Abstract
Background
Premature ejaculation (PE) is a common problem among men that occurs when ejaculation happens sooner than a man or his partner would like during sex; it may cause unhappiness and relationship problems. Selective serotonin re‐uptake inhibitors (SSRIs), which are most commonly used as antidepressants are being used to treat this condition.
Objectives
To assess the effects of SSRIs in the treatment of PE in adult men.
Search methods
We performed a comprehensive search using multiple databases (the Cochrane Library, MEDLINE, Embase, Scopus, CINAHL), clinical trial registries, conference proceedings, and other sources of grey literature, up to 1 May 2020. We applied no restrictions on publication language or status.
Selection criteria
We included only randomized controlled clinical trials (parallel group and cross‐over trials) in which men with PE were administered SSRIs or placebo. We also considered 'no treatment' to be an eligible comparator but did not find any relevant studies.
Data collection and analysis
Two review authors independently classified and abstracted data from the included studies. Primary outcomes were participant‐perceived change with treatment, satisfaction with intercourse and study withdrawal due to adverse events. Secondary outcomes included self‐perceived control over ejaculation, participant distress about PE, adverse events and intravaginal ejaculatory latency time (IELT). We performed statistical analyses using a random‐effects model. We rated the certainty of evidence according to GRADE.
Main results
We identified 31 studies in which 8254 participants were randomized to receiving either SSRIs or placebo.
Primary outcomes: SSRI treatment probably improves self‐perceived PE symptoms (defined as a rating of 'better' or 'much better') compared to placebo (risk ratio (RR) 1.92, 95% confidence interval (CI) 1.66 to 2.23; moderate‐certainty evidence). Based on 220 participants per 1000 reporting improvement with placebo, this corresponds to 202 more men per 1000 (95% CI 145 more to 270 more) with improved symptoms with SSRIs.
SSRI treatment probably improves satisfaction with intercourse compared to placebo (defined as a rating of 'good' or 'very good'; RR 1.63, 95% CI 1.42 to 1.87; moderate‐certainty evidence). Based on 278 participants per 1000 reporting improved satisfaction with placebo, this corresponds to 175 more (117 more to 242 more) per 1000 men with greater satisfaction with intercourse with SSRIs.
SSRI treatment may increase treatment cessations due to adverse events compared to placebo (RR 3.80, 95% CI 2.61 to 5.51; low‐certainty evidence). Based 11 study withdrawals per 1000 participants with placebo, this corresponds to 30 more men per 1000 (95% CI 17 more to 49 more) ceasing treatment due to adverse events with SSRIs.
Secondary outcomes: SSRI treatment likely improve participants' self‐perceived control over ejaculation (defined as rating of 'good' or 'very good') compared to placebo (RR 2.29, 95% CI 1.72 to 3.05; moderate‐certainty evidence). Assuming 132 per 1000 participants perceived at least good control, this corresponds to 170 more (95 more to 270 more) reporting at least good control with SSRIs.
SSRI probably lessens distress (defined as rating of 'a little bit' or 'not at all') about PE (RR 1.54, 95% CI 1.26 to 1.88; moderate‐certainty evidence). Based on 353 per 1000 participants reporting low levels of distress, this corresponds to 191 more men (92 more to 311 more) per 1000 reporting low levels of distress with SSRIs.
SSRI treatment probably increases adverse events compared to placebo (RR 1.71, 95% CI 1.48 to 1.99; moderate‐certainty evidence). Based on 243 adverse events per 1000 among men receiving placebo, this corresponds to 173 more (117 more to 241 more) men having an adverse event with SSRIs.
SSRI treatment may increase IELT compared to placebo (mean difference (MD) 3.09 minutes longer, 95% CI 1.94 longer to 4.25 longer; low‐certainty evidence).
Authors' conclusions
SSRI treatment for PE appears to substantially improve a number of outcomes of direct patient importance such as symptom improvement, satisfaction with intercourse and perceived control over ejaculation when compared to placebo. Undesirable effects are a small increase in treatment withdrawals due to adverse events as well as substantially increased adverse event rates. Issues affecting the certainty of evidence of outcomes were study limitations and imprecision.
Plain language summary
Selective serotonin re‐uptake inhibitors for premature ejaculation
Review question
We wanted to find out if medicines called selective serotonin re‐uptake inhibitors (SSRIs), which are used mostly to treat depression, can help men that ejaculate faster than they want, to slow down.
Background
Premature ejaculation is a common problem among men, that occurs when ejaculation happens sooner than a man or his partner would like during sex; it may cause unhappiness and relationship problems. SSRIs are medicines that are often given to help treat premature ejaculation, but we do not understand how well they actually work and what unwanted effects they might cause.
Study characteristics
We studied the evidence up to 1 May 2020. We found 31 studies with 8254 men. The studies compared SSRIs to placebo (a pill with inactive ingredients).
Key results
SSRIs probably improve sexual satisfaction for men with premature ejaculation compared to placebo. They probably also improve the sense of control over ejaculation and decrease unhappiness and relationship problems. However, they likely increase side effects.
Quality of evidence
We judged the quality of evidence to be moderate for SSRIs, helping men’s sense of change with treatment, happiness with intercourse, and feeling of control over ejaculation. The quality of evidence was also moderate for medicine side effects. These results mean that our evaluation is likely to be close to the truth. However, the evidence on improving relationship problems and the time to ejaculation is of low certainty. This means that the true effect of treatment on those two concerns could be different from the results of this review. That may be caused by weaknesses and variations in the studies we examined.
Summary of findings
Summary of findings 1. SSRI compared to placebo for premature ejaculation.
| SSRI compared to placebo for premature ejaculation in adult men | ||||||
| Patient or population: adult men with premature ejaculation Setting: outpatient Intervention: SSRI Comparison: placebo | ||||||
| Outcomes | № of participants (studies) | Certainty of the evidence (GRADE) | Relative effect (95% CI) | Anticipated absolute effects* (95% CI) | What happens | |
| Risk with placebo | Risk difference with SSRI | |||||
| Participant perception of change with treatment assessed with: Clinical Global Impression of Change questionnaire (event is good as it represents improvement in symptoms) | 3260 (6 RCTs) | ⊕⊕⊕⊝ Moderatea | RR 1.92 (1.66 to 2.23) | Study population | SSRI probably results in perceived improvement compared to placebo. | |
| 220 per 1000 | 202 more per 1000 (145 more to 270 more) | |||||
| Participant satisfaction with intercourse assessed with: Premature Ejaculation Profile questionnaire (event is good as it represents increased satisfaction) | 4273 (3 RCTs) | ⊕⊕⊕⊝ Moderatea,b | RR 1.63 (1.42 to 1.87) | Study population | SSRI probably results in improved satisfaction with intercourse compared to placebo. | |
| 278 per 1000 | 175 more per 1000 (117 more to 242 more) | |||||
| Study withdrawal due to adverse events | 7367 (20 RCTs) | ⊕⊕⊝⊝ Lowa,c | RR 3.80 (2.61 to 5.51) | Study population | SSRI may result in more withdrawals due to adverse events compared to placebo. | |
| 11 per 1000 | 30 more per 1000 (17 more to 49 more) | |||||
| Perceived control over ejaculation assessed with: Premature Ejaculation Profile questionnaire (event is good as it represents increased control over ejaculation) | 4273 (3 RCTs) | ⊕⊕⊕⊝ Moderatea | RR 2.29 (1.72 to 3.05) | Study population | SSRI probably results in improved perceived control over ejaculation compared to placebo. | |
| 132 per 1000 | 170 more per 1000 (95 more to 270 more) | |||||
| Participant distress about PE assessed with: Premature Ejaculation Profile questionnaire (event is good as it represents less distress) | 652 (1 RCT) | ⊕⊕⊕⊝ Moderatea | RR 1.54 (1.26 to 1.88) | Study population | SSRI probably results in increased numbers of men not distressed about PE compared to placebo. | |
| 353 per 1000 | 191 more per 1000 (92 more to 311 more) | |||||
| Adverse events | 4624 (17 RCTs) | ⊕⊕⊕⊝ Moderatea | RR 1.71 (1.48 to 1.99) | Study population | SSRI probably results in increased adverse events compared to placebo. | |
| 243 per 1000 | 173 more per 1000 (117 more to 241 more) | |||||
| IELT | 5872 (20 RCTs) | ⊕⊕⊝⊝ Lowa,d | — | The mean IELT was 1.41 minutes | MD 3.09 minutes higher (1.94 higher to 4.25 higher) | SSRI probably results in extended IELT compared to placebo. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; IELT: intravaginal ejaculatory latency time; MD: mean difference; PE: premature ejaculate; RCT: randomized controlled trial; RR: risk ratio; SSRI: selective serotonin reuptake inhibitor. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded one level for study limitations: most studies had an unclear or high risk of selection, performance and detection bias. bNot downgraded for high I² statistic since observed inconsistency did not appear clinically relevant. cDowngraded one level due to serious concerns regarding attrition bias. dDowngraded one level for serious inconsistency.
Background
Description of the condition
Premature ejaculation (PE) is broadly defined as a male sexual disorder in which ejaculation occurs at a time earlier than desired by the patient or his partner, or both, usually with minimal sexual stimulation before, or shortly after penetration. Other names for this condition are early ejaculation, rapid ejaculation, rapid climax, premature climax and (historically) ejaculatio praecox. The International Society of Sexual Medicine's guideline for PE provides a more specific definition: "a male sexual dysfunction characterized by ejaculation that always or nearly always occurs prior to or within one minute of vaginal penetration, either present from the first sexual experience or following a new bothersome change in ejaculatory latency, and the inability to delay ejaculation on all or nearly all vaginal penetrations, and negative personal consequences, such as distress, bother, frustration, and/or the avoidance of sexual intimacy" (Serefoglu 2014). It should be noted that other definitions of PE have been proposed but these have not been widely adopted or have not been evidence‐based (McMahon 2004). However, all these definitions were based around time to ejaculation, the inability to control ejaculation and the negative impact on an individual.
There are several classification systems for subtypes of PE, but the commonly used Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM‐V) and International Classification of Diseases 11th Revision (ICD‐11) define four broad subtypes: lifelong, acquired, natural variable and premature‐like ejaculatory dysfunction (Waldinger 2006; Waldinger 2007). This classification likely encompasses most types of patients encountered in clinical practice. A clinical differentiation has been made between primary or lifelong versus secondary or acquired PE. With lifelong (primary) PE, the patient has experienced PE since the beginning of sexual life and it occurs in the absence of organic illnesses. Men with acquired PE encounter ejaculatory problems later in their lifetime after normal encounters in adolescence. There is generally a somatic or psychological dysfunction that is underpinning the ejaculatory problems, such as, urogenital disease, thyroid abnormalities or relationship problems. The treatment of acquired PE is based on addressing the underlying issue.
PE has a significant negative impact on a man's quality of life. Rowlands 2007 reported that men with PE have lower satisfaction with intercourse, increased personal distress and more interpersonal difficulty. These issues are also reflected in the female partners of men with PE. There are reports that the adverse effects of PE extend into a man's overall quality of life with lower 36‐item Short Form (SF‐36) scores in the following domains: general health, vitality, social function, emotional, mental health, role‐physical and the mental health component score (Rowlands 2007). Thus, successful treatment of PE has the potential to markedly improve quality of life.
Pathophysiology of premature ejaculation
The pathophysiology of PE is not completely understood. Ejaculation represents the last phase of the sexual response cycle. It is a reflex requiring interaction of somatic, sympathetic and parasympathetic nerve functions of mostly central dopaminergic and serotonergic neurons (Buvat 2011; McMahon 2004). The somatic system with the pudendal nerve enables the expulsion phase of ejaculation. Based on experimental studies in animals, serotonin has an important regulatory role in ejaculation. Different types of serotonin receptors exist in the brain, spine and peripheral autonomic ganglia, where they either have a stimulatory or inhibitory effect on ejaculation (Waldinger 2002). One of the underlying issues in PE appears to be a diminished sensitivity of one type of receptor versus the increased sensitivity of another type of receptor to serotonin. The exact cause of this problem remains unclear. Genetic, neurobiologic, pharmacologic, psychological, urologic and endocrine factors have been implicated (Buvat 2011). Genetic factors include variations in the serotonin‐transporter‐linked promoter region (5‐HTTLPR) on chromosome 17 where the short allele has been shown to be more prevalent in men with PE compared to controls (Ozbek 2011). It is likely that PE is multifactorial and that psychological and somatic factors and psychological stress contribute (Buvat 2011). Developmental factors such as history of sexual abuse, negative attitudes towards sex or individual psychological factors such as a negative body image, depression and performance anxiety may also play a role at times (Althof 2014).
Epidemiology
There have been largely variable estimates of PE prevalence because of the contention in the exact definition. Historical data from The USA National Health and Social Life Survey estimated that nearly one‐third of all adult males under 60 years of age in 1992 had PE (Laumann 1999). However, it is thought this is a gross overestimate given the number of men that present for medical attention. Contemporary data estimates the prevalence of lifelong and acquired PE as 5% of the general population (Althof 2014).
Diagnosis
Diagnosis of PE is predominantly based on the medical and sexual history of the man (Shabsigh 2006). Specifically, clinicians should ask patients how long they have had PE; how often it occurs; whether it happens during all sexual encounters and with all partners; whether the degree of sexual stimulation matters and how often they engage in sexual activity including masturbation, foreplay and intercourse. Clinicians should also ask the patient to estimate their intravaginal ejaculatory latency time (IELT), ideally with corroboration of this information by a partner if present. While assessing IELT with a stopwatch is widely used in clinical trials, it is not routinely used in clinical practice due to the intrusive nature of this measurement method and because it has been shown to be relatively comparable to self‐estimated IELT (Althof 2014; Rosen 2007a).
It is also helpful to ask the patient to define his perceived control over ejaculation, the perceived degree of bother related to PE and the impact it has on his relationship(s). Kempeneers 2013 reported that sexual satisfaction and distress better reflected the feeling of control than self‐estimated IELT. There are several questionnaires that have been developed to diagnose PE and characterize its effect on quality of life. These include the Premature Ejaculation Diagnostic Tool (PEDT) (Symonds 2007), Arabic Index of Premature Ejaculation (Arafa 2007), Premature Ejaculation Profile (PEP) (Patrick 2009), and Male Sexual Health Questionnaire Ejaculatory Dysfunction (Rosen 2007b).
It is important to distinguish between PE and erectile dysfunction (ED), recognizing that some men with ED may develop secondary PE. Vice versa, men with lifelong PE may develop ED as they age. Furthermore, possible acquired (secondary) causes of PE should be explored in an attempt to define the relevant subtype. Although physical examination is an essential part of the patient evaluation, it is unusual to find anything that explains the etiology of the patient's PE (Shabsigh 2006).
Treatment
Treatment approaches to PE, other than selective serotonin re‐uptake inhibitors (SSRIs), can be broadly categorized into behavioral therapy, oral agents and topical agents (Althof 2014; Castiglione 2016). We have introduced the most widely used treatment options below.
Behavioral therapy
Behavioral psychosexual therapies predate the use of pharmacologic agents by decades (Cooper 2015).
One early approach was referred to as the 'stop‐start' technique (Semans 1956). It involves partner stimulation of the man's penis until the sensation of near climaxing at which time stimulation is abruptly stopped until the sensation of imminent orgasm disappears. This exercise is repeated until the patient learns to voluntarily control his ejaculations.
Masters and Johnson reported a similar maneuver in which the partner squeezes the penis and stops penile stimulation (Melnik 2011). After a short interval, the female partner restarts the stimulation. This is referred to as the 'squeeze' technique.
The common feature of both approaches is distraction and the reduction of sexual excitement. It is intended to help men recognize the early signs for ejaculation/orgasm and work with their partner in improving self‐control.
Oral agents
Clomipramine: a tricyclic antidepressant that inhibits the uptake of norepinephrine and serotonin. Findings of several randomized controlled trials (RCTs) summarized in systematic reviews and meta‐analyses indicate that the daily use of clomipramine increases IELT (Choi 2019; Cooper 2015; Kim 2018; McMahon 2011).
Tramadol: a synthetic opiate analgesic that is primarily used for pain control. Its mechanism of action in PE is not fully understood. Several RCTs and reviews suggest that it results in an increase in IELT (Kirby 2015; Martyn‐St James 2015; Safarinejad 2006a; Salem 2008).
Phosphodiesterase‐5 inhibitors: the primary role of this therapy is in treating ED. However, ED is also common among men with PE and there appears to be a benefit with sildenafil or tadalafil treatment (El‐Hamd 2018; Martyn‐St James 2017)
Alfa‐adrenoreceptor antagonists: this drug class is primarily used to treat lower urinary tract symptoms associated with benign prostatic hyperplasia, but there are studies that have shown that it can improve PE (Cavallini 1995).
Topical agents
Topical agents decrease the sensitivity of the penis to sexual stimulation. Perceived advantages of these agents are the absence of systemic adverse effects.
Lidocaine‐prilocaine (marketed as EMLA) is a local anesthetic cream for topical use that can anesthetize intact skin. Several trials indicate an increase in IELT (Martyn‐St James 2016; Pu 2013; Xia 2013). Adverse effects include some loss of penile sensitivity, ED and female genital anesthesia.
Description of the intervention
SSRIs are oral drugs primarily used to treat depression. Their effect on delaying ejaculation was first identified as an adverse effect in this setting (Althof 2014; Buvat 2009). Depending on the type of agent and its half‐life, these drugs are used either daily or on‐demand.
Adverse effects of the intervention
The adverse effects of SSRIs are fairly well understood through their widespread and long‐term use in people with depression.
The most common short‐term adverse effects are reported to be drowsiness, weight gain, dry mouth, insomnia, fatigue and nausea (Cascade 2009).
Sexual adverse effects such as reduced libido and new‐onset or worsening ED have been reported (Cascade 2009).
Stopping long‐term treatment of SSRIs may lead to 'SSRI discontinuation syndrome,' beginning one to three days after drug cessation and possibly continuing for more than one week. Symptoms include nausea, vomiting, dizziness, headache, ataxia, drowsiness, anxiety and insomnia. Therefore, it is recommended that SSRIs be gradually withdrawn over several weeks (Mulhall 2012).
Multiple drug interactions exist and can potentially lead to 'serotonin syndrome,' a group of serious, persistent symptoms including myoclonus, hyper‐reflexia, sweating, shivering, and motor co‐ordination and mental status changes (Iqbal 2012).
Studies of depressed people treated with SSRIs have indicated a small increase in the risk of suicide ideation or suicide attempts, especially in younger age groups, but the evidence remains weak (Pompili 2010). Nonetheless, caution is urged in younger people with PE and concomitant depression or suicidal ideation, or both. Based on current guidelines, patients should also be advised to avoid sudden cessation or rapid dose reduction of daily dose SSRIs.
How the intervention might work
The role of 5‐hydroxytryptamine (5‐HT) (also known as serotonin) in the process of ejaculation appears to be inhibitory. SSRIs work by the blockage of serotonin transporters at the level of the synapse resulting in increased concentrations (Fuller 1994; Giuliano 2006; Waldinger 2005a). Based on a study of monkeys, administration of sertraline 20 mg/kg (an SSRI) resulted in the serotonin concentration in cerebrospinal fluid increasing by nearly 300% within hours of administration (Anderson 2005). Due to increased serotonin levels in the synapse, 5‐HT1A and 5‐HT1B receptors on the postsynaptic and presynaptic membranes become activated, causing a reduction in secretion of serotonin into the synapse (Waldinger 2005a). These receptors ultimately become desensitized, resulting in the serotonin release into the synapse, but this time because of transport inhibition by the SSRI, the synaptic serotonin levels remain high, causing persistent activation of postsynaptic receptors, which is thought to mediate the clinical effects of SSRI including the prolongation of IELT (Sprouse 2001).
Why it is important to do this review
SSRIs are among the most widely used drugs for PE (Althof 2014), but others have also argued that PE is not a disease at all (Puppo 2014), or have raised the notion that the fairly recent availability of pharmacologic treatment of PE, including SSRIs, has reinforced stereotypes of 'normal' sexual conduct and thereby reinforced social norms that cause men distress (Soderfeldt 2017). While most use of these agents is off‐label, dapoxetine, a short‐acting SSRI, is also approved for the treatment of PE in many countries outside the USA. Therefore, it is important for clinicians to fully understand both the benefits and potential harms associated with these agents as Feys 2014 raised the concern that dapoxetine may be a costly and dangerous placebo. Although multiple systematic reviews have been conducted on the treatment of PE, including the use of SSRIs (Castiglione 2016; Cooper 2015; Feys 2014; Russo 2016; Waldinger 2004; Yue 2015), these have not been performed in a methodologically rigorous manner. This review distinguishes itself by virtue of a published, a priori protocol governing all aspects of this study (New Reference), a comprehensive search of the literature not limited by publication status or language and its focus on patient‐important outcomes with rating of the certainty of evidence using the GRADE approach on a per‐outcome basis. Cochrane Reviews such as ours are also governed by a strict conflict of interest policy. Therefore, we expect this review to provide important, evidence‐based information for patients, clinicians, guideline developers and health policy makers.
Objectives
To assess the effects of SSRIs in the treatment of PE in adult men.
Methods
Criteria for considering studies for this review
Types of studies
We included RCTs in which participants were allocated to receive either SSRI or placebo/no treatment. We also included cross‐over clinical trials because we believed that this would be a suitable design to test interventions in PE as this is a relatively stable condition and SSRIs have a short half‐life (Elbourne 2002). We did not consider cluster‐RCTs as they did not appear applicable to this particular clinical question.
Types of participants
We included studies of men aged ≥ 18 years with lifelong PE only (from first sexual experience). We excluded men with PE secondary to other known conditions such as prostatitis or PE as a medication side effect (acquired PE).
Diagnostic criteria for premature ejaculation
Since a standardized definition was developed by the International Society of Sexual Medicine in 2014 (see Description of the condition), we included studies whether they used this definition or not (but recorded all definitions used).
Types of interventions
We investigated the following comparisons of intervention versus control/comparator.
Intervention
SSRI.
Comparator
Placebo.
No treatment (but we found no trials with no treatment as the comparator).
Concomitant interventions were the same in both the intervention and comparator groups to establish fair comparisons.
For trials with multiple arms, we included any arm that met the inclusion criteria in the review and listed all arms in the Characteristics of included studies table).
We did not consider agents classified as serotonin‐norepinephrine re‐uptake inhibitors such as duloxetine.
Minimum duration of intervention and follow‐up
Four weeks.
We defined the trial duration according to the number of weeks over which the interventions and comparators were conducted and only included trials in the analyses with treatments that lasted at least four weeks.
Exclusion criteria
Males aged less than 18 years.
Men with known conditions thought to cause PE or in whom PE was thought to be secondary to other medications.
Types of outcome measures
We did not exclude trials because one or several of our primary or secondary outcome measures were not reported in the publication. In case none of our primary or secondary outcomes were reported, we were unable to include such trials in the analysis but provided information for these trials in Table 2 and Table 3.
1. Description of the interventions.
| Study | Intervention(s) (route, frequency, total dose/day) | Comparator(s) (route, frequency, total dose/day) |
| Ahn 1996 | I1: fluoxetine 20 mg daily for first 1 week and 40 mg daily for remaining 5 weeks after breakfast | C1: placebo daily |
| Athanasios 2007 | I1: duloxetine 20 mg daily for 1 week followed by 40 mg daily | C1: placebo daily |
| Atmaca 2002 | I1: citalopram 20 mg daily up to 60 mg | C1: placebo daily up to 3 tablets |
| Biri 1998 | I1: sertraline 50 mg daily | C1: placebo daily |
| Buvat 2009 | I1: dapoxetine 30 mg on‐demand I2: dapoxetine 60 mg on‐demand |
C1: placebo daily C2: placebo daily |
| Farnia 2009 | I1: citalopram 20 mg on‐demand | C1: placebo on‐demand |
| Gameel 2013 | I1: paroxetine 20 mg on‐demand + lubricating jelly | C1: placebo on‐demand + lubricating jelly |
| Gong 2011 | I1: paroxetine 20 mg daily | C1: placebo |
| Hamidi Madani 2016 | I1: tramadol 50 mg I2: paroxetine 20 mg |
C1: placebo daily |
| Kara 1996 | I1: fluoxetine 20 mg daily | C1: placebo daily |
| Kaufman 2009 | I1: dapoxetine 60 mg on‐demand | C1: placebo daily |
| Khelaia 2012 | I1: paroxetine 20 mg I2: paroxetine 20 mg 2–3 hours before intercourse |
C1: placebo daily |
| Kim 1998 | I1: fluoxetine 40 mg daily for 1 week then 80 mg for 3 weeks I2: sertraline 100 mg for 1 week then 200 mg for 3 weeks |
C1: placebo daily C2: placebo daily |
| Mattos 2008 | I1: fluoxetine 90 mg daily I2: fluoxetine 90 mg daily + tadalafil 20 mg on‐demand |
C1: placebo daily C2: placebo + tadalafil 20 mg on‐demand |
| McMahon 1998 | I1: sertraline 50 mg daily | C1: placebo daily |
| McMahon 1999 | I1: paroxetine 20 mg I2: paroxetine as needed 3–4 hours before planned sexual intercourse I3: paroxetine 10 mg for 3 weeks then 20 mg paroxetine as needed for 4 weeks |
C1: placebo daily for 3 weeks then placebo daily for 4 weeks |
| McMahon 2010 | I1: dapoxetine 30 mg daily I2: dapoxetine 60 mg daily |
C1: placebo daily C2: placebo daily |
| McMahon 2013 | I1: dapoxetine 30 mg on‐demand, from week 4 up to 60 mg if tolerated + PDE5 inhibitor | C1: placebo on‐demand + PDE5 inhibitor |
| Mendels 1995 | I1: sertraline 50 mg daily that could be titrated up to 200 mg daily | C1: placebo daily |
| Na 1996 | I1: sertraline 50 mg at night that could be titrated up to 100 mg daily | C1: placebo daily |
| Novaretti 2002 | I1: fluoxetine 20 mg daily | C1: placebo daily |
| Pryor 2006 | I1: dapoxetine 30 mg on‐demand I2: dapoxetine 60 mg on‐demand |
C1: placebo on‐demand 1–3 hours before anticipated sexual activity |
| Safarinejad 2006b | I1: dapoxetine 60 mg daily I2: paroxetine 20 mg daily |
C1: placebo daily |
| Safarinejad 2006c | I1: citalopram 20 mg daily | C1: placebo daily |
| Safarinejad 2007 | I1: escitalopram 10 mg daily | C1: placebo daily |
| Safarinejad 2008 | I1: dapoxetine 30 mg twice daily | C1: placebo twice daily |
| Shang 2012 | I1: citalopram 20 mg daily | C1: placebo daily |
| Tuncel 2008 | I1: sertraline 50 mg nightly for 2 months | C1: placebo daily for 2 months |
| Waldinger 1994 | I1: paroxetine 20 mg daily for 1 week and then 40 mg daily from week 2–6 | C1: placebo daily |
| Waldinger 1998 | I1: fluoxetine 20 mg daily I2: fluvoxamine 100 mg daily I3: paroxetine 20 mg daily I4: sertraline 50 mg daily |
C1: placebo daily |
| Yilmaz 1999 | I1: fluoxetine 20 mg daily | C1: placebo daily |
C: comparator; I: intervention; PDE5: phosphodiesterase‐5.
2. Baseline characteristics.
| Study | Intervention(s) and comparator(s) | Duration of intervention | Trial period | Country | Setting | Age in years (mean) | Baseline IELT in minutes (mean) | Number of participants with primary/secondary PE |
| Ahn 1996 | I1: fluoxetine 20 mg daily for first 1 week and 40 mg daily for remaining 5 weeks after breakfast C1: placebo daily |
6 weeks | NR | South Korea | Outpatient | 39.8 (range 34–48) | 0.78 (range 0.17–2.0) | NA/NA |
| 39.8 (range 34–48) | 0.78 (range 0.17–2.0) | NA/NA | ||||||
| Athanasios 2007 | I1: duloxetine 20 mg daily for 1 week followed by 40 mg daily C1: placebo daily |
12 weeks | NR | Greece | Academic | 31.35 (SD 8.23) | 0.63 (SD 0.27) | NA/NA |
| 32.65 (SD 7.49) | 0.58 (SD 0.30) | NA/NA | ||||||
| Atmaca 2002 | I1: citalopram 20 mg daily up to 60 mg C1: placebo daily |
8 weeks | NR | Turkey | Outpatient | Range 24–46 | 0.55 (SD 0.29) | NA/NA |
| Range 24–46 | 0.50 (SD 0.24) | NA/NA | ||||||
| Biri 1998 | I1: sertraline 50 mg C1: placebo daily |
4 weeks | 1995–1997 | Turkey | Outpatient | NR | 0.68 (SD 0.21) | NA/NA |
| NR | 0.72 (SD 0.33) | NA/NA | ||||||
| Buvat 2009 | I1: dapoxetine 30 mg on‐demand I2: dapoxetine 60 mg on‐demand C1: placebo daily |
24 weeks | 2004–2006 | France | Academic | 39.6 (SD 9.53) | 0.9 (SD 0.50) | NA/NA |
| 40.5 (SD 9.62) | 0.9 (SD 0.49) | NA/NA | ||||||
| 40.1 (SD 9.98) | 0.9 (SD 0.51) | NA/NA | ||||||
| Farnia 2009 | I1: citalopram 20 mg on‐demand C1: placebo daily |
4 weeks | 2006–2007 | Iran | Outpatient | 34.28 (SD 6.67) | 1.11 (SD 0.61) | NA/NA |
| 33.76 (SD 5.93) | 1.10 (SD 0.56) | NA/NA | ||||||
| Gameel 2013 | I1: paroxetine 20 mg on‐demand + lubricating jelly C1: placebo on‐demand + lubricating jelly |
4 weeks | 2009–2012 | Egypt | Outpatient | NR | 0.16 (SD 0.47) | NA/NA |
| Gong 2011 | I1: paroxetine 20 mg daily C1: placebo daily |
30 days | NR | China | likely outpatient | 26.8 (SD 5.5) | 0.89 (SD 0.21) | NA/NA |
| 29.2 (SD 6.7) | 0.97 (SD 0.18) | |||||||
| Hamidi Madani 2016 | I1: tramadol 50 mg I2: paroxetine 20 mg C1: placebo |
12 weeks | NR | Iran | Outpatient | NR | NR | NA/NA |
| NR | NR | NA/NA | ||||||
| NR | NR | NA/NA | ||||||
| Kara 1996 | I1: fluoxetine 20 mg daily C1: placebo daily |
NR | NR | Turkey | Outpatient | Range 15–50 | 0.42 (SD 0.21) | NA/NA |
| Range 15–50 | 0.5 (SD 0.14) | NA/NA | ||||||
| Kaufman 2009 | I1: dapoxetine 60 mg on‐demand C1: placebo on‐demand |
9 weeks | NR | USA and Canada | Outpatient | 41.8 (SD 9.80) | NR | NA/NA |
| 40.98 (SD 9.71) | NR | NA/NA | ||||||
| Khelaia 2012 | I1: paroxetine 20 mg I2: paroxetine 20 mg 2–3 hours before intercourse C1: placebo |
4 weeks | NR | Georgia | Academic | 22.7 (range 19–39) | NR | NA/NA |
| 22.7 (range 19–39) | NR | NA/NA | ||||||
| 22.7 (range 19–39) | NR | NA/NA | ||||||
| Kim 1998 | I1: fluoxetine 40 mg daily for 1 week then 80 mg for 3 weeks I2: sertraline 100 mg for 1 week then 200 mg for 3 weeks C1: placebo daily |
16 weeks | NR | South Korea | Academic | 44 (range 30–60) | 0.77 (SD 0.68) | NA/NA |
| 44 (range 30–60) | 0.77 (SD 0.68) | NA/NA | ||||||
| 44 (range 30–60) | 0.77 (SD 0.68) | NA/NA | ||||||
| Mattos 2008 | I1: fluoxetine 90 mg daily I2: fluoxetine 90 mg daily + tadalafil 20 mg on‐demand C1: placebo daily C2: placebo + tadalafil 20 mg on‐demand |
12 weeks | NR | Brazil | Academic | 50 (SD 8.51) | 0.94 (SD 0.31) | NA/NA |
| 42.81 (SD 7.73) | 0.83 (SD 0.43) | NA/NA | ||||||
| 45.93 (SD 9.96) | 0.83 (SD 0.31) | NA/NA | ||||||
| 43.2 (SD 11.3) | 0.83 (SD 0.32) | NA/NA | ||||||
| McMahon 1998 | I1: sertraline 50 mg C1: placebo daily |
12 weeks | NR | Australia | Academic | 41 (range 19–70) | 0.3 | NA/NA |
| 41 (range 19–70) | 0.3 | NA/NA | ||||||
| McMahon 1999 |
Study 1: I1: paroxetine 20 mg C1: paroxetine as needed 3–4 hours before planned sexual intercourse |
17 weeks | NR | Australia | Academic | 39.5 | 0.3 | 19/7 |
| 39.5 | 0.3 | 19/7 | ||||||
|
Study 2: I2: paroxetine 10 mg for 3 weeks then 20 mg paroxetine as needed for 4 weeks C2: placebo daily for 3 weeks then placebo daily for 4 weeks |
40.5 | 0.5 | 32/10 | |||||
| 40.5 | 0.5 | 32/10 | ||||||
| McMahon 2010 | I1: dapoxetine 30 mg on‐demand I2: dapoxetine 60 mg on‐demand C1: placebo daily |
12 weeks | 2005–2006 | Multicenter in Asia/Pacific | Academic | 41.2 (SD 10.74) | 3.9 | 92 (42.2%)/NA |
| 41.0 (SD 10.78) | 4.2 | 92 (42.2%)/NA | ||||||
| 40.6 (SD 9.71) | 2.4 | 96 (45.9%)/NA | ||||||
| McMahon 2013 | I1: dapoxetine 30 mg on‐demand, from week 4 up to 60 mg if tolerated + PDE5 inhibitor taken 1–3 hours prior to sexual intercourse C1: placebo daily + PDE5 inhibitor taken 1–3 hours prior to intercourse |
12 weeks | 2010–2011 | Australia | Academic | 49.5 (SD 11.23) | NR | 92 (42.2%)/NA |
| 47.9 (SD 11.96) | NR | 96 (45.9%)/NA | ||||||
| Mendels 1995 | I1: sertraline 50 mg daily that could be titrated up to 200 mg daily C1: placebo daily |
10 weeks | NR | USA | Academic | NR | 0.98 (SD 1.15) | NA/NA |
| NR | 1.10 (SD 1.35) | NA/NA | ||||||
| Na 1996 | I1: sertraline 50 mg at night that could be titrated up to 100 mg daily C1: placebo daily |
6 weeks | NR | South Korea | Academic | NR | NR | NA/NA |
| NR | NR | |||||||
| Novaretti 2002 | I1: fluoxetine 20 mg C1: placebo daily |
20 weeks | 1998–2000 | Brazil | Academic | 37.4 (SD 10.7) | 1.01 (SD 0.86) | NA/NA |
| 37.4 (SD 10.7) | 1.05 (SD 1.07) | NA/NA | ||||||
| Pryor 2006 | I1: dapoxetine 30 mg on‐demand 1–3 hours before anticipated sexual activity I2: dapoxetine 60 mg on‐demand 1–3 hours before anticipated sexual activity C1: placebo on‐demand 1–3 hours before anticipated sexual activity |
12 weeks | 2003–2004 | USA | Academic | 40.3 (SD 9.10) | 0.90 (SD 0.47) | 563/227 |
| 40.9 (SD 9.09) | 0.92 (SD 0.50) | 571/234 | ||||||
| 40.3 (SD 9.55) | 0.91 (SD 0.48) | 560/248 | ||||||
| Safarinejad 2006b | I1: dapoxetine 60 mg daily I2: paroxetine 20 mg daily C1: placebo daily |
12 weeks | 2003–2005 | Iran | Academic | 33.4 (range 20–50) | 0.63 | 64 (61.5%)/NA |
| 34.6 (range 21–49) | 0.52 | 63 (60.0%)/NA | ||||||
| 34.3 (range 21–50) | 0.57 | 11 (44.0%)/NA | ||||||
| Safarinejad 2006c | I1: citalopram 30 mg C1: placebo daily |
6 months | NR | Iran | Academic | 32 (21–49) | 0.53 | 10/16 |
| 34 (21–49) | 0.47 | 11/14 | ||||||
| Safarinejad 2007 | I1: escitalopram 10 mg daily C1: placebo daily |
12 weeks | 2003–2005 | Iran | Academic | 33.5 (range 21–44) | NR | 87 (70%)/NA |
| 33.3 (range 19–46) | NR | 88 (69.8%)/NA | ||||||
| Safarinejad 2008 | I1: dapoxetine 30 mg daily C1: placebo daily |
12 weeks | 2004–2006 | Iran | Academic | 35.7 (range 21–54) | 0.37 | 40 (37.7%)/NA |
| 36.3 (range 19–56) | 0.48 | 43 (40.6%)/NA | ||||||
| Shang 2012 | I1: citalopram 20 mg daily C1: placebo daily |
4 weeks | 2011–2012 | China | Academic | 39.1 (SD 2.5) | 0.91 (SD 0.18) | NA/NA |
| 37.8 (SD 2.8) | 0.95 (SD 0.17) | |||||||
| Tuncel 2008 | I1: sertraline 50 mg nightly for 2 months C1: placebo daily |
8 weeks | NR | Turkey | Academic | 36.9 (median) (SD 6.9) | NR | NA/NA |
| 34.9 (median) (SD 9.0) | NR | NA/NA | ||||||
| Waldinger 1994 | I1: paroxetine 20 mg daily for 1 week and then 40 mg daily from week 2–6 C1: placebo daily |
6 weeks | NR | The Netherlands | Outpatient | 41 (range 27–48) | NR | 7/8 (87.5%)/NA |
| 38 (range 30–47) | NR | 7/9 (77.7%)/NA | ||||||
| Waldinger 1998 | I1: fluoxetine 20 mg daily I2: fluvoxamine 100 mg daily I3: paroxetine 20 mg daily I4: sertraline 50 mg daily C1: placebo daily |
6 weeks | NR | The Netherlands | Outpatient | 38 (SD 7.0) | 0.3 (SD 0.22) | NA/NA |
| 44 (SD 10.0) | 0.3 (SD 0.22) | NA/NA | ||||||
| 41 (SD 8.0) | 0.3 (SD 0.22) | NA/NA | ||||||
| 40 (SD 9.0) | 0.3 (SD 0.22) | NA/NA | ||||||
| 45 (SD 4.0) | 0.3 (SD 0.22) | NA/NA | ||||||
| Yilmaz 1999 | I1: fluoxetine 20 mg daily C1: placebo |
1 month | 1997–1997 | Turkey | Academic | 36.5 (range 22–56) | 1.2 (SD 1.0) | NA/NA |
| 37.3 (range 24–58) | 1.1 (SD 1.1) | NA/NA |
C: comparator; I: intervention; IELT: intravaginal ejaculatory latency time; NA: not available; NR: not reported; PDE5: phosphodiesterase‐5; PE: premature ejaculation; SD: standard deviation.
Primary outcomes
We focused on outcomes of direct patient importance that are directly applicable to routine clinical practice using instruments that have undergone validation.
Participant perception of change with treatment.
Participant satisfaction with intercourse.
Study withdrawal due to adverse events.
We assessed participant perception of change using the Clinical Global Impression of Change (CGIC) questionnaire, which is a validated instrument that is administered after treatment (Althof 2010). We recorded the number of participants describing the change as 'better' or 'much better' after treatment in a dichotomous manner. An event was considered 'good' as it represented 'better' or 'much better' symptoms after treatment. No minimal clinically important difference (MCID) has been reported; we considered a 10% difference between groups as clinically meaningful. This was a participant self‐reported outcome.
We assessed participant satisfaction with intercourse using the PEP questionnaire (Patrick 2009), a validated instrument that addresses four domains. We recorded the number of participants describing their satisfaction as 'good' or 'very good' before and after treatment (for satisfaction and control) in a dichotomous manner. An event was considered 'good' as it represented 'good' or 'very good' satisfaction after treatment.
We recorded the number of participants withdrawing from the trial due to adverse events in a dichotomous manner. We considered a 5% difference between groups as clinically meaningful. This was an investigator‐assessed outcome.
For study withdrawals due to adverse events, we considered a 2% absolute difference as clinically meaningful.
In the absence of any reported MCIDs for these three outcomes, all thresholds were informed by the clinical expertise and experience of the clinical authors. We did not formally involve any external stakeholders (such as men with PE) in this process. This also applies to the secondary outcomes (listed below).
Secondary outcomes
Perceived control over ejaculation.
Participant distress about PE.
Relationship difficulties.
Adverse events.
IELT.
Depression.
We also used the PEP questionnaire to assess participant satisfaction with control over ejaculation, distress about PE and relationship difficulties (Patrick 2009). We recorded the number of participants describing their satisfaction as 'good' or 'very good' before and after treatment (for satisfaction and control). An event was good as it represented 'good' or 'very good' control after treatment. This was measured in a dichotomous manner. For distress and relationship difficulties, we recorded the number of participants describing their distress 'a little bit' or 'not at all.' An event was considered good as it represented 'a little bit' or 'not at all' relationship difficulties/distress after treatment. This was also measured in a dichotomous manner. No MCID has been reported; we considered a 10% difference between groups as clinically meaningful. All of these were participant self‐reported outcomes.
We further assessed the cumulative number of adverse events in a dichotomous manner. We considered a 5% difference between groups as clinically meaningful. This was an investigator‐assessed outcome. We also provided descriptive information on the most common adverse events contributing to this analysis.
We assessed IELT as measured using a stopwatch in minutes (Waldinger 2005b). Although this method of measurement is not routinely used in clinical practice, it represents the best current method for assessing the fundamental issue that defines PE. This was measured as a continuous outcome. No MCID has been reported in the literature. Therefore, we assumed a one‐minute difference as the smallest difference between groups to be clinically meaningful. This was based on the mean IELT; we did not use the geometric mean IELT, which has been proposed as an alternative measure more robust to non‐normal distributions (Waldinger 2008).
We recorded the incidence of new symptoms of depression in participants in a dichotomous manner. We looked for information using validated instruments such as the Beck Depression Inventory questionnaire (Novaretti 2002), but also recorded other types of information as collected by the investigators. No MCID has been reported; we considered a 10% difference between groups as clinically meaningful. This may have been a participant self‐reported or investigator‐assessed outcome.
Search methods for identification of studies
A dedicated information specialist (JL) conducted all systematic searches. We applied no restrictions regarding language or publication status.
Electronic searches
We searched the following sources from the inception of each database. Complete search strategies for each resource are available in the Appendices.
Cochrane Central Register of Controlled Trials (CENTRAL) via the Cochrane Library (2020, Issue 4) (Appendix 1).
PubMed MEDLINE (from 1946) (Appendix 2).
Embase via Elsevier (from 1947) (Appendix 3).
Cumulative Index of Nursing and Allied Health Literature (CINAHL) via EBSCOhost (from 1981) (Appendix 4)
Latin American and Caribbean Health Sciences Literature (LILACS) via BIREME‐PAHO‐WHO (from 1982) (Appendix 5).
Scopus via Elsevier (from 1970) (Appendix 6).
US National Institutes of Health ClinicalTrials.gov Registry (clinicaltrials.gov) (Appendix 7).
World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) (apps.who.int/trialsearch/) (Appendix 8).
ProQuest Dissertations & Theses (PQDT; from 1861) (Appendix 9).
OCLC WorldCat Dissertations and Theses (Appendix 10).
We applied publication type filters as follows. For CENTRAL, we selected only clinical trials via the Cochrane Library results interface. For PubMed, we applied the Cochrane Highly Sensitive Search Strategy for identifying RCTs in MEDLINE: sensitivity‐maximizing version (2008 revision); PubMed format from the Cochrane Handbook for Systematic Reviews of Interventions (accessed 16 June 2017). For Embase, we translated the RCT filter from SIGN (Scottish Intercollegiate Guidelines Network) (accessed from www.sign.ac.uk/search-filters.html on 19 June 2017) to appropriate syntax for Embase‐Elsevier. For CINAHL, we used the RCT filter from SIGN (accessed from www.sign.ac.uk/search-filters.html on 19 June 2017). We applied no filter for LILACS due to a low yield. For Scopus, as a published or validated filter was not available, the Cochrane Urology Assistant Information Specialist developed one based loosely on the CINAHL filter. No filter was needed for PQDT. For WorldCat, we selected Content Type: Thesis/Dissertation. We applied no other filters or limits to the searches. The search strategies were peer reviewed by a second Cochrane Urology Assistant Information Specialist, and recommendations were incorporated into the final strategies.
We applied a PubMed (MEDLINE) email alert through 1 May 2020 to identify newly published trials using the same search strategy as described for MEDLINE (see Appendix 2 for search strategy). After we submitted the final review draft for editorial approval, the Information Specialist on our review team performed a complete search update (1 May 2020) on all databases and sent the results to the review authors. New trials were evaluated and we incorporated the findings from the new trials into our review for all included trials.
If we detected additional relevant keywords during any electronic or other searches, we modified the electronic search strategies to incorporate these terms and documented the changes.
Searching other resources
We identified other potentially eligible trials or ancillary publications by searching the reference lists of included trials, as well as related systematic reviews, meta‐analyses and health technology assessment reports. We also contacted authors of included trials to identify additional information on the retrieved trials and any trials that we might have missed.
We included studies presented in abstract form only as well, focusing on these relevant meetings from 2017 to 2020. For these years, abstract proceedings from can be searched and identified through electronic searches of the journals identified and captured through our electronic MEDLINE search. This included the following meetings:
American Urological Association (AUA); Journal of Urology;
European Urology Association (EAU); European Urology Supplements;
International Society of Sexual Medicine (ISSM); Journal of Sexual Medicine;
World Association for Sexual Health (WASH); Journal of Sexual Medicine;
European Society for Sexual Medicine (ESSM); Journal of Sexual Medicine;
World Meeting on Sexual Medicine (WMSM); Journal of Sexual Medicine;
Sexual Medicine Society of North America (SMSNA); Journal of Sexual Medicine.
Data collection and analysis
Selection of studies
At least two of four review authors (RM, AS, JB, SS) independently scanned the abstract, title, or both of every record we retrieved in the literature searches, to determine which trials we should assess further. We obtained the full text of all potentially relevant records. We resolved any disagreements through consensus or by recourse to a third review author (PD). If we could not resolve a disagreement, we categorized the trial as a 'study awaiting classification' and contacted the trial authors for clarification. We presented an adapted PRISMA flow diagram to show the process of trial selection (Liberati 2009).
Data extraction and management
For trials that fulfilled our inclusion criteria, at least two of four review authors (RM, AS, JB, SS) independently extracted key participant and intervention characteristics. We reported data on efficacy outcomes and adverse events using standardized data extraction sheets from the Cochrane Metabolic and Endocrine Disorders Group. We resolved any disagreements by discussion or, if required, by consultation with a third review author (PD).
We provided information about potentially relevant ongoing trials, including the trial identifier, in the Characteristics of ongoing studies table. We attempted to find the protocol for each included trial and reported primary, secondary and other outcomes.
We emailed all authors of included trials to ask if they were willing to answer questions regarding their trials. Thereafter we requested relevant missing information on the trial from the primary trial author(s).
Dealing with duplicate and companion publications
In the event of duplicate publications, companion documents or multiple reports of a primary trial, we maximized the information yielded by collating all available data and used the most complete data set aggregated across all known publications. We listed duplicate publications, companion documents, multiple reports of a primary trial and trial documents of included trials (such as trial registry information) as secondary references under the study ID of included trials. Furthermore, we listed duplicate publications, companion documents, multiple reports of a trial and trial documents of excluded trials (such as trial registry information) as secondary references under the study ID of excluded trials.
Data from clinical trial registers
If data of included trials were available as study results in clinical trial registers such as ClinicalTrials.gov, we made full use of this information and extracted the data. If there is also a full publication of the trial, we collated and critically appraised all available data. If an included trial was marked as a completed study in a clinical trial register but no additional information was available, we added this trial to the Characteristics of studies awaiting classification table.
Assessment of risk of bias in included studies
Two review authors (RM, SS) independently assessed the risk of bias of each included trial. We resolved any disagreements by consensus or by consulting a third review author (PD). In case of disagreement, we consulted the rest of the group and made a judgment based on consensus. If adequate information was not available from trial authors, trial protocols, or both, we contacted the trial authors for missing data on 'Risk of bias' items.
We used the Cochrane 'Risk of bias' assessment tool and judged 'Risk of bias' criteria as low, high or unclear risk (Higgins 2011a; Higgins 2011b). We evaluated individual bias items as described in the Cochrane Handbook for Systematic Reviews of Interventions according to the criteria and associated categorizations contained therein (Higgins 2011a).
Random sequence generation (selection bias due to inadequate generation of a randomized sequence) – assessment at trial level
For each included trial, we described the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
Low risk of bias: the trial authors achieved sequence generation using computer‐generated random numbers or a random numbers table. Drawing of lots, tossing a coin, shuffling cards or envelopes, and throwing dice were adequate if an independent person performed this who was not otherwise involved in the trial. We considered the use of the minimization technique as equivalent to being random.
Unclear risk of bias: insufficient information about the sequence generation process.
High risk of bias: the sequence generation method was non‐random or quasi‐random (e.g. sequence generated by odd or even date of birth; sequence generated by some rule based on date (or day) of admission; sequence generated by some rule based on hospital or clinic record number; allocation by judgment of the clinician; allocation by preference of the participant; allocation based on the results of a laboratory test or a series of tests; or allocation by availability of the intervention).
Allocation concealment (selection bias due to inadequate concealment of allocation prior to assignment) – assessment at trial level
We described for each included trial the method used to conceal allocation to interventions prior to assignment and assessed whether intervention allocation could have been foreseen in advance of or during recruitment, or changed after assignment.
Low risk of bias: central allocation (including telephone, interactive voice‐recorder, web‐based and pharmacy‐controlled randomization); sequentially numbered drug containers of identical appearance; sequentially numbered, opaque, sealed envelopes.
Unclear risk of bias: insufficient information about the allocation concealment.
High risk of bias: using an open random allocation schedule (e.g. a list of random numbers); assignment envelopes were used without appropriate safeguards; alternation or rotation; date of birth; case record number; any other explicitly unconcealed procedure.
We also evaluated trial baseline data to incorporate assessment of baseline imbalance into the 'Risk of bias' judgment for selection bias (Corbett 2014). Chance imbalances may also affect judgments on the risk of attrition bias. In case of unadjusted analyses, we distinguished between studies we rated at low risk of bias on the basis of both randomization methods and baseline similarity, and studies we rated at low risk of bias on the basis of baseline similarity alone (Corbett 2014). We reclassified judgments of unclear, low or high risk of selection bias.
Blinding of participants and study personnel (performance bias due to knowledge of the allocated interventions by participants and personnel during the trial) – assessment at outcome level
We evaluated the risk of detection bias separately for each outcome (Hróbjartsson 2013). We noted whether endpoints were self‐reported, investigator assessed or adjudicated outcome measures (see below).
Low risk of bias: blinding of participants and key study personnel was ensured, and it was unlikely that the blinding could have been broken; no blinding or incomplete blinding, but we judged that the outcome was unlikely to have been influenced by lack of blinding.
Unclear risk of bias: insufficient information about the blinding of participants and study personnel; the trial did not address this outcome.
High risk of bias: no blinding or incomplete blinding, and the outcome was likely to have been influenced by lack of blinding; blinding of trial participants and key personnel attempted, but likely that the blinding could have been broken, and the outcome was likely to have been influenced by lack of blinding.
Blinding of outcome assessment (detection bias due to knowledge of the allocated interventions by outcome assessors) – assessment at outcome level
We evaluated the risk of detection bias separately for each outcome (Hróbjartsson 2013). We noted whether endpoints were self‐reported, investigator assessed or adjudicated outcome measures (see below).
Low risk of bias: blinding of outcome assessment was ensured, and it was unlikely that the blinding could have been broken; no blinding of outcome assessment, but we judged that the outcome measurement was unlikely to have been influenced by lack of blinding.
Unclear risk of bias: insufficient information about the blinding of outcome assessors; the trial did not address this outcome.
High risk of bias: no blinding of outcome assessment, and the outcome measurement was likely to have been influenced by lack of blinding; blinding of outcome assessment, but likely that the blinding could have been broken, and the outcome measurement was likely to be influenced by lack of blinding.
Incomplete outcome data (attrition bias due to amount, nature, or handling of incomplete outcome data) – assessment at outcome level
For each included trial for each outcome, we described the completeness of data, including attrition and exclusions from the analyses. We stated whether the trial reported attrition and exclusions, and the number of participants included in the analysis at each stage (compared with the number of randomized participants per intervention/comparator groups). We also noted if the trial reported the reasons for attrition or exclusion and whether missing data were balanced across groups or were related to outcomes. We considered the implications of missing outcome data per outcome such as high dropout rates (e.g. above 15%) or disparate attrition rates (e.g. difference of 10% or more between trial arms).
Low risk of bias: no missing outcome data; reasons for missing outcome data unlikely to be related to true outcome (for survival data, censoring unlikely to introduce bias); missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across groups; for dichotomous outcome data, the proportion of missing outcomes compared with observed event risk was not enough to have a clinically relevant impact on the intervention effect estimate; for continuous outcome data, plausible effect size (mean difference (MD) or standardized mean difference (SMD)) among missing outcomes was not enough to have a clinically relevant impact on observed effect size; appropriate methods such as multiple imputation were used to handle missing data.
Unclear risk of bias: insufficient information to assess whether missing data in combination with the method used to handle missing data were likely to introduce bias; the trial did not address this outcome.
High risk of bias: reason for missing outcome data was likely to be related to true outcome, with either imbalance in numbers or reasons for missing data across intervention groups; for dichotomous outcome data, the proportion of missing outcomes compared with observed event risk enough to induce clinically relevant bias in intervention effect estimate; for continuous outcome data, plausible effect size (MD or SMD) among missing outcomes enough to induce clinically relevant bias in observed effect size; 'as‐treated' or similar analysis done with substantial departure of the intervention received from that assigned at randomization; potentially inappropriate application of simple imputation.
Selective reporting (reporting bias due to selective outcome reporting) – assessment at trial level
We assessed outcome reporting bias by comparing the published data to the study protocol (if available).
Low risk of bias: the trial protocol was available and all of the trial's prespecified (primary and secondary) outcomes that were of interest in the review were reported in the prespecified way; the study protocol was unavailable, but it was clear that the published reports included all expected outcomes (Outcome Reporting Bias in Trials (ORBIT) classification).
Unclear risk of bias: insufficient information about selective reporting.
High risk of bias: not all of the trial's prespecified primary outcomes were reported; one or more primary outcomes were reported using measurements, analysis methods or subsets of the data (e.g. subscales) that were not prespecified; one or more reported primary outcomes were not prespecified (unless clear justification for their reporting was provided, such as an unexpected adverse effect); one or more outcomes of interest in the Cochrane Review were reported incompletely so that we could not enter them in a meta‐analysis; the trial report failed to include results for a key outcome that would have been expected to have been reported for such a trial (ORBIT classification).
Other bias (bias due to problems not covered elsewhere) – assessment at trial level
Low risk of bias: the trial appeared free of other sources of bias.
Unclear risk of bias: insufficient information to assess whether an important risk of bias existed; insufficient rationale or evidence that an identified problem introduced bias.
High risk of bias: the trial had a potential source of bias related to the specific trial design used; the trial was claimed to have been fraudulent; or the trial had some other serious problem.
We presented a 'Risk of bias' graph and a 'Risk of bias' summary figure.
We distinguished between self‐reported, investigator assessed, objective and adjudicated outcome measures.
We accepted the following outcomes as self‐reported.
Participant perception of change with treatment.
Participant satisfaction with intercourse.
Perceived control over ejaculation.
Participant distress about PE.
Relationship difficulties.
Depression.
We required the following outcomes to be investigator assessed.
Study withdrawal due to adverse events.
Adverse events.
We classified the following outcome as objective.
IELT.
We did not anticipate encountering any adjudicated outcome measures.
Summary assessment of risk of bias
Risk of bias for a trial across outcomes
Some 'Risk of bias' domains such as selection bias (sequence generation and allocation sequence concealment) affect the risk of bias across all outcome measures in a trial. In case of high risk of selection bias, we marked all endpoints investigated in the associated trial as high risk. Otherwise, we did not perform a summary assessment of the risk of bias across all outcomes for a trial.
Risk of bias for an outcome within a trial and across domains
We assessed the risk of bias for an outcome measure by including all entries relevant to that outcome (i.e. both trial‐level entries and outcome‐specific entries). We considered low risk of bias to denote a low risk of bias for all key domains; unclear risk to denote an unclear risk of bias for one or more key domains; and high risk to denote a high risk of bias for one or more key domains.
Risk of bias for an outcome across trials and across domains
These are our main summary assessments, which we incorporated into our judgments about the certainty of evidence in a 'Summary of findings' table. We defined outcomes as low risk of bias when most information came from trials at low risk of bias; unclear risk when most information came from trials at low or unclear risk of bias; and high risk when a sufficient proportion of information came from trials at high risk of bias.
Measures of treatment effect
When at least two included trials were available for a comparison and a given outcome, we expressed dichotomous data as a risk ratio (RR) with 95% confidence interval (CI) for ease of interpretation rather than using odds ratios (ORs). For continuous outcomes measured on the same scale (e.g. weight loss in kilograms), we estimated the intervention effect using the MD with 95% CI. For continuous outcomes measuring the same underlying concept (e.g. health‐related quality of life) but using different measurement scales, we calculated the SMD with 95% CI.
Unit of analysis issues
We took into account the level at which randomization occurred, such as cross‐over trials, and multiple observations for the same outcome. If more than one comparison from the same trial was eligible for inclusion in the same meta‐analysis, we either combined groups to create a single pair‐wise comparison or appropriately reduced the sample size so that the same participants did not contribute multiple times (e.g. by splitting the 'shared' group into two or more groups). While the latter approach offers some solutions to adjusting the precision of the comparison, it does not account for correlation arising from the same set of participants being in multiple comparisons (Higgins 2011a). When we included cross‐over trials, we only included data from the first period to mitigate any confounding effect from carry‐over.
Dealing with missing data
We obtained missing data from the authors of the included trials. We carefully evaluated important numerical data such as screened, randomly assigned participants as well as intention‐to‐treat, as‐treated and per‐protocol populations. We investigated attrition rates (e.g. dropouts, losses to follow‐up, withdrawals) and critically appraised issues concerning missing data and use of imputation methods (e.g. last observation carried forward).
In trials where the standard deviation of the outcome was not available at follow‐up or could not be re‐created, we standardized by the mean of the pooled baseline standard deviation from those trials in which this information was reported.
Where included trials did not report means and standard deviations for outcomes and we were unable to obtain the required information from trial authors, we imputed these values by estimating the mean and variance from the median, range and the size of the sample (Hozo 2005). We investigated the impact of imputation on meta‐analyses by performing sensitivity analyses and reported per outcome which trials were included with imputed standard deviations.
Assessment of heterogeneity
In the event of excessive clinical or methodologic heterogeneity, we would not have reported trial results as the pooled effect estimate in a meta‐analysis.
We identified heterogeneity (inconsistency) by visually inspecting the forest plots and by using a standard Chi² test with a significance level of α = 0.1. In view of the low power of this test, we also considered the I² statistic, which quantifies inconsistency across trials, to assess the impact of heterogeneity on the meta‐analysis.
We interpreted the I² statistic as follows (Higgins 2002; Higgins 2003; Higgins 2011a).
0% to 40%: may not be important.
30% to 60%: may indicate moderate heterogeneity.
50% to 90%: may indicate substantial heterogeneity.
75% to 100%: considerable heterogeneity.
When we found heterogeneity, we attempted to determine the possible reasons for it by examining individual trial and subgroup characteristics.
Assessment of reporting biases
If we included 10 or more trials that investigated a particular outcome, we used funnel plots to assess small‐trial effects. Several explanations can account for funnel plot asymmetry, including true heterogeneity of effect with respect to trial size, poor methodologic design (and hence bias of small trials) and publication bias. Therefore, we carefully interpreted the results (Sterne 2011).
Data synthesis
We undertook (or displayed) a meta‐analysis only if we judged participants, interventions, comparisons and outcomes to be sufficiently similar to ensure an answer that was clinically meaningful. Unless good evidence showed homogeneous effects across trials, we primarily summarized data at low risk of bias using a random‐effects model (Wood 2008). We interpreted random‐effects meta‐analyses with due consideration to the whole distribution of effects, ideally by presenting a prediction interval (Higgins 2009). A prediction interval specifies a predicted range for the true treatment effect in an individual trial (Riley 2011). For rare events such as event rates below 1%, we planned to use the Peto's OR method, provided that there was no substantial imbalance between intervention and comparator group sizes, and intervention effects were not exceptionally large. We performed statistical analyses according to the statistical guidelines presented in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a).
Subgroup analysis and investigation of heterogeneity
We expected the following characteristics to introduce clinical heterogeneity, and carried out the following subgroup analyses including investigation of interactions.
Long‐acting SSRIs (e.g. paroxetine, fluoxetine, sertraline, citalopram and fluvoxamine) versus short‐acting (on‐demand type) SSRIs (e.g. dapoxetine). We compared the long‐ versus short‐acting SSRIs because not only may there be a difference in efficacy, but the incidence of adverse effects may vary by taking SSRIs daily rather than on‐demand.
Among the long‐acting SSRIs, comparison of individual agents (e.g. paroxetine versus fluoxetine versus sertraline versus citalopram versus fluvoxamine). We compared these agents because although they are from the same class, there is evidence to suggest that they have varying efficacy and adverse effect profile (Sanchez 2014)
If applicable, different dose levels (e.g. dapoxetine 30 mg versus 60 mg). Dose levels are compared because the use of SSRIs in PE is an off‐label indication and there is no clear evidence on the optimal dosage for the best trade‐off of benefit versus risk.
Sensitivity analysis
We performed a sensitivity analysis to explore the influence of the following factors (when applicable) on effect sizes by restricting analysis to the following.
Taking into account risk of bias, as specified in the Assessment of risk of bias in included studies section, by removing studies judged at high risk of bias.
Summary of findings and assessment of the certainty of the evidence
We presented the overall certainty of the evidence for each outcome according to the GRADE approach, which takes into account issues related to internal validity (risk of bias, inconsistency, imprecision, publication bias) and external validity, such as directness of results. Two review authors (RM, PD) independently rated the certainty of the evidence for each outcome.
We presented a summary of the evidence in a 'Summary of findings' table, which provides key information about the best estimate of the magnitude of the effect, in relative terms and as absolute differences, for each relevant comparison of alternative management strategies, numbers of participants and trials addressing each important outcome, and rating of overall confidence in effect estimates for each outcome. We created the 'Summary of findings' table based on the methods described in the Cochrane Handbook for Systematic Reviews of Interventions by means of the table editor in Review Manager 5 (Review Manager 2014). We used GRADEpro GDT software and present evidence profile tables as an appendix (GRADEpro GDT 2015). We presented results for the outcomes as described in the Types of outcome measures section. If meta‐analysis was not possible, we presented the results in a narrative format in the 'Summary of findings' table. We justified all decisions to downgrade the certainty of studies using footnotes, and made comments to aid the reader's understanding of the Cochrane Review where necessary.
The 'Summary of findings' table includes following outcomes, listed according to priority.
Participant perception of change with treatment.
Participant satisfaction with intercourse.
Study withdrawal due to adverse events.
Perceived control over ejaculation.
Participant distress about PE.
Adverse events.
IELT.
Although we did not include relationship difficulties and depression as outcomes in the 'Summary of findings' table (due to a limit of seven outcomes), we provided the same type of analysis in the Results section and also rated the certainty of the evidence using GRADE for these outcomes.
Results
Description of studies
We presented details of included studies in the Characteristics of included studies and Table 2 and Table 3.
Results of the search
Our search of multiple electronic databases up to May 2020 yielded 1218 references (Figure 1). After exclusion of duplicates, we screened 922 references at the title/abstract stage. Subsequently after screening titles/abstracts, 124 unique studies entered the full‐text screening stage. We included 31 studies (40 records) in the quantitative analyses. We summarized reasons for exclusion at the full‐text stage in the PRISMA flow diagram (Figure 1), and we provided further details Characteristics of excluded studies table.
1.
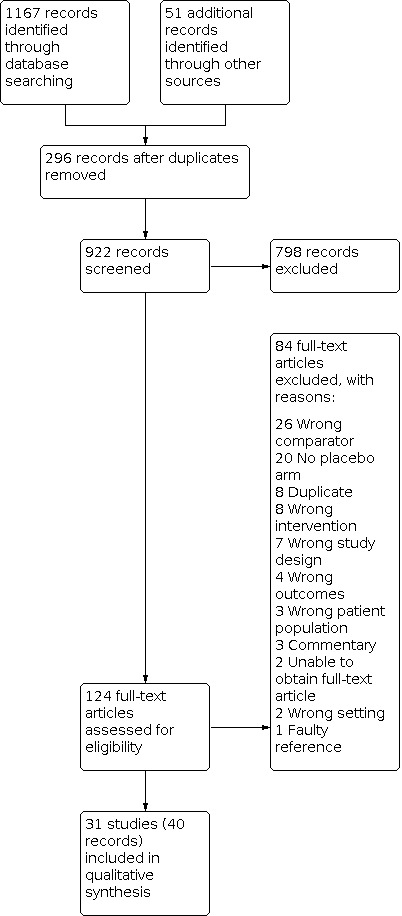
Study flow diagram.
Included studies
Source of data
We included 29 studies published in full‐text and two additional studies only available as abstract proceedings (Hamidi Madani 2016; Khelaia 2012), for a total of 31 unique studies. Two studies were published in Korean (Ahn 1996; Na 1996), and two studies were published in Chinese (Gong 2011; Shang 2012). One review author (ECH) translated the Korean studies into English and Dr Yu Xie translated the Chinese studies into English. The remaining 27 studies were published in English.
Study design and settings
Four studies were cross‐over trials (Kim 1998; McMahon 1998; McMahon 1999; Novaretti 2002), and remaining studies were parallel, RCTs. All studies were likely conducted in an outpatient clinic setting.
Participants
We included 8254 randomized participants (SSRI 4990, placebo 2928, other drug 131). Two studies did not report the number of participants in each arm (Hamidi Madani 2016; Novaretti 2002). All studies included sexually active men aged over 18 years with PE.
Interventions and comparators
Studies used a range of SSRIs with different doses. Seven studies used fluoxetine (Ahn 1996; Kara 1996; Kim 1998; Mattos 2008; Novaretti 2002; Waldinger 1998; Yilmaz 1999), one used duloxetine (Athanasios 2007), three used citalopram (Atmaca 2002; Farnia 2009; Shang 2012), seven used sertraline (Biri 1998; Kim 1998; McMahon 1998; Mendels 1995; Na 1996; Tuncel 2008; Waldinger 1998), seven used dapoxetine (Buvat 2009; Kaufman 2009; McMahon 2010; McMahon 2013; Pryor 2006; Safarinejad 2006b; Safarinejad 2008), eight used paroxetine (Gameel 2013; Gong 2011; Hamidi Madani 2016; Khelaia 2012; McMahon 1999; Safarinejad 2006c; Waldinger 1994; Waldinger 1998), one used escitalopram (Safarinejad 2007), and one used fluvoxamine (Waldinger 1998).
All studies used placebo as the comparator.
Outcomes
For our predefined primary outcomes, six studies reported participant perception of change with treatment (Athanasios 2007; Atmaca 2002; Buvat 2009; Kaufman 2009; McMahon 2010; McMahon 2013), three reported participant satisfaction with intercourse (Kaufman 2009; McMahon 2010; Pryor 2006), and 20 studies reported study withdrawal due to adverse events (Athanasios 2007; Atmaca 2002; Biri 1998; Buvat 2009; Gameel 2013; Gong 2011; Kara 1996; Kaufman 2009; McMahon 2010; McMahon 2013; Mendels 1995; Pryor 2006; Safarinejad 2006b; Safarinejad 2006c; Safarinejad 2007; Safarinejad 2008; Shang 2012; Waldinger 1994; Waldinger 1998; Yilmaz 1999).
In terms of predefined secondary outcomes, three studies reported perceived control over ejaculation (Kaufman 2009; McMahon 2010; Pryor 2006), 17 reported adverse events (Ahn 1996; Athanasios 2007; Atmaca 2002; Biri 1998; Buvat 2009; Kara 1996; Kaufman 2009; Mattos 2008; McMahon 2010; McMahon 2013; Mendels 1995; Safarinejad 2006b; Safarinejad 2007; Safarinejad 2008; Shang 2012; Tuncel 2008; Yilmaz 1999), 20 reported IELT (Ahn 1996; Athanasios 2007; Atmaca 2002; Biri 1998; Buvat 2009; Gameel 2013; Gong 2011; Kara 1996; Mattos 2008; McMahon 1998; McMahon 1999; McMahon 2010; McMahon 2013; Mendels 1995; Pryor 2006; Safarinejad 2006c; Shang 2012; Waldinger 1994; Waldinger 1998; Yilmaz 1999), and one reported depression (Kara 1996). One study reported participant distress about PE and relationship difficulties (Kaufman 2009)
Please refer to Analysis 1.1 through Analysis 1.9.
1.1. Analysis.

Comparison 1: SSRI versus placebo, Outcome 1: Participant perception of change with treatment
1.9. Analysis.

Comparison 1: SSRI versus placebo, Outcome 9: Depression
Funding sources and conflicts of interest
Four studies reported no funding source (Gameel 2013; Mattos 2008; Safarinejad 2007; Safarinejad 2008), and pharmaceutical companies supported seven studies (Buvat 2009; Kaufman 2009; McMahon 2010; McMahon 2013; Novaretti 2002; Pryor 2006; Waldinger 1998). The remaining studies did not address their funding source.
Two studies reported no conflicts of interest (Gameel 2013; Safarinejad 2008), and six studies reported investigators having relationships with pharmaceutical companies (Buvat 2009; Kaufman 2009; McMahon 2010; McMahon 2013; Mendels 1995; Pryor 2006). The remaining studies did not address conflicts of interest.
Excluded studies
We excluded 84 records after evaluation of the full‐text publications for which we presented details in the Characteristics of excluded studies table.
Studies awaiting classification
We found one study awaiting classification that has not provided usable outcome data at this time (Kolomazník 2002; see Characteristics of studies awaiting classification table).
Ongoing trials
We identified no ongoing studies.
Risk of bias in included studies
A summary of the risk of bias in included studies are provided graphically in Figure 2 and Figure 3.
2.

Risk of bias graph: review authors' judgments about each risk of bias item presented as percentages across all included studies.
3.

Risk of bias summary: review authors' judgments about each risk of bias item for each included study.
Allocation
Random sequence generation
Eleven of 31 studies were at low risk of bias because they employed an appropriate method of generating a random sequence (Buvat 2009; Gameel 2013; Mattos 2008; McMahon 2013; Mendels 1995; Pryor 2006; Safarinejad 2006b; Safarinejad 2006c; Safarinejad 2007; Safarinejad 2008; Waldinger 1998). The remaining 20 studies were at unclear risk because they did not explicitly describe the method of random sequence generation (Figure 2; Figure 3).
Allocation concealment
Eight of 31 studies were at low risk of bias because they implemented appropriate mechanisms to ensure that individuals enrolling participants were unaware of the upcoming group assignment for that participant (Buvat 2009; Mattos 2008; McMahon 2013; Novaretti 2002; Pryor 2006; Safarinejad 2006b; Safarinejad 2007; Safarinejad 2008). The 23 remaining studies were at unclear risk because they did not explicitly describe the methods utilized to ensure allocation concealment (Figure 2; Figure 3).
Blinding
Blinding of participants and personnel
Fifteen of 31 studies appropriately blinded both participants and personnel and were at low risk of bias (Ahn 1996; Atmaca 2002; Biri 1998; Kaufman 2009; Mattos 2008; McMahon 2013; Mendels 1995; Novaretti 2002; Pryor 2006; Safarinejad 2006b; Safarinejad 2006c; Safarinejad 2007; Safarinejad 2008; Waldinger 1994; Waldinger 1998). Twelve studies were at unclear risk of bias because they did not clearly describe which party was blinded (Athanasios 2007; Buvat 2009; Farnia 2009; Gong 2011; Hamidi Madani 2016; Kara 1996; Khelaia 2012; Kim 1998; McMahon 2010; Na 1996; Shang 2012; Yilmaz 1999). Four studies were at high risk of bias because they were single‐blind in which personnel were not blinded (Gameel 2013; McMahon 1998; McMahon 1999; Tuncel 2008). (Figure 2; Figure 3).
Blinding of outcome assessment
For participant‐reported outcomes, 26 studies were at low risk of bias because participants appeared to adequately blinded and five studies were at unclear risk of bias (Buvat 2009; Farnia 2009; Hamidi Madani 2016; Khelaia 2012; Na 1996). No study was at high risk (Figure 2; Figure 3).
For investigator‐assessed outcomes, seven studies were at low risk of bias because the outcome assessors were adequately blinded (Ahn 1996; Biri 1998; McMahon 2013; Novaretti 2002; Pryor 2006; Safarinejad 2006b; Safarinejad 2007). Twenty studies were at unclear risk because it was not clearly described whether outcome assessors were blinded (Athanasios 2007; Atmaca 2002; Buvat 2009; Farnia 2009; Gong 2011; Hamidi Madani 2016; Kara 1996; Kaufman 2009; Khelaia 2012; Kim 1998; Mattos 2008; McMahon 2010; Mendels 1995; Na 1996; Safarinejad 2006c; Safarinejad 2008; Shang 2012; Waldinger 1994; Waldinger 1998; Yilmaz 1999) Four studies were at high risk of bias because the investigators were not blinded (Gameel 2013; McMahon 1998; McMahon 1999; Tuncel 2008). (Figure 2; Figure 3).
All studies were at low risk of bias for the IELT outcome because this is an objectively assessed measure that would have been expected to be affected by blinding or lack thereof in terms of detection bias (Figure 2; Figure 3).
Incomplete outcome data
We assessed the risk of attrition bias on a per‐outcome basis but then collapsed these rating into one group since all judgments were identical. Twelve studies were at low risk of bias (Ahn 1996; Gameel 2013; Gong 2011; Mattos 2008; McMahon 1998; McMahon 1999; Novaretti 2002; Pryor 2006; Safarinejad 2006b; Safarinejad 2007; Shang 2012; Tuncel 2008). Thirteen studies were at unclear risk of bias as the proportion of randomized participants not included in the analyses was not clearly reported and the risk of attrition bias could not be estimated (Athanasios 2007; Atmaca 2002; Biri 1998; Farnia 2009; Hamidi Madani 2016; Kaufman 2009; Khelaia 2012; McMahon 2013; Mendels 1995; Safarinejad 2006c; Safarinejad 2008; Waldinger 1998; Yilmaz 1999). Six studies were at high risk of bias because large proportions of participants were excluded from the final analysis (Buvat 2009; Kara 1996; Kim 1998; McMahon 2010; Na 1996; Waldinger 1994).
Selective reporting
Four studies were at low risk of bias as they reported all outcomes according to their protocol and conducted their analyses according to their a priori plans (Buvat 2009; McMahon 2010; McMahon 2013; Pryor 2006). Twenty‐five studies were at unclear risk of bias because the no study protocols were available (Ahn 1996; Athanasios 2007; Atmaca 2002; Biri 1998; Farnia 2009; Gameel 2013; Gong 2011; Hamidi Madani 2016; Kara 1996; Khelaia 2012; Kim 1998; Mattos 2008; McMahon 1998; McMahon 1999; Mendels 1995; Na 1996; Novaretti 2002Safarinejad 2006b; Safarinejad 2006c; Safarinejad 2007; Safarinejad 2008; Shang 2012; Tuncel 2008; Waldinger 1994; Yilmaz 1999). Two studies were at high risk of bias because one did not complete report outcomes on one of their group (Kaufman 2009), and another did not completely report on side effects (Waldinger 1998) (Figure 2; Figure 3).
Other potential sources of bias
Twenty‐seven studies were at low risk of bias (Ahn 1996; Athanasios 2007; Atmaca 2002; Biri 1998; Buvat 2009; Farnia 2009; Gameel 2013; Gong 2011; Kara 1996; Kaufman 2009; Kim 1998; McMahon 1998; McMahon 1999; McMahon 2010; McMahon 2013; Na 1996; Novaretti 2002; Pryor 2006; Safarinejad 2006b; Safarinejad 2006c; Safarinejad 2007; Safarinejad 2008; Shang 2012; Tuncel 2008; Waldinger 1994; Waldinger 1998; Yilmaz 1999). Three studies were at unclear risk of bias because there was imbalance in the baseline characteristics (Mendels 1995), or they were only reported in abstract form and there was insufficient information to make a judgment (Hamidi Madani 2016; Khelaia 2012). One study was at high risk of bias because it only evaluated specific adverse effects (Mattos 2008) (Figure 2; Figure 3).
Effects of interventions
See: Table 1
Primary outcomes
1.1 Participant perception of change with treatment
SSRI treatment probably results in an improvement in PE‐related symptoms defined as a rating of 'better' or 'much better' using the CGIC questionnaire compared to placebo (RR 1.92, 95% CI 1.66 to 2.23; I² = 24%; studies = 6, participants = 3260; Analysis 1.1; Figure 4). Compared to placebo and a baseline risk of 220 per 1000 men, this corresponds to 202 more men per 1000 (95% CI 145 more to 270 more) perceiving that their condition as 'better' or 'much better' with SSRIs.
4.

Forest plot of comparison: 1 SSRI versus placebo, outcome: 1.1 Participant perception of change with treatment.
We rated the certainty of evidence as moderate, downgrading one level due to serious study limitations given that of the six studies included in this analysis, four had an unclear risk of selection bias, three had an unclear risk of performance bias and one had an unclear risk of detection bias. In addition, two were at high risk for attrition bias.
1.2 Participant satisfaction with intercourse
SSRI treatment probably improves satisfaction with intercourse defined as a rating of 'good' or 'very good' using the CGIC questionnaire compared to placebo (RR 1.63, 95% CI 1.42 to 1.87; I² = 53%; studies = 3, participants = 4273; Analysis 1.2; Figure 5). Compared to placebo and a baseline risk of 278 per 1000 men, this corresponds to 175 more men per 1000 (95% CI 117 more to 242 more) describing their satisfaction with intercourse as being 'good' or 'very good' with SSRIs.
1.2. Analysis.

Comparison 1: SSRI versus placebo, Outcome 2: Participant satisfaction with intercourse
5.

Forest plot of comparison: 1 SSRI versus placebo, outcome: 1.2 Participant satisfaction with intercourse.
We rated the certainty of evidence as moderate, downgrading one level due to serious study limitations. Two of three included studies were at unclear risk of selection bias, one was at unclear risk of performance bias and one study that contributed a weight of 61.6% to the analysis was at high risk of attrition bias. However, we did not downgrade for the I² statistic of 53% since we did not judge the observed inconsistency to be clinically relevant.
1.3 Study withdrawal due to adverse events
SSRI treatment may result in an increase in the number of treatment cessations due to adverse events compared to placebo (RR 3.80, 95% CI 2.61 to 5.51; I² = 0%; studies = 20, participants = 7367; Analysis 1.3; Figure 6). Compared to placebo and a baseline risk of 11 per 1000 men, this corresponds to 30 more men per 1000 (95% CI 17 more to 49 more) stopping treatment due to adverse events due to SSRI treatment.
1.3. Analysis.

Comparison 1: SSRI versus placebo, Outcome 3: Study withdrawal due to adverse events
6.

Forest plot of comparison: 1 SSRI versus placebo, outcome: 1.3 Study withdrawal due to adverse events.
We rated the certainty of evidence as low, downgrading two levels due to very serious study limitations because more than half the included studies were at unclear risk of selection bias or performance bias, or both. Four studies were at high risk of attrition bias for this outcome and two studies were at high risk of selective reporting bias.
Secondary outcomes
1.4 Perceived control over ejaculation
SSRI treatment probably improves participants' control over ejaculation defined as a rating of 'good' or 'very good' based on the PEP questionnaire compared to placebo (RR 2.29, 95% CI 1.72 to 3.05; I² = 75%; studies = 3, participants = 4273; Analysis 1.4). Compared to placebo and a baseline risk of 132 per 1000 men, this corresponds to 170 more men per 1000 (95% CI 95 more to 270 more) describing their control over ejaculation as being 'good' or 'very good' with SSRIs.
1.4. Analysis.

Comparison 1: SSRI versus placebo, Outcome 4: Perceived control over ejaculation
We rated the certainty of evidence as moderate, downgrading one level due to serious study limitations. Two of three studies had an unclear risk of selection bias, one had an unclear risk of performance bias and one had a high risk of attrition bias.
1.5 Participant distress about premature ejaculation
SSRI treatment probably decreases PE‐related distress defined as 'a little bit' or 'not at all' distressing based on the PEP questionnaire compared to placebo (RR 1.54, 95% CI 1.26 to 1.88; studies = 1, participants = 652; Analysis 1.5). Compared to placebo and a baseline risk of 353 per 1000 men, this corresponds to 191 men more per 1000 (95% CI 92 more to 311 more) reporting their distress about PE as being only 'a little bit' or 'not at all' with SSRIs.
1.5. Analysis.

Comparison 1: SSRI versus placebo, Outcome 5: Participant distress about PE
We rated the certainty of evidence as moderate, downgrading one level due to serious study limitations because the only included study had unclear risk of selection bias, an unclear risk of attrition bias and a high risk of selective reporting bias.
1.6 Relationship difficulties
SSRI treatment may reduce relationship difficulties to only 'a little bit' or 'not at all' based on the PEP questionnaire compared to placebo (RR 1.20, 95% CI 1.07 to 1.34; studies = 1, participants = 652; Analysis 1.6). Compared to placebo, this corresponds to 129 men more per 1000 (95% CI 45 more to 218 more) reporting their relationship difficulties as being only 'a little bit' or 'not at all' with SSRIs.
1.6. Analysis.

Comparison 1: SSRI versus placebo, Outcome 6: Relationship difficulties
We rated the certainty of evidence as low, downgrading one level each for serious study limitations and imprecision. The only included study had an unclear risk of selection bias, an unclear risk of attrition bias and a high risk of selective reporting bias. We perceived the absolute effect size to cross the threshold for a clinically important difference of 10% and, therefore, downgraded a further level for imprecision.
1.7 Adverse events
SSRI treatment probably increases adverse events substantially compared to placebo (RR 1.71, 95% CI 1.48 to 1.99; I² = 41%; studies = 17, participants = 4624; Analysis 1.7). Compared to placebo and a baseline risk of 243 per 1000, this corresponds to 173 more adverse events per 1000 men (95% CI 117 more to 241 more).
1.7. Analysis.

Comparison 1: SSRI versus placebo, Outcome 7: Adverse events
We rated the certainty of evidence as moderate, downgrading one level due to serious study limitations because more than half the included studies were rated as unclear risk for selection bias or performance bias, or both. Two studies had a high risk of attrition bias and over half had an unclear risk of selective reporting bias.
1.8 Intravaginal ejaculatory latency time
SSRI treatment may increase IELT compared to placebo (MD 3.09 minutes longer, 95% CI 1.94 longer to 4.25 longer; I² = 99%; studies = 20, participants = 5872; Analysis 1.8).
1.8. Analysis.

Comparison 1: SSRI versus placebo, Outcome 8: Intravaginal ejaculatory latency time
We rated the certainty of evidence as low, downgrading one level due to serious study limitations; most studies had an unclear or high risk of selection, performance, attrition and reporting bias. We also downgraded one level for serious concerns about inconsistency. These may in part be attributable to the duration of action (long versus short acting; Analysis 3.4) and type of SSRI (Analysis 3.4).
3.4. Analysis.

Comparison 3: Subgroup analysis: comparison of long‐acting agents, Outcome 4: Intravaginal ejaculatory latency time
1.9 Depression
We are very uncertain whether SSRI treatment compared to placebo increases depression (RR 2.00, 95% CI 0.23 to 17.34; studies = 1, participants = 14; Analysis 1.9). We rated the certainty of evidence as very low, downgrading due to serious study limitations (unclear risk of selection and performance bias, high risk of attrition bias and unclear risk of selective reporting bias) and very serious imprecision.
Subgroup analyses
2 Long‐acting versus short‐acting SSRIs
2.1 Participant perception of change with treatment
The RR for participant perception of change with treatment as being 'better' or 'much better' was 8.48 (95% CI 2.21 to 32.51) for long‐acting SSRIs and 1.87 (95% CI 1.66 to 2.10) for short‐acting SSRIs (Analysis 2.1). The test for interaction was significant (P = 0.03; I² = 79.3%).
2.1. Analysis.

Comparison 2: Subgroup analysis: long‐acting versus short‐acting SSRI, Outcome 1: Participant perception of change with treatment
2.2 Participant satisfaction with intercourse
There were no studies of long‐acting SSRIs that evaluated participant satisfaction with intercourse.
2.3 Study withdrawal due to adverse events
The RR for study withdrawal due to adverse events was 2.00 (95% CI 0.92 to 4.34) for long‐acting SSRIs and 4.33 (95% CI 2.60 to 7.23) for short‐acting SSRIs (Analysis 2.3). The test for interaction was not significant (P = 0.10; I² = 62.4%).
2.3. Analysis.

Comparison 2: Subgroup analysis: long‐acting versus short‐acting SSRI, Outcome 3: Study withdrawal due to adverse events
2.4 Perceived control over ejaculation
There were no studies of long‐acting SSRIs that evaluated perceived control over ejaculation.
2.5 Participant distress about premature ejaculation
There were no studies of long‐acting SSRIs that evaluated participant distress about PE.
2.6 Relationship difficulties
There were no studies of long‐acting SSRIs that evaluated relationship difficulties.
2.7 Adverse events
The RR for adverse events was 1.90 (95% CI 1.37 to 2.64) for long‐acting SSRIs and 1.70 (95% CI 1.42 to 2.03) for short‐acting SSRIs (Analysis 2.7). The test for interaction was not significant (P = 0.54; I² = 0%).
2.7. Analysis.

Comparison 2: Subgroup analysis: long‐acting versus short‐acting SSRI, Outcome 7: Adverse events
2.8 Intravaginal ejaculatory latency time
The MD for IELT was 3.36 minutes (95% CI 1.62 to 5.10) for long‐acting SSRIs and 1.52 minutes (95% CI 1.27 to 1.77) for short‐acting SSRIs (Analysis 2.8). The test for interaction was significant (P = 0.04; I² = 76.2%).
2.8. Analysis.

Comparison 2: Subgroup analysis: long‐acting versus short‐acting SSRI, Outcome 8: Intravaginal ejaculatory latency time
2.9 Depression
There were no studies of short‐acting SSRIs that evaluated depression.
3 Types of long‐acting SSRIs
3.1 Participant perception of change with treatment
We found one study of citalopram (Atmaca 2002) and one of duloxetine (Athanasios 2007), which evaluated participant perception of change with treatment. The RR for participant perception of change with treatment as being 'better' or 'much better' was 9.00 (95% CI 1.32 to 61.24) for citalopram and 8.00 (95% CI 1.21 to 52.69) for duloxetine (Analysis 3.1). The test for interaction was not significant (P = 0.93; I² = 0%).
3.1. Analysis.

Comparison 3: Subgroup analysis: comparison of long‐acting agents, Outcome 1: Participant perception of change with treatment
3.2 Participant satisfaction with intercourse
There were no studies of long‐acting SSRIs that evaluated participant satisfaction with intercourse.
3.3 Study withdrawal due to adverse events
We found 14 studies of long‐acting SSRIs that evaluated this outcome.
The RR for study withdrawal due to adverse events was 3.00 (95% CI 0.13 to 70.74) for citalopram, 7.64 (95% CI 0.99 to 58.71) for dapoxetine, not estimable for duloxetine, 2.00 (95% CI 0.37 to 10.74) for escitalopram, 2.59 (95% CI 0.34 to 19.59) for fluoxetine, 1.54 (95% CI 0.09 to 25.86) for fluvoxamine, 1.76 (95% CI 0.35 to 8.91) for paroxetine and 0.43 (95% CI 0.05 to 3.56) for sertraline (Analysis 3.2). The test for interaction was not significant (P = 0.69; I² = 0%).
3.2. Analysis.

Comparison 3: Subgroup analysis: comparison of long‐acting agents, Outcome 2: Study withdrawal due to adverse events
3.4 Perceived control over ejaculation
There were no studies of long‐acting SSRIs that evaluated perceived control over ejaculation.
3.5 Participant distress about premature ejaculation
There were no studies of long‐acting SSRIs that evaluated participant distress about PE.
3.6 Relationship difficulties
There were no studies of long‐acting SSRIs that evaluated relationship difficulties.
3.7 Adverse events
We found 13 studies of long‐acting SSRIs that evaluated adverse effects. The RR for adverse effects was 3.00 (95% CI 0.51 to 17.57) for citalopram, 4.40 (95% CI 1.06 to 18.32) for clomipramine, 2.54 (95% CI 1.34 to 4.81) for dapoxetine, 3.00 (95% CI 0.37 to 24.17) for duloxetine, 1.69 (95% CI 0.69 to 4.15) for escitalopram, 2.50 (95% CI 1.29, to 4.86) for fluoxetine, 2.50 (95% CI 0.91 to 6.90) for paroxetine and 1.33 (95% CI 0.74 to 2.39) for sertraline (Analysis 3.3). The test for interaction was not significant (P = 0.71; I² = 0%).
3.3. Analysis.

Comparison 3: Subgroup analysis: comparison of long‐acting agents, Outcome 3: Adverse events
3.8 Intravaginal ejaculatory latency time
We found 14 studies of long‐acting SSRIs that evaluated IELT. The MD for IELT was 4.85 (95% CI 3.14 to 6.56) for citalopram, 1.52 (95% CI 0.80 to 2.24) for duloxetine, 2.46 (95% CI 1.51 to 3.39) for fluoxetine, 0.59 (95% CI –0.35 to 1.53) for fluvoxamine, 6.51 (95% CI 0.33 to 12.68) for paroxetine and 2.55 (95% CI 1.54 to 3.56) for sertraline (Analysis 3.4). The test for interaction was significant (P < 0.001, I² = 80.0%).
3.9 Depression
We only found one study using long‐acting fluoxetine that evaluated depression and were unable to perform any secondary analyses (Kara 1996).
4 Different doses: dapoxetine
4.1 Participant perception of change with treatment
We found four studies that administered dapoxetine at the following doses: 30 mg daily (McMahon 2010), 30 mg on‐demand (Buvat 2009; McMahon 2013), 60 mg daily (McMahon 2010), and 60 mg on‐demand (Buvat 2009; Kaufman 2009). The RR for participant perception of change with treatment as being 'better' or 'much better' was 1.87 (95% CI 1.37 to 2.54) with 30 mg daily, 2.00 (95% CI 1.33 to 3.01) with 30 mg on‐demand, 1.68 (95% CI 1.23 to 2.30) with 60 mg daily and 1.98 (95% CI 1.58 to 2.48) with 60 mg on‐demand (Analysis 4.1). The test for interaction was not significant (P = 0.85; I² = 0%).
4.1. Analysis.

Comparison 4: Subgroup analysis: different doses of dapoxetine, Outcome 1: Participant perception of change with treatment
4.2 Participant satisfaction with intercourse
We found three studies that administered dapoxetine at the following doses: 30 mg daily (McMahon 2010), 30 mg on‐demand (Pryor 2006), 60 mg daily (McMahon 2010), and 60 mg on‐demand (Kaufman 2009). The RR for participant satisfaction with intercourse defined as a rating of 'good' or 'very good' was 1.41 (95% CI 1.08 to 1.85) with 30 mg daily, 1.59 (95% CI 1.33 to 1.90) with 30 mg on‐demand, 1.39 (95% CI 1.07 to 1.82) with 60 mg daily and 1.61 (95% CI 1.32 to 1.98) with 60 mg on‐demand (Analysis 4.2). The test for interaction was not significant (P = 0.74; I² = 0%).
4.2. Analysis.

Comparison 4: Subgroup analysis: different doses of dapoxetine, Outcome 2: Participant satisfaction with intercourse
4.3 Study withdrawal due to adverse events
We found three studies that administered dapoxetine at the following doses: 30 mg daily (McMahon 2010), 30 mg on‐demand (Buvat 2009; McMahon 2013; Pryor 2006), 60 mg daily (McMahon 2010; Safarinejad 2006b; Safarinejad 2008), and 60 mg on‐demand (Buvat 2009; Kaufman 2009; Pryor 2006). The RR for study withdrawal due to adverse events was 3.03 (95% CI 0.37 to 25.01) with 30 mg daily, 2.44 (95% CI 1.06 to 5.59) with 30 mg on‐demand, 8.76 (95% CI 2.10 to 36.49) with 60 mg daily and 6.51 (95% CI 3.64 to 11.66) with 60 mg on‐demand (Analysis 4.3). The test for interaction was not significant (P = 0.22, I² = 33%).
4.3. Analysis.

Comparison 4: Subgroup analysis: different doses of dapoxetine, Outcome 3: Study withdrawal due to adverse events
4.4 Perceived control over ejaculation
We found three studies that administered dapoxetine at the following doses: 30 mg daily (McMahon 2010), 30 mg on‐demand (Pryor 2006), 60 mg daily (McMahon 2010), and 60 mg on‐demand (Kaufman 2009; Pryor 2006). The RR of participants' control over ejaculation defined as a rating of 'good' or 'very good' was 1.79 (95% CI 1.26 to 2.53) with 30 mg daily, 3.70 (95% CI 2.72 to 5.04) with 30 mg on‐demand, 1.78 (95% CI 1.26 to 2.52) with 60 mg daily and 2.28 (95% CI 1.65 to 3.16) with 60 mg on‐demand (Analysis 4.4). The test for interaction was significant (P = 0.004; I² = 77.2%).
4.4. Analysis.

Comparison 4: Subgroup analysis: different doses of dapoxetine, Outcome 4: Perceived control over ejaculation
4.5 Participant distress about premature ejaculation
We found one study that administered dapoxetine 60 mg on‐demand (Kaufman 2009). The RR for PE‐related distress defined as a rating of its severity of only 'a little bit' or 'not at all' was 1.54 (95% CI 1.26 to 1.88; Analysis 4.5). We could not test for subgroup differences.
4.5. Analysis.

Comparison 4: Subgroup analysis: different doses of dapoxetine, Outcome 5: Participant distress about PE
4.6 Relationship difficulties
We found one study that administered dapoxetine 60 mg on‐demand (Kaufman 2009). The RR for reducing relationship difficulties to only 'a little bit' or 'not at all' with this study was 1.20 (95% CI 1.07 to 1.34; Analysis 4.6). We could not test for subgroup differences.
4.6. Analysis.

Comparison 4: Subgroup analysis: different doses of dapoxetine, Outcome 6: Relationship difficulties
4.7 Adverse events
We found five studies that administered dapoxetine at the following doses: 30 mg daily (McMahon 2010; McMahon 2013), 30 mg on‐demand (Buvat 2009), 60 mg daily (McMahon 2010; Safarinejad 2006b; Safarinejad 2008), and 60 mg on‐demand (Buvat 2009; Kaufman 2009). The RR for adverse events was 1.64 (95% CI 1.30 to 2.07) with 30 mg daily, 1.47 (95% CI 1.20 to 1.79) with 30 mg on‐demand, 2.73 (95% CI 2.03 to 3.66) with 60 mg daily and 1.56 (95% CI 1.23 to 1.99) with 60 mg on‐demand (Analysis 4.7). The test for interaction was significant (P = 0.006; I² = 76.2%).
4.7. Analysis.

Comparison 4: Subgroup analysis: different doses of dapoxetine, Outcome 7: Adverse events
4.8 Intravaginal ejaculatory latency time
We found four studies that administered dapoxetine as the following doses: 30 mg daily (McMahon 2010), 30 mg on‐demand (Buvat 2009; McMahon 2013; Pryor 2006), 60 mg daily (McMahon 2010), and 60 mg on‐demand (Buvat 2009; Pryor 2006). The MD for IELT was 1.80 (95% CI 1.27 to 2.33) with 30 mg daily, 1.37 (95% CI 0.86 to 1.89) with 30 mg on‐demand, 1.50 (95% CI 0.98 to 2.02) with 60 mg daily and 1.53 (95% CI 1.09 to 1.97) with 60 mg on‐demand (Analysis 4.8). The test for interaction was not significant (P = 0.71, I² = 0%).
4.8. Analysis.

Comparison 4: Subgroup analysis: different doses of dapoxetine, Outcome 8: Intravaginal ejaculatory latency time
4.9 Depression
We found no studies using dapoxetine that evaluated depression.
5 Different doses: fluoxetine
5.1 Participant perception of change with treatment
We found no studies using fluoxetine that evaluated participant perception of change with treatment.
5.2 Participant satisfaction with intercourse
We found no studies using fluoxetine that evaluated participant satisfaction with intercourse.
5.3 Study withdrawal due to adverse events
We found three studies that administered fluoxetine 20 mg daily (Kara 1996; Waldinger 1998; Yilmaz 1999). The RR for study withdrawal due to adverse events using this dose was 2.09 (95% CI 0.26 to 16.82; Analysis 5.1). We could not test for subgroup differences.
5.1. Analysis.

Comparison 5: Subgroup analysis: different doses of fluoxetine, Outcome 1: Study withdrawal due to adverse events
5.4 Perceived control over ejaculation
We found no studies using fluoxetine that evaluated perceived control over ejaculation.
5.5 Participant distress about premature ejaculation
We found no studies using fluoxetine that evaluated participant distress about PE.
5.6 Relationship difficulties
We found no studies using fluoxetine that evaluated relationship difficulties.
5.7 Adverse events
We found four studies that administered fluoxetine at the following doses: 20 mg daily (Kara 1996; Yilmaz 1999), 40 mg daily (Ahn 1996), and 90 mg daily (Mattos 2008). The RR for adverse events was 9.32 (95% CI 1.88 to 46.26) with 20 mg daily, 2.29 (95% CI 0.55 to 9.49) with 40 mg daily and 1.78 (95% CI 0.76 to 4.17) with 90 mg daily (Analysis 5.2). The test for interaction was not significant (P = 0.2; I² = 37.9%).
5.2. Analysis.

Comparison 5: Subgroup analysis: different doses of fluoxetine, Outcome 2: Adverse events
5.8 Intravaginal ejaculatory latency time
We found five studies that administered fluoxetine at the following doses: 20 mg daily (Kara 1996; Waldinger 1998; Yilmaz 1999), 40 mg daily (Ahn 1996), and 90 mg daily (Mattos 2008). The MD for IELT was 2.87 (95% CI 1.26 to 4.48) with 20 mg daily, –0.54 (95% CI –3.54 to 2.46) with 40 mg daily and 2.72 (95% CI 1.83 to 3.61) with 90 mg daily (Analysis 5.3). The test for interaction was not significant (P = 0.11, I² = 54.1%).
5.3. Analysis.

Comparison 5: Subgroup analysis: different doses of fluoxetine, Outcome 3: Intravaginal ejaculatory latency time
5.9 Depression
We found one study that administered fluoxetine 20 mg daily (Kara 1996). The RR for depression in this study was 2.00 (95% CI 0.23 to 17.34; Analysis 5.4). We could not test for subgroup differences.
5.4. Analysis.

Comparison 5: Subgroup analysis: different doses of fluoxetine, Outcome 4: Depression
Discussion
Summary of main results
We included 31 RCTs with 8254 participants and found that compared to placebo, SSRI treatment for PE probably improves perception of change with treatment, satisfaction with intercourse, perceived control over ejaculation, participant distress about PE, relationship difficulties and IELT. However, the administration of SSRIs may increase study withdrawals due to adverse events and probably increases adverse events.
Overall completeness and applicability of evidence
This review included 31 RCTs of 8254 participants with PE with diverse clinical characteristics that, therefore, likely reflect the population encountered in day‐to‐day clinical practice. They also included a range of SSRI drugs and dosing schedules utilized in the included trials.
The review did not include any active comparators and, therefore, is unable to address how these drugs compare to other management approaches such as topical anesthetics, tramadol or α1‐adrenoreceptor antagonists, which are recommended as treatment alternatives in the recent AUA guideline (Shindel 2020).
A specific concern in the use of SSRI for depression is the potential risk of promoting suicidal ideation, although this remains an issue of controversy (Khan 2003; Sharma 2016). The reported adverse events and study withdrawals of the included studies did not provide a signal for this outcome, but we also recognize that the overall number of participants and the relatively short follow‐up of these studies limit the ability to identify infrequent outcomes that might be associated with long‐term use.
Quality of the evidence
We consistently downgraded the certainty of evidence by one or two steps to moderate or low. Our confidence in the estimates of effect were primarily limited by study limitations and heterogeneity. Most studies were classified at unclear or high risk of bias for multiple domains and, therefore, the potential biases in those studies introduced a degree of uncertainty in the calculated summary estimates.
Potential biases in the review process
Despite a comprehensive search strategy without any publication or language restrictions, there is a possibility that we may have missed studies published in a language other than English, published in non‐indexed journals or unpublished.
There were fewer than 10 studies included for most outcomes and, therefore, we were unable to generate funnel plots thus possibly underestimating the risk of publication bias.
We contacted authors of each of the studies for further information, but only one responded to these requests (Mattos 2008), and this may be a further source of bias.
One author contributing several individual studies to this review, which were all at unclear risk of selective bias (as most included studies of this review) has had six studies on men's sexual health retracted due to alleged fraud (Retractionwatch 2015). Since none of the included studies were involved (Safarinejad 2006b; Safarinejad 2006c; Safarinejad 2007; Safarinejad 2008), we included these studies in this review. However, it does underscore the issue of how important a priori trial registration is (Roberts 2015).
Agreements and disagreements with other studies or reviews
There is a limited number of reviews that have compared SSRIs with placebo for PE. In contrast to our review, which focused on outcome of direct patient importance, they typically used IELT as a primary outcome. Also, none applied the same methodologic rigor as we applied in this review.
Castiglione 2016 assessed various pharmacologic interventions for PE using IELT as the primary outcome found that SSRIs prolonged IELT compared to placebo based on the 14 included trials.
Zhang 2019 found that paroxetine was more effective than fluoxetine and escitalopram in delaying ejaculation. The review also found that paroxetine combined with tadalafil or behavior therapy was more effective than paroxetine alone. This is consistent with Sun 2017, which reported that the pooled effects of SSRIs were superior to placebo in prolonging IELT in men with PE but found that SSRI alone was inferior to combination treatment of SSRI and phosphodiesterase‐5 inhibitors. However, there was no difference in IELT between paroxetine, tramadol, sertraline, phosphodiesterase 5 inhibitors, topical lidocaine gel, behavioral therapy or dapoxetine (Zhang 2019). These assessments were outside the scope of this review which focused on the comparison with placebo/no intervention.
Again using IELT as the primary outcome, one network meta‐analysis reported that a range of SSRI agents outperformed placebo (Jian 2018). However, this study reported that topical anesthetics or phosphodiesterase‐5 inhibitors plus SSRIs were likely to be the most efficacious treatment strategies for PE.
Another network meta‐analysis of 44 studies including a range of pharmacologic agents for PE reported that dapoxetine was likely to be the most efficacious (Sridharan 2018). Similar to this review, Sridharan 2018 also found that dapoxetine, venlafaxine and fluoxetine all increased the incidence of adverse events.
Other relevant document are currently available guidelines on this topic. These use varying methodology when it comes not only to the framework of moving from evidence to recommendations but also to what extent these are supported by rigorous systematic reviews.
The European Association for Urology (EAU) guidelines on ED, PE, penile curvature and priapism recommend pharmacotherapy as first‐line therapy of lifelong PE (grade A) states that on‐demand dapoxetine (as the only approved pharmacologic therapy for PE) or other off‐label antidepressants such as daily SSRIs (Hatzimouratidis 2010). This report was supported by a literature search; then "… the panel reviewed and selected the articles with the highest evidence available." The EAU did not perform its own meta‐analysis.
The International Society of Sexual Medicine's Guidelines for the Diagnosis and Treatment of PE states that there is "robust evidence to support the efficacy and safety of on‐demand dosing of dapoxetine for the treatment of lifelong and acquired PE" and to "support the efficacy and safety of off‐label daily dosing of the SSRIs paroxetine sertraline, citalopram, fluoxetine" (Althof 2014). These recommendations were supported by a comprehensive literature search and a consensus‐based process.
Guidelines of the AUA are the most recent; they are also the most methodologically rigorous supported by a systematic review conducted by the Pacific Northwest Evidence‐based Practice Centre that was up‐to‐date up to March 2019 (Shindel 2020). This document makes a strong recommendation that "clinicians should recommend daily SSRIs; on‐demand clomipramine or dapoxetine (where available) … as first‐line pharmacotherapies in the treatment of PE." However, the guideline group did not conduct their meta‐analysis or own update meta‐analyses from previously published reviews systematic reviews.
Authors' conclusions
Implications for practice.
Compared to placebo, the administration of selective serotonin re‐uptake inhibitors (SSRIs) for premature ejaculation (PE) may improve perception of change with treatment and satisfaction with intercourse. SSRIs may also improve perceived control over ejaculation and reduce both distress about PE and relationship difficulties. These potential benefits need to be weighed up against the possible increase in adverse events with SSRIs. Moreover, men should be counseled about the low certainty of evidence in this subject and, therefore, the possibility that the effects they experience from SSRI treatment for PE may be different to that shown in this review.
Implications for research.
Considering the moderate‐ to low‐certainty evidence for the patient‐centered outcomes assessed in this review, future trials should be designed and conducted with higher methodologic standards so that we can have more certainty in the estimates. Future studies should also focus on patient‐important outcomes such as perception of change with treatment, satisfaction with intercourse, perceived control over ejaculation, participant distress about PE and relationship difficulties, which only a limited number of trials included in this review measured. Additionally, it is important that the effectiveness of SSRIs is compared to other active treatments directly to characterize the most efficacious management option. Currently, we are mostly relying on indirect evidence when trying to choose between the available pharmacologic agents (Sridharan 2018).
History
Protocol first published: Issue 9, 2017 Review first published: Issue 3, 2021
Notes
We have based parts of the Methods and Appendix 2 sections of this Cochrane Review on a standard template established by the Cochrane Metabolic and Endocrine Disorders Group.
Acknowledgements
We thank Cochrane Urology for its support. We are grateful to Dr Yu Xie for translating articles. We are also appreciative of the feedback provided by Dr Josip Vukina, MD, MPH (University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania, USA) and Dr Ege Can Serefoglu, MD, FECSM (Professor of Urology, Biruni University School of Medicine, Istanbul, Turkey; Editor‐in‐Chief, International Journal of Impotence Research, London, UK) who served as peer referees.
Appendices
Appendix 1. Cochrane CENTRAL (Wiley) search strategy
| #1 | [mh "Premature Ejaculation"] |
| #2 | "early ejaculation":ti,ab,kw OR "rapid ejaculation":ti,ab,kw OR "rapid climax":ti,ab,kw OR "premature climax":ti,ab,kw OR "ejaculatio praecox":ti,ab,kw OR "ejaculatio precox":ti,ab,kw OR "premature ejaculation":ti,ab,kw OR "premature ejaculations":ti,ab,kw OR "early ejaculations":ti,ab,kw OR "premature ejaculator":ti,ab,kw OR "premature ejaculators":ti,ab,kw |
| #3 | #1 OR #2 |
| #4 | [mh "Serotonin Uptake Inhibitors"] OR [mh "Serotonin and Noradrenaline Reuptake Inhibitors"] |
| #5 | "5‐ht uptake inhibitor":ti,ab,kw OR "5‐ht uptake inhibitors":ti,ab,kw OR "5‐hydroxytryptamine uptake inhibitor":ti,ab,kw OR "5‐hydroxytryptamine uptake inhibitors":ti,ab,kw OR "serotonin and noradrenaline re uptake inhibitor":ti,ab,kw OR "serotonin and noradrenaline reuptake inhibitor":ti,ab,kw OR "serotonin and noradrenaline reuptake inhibitors":ti,ab,kw OR "serotonin and norepinephrine re uptake inhibitor":ti,ab,kw OR "serotonin and norepinephrine reuptake inhibitor":ti,ab,kw OR "serotonin and norepinephrine reuptake inhibitors":ti,ab,kw OR "serotonin norepinephrine re uptake inhibitor":ti,ab,kw OR "serotonin norepinephrine reuptake inhibitor":ti,ab,kw OR "serotonin norepinephrine reuptake inhibitors":ti,ab,kw OR "serotonin reuptake inhibitor":ti,ab,kw OR "serotonin reuptake inhibitor":ti,ab,kw OR "serotonin reuptake inhibitors":ti,ab,kw OR "serotonin uptake inhibitor":ti,ab,kw OR "serotonin uptake inhibitor":ti,ab,kw OR "serotonin uptake inhibitors":ti,ab,kw OR "serotonine and noradrenaline reuptake inhibitor":ti,ab,kw OR "serotonine and noradrenaline reuptake inhibitors":ti,ab,kw OR "serotonine and norepinephrine re uptake inhibitor":ti,ab,kw OR "serotonine and norepinephrine reuptake inhibitor":ti,ab,kw OR "serotonine and norepinephrine reuptake inhibitors":ti,ab,kw OR "serotonine norepinephrine re uptake inhibitor":ti,ab,kw OR "serotonine norepinephrine reuptake inhibitor":ti,ab,kw OR "serotonine norepinephrine reuptake inhibitors":ti,ab,kw OR "serotonine reuptake inhibitor":ti,ab,kw OR "serotonine reuptake inhibitor":ti,ab,kw OR "serotonine reuptake inhibitors":ti,ab,kw OR "serotonine uptake inhibitor":ti,ab,kw OR "serotonine uptake inhibitor":ti,ab,kw OR "serotonine uptake inhibitors":ti,ab,kw OR "serotonine and noradrenaline re uptake inhibitor":ti,ab,kw OR snris:ti,ab,kw OR ssnris:ti,ab,kw OR ssris:ti,ab,kw OR snri:ti,ab,kw OR ssnri:ti,ab,kw OR ssri:ti,ab,kw |
| #6 | Cericlamine:ti,ab,kw OR [mh Citalopram] OR Citalopram:ti,ab,kw OR celexa:ti,ab,kw OR escitalopram:ti,ab,kw OR lexapro:ti,ab,kw OR Cipralex:ti,ab,kw |
| #7 | Dapoxetine:ti,ab,kw OR Priligy:ti,ab,kw OR Westoxetin:ti,ab,kw |
| #8 | [mh "Desvenlafaxine Succinate"] OR Desvenlafaxine:ti,ab,kw OR [mh "Duloxetine Hydrochloride"] OR Duloxetine:ti,ab,kw |
| #9 | femoxetine:ti,ab,kw OR [mh Fluoxetine] OR fluoxetine:ti,ab,kw OR prozac:ti,ab,kw OR Sarafem:ti,ab,kw |
| #10 | [mh Fluvoxamine] OR Fluvoxamine:ti,ab,kw OR luvox:ti,ab,kw |
| #11 | hydroxynefazodone:ti,ab,kw OR hyperforin:ti,ab,kw OR ifoxetine:ti,ab,kw OR indalpine:ti,ab,kw OR liafensine:ti,ab,kw |
| #12 | litoxetine:ti,ab,kw OR lubazodone:ti,ab,kw OR medifoxamine:ti,ab,kw OR milnacipran:ti,ab,kw |
| #13 | moxifetin:ti,ab,kw OR nefazodone:ti,ab,kw OR nomelidine:ti,ab,kw OR norcitalopram:ti,ab,kw |
| #14 | norfluoxetine:ti,ab,kw OR norsertraline:ti,ab,kw OR omiloxetine:ti,ab,kw |
| #15 | [mh Paroxetine] OR Paroxetine:ti,ab,kw OR paxil:ti,ab,kw OR Pexeva:ti,ab,kw OR [mh Sertraline] OR sertraline:ti,ab,kw OR zoloft:ti,ab,kw |
| #16 | tedatioxetine:ti,ab,kw OR [mh Trazodone] OR trazodone:ti,ab,kw OR Desyrel:ti,ab,kw |
| #17 | [mh "Vilazodone Hydrochloride"] OR Vilazodone:ti,ab,kw OR [mh "Venlafaxine Hydrochloride"] OR Venlafaxine:ti,ab,kw OR Pristiq:ti,ab,kw OR Effexor:ti,ab,kw OR Cymbalta:ti,ab,kw |
| #18 | [mh vortioxetine] OR vortioxetine:ti,ab,kw OR [mh Zimeldine] OR Zimeldine:ti,ab,kw OR zimlidine:ti,ab,kw OR zimelidin:ti,ab,kw |
| #19 | #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 |
| #20 | #3 AND #19 |
Appendix 2. MEDLINE (PubMed) search strategy
| #1 | "Premature Ejaculation"[mh] |
| #2 | "early ejaculation"[tw] OR "rapid ejaculation"[tw] OR "rapid climax"[tw] OR "premature climax"[tw] OR "ejaculatio praecox"[tw] OR "ejaculatio precox"[tw] OR "premature ejaculation"[tw] OR "premature ejaculations"[tw] OR "early ejaculations"[tw] OR "premature ejaculator"[tw] OR "premature ejaculators"[tw] |
| #3 | #1 OR #2 |
| #4 | Serotonin Uptake Inhibitors[mh] OR Serotonin Uptake Inhibitors[pa] OR "Serotonin and Noradrenaline Reuptake Inhibitors"[mh] OR "Serotonin and Noradrenaline Reuptake Inhibitors"[pa] |
| #5 | "5‐ht uptake inhibitor"[tw] OR "5‐ht uptake inhibitors"[tw] OR "5‐hydroxytryptamine uptake inhibitor"[tw] OR "5‐hydroxytryptamine uptake inhibitors"[tw] OR "serotonin and noradrenaline re uptake inhibitor"[tw] OR "serotonin and noradrenaline reuptake inhibitor"[tw] OR "serotonin and noradrenaline reuptake inhibitors"[tw] OR "serotonin and norepinephrine re uptake inhibitor"[tw] OR "serotonin and norepinephrine reuptake inhibitor"[tw] OR "serotonin and norepinephrine reuptake inhibitors"[tw] OR "serotonin norepinephrine re uptake inhibitor"[tw] OR "serotonin norepinephrine reuptake inhibitor"[tw] OR "serotonin norepinephrine reuptake inhibitors"[tw] OR "serotonin reuptake inhibitor"[tw] OR "serotonin reuptake inhibitor"[tw] OR "serotonin reuptake inhibitors"[tw] OR "serotonin uptake inhibitor"[tw] OR "serotonin uptake inhibitor"[tw] OR "serotonin uptake inhibitors"[tw] OR "serotonine and noradrenaline reuptake inhibitor"[tw] OR "serotonine and noradrenaline reuptake inhibitors"[tw] OR "serotonine and norepinephrine re uptake inhibitor"[tw] OR "serotonine and norepinephrine reuptake inhibitor"[tw] OR "serotonine and norepinephrine reuptake inhibitors"[tw] OR "serotonine norepinephrine re uptake inhibitor"[tw] OR "serotonine norepinephrine reuptake inhibitor"[tw] OR "serotonine norepinephrine reuptake inhibitors"[tw] OR "serotonine reuptake inhibitor"[tw] OR "serotonine reuptake inhibitor"[tw] OR "serotonine reuptake inhibitors"[tw] OR "serotonine uptake inhibitor"[tw] OR "serotonine uptake inhibitor"[tw] OR "serotonine uptake inhibitors"[tw] OR "serotonine and noradrenaline re uptake inhibitor"[tw] OR snris[tw] OR ssnris[tw] OR ssris[tw] OR snri[tw] OR ssnri[tw] OR ssri[tw] |
| #6 | Cericlamine[tw] OR Citalopram[mh] OR Citalopram[tw] OR celexa[tw] OR escitalopram[tw] OR lexapro[tw] OR Cipralex[tw] |
| #7 | Dapoxetine[tw] OR Dapoxetine[NM] OR Priligy[tw] OR Westoxetin[tw] |
| #8 | "Desvenlafaxine Succinate"[mh] OR Desvenlafaxine[tw] OR "Duloxetine Hydrochloride"[mh] OR Duloxetine[tw] |
| #9 | femoxetine[NM] OR femoxetine[tw] OR Fluoxetine[mh] OR fluoxetine[tw] OR prozac[tw] OR Sarafem[tw] |
| #10 | Fluvoxamine[mh] OR Fluvoxamine[tw] OR luvox[tw] |
| #11 | hydroxynefazodone[tw] OR hyperforin[tw] OR ifoxetine[tw] OR indalpine[NM] OR indalpine[tw] OR liafensine[tw] |
| #12 | litoxetine[tw] OR lubazodone[tw] OR medifoxamine[tw] OR milnacipran[NM] OR milnacipran[tw] |
| #13 | moxifetin[tw] OR nefazodone[tw] OR nomelidine[tw] OR norcitalopram[tw] |
| #14 | norfluoxetine[tw] OR norsertraline[tw] OR omiloxetine[tw] |
| #15 | Paroxetine[mh] OR Paroxetine[tw] OR paxil[tw] OR Pexeva[tw] OR Sertraline[mh] OR sertraline[tw] OR zoloft[tw] |
| #16 | tedatioxetine[tw] OR Trazodone[mh] OR trazodone[tw] OR Desyrel[tw] |
| #17 | "Vilazodone Hydrochloride"[mh] OR Vilazodone[tw] OR "Venlafaxine Hydrochloride"[mh] OR Venlafaxine[tw] OR Pristiq[tw] OR Effexor[tw] OR Cymbalta[tw] |
| #18 | vortioxetine[NM] OR vortioxetine[tw] OR Zimeldine[mh] OR Zimeldine[tw] OR zimlidine[tw] OR zimelidin[tw] |
| #19 | #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 |
| #20 | randomized controlled trial[pt] |
| #21 | controlled clinical trial[pt] |
| #22 | randomized[tiab] |
| #23 | placebo[tiab] |
| #24 | drug therapy[sh] |
| #25 | randomly[tiab] |
| #26 | trial[tiab] |
| #27 | groups[tiab] |
| #28 | #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 |
| #29 | animals[mh] NOT humans[mh] |
| #30 | #28 NOT #29 |
| #31 | #3 AND #19 AND #30 |
Appendix 3. Embase (Elsevier) search strategy
| #1 | 'Premature Ejaculation'/exp |
| #2 | 'early ejaculation':ti,ab OR 'rapid ejaculation':ti,ab OR 'rapid climax':ti,ab OR 'premature climax':ti,ab OR 'ejaculatio praecox':ti,ab OR 'ejaculatio precox':ti,ab OR 'premature ejaculation':ti,ab OR 'premature ejaculations':ti,ab OR 'early ejaculations':ti,ab OR 'premature ejaculator':ti,ab OR 'premature ejaculators':ti,ab |
| #3 | #1 OR #2 |
| #4 | 'Serotonin Uptake Inhibitor'/exp OR 'Serotonin and Noradrenaline Reuptake Inhibitors'/exp |
| #5 | '5‐ht uptake inhibitor':ti,ab OR '5‐ht uptake inhibitors':ti,ab OR '5‐hydroxytryptamine uptake inhibitor':ti,ab OR '5‐hydroxytryptamine uptake inhibitors':ti,ab OR 'serotonin and noradrenaline re uptake inhibitor':ti,ab OR 'serotonin and noradrenaline reuptake inhibitor':ti,ab OR 'serotonin and noradrenaline reuptake inhibitors':ti,ab OR 'serotonin and norepinephrine re uptake inhibitor':ti,ab OR 'serotonin and norepinephrine reuptake inhibitor':ti,ab OR 'serotonin and norepinephrine reuptake inhibitors':ti,ab OR 'serotonin norepinephrine re uptake inhibitor':ti,ab OR 'serotonin norepinephrine reuptake inhibitor':ti,ab OR 'serotonin norepinephrine reuptake inhibitors':ti,ab OR 'serotonin reuptake inhibitor':ti,ab OR 'serotonin reuptake inhibitor':ti,ab OR 'serotonin reuptake inhibitors':ti,ab OR 'serotonin uptake inhibitor':ti,ab OR 'serotonin uptake inhibitor':ti,ab OR 'serotonin uptake inhibitors':ti,ab OR 'serotonine and noradrenaline reuptake inhibitor':ti,ab OR 'serotonine and noradrenaline reuptake inhibitors':ti,ab OR 'serotonine and norepinephrine re uptake inhibitor':ti,ab OR 'serotonine and norepinephrine reuptake inhibitor':ti,ab OR 'serotonine and norepinephrine reuptake inhibitors':ti,ab OR 'serotonine norepinephrine re uptake inhibitor':ti,ab OR 'serotonine norepinephrine reuptake inhibitor':ti,ab OR 'serotonine norepinephrine reuptake inhibitors':ti,ab OR 'serotonine reuptake inhibitor':ti,ab OR 'serotonine reuptake inhibitor':ti,ab OR 'serotonine reuptake inhibitors':ti,ab OR 'serotonine uptake inhibitor':ti,ab OR 'serotonine uptake inhibitor':ti,ab OR 'serotonine uptake inhibitors':ti,ab OR 'serotonine and noradrenaline re uptake inhibitor':ti,ab OR snris:ti,ab OR ssnris:ti,ab OR ssris:ti,ab OR snri:ti,ab OR ssnri:ti,ab OR ssri:ti,ab |
| #6 | 'Cericlamine'/exp OR cericlamine:ti,ab OR 'Citalopram'/exp OR Citalopram:ti,ab OR celexa:ti,ab OR 'escitalopram'/exp OR escitalopram:ti,ab OR lexapro:ti,ab OR Cipralex:ti,ab |
| #7 | 'Dapoxetine'/exp OR Dapoxetine:ti,ab OR Priligy:ti,ab OR Westoxetin:ti,ab |
| #8 | 'Desvenlafaxine'/exp OR Desvenlafaxine:ti,ab OR 'Duloxetine Hydrochloride'/exp OR Duloxetine:ti,ab |
| #9 | femoxetine/exp OR femoxetine:ti,ab OR 'Fluoxetine'/exp OR fluoxetine:ti,ab OR prozac:ti,ab OR Sarafem:ti,ab |
| #10 | 'Fluvoxamine'/exp OR Fluvoxamine:ti,ab OR luvox:ti,ab |
| #11 | 'hydroxynefazodone'/exp OR hydroxynefazodone:ti,ab OR 'hyperforin'/exp OR hyperforin:ti,ab OR 'ifoxetine'/exp OR ifoxetine:ti,ab OR indalpine:ti,ab OR 'liafensine'/exp OR liafensine:ti,ab |
| #12 | 'litoxetine'/exp OR litoxetine:ti,ab OR 'lubazodone'/exp OR lubazodone:ti,ab OR 'medifoxamine'/exp OR medifoxamine:ti,ab OR 'milnacipran'/exp OR milnacipran:ti,ab |
| #13 | 'moxifetin'/exp OR moxifetin:ti,ab OR 'nefazodone'/exp OR nefazodone:ti,ab OR 'nomelidine'/exp OR nomelidine:ti,ab OR 'norcitalopram'/exp OR norcitalopram:ti,ab |
| #14 | 'norfluoxetine'/exp OR norfluoxetine:ti,ab OR 'norsertraline'/exp OR norsertraline:ti,ab OR 'omiloxetine'/exp OR omiloxetine:ti,ab |
| #15 | 'Paroxetine'/exp OR Paroxetine:ti,ab OR paxil:ti,ab OR Pexeva:ti,ab OR 'Sertraline'/exp OR sertraline:ti,ab OR zoloft:ti,ab |
| #16 | 'tedatioxetine'/exp OR tedatioxetine:ti,ab OR 'Trazodone'/exp OR trazodone:ti,ab OR Desyrel:ti,ab |
| #17 | 'Vilazodone'/exp OR Vilazodone:ti,ab OR 'Venlafaxine Hydrochloride'/exp OR Venlafaxine:ti,ab OR Pristiq:ti,ab OR Effexor:ti,ab OR Cymbalta:ti,ab |
| #18 | 'vortioxetine'/exp OR vortioxetine:ti,ab OR 'Zimeldine'/exp OR Zimeldine:ti,ab OR zimlidine:ti,ab OR zimelidin:ti,ab |
| #19 | #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 |
| #20 | 'Clinical Trial'/exp |
| #21 | 'Randomized Controlled Trial'/exp |
| #22 | 'controlled clinical trial'/exp |
| #23 | 'multicenter study'/exp |
| #24 | 'Phase 3 clinical trial'/exp |
| #25 | 'Phase 4 clinical trial'/exp |
| #26 | 'Randomization'/exp |
| #27 | 'Single Blind Procedure'/exp |
| #28 | 'Double Blind Procedure'/exp |
| #29 | 'Crossover Procedure'/exp |
| #30 | 'Placebo'/exp |
| #31 | randomi?ed controlled trial*:ti,ab |
| #32 | rct:ti,ab |
| #33 | (random* NEAR/2 allocat*):ti,ab |
| #34 | single blind*:ti,ab |
| #35 | double blind*:ti,ab |
| #36 | ((treble OR triple) NEAR/1 blind*):ti,ab |
| #37 | placebo*:ti,ab |
| #38 | 'Prospective Study'/exp |
| #39 | #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28 OR #29 OR #30 OR #31 OR #32 OR #33 OR #34 OR #35 OR #36 OR #37 OR #38 |
| #40 | 'Case Study'/exp |
| #41 | case report:ti,ab |
| #42 | 'abstract report'/exp OR 'letter'/exp |
| #43 | 'Conference proceeding':pt |
| #44 | 'Conference abstract':pt |
| #45 | Editorial.pt |
| #46 | Letter.pt |
| #47 | Note.pt |
| #48 | #40 OR #41 OR #42 OR #43 OR #44 OR #45 OR #46 OR #47 |
| #49 | #39 NOT #48 |
| #50 | #3 AND #19 AND #49 |
Appendix 4. CINAHL (EBSCOhost) search strategy
| #1 | (MH "Premature Ejaculation+") |
| #2 | TX "early ejaculation" OR TX "rapid ejaculation" OR TX "rapid climax" OR TX "premature climax" OR TX "ejaculatio praecox" OR TX "ejaculatio precox" OR TX "premature ejaculation" OR TX "premature ejaculations" OR TX "early ejaculations" OR TX "premature ejaculator" OR TX "premature ejaculators" |
| #3 | S1 AND S2 |
| #4 | (MH "Serotonin Uptake Inhibitors+") |
| #5 | TX "5‐ht uptake inhibitor" OR TX "5‐ht uptake inhibitors" OR TX "5‐hydroxytryptamine uptake inhibitor" OR TX "5‐hydroxytryptamine uptake inhibitors" OR TX "serotonin and noradrenaline re uptake inhibitor" OR TX "serotonin and noradrenaline reuptake inhibitor" OR TX "serotonin and noradrenaline reuptake inhibitors" OR TX "serotonin and norepinephrine re uptake inhibitor" OR TX "serotonin and norepinephrine reuptake inhibitor" OR TX "serotonin and norepinephrine reuptake inhibitors" OR TX "serotonin norepinephrine re uptake inhibitor" OR TX "serotonin norepinephrine reuptake inhibitor" OR TX "serotonin norepinephrine reuptake inhibitors" OR TX "serotonin reuptake inhibitor" OR TX "serotonin reuptake inhibitor" OR TX "serotonin reuptake inhibitors" OR TX "serotonin uptake inhibitor" OR TX "serotonin uptake inhibitor" OR TX "serotonin uptake inhibitors" OR TX "serotonine and noradrenaline reuptake inhibitor" OR TX "serotonine and noradrenaline reuptake inhibitors" OR TX "serotonine and norepinephrine re uptake inhibitor" OR TX "serotonine and norepinephrine reuptake inhibitor" OR TX "serotonine and norepinephrine reuptake inhibitors" OR TX "serotonine norepinephrine re uptake inhibitor" OR TX "serotonine norepinephrine reuptake inhibitor" OR TX "serotonine norepinephrine reuptake inhibitors" OR TX "serotonine reuptake inhibitor" OR TX "serotonine reuptake inhibitor" OR TX "serotonine reuptake inhibitors" OR TX "serotonine uptake inhibitor" OR TX "serotonine uptake inhibitor" OR TX "serotonine uptake inhibitors" OR TX "serotonine and noradrenaline re uptake inhibitor" OR TX snris OR TX ssnris OR TX ssris OR TX snri OR TX ssnri OR TX ssri |
| #6 | TX Cericlamine OR (MH "Citalopram+") OR TX Citalopram OR TX celexa OR TX escitalopram OR TX lexapro OR TX Cipralex |
| #7 | TX Dapoxetine OR TX Priligy OR TX Westoxetin |
| #8 | (MH "Desvenlafaxine Succinate+") OR TX Desvenlafaxine OR (MH "Duloxetine Hydrochloride+") OR TX Duloxetine |
| #9 | TX femoxetine OR (MH "Fluoxetine+") OR TX fluoxetine OR TX prozac OR TX Sarafem |
| #10 | (MH "Fluvoxamine Maleate+") OR TX Fluvoxamine OR TX luvox |
| #11 | TX hydroxynefazodone OR TX hyperforin OR TX ifoxetine OR TX indalpine OR TX liafensine |
| #12 | TX litoxetine OR TX lubazodone OR TX medifoxamine OR TX milnacipran |
| #13 | TX moxifetin OR TX nefazodone OR TX nomelidine OR TX norcitalopram |
| #14 | TX norfluoxetine OR TX norsertraline OR TX omiloxetine |
| #15 | (MH "Paroxetine+") OR TX Paroxetine OR TX paxil OR TX Pexeva OR (MH "Sertraline Hydrochloride+") OR TX sertraline OR TX zoloft |
| #16 | TX tedatioxetine OR (MH "Trazodone+") OR TX trazodone OR TX Desyrel |
| #17 | TX Vilazodone OR (MH "Venlafaxine+") OR TX Venlafaxine OR TX Pristiq OR TX Effexor OR TX Cymbalta |
| #18 | TX vortioxetine OR TX Zimeldine OR TX zimlidine OR TX zimelidin |
| #19 | S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 |
| #20 | MH "Clinical Trials+" |
| #21 | PT "Clinical trial" |
| #22 | TX clinic* n1 trial* |
| #23 | TX (singl* n1 blind*) OR TX (singl* n1 mask*) OR TX (doubl* n1 blind*) OR TX (doubl* n1 mask*) OR TX (tripl* n1 blind*) OR TX (tripl* n1 mask*) OR TX (trebl* n1 blind*) OR TX (trebl* n1 mask*) |
| #24 | TX randomi* control* trial* |
| #25 | MH "Random Assignment" |
| #26 | TX random* allocat* |
| #27 | TX placebo* |
| #28 | MH "Placebos" |
| #29 | MH "Quantitative Studies" |
| #30 | TX allocat* random* |
| #31 | S20 or S21 or S22 or S23 or S24 or S25 or S26 or S27 or S28 or S29 or S30 |
| #32 | S3 AND S19 AND S31 |
Appendix 5. LILACS (BIREME/PAHO/WHO) search strategy
UsingiAH Search Interface; In Field ‐ Words:
(MH:"Premature Ejaculation" OR MH:"Eyaculación Prematura" OR MH:"Ejaculação Precoce" OR "Ejaculatio Praecox" OR "Premature ejaculation" OR "early ejaculation" OR "rapid ejaculation" OR "rapid climax" OR "premature climax" OR "ejaculatio precox" OR "premature ejaculation" OR "premature ejaculations" OR "early ejaculations" OR "premature ejaculator" OR "premature ejaculators")
AND
(MH:"Serotonin Uptake Inhibitors" OR MH:"Inhibidores de la Captación de Serotonina" OR MH:"Inibidores da Captação de Serotonina" OR "5‐ht uptake inhibitor" OR "5‐ht uptake inhibitors" OR "5‐hydroxytryptamine uptake inhibitor" OR "5‐hydroxytryptamine uptake inhibitors" OR "serotonin and noradrenaline re uptake inhibitor" OR "serotonin and noradrenaline reuptake inhibitor" OR "serotonin and noradrenaline reuptake inhibitors" OR "serotonin and norepinephrine re uptake inhibitor" OR "serotonin and norepinephrine reuptake inhibitor" OR "serotonin and norepinephrine reuptake inhibitors" OR "serotonin norepinephrine re uptake inhibitor" OR "serotonin norepinephrine reuptake inhibitor" OR "serotonin norepinephrine reuptake inhibitors" OR "serotonin reuptake inhibitor" OR "serotonin reuptake inhibitor" OR "serotonin reuptake inhibitors" OR "serotonin uptake inhibitor" OR "serotonin uptake inhibitor" OR "serotonin uptake inhibitors" OR "serotonine and noradrenaline reuptake inhibitor" OR "serotonine and noradrenaline reuptake inhibitors" OR "serotonine and norepinephrine re uptake inhibitor" OR "serotonine and norepinephrine reuptake inhibitor" OR "serotonine and norepinephrine reuptake inhibitors" OR "serotonine norepinephrine re uptake inhibitor" OR "serotonine norepinephrine reuptake inhibitor" OR "serotonine norepinephrine reuptake inhibitors" OR "serotonine reuptake inhibitor" OR "serotonine reuptake inhibitor" OR "serotonine reuptake inhibitors" OR "serotonine uptake inhibitor" OR "serotonine uptake inhibitor" OR "serotonine uptake inhibitors" OR "serotonine and noradrenaline re uptake inhibitor" OR snris OR ssnris OR ssris OR snri OR ssnri OR ssri OR Cericlamine OR MH:Citalopram OR Citalopram OR celexa OR escitalopram OR lexapro OR Cipralex OR Dapoxetine OR Priligy OR Westoxetin OR MH:"Desvenlafaxine Succinate" OR MH:"Succinato de Desvenlafaxina" OR Desvenlafaxine OR MH:"Duloxetine Hydrochloride" OR MH:"Clorhidrato de Duloxetina" OR MH:"Cloridrato de Duloxetina" OR Duloxetine OR femoxetine OR MH:Fluoxetine OR MH:Fluoxetina OR fluoxetine OR prozac OR Sarafem OR MH:Fluvoxamine OR MH:Fluvoxamina OR Fluvoxamine OR luvox OR hydroxynefazodone OR hyperforin OR ifoxetine OR indalpine OR liafensine OR litoxetine OR lubazodone OR medifoxamine OR milnacipran OR moxifetin OR nefazodone OR nomelidine OR norcitalopram OR norfluoxetine OR norsertraline OR omiloxetine OR MH:Paroxetine OR MH:Paroxetine OR Paroxetine OR paxil OR Pexeva OR MH:Sertraline OR MH:Sertralina OR sertraline OR zoloft OR tedatioxetine OR MH:Trazodone OR MH:Trazodona OR trazodone OR Desyrel OR MH:"Vilazodone Hydrochloride" OR MH:"Clorhidrato de Vilazodona" OR MH:"Cloridrato de Vilazodona" OR Vilazodone OR MH:"Venlafaxine Hydrochloride" OR MH:"Clorhidrato de Venlafaxina" OR MH:"Cloridrato de Venlafaxina" OR Venlafaxine OR Pristiq OR Effexor OR Cymbalta OR vortioxetine OR MH:Zimeldine OR MH:Zimeldina OR Zimeldine OR zimlidine OR zimelidin)
Appendix 6. Scopus (Elsevier) search strategy
In Advanced Search:
TITLE‐ABS‐KEY("Premature Ejaculation" OR "early ejaculation" OR "rapid ejaculation" OR "rapid climax" OR "premature climax" OR "ejaculatio praecox" OR "ejaculatio precox" OR "premature ejaculation" OR "premature ejaculations" OR "early ejaculations" OR "premature ejaculator" OR "premature ejaculators") AND TITLE‐ABS‐KEY("5‐ht uptake inhibitor" OR "5‐ht uptake inhibitors" OR "5‐hydroxytryptamine uptake inhibitor" OR "5‐hydroxytryptamine uptake inhibitors" OR "serotonin and noradrenaline re uptake inhibitor" OR "serotonin and noradrenaline reuptake inhibitor" OR "serotonin and noradrenaline reuptake inhibitors" OR "serotonin and norepinephrine re uptake inhibitor" OR "serotonin and norepinephrine reuptake inhibitor" OR "serotonin and norepinephrine reuptake inhibitors" OR "serotonin norepinephrine re uptake inhibitor" OR "serotonin norepinephrine reuptake inhibitor" OR "serotonin norepinephrine reuptake inhibitors" OR "serotonin reuptake inhibitor" OR "serotonin reuptake inhibitor" OR "serotonin reuptake inhibitors" OR "serotonin uptake inhibitor" OR "serotonin uptake inhibitor" OR "serotonin uptake inhibitors" OR "serotonine and noradrenaline reuptake inhibitor" OR "serotonine and noradrenaline reuptake inhibitors" OR "serotonine and norepinephrine re uptake inhibitor" OR "serotonine and norepinephrine reuptake inhibitor" OR "serotonine and norepinephrine reuptake inhibitors" OR "serotonine norepinephrine re uptake inhibitor" OR "serotonine norepinephrine reuptake inhibitor" OR "serotonine norepinephrine reuptake inhibitors" OR "serotonine reuptake inhibitor" OR "serotonine reuptake inhibitor" OR "serotonine reuptake inhibitors" OR "serotonine uptake inhibitor" OR "serotonine uptake inhibitor" OR "serotonine uptake inhibitors" OR "serotonine and noradrenaline re uptake inhibitor" OR snris OR ssnris OR ssris OR snri OR ssnri OR ssri OR Cericlamine OR Citalopram OR celexa OR escitalopram OR lexapro OR Cipralex OR Dapoxetine OR Priligy OR Westoxetin OR Desvenlafaxine OR Duloxetine OR femoxetine OR Fluoxetine OR fluoxetine OR prozac OR Sarafem OR Fluvoxamine OR luvox OR hydroxynefazodone OR hyperforin OR ifoxetine OR indalpine OR liafensine OR litoxetine OR lubazodone OR medifoxamine OR milnacipran OR moxifetin OR nefazodone OR nomelidine OR norcitalopram OR norfluoxetine OR norsertraline OR omiloxetine OR Paroxetine OR paxil OR Pexeva OR Sertraline OR zoloft OR tedatioxetine OR Trazodone OR Desyrel OR Vilazodone OR Venlafaxine OR Pristiq OR Effexor OR Cymbalta OR vortioxetine OR Zimeldine OR zimlidine OR zimelidin) AND TITLE‐ABS‐KEY((clinic* w/1 trial*) OR (randomi* w/1 control*) OR (randomi* w/2 trial*) OR (random* w/1 assign*) OR (random* w/1 allocat*) OR (control* w/1 clinic*) OR (control* w/1 trial) OR placebo* OR (Quantitat* w/1 Stud*) OR (control* w/1 stud*) OR (randomi* w/1 stud*) OR (singl* w/1 blind*) or (singl* w/1 mask*) OR (doubl* w/1 blind*) OR (doubl* w/1 mask*) OR (tripl* w/1 blind*) OR (tripl* w/1 mask*) OR (trebl* w/1 blind*) OR (trebl* w/1 mask*)) AND NOT (SRCTYPE(b) OR SRCTYPE(k) OR SRCTYPE(p) OR SRCTYPE(r) OR SRCTYPE(d) OR DOCTYPE(ab) OR DOCTYPE(bk) OR DOCTYPE(ch) OR DOCTYPE(bz) OR DOCTYPE(cr) OR DOCTYPE(ed) OR DOCTYPE(er) OR DOCTYPE(le) OR DOCTYPE(no) OR DOCTYPE(pr) OR DOCTYPE(rp) OR DOCTYPE(re) OR DOCTYPE(sh))
Appendix 7. ClinicalTrials.gov search strategy
clinicaltrials.gov
Advanced Search – Targeted Search (Note: length of search strings limited for this interface)
Condition/Disease: "Premature Ejaculation" OR "early ejaculation" OR "rapid ejaculation" OR "rapid climax" OR "premature climax" OR "ejaculatio praecox" OR "ejaculatio precox" OR "premature ejaculator" OR "premature ejaculators"
Intervention/Treatment: "Serotonin Reuptake Inhibitors" OR "Serotonin Uptake Inhibitors" OR "5‐Hydroxytryptamine Uptake Inhibitors" OR "5‐HT Uptake Inhibitors" OR SSRI OR "Serotonin and Noradrenaline Reuptake Inhibitors" OR "serotonin and norepinephrine reuptake inhibitors"
Appendix 8. WHO International Clinical Trials Registry Platform (ICTRP) search strategy
apps.who.int/trialsearch/
In Advanced Search:
In Condition: Premature Ejaculation OR early ejaculation OR rapid ejaculation OR rapid climax OR premature climax OR ejaculatio praecox OR ejaculatio precox OR premature ejaculations OR early ejaculations OR premature ejaculator OR premature ejaculators
Appendix 9. ProQuest Dissertations & Theses search strategy
Advanced Search (Leave field choice on "anywhere"):
"Premature Ejaculation" OR "early ejaculation" OR "rapid ejaculation" OR "rapid climax" OR "premature climax" OR "ejaculatio praecox" OR "ejaculatio precox" OR "premature ejaculations" OR "early ejaculations" OR "premature ejaculator" OR "premature ejaculators"
AND
"5‐ht uptake inhibitor" OR "5‐ht uptake inhibitors" OR "5‐hydroxytryptamine uptake inhibitor" OR "5‐hydroxytryptamine uptake inhibitors" OR "serotonin and noradrenaline re uptake inhibitor" OR "serotonin and noradrenaline reuptake inhibitor" OR "serotonin and noradrenaline reuptake inhibitors" OR "serotonin and norepinephrine re uptake inhibitor" OR "serotonin and norepinephrine reuptake inhibitor" OR "serotonin and norepinephrine reuptake inhibitors" OR "serotonin norepinephrine re uptake inhibitor" OR "serotonin norepinephrine reuptake inhibitor" OR "serotonin norepinephrine reuptake inhibitors" OR "serotonin reuptake inhibitor" OR "serotonin reuptake inhibitor" OR "serotonin reuptake inhibitors" OR "serotonin uptake inhibitor" OR "serotonin uptake inhibitor" OR "serotonin uptake inhibitors" OR "serotonine and noradrenaline reuptake inhibitor" OR "serotonine and noradrenaline reuptake inhibitors" OR "serotonine and norepinephrine re uptake inhibitor" OR "serotonine and norepinephrine reuptake inhibitor" OR "serotonine and norepinephrine reuptake inhibitors" OR "serotonine norepinephrine re uptake inhibitor" OR "serotonine norepinephrine reuptake inhibitor" OR "serotonine norepinephrine reuptake inhibitors" OR "serotonine reuptake inhibitor" OR "serotonine reuptake inhibitor" OR "serotonine reuptake inhibitors" OR "serotonine uptake inhibitor" OR "serotonine uptake inhibitor" OR "serotonine uptake inhibitors" OR "serotonine and noradrenaline re uptake inhibitor" OR snris OR ssnris OR ssris OR snri OR ssnri OR ssri OR Cericlamine OR Citalopram OR celexa OR escitalopram OR lexapro OR Cipralex OR Dapoxetine OR Priligy OR Westoxetin OR Desvenlafaxine OR Duloxetine OR femoxetine OR Fluoxetine OR fluoxetine OR prozac OR Sarafem OR Fluvoxamine OR luvox OR hydroxynefazodone OR hyperforin OR ifoxetine OR indalpine OR liafensine OR litoxetine OR lubazodone OR medifoxamine OR milnacipran OR moxifetin OR nefazodone OR nomelidine OR norcitalopram OR norfluoxetine OR norsertraline OR omiloxetine OR Paroxetine OR paxil OR Pexeva OR Sertraline OR zoloft OR tedatioxetine OR Trazodone OR Desyrel OR Vilazodone OR Venlafaxine OR Pristiq OR Effexor OR Cymbalta OR vortioxetine OR Zimeldine OR zimlidine OR zimelidin
Appendix 10. OCLC WorldCat Dissertations and Theses search strategy
Advanced Search
Keyword: ("Premature Ejaculation" OR "early ejaculation" OR "rapid ejaculation" OR "rapid climax" OR "premature climax" OR "ejaculatio praecox" OR "ejaculatio precox" OR "premature ejaculations" OR "early ejaculations" OR "premature ejaculator" OR "premature ejaculators") AND ("5‐ht uptake inhibitor" OR "5‐ht uptake inhibitors" OR "5‐hydroxytryptamine uptake inhibitor" OR "5‐hydroxytryptamine uptake inhibitors" OR "serotonin and noradrenaline re uptake inhibitor" OR "serotonin and noradrenaline reuptake inhibitor" OR "serotonin and noradrenaline reuptake inhibitors" OR "serotonin and norepinephrine re uptake inhibitor" OR "serotonin and norepinephrine reuptake inhibitor" OR "serotonin and norepinephrine reuptake inhibitors" OR "serotonin norepinephrine re uptake inhibitor" OR "serotonin norepinephrine reuptake inhibitor" OR "serotonin norepinephrine reuptake inhibitors" OR "serotonin reuptake inhibitor" OR "serotonin reuptake inhibitor" OR "serotonin reuptake inhibitors" OR "serotonin uptake inhibitor" OR "serotonin uptake inhibitor" OR "serotonin uptake inhibitors" OR "serotonine and noradrenaline reuptake inhibitor" OR "serotonine and noradrenaline reuptake inhibitors" OR "serotonine and norepinephrine re uptake inhibitor" OR "serotonine and norepinephrine reuptake inhibitor" OR "serotonine and norepinephrine reuptake inhibitors" OR "serotonine norepinephrine re uptake inhibitor" OR "serotonine norepinephrine reuptake inhibitor" OR "serotonine norepinephrine reuptake inhibitors" OR "serotonine reuptake inhibitor" OR "serotonine reuptake inhibitor" OR "serotonine reuptake inhibitors" OR "serotonine uptake inhibitor" OR "serotonine uptake inhibitor" OR "serotonine uptake inhibitors" OR "serotonine and noradrenaline re uptake inhibitor" OR snris OR ssnris OR ssris OR snri OR ssnri OR ssri OR Cericlamine OR Citalopram OR celexa OR escitalopram OR lexapro OR Cipralex OR Dapoxetine OR Priligy OR Westoxetin OR Desvenlafaxine OR Duloxetine OR femoxetine OR Fluoxetine OR fluoxetine OR prozac OR Sarafem OR Fluvoxamine OR luvox OR hydroxynefazodone OR hyperforin OR ifoxetine OR indalpine OR liafensine OR litoxetine OR lubazodone OR medifoxamine OR milnacipran OR moxifetin OR nefazodone OR nomelidine OR norcitalopram OR norfluoxetine OR norsertraline OR omiloxetine OR Paroxetine OR paxil OR Pexeva OR Sertraline OR zoloft OR tedatioxetine OR Trazodone OR Desyrel OR Vilazodone OR Venlafaxine OR Pristiq OR Effexor OR Cymbalta OR vortioxetine OR Zimeldine OR zimlidine OR zimelidin)
Select Content: Thesis/Dissertation
Data and analyses
Comparison 1. SSRI versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Participant perception of change with treatment | 6 | 3260 | Risk Ratio (M‐H, Random, 95% CI) | 1.92 [1.66, 2.23] |
| 1.2 Participant satisfaction with intercourse | 3 | 4273 | Risk Ratio (M‐H, Random, 95% CI) | 1.63 [1.42, 1.87] |
| 1.3 Study withdrawal due to adverse events | 20 | 7367 | Risk Ratio (M‐H, Random, 95% CI) | 3.80 [2.61, 5.51] |
| 1.4 Perceived control over ejaculation | 3 | 4273 | Risk Ratio (M‐H, Random, 95% CI) | 2.29 [1.72, 3.05] |
| 1.5 Participant distress about PE | 1 | 652 | Risk Ratio (M‐H, Random, 95% CI) | 1.54 [1.26, 1.88] |
| 1.6 Relationship difficulties | 1 | 652 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [1.07, 1.34] |
| 1.7 Adverse events | 17 | 4624 | Risk Ratio (M‐H, Random, 95% CI) | 1.71 [1.48, 1.99] |
| 1.8 Intravaginal ejaculatory latency time | 20 | 5872 | Mean Difference (IV, Random, 95% CI) | 3.09 [1.94, 4.25] |
| 1.9 Depression | 1 | 14 | Risk Ratio (M‐H, Random, 95% CI) | 2.00 [0.23, 17.34] |
Comparison 2. Subgroup analysis: long‐acting versus short‐acting SSRI.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Participant perception of change with treatment | 6 | 3260 | Risk Ratio (M‐H, Random, 95% CI) | 1.92 [1.66, 2.23] |
| 2.1.1 Long‐acting SSRI | 2 | 46 | Risk Ratio (M‐H, Random, 95% CI) | 8.48 [2.21, 32.51] |
| 2.1.2 Short‐acting SSRI | 4 | 3214 | Risk Ratio (M‐H, Random, 95% CI) | 1.87 [1.66, 2.10] |
| 2.2 Participant satisfaction with intercourse | 3 | 4273 | Risk Ratio (M‐H, Random, 95% CI) | 1.63 [1.42, 1.87] |
| 2.2.1 Short‐acting SSRI | 3 | 4273 | Risk Ratio (M‐H, Random, 95% CI) | 1.63 [1.42, 1.87] |
| 2.3 Study withdrawal due to adverse events | 20 | 7367 | Risk Ratio (M‐H, Random, 95% CI) | 3.71 [2.56, 5.38] |
| 2.3.1 Long‐acting SSRI | 14 | 1315 | Risk Ratio (M‐H, Random, 95% CI) | 2.00 [0.92, 4.34] |
| 2.3.2 Short‐acting SSRI | 6 | 6052 | Risk Ratio (M‐H, Random, 95% CI) | 4.33 [2.60, 7.23] |
| 2.4 Perceived control over ejaculation | 3 | 4273 | Risk Ratio (M‐H, Random, 95% CI) | 2.29 [1.72, 3.05] |
| 2.4.1 Short‐acting SSRI | 3 | 4273 | Risk Ratio (M‐H, Random, 95% CI) | 2.29 [1.72, 3.05] |
| 2.5 Participant distress about PE | 1 | 652 | Risk Ratio (M‐H, Random, 95% CI) | 1.54 [1.26, 1.88] |
| 2.5.1 Short‐acting SSRI | 1 | 652 | Risk Ratio (M‐H, Random, 95% CI) | 1.54 [1.26, 1.88] |
| 2.6 Relationship difficulties | 1 | 652 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [1.07, 1.34] |
| 2.6.1 Short‐acting SSRI | 1 | 652 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [1.07, 1.34] |
| 2.7 Adverse events | 17 | 4624 | Risk Ratio (M‐H, Random, 95% CI) | 1.71 [1.48, 1.99] |
| 2.7.1 Long‐acting SSRI | 13 | 1162 | Risk Ratio (M‐H, Random, 95% CI) | 1.90 [1.37, 2.64] |
| 2.7.2 Short‐acting SSRI | 4 | 3462 | Risk Ratio (M‐H, Random, 95% CI) | 1.70 [1.42, 2.03] |
| 2.8 Intravaginal ejaculatory latency time | 19 | 5804 | Mean Difference (IV, Random, 95% CI) | 2.74 [1.57, 3.92] |
| 2.8.1 Long‐acting SSRI | 14 | 576 | Mean Difference (IV, Random, 95% CI) | 3.36 [1.62, 5.10] |
| 2.8.2 Short‐acting SSRI | 5 | 5228 | Mean Difference (IV, Random, 95% CI) | 1.52 [1.27, 1.77] |
| 2.9 Depression | 1 | 14 | Risk Ratio (M‐H, Random, 95% CI) | 2.00 [0.23, 17.34] |
| 2.9.1 Long‐acting SSRI | 1 | 14 | Risk Ratio (M‐H, Random, 95% CI) | 2.00 [0.23, 17.34] |
2.2. Analysis.

Comparison 2: Subgroup analysis: long‐acting versus short‐acting SSRI, Outcome 2: Participant satisfaction with intercourse
2.4. Analysis.

Comparison 2: Subgroup analysis: long‐acting versus short‐acting SSRI, Outcome 4: Perceived control over ejaculation
2.5. Analysis.

Comparison 2: Subgroup analysis: long‐acting versus short‐acting SSRI, Outcome 5: Participant distress about PE
2.6. Analysis.

Comparison 2: Subgroup analysis: long‐acting versus short‐acting SSRI, Outcome 6: Relationship difficulties
2.9. Analysis.

Comparison 2: Subgroup analysis: long‐acting versus short‐acting SSRI, Outcome 9: Depression
Comparison 3. Subgroup analysis: comparison of long‐acting agents.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Participant perception of change with treatment | 2 | 46 | Risk Ratio (M‐H, Random, 95% CI) | 8.48 [2.21, 32.51] |
| 3.1.1 Citalopram | 1 | 26 | Risk Ratio (M‐H, Random, 95% CI) | 9.00 [1.32, 61.24] |
| 3.1.2 Duloxetine | 1 | 20 | Risk Ratio (M‐H, Random, 95% CI) | 8.00 [1.21, 52.69] |
| 3.2 Study withdrawal due to adverse events | 14 | 1315 | Risk Ratio (M‐H, Random, 95% CI) | 2.00 [0.92, 4.34] |
| 3.2.1 Citalopram | 3 | 164 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [0.13, 70.74] |
| 3.2.2 Dapoxetine | 2 | 383 | Risk Ratio (M‐H, Random, 95% CI) | 7.64 [0.99, 58.71] |
| 3.2.3 Duloxetine | 1 | 20 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 3.2.4 Escitalopram | 1 | 276 | Risk Ratio (M‐H, Random, 95% CI) | 2.00 [0.37, 10.74] |
| 3.2.5 Fluoxetine | 3 | 72 | Risk Ratio (M‐H, Random, 95% CI) | 2.59 [0.34, 19.59] |
| 3.2.6 Fluvoxamine | 1 | 15 | Risk Ratio (M‐H, Random, 95% CI) | 1.54 [0.09, 25.86] |
| 3.2.7 Paroxetine | 4 | 281 | Risk Ratio (M‐H, Random, 95% CI) | 1.76 [0.35, 8.91] |
| 3.2.8 Sertraline | 3 | 104 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.05, 3.56] |
| 3.3 Adverse events | 13 | 1204 | Risk Ratio (M‐H, Random, 95% CI) | 2.00 [1.44, 2.78] |
| 3.3.1 Citalopram | 2 | 106 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [0.51, 17.57] |
| 3.3.2 Clomipramine | 1 | 42 | Risk Ratio (M‐H, Random, 95% CI) | 4.40 [1.06, 18.32] |
| 3.3.3 Dapoxetine | 2 | 356 | Risk Ratio (M‐H, Random, 95% CI) | 2.54 [1.34, 4.81] |
| 3.3.4 Duloxetine | 1 | 20 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [0.37, 24.17] |
| 3.3.5 Escitalopram | 1 | 254 | Risk Ratio (M‐H, Random, 95% CI) | 1.69 [0.69, 4.15] |
| 3.3.6 Fluoxetine | 4 | 140 | Risk Ratio (M‐H, Random, 95% CI) | 2.50 [1.29, 4.86] |
| 3.3.7 Paroxetine | 1 | 155 | Risk Ratio (M‐H, Random, 95% CI) | 2.50 [0.91, 6.90] |
| 3.3.8 Sertraline | 3 | 131 | Risk Ratio (M‐H, Random, 95% CI) | 1.33 [0.74, 2.39] |
| 3.4 Intravaginal ejaculatory latency time | 14 | 576 | Mean Difference (IV, Random, 95% CI) | 3.36 [1.62, 5.10] |
| 3.4.1 Citalopram | 3 | 157 | Mean Difference (IV, Random, 95% CI) | 4.85 [3.14, 6.56] |
| 3.4.2 Duloxetine | 1 | 20 | Mean Difference (IV, Random, 95% CI) | 1.52 [0.80, 2.24] |
| 3.4.3 Fluoxetine | 5 | 149 | Mean Difference (IV, Random, 95% CI) | 2.46 [1.52, 3.39] |
| 3.4.4 Fluvoxamine | 1 | 12 | Mean Difference (IV, Random, 95% CI) | 0.59 [‐0.35, 1.53] |
| 3.4.5 Paroxetine | 3 | 107 | Mean Difference (IV, Random, 95% CI) | 6.51 [0.33, 12.68] |
| 3.4.6 Sertraline | 4 | 131 | Mean Difference (IV, Random, 95% CI) | 2.55 [1.54, 3.56] |
| 3.5 Depression | 1 | 14 | Risk Ratio (M‐H, Random, 95% CI) | 2.00 [0.23, 17.34] |
| 3.5.1 Fluoxetine | 1 | 14 | Risk Ratio (M‐H, Random, 95% CI) | 2.00 [0.23, 17.34] |
3.5. Analysis.

Comparison 3: Subgroup analysis: comparison of long‐acting agents, Outcome 5: Depression
Comparison 4. Subgroup analysis: different doses of dapoxetine.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Participant perception of change with treatment | 4 | 3214 | Risk Ratio (M‐H, Random, 95% CI) | 1.87 [1.66, 2.10] |
| 4.1.1 Dapoxetine 30 mg daily | 1 | 508 | Risk Ratio (M‐H, Random, 95% CI) | 1.87 [1.37, 2.54] |
| 4.1.2 Dapoxetine 30 mg on‐demand | 2 | 1021 | Risk Ratio (M‐H, Random, 95% CI) | 2.00 [1.33, 3.01] |
| 4.1.3 Dapoxetine 60 mg daily | 1 | 500 | Risk Ratio (M‐H, Random, 95% CI) | 1.68 [1.23, 2.30] |
| 4.1.4 Dapoxetine 60 mg on‐demand | 2 | 1185 | Risk Ratio (M‐H, Random, 95% CI) | 1.98 [1.58, 2.48] |
| 4.2 Participant satisfaction with intercourse | 3 | 2968 | Risk Ratio (M‐H, Random, 95% CI) | 1.53 [1.37, 1.71] |
| 4.2.1 Dapoxetine 30 mg daily | 1 | 500 | Risk Ratio (M‐H, Random, 95% CI) | 1.41 [1.08, 1.85] |
| 4.2.2 Dapoxetine 30 mg on‐demand | 1 | 1309 | Risk Ratio (M‐H, Random, 95% CI) | 1.59 [1.33, 1.90] |
| 4.2.3 Dapoxetine 60 mg daily | 1 | 507 | Risk Ratio (M‐H, Random, 95% CI) | 1.39 [1.07, 1.82] |
| 4.2.4 Dapoxetine 60 mg on‐demand | 1 | 652 | Risk Ratio (M‐H, Random, 95% CI) | 1.61 [1.32, 1.98] |
| 4.3 Study withdrawal due to adverse events | 7 | 6378 | Risk Ratio (M‐H, Random, 95% CI) | 4.54 [2.89, 7.14] |
| 4.3.1 Dapoxetine 30 mg daily | 1 | 533 | Risk Ratio (M‐H, Random, 95% CI) | 3.03 [0.37, 25.01] |
| 4.3.2 Dapoxetine 30 mg on‐demand | 3 | 2390 | Risk Ratio (M‐H, Random, 95% CI) | 2.44 [1.06, 5.59] |
| 4.3.3 Dapoxetine 60 mg daily | 3 | 916 | Risk Ratio (M‐H, Random, 95% CI) | 8.76 [2.10, 36.49] |
| 4.3.4 Dapoxetine 60 mg on‐demand | 3 | 2539 | Risk Ratio (M‐H, Random, 95% CI) | 6.51 [3.64, 11.66] |
| 4.4 Perceived control over ejaculation | 3 | 4273 | Risk Ratio (M‐H, Random, 95% CI) | 2.29 [1.72, 3.05] |
| 4.4.1 Dapoxetine 30 mg daily | 1 | 500 | Risk Ratio (M‐H, Random, 95% CI) | 1.79 [1.26, 2.53] |
| 4.4.2 Dapoxetine 30 mg on‐demand | 1 | 1305 | Risk Ratio (M‐H, Random, 95% CI) | 3.70 [2.72, 5.04] |
| 4.4.3 Dapoxetine 60 mg daily | 1 | 507 | Risk Ratio (M‐H, Random, 95% CI) | 1.78 [1.26, 2.52] |
| 4.4.4 Dapoxetine 60 mg on‐demand | 2 | 1961 | Risk Ratio (M‐H, Random, 95% CI) | 2.28 [1.65, 3.16] |
| 4.5 Participant distress about PE | 1 | 652 | Risk Ratio (M‐H, Random, 95% CI) | 1.54 [1.26, 1.88] |
| 4.5.1 Dapoxetine 60 mg on‐demand | 1 | 652 | Risk Ratio (M‐H, Random, 95% CI) | 1.54 [1.26, 1.88] |
| 4.6 Relationship difficulties | 1 | 652 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [1.07, 1.34] |
| 4.6.1 Dapoxetine 60 mg on‐demand | 1 | 652 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [1.07, 1.34] |
| 4.7 Adverse events | 6 | 3818 | Risk Ratio (M‐H, Random, 95% CI) | 1.74 [1.46, 2.07] |
| 4.7.1 Dapoxetine 30 mg daily | 2 | 1028 | Risk Ratio (M‐H, Random, 95% CI) | 1.64 [1.30, 2.07] |
| 4.7.2 Dapoxetine 30 mg on‐demand | 1 | 581 | Risk Ratio (M‐H, Random, 95% CI) | 1.47 [1.20, 1.79] |
| 4.7.3 Dapoxetine 60 mg daily | 3 | 891 | Risk Ratio (M‐H, Random, 95% CI) | 2.73 [2.03, 3.66] |
| 4.7.4 Dapoxetine 60 mg on‐demand | 2 | 1318 | Risk Ratio (M‐H, Random, 95% CI) | 1.56 [1.23, 1.99] |
| 4.8 Intravaginal ejaculatory latency time | 4 | 5173 | Mean Difference (IV, Random, 95% CI) | 1.48 [1.20, 1.75] |
| 4.8.1 Dapoxetine 30 mg daily | 1 | 502 | Mean Difference (IV, Random, 95% CI) | 1.80 [1.27, 2.33] |
| 4.8.2 Dapoxetine 30 mg on‐demand | 3 | 2329 | Mean Difference (IV, Random, 95% CI) | 1.37 [0.86, 1.89] |
| 4.8.3 Dapoxetine 60 mg daily | 1 | 504 | Mean Difference (IV, Random, 95% CI) | 1.50 [0.98, 2.02] |
| 4.8.4 Dapoxetine 60 mg on‐demand | 2 | 1838 | Mean Difference (IV, Random, 95% CI) | 1.53 [1.09, 1.97] |
Comparison 5. Subgroup analysis: different doses of fluoxetine.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Study withdrawal due to adverse events | 3 | 72 | Risk Ratio (M‐H, Random, 95% CI) | 2.09 [0.26, 16.82] |
| 5.1.1 Fluoxetine 20 mg daily | 3 | 72 | Risk Ratio (M‐H, Random, 95% CI) | 2.09 [0.26, 16.82] |
| 5.2 Adverse events | 4 | 140 | Risk Ratio (M‐H, Random, 95% CI) | 2.50 [1.29, 4.86] |
| 5.2.1 Fluoxetine 20 mg daily | 2 | 57 | Risk Ratio (M‐H, Random, 95% CI) | 9.32 [1.88, 46.26] |
| 5.2.2 Fluoxetine 40 mg daily | 1 | 23 | Risk Ratio (M‐H, Random, 95% CI) | 2.29 [0.55, 9.49] |
| 5.2.3 Fluoxetine 90 mg daily | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 1.78 [0.76, 4.17] |
| 5.3 Intravaginal ejaculatory latency time | 5 | 149 | Mean Difference (IV, Random, 95% CI) | 2.46 [1.52, 3.39] |
| 5.3.1 Fluoxetine 20 mg daily | 3 | 66 | Mean Difference (IV, Random, 95% CI) | 2.87 [1.26, 4.48] |
| 5.3.2 Fluoxetine 40 mg daily | 1 | 23 | Mean Difference (IV, Random, 95% CI) | ‐0.54 [‐3.57, 2.49] |
| 5.3.3 Fluoxetine 90 mg daily | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 2.72 [1.83, 3.61] |
| 5.4 Depression | 1 | 14 | Risk Ratio (M‐H, Random, 95% CI) | 2.00 [0.23, 17.34] |
| 5.4.1 Fluoxetine 20 mg daily | 1 | 14 | Risk Ratio (M‐H, Random, 95% CI) | 2.00 [0.23, 17.34] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ahn 1996.
| Study characteristics | ||
| Methods | Study design: randomized controlled, parallel‐group trial Setting/country: Department of Urology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, South Korea Dates study conducted: NR |
|
| Participants | Inclusion criteria:
Exclusion criteria:
Number of participants randomized: 23 Group 1 (fluoxetine)
Group 2 (placebo)
|
|
| Interventions | Group 1: fluoxetine 20 mg daily for first 1 week and 40 mg daily for remaining 5 weeks after breakfast Group 2: multivitamin as placebo daily |
|
| Outcomes | Primary outcomes:
Safety outcomes:
|
|
| Funding sources | NR | |
| Declarations of interest | NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "participants and investigator were blinded for the randomization," "randomized placebo controlled trial." |
| Blinding of outcome assessment (detection bias) Participant‐reported outcomes | Low risk | Quote: "participants and investigator were blinded for the randomization," "randomized placebo controlled trial." |
| Blinding of outcome assessment (detection bias) Investigator‐assessed outcomes | Low risk | Quote: "investigator were blinded for the randomization." |
| Blinding of outcome assessment (detection bias) IELT | Low risk | Objective measurement that was unlikely to be influenced by blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants included in analysis. |
| Selective reporting (reporting bias) | Unclear risk | Unpublished protocol/prespecified outcomes (intercourse frequency, libido) in method were not or were partially reported in the results. |
| Other bias | Low risk | No additional sources of bias identified. |
Athanasios 2007.
| Study characteristics | ||
| Methods | Study design: parallel‐group, randomized controlled trial Setting/country: Urology Department, ELPIS Hospital, Volos, Greece Dates study conducted: NR |
|
| Participants | Inclusion criteria:
Exclusion criteria:
Number of participants randomized: 20 Study length: 12 months Group 1 (duloxetine):
Group 2 (placebo):
|
|
| Interventions | Group 1: duloxetine 20 mg daily for 1 week followed by 40 mg daily Group 2: placebo daily |
|
| Outcomes | Primary outcome:
Secondary outcome:
Safety outcome:
|
|
| Funding sources | NR | |
| Declarations of interest | NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Did not explicitly state that personnel were blinded, only "double blind." |
| Blinding of outcome assessment (detection bias) Participant‐reported outcomes | Low risk | Participants appeared to be appropriately blinded. |
| Blinding of outcome assessment (detection bias) Investigator‐assessed outcomes | Unclear risk | No explicit description as to how these outcomes were assessed. |
| Blinding of outcome assessment (detection bias) IELT | Low risk | Objective measurement that was unlikely to be influenced by blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unclear how many participants were included in analyses. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | No additional sources of bias identified. |
Atmaca 2002.
| Study characteristics | ||
| Methods | Study design: randomized controlled, parallel‐group trial Setting/country: Firat University, Elazig, Turkey Dates study conducted: NR |
|
| Participants | Inclusion criteria:
Exclusion criteria:
Number of total participants randomized: 26 Group 1 (citalopram):
Group 2 (placebo):
|
|
| Interventions | Group 1: citalopram 20 mg daily up to 60 mg Group 2: placebo daily |
|
| Outcomes | Primary outcome:
Secondary outcomes:
Safety outcomes:
Other outcomes:
|
|
| Funding sources | NR | |
| Declarations of interest | NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Methods not described. |
| Allocation concealment (selection bias) | Unclear risk | Methods not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Appropriate use of placebo. Quote: "In group II, the patients received initially identical one placebo tablet per day and placebo was titrated to three capsules according to the clinical response, with increase of one tablet in two weeks’ period." |
| Blinding of outcome assessment (detection bias) Participant‐reported outcomes | Low risk | Participants appropriately blinded. |
| Blinding of outcome assessment (detection bias) Investigator‐assessed outcomes | Unclear risk | No blinding of outcome assessors explicitly described. |
| Blinding of outcome assessment (detection bias) IELT | Low risk | Objective measurement that was unlikely to be influenced by blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not explicit whether all participants included in final analysis. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | No additional sources of bias identified. |
Biri 1998.
| Study characteristics | ||
| Methods | Study design: double blind, parallel‐group, randomized controlled trial Setting/country: Department of Urology, Medical School of Gazi University, Ankara, Turkey Dates study conducted: January 1995 to April 1997 |
|
| Participants | Inclusion criteria:
Exclusion criteria:
Total number of participants randomized: 37 Total length of study: 4 weeks Group 1 (sertraline):
Group 2 (placebo):
|
|
| Interventions | Group 1: sertraline 50 mg daily Group 2: placebo daily |
|
| Outcomes | Primary outcomes:
Safety outcomes:
|
|
| Funding sources | NR | |
| Declarations of interest | NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of sequence generation not described. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not addressed. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants and personnel appeared appropriately blinded. Quote: "double‐blind treatment with sertraline or placebo." |
| Blinding of outcome assessment (detection bias) Participant‐reported outcomes | Low risk | Participants appeared to be blinded. |
| Blinding of outcome assessment (detection bias) Investigator‐assessed outcomes | Low risk | Blinding of outcome assessors not explicitly addressed. |
| Blinding of outcome assessment (detection bias) IELT | Low risk | Objective measurement that was unlikely to be influenced by blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unclear whether all participants were included in final analyses. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | No additional sources of bias identified. |
Buvat 2009.
| Study characteristics | ||
| Methods | Study design: parallel group, randomized controlled trial Setting/country: Centre ETPARP, Rue Carolus, Lille, France Dates study conducted: December 2004 to October 2006 |
|
| Participants | Inclusion criteria:
Exclusion criteria:
Total number of participants randomized: 1162 Total length of study: 24 weeks Group 1 (dapoxetine 30 mg):
Group 2 (dapoxetine 60 mg):
Group 3 (placebo):
|
|
| Interventions | Group 1: dapoxetine 30 mg on‐demand Group 2: dapoxetine 60 mg on‐demand Group 3: placebo daily |
|
| Outcomes | Primary outcomes:
Secondary outcomes:
Safety outcomes:
Other outcomes:
|
|
| Funding sources | Johnson & Johnson Pharmaceutical Research & Development, LLC provided funding or other financial support and material support for this research or work that included the following: design and conduct of the study, management of the data, analysis, interpretation of the data, preparation, review, and approval of the manuscript. | |
| Declarations of interest | Buvan and Giuliano are consultants or investigators (or both) for Johnson & Johnson Rivas, Rothamn and Tsfaye are employees of Johnson & Johnson. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated. |
| Allocation concealment (selection bias) | Low risk | Allocation concealed. Quote: "computer‐generated randomization schedule (assigned and coded using an interactive voice response system)." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Study described as double‐blind; no information beyond that. |
| Blinding of outcome assessment (detection bias) Participant‐reported outcomes | Unclear risk | Study described as double‐blind; no information beyond that. |
| Blinding of outcome assessment (detection bias) Investigator‐assessed outcomes | Unclear risk | No explicit blinding reported. |
| Blinding of outcome assessment (detection bias) IELT | Low risk | Objective measurement that was unlikely to be influenced by blinding. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Large proportions of participants not included in the final analysis; > 20% per treatment arm. |
| Selective reporting (reporting bias) | Low risk | Protocol was provided (NCT00229073) and all outcomes were reported. |
| Other bias | Low risk | No additional sources of bias identified. |
Farnia 2009.
| Study characteristics | ||
| Methods | Study design: parallel group, randomized controlled trial Setting/country: Department of Psychiatry, School of Medicine, Tehran University of Medical Sciences, Tehran, Iran Dates study conducted: May 2006 to June 2007 |
|
| Participants | Inclusion criteria:
Exclusion criteria:
Total number of participants randomized: 80 Total length of study: 4 weeks Group 1 (citalopram):
Group 2 (placebo):
|
|
| Interventions | Group 1: citalopram 20 mg 4 hours prior to sexual intercourse Group 2: placebo 4 hours prior to sexual intercourse |
|
| Outcomes | Primary outcomes:
Secondary outcomes:
Other outcomes:
|
|
| Funding sources | NR | |
| Declarations of interest | NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation concealment not described. |
| Allocation concealment (selection bias) | Unclear risk | No information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information provided beyond "double‐blind" design. |
| Blinding of outcome assessment (detection bias) Participant‐reported outcomes | Unclear risk | No information provided beyond "double‐blind" design. |
| Blinding of outcome assessment (detection bias) Investigator‐assessed outcomes | Unclear risk | Unclear whether outcome assessors blinded. |
| Blinding of outcome assessment (detection bias) IELT | Low risk | Objective measurement that was unlikely to be influenced by blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 7/49 (14.2%) in SSRI arm and 5/43 (11.6%) in placebo arm did not complete the trial. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | No additional sources of bias identified. |
Gameel 2013.
| Study characteristics | ||
| Methods | Study design: single‐blind, parallel‐group randomized controlled trial Setting/country: Urology Department, Tanta University Hospitals, Tanta, Egypt Dates study conducted: November 2009 to January 2012 |
|
| Participants | Inclusion criteria:
Exclusion criteria:
Total number of participants randomized: 150 Total length of study: 4 weeks Group 1 (paroxetine):
Group 2 (placebo):
|
|
| Interventions | Group 1: paroxetine 20 mg on‐demand + lubricating jelly Group 2: placebo on‐demand + lubricating jelly |
|
| Outcomes | Primary outcomes:
Secondary outcomes:
Safety outcomes:
|
|
| Funding sources | None | |
| Declarations of interest | None | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence created from "shuffling coded cards." |
| Allocation concealment (selection bias) | Unclear risk | Methods not described. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Personnel not blinded. Quote: "single blind study." |
| Blinding of outcome assessment (detection bias) Participant‐reported outcomes | Low risk | Appropriate use of placebo, participants likely blinded. Quote: "Group 5 was a placebo arm and received oral multivitamin pills 1–4 h before intercourse. To ensure that patients were unaware of the drug used, those receiving oral medication were also given local penile lubricating jelly before intercourse, whilst group 4 was also given oral multivitamin pills 1–4 h before intercourse." |
| Blinding of outcome assessment (detection bias) Investigator‐assessed outcomes | High risk | Assessors unlikely blinded. Quote: "single blind study." |
| Blinding of outcome assessment (detection bias) IELT | Low risk | Objective measurement that was unlikely to be influenced by blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low proportion of missing data (28/30 (94%) in SSRI arm and 27/30 (90%) in placebo arm included in final analysis). |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | No additional sources of bias identified. |
Gong 2011.
| Study characteristics | ||
| Methods | Study design: randomized controlled, parallel‐group trial Setting/country: Outpatient/Department of Urology, The affiliated hospital of Chuanbei Medical University, Nanchong, China Dates study conducted: NR |
|
| Participants | Inclusion criteria:
Exclusion criteria:
Number of participants randomized: 80 Group 1 (paroxetine):
Group 2 (placebo):
|
|
| Interventions | Group 1: paroxetine 20 mg daily orally Group 2: oral soda tablets as a placebo |
|
| Outcomes | Primary outcomes:
Safety outcomes:
|
|
| Funding sources | NR | |
| Declarations of interest | NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Methods not described. |
| Allocation concealment (selection bias) | Unclear risk | Methods not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not explicitly stated whether personnel were blinded; participants appeared to be blinded. |
| Blinding of outcome assessment (detection bias) Participant‐reported outcomes | Low risk | Participants likely blinded through the use of placebo. |
| Blinding of outcome assessment (detection bias) Investigator‐assessed outcomes | Unclear risk | Not explicitly described. |
| Blinding of outcome assessment (detection bias) IELT | Low risk | Objective measurement that was unlikely to be influenced by blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "All patients were followed up for 6 to 10 weeks." |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | No additional sources of bias identified. |
Hamidi Madani 2016.
| Study characteristics | ||
| Methods | Study design: double‐blind, placebo‐controlled randomized trial Setting/country: Department of Urology, Guilan University of Medical Sciences Rasht, Iran Dates study conducted: NR |
|
| Participants | Inclusion criteria:
Exclusion criteria:
Total number of participants randomized: 150 Total length of study: 12 weeks Group 1 (tramadol):
Group 2 (paroxetine):
Group 3 (placebo):
|
|
| Interventions | Group 1: tramadol 50 mg Group 2: paroxetine 20 mg Group 3: placebo |
|
| Outcomes | Primary outcomes:
Other outcomes:
|
|
| Funding sources | NR | |
| Declarations of interest | NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Abstract only; insufficient information to judge domain. |
| Allocation concealment (selection bias) | Unclear risk | Abstract only; insufficient information to judge domain. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Abstract only; insufficient information to judge domain. |
| Blinding of outcome assessment (detection bias) Participant‐reported outcomes | Unclear risk | Abstract only; insufficient information to judge domain. |
| Blinding of outcome assessment (detection bias) Investigator‐assessed outcomes | Unclear risk | Abstract only; insufficient information to judge domain. |
| Blinding of outcome assessment (detection bias) IELT | Low risk | Objective measurement that was unlikely to be influenced by blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Abstract only; insufficient information to judge domain. |
| Selective reporting (reporting bias) | Unclear risk | Abstract only; insufficient information to judge domain. |
| Other bias | Unclear risk | Abstract only; insufficient information to judge domain. |
Kara 1996.
| Study characteristics | ||
| Methods | Study design: double‐blind, placebo‐controlled, parallel‐group trial Setting/country: Department of Psychiatry and Urology Yuzunku Yil University, Van, Turkey Dates study conducted: NR |
|
| Participants | Inclusion criteria:
Exclusion criteria:
Total number of participants randomized: 14 Total length of study: 4 weeks Group 1 (fluoxetine):
Group 2 (placebo):
|
|
| Interventions | Group 1: fluoxetine 20 mg daily for 1 week and fluoxetine 40 mg afterwards Group 2: placebo 1 tablet at breakfast daily for week and 2 tablets afterwards |
|
| Outcomes | Primary outcomes:
Other outcomes:
|
|
| Funding sources | NR | |
| Declarations of interest | NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of sequence generation not described. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not addressed. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Participants may be blinded but blinding of personnel was not described. |
| Blinding of outcome assessment (detection bias) Participant‐reported outcomes | Low risk | Participants likely blinded appropriately. |
| Blinding of outcome assessment (detection bias) Investigator‐assessed outcomes | Unclear risk | Not explicitly described. |
| Blinding of outcome assessment (detection bias) IELT | Low risk | Objective measurement that was unlikely to be influenced by blinding. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 7/9 participants in fluoxetine arm and 7/8 participants in placebo arm included in final analysis. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | No additional sources of bias identified. |
Kaufman 2009.
| Study characteristics | ||
| Methods | Study design: blind, randomized controlled, parallel‐group trial Setting/country: multi‐institutional Aurora, USA Dates study conducted: November 2009 to January 2012 |
|
| Participants | Inclusion criteria:
Exclusion criteria:
Total number of participants randomized: 736 Total length of study: 9 weeks Group 1 (dapoxetine):
Group 2 (placebo):
|
|
| Interventions | Group 1: dapoxetine 60 mg on‐demand Group 2: placebo on‐demand |
|
| Outcomes | Primary outcomes:
Secondary outcomes:
Safety outcomes:
Other outcomes:
Other outcomes:
Other outcomes:
|
|
| Funding sources | Funded by Johnson & Johnson Pharmaceutical Research & Development, LLC, Raritan, NJ | |
| Declarations of interest | Funded by Johnson & Johnson Pharmaceutical Research & Development, LLC, Raritan, NJ, USA. Drs Mudumbi, Tesfaye and Rivas are employees of Johnson & Johnson; Dr Hashmonay was an employee of Johnson & Johnson at the time of the study. Dr Kaufman is an investigator for Johnson & Johnson. Dr Rosen is an investigator/consultant for Johnson & Johnson. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Methods not described. |
| Allocation concealment (selection bias) | Unclear risk | Methods not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Likely appropriately blinded. Quote: "dosing carried out in a double‐blind, double‐dummy fashion." |
| Blinding of outcome assessment (detection bias) Participant‐reported outcomes | Low risk | Participants likely to be appropriately blinded. Quote: "dosing carried out in a double‐blind, double‐dummy fashion." |
| Blinding of outcome assessment (detection bias) Investigator‐assessed outcomes | Unclear risk | Not explicitly described who was assessing adverse effects. |
| Blinding of outcome assessment (detection bias) IELT | Low risk | Objective measurement that was unlikely to be influenced by blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Large numbers excluded from analysis and not even lost to follow‐up between groups (60/491 in dapoxetine arm and 24/245 in placebo arm were excluded). |
| Selective reporting (reporting bias) | High risk | Data on participants receiving dapoxetine 60 mg daily NR. |
| Other bias | Low risk | No additional sources of bias identified. |
Khelaia 2012.
| Study characteristics | ||
| Methods | Study design: randomized controlled, parallel‐group trial Setting/country: National Center of Urology, Department of Urology Tbilisi, Georgia Dates study conducted: NR |
|
| Participants | Inclusion criteria:
Exclusion criteria:
Total number of participants randomized: 78 Total length of study: 4 weeks Group 1 (paroxetine 20 mg):
Group 2 (paroxetine 20 mg 2–3 hours before intercourse):
Group 3 (placebo):
|
|
| Interventions | Group 1: paroxetine 20 mg Group 2: paroxetine 20 mg 2–3 hours before intercourse Group 3: placebo |
|
| Outcomes | Primary outcomes:
Secondary outcomes:
Secondary outcomes:
Safety outcomes:
|
|
| Funding sources | NR | |
| Declarations of interest | NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Abstract only; insufficient information to judge domain. |
| Allocation concealment (selection bias) | Unclear risk | Abstract only; insufficient information to judge domain. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Abstract only; insufficient information to judge domain. |
| Blinding of outcome assessment (detection bias) Participant‐reported outcomes | Unclear risk | Abstract only; insufficient information to judge domain. |
| Blinding of outcome assessment (detection bias) Investigator‐assessed outcomes | Unclear risk | Abstract only; insufficient information to judge domain. |
| Blinding of outcome assessment (detection bias) IELT | Low risk | Objective measurement that was unlikely to be influenced by blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Abstract only; insufficient information to judge domain. |
| Selective reporting (reporting bias) | Unclear risk | Abstract only; insufficient information to judge domain. |
| Other bias | Unclear risk | Abstract only; insufficient information to judge domain. |
Kim 1998.
| Study characteristics | ||
| Methods | Study design: cross‐over randomized controlled trial Setting/country: College of Medicine, Chung‐Ang University, Seoul, Korea Dates study conducted: NR |
|
| Participants | Inclusion criteria:
Exclusion criteria:
Total number of participants randomized: 37 Total length of study: 16 weeks total (4 weeks each intervention) Group 1 (fluoxetine):
Group 2 (sertraline):
(Note that the comparison in this study was the placebo cross‐over period) |
|
| Interventions | Group 1: fluoxetine 40 mg daily for 1 week then 80 mg for 3 weeks Group 2: sertraline 100 mg for 1 week then 200 mg for 3 weeks |
|
| Outcomes | Primary outcomes:
Secondary outcomes:
Safety outcomes:
|
|
| Funding sources | NR | |
| Declarations of interest | NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described whether order of treatment was randomized. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Title stated "double‐blind" and described medication being identical but did not explicitly state that personnel were blinded. |
| Blinding of outcome assessment (detection bias) Participant‐reported outcomes | Low risk | Participants likely blinded appropriately. Quote: "capsules were identical." |
| Blinding of outcome assessment (detection bias) Investigator‐assessed outcomes | Unclear risk | Not explicitly described. |
| Blinding of outcome assessment (detection bias) IELT | Low risk | Objective measurement that was unlikely to be influenced by blinding. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 16/53 participants did not complete the study and no details provided on when or why they dropped out. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | No additional sources of bias identified. |
Mattos 2008.
| Study characteristics | ||
| Methods | Study design: randomized controlled, parallel‐group trial Setting/country: Universidade de Sao Paulo, Institute of Urology, Sao Paulo, Brazil Dates study conducted: NR |
|
| Participants | Inclusion criteria:
Exclusion criteria:
Total number of participants randomized: 60 Total length of study: 12 weeks Group 1 (fluoxetine):
Group 2 (placebo):
Group 3 (fluoxetine + tadalafil):
Group 4 (placebo + tadalafil):
|
|
| Interventions | Group 1: fluoxetine 90 mg daily Group 2: placebo daily Group 3: fluoxetine 90 mg daily + tadalafil 20 mg on‐demand Group 4: placebo + tadalafil 20 mg on‐demand |
|
| Outcomes | Primary outcomes:
Safety outcomes:
|
|
| Funding sources | None | |
| Declarations of interest | NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "four groups were randomly distributed…chosen blindly from one envelope with numbers and another envelope with colors designating a treatment." |
| Allocation concealment (selection bias) | Low risk | Quote: "…were concealed by a third party that blinded the placebo and active capsules to the investigator and patients alike." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Appropriate blinding. Quote: "neither the investigator nor the patient knew which treatment was being used." |
| Blinding of outcome assessment (detection bias) Participant‐reported outcomes | Low risk | Quote: "… were concealed by a third party that blinded the placebo and active capsules to the investigator and patients alike." |
| Blinding of outcome assessment (detection bias) Investigator‐assessed outcomes | Unclear risk | Not explicitly described who was assessing adverse effects. |
| Blinding of outcome assessment (detection bias) IELT | Low risk | Objective measurement that was unlikely to be influenced by blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants randomized were included. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | No source identified. |
McMahon 1998.
| Study characteristics | ||
| Methods | Study design: randomized controlled, cross‐over study Setting/country: St. Luke's Hospital, Sydney, Australia Dates study conducted: NR |
|
| Participants | Inclusion criteria:
Exclusion criteria:
Total number of participants randomized: 37 Total length of study: 12 weeks Group 1 (sertraline):
Group 2 (placebo):
|
|
| Interventions | Group 1: sertraline 50 mg Group 2: placebo daily |
|
| Outcomes | Primary outcomes:
Safety outcomes:
|
|
| Funding sources | NR | |
| Declarations of interest | NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "single blind;" "placebo tablets were identical to the active drug." Likely participants were blinded but personnel were not blinded |
| Blinding of outcome assessment (detection bias) Participant‐reported outcomes | Low risk | Single blind. Likely participants were blinded. Quote: "placebo were identical to the active drug." |
| Blinding of outcome assessment (detection bias) Investigator‐assessed outcomes | High risk | Assessors unlikely blinded. Quote: "single blind study." |
| Blinding of outcome assessment (detection bias) IELT | Low risk | Objective measurement that was unlikely to be influenced by blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants that were randomized appeared to be included in final analysis. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | No additional sources of bias identified. |
McMahon 1999.
| Study characteristics | ||
| Methods | Study design: controlled, single‐blind, cross‐over study Setting/country: St. Luke's Hospital, Sydney, Australia Dates study conducted: NR |
|
| Participants | Inclusion criteria:
Exclusion criteria:
Length of study: 17 weeks Study 1: Total number of participants randomized: 26 Number of participants with primary ejaculation: 19 Number of participants with secondary ejaculation: 7 Group 1 (paroxetine 20 mg):
Group 2 (paroxetine as needed 3–4 hours before planned sexual intercourse):
Study 2: Total number of participants randomized in study 2: 42 Number of participants with primary ejaculation: 32 Number of participants with secondary ejaculation: 10 Group 3 (paroxetine 10 mg for 3 weeks then 20 mg paroxetine as needed for 4 weeks):
Group 4 (placebo daily for 3 weeks then placebo daily for 4 weeks):
|
|
| Interventions | Group 1: paroxetine 20 mg Group 2: paroxetine as needed 3–4 hours before planned sexual intercourse Group 3: paroxetine 10 mg for 3 weeks then 20 mg paroxetine as needed for 4 weeks Group 4: placebo daily for 3 weeks then placebo daily for 4 weeks |
|
| Outcomes | Primary outcomes:
Safety outcomes:
|
|
| Funding sources | NR | |
| Declarations of interest | NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "single blind;" "placebo were identical to the active drug." Likely participants were blinded but personnel were not blinded. |
| Blinding of outcome assessment (detection bias) Participant‐reported outcomes | Low risk | Single blind. Likely participants were blinded. Quote: "placebo tablets were identical to the active drug." |
| Blinding of outcome assessment (detection bias) Investigator‐assessed outcomes | High risk | Assessors unlikely blinded. Quote: "single blind study." |
| Blinding of outcome assessment (detection bias) IELT | Low risk | Objective measurement that was unlikely to be influenced by blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants who were randomized appeared to be included in final analysis. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | No additional sources of bias identified. |
McMahon 2010.
| Study characteristics | ||
| Methods | Study design: blinded, randomized controlled, parallel‐group trial Setting/country: multicenter in Asia Pacific Dates study conducted: March 2005 to June 2006 |
|
| Participants | Inclusion criteria:
Exclusion criteria:
Total number of participants randomized: 1067 Total length of study: 12 weeks Group 1 (dapoxetine 30 mg):
Group 2 (dapoxetine 60 mg):
Group 3 (placebo):
|
|
| Interventions | Group 1: dapoxetine 30 mg on‐demand Group 2: dapoxetine 60 mg on‐demand Group 3: placebo on‐demand |
|
| Outcomes | Primary outcomes:
Secondary outcomes:
Safety outcomes:
|
|
| Funding sources | Study funded by Johnson & Johnson Pharmaceutical Research & Development, LLC, Raritan, NJ, USA. | |
| Declarations of interest | Dr McMahon is a consultant/investigator for Johnson & Johnson. Drs Kim, Park and Chang are investigators for Johnson & Johnson. Drs Rivas, Tesfaye, Rothman and Aquilina are employees of Johnson & Johnson. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Methods not described. |
| Allocation concealment (selection bias) | Unclear risk | Methods not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Study described as double‐blind; no further information. |
| Blinding of outcome assessment (detection bias) Participant‐reported outcomes | Low risk | Likely appropriate blinding, "double‐blind" and placebo was used. |
| Blinding of outcome assessment (detection bias) Investigator‐assessed outcomes | Unclear risk | Not explicitly described. |
| Blinding of outcome assessment (detection bias) IELT | Low risk | Objective measurement that was unlikely to be influenced by blinding. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 62/395 (17%) in placebo, 70/354 (20%) in dapoxetine 30 mg, 77/356 (22%) in dapoxetine 60 mg were not included in the analysis. |
| Selective reporting (reporting bias) | Low risk | As reported in protocol in ClinicalTrials.gov. |
| Other bias | Low risk | No additional sources of bias identified. |
McMahon 2013.
| Study characteristics | ||
| Methods | Study design: randomized controlled, parallel‐group trial Setting/country: Berry Road Medical Center, the Leonards, Australia Dates study conducted: April 2010 to August 2011 |
|
| Participants | Inclusion criteria:
Exclusion criteria:
Total number of participants randomized: 495 Total length of study: 18 weeks Group 1 (dapoxetine):
Group 2 (placebo):
|
|
| Interventions | Group 1: dapoxetine 30 mg on‐demand, from week 4 up to 60 mg if tolerated + PDE5 inhibitor taken 1–3 hours prior to sexual intercourse Group 2: placebo daily + PDE5 inhibitor taken 1–3 hours prior to intercourse |
|
| Outcomes | Primary outcomes:
Secondary outcomes:
Safety outcomes:
|
|
| Funding sources | Janssen Research & Development, LLC funded this study (R096769PRE3008) and provided formal review of the article. | |
| Declarations of interest | Janssen Research & Development, LLC funded this study (R096769PRE3008) and provided formal review of the article. Bradford Challis, PhD, an employee of the company, provided writing assistance for the manuscript. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization relied on a computer‐generated random sequence and an interactive voice response system." |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomization relied on a computer‐generated random sequence and an interactive voice response system." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Only the IDMC statistician was unblinded to the treatment assignments at the interim analysis." Therefore, can assume that participants, investigators and personnel were blinded. |
| Blinding of outcome assessment (detection bias) Participant‐reported outcomes | Low risk | Likely appropriately blinded. Quote: "subjects were instructed to administer study drug (dapoxetine or matching placebo)." |
| Blinding of outcome assessment (detection bias) Investigator‐assessed outcomes | Low risk | Quote: "Only the IDMC statistician was unblinded to the treatment assignments at the interim analysis." Therefore, can assume that investigators and personnel were blinded. |
| Blinding of outcome assessment (detection bias) IELT | Low risk | Objective measurement that was unlikely to be influenced by blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Large number of discontinuations and not balanced between groups (29/250 in dapoxetine arm and 37/245 in placebo arm). |
| Selective reporting (reporting bias) | Low risk | As reported in protocol in ClinicalTrials.gov. |
| Other bias | Low risk | No additional sources of bias identified. |
Mendels 1995.
| Study characteristics | ||
| Methods | Study design: randomized controlled, parallel‐group trial Setting/country: Philadelphia Medical Institute, USA Dates study conducted: NR |
|
| Participants | Inclusion criteria:
Exclusion criteria:
Total number of participants randomized: 52 Total length of study: 10 weeks Group 1 (sertraline):
Group 2 (placebo):
|
|
| Interventions | Group 1: sertraline 50 mg daily that could be titrated up to 200 mg daily Group 2: placebo daily |
|
| Outcomes | Primary outcomes:
Secondary outcomes:
Safety outcomes:
Other outcomes:
|
|
| Funding sources | None | |
| Declarations of interest | Pfizer involved but not specified | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated. |
| Allocation concealment (selection bias) | Unclear risk | Methods not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Likely blinded appropriately as study was "double blind" and patients received "matching placebo." |
| Blinding of outcome assessment (detection bias) Participant‐reported outcomes | Low risk | Likely appropriately blinded. Quote: "patients were provided with bottles containing 50mg sertraline tablets or matching placebo." |
| Blinding of outcome assessment (detection bias) Investigator‐assessed outcomes | Unclear risk | Not explicitly described. |
| Blinding of outcome assessment (detection bias) IELT | Low risk | Objective measurement that was unlikely to be influenced by blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Efficacy analysis; 3/26 (11.5%) in sertraline arm and 2/26 (7.6%) in placebo arm were not included in the efficacy analysis. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Unclear risk | Quote: "sertraline patients had a longer previous Hx of premature ejaculation" (baseline imbalance), and "1 week single blind washout period," which may both exaggerate treatment effect. |
Na 1996.
| Study characteristics | ||
| Methods | Study design: randomized controlled, parallel‐group trial Setting/country: Outpatient/Department of Urology, Korea University College of Medicine, Seoul, South Korea Dates study conducted: NR |
|
| Participants | Inclusion criteria:
Exclusion criteria:
Number of participants randomized: 40 Group 1 (sertraline):
Group 2 (placebo):
|
|
| Interventions | Group 1: sertraline 50 mg at night that could be titrated up to 100 mg daily Group 2: digestive medicine with same manner of intervention |
|
| Outcomes | Primary outcomes:
Safety outcomes:
|
|
| Funding sources | NR | |
| Declarations of interest | NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of sequence generation not described. |
| Allocation concealment (selection bias) | Unclear risk | Methods not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Study described as double‐blind; no further information. |
| Blinding of outcome assessment (detection bias) Participant‐reported outcomes | Unclear risk | No information. |
| Blinding of outcome assessment (detection bias) Investigator‐assessed outcomes | Unclear risk | No information. |
| Blinding of outcome assessment (detection bias) IELT | Low risk | Objective measurement that was unlikely to be influenced by blinding. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 12/20 in sertraline arm and 8/20 participants in placebo arm were included in analysis. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available and review outcomes were not clearly defined in method section. |
| Other bias | Low risk | No additional sources of bias identified. |
Novaretti 2002.
| Study characteristics | ||
| Methods | Study design: cross‐over RCT Setting/country: University of São Paulo (USP), São Paulo, SP, Brazil Dates study conducted: June 1998 to January 2000 |
|
| Participants | Inclusion criteria:
Exclusion criteria:
Total number of participants randomized: 55 Total length of study: 20 weeks Group 1 (fluoxetine):
Group 2 (placebo):
|
|
| Interventions | Group 1: fluoxetine 20 mg daily Group 2: placebo daily |
|
| Outcomes | Primary outcomes:
Secondary outcomes:
Safety outcomes:
Other outcomes:
Other outcomes:
|
|
| Funding sources | FARMASA laboratory provided the fluoxetine and the placebo. | |
| Declarations of interest | NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of sequence generation not described. |
| Allocation concealment (selection bias) | Low risk | The code (the letter corresponding to the fluoxetine or the letter corresponding to the placebo) was kept in a sealed envelope until the completion of data collection from all participants. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Both the researcher and the patients did not know who was taking the active drug and who was taking the placebo." |
| Blinding of outcome assessment (detection bias) Participant‐reported outcomes | Low risk | Quote: "Both the researcher and the patients did not know who was taking the active drug and who was taking the placebo." |
| Blinding of outcome assessment (detection bias) Investigator‐assessed outcomes | Low risk | Quote: "Both the researcher and the patients did not know who was taking the active drug and who was taking the placebo." |
| Blinding of outcome assessment (detection bias) IELT | Low risk | Objective measurement that was unlikely to be influenced by blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants included in analysis. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | No additional sources of bias identified. |
Pryor 2006.
| Study characteristics | ||
| Methods | Study design: blinded, randomized controlled, parallel‐group trial Setting/country: multi‐institution, Dapoxetine Study Group in DE&MN, USA Dates study conducted: June 2003 to June 2004 |
|
| Participants | Inclusion criteria:
Exclusion criteria:
Total number of participants randomized: NR Total length of study: 12 weeks Group 1 (dapoxetine 30 mg):
Group 2 (dapoxetine 60 mg):
Group 3 (placebo):
|
|
| Interventions | Group 1: dapoxetine 30 mg on‐demand 1–3 hours before anticipated sexual activity Group 2: dapoxetine 60 mg on‐demand 1–3 hours before anticipated sexual activity Group 3: placebo on‐demand 1–3 hours before anticipated sexual activity |
|
| Outcomes | Primary outcomes:
Secondary outcomes:
Other outcomes:
Other outcomes:
Other outcomes:
Other outcomes:
|
|
| Funding sources | NR | |
| Declarations of interest | SE Althof, RC Rosen, WJG Hellstrom and R Shabsigh have served as consultants for Johnson & Johnson. R Shabsigh has also received grant/research support from Johnson & Johnson. M Miloslavsky and S Kell are employees of ALZA Corporation. JL Pryor and C Steidle have served on advisory boards for ALZA Corporation. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "randomly assigned within each stratum 1:1:1 by a computerised interactive voice recognition system." |
| Allocation concealment (selection bias) | Low risk | Randomly assigned within each stratum 1:1:1 by a computerized interactive voice recognition system. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Probably double blind. Quote: "tablets in all groups were identical in appearance;" "Investigator assessed adverse event severity." |
| Blinding of outcome assessment (detection bias) Participant‐reported outcomes | Low risk | Tablets in all groups were identical in appearance. |
| Blinding of outcome assessment (detection bias) Investigator‐assessed outcomes | Low risk | Investigator assessed adverse event severity. |
| Blinding of outcome assessment (detection bias) IELT | Low risk | Objective measurement that is unlikely to be influenced by blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "All analyses were done on an intention‐to‐treat basis." All participants were included in the analysis. |
| Selective reporting (reporting bias) | Low risk | As reported in protocol in ClinicalTrials.gov. |
| Other bias | Low risk | No clear source identified. |
Safarinejad 2006b.
| Study characteristics | ||
| Methods | Study design: randomized controlled, parallel‐group trial Setting/country: single institute, Tehran, Iran Dates study conducted: March 2003 to April 2005 |
|
| Participants | Inclusion criteria:
Exclusion criteria:
Total number of participants randomized: 340 Total length of study: 12 weeks Group 1 (dapoxetine):
Group 2 (paroxetine):
Group 3 (placebo):
|
|
| Interventions | Group 1: dapoxetine 60 mg daily Group 2: paroxetine 20 mg daily Group 3: placebo daily |
|
| Outcomes | Primary outcomes:
Secondary outcomes:
Safety outcomes:
|
|
| Funding sources | NR | |
| Declarations of interest | NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Likely random Quote: "a randomization table generated by the method of randomly permuted blocks." |
| Allocation concealment (selection bias) | Low risk | Quote: "Each eligible patient was given a randomization number using an interactive voice response system … Persons who geographically and operationally were independent from the study investigator did the randomization of the study." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Likely appropriate. Quote: "Treatment was administered in a randomized sequence that remained unknown to the patient and to the physician." |
| Blinding of outcome assessment (detection bias) Participant‐reported outcomes | Low risk | Likely appropriate blinding as participants received a placebo. Quote: "Active drugs and placebo were identical in color and size." |
| Blinding of outcome assessment (detection bias) Investigator‐assessed outcomes | Low risk | Adverse effects were evaluated by investigator that was likely blinded appropriately. Quote: "For the analysis of efficacy and safety, all patients were evaluated in each visit by the author" and an individual "independent from the study investigator did the randomization of the study." |
| Blinding of outcome assessment (detection bias) IELT | Low risk | Objective measurement that was unlikely to be influenced by blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | < 10% of participants excluded from each arm (10/115 in dapoxetine arm, 11/113 in paroxetine arm and 10/112 in placebo arm, including 3 in dapoxetine arm vs 2 in paroxetine vs 6 in placebo arm excluded for lack of efficacy). |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | No additional sources of bias identified. |
Safarinejad 2006c.
| Study characteristics | ||
| Methods | Study design: randomized controlled, parallel‐group trial Setting/country: University of Medical Sciences, Tehran, Iran Dates study conducted: NR |
|
| Participants | Inclusion criteria:
Exclusion criteria:
Total number of participants randomized: 58 Total length of study: 6 months Group 1 (citalopram):
Group 2 (placebo):
|
|
| Interventions | Group 1: citalopram 20 mg daily Group 2: placebo daily |
|
| Outcomes | Primary outcomes:
Secondary outcomes:
Secondary outcomes:
Safety outcomes:
|
|
| Funding sources | NR | |
| Declarations of interest | NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was determined by a computer‐generated schedule." |
| Allocation concealment (selection bias) | Unclear risk | Methods not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Likely appropriate blinding. Quote: "Treatment was administered in a randomized sequence that remained unknown to the patient and to the physicians." |
| Blinding of outcome assessment (detection bias) Participant‐reported outcomes | Low risk | Likely appropriate blinding. Quote: "Treatment was administered in a randomized sequence that remained unknown to the patient and to the physicians." |
| Blinding of outcome assessment (detection bias) Investigator‐assessed outcomes | Unclear risk | Not explicitly described. |
| Blinding of outcome assessment (detection bias) IELT | Low risk | Objective measurement that is unlikely to be influenced by blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 3/29 (10.3%) in citalopram arm and 4/39 (13.7%) in placebo arm were not included. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | No additional sources of bias identified. |
Safarinejad 2007.
| Study characteristics | ||
| Methods | Study design: randomized controlled, parallel‐group trial Setting/country: single institute, Tehran, Iran Dates study conducted: March 2003 to April 2005 |
|
| Participants | Inclusion criteria:
Exclusion criteria:
Total number of participants randomized: 276 Total length of study: 12 weeks Group 1 (escitalopram):
Group 2 (placebo):
|
|
| Interventions | Group 1: escitalopram 10 mg daily Group 2: placebo daily |
|
| Outcomes | Primary outcomes:
Secondary outcomes:
Safety outcomes:
|
|
| Funding sources | None | |
| Declarations of interest | NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "a randomization table generated by the method of random permuted block. Patient randomization numbers were allocated to each site in ascending sequence in blocks." |
| Allocation concealment (selection bias) | Low risk | Quote: "Assignment to treatment group was performed using an interactive voice response system." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Likely appropriate blinding. Quote: "Group 2 received a similar regimen of placebo. Placebo and escitalopram tablets were identical in appearance, allowing for blinding of treatment assignment." Randomization was done by an individual separate from the single investigator who assessed each participant. |
| Blinding of outcome assessment (detection bias) Participant‐reported outcomes | Low risk | Likely appropriate blinding. Quote: "Group 2 received a similar regimen of placebo. Placebo and escitalopram tablets were identical in appearance, allowing for blinding of treatment assignment." |
| Blinding of outcome assessment (detection bias) Investigator‐assessed outcomes | Low risk | Single investigator who was likely blinded interviewed participants at each visit. |
| Blinding of outcome assessment (detection bias) IELT | Low risk | Objective measurement that was unlikely to be influenced by blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 10/138 in the escitalopram arm and 12/138 in the placebo arm excluded. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | No additional sources of bias identified. |
Safarinejad 2008.
| Study characteristics | ||
| Methods | Study design: randomized controlled, parallel‐group trial Setting/country: single institute, Tehran, Iran Dates study conducted: February 2004 to March 2006 |
|
| Participants | Inclusion criteria:
Exclusion criteria:
Total number of participants randomized: 212 Total length of study: 12 weeks Group 1 (dapoxetine):
Group 2 (placebo):
|
|
| Interventions | Group 1: dapoxetine 30 mg twice daily Group 2: placebo daily |
|
| Outcomes | Primary outcomes:
Secondary outcomes:
Safety outcomes:
|
|
| Funding sources | None | |
| Declarations of interest | None | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Likely random. Quote: "randomization table generated by the method of random permuted blocks." |
| Allocation concealment (selection bias) | Low risk | Quote: "interactive voice response system … Persons who geographically and operationally were independent from the study investigator did the randomization of the study." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Likely appropriately blinded. Quote: "Treatment was administered in a randomized sequence that remained unknown to the patient and to the physician." |
| Blinding of outcome assessment (detection bias) Participant‐reported outcomes | Low risk | Likely appropriately blinded. Quote: "Treatment was administered in a randomized sequence that remained unknown to the patient." |
| Blinding of outcome assessment (detection bias) Investigator‐assessed outcomes | Unclear risk | Not explicitly described. |
| Blinding of outcome assessment (detection bias) IELT | Low risk | Objective measurement that is unlikely to be influenced by blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 13/106 (12.2%) in dapoxetine arm and 10/106 (9.4%) in placebo arm excluded from final analysis. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | No additional sources of bias identified. |
Shang 2012.
| Study characteristics | ||
| Methods | Study design: randomized controlled, parallel‐group trial Setting/country: multi‐institution, China Dates study conducted: May 2011 to May 2012 |
|
| Participants | Inclusion criteria:
Exclusion criteria:
Number of participants randomized: 80 Group 1 (citalopram 20 mg daily):
Group 2 (placebo):
|
|
| Interventions | Group 1: paroxetine 20 mg daily orally Group 2: soda tablets as a placebo orally |
|
| Outcomes | Primary outcomes:
Safety outcomes:
|
|
| Funding sources | NR | |
| Declarations of interest | NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Did not explicitly state whether investigators were blinded; participants appeared to be blinded. |
| Blinding of outcome assessment (detection bias) Participant‐reported outcomes | Low risk | Participants appeared to be appropriately blinded. Quote: "In the control group, oral placebo medication is the same colour and size as treatment group containing starch complexes." |
| Blinding of outcome assessment (detection bias) Investigator‐assessed outcomes | Unclear risk | Not explicitly described. |
| Blinding of outcome assessment (detection bias) IELT | Low risk | Objective measurement that was unlikely to be influenced by blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants included in analysis. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | No additional sources of bias identified. |
Tuncel 2008.
| Study characteristics | ||
| Methods | Study design: randomized controlled, parallel‐group trial Setting/country: Third Department of Urology, Ministry of Health, Ankara Numune Research and Training Hospital, Ankara, Turkey Dates study conducted: NR |
|
| Participants | Inclusion criteria:
Exclusion criteria:
Total number of participants randomized: 90 Total length of study: 8 weeks Group 1 (sertraline):
Group 2 (placebo):
|
|
| Interventions | Group 1: sertraline 50 mg nightly for 2 months Group 2: placebo daily |
|
| Outcomes | Primary outcomes:
Safety outcomes:
|
|
| Funding sources | NR | |
| Declarations of interest | NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Methods not described. |
| Allocation concealment (selection bias) | Unclear risk | Methods not described. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Personnel not blinded. Quote: "single blind study." |
| Blinding of outcome assessment (detection bias) Participant‐reported outcomes | Low risk | Likely appropriate blinding with use of placebo. Quote: "Group 1 (n = 22 took placebo)" |
| Blinding of outcome assessment (detection bias) Investigator‐assessed outcomes | High risk | Assessors unlikely blinded. Quote: "single blind study." |
| Blinding of outcome assessment (detection bias) IELT | Low risk | Objective measurement that was unlikely to be influenced by blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants who were randomized appeared to be included in final analysis. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | No additional sources of bias identified. |
Waldinger 1994.
| Study characteristics | ||
| Methods | Study design: randomized controlled, parallel‐group trial Setting/country: Department of Psychiatry and Neurosexology, Leyenburg Hospital, The Hague, The Netherlands Dates study conducted: NR |
|
| Participants | Inclusion criteria:
Exclusion criteria:
Total number of participants randomized: 17 Total length of study: 6 weeks Group 1 (paroxetine):
Group 2 (placebo):
|
|
| Interventions | Group 1: paroxetine 20 mg daily for 1 week and then 40 mg daily from week 2–6 Group 2: placebo daily |
|
| Outcomes | Primary outcomes:
Secondary outcomes:
Safety outcomes:
|
|
| Funding sources | NR | |
| Declarations of interest | NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Methods not described. |
| Allocation concealment (selection bias) | Unclear risk | Methods not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Likely appropriate blinding. Quote: "capsules [treatment and placebo] were identical." |
| Blinding of outcome assessment (detection bias) Participant‐reported outcomes | Low risk | Use of placebo and participants likely appropriately blinded. Quote: "capsules were identical." |
| Blinding of outcome assessment (detection bias) Investigator‐assessed outcomes | Unclear risk | Not explicitly described. |
| Blinding of outcome assessment (detection bias) IELT | Low risk | Objective measurement that was unlikely to be influenced by blinding. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 2 participants from paroxetine arm (2/8 (25%)), 1 participant from placebo arm (1/9 (10.1%)) were dropped out. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | No additional sources of bias identified. |
Waldinger 1998.
| Study characteristics | ||
| Methods | Study design: randomized controlled, parallel‐group trial Setting/country: Department of Psychiatry and Neurosexology, Leyenburg Hospital, The Hague, The Netherlands Dates study conducted: NR |
|
| Participants | Inclusion criteria:
Exclusion criteria:
Total number of participants randomized: 60 Total length of study: 6 weeks Group 1 (fluoxetine):
Group 2 (fluvoxamine):
Group 3 (paroxetine):
Group 4 (sertraline):
Group 5 (placebo):
|
|
| Interventions | Group 1: fluoxetine 20 mg daily Group 2: fluvoxamine 100 mg daily Group 3: paroxetine 20 mg daily Group 4: sertraline 50 mg daily Group 5: placebo daily |
|
| Outcomes | Primary outcomes:
Secondary outcomes:
Safety outcomes:
Other outcomes:
|
|
| Funding sources | Solvay Pharmaceuticals | |
| Declarations of interest | NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "standard random number generator." |
| Allocation concealment (selection bias) | Unclear risk | Methods not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Likely appropriate blinding. Quote: "capsules [treatment and placebo] were identical." |
| Blinding of outcome assessment (detection bias) Participant‐reported outcomes | Low risk | Likely appropriately blinded. Quote: "patients in the first study were randomly assigned, in a double‐blind manner, to receive either fluoxetine 20 mg/day, fluvoxamine 100 mg/day, paroxetine 20 mg/day, sertraline 50 mg/day, or placebo in the form of 2 identical capsules per day given in a single morning dose." |
| Blinding of outcome assessment (detection bias) Investigator‐assessed outcomes | Unclear risk | Not explicitly described who was assessing adverse effects. |
| Blinding of outcome assessment (detection bias) IELT | Low risk | Objective measurement that was unlikely to be influenced by blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Large proportion of participants excluded from final analysis (9/60) with no ITT performed. |
| Selective reporting (reporting bias) | High risk | No protocol available and adverse effects outcome was only partially reported in the results. |
| Other bias | Low risk | No additional sources of bias identified. |
Yilmaz 1999.
| Study characteristics | ||
| Methods | Study design: blinded, randomized controlled, parallel‐group trial Setting/country: Department of Urology and Neurology, Erciyes University Medical Faculty, Gevher Nesiber Research and Training Hospital, Kayseri, Turkey Dates study conducted: January 1997 to November 1997 |
|
| Participants | Inclusion criteria:
Exclusion criteria:
Total number of participants randomized: 40 Total length of study: 1 month Group 1 (fluoxetine):
Group 2 (placebo):
|
|
| Interventions | Group 1: fluoxetine 20 mg daily Group 2: placebo daily |
|
| Outcomes | Primary outcomes:
Secondary outcomes:
Safety outcomes:
Other outcomes:
Other outcomes:
|
|
| Funding sources | NR | |
| Declarations of interest | NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Methods not described. |
| Allocation concealment (selection bias) | Unclear risk | Methods not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Study described as "double blind," but not clear whether personnel who interviewed participants at the end regarding adverse effects were blinded. |
| Blinding of outcome assessment (detection bias) Participant‐reported outcomes | Low risk | Likely appropriately blinded. Quote: "control group received placebo." |
| Blinding of outcome assessment (detection bias) Investigator‐assessed outcomes | Unclear risk | Not explicitly described. |
| Blinding of outcome assessment (detection bias) IELT | Low risk | Objective measurement that was unlikely to be influenced by blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Number of participants included in the final analysis was not clearly described. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | No additional sources of bias identified. |
CGI: Clinical Global Impression; CGIC: Clinical Global Impression of Change; DSM‐IV: Diagnostic and Statistical Manual of Mental Disorders, fourth edition; DSM‐IV‐TR: Diagnostic and Statistical Manual of Mental Disorders, fourth edition, text revision; ED: erectile dysfunction; HBsAg: hepatitis B surface antigen; IELT: intravaginal ejaculatory latency time; IIEF: International Index of Erectile Function; ITT: intention to treat; NR: not reported; PDE5: phosphodiesterase‐5; PE: premature ejaculation; PEP: Premature Ejaculation Profile; SCL‐90: Symptom Checklist‐90; SD: standard deviation; SSRI: selective serotonin reuptake inhibitor.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Abdel‐Hamid 2001 | Wrong intervention |
| Abdollahian 2006 | Wrong patient population |
| Abu El‐Hamd 2018 | Multivitamin used instead of placebo. |
| Akgul 2008 | No placebo control arm |
| Alghobary 2010 | No placebo control arm |
| Althof 2010b | Duplicate |
| Alza 2006 | Duplicate |
| Arafa 2006 | Wrong outcomes |
| Arafa 2007b | No placebo control arm |
| Boulos 2015 | No placebo control arm |
| Brock 2009 | Wrong study design |
| Catalán 2002 | Wrong study design |
| Chen 2016 | Wrong comparator |
| Crenshaw 1992 | Unable to obtain full text article |
| Culba 2008 | Wrong intervention |
| Dhikav 2007 | Wrong comparator |
| Eltonsi 2017 | Wrong setting |
| Ghaffar 2010 | Unable to obtain full text article |
| Giammusso 1997 | Wrong comparator |
| Giammusso 1997a | No placebo control arm |
| Guo 2016 | Wrong comparator |
| Hosseini 2007 | Wrong intervention |
| Khazaie 2015 | Wrong patient population |
| Khelaia 2012a | Duplicate |
| Kilic 2005 | Wrong intervention |
| Kim 2018a | Wrong intervention |
| Kirecci 2014 | Wrong outcomes |
| Kirecci 2014a | Wrong outcomes |
| Lee 2013 | Wrong intervention |
| Li 2015 | Wrong comparator |
| Li 2015a | Wrong intervention |
| Luigi 2012 | Wrong comparator |
| Manasia 2003 | No placebo control arm |
| Mathers 2009 | No placebo control arm |
| McMahon 2002 | Wrong study design |
| McMahon 2007 | Commentary |
| McMahon 2010a | Duplicate |
| McMahon 2010b | Duplicate |
| McMahon 2016 | Wrong study design |
| Mostafa 2017 | Wrong comparator |
| Murat 1999 | No placebo control arm |
| Nada 2009 | Duplicate |
| Nada 2012 | Only SSRI vs SSRI; protocol stated SSRI vs placebo. |
| Okulu 2013 | Wrong outcomes |
| Otunctemur 2014 | Only SSRI vs SSRI; protocol stated SSRI vs placebo. |
| Ozcan 2015 | No placebo control arm |
| Pastore 2011 | Wrong comparator |
| Pastore 2012 | Wrong comparator |
| Polat 2015 | Wrong comparator |
| Rezakhaniha 2010 | No placebo control arm |
| Rezakhaniha 2014 | Wrong patient population |
| Rivera 2005 | Wrong study design |
| Safarinejad 2008a | Wrong intervention |
| Sahin 2016 | Wrong comparator |
| Sahin 2016a | Wrong comparator |
| Salokangas 2006 | Commentary |
| Sanzovo 2011 | Wrong comparator |
| Schmidt 2001 | Wrong setting |
| Shang 2010 | No placebo control arm |
| Shao 2008 | Wrong comparator |
| Shin 2017 | Wrong study design |
| Sun 2004 | No placebo control arm |
| Sun 2007 | Wrong comparator |
| Sun 2010 | Wrong comparator |
| Sunay 2011 | Wrong comparator |
| Swartz 1994 | Wrong study design |
| Vella 2015 | Wrong comparator |
| Waldinger 1997 | Only SSRI vs SSRI; protocol stated SSRI vs placebo. |
| Waldinger 2000 | Wrong comparator |
| Waldinger 2001 | No placebo control arm |
| Waldinger 2001a | No placebo control arm |
| Waldinger 2001b | Wrong comparator |
| Waldinger 2003 | Wrong comparator |
| Waldinger 2004b | No placebo control arm |
| Waldinger 2006b | Commentary |
| Weixing 2012 | No placebo control arm |
| Xu 2014 | Wrong comparator |
| Yang 2015 | No placebo control arm |
| Yang 2016 | No placebo control arm |
| Yang 2017 | Only SSRI vs SSRI; protocol stated SSRI vs placebo. |
| Yang 2017a | No placebo control arm |
| Yuan 2008 | Wrong comparator |
| Zhang 2005 | Wrong comparator |
| Zhu 2015 | Wrong comparator |
SSRI: selective serotonin reuptake inhibitor.
Characteristics of studies awaiting classification [ordered by study ID]
Kolomazník 2002.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Study details | |
| Publication details | |
| Stated aim of study | |
| Notes | Awaiting translation of full text into English |
Differences between protocol and review
This review is based on a published protocol (Mian 2017) but there are two additional authors to this review: Dr Niranjan J Sathianathen and Dr Eu Chang Hwang.
Contributions of authors
NS: screened studies; performed full‐text review, data extraction and data analysis; and wrote the review.
ECH: screened studies; performed full‐text review, data extraction and data analysis; and revised the review.
RM: drafted the first version of the protocol; screened studies; performed full‐text review, data extraction and data analysis; and revised the review.
JB: provided clinical content expertise, reviewed and revised the protocol/review.
AS: provided clinical content expertise, reviewed and revised the protocol/review.
JL: developed the search strategies; performed and updated the search; and revised the protocol/review.
SS: provided methodologic expertise, reviewed and revised the protocol/review.
PD: provided guidance and oversight; screened studies; performed full‐text review, data extraction and data analysis; and revised the protocol/review.
Sources of support
Internal sources
-
Minneapolis VAMC, USA
Salary support for Philipp Dahm, Ayman Soubra, and Shahnaz Sultan
-
University of Minnesota, USA
Salary support for Niranjan Sathianathen, Joshua Bodie and Ayman Soubra
External sources
-
None, USA
N/A
Declarations of interest
NS: none.
ECH: none.
RM: none.
JB: none.
AS: none.
JL: none.
SS: none.
PD: none.
New
References
References to studies included in this review
Ahn 1996 {published data only}
- Ahn Ty, Park H, Choi Eh, Choo MS, Park T. Fluoxetine as a treatment for premature ejaculation: a double-blind, randomized, placebo-controlled study. Korean Journal of Urology 1996;37(8):926-31. [Google Scholar]
Athanasios 2007 {published data only}
- Athanasios Z, Polyanthi P, George K. The efficacy of duloxetine in the treatment of premature ejaculation. International Urology and Nephrology 2007;39(1):115-8. [DOI] [PubMed] [Google Scholar]
Atmaca 2002 {published data only}
- Atmaca M, Kuloglu M, Tezcan E, Semercioz A. The efficacy of citalopram in the treatment of premature ejaculation: a placebo-controlled study. International Journal of Impotence Research 2002;14(6):502-5. [DOI] [PubMed] [Google Scholar]
Biri 1998 {published data only}
- Biri H, Isen K, Sinik Z, Onaran M, Kupeli B, Bozkirli I. Sertraline in the treatment of premature ejaculation: a double-blind placebo controlled study. International Urology and Nephrology 1998;30(5):611-5. [DOI] [PubMed] [Google Scholar]
Buvat 2009 {published data only}
- Buvat J, Tesfaye F, Rothman M, Rivas DA, Giuliano F. Dapoxetine for the treatment of premature ejaculation: results from a randomized, double-blind, placebo-controlled phase 3 trial in 22 countries. European Urology 2009;55(4):957-67. [DOI] [PubMed] [Google Scholar]
Farnia 2009 {published data only}
- Farnia V, Raisi F, Mohseni MG, Atharikia D, Ghafuri Z. On-demand treatment of premature ejaculation with citalopram: a randomized double-blind study. Acta Medica Iranica 2009;47:353-5. [Google Scholar]
Gameel 2013 {published data only}
- Gameel T, Tawfeek A, Abou Farha M, Bastawesy M, Bendary M, Gamasy A. On-demand use of tramadol, sildenafil, paroxetine and local anaesthetics for the management of premature ejaculation: a randomized placebo-controlled clinical trial. Journal of Sexual Medicine 2018;15(2):S54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gameel TA, Tawfik AM, Abou-Farha MO, Bastawisy MG, El-Bendary MA, El-Gamasy Ael N. On-demand use of tramadol, sildenafil, paroxetine and local anaesthetics for the management of premature ejaculation: a randomised placebo-controlled clinical trial. Arab Journal of Urology 2013;11(4):392-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gameel TA, Tawfik AM, Soliman MG, El-Bendary MA, Abo-Elenen M, Tawfik TI, et al. On demand use of tramadol, sildenafil, paroxetine or local anesthetics for management of premature ejaculation, a randomized placebo controlled clinical trial. European Urology, Supplements 2013;12(1):e214. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gong 2011 {published data only}
- Gong ZY, Tang TL, Cui S, Wang JZ, Deng XZ. Oral paroxetine for premature ejaculation: a randomized controlled study. Zhonghua Nan Ke Xue [National Journal of Andrology] 2011;17(10):923-5. [PubMed] [Google Scholar]
Hamidi Madani 2016 {published data only}
- Hamidi-Madani A, Motiee R, Mokhtari G, Nasseh H, Esmaeili S, Kazemnezhad E. The efficacy and safety of on-demand tramadol and paroxetine use in treatment of life long premature ejaculation: a randomized double-blind placebo-controlled clinical trial. Journal of Reproduction and Infertility 2016;19(1):10-5. [PMC free article] [PubMed] [Google Scholar]
- Hamidi Madani A, Motiee R, Mokhtari G, Nasseh H, Esmaeili S, Kazemnezhad E. The efficiency and safety of tramadol, paroxetine and placebo in treatment of life long premature ejaculation. European Urology, Supplements 2016;15(3):e1001. [Google Scholar]
Kara 1996 {published data only}
- Kara H, Aydin S, Yucel M, Agargun MY, Odabas O, Yilmaz Y. The efficacy of fluoxetine in the treatment of premature ejaculation: a double-blind placebo controlled study. Journal of Urology 1996;156(5):1631-2. [PubMed] [Google Scholar]
Kaufman 2009 {published data only}
- Kaufman JM, Rosen RC, Mudumbi RV, Tesfaye F, Hashmonay R, Rivas D. Treatment benefit of dapoxetine for premature ejaculation: results from a placebo-controlled phase III trial. BJU International 2009;103(5):651-8. [DOI] [PubMed] [Google Scholar]
Khelaia 2012 {published data only}
- Khelaia A, Managadze L. Does still is a place for paroxetine in the era of dapoxetine. Andrology 2014;2:100. [Google Scholar]
- Khelaia A. Does still is a place for paroxetine in the era of dapoxetine. Journal of Sexual Medicine 2015;12:214. [Google Scholar]
- Khelaia AV, Bochorishvili GG, Managadze LG. 697 Assessment of paroxetine in the treatment of premature ejaculation and dosage optimization. European Urology Supplements 2012;11(1):e697-e697a. [Google Scholar]
Kim 1998 {published data only}
- Kim SC, Seo KK. Efficacy and safety of fluoxetine, sertraline and clomipramine in patients with premature ejaculation: a double-blind, placebo controlled study. Journal of Urology 1998;159(2):425-7. [DOI] [PubMed] [Google Scholar]
Mattos 2008 {published data only}
- Mattos RM, Marmo Lucon A, Srougi M. Tadalafil and fluoxetine in premature ejaculation: prospective, randomized, double-blind, placebo-controlled study. Urologia Internationalis 2008;80(2):162-5. [DOI] [PubMed] [Google Scholar]
McMahon 1998 {published data only}
- McMahon CG. Treatment of premature ejaculation with sertraline hydrochloride: a single-blind placebo controlled crossover study. Journal of Urology 1998;159(6):1935-8. [DOI] [PubMed] [Google Scholar]
McMahon 1999 {published data only}
- McMahon CG, Touma K. Treatment of premature ejaculation with paroxetine hydrochloride as needed: 2 single-blind placebo controlled crossover studies. Journal of Urology 1999;161(6):1826-30. [PubMed] [Google Scholar]
McMahon 2010 {published data only}
- Giuliano F, Levine SB, Buvat J, Rosen RC, Kaufman JM, Tesfaye F, et al. Lack of withdrawal syndrome or effects on anxiety with dapoxetine (DPX) for the treatment of premature ejaculation (PE): results from 2 phase III trials. European Urology Supplements 2008;7(3):187. [Google Scholar]
- McMahon C, Kim SW, Park NC, Chang CP, Rivas D, Tesfaye F, et al. Treatment of premature ejaculation in the Asia-Pacific region: results from a phase III double-blind, parallel-group study of dapoxetine. Journal of Sexual Medicine 2010;7(1 Pt 1):256-68. [DOI] [PubMed] [Google Scholar]
- McMahon C, Park NC, Zhao Y, Rivas D, Rothman M. Treatment of premature ejaculation (PE) in the Asia-Pacific region: results from a phase III double-blind, parallel-group study of dapoxetine. International Journal of Urology 2010;17:A195. [DOI] [PubMed] [Google Scholar]
McMahon 2013 {published data only}
- McMahon CG, Giuliano F, Dean J, Hellstrom WJ, Bull S, Tesfaye F, et al. Efficacy and safety of dapoxetine in men with premature ejaculation and concomitant erectile dysfunction treated with a phosphodiesterase type 5 inhibitor: randomized, placebo-controlled, phase III study. Journal of Sexual Medicine 2013;10(9):2312-25. [DOI] [PubMed] [Google Scholar]
Mendels 1995 {published data only}
- Mendels J, Camera A, Sikes C. Sertraline treatment for premature ejaculation. Journal of Clinical Psychopharmacology 1995;15(5):341-6. [DOI] [PubMed] [Google Scholar]
Na 1996 {published data only}
- Na KI, Kim JJ. Sertraline treatment in premature ejaculation: a double blind, randomized, placebo-controlled study. Journal of Korean Andrological Society 1996;14(2):101-4.
Novaretti 2002 {published data only}
- Novaretti JP, Pompeo AC, Arap S. Selective serotonin uptake inhibitor in the treatment of premature ejaculation. Brazilian Journal of Urology 2002;28:116-22. [Google Scholar]
Pryor 2006 {published data only}
- Pryor JL, Althof SE, Steidle C, Miloslavsky M, Kell S. Efficacy and tolerability of dapoxetine in the treatment of premature ejaculation. Journal of Urology 2005;173(4):S201. [DOI] [PubMed] [Google Scholar]
- Pryor JL, Althof SE, Steidle C, Rosen RC, Hellstrom WJ, Shabsigh R, et al. Efficacy and tolerability of dapoxetine in treatment of premature ejaculation: an integrated analysis of two double-blind, randomised controlled trials. Lancet 2006;368(9539):929-37. [DOI] [PubMed] [Google Scholar]
Safarinejad 2006b {published data only}
- Safarinejad MR. Comparison of dapoxetine versus paroxetine in patients with premature ejaculation: a double-blind, placebo-controlled, fixed-dose, randomized study. Clinical Neuropharmacology 2006;29(5):243-52. [DOI] [PubMed] [Google Scholar]
Safarinejad 2006c {published data only}
- Safarinejad MR, Hosseini SY. Safety and efficacy of citalopram in the treatment of premature ejaculation: a double-blind placebo-controlled, fixed dose, randomized study. International Journal of Impotence Research 2006;18(2):164-9. [DOI] [PubMed] [Google Scholar]
Safarinejad 2007 {published data only}
- Safarinejad MR. Safety and efficacy of escitalopram in the treatment of premature ejaculation: a double-blind, placebo-controlled, fixed-dose, randomized study. Journal of Clinical Psychopharmacology 2007;27(5):444-50. [DOI] [PubMed] [Google Scholar]
Safarinejad 2008 {published data only}
- Safarinejad MR. Safety and efficacy of dapoxetine in the treatment of premature ejaculation: a double-blind, placebo-controlled, fixed-dose, randomized study. Neuropsychopharmacology 2008;33(6):1259-65. [DOI] [PubMed] [Google Scholar]
Shang 2012 {published data only}
- Shang XJ, Geng Q, Zhang K, Xia XY, Shao Y, Huang YF. Efficacy of citalopram on premature ejaculation: a clinical observation. Zhonghua Nan Ke Xue [National Journal of Andrology] 2012;18(12):1097-100. [PubMed] [Google Scholar]
Tuncel 2008 {published data only}
- Tuncel A, Aslan Y, Başar MM, Atan A. Efficacy of clomipramine, sertraline and terazosin treatments in premature ejaculation. Turkish Journal of Medical Sciences 2008;38(1):59-64. [Google Scholar]
Waldinger 1994 {published data only}
- Waldinger MD, Hengeveld MW, Zwinderman AH. Paroxetine treatment of premature ejaculation: a double-blind, randomized, placebo-controlled study. American Journal of Psychiatry 1994;151(9):1377-9. [DOI] [PubMed] [Google Scholar]
Waldinger 1998 {published data only}
- Waldinger MD, Hengeveld MW, Zwinderman AH, Olivier B. Effect of SSRI antidepressants on ejaculation: a double-blind, randomized, placebo-controlled study with fluoxetine, fluvoxamine, paroxetine, and sertraline. Journal of Clinical Psychopharmacology 1998;18(4):274-81. [DOI] [PubMed] [Google Scholar]
Yilmaz 1999 {published data only}
- Yilmaz U, Tatlisen A, Turan H, Arman F, Ekmekcioglu O. The effects of fluoxetine on several neurophysiological variables in patients with premature ejaculation. Journal of Urology 1999;161(1):107-11. [PubMed] [Google Scholar]
References to studies excluded from this review
Abdel‐Hamid 2001 {published data only}
- Abdel-Hamid I A, El Naggar E A, El Gilany A H. Assessment of as needed use of pharmacotherapy and the pause-squeeze technique in premature ejaculation. International journal of impotence research 2001;13(1):41-5. [DOI] [PubMed] [Google Scholar]
Abdollahian 2006 {published data only}
- Abdollahian E, Javanbakht A, Javidi K, Samari A A, Shakiba M, Sargolzaee M R. Study of the efficacy of fluoxetine and clomipramine in the treatment of premature ejaculation after opioid detoxification. The American journal on addictions 2006;15(1):100-4. [DOI] [PubMed] [Google Scholar]
Abu El‐Hamd 2018 {published data only}
- Abu El-Hamd M, Abdelhamed A. Comparison of the clinical efficacy and safety of the on-demand use of paroxetine, dapoxetine, sildenafil and combined dapoxetine with sildenafil in treatment of patients with premature ejaculation: a randomised placebo-controlled clinical trial. Andrologia 2018;50(1):e12829. [DOI] [PubMed] [Google Scholar]
Akgul 2008 {published data only}
- Akgul T, Karakan T, Ayyildiz A, Germiyanoglu C. Comparison of sertraline and citalopram for treatment of premature ejaculation. Urol J 2008;5(1):41-5. [PubMed] [Google Scholar]
Alghobary 2010 {published data only}
- Alghobary M, El-Bayoumy Y, Mostafa Y, Mahmoud el H M, Amr M. Evaluation of tramadol on demand vs. daily paroxetine as a long-term treatment of lifelong premature ejaculation. The journal of sexual medicine 2010;7(8):2860-7. [DOI] [PubMed] [Google Scholar]
Althof 2010b {published data only}
- Althof S E, Brock G B, Rosen R C, Rowland D L, Aquilina J W, Rothman M, Tesfaye F, Bull S. Validity of the patient-reported Clinical Global Impression of Change as a measure of treatment response in men with premature ejaculation. The journal of sexual medicine 2010;7(6):2243-52. [DOI] [PubMed] [Google Scholar]
Alza 2006 {published data only}
- Alza Corporation. A placebo-controlled, double-blind, randomized, parallel study of the efficacy and safety of dapoxetine HCl in the treatment of rapid ejaculation. Clinicaltrials.gov 2006.
Arafa 2006 {published data only}
- Arafa M, Shamloul R. Efficacy of sertraline hydrochloride in treatment of premature ejaculation: a placebo-controlled study using a validated questionnaire. Int J Impot Res 2006;18(6):534-8. [DOI] [PubMed] [Google Scholar]
Arafa 2007b {published data only}
- Arafa M, Shamloul R. A randomized study examining the effect of 3 SSRI on premature ejaculation using a validated questionnaire. Ther Clin Risk Manag 2007;3(4):527-31. [PMC free article] [PubMed] [Google Scholar]
Boulos 2015 {published data only}
- Boulos V, Hassanin A, Roaiah M F. Is on demand use of tramadol more effective than selective serotonin reuptake inhibitors and/or sildenafil and/or topical penile anesthetics in treating premature ejaculation (PE)? European Urology Supplements 2015;14(2):e242. [Google Scholar]
Brock 2009 {published data only}
- Brock G B, Althof S E, Rosen R C, Bull S, Tesfaye F, Rothman M, Aquilina J W. Treatment outcomes in men with premature ejaculation treated with dapoxetine by their baseline intravaginal ejaculatory latency time. Journal of Urology 2009;181(4):529. [Google Scholar]
Catalán 2002 {published data only}
- Catalán J. Paroxetine and sertraline delayed ejaculation in heterosexual men with lifelong rapid ejaculation. Evidence Based Mental Health 2002;5(1):25. [DOI] [PubMed] [Google Scholar]
Chen 2016 {published data only}
- Chen X Y, Qu Y W, Wang S G. Efficacy and safety of dapoxetine in the treatment of premature ejaculation. National journal of andrology 2016;22(5):411-4. [PubMed] [Google Scholar]
Crenshaw 1992 {published data only}
- Crenshaw R. Treatment of premature ejaculation with fluoxetine. In: American Psychiatric Association Meeting. 1992.
Culba 2008 {published data only}
- Culba M. Comparison of fluoxetine vs. fluoxetine plus tadalafil in the treatment of premature ejaculation – a double blind, placebo control study. J Sex Med 2008;5:60-1. [Google Scholar]
Dhikav 2007 {published data only}
Eltonsi 2017 {published data only}
- Eltonsi TK, Tawfik TM, Rashed LA, GamalEl Din SF, Mahmoud MA. Study of the link between dopamine transporter gene polymorphisms and response to paroxetin and escitalopram in patients with lifelong premature ejaculation.. Int J Impot Res 2017;29:235–239. [DOI] [PubMed] [Google Scholar]
Ghaffar 2010 {published data only}
- Ghaffar A, Tariq Q A, Ahmed R. Efficacy of paroxitine for the management of premature ejaculation. Medical Forum Monthly 2010;21(3):21-26. [Google Scholar]
Giammusso 1997 {published data only}
- Giammusso B, Morgia G, Spampinato A, Motta M. Paroxetine in the treatment of premature ejaculation. Arch Ital Urol Androl 1997;69(1):11-3. [PubMed] [Google Scholar]
Giammusso 1997a {published data only}
- Giammusso B, Morgia G, Spampinato A, Motta M. Paroxetine as a treatment for premature ejaculation. Arch Ital Urol Androl 1997;69(1):11-13. [PubMed] [Google Scholar]
Guo 2016 {published data only}
- Guo J, Gao Q H, Wang F, Yu G J, Zhang J W, Zeng Y, Geng Q, Guo B D, Han Q. Efficacy and safety of Qiaoshao Formula () on patients with lifelong premature ejaculation of Gan (Liver) depression and Shen (Kidney) deficiency syndrome: A randomized controlled trial. Chinese journal of integrative medicine 2016;22(12):889-893. [DOI] [PubMed] [Google Scholar]
Hosseini 2007 {published data only}
- Hosseini M M, Yarmohammadi H. Effect of fluoxetine alone and in combination with sildenafil in patients with premature ejaculation. Urol Int 2007;79(1):28-32. [DOI] [PubMed] [Google Scholar]
Khazaie 2015 {published data only}
Khelaia 2012a {published data only}
- Khelaia A V, Bochorishvili G G, Managadze L G. Assessment of paroxetine in the treatment of premature ejaculation and dosage optimization. European Urology Supplements 2012;11(1):e697-e697a. [Google Scholar]
Kilic 2005 {published data only}
- Kilic S, Ergin H, Baydinc Y C. Venlafaxine extended release for the treatment of patients with premature ejaculation: a pilot, single-blind, placebo-controlled, fixed-dose crossover study on short-term administration of an antidepressant drug. International journal of andrology 2005;28(1):47-52. [DOI] [PubMed] [Google Scholar]
Kim 2018a {published data only}
- Kim S W, Choi J B, Kim S J, Kim K S, Kim C M, Lee D H, Choi W S. Tolerability and adequate therapeutic dosage of oral clomipramine for the treatment of premature ejaculation: A randomized, double-blind, placebo-controlled, fixed-dose, parallel-grouped clinical study. International journal of impotence research 2018;30(2):65-70. [DOI] [PubMed] [Google Scholar]
Kirecci 2014 {published data only}
- Kirecci S L, Simsek A, Gurbuz Z G, Mimaroglu S, Yuksel A, Vural P, Degirmencioglu S. Relationship between plasma melatonin levels and the efficacy of selective serotonin reuptake inhibitors treatment on premature ejaculation. International journal of urology 2014;21(9):917-20. [DOI] [PubMed] [Google Scholar]
Kirecci 2014a {published data only}
- Kirecci S L, Simsek A, Yuksel A, Gurdal H, Gurbuz Z G, Usanmaz S. Relevance of seminal plasma nitric oxide levels and the efficacy of SSRI treatment on lifelong premature ejaculation. Andrologia 2014;46(10):1169-75. [DOI] [PubMed] [Google Scholar]
Lee 2013 {published data only}
- Lee W K, Lee S H, Cho S T, Lee Y S, Oh C Y, Yoo C, Cho J S, Lee S K, Yang D Y. Comparison between on-demand dosing of dapoxetine alone and dapoxetine plus mirodenafil in patients with lifelong premature ejaculation: prospective, randomized, double-blind, placebo-controlled, multicenter study. J Sex Med 2013;10(11):2832-41. [DOI] [PubMed] [Google Scholar]
Li 2015 {published data only}
- Li J X, Lu Q G. Efficacy of Qilin Pills combined with sertraline in the treatment of secondary non-consolidated kidney qi premature ejaculation. National journal of andrology 2015;21(5):443-6. [PubMed] [Google Scholar]
Li 2015a {published data only}
- Li T, Tan Y, Xie Z P, Wang W R, Wang S H, Ouyang H, Kang Z P, Xie S. Clinical efficacy of Paroxetine combined with mid-frequency electrical pulse acupoint stimulation for premature ejaculation. National journal of andrology 2015;21(10):921-4. [PubMed] [Google Scholar]
Luigi 2012 {published data only}
- Luigi P A, Giovanni P, Luigi S, Antonino L, Domenico A, Andrea R, Antonio C. A prospective randomized study to compare pelvic floor muscle rehabilitation and dapoxetine for treatment of lifelong premature ejaculation. Neurourology and Urodynamics 2012;31:S36-S37. [Google Scholar]
Manasia 2003 {published data only}
- Manasia P, Pomerol J, Ribe N, Gutierrez del Pozo R, Alcover Garcia J. Comparison of the efficacy and safety of 90 mg versus 20 mg fluoxetine in the treatment of premature ejaculation. The Journal of Urology 2003;170(1):164-5. [DOI] [PubMed] [Google Scholar]
Mathers 2009 {published data only}
- Mathers M J, Klotz T, Roth S, Lummen G, Sommer F. Safety and efficacy of vardenafil versus sertraline in the treatment of premature ejaculation: a randomised, prospective and crossover study. Andrologia 2009;41(3):169-75. [DOI] [PubMed] [Google Scholar]
McMahon 2002 {published data only}
- McMahon CG. Long term results of treatment of premature ejaculation with selective serotonin re-uptake inhibitors. Int J Impot Res 2002;14:3. [Google Scholar]
McMahon 2007 {published data only}
- McMahon C. Dapoxetine in the treatment of premature ejaculation. Clinical Neuropharmacology 2007;30(5):314-315. [DOI] [PubMed] [Google Scholar]
McMahon 2010a {published data only}
- McMahon C G, Kim S W, Park N C, Chang C P, Rivas D, Tesfaye F, Rothman M, Aquilina J W. Improvements in intravaginal ejaculatory latency time (IELT) and patient-reported outcomes (PROS) in dapoxetine-treated men from the Asia-Pacific region with lifelong or acquired premature ejaculation (PE). Journal of Sexual Medicine 2010;7:177. [Google Scholar]
McMahon 2010b {published data only}
- McMahon C G, Kim S W, Park N C, Chang C P, Rivas D, Tesfaye F, Rothman M, Aquilina J W. Comparison of baseline characteristics of men with lifelong and acquired premature ejaculation (PE) in the Asia-Pacific region. Journal of Sexual Medicine 2010;7:176. [DOI] [PubMed] [Google Scholar]
McMahon 2016 {published data only}
- McMahon C, Lee S W, Kim S W, Moon du G, Kongkanand A, Tantiwongse K. The Asia-Pacific Flexible Dose Study of Dapoxetine and Patient Satisfaction in Premature Ejaculation Therapy: The PASSION Study. Sexual Medicine 2016;4(1):e18-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mostafa 2017 {published data only}
- Mostafa R, Hassan M, NasrAlla Y, Mohammed R, Naguib N. A comparative study between two different doses of dapoxetine and a single dose of paroxetine on demand in the treatment of cases of premature ejaculation. Journal of Sexual Medicine 2017;14(1):S129. [Google Scholar]
Murat 1999 {published data only}
- Murat Basar M, Atan A, Yildiz M, Baykam M, Aydoganli L. Comparison of sertraline to fluoxetine with regard to their efficacy and side effects in the treatment of premature ejaculation. Archivos espanoles de urologia 1999;52(9):1008-11. [PubMed] [Google Scholar]
Nada 2009 {published data only}
- Nada E. The use of escitalopram in treatment of patients with premature ejaculation: A randomized, double-blind, placebo-controlled study. J Sex Med 2009;6(S2):182. [Google Scholar]
Nada 2012 {published data only}
- Nada E, Saleh R, Ali M, Azab H. A comparison between citalopram and escitalopram in treatment of patients with premature ejaculation: a double-blind controlled clinical study. Journal of Sexual Medicine 2012;9:261-2.
Okulu 2013 {published data only}
- Okulu E, Ener K, Aldemir M, Aǧras K, Fuat Özcan M, Kayigil O. Comparison of efficacy of sertralin on patients with premature ejaculation by penile biothesiometry. Journal of Clinical and Analytical Medicine 2013;4(4):302-306. [Google Scholar]
Otunctemur 2014 {published data only}
- Otunctemur A, Ozbek E, Kirecci SL, Ozcan L, Dursun M, Cekmen M, et al. Relevance of serum nitric oxide levels and the efficacy of selective serotonin reuptake inhibitors treatment on premature ejaculation: decreased nitric oxide is associated with premature ejaculation. Andrologia 2014;46(9):951-5. [DOI] [PubMed] [Google Scholar]
Ozcan 2015 {published data only}
- Ozcan L, Polat E C, Otunctemur A, Ozbek E. Duloxetine, dual serotonin and norepinephrine reuptake inhibitor, versus paroxetine, selective serotonin reuptake inhibitor, in the treatment for premature ejaculation. International urology and nephrology 2015;47(2):283-7. [DOI] [PubMed] [Google Scholar]
Pastore 2011 {published data only}
- Pastore Al, Palleschi G, Silvestri L, Ripoli A, Autieri D, Leto A, Carbone A. Premature ejaculation: A prospective randomized study to compare pelvic floor rehabilitation and dapoxetine, a novel selective serotonin reuptake inhibitor. Journal of sexual medicine 2011;8:374. [Google Scholar]
Pastore 2012 {published data only}
- Pastore Al, Palleschi G, Leto A, Iori F, Leonardo C, Petrozza V, Pacini L, Carbone A. Premature ejaculation: A prospective randomized study to compare pelvic floor rehabilitation and dapoxetine, a novel selective serotonin reuptake inhibitor. European Urology Supplements 2012;11(1):e696-e696a. [DOI] [PubMed]
Polat 2015 {published data only}
- Polat E C, Ozbek E, Otunctemur A, Ozcan L, Simsek A. Combination therapy with selective serotonin reuptake inhibitors and phosphodiesterase-5 inhibitors in the treatment of premature ejaculation. Andrologia 2015;47(5):487-92. [DOI] [PubMed] [Google Scholar]
Rezakhaniha 2010 {published data only}
- Rezakhaniha B, Sirosbakht S. Efficacy of selective serotonin reuptake inhibitor (SSRI) in patient with premature ejaculation. Iranian Journal of Reproductive Medicine 2010;8(2):55-59. [Google Scholar]
Rezakhaniha 2014 {published data only}
- Rezakhaniha B, Siroosbakhat S. Comparative study of therapeutic effects of two medicinal procedures of citalopram in premature ejaculation. Biosciences Biotechnology Research Asia 2014;11(2):953-958. [Google Scholar]
Rivera 2005 {published data only}
- Rivera P, Gonzalez R, Gonzalez F, Storme O. Use of paroxetine on-demand in premature ejaculation. Actas urologicas espanolas 2005;29(4):387-91. [DOI] [PubMed] [Google Scholar]
Safarinejad 2008a {published data only}
- Safarinejad MR. Safety and efficacy of venlafaxine in the treatment of premature ejaculation: a double-blind, placebo-controlled, fixed-dose, randomised study. Andrologia 2008;40(1):49-55. [DOI] [PubMed] [Google Scholar]
Sahin 2016 {published data only}
- Sahin S, Bicer M, Seker K G, Yenice M G, Tugcu V. A placebo controlled prospective randomized study to compare acupuncture and dapoxetine for treatment of lifelong premature ejaculation. European Urology Supplements 2016;15(3):e1003. [DOI] [PubMed] [Google Scholar]
Sahin 2016a {published data only}
- Sahin S, Bicer M, Yenice M G, Seker K G, Yavuzsan A H, Tugcu V. A Prospective Randomized Controlled Study to Compare Acupuncture and Dapoxetine for the Treatment of Premature Ejaculation. Urologia internationalis 2016;97(1):104-11. [DOI] [PubMed] [Google Scholar]
Salokangas 2006 {published data only}
- Salokangas RKR, Pryor JL. Lancet. Vol. 368. Philadelphia, Pennsylvania: Lancet, 2006. [Google Scholar]
Sanzovo 2011 {published data only}
- Sanzovo S, Prior M, Bianchin G L, Rosso C, Furlan P M. Premature ejaculation therapies: Randomized controlled experimental study escitalopram vs. cognitive behavioural therapy. Gazzetta Medica Italiana Archivio per le Scienze Mediche 2011;170(2):129-134. [Google Scholar]
Schmidt 2001 {published data only}
- Schmidt M E, Gonzales J, Michelson D. Sexual functioning during acute and continuation therapy with fluoxetine: A prospective assessment. Psychosomatics 2001;42(2):196. [Google Scholar]
Shang 2010 {published data only}
- Shang X, Xia X, Shao Y, Huang Y. Clinical observation of citalopram on the treatment of premature ejaculation. Journal of Sexual Medicine 2010;7:448. [Google Scholar]
Shao 2008 {published data only}
- Shao X, Li J. Clinical study on treatment of premature ejaculation with Paroxetine and behavior-therapy. Chinese Journal of Andrology 2008;22(1):18-20. [Google Scholar]
Shin 2017 {published data only}
- Shin D, Lee S, Yi S, Yoon S H, Cho J Y, Bahng M Y, Jang I J, Yu K S. Pharmacokinetics and tolerability of DA-8031, a novel selective serotonin reuptake inhibitor for premature ejaculation in healthy male subjects. Drug Des Devel Ther 2017;11:713-723. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sun 2004 {published data only}
- Sun C, Liu J, Wang S Yang W, Ye Z. Effects of fluoxetine, paroxetine and clomipramine on premature ejaculation: a clinical trial. Journal of clinical urology 2004;19(2):91-92.
Sun 2007 {published data only}
- Sun X Z, Deng C H, Dai Y P. A clinical study of sertraline and vardenafil in the treatment of premature ejaculation complicated by erectile dysfunction. National journal of andrology 2007;13(7):610-2. [PubMed] [Google Scholar]
Sun 2010 {published data only}
- Sun Z, Wang Y, Chen L, Jin F. Clinical study on treatment of premature ejaculation with fluoxetine hydrochloride and tamsulosion. Chinese journal of andrology 2010;24(5):43-45.
Sunay 2011 {published data only}
- Sunay D, Sunay M, Aydogmus Y, Bagbanci S, Arslan H, Karabulut A, Emir L. Acupuncture versus paroxetine for the treatment of premature ejaculation: a randomized, placebo-controlled clinical trial. European Urology 2011;59(5):765-71. [DOI] [PubMed] [Google Scholar]
Swartz 1994 {published data only}
- Swartz D A. Sertraline hydrochloride for premature ejaculation. J Urol 1994;151:Suppl. [Google Scholar]
Vella 2015 {published data only}
- Vella M, Scalici Gesolfo C, Scaduto G, Gambino G, Abbadessa D, Falgares G, Pavone C. Premature ejaculation: Comparison of treatment. Pharmacotherapy vs pharmacotherapy in association with group psychotherapy vs group psychotherapy. European Urology Supplements 2015;14(2):e246. [Google Scholar]
Waldinger 1997 {published data only}
- Waldinger MD, Hengeveld MW, Zwinderman AH. Ejaculation-retarding properties of paroxetine in patients with primary premature ejaculation: a double-blind, randomized, dose-response study. British Journal of Urology 1997;79(4):592-5. [DOI] [PubMed] [Google Scholar]
Waldinger 2000 {published data only}
- Waldinger M D, Olivier B. Selective serotonin reuptake inhibitors (SSRIs) and sexual side effects: Differences in delaying ejaculation. Advances in Preclinical and Clinical Psychiatry, 2000;1:117-130. [Google Scholar]
Waldinger 2001 {published data only}
- Waldinger M D, Zwinderman A H, Olivier B. Antidepressants and ejaculation: a double-blind, randomized, placebo-controlled, fixed-dose study with paroxetine, sertraline, and nefazodone. J Clin Psychopharmacol 2001;21(3):293-7. [DOI] [PubMed] [Google Scholar]
Waldinger 2001a {published data only}
Waldinger 2001b {published data only}
- Waldinger M D, Zwinderman A H, Olivier B. Antidepressants and ejaculation: A double-blind, randomised, fixed-dose study with mirtazapine and paroxetine. New Research Program of 2001 Annual Meeting of American Psychiatric Association 2001;1(715):52. [Google Scholar]
Waldinger 2003 {published data only}
- Waldinger M D, Zwinderman A H, Olivier B. Antidepressants and ejaculation: a double-blind, randomized, fixed-dose study with mirtazapine and paroxetine. J Clin Psychopharmacol 2003;23(5):467-70. [DOI] [PubMed] [Google Scholar]
Waldinger 2004b {published data only}
- Waldinger M D, Zwinderman A H, Olivier B. On-demand treatment of premature ejaculation with clomipramine and paroxetine: a randomized, double-blind fixed-dose study with stopwatch assessment. Eur Urol 2004;46(4):510-5. [DOI] [PubMed] [Google Scholar]
Waldinger 2006b {published data only}
- Waldinger MD, Schweitzer DH, Olivier B, Pryor JL. Dapoxetine treatment of premature ejaculation...Pryor JL, Althof SE, Steidle C et al. Efficacy and tolerability of dapoxetine in treatment of premature ejaculation: an integrated analysis of two double-blind, randomised controlled trials. Lancet 2006;368:927-37. Lancet 2006;368(9550):1869-1870. [DOI] [PubMed] [Google Scholar]
Weixing 2012 {published data only}
- Weixing Z, Junchang Q, Rui W, Lei W, Jie Z. Effect evaluation of Paroxetine and Sertraline in the treatment of premature ejaculation. Chinese Journal of Andrology 2012;26(1):41-43. [Google Scholar]
Xu 2014 {published data only}
- Xu G, Jiang H W, Fang J, Wen H, Gu B, Liu J, Zhang L M, Ding Q, Zhang Y F. An improved dosage regimen of sertraline hydrochloride in the treatment for premature ejaculation: an 8-week, single-blind, randomized controlled study followed by a 4-week, open-label extension study. Journal of clinical pharmacy and therapeutics 2014;39(1):84-90. [DOI] [PubMed] [Google Scholar]
Yang 2015 {published data only}
- Yang L, Luo L, Chen X F, Fan J H, Liu R M, Wang X N, Nan X Y, Zhang Y, Lin X F, Wang M Z, Xing J P, Yang Z S, Jian B L, He H, Wu D P, He D L. Efficacy and tolerability of dapoxetine in the treatment of premature ejaculation. Journal of Sexual Medicine 2015;21(10):892-5. [PubMed] [Google Scholar]
Yang 2016 {published data only}
- Yang L, Chen X, He D. Efficacy and tolerability of dapoxetine and sertraline for the treatment of chinese patients with premature ejaculation. Journal of Sexual Medicine 2016;13(5):S79.
Yang 2017 {published data only}
- Yang L, Chen XF, He DL. Efficacy and tolerability of dapoxetine and sertraline for the treatment of Chinese patients with premature ejaculation. Journal of Sexual Medicine 2017;14(1):S17. [Google Scholar]
Yang 2017a {published data only}
- Yang L, Chen X F, He D L. Efficacy and tolerability of dapoxetine and sertraline for the treatment of Chinese patients with premature ejaculation. Journal of Sexual Medicine 2017;14(1):S17. [Google Scholar]
Yuan 2008 {published data only}
- Yuan P, Dai J, Yang Y, Guo J, Liang R. A comparative study on treatment for premature ejaculation: citalopram used in combination with behavioral therapy versus either Citalopram or behavioral therapy alone. Chinese journal of andrology 2008;22(5):35-38.
Zhang 2005 {published data only}
- Zhang X S, Wang Y X, Huang X Y, Leng J, Li Z, Han Y F. [Comparison between sildenafil plus sertraline and sertraline alone in the treatment of premature ejaculation]. Zhonghua Nan Ke Xue 2005;11(7):520-2. [PubMed] [Google Scholar]
Zhu 2015 {published data only}
- Zhu Y, Yue J, Liu Z J, Huang J, Bian T S, Wang J S, Zeng Q Q. [Sertraline hydrochloride combined with four-spot caressing for primary premature ejaculation]. National journal of andrology 2015;21(12):1116-20. [PubMed] [Google Scholar]
References to studies awaiting assessment
Kolomazník 2002 {published data only}
- Kolomazník M, Červinka L, Kutílek Š, Pohanka M, Skibová J, Tauš L, et al. Fluoxetine in the treatment of ejaculatio praecox. Psychiatrie 2002;6(1):6-9. [Google Scholar]
Additional references
Althof 2010
- Althof SE, Brock GB, Rosen RC, Rowland DL, Aquilina JW, Rothman M, et al. Validity of the patient-reported Clinical Global Impression of Change as a measure of treatment response in men with premature ejaculation. Journal of Sexual Medicine 2010;7(6):2243-52. [DOI] [PubMed] [Google Scholar]
Althof 2014
- Althof SE, McMahon CG, Waldinger MD, Serefoglu EC, Shindel AW, Adaikan PG, et al. An update of the International Society of Sexual Medicine's guidelines for the diagnosis and treatment of premature ejaculation (PE). Journal of Sexual Medicine 2014;11(6):1392-422. [DOI: 10.1111/jsm.12504] [DOI] [PubMed] [Google Scholar]
Anderson 2005
- Anderson GM, Barr CS, Lindell S, Durham AC, Shifrovich I, Higley JD. Time course of the effects of the serotonin-selective reuptake inhibitor sertraline on central and peripheral serotonin neurochemistry in the Rhesus monkey. Psychopharmacology 2005;178(2-3):339-46. [DOI] [PubMed] [Google Scholar]
Arafa 2007
- Arafa M, Shamloul R. Development and evaluation of the Arabic Index of Premature Ejaculation (AIPE). Journal of Sexual Medicine 2007;4(6):1750-6. [DOI] [PubMed] [Google Scholar]
Buvat 2011
- Buvat J. Pathophysiology of premature ejaculation. Journal of Sexual Medicine 2011;8 Suppl 4:316-27. [DOI] [PubMed] [Google Scholar]
Cascade 2009
- Cascade E, Kalali AH, Kennedy SH. Real-world data on SSRI antidepressant side effects. Psychiatry 2009;6(2):16-8. [PMC free article] [PubMed] [Google Scholar]
Castiglione 2016
- Castiglione F, Albersen M, Hedlund P, Gratzke C, Salonia A, Giuliano F. Current pharmacological management of premature ejaculation: a systematic review and meta-analysis. European Urology 2016;69(5):904-16. [DOI] [PubMed] [Google Scholar]
Cavallini 1995
- Cavallini G. Alpha-1 blockade pharmacotherapy in primitive psychogenic premature ejaculation resistant to psychotherapy. European Urology 1995;28(2):126-30. [DOI] [PubMed] [Google Scholar]
Choi 2019
- Choi JB, Kang SH, Lee DH, Kim YS, Jeon JS, Choi WS, et al. Efficacy and safety of on demand clomipramine for the treatment of premature ejaculation: a multicenter, randomized, double-blind, phase III clinical trial. Journal of Urology 2019;201(1):147-52. [DOI] [PubMed] [Google Scholar]
Cooper 2015
- Cooper K, Martyn-St James M, Kaltenthaler E, Dickinson K, Cantrell A. Interventions to treat premature ejaculation: a systematic review short report. Health Technology Assessment 2015;19(21):1-180, v-vi. [DOI] [PMC free article] [PubMed] [Google Scholar]
Corbett 2014
- Corbett MS, Higgins JP, Woolacott NF. Assessing baseline imbalance in randomised trials: implications for the Cochrane risk of bias tool. Research Synthesis Methods 2014;5:79-85. [DOI] [PubMed] [Google Scholar]
Elbourne 2002
- Elbourne DR, Altman DG, Higgins JP, Curtin F, Worthington HV, Vail A. Meta-analyses involving cross-over trials: methodological issues. International Journal of Epidemiology 2002;31(1):140-9. [DOI] [PubMed] [Google Scholar]
El‐Hamd 2018
- El-Hamd MA. Efficacy and safety of daily use of tadalafil in treatment of patients with premature ejaculation: a randomised placebo-controlled clinical trial. Andrologia 2018;50(5):e13005. [DOI] [PubMed] [Google Scholar]
Feys 2014
- Feys F, Devroey D. Dapoxetine for Premature Ejaculation: a Harmful Placebo? [PhD thesis]. Brussels: Brussels University Press, 2014. [DOI: 10.13140/2.1.3428.4169] [Google Scholar]
Fuller 1994
- Fuller RW. Uptake inhibitors increase extracellular serotonin concentration measured by brain microdialysis. Life Sciences 1994;55(3):163-7. [DOI] [PubMed] [Google Scholar]
Giuliano 2006
- Giuliano F, Clement P. Serotonin and premature ejaculation: from physiology to patient management. European Urology 2006;50(3):454-66. [DOI] [PubMed] [Google Scholar]
GRADEpro GDT 2015 [Computer program]
- McMaster University (developed by Evidence Prime) GRADEpro GDT. Version (accessed 5 July 2017). Hamilton (ON): McMaster University (developed by Evidence Prime), 2015. Available at gradepro.org.
Hatzimouratidis 2010
- Hatzimouratidis K, Amar E, Eardley I, Giuliano F, Hatzichristou D, Montorsi F, et al. Guidelines on male sexual dysfunction: erectile dysfunction and premature ejaculation. European Urology 2010;57(5):804-14. [DOI] [PubMed] [Google Scholar]
Higgins 2002
- Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Statistics in Medicine 2002;21:1539-58. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analysis. BMJ 2003;327(7414):557-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2009
- Higgins JP, Thompson SG, Spiegelhalter DJ. A re-evaluation of random-effects meta-analysis. Journal of the Royal Statistical Society. Series A, (Statistics in Society) 2009;172(1):137-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011a
- Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available at handbook.cochrane.org.
Higgins 2011b
- Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hozo 2005
- Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Medical Research Methodology 2005;5:13. [DOI: 10.1186/1471-2288-5-13] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hróbjartsson 2013
- Hróbjartsson A, Thomsen AS, Emanuelsson F, Tendal B, Hilden J, Boutron I, et al. Observer bias in randomized clinical trials with measurement scale outcomes: a systematic review of trials with both blinded and nonblinded assessors. Canadian Medical Association Journal 2013;185(4):E201-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Iqbal 2012
- Iqbal MM, Basil MJ, Kaplan J, Iqbal MT. Overview of serotonin syndrome. Annals of Clinical Psychiatry 2012;24(4):310-18. [PubMed] [Google Scholar]
Jian 2018
- Jian Z, Wei X, Ye D, Li H, Wang K. Pharmacotherapy of premature ejaculation: a systematic review and network meta-analysis. International Urology and Nephrology 2018;50(11):1939-48. [DOI] [PubMed] [Google Scholar]
Kempeneers 2013
- Kempeneers P, Andrianne R, Bauwens S, Georis I, Pairoux JF, Blairy S. Functional and psychological characteristics of Belgian men with premature ejaculation and their partners. Archives of Sexual Behavior 2013;42(1):51-66. [DOI] [PubMed] [Google Scholar]
Khan 2003
- Khan A, Khan S, Kolts R, Brown WA. Suicide rates in clinical trials of SSRIs, other antidepressants, and placebo: analysis of FDA reports. American Journal of Psychiatry 2003;160(4):790-2. [DOI] [PubMed] [Google Scholar]
Kim 2018
- Kim SW, Choi JB, Kim SJ, Kim KS, Kim CM, Lee DH. Tolerability and adequate therapeutic dosage of oral clomipramine for the treatment of premature ejaculation: a randomized, double-blind, placebo-controlled, fixed-dose, parallel-grouped clinical study. International Journal of Impotence Research 2018;30(2):65-70. [DOI] [PubMed] [Google Scholar]
Kirby 2015
- Kirby EW, Carson CC, Coward RM. Tramadol for the management of premature ejaculation: a timely systematic review. International Journal of Impotence Research 2015;27(4):121-7. [DOI] [PubMed] [Google Scholar]
Laumann 1999
- Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: prevalence and predictors. JAMA 1999;281(6):537-44. [DOI] [PubMed] [Google Scholar]
Liberati 2009
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Medicine 2009;6(7):1-28. [DOI: 10.1371/journal.pmed.1000100] [DOI] [PMC free article] [PubMed] [Google Scholar]
Martyn‐St James 2015
- Martyn-St James M, Cooper K, Kaltenthaler E, Dickinson K, Cantrell A, Wylie K, et al. Tramadol for premature ejaculation: a systematic review and meta-analysis. BMC Urology 2015;15:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Martyn‐St James 2016
- Martyn-St James M, Cooper K, Ren K, Kaltenthaler E, Dickinson K, Cantrell A, et al. Topical anaesthetics for premature ejaculation: a systematic review and meta-analysis. Sexual Health 2016;13(1):114-23. [DOI] [PubMed] [Google Scholar]
Martyn‐St James 2017
- Martyn-St James M, Cooper K, Ren S, Kaltenthaler E, Dickinson, Cantrell A. Phosphodiesterase type 5 inhibitors for premature ejaculation: a systematic review and meta-analysis. European Urology Focus 2017;3(1):119-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
McMahon 2004
- McMahon CG, Abdo C, Incrocci L, Perelman M, Rowland D, Waldinger M, et al. Disorders of orgasm and ejaculation in men. Journal of Sexual Medicine 2004;1(1):58-65. [DOI] [PubMed] [Google Scholar]
McMahon 2011
- McMahon CG, Porst H. Oral agents for the treatment of premature ejaculation: review of efficacy and safety in the context of the recent International Society for Sexual Medicine criteria for lifelong premature ejaculation. Journal of Sexual Medicine 2011;8(10):2707-25. [DOI] [PubMed] [Google Scholar]
Melnik 2011
- Melnik T, Althof S, Atallah AN, Puga ME, Glina S, Riera R. Psychosocial interventions for premature ejaculation. Cochrane Database of Systematic Reviews 2011, Issue 8. Art. No: CD008195. [DOI: 10.1002/14651858.CD008195.pub2] [DOI] [PubMed] [Google Scholar]
Mulhall 2012
- Mulhall JP. Premature ejaculation. In: Wein AJ, Kavoussi LR, Novick A, Partin AW, Peters CA, editors(s). Campbell-Walsh Urology. 1st edition. Philadelphia: Elsevier Saunders, 2012:770-9. [Google Scholar]
Ozbek 2011
- Ozbek E, Tasci AI, Tugcu V, Ilbey YO, Simsek A, Ozcan L, et al. Possible association of the 5-HTTLPR serotonin transporter promoter gene polymorphism with premature ejaculation in a Turkish population. Asian Journal of Andrology 2009;11(3):351-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Patrick 2009
- Patrick DL, Giuliano F, Ho KF, Gagnon DD, McNulty P, Rothman M. The Premature Ejaculation Profile: validation of self-reported outcome measures for research and practice. BJU International 2009;103(3):358-64. [DOI] [PubMed] [Google Scholar]
Pompili 2010
- Pompili M, Serafini G, Innamorati M, Ambrosi E, Giordano G, Girardi P, et al. Antidepressants and suicide risk: a comprehensive overview. Pharmaceuticals 2010;3(9):2861-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pu 2013
- Pu C, Yang L, Liu L, Yuan H, Wei Q, Han P. Topical anesthetic agents for premature ejaculation: a systematic review and meta-analysis. Urology 2013;81(4):799-804. [DOI] [PubMed] [Google Scholar]
Puppo 2014
- Puppo V. Premature ejaculation during vaginal intercourse is not a male sexual dysfunction. Internal Medicine Journal 2014;44(10):1049. [DOI] [PubMed] [Google Scholar]
Retractionwatch 2015
- Retractionwatch. Urology researcher in Iran up to six retractions, 2015. retractionwatch.com/2015/04/24/urology-researcher-in-iran-up-to-six-retractions/ (accessed 28 October 2020).
Review Manager 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Riley 2011
- Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta-analyses. BMJ 2011;342:d549. [DOI] [PubMed] [Google Scholar]
Roberts 2015
- Roberts I, Ker K, Edwards P, Beecher D, Manno D, Sydenham E. The knowledge system underpinning healthcare is not fit for purpose and must change. BMJ 2015;350:h2463. [DOI] [PubMed] [Google Scholar]
Rosen 2007a
- Rosen RC, McMahon CG, Niederberger C, Broderick GA, Jamieson C, Gagnon DD. Correlates to the clinical diagnosis of premature ejaculation: results from a large observational study of men and their partners. Journal of Urology 2007;177(3):1059-64. [DOI] [PubMed] [Google Scholar]
Rosen 2007b
- Rosen RC, Catania JA, Althof SE, Pollack LM, O'Leary M, Seftel AD, et al. Development and validation of four-item version of male sexual health questionnaire to assess ejaculatory dysfunction. Urology 2007;69(5):805-9. [DOI] [PubMed] [Google Scholar]
Rowlands 2007
- Rowlands DL, Patrick DL, Rothamn M, Gagnon DD. The psychological burden of premature ejaculation. Journal of Urology 2007;177(3):1065-70. [DOI] [PubMed] [Google Scholar]
Russo 2016
- Russo A, Capogrosso P, Ventimiglia E, La Croce G, Boeri L, Montorsi F, et al. Efficacy and safety of dapoxetine in treatment of premature ejaculation: an evidence-based review. International Journal of Clinical Practice 2016;70(9):723-33. [DOI] [PubMed] [Google Scholar]
Safarinejad 2006a
- Safarinejad MR, Hosseini SY. Safety and efficacy of tramadol in the treatment of premature ejaculation: a double-blind, placebo-controlled, fixed-dose, randomized study. Journal of Clinical Psychopharmacology 2006;26(1):27-31. [DOI] [PubMed] [Google Scholar]
Salem 2008
- Salem EA, Wilson SK, Bissada NK, Delk JR, Hellstrom WJ, Cleves MA. Tramadol HCl has promise in on-demand use to treat premature ejaculation. Journal of Sexual Medicine 2008;5(1):188-93. [DOI] [PubMed] [Google Scholar]
Sanchez 2014
- Sanchez C, Reines EH, Montgomery SA. A comparative review of escitalopram, paroxetine, and sertraline: are they all alike? International Clinical Psychopharmacology 2014;29(4):185-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
Semans 1956
- Semans JH. Premature ejaculation: a new approach. Southern Medical Journal 1956;49(4):353-8. [DOI] [PubMed] [Google Scholar]
Serefoglu 2014
- Serefoglu EC, McMahon CG, Waldinger MD, Althof SE, Shindel A, Adaikan G, et al. An evidence-based unified definition of lifelong and acquired premature ejaculation: report of the Second International Society for Sexual Medicine Ad Hoc Committee for the Definition of Premature Ejaculation. Journal of Sexual Medicine 2014;11(6):1423-41. [DOI] [PubMed] [Google Scholar]
Shabsigh 2006
- Shabsigh R. Diagnosing premature ejaculation: a review. Journal of Sexual Medicine 2006;3(Suppl 4):318-23. [DOI] [PubMed] [Google Scholar]
Sharma 2016
- Sharma T, Guski LS, Freund N, Gotzsche PC. Suicidality and aggression during antidepressant treatment: systematic review and meta-analyses based on clinical study reports. BMJ 2016;352:i65. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shindel 2020
- Shindel AW, Althof SE, Carrier S, Chou R, McMahon CG, Mulhall JP, et al. Disorders of ejaculation: an AUA/SMSNA guideline, 2020. www.auanet.org/guidelines/disorders-of-ejaculation (accessed 28 October 2020).
Soderfeldt 2017
- Soderfeldt Y, Droppe A, Ohnhauser T. Distress, disease, desire: perspectives on the medicalisation of premature ejaculation. Journal of Medical Ethics 2017;1:1-2. [DOI] [PubMed] [Google Scholar]
Sprouse 2001
- Sprouse J, Braselton J, Reynolds L, Clarke T, Rollema H. Activation of postsynaptic 5-HT(1A) receptors by fluoxetine despite the loss of firing-dependent serotonergic input: electrophysiological and neurochemical studies. Synapse 2001;41(1):49-57. [DOI] [PubMed] [Google Scholar]
Sridharan 2018
- Sridharan K, Sivaramakrishnan G, Sequeira R, Al-Khaja KA. Pharmacological interventions for premature ejaculation: a mixed-treatment comparison network meta-analysis of randomized clinical trials. International Journal of Impotence Research 2018;30(5):215-23. [DOI] [PubMed] [Google Scholar]
Sterne 2011
- Sterne JA, Sutton AJ, Ioannidis JP, Terrin N, Jones DR, Lau J, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 2011;343:d4002. [DOI] [PubMed] [Google Scholar]
Sun 2017
- Sun Y, Yang L, Bao Y, Liu Z, Liu L, Wei Q. Efficacy of PDE5Is and SSRIs in men with premature ejaculation: a new systematic review and five meta-analyses. World Journal of Urology 2017;35(12):1817-31. [DOI] [PubMed] [Google Scholar]
Symonds 2007
- Symonds T, Perelman MA, Althof S, Giuliano F, Martin M, May K, et al. Development and validation of a premature ejaculation diagnostic tool. European Urology 2007;52(2):565-73. [DOI] [PubMed] [Google Scholar]
Waldinger 2002
- Waldinger MD. The neurobiological approach to premature ejaculation. Journal of Urology 2002;168(6):2359-67. [DOI] [PubMed] [Google Scholar]
Waldinger 2004
- Waldinger MD, Zwinderman AH, Schweitzer DH, Olivier B. Relevance of methodological design for the interpretation of efficacy of drug treatment of premature ejaculation: a systematic review and meta-analysis. International Journal of Impotence Research 2004;16(4):369-81. [DOI] [PubMed] [Google Scholar]
Waldinger 2005a
- Waldinger MD, Schweitzer DH, Olivier B. On-demand SSRI treatment of premature ejaculation: pharmacodynamic limitations for relevant ejaculation delay and consequent solutions. Journal of Sexual Medicine 2005;2(1):121-31. [DOI] [PubMed] [Google Scholar]
Waldinger 2005b
- Waldinger MD, Zwinderman AH, Olivier B, Schweitzer DH. Proposal for a definition of lifelong premature ejaculation based on epidemiological Stopwatch data. Journal of Sexual Medicine 2005;2(4):498-507. [DOI] [PubMed] [Google Scholar]
Waldinger 2006
- Waldinger MD, Schweitzer DH. Changing paradigms from a historical DSM-III and DSM-IV view toward an evidence-based definition of premature ejaculation. Part II – proposals for DSM-V and ICD-11. Journal of Sexual Medicine 2006;3(4):693-705. [DOI] [PubMed] [Google Scholar]
Waldinger 2007
- Waldinger MD. Premature ejaculation: state of the art. Urologic Clinics of North America 2007;34(4):591-9, vii-viii. [DOI] [PubMed] [Google Scholar]
Waldinger 2008
- Waldinger MD, Zwinderman AH, Olivier B, Schweitzer DH. Geometric mean IELT and premature ejaculation: appropriate statistics to avoid overestimation of treatment efficacy. Journal of Sexual Medicine 2008;5(2):492-9. [DOI] [PubMed] [Google Scholar]
Wood 2008
- Wood L, Egger M, Gluud LL, Schulz KF, Jüni P, Altman DG, et al. Empirical evidence of bias in treatment effect estimates in controlled trials with different interventions and outcomes: meta-epidemiological study. BMJ 2008;336(7644):601-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Xia 2013
- Xia JD, Han YF, Zhou LH, Chen Y, Dai YT. Efficacy and safety of local anaesthetics for premature ejaculation: a systematic review and meta-analysis. Asian Journal of Andrology 2013;15(4):497-502. [DOI] [PMC free article] [PubMed] [Google Scholar]
Yue 2015
- Yue FG, Dong L, Hu TT, Qu XY. Efficacy of dapoxetine for the treatment of premature ejaculation: a meta-analysis of randomized clinical trials on intravaginal ejaculatory latency time, patient-reported outcomes, and adverse events. Urology 2015;85(4):856-61. [DOI] [PubMed] [Google Scholar]
Zhang 2019
- Zhang D, Cheng Y, Wu K, Ma Q, Jiang J, Yan Z. Paroxetine in the treatment of premature ejaculation: a systematic review and meta-analysis. BMC Urology 2019;19(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Mian 2017
- Mian R, Bodie JA, Soubra A, Lyon JA, Sultan S, Dahm P. Selective serotonin re-uptake inhibitors for premature ejaculation. Cochrane Database of Systematic Reviews 2017, Issue 9. Art. No: CD012799. [DOI: 10.1002/14651858.CD012799] [DOI] [PMC free article] [PubMed] [Google Scholar]


