Abstract
Background
The incidence of Brugada syndrome has been reported to occur mostly in Asian countries. However, key countries such as Indonesia, the largest-populated Southeast Asian country, have yet to report any existing data regarding the incidence of Brugada syndrome among its population. Detecting these patients has been challenging, especially in primary healthcare settings, which generally have limited resources. Telemedicine may represent an ideal solution for initial diagnosis to determine if a patient may have this condition.
Methods
We collected and analyzed numerous 12-lead electrocardiograms (ECG) of patients who visited various healthcare centers in Makassar for routine medical check-up between June 2017–April 2018. Electrocardiograms from these centers were sent to the Cardiac Center at Dr. Wahidin Sudirohusodo Hospital in Makassar via telemedicine.
Results
During the period, we successfully obtained 9558 ECGs. While none of the patients were initially suspected of Brugada Syndrome, we found 102 (1.07%) among them to have a Brugada ECG pattern (BrEP). BrEP was more commonly found in males compared to females (67.6% vs. 32.4% of the cases found). There were significant differences in the number of confirmed cases among the types of BrEP for male and female patients. The number of confirmed cases of BrEP in male and female patients were significantly different (p < 0.05), where the number of cases for male vs. female was 8 vs. 4 for type 1, 17 vs. 1 for type 2, and 44 vs. 28 for type 3.
Conclusion
Brugada syndrome is a disease that is at grave risk of being frequently underdiagnosed. Our study indicates that telemedicine can become an appropriate tool that can assist physicians in detecting suspected patients. Future efforts should also be directed at studying the possible use of telemedicine for detecting other similarly rare conditions.
Keywords: Telemedicine, Brugada electrocardiogram pattern, Brugada syndrome, Southeast Asia, Prevalence
Highlights
-
•
Brugada syndrome is a rare and dangerous condition which is challenging to detect in developing countries with low resources.
-
•
GPs are heavily relied on to provide an early diagnosis for patients, including those suspected of Brugada syndrome.
-
•
Telemedicine allows a faster way for GPs to consult ECG images with cardiologists in order to provide an initial diagnosis.
1. Introduction
Brugada syndrome (BrS) was first described by Pedro and Joseph Brugada in 1992 [1]. This syndrome has been universally known as a rare and dangerous condition which can cause sudden cardiac death (SCD) among seemingly healthy and young individuals. This deathly and inherited disease has a typical electrocardiogram (ECG) which is characterized by a complete or incomplete right bundle branch block (RBBB) with ST segment elevation of 2 mm at the right precordial lead (V1–V3) followed by a negative T-wave [[2], [3], [4], [5]].
Existing reports on the prevalence of Brugada syndrome are extremely limited in number. However, several researchers have estimated that this disease affects 0.05% of the world population and is most prevalent in Southeast Asian countries and Japan [[6], [7], [8], [9]]. Despite its minor effects on the global population, this condition is believed to be responsible for more than 10% of all sudden deaths and up to 20% of sudden deaths in structurally normal hearts [10]. Therefore, given its deathly nature, early detection should be of utmost priority, especially in regions that are proven to have a higher prevalence.
The exact burden of this syndrome is challenging to assess, primarily due to this disease's asymptomatic nature. As an effect, there is currently no existing data regarding the incidence of Brugada syndrome in several key countries, including Indonesia, the largest-populated Southeast Asian country with a population that comprises 40% of the ASEAN population [11]. Most BrS cases are found incidentally during routine medical check-up, and extremely high numbers of undetected and underreported cases are then expected [10]. If one can move past these difficulties, then those in need will surely benefit by getting access to life-saving treatments such as Implantable Cardioverter Defibrillator (ICD) implantation. Most patients who have received this treatment are expected not to experience any deadly arrhythmic events after the treatment [12].
In order to come up with an appropriate solution to the challenges in diagnosing BrS, we must take into account the fact that developing countries like Indonesia have established a national healthcare system which heavily relies on primary healthcare centers as well as general practitioners to provide an early diagnosis. Only after the physician found that the case cannot be handled at the center that the center refers the case to a hospital which has more complete equipment and diagnostic instruments and specialists who are more experienced and are considered experts in specific fields of practice [13]. This system can provide easy access to healthcare services to every citizen but it brings about a huge burden on primary care physicians, which are often equipped with minimal resources, to provide proper diagnosis. This may cause delay in getting more thorough diagnosis and treatments to the patients [14].
Telemedicine may provide a practical solution for this problem. The telemedicine system used in this study is a cost-effective system developed by researchers at Hasanuddin University which combines information technology and knowledge that enables electronic medical data to be transferred from one health facility to another [15]. This system allows primary physicians to have direct access to experts competent in specific fields which can strengthen the primary physician's diagnostic skills by having direct guidance and quality control from specialists. This system can ensure that patients with complex conditions can obtain timely referral to a hospital which can provide appropriate medical cares [16]. This innovation is considered novel in the developing world and has recently been implemented in primary health care centers in Makassar, Indonesia. Its current use has been primarily to diagnose other emergency life-threatening conditions such as acute coronary syndrome, while its use for detecting rare conditions such as Brugada syndrome is yet to be reported [17]. This study focuses on the firsthand experience on telemedicine support through pre-hospital electrocardiograms and remote tele-consultation with cardiologists which has been implemented at Dr. Wahidin Sudirohusodo Hospital's Cardiac Center in Makassar, a National Cardiovascular Center in Eastern Indonesia.
2. Methods
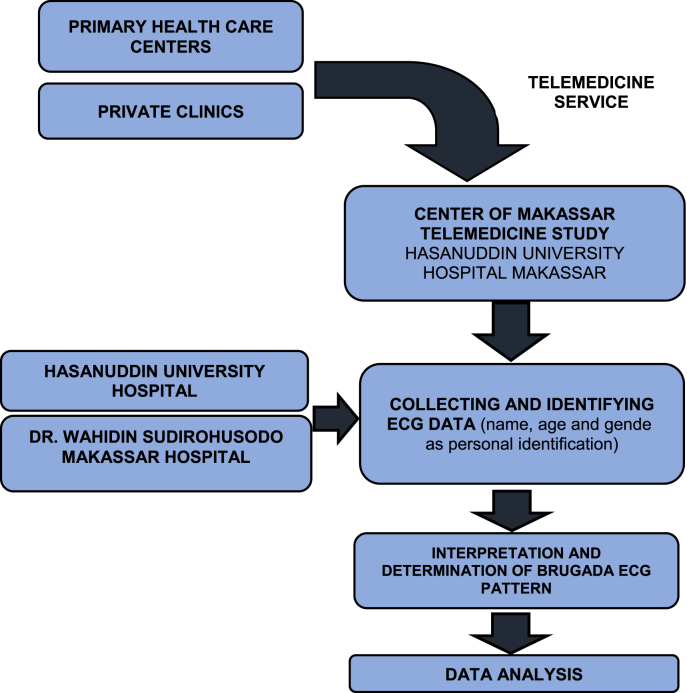
The subjects of this prospective observational study were the general population of Makassar who visited primary care centers as well as private clinics which were equipped with an electrocardiogram (ECG) and have implemented Tele-ECG into their services. We also included in this study patients who underwent routine medical check-up at Hasanuddin University Hospital and Dr. Wahidin Sudirohusodo Hospital's Cardiac Center. We only excluded patients who were not willing to be included in this research. All patients underwent standard ECG examination (12–lead standard ECG (BTL–cardio point)) with default settings of 10 mm/mV and 25 mm/s. Electrocardiograms were taken by a medical doctor or professional nurse in each respective healthcare center in the period from June 2017–April 2018. All patients presented to us did not have previous symptoms of pre-syncope, syncope, or palpitations. Data from these centers were sent to us via telemedicine system. All ECGs recorded were analyzed retrospectively and interpreted by independent cardiologists. A third cardiologist adjudicated any disagreements throughout the ECG interpreting process. The flow chart of the data collection and interpretation process is shown in Fig. 1.
Fig. 1.
Flow chart of data collection process.
The diagnosis of Brugada Syndrome was made based on the first consensus report of 2002 which uses ECG criteria alone to define Brugada ECG pattern (BrEP) [18]. There are 3 types of BrEP [1,19]:
-
1.
Type 1: Cove–shaped ST elevation in right precordial leads with J wave or ST elevation of ≥ 2 mm(mV) at its peak followed by a negative T wave with little or no isoelectric interval in more than one right precordial leadsV1–V3.
-
2.
Type 2: The ST segments also have a high take–off but the J amplitude of ≥2 mV gives rise to a gradually descending ST elevation remaining ≥1 mV above the baseline followed by a positive or biphasic T wave that results in a saddle-back configuration.
-
3.
Type 3: Right precordial ST elevation of <1 mm of saddle–back type or coved type
Prevalence rates of BrEP are represented in percentages with a 95% confidence interval. Statical analysis was performed using the chi–square test (X2) and one–way ANOVA using the Statistical Package for Social Science (SPSS) program version 21. A p-value of <0.05 was considered statistically significant.
This work has been reported in line with the STROCSS criteria [20] and was approved by the Committee for Biomedical Research on Humans, Faculty of Medicine, Hasanuddin University and Dr. Wahidin Sudirohusodo Hospital and is registered on a publicly accessible database, Research Registry (UIN: researchregistry6644).
3. Results
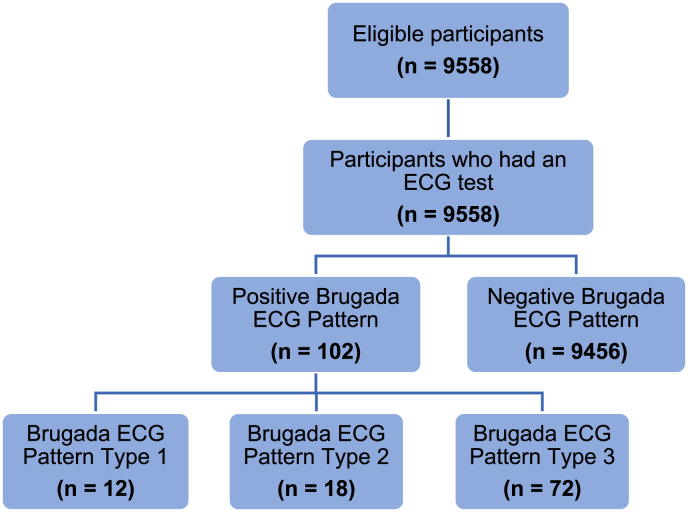
A total of 9558 electrocardiograms were obtained from eligible participants during the period from June 2017–April 2018 where 8495 (88.88%) were collected via telemedicine from multiple healthcare centers across Makassar, 401 (4.22%) electrocardiograms were obtained from Hasanuddin University Hospital and the remaining 662 (6.9%) were from Dr. Wahidin Sudirohusodo Hospital's Cardiac Center in Makassar (Fig. 2). Out of the total, 4827 (50.5%) were male patients while the remaining 4731 (49.5%) were female patients. All ECGs that were received via telemedicine were initially diagnosed by primary healthcare physicians at various community healthcare centers and the results are displayed in Table 1.
Fig. 2.
Flow chart of research participants through the study.
Table 1.
Initial ECG diagnosis by primary physicians.
| Total n = 9558 | |
|---|---|
| No ECG abnormalities | 8160 |
| Supraventricular tachycardia | 11 |
| Atrial fibrillation | 110 |
| Atrial flutter | 9 |
| Atrial premature complexes | 94 |
| Ventricular premature complexes | 105 |
| Sinoatrial block | 6 |
| Atrioventricular block (1st degree, 2nd degree, 3rd degree) | 49 |
| Right bundle branch block | 140 |
| Left bundle branch block | 21 |
| Myocardial infarction | 613 |
| ST and/or T wave changes suggestive for myocardial ischemia | 509 |
| Non-specific ST and/or T wave changes | 99 |
| Early repolarization | 72 |
| Left atrial enlargement | 45 |
| Right atrial enlargement | 48 |
| Left ventricular hypertrophy (Sokolow-Lyon) | 418 |
| Right ventricular hypertrophy | 23 |
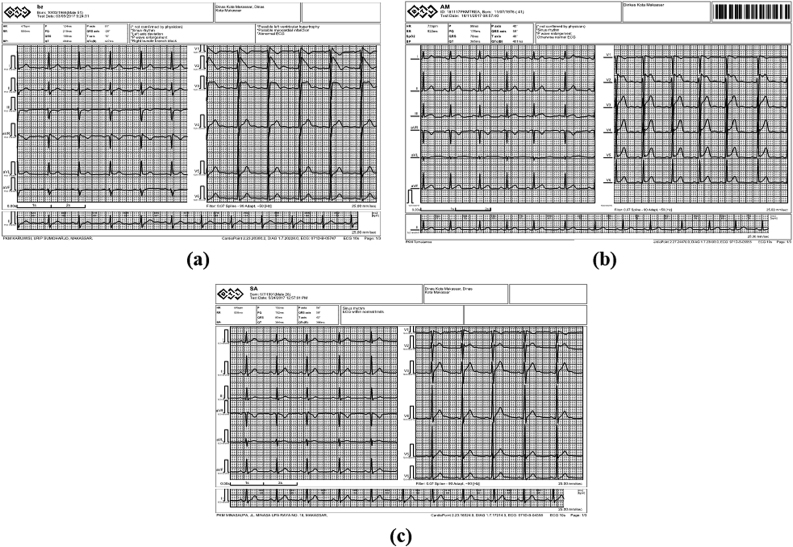
All ECGs were immediately further evaluated by independent cardiologists and although none of the ECGs that were referred for further consultation had an initial diagnosis of Brugada, patients (1.07%) (95% CI: 0.08–0.12) turned out to have a BrEP (Fig. 3) based on the results of final consultation via telemedicine.
Fig. 3.
Electrocardiogram Samples of Brugada Syndrome received using Telemedicine
(a) Brugada syndrome type 1, (b) Brugada syndrome type 2, (c) Brugada syndrome type 3.
These patients had a mean age of 51.1 ± 12.1 years and ranged from 24 to 78 years old. BrEP was found more frequent in males compared to females (69 (67.6%) vs 33 (32.4%)). Based on the BrEP type, the number of patients who had a BrEP type 1, type 2 and type 3 were 12 (0.11%) (95% CI 0.001–0.002); 18 (0.167%) (95% CI:0.001–0.003); and 72 (0.67%) (95% CI:0.005–0.08) respectively. Other baseline characteristics are shown in Table 2.
Table 2.
Baseline characteristics of patients with brugada electrocardiogram pattern.
| Type 1 N = 12 (11.76%) |
Type 2 N = 18 (17.64%) |
Type 3 N = 72 (70.69%) |
|
|---|---|---|---|
| Age (y±SD) | 58 ± 9.9 | 53.2 ± 12.3 | 49.4 ± 12.0 |
| Male | 8 (67%) | 17 (94%) | 44 (61%) |
| Sinus Rhythm | 6 | 14 | 64 |
| Sinus Bradycardia | 3 | 3 | 4 |
| Sinus Tachycardia | 3 | 1 | 3 |
| Atrial Fibrillation | 0 | 0 | 1 |
| PR Interval (ms) | 161.6 ± 29.7 | 169.3 ± 17.3 | 163.8 ± 23.8 |
| QRS duration (ms) | 85.8 ± 14.5 | 87.5 ± 10.1 | 86.7 ± 8.6 |
| Left Ventricle Hypertrophy | 3 (25%) | 2 (11%) | 1 (1.3%) |
| QT Interval Correction (ms) | 425.3 ± 33.2 | 411.8 ± 39.0 | 424.03 ± 25.5 |
There were significant differences between the types of BrEP based on gender where male patients dominated over female patients in all BrEP types (8 vs 4 for type 1, 17 vs 1 for type 2, and 44 vs 28 for type 3) with a p value of 0.026 (p < 0.05). Out of the 102 patients with a BrEP sign, all were asked to visit their respective healthcare center for further history taking. None reported of previous syncope episodes or hospitalization due to sudden cardiac arrest despite their current ECG results. All of the suspected patients were referred to referral hospitals for further investigations and the occurrence of Brugada Syndrome in these patients were further assessed by competent cardiologists.
4. Discussion
Recent studies on the prevalence of Brugada Syndrome and BrEP have reported high prevalence of BrEP in Asian countries [21]. Although Indonesia is the most populated country in Southeast Asia, study on the prevalence of Brugada Syndrome is still lacking and this is the first study that reports the incidence of BrEP in Indonesia. We gathered ECGs from numerous community health centers, clinics, and hospitals in Makassar, Indonesia. Such combination of community-based and hospital-based data is the first one to be reported in the study of BrEP.
This study was successfully completed with the help of a telemedicine system. Telemedicine services is a well-established program provided in our center since 2016. The recent development of an internet-based system has created the possibility of digitizing a 12-lead ECG and sending it instantly to the telemedicine system. This system has been applied at other medical centers and has provided numerous advantages such as convenient, cost-effective, and fast, especially for patients who live in remote areas. This system is especially suitable for archipelagic countries such as Indonesia [14,22]. Moreover, pre-hospital ECG could be implemented as a screening tool to establish a proper management strategy in handling cardiovascular diseases, especially in providing the diagnosis of serious conditions such as myocardial ischemia and arrhythmia diseases [23].
An important finding from our study was that it highlighted the important reasons for primary physicians to seek consultation from telecardiologists. Most of the time, the reason for seeking consultation is due to the need of a second opinion on an ECG that is seemingly normal, yet the physician believes otherwise. The next most frequent reason would be due to suspected myocardium ischemia or infarct. Our findings were quite similar to those reported in a previous study conducted in Israel which stated that the treating physician would often not always indicate a specific reason for consultation due to their own confusion on interpreting the ECG results themselves [24].
All of the ECGs submitted to our telemedicine system by various healthcare centers during the period of this study were submitted for evaluation by cardiologists for various reasons. However, none of the ECGs were initially suspected of BrS or BrEP by primary physicians before consultation with cardiologists via telemedicine. Yet, 102 patients turned out to have a BrEP apparent on their ECG. The prevalence of BrEP in this study was 1.07%. This finding was similar to the reported prevalence in Asia which is 0.9%, and was fairly higher than those in Europe (0.3%) and North America (0.2%) [21]. Reasons as to how this condition is somewhat more prevalent in Asian countries has been previously studied by Bezzina et al. These researchers identified a haplotype variant which consists of 6 polymorphisms that were found in 22% Asians but were not found in either Caucasians or Africans [25]. Haplotype B (HapB), which was commonly found among Asians, had been linked to a deleterious outcome in heart conduction [25]. This might indicate the contribution of race and ethnicity in the prevalence of BrS. A prevalence of 2.07% was reported in Japan [26], 2.41% in Philippines [27], and 3.31% in Taiwan [28].
Survey on Arrhythmic Events in Brugada Syndrome (SABRUS) reported that most patients with BrS experienced a first arrhythmia event between age 16 and 70 years old [29]. In our study, the Brugada electrocardiogram pattern was found among patients with age between 16 and 70 years old (94,2%). This finding is similar to the result of a study conducted in Japan by Ito et al. [30] which indicated that the mean age of BrEP patients was 52.9 ± 4.5 years. However, this study only included male subjects.
Different prevalence of BrEP was found in different gender groups, where males had a higher prevalence in all three types of BrEP (p = 0.026). This may be related to the clinical phenotype that was found more frequent in male subjects. Moreover, different pattern of outward wave is more prominent in the male subject, which results in a more negative end of phase I in the right ventricular epicardium that increase the risk of ventricular tachycardia [31].
Previous studies also reported that BrS patients with conduction abnormalities such as longer PR interval, longer QRS duration, and longer QT interval on surface ECG are more likely to develop syncope [32]. This report is consistent with the result of our study since none of our patients showed ECG conduction abnormalities as presented in Table 2 and none reported to have history of syncope. The diagnosis of BrS in our case was found incidentally during medical check-up.
Since the last two decades, epidemiological studies with a community–based and hospital–based concept have produced data on global prevalence of Type I BrEP which show that the highest prevalence is in Asian regions [28]. This may indicate that the high risk of cardiac events related to sudden cardiac death among Asian population might be due to this condition. Type 2 and 3 Brugada patterns were highly prevalent in Southeast Asia (3.7 per 1,000, 95% CI: 0.7–6.7) [7]. We also discovered similar findings in our study with both type 2 and 3 BrEP being more prevalent compared to type 1 BrEP (88.33% vs 11.67%).
According to current guidelines, thorough medical evaluation and patient follow-up is of utmost priority [2]. The use of telemedicine as a screening tool to detect the possible occurrence of Brugada Syndrome is an important step in providing timely evaluation and treatment which can help avoid deadly events, especially for patients who are far from well-equipped hospitals. In addition, telemedicine system has enabled us to obtain large number of ECG images cheaply and rapidly such that we can perform large scale studies as we have done in this study.
The limitation of this study is that complete diagnostic tests and risk stratification could not be performed due to limited resources that were available at primary healthcare centers, therefore a final diagnosis of Brugada Syndrome could not be made, instead, we were only able to detect those suspected of this disease according to their ECG patterns. Follow-up studies are certainly needed in order to fully understand the prevalence of this disease in Indonesia.
5. Conclusion
Establishing a clear diagnosis for Brugada syndrome may be difficult to accomplish in daily practices especially at primary care centers with limited resources. Our study proved that this disease is at a grave risk of being frequently underdiagnosed. In addition, we found that telemedicine system can provide a faster and inexpensive way to obtain ECG images that can be analyzed by cardiologists who can provide initial diagnosis. Future efforts should be directed in utilizing this innovation in detecting and managing other serious and rare conditions.
Ethical approval
This study was approved by the Ethics Committee of Hasanuddin University and Dr. Wahidin Sudirohusodo Hospital on April 16, 2018, with protocol number UH18030155. All data collection and work done was carried out in accordance with the Code of Ethics of the World Medical Association (Declaration of Helsinki). Informed consent was obtained from all human subjects and their privacy remained observed. No information which could identify subject or breach their privacy was included.
Sources of funding
This study was self-funded and there were no external funding sources.
Author contribution
MA – Data collection, ECG assessment and interpretation, editing of the manuscript.
MM – Drafting of the manuscript, literature review.
IM – Data collection, ECG assessment and interpretation, literature review.
ATSA – Editing of the manuscript.
Registration of research studies
This study has been registered on Research Registry with registration number researchregistry6644 (https://www.researchregistry.com/browse-the-registry#home/registrationdetails/60499ad1939e00001d8ca3d0/).
Guarantor
Muzakkir Amir.
Muhaimin Munizu.
Idar Mappangara.
Andi Tiara Salengke Adam.
Availability of data and materials
The datasets generated and/or analyzed during this study are not publicly available since they contain private data owned by multiple centers which were involved in this study. However, subject data are available from the corresponding author on reasonable request.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Notes
Provenance and peer review: Not commissioned, externally peer-reviewed.
Declaration of competing interest
All of the authors declare that they have no conflict of interest.
Acknowledgements
This research was supported by the Faculty of Medicine Hasanuddin University and Dr. Wahidin Sudirohusodo Hospital's Cardiac Center, Makassar, Indonesia. Research supports were provided by Hasanuddin University. The authors would also thank every primary healthcare centers in Makassar for their participations in this study.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2021.102334.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Antzelevitch C., Brugada P., Borggrefe M., Brugada J., Brugada R., Corrado D., Gussak I., LeMarec H., Nademanee K., Perez Riera A.R. Brugada syndrome: report of the second consensus conference: endorsed by the heart rhythm society and the European heart rhythm association. Circulation. 2005 doi: 10.1161/01.CIR.0000152479.54298.51. others. [DOI] [PubMed] [Google Scholar]
- 2.Gourraud J.-B., Barc J., Thollet A., Le Marec H., Probst V. Brugada syndrome: diagnosis, risk stratification and management. Arch. Cardiovasc. Dis. 2017 doi: 10.1016/j.acvd.2016.09.009. [DOI] [PubMed] [Google Scholar]
- 3.Miyazaki T., Mitamura H., Miyoshi S., Soejima K., Aizawa Y., Ogawa S. Autonomic and antiarrhythmic drug modulation of ST segment elevation in patients with Brugada syndrome. J. Am. Coll. Cardiol. 1996 doi: 10.1016/0735-1097(95)00613-3. [DOI] [PubMed] [Google Scholar]
- 4.Meregalli P.G., Tan H.L., Wilde A.A.M. Brugada syndrome: clinical and genetic aspects. Electr. Dis. Hear. 2013;1 doi: 10.1007/978-1-4471-4881-4_28. Basic Found. Prim. Electr. Dis. [DOI] [Google Scholar]
- 5.Akram M., AbdelWahab A., Salama S., Mokhtar M. Low prevalence of Brugada-type electrocardiogram in a prospective large cohort of Egyptians, Egypt. Hear. J. 2013;65:259–263. doi: 10.1016/j.ehj.2013.05.005. [DOI] [Google Scholar]
- 6.Honarbakhsh S., Providencia R., Lambiase P.D. Risk stratification in brugada syndrome: current status and emerging approaches. Arrhythmia Electrophysiol. Rev. 2018 doi: 10.15420/aer.2018.2.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vutthikraivit W., Rattanawong P., Putthapiban P., Sukhumthammarat W., Vathesatogkit P., Ngarmukos T., Thakkinstian A. Worldwide prevalence of Brugada syndrome: a systematic review and meta-analysis. Acta Cardiol. Sin. 2018 doi: 10.6515/ACS.201805_34(3).20180302B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shen X., Tan B.Y.Q., Sia C.-H., Lee J.S.W., Dalakoti M., Wang K., Lim D.Y.Z., Sng G.G.R., Lee E.C.Y., Chow W. Prevalence of brugada syndrome in a large population of young Singaporean men. Circulation. 2020;141:155–157. doi: 10.1161/CIRCULATIONAHA.119.043670. [DOI] [PubMed] [Google Scholar]
- 9.Brugada R., Campuzano O., Sarquella-Brugada G., Brugada J., Brugada P. Brugada syndrome, methodist debakey cardiovasc. J. 2014;10:25–28. doi: 10.14797/mdcj-10-1-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pappone C., Santinelli V. Brugada syndrome: progress in diagnosis and management. Arrhythmia Electrophysiol. Rev. 2019;8:13. doi: 10.15420/aer.2018.73.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wibowo M.G. Human capital relation with welfare in Indonesia and asean countries. Econ. Dev. Anal. J. 2019;8:81–93. [Google Scholar]
- 12.Delise P., Allocca G., Sitta N. Brugada type 1 electrocardiogram: should we treat the electrocardiogram or the patient? World J. Cardiol. 2017 doi: 10.4330/wjc.v9.i9.737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mboi N. Indonesia: on the way to universal health care. Heal. Syst. Reform. 2015;1:91–97. doi: 10.1080/23288604.2015.1020642. [DOI] [PubMed] [Google Scholar]
- 14.Brunetti N.D., Dellegrottaglie G., De Gennaro L., Di Biase M. Telemedicine pre-hospital electrocardiogram for acute cardiovascular disease management in detainees: an update. Eur. Res. Telemed. 2015 doi: 10.1016/j.eurtel.2015.02.002. [DOI] [PubMed] [Google Scholar]
- 15.Amir M., Mappangara I., Setiadji R., Zam S.M. Characteristics and prevalence of premature ventricular complex: a telemedicine study. Cardiol. Res. 2019 doi: 10.14740/cr887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blozik E., Wildeisen I.E., Fueglistaler P., von Overbeck J. Telemedicine can help to ensure that patients receive timely medical care. J. Telemed. Telecare. 2012;18:119–121. doi: 10.1258/jtt.2011.110812. [DOI] [PubMed] [Google Scholar]
- 17.Lazarus G., Kirchner H.L., Siswanto B.B. Prehospital tele-electrocardiographic triage improves the management of acute coronary syndrome in rural populations: a systematic review and meta-analysis. J. Telemed. Telecare. 2020 doi: 10.1177/1357633X20960627. 1357633X20960627. [DOI] [PubMed] [Google Scholar]
- 18.Nishizaki M., Yamawake N., Sakurada H., Hiraoka M. ECG interpretation in Brugada syndrome. J. Arrhythmia. 2013;29:56–64. doi: 10.1016/j.joa.2013.01.001. [DOI] [Google Scholar]
- 19.Wilde A.A.M., Antzelevitch C., Borggrefe M., Brugada J., Brugada R., Brugada P., Corrado D., Hauer R.N.W., Kass R.S., Nademanee K., Priori S.G., Towbin J.A. Proposed diagnostic criteria for the Brugada syndrome. Eur. Heart J. 2002 doi: 10.1016/S0195-668X(02)93382-8. [DOI] [PubMed] [Google Scholar]
- 20.Agha R., Abdall-Razak A., Crossley E., Dowlut N., Iosifidis C., Mathew G., Beamishaj, Bashashati M., Millham F.H., Orgill D.P., Noureldin A., Nixon I.J., Alsawadi A., Bradley P.J., Giordano S., Laskin D.M., Basu S., Johnston M., Muensterer O.J., Mukherjee I., Ngu J.C.-Y., Valmasoni M., Pagano D., Vasudevan B., Rosin R.D., McCaul J.A., Albrecht J., Hoffman J.R., Thorat M.A., Massarut S., Thoma A., Kirshtein B., Afifi R.Y., Farooq N., Challacombe B., Pai P.S., Perakath B., Kadioglu H., Aronson J.K., Raveendran K., Machado-Aranda D., Klappenbach R., Healy D., Miguel D., Leles C.R., Ather M.H. STROCSS 2019 Guideline: strengthening the reporting of cohort studies in surgery. Int. J. Surg. 2019;72:156–165. doi: 10.1016/j.ijsu.2019.11.002. [DOI] [PubMed] [Google Scholar]
- 21.Quan X.Q., Li S., Liu R., Kai Z., Wu X.F., Tang Q. A meta-analytic review of prevalence for Brugada ECG patterns and the risk for death. Med. (United States) 2016 doi: 10.1097/MD.0000000000005643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Elgendi M., Mohamed A., Ward R. Efficient ECG compression and QRS detection for E-health applications. Sci. Rep. 2017 doi: 10.1038/s41598-017-00540-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brunetti N.D., Scalvini S., Molinari G. Innovations in telemedicine for cardiovascular care. Expert Rev. Cardiovasc Ther. 2016 doi: 10.1586/14779072.2016.1140572. [DOI] [PubMed] [Google Scholar]
- 24.Nikus K., Virtanen V., Sclarovsky S., Eskola M. The role of standard 12-lead ECG in a telecardiology consultation service. Telemed. Tech. Appl. 2011 [Google Scholar]
- 25.Bezzina C.R., Shimizu W., Yang P., Koopmann T.T., Tanck M.W.T., Miyamoto Y., Kamakura S., Roden D.M., Wilde A.A.M. Common sodium channel promoter haplotype in Asian subjects underlies variability in cardiac conduction. Circulation. 2006 doi: 10.1161/CIRCULATIONAHA.105.580811. [DOI] [PubMed] [Google Scholar]
- 26.Sakabe M., Fujiki A., Tani M., Nishida K., Mizumaki K., Inoue H. Proportion and prognosis of healthy people with coved or saddle-back type ST segment elevation in the right precordial leads during 10 years follow-up. Eur. Heart J. 2003 doi: 10.1016/S0195-668X(03)00323-3. [DOI] [PubMed] [Google Scholar]
- 27.Gervacio-Domingo G., Isidro J., Tirona J., Gabriel E., David G., Amarillo M.L., Morales D., Dans A. The Brugada type 1 electrocardiographic pattern is common among Filipinos. J. Clin. Epidemiol. 2008 doi: 10.1016/j.jclinepi.2007.11.009. [DOI] [PubMed] [Google Scholar]
- 28.Juang J.M.J., Chen C.Y.J., Chen Y.H., Wu I.C., Hsu C.C., Chen L.N., Tang F.C., Wang C.C., Juan C.C., Chiu H.C., Lo H.M., Chang I.S., Hwang J.J., Lai L.P., Chiang F.T., Lin J.L., Hsiung C.A. Prevalence and prognosis of Brugada electrocardiogram patterns in an elderly Han Chinese population: a nation-wide community-based study (HALST cohort) Europace. 2015 doi: 10.1093/europace/euv141. [DOI] [PubMed] [Google Scholar]
- 29.Milman A., Andorin A., Gourraud J.B., Sacher F., Mabo P., Kim S.H., Maeda S., Takahashi Y., Kamakura T., Aiba T., Conte G., Juang J.J.M., Leshem E., Rahkovich M., Hochstadt A., Mizusawa Y., Postema P.G., Arbelo E., Huang Z., Denjoy I., Giustetto C., Wijeyeratne Y.D., Napolitano C., Michowitz Y., Brugada R., Casado-Arroyo R., Champagne J., Calo L., Sarquella-Brugada G., Tfelt-Hansen J., Priori S.G., Takagi M., Veltmann C., Delise P., Corrado D., Behr E.R., Gaita F., Yan G.X., Brugada J., Leenhardt A., Wilde A.A.M., Brugada P., Kusano K.F., Hirao K., Nam G.B., Probst V., Belhassen B. Age of first arrhythmic event in brugada syndrome: data from the SABRUS (survey on arrhythmic events in brugada syndrome) in 678 patients. Circ. Arrhythmia Electrophysiol. 2017 doi: 10.1161/CIRCEP.117.005222. [DOI] [PubMed] [Google Scholar]
- 30.Ito H., Yano K., Chen R., He Q., Curb J.D. The prevalence and prognosis of a Brugada-type electrocardiogram in a population of middle-aged Japanese-American men with follow-up of three decades. Am. J. Med. Sci. 2006;331:25–29. doi: 10.1097/00000441-200601000-00008. [DOI] [PubMed] [Google Scholar]
- 31.Antzelevitch C., Brugada P., Brugada J., Brugada R. Brugada syndrome: from cell to bedside. Curr. Probl. Cardiol. 2005;30:9–54. doi: 10.1016/j.cpcardiol.2004.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Raharjo S.B., Maulana R., Maghfirah I., Alzahra F., Putrinarita A.D., Hanafy D.A., Yuniadi Y. SCN5A gene mutations and the risk of ventricular fibrillation and syncope in brugada syndrome patients: a meta‐analysis. J. Arrhythmia. 2018 doi: 10.1002/joa3.12097. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated and/or analyzed during this study are not publicly available since they contain private data owned by multiple centers which were involved in this study. However, subject data are available from the corresponding author on reasonable request.