite the resolution of clinical symptoms (Ness 2002; Savaris 2007).
The financial cost of pelvic infection has been estimated to exceed USD 2.4 billion in the USA, and the mean total cost per episode is around USD 5000 (Trent 2011). In the UK, the mean cost of a non‐complicated episode of PID is GBP 163 (Aghaizu 2011).
Description of the intervention
The main intervention for acute PID is the use of broad‐spectrum antibiotics which cover C trachomatis, N gonorrhoeae, and anaerobic bacteria. There are three effective routes of administration (intravenous (IV), intramuscular (IM), or oral (PO)) (Ness 2002; Walker 2007). In refractory cases, surgery to drain an abscess or hydrosalpinx may be necessary. When parenteral treatment is used, it is usually discontinued 24 hours after a woman improves clinically (Workowski 2015).
The optimal treatment strategy is unclear. A variety of antibiotic regimens have been used, with marked geographical variation. Current practice generally involves the use of multiple agents to cover C trachomatis, N gonorrhoeae, and anaerobic bacteria, but the best combination of agents is unknown. The background prevalence and antimicrobial resistance patterns of bacterial pathogens in different regions may influence the choice of empirical therapy.
Guidelines have been produced in the USA (Workowski 2015), and Europe (Judlin 2010a; Ross 2014b), to guide therapy, but these have not been based on a formal systematic review. In addition, to choose an antibiotic for PID treatment, it is necessary to consider its spectrum, cost, adverse effects, and posology (i.e. dosage, interval) to achieve the best balance between compliance and efficacy. There are no current systematic reviews on this topic.
The different antibiotic regimens proposed to treat PID vary in cost, efficacy, and adverse effects. Potential adverse effects include allergic reactions and gastrointestinal symptoms, which can lead to discontinuation of therapy. Lack of evidence is revealed in the current CDC and British Association for Sexual Health and HIV (BASHH) guidelines, where the authors state that there is limited evidence for the need to eradicate anaerobes and for the use of alternative regimens, such as azithromycin (Workowski 2015), and the comparison between clindamycin plus aminoglycoside and fluoroquinolones (Ross 2014b). Likewise, if the prevalence of N gonorrhoeae is low, the use of fluoroquinolones can be considered if allergy to cephalosporin is an issue (Workowski 2015).
How the intervention might work
It is likely that the intervention works by eradicating bacterial pathogens and reducing the associated inflammation which leads to scarring. Necrotic tissue and pus present in an abscess may prevent antibiotics reaching the infected area. Mechanical drainage of the abscess through open surgery, laparoscopy, or aspiration through a large‐bore needle is likely to work by removing infected material which antibiotics are unable to treat (Workowski 2015). Clinical cure without surgery in women with a tubo‐ovarian abscess is around 75% (DeWitt 2010). The rationale for using broad‐spectrum antibiotics is to cover the wide variety of pathogens found in PID, which include gram‐positive (e.g. Streptococcus), gram‐negative (e.g. Chlamydia, Klebsiella, Escherichia coli, Neisseria), and anaerobic bacteria (gram positive or negative: Peptostreptococcus, Bacteroides).
Why it is important to do this review
PID is a common disease; for women aged 35 to 44 years in England, it is estimated that 33.6% have experienced at least one episode of PID, diagnosed or not (Price 2017). PID is accompanied by high rates of morbidity in young women (Ness 2002; Morris 2014). It requires effective treatment to reduce the incidence of chronic pelvic pain, infertility, and transmitted STDs. A variety of antibiotic regimens have been proposed to treat PID, which vary in cost, efficacy, and adverse effects, but the optimal treatment strategy is unclear.
Currently there are no systematic reviews of this subject and the optimal treatment strategy is unclear. This review will address clinical questions raised by current guidelines on the treatment of PID (Ross 2014b; Workowski 2015), regarding the effectiveness and safety of nitroimidazole, the relative benefits of azithromycin versus doxycycline, the use of quinolones, and the relative benefits of cephalosporins compared to the most‐used regimen of clindamycin plus aminoglycoside, to inform future guideline development and clinical practice.
Objectives
To assess the effectiveness and safety of antibiotic regimens to treat PID.
Methods
Criteria for considering studies for this review
Types of studies
Randomized controlled trials (RCTs), including those which did not describe their method of randomization (i.e. where the authors stated that treatment was randomized without providing further details). We chose randomized trials as they provide the strongest evidence for evaluating the efficacy of therapy (Higgins 2011). We included studies irrespective of publication status or language.
We excluded quasi‐randomized trials because they produce effect estimates indicating more extreme benefits when compared with RCTs (Higgins 2011). We also excluded cross‐over and cluster trials.
Types of participants
Women of reproductive age (14 years or older) diagnosed as having acute PID (symptoms for less than six weeks) based on clinical findings, laparoscopy, endometrial biopsy, or detectable gonorrhoea or chlamydia in the upper genital tract.
We divided women into two groups: mild‐moderate (e.g. absence of tubo‐ovarian abscess) and severe (e.g. systemically unwell, presence of tubo‐ovarian abscess).
Types of interventions
We limited our review to comparison of drugs in current use that are recommended for consideration by the 2015 US CDC guidelines for treatment of PID (Workowski 2015).
We included trials that contained, at least, the following treatments for PID:
azithromycin versus doxycycline;
quinolone versus cephalosporin;
nitroimidazole versus no nitroimidazole;
clindamycin plus aminoglycoside versus quinolone;
clindamycin plus aminoglycoside versus cephalosporin.
Types of outcome measures
The following outcomes were measured.
Primary outcomes
Effectiveness: clinical cure according to the criteria defined by the treating physician (e.g. resolution or improvement of signs and symptoms related to PID).
Adverse events: any antibiotic‐related adverse event leading to discontinuation of therapy.
Secondary outcomes
Microbiological clearance of C trachomatis (chlamydia) from either the upper or lower genital tract, according to the method provided by the authors.
Microbiological clearance of N gonorrhoeae (gonorrhoea) from either the upper or lower genital tract, according to the method provided by the authors.
Laparoscopic evidence of resolution of PID based on physician opinion.
Length of stay (for inpatient care).
Fertility outcome based on at least one participant‐reported live birth following PID treatment in women not using effective contraception.
Where studies included women with various types of pelvic infection, we considered only women with endometritis, salpingitis, parametritis, or oophoritis (not related to labour, delivery, cancer, or surgery).
Where studies reported multiple time points, we considered the period between 14 and 28 days after initiation of treatment.
Search methods for identification of studies
We identified relevant RCTs of 'antibiotic therapy' for 'PID', irrespective of their language of publication, publication date, and publication status (published, unpublished, in press, and in progress). We used both electronic searching in bibliographic databases and handsearching, as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Electronic searches
We contacted the Information Specialist of the Cochrane Sexually Transmitted Infections Review Group to implement a comprehensive search strategy capturing as many relevant RCTs as possible in electronic databases. We used a combination of controlled vocabulary (MeSH, Emtree, DeCS, including exploded terms) and free‐text terms (considering spelling variants, synonyms, acronyms, and truncation) for 'pelvic inflammatory disease (PID)' and 'antibiotic therapy', with field labels, proximity operators, and Boolean operators. We presented the search strategies in Appendix 1. Specifically, we searched the following electronic databases.
The Cochrane Sexually Transmitted Infections Review Group's Specialized Register, which includes RCTs from 1944 to 2020 located through electronic searching and handsearching. The electronic databases searched for the register are the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, and Embase.
CENTRAL, Ovid platform (1991 to 10 January 2020).
MEDLINE, Ovid platform (1946 to 10 January 2020).
MEDLINE In‐Process & Other Non‐Indexed Citations, Ovid platform (1946 to 10 January 2020).
MEDLINE Daily Update, Ovid platform (1946 to 10 January 2020).
Embase (1947 to 10 January 2020).
LILACS, iAHx interface (1982 to 10 January 2020).
Web of Science (2001 to 10 January 2020).
In MEDLINE, we used the Cochrane Highly Sensitive Search Strategy for identifying RCTs: sensitivity and precision maximizing version (2008 revision), Ovid format (Higgins 2011). The LILACS search strategy combined RCTs filter of iAHx interface.
Searching other resources
We searched the following trials registers:
World Health Organization International Clinical Trials Registry Platform (WHO ICTRP) (apps.who.int/trialsearch/);
ClinicalTrials.gov (clinicaltrials.gov/).
We searched for grey literature in OpenGrey (www.opengrey.eu/) (from 1993 to 2014). We contacted authors of all RCTs identified by other methods as well as pharmaceutical companies producing 'antibiotic therapy' for 'pelvic inflammatory disease (PID).'
We handsearched conference proceeding abstracts in the following publications: Indian Journal of Sexually Transmitted Diseases (2008 to January 2020), Sexually Transmitted Diseases (1974 to January 2020), Sexually Transmitted Infections (1996 to January 2020), Journal of Sexual Medicine (2004 to January 2020), Sexual and Relationship Therapy (2000 to January 2020), and the Society for the Scientific Study of Sexuality's Sexual Science Newsletter (2000 to January 2020).
We handsearched previous systematic reviews on similar topics identified from:
the Cochrane Library (www.thecochranelibrary.com/);
Epistemonikos (www.epistemonikos.org/).
We handsearched the reference lists of all identified RCTs.
Data collection and analysis
Selection of studies
In this updated version, two review authors (DGF and JM) performed an initial screen of titles and abstracts retrieved by the updated search, and we retrieved the full text of all potentially eligible studies. Two review authors (DGF and JM) independently examined these studies for compliance with the inclusion criteria and selected studies that met these criteria. We resolved disagreements regarding eligibility by discussion or by consulting a third review author (RFS). We documented the selection process in a PRISMA flow chart. We excluded pelvic infection related to obstetric surgical procedures or in animals. Where a study contained both 'eligible' and 'ineligible' participants, we included a subset of data relating to the 'eligible' participants if sufficient details were provided for analysis.
Data extraction and management
Two review authors (DGF, JM) independently extracted the data from each study using a data extraction form that the review authors designed and pilot tested. We collected data from the included studies in sufficient detail to complete the Characteristics of included studies table. We also extracted detailed numerical outcome data in duplicate to allow calculation of Mantel‐Haenszel RRs for each comparison. We examined data for errata, retraction, fraud, and inconsistencies. We resolved disagreements by consensus or by consulting a fourth review author (JR or RFS).
If a study had more than two intervention arms, we included or combined only those that met the predefined inclusion criteria. For instance, if the study compared azithromycin (group A) versus azithromycin plus metronidazole (group B) versus metronidazole plus cefoxitin or doxycycline (group C), and the analysis was between the use or not of metronidazole, we combined groups B and C versus group A. The treatment effect was expressed as rate of cure (%) and its magnitude and direction checked in forest plots to ensure consistency with the original study. Where studies had multiple publications, we used the main trial report as the reference and derived additional details from secondary papers. We corresponded with study investigators for further data as required.
Data collected with the data extraction form included:
-
Study factors:
author, date of publication, journal;
date of study;
study design;
location;
setting;
quality of randomization, treatment allocation, and blinding;
method of PID diagnosis;
sample size.
-
Participant factors:
age, ethnicity;
pregnancy;
presence of intrauterine device (IUD);
duration of symptoms;
presence of abscess (pyosalpinx, tubo‐ovarian abscess).
-
Outcome measured:
method of assessment of pelvic pain and score;
timing of assessment;
adverse events;
additional assessments of outcome: laparoscopy, microbiology, fertility.
-
Intervention factors:
antibiotic given: dose, route, length of therapy;
comparator regimen: dose, route, length of therapy;
additional treatment given.
-
Additional data:
whether contact tracing was performed.
Assessment of risk of bias in included studies
Two review authors (DGF, JM) independently assessed the risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2019). We resolved disagreements between two review authors by consensus or by involving a third review author (RFS). We assessed risk of bias using the Cochrane 'Risk of bias' tool provided in RevMan Web (RevMan Web 2019). We provided justification for risk of bias (high, low, unclear) in the 'Risk of bias' table by direct reference to the relevant report. We requested missing information from the study investigators using open‐ended questions.
1. Random sequence generation (checking for possible selection bias)
For each included study, we verified the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
We assessed the method as:
low risk of bias (any truly random process, e.g. random number table; computer random number generator);
high risk of bias (no randomization);
unclear risk of bias (e.g. authors stated that women were randomized to one of the treatments, without further explanation).
2. Allocation concealment (checking for possible selection bias)
For each included study, we verified the method used to conceal allocation to interventions prior to assignment, and we assessed whether intervention allocation could have been foreseen in advance of, or during, recruitment, or changed after assignment.
We assessed the methods as:
low risk of bias (e.g. telephone or central randomization; consecutively numbered, sealed, opaque envelopes);
high risk of bias (open random allocation; unsealed or non‐opaque envelopes; alternation; date of birth); or
unclear risk of bias (allocation was mentioned without further details).
3.1. Blinding of participants and personnel (checking for possible performance bias)
For each included study, we verified the methods used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. We considered studies to be at:
low risk of bias if participants and personnel were blinded, or if we judged that the lack of blinding would be unlikely to affect results (e.g. culture for N gonorrhoeae);
high risk if participants and personnel were not blinded;
unclear risk of bias if no further details were provided.
3.2. Blinding of outcome assessment (checking for possible detection bias)
For each included study, we verified the methods used, if any, to blind outcome assessors from knowledge of which intervention a participant received. We assessed blinding separately for different outcomes or classes of outcomes. We assessed methods used to blind outcome assessment as:
low risk of bias if assessors were blinded, or if we judged that the lack of blinding would be unlikely to affect results (e.g. culture for N gonorrhoeae);
high risk if assessors were not blinded;
unclear risk of bias if no further details were provided.
4. Incomplete outcome data (checking for possible attrition bias due to the amount, nature, and handling of incomplete outcome data)
For each included study, and for each outcome or class of outcomes, we verified the completeness of data, including attrition and exclusions from the analysis. We stated whether attrition and exclusions were reported and the numbers included in the analysis at each stage (compared with the total randomized participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported, or could be supplied by the trial authors, we re‐included missing data in the analyses we undertook.
We assessed methods as:
low risk of bias (e.g. no missing outcome data; missing outcome data balanced across groups);
high risk of bias (e.g. numbers or reasons for missing data imbalanced across groups; 'as treated' analysis done with substantial departure of intervention received from that assigned at randomization); or
unclear risk of bias: no further details were provided.
We used a cutoff point of 20% missing data in determining if a study was at low or high risk of bias (Fewtrell 2008).
5. Selective reporting (checking for reporting bias)
For each included study, we described how we investigated the possibility of selective outcome reporting bias and what we found.
We assessed the methods as:
low risk of bias (where it was clear that all the study's prespecified outcomes and all expected outcomes of interest to the review were reported);
high risk of bias (where not all the study's prespecified outcomes were reported; one or more reported primary outcomes were not prespecified; outcomes of interest were reported incompletely and so could not be used; study did not include results of a key outcome that would have been expected to have been reported); or
unclear risk of bias: no further details were provided.
6. Other bias (checking for bias due to problems not covered by 1. to 5. above)
For each included study, we described any important concerns we had about other possible sources of bias.
We assessed whether each study was free of other problems that could put it at risk of bias:
low risk of bias;
high risk of bias; or
unclear whether there was risk of bias.
7. Overall risk of bias
We made explicit judgements about whether studies were at high risk of bias, according to criteria described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2019). With reference to 1. to 6. above, we assessed the likely magnitude and direction of the bias and whether we considered that it was likely to impact on the findings. We explored the impact of the level of bias by undertaking sensitivity analyses (see Sensitivity analysis).
Measures of treatment effect
For dichotomous data, we used number of events (cure) in the control and intervention groups to calculate Mantel‐Haenszel risk ratios (RR). We presented 95% confidence intervals (CI) for all outcomes. For number need to treat for an additional beneficial (NNTB) or harmful (NNTH) outcome, we followed the recommendation given by Altman (Altman 1998). When we observed a treatment effect (cure), we reported the NNTB with 95% CIs.
When possible, we performed analysis based on intention to treat (ITT). When information for an ITT analysis was not available, we used the results provided by the authors.
We performed meta‐analysis separately for mild‐moderate PID and severe PID. We defined severe PID as the presence of tubo‐ovarian abscess, being systemically unwell, or the presence of peritonitis; mild‐moderate PID as no presence of tubo‐ovarian abscess. We further analyzed cases in these two groups across different classes of antibiotics.
Unit of analysis issues
The primary unit of analysis was an event per woman randomized, which was used to calculate the percentage response rate (e.g. clinical cure).
Dealing with missing data
We analyzed the data on an ITT basis to the greatest degree possible and made attempts to obtain missing data from the original trials. Where we were unable to obtain these data, we considered cases that were lost to follow‐up as treatment failure (worst‐case scenario) in the primary analysis. For other outcomes, we analyzed the available data. We did not analyze data from other reported outcomes (e.g. pooled rates of cure of different diseases, including PID).
Assessment of heterogeneity
We considered whether the clinical and methodological characteristics of the included studies were sufficiently similar for meta‐analysis to provide a clinically meaningful summary. We assessed statistical heterogeneity using the I2 statistic as follows: low (l2 value below 40%), moderate (l2 value 40% to 75%), or high (l2 value above 75%) (Sutton 2008; Higgins 2011). We also assessed statistical heterogeneity in each meta‐analysis using the t2 and Chi2 statistics.
We regarded heterogeneity as substantial if the I2 statistic was greater than 40% and either t2 was greater than zero, or there was a low P value (less than 0.10) in the Chi2 test for heterogeneity. If we detected substantial heterogeneity, we explored possible explanations for it in subgroup analyses (see Subgroup analysis and investigation of heterogeneity). We took statistical heterogeneity into account when interpreting the results, especially if there was any variation in the direction of effect. If so, we used a random‐effects analysis, instead of fixed‐effect analysis.
Assessment of reporting biases
Reporting biases arise when the dissemination of research findings is influenced by the nature and direction of results. Some types of reporting bias (e.g. publication bias, multiple publication bias, language bias, etc.) reduce the likelihood that all studies eligible for a review are retrieved (Higgins 2011). If all eligible studies are not retrieved, the review would be biased. In view of the difficulty of detecting and correcting for publication bias and other reporting biases, we aimed to minimize their potential impact by ensuring a comprehensive search for eligible studies and by being alert for duplication of data. If there were 10 or more studies in an analysis, we used a funnel plot to explore the possibility of small‐study effects (a tendency for estimates of the intervention effect to be more beneficial in smaller studies). There are five possible causes for the asymmetric funnel plot: reporting bias, poor methodological quality, true heterogeneity, artefactual, and chance (Egger 1997). Only through formal statistical analysis or using a 'contour‐enhanced' funnel plot is an explication for these asymmetrical funnel plots possible, which was not performed herein.
Data synthesis
We performed statistical analyses using Review Manager Web (RevMan Web 2019). We used a fixed‐effect meta‐analysis for combining data where it was reasonable to assume that trials were estimating the same underlying treatment effect (i.e. where trials were examining the same intervention, and the trials' populations and methods were sufficiently similar). We conducted separate analyses for mild‐moderate and severe PID.
If there was clinical heterogeneity sufficient to expect that the underlying treatment effects differed between trials, or if we detected substantial statistical heterogeneity (I2 = 40% or greater), we used a random‐effects meta‐analysis to produce an overall summary if a mean treatment effect across trials was considered clinically meaningful. We treated the random‐effects summary as the mean range of possible treatment effects, and discussed the clinical implications of treatment effects differing between trials.
If the mean treatment effect was not clinically meaningful, we did not combine trials. Where we used random‐effects analyses, we presented the results as the mean treatment effect with 95% CIs, and the estimates of the t2 and I2 statistics.
Subgroup analysis and investigation of heterogeneity
Where data were available, we performed the following prespecified subgroup analyses:
route of antibiotic administration (PO, IM, or IV);
length of therapy (less or more than seven continuous days of receiving antibiotics);
detection of chlamydia;
detection of gonorrhoea;
site of initiation of treatment (inpatient or outpatient).
We avoided selective reporting of a particular subgroup by not performing multiple subgroup analyses. If we identified substantial heterogeneity (I2 = 40% or greater), we used a random‐effects analysis as the primary statistical analysis.
Where there was substantial heterogeneity, we explored possible reasons for this finding by stratifying results according to the characteristics of the study population (e.g. method of PID diagnosis), the intervention (e.g. class of antibiotic used, dose of antibiotic, route of administration), or methodological characteristics (e.g. length of time to outcome measurement).
Sensitivity analysis
We undertook the following sensitivity analysis to investigate whether our conclusions were robust to methodological decisions made by review authors:
risk of bias (restricting analysis to blinded studies at low risk of selection bias).
Summary of findings and assessment of the quality of the evidence
We used GRADEpro software to produce 'Summary of findings' tables (GRADEpro GDT). The GRADE approach considers the following criteria: risk of bias, inconsistency, indirectness of evidence, imprecision, and publication bias, and specifies four levels of quality: high, moderate, low, and very low, starting from high for RCTs. If there was a flaw in the RCT, we downgraded the quality of the evidence by one or two levels.
Two review authors independently applied GRADE in the 'Summary of findings' tables. We resolved any disagreements by consensus. We downgraded for risk of bias due to crucial risk of bias for two or more criteria. The evidence was downgraded further if there was inconsistency. Inconsistency was based on statistical test for heterogeneity and how much variation there was in the findings of the studies that contributed to the outcome. We also considered imprecision, and downgraded if the CIs were compatible with benefit in one or both groups, or with no difference between the groups. In each domain, we downgraded one level for serious risk of bias and two levels for very serious risk of bias.
'Summary of findings' tables considering clinical cure in PID according to its severity (mild‐moderate, severe) and the number of adverse events leading to discontinuation of therapy were presented for the following comparisons of PID treatment with regimens containing:
macrolides (azithromycin) compared to tetracycline (doxycycline);
quinolone compared to cephalosporins;
nitroimidazole compared to no nitroimidazole;
clindamycin plus aminoglycoside compared to quinolone;
clindamycin plus aminoglycoside compared to cephalosporin.
Summary of findings and assessment of the certainty of the evidence
We used GRADEpro software ( GRADEpro GDT) to produce 'Summary of findings' tables. The GRADE approach considers the following criteria: risk of bias, inconsistency, indirectness of evidence, imprecision, and publication bias, and specifies four levels of quality: high, moderate, low, and very low, starting from high for RCTs. If there was a flaw in the RCT, we downgraded the quality of the evidence by one or two levels.
Two review authors independently applied a consistent grading for GRADE in the 'Summary of findings' tables. We resolved any disagreements by consensus. We downgraded for risk of bias due to crucial risk of bias for two or more criteria. The evidence was downgraded further if there was inconsistency. Inconsistency was based on statistical test for heterogeneity and how much variation there was in the findings of the studies that contributed to the outcome. We also considered imprecision, and downgraded if the CIs were compatible with benefit in one or both groups, or with no difference between the groups. In each domain, we downgraded one level for serious risk of bias and two levels for very serious risk of bias.
Summary of Findings (SoF) tables considering clinical cure in PID according to its severity (mild‐moderate, severe) and the number of adverse events leading to discontinuation of therapy were presented for the following comparisons of PID treatment with regimens containing
macrolides (azithromycin) compared to tetracycline (doxycycline);
quinolone compared to cephalosporins;
nitroimidazole compared to no nitroimidazole;
clindamycin plus aminoglycoside compared to quinolone;
clindamycin plus aminoglycoside compared to cephalosporin
Results
Description of studies
We included 39 RCTs (two new studies) with a wide range of sample sizes and the quality of evidence ranged from very low to high by some limitations with potentially serious risk of bias.
Results of the search
In the 2017 version, we retrieved 2133 references and screened 2094 records after removing duplicated references. We discarded 1955 records as clearly irrelevant and considered 139 full‐text articles.
For this updated version, we retrieved 479 references and screened 478 records after removing duplicate references. We discarded 68 records for not dealing with humans, 269 records for not being RCTs, 125 for not being related to PID, and six for not comparing antibiotics. We considered 10 full‐text articles. After full‐text analysis, two new studies met our inclusion criteria and they were included (Figure 1). The reasons for exclusion of the eight full‐text studies are explained in the Characteristics of excluded studies table. We extracted data from the full‐text article for each study.
1.
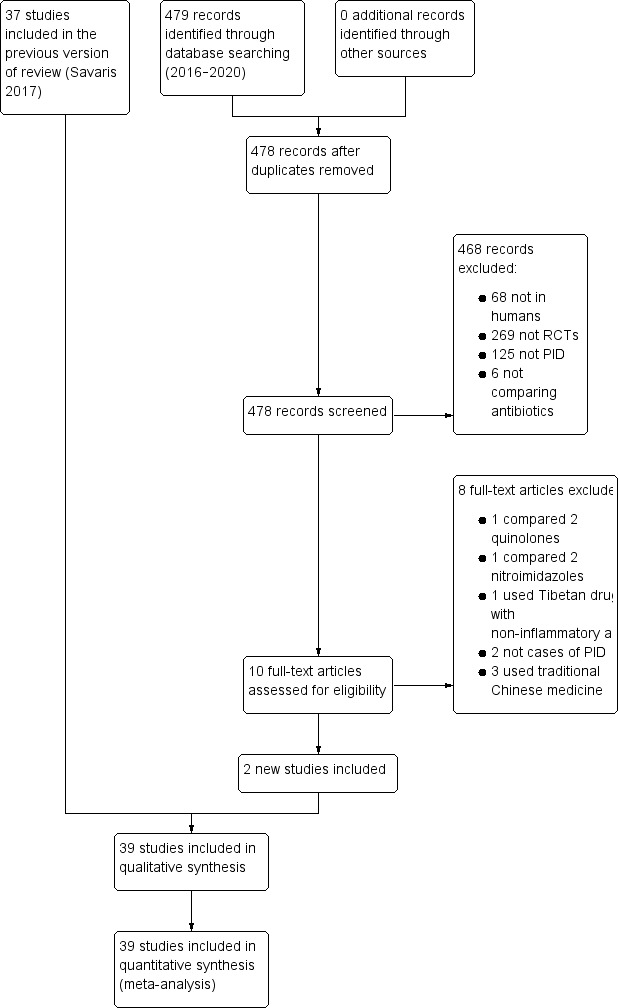
Study flow diagram. PID: pelvic inflammatory disease; RCT: randomised controlled trial.
Included studies
The 39 included trials had 6894 women, with a sample size ranging from 25 (Apuzzio 1989) to 1156 (Aşicioğlu 2013). Retrieved studies came from a wide range of inpatient and outpatient settings from different continents (Americas, Europe, Asia, Oceania, and Africa) and were written in English, German, French, Japanese, and Italian.
For this update, two studies, one from the UK (Dean 2016), and the other from the USA (Wiesenfeld 2017), were added. Dean 2016 compared the rate of cure between ofloxacin 400 mg twice daily plus metronidazole 400 mg twice daily for 14 days versus five days of azithromycin plus metronidazole for 14 days plus ceftriaxone IM. Wiesenfeld 2017 compared ceftriaxone 250 mg IM single dose plus doxycycline 100 mg PO twice daily for 14 days plus placebo PO twice daily for 14 days versus ceftriaxone 250 mg IM single dose plus doxycycline 100 mg PO twice daily for 14 days plus metronidazole 500 mg PO twice daily for 14 days.
Population
The included trials recruited girls and women aged 14 years and over with a diagnosis of PID according to CDC criteria (pelvic or lower abdominal pain and one or more of the following clinical criteria: cervical motion tenderness, uterine tenderness, or adnexal tenderness) (Workowski 2015). Studies varied in degree of disease severity of participants, treatment location (i.e. inpatient or outpatient), and countries and continents. PID was considered severe in the presence of systemically unwell women, peritonitis, or pelvic abscess.
Interventions
The 39 RCTs yielded 6894 women and made the following comparisons.
For mild‐moderate PID:
macrolides (azithromycin) compared to tetracycline (doxycycline) (Malhotra 2003; Savaris 2007);
quinolone compared to cephalosporins (Wendel 1991; Martens 1993; Arredondo 1997; Dean 2016);
nitroimidazole compared to no use of nitroimidazole (Burchell 1987; Tison 1988; Hoyme 1993; Ross 2006; Judlin 2010b; Aşicioğlu 2013; Wiesenfeld 2017);
clindamycin plus aminoglycoside compared to quinolone (Apuzzio 1989);
clindamycin plus aminoglycoside compared to cephalosporin (Walters 1990).
For severe PID:
macrolides (azithromycin) compared to tetracycline (doxycycline) (Bevan 2003);
quinolone compared to cephalosporins (Okada 1988; Martens 1993; Fischbach 1994);
nitroimidazole compared to no use of nitroimidazole (Ciraru‐Vigneron 1986; Crombleholme 1986; Crombleholme 1987; Leboeuf 1987; Buisson 1989; Ciraru‐Vigneron 1989; Giraud 1989; Heinonen 1989; Fischbach 1994; Sirayapiwat 2002; Heystek 2009);
clindamycin plus aminoglycoside compared to quinolone (Crombleholme 1989; Thadepalli 1991);
clindamycin plus aminoglycoside compared to cephalosporin (Roy 1985; Sweet 1985; Soper 1988; Martens 1990; Roy 1990; Walters 1990; Landers 1991; Maria 1992; Hemsell 1994; Balbi 1996).
Outcomes
The main outcome was clinical cure, and 5475 women were reported as clinically cured. We defined clinical cure according to the authors' definitions, which ranged from absence of symptoms for 24 hours (Apuzzio 1989), to a 60% or greater reduction in total pain score at day 21 combined with an absence of pelvic discomfort/tenderness, temperature less than 37.8 °C, and white blood cell count less than 10,000/mm3 on day 21 (Aşicioğlu 2013). Most trials used clinical parameters for cure, that is, reduction of fever, and reduction or absence of pain at different time points after treatment. We identified adverse effects leading to discontinuation of treatment as those related to the suspension of therapeutic regimen.
Excluded studies
We excluded 106 studies. The most common reason for exclusion was that the study did not report a comparison of interest to this review (63 studies). Other common reasons for exclusion were that PID cases were not distinguished from other pelvic infectious conditions (26 studies), the studies were not randomized (15 studies), or were suspected of fraud (two studies) (see Characteristics of excluded studies table).
In the updated 2020 version, we analyzed and excluded eight full‐text articles (Figure 1). Two articles were not related to PID (Brittain 2016; Baery 2018); one compared two nitroimidazoles (morinidazole and ornidazole) for treating PID (Cao 2017); one used a Tibetan drug with non‐inflammatory activity (Honghua Ruyi Wan) with moxifloxacin compared to moxifloxacin plus placebo (Zhang 2017); one compared two quinolones (levofloxacin and ciprofloxacin) (Zou 2019), which it is not a comparison we wanted; and three used traditional Chinese medicine (Kangfu, an anti‐inflammatory drug (NCT04035785), gynaecological Qianjin with levofloxacin and metronidazole versus levofloxacin and metronidazole (NCT04031664), and Fuyanshu capsules (Feng 2019)). We extracted data from the full‐text article for each study (see Characteristics of excluded studies table).
Risk of bias in included studies
We performed a full risk of bias assessment on all included studies. We classified those studies where authors stated that women were randomized to one of two treatments, without further details, as at unclear risk of selection bias. Twenty‐seven studies occurred before 1996, and predated the introduction of CONSORT guidelines, so many studies had unclear risk of bias.
We summarized the risk of bias in Figure 2 and Figure 3. Additional details of the included trials are provided in the Characteristics of included studies table.
2.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
3.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Allocation
Fourteen trials adequately reported a truly random process of sequence generation, for example, random number table or computer random number generator, making selection bias at entry unlikely (Sweet 1985; Soper 1988; Martens 1990; Walters 1990; Thadepalli 1991; Martens 1993; Sirayapiwat 2002; Malhotra 2003; Ross 2006; Savaris 2007; Judlin 2010b; Aşicioğlu 2013; Dean 2016; Wiesenfeld 2017). The remaining included trials did not report the random sequence generation methods, making the risk of selection bias at entry unclear.
For allocation concealment, four trials implemented sequentially numbered drug containers as a concealment allocation method, making selection bias at entry unlikely (Ross 2006; Savaris 2007; Judlin 2010b; Aşicioğlu 2013). The remaining included trials did not report the method used to conceal allocation to interventions prior to assignment, making the risk of selection bias at entry unclear.
Blinding
Seven trials used placebo with an identical appearance for the control group to blind trial participants and personnel, making performance and detection bias unlikely (Figure 2) (Okada 1988; Arredondo 1997; Ross 2006; Savaris 2007; Heystek 2009; Judlin 2010b; Wiesenfeld 2017). Twelve studies did not blind investigators and participants to the allocation, making them at high risk of bias (Crombleholme 1986; Crombleholme 1989; Walters 1990; Landers 1991; Wendel 1991; Maria 1992; Hemsell 1994; Bevan 2003; Malhotra 2003; Aşicioğlu 2013; Dean 2016; Tison 1988). The remaining included trials did not specify how the participants and the personnel were blinded from knowledge of which intervention a participant received, making the risk of performance and detection bias unclear.
Incomplete outcome data
Completeness of data was adequate (i.e. less than 20% of data missing) for 32 of the studies (Figure 2) (Roy 1985; Sweet 1985; Crombleholme 1986; Crombleholme 1987; Leboeuf 1987; Okada 1988; Soper 1988; Apuzzio 1989; Buisson 1989; Ciraru‐Vigneron 1989; Crombleholme 1989; Giraud 1989; Heinonen 1989; Martens 1990; Roy 1990; Walters 1990; Landers 1991; Thadepalli 1991; Hoyme 1993; Martens 1993; Fischbach 1994; Hemsell 1994; Balbi 1996; Sirayapiwat 2002; Bevan 2003; Malhotra 2003; Ross 2006; Savaris 2007; Heystek 2009; Judlin 2010b; Aşicioğlu 2013; Wiesenfeld 2017).
Four studies were unclear about the risk of attrition bias (Ciraru‐Vigneron 1986; Burchell 1987; Tison 1988; Arredondo 1997)
The remaining studies had more than 20% of data missing, with an associated high risk of attrition bias.
Selective reporting
The trial protocol was available for five studies, and it was clear that the published reports included all the expected outcomes, including those that were prespecified, making reporting bias unlikely (Ross 2006; Savaris 2007; Aşicioğlu 2013; Dean 2016; Wiesenfeld 2017). For the remaining studies, trial protocol was unavailable, and it was unclear whether the published reports included all the expected outcomes, including those that were prespecified. The reports had insufficient information to permit judgment of 'yes' or 'no' and were, therefore, at unclear risk of bias.
Other potential sources of bias
One study had imbalances in baseline characteristics and was at high risk of potential bias (Soper 1988). Out of 39 trials, 13 had some form of funding by pharmaceutical companies (Crombleholme 1989; Roy 1990; Walters 1990; Landers 1991; Thadepalli 1991; Wendel 1991; Martens 1993; Hemsell 1994; Arredondo 1997; Ross 2006; Savaris 2007; Heystek 2009; Judlin 2010b); however, there is no clear evidence that trial methods are more likely to be flawed if a trial is industry‐funded (Sterne 2013), therefore these trials were at unclear risk. The remaining trials provided insufficient information to permit a judgement of 'yes' or 'no' and were, therefore, at unclear risk of bias.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4; Table 5
Summary of findings 1. Regimens containing macrolides (azithromycin) compared to regimens containing tetracycline (doxycycline) for pelvic inflammatory disease.
| Azithromycin compared to doxycycline for PID | |||||||
|
Population: women with PID Setting: hospital ward or outpatient clinic Intervention: regimens containing azithromycin Comparison: regimens containing doxycycline | |||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No of women (studies) | Quality of the evidence (GRADE) | Comments | ||
| Risk with doxycycline | Risk with azithromycin | ||||||
|
Clinical cure according to criteria established by study authors Mild‐moderate PID Follow‐up: median 14 days |
689 per 1000 | 818 per 1000 (740 to 876) |
RR 1.18 (0.89 to 1.55) |
243 (2 RCTs) | ⊕⊝⊝⊝ Very lowa,b,c | NNTB 13 NNTH 3 |
|
|
Clinical cure according to criteria established by study author Mild‐moderate PID Follow‐up: median 14 days Sensitivity analysis restricted to study at low risk of bias |
627 per 1000 | 848 per 1000 (743 to 921) |
RR 1.35 (1.10 to 1.67) |
133 (1 RCT) |
⊕⊕⊕⊝ Moderated | NNTB 5 (3 to 14) | |
|
Clinical cure according to criteria established by study authors Severe PID Follow‐up: range 13–18 days |
969 per 1000 | 971 per 1000 (940 to 987) |
RR 1.00 (0.96 to 1.05) |
309 (1 RCT) | ⊕⊕⊝⊝ Lowe | NNTB 16 NNTH 29 |
|
|
Adverse events: any antibiotic‐related adverse event leading to discontinuation of therapy Follow‐up: range 13–18 days |
78 per 1000 | 48 per 1000 (30 to 76) |
RR 0.71 (0.38 to 1.34) |
552 (3 RCTs) | ⊕⊕⊝⊝ Lowa,c | NNTB 13 NNTH 101 |
|
| Microbiological clearance | C trachomatis | 980 per 1000 | 1000 per 1000 (900 to 1000) |
RR 1.02 (0.98 to 1.06) |
243 (2 RCTs) | — | NNTB 10 NNTH 8 |
| N gonorrhoeae | 1000 per 1000 | 1000 per 1000 (741 to 1000) |
RR 1.0 (0.76 to 1.31) |
309 (1 RCT) | ⊕⊝⊝⊝ Very lowa,e | Just 1 RCT found cases of N gonorrhoeae | |
| Laparoscopic evidence of resolution of PID based on physician opinion | No studies reported. | ||||||
| Length of stay (for inpatient care) | Reported results are not sufficient for analysis. | ||||||
| Fertility outcome | No studies reported. | ||||||
| * The risk in the intervention group (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; NNTB: number needed to treat for an additional beneficial outcome; NNTH: number needed to treat for an additional harmful outcome; PID: pelvic inflammatory disease; RCT: randomized controlled trial; RR: risk ratio. | |||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low quality: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | |||||||
aDowngraded one level for serious risk of bias (poor reporting of methods and high risk of performance and detection bias in one or more studies). bDowngraded one level for serious inconsistency (I2 = 72%). cDowngraded one level for serious imprecision: confidence intervals compatible with benefit in one or both groups, or with no difference between the groups. dDowngraded one level for serious imprecision: single study with only 98 events. eDowngraded two levels for very serious risk of bias: single unblinded study with poor reporting of methods.
Summary of findings 2. Regimens containing quinolone compared to regimens containing cephalosporins for pelvic inflammatory disease.
| Quinolone compared to cephalosporins for PID | |||||||
|
Population: women with PID Setting: hospital ward or outpatient clinic Intervention: quinolone Comparison: cephalosporins | |||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No of women (studies) | Quality of the evidence (GRADE) | Comments | ||
| Risk with cephalosporins | Risk with quinolone | ||||||
|
Clinical cure according to criteria established by study authors Mild‐moderate PID Follow‐up: range 14–28 days |
691 per 1000 | 719 per 1000 (677 to 760) |
RR 1.05 (0.98 to 1.14) |
772 (4 RCTs) | ⊕⊕⊝⊝ Lowa,b | NNTB 9 NNTH 64 |
|
|
Clinical cure according to criteria established by study authors Severe PID Follow‐up: range 14–28 days |
643 per 1000 | 700 per 1000 (622 to 766) |
RR 1.06 (0.91 to 1.23) |
313 (2 RCTs) | ⊕⊕⊝⊝ Lowa,b | NNTB 7 NNTH 15 |
|
|
Adverse events: any antibiotic‐related adverse event leading to discontinuation of therapy Follow‐up: mean 14 days |
5 per 1000 | 12 per 1000 (5 to 29) |
RR 2.24 (0.52 to 9.72) |
1085 (6 RCTs) | ⊕⊝⊝⊝ Very lowa,c | 2/6 RCTs (502 women) did not contribute to this analysis because the authors reported 0 events. NNTB 40 NNTH 129 |
|
| Microbiological clearance | C trachomatis | 1000 per 1000 | 952 per 1000 (773 to 992) | RR 0.95 (0.84 to 1.08) | 270 (3 RCTs) | ⊕⊝⊝⊝ Very lowa,c |
NNTB 4 NNTH 11 |
| N gonorrhoeae | 952 per 1000 | 900 per 1000 (744 to 965) | RR 1.13 (0.89 to 1.42) | 270 (3 RCTs) | ⊕⊝⊝⊝ Very lowa,c |
NNTB 23 NNTH 9 |
|
| Laparoscopic evidence of resolution of PID based on physician opinion | No studies reported. | ||||||
| Length of stay (for inpatient care) | Reported results are not sufficient for analysis. | ||||||
| Fertility outcome | No studies reported. | ||||||
| * The risk in the intervention group (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; NNTB: number needed to treat for an additional beneficial outcome; NNTH: number needed to treat for an additional harmful outcome; PID: pelvic inflammatory disease; RCT: randomized controlled trial; RR: risk ratio. | |||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low quality: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | |||||||
aDowngraded one level for serious risk of bias (poor reporting of methods and high or unclear risk of performance and detection bias in one or more studies). bDowngraded one level for serious imprecision: confidence intervals compatible with benefit in one or both groups, or with no difference between the groups. cDowngraded two levels for very serious imprecision: confidence intervals compatible with benefit in one or both groups, or with no difference between the groups, only seven events overall.
Summary of findings 3. Regimens containing nitroimidazole compared to no nitroimidazole for pelvic inflammatory disease.
| Nitroimidazole compared to regimens without use of nitroimidazole for PID | |||||||
|
Population: women with PID Setting: hospital ward or outpatient clinic Intervention: regimens containing nitroimidazole Comparison: regimens containing no nitroimidazole | |||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No of women (studies) | Quality of the evidence (GRADE) | Comments | ||
| Risk with no nitroimidazole | Risk with nitroimidazole | ||||||
|
Clinical cure according to criteria established by study authors Mild‐moderate PID Follow‐up: range 14–28 days |
766 per 1000 | 781 per 1000 (727 to 834) |
RR 1.02 (0.95 to 1.09) |
2660 (6 RCTs) | ⊕⊕⊕⊝ Moderatea,b | NNTB 19 NNTH 91 |
|
|
Clinical cure according to criteria established by study authors Mild‐moderate PID Follow‐up: range 14–28 days Sensitivity analysis restricted to studies at low risk of bias |
755 per 1000 | 800 per 1000 (740 to 868) |
RR 1.05 (1.00 to 1.12) |
1434 (3 RCTs) |
⊕⊕⊕⊕ High |
NNTB 19 NNTH 91 |
|
|
Clinical cure according to criteria established by study authors Severe PID Follow‐up: range 14–28 days |
832 per 1000 | 804 per 1000 (772 to 831) |
RR 0.96 (0.92 to 1.01) |
1383 (11 RCTs) | ⊕⊕⊕⊝ Moderatea | NNTB 15 NNTH 76 |
|
|
Adverse events: any antibiotic‐related adverse event leading to discontinuation of therapy Follow‐up: mean 14 days |
20 per 1000 | 20 per 1000 (13 to 32) |
RR 1.05 (0.69 to 1.61) |
4021 (17 RCTs) | ⊕⊕⊝⊝ Lowa,c | 10/17 studies (1088 women) did not contribute data to the analysis because the authors reported no events. NNTB 108 NNTH 121 |
|
| Microbiological clearance | C trachomatis | Not applicable, nitroimidazoles have no activity against chlamydia. | |||||
| N gonorrhoeae | Not applicable, nitroimidazoles have no activity against gonorrhoea. | ||||||
| Laparoscopic evidence of resolution of PID based on physician opinion | No studies reported. | ||||||
| Length of stay (for inpatient care) | Reported results were insufficient for analysis. | ||||||
| Fertility outcome | No studies reported any fertility outcomes. | ||||||
| * The risk in the intervention group (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; NNTB: number needed to treat for an additional beneficial outcome; NNTH: number needed to treat for an additional harmful outcome; PID: pelvic inflammatory disease; RCT: randomized controlled trial; RR: risk ratio. | |||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low quality: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | |||||||
aDowngraded one level for serious risk of bias (poor reporting of methods and high or unclear risk of selection, performance, detection, attrition, and reporting bias in one or more studies). bSubstantial inconsistency (I2 = 50%). Not downgraded because of all inconsistency related to a single small study (30 women) which barely influenced the overall estimate. cDowngraded one level for serious imprecision: confidence intervals compatible with benefit in one or both groups, or with no difference between the groups, only 79 events overall.
Summary of findings 4. Regimens containing clindamycin plus aminoglycoside compared to regimens containing quinolone for pelvic inflammatory disease.
| Clindamycin + aminoglycoside compared to quinolone for PID | |||||||
|
Population: women with PID Setting: hospital ward or outpatient clinic Intervention: regimens containing clindamycin + aminoglycoside Comparison: regimens containing quinolone | |||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No of women (studies) | Quality of the evidence (GRADE) | Comments | ||
| Risk with quinolone | Risk with clindamycin + aminoglycoside | ||||||
|
Clinical cure according to criteria established by authors Mild‐moderate PID Follow‐up: median 14 days |
1000 per 1000 | 867 per 1000 (621 to 962) |
RR 0.88 (0.69 to 1.13) |
25 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b | NNTB 3 NNTH 6 |
|
|
Clinical cure according to criteria established by authors Severe PID Follow‐up: median 14 days |
800 per 1000 | 816 per 1000 (714 to 887) |
RR 1.02 (0.87 to 1.19) |
151 (2 RCTs) | ⊕⊕⊝⊝ Lowc,d | NNTB 7 NNTH 9 |
|
|
Adverse events: any antibiotic‐related adverse event leading to discontinuation of therapy Follow‐up: mean 14 days |
50 per 1000 | 0 per 1000 (0 to 44) |
RR 0.21 (0.02 to 1.72) |
163 (3 RCTs) | ⊕⊝⊝⊝ Very lowa,b | 1/3 RCTs (25 women) did not contribute data to the analysis because the authors reported 0 events. NNTB 8 NNTH 273 |
|
| Microbiological clearance | C trachomatis | 800 per 1000 | 1000 per 1000 (722 to 1000) | RR 1.08 (0.85 to 1.36) | 176 (3 RCT) | ⊕⊝⊝⊝ Very lowa,b |
NNTB 3 NNTH 5 |
| N gonorrhoeae | 1000 per 1000 | 1000 per 1000 (920 to 1000) | RR 1.00 (0.96 to 1.05) | 176 (3 RCT) | ⊕⊝⊝⊝ Very lowa,b |
— | |
| Laparoscopic evidence of resolution of PID based on physician opinion | No data available. | ||||||
| Length of stay (for inpatient care) | Reported results are not sufficient for analysis. | ||||||
| Fertility outcome | No data available. | ||||||
| * The risk in the intervention group (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; NNTB: number needed to treat for an additional beneficial outcome; NNTH: number needed to treat for an additional harmful outcome; PID: pelvic inflammatory disease; RCT: randomized controlled trial; RR: risk ratio. | |||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low quality: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | |||||||
aDowngraded two levels for very serious risk of bias: single unblinded study with poor reporting of methods. bDowngraded two levels for serious imprecision (though further downgrading not possible): confidence intervals compatible with benefit in one or both groups, or with no difference between the groups, very few events overall. cDowngraded one level for serious risk of bias (poor reporting of methods and high or unclear risk of performance and detection bias in both studies). dDowngraded one level for serious imprecision: confidence intervals compatible with benefit in one or both groups, or with no difference between the groups.
Summary of findings 5. Regimens containing clindamycin plus aminoglycoside compared to regimens containing cephalosporin for pelvic inflammatory disease.
| Clindamycin + aminoglycoside compared to cephalosporin for PID | |||||||
|
Population: women with PID Setting: hospital ward or outpatient clinic Intervention: regimens containing clindamycin + aminoglycoside Comparison: regimens containing cephalosporin | |||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No of women (studies) | Quality of the evidence (GRADE) | Comments | ||
| Risk with cephalosporin | Risk with clindamycin + aminoglycoside | ||||||
|
Clinical cure according to criteria established by authors Mild‐moderate PID Follow‐up: median 14 days |
958 per 1000 | 974 per 1000 (911 to 993) |
RR 1.02 (0.95 to 1.09) |
150 (2 RCTs) | ⊕⊕⊝⊝ Lowa,b | NNTB 11 NNTH 19 |
|
|
Clinical cure according to criteria established by authors Severe PID Follow‐up: median 14 days |
840 per 1000 | 838 per 1000 (801 to 870) |
RR 1.00 (0.95 to 1.06) |
959 (10 RCTs) | ⊕⊕⊕⊝ Moderatea | NNTB 21 NNTH 22 |
|
|
Adverse events: any antibiotic‐related adverse event leading to discontinuation of therapy Follow‐up: mean 14 days |
4 per 1000 | 6 per 1000 (2 to 17) | RR 0.78 (0.18 to 3.42) | 1172 (10 RCTs) | ⊕⊝⊝⊝ Very lowa,c | 7/10 RCTs (617 women) did not contribute data to the analysis reported because the authors reported no events. NNTB 75 NNTH 126 |
|
| Microbiological clearance | C trachomatis | 946 per 1000 | 962 per 1000 (893 to 987) | RR 1.02 (0.94 to 1.1) | 327 (5 RCTs) | ⊕⊝⊝⊝ Very lowa,c | NNTB 9 NNTH 16 |
| N gonorrhoeae | 983 per 1000 | 1000 per 1000 (962 to 1000) | RR 1.02 (0.99 to 1.05) | 327 (5 RCTs) | ⊕⊝⊝⊝ Very lowa,c |
NNTB 17 NNTH 43 |
|
| Laparoscopic evidence of resolution of PID based on physician opinion | No data available. | ||||||
| Length of stay (for inpatient care) | Reported results are not sufficient for analysis. | ||||||
| Fertility outcome | No data available. | ||||||
| * The risk in the intervention group (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95 CI). CI: confidence interval; NNTB: number needed to treat for an additional beneficial outcome; NNTH: number needed to treat for an additional harmful outcome; PID: pelvic inflammatory disease; RCT: randomized controlled trial; RR: risk ratio. | |||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low quality: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | |||||||
aDowngraded one level for serious risk of bias (poor reporting of methods and high or unclear risk of performance and detection bias in one or more studies). bDowngraded one level for serious imprecision, small overall sample size. cDowngraded two levels for serious imprecision (though further downgrading not possible): confidence intervals compatible with benefit in one or both groups, or with no difference between the groups, only six events overall.
We analyzed the effectiveness of clinical cure and adverse effects leading to discontinuation of treatment in five scenarios based on drug class:
macrolides (azithromycin) compared to tetracycline (doxycycline);
quinolone compared to cephalosporins;
nitroimidazole compared to no nitroimidazole;
clindamycin plus aminoglycoside compared to quinolone;
clindamycin plus aminoglycoside compared to cephalosporin.
We analyzed the efficacy of therapy in these five comparisons in women with mild‐moderate PID and women with severe PID. We also compared adverse events leading to discontinuation of the therapy. Lack of further analysis is discussed in the Differences between protocol and review section.
1. Regimens containing macrolides (azithromycin) compared to regimens containing tetracycline (doxycycline)
Three studies compared azithromycin versus doxycycline in mild‐moderate (Malhotra 2003; Savaris 2007) or severe (Bevan 2003) PID.
Primary outcomes
1.1. Effectiveness
1.1a. Clinical cure in mild‐moderate pelvic inflammatory disease
We included two trials in the analysis of clinical cure in mild‐moderate PID (Malhotra 2003; Savaris 2007). We are uncertain whether there was a clinically relevant difference between azithromycin and doxycycline in rates of cure for mild‐moderate PID (RR 1.18, 95% CI 0.89 to 1.55; 2 studies, 243 women; I2 = 72%; very low‐quality evidence) (Analysis 1.1; Figure 4).
1.1. Analysis.

Comparison 1: Regimens containing macrolides (azithromycin) versus tetracycline (doxycycline), Outcome 1: Effectiveness of cure in mild‐moderate PID
4.

Forest plot of comparison: 1 Regimens containing macrolides (azithromycin) versus tetracycline (doxycycline), outcome: 1.1 Effectiveness of cure in mild‐moderate PID.
This suggests that if the rate of clinical cure in women with mild‐moderate PID using regimens including doxycycline was 69%, the rate using regimens including azithromycin would be 74% to 88%.
In a sensitivity analysis limited to the study at low risk of bias, azithromycin probably improves the rates of cure in mild‐moderate PID (RR 1.35, 95% CI 1.10 to 1.67; 1 study, 133 women; moderate‐quality evidence) (Analysis 1.2; Figure 5).
1.2. Analysis.

Comparison 1: Regimens containing macrolides (azithromycin) versus tetracycline (doxycycline), Outcome 2: Sensitivity analysis by risk of bias: effectiveness of cure in mild‐moderate PID
5.

Forest plot of comparison: 1 Regimens containing macrolides (azithromycin) versus tetracycline (doxycycline), outcome: 1.2 Sensitivity analysis by risk of bias: effectiveness of cure in mild‐moderate PID.
The evidence derived from this sensitivity analysis suggests that in mild‐moderate PID, if the rate of clinical cure in women using regimens including doxycycline was 63%, the rate using regimens including azithromycin would be 74% to 92%.
1.1b. Clinical cure in severe pelvic inflammatory disease
One trial reported clinical cure in severe PID (Bevan 2003). The analysis may result in little or no difference between azithromycin and doxycycline in rates of severe PID (RR 1.00, 95% CI 0.96 to 1.05; 1 study, 309 women; low‐quality evidence) (Analysis 1.3; Figure 6).
1.3. Analysis.

Comparison 1: Regimens containing macrolides (azithromycin) versus tetracycline (doxycycline), Outcome 3: Effectiveness of cure in severe PID
6.

Forest plot of comparison: 1 Regimens containing macrolides (azithromycin) versus tetracycline (doxycycline), outcome: 1.3 Effectiveness of cure in severe PID.
This suggests that if clinical cure in severe PID in women using regimens including doxycycline was 97%, the rate using regimens including azithromycin would be 94% to 99%.
1.2. Adverse events
1.2.1. Antibiotic‐related adverse effects leading to discontinuation of therapy
We included three trials in the analysis of antibiotic‐related adverse effects leading to discontinuation of therapy (Bevan 2003; Malhotra 2003; Savaris 2007). We are uncertain of a clinically relevant difference between azithromycin and doxycycline in rates of discontinuation between the groups (RR 0.71, 95% CI 0.38 to 1.34; 3 studies, 552 women; I2 = 0%; low‐quality evidence) (Analysis 1.4).
1.4. Analysis.

Comparison 1: Regimens containing macrolides (azithromycin) versus tetracycline (doxycycline), Outcome 4: Any antibiotic‐related adverse effect leading to discontinuation use of macrolide versus tetracycline
This suggests that if the rate of adverse events in women using regimens including doxycycline was 8%, the rate using regimens including azithromycin would be 3% to 8%.
Data are depicted in Table 1.
Secondary outcomes
1.3. Microbiological clearance of chlamydia
Two studies reported chlamydia clearance (Bevan 2003; Savaris 2007). Cure was obtained in 49/50 women in the azithromycin group (98%, 95% CI 89% to 100%) and 33/33 women in the doxycycline group (100%, 95% CI 90% to 100%).
This suggests that if the rate of microbiological clearance of C trachomatis in women using regimens including doxycycline was 98%, the rate using regimens including azithromycin would be 90% to 100%.
1.4. Microbiological clearance of gonorrhoea
Two studies reported gonorrhoea clearance (Bevan 2003; Savaris 2007), but only one found evidence of N gonorrhoeae (Bevan 2003). In the azithromycin group, there was cure in 11/11 cases (100%, 95% CI 74% to 100%). Cure was also 100% in the doxycycline group (5/5 cases; 100%, 95% CI 57% to 100%).
This suggests that if the rate of microbiological clearance of N gonorrhoeae in women using regimens including doxycycline was 100%, the rate using regimens including azithromycin would be 74% to 100%.
1.5. Laparoscopic evidence of resolution of pelvic inflammatory disease based on physician opinion
We found no data for laparoscopic evidence of resolution of PID.
1.6. Length of stay (for inpatient care)
One study reported length of hospital stay (Bevan 2003). Women were kept in the hospital, per protocol, for 13 to 18 days.
1.7. Fertility outcome
No studies reported live birth rate.
2. Regimens containing quinolones versus regimens containing cephalosporins
Six studies compared quinolones versus cephalosporins in mild‐moderate PID (Wendel 1991; Martens 1993; Arredondo 1997; Dean 2016), or severe PID (Okada 1988; Martens 1993; Fischbach 1994).
Primary outcomes
2.1. Effectiveness
2.1a. Clinical cure in mild‐moderate pelvic inflammatory disease
We included four trials in the analysis of clinical cure in mild‐moderate PID (Wendel 1991; Martens 1993; Arredondo 1997; Dean 2016). The analysis shows there may be little or no clinically relevant difference between quinolones and cephalosporins in rates of cure in mild‐moderate PID (RR 1.05, 95% CI 0.98 to 1.14; 4 studies, 772 women; I2 = 15%; low‐quality evidence) (Analysis 2.1; Figure 7).
2.1. Analysis.

Comparison 2: Regimens containing quinolones versus cephalosporins, Outcome 1: Effectiveness of cure in mild‐moderate PID
7.

Forest plot of comparison: 2 Regimens containing quinolones versus cephalosporins, outcome: 2.1 Effectiveness of cure in mild‐moderate PID.
This suggests that if the rate of clinical cure in women with mild‐moderate PID using regimens including cephalosporins was 69%, the rate using regimens including quinolones would be 68% to 76%.
2.1b. Clinical cure in severe pelvic inflammatory disease
We included two trials in the analysis of clinical cure in severe PID (Okada 1988; Fischbach 1994). The analysis shows there may be little or no clinically relevant difference between quinolones and cephalosporins in rates of cure of severe PID (RR 1.06, 95% CI 0.91 to 1.23; 2 studies, 313 women; I2 = 7%; low‐quality evidence) (Analysis 2.2; Figure 8).
2.2. Analysis.

Comparison 2: Regimens containing quinolones versus cephalosporins, Outcome 2: Effectiveness of cure in severe PID
8.

Forest plot of comparison: 2 Regimens containing quinolones versus cephalosporins, outcome: 2.2 Effectiveness of cure in severe PID.
This suggests that if clinical cure in women with severe PID using regimens including cephalosporin was 64%, the rate using regimens including quinolone would be 62% to 77%.
2.2. Adverse events
2.2.1. Antibiotic‐related adverse effect leading to discontinuation of therapy
The trials reported few adverse effects leading to discontinuation of treatment (quinolones: 1.2%, 95% CI 0.5% to 2.9% versus cephalosporin: 0.5%, 95% CI 0.1% to 1.9%); we are uncertain whether there was a difference between quinolones and cephalosporins in rates of discontinuation (RR 2.24, 95% CI 0.52 to 9.72; 6 studies, 1085 women; I2 = 0%; very low‐quality evidence) (Analysis 2.3; Figure 9).
2.3. Analysis.

Comparison 2: Regimens containing quinolones versus cephalosporins, Outcome 3: Any antibiotic‐related adverse effect leading to discontinuation
9.

Forest plot of comparison: 2 Regimens containing quinolones versus cephalosporins, outcome: 2.3 Any antibiotic‐related adverse effect leading to discontinuation.
This suggests that if the rate of adverse events in women using regimens including cephalosporin was 0.5%, the rate using regimens including quinolones would be 0.5% to 2.9%.
Data are depicted in Table 2.
Secondary outcomes
2.3. Microbiological clearance of chlamydia
Three studies reported clearance of chlamydia (Wendel 1991; Fischbach 1994; Arredondo 1997). Cure occurred in 20/21 women in the quinolone group (95.2%, 95% CI 77% to 99%) and 25/25 women in the cephalosporin group (100%, 95% CI 86% to 100%).
This suggests that if the rate of microbiological clearance of C trachomatis in women using regimens including cephalosporin was 100%, the rate using regimens including quinolones would be 77% to 99%.
2.4. Microbiological clearance of gonorrhoea
Three studies reported clearance of gonorrhoea (Wendel 1991; Fischbach 1994; Arredondo 1997). Cure occurred in 27/30 women in the quinolone group (90%, 95% CI 74% to 96%) and 20/21 women in the cephalosporin group (95.2%, 95% CI 77% to 99%).
This suggests that if the rate of microbiological clearance of N gonorrhoeae in women using regimens including cephalosporin was 95%, the rate using regimens including quinolone would be 74% to 96%.
2.5. Laparoscopic evidence of resolution of pelvic inflammatory disease based on physician opinion
We found no data for laparoscopic evidence of resolution of PID.
2.6. Length of stay (for inpatient care)
We found no data suitable for analysis for the length of hospital stay. Fischbach and colleagues admitted women for IV treatment for two to five days, followed by seven to 12 days of PO therapy, without further details (Fischbach 1994).
2.7. Fertility outcome
No studies reported live birth rate.
3. Regimens containing nitroimidazoles versus regimens without the use of nitroimidazoles
Seventeen studies compared multiple or single antibiotics associated with or without nitroimidazoles in mild‐moderate PID (Burchell 1987; Tison 1988; Ross 2006; Judlin 2010b; Aşicioğlu 2013; Wiesenfeld 2017) or severe PID (Ciraru‐Vigneron 1986; Crombleholme 1986; Crombleholme 1987; Leboeuf 1987; Buisson 1989; Ciraru‐Vigneron 1989; Giraud 1989; Heinonen 1989; Fischbach 1994; Sirayapiwat 2002; Heystek 2009).
Primary outcomes
3.1. Effectiveness
3.1a. Clinical cure in mild‐moderate pelvic inflammatory disease
We included six studies in the analysis of clinical cure in mild‐moderate PID (Burchell 1987; Tison 1988; Ross 2006; Judlin 2010b; Aşicioğlu 2013; Wiesenfeld 2017). All studies used metronidazole as the nitroimidazole. There was probably little or no difference in rates of cure between metronidazole or no metronidazole in mild‐moderate PID (RR 1.02, 95% CI 0.95 to 1.09; 6 studies, 2660 women; I2 = 50%; moderate‐quality evidence) (Analysis 3.1; Figure 10).
3.1. Analysis.

Comparison 3: Regimens containing nitroimidazoles versus no nitroimidazoles, Outcome 1: Effectiveness of cure in mild‐moderate PID
10.

Forest plot of comparison: 3 Regimens containing nitroimidazoles versus no nitroimidazoles, outcome: 3.1 Effectiveness of cure in mild‐moderate PID.
This suggests that if the rate of cure in women with mild‐moderate PID using regimens including nitroimidazoles was 77%, the rate using no nitroimidazoles would be 72% to 83%.
Sensitivity analysis restricted to the three studies at low risk of bias shows little or no difference in rates of cure between the use or not of metronidazole in mild‐moderate PID (RR 1.05, 95% CI 1.00 to 1.12; 3 studies, 1434 women; I2 = 0%; high‐quality evidence) (Ross 2006; Judlin 2010b; Wiesenfeld 2017). (Analysis 3.2).
3.2. Analysis.

Comparison 3: Regimens containing nitroimidazoles versus no nitroimidazoles, Outcome 2: Sensitivity analysis by risk of bias: effectiveness of cure in mild‐moderate PID
In this sensitive analysis, this suggests that if the rate of cure in women with mild‐moderate PID using regimens including nitroimidazoles was 75%, the rate using no nitroimidazoles would be 74% to 87%.
3.1b. Clinical cure in severe pelvic inflammatory disease
Eleven studies evaluated nitroimidazole in severe PID and all studies used metronidazole (Ciraru‐Vigneron 1986; Crombleholme 1986; Crombleholme 1987; Leboeuf 1987; Buisson 1989; Ciraru‐Vigneron 1989; Giraud 1989; Heinonen 1989; Fischbach 1994; Sirayapiwat 2002; Heystek 2009). There was probably little or no difference in rates of cure between the use or not of metronidazole in severe PID (RR 0.96, 95% CI 0.92 to 1.01; 11 studies, 1383 women; I2 = 3%; moderate‐quality evidence) (Analysis 3.3; Figure 11).
3.3. Analysis.

Comparison 3: Regimens containing nitroimidazoles versus no nitroimidazoles, Outcome 3: Effectiveness of cure in severe PID
11.

Forest plot of comparison: 3 Regimens containing nitroimidazoles versus no nitroimidazoles, outcome: 3.3 Effectiveness of cure in severe PID.
This suggests that if the rate of cure in women with severe PID using regimens including nitroimidazoles was 83%, the rate using no nitroimidazoles would be 77% to 83%.
3.2. Adverse events
3.2.1. Antibiotic‐related adverse effects leading to discontinuation of therapy
We analyzed 17 studies of antibiotic‐related adverse effects leading to discontinuation of therapy (Ciraru‐Vigneron 1986; Crombleholme 1986; Burchell 1987; Crombleholme 1987; Leboeuf 1987; Tison 1988; Buisson 1989; Ciraru‐Vigneron 1989; Giraud 1989; Heinonen 1989; Fischbach 1994; Sirayapiwat 2002; Ross 2006; Heystek 2009; Judlin 2010b; Aşicioğlu 2013; Wiesenfeld 2017). We are uncertain of the effect of discontinuation of therapy between groups due to adverse effects (RR 1.05, 95% CI 0.69 to 1.61; 17 studies, 4021 women; I2 = 0%; low‐quality evidence). Of note, 10/17 RCTs did not contribute data to the analysis because the authors reported no adverse effects (Ciraru‐Vigneron 1986; Crombleholme 1986; Burchell 1987; Leboeuf 1987; Tison 1988; Ciraru‐Vigneron 1989; Giraud 1989; Heinonen 1989; Sirayapiwat 2002; Heystek 2009). Only six studies reported adverse effects leading to discontinuation of treatment, yielding a rate of 2% of severe adverse effects (95% CI 1.5% to 2.7%) in the nitroimidazole group and 1.9% (95% CI 1.4% to 2.6%) in the no nitroimidazole group.
This suggests that if the rate of adverse outcomes in women with PID using regimens including nitroimidazoles was 2%, the rate using no nitroimidazoles would be 1% to 3%.
Data are depicted in Table 3.
Secondary outcomes
3.3. Microbiological clearance of chlamydia
This is not applicable since nitroimidazoles do not have activity against chlamydia.
3.4. Microbiological clearance of gonorrhoea
This is not applicable since nitroimidazoles do not have activity against gonorrhoea.
3.5. Laparoscopic evidence of resolution of pelvic inflammatory disease based on physician opinion
We found no data for laparoscopic evidence of resolution of PID.
3.6. Length of stay (for inpatient care)
Burchell and colleagues did not give details of the length of hospital stay: the authors mentioned that "ampicillin plus metronidazole in group II began with four 1 g intravenous doses given at 6‐hourly intervals and then 400 mg 8‐hourly orally for 14 days" and in Table III stated, "patient response after 4 days treatment" (Burchell 1987).
Ciraru‐Vigneron and colleagues reported that women treated with amoxicillin plus clavulanate had a stay of 3.6 days and with ampicillin plus gentamicin plus metronidazole had a stay of 3.7 days (Ciraru‐Vigneron 1986).
Buisson and colleagues reported that the mean treatment for the amoxicillin plus clavulanate group was four days followed by a mean of 17 days of PO therapy, and for ampicillin plus gentamicin plus metronidazole, it was seven days per protocol, due to the use of gentamicin, followed by ampicillin plus metronidazole until clinical improvement (Buisson 1989).
Ciraru‐Vigneron and colleagues reported that the mean duration of IV therapy was 7.6 (SD 2.1) days in the amoxicillin plus clavulanate group and 7.7 (SD 2.2) days in the ampicillin plus gentamicin plus metronidazole group. They did not specify if the PO treatment following IV treatment was performed in hospital, but they were similar (11.2 (SD 4.8) days with amoxicillin plus clavulanate and 11.1 (SD 6.6) days with ampicillin plus gentamicin plus metronidazole) (Ciraru‐Vigneron 1989).
Crombleholme and colleagues reported that treatment was for 14 days, starting with IV infusion and switched to PO, but they did not report if PO therapy was in hospital (Crombleholme 1989). In their previous study, IV treatment length was mentioned as at least five days, without further details (Crombleholme 1986).
Fischbach and colleagues admitted women for IV treatment for two to five days, followed by seven to 12 days of PO therapy, without further details (Fischbach 1994).
3.7. Fertility outcome
No studies reported live birth rate.
3.8. Other analyses
We explored publication bias through visual assessment of funnel plot asymmetry when there were data from 10 or more trials in the same analysis. We constructed a funnel plot for severe PID using regimens containing nitroimidazoles versus no nitroimidazoles (Analysis 3.3, Figure 12) and noted some asymmetry in the plot, suggestive of potential publication bias. Although it is usually impossible to know the precise mechanism for funnel plot asymmetry, publication bias could explain the presence of an asymmetrical funnel plot.
12.

Funnel plot of comparison: 3.3 Effectiveness of cure in severe pelvic inflammatory disease in regimens containing nitroimidazoles versus without nitroimidazoles.
4. Regimens containing clindamycin plus aminoglycoside versus regimens containing quinolone
Three studies compared clindamycin plus aminoglycoside versus quinolone in mild‐moderate PID (Apuzzio 1989) or severe PID (Crombleholme 1989; Thadepalli 1991).
Primary outcomes
4.1. Effectiveness
4.1a. Clinical cure in mild‐moderate pelvic inflammatory disease
One study compared clindamycin with an aminoglycoside (gentamicin) versus a quinolone (ciprofloxacin) (Apuzzio 1989). We are uncertain whether clindamycin plus aminoglycoside improves rates of cure in mild‐moderate PID compared to quinolone (RR 0.88, 95% CI 0.69 to 1.13; 1 study, 25 women; I2 = 0%; very low‐quality evidence) (Analysis 4.1;Figure 13).
4.1. Analysis.

Comparison 4: Regimens containing clindamycin plus aminoglycoside versus quinolone, Outcome 1: Effectiveness of cure in mild‐moderate PID
13.

Forest plot of comparison: 4 Regimens containing clindamycin plus aminoglycoside versus quinolone, outcome: 4.1 Effectiveness of cure in mild‐moderate pelvic inflammatory disease.
This suggests that if the rate of clinical cure in women with mild‐moderate PID using regimens including quinolone was 2%, the rate using regimens including clindamycin and aminoglycoside would be 62% to 96%.
4.1b. Clinical cure in severe pelvic inflammatory disease
We included two studies in the analysis of clinical cure in severe PID (Crombleholme 1989; Thadepalli 1991). We are uncertain whether clindamycin plus aminoglycoside improves rates of cure for severe PID compared to quinolones (RR 1.02, 95% CI 0.87 to 1.19; 2 studies, 151 women; I2 = 0%; low‐quality evidence) (Analysis 4.2;Figure 14).
4.2. Analysis.

Comparison 4: Regimens containing clindamycin plus aminoglycoside versus quinolone, Outcome 2: Effectiveness of cure in severe PID
14.

Forest plot of comparison: 4 Regimens containing clindamycin plus aminoglycoside versus quinolone, outcome: 4.2 Effectiveness of cure in severe pelvic inflammatory disease.
The evidence suggests that if the rate of clinical cure in women with severe PID using regimens including quinolone was 80%, the rate using regimens including clindamycin and aminoglycoside would be 71% to 89%.
4.2. Adverse events
4.2.1. Antibiotic‐related adverse effects leading to discontinuation of therapy
The incidence of antibiotic‐related adverse effects leading to discontinuation of therapy with clindamycin with aminoglycoside was 0% (95% CI 0% to 4.4%) and with quinolone was 5% (95% CI 1.9% to 12%). We are uncertain whether clindamycin plus aminoglycoside improves the rates of discontinuation compared to quinolones (RR 0.21, 95% CI 0.02 to 1.72; 3 studies, 163 women; I2 = 0%; very low‐quality evidence) (Analysis 4.3).
4.3. Analysis.

Comparison 4: Regimens containing clindamycin plus aminoglycoside versus quinolone, Outcome 3: Any antibiotic‐related adverse effect leading to discontinuation
This suggests that if the rate of adverse outcomes in women with PID using regimens including quinolone was 5%, the rate using regimens with clindamycin and aminoglycoside would be 0% to 4.4%.
Data are depicted in Table 4.
Secondary outcomes
4.3. Microbiological clearance of chlamydia
Three studies reported chlamydia clearance (Apuzzio 1989; Crombleholme 1989; Thadepalli 1991). Cure occurred in 10/10 women in the clindamycin plus aminoglycoside group (100%, 95% CI 72% to 100%) and in 11/12 women in the quinolone group (92%, 95% CI 65% to 99%).
This suggests that if the rate of microbiological clearance of C trachomatis in women using regimens including quinolone was 80%, the rate using regimens including clindamycin and aminoglycoside would be 72% to 100%.
4.4. Microbiological clearance of gonorrhoea
Three studies reported gonorrhoea clearance (Apuzzio 1989; Crombleholme 1989; Thadepalli 1991). Cure occurred in 44/44 women in the clindamycin plus aminoglycoside group (100%, 95% CI 92% to 100%) and in 41/41 women in the quinolone group (100%, 95% CI 91% to 100%).
This suggests that if the rate of microbiological clearance of N gonorrhoeae in women using regimens including quinolone was 100%, the rate using regimens including clindamycin and aminoglycoside would be 92% to 100%.
4.5. Laparoscopic evidence of resolution of pelvic inflammatory disease based on physician opinion
We found no data for laparoscopic evidence of resolution of PID.
4.6. Length of stay (for inpatient care)
We found no data suitable for analysis for length of hospital stay. Crombleholme and colleagues reported that treatment was for 14 days, starting with IV infusion and then switched to PO, but they did not report if PO therapy was in hospital (Crombleholme 1989). Apuzzio and colleagues did not give many details of the length of stay. They mentioned that women received IV antibiotics for three to five days until they were asymptomatic for 24 hours (Apuzzio 1989). Likewise, Thadepalli reported that women received IV ciprofloxacin for three or more days, followed by PO ciprofloxacin for about one week (Thadepalli 1991).
4.7. Fertility outcome
No studies reported live birth rate.
5. Regimens containing clindamycin plus aminoglycoside versus regimens containing cephalosporin
Ten studies compared clindamycin plus aminoglycoside versus cephalosporin in mild‐moderate PID (Sweet 1985; Walters 1990) or severe PID (Roy 1985; Sweet 1985; Soper 1988; Martens 1990; Roy 1990; Walters 1990; Landers 1991; Maria 1992; Hemsell 1994; Balbi 1996). Studies from Sweet 1985 and Walters 1990 had both populations with mild‐moderate and severe PID, thus they were used in both analyses.
Primary outcomes
5.1. Effectiveness
5.1a. Clinical cure in mild‐moderate pelvic inflammatory disease
We analyzed two studies for clinical cure in mild‐moderate PID (Sweet 1985; Walters 1990). There was probably little or no difference between clindamycin plus aminoglycoside and cephalosporin in rates of cure for mild‐moderate PID (RR 1.02, 95% CI 0.95 to 1.09; 2 studies, 150 women; I2 = 0%; low‐quality evidence) (Analysis 5.1; Figure 15).
5.1. Analysis.

Comparison 5: Regimens containing clindamycin plus aminoglycoside versus cephalosporin, Outcome 1: Effectiveness of cure in mild‐moderate PID
15.

Forest plot of comparison: 5 Regimens containing clindamycin plus aminoglycoside versus cephalosporin, outcome: 5.1 Effectiveness of cure in mild‐moderate pelvic inflammatory disease.
This suggests that if the rate of clinical cure in women with mild‐moderate PID using regimens including cephalosporin was 96%, the rate using regimens including clindamycin and aminoglycoside would be 91% to 99%.
5.1b. Clinical cure in severe pelvic inflammatory disease
We included 10 studies in the analysis of clinical cure in severe PID (Roy 1985; Sweet 1985; Soper 1988; Martens 1990; Roy 1990; Walters 1990; Landers 1991; Maria 1992; Hemsell 1994; Balbi 1996). There was probably little or no difference between clindamycin plus aminoglycoside and cephalosporin in rates of cure of severe PID (RR 1.00, 95% CI 0.95 to 1.06; 10 studies, 959 women; I2 = 21%; moderate‐quality evidence) (Analysis 5.2; Figure 16).
5.2. Analysis.

Comparison 5: Regimens containing clindamycin plus aminoglycoside versus cephalosporin, Outcome 2: Effectiveness of cure in severe PID
16.

5.2 Effectiveness of cure in severe pelvic inflammatory disease in regimens containing clindamycin plus aminoglycoside versus cephalosporin.
This suggests that if the rate of clinical cure in women with severe PID using regimens including cephalosporin was 84%, the rate using regimens including clindamycin and aminoglycoside would be 80% to 87%.
5.2. Adverse events
5.2.1. Antibiotic‐related adverse effects leading to discontinuation of therapy
We included 10 studies in the analysis of antibiotic‐related adverse effects leading to discontinuation of therapy (Roy 1985; Sweet 1985; Soper 1988; Martens 1990; Roy 1990; Walters 1990; Landers 1991; Maria 1992; Hemsell 1994; Balbi 1996). We are uncertain whether clindamycin plus aminoglycoside improves the rates of discontinuation of treatment compared to cephalosporin (RR 0.78, 95% CI 0.18 to 3.42; 10 studies, 1172 women; I2 = 0%; very low‐quality evidence) (Analysis 5.3).
5.3. Analysis.

Comparison 5: Regimens containing clindamycin plus aminoglycoside versus cephalosporin, Outcome 3: Any antibiotic‐related adverse effect leading to discontinuation
This suggests that if the rate of adverse outcomes in women with PID using regimens including cephalosporin was 4%, the rate using regimens with clindamycin and aminoglycoside would be 0% to 2%.
Data are depicted in Table 5.
Secondary outcomes
5.3. Microbiological clearance of chlamydia
Five studies reported chlamydia clearance (Sweet 1985; Roy 1990; Walters 1990; Maria 1992; Balbi 1996). Cure occurred in 53/56 women in the cephalosporin group (94.6%, 95% CI 85% to 98%) and in 75/78 women in the clindamycin plus aminoglycoside group (96%, 95% CI 89% to 99%).
This suggests that if the rate of microbiological clearance of C trachomatis in women using regimens including cephalosporin was 95%, the rate using regimens including clindamycin and aminoglycoside would be 89% to 99%.
5.4. Microbiological clearance of gonorrhoea
Five studies reported gonorrhoea clearance (Sweet 1985; Roy 1990; Walters 1990; Maria 1992; Balbi 1996). Cure occurred in 96/96 women in the clindamycin plus aminoglycoside group (100%, 95% CI 96% to 100%) and 115/117 women in the cephalosporin group (98%, 95% CI 94% to 99%).
This suggests that if the rate of microbiological clearance of N gonorrhoeae in women using regimens including cephalosporin was 98%, the rate using regimens including clindamycin and aminoglycoside would be 96% to 100%.
5.5. Laparoscopic evidence of resolution of pelvic inflammatory disease based on physician opinion
We found no data for laparoscopic evidence of resolution of PID.
5.6. Length of stay (for inpatient care)
Seven studies provided insufficient data for analysis of length of hospital stay (Roy 1985; Sweet 1985; Roy 1990; Walters 1990; Landers 1991; Maria 1992; Balbi 1996). Three studies provided the mean and SDs of hospital stay, or range of days (Soper 1988; Martens 1990; Hemsell 1994). The mean length of stay for the cephalosporin group varied from 5.8 days to 9.6 days (range 3 days to 18 days) and in the clindamycin plus aminoglycoside group varied from 5.8 days to 9.8 days (range 2 days to 25 days).
5.7. Fertility outcome
No studies reported live birth rate.
Other analyses
We were unable to conduct our planned subgroup analyses due to insufficient data in the included studies.
Discussion
Summary of main results
We included 39 trials with 6894 women in the review. We found no clear evidence of a difference between any of the regimens studied in terms of effectiveness or safety.
The only comparison that clearly suggested a difference between the interventions was the sensitivity analysis of cases of mild‐moderate PID for the comparison macrolide (azithromycin) versus tetracycline (doxycycline). When we limited analysis to the single study at low risk of bias, moderate‐quality evidence suggested that azithromycin was superior to doxycycline in achieving clinical cure (Table 1).
Some guidelines have recommended the use of nitroimidazoles for treating PID (Ross 2007; Workowski 2015). We found no conclusive evidence of a difference between the use or not of nitroimidazoles (metronidazole) in rates of cure in either mild‐moderate or severe PID. There was also no clear evidence of a difference in rates of adverse effects.
Overall completeness and applicability of evidence
Although we conducted comprehensive searches to identify all published and unpublished RCTs, this systematic review included trials at high risk of bias and consequently with low confidence in the estimate of effect (see Table 1; Table 2; Table 3; Table 4; Table 5). When we used ITT analysis, there was substantial heterogeneity in the azithromycin trial results, which may limit our conclusions.
Data were lacking for several of our secondary outcomes. None of the included studies reported data on fertility or laparoscopic evidence of PID resolution, and data were very scant on length of hospital stay.
The applicability of the evidence to the target population (women of reproductive age diagnosed with PID) was broad because the included trials were conducted in different clinical settings and implemented varying diagnostic approaches. Additionally, the interventions analyzed in the review are available in various clinical settings and represent the most frequently used therapeutic schemes in current clinical practice. Given these factors, we consider that the evidence identified applies to a wide range of women with PID varying in disease severity, age, geographical location, and diagnostic criteria, which provides external validity.
Our results on the use or no use of nitroimidazole should be interpreted with caution. The rationale for using nitroimidazole is to cover anaerobic bacteria and it is commonly used with other drugs (e.g. doxycycline and ceftriaxone). In most of the comparisons, anaerobic coverage was given with other medications, such as moxifloxacin (Heystek 2009; Aşicioğlu 2013), amoxicillin plus clavulanate (Tison 1988; Buisson 1989; Ciraru‐Vigneron 1989), ampicillin plus sulbactam (Crombleholme 1986; Crombleholme 1987), or clindamycin (Leboeuf 1987; Sirayapiwat 2002), and this may explain the lack of evidence of the superiority on the use of nitroimidazole. Data derived from the tabular section of the ClinicalTrials.gov from the study that compared doxycycline plus metronidazole versus doxycycline plus placebo may clarify this topic (Wiesenfeld 2017). These authors reported a clinical cure in 96/116 women in the metronidazole group, compared to 94/117 women in the placebo group. There was probably little or no difference between groups (RR 1.03, 95% CI 0.91 to 1.16; 233 women; some concerns regarding of bias) in clinical cure after three days of treatment. In contrast, metronidazole probably improves the rates of clearance of anaerobic bacteria compared to placebo (RR 1.42, 95% CI 1.03 to 1.95; 40 women; some concerns regarding of bias; NNTB 3) when endometrial culture was employed for diagnosis, using a per‐protocol analysis. In an ITT analysis (six women were lost to follow‐up in each group), there is probably little or no difference in use or not metronidazole (RR 1.38, 95% CI 0.89 to 2.15; 52 women; some concerns regarding of bias). Without the final published data, these results must be interpreted with caution.
PID can be life or fertility threatening, and treatment is routinely started before laboratory cultures or laparoscopic confirmation. In some cases, women were subsequently diagnosed with another condition; however, we included all women in our ITT analysis, in accordance with our review protocol.
Quality of the evidence
Most of the 39 included studies had unclear or high risk of bias in most domains, and only three were at low risk of bias in most domains (Ross 2006; Savaris 2007; Judlin 2010b). The remaining studies had several limitations, for instance, 26 trials did not clearly define randomization, and there was potential performance and detection bias in 20 studies (Figure 3).
The overall quality of the evidence ranged from very low to high, the main limitations being serious risk of bias (due to poor reporting of study methods and lack of blinding), serious inconsistency, and serious imprecision. There was substantial heterogeneity in the comparison between azithromycin and doxycycline (I2 = 72%; Figure 4), and in the comparison of nitroimidazole versus no nitroimidazole (I2 = 60%; Figure 10). Imprecision was related to suboptimal sample sizes and the low number of studies for some comparisons.
Of note, in Analysis 1.1, if the results were considered as failure, instead of cure, the results analyzed using RR would not be consistent; however, using odds ratio, results would be consistent. By using OR, the results were similar, revealing similar interpretation of the results in either method of analysis (OR 1.95, 95% CI 0.66 to 7.72; 243 women, 2 studies, I2 = 68%; very low‐quality evidence; data not shown).
The quality of evidence for the outcomes analyzed is provided in Table 1; Table 2; Table 3; Table 4; Table 5. The only high‐quality evidence was for the sensitivity analysis regarding the use (or not) of nitroimidazole. There was moderate‐quality evidence in the sensitivity analysis regarding the use of azithromycin in mild‐moderate cases of PID, in comparisons between the use or not of nitroimidazole for curing mild‐moderate or severe PID, and in comparisons between clindamycin plus aminoglycoside versus cephalosporins for curing severe PID.
For all other comparisons, the evidence was low or very‐low quality.
Potential biases in the review process
An important limitation of this systematic review was the potential for measurement bias introduced by using the investigators' definitions of cure. There was a wide variation in methods used and a widely accepted objective outcome was lacking. Despite the clinical outcomes being relevant and their assessment being sufficient to understand the effects of interventions in the short term, the short‐term follow‐up only of most of the studies prevented a more detailed identification of long‐term sequelae. In addition, the inaccuracy of clinical diagnosis for PID and the wide variety of assessment criteria used for a clinical cure may have reduced the power of the analysis to detect a significant effect. For instance, some authors have used a reduction of 70% of initial pain over a period of time to define clinical cure. This approach may seem adequate; consider, however, two cases, both on the same 10‐point visual analog scale for pain: one woman started with a pain score of 10 out of 10 and the other with a pain score of 5 out of 10. After treatment, both cases report a pain score of 2. The former would be considered as cured and the latter not. Therefore, there is a clear need for core outcome measures to be developed that take into account the different effect measures in use.
Some studies identified PID and endometritis separately but these were pooled for our analysis.
Agreements and disagreements with other studies or reviews
One previous meta‐analysis, published in 1993, formed the basis for the CDC guidelines (Walker 1993). The authors reported pooled clinical cure rates ranging from 75% to 94%, which is similar to the 2017 Cochrane Review (Savaris 2017). The addition of two new references in our updated review did not change our previous results. Therefore, our results support the updated 2015 CDC guidelines (Workowski 2015), and the British Association of Sexual Health and HIV (BASHH Guidelines 2019), but not the inclusion of nitroimidazoles in treatment regimens.
Authors' conclusions
Implications for practice.
We found no conclusive evidence that one regimen is safer or more effective than any other for the cure of PID, and there is no clear evidence for the use of nitroimidazoles (metronidazole) compared to other drugs with activity over anaerobes. Moderate‐quality evidence from a single study at low risk of bias suggests that a macrolide (azithromycin) may be more effective than a tetracycline (doxycycline) for curing mild‐moderate PID. There was probably little or no difference in rates of cure between metronidazole or no metronidazole in mild‐moderate or severe PID. Our review considers only the drugs that are in current use and mentioned by the US Centers for Disease Control and Prevention (CDC).
Implications for research.
There is a need for high‐quality randomized controlled trials to assess treatments for women with PID, particularly further trials comparing PO azithromycin versus PO doxycycline and with or without nitroimidazoles. Of note, the comparison against nitroimidazoles must be with drugs without activity against anaerobic bacteria. The lack of a consistent outcome to assess response to therapy is a major limitation. For instance, some authors have used a reduction of 70% of initial pain over a period of time to assess this outcome. This approach may seem adequate; however, consider two cases, both on a 10‐point visual analog scale: one woman started with a pain score of 10 out of 10 and the other with a pain score of 5 out of 10. After treatment, both cases report a pain score of 2. The former would be considered as cured and the latter not. Therefore, there is a clear need for core outcome measures to be developed that take into account the different effect measures in use.
Long term sequelae, such as infertility, chronic pelvic pain, and the incidence of ectopic pregnancy should be collected and analyzed prospectively in randomized clinical trials.
What's new
| Date | Event | Description |
|---|---|---|
| 10 January 2020 | New citation required but conclusions have not changed | The updated version of this review added two new studies. One study compared the use or not of metronidazole plus doxycycline (Wiesenfeld 2017); the other, the use of azithromycin plus ceftriaxone plus metronidazole versus ofloxacin plus metronidazole (Dean 2016). Both studies verified the rates of cure in mild‐moderate cases of PID. There were no changes in the previous conclusions. |
| 20 December 2019 | New search has been performed | Two new studies added (Dean 2016; Wiesenfeld 2017). |
History
Protocol first published: Issue 1, 2013 Review first published: Issue 4, 2017
Notes
Acknowledgements
The authors of the 2020 update thank Dr Sebastian Franik for his contributions to the previous published version of this review (Savaris 2017).
The authors of the 2020 review thank Edith Angel‐Műller and Nicola Low for providing peer review comments.
We acknowledge the support of Helen Nagels, Motokazu Yanagi, Kensuke Takaoka, and Chen Hengxi with the non‐English language studies.
Appendices
Appendix 1. Electronic search strategies
CENTRAL (Ovid platform)
1 exp Pelvic Inflammatory Disease/ (418)
2 (pelvic adj5 inflammatory adj5 disease$).tw. (282)
3 pid.tw. (273)
4 pelvic inflammat$.tw. (310)
5 pelvic peritonitis.tw. (0)
6 adnexitis.tw. (10)
7 exp Pelvic Infection/ (196)
8 (pelvic adj5 infection$).tw. (208)
9 (ovar$ adj5 inflammation).tw. (16)
10 exp Oophoritis/ (7)
11 oophoriti$.tw. (7)
12 exp Endometritis/ (216)
13 endometritis.tw. (356)
14 endomyometritis.tw. (56)
15 exp Salpingitis/ (42)
16 salpingiti$.tw. (56)
17 exp Parametritis/ (9)
18 parametriti$.tw. (2)
19 (celluliti$ adj5 pelvic).tw. (26)
20 exp Fallopian Tube Diseases/ (134)
21 (fallopian adj5 tube adj5 disease$).tw. (5)
22 (tubal adj5 obstruction$).tw. (19)
23 (uterine adj5 tube adj5 disease$).tw. (0)
24 (tuboovarian adj5 abscess).tw. (5)
25 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 (1286)
26 exp Anti‐Bacterial Agents/ (20463)
27 (anti adj5 bacterial$).tw. (90)
28 antibacterial$.tw. (1562)
29 antibiotic$.tw. (13603)
30 bacteriocid$.tw. (13)
31 bactericide$.tw. (5)
32 exp Anti‐Infective Agents/ (48142)
33 (anti adj5 infective$).tw. (127)
34 antiinfective$.tw. (21)
35 microbicid$.tw. (257)
36 antimicrobial$.tw. (3551)
37 (anti adj5 microbial$).tw. (93)
38 exp Aminoglycosides/ (6672)
39 aminoglycosides.tw. (211)
40 exp Amoxicillin‐Potassium Clavulanate Combination/ (461)
41 amoxicillin.tw. (2645)
42 exp Azithromycin/ (702)
43 azithromycin.tw. (1283)
44 exp Cefotaxime/ (1574)
45 cefotaxime.tw. (598)
46 exp Cefotetan/ (105)
47 cefotetan.tw. (155)
48 exp Cefoxitin/ (274)
49 cefoxitin.tw. (410)
50 exp Ceftizoxime/ (164)
51 ceftizoxime.tw. (125)
52 exp Ceftriaxone/ (565)
53 ceftriaxone.tw. (940)
54 exp Ciprofloxacin/ (941)
55 ciprofloxacin.tw. (1597)
56 exp Clindamycin/ (664)
57 clindamycin.tw. (1082)
58 exp Doxycycline/ (731)
59 doxycycline.tw. (1120)
60 exp Gentamicins/ (1044)
61 gentamicin.tw. (1284)
62 exp Metronidazole/ (1688)
63 metronidazole.tw. (2693)
64 moxifloxacin.tw. (667)
65 exp Ofloxacin/ (752)
66 ofloxacin.tw. (824)
67 levofloxacin.tw. (730)
68 sultamicillin.tw. (44)
69 (ampicillin adj5 sulbactam).tw. (229)
70 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49 or 50 or 51 or 52 or 53 or 54 or 55 or 56 or 57 or 58 or 59 or 60 or 61 or 62 or 63 or 64 or 65 or 66 or 67 or 68 or 69 (63988)
71 25 and 70 (611)
MEDLINE(Ovid platform)
1 exp Pelvic Inflammatory Disease/ (10207)
2 (pelvic adj5 inflammatory adj5 disease$).tw. (4083)
3 pid.tw. (3492)
4 pelvic inflammat$.tw. (4283)
5 pelvic peritonitis.tw. (105)
6 adnexitis.tw. (496)
7 exp Pelvic Infection/ (5135)
8 (pelvic adj5 infection$).tw. (1833)
9 (ovar$ adj5 inflammation).tw. (279)
10 exp Oophoritis/ (499)
11 oophoriti$.tw. (407)
12 exp Endometritis/ (3599)
13 endometritis.tw. (3169)
14 endomyometritis.tw. (200)
15 exp Salpingitis/ (1994)
16 salpingiti$.tw. (1513)
17 exp Parametritis/ (198)
18 parametriti$.tw. (112)
19 (celluliti$ adj5 pelvic).tw. (97)
20 exp Fallopian Tube Diseases/ (7297)
21 (fallopian adj5 tube adj5 disease$).tw. (84)
22 (tubal adj5 obstruction$).tw. (423)
23 (uterine adj5 tube adj5 disease$).tw. (3)
24 (tuboovarian adj5 abscess).tw. (143)
25 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 (23104)
26 exp Anti‐Bacterial Agents/ (613243)
27 (anti adj5 bacterial$).tw. (2879)
28 antibacterial$.tw. (52343)
29 antibiotic$.tw. (261141)
30 bacteriocid$.tw. (544)
31 bactericide$.tw. (658)
32 exp Anti‐Infective Agents/ (1415302)
33 (anti adj5 infective$).tw. (3071)
34 antiinfective$.tw. (417)
35 microbicid$.tw. (5363)
36 antimicrobial$.tw. (111599)
37 (anti adj5 microbial$).tw. (2944)
38 exp Aminoglycosides/ (140356)
39 aminoglycosides.tw. (8449)
40 exp Amoxicillin‐Potassium Clavulanate Combination/ (2250)
41 amoxicillin.tw. (11786)
42 exp Azithromycin/ (4124)
43 azithromycin.tw. (6083)
44 exp Cefotaxime/ (12415)
45 cefotaxime.tw. (7263)
46 exp Cefotetan/ (485)
47 cefotetan.tw. (734)
48 exp Cefoxitin/ (1763)
49 cefoxitin.tw. (3821)
50 exp Ceftizoxime/ (1101)
51 ceftizoxime.tw. (887)
52 exp Ceftriaxone/ (5094)
53 ceftriaxone.tw. (8422)
54 exp Ciprofloxacin/ (11440)
55 ciprofloxacin.tw. (20547)
56 exp Clindamycin/ (5195)
57 clindamycin.tw. (8787)
58 exp Doxycycline/ (8330)
59 doxycycline.tw. (10686)
60 exp Gentamicins/ (17804)
61 gentamicin.tw. (21225)
62 exp Metronidazole/ (11543)
63 metronidazole.tw. (13091)
64 moxifloxacin.tw. (3450)
65 exp Ofloxacin/ (6176)
66 ofloxacin.tw. (5988)
67 levofloxacin.tw. (5700)
68 sultamicillin.tw. (141)
69 (ampicillin adj5 sulbactam).tw. (1564)
70 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49 or 50 or 51 or 52 or 53 or 54 or 55 or 56 or 57 or 58 or 59 or 60 or 61 or 62 or 63 or 64 or 65 or 66 or 67 or 68 or 69 (1632933)
71 randomized controlled trial.pt. (425167)
72 controlled clinical trial.pt. (91285)
73 randomized.ab. (355829)
74 placebo.ab. (174189)
75 clinical trials as topic.sh. (178323)
76 randomly.ab. (254885)
77 trial.ti. (155344)
78 71 or 72 or 73 or 74 or 75 or 76 or 77 (1039211)
79 exp animals/ not humans.sh. (4280378)
80 78 not 79 (957018)
81 25 and 70 and 80 (684)
Embase
#1 'pelvic inflammatory disease'/exp (13,726)
#2 'pelvic inflammatory disease':ti,ab (4326)
#3 p.i.d.:ti,ab (55)
#4 pid:ti,ab (5,216)
#5 'pelvic infection':ti,ab (731)
#6 (pelvi? NEAR/5 inflammat*):ti,ab (5,453)
#7 'pelvic peritonitis':ti,ab (137)
#8 'ovary inflammation'/exp (695)
#9 (ovar* NEAR/5 inflammatio*):ti,ab (377)
#10 oophoriti*:ti,ab (471)
#11 ovaritis:ti,ab (48)
#12 'endometritis'/exp (5,280)
#13 endometritis:ti,ab (3,647)
#14 'salpingitis'/exp (2,633)
#15 salpingitis:ti,ab (1,657)
#16 'uterine tube disease'/exp (9,070)
#17 'uterine tube disease':ti,ab (1)
#18 'uterine tube inflammation':ti,ab (1)
#19 'fallopian tube diseases':ti,ab (3)
#20 'fallopian tube inflammation':ti,ab (2)
#21 'adnexitis'/exp (1,019)
#22 adnexitis:ti,ab (552)
#23 'adnex inflammation uterine':ti,ab (0)
#24 'adnexa infection':ti,ab (0)
#25 'adnexa inflammation':ti,ab (0)
#26 parametriti*:ti,ab (112)
#27 (para NEAR/5 metriosis):ti,ab (0)
#28 'tuboovarian abscess':ti,ab (190)
#29 #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16
OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28 (31,956)
#30 'antiinfective agent'/exp (2,566,913)
#31 'antiinfective agent':ti,ab (25)
#32 antibacterial*:ti,ab (70,680)
#33 'anti bacterial':ti,ab (3,425)
#34 'anti infective':ti,ab (3,462)
#35 antimicrobial*:ti,ab (147,222)
#36 bacteriocid*:ti,ab (660)
#37 bactericide*:ti,ab (1,159)
#38 microbicid*:ti,ab (6,092)
#39 'antibiotic agent'/exp (1,121,485)
#40 antibiotic*:ti,ab (338,040)
#41 'aminoglycoside'/exp (13,112)
#42 aminoglycoside:ti,ab (12,338)
#43 'amoxicillin plus clavulanic acid'/exp (29,766)
#44 'amoxicillin':ti,ab (16,673)
#45 'azithromycin'/exp (26,174)
#46 azithromycin:ti,ab (8,812)
#47 'cefotaxime'/exp (35,191)
#48 cefotaxime:ti,ab (9,344)
#49 'cefotetan'/exp (3,075)
#50 cefotetan:ti,ab (977)
#51 'cefoxitin'/exp (15,495)
#52 cefoxitin:ti,ab (4,658)
#53 'ceftizoxime'/exp (3,860)
#54 ceftizoxime:ti,ab (1,234)
#55 'ceftriaxone'/exp (45,306)
#56 ceftriaxone:ti,ab (12,087)
#57 'ciprofloxacin'/exp (77,874)
#58 ciprofloxacin:ti,ab (27,319)
#59 'clindamycin'/exp (42,275)
#60 clindamycin:ti,ab (11,122)
#61 'doxycycline'/exp (41,407)
#62 doxycycline:ti,ab (14,273)
#63 'gentamicin'/exp (90,658)
#64 gentamicin:ti,ab (26,194)
#65 'metronidazole'/exp (56,425)
#66 metronidazole:ti,ab (17,513)
#67 'moxifloxacin'/exp (13,514)
#68 moxifloxacin:ti,ab (4,833)
#69 'ofloxacin'/exp (22,915)
#70 ofloxacin:ti,ab (7,905)
#71 'levofloxacin'/exp (25,916)
#72 levofloxacin:ti,ab (8,786)
#73 'sultamicillin'/exp (8,641)
#74 sultamicillin:ti,ab (277)
#75 'ampicillin sulbactam':ti,ab (1,567)
#76 #30 OR #31 OR #32 OR #33 OR #34 OR #35 OR #36 OR #37 OR #38 OR #39 OR #40 OR #41 OR #42 OR #43 OR #44 OR #45 OR #46 OR #47 OR #48 OR #49 OR #50 OR #51 OR #52 OR #53 OR #54 OR #55 OR #56 OR #57 OR #58 OR #59 OR #60 OR #61 OR #62 OR #63 OR #64 OR #65 OR #66 OR #67 OR #68 OR #69 OR #70 OR #71 OR #72 OR #73 OR #74 OR #75 (2,684,527)
#77 'randomized controlled trial'/exp OR 'single blind procedure'/exp OR 'double blind procedure'/exp OR 'crossover procedure'/exp OR random*:ab,ti OR placebo*:ab,ti OR allocat*:ab,ti OR crossover*:ab,ti OR 'cross over':ab,ti OR trial:ti OR (doubl* NEXT/1 blind*):ab,ti NOT ('animal'/de OR 'animal experiment'/de OR 'nonhuman'/de NOT ('animal'/de OR 'animal experiment'/de OR 'nonhuman'/de AND 'human'/de)) (1,286,106)
#78 #29 AND #76 AND #77 (812)
LILACS (IAHx interface)
((mh:"Enfermedad Inflamatoria Pélvica" OR tw:"enfermedad inflamatoria pélvica" OR tw:"pelvic inflammatory disease" OR tw:"doença inflamatória pélvica" OR tw:"doença pélvica inflamatória" OR tw:"doença inflamatória da pelve" OR tw:anexit$ OR tw:adnexitis OR tw:epi OR tw:eip OR tw:"inflamación pélvica" OR tw:"inflamación del ovario" OR tw:"peritonitis pélvica" OR tw:"absceso tubo ovárico" OR mh:Endometritis OR tw:endometrit$ OR tw:endomiometrit$ OR tw:endomyometritis OR mh:Ooforitis OR tw:ooforit$ OR tw:oophoritis OR mh:Parametritis OR tw:parametrit$ OR tw:"celulitis pélvica" OR tw:"cellulitis pelvic" OR tw:"celulite pélvica" OR mh:Salpingitis OR tw:salpingit$ OR mh:"Infección Pélvica" OR tw:"infección pélvica" OR tw:"pelvic infection" OR tw:"infecção pélvica" OR mh:"Enfermedades de las Trompas Uterinas" OR tw:"enfermedades de las trompas uterinas" OR tw:"fallopian tube diseases" OR tw:"doenças das tubas uterinas" OR tw:"enfermedades de las trompas de falopio" OR tw:"doenças das trompas de falópio") AND (mh:Antibacterianos OR tw:antibacterian$ OR tw:"anti bacterial" OR tw:antibacterial$ OR tw:antibiótic$ OR tw:antibiotic$ OR tw:bactericid$ OR mh:Antiinfecciosos OR tw:antiinfeccioso$ OR tw:"anti infective" OR tw:microbicid$ OR tw:antimicrobian$ OR mh:Aminoglicósidos OR tw:aminoglicósidos OR tw:aminoglycosides OR tw:aminoglicosídeos OR mh:"Combinación Amoxicilina‐Clavulanato de Potasio" OR tw:"combinación amoxicilina clavulanato de potasio" OR tw:"amoxicillin potassium clavulanate combination" OR tw:"combinação amoxicilina clavulanato de potássio" OR mh:Azitromicina OR tw:azitromicina OR tw:azithromycin OR mh:Cefotaxima OR tw:cefotaxim$ OR mh:Cefotetán OR tw:cefotetán OR tw:cefotetan OR mh:Cefoxitina OR tw:cefoxitin$ OR mh:Ceftizoxima OR tw:ceftizoxim$ OR mh:Ceftriaxona OR tw:ceftriaxon$ OR mh:Ciprofloxacino OR tw:ciprofloxacin$ OR mh:Clindamicina OR tw:clindamicina OR tw:clindamycin OR mh:Doxiciclina OR tw:doxiciclina OR tw:doxycycline OR mh:Gentamicinas OR tw:gentamicin$ OR mh:Metronidazol OR tw:metronidazol$ OR tw:moxifloxacina OR mh:Ofloxacino OR tw:ofloxacin$ OR tw:levofloxacino OR tw:"ampicilina sulbactam"))
RCTs filter:
((PT:"ensayo clinico controlado aleatorio" OR PT:"ensayo clinico controlado" OR PT:"estudio multicéntrico" OR MH:"ensayos clinicos controlados aleatorios como asunto" OR MH:"ensayos clinicos controlados como asunto" OR MH:"estudios multicéntricos como asunto" OR MH:"distribución aleatoria" OR MH:"método doble ciego" OR MH:"metodo simple‐ciego") OR ((ensaio$ OR ensayo$ OR trial$) AND (azar OR acaso OR placebo OR control$ OR aleat$ OR random$ OR enmascarado$ OR simpleciego OR ((simple$ OR single OR duplo$ OR doble$ OR double$) AND (cego OR ciego OR blind OR mask))) AND clinic$)) AND NOT (MH:animales OR MH:conejos OR MH:ratones OR MH:ratas OR MH:primates OR MH:perros OR MH:gatos OR MH:porcinos OR PT:"in vitro")
Appendix 2. Electronic search strategies – 2019 update
MEDLINE
| Type of search | UPDATE |
| Database |
|
| Platform | Ovid |
| Search date | 1 February 2019 |
| Range of search date | 2016–2019 |
| Language restrictions | None |
| Other limits | None |
| Search strategy (results) | 1. exp Pelvic Inflammatory Disease/ (10558) 2. (pelvic adj5 inflammatory adj5 disease$).tw. (4130) 3. pid.tw. (3601) 4. pelvic inflammat$.tw. (4333) 5. pelvic peritonitis.tw. (99) 6. adnexitis.tw. (492) 7. exp Pelvic Infection/ (5272) 8. (pelvic adj5 infection$).tw. (1838) 9. (ovar$ adj5 inflammation).tw. (312) 10. exp Oophoritis/ (507) 11. oophoriti$.tw. (411) 12. exp Endometritis/ (3819) 13. endometritis.tw. (3296) 14. endomyometritis.tw. (197) 15. exp Salpingitis/ (2012) 16. salpingiti$.tw. (1488) 17. exp Parametritis/ (197) 18. parametriti$.tw. (113) 19. (celluliti$ adj5 pelvic).tw. (94) 20. exp Fallopian Tube Diseases/ (7629) 21. (fallopian adj5 tube adj5 disease$).tw. (88) 22. (tubal adj5 obstruction$).tw. (429) 23. (uterine adj5 tube adj5 disease$).tw. (3) 24. (tuboovarian adj5 abscess).tw. (143) 25. or/1‐24 (23765) 26. exp Anti‐Bacterial Agents/ (690305) 27. (anti adj5 bacterial$).tw. (3293) 28. antibacterial$.tw. (57919) 29. antibiotic$.tw. (273630) 30. bacteriocid$.tw. (535) 31. bactericide$.tw. (717) 32. exp Anti‐Infective Agents/ (1544784) 33. (anti adj5 infective$).tw. (3369) 34. antiinfective$.tw. (428) 35. microbicid$.tw. (5526) 36. antimicrobial$.tw. (123452) 37. (anti adj5 microbial$).tw. (3175) 38. exp Aminoglycosides/ (149429) 39. aminoglycosides.tw. (8782) 40. exp Amoxicillin‐Potassium Clavulanate Combination/ (2436) 41. amoxicillin.tw. (12377) 42. exp Azithromycin/ (4687) 43. azithromycin.tw. (6570) 44. exp Cefotaxime/ (11391) 45. cefotaxime.tw. (7412) 46. exp Cefotetan/ (485) 47. cefotetan.tw. (728) 48. exp Cefoxitin/ (1836) 49. cefoxitin.tw. (3903) 50. exp Ceftizoxime/ (1120) 51. ceftizoxime.tw. (871) 52. exp Ceftriaxone/ (5627) 53. ceftriaxone.tw. (8676) 54. exp Ciprofloxacin/ (12623) 55. ciprofloxacin.tw. (21496) 56. exp Clindamycin/ (5516) 57. clindamycin.tw. (9055) 58. exp Doxycycline/ (9127) 59. doxycycline.tw. (11189) 60. exp Gentamicins/ (18504) 61. gentamicin.tw. (21740) 62. exp Metronidazole/ (12272) 63. metronidazole.tw. (13434) 64. exp Moxifloxacin/ (2290) 65. moxifloxacin.tw. (3716) 66. exp Ofloxacin/ (6844) 67. ofloxacin.tw. (6105) 68. levofloxacin.tw. (6158) 69. sultamicillin.tw. (136) 70. (ampicillin adj5 sulbactam).tw. (1596) 71. or/26‐70 (1757952) 72. randomized controlled trial.pt. (475257) 73. controlled clinical trial.pt. (92865) 74. randomized.ab. (386444) 75. placebo.ab. (180327) 76. clinical trials as topic.sh. (185910) 77. randomly.ab. (266755) 78. trial.ti. (170910) 79. 72 or 73 or 74 or 75 or 76 or 77 or 78 (1101129) 80. exp animals/ not humans.sh. (4542355) 81. 79 not 80 (1005272) 82. 25 and 71 and 81 (689) 83. limit 82 to yr="2016 ‐Current" (36) |
Embase
| Type of search | Update |
| Database | Embase |
| Platform | Embase.com |
| Search date | 1 February 2019 |
| Range of search date | 2016–2019 |
| Language restrictions | None |
| Other limits | None |
| Search strategy (results) | 1. 'pelvic inflammatory disease'/exp (15337) 2. 'pelvic inflammatory disease':ti,ab (4870) 3. p.i.d.:ti,ab (55) 4. pid:ti,ab (6235) 5. 'pelvic infection':ti,ab (807) 6. (pelvi? NEAR/5 inflammat*):ti,ab (6179) 7. 'pelvic peritonitis':ti,ab (146) 8. 'ovary inflammation'/exp (752) 9. (ovar* NEAR/5 inflammatio*):ti,ab (484) 10. oophoriti*:ti,ab (508) 11. ovaritis:ti,ab (49) 12. 'endometritis'/exp (6133) 13. endometritis:ti,ab (4374) 14. 'salpingitis'/exp (2740) 15. salpingitis:ti,ab (1729) 16. 'uterine tube disease'/exp (10179) 17. 'uterine tube disease':ti,ab (1) 18. 'uterine tube inflammation':ti,ab (1) 19. 'fallopian tube diseases':ti,ab (4) 20. 'fallopian tube inflammation':ti,ab (2) 21. 'adnexitis'/exp (1066) 22. adnexitis:ti,ab (548) 23. 'adnex inflammation uterine':ti,ab (0) 24. 'adnexa infection':ti,ab (0) 25. 'adnexa inflammation':ti,ab (1) 26. parametriti*:ti,ab (111) 27. (para NEAR/5 metriosis):ti,ab (0) 28. 'tuboovarian abscess':ti,ab (216) 29. #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28 (36631) 30. 'antiinfective agent'/exp (3364785) 31. 'antiinfective agent':ti,ab (32) 32. antibacterial*:ti,ab (88166) 33. 'anti bacterial':ti,ab (4638) 34. 'anti infective':ti,ab (4406) 35. antimicrobial*:ti,ab (186144) 36. bacteriocid*:ti,ab (690) 37. bactericide*:ti,ab (1069) 38. microbicid*:ti,ab (6953) 39. 'antibiotic agent'/exp (1414466) 40. antibiotic*:ti,ab (404425) 41. 'aminoglycoside'/exp (15071) 42. aminoglycoside:ti,ab (13589) 43. 'amoxicillin plus clavulanic acid'/exp (35098) 44. 'amoxicillin':ti,ab (20313) 45. 'azithromycin'/exp (31695) 46. azithromycin:ti,ab (11220) 47. 'cefotaxime'/exp (39257) 48. cefotaxime:ti,ab (10392) 49. 'cefotetan'/exp (3227) 50. cefotetan:ti,ab (1007) 51. 'cefoxitin'/exp (17434) 52. cefoxitin:ti,ab (5183) 53. 'ceftizoxime'/exp (3960) 54. ceftizoxime:ti,ab (1261) 55. 'ceftriaxone'/exp (54135) 56. ceftriaxone:ti,ab (14760) 57. 'ciprofloxacin'/exp (90877) 58. ciprofloxacin:ti,ab (32244) 59. 'clindamycin'/exp (47715) 60. clindamycin:ti,ab (12811) 61. 'doxycycline'/exp (48449) 62. doxycycline:ti,ab (17572) 63. 'gentamicin'/exp (101466) 64. gentamicin:ti,ab (29506) 65. 'metronidazole'/exp (63734) 66. metronidazole:ti,ab (20376) 67. 'moxifloxacin'/exp (16551) 68. moxifloxacin:ti,ab (5936) 69. 'ofloxacin'/exp (25005) 70. ofloxacin:ti,ab (8619) 71. 'levofloxacin'/exp (32243) 72. levofloxacin:ti,ab (10880) 73. 'sultamicillin'/exp (10259) 74. sultamicillin:ti,ab (285) 75. 'ampicillin sulbactam':ti,ab (1880) 76. #30 OR #31 OR #32 OR #33 OR #34 OR #35 OR #36 OR #37 OR #38 OR #39 OR #40 OR #41 OR #42 OR #43 OR #44 OR #45 OR #46 OR #47OR #48 OR #49 OR #50 OR #51 OR #52 OR #53 OR #54 OR #55 OR #56 OR #57 OR #58 OR #59 OR #60 OR #61 OR #62 OR #63 OR #64 OR #65 OR #66 OR #67 OR #68 OR #69 OR #70 OR #71 OR #72 OR #73 OR #74 OR #75 (3505837) 77. 'randomized controlled trial'/de (532805) 78. 'controlled clinical study'/de (426036) 79. random*:ti,ab (1367023) 80. 'randomization'/de (80722) 81. 'intermethod comparison'/de (244603) 82. placebo:ti,ab (281838) 83. compare:ti OR compared:ti OR comparison:ti (491480) 84. (evaluated:ab OR evaluate:ab OR evaluating:ab OR assessed:ab OR assess:ab) AND (compare:ab OR compared:ab OR comparing:ab OR comparison:ab) (1849974) 85. (open NEAR/1 label):ti,ab (68292) 86. ((double OR single OR doubly OR singly) NEAR/1 (blind OR blinded OR blindly)):ti,ab (216128) 87. 'double blind procedure'/de (157170) 88. (parallel NEXT/1 group*):ti,ab (22738) 89. crossover:ti,ab OR 'cross over':ti,ab (96212) 90. ((assign* OR match OR matched OR allocation) NEAR/5 (alternate OR group* OR intervention* OR patient* OR subject* OR participant*)):ti,ab (295547) 91. assigned:ti,ab OR allocated:ti,ab (346990) 92. (controlled NEAR/7 (study OR design OR trial)):ti,ab (310110) 93. volunteer:ti,ab OR volunteers:ti,ab (231464) 94. trial:ti (266539) 95. 'human experiment'/de (436152) 96. #77 OR #78 OR #79 OR #80 OR #81 OR #82 OR #83 OR #84 OR #85 OR #86 OR #87 OR #88 OR #89 OR #90 OR #91 OR #92 OR #93 OR #94OR #95 (4510062) 97. #29 AND #76 AND #96 (1668) 98. #29 AND #76 AND #96 AND [embase]/lim AND [2016‐2019]/py (307) |
CENTRAL
| Type of search | Update |
| Database | CENTRAL |
| Platform | Ovid |
| Search date | 1 February 2019 |
| Range of search date | 2016–2019 |
| Language restrictions | None |
| Other limits | None |
| Search strategy (results) | 1. exp Pelvic Inflammatory Disease/ (473) 2. (pelvic adj5 inflammatory adj5 disease$).tw. (388) 3. pid.tw. (386) 4. pelvic inflammat$.tw. (433) 5. pelvic peritonitis.tw. (1) 6. adnexitis.tw. (10) 7. exp Pelvic Infection/ (219) 8. (pelvic adj5 infection$).tw. (254) 9. (ovar$ adj5 inflammation).tw. (38) 10. exp Oophoritis/ (7) 11. oophoriti$.tw. (9) 12. exp Endometritis/ (250) 13. endometritis.tw. (470) 14. endomyometritis.tw. (61) 15. exp Salpingitis/ (42) 16. salpingiti$.tw. (57) 17. exp Parametritis/ (9) 18. parametriti$.tw. (3) 19. (celluliti$ adj5 pelvic).tw. (26) 20. exp Fallopian Tube Diseases/ (281) 21. (fallopian adj5 tube adj5 disease$).tw. (14) 22. (tubal adj5 obstruction$).tw. (25) 23. (uterine adj5 tube adj5 disease$).tw. (0) 24. (tuboovarian adj5 abscess).tw. (6) 25. or/1‐24 (1823) 26. exp Anti‐Bacterial Agents/ (26002) 27. (anti adj5 bacterial$).tw. (154) 28. antibacterial$.tw. (2057) 29. antibiotic$.tw. (19397) 30. bacteriocid$.tw. (19) 31. bactericide$.tw. (8) 32. exp Anti‐Infective Agents/ (61195) 33. (anti adj5 infective$).tw. (217) 34. antiinfective$.tw. (28) 35. microbicid$.tw. (355) 36. antimicrobial$.tw. (5210) 37. (anti adj5 microbial$).tw. (146) 38. exp Aminoglycosides/ (8026) 39. aminoglycosides.tw. (265) 40. exp Amoxicillin‐Potassium Clavulanate Combination/ (564) 41. amoxicillin.tw. (3418) 42. exp Azithromycin/ (824) 43. azithromycin.tw. (1804) 44. exp Cefotaxime/ (1741) 45. cefotaxime.tw. (651) 46. exp Cefotetan/ (107) 47. cefotetan.tw. (157) 48. exp Cefoxitin/ (293) 49. cefoxitin.tw. (421) 50. exp Ceftizoxime/ (170) 51. ceftizoxime.tw. (126) 52. exp Ceftriaxone/ (668) 53. ceftriaxone.tw. (1157) 54. exp Ciprofloxacin/ (1105) 55. ciprofloxacin.tw. (1951) 56. exp Clindamycin/ (822) 57. clindamycin.tw. (1307) 58. exp Doxycycline/ (956) 59. doxycycline.tw. (1461) 60. exp Gentamicins/ (1144) 61. gentamicin.tw. (1482) 62. exp Metronidazole/ (2093) 63. metronidazole.tw. (3357) 64. exp Moxifloxacin/ (0) 65. moxifloxacin.tw. (1022) 66. exp Ofloxacin/ (954) 67. ofloxacin.tw. (878) 68. levofloxacin.tw. (1065) 69. sultamicillin.tw. (46) 70. (ampicillin adj5 sulbactam).tw. (253) 71. or/26‐70 (83861) 72. 25 and 71 (762) 73. limit 72 to yr="2016 ‐Current" (69) |
Appendix 3. Electronic search strategies – 2020 update
| Type of search | Update |
| Database | MEDLINE (all) |
| Platform | Ovid |
| Search date | 11 November 2020 |
| Range of search date | 2019–2020 |
| Language restrictions | None |
| Other limits | None |
| Search strategy (results) |
|
| Number of references identified | 128 |
| Type of search | Update |
| Database | Embase |
| Platform | Embase.com |
| Search date | 9 January 2020 |
| Range of search date | 2019–2020 |
| Language restrictions | None |
| Other limits | None |
| Search strategy (results) |
|
| Number of references identified | 128 |
| Type of search | Update |
| Database | CENTRAL |
| Platform | Ovid |
| Search date | 11 January 2020 |
| Range of search date | 2019–2020 |
| Language restrictions | None |
| Other limits | None |
| Search strategy (results) |
|
| Number of references identified | 26 |
Data and analyses
Comparison 1. Regimens containing macrolides (azithromycin) versus tetracycline (doxycycline).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Effectiveness of cure in mild‐moderate PID | 2 | 243 | Risk Ratio (M‐H, Random, 95% CI) | 1.18 [0.89, 1.55] |
| 1.2 Sensitivity analysis by risk of bias: effectiveness of cure in mild‐moderate PID | 1 | 133 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.35 [1.10, 1.67] |
| 1.3 Effectiveness of cure in severe PID | 1 | 309 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.96, 1.05] |
| 1.4 Any antibiotic‐related adverse effect leading to discontinuation use of macrolide versus tetracycline | 3 | 552 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.38, 1.34] |
Comparison 2. Regimens containing quinolones versus cephalosporins.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Effectiveness of cure in mild‐moderate PID | 4 | 772 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.98, 1.14] |
| 2.2 Effectiveness of cure in severe PID | 2 | 313 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.91, 1.23] |
| 2.3 Any antibiotic‐related adverse effect leading to discontinuation | 6 | 1085 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.24 [0.52, 9.72] |
Comparison 3. Regimens containing nitroimidazoles versus no nitroimidazoles.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Effectiveness of cure in mild‐moderate PID | 6 | 2660 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.95, 1.09] |
| 3.2 Sensitivity analysis by risk of bias: effectiveness of cure in mild‐moderate PID | 3 | 1434 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [1.00, 1.12] |
| 3.3 Effectiveness of cure in severe PID | 11 | 1383 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.92, 1.01] |
| 3.4 Any antibiotic‐related adverse effect leading to discontinuation | 17 | 4021 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.69, 1.61] |
3.4. Analysis.

Comparison 3: Regimens containing nitroimidazoles versus no nitroimidazoles, Outcome 4: Any antibiotic‐related adverse effect leading to discontinuation
Comparison 4. Regimens containing clindamycin plus aminoglycoside versus quinolone.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Effectiveness of cure in mild‐moderate PID | 1 | 25 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.69, 1.13] |
| 4.2 Effectiveness of cure in severe PID | 2 | 151 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.87, 1.19] |
| 4.3 Any antibiotic‐related adverse effect leading to discontinuation | 3 | 163 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.21 [0.02, 1.72] |
Comparison 5. Regimens containing clindamycin plus aminoglycoside versus cephalosporin.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Effectiveness of cure in mild‐moderate PID | 2 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.95, 1.09] |
| 5.2 Effectiveness of cure in severe PID | 10 | 959 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.95, 1.06] |
| 5.3 Any antibiotic‐related adverse effect leading to discontinuation | 10 | 1172 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.18, 3.42] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Apuzzio 1989.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: women admitted to University Hospital of the University of Medicine and Dentistry of New Jersey from February 1987 to October 1988 with diagnosis of either postpartum endometritis or acute salpingitis. Diagnosis of uncomplicated PID was based on the clinical criteria described by Hager and colleagues (Hager 1989). Exclusion criteria: history of allergy to study drugs or received any antibiotic in 2‐week period prior to study (exclusive of prophylactic antibiotics for caesarean delivery). Number of women randomized: 25 for PID. Number of women analyzed: group A: 10; group B: 15. Number of withdrawals/exclusions/loss to follow‐up and reasons: 0. Number of centres: 1. Age (years): group A: 23.2; group B: 23.2. Country: US. |
|
| Interventions |
Group A: ciprofloxacin 300 mg IV every 12 h; treatment continued for 3–5 days until the woman was asymptomatic for 24 h. On discharge from hospital, women received PO antibiotics to complete 10–14 days of ciprofloxacin 750 mg PO twice daily. Group B: clindamycin 900 mg IV every 8 h + gentamicin 1.5 mg/kg IV every 8 h. On discharge from hospital, women received PO antibiotics to complete 10–14 days of clindamycin 450 mg PO every 6 h. |
|
| Outcomes | Primary outcome: treatment success, defined as women asymptomatic for 24 h. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Women randomly assigned to receive clindamycin + gentamicin or ciprofloxacin IV. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All women randomized were analyzed. |
| Selective reporting (reporting bias) | Unclear risk | No trial protocol found. |
| Other bias | Unclear risk | 25 women with uncomplicated PID randomized. 10 women received ciprofloxacin and 15 women received clindamycin + gentamicin. 1 woman prescribed clindamycin + gentamicin was not available because triple therapy was initially started. This woman was included in the analysis as treatment success. The authors did not clarify that. |
Arredondo 1997.
| Study characteristics | ||
| Methods | Randomized, double‐blind, comparative study. | |
| Participants |
Inclusion criteria: women aged 18–55 years with clinical diagnosis of mild or moderate PID, as confirmed by laparoscopy graded according to the methods of Hager and colleagues (Hager 1983) and Soper (Soper 1991). Exclusion criteria: observable pelvic mass; laparoscopic evidence of severe PID; pregnant or breastfeeding; allergic to clindamycin, ciprofloxacin, ceftriaxone, or doxycycline; required other antibiotic therapy for non‐protocol reasons; had pelvic or abdominal surgery in 30 days prior to admission (except emergency exploratory laparoscopy resulting in a primary diagnosis of PID that did not require pelvic clean‐up); concomitant disease that could have affected the evaluation of response to protocol therapy (such as inflammatory bowel disease or significant renal or hepatic disease); history of colitis; known to have frequent sexual contacts with multiple partners; seropositive for syphilis; severe medical condition(s) (e.g. neoplasms or haematological malignancy); had taken ≥ 2 antibiotics within 72 h before evaluation for enrolment in study; received any investigational drug 30 days before evaluation for enrolment; or had been previously enrolled in study. Number of women randomized: 69 per group. Number of women analyzed: 69 per group. Number of withdrawals/exclusions/loss to follow‐up and reasons: 2 in clindamycin + ciprofloxacin group; 1 chose to discontinue because she was asymptomatic and 1 withdrew because of adverse effect. In ceftriaxone + doxycycline group, 1 withdrew because of adverse effect, 1 lost to follow‐up and 1 withdrawn as receiving additional antibiotic treatment for syphilis after initiation of study medication. Number of centres: 6; Chile (1), Peru (2), Colombia (2), and Mexico (1). Age (mean) (years): group A: 28.9; group B: 30.7. Country: Mexico. |
|
| Interventions |
Group A: clindamycin 300 mg (2 capsules 3 times daily) + ciprofloxacin (250 mg, 1 tablet twice daily) for 14 days and placebo IM (for an equivalent of 1 dose of ceftriaxone). Group B: ceftriaxone 250 mg IM (single dose) + doxycycline 100 mg (1 capsule twice daily) and placebo (2 capsules 3 times daily for equivalent doses of clindamycin) for 14 days. |
|
| Outcomes | Clinical cure defined by the absence of, or minimal, pelvic tenderness, body temperature < 37.5 °C, and WBC count 10,000/mm3, if a minimum of 4 days of treatment had been completed. Clinical improvement defined as resolution of 2 of these 3 symptoms. Failure when 1 of the following circumstances was noted after ≥ 48 h of protocol therapy: signs and symptoms remained unchanged or worsened (during first 72 h of therapy). Microbiological cure defined as eradication of N gonorrhoeae or C trachomatis (or both) from clinically cured women. Failure defined as persistence of 1 or both of these 2 organisms or, in case of clinical improvement or failure, the presence of endocervical pathogens. Superinfection defined as the isolation of ≥ 1 new pathogens. Adverse effects leading to discontinuation of treatment. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | All eligible women randomized to 1 of the treatment groups. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Placebo medication was added as necessary to complete the double‐blind design. All PO medication was encapsulated to ensure blinding. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Placebo medication was added as necessary to complete the double‐blind design. All PO medication was encapsulated to ensure blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated. |
| Selective reporting (reporting bias) | Unclear risk | No trial protocol found. |
| Other bias | Unclear risk | Not stated. |
Aşicioğlu 2013.
| Study characteristics | ||
| Methods | Randomized, parallel‐group study. | |
| Participants |
Inclusion criteria: women aged 14–45 years with acute uncomplicated PID based on presence of all the following symptoms and signs: pelvic discomfort, direct lower abdominal tenderness, adnexal and cervical motion tenderness on bimanual vaginal examination, and pelvic pain for < 30 days, as well as ≥ 1 of following signs: pyrexia (rectal, tympanic, or oral temperature > 38.8 °C or axillary temperature > 37.5 °C), elevated CRP > 6 mg/L, WBC count > 10,500/mm3, and normal ultrasonographic scan. Exclusion criteria: UTI; complicated PID (such as tubo‐ovarian abscess); endometriosis; pelvic pain > 30 days; history of antibiotic therapy within last week; previous failure to adhere to antibiotic treatment; other causes of abdominopelvic pain such as appendicitis, diverticulitis, or ovarian cysts; oral intolerance, defined as 1 episode of vomiting after the first PO medication administration; and delivery, abortion, or surgery within the last month. Number of women randomized: 1156. Number of women analyzed: group A: 578; group B: 578. Number of withdrawals/exclusions/loss to follow‐up and reasons: group A: 18 women lost (oral intolerance n = 2; non‐compliance n = 5; worsening of pain n = 3; tubo‐ovarian abscess n = 2; UTI = 2; other n = 4); group B: 35 women lost (oral intolerance n = 4; non‐compliance n = 18; worsening of pain n = 2; tubo‐ovarian abscess n = 2; UTI n = 4; other n = 5). Number of centres: 4. Age (mean) (years): group A: 30.3 (SD 3.7); group B: 29.3 (SD 3.5). Country: Turkey. |
|
| Interventions |
Group A: moxifloxacin 400 mg once daily for 14 days. Group B: ofloxacin 400 mg twice daily + metronidazole 500 mg PO twice daily. |
|
| Outcomes | Clinical cure, microbiological cure, adverse effects. Primary outcome: clinical cure, defined as a ≥ 60% reduction in the total pain score at day 21 compared with baseline and the absence of pelvic discomfort and tenderness, temperature < 37.8 °C, and WBC count < 10,000/mm3 on day 21. |
|
| Notes |
Ethical approval: yes. Informed consent: yes, women gave written informed consent. Source of funding: not stated, and no conflicts of interest reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used random‐numbers table. |
| Allocation concealment (selection bias) | Low risk | Assigned treatments written on cards and sealed in secure opaque envelopes numbered in sequence. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Investigators not blinded to the procedure allocation. Moxifloxacin group received just 1 tablet, whereas ofloxacin + metronidazole group received 4 tablets daily. No placebo was added to blind groups. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | 7 days after drug treatment at secondary visits (day 21), all women underwent evaluation by same physician who allocated women. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | From 1156 women, 53 lost to follow‐up. |
| Selective reporting (reporting bias) | Low risk | Trial registered in ClinicalTrial.gov (NCT01799356). |
| Other bias | Unclear risk | Risk of potential bias unclear. |
Balbi 1996.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: women with PID diagnosis based on all following criteria: pelvic pain, either spontaneous or at palpation; cervical motion tenderness; and adnexal pain. Exclusion criteria: aged < 16 years, current pregnancy, allergy to 1 of medications used in study or to penicillin, serum creatinine > 1.5 mg/dL, previous or current hepatic disease, use of antibiotics in last 7 days, in situ IUD. Number of women randomized: 78. Number of women analyzed: 76; group A: 40; group B: 36. Number of withdrawals/exclusions/loss to follow‐up and reasons: 2, intolerance to penicillin. Number of centres: 1. Age (mean) (years): group A: 25.3 (SD 7.7); group B: 29.4 (SD 7.8). Country: Italy. |
|
| Interventions |
Group A: gentamicin, 2 mg/kg IV (loading dose), followed by 1.5 mg/kg IV every 8 h + clindamycin 900 mg IV every 8 h for 4 days, followed by clindamycin 450 mg PO every 6 h for total of 14 days of treatment. Group B: ceftazidime 1 g IV every 8 h + doxycycline 100 mg PO every 12 h for 4 days, followed by doxycycline 100 mg PO every 12 h for total of 14 days of treatment. |
|
| Outcomes |
Primary outcome: clinical recovery, defined as: body temperature < 37 °C for 48 h, disappearance of pelvic pain, no increase of eventual adnexal mass after 7 days of end of treatment. Secondary outcome: follow‐up performed 30 days after treatment finished; endocervical culture for N gonorrhoeae and C trachomatis and endometrial culture for C Trachomatis performed in all positive cases at admission. |
|
| Notes |
Ethical approval: not stated. Informed consent: not stated. Funding source: no funding stated or declaration of interest. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Women randomly allocated into 2 treatment groups. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 2/78 women excluded from analysis. |
| Selective reporting (reporting bias) | Unclear risk | Not stated. |
| Other bias | Unclear risk | Not stated. |
Bevan 2003.
| Study characteristics | ||
| Methods | Randomized, open‐label, comparative, multicentre, multinational trial. | |
| Participants |
Inclusion criteria: aged ≥ 18 years, fulfilling Hager's criteria for a clinical diagnosis of acute PID (Hager 1983), and requiring hospitalization for treatment. Diagnosis of acute PID confirmed by laparoscopy unless impossible due to need for immediate treatment. Exclusion criteria: palpable tubo‐ovarian abscess (i.e. ultrasound diameter ≥ 5 cm); use of additional antimicrobial therapy for a concurrent infection; use of antibiotic therapy during preceding 2 weeks; terminal illness; immunosuppression; impaired gastrointestinal function or absorption (or both); hepatic or renal impairment; known allergy to macrolides, tetracycline, metronidazole, penicillin, cephalosporins, or clavulanic acid; use of oral hypoglycaemic drugs, ergot, dicoumarin anticoagulants, carbamazepine, ciclosporin, digoxin, or theophylline; and known drug addiction, alcoholism, or taking of recreational drugs. Number of women randomized: 310. Number of women analyzed: 309; group A: 106; group B: 107; group C: 96. Number of withdrawals/exclusions/loss to follow‐up and reasons: 10 women excluded from analysis at end of treatment because of following protocol violations: did not receive study medication (n = 1); inappropriate primary diagnosis (n = 2); concomitant antibacterial treatment (n = 1); no signs/symptoms recorded at day evaluation (n = 1); and missing data or mistimed evaluation (n = 5). Number of centres: multiple, but authors did not specify how many. Age (mean) (years): group A: 28.4 (range 18–54); group B: 27.6 (range 18–46); group C: 27.6 (range 17–54). Country: UK and others that were not stated. |
|
| Interventions |
Group A: azithromycin 500 mg IV single dose, days 2–7: 250 mg PO once daily or days 1–2: azithromycin 500 mg IV once daily; days 3–7: 250 mg PO once daily. Group B: as group A + day 1: metronidazole 500 mg IV 3 times daily or 400 mg PO 3 times daily, days 2–12: metronidazole 400 mg PO 3 times daily or days 1–2: azithromycin 500 mg IV once daily; days 3–7: 250 mg PO once daily plus day 1–2: metronidazole 500 mg IV 3 times daily, or 500 mg PO 3 times daily. Days 3–12: metronidazole 500 mg PO 3 times daily or days 1–21: metronidazole 500 mg PO 3 times daily. Group C: day 1: metronidazole 500 mg IV 3 times daily, or metronidazole 400 mg PO 3 times daily; day 2–12: metronidazole 400 mg PO 3 times daily + days 1–14: cefoxitin 2 g IV or IM 4 times daily + day 1: probenecid 1 g PO single dose or day 1–21: doxycycline 100 mg PO twice daily + day 1–5: amoxicillin/clavulanate 1 g IV + times daily; day 6–21 amoxicillin/clavulanate 500 mg PO 3 times daily. |
|
| Outcomes | Clinical response to treatment: cure, resolution of all baseline signs and symptoms; improvement, lessening of baseline signs and symptoms or absence of ≥ 1, but not all, of baseline findings; or failure, no improvement or deterioration of baseline condition. Successful clinical outcome defined as cure or improvement. Assessment on day 15 (9–26 inclusive) and at follow‐up (day 35–44). Microbiological outcome: eradication, absence of the baseline isolate(s); persistence, presence of baseline isolate(s); or superinfection, presence of a micro‐organism different from that found at baseline. |
|
| Notes |
Ethical approval: yes "European Ethical Review Committee and by local hospital ethical committees." Informed consent: yes, prior to entry into either study, written informed or witnessed oral consent was obtained from each woman. Source of funding: not stated, but 1 author was from Pfizer Inc. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Women randomized to 1 of 3 treatment groups. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Open‐label. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition rate (< 20%). |
| Selective reporting (reporting bias) | Unclear risk | No trial protocol found. |
| Other bias | Unclear risk | Trial had support of pharmaceutical industry. 1 case missing from the analysis and not specified in report. |
Buisson 1989.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: women with PID associated or not associated with endometritis confirmed by laparoscopy according to the clinical criteria described by Hager and colleagues (Hager 1989). Exclusion criteria: known allergy to betalactamics, pregnant, renal and liver insufficiency. Number of women randomized: 82. Number of women analyzed: group A: 42; group B: 40. Number of withdrawals/exclusions/loss to follow‐up and reasons: 1 abandoned the amoxicillin‐clavulanic acid after knowing that the bacteria (Klebsiella pneumoniae) was resistant to the antibiotic. 1 stopped amoxicillin‐clavulanic acid after 6 days of treatment due to no clinical improvement and she was switched to group B; In group B, 1 woman stopped the treatment due to adverse effect (Quincke oedema). Number of centres: 8. Age (mean) (years): group A: 27.7 (range 18–46); group B: 28.7 (range 15–49). Country: France. |
|
| Interventions |
Group A: amoxicillin‐clavulanic acid 1 g IV every 8 h for ≥ 48 h, then 1.5–2 g PO twice daily. Mean length of treatment 19 days, never less than 14 days. Group B: amoxicillin 3–4 g IV per 24 h, mean 4 days, then 1.5–2 g PO daily. Mean length of treatment 17 days + aminoside (chosen by researcher's preference) 3–5 mg/kg IM per 24 h 2 or 3 times daily depending of the aminoside, mean length of treatment 7 days + metronidazole 1 g or 1.5 g IV or suppository daily. For each case, a secondary prescription for a tetracycline 200 mg per 24 h was given, either immediately if results of laparoscopy or other investigations justified it, or later on positive chlamydia serology. Length of this treatment 3–4 weeks as decided by the researcher. |
|
| Outcomes |
Primary outcomes: clinical cure; defined as absence of fever, pain, and previously observed adnexal masses at 5–8 weeks' follow‐up; adverse events leading to discontinuation of treatment. Secondary outcome: none reported. |
|
| Notes |
Ethical approval: not stated. Informed consent: not stated. Source of funding: not stated, and no conflicts of interest reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Choice of treatment fixed by randomization. |
| Allocation concealment (selection bias) | Unclear risk | Choice of treatment fixed by randomization. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 1/82 women lost to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | No protocol found. |
| Other bias | Unclear risk | Not stated. |
Burchell 1987.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: 40 women with PID established by blood sampling, laparoscopic, follow‐up clinical evaluations, and taking of microbiological specimens for culture done by same physician to ensure uniformity. Women had laparoscopic examination and microbiological cultures to confirm the clinical diagnosis of acute PID. Exclusion criteria: general peritonitis or with abdominal distension and absent bowel sounds; large pelvic masses extending into the abdomen; toxic; in poor general condition; pregnant (e.g. postabortal); and antibiotics in the 14 days before presentation. Number of women randomized: 30; 10 per group. Number of women analyzed: 30; 10 per group. Number of withdrawals/exclusions/loss to follow‐up and reasons: 10 women excluded because laparoscopic examination and microbiological cultures did not confirm the clinical diagnosis of acute PID. Number of centres: not stated. Age: not stated. Country: South Africa. |
|
| Interventions |
Group A: doxycycline infusion 200 mg in 200 mL 5% dextrose over 2 h + doxycycline 100 mg after 24 h. The course was completed with oxytetracycline 250 mg every 6 h for 14 days. Group B: ampicillin + metronidazole 1 g IV every 6 h and then 500 mg PO every 6 h for 14 days. Group C: tetracycline + metronidazole with 3 × 1 g suppositories every 8 h and then 400 mg PO every 8 h for 14 days. |
|
| Outcomes | Primary outcome: clinical cure. | |
| Notes |
Ethical approval: not stated. Informed consent: yes, informed consent obtained from all women. Source of funding: not stated, and no conflicts of interest reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol found. |
| Other bias | Unclear risk | No study group characteristics reported. |
Ciraru‐Vigneron 1986.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: severe PID, defined as signs of fever, pain. Local signs (adnexal mass), discovery of pathogen, leukocytosis, elevated ESR, pelvic ultrasound, and possibly laparoscopy. Exclusion criteria: not stated. Number of women randomized: 44; 22 per group. Number of women analyzed: 44; 22 per group. Number of withdrawals/exclusions/loss to follow‐up and reasons: only 20% of women seen. Number of centres: 1. Age: not stated. Country: France. |
|
| Interventions |
Group A: amoxicillin‐clavulanic acid while in hospital, 4 g per 24 h, first by IV, then PO once symptoms improved. At discharge, amoxicillin‐clavulanic acid PO if chlamydia serology was negative; if positive for chlamydia, doxycycline prescribed for 3 weeks (dose not stated). Group B: ampicillin 6 g per 24 h IV + gentamicin 160 mg per 24 h IM + metronidazole 1.5 g per 24 h IV; when switched to oral administration, ampicillin replaced by amoxicillin 3 g per 24 h + metronidazole 1.5 g per 24 h PO and gentamicin 160 mg per 24 h IM for minimum of 7 days. At discharge, amoxicillin‐clavulanic acid PO if chlamydia serology negative; if positive for chlamydia, doxycycline for 3 weeks (dose not stated). |
|
| Outcomes |
Primary outcomes: clinical cure, defined by no fever, reduction of pain, and normal WBC count at discharge and in 30 days; adverse events leading to discontinuation of treatment. Secondary outcomes: microbial cure of N gonorrhoeae and C trachomatis; length of hospital stay. |
|
| Notes |
Ethical approval: not stated. Informed consent: not stated. Source of funding: not stated, and no conflicts of interest reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomized study. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated. |
| Selective reporting (reporting bias) | Unclear risk | Not stated. |
| Other bias | Unclear risk | Assumed that assessment of 'cure', 'improvement,' and 'failure' performed during hospitalization or at discharge. Follow‐up at 30 days; only 20% in each group seen. In those women, no secondary adverse events seen. |
Ciraru‐Vigneron 1989.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: not stated. Exclusion criteria: required systemic or local antibiotic therapy other than those specified in the protocol; pregnant or likely to become pregnant; or allergic to penicillins or cephalosporins. Number of women randomized: 165; group A: 78; group B: 87. Number of women analyzed: 152; group A: 70; group B: 82. Number of withdrawals/exclusions/loss to follow‐up and reasons: group A: 8; group B: 5 due to poor compliance. Number of centres: 8. Age (mean) (years): group A: 26.9; group B: 25.1. Country: France. |
|
| Interventions |
Group A: amoxicillin 1 g IV + clavulanic acid 200 mg (Augmentin 1.2 g), 3 or 4 times daily until clinical and laboratory findings improved, after which 4–6 tablets containing amoxicillin 500 mg + clavulanic acid 125 mg (Augmentin 625 mg) per tablet. Group B: amoxicillin or ampicillin 3–4 g daily, with an aminoglycoside (gentamicin 160 mg, dibekacin 150 mg, or tobramycin 150 mg) + metronidazole 1.5 g daily parenterally. Subsequent conversion was to oral combination of amoxicillin or ampicillin 2–3 g + metronidazole 1–1.5 g daily. |
|
| Outcomes | Primary outcomes: excellent response defined as resolution of physical findings with continued improvements in laboratory values; favourable response equate with a favourable course, allowing the persistence of ≥ 1 clinical signs or abnormal laboratory values (or both); failure defined as absence of therapeutic efficacy or of a favourable course after ≥ 6 days of therapy that a change in management, either surgery or an alternative antibiotic treatment was warranted. | |
| Notes |
Ethical approval: not stated. Informed consent: not stated. Source of funding: not stated, and no conflicts of interest reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 152/165 women included in analysis. |
| Selective reporting (reporting bias) | Unclear risk | No trial protocol found. |
| Other bias | Unclear risk | Not stated. |
Crombleholme 1986.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: severe acute PID with peritonitis, tubo‐ovarian abscess, endometritis, and pelvic cellulitis. Exclusion criteria: not stated. Number of women randomized: 39; group A: 20; group B: 19. Number of women analyzed: 39; group A: 20; group B: 19. Number of withdrawals/exclusions/loss to follow‐up and reasons: not stated. Number of centres: not stated. Age: not stated. Country: not stated. |
|
| Interventions |
Group A: sulbactam 1 g + ampicillin 2 g IV every 6 h. Group B: metronidazole 15 mg/kg loading followed by 7.5 mg/kg IV every 6 h and gentamicin 1.5 mg/kg IV every 8 h. Antibiotics in both groups continued for minimum of 5 days. |
|
| Outcomes | No relevant outcomes reported for our analysis because the outcomes were not separately reported for the different diagnoses within the study groups. Authors stated clinical cure occurred in 19/20 women in group A and 16/19 women in group B. | |
| Notes |
Ethical approval: not stated. Informed consent: not stated. Source of funding: not stated, and no conflicts of interest reported. 2 cases of posthysterectomy pelvic cellulitis were included in analysis. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Non‐blinded study. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Non‐blinded study. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All women randomized were analyzed. |
| Selective reporting (reporting bias) | Unclear risk | No trial protocol found. |
| Other bias | Unclear risk | Not stated. |
Crombleholme 1987.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: hospitalized women aged ≥ 18 years with documented or clinical diagnosis of mixed aerobic‐anaerobic PID. Exclusion criteria: pregnant or lactating; allergy to penicillins, cephalosporins, aminoglycosides, or metronidazole; impaired renal function (serum creatinine > 1.8 mg/100 mL); family history of glycogen storage disease or recurrent hypoglycaemia; history of unstable cardiovascular, hepatic, renal, or neurological disease. Number of women randomized: 44; 22 per group. Number of women analyzed: 42; 21 per group. Number of withdrawals/exclusions/loss to follow‐up and reasons: 1 women in group A with a clinical diagnosis of PID and a right adnexal mass excluded. Laparoscopy revealed a right ovarian cyst, no visual evidence of infection, and essentially no growth from cervical and endometrial cultures. 1 woman in group B with clinical diagnosis of PID excluded; she left the hospital against medical advice on the third hospital day. Number of centres: 1. Age (mean) (years): group A: 27.7 (SD 6.9); group B: 29.0 (SD 12.1). Country: US. |
|
| Interventions |
Group A: ampicillin 2 g + sulbactam 1 g IV every 6 h. Group B: metronidazole 15 mg/kg IV every 6 h + gentamicin 1.5 mg/kg IV every 8 h. Therapy continued until women became afebrile and were without clinical signs of infection for 48 h or until clinical judgement dictated cessation of therapy. Range of treatment 3–11 days. |
|
| Outcomes | Primary outcome: clinical cure defined as absence of fever, without clinical signs of infections for 48 h or until clinical judgement. | |
| Notes |
Ethical approval: not stated. Informed consent: not stated. Source of funding: not stated, and no conflicts of interest reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 1 woman missing in each group. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol found. |
| Other bias | Unclear risk | Not stated. |
Crombleholme 1989.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: women aged ≥ 18 years admitted to San Francisco General Hospital with diagnosis of acute PID according to established criteria: history of lower abdominal pain and direct lower abdominal tenderness with or without rebound; tenderness with motion of cervix and uterus; and adnexal tenderness. ≥ 1 of: endocervix positive for gram‐negative intracellular diplococci or direct fluorescent antibody test revealing C trachomatis, elevated ESR, temperature > 38 °C, leukocytosis (WBC count > 10,500/mm3), purulent material (WBCs and bacteria) from peritoneal cavity by culdocentesis, or a pelvic abscess or inflammatory complex on bimanual examination or by sonography. Exclusion criteria: history of allergy to any study drug; mild infections not requiring parenteral antimicrobial therapy; pregnancy or lactation; severe underlying terminal illness; need for concomitant antimicrobial with a spectrum of activity similar to that of study drug; or severe impairment of renal function (creatinine level > 2 mg/dL or creatinine clearance < 50 mL/minute). Number of women randomized: 80; 40 per group. Number of women analyzed: 80; 40 per group. Number of withdrawals/exclusions/loss to follow‐up and reasons: none reported. Number of centres: 1. Age (mean) (years): group A: 25.7 (SD 4.8); group B: 25.3 (SD 6.2). Country: US. |
|
| Interventions |
Group A: ciprofloxacin 300 mg IV every 12 h for 2–5 days, with ≥ 2 days of parenteral therapy and 48 h without fever before switching to ciprofloxacin 750 mg PO every 12 h, to complete a 14‐day course. Group B: clindamycin 600 mg IV every 6 h + 1 mg/kg IV every 8 h after ≥ 4 days of parenteral gentamicin and 48 h without fever before switching to clindamycin 300 mg PO every 6 h, to complete a 14‐day course. |
|
| Outcomes |
Primary outcome: clinical cure at 3 days: improvement in clinical signs and symptoms. Secondary outcomes: microbial cure of C trachomatis and N gonorrhoeae. |
|
| Notes |
Ethical approval: yes, women gave written informed consent as approved by the Committee of Human Research of the University of California, San Francisco. Informed consent: yes, women gave written informed consent as approved by the Committee of Human Research of the University of California, San Francisco. Source of funding: not stated, and no conflicts of interest reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Non‐blinded study. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Non‐blinded study. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All women randomized were analyzed. |
| Selective reporting (reporting bias) | Unclear risk | No trial protocol found. |
| Other bias | Unclear risk | Not stated. |
Dean 2016.
| Study characteristics | ||
| Methods | Multicentre (running in hospitals of Brighton, London, Birmingham, Eastbourne/Hastings and Sheffield, UK), open‐label, randomized controlled trial, non‐inferiority study. | |
| Participants |
Inclusion criteria: women who attend the genitourinary clinic with mild‐moderate symptoms of PID (pain for < 30 days and adnexal tenderness). Exclusion criteria: aged < 16 years; severe PID requiring hospital admission; positive pregnancy test or breastfeeding, UTI (leukocytes AND nitrites); intracellular gram‐negative diplococci on microscopy or contact with genitourinary clinic < 3 months; antibiotics within the last 7 days; known allergy to antibiotic component; ultrasound scan showing other pathology; history of epilepsy/severe depression. Methods of recruitment of participants: randomized population: all women regardless of whether the treatment was taken or they returned for a follow‐up visit; per‐protocol population: women who returned for a day 14–21 visit in whom the primary outcome was assessed. Number of women randomized: 313; group A: 153; group B: 160. |
|
| Interventions |
Group A: ofloxacin 400 mg twice daily + metronidazole 400 mg twice daily every 12 h for 14 days. Group B: 5 days of azithromycin 1 g day 1, then 500 mg once daily + metronidazole 400 mg twice daily + 1 dose of ceftriaxone IM. |
|
| Outcomes | Clinical efficacy at day 14–21 days (pain by McCormack Pain Scale and tenderness by physical examination, cure > 70% of pain reduction on day 14–21 compared to day 1); tolerability (comparing incidence of adverse effects in each group: baseline to day 14–21, when women returned for a follow‐up visit); adherence (assessing therapy adherence of each woman: baseline to day 14–21, when women returned for a follow‐up visit); prevalence of causative organisms (analysis of causative organisms: baseline to day 14–21, when women returned for a follow‐up visit). | |
| Notes |
Ethical approval: not stated. Informed consent: yes, according to ISRCTN website. Source of funding: National Institute for Health Research (UK). No references to theoretical basis. Risk of bias' judgements: according to Cochrane Handbook for Systematic Reviews of Interventions. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Women randomly allocated to either 14 days of antibiotics or 5‐day course of antibiotics. |
| Allocation concealment (selection bias) | Unclear risk | Not clearly stated. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label: the women and research nurse know which antibiotics they are taking, but not the doctor. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Open‐label: the women and research nurse know which antibiotics they are taking, but not the doctor. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Group A: 46 cases lost to follow‐up; 30%; group B: 40 cases lost to follow‐up; 25%. |
| Selective reporting (reporting bias) | Low risk | The same outcome report from randomized controlled trial published in ISRCTN. |
| Other bias | Unclear risk | Final publication and details of the trial not available. |
Fischbach 1994.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: women aged > 18 years, acute PID (endometriosis, salpingitis, pyosalpinx, adnexitis, pelvic peritonitis, tubo‐ovarian abscess). Diagnosis by manual examination, echography, laparoscopy, and clinical parameters such as fever, leukocytosis, ESR, and positive bacterial culturing (anaerobe, aerobe, chlamydia). Exclusion criteria: aged < 18 years; pregnancy or lactation; antibiotic therapy up to 3 days before inclusion; known allergies against gyrase inhibitors, cephalosporin, metronidazole, and tetracycline; serious impaired renal and liver function; and other serious comorbidities. Number of women randomized: 60. Number of women analyzed: 57; group A: 26; group B: 31. Number of withdrawals/exclusions/loss to follow‐up and reasons: group A: 3 women excluded from analysis due to adverse effects. Number of centres: not stated. Age in years ‐ mean (SD) and [median] : group A: 30 (± 10) [27]; group B: 26 (± 7) [22]. Country: Germany. |
|
| Interventions |
Group A: ciprofloxacin 2 × 0.2 g IV daily + metronidazole 3 × 0.5 g IV daily. Group B: cefoxitin 3 × 2 g IV daily + doxycycline 2 × 0.1 g IV daily. After 2–5 days of treatment, ciprofloxacin, metronidazole, and doxycycline given PO. Both groups treated for 7–14 days. |
|
| Outcomes | Primary outcome: clinical cure defined as subjective lack of symptoms; improvement upon gynaecological examination; normal leukocytes count; declining ESR; no fever; and elimination of bacteria. | |
| Notes |
Ethical approval: not mentioned. Informed consent: yes, women gave written informed consent. Source of funding: not stated, and no conflicts of interest reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 57/60 women were available for analysis. |
| Selective reporting (reporting bias) | Unclear risk | No trial protocol found. |
| Other bias | Unclear risk | Not stated. |
Giraud 1989.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: women with severe PID. Exclusion criteria: pregnant or likely to be pregnant, allergic to penicillin or to cephalosporins, receiving concomitant treatment with allopurinol, needing to receive a different antibiotic during hospitalization, infectious mononucleosis. Number of women randomized: 152. Number of women analyzed: group A: 70; group B: 82. Number of withdrawals/exclusions/loss to follow‐up and reasons: 0. Number of centres: unclear. Age (mean) (years): group A: 26.9; group B: 25.1. Country: France. |
|
| Interventions |
Group A: amoxicillin‐clavulanic acid; while in hospital, 3 g or 4 g per 24 h, by IV injection or perfusion, then 2 g or 3 g per 24 h PO. Group B: parenteral: ampicillin 3 g or 4 g IV per 24 h, OR amoxicillin 3 g IV per 24 h + gentamicin 160 mg IM per 24 h OR dibekacin 150 g IM per 24 h + metronidazole 1.5 g IV per 24 h. Oral administration: ampicillin 3 g per 24 h OR amoxicillin 2 g per 24 h + metronidazole 1.5 or 2 g per 24 h. Additional treatments were limited, but could have included: surgical or laparoscopic drainage of pus, local antibiotic for treatment of trichomonacides, non‐steroidal anti‐inflammatory drugs, corticoids. |
|
| Outcomes |
Primary outcomes: clinical cure at 10th day; clinical progress and improvement of biological parameters. Secondary outcome: length of hospital stay. |
|
| Notes |
Ethical approval: not stated. Informed consent: not stated. Source of funding: not stated. No conflicts of interest reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear how women were randomized. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | < 20% attrition. |
| Selective reporting (reporting bias) | Unclear risk | No trial protocol found. |
| Other bias | Unclear risk | Not stated. |
Heinonen 1989.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants | Women referred to Department of Obstetrics and Gynecology with suspected PID with different degrees of severity (none, mild, moderate, and severe); 53% with mild salpingitis. Inclusion criteria: history of lower abdominal pain < 3 weeks' duration, and presence of cervical motion tenderness, uterine and adnexal tenderness on bimanual examination. Exclusion criteria: use of antibiotics, had any gynaecological operation or instrumentation of the upper genital tract in the preceding month, had systemic disease or epilepsy, pregnant, suspected allergy to any of the drugs used, or puerperal infection. Number of women randomized: 40. Number of women analyzed: group A: 16; group B: 20. Number of withdrawal/exclusions/loss to follow‐up and reasons: 4 due to other diagnosis: toxoplasmosis, urinary infection, periappendicular abscess, no pathological findings. Number of centres: 1. Age (mean) (years): group A: 29 (SD 8) (range 18–43); group B: 29 (SD 1) (range 16–50). Country: Finland. |
|
| Interventions |
Group A: ciprofloxacin 200 mg IV every 12 h for 2 days followed by 750 mg PO every 12 h to complete 14‐day course. Group B: doxycycline 100 mg IV every 12 h + metronidazole 500 mg IV every 8 h for the first 2 days, followed by doxycycline 150 mg PO every 24 h + metronidazole 400 mg PO every 8 h to complete a 14‐day course. |
|
| Outcomes |
Primary outcomes: clinical response based on a scale from 0 (absent or normal) to 3+ (severe) assessed on days 3, 6, 14, and 21 after the antimicrobial treatment was started. Failure defined as the presence of ≥ 1 of following criteria: no improvement in the clinical severity score at day 3 after the microbial treatment was started; CRP > 20 mg/L or a decline < 50% in the initial CRP level at day 6; positive cervical culture of N gonorrhoeae or C trachomatis at days 14 or 21; or the need for additional antimicrobial agents or surgical intervention. Secondary outcomes: adverse reactions and effects. |
|
| Notes |
Ethical approval: not stated. Informed consent: signed consent obtained. Source of funding: not stated. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated how randomization was done. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All women randomized were analyzed. |
| Selective reporting (reporting bias) | Unclear risk | No trial protocol found. |
| Other bias | Unclear risk | Not stated if all women were assessed 21 days after the antimicrobial treatment was started. |
Hemsell 1994.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: clinical diagnosis of acute PID hospitalized at 1 of 6 sites for treatment. Acute PID diagnosed in women with lower abdominal and pelvic pain and lower abdominal and cervical motion and adnexal tenderness in addition to ≥ 1 of the following: oral temperature ≥ 38.0 °C; leukocyte count ≥ 10,500/mm3; elevated ESR; endocervical specimen positive for gram‐negative intracellular diplococci; endocervical or endometrial culture positive for N gonorrhoeae or C trachomatis; ultrasound findings consistent with an adnexal inflammatory mass; or purulence in or a positive culture of intraperitoneal material obtained at either culdocentesis or optional laparoscopy. Exclusion criteria: ruptured tubo‐ovarian or pelvic abscess; history of hypersensitivity to penicillin, cephalosporins, clindamycin, aminoglycosides, or tetracycline; among women with IUD in place, those who permitted the removal of the device within 48 h were included and those who did not were excluded; pregnancy or lactation; renal impairment (serum creatinine level about 2 mg/dL), neutropenia (< 1000 neutrophils/mm3), receipt of another investigational drug or another antibiotic up to 2 weeks before the time of anticipated enrolment; and known or suspected active bacterial infection other than acute PID that might subsequently require concomitant therapy. Number of women randomized: 344. Number of women analyzed: group A: 109; group B: 110; group C: 108. Number of withdrawal/exclusions/loss to follow‐up and reasons: 52 women (15%) were not evaluable, 21 enrolled incorrectly (i.e. despite a violation of inclusion or exclusion criteria, or both), aII given an incorrect first dose of study drug or were subsequently given incorrect doses, 10 left hospital against medical advice, 5 treated for < 48 h, 2 withdrew, 2 had adverse reactions resulting in the cessation of treatment, and 1 given penicillin for the treatment of syphilis. Of the 2 women with adverse reactions, 1 developed blisters on her lips after the third dose of cefotetan + doxycycline, and the other developed hives after the initial dose of cefoxitin. All 5 women who were not evaluable because they received < 48 h of therapy had ≥ 1 abscesses, and 3/5 women underwent surgery because of worsening symptoms. 2/5 women were in group A, 2 were in group B, and 1 was in group 3. 20 of the unevaluable women were in group A, 20 were in group B, and 12 were in group C. Number of centres: 6. Age (mean) (years): success group: 24.7 (SD 4.9); failure group: 26.2 (SD 5.7). Country: US. |
|
| Interventions |
Group A: cefoxitin 2 g IV every 6 h + doxycycline 100 mg every 12 h; followed by doxycycline 100 mg PO twice daily for a total of 10–14 days. Group B: clindamycin 900 mg IV + gentamicin 1.5 mg/kg every 8 h after an initial gentamicin loading dose calculated at 2 mg/kg followed by clindamycin 450 mg PO 4 times daily for a total of 10–14 days. Group C: cefotetan 2 g IV + doxycycline 100 mg every 12 h, followed by doxycycline 100 mg PO twice daily for a total of 10–14 days. |
|
| Outcomes | Primary outcome: clinical cure defined as reduction of the severity score by ≥ 70%, with a normal temperature and leukocyte count. | |
| Notes |
Ethical approval: consent forms were approved by the local institutional review board at each centre. Informed consent: women aged 16–18 years old had to have parental consent, and women aged ≥19 years had to give their own consent. Source of funding: ICI Pharmaceuticals Group (now ZENECA, Inc.), Wilmington, Delaware. No conflicts of interest reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described how randomization codes were generated. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label study. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Open‐label study. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 292/343 women were analyzed (15% were not evaluable). |
| Selective reporting (reporting bias) | Unclear risk | No trial protocol found. |
| Other bias | Unclear risk | Not stated. |
Heystek 2009.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: women aged ≥ 18 years and receiving either hospital or outpatient care for uncomplicated acute PID and using a reliable form of contraception. Exclusion criteria: positive serological test for syphilis or evidence of a pelvic abscess on sonographic or laparoscopic examination. Number of women randomized: 686. Number of women analyzed: 669; group A: 343; group B: 326. Number of withdrawals/exclusions/loss to follow‐up and reasons: 17; 2 never randomized and in 15 it was impossible to confirm if they received study medication. Number of centres: 43. Age (mean) (years): group A: 29.0 (SD 7.3); group B: 28.2 (SD 7.2). Country: 14 countries. |
|
| Interventions |
Group A: moxifloxacin 400 mg PO once daily for 14 days. Group B: doxycycline 100 mg PO twice daily + metronidazole 400 mg PO 3 times daily for 14 days + ciprofloxacin 500 mg PO once. |
|
| Outcomes |
Primary outcome (modified ITT): clinical cure at 2–14 days' post‐treatment: clinical success defined as cure (severity score reduced by ≥ 70% + normal temperature and leukocyte count) or improvement (severity score reduced < 70% but > 30% + normal temperature and leukocyte count). Therapy considered to have failed if symptoms and signs of infection persisted or worsened, as shown by persistent fever, leukocytosis, reduction in severity score ≤ 30%, or a combination of these. Clinical efficacy was 'unevaluable' when a woman could not be assessed. Secondary outcome (PP): microbiological clearance of chlamydia, microbiological clearance of gonorrhoea. |
|
| Notes |
Ethical approval: yes, study protocol prepared in accordance with the European Guidelines for Good Clinical Practice (1991) and National Rules and Regulations. Study conducted in accordance with the Declaration of Helsinki. Informed consent: not stated. Source of funding: Bayer Schering Pharma, Germany, provided financial and logistical support. No conflicts of interest reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind study. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Double‐blind study. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition rate (< 20%). |
| Selective reporting (reporting bias) | Unclear risk | No study protocol found. |
| Other bias | Unclear risk | Not stated. |
Hoyme 1993.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: women with laparoscopically verified salpingitis. Exclusion criteria: none stated. Number of women randomized: 33. Number of women analyzed: 33; group A: 15; group B: 18. Number of withdrawals/exclusions/loss to follow‐up and reasons: 0. Number of centres: 1. Age: not stated. Country: Germany. |
|
| Interventions |
Group 1: ofloxacin 2 × 200 mg + metronidazole 2 × 500 mg, first IV and then PO for 10 days in total. Group 2: gentamicin 3 × 80 mg + clindamycin 4 × 600 mg (initially 1200 mg IV) for 10 days in total. |
|
| Outcomes | Primary outcome: clinical cure, no raw data reported for outcomes. | |
| Notes |
Ethical approval: judged by the ethics committee. Informed consent: yes, women gave written informed consent. Source of funding: not stated, and no conflicts of interest reported. All women hospitalized for the whole treatment. Only percentages and no numbers reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All women randomized were analyzed. |
| Selective reporting (reporting bias) | Unclear risk | No trial protocol found. |
| Other bias | Unclear risk | Not stated. |
Judlin 2010b.
| Study characteristics | ||
| Methods | Prospective, randomized, double‐blind, double‐dummy, parallel‐group study. | |
| Participants | No significant differences between treatment groups in demographic characteristics. Inclusion criteria: diagnosis of uncomplicated PID based on presence of all following symptoms and signs: pelvic discomfort; direct lower abdominal tenderness; adnexal and cervical motion tenderness on bimanual vaginal examination; and ≥ 1 of the following signs: pyrexia (rectal, tympanic, or oral temperature > 38 °C or axillary temperature > 37.5 °C), CRP > 6 mg/L, WBC count > 10,500/mm3, laparoscopic evidence of PID, cervical infection including mucopurulent cervical discharge or positive stain for gram‐negative intracellular diplococci from the endocervix, and untreated, recent (< 14 days) documented gonococcal or chlamydial cervicitis. Exclusion criteria: pregnant or lactating; complicated PID (pelvic or tubo‐ovarian abscess ruled out by pelvic ultrasonography or laparoscopic examination within 48 h before or 24 h after the start of therapy) or any condition likely to require surgical intervention within 24 h of the start of treatment (or both); hypersensitivity to any study drug, related compound, or excipient; a history of tendon disorders associated with quinolones; history of clinically relevant cardiovascular abnormalities; history of epilepsy; defect in glucose‐6‐phosphate dehydrogenase; receipt of systemic antibacterial therapy ≤ 7 days before enrolment; history of uterine or pelvic or abdominal surgery ≤ 30 days before treatment; intolerance to or inability to follow an oral antibiotic regimen; impaired liver function (Child‐Pugh C) or transaminase levels > 5 times the upper limit of normal (or both); impaired renal function (creatinine clearance ≤ 50 mL/minute); neutropenia (< 1000/mm3); infection with HIV and CD4 count < 200/mm3; AIDS; and active antiretroviral therapy. Number of women randomized: 460. Number of women analyzed: ITT: group A: 228; group B: 232; PP: group A: 194; group B: 190. Number of withdrawals/exclusions/loss to follow‐up and reasons: group A: 34 (violations of inclusion/exclusion criteria (n = 11); not treated with study drug (n = 3), non‐compliance with study drug (n = 4), insufficient duration of therapy (n = 9), violation of time schedule (n = 5), informed consent withdrawn (n = 2), essential data missing/invalid (n = 14), lost to follow‐up (n = 2), use of prohibited concomitant medication (n = 4); group B: 42 (violations of inclusion/exclusion criteria (n = 16); not treated with study drug (n = 2), non‐compliance with study drug (n = 2), insufficient duration of therapy (n = 9), violation of time schedule (n = 6), informed consent withdrawn (n = 2), essential data missing/invalid (n = 18), lost to follow‐up (n = 2), use of prohibited concomitant medication (n = 6). Number of centres: 7. Age (mean) (years): group A: 35.2 (SD 8.4); group B: 35.4 (SD 8.7). Countries: China, Indonesia, South Korea, The Philippines, Pakistan, Thailand, Taiwan. |
|
| Interventions |
Group A: moxifloxacin 400 mg PO once daily for 14 days. Group B: levofloxacin 500 mg (2 × 250 mg tablets) PO once daily + metronidazole 500 mg (1 tablet) PO twice daily for 14 days. |
|
| Outcomes | Efficacy: primary efficacy variable was clinical response at test‐of‐cure in the PP population.
Secondary efficacy variables.
Safety: occurrence of adverse events (ITT population), including most commonly occurring drug‐related treatment‐emergent events seen in > 2% of either group (ITT/safety population). Safety evaluations included a physical examination (including vital signs) at enrolment, during treatment, at the test‐of‐cure visit and at follow‐up. Clinical laboratory assessments (for blood chemistry and haematological parameters) performed on blood samples taken within 48 h of first dose of study drug, and repeated at test‐of‐cure and follow‐up (in case abnormalities arose on or after test‐of‐cure visit). |
|
| Notes | Study funded by Bayer HealthCare AG, Leverkusen, Germany. 1 author (PJ) received travel grants and consulting fees from GlaxoSmithKline and Sanofi‐Pasteur‐MSD, and consulting fees from Bayer HealthCare. 2 authors (QL and ZL) declared no conflicts of interest. 1 author (PR) was an employee of Bayer Vital GmbH; 2 authors (PA and BH) were employees of Bayer Schering Pharma. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random code provided by Bayer Biometry (Wuppertal, Germany); numbers assigned in sequential ascending order; no numbers left out or substituted. |
| Allocation concealment (selection bias) | Low risk | Provided by the investigator in sealed envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants and personnel administering and assessing outcome blinded to treatment given. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants and personnel administering and assessing outcome blinded to treatment given. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition rate (< 20%). |
| Selective reporting (reporting bias) | Unclear risk | No trial protocol found. |
| Other bias | Low risk | No other source of potential bias found for ITT analysis. |
Landers 1991.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: women with either laparoscopically confirmed salpingitis or histologically confirmed plasma cell endometritis or they met previously published criteria for non‐invasive diagnosis of salpingitis. Criteria included direct abdominal tenderness, cervical motion tenderness, and adnexal tenderness, plus ≥ 1 of the following: temperature ≥ 38 °C, peripheral blood leukocytosis WBC count > 10,500/mm3, purulent material or culdocentesis, evidence of pelvic abscess on ultrasonography or pelvic examination, evidence of gonococcal or chlamydial cervicitis (by positive monoclonal antibody test or by Gram's stain showing gram‐negative intracellular diplococcic), or mucopurulent cervicitis as previously defined. Exclusion criteria: allergy to any of 4 antibiotics involved in trial; pregnancy; or history of pelvic surgery, abortion, uterine curettage, or delivery within 6 weeks of admission. Number of women randomized: 162. Number of women analyzed: 148; group A: 75; group B: 73. Number of withdrawals/exclusions/loss to follow‐up and reasons: 14; reasons for exclusion: incorrect diagnosis that was discovered at laparoscopy or laparotomy, refusal of the woman to remain hospitalized long enough to complete treatment. Number of centres: 2. Age (mean) (years): total: 23.5 (SD 6.1); group A: 23.3 (SD 5.3); group B: 23.8 (SD 6.0). Country: US. |
|
| Interventions |
Group A: cefoxitin 2 g IV every 6 h + doxycycline 100 mg IV every 12 h for minimum 4 days and ≥ 48 h after disappearance of fever. Women without fever on admission treated for minimum of 4 days in hospital for ≥ 24 h beyond the adequate relief of pain and tenderness to a normal lifestyle without surgical intervention. After discharge from hospital, doxycycline 100 mg PO twice daily was continued to complete a total of 14 days of treatment. Group B: clindamycin 600 mg IV every 6 h + tobramycin 2 mg/kg IV for 1 dose, followed by 1.5 mg/kg IV every 8 h for minimum of 4 days and for ≥ 48 h after disappearance of fever. Women without fever on admission treated for minimum of 4 days in hospital for ≥ 24 h beyond adequate relief of pain and tenderness to a normal lifestyle without surgical intervention. After discharge from hospital, clindamycin 450 mg PO 4 times daily continued to complete a total of 14 days of treatment. |
|
| Outcomes |
Primary outcome (ITT): clinical response for a satisfactory initial clinical response defined as an improvement of admitting signs and symptoms, included abdominal‐pelvic pain, fever, and pelvic tenderness. Follow‐up evaluation performed at hospital discharge and at 2–6 weeks after initial enrolment. Secondary outcomes (PP): microbiological clearance of C trachomatis and reduction in tenderness score. |
|
| Notes |
Ethical approval: yes, study reviewed and approved by institutional review board at both hospitals. Informed consent: yes, written informed consent obtained from all women before enrolment. Source of funding: supported in part by National Institutes of Health grants AI12192 and 1PO1 AI24768 and by Merck, Sharp & Dohme, Westpoint, PA. No conflicts of interest reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Non‐blinded study. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Non‐blinded study. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 100% follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol found. |
| Other bias | Unclear risk | Not stated. |
Leboeuf 1987.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: women aged ≥ 18 years hospitalized with 1 of the following conditions: endometritis, myometritis, postoperative infections in pelvic region, pelvic peritonitis, acute adnexal infections such as salpingitis or pyosalpinx.
Exclusion criteria: allergy to clindamycin, lincomycin, metronidazole, or gentamicin; colitis when taking antibiotics; taken antibiotics in 48 h before entering study; pregnant or lactating; vestibular or cochlear lesion; renal insufficiency (creatinine > 12 mg/L; WBC count < 2000/mm2; platelets < 100,000/mm3; history of thrombopathy; peripheral neuropathy; participation in another clinical trial. Number of women randomized: 45; group A: 23; group B: 22. Number of women analyzed: 39; group A: 21; group B: 18. Number of withdrawals/exclusions/loss to follow‐up and reasons: group A: 2; group B: 4. All unexplained. Number of centres: 2. Age (mean) (years): group A: 27.9 (SD 5.2); group B: 29.1 (SD 9.5). Country: France. |
|
| Interventions |
Group A: clindamycin 900 mg IV every 8 h diluted in 150 mL (minimum volume) saline slow perfusion (30–60 minutes) + gentamicin 1 mg/kg IM every 8 h (with minimum dose prescribed of 60 mg every 8 h, according to bodyweight). Treatment given for minimum of 5 days in hospital. Clindamycin perfusion not stopped until 48 consecutive h with temperature below 37.5 °C; at that point treatment could be PO. Maximum length of treatment at discretion of therapist. If also treated with a tetracycline, this was not prescribed < 48 h after the end of the treatment protocol (either clindamycin + gentamicin or metronidazole + gentamicin). Group B: metronidazole 500 mg every 8 h in slow IV perfusion (30–60 minutes) + gentamicin 1 mg/kg IM every 8 h (with minimum dose prescribed of 60 mg every 8 h, according to bodyweight). Treatment given for 6 weeks. |
|
| Outcomes |
Primary outcome: clinical cure: absence of infection in the days following cessation of treatment according to clinical observations, microbe eradicated during or after treatment. Secondary outcome: length of hospital stay. |
|
| Notes |
Ethical approval: not stated. Informed consent: not stated. Source of funding: not stated, and no conflicts of interest reported. Mean days of hospitalization: 11.17 days. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition < 20%. |
| Selective reporting (reporting bias) | Unclear risk | No trial protocol found. |
| Other bias | Unclear risk | Not stated. |
Malhotra 2003.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: women with first episode of PID. Exclusion criteria: women with recurrent PID or with previous antibiotic therapy. Number of women randomized: 165. Number of women analyzed: 153; group A: 52; group B: 48; group C: 53. Number of withdrawals/exclusions/loss to follow‐up and reasons: group A: 3 women excluded from analysis; group B: 7; group C: 2. Number of centres: 1. Age (mean) (years): group A without women excluded from analysis: 25.6 (SD 3.9); group B without women excluded from analysis: 25.8 (SD 3.2); group C without women excluded from analysis: 25.5 (SD 4.9). Country: India. |
|
| Interventions |
Group A: ciprofloxacin 500 mg + tinidazole 600 mg (Table Brakke, Franko India Pharma, Mumbai, India) twice daily for 7 days. Group B: fluconazole 150 mg (1 tablet) + azithromycin 1 g (1 tablet) + secnidazole 2 g (2 tablets) (Fas‐3 kit Lyka, Mumbai, India). Advised to take azithromycin on empty stomach in the morning, secnidazole with or after food and fluconazole in the evening. Group C: doxycycline 100 mg twice daily + metronidazole 200 mg 3 times daily for 1 week. The 2 drugs were available in the hospital pharmacy free of cost. |
|
| Outcomes |
Primary outcome: clinical cure: women assessed at the first visit by a severity score (Modified Severity Score of Soper 1988) the findings at the first examination and severity score noted in the Performa filled for every woman. The women were asked to report after 1 week and 4 weeks. Repeat gynaecological examination and severity score performed and recorded in the Performa. All women were advised to report within 3 days if there was no improvement in symptoms, any deterioration in their condition, or inability to carry on with the oral therapy when they were hospitalized. Clinical cure defined as ≥ 70% reduction in severity score, no more than mild abdominal pain, and no recurrence of symptoms or signs of PID within 4 weeks of therapy. Treatment failure defined as < 20% decrease in tenderness score. Modified ITT (cases that were not PID were excluded). Group A: 52. Group B: 48. Group C: 53. |
|
| Notes |
Ethical approval: yes, the departmental ethical committee approved the study. Informed consent: yes, verbal informed consent taken from all the women. Source of funding: not stated, and no conflicts of interest reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Using a computer‐generated number, all women were randomized to 1 of 3 treatment groups initially, and later it was a block randomization to equalize the groups. |
| Allocation concealment (selection bias) | Unclear risk | Not reported by whom allocation was done and how. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Unfortunately we could not get similar looking packs from the market so the assignment was not concealed from the investigator." |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: "Unfortunately we could not get similar looking packs from the market so the assignment was not concealed from the investigator." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 12/165 women excluded from analysis. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol found. |
| Other bias | Unclear risk | Not stated. |
Maria 1992.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: women aged 15–51 years who required hospitalization for treatment of acute PID based on clinical and laboratory evidence. All women had abdominal, parametrial, and cervical motion tenderness. The additional finding of fever, leukocytosis, pelvic mass, or purulent material in the peritoneal cavity confirmed the diagnosis. Exclusion criteria: allergies to study drugs, requirement for concomitant therapy with other antibiotics, and > 2 doses of antibiotics in the 7 days prior to admission. Number of women randomized: 170; group A: 88; group B: 82. Number of women analyzed: 170; group A: 88; group B: 82. Number of withdrawals/exclusions/loss to follow‐up and reasons: group A: 28; group B: 27 due to failure to follow randomization scheme, protocol deviation, and incorrect diagnoses. Number of centres: 10. Age (mean) (years): whole study group: 28; age per group not stated. Country: 9 in Europe and 1 Africa. |
|
| Interventions |
Group A: clindamycin 900 mg IV every 8 h + gentamicin 2 mg/kg IV, followed by 1.5 mg/kg IV every 8 h for minimum of 4 days. At the end of the period of IV therapy, clindamycin 450 mg PO every 6 h was given to complete 14 days of treatment. Group B: cefoxitin 2 g IV every 6 h + doxycycline 100 mg IV every 12 h were given for ≥ 4 days. At the end of IV therapy, doxycycline 100 mg PO was given every 12 h to complete a total of 14 days of treatment. |
|
| Outcomes |
Primary outcomes: clinical failure, minimum of 48 h of protocol therapy and characterized by signs and symptoms as unchanged or worsened during the first 48–72 h of treatment, or worsening later, failure to improve further; need of additional antibiotics or need for surgery considered as failure; adverse events leading to discontinuation of therapy. Secondary outcomes: microbial cure of C trachomatis and N gonorrhoeae. |
|
| Notes |
Ethical approval: not stated. Informed consent: yes, informed consent obtained from all women prior to entry into trial. Source of funding: not stated, and no conflicts of interest reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated how randomization sequence was generated. |
| Allocation concealment (selection bias) | Unclear risk | Not stated by whom allocation concealment was done. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label study. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Open‐label study. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 115/170 (68%) women analyzed. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol found. |
| Other bias | Unclear risk | Not stated. |
Martens 1990.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: diagnosis of PID based on: oral body temperature ≥ 38.3 °C, lower abdominal tenderness, cervical or uterine tenderness on palpation and motion, and tenderness on palpation of adnexa. In addition, the following may have been present: purulent endocervical discharge, WBC count ≥ 14,000/mm3, adnexal mass or abscess, nausea, and vomiting. Women selected for the uncomplicated PID group if the above criteria were met, but no adnexal mass was noted on palpation, ultrasonography, or at the time of surgery. In the complicated PID group, women with tubo‐ovarian complex did not meet the above criteria and had evidence of a unilateral or bilateral adnexal mass on pelvic examination, not confirmed by a radiolucent area on ultrasound examination or surgery. Women with tubo‐ovarian abscess had the above findings including a radiolucent area on ultrasound, consistent with an abscess or pus‐filled cavity noted at surgery. Exclusion criteria: not stated. Number of women randomized: 99. Number of women analyzed: 94. Number of withdrawals/exclusions/loss to follow‐up and reasons: 5 women were excluded from evaluation due to protocol violations. Number of centres: not stated. Age (mean) (years): group A: 26 (SD 7); group B: 25 (SD 7); group C: 26 (SD 7). Country: not stated. |
|
| Interventions |
Group A: cefoxitin 2 g every 6 h for minimum of 4 days and continued until the woman was apyrexial with improvement of symptoms for ≥ 48 h. Group B: cefotaxime 2 g every 8 h for minimum of 4 days and continued until the woman was apyrexial with improvement of symptoms for ≥ 48 h. Group C: clindamycin 900 mg every 8 h + gentamicin at initial loading dose of 120 mg, followed by maintenance doses of 80 mg every 8 h. Subsequent maintenance doses determined by evaluating trough and peak serum aminoglycoside concentrations. Antibiotics given for minimum of 4 days, and continued until the woman was apyrexial with improvement of symptoms for ≥ 48 h. |
|
| Outcomes | Primary outcome: clinical failure: evaluated on a daily basis. Women who had not demonstrated signs of improvement after 48–72 h of antibiotic therapy were considered an unsuccessful result. | |
| Notes |
Ethical approval: not stated. Informed consent: not stated. Source of funding: not stated, and no conflicts of interest declared. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | There were 2 randomization codes, 1 for each diagnosis group. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 94/99 women included in analysis. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol found. |
| Other bias | Unclear risk | Not stated. |
Martens 1993.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: non‐pregnant, non‐lactating women using a reliable form of contraception and who fulfilled the diagnostic criteria for uncomplicated PID. Diagnostic inclusion criteria for uncomplicated PID were all the following: direct lower abdominal tenderness with or without rebound tenderness, cervical motion tenderness, and adnexal tenderness. Plus ≥ 1 of the following: recent positive endocervical culture for N gonorrhoeae or C trachomatis, temperature > 38 °C, WBC count > 10,000/mm3, leukocytic endocervical discharge. Exclusion criteria: pelvic infection severe enough to require parenteral antimicrobial therapy or if surgical intervention within the next 24 h was anticipated; evidence of a pelvic abscess by ultrasonography or clinical examination; if pain had been present for > 2 weeks; allergy to study medications; major gastrointestinal, renal, or hepatic disorders; used other antimicrobial agents within previous 2 weeks; IUD in place; or alcohol or drug abusers. Number of women randomized: 295; group A: 150; group B: 145. Number of women analyzed: 249; group A: 128; group B: 121. Number of withdrawals/exclusions/loss to follow‐up and reasons: 46 women excluded from analysis due to protocol violations or loss to follow‐up. Number of centres: 16. Age (mean) (years): group A: 25.9 (SD 5.8); group B: 26.0 (SD 6.8). Country: US. |
|
| Interventions |
Group A: ofloxacin 400 mg PO every 12 h for 10 days. Group B: cefoxitin 2 g IM + probenecid 1 g PO, followed by doxycycline 100 mg PO every 12 h for 10 days. |
|
| Outcomes |
Primary outcomes: clinical cure: complete resolution of tenderness; clinical improvement: partial resolution of tenderness without the need for additional antibiotic therapy. Secondary outcomes: microbial cure of C trachomatis, microbial cure of N gonorrhoeae. |
|
| Notes |
Ethical approval: yes, "with approval from their respective institutional review boards." Informed consent: yes, "the subjects were enrolled after giving informed consent." Source of funding: supported in part by a grant from Ortho Pharmaceutical Corporation, Raritan, NJ. No conflicts of interest declared. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | After obtaining informed consent, women given a computer‐generated randomization code number and assigned to either treatment regimen using 1:1 ratio. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 46/295 women excluded from analysis due to protocol violations or loss to follow‐up (< 20%). |
| Selective reporting (reporting bias) | Unclear risk | No study protocol found. |
| Other bias | Unclear risk | Not stated. |
Okada 1988.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: women aged ≥ 16 years, inpatients and outpatients; intrauterine infection, uterine adnexitis, bartholinitis, or bartholin's abscess. Exclusion criteria: age < 16 years; premedication with ciprofloxacin or cefroxadine; women improving with other treatments; allergy to cephem or pyridonecarboxylic acid; taking theophylline or fenbufen, severe problems in the heart, liver, or kidneys; women with epilepsy; pregnant or breastfeeding; rejection by the doctor. Number of women randomized: 253; group A: 124; group B: 129. Number of women analyzed: 209; group A: 104; group B: 105. Number of withdrawals/exclusions/loss to follow‐up and reasons: total: 44; group A: 20; group B: 24. No reasons presented. Number of centres: 55. Age (years): only presented as frequencies within age groups. Country: Japan. |
|
| Interventions |
Group A: ciprofloxacin 200 mg PO + dummy cefroxadine placebo, 3 times daily for 7 consecutive days. Group B: cefroxadine 250 mg PO + dummy ciprofloxacin placebo, 3 times daily for 7 consecutive days. |
|
| Outcomes |
Primary outcomes: clinical cure at 7th day of treatment: excellent: clinical marked improvement and clearance of bacteria; good: clear clinical improvement; poor: no clear clinical improvement; adverse events. Secondary outcome: local tenderness around uterus. |
|
| Notes |
Ethical approval: not stated. Informed consent: not stated. Source of funding: not stated, and no conflicts of interest reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 2 ciprofloxacin and 2 cefroxadine each with dummy placebo were arranged for 7‐day use and numbered. Numbers randomly assigned. 4 series of numbered medicine packed in a box. Then, some boxes were delivered to every institution. |
| Allocation concealment (selection bias) | Unclear risk | Having used numbered series of medicine to women consecutively. Block size of 4 and might be too small for concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐dummy placebo method. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Double‐blind method. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition < 20%. |
| Selective reporting (reporting bias) | Unclear risk | No trial protocol found. |
| Other bias | Unclear risk | Not stated. |
Ross 2006.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: women with uncomplicated PID, confirmed by absence of pelvic or tubo‐ovarian abscess on transabdominal/transvaginal pelvic ultrasound or laparoscopy (within 2 days before or 1 day after the start of treatment), or both ultrasound and laparoscopy. Diagnosis of PID was based on the presence of all the following: pelvic discomfort, direct lower abdominal tenderness with or without rebound tenderness, and adnexal/cervical motion tenderness on bimanual vaginal examination. In addition, ≥ 1 of the following signs: raised temperature (> 37.5 °C); ESR > 15 mm in first hour; CRP value > upper limit of normal range; WBC count > 10,500/mm3; laparoscopic evidence of PID; signs suggestive of cervical infection (e.g. mucopurulent cervical discharge); or untreated, documented gonococcal or chlamydial cervicitis within previous 14 days. Exclusion criteria: contraindications to study drugs; required surgery within the next 24 h or had a history of uterine or pelvic or abdominal surgery within the past 30 days; or previous treatment with systemic antibiotic therapy in the last 7 days. Number of women randomized: 749. Number of women analyzed: group A: 384; group B: 365. Number of withdrawals/exclusions/loss to follow‐up and reasons: group A: 51 (24 due to adverse events; 14 consent withdrawn; 7 lost to follow‐up; 2 non‐compliant; 1 protocol violation; 2 insufficient therapeutic effect; 1 investigator decision); group B: 38 (17 due to adverse events; 9 consent withdrawn; 5 lost to follow‐up; 4 non‐compliant; 3 protocol violation). Number of centres: 13. Age (mean) (years): group A: 30.1 (SD 8.4); group B: 30.5 (SD 8.5). Countries: Denmark; Finland; France; Germany; Greece; Hungary; Italy; Lithuania; Poland; Russia; South Africa; Sweden; UK. |
|
| Interventions |
Group A: moxifloxacin 400 mg PO once daily for 14 days. Group B: ofloxacin 400 mg PO twice daily + metronidazole 500 mg PO twice daily for 14 days. |
|
| Outcomes |
Primary outcome: clinical cure (5–24 days post‐therapy): reduction of the pelvic pain score by > 70% (McCormack score, table A) + apyrexia (rectal/tympanic/oral temperature < 38.0 °C or axillary/cutaneous temperature < 37.5 °C) + WBC count < 10,500/mm3. Secondary outcomes: microbial cure of C trachomatis; microbial cure of N gonorrhoeae. |
|
| Notes |
Ethical approval: study protocol prepared in accordance with the Declaration of Helsinki and ethical approval obtained for each centre. Informed consent: written, informed consent obtained from each woman. Source of funding: grant from Bayer HealthCare. No competing interests declared for 4 authors (HC, TP, IR, or DV). 1 author (JR) received payment as a consultant and lecturer, and sponsorship to attend medical conferences from Bayer HealthCare. 1 author (JR) was an associate editor of Sexually Transmitted Infections. 4 authors (AK, MA, PA, and PR) were employees of Bayer HealthCare. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | No description of how randomization was generated. Author retrieved information from full report. |
| Allocation concealment (selection bias) | Low risk | No description if allocation was concealed. After consulting the full report, the author stated that allocation was made by the pharmacy. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding achieved by dispensing medication with identical packaging (blister packs) and appearance (all drugs and placebo tablets were encapsulated). |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Double blind. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition < 20%. |
| Selective reporting (reporting bias) | Low risk | Trial protocol was published in www.stijournal.com/supplemental. |
| Other bias | Unclear risk | Not stated. |
Roy 1985.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: not stated. Exclusion criteria: not stated. Number of women randomized: 46 (36 with acute PID). Number of women analyzed: group A: 19; group B: 9; group C: 9. Number of withdrawals/exclusions/loss to follow‐up and reasons: all 46 women completed the study; however, only 36 had acute PID. Number of centres: 1. Age: not stated. Country: US. |
|
| Interventions |
Group A: cefotaxime 2 g IV or IM every 8 h. Group B: clindamycin 600 mg IV every 6 h + gentamicin 1.5 mg/kg lean bodyweight IV or IM every 8 h. Group C: clindamycin 600 mg IV every 6 h + gentamicin 1.5 mg/kg lean bodyweight IV or IM every 8 h + penicillin G 5 million units IM every 4 h. |
|
| Outcomes |
Primary outcomes: clinical cure: antibiotic change was made for treatment failure from an assigned regimen based upon persistence or worsening of signs and symptoms after 48 h. Secondary outcomes: none reported. |
|
| Notes |
Ethical approval: not stated. Informed consent: yes, enrolled after informed consent obtained. Source of funding: not stated, and no conflicts of interest reported. Range of hospital stay: 3–11 days. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All women randomized completed the study. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol found. |
| Other bias | Unclear risk | Not stated. |
Roy 1990.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: lower abdominal pain and tenderness, cervical motion or adnexal tenderness, and 1 of the following: oral temperature > 38 °C, leukocytosis > 10,500/mm3, or presence of a suspected inflammatory pelvic mass on examination or by ultrasound. Exclusion criteria: allergy to cephalosporins or penicillins; had taken antibiotics in the previous 3 days; had received any investigational drugs in the previous 30 days; pregnant or breastfeeding; rapidly progressive underlying disease that could preclude evaluation of therapy; or required other systemic antibiotics on admission. Number of women randomized: 67. Number of women analyzed: 67; group A: 13; group B: 14; group C: 19; group D: 21. Number of withdrawals/exclusions/loss to follow‐up and reasons: 3 women, 1 because of protocol violation and 2 left the study before completion of therapy. Number of centres: 1. Age (mean) (years): group A: 26.6 (SEM 1.9); group B: 28.9 (SEM 1.7); group C: 27.1 (SEM 1.3); group D: 28.3 (SEM 1.0). Country: US. |
|
| Interventions |
Group A: ceftizoxime 2 g IV every 12 h + doxycycline 100 mg IV twice daily. Group B: ceftizoxime 2 g IV every 6 h + doxycycline 100 mg IV twice daily. Group C: ceftizoxime 2 g IV every 8 h + doxycycline 100 mg IV twice daily. Group D: clindamycin 900 mg IV every 8 h + gentamicin 2 mg/kg loading dose followed by 1.5 mg/kg IV every 8 h with adjustments if necessary. |
|
| Outcomes |
Primary outcomes: clinical cure: adequate response to therapy: clinically improved and afebrile for 48 h at time of discharge; 8–24 before discharge; no pelvic tenderness; adverse events leading to discontinuation of therapy. Secondary outcomes: microbial cure of C trachomatis, microbial cure of N gonorrhoeae, and length of hospital stay. |
|
| Notes |
Ethical approval: not stated. Informed consent: yes, women signed informed consent forms previously approved by institutional review board. Source of funding: financial assistance, in part, provided by Smith Kline & French Laboratories, Philadelphia, PA. No conflicts of interest reported. Follow‐up: 10–14 days. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 3 women withdrew from the study or were lost to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol found. |
| Other bias | Unclear risk | Not stated. |
Savaris 2007.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: history of pelvic discomfort for < 30 days, with findings of pelvic organ tenderness (uterine or adnexal) on bimanual examination, and leukorrhoea or mucopurulent cervicitis. Exclusion criteria: current UTI; pregnancy; presence of tubo‐ovarian abscess, endometriosis, appendicitis, diverticulitis, haemorrhagic ovarian cysts or torsion; abdominal hernia; homelessness; fever > 38 °C; abdominal rebound tenderness; pelvic pain > 30 days' duration; allergy to ceftriaxone, azithromycin, or doxycycline; history of antimicrobial therapy within 7 days of recruitment; delivery, abortion, or gynaecological surgery within 30 days; prior hysterectomy or bilateral salpingectomy; and oral intolerance for the antibiotics. Number of women randomized: 133. Number of women analyzed: group A: 66; group B: 67. Number of withdrawals/exclusions/loss to follow‐up and reasons: group A: 4 lost to follow‐up, 2 discontinued intervention (1 oral intolerance, 1 worsening of the pain); group B: 7 lost to follow‐up: 9 discontinued intervention (2 oral intolerance, 7 worsening of pain). Number of centres: 1. Age (mean) (years): group A: 28.3 (SD 0.8); group B: 29.27 (SD 1.1). Country: Brazil. |
|
| Interventions |
Group A: ceftriaxone IM 250 mg + azithromycin 1 g PO single dose and repeated after 7 days. Group B: ceftriaxone IM 250 mg + doxycycline 200 mg PO for 14 days. |
|
| Outcomes |
Primary outcome: clinical cure defined as ≥ 70% reduction in the total tenderness score at day 14 compared with baseline, for both visual analogue scale and McCormack pain scale. Secondary outcome: microbial cure of C trachomatis. |
|
| Notes |
Ethical approval: study protocol approved by ethics committee of Hospital de Clínicas de Porto Alegre, and registered at isrctn.org under ISRCTN46117662. Informed consent: enrolled in study after signing the informed consent. Source of funding: supported by Grupo de Pesquisa e Pos‐Graduacão Do Hospital de Clínicas de Porto Alegre under grant # 03/006. GenProbe (San Diego, CA) donated the kits to run the bacteriological analysis, and Pfizer (New York, NY) donated azithromycin to the Global Program to Eliminate Trachoma (Dr Schachter had a National Institutes of Health grant to do operational research on azithromycin treatment of trachoma, and the company donated the drug). The drug used in this study was obtained independently in Brazil, without Pfizer support. The other authors had no potential conflicts of interest to disclose. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used computer‐generated table for allocation sequence. Women allocated in blocks of 4. |
| Allocation concealment (selection bias) | Low risk | To avoid bias, both medications were manipulated by the hospital pharmacy and put in identically coded blisters and capsules. Because of the difference in the number of capsules in each treatment, the empty azithromycin blisters were filled with placebo. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Women and assessors blinded to group assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Women and assessors blinded to group assignment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition rate (< 20%). |
| Selective reporting (reporting bias) | Low risk | Trial protocol published (ISRCTN46117662). |
| Other bias | Unclear risk | The drug used in this study was obtained independently in Brazil, without Pfizer support. Analysis was provided as modified ITT, where conditions others than PID were excluded from analysis after randomization. |
Sirayapiwat 2002.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: aged > 16 years; gave written consent prior to entry; clinical diagnosis of acute PID made when woman had all following: lower abdominal tenderness, adnexal tenderness, and cervical motion tenderness; ≥ 1 of following: oral temperature ≥ 38.3 °C, abnormal cervical discharge, elevated ESR or CRP, and endocervical specimen positive for N gonorrhoeae or C trachomatis. Exclusion criteria: pregnant or lactating; history of hypersensitivity to penicillin, aminoglycoside, clindamycin, or metronidazole; severe hepatic disease; renal impairment (serum creatinine level > 2 mg/dL), or evidence of ruptured tubo‐ovarian abscess. Number of women randomized: 44; 22 per group. Number of women analyzed: 44; 22 per group. Number of withdrawals/exclusions/loss to follow‐up and reasons: 0 reported as lost to follow‐up. Number of centres: 1. Age (mean) (years): group A: 31.2 (SD 9.1); group B: 24.9 (SD 7.6). Country: Thailand. |
|
| Interventions |
Group A: (triple therapies) received ampicillin 1 g IV every 6 h + gentamicin 5 mg/kg (not exceeding 240 mg) daily + metronidazole 500 mg every 8 h. Group B: clindamycin 600 mg IV every 8 h + gentamicin 5 mg/kg (not exceeding 240 mg) once daily. In both groups, parenteral therapies continued until women were afebrile for minimum of 48 h then all women received doxycycline 100 mg PO every 12 h to complete a 14‐day course. |
|
| Outcomes |
Primary outcomes: clinical cure; adverse events leading to discontinuation of therapy. Secondary outcome: length of hospital stay. Visual analogue scale on day 3 of treatment. |
|
| Notes |
Ethical approval: yes, approval for study obtained from the Ethical Committee of the Faculty of Medicine, Chulalongkorn University before trial was started. Informed consent: yes, all women gave written consent before entering study. Source of funding: not stated, and no conflicts of interest reported. Significant baseline imbalances between groups. Age, infertility, and severity of pain prior to this study significantly lower in group B (clindamycin/gentamicin). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization codes computer‐generated and sealed in envelope, then women were randomly assigned to 1 of the 2 regimens depending on their codes (A or B). |
| Allocation concealment (selection bias) | Unclear risk | Not stated by whom allocation concealment was done. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All women randomized were analyzed. |
| Selective reporting (reporting bias) | Unclear risk | No trial protocol found. |
| Other bias | Unclear risk | Not stated. |
Soper 1988.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: written informed consent; met criteria for diagnosis of PID with the following: lower abdominal pain and bilateral adnexal tenderness on bimanual pelvic examination; microscopy of a wet mount of the vaginal contents revealing marked increase in the number of leukocytes (i.e. leukocytes outnumbered all other cellular elements in the smear); ≥ 2 of the following: temperature > 38 °C, leukocytosis (> 11,000/mm3), purulent material from the peritoneal cavity by culdocentesis, inflammatory complex on bimanual examination or sonography, ESR > 20 mm/h; uncomplicated salpingitis limited to tube(s) or ovary(ies) (or both) without pelvic peritonitis; complicated (inflammatory mass or abscess involving tube(s) or ovary(ies) (or both) with or without pelvic peritonitis. Exclusion criteria: pregnant; history of allergy to 1 of study drugs. Number of women randomized: 62; 31 per group. Number of women analyzed: 62; 31 per group. Number of withdrawals/exclusions/loss to follow‐up and reasons: 0 reported as lost to follow‐up. Number of centres: 1. Age (mean) (years): group A: 23.4 (SD 5.8); group B: 21.9 (SD 3.7). Country: US. |
|
| Interventions |
Group A: cefoxitin 2 g IV every 6 h + doxycycline 100 mg IV every 12 h. Women discharged with doxycycline 100 mg PO twice daily to complete a 10‐day course. Group B: clindamycin 600 mg IV every 6 h + amikacin 7.5 mg/kg IV every 12 h. Women discharged with clindamycin 300 mg PO 4 times daily to complete a 10‐day course. |
|
| Outcomes |
Primary outcome: clinical failure: persistence of fever (> 38 °C), elevated WBC count (> 11,000/mm3), moderate‐severe pelvic organ tenderness despite 96 h of antibiotic therapy, need of laparotomy. Secondary outcome: length of hospital stay. |
|
| Notes |
Ethical approval: not stated. Informed consent: yes, enrolled after obtaining informed consent according to guidelines of the Human Research Committee. Source of funding: not stated, and no conflicts of interest reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Women admitted to hospital and assigned randomly in a double‐blind method, to 1 of 2 treatment regimens by sealed envelope, generated from a table of random numbers. |
| Allocation concealment (selection bias) | Unclear risk | Allocation reported to have taken place in sealed envelopes, but it was not reported who distributed them. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated who was blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated who was blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All women randomized were analyzed. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol found. |
| Other bias | High risk | Significant baseline imbalances between groups. Age, infertility, and severity of pain prior to this study was significant lower in group B (clindamycin/gentamicin). |
Sweet 1985.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: none stated. Exclusion criteria: none stated. Number of women randomized: 60; 30 per group. Number of women analyzed: 60; 30 per group. Number of withdrawals/exclusions/loss to follow‐up and reasons: 0 reported as lost to follow‐up. Number of centres: 1. Age (mean) (years): group A: 24.2 (SD 5.1); group B: 24.7 (SD 7.2). Country: US. |
|
| Interventions |
Group A: moxalactam 2 g IV every 8 h. Group B: clindamycin 600 mg IV every 6 h + tobramycin 1.5 mg/kg every 8 h. |
|
| Outcomes |
Primary outcome: microbiological cure. Secondary outcome: length of hospital stay. |
|
| Notes |
Ethical approval: not stated. Informed consent: yes, all women gave informed consent approved by the University of California (San Francisco) Committee on Human Research. Source of funding: not stated, and no conflicts of interest reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomized schedule. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All women randomized were analyzed. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol found. |
| Other bias | Unclear risk | Not stated. |
Thadepalli 1991.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: women of reproductive age who had clinical features of PID, acute salpingitis, or suspected pelvic abscess, such as lower abdominal pain associated with fever and chills, and cervical motion tenderness with or without signs of adnexal masses; required hospitalization for IV antibiotic therapy. In all cases, CDC criteria for PID satisfied. Exclusion criteria: suspected or known to be pregnant; breastfeeding. Number of women randomized: 71; group A: 35; group B: 36. Number of women analyzed: 61; group A: 31; group B: 30. Number of withdrawals/exclusions/loss to follow‐up and reasons: 10 women; group A: 4; group B: 6 later excluded from evaluation due to wrong diagnosis or protocol violations. Number of centres: not stated. Age (mean) (years): group A: 27.5 (range 15–37); group B: 26.5 (range 19–36). Country: not stated. |
|
| Interventions |
Group A: ciprofloxacin 300 mg IV twice daily for ≥ 3 days followed by ciprofloxacin 500 mg PO twice daily for about 1 week. Group B: clindamycin 600 mg IV every 6 h + gentamicin 80 mg IV every 8 h, administered separately. Clindamycin by IV route for 3 days, followed by oral administration for about 1 week. Gentamicin dose adjusted based on serum creatinine and gentamicin levels. |
|
| Outcomes |
Primary outcomes: clinical cure: when there was resolution or clearing (or both) of signs of infection as evidenced by defervescence, reversal of leukocytosis, and abatement of abdominal pain and cervical motion tenderness; adverse events leading to discontinuation of therapy. Secondary outcome: length of hospital stay. |
|
| Notes |
Ethical approval: study protocol approved by the Human Rights Committee of their institution. Informed consent: yes, all women entered in study were informed in full and required to read and sign a consent form. Source of funding: supported by Miles Laboratory, New Haven, CT, a subsidiary of Bayer, Leverkusen, West Germany. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 10/71 (14%) women not analyzed. |
| Selective reporting (reporting bias) | Unclear risk | No trial protocol found. |
| Other bias | Unclear risk | Not stated. |
Tison 1988.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: upper genital tract infection, pelvic pain (bilateral, unilateral), fever > 37.5 °C, leukorrhoea, bleeding, digestive and urinary signs, pain in right hypochondrium. Diagnosis confirmed by laparoscopy. Exclusion criteria: pregnant or likely to be; allergy to penicillin or cephalosporins; receiving concomitant treatment with allopurinol; already received an antibiotic before admission; renal insufficiency. Number of women randomized: 40; 20 per group. Number of women analyzed: 40; 20 per group. Number of withdrawals/exclusions/loss to follow‐up and reasons: 1 woman withdrawn during hospital admission; 13 women lost to follow‐up. Number of centres: 1. Age (mean) (years): group A: 27.5 (range 17–39); group B: 22.5 (range 17–34). Country: France. |
|
| Interventions |
Group A: amoxicillin‐clavulanate 1 g slow IV perfusion every 8 h. PO once temperature normal for 48 h, 4 tablets of 500 mg, 2 at a time as long as hospitalized. After discharge, treatment continued with 3 tablets daily of amoxicillin‐clavulanate for 3 weeks. Group B: penicillin G 10 million units/24 h IV, followed by penicillin V PO + gentamicin 160 mg/24 h IM for 10 days + metronidazole 500 mg IV 3 times daily followed by metronidazole 500 mg PO 3 times daily. Duration of treatment unclear. |
|
| Outcomes | Effectiveness: cure: absence of pelvic pain on examination and referred by women, normal body temperature at discharge and 3 weeks later. Adverse events: any antibiotic‐related adverse event leading to discontinuation of therapy during hospital stay and after 30 days. |
|
| Notes |
Ethical approval: not stated. Informed consent: not stated. Source of funding: not stated, and no conflicts of interest reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open trial. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated. |
| Selective reporting (reporting bias) | Unclear risk | Not stated. |
| Other bias | Unclear risk | Not possible to identify. |
Walters 1990.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: women hospitalized from July 1986 to December 1988 with clinical diagnosis of acute PID diagnosed using the criteria proposed by Hager and colleagues (Hager 1983), and candidates for therapy. Exclusion criteria: aged < 15 years; pregnant; allergy to 1 of the study drugs or penicillin; concomitant infection requiring another antibiotic; serum creatinine level > 1.5 mg/dL; received any antibiotic therapy during past 7 days; or pelvic or abdominal surgery in the past 30 days. Number of women randomized: 147; unclear how many per group. Number of women analyzed: group A: 63; group B: 67. PP analysis only. Number of withdrawals/exclusions/loss to follow‐up and reasons: 17 women received < 48 h of protocol therapy and were removed from the study. Of these exclusions, diagnosis was made in error in 11 women; 2 did not meet the inclusion criteria; 2 required emergency surgery for ruptured tubo‐ovarian abscess within 24 h of admission and 2 left hospital against medical advice. Number of centres: 1. Age (mean) (years): total age not stated; group A: 25.4 (SD 7.7); group B: 24.5 (SD 7.8). Country: US. |
|
| Interventions |
Group A: gentamicin 2.0 mg/kg IV as loading dose, then 1.5 mg/kg IV every 8 h + clindamycin 900 mg IV every 8 h for minimum 4 days. After discharge, clindamycin 450 mg PO every 6 h for total 14 days. Group B: cefoxitin 2 g IV every 6 h + doxycycline 100 mg IV every 12 h for minimum 4 days. After discharge, doxycycline 100 mg PO every 12 h for total 14 days. |
|
| Outcomes |
Primary outcomes: clinical cure defined as oral temperature < 38 °C for 48 h, resolution of pain and tenderness, and no increase in the size of any pelvic mass after 21 days of initiation of treatment. Secondary outcomes: microbiological clearance of chlamydia; microbiological clearance of gonorrhoea after 21 days of initiation of treatment. |
|
| Notes |
Ethical approval: not stated. Informed consent: informed consent obtained and approved by Institutional Review Board of The University of Texas Health Science Center at San Antonio. Source of funding: supported by grant from the Upjohn Co., Kalamazoo, MI. No conflicts of interest reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated table. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Open‐label. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Of 147 women randomized, 17 received < 48 h of protocol therapy and were removed from the study. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol found. |
| Other bias | Unclear risk | Not stated. |
Wendel 1991.
| Study characteristics | ||
| Methods | Randomized controlled trial. | |
| Participants |
Inclusion criteria: non‐pregnant, non‐lactating women using a reliable form of contraception who met the inclusion criteria for acute salpingitis. Exclusion criteria: pelvic infection severe enough to require parenteral antimicrobial therapy (diffuse peritonitis) or if surgical intervention within the next 24 h was anticipated; evidence of a pelvic abscess on sonographic or clinical examination. Number of women randomized: 96; unclear how many to each group. Number of women analyzed: group A: 35; group B: 37. PP analysis only. Number of withdrawals/exclusions/loss to follow‐up and reasons: 24 women considered unevaluable because of total non‐compliance with study drug (1 woman) or lack of attendance at any follow‐up visits (23 women). Number of centres: 1. Age (mean) (years): total age not stated; group A: 24.7; group B: 23.3. Country: US. |
|
| Interventions |
Group A: cefoxitin 2 g IM + probenecid 1 g PO followed by doxycycline 100 mg PO every 12 h for 10 days. Group B: ofloxacin 400 mg PO every 12 h for 10 days. |
|
| Outcomes |
Primary outcomes: clinical cure defined as complete resolution of tenderness (> 65% decrease in clinical score); adverse events leading to discontinuation of therapy. Secondary outcomes: microbiological clearance of chlamydia; microbiological clearance of gonorrhoea. |
|
| Notes |
Ethical approval: unclear. Study approved by Texas Southwestern Medical Center Institutional Review Board. Informed consent: women enrolled after they gave informed consent. Source of funding: supported in part by a grant from Ortho Pharmaceutical Corporation, Raritan, NJ. No conflicts of interest reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Open‐label. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 24/96 women considered unevaluable. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol found. |
| Other bias | Unclear risk | Not stated. |
Wiesenfeld 2017.
| Study characteristics | ||
| Methods | Randomized placebo‐controlled trial | |
| Participants |
Inclusion criteria: aged 15–40 years at time of enrolment (participants aged 15–17 years required written informed consent from parent/legal guardian. Written assent also obtained from the minor); acute PID, defined by symptoms and signs guided by current CDC guidelines: current symptoms of lower abdominal or pelvic pain (present for ≤ 30 days) AND cervical motion tenderness, uterine tenderness, adnexal tenderness (or a combination) on pelvic examination; ability to provide written informed consent. Exclusion criteria: pregnant or breastfeeding; uterine procedure (e.g. dilation and curettage, abortion) or miscarriage within past 6 weeks; allergy to any of the study medications (cephalosporins, doxycycline, or metronidazole) or Type 1 hypersensitivity allergic reaction to penicillin for those with unknown tolerance to cephalosporins; systemic or vaginal antibiotic therapy in preceding 7 days; required inpatient PID therapy (per the current CDC guidelines); inability to obtain an endometrial biopsy at enrolment; known inability to comply with the follow‐up visits; prior hysterectomy; menopause (including natural menopause defined as lack of menses for 12 consecutive months (in absence of pregnancy) and surgical menopause defined as a woman who has had both ovaries removed); inability to swallow tablets; unwilling to refrain from alcohol during the 2‐week treatment period (and 2 additional days following completion of study medication); other condition present at enrolment that required additional antibiotic treatment; current use of any of the following medications: anticoagulants, coumarin‐ or indandione‐derivative: warfarin, cimetidine, disulfiram, seizure medications (including: phenytoin, carbamazepine, barbiturates), lithium, immunosuppressive drugs (including: cyclosporin, amprenavir), antacids, minerals or bismuth subsalicylate; any condition, in the opinion of the investigator, that would interfere with the participant's safety or with study outcomes; participation in any study involving an investigational product in the past 30 days or anticipation of participation in any study using an investigational product in the next 30 days; previous participation in this study; evidence of tubo‐ovarian abscess. Number of women randomized: 233. Number of women analyzed: 233 per ITT; group A: 117; group B: 116. Number of withdrawals/exclusions/loss to follow‐up and reasons: group A: 4 (3 physician decision, 1 incarceration); group B: 6 (3 physician decision; 3 withdrawal). Number of centres: 1. Age (range) (years): 15–40 Country: US. |
|
| Interventions |
Group A: ceftriaxone 250 mg IM single dose + doxycycline 100 mg PO twice daily for 14 days + placebo capsule PO twice daily for 14 days. Group B: ceftriaxone 250 mg IM single dose + doxycycline 100 mg PO twice daily for 14 days + metronidazole 500 mg PO twice daily for 14 days. |
|
| Outcomes |
Primary: clearance of anaerobic organisms from the endometrium at 30 days. Secondary:M genitalium detected in cervical and endometrial biopsy cultures by nucleic acid amplification tests at enrolment; M genitalium not detected in cervical and endometrial cultures by nucleic acid amplification testing at 30‐day visit among women who had M genitalium detected at either anatomical site at the enrolment visit; clinical response to treatment as improvement (reduction) of McCormack Scale total score from baseline to day 3 follow‐up visit (participants without a 3‐day measure were considered treatment failures); identification of endometrial micro‐organisms present obtained from women with or without evidence of endometritis using a combination of culture methods, ribosomal ribonucleic acid sequencing and whole genomic sequencing. |
|
| Notes |
Ethical approval: yes Informed consent: yes Source of funding: NIH Grant U19AI084024 Data derived from tabular results from ClinicalTrial.gov. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quadruple (participant, care provider, investigator, outcomes assessor). |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quadruple (participant, care provider, investigator, outcomes assessor). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 10/233 cases lost to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol found. |
| Other bias | Unclear risk | Data derived from clinicalTrial.gov, not published yet. |
CDC: Centers for Disease Control and Prevention; CRP: C‐reactive protein; ESR: erythrocyte sedimentation rate; h: hour; IM: intramuscular; ITT: intention to treat; IUD: intrauterine device; IV: intravenous; n: number of women; PID: pelvic inflammatory disease; PO: per os; PP: per protocol; SD: standard deviation; UTI: urinary tract infection; WBC: white blood cell.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Acar 1989 | Results not separate for PID. |
| Andersson 1980 | Quasi‐RCT and not randomized to doxycycline. |
| Baery 2018 | Not PID. |
| Bartlett 1982 | Not an RCT. |
| Berkeley 1986 | Results not separate for PID. |
| Blanco 1983 | Results not separate for PID. |
| Brihmer 1988 | Did not report effectiveness or safety outcomes. |
| Brihmer 1989 | Not a comparison of interest. Group A: doxycycline 200 mg IV the first day, followed by 100 mg PO daily for 10 days + benzylpenicillin‐procaine 2.25 millions IM twice daily for 2 days. Group B: trimethoprim 160 mg + sulfamethoxazole 800 mg IV twice daily the first day, followed by 800 mg PO for 10 days. |
| Brittain 2016 | Description of the trial and it does not involve PID cases, just gonorrhoea. |
| Bruhat 1986 | Not a comparison of interest. Group A: sulbactam 2 g daily IV + ampicillin 4 g daily for 5 days, followed by 15 days of sulbactam IM + ampicillin 2 g daily (n = 9). Group B: cefoxitin 6 g daily IV for 5 days, followed by 15 days of cefoxitin 2 g daily IM (n = 11). In both groups, if there was evidence of chlamydial infection, doxycycline 200 mg PO daily for 30 days given. |
| Bruhat 1989 | Not a comparison of interest. Group A: sulbactam 2 g daily IV + ampicillin 4 g daily for 5 days, followed by 15 days of sulbactam IM + ampicillin 2 g daily (n = 20). Group B: cefoxitin 6 g daily IV for 5 days, followed by 15 days of cefoxitin 2 g daily IM (n = 20). |
| Bruno 1985 | Not an RCT. |
| Cao 2017 | Not a comparison of interest. Study compared efficacy and safety of twice‐daily IV morinidazole with those of twice‐daily IV ornidazole in women with PID. Both are nitroimidazolic drugs. |
| Carty 1973 | Not antibiotic. |
| Chatwani 1997 | Not a comparison of interest. Group A: trospectomycin 500 mg IV every 8 h for ≥ 4 days of inpatient treatment and had achieved complete resolution of sign and symptoms of acute PID, followed by 10 days of doxycycline PO (n = 26). Group B: cefoxitin 2 g every 6 h + doxycycline 100 mg PO or IV for ≥ 4 days of inpatient treatment and had achieved complete resolution of sign and symptoms of acute PID, followed by 10 days of doxycycline PO (n = 13). |
| Confino 1988 | Did not report effectiveness or safety outcomes. |
| De Beer 1983 | Not a comparison of interest. Group A: ampicillin 2 g IV on admission and then 1 g IV every 4 h thereafter. If the response was good, ampicillin was administered PO after 48 h. Group B: cefoxitin 2 g IV followed by 1 g IV every 8 h. This was continued for ≥ 72 h. |
| Drasa 2010 | Results not separate for PID. |
| Drusano 1982 | Results not separate for PID. |
| Duarte 1995 | Not an RCT. |
| Faro 1988 | Not a comparison of interest. Group A: ceftizoxime 2 g IV every 8 h for ≥ 5 days (n = 18). Group B: cefotaxime 2 g IV every 8 h for ≥ 5 days (n = 19). |
| Fedele 1989 | Not PID. |
| Feng 2019 | Fuyanshu capsules are not a type of antibiotic, but a mix of Caulis Lonicerae 450 g, Caulis Sargentodoxae 450 g, Radix Glycyrrhizae 45 g, Folium Isatidis 45 g, Herba Taraxaci 135 g, Radix Paeoniae Rubra 135 g, Radix Et Rhizoma Rhei 90 g, Radix Salviae Miltiorrhizae 135 g, Rhizoma Polygoni Cuspidati 135 g, Fructus Toosendan 135 g, Rhizoma Corydalis 135 g. |
| Frongillo 1992 | Results not separate for PID. |
| Gall 1981 | Not all participants randomized. |
| Gall 1990a | Not an RCT. |
| Gall 1990b | Not a comparison of interest. Group A: clindamycin 900 mg + tobramycin 80 mg/m2 IV every 8 h for ≥ 4 days. Group B: clindamycin 900 mg + placebo IV every 8 h for ≥ 4 days. Both treatment were followed by clindamycin 450 mg PO every 6 h, to complete 14 days of treatment. |
| Gerber 1992 | Not a comparison of interest. Group A: oxytetracycline 4 × 0.5 g PO daily or doxycycline 2 × 0.1 g PO daily, initially IV + metronidazole first 2 days 2 × 0.5 g IV from day 3, 2 × 0.25 g PO daily). Group B: oxytetracycline 4 × 0.5 g PO daily or doxycycline 2 × 0.1 g PO daily, initially IV + metronidazole first 2 days 2 × 0.5 g IV from day 3, 2 × 0.25 g PO daily) + additional bathing therapy. Group C: amoxicillin‐clavulanic acid 1st + 2nd day 1.2 g daily IV, 3rd to 10th day 3 × 0.75 g PO daily. Group D: ciprofloxacin initial 2 × 0.2 g IV then to day 10 2 × 0.5 g PO daily + metronidazole 1st and 2nd day 2 × 0.5 g day IV from day 3, 2 × 0.25 g PO daily. |
| Gerstner 1990 | Results not separate for PID. |
| Ghomian 2012 | Many inconsistencies in study, author did not respond. |
| Giamarellou 1982 | Results not separate for PID. |
| Gibbs 1980 | Not a comparison of interest. Group A: penicillin G 5 × 106 units IV every 6 h + kanamycin 500 mg IM every 12 h for 4–7 days after good clinical response (n = 5). Group B: spectinomycin 500 mg IM every 12 h for 4–7 days after good clinical response (n = 7). |
| Gjonnaess 1981 | Not all participants randomized. |
| Grafford 1980 | Not a comparison of interest. Group A: bacampicillin 400 mg PO 3 times daily for 14 days (n = 39). Group B: bacampicillin 800 mg PO 3 times daily for 14 days (n = 31). |
| Grafford 1981 | Not an RCT. |
| Gunning 1986a | Not a comparison of interest. Group A: piperacillin 250 mg/kg daily IV divided into every 6 h for 5–11 days (n = 31). Group B: clindamycin 600 mg IV 6/6 h + gentamicin 1.5 mg/kg IV every 8 h for 3–8 days (n = 33). |
| Gunning 1986b | Not a comparison of interest. Group A: sulbactam 1 g + ampicillin 2 g IV every 6 h until asymptomatic and without clinical signs or pathogen sensitivity testing dictated a change in therapy (n = 21). Group B: clindamycin 600 mg IV 6/6 h + gentamicin 1.5 mg/kg IV every 8 h until asymptomatic and without clinical signs or pathogen sensitivity testing dictated a change in therapy (n = 18). |
| Hager 1989 | Not PID. |
| Harding 1982 | Not PID. |
| Harding 1984 | Not PID. |
| Hemsell 1982 | Results not separate for PID. |
| Hemsell 1987 | Not an RCT. |
| Hemsell 1988a | Authors reported data without details of clinical cure. |
| Hemsell 1988b | Results not separate for PID. |
| Hemsell 1988c | Not a comparison of interest. Group A: cefoxitin 2 g IV every 6 h + doxycycline 100 mg every 12 h for minimum of 4 days and for ≥ 48 h after defervescence, followed by doxycycline 100 mg PO when discharged from the hospital to complete 14 days of therapy (n = 32). Group B: ceftizoxime 2 g IV every 12 h + doxycycline 100 mg was given separately in 250 mL diluent and infused over 2 h for minimum of 4 days and for ≥ 48 h after defervescence, followed by doxycycline 100 mg PO when discharged from the hospital to complete 14 days of therapy (n = 30). Group C: ceftizoxime 2 g IV 3 times daily every 8 h for minimum of 4 days and for ≥ 48 h after defervescence (n = 29). Group D: ceftizoxime 2 g IV twice daily every 12 h for minimum of 4 days and for ≥ 48 h after defervescence (n = 30). |
| Hemsell 1988d | Results not separate for PID. |
| Hemsell 1990 | Not a comparison of interest. Group A: ampicillin 2 g + sulbactam 1 g IV every 6 h. Women whose treatment was successful received therapy for a mean of 4.5 (SD 0.9 days) (n = 35). Group B: cefoxitin 2 g IV every 6 h. Women whose treatment was successful received therapy for a mean of 4.5 (SD 0.9) days (n = 19). |
| Hemsell 1991 | Did not report effectiveness or safety outcomes. |
| Hemsell 1993 | Not a comparison of interest. Group A: ampicillin/sulbactam 3 g IV every 6 h on ≥ 4 consecutive days and until the woman was afebrile for ≥ 48 h. Women with Chlamydia trachomatis at study entry received doxycycline 100 mg PO twice daily for 10–14 days when discharged from hospital. Women negative for C trachomatis discharged on no PO antibiotic (n = 76). Group B: cefoxitin 2 g IV every 6 h on ≥ 4 consecutive days and until the woman was afebrile for ≥ 48 h. Women with C trachomatis at study entry received doxycycline 100 mg PO twice daily for 10–14 days when discharged from hospital. Women negative for C trachomatis discharged on no PO antibiotic (n = 41). |
| Hemsell 1997 | Not a comparison of interest. Group A: meropenem 500 mg IV given over 20–30 minutes every 8 h for ≥ 48 h, for clinical evaluation (suggested treatment duration 4–10 days, with a maximum duration of 28 days). Group B: clindamycin 900 mg IV + gentamicin 1.5 mg/kg following a loading dose of 2 mg/kg every 8 h for ≥ 48 h, for clinical evaluation (suggested treatment duration 4–10 days, with a maximum duration of 28 days). |
| Henry 1985 | Not a comparison of interest. Group A: aztreonam 1–2 g every 8–12 h. Most women received 1 g or 2 g 3 times daily. Clindamycin (usually at 600 mg every 8 h) administered concurrently with aztreonam as a means of providing coverage against gram‐positive and anaerobic organisms (n = 50; 5 with PID). Group B: gentamicin 3–5 mg/kg daily in 3 equally divided doses + clindamycin 600 mg every 8 h (n = 38; 8 with PID). In both groups, antibiotics usually administered IM or IV; however, PO administration of clindamycin was permitted. |
| Holloway 1988 | Results not separate for PID. |
| Ibrahim 1990 | Not a comparison of interest. Group A: amikacin 14 mg/kg IV infusion in 150 mL saline over 30 minutes once daily for 7–9 days. Group B: amikacin 14 mg/kg IV infusion in 150 mL saline over 30 minutes twice daily for 7–9 days. Group C: netilmicin 6.6 mg/kg IV infusion in 150 mL saline over 30 minutes once daily for 7–9 days. Group D: netilmicin 6.6 mg/kg IV infusion in 150 mL saline over 30 minutes 3 times daily for 7–9 days. All 4 groups also received tinidazole 0.8 g once daily + ampicillin 4 g daily. |
| Jemsek 1997 | Not a comparison of interest. Group A: minimum 12 doses = 3 days of ampicillin 2 g/sulbactam 1 g IV every 6 h. Group B: minimum 12 doses = 3 days of cefoxitin 2 g IV every 6 h. Doxycycline 100 mg PO or IV twice daily administered concurrently to women with cultures positive for Chlamydia trachomatis. Because of the significant possibility of false negatives, women with cultures negative for C trachomatis were empirically treated with 10–14 days of doxycycline 100 mg PO twice daily after the study ended. |
| Jordheim 1974 | Not a comparison of interest. Group A: pivampicillin 175 mg PO capsule 4 times daily for 0–4/5–9/10–14/15–19 days (n = 28). Group B: pivampicillin 350 mg PO capsule 4 times daily for 0–4/5–9/10–14/15–19 days (n = 30). In some cases, duration of therapy was longer or shorter depending on clinical response. |
| Judlin 1995 | Not a comparison of interest. Group A: ofloxacin 400 mg daily in 2 × 200 mg tablets morning and night; amoxicillin‐clavulanic acid 2 g daily, 2 × 500 mg tablets morning and night. Combination given for 3 weeks. Group B: doxycycline 200 mg daily, 1 × 100 mg tablet morning and night; amoxicillin‐clavulanic acid 2 g daily, 2 × 500 mg tablets morning and night. Combination given for 6 weeks. |
| Knuppel 1988 | Not a comparison of interest. Group A: cefotetan 2 g IV every 12 h, mean duration of therapy 6.1 days (n = 36). Group B: cefoxitin 2 g IV every 6 h or 8 h, mean duration of therapy 6.4 days (n = 17). |
| Kosseim 1991 | Not a comparison of interest. Group A: ampicillin‐sulbactam 750 mg PO twice daily for 10 days (n = 38). Group B: cefoxitin 2 g IM + probenecid 1 g PO, followed by doxycycline 100 mg twice daily for 10 days (n = 37). |
| Kotoulas 1992 | Not an RCT. |
| Kunzig 1990 | Results not separate for PID. |
| Kvile 1980 | Compared same drug with different doses. |
| Larsen 1986 | Results not separate for PID. |
| Larsen 1992 | Not a comparison of interest. Group A: imipenem‐cilastatin 500 mg IV every 6 h or 8 h. Treatment continued for ≥ 3 days or until woman was afebrile for 24–48 h (n = 44). Group B: clindamycin 900 mg IV every 8 h + gentamicin 1.5 mg/kg IV or IM for first dose, and 1 mg/kg every 8 h for succeeding doses. Treatment continued for ≥ 3 days or until the woman had been afebrile for 24–48 h (n = 50). In both treatments, if therapy for Chlamydia spp was indicated, doxycycline 100 mg PO or IV added to either regimen every 12 h. |
| Livengood 1992 | Not a comparison of interest. Group A: clindamycin 600 mg IV every 6 h + cefamandole 2 g every 6 h. Group B: clindamycin 600 mg IV every 6 h + doxycycline 100 mg + 10 mL of 4% sodium bicarbonate alternating with placebo (5% dextrose in water) every 6 h. Protocol antibiotic therapy continued for 48 h after declaration of response and for minimum of 5 days (20 doses), after which women discharge without supplemental PO antibiotic treatment. |
| Ma 2010 | Not a comparison of interest. Group A: levornidazole 0.5 g twice daily for 5–7 days. Group B: ornidazole 0.5 g twice daily for 5–7 days. |
| Maggioni 1998 | Results not separate for PID. |
| Maki 1979 | Not PID. |
| Mandell 1993 | Results not separate for PID. |
| Marier 1982 | Not a comparison of interest. Group A: piperacillin 250 mg/kg daily IV every 4–6 h. Group B: carbenicillin 450 mg/kg daily IV every 4–6 h. |
| Marshall 1982 | Not PID. |
| Matsuda 1988 | Not a comparison of interest. Group A: cefpodoxime proxetil 100 mg tablet + dummy bacampicillin placebo, twice daily. Alternately, dummy CS‐807 + dummy bacampicillin, twice daily; therefore, women took tablets 4 times daily for 7 consecutive days. Group B: bacampicillin 250 mg tablet + dummy cefpodoxime proxetil placebo, 4 times daily for 7 consecutive days. |
| Matsuda 1989 | Not a comparison of interest. Group A: ceftibuten 100 mg 3 times daily. The shape of 2 tablets (7432‐S, bacampicillin) was different, so women took 8 tablets daily (after meal and before sleep) with placebo. ≥ 3‐day administration when a primary physician found cure of the infection, or assessed no efficacy and need to change a different drug. Group B: bacampicillin 250 mg 4 times daily. The shape of 2 tablets (7432‐S, bacampicillin) was different, so women took 8 tablets daily (after meal and before sleep) with placebo. ≥ 3‐day administration when a primary physician found cure of the infection, or assessed no efficacy and need to change a different drug. |
| Moghtadaei 2008a | Risk of fraud, no reply from author. |
| Moghtadaei 2008b | Risk of fraud, no reply from author. |
| NCT04031664 | Not a comparison of interest. Group A: levofloxacin + metronidazole for 14 days, gynaecological Qianjin capsule for 28 days. Group B: levofloxacin + metronidazole for 14 days. |
| NCT04035785 | Kangfu is an anti‐inflammatory drug from traditional Chinese medicine. Not a comparison of interest. |
| Ness 2002 | Compared the same drugs as inpatient versus outpatient. |
| Ness 2005 | Not a comparison of interest. Group A: inpatient strategy cefoxitin 2 g IV every 6 h + doxycycline 100 mg IV or PO twice daily for ≥ 72 h, followed by doxycycline 100 mg PO twice daily for a total 14‐day course. Group B: outpatient treatment consisted of cefoxitin 2 g IM + probenecid 1 g PO, followed by doxycycline 100 mg PO twice daily for 14 days. |
| Nicolle 1986 | Not PID. |
| Paavonen 1985 | Did not report effectiveness or safety outcomes. |
| Pastorek 1985 | Results not separate for PID. |
| Roy 1998 | Not PID. |
| Ruiz Conde 1999 | Results not separate for PID. |
| Sanfilippo 1989 | Not a comparison of interest. Group A: mezlocillin 250 mg daily every 6 h + appropriate IV solution containing no antibiotic but identical in appearance to tobramycin solution every 8 h. Group B: aqueous crystalline penicillin G 480,000 U/kg every 6 h (maximum of 20 million units daily) + tobramycin 3 mg/kg daily every 8 h. Dose of tobramycin was then adjusted according to peak and trough blood levels to keep tobramycin levels within therapeutic range. Another physician, not directly involved with clinical management, evaluated tobramycin levels and contacted the pharmacy for changes of tobramycin levels. |
| Schnider 1979 | Not a comparison of interest. Group A: penicillin G 30 million units daily + netilmicin 2 mg/kg daily parenterally over 5 days. Group B: penicillin G 30 million units daily + gentamicin 3 mg/kg daily parenterally over 5 days. |
| Senft 1986 | Results not separate for PID. |
| Sesti 1990 | Not an RCT. |
| Sharma 2007 | Not a comparison of interest. Group A: ofloxacin 400 mg/ornidazole 500 mg/Saccharomyces boulardii (2 million spores)/lactic acid bacillus (60 million spores)/serratiopeptidase 10 mg once daily for total of 10 days (n = 98). Group B: doxycycline 100 mg twice daily + metronidazole 400 mg 3 times daily + serratiopeptidase 10 mg once daily for total of 10 days (n = 95). |
| Silva 1990 | Results not separate for PID. |
| Skerk 2003 | Compared same drug with different doses. |
| Spence 1981 | Not a comparison of interest. Group A: ampicillin 2 g IV every 4 h for minimum of 96 h followed by 0.5 g PO every 6 h to complete 10 days of treatment. Group B: doxycycline 200 mg IV initially, then 100 mg IV every 12 h for ≥ 96 h followed by 100 mg PO every 12 h to complete 10 days of treatment. |
| Stamm 1984 | Not PID. |
| Stiglmayer 1996 | Not a comparison of interest. Group A: sulbactam 1 g + ampicillin 2 g IV every 8 h. Group B: cefoxitin 2 g IV every 8 h. |
| Sweet 1988 | Not a comparison of interest. Group A: cefotetan 2 g IV every 12 h + doxycycline 100 mg IV every 12 h. Group B: cefoxitin 2 g IV every 6 h + doxycycline 100 mg IV every 12 h. Both treatments had a minimum of 4 days, ≥ for 48 h after disappearance of fever, after hospital discharge, doxycycline 100 mg PO every 12 h to complete 14 days of treatment. |
| Sweet 1994 | Results not separate for PID. |
| Takase 1986 | Not a comparison of interest. Group A: ofloxacin 1 dose 200 mg 3 times daily for 7 days. Group B: amoxicillin 1 dose 250 mg 4 times daily for 7 days. |
| Tellado 2002a | Not an RCT. |
| Tellado 2002b | Not an RCT. |
| Teppler 2002 | Not an RCT. |
| Thompson 1980 | Not a comparison of interest. Group A: aqueous penicillin G, 5 million units IV every 4 h + gentamicin 60 mg or 80 mg IV every 8 h based on weight. Group B: amoxicillin 1 g PO every 4 h. If the woman could not take oral medicines, she received ampicillin 1 g IV every 4 h, until she could be changed to PO amoxicillin. She was switched as soon as possible to ampicillin 2 g PO daily if in group A, or amoxicillin 2 g PO daily if in group B, to complete 10 consecutive days of antibiotic treatment. |
| Thompson 1985 | Not a comparison of interest. Group A: aqueous procaine penicillin G, 4.8 million units IM + probenecid 1 g PO, followed by ampicillin monohydrate 0.5 g PO 4 times daily for 10 days. Group B: tetracycline hydrochloride 1.5 g PO as a single loading dose, followed by tetracycline 0.5 g PO 4 times daily for 10 days. |
| Tulkens 1988 | Not a comparison of interest. Group A: netilmicin 6.6 mg/kg IV once daily + tinidazole 0.8 g daily (once daily) + ampicillin 4 g daily (twice daily) for mean duration of 7 days. Group B: netilmicin 2.2 mg/kg IV 3 times daily + tinidazole 0.8 g daily (once daily) + ampicillin 4 g daily (twice daily) for a mean duration of 7 days. |
| Tulkens 1991 | Not an RCT. |
| Van Gelderen 1987 | Not a comparison of interest. Group A: ceftriaxone 2 g IV once daily for 2 days followed by 1 g once daily for the next 2–8 days. Group B: penicillin G sodium 4200 mg IV + chloramphenicol 500 mg 4 times daily for 4–10 days. Additional treatment: because there was a strong suspicion that anaerobic bacteria (which were not isolated specifically) were present, 5 ceftriaxone‐treated women and 8 penicillin/chloramphenicol‐treated women also received nitroimidazole 400–500 mg every 8 h. |
| Walker 1991 | Not a comparison of interest. Group A: cefotetan 2 g IV every 12 h + doxycycline 100 mg IV every 12 h for minimum of 4 days and for ≥ 48 h after clinical response, followed by doxycycline 100 mg PO every 12 h was continued to complete a 14‐day course after the woman was discharged (n = 54). Group B: cefoxitin 2 g IV every 6 h + doxycycline 100 mg IV every 12 h for minimum of 4 days and for ≥ 48 h after clinical response, followed by doxycycline 100 mg PO every 12 h was continued to complete a 14‐day course after the woman was discharged (n = 54). |
| Wikler 1989 | Not a comparison of interest. Group A: ceftizoxime 2 g every 12 h. Group B: ceftizoxime 2 g every 8 h. Group C: ceftizoxime 2 g + doxycycline 100 mg every 12 h. Group D: cefoxitin 2 g every 6 h + doxycycline 100 mg every 12 h. Women receiving IV doxycycline continued to receive doxycycline 100 mg PO every 12 h after discharge from hospital for a total duration of 14 days (IV + PO therapy). |
| Witte 1993 | Not a comparison of interest. Group A: pefloxacin 800 mg daily + metronidazole 500 mg every 8 h. Group B: doxycycline initial dose of 200 mg followed by 100 mg daily + metronidazole 500 mg every 8 h. For both group A and B, the duration of treatment was ≥ 10 days, and maximal 14 days, unless the clinical response was considered insufficient after 5 days. The minimal duration of therapy to allow efficacy assessment was 5 days. |
| Wynd 1999 | Cost‐effectiveness study comparing ampicillin/sulbactam versus cefoxitin for the treatment of PID. |
| Zhang 2017 | Not a comparison of interest. This study uses a traditional Tibetan drug (Honghua Ruyi Wan), which has non‐inflammatory properties, compared to placebo. |
| Zou 2019 | Not a comparison of interest. 2 quinolones are compared. Group A: levofloxacin 200 mg IV twice daily for 7 days. Group B: ciprofloxacin 400 mg IV twice daily for 7 days. |
h: hour; IM: intramuscular; IV: intravenous; n: number; PID: pelvic inflammatory disease; PO: per os; RCT: randomized controlled trial.
Differences between protocol and review
For the 2017 review, we made the following changes to the protocol.
Criteria for considering studies
Types of interventions
In our protocol, we stated: "Trials comparing any antibiotics regimen compared to an alternative regimen or placebo will be eligible for inclusion."
After a long debate involving discussion with editorial board and reviewers, we decided to focus on the most clinically relevant interventions and comparisons, as identified in current clinical guidelines for treatment of PID.
Types of outcomes
The protocol listed a secondary outcome of "If the percentage of pain is available, a treatment will be considered effective when the reduction is 50% or more." However, from the clinical point of view, a reduction of pain over 50% is not relevant. For instance, if a woman with PID has an initial pain level of 10 and after treatment, the pain level was 4, this woman had a 60% reduction. However, in another case, a women with PID had an initial pain level of 5, and after treatment, her pain level was 3. In these two cases, if the 50% reduction in pain score criteria was used, the first woman would have obtained clinical cure while the second woman would not, despite the second woman having a lower pain level. Therefore, we did not perform this analysis, and used the clinical cure according to the criteria defined by the treating physician (e.g. resolution or improvement of signs and symptoms related to PID).
We amended the wording under secondary outcomes to clarify that where studies reported multiple time points, we considered the period between 14 and 28 days after initiation of treatment.
Search
In our protocol, we planned that searches would be updated within six months of publication in the review. Due to a lengthy publication process, we have extended this to 12 months.
Data collection and analysis
Data extraction and management
In our protocol, we did not plan to conduct separate analyses for differing severity of disease. However, while preparing our review, we determined that severe PID (i.e. with tubo‐ovarian abscess) is a distinct condition from mild‐moderate PID (i.e. without tubo‐ovarian abscess). Therefore, we decided to present separate analyses for these two groups.
Statistical model
The protocol planned fixed‐effect models. However, we decided to use a random‐effects model where analyses had substantial heterogeneity (I2 = 40% or greater), to present a more conservative effect estimate.
Effect measure
We stated in the protocol that we would calculate Peto odds ratios for dichotomous outcomes. However, we noted that the Cochrane Handbook for Systematic Reviews of Interventions suggests avoiding using the Peto method as a default method of analysis because it may cause bias unless events are not particularly common and there are similar numbers in the intervention and control groups (Higgins 2011). As these criteria were not fulfilled in the review, we therefore, used Mantel‐Haenszel risk ratios for all dichotomous outcomes,
Subgroup analysis
In our protocol, we planned to undertake a subgroup analysis by PID severity, but in view of our decision to present separate analyses for mild‐moderate and severe PID, the subgroup analysis was no longer appropriate.
Sensitivity analyses
In our protocol, we planned to undertake sensitivity analyses for the following factors: risk of bias, heterogeneity (I2 = 40% or greater), length of time to measurement of outcomes, and method of PID diagnosis.
In the review, we listed variables that would be used to explore heterogeneity under the heading "Investigation of heterogeneity", and we included length of time to outcome measurement and method of PID diagnosis as two of these variables.
For the sensitivity analysis by risk of bias, we added a definition of low risk of bias (which we defined as blinded, and at low risk of selection bias).
Quality assessment
We added the reporting of quality of evidence following MECIR guidelines.
Contributions of authors
RFS: co‐ordination, study design, statistical analysis and review, writing the manuscript, grading the evidence in GRADE, and final approval of the manuscript.
DGF: data collection, extraction, grading risk of bias, and final approval of the manuscript.
JM: data collection, extraction, grading risk of bias, and final approval of the manuscript.
RVD: data collection, extraction, grading risk of bias, and final approval of the manuscript.
JR: study design, writing the manuscript, grading the evidence in GRADE, and final approval of the manuscript.
Sources of support
Internal sources
No sources of support supplied
External sources
-
NIHR's 2012 Cochrane Review Incentive Scheme Award, UK
The NIHR Cochrane Review Incentive Awards are an annual scheme whereby small incentive payments (up to £10,000 maximum) are offered to Cochrane Review Groups (CRGs; www.cochrane.org/about-us/our-global-community/review-group-networks) for preparing new or updated Cochrane reviews by agreed dates.
Declarations of interest
RFS, DGF, JM and RVD certify that they do not have any affiliations with, or involvement in, any organization or entity with a direct financial interest in the subject matter of this review (e.g. employment, consultancy, stock ownership, honoraria, expert testimony). JR has received consultancy payments from Mycovia and GlaxoSmithKline and conference support from Janssen and American Society for Microbiology, has research grants pending from Gilead, Viiv and Pfizer, and owns stock options in AstraZeneca and GlaxoSmithKline.
They disclose that two of the authors (RFS and JR) had two publications used in the analysis. RFS and JR did not participate in the process for considering these studies for inclusion, data extraction, and grading for risk of bias.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Apuzzio 1989 {published data only}
- Apuzzio JJ, Stankiewicz R, Ganesh V, Jain S, Kaminski Z, Louria D. Comparison of parenteral ciprofloxacin with clindamycin-gentamicin in the treatment of pelvic infection. American Journal of Medicine 1989;87(5A):148S-51S. [DOI] [PubMed] [Google Scholar]
Arredondo 1997 {published data only}
- Arredondo JL, Diaz V, Gaitan H, Maradiegue E, Oyarzún E, Paz R, et al. Oral clindamycin and ciprofloxacin versus intramuscular ceftriaxone and oral doxycycline in the treatment of mild-to-moderate pelvic inflammatory disease in outpatients. Clinical Infectious Diseases 1997;24(2):170-8. [DOI] [PubMed] [Google Scholar]
Aşicioğlu 2013 {published data only (unpublished sought but not used)}
- Aşicioğlu O, Gungorduk K, Ozdemir A, Ertas IE, Yildirim G, Sanci M, et al. Single daily dose of moxifloxacin versus ofloxacin plus metronidazole as a new treatment approach to uncomplicated pelvic inflammatory disease: a multicentre prospective randomized trial. European Journal of Obstetrics, Gynecology, and Reproductive Biology 2013;171(1):116-21. [DOI] [PubMed] [Google Scholar]
Balbi 1996 {published data only}
- Balbi G, Piscitelli V, Di Grazia F, Martini S, Balbi C, Cardone A. Acute pelvic inflammatory disease: comparison of therapeutic protocols [Malattia infiammatoria pelvica acuta: protocolli terapeutici a confronto]. Minerva Ginecologica 1996;48(1-2):19-23. [PubMed] [Google Scholar]
Bevan 2003 {published data only}
- Bevan CD, Ridgway GL, Rothermel CD. Efficacy and safety of azithromycin as monotherapy or combined with metronidazole compared with two standard multidrug regimens for the treatment of acute pelvic inflammatory disease. Journal of International Medical Research 2003;31(1):45-54. [DOI] [PubMed] [Google Scholar]
Buisson 1989 {published data only}
- Buisson P, Mulard C, Baudet J, Bernard P, Mares P, Montero M, et al. Treatment of upper genital infections in women. Multicenter study of the comparative efficacy and tolerance of an amoxicillin-clavulanic acid combination and of a triple antibiotic combination [Étude multicentrique de l'efficacité et de la tolérance comparées de l'association amoxicilline-acide clavulanique et d'une triple association antibiotique]. Revue Francaise de Gynecologie et d'Obstetrique 1989;84(10):699-703. [PubMed] [Google Scholar]
Burchell 1987 {published data only}
- Burchell HJ, Cronje HS, De Wet JI. Efficacy of different antibiotics in the treatment of pelvic inflammatory disease. South African Medical Journal 1987;72:248-9. [PubMed] [Google Scholar]
Ciraru‐Vigneron 1986 {published data only}
- Ciraru-Vigneron N, Bercau G, Sauvanet E, Nguyen Tan Lung R, Felten A, Leaute JB, et al. The drug combination amoxicillin-clavulanic acid compared to the triple combination ampicillin-gentamicin-metronidazole in the treatment of severe adnexal infections [L'association amoxicilline-acide clavulanique comparée à la triple association ampicilline-gentamicine-métronidazole dans le traitement des infections utéro-annexielles sévères]. Pathologie Biologie 1986;34(5 Pt 2):665-8. [PubMed] [Google Scholar]
Ciraru‐Vigneron 1989 {published data only}
- Ciraru-Vigneron N, Barrier J, Becue J, Chartier M, Giraud JR, Landes P, et al. Amoxycillin/clavulanic acid ('Augmentin') compared with a combination of aminopenicillin, aminoglycoside and metronidazole in the treatment of pelvic inflammatory disease. Pharmatherapeutica 1989;5(5):312-9. [PubMed] [Google Scholar]
Crombleholme 1986 {published data only}
- Crombleholme D, Landers D, Ohm-Smith M, Robbie MO, Hadley WK, DeKay V, et al. Sulbactam/ampicillin versus metronidazole/gentamicin in the treatment of severe pelvic infections. Drugs 1986;31(Suppl 2):11-3. [DOI] [PubMed] [Google Scholar]
Crombleholme 1987 {published data only}
- Crombleholme WR, Ohm-Smith M, Robbie MO, DeKay V, Sweet RL. Ampicillin/sulbactam versus metronidazole-gentamicin in the treatment of soft tissue pelvic infections. American Journal of Obstetrics and Gynecology 1987;156(2):507-12. [DOI] [PubMed] [Google Scholar]
Crombleholme 1989 {published data only}
- Crombleholme WR, Schachter J, Ohm-Smith M, Luft J, Whidden R, Sweet RL. Efficacy of single-agent therapy for the treatment of acute pelvic inflammatory disease with ciprofloxacin. American Journal of Medicine 1989;87(Suppl 5A):142S-7S. [DOI] [PubMed] [Google Scholar]
Dean 2016 {published and unpublished data}ISRCTN51790058
- Dean G, Whetham J, Soni S, Kerr L, Greene L, Ross J, et al. Is a short course of azithromycin effective in the treatment of mild to moderate pelvic inflammatory disease (PID)? Sexually Transmitted Infections 2016;92 (Suppl):A3. [DOI: 10.1186/ISRCTN51790058] [DOI] [PubMed] [Google Scholar]
Fischbach 1994 {published data only}
- Fischbach F, Deckardt R, Graeff H. Ciprofloxacin/metronidazol vs. cefoxitin/doxycyclin: vergleich zweier therapieschemata zur behandlung der akuten pelvinen infektion. Geburtshilfe und Frauenheilkunde 1994;54:337-40. [DOI] [PubMed] [Google Scholar]
Giraud 1989 {published data only}
- Giraud JR, Chartier M, Ciraru Vigneron N, Becue J, Landes P, Leng JJ, et al. A comparison of the efficacy of and tolerance to Augmentin used alone and as one of three drugs used to treat acute upper genital tract infections. Results of a multicentre trial 152 cases [Comparaison de l'efficacite et de la tolerance de l'Augmentine en monotherapie versus triple association dans le traitment des infections genitales hautes aigues. Resultats d'une etude multicentrique portant sur 152 cas]. Contraception, Fertilite, Sexualite 1989;17(10):941-8. [Google Scholar]
Heinonen 1989 {published data only}
- Heinonen PK, Teisala K, Miettinen A, Aine R, Punnonen R, Grönroos P. A comparison of ciprofloxacin with doxycycline plus metronidazole in the treatment of acute pelvic inflammatory disease. Scandinavian Journal of Infectious Diseases. Supplementum 1989;60:66-73. [PubMed] [Google Scholar]
Hemsell 1994 {published data only}
- Hemsell DL, Little BB, Faro S, Sweet RL, Ledger WJ, Berkeley AS, et al. Comparison of three regimens recommended by the Centers for Disease Control and Prevention for the treatment of women hospitalized with acute pelvic inflammatory disease. Clinical Infectious Diseases 1994;19(4):720-7. [DOI] [PubMed] [Google Scholar]
Heystek 2009 {published data only}
- Heystek M, Ross JD, PID Study Group. A randomized double-blind comparison of moxifloxacin and doxycycline/metronidazole/ciprofloxacin in the treatment of acute, uncomplicated pelvic inflammatory disease. International Journal of STD & AIDS 2009;20(10):690-5. [DOI] [PubMed] [Google Scholar]
Hoyme 1993 {published data only}
- Hoyme UB, Ansorg R, Recklinghausen G, Schindler AE. Quinolones in the treatment of uncomplicated salpingitis: ofloxacin/metronidazole vs gentamicin/clindamycin [Chinolone in der therapie der unkoplizierten salpingitis: ofloxacin/metronidazol vs gentamicin/clindamicin]. Infektionen in der Gynäcologie und geburtshilfe 1993;VII.8a:607-8. [Google Scholar]
Judlin 2010b {published data only}
- Judlin P, Liao Q, Liu Z, Reimnitz P, Hampel B, Arvis P. Efficacy and safety of moxifloxacin in uncomplicated pelvic inflammatory disease: the MONALISA study. BJOG 2010;117:1475-84. [DOI] [PubMed] [Google Scholar]
Landers 1991 {published data only}
- Landers DV, Wolner-Hanssen P, Paavonen J, Thorpe E, Kiviat N, Ohm-Smith M, et al. Combination antimicrobial therapy in the treatment of acute pelvic inflammatory disease. American Journal of Obstetrics and Gynecology 1991;164(3):849-58. [DOI] [PubMed] [Google Scholar]
Leboeuf 1987 {published data only}
- Leboeuf D, Rousset D, Cacault JA, Engelman P. Prospective randomized trial comparing the efficacy and the tolerance of clindamycin-gentamicin versus metronidazole-gentamicin in acute utero-adnexal infections in hospitalized patients [Essai prospectif randomise comparant l'efficacite et la tolerance de la clindamycine-gentamycine versus metronidazole-gentamycine dans les infections utero-annexielles aigues chez des patientes hospitalisees]. Revue Francaise de Gynecologie et d'Obstetrique 1987;82(1):9-15. [PubMed] [Google Scholar]
Malhotra 2003 {published data only}
- Malhotra M, Sharma JB, Batra S, Arora R, Sharma S. Ciprofloxacin-tinidazole combination, fluconazole-azithromycin-secnidazole-kit and doxycycline-metronidazole combination therapy in syndromic management of pelvic inflammatory disease: a prospective randomized controlled trial. Indian Journal of Medical Sciences 2003;57(12):549-55. [PubMed] [Google Scholar]
Maria 1992 {published data only}
- Maria B, Dublanchet A, Strecker J, Dennemark N, Genazzani A, Fioretti P, et al. Comparative evaluation of clindamycin/gentamicin and cefoxitin/doxycycline for treatment of pelvic inflammatory disease: a multi-center trial. Acta Obstetricia et Gynecologica Scandinavica 1992;71(2):129-34. [DOI] [PubMed] [Google Scholar]
Martens 1990 {published data only}
- Martens MG, Faro S, Hammill H, Maccato M, Riddle GD, LaPread E. Comparison of cefotaxime, cefoxitin and clindamycin plus gentamicin in the treatment of uncomplicated and complicated pelvic inflammatory disease. Journal of Antimicrobial Chemotherapy 1990;26(Suppl A):37-43. [DOI] [PubMed] [Google Scholar]
Martens 1993 {published data only}
- Martens MG, Gordon S, Yarborough DR, Faro S, Binder D, Berkeley A, Ambulatory PID Research Group. Multicenter randomized trial of ofloxacin versus cefoxitin and doxycycline in outpatient treatment of pelvic inflammatory disease. Southern Medical Journal 1993;86(6):604-10. [DOI] [PubMed] [Google Scholar]
Okada 1988 {published data only}
- Okada H, Yamamoto T, Yasuda J, Kanao M, Shimizu T, Yorozu Y, et al. Comparative clinical study on ciprofloxacin and cefroxadine in the treatment of infections in obstetrics and gynecology [in Japanese]. Chemotherapy 1988;36(11):821-57. [Google Scholar]
Ross 2006 {published data only}
- Ross JD, Cronjé HS, Paszkowski T, Rakoczi I, Vildaite D, Kureishi A, et al, MAIDEN Study Group. Moxifloxacin versus ofloxacin plus metronidazole in uncomplicated pelvic inflammatory disease: results of a multicentre, double blind, randomised trial. Sexually Transmitted Infections 2006;82(6):446-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Roy 1985 {published data only}
- Roy S, Wilkins J. Cefotaxime in the treatment of female pelvic soft tissue infections. Infection 1985;13(Suppl 1):S56-61. [DOI] [PubMed] [Google Scholar]
Roy 1990 {published data only}
- Roy S, Wilkins J, March CM, Solera NC, Galvan NI, Ressler RL, et al. A comparison of the efficacy and safety of ceftizoxime with doxycycline versus conventional CDC therapies in the treatment of upper genital tract infection with or without a mass. Clinical Therapeutics 1990;12(Suppl C):53-73. [PubMed] [Google Scholar]
Savaris 2007 {published data only}46117662
- Savaris RF, Teixeira LM, Torre TG, Edelweiss MIA, Moncada J, Schachter J. Comparing ceftriaxone plus azithromycin or doxycycline for pelvic inflammatory disease: a randomized controlled trial. Obstetrics and Gynecology 2007;110(1):53-60. [DOI] [PubMed] [Google Scholar]
Sirayapiwat 2002 {published data only}
- Sirayapiwat P, Chaithongwongwatthana S, Tirawatnapong S. Triple therapies versus clindamycin plus gentamicin in the treatment of acute pelvic inflammatory disease: a randomized controlled trial. Thai Journal of Obstetrics and Gynaecology 2002;14:215-21. [Google Scholar]
Soper 1988 {published data only}
- Soper DE, Despres B. A comparison of two antibiotic regiments for treatment of pelvic inflammatory disease. Obstetrics and Gynecology 1988;72(7):7-12. [PubMed] [Google Scholar]
Sweet 1985 {published data only}
- Sweet RL, Ohm-Smith M, Landers DV, Robbie MO. Moxalactam versus clindamycin plus tobramycin in the treatment of obstetric and gynecologic infections. American Journal of Obstetrics and Gynecology 1985;152:808-17. [DOI] [PubMed] [Google Scholar]
Thadepalli 1991 {published data only}
- Thadepalli H, Mathai D, Scottie R, Bansal MB, Savage E. Ciprofloxacin monotherapy for acute pelvic infections: a comparison with clindamycin plus gentamicin. Obstetrics and Gynaecology 1991;78(4):696-701. [PubMed] [Google Scholar]
Tison 1988 {published data only}
- Tison E, Marpeau L, Pigné A, Tessier F, Barrat J. Treatment of acute non-chlamydial salpingitis. Study of the efficacy and tolerance of a single-therapy antibiotic: Augmentin [Traitement des salpingites aiguës non chlamydiennes. Etude de l'efficacité et de la tolérance d'un antibiotique en monothérapie: l'Augmentin]. Journal de Gynecologie, Obstetrique et Biologie de la Reproduction 1988;17(4):513-9. [PubMed] [Google Scholar]
Walters 1990 {published data only}
- Walters MD, Gibbs RS. A randomized comparison of gentamicin-clindamycin and cefoxitin-doxycycline in the treatment of acute pelvic inflammatory disease. Obstetrics and Gynecology 1990;75(5):867-72. [PubMed] [Google Scholar]
Wendel 1991 {published data only}
- Wendel GD Jr, Cox SM, Bawdon RE, Theriot SK, Heard MC, Nobles BJ. A randomized trial of ofloxacin versus cefoxitin and doxycycline in the outpatient treatment of acute salpingitis. American Journal of Obstetrics and Gynecology 1991;164(5 Pt 2):1390-6. [DOI] [PubMed] [Google Scholar]
Wiesenfeld 2017 {unpublished data only}
- Wiesenfeld H, Hillier S, Meyn L, Rabe L, Macio I, Priest C, et al. Impact of metronidazole on clearance of anaerobes in women with acute pelvic inflammatory disease: the ACE trial. American Journal of Obstetrics and Gynecology 2017;217(6):714. [DOI: ] [Google Scholar]
References to studies excluded from this review
Acar 1989 {published data only}
- Acar B, Zissis NP. Piperacillin alone vs triple antibiotic combination in gynecological infections. Journal of Chemotherapy 1989;1(6):403-6. [DOI] [PubMed] [Google Scholar]
Andersson 1980 {published data only}
- Andersson PO, Hackl H, Jensen P, Larsen KR. A comparison of two different dosages of pivampicillin and doxycycline in patients with gynaecological infections. Current Medical Research and Opinion 1980;6(8):513-7. [DOI] [PubMed] [Google Scholar]
Baery 2018 {published data only}
- Baery N, Ghasemi Nejad A, Amin M, Mahroozade S, Mokaberinejad R, Bioos S, et al. Effect of vaginal suppository on bacterial vaginitis based on Persian medicine (Iranian traditional medicine): a randomised double blind clinical study. Journal of Obstetrics and Gynaecology 2018;38(8):1110-4. [DOI: 10.1080/01443615.2018.1445706] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bartlett 1982 {published data only}
- Bartlett JG. Therapeutic trial of moxalactam in intra-abdominal sepsis and gynaecological infections. Drugs under Experimental and Clinical Research 1982;VIII(5):483-6. [Google Scholar]
Berkeley 1986 {published data only}
- Berkeley AS, Freedman KS, Hirsch JC, Ledger WJ. Randomized, comparative trial of imipenem/cilastatin and moxalactam in the treatment of serious obstetric and gynecologic infections. Surgery, Gynecology & Obstetrics 1986;162(3):204-8. [PubMed] [Google Scholar]
Blanco 1983 {published data only}
- Blanco JD, Gibbs RS, Duff P, Castaneda YS, St Clair PJ. Randomized comparison of ceftazidime versus clindamycin-tobramycin in the treatment of obstetrical and gynecological infections. Antimicrobial Agents and Chemotherapy 1983;24(4):500-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brihmer 1988 {published data only}
- Brihmer C, Brundin J. Second look laparoscopy after treatment of acute salpingitis with doxycycline/benzylpenicillin procaine or trimethoprim-sulfamethoxazole. Scandinavian Journal of Infectious Diseases 1988;53:63-9. [PubMed] [Google Scholar]
Brihmer 1989 {published data only}
- Brihmer C, Kallings I, Nord CE, Brundin J. Second look laparoscopy; evaluation of two different antibiotic regimens after treatment of acute salpingitis. European Journal of Obstetrics & Gynecology 1989;30(3):263-74. [DOI] [PubMed] [Google Scholar]
Brittain 2016 {published data only}
- Brittain C, Childs M, Duley L, Harding J, Hepburn T, Meakin G, et al. Gentamicin versus ceftriaxone for the treatment of gonorrhoea (G-TOG trial): study protocol for a randomised trial. Trials 2016;17(1):558. [DOI: 10.1186/s13063-016-1683-8] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bruhat 1986 {published data only}
- Bruhat MA, Pouly JL, Le Boedec G, Mage G. Treatment of acute salpingitis with sulbactam/ampicillin. Drugs 1986;31 Suppl(2):7-10. [DOI] [PubMed] [Google Scholar]
Bruhat 1989 {published data only}
- Bruhat MA, Le Bouedec G, Pouly JL, Mage G, Canis M. Treatment of acute salpingitis with sulbactam/ampicillin. International Journal of Gynecology & Obstetrics 1989;31 Suppl(2):41-6. [DOI] [PubMed] [Google Scholar]
Bruno 1985 {published data only}
- Bruno V, Lombardo M, Schimberni M, Torregrossa G, Pepe C, Carenza L. A clinical trial with the new antibiotic combination piperacillin/flucloxacillin used on gynaecological postoperative infections. Current Therapeutic Research 1985;38(3):465-73. [Google Scholar]
Cao 2017 {published data only}
- Cao C, Luo A, Wu P, Weng D, Zheng H, Wang S. Efficacy and safety of morinidazole in pelvic inflammatory disease: results of a multicenter, double-blind, randomized trial. European Journal of Clinical Microbiology & Infectious Diseases 2017;36:1225-30. [DOI: 10.1007/s10096-017-2913-z] [PMID: ] [DOI] [PubMed] [Google Scholar]
Carty 1973 {published data only}
- Carty MJ. The use of oxyphenbutazone ('Tanderil') in acute pelvic inflammatory disease. Current Medical Research and Opinion 1973;1(4):203-4. [DOI] [PubMed] [Google Scholar]
Chatwani 1997 {published data only}
- Chatwani A, Dandalou V, Harmanli O, Nyirjesy P. Trospectomycin in acute pelvic inflammatory disease: a preliminary report. Infectious Diseases in Obstetrics and Gynecology 1997;5(3):215-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Confino 1988 {published data only}
- Confino E, Friberg J, Vermesh M, Madanes A, Suarez M, Gleicher N. Mezlocillin versus doxycycline in the treatment of acute salpingitis. Mount Sinai Journal of Medicine 1988;55(2):154-8. [PubMed] [Google Scholar]
De Beer 1983 {published data only}
- De Beer JA, Van den Ende J, Odendaal HJ. Efficacy of ampicillin and cefoxitin in the treatment of acute pelvic inflammatory disease. A comparative study. South African Medical Journal 1983;64:733-5. [PubMed] [Google Scholar]
Drasa 2010 {published data only}
- Drasa K, Koci E. Azithromycin vs. clarithromycin and both combination in treatment of mycoplasma genitalium. European Urology Supplements 2010;9(2):172. [Google Scholar]
Drusano 1982 {published data only}
- Drusano GL, Warren JW, Saah AJ, Caplan ES, Tenney JH, Hansen S, et al. A prospective randomized controlled trial of cefoxitin versus clindamycin-aminoglycoside in mixed anaerobic-aerobic infections. Surgery, Gynecology & Obstetrics 1982;154(5):715-20. [PubMed] [Google Scholar]
Duarte 1995 {published data only}
- Duarte G, Quintana SM, Gir E, Marana HR, Cunha SP. Evaluation of doxycycline for the complementary treatment of acute inflammatory pelvic disease. A double-blind study [Avaliação da doxiciclina como tratamento complementar da doença inflamatória pélvica aguda – Estudo duplo-cego]. Revista Brasileira de Medicina do Esporte 1995;52(6):651-6. [Google Scholar]
Faro 1988 {published data only}
- Faro S, Martens MG, Phillips LE, Lapread E, Riddle GD, Turner RM. Ceftizoxime versus cefotaxime in the treatment of hospitalized patients with pelvic inflammatory disease. Current Therapeutic Research 1988;43(3):349-54. [Google Scholar]
Fedele 1989 {published data only}
- Fedele L, Acaia B, Marchini M, Grassi R, Benzi-Cipelli R, Bonino S. Treatment of Chlamydia trachomatis endometritis with josamycin. Journal of Chemotherapy 1989;1(4 Suppl):911-2. [PubMed] [Google Scholar]
Feng 2019 {published data only}
- Feng XL, Jiang S, Chen J, Liu X, Zhang Y, Chen L. Effect of Fuyanshu capsules combined with antibiotics on inflammatory factors in patients with pelvic inflammatory disease. Zhongguo Zhong Yao za Zhi [China Journal of Chinese Materia Medica] 2019;44(12):2637-43. [DOI] [PubMed] [Google Scholar]
Frongillo 1992 {published data only}
- Frongillo RF, Custo GM, Gilardi G, Martella L, Palumbo M. Imipenem versus netilmicin plus chloramphenicol in gynecological upper tract infections: a comparative study. Chemotherapy 1992;5(1):41-4. [Google Scholar]
Gall 1981 {published data only}
- Gall SA, Kohan AP, Ayers OM, Hughes CE, Addison WA, Hill GB. Intravenous metronidazole or clindamycin with tobramycin for therapy of pelvic infections. Obstetrics & Gynecology 1981;57(1):51-8. [PubMed] [Google Scholar]
Gall 1990a {published data only}
- Gall S. Therapeutic dilemmas in the treatment of pelvic infections. Journal of Reproductive Medicine 1990;35(11 Suppl):1091-4. [PubMed] [Google Scholar]
Gall 1990b {published data only}
- Gall SA, Constantine L. Comparative evaluation of clindamycin versus clindamycin plus tobramycin in the treatment of acute pelvic inflammatory disease. Obstetrics & Gynecology 1990;75(2):282-6. [PubMed] [Google Scholar]
Gerber 1992 {published data only}
- Gerber B, Wilken H, Zacharias K, Barten G, Splitt G. Treatment of acute salpingitis with tetracycline/metronidazole with or without additional balneotherapy. Augmentan or ciprofloxacin/metronidazole: a second-look-laparoscopy study [Zur Behandlung der akuten Salpingitis mit Tetracyclin/Metronidazol mit oder ohne zusätzliche Heilbadkur, Augmentan oder Ciprofloxacin/Metronidazol: Eine second look-Laparoskopie-Studie]. Geburtshilfe und Frauenheilkunde 1992;52:165-70. [DOI] [PubMed] [Google Scholar]
Gerstner 1990 {published data only}
- Gerstner GJ. Comparison of ceftriaxone (1 x 1 g/day) versus cefotaxime (3 x 1 g/day) for gynecologic and obstetric infections. A randomized clinical trial. Gynecologic and Obstetric Investigation 1990;29(4):273-7. [DOI] [PubMed] [Google Scholar]
Ghomian 2012 {published data only}
- Ghomian N, HafiziI L, Tavassoli F, Ahrari RT. Comparing ceftriaxone plus azithromycin or doxycycline for outpatient treatment in pelvic inflammatory disease [مقايسه سفترياكسون و آزيترومايسين با سفترياكسون و داكسي سيكلين در درمان سرپايي بيماري التهابي لگن]. Iranian Journal of Obstetrics, Gynecology and Infertility 2012;14(8):1-8. [Google Scholar]
Giamarellou 1982 {published data only}
- Giamarellou H, Volanaki M, Avlami A, Tsatsiadis K, Petrochilos E, Daikos GK. Ornidazole versus clindamycin: comparative evaluation in the treatment of 140 serious anaerobic infections. Chemotherapy 1982;28(6):502-11. [DOI] [PubMed] [Google Scholar]
Gibbs 1980 {published data only}
- Gibbs RS. A trial of spectinomycin hydrochloride compared with aqueous penicillin G plus kanamycin for treatment of severe pelvic inflammatory disease. Sexually Transmitted Diseases 1980;7(1):21-3. [DOI] [PubMed] [Google Scholar]
Gjonnaess 1981 {published data only}
- Gjonnaess H, Dalaker K, Urnes A, Norling B, Kville G, Mardh P, et al. Treatment of pelvic inflammatory disease. Effects of lymecycline and clindamycin. Current Therapeutic Research 1981;29(6):885-92. [Google Scholar]
Grafford 1980 {published data only}
- Grafford K, Guttorm E, Kristensen GB, Philipson T, Selnes A. Bacampicillin in the treatment of pelvic inflammatory disease: a study of two dosage regimens. Infection 1980;8(6):290-2. [Google Scholar]
Grafford 1981 {published data only}
- Grafford K, Nilsson BS. Twice daily dosage of bacampicillin: a summary of clinical documentation. Journal of Antimicrobial Chemotherapy 1981;8(Suppl C):119-27. [DOI] [PubMed] [Google Scholar]
Gunning 1986a {published data only}
- Gunning JE. A comparison of piperacillin and clindamycin plus gentamicin in women with pelvic infections. Surgery, Gynecology & Obstetrics 1986;163:156-62. [PubMed] [Google Scholar]
Gunning 1986b {published data only}
- Gunning J. A comparison of parenteral sulbactam/ampicillin versus clindamycin/gentamicin in the treatment of pelvic inflammatory disease. Drugs 1986;31(Suppl 2):14-7. [DOI] [PubMed] [Google Scholar]
Hager 1989 {published data only}
- Hager WD, Pascuzzi M, Vernon M. Efficacy of oral antibiotics following parenteral antibiotics for serious infections in obstetrics and gynecology. Obstetrics & Gynecology 1989;73(3 Pt 1):326-29. [PubMed] [Google Scholar]
Harding 1982 {published data only}
- Harding G, Vincelette J, Rachlis A, Fong I, Mandell L, Feld R, et al. A preliminary report on the use of ceftizoxime versus clindamycin/tobramycin for the therapy of intra-abdominal and pelvic infections. Journal of Antimicrobial Chemotherapy 1982;10(Suppl C):191-2. [DOI] [PubMed] [Google Scholar]
Harding 1984 {published data only}
- Harding GK, Nicolle LE, Haase DA, Aoki FY, Stiver HG, Blanchard RJ, et al. Prospective, randomized, comparative trials in the therapy for intraabdominal and female genital tract infections. Reviews of Infectious Diseases 1984;6(Suppl 1):S283-92. [DOI] [PubMed] [Google Scholar]
Hemsell 1982 {published data only}
- Hemsell DL, Cunningham FG, Nolan CM, Miller TT. Clinical experience with cefotaxime in obstetric and gynecologic infections. Reviews of Infectious Diseases 1982;4(Suppl):S432-8. [DOI] [PubMed] [Google Scholar]
Hemsell 1987 {published data only}
- Hemsell DL, Hemsell PG, Heard MC, Nobles BJ. Piperacillin and a combination of clindamycin and gentamicin for the treatment of hospital and community acquired acute pelvic infections including pelvic abscess. Surgery, Gynecology & Obstetrics 1987;165(3):223-9. [PubMed] [Google Scholar]
Hemsell 1988a {published data only}
- Hemsell DL, Heard MC, Hemsell PG, Nobles BJ. Sulbactam/ampicillin versus cefoxitin for uncomplicated and complicated acute pelvic inflammatory disease. Drugs 1988;35(Suppl 7):39-42. [DOI] [PubMed] [Google Scholar]
Hemsell 1988b {published data only}
- Hemsell DL, Wendel GD, Gall SA, Newton ER, Gibbs RS, Knuppel RA, et al. Multicenter comparison of cefotetan and cefoxitin in the treatment of acute obstetric and gynecologic infections. American Journal of Obstetrics & Gynecology 1988;158(3 pt 2):722-77. [DOI] [PubMed] [Google Scholar]
Hemsell 1988c {published data only}
- Hemsell DL, Nobles BJ, Heard MC, Hemsell PG. Upper and lower reproductive tract bacteria in 126 women with acute pelvic inflammatory disease. Microbial susceptibility and clinical response to four therapeutic regimens. Journal of Reproductive Medicine 1988;33(10):799-805. [PubMed] [Google Scholar]
Hemsell 1988d {published data only}
- Hemsell DL, Heard MC, Hemsell PG, Nobles BJ. Sulbactam/ampicillin versus cefoxitin for uncomplicated and complicated acute pelvic inflammatory disease. Drugs 1988;35(Suppl 7):39-42. [DOI] [PubMed] [Google Scholar]
Hemsell 1990 {published data only}
- Hemsell DL, Bawdon RE, Hemsell PG, Nobles BJ, Heard MC. Single-agent therapy for acute pelvic inflammatory disease: sulbactam/ampicillin versus cefoxitin. Journal of International Medical Research 1990;18(Suppl 4):85D-9D. [PubMed] [Google Scholar]
Hemsell 1991 {published data only}
- Hemsell DL, Heard MC, Nobles BJ. Comparative bacteriology of parenteral single-agent vs. combination therapy in salpingitis. Advances in Therapy 1991;8(1):27-35. [Google Scholar]
Hemsell 1993 {published data only}
- Hemsell DL, Wendel GD, Hemsell PG, Heard ML, Nobles BJ. Inpatient treatment for uncomplicated and complicated acute pelvic inflammatory disease: ampicillin/sulbactam vs. cefoxitin. Infectious Diseases in Obstetrics and Gynecology 1993;1(3):123-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hemsell 1997 {published data only}
- Hemsell DL, Martens MG, Faro S, Gall S, McGregor JA. A multicenter study comparing intravenous meropenem with clindamycin plus gentamicin for the treatment of acute gynecologic and obstetric pelvic infections in hospitalized women. Clinical Infectious Diseases 1997;24(Suppl 2):S222-30. [DOI] [PubMed] [Google Scholar]
Henry 1985 {published data only}
- Henry SA. Overall clinical experience with aztreonam in the treatment of obstetric-gynecologic infections. Reviews of Infectious Diseases 1985;7(Suppl 4):S703-8. [DOI] [PubMed] [Google Scholar]
Holloway 1988 {published data only}
- Holloway WJ. Infection in women. Clinical experience with beta-lactamase inhibitors. Journal of Reproductive Medicine 1988;33(6 Suppl):595-7. [PubMed] [Google Scholar]
Ibrahim 1990 {published data only}
- Ibrahim S, Derde MP, Kaufman L, Clerckx-Braun F, Jacqmin P, Brulein V, et al. Safety, pharmacokinetics and efficacy of once-a-day netilmicin and amikacin versus their conventional schedules in patients suffering from pelvic inflammatory disease. Renal Failure 1990;12(3):199-203. [DOI] [PubMed] [Google Scholar]
Jemsek 1997 {published data only}
- Jemsek JG, Harrison F. Ampicillin/sulbactam vs. cefoxitin for the treatment of pelvic inflammatory disease. Infectious Diseases in Obstetrics and Gynecology 1997;5(5):319-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jordheim 1974 {published data only}
- Jordheim O. Pivampicillin treatment of urogenital infections in gynaecological patients. Clinical evaluation. Infection 1974;2(3):142-4. [DOI] [PubMed] [Google Scholar]
Judlin 1995 {published data only}
- Judlin P, Koebele A, Zaccabri A, Walleghen E, Pavis A, Badonnel Y, et al. Comparative study of ofloxacin+amoxicillin-clavulanic acid versus doxycycline+amoxicillin-clavulanic acid combination in the treatment of pelvic Chlamydia trachomatis infections [Etude comparative des associations ofloxacine+amoxicilline-acide clavulanique versus doxycycline+amoxicilline-acide clavulanique dans le traitment des infections génitales hautes à Chlamydia Trachomatis]. Journal de Gynecologie Obstetrique et Biologie de la Reproduction 1995;24(3):253-9. [PubMed] [Google Scholar]
Knuppel 1988 {published data only}
- Knuppel RA, O'Bryan D, Lake M. Cefotetan: comparative and non comparative studies in obstetric and gynecologic infections. Southern Medical Journal 1988;81(2):185-8. [PubMed] [Google Scholar]
Kosseim 1991 {published data only}
- Kosseim M, Rondald A, Plummer FA, D'Costa L, Brunham RC. Treatment of acute pelvic inflammatory disease in the ambulatory setting: trial of cefoxitin and doxycycline versus ampicillin-sulbactam. Antimicrobial Agents and Chemotherapy 1991;35(8):1651-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kotoulas 1992 {published data only}
- Kotoulas IG, Cardamakis E, Michopoulos J, Chronis G, Antoniou S. Comparison of ceftriaxone plus ornidazole, ceftazidime plus ornidazole, and ornidazole in the treatment of pelvic inflammatory disease (PID). Chemotherapy 1992;5(3):159-64. [Google Scholar]
Kunzig 1990 {published data only}
- Kunzig HJ, Petersen EE, Hoyme UB, Martius J, Busch W. Sequential therapy with ciprofloxacin i.v./p.o. and metronidazole compared with cefotiam and metronidazole in the treatment of gynecological infections. Chemotherapy 1990;3(4):225-8. [Google Scholar]
Kvile 1980 {published data only}
- Kvile G, Langeland P, Norling B. Treatment of salpingitis with pivampicillin. A comparison of twice-daily and thrice-daily dosages. Infection 1980;8(1):32-6. [DOI] [PubMed] [Google Scholar]
Larsen 1986 {published data only}
- Larsen JW Jr, Voise CT, Grossman JH 3rd. Comparison of cefoxitin and clindamycin-gentamicin for pelvic infections. Clinical Therapeutics 1986;9(1):77-83. [PubMed] [Google Scholar]
Larsen 1992 {published data only}
- Larsen JW, Gabel-Hughes K, Kreter B. Efficacy and tolerability of imipenem-cilastatin versus clindamycin+gentamicin for serious pelvic infections. Clinical Therapeutics 1992;14(1):90-6. [PubMed] [Google Scholar]
Livengood 1992 {published data only}
- Livengood CH 3rd, Hill GB, Addison WA. Pelvic inflammatory disease: findings during inpatient treatment of clinically severe, laparoscopy-documented disease. American Journal of Obstetrics and Gynecology 1992;166(2):519-24. [DOI] [PubMed] [Google Scholar]
Ma 2010 {published data only}
- Ma L, Zhang YZ, Zheng YL, Wang ZH, Xu YD, Kong LN. Multicenter randomized controlled clinical study on levornidazole and sodium chloride injection in the treatment of pelvic anaerobic infections [in Chinese]. Chinese Journal of Obstetrics & Gynecology 2010;45(10):754-6. [PubMed] [Google Scholar]
Maggioni 1998 {published data only}
- Maggioni P, Di Stefano F, Facchini V, Irato S, Mancuso S, Colombo M, et al. Treatment of obstetric and gynecologic infections with meropenem: comparison with imipenem/cilastatin. Journal of Chemotherapy 1998;10(2):114-21. [DOI] [PubMed] [Google Scholar]
Maki 1979 {published data only}
- Maki DG, Craig WA, Agger WA. A comparative clinical trial of sisomicin and gentamicin in major gram-negative infections. Infection 1979;7(Suppl 3):S298-300. [Google Scholar]
Mandell 1993 {published data only}
- Mandell LA, Turgeon PL, Ronalds AR, Canadian Clinical Trials Group. A prospective randomized trial of imipenem-cilastatin versus clindamycin/tobramycin in the treatment of intra-abdominal and pelvic infections. Canadian Journal of Infectious Diseases 1993;4(5):279-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
Marier 1982 {published data only}
- Marier RL, Sanders CV, Faro S, Janney A, Williams WW, Derks F, et al. Piperacillin v carbenicillin in the therapy for serious infections. Archives of Internal Medicine 1982;142(11):2000-5. [PubMed] [Google Scholar]
Marshall 1982 {published data only}
- Marshall JR, Chow AW, Sorrell TC. Effectiveness of mezlocillin in female genital tract infections. Journal of Antimicrobial Chemotherapy 1982;9(Suppl A):149-58. [DOI] [PubMed] [Google Scholar]
Matsuda 1988 {published data only}
- Matsuda S, Suzuki M, Shimizu T, Ishikawa M, Haga H, Mizoguchi H, et al. Comparative clinical study of CS-807 (cefpodoxime proxetil) and bacampicillin (BAPC) on the infectious disease in the field of obstetrics and gynecology [in Japanese]. Rinsho Iyaku (Journal of Clinical Therapeutics and Medicines) 1988;4(9):1641-85. [Google Scholar]
Matsuda 1989 {published data only}
- Matsuda S, Shimizu T, Maki M, Chimura T, Yajima A, Takahashi K, et al. Comparative double-blind clinical trial of ceftibuten (7432-S) and bacampicillin (BAPC) against gynecological infections [in Japanese]. Chemotherapy 1989;37(Suppl 1):667-700. [Google Scholar]
Moghtadaei 2008a {published data only}
- Moghtadaei P, Sardari F, Esmaeilian S. Comparison of ceftriaxone plus weekly azithromycin or daily ofloxacin for outpatient treatment of pelvic inflammatory disease: a randomized clinical trial. Journal of Family and Reproductive Health 2008;2(2):87-93. [Google Scholar]
Moghtadaei 2008b {published data only}
- Moghtadaei P, Sardari F, Esmaeilian S. Comparison of ceftriaxone plus weekly azithromycin or daily ofloxacin for outpatient treatment of pelvic inflammatory disease: a randomized clinical trial. Journal of Family and Reproductive Health 2008;2(2):87-93. [Google Scholar]
NCT04031664 {unpublished data only}
- NCT04031664. A clinical study on Qianjin capsule of gynaecology combined with antibiotics for pelvic inflammatory diseases (damp-heat stasis and Qi deficiency syndrome). clinicaltrials.gov/ct2/show/NCT04031664 2019.
NCT04035785 {published data only}
- NCT04035785. A clinical study on Kangfu anti-inflammatory suppository of gynaecology combined with antibiotics for pelvic inflammatory diseases (evidence of dampness and heat accumulation): a randomized, double blind, parallel Control of positive drugs, multi-center clinical study. clinicaltrials.gov/ct2/show/study/NCT04035785.
Ness 2002 {published data only}
- Ness RB, Soper DE, Holley RL, Peipert J, Randall H, Sweet RL, et al. Effectiveness of inpatient and outpatient treatment strategies for women with pelvic inflammatory disease: results from the Pelvic Inflammatory Disease Evaluation and Clinical Health (PEACH) randomized trial. American Journal of Obstetric and Gynecology 2002;186(5):929-37. [PMID: ] [DOI] [PubMed] [Google Scholar]
Ness 2005 {published data only}
- Ness RB, Trautmann G, Richter HE, Randall H, Peipert JF, Nelson DB, et al. Effectiveness of treatment strategies of some women with pelvic inflammatory disease a randomized trial. Obstetrics and Gynaecology 2005;106(3):573-80. [DOI] [PubMed] [Google Scholar]
Nicolle 1986 {published data only}
- Nicolle LE, Harding GK, Louie TJ, Thomson MJ, Blanchard RJ. Cefoxitin plus tobramycin and clindamycin plus tobramycin. A prospective randomized comparison in the therapy of mixed aerobic/anaerobic infections. Archives of Surgery 1986;121(8):891-6. [DOI] [PubMed] [Google Scholar]
Paavonen 1985 {published data only}
- Paavonen J, Vesterinen E, Aantaa K, Räsänen J. Factors predicting abnormal hysterosalpingographic findings in patients treated for acute pelvic inflammatory disease. International Journal of Gynaecology and Obstetrics 1985;23(3):171-5. [DOI] [PubMed] [Google Scholar]
Pastorek 1985 {published data only}
- Pastorek JG Jr, Aldridge KE, Cunningham GL, Faro S, Graffeo S, McNeeley GS, et al. Comparison of ticarcillin plus clavulanic acid with cefoxitin in the treatment of female pelvic infection. American Journal of Medicine 1985;29(79):161-3. [DOI] [PubMed] [Google Scholar]
Roy 1998 {published data only}
- Roy S, Koltun W, Chatwani A, Martens MG, Dittrich R, Luke DR. Treatment of acute gynecologic infections with trovafloxacin. Trovafloxacin Surgical Group. American Journal of Surgery 1998;178(6A Suppl):67S-73S. [DOI] [PubMed] [Google Scholar]
Ruiz Conde 1999 {published data only}
- Ruiz Conde MA, Grupo de Estudio Multicêntrico. Comparative multicenter study between meropenem versus clindamycin with gentamicin for the treatment of inpatient with obstetrics and/or gynecologic infections [Estudio multicéntrico comparativo entre meropenem y la asociación clindamicina-gentamicina en el tratamentiento de infecciones obstétricas y/o ginecológicas en pacientes hospitalizadas]. Clinica e Investigacion en Ginecologia y Obstetricia 1999;26(5):202-7. [Google Scholar]
Sanfilippo 1989 {published data only}
- Sanfilippo JS, Schikler KN. Mezlocillin versus penicillin and tobramycin in adolescent pelvic inflammatory disease: a prospective study. Internal Pediatrics 1989;4:53-6. [Google Scholar]
Schnider 1979 {published data only}
- Schnider G, Birken RA, Poindexter AN. A comparison of netilmicin and gentamicin in the treatment of pelvic infections. Obstetrics & Gynecology 1979;54(5):554-7. [PubMed] [Google Scholar]
Senft 1986 {published data only}
- Senft HH, Stiglmayer R, Eibach HW, Koerner H. Sulbactam/ampicillin versus cefoxitin in the treatment of obstetric and gynaecological infections. Drugs 1986;31(Suppl 2):18-21. [DOI] [PubMed] [Google Scholar]
Sesti 1990 {published data only}
- Sesti F, Farnè C, Piccione E. Medical treatment of pelvic inflammatory disease. A clinical study on the therapeutic effectiveness of piperacillin + erythromycin and of piperacillin + clindamycin + gentamycin [Trattamento medico della malattia infiammatoria pelvica. studio clinico sull'efficacia terapeutica de piperacillina + eritromicina e di piperacillina + clindamicina + gentamicina]. La Clinica Terapeutica 1990;132(1):41-4. [PubMed] [Google Scholar]
Sharma 2007 {published data only}
- Sharma JB, Chanana C, Sunesh K, Roy K, Malhotra N. Comparison of ofloxacin and ornidazole with probiotic versus doxycycline and metronidazole for the outpatient treatment of pelvic inflammatory disease. JK Science 2007;9(2):66-9. [Google Scholar]
Silva 1990 {published data only}
- Silva JL, Credidio RM, Gabiatti JR, Polli CH, Bedone AJ, Silva JC, et al. Imipenen/cilastatin in the treatment of pelvic infections [Imipenem/cilastatina no tratamento de infecções pélvicas]. Revista Brasileira de Medicina 1990;47:196-200. [Google Scholar]
Skerk 2003 {published data only}
- Skerk V, Puntaric A, Begovac J, Jaksic J, Strapac Z, Vickovic N, et al. Comparative study of intravenous azithromycin alone or intravenous and oral azithromycin for the treatment of pelvic inflammatory disease caused by Chlamydia trachomatis [in Croatian]. Croatian Journal of Infection 2003;23(3):125-8. [Google Scholar]
Spence 1981 {published data only}
- Spence MR, Genadry R, Raffel L. Randomized prospective comparison of ampicillin and doxycycline in the treatment of acute pelvic inflammatory disease in hospitalized patients. Sexually Transmitted Diseases 1981;8(Suppl 2):164-6. [Google Scholar]
Stamm 1984 {published data only}
- Stamm WE, Guinan ME, Johnson C, Starcher T, Holmes KK, McCormack WM. Effect of treatment regimens for Neisseria gonorrhoeae on simultaneous infection with Chlamydia trachomatis. New England Journal of Medicine 1984;310(9):545-9. [DOI] [PubMed] [Google Scholar]
Stiglmayer 1996 {published data only}
- Stiglmayer R, Senft HH, Eibach HW, Körner J. Sulbactam/ampicillin versus cefoxitin in the treatment of gynaecological infection: an antibiotic therapeutic study. International Journal of Antimicrobial Agents 1996;6:61-5. [PubMed] [Google Scholar]
Sweet 1988 {published data only}
- Sweet RL, Schachter J, Landers DV, Ohm-Smith M, Robbie MO. Treatment of hospitalized patients with acute pelvic inflammatory disease: comparison of cefotetan plus doxycycline and cefoxitin plus doxycycline. American Journal of Obstetrics and Gynecology 1988;158(3):736-41. [DOI] [PubMed] [Google Scholar]
Sweet 1994 {published data only}
- Sweet RL, Roy S, Faro S, O'Brien WF, Sanfilippo JS, Seidlin M. Piperacillin and tazobactam versus clindamycin and gentamicin in the treatment of hospitalized women with pelvic infection. Obstetrics & Gynecology 1994;83(2):280-6. [PubMed] [Google Scholar]
Takase 1986 {published data only}
- Takase Z, Komoto K, Katayama M. Comparative clinical study of ofloxacin (OFLX) and amoxicillin (AMPC) of the infectious disease in the field of obstetrics and gynecology [in Japanese]. Chemotherapy 1986;34(1):31-63. [Google Scholar]
Tellado 2002a {published data only}
- Tellado J, Woods GL, Gesser R, McCarroll K, Teppler H. Ertapenem versus piperacillin-tazobactam for treatment of mixed anaerobic complicated intra-abdominal, complicated skin and skin structure, and acute pelvic infections. Surgical Infection Society 2002;3(4):303-14. [DOI] [PubMed] [Google Scholar]
Tellado 2002b {published data only}
- Tellado J, Woods GL, Gesser R, McCarroll K, Teppler H. Ertapenem versus piperacillin-tazobactam for treatment of mixed anaerobic complicated intra-abdominal, complicated skin and skin structure, and acute pelvic infections. Surgical Infection Society 2002;3(4):303-14. [DOI] [PubMed] [Google Scholar]
Teppler 2002 {published data only}
- Teppler H, McCarroll K, Gesser RM, Woods GL. Surgical infections with enterococcus: outcome in patients treated with ertapenem versus piperacillin-tazobactam. Surgical Infection Society 2002;3(4):337-49. [DOI] [PubMed] [Google Scholar]
Thompson 1980 {published data only}
- Thompson SE III, Hager WD, Wong KH, Lopez B, Ramsey C, Allen SD, et al. The microbiology and therapy of acute pelvic inflammatory disease. American Journal of Obstetrics and Gynecology 1980;136(2):179-86. [DOI] [PubMed] [Google Scholar]
Thompson 1985 {published data only}
- Thompson SE, Brooks C, Eschenbach DA, Spence MR, Cheng S, Sweet R, et al. High failure rates in outpatient treatment of salpingitis with either tetracycline alone or penicillin/ampicillin combination. American Journal of Obstetrics and Gynecology 1985;152(6):635-41. [DOI] [PubMed] [Google Scholar]
Tulkens 1988 {published data only}
- Tulkens PM, Cerckx-Braun F, Donnez J, Ibrahim S, Kallay Z, Delmee M, et al. Safety and efficacy of aminoglycosides once-a-day: experimental data and randomized controlled evaluation in patients suffering from pelvic inflammatory disease. Journal of Drug Development 1988;1(Suppl 3):71-82. [Google Scholar]
Tulkens 1991 {published data only}
- Tulkens PM. Pharmacokinetic and toxicological evaluation of a once-daily regimen versus conventional schedules of netilmicin and amikacin. Journal of Antimicrobial Chemotherapy 1991;27(Suppl C):49-61. [DOI] [PubMed] [Google Scholar]
Van Gelderen 1987 {published data only}
- Van Gelderen CJ. A comparative trial of ceftriaxone and a penicillin/chloramphenicol combination in gynaecological infections complicated by peritonitis. South African Medical Journal 1987;Suppl 2:13-5. [PubMed] [Google Scholar]
Walker 1991 {published data only}
- Walker CK, Landers DV, Ohm-Smith MJ, Robbie MO, Luft J, Schachter J, et al. Comparison of cefotetan plus doxycycline with cefoxitin plus doxycycline in the inpatient treatment of acute salpingitis. Sexually Transmitted Diseases 1991;18(2):119-23. [PMID: ] [DOI] [PubMed] [Google Scholar]
Wikler 1989 {published data only}
- Wikler MA, Moonsammy GI, Hemsell DL. Comparison of ceftizoxime versus combination therapy in the treatment of pelvic inflammatory disease (PID). Journal of Chemotherapy 1989;1(4 Suppl):882-3. [PubMed] [Google Scholar]
Witte 1993 {published data only}
- Witte EH, Peters AA, Smit IB, Linden MC, Mouton RP, Meer JW, et al. A comparison of pefloxacin/metronidazole and doxycycline/metronidazole in the treatment of laparoscopically confirmed acute pelvic inflammatory disease. European Journal of Obstetrics, Gynecology, and Reproductive Biology 1993;50(2):153-8. [DOI] [PubMed] [Google Scholar]
Wynd 1999 {published data only}
- Wynd MA, Hemsell DL, Paladino JA. Cost-effectiveness of ampicillin/sulbactam versus cefoxitin in the treatment of pelvic inflammatory disease. Journal of Infectious Disease Pharmacotherapy 1999;4(1):35-48. [Google Scholar]
Zhang 2017 {published data only}
- Zhang D, Liu Z, Lin H, Liao Q, Li S, Sui L, et al. Effectiveness of Honghua Ruyi Wan combined with antibiotics for relief of pelvic inflammatory disease pain in women. Biomedical Research 2017;28(10):4665-70. [Google Scholar]
Zou 2019 {published data only}
- Zou H, Zhang W, Wang M, Li Z. Effects of levofloxacin hydrochloride and ciprofloxacin on pelvic inflammation and risk factors related to their effects. International Journal of Clinical and Experimental Medicine 2019;12(9):11754-61. [Google Scholar]
Additional references
Aghaizu 2011
- Aghaizu A, Adams EJ, Turner K, Kerry S, Hay P, Simms I, et al. What is the cost of pelvic inflammatory disease and how much could be prevented by screening for chlamydia trachomatis? Cost analysis of the Prevention of Pelvic Infection (POPI) trial. Sexually Transmitted Infections 2011;87(4):312-7. [DOI] [PubMed] [Google Scholar]
Altman 1998
- Altman DG. Confidence intervals for the number needed to treat. BMJ 1998;317(7168):1309-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
BASHH Guidelines 2019
- Ross J, Cole M, Evans C, Lyons D, Dean G, Cousins D. United Kingdom national guideline for the management of pelvic inflammatory disease (2019 interim update). www.bashhguidelines.org/media/1217/pid-update-2019.pdf (accessed prior to 27 May 2020).
Baveja 2001
- Baveja G, Saini S, Sangwan K, Arora DR. A study of bacterial pathogens in acute pelvic inflammatory disease. Journal of Communicable Diseases 2001;88:121-5. [PubMed] [Google Scholar]
Blanchard 1998
- Blanchard JF, Moses S, Greenaway C, Orr P, Hammond GW, Brunham RC. The evolving epidemiology of chlamydial and gonococcal infections in response to control programs in Winnipeg, Canada. American Journal of Public Health 1998;88(10):1496-502. [DOI] [PMC free article] [PubMed] [Google Scholar]
CDC 2018
- Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2018. www.cdc.gov/std/stats18/womenandinf.htm#pid (accessed prior to 27 May 2020).
Datta 2012
- Datta SD, Torrone E, Kruszon-Moran D, Berman S, Johnson R, Satterwhite CL, et al. Chlamydia trachomatis trends in the United States among persons 14 to 39 years of age, 1999-2008. Sexually Transmitted Diseases 2012;39(2):92-6. [DOI] [PubMed] [Google Scholar]
DeWitt 2010
- DeWitt J, Reining A, Allsworth JE, Peipert JF. Tuboovarian abscess: is size associated with duration of hospitalization and complications? Obstetrics and Gynecology International 2010;2010:1-5. [DOI: 10.1155/2010/847041] [DOI] [PMC free article] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315(629):634. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Eschenbach 1975
- Eschenbach DA, Buchanan TM, Pollock HM, Forsyth PS, Alexander ER, Lin JS, et al. Polymicrobial etiology of acute pelvic inflammatory disease. New England Journal of Medicine 1975;293(4):166-71. [DOI] [PubMed] [Google Scholar]
Fewtrell 2008
- Fewtrell MS, Kennedy K, Singhal A, Martin RM, Ness A, Hadders-Algra M, et al. How much loss to follow-up is acceptable in long-term randomised trials and prospective studies? Archives of Disease in Childhood 2008;93(6):458-61. [DOI: 10.1136/adc.2007.127316] [DOI] [PubMed] [Google Scholar]
Goller 2016
- Goller JL, De Livera AM, Fairley CK, Guy RJ, Bradshaw CS, Chen MY, et al. Population attributable fraction of pelvic inflammatory disease associated with chlamydia and gonorrhoea: a cross-sectional analysis of Australian sexual health clinic data. Sexually Transmitted Infections 2016;92(7):525-31. [DOI: 10.1136/sextrans-2015-052195] [PMID: ] [DOI] [PubMed] [Google Scholar]
GRADEpro GDT [Computer program]
- McMaster University (developed by Evidence Prime) GRADEpro GDT. Version accessed prior to February 2017. Hamilton (ON): McMaster University (developed by Evidence Prime), 2014. Available at gradepro.org.
Hager 1983
- Hager WD, Eschenbach DA, Spence MR, Sweet RL. Criteria for diagnosis and grading of salpingitis [editorial]. Obstetrics and Gynecology 1983;61(1):113-4. [PMID: ] [PubMed] [Google Scholar]
Haggerty 2006
- Haggerty CL, Ness RB. Epidemiology, pathogenesis and treatment of pelvic inflammatory disease. Expert Review of Anti-infective Therapy 2006;4(2):235-47. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Higgins 2019
- Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editor(s). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Available from www.training.cochrane.org/handbook. [DOI] [PMC free article] [PubMed]
Judlin 2010a
- Judlin P. Current concepts in managing pelvic inflammatory disease. Current Opinion in Infectious Diseases 2010;23(1):83. [DOI] [PubMed] [Google Scholar]
Mahafzah 2008
- Mahafzah AM, Al-Ramahi MQ, Asa'd AM, El-Khateeb MS. Prevalence of sexually transmitted infections among sexually active Jordanian females. Sexually Transmitted Diseases 2008;35(6):607-10. [DOI] [PubMed] [Google Scholar]
McCormack 1977
- McCormack WM, Nowroozi K, Alpert S, Sackel SG, Lee YH, Lowe EW, et al. Acute pelvic inflammatory disease: characteristics of patients with gonococcal and nongonococcal infection and evaluation of their response to treatment with aqueous procaine penicillin G and spectinomycin hydrochloride. Sexually Transmitted Diseases 1977;4(4):125-31. [PubMed] [Google Scholar]
Molander 2003
- Molander P, Finne P, Sjoberg J, Sellors J, Paavonen J. Observer agreement with laparoscopic diagnosis of pelvic inflammatory disease using photographs. Obstetrics and Gynecology 2003;101:875-80. [DOI] [PubMed] [Google Scholar]
Morris 2014
- Morris GC, Stewart CM, Schoeman SA, Wilson JD. A cross-sectional study showing differences in the clinical diagnosis of pelvic inflammatory disease according to the experience of clinicians: implications for training and audit. Sexually Transmitted Infections 2014;90(6):445-51. [DOI: 10.1136/sextrans-2014-051646] [DOI] [PubMed] [Google Scholar]
Ness 2006
- Ness RB, Smith KJ, Chang CC, Schisterman EF, Bass DC, Gynecologic Infection Follow-Through, GIFT, Investigators. Prediction of pelvic inflammatory disease among young, single, sexually active women. Sexually Transmitted Diseases 2006;33(3):137-42. [DOI] [PubMed] [Google Scholar]
Newman 2015
- Newman L, Rowley J, Vander Hoorn S, Wijesooriya NS, Unemo M, Low N, et al. Global estimates of the prevalence and incidence of four curable sexually transmitted infections in 2012 based on systematic review and global reporting. PloS One 2015;10(12):e0143304. [DOI: 10.1371/journal.pone.0143304] [DOI] [PMC free article] [PubMed] [Google Scholar]
Price 2017
- Price MJ, Ades AE, Welton NJ, Simms I, Horner PJ. Pelvic inflammatory disease and salpingitis: incidence of primary and repeat episodes in England. Epidemiology and Infection 2017;145(1):208-15. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
RevMan Web 2019 [Computer program]
- The Cochrane Collaboration Review Manager Web (RevMan Web). The Cochrane Collaboration, 2019. Available at: revman.cochrane.org.
Ross 2004
- Ross JD. What is endometritis and does it require treatment? Sexually Transmitted Infections 2004;80(4):252-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ross 2007
- Ross J, Judlin P, Nilas L. European guidelines of the management of pelvic inflammatory disease. International Journal of STD and AIDS 2007;18:662-6. [DOI] [PubMed] [Google Scholar]
Ross 2014a
- Ross JD. Pelvic inflammatory disease. American Family Physician 2014;90(10):725-6. [Google Scholar]
Ross 2014b
- Ross J, Judlin P, Jensen J. 2012 European guideline for the management of pelvic inflammatory disease. International Journal of STD & AIDS 2014;25(1):1-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Rowley 2019
- Rowley J, Hoorn VS, Korenromp E, Low N, Unemo M, AbuRaddad LJ, et al. Chlamydia, gonorrhoea, trichomoniasis and syphilis: global prevalence and incidence estimates, 2016. Bulletin of the World Health Organization 2019;97:548-62. [DOI: 10.2471/BLT.18.228486] [DOI] [PMC free article] [PubMed] [Google Scholar]
Simms 1999
- Simms I, Rogers P, Charlett A. The rate of diagnosis and demography of pelvic inflammatory disease in general practice: England and Wales. International Journal of STD and AIDS 1999;10(7):448-51. [DOI] [PubMed] [Google Scholar]
Soper 1991
- Soper DE. Diagnosis and laparoscopic grading of acute salpingitis. American Journal of Obstetrics and Gynecology 1991;164(5):1370-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Soper 2010
- Soper DE. Pelvic inflammatory disease. Obstetrics and Gynecology 2010;116(2 Pt 1):419-28. [DOI] [PubMed] [Google Scholar]
Sterne 2013
- Sterne J. Why the Cochrane risk of bias tool should not include funding source as a standard item [editorial]. Cochrane Database of Systematic Reviews 2013;12:ED000076. [10.1002/14651858.ED000076] [DOI] [PMC free article] [PubMed]
Sutton 2008
- Sutton AJ, Higgins J. Recent developments in meta-analysis. Statistics in Medicine 2008;27(5):625-50. [DOI] [PubMed] [Google Scholar]
Trent 2011
- Trent M, Ellen JM, Frick KD. Estimating the direct costs of pelvic inflammatory disease in adolescents: a within-system analysis. Sexually Transmitted Diseases 2011;38(4):326-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Walker 1993
- Walker CK, Kahn JG, Washington AE, Peterson HB, Sweet RL. Pelvic inflammatory disease: metaanalysis of antimicrobial regimen efficacy. Journal of Infectious Diseases 1993;168(4):969-78. [DOI] [PubMed] [Google Scholar]
Walker 2007
- Walker CK, Wiesenfeld H. Antibiotic therapy for acute pelvic inflammatory disease: the 2006 Centers for Disease Control and Prevention Sexually Transmitted Diseases Treatment Guidelines. Clinical Infectious Diseases 2007;28 (Suppl 1):S29-36. [DOI] [PubMed] [Google Scholar]
Workowski 2015
- Workowski KA, Bolan GA. Sexually transmitted diseases treatment guidelines, 2015. MMWR. Recommendations and Reports : Morbidity and Mortality Weekly Report 2015;64(RR-03):1-137. [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Savaris 2012
- Savaris RF, Ross J, Fuhrich DG, Rodriguez-Malagon N, Duarte RV. Antibiotic therapy for pelvic inflammatory disease (PID). Cochrane Database of Systematic Reviews 2013, Issue 1. Art. No: CD010285. [DOI: 10.1002/14651858.CD010285] [DOI] [PMC free article] [PubMed] [Google Scholar]
Savaris 2017
- Savaris RF, Fuhrich DG, Duarte RV, Franik S, Ross J. Antibiotic therapy for pelvic inflammatory disease. Cochrane Database of Systematic Reviews 2017, Issue 4. Art. No: CD010285. [DOI: 10.1002/14651858.CD010285.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]


