Abstract
Background
Chronic nonspecific low back pain (LBP) is very common; it is defined as pain without a recognizable etiology that lasts for more than three months. Some clinical practice guidelines suggest that acupuncture can offer an effective alternative therapy. This review is a split from an earlier Cochrane review and it focuses on chronic LBP.
Objectives
To assess the effects of acupuncture compared to sham intervention, no treatment, or usual care for chronic nonspecific LBP.
Search methods
We searched CENTRAL, MEDLINE, Embase, CINAHL, two Chinese databases, and two trial registers to 29 August 2019 without restrictions on language or publication status. We also screened reference lists and LBP guidelines to identify potentially relevant studies.
Selection criteria
We included only randomized controlled trials (RCTs) of acupuncture for chronic nonspecific LBP in adults. We excluded RCTs that investigated LBP with a specific etiology. We included trials comparing acupuncture with sham intervention, no treatment, and usual care. The primary outcomes were pain, back‐specific functional status, and quality of life; the secondary outcomes were pain‐related disability, global assessment, or adverse events.
Data collection and analysis
Two review authors independently screened the studies, assessed the risk of bias and extracted the data. We meta‐analyzed data that were clinically homogeneous using a random‐effects model in Review Manager 5.3. Otherwise, we reported the data qualitatively. We used the GRADE approach to assess the certainty of the evidence.
Main results
We included 33 studies (37 articles) with 8270 participants. The majority of studies were carried out in Europe, Asia, North and South America. Seven studies (5572 participants) conducted in Germany accounted for 67% of the participants. Sixteen trials compared acupuncture with sham intervention, usual care, or no treatment. Most studies had high risk of performance bias due to lack of blinding of the acupuncturist. A few studies were found to have high risk of detection, attrition, reporting or selection bias.
We found low‐certainty evidence (seven trials, 1403 participants) that acupuncture may relieve pain in the immediate term (up to seven days) compared to sham intervention (mean difference (MD) ‐9.22, 95% confidence interval (CI) ‐13.82 to ‐4.61, visual analogue scale (VAS) 0‐100). The difference did not meet the clinically important threshold of 15 points or 30% relative change. Very low‐certainty evidence from five trials (1481 participants) showed that acupuncture was not more effective than sham in improving back‐specific function in the immediate term (standardized mean difference (SMD) ‐0.16, 95% CI ‐0.38 to 0.06; corresponding to the Hannover Function Ability Questionnaire (HFAQ, 0 to 100, higher values better) change (MD 3.33 points; 95% CI ‐1.25 to 7.90)). Three trials (1068 participants) yielded low‐certainty evidence that acupuncture seemed not to be more effective clinically in the short term for quality of life (SMD 0.24, 95% CI 0.03 to 0.45; corresponding to the physical 12‐item Short Form Health Survey (SF‐12, 0‐100, higher values better) change (MD 2.33 points; 95% CI 0.29 to 4.37)). The reasons for downgrading the certainty of the evidence to either low to very low were risk of bias, inconsistency, and imprecision.
We found moderate‐certainty evidence that acupuncture produced greater and clinically important pain relief (MD ‐20.32, 95% CI ‐24.50 to ‐16.14; four trials, 366 participants; (VAS, 0 to 100), and improved back function (SMD ‐0.53, 95% CI ‐0.73 to ‐0.34; five trials, 2960 participants; corresponding to the HFAQ change (MD 11.50 points; 95% CI 7.38 to 15.84)) in the immediate term compared to no treatment. The evidence was downgraded to moderate certainty due to risk of bias. No studies reported on quality of life in the short term or adverse events.
Low‐certainty evidence (five trials, 1054 participants) suggested that acupuncture may reduce pain (MD ‐10.26, 95% CI ‐17.11 to ‐3.40; not clinically important on 0 to 100 VAS), and improve back‐specific function immediately after treatment (SMD: ‐0.47; 95% CI: ‐0.77 to ‐0.17; five trials, 1381 participants; corresponding to the HFAQ change (MD 9.78 points, 95% CI 3.54 to 16.02)) compared to usual care. Moderate‐certainty evidence from one trial (731 participants) found that acupuncture was more effective in improving physical quality of life (MD 4.20, 95% CI 2.82 to 5.58) but not mental quality of life in the short term (MD 1.90, 95% CI 0.25 to 3.55). The certainty of evidence was downgraded to moderate to low because of risk of bias, inconsistency, and imprecision.
Low‐certainty evidence suggested a similar incidence of adverse events immediately after treatment in the acupuncture and sham intervention groups (four trials, 465 participants) (RR 0.68 95% CI 0.46 to 1.01), and the acupuncture and usual care groups (one trial, 74 participants) (RR 3.34, 95% CI 0.36 to 30.68). The certainty of the evidence was downgraded due to risk of bias and imprecision. No trial reported adverse events for acupuncture when compared to no treatment. The most commonly reported adverse events in the acupuncture groups were insertion point pain, bruising, hematoma, bleeding, worsening of LBP, and pain other than LBP (pain in leg and shoulder).
Authors' conclusions
We found that acupuncture may not play a more clinically meaningful role than sham in relieving pain immediately after treatment or in improving quality of life in the short term, and acupuncture possibly did not improve back function compared to sham in the immediate term. However, acupuncture was more effective than no treatment in improving pain and function in the immediate term. Trials with usual care as the control showed acupuncture may not reduce pain clinically, but the therapy may improve function immediately after sessions as well as physical but not mental quality of life in the short term. The evidence was downgraded to moderate to very low‐certainty considering most of studies had high risk of bias, inconsistency, and small sample size introducing imprecision. The decision to use acupuncture to treat chronic low back pain might depend on the availability, cost and patient's preferences.
Keywords: Humans, Acupuncture Therapy, Acupuncture Therapy/adverse effects, Acupuncture Therapy/methods, Bias, Chronic Pain, Chronic Pain/therapy, Confidence Intervals, Low Back Pain, Low Back Pain/therapy, Quality of Life, Randomized Controlled Trials as Topic, Treatment Outcome
Plain language summary
Acupuncture for chronic non‐specific low‐back pain (LBP)
Review question
Does acupuncture safely reduce pain and improve back‐related function and quality of life for people with chronic nonspecific LBP?
Background
Most people have experienced chronic LBP. Some of them choose acupuncture to relieve their pain and other symptoms.
Search date
The evidence is current to 29 August 2019.
Study characteristics.
We reviewed 33 trials (37 articles) with 8270 participants. The trials were carried out in Europe, Asia, North and South America. The studies compared acupuncture with sham (placebo), no treatment and usual care.
Key results
Compared with sham, acupuncture may not be more effective in reducing pain immediately after treatment. Acupuncture perhaps did not appear to improve back‐specific function immediately after treatment, or may not enhance quality of life in the short term.
Acupuncture was better than no treatment for pain relief and functional improvement immediately after treatment.
Compared with usual care, acupuncture did not appear to significantly clinically reduce pain, but seemed more effective in improving function immediately after treatment. Acupuncture did not improve quality of life in the short‐term.
The incidence of adverse events may be similar between acupuncture and sham, and between acupuncture and usual care. Adverse effects related to acupuncture were considered minor or moderate.
Certainty of the evidence
The certainty of the evidence ranged from very low to moderate. Many trials showed a high risk of bias due to problems with masking the acupuncturists or participants. This may affect the participants reported outcomes and trialists computed effects. Some outcomes were based on small samples, resulting in inconsistency and imprecision of results.
Summary of findings
Summary of findings 1. Acupuncture compared to sham intervention for chronic nonspecific low back pain.
| Acupuncture compared to sham intervention for chronic nonspecific low back pain | ||||||
| Patient or population: chronic nonspecific low back pain Setting: outpatient clinics or inpatient units, in hospitals or the community Intervention: acupuncture Comparison: sham intervention | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk with sham intervention | Corresponding risk with acupuncture | |||||
| Pain intensity VAS (0 to 100; 0 = no pain, 100 = worst pain) Follow‐up: immediately after; < 7 days after the end of the sessions |
The mean pain intensity in the sham group immediately after was 51.0 points (SD 18.7) | The MD was 9.22 lower in the acupuncture group (13.82 lower to 4.61 lower) | Not applicable | 1403 (7 RCTs) | ⊕⊕⊝⊝ LOWa,b | The difference did not meet predefined clinically relevant change. |
| Back‐specific functional status HFAQ (0 to 100; 0 = disabled, 100 = full function) Follow‐up: immediately after; < 7 days after the end of the sessions |
The mean back‐specific function in the sham group immediately after was 61.3 points (SD 20.8) | The MD was 3.33 points higher in the acupuncture group (1.25 lower to 7.90 higher) | Not applicable | 1481 (5 RCTs) | ⊕⊝⊝⊝ VERY LOWa,b,c | The corresponding risk estimated using SMD was ‐0.16 (95% CI ‐0.38 to 0.06). |
| Quality of life (QoL) SF‐12 (0 to 100; 0 = poor QoL, 100 = high QoL) Follow‐up: short term; 8 days to 3 months |
The mean quality of life in the sham group in the short term was 39.2 points (SD 9.7) ‐ |
The MD was 2.33 points higher in the acupuncture group
(0.29 higher to 4.37 higher) ‐ |
Not applicable ‐ |
1068
(3 RCTs) ‐ |
⊕⊕⊝⊝
LOWa,b ‐ |
The corresponding risk estimated using SMD was 0.24 (95% CI 0.03 to 0.45). The difference did not meet predefined clinically relevant change. Not reported |
| Mental health Follow‐up: short term; 8 days to 3 months mental health | ||||||
| Adverse events Self‐reported Follow‐up: immediately after; < 7 days after the end of the sessions |
Study population | RR 0.68 (0.46 to 1.01) | 465 (4 RCTs) | ⊕⊕⊝⊝ LOWa,c | The most common adverse events were pain at insertion points, hematoma, bleeding, worsening of LBP, pain other than LBP (pain in leg and shoulder). | |
| 159 per 1000 | 108 per 1000 (73 to 161) | |||||
|
* The risk in the acupuncture group (and its 95% CI) was based on the assumed risk in the sham intervention group and the relative effect of the acupuncture (and its 95% CI). When there was more than one study for an outcome, we chose the sham control group mean from the included study that had the most representative study population and the largest weighting in the overall result in Review Manager 5. For pain and back‐specific functional status, this was Haake 2007 in the immediate term. For quality of life, this was Haake 2007 in the short term. CI: confidence interval; MD: mean difference; SMD: standardized mean difference; SD: standard deviation; RR: risk ratio; RCTs: randomized controlled trials; VAS: Visual Analog Scale; HFAQ: Hannover Function Ability Questionnaire; SF‐36: Short Form Health Survey. | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
aDowngraded one level for risk of bias (performance and attrition bias). bDowngraded one level for inconsistency (I² ≥ 50%). cDowngraded one level for imprecision (CI included the null effect).
Summary of findings 2. Acupuncture compared to no treatment for chronic nonspecific low back pain.
| Acupuncture compared to no treatment for chronic nonspecific low back pain | ||||||
| Patient or population: chronic nonspecific low back pain Setting: outpatient clinics or inpatient units, in hospitals or the community Intervention: acupuncture Comparison: no treatment | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk with no treatment | Corresponding risk with acupuncture | |||||
| Pain intensity VAS (0 to 100; 0 = no pain, 100 = worst pain) Follow‐up: immediately after; < 7 days after the end of the sessions |
The mean pain intensity in the no treatment group immediately after the sessions was 50.86 points (SD 20.51) | The MD was 20.32 points lower in the acupuncture group (24.50 lower to 16.14 lower) | Not applicable | 366 (4 RCTs) | ⊕⊕⊕⊝ MODERATEa | Acupuncture reduced pain more than no treatment in the immediate term. |
| Back‐specific functional status HFAQ (0 to 100; 0 = disabled, 100 = full function) Follow‐up: immediately after; < 7 days after the end of the sessions |
The mean back‐specific function in the no treatment group immediately after the sessions was 65.5 points (SD 21.7) | The MD was 11.50 points higher in the acupuncture group (7.38 higher to 15.84 higher) | Not applicable | 2960 (5 RCTs) | ⊕⊕⊕⊝ MODERATEa | The corresponding risk estimated using SMD was ‐0.53 (95% CI ‐0.73 to ‐0.34). The difference did not meet predefined clinically relevant change. |
| Quality of life (QoL) physical health, mental health Follow‐up: short term; 8 days to 3 months |
‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| Adverse events Self‐reported Follow‐up: immediately after; < 7 days after the end of the sessions |
‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
|
* The risk in the acupuncture group (and its 95% CI) was based on the assumed risk in the no treatment group and the relative effect of the acupuncture (and its 95% CI). CI: confidence interval; MD: mean difference; SMD: standardized mean difference; SD: standard deviation; RR: risk ratio; RCTs: randomized controlled trials; VAS: Visual Analog Scale; HFAQ: Hannover Function Ability Questionnaire; SF‐36: Short Form Health Survey. | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
aDowngraded one level for risk of bias (performance, detection, and attrition bias).
Summary of findings 3. Acupuncture compared to usual care for chronic nonspecific low back pain.
| Acupuncture compared to usual care for chronic nonspecific low back pain | ||||||
| Patient or population: chronic nonspecific low back pain Setting: outpatient clinics or inpatient units, in hospitals or the community Intervention: acupuncture Comparison: usual care | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk with usual care | Corresponding risk with acupuncture | |||||
| Pain intensity VAS (0 to 100; 0 = no pain, 100 = worst pain) Follow‐up: immediately after; < 7 days after the end of the sessions |
The mean pain intensity in the usual care groups immediately after the sessions was 57.1 points (SD 16.5) | The MD was 10.26 points lower in the acupuncture groups (17.11 lower to 3.40 lower) | Not applicable | 1054 (5 RCTs) | ⊕⊕⊝⊝ LOWa,b | The difference did not meet the predefined clinically relevant change. |
| Back‐specific functional status HFAQ (0 to 100; 0 = disabled, 100 = full function) Follow‐up: immediately after; < 7 days after the end of the sessions |
The mean back‐specific function immediately after the sessions was 56.3 points (SD 20.8) | The MD was 9.78 points higher in the acupuncture groups (3.54 higher to 16.02 higher) | Not applicable | 1381 (5 RCTs) | ⊕⊕⊝⊝ LOWa,b | The corresponding risk estimated using SMD was ‐0.47 (95% CI ‐0.77 to ‐0.17). The difference did not meet the predefined clinically relevant change. |
| Quality of life (QoL) – physical health SF‐12 (0 to 100; 0 = poor QoL, 100 = high QoL) Follow‐up: short term; 8 days to 3 months |
The mean QoL – physical health – in the usual care group in the short term was 36.1 points (SD 8.9) The mean QoL – mental health – in the usual care group in the short term was 48.6 points (SD 11.6) |
The MD was 4.20 points higher in the acupuncture group (2.82 higher to 5.58 higher) The MD was 1.90 points higher in the acupuncture group (0.25 higher to 3.55 higher) |
Not applicable Not applicable |
731
(1 RCT) 731 (1 RCT) |
⊕⊕⊕⊝
MODERATEc ⊕⊕⊕⊝ MODERATEc |
The authors of this study did not provide the total results of the SF‐12, only the subgroups. The difference did not meet the predefined clinically relevant change. The authors of this study did not provide the total results of the SF‐12, only the subgroups. |
| QoL: mental health SF‐12 (0 to 100; 0 = poor QoL, 100 = high QoL) Follow‐up: short term; 8 days to 3 months | ||||||
| Adverse events Self‐reported Follow‐up: immediately after; < 7 days after the end of the sessions |
Study population | RR 3.34 (0.36 to 30.68) | 74 (1 RCT) | ⊕⊕⊝⊝ LOWc,d | One study reported three adverse events (2 pain and 1 circulation problem) in the acupuncture group and one in the usual care group (persisting pain). | |
| 26 per 1000 | 86 per 1000 (9 to 787) | |||||
|
* The risk in the acupuncture group (and its 95% CI) was based on the assumed risk in the sham intervention group and the relative effect of the acupuncture (and its 95% CI). When there was more than one study for an outcome, we chose the sham control group mean from the included study that had the most representative study population and the largest weighting in the overall result in Review Manager 5. For pain and back‐specific functional status, this was Haake 2007 in the immediate term. CI: confidence interval; MD: mean difference; SMD: standardized mean difference; SD: standard deviation; RR: risk ratio; RCTs: randomized controlled trials; VAS: Visual Analog Scale; HFAQ: Hannover Function Ability Questionnaire; SF‐12: Short Form Health Survey. | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
aDowngraded one level for risk of bias (performance, attrition, and selection bias). bDowngraded one level for inconsistency (I² ≥ 75%) that could only be partly explained. cDowngraded one level for risk of bias (performance and attrition bias). dDowngraded one level for imprecision (CI included a null effect).
Background
Description of the condition
Low back pain (LBP) is defined as pain or discomfort localised between the lower rib and the inferior gluteal fold. Chronic nonspecific LBP is defined as pain occurring for more than three months that is not attributable to a recognisable specific pathology (e.g. infection, tumor, osteoporosis, lumbar spine fracture, structural deformity, inflammatory disorder, radicular syndrome, or cauda equina syndrome (Balague 2012)). LBP is prevalent in the general population and chronic nonspecific LBP accounts for the majority of cases (Berman 2010; Furlan 2012). The adjusted lifetime prevalence of LBP has been reported to be 31.0% ± 0.6% (Hoy 2012), and in some cases, as high as 84% (Balague 2012). Prevalence increases and peaks between 40 and 69 years of age (Hoy 2012). Chronic LBP is a major cause of disablement, absenteeism, and high medical expenses. Such problems place a great economic burden on society, with an estimated USD 1.93 to 81.24 billion per person, adjusted in 2015, spent in developed countries (Hartvigsen 2018). People with chronic LBP often require long‐term treatment, but do not always respond to conventional therapies, such as physiotherapy, exercise, or mild analgesics (Balague 2012; Chou 2007; NICE 2016). In such cases, acupuncture, an ancient therapy, could be recommended for LBP treatment (Liu 2015a; Qaseem 2017).
Description of the intervention
Acupuncture originated in China 4000 years ago (Lao 1996). The practice is based on traditional Chinese medicine, according to which, the body's vital energy, known as Qi, flows through 12 primary and eight secondary meridians in the body (Berman 2010). The proper flow of Qi is believed to be restored when acupuncture needles are inserted into the skin, with or without manipulation, at specific points along the meridians (Berman 2010). The manipulation of the needles can elicit in patients a 'needle grasp' sensation called 'De Qi', a subjective feeling of soreness, fullness, numbness, or tingling (Lao 1996). Dry needling, also known as myofascial trigger point needling, is similar to the use of acupuncture at Ah Shi points, which often correspond to trigger points or tender points (or both) in the myofascial tissue. Dry needling is now known as myofascial acupuncture. Both acupuncture and dry needling can be given further stimulatory effects using small electrical currents (electroacupuncture), moxibustion (burning the herb moxa at the handle of the needle), or heat lamps (Lao 1996). No optimal protocol for treating people with chronic LBP has yet been established.
How the intervention might work
Various hypotheses have been proposed regarding the mechanism of acupuncture, but none offer a complete explanation. The gate control theory, one of the most popular, posits that one type of sensory input – 'pain' ‐ can be 'inhibited in the central nervous system by another type of input – 'needling insertion' (Melzack 1981). Acupuncture has been shown to stimulate the release of endogenous opioids in the brain‐stem, sub‐cortical, and limbic structures (Han 2003; Pomeranz 1996), and adrenocorticotropic hormone and cortisol in the pituitary gland (Li 2008). Functional magnetic resonance imaging (MRI) images have shown that prolonged acupuncture stimulation has immediate effects in the human limbic and basal forebrain areas, which are thought to be involved in pain processing (Dhond 2007). Additionally, research has indicated that the sensation of De Qi is related to the mechanical grasp of connective tissue under the skin, inducing an unknown psychological change (Langevin 2002). Acupuncture has also been reported to stimulate the release of adenosine at the site of needle stimulation (Goldman 2010), and to increase local blood flow (Kim 2016). The effect of acupuncture is thought to be strongly related to psychosocial factors, including patients’ expectations, beliefs, and therapeutic environment (Berman 2010).
Why it is important to do this review
Many systematic reviews have investigated the effectiveness of acupuncture for chronic LBP (Ammendolia 2008; Lam 2013; Liu 2015a; Manheimer 2005; Rubinstein 2010; Xu 2013). However, the findings reported in these reviews, particularly those of studies comparing true acupuncture with sham, have been inconsistent. Evidence is lacking on the effectiveness of acupuncture versus other active therapies, different styles of acupuncture, and acupuncture plus a therapy versus the therapy alone. As the body of literature has grown substantially since our previous review (Furlan 2005), we decided to update the evidence. We split the previous review into two separate reviews, focusing individually on acute and chronic nonspecific LBP. This review covers the scientific evidence of the effectiveness of acupuncture for chronic nonspecific LBP.
Objectives
To assess the effects of acupuncture compared to sham intervention, no treatment, and usual care, for chronic nonspecific LBP, measuring outcomes related to pain, function, quality of life, and adverse events.
The secondary objectives were to assess the effects of acupuncture compared to another intervention, acupuncture supplemented by an intervention versus the intervention alone, and different styles of acupuncture.
Methods
Criteria for considering studies for this review
Types of studies
We included only randomized controlled trials (RCTs) that examined the effects of acupuncture on chronic nonspecific LBP; we excluded quasi‐randomized trials.
Types of participants
We studied adults, 18 years and older, with chronic nonspecific LBP, defined as pain lasting more than three months without a specific etiology. In studies with mixed population of acute and chronic LBP, we included studies in which the majority of the participants (> 50%) had chronic nonspecific LBP, or if we could extract the results separately for the group with chronic LBP.
We excluded RCTs if they investigated LBP caused by specific etiology, including infection, metastatic diseases, neoplasm, osteoarthritis, rheumatoid arthritis, fractures of the spine, protrusion of a disk, and nerve root involvement, such as sciatica with radiation below the knee. We also excluded studies of LBP occurring during pregnancy and the postpartum period.
Types of interventions
We included studies in which acupuncture treatment was conducted according to Traditional Chinese Medicine (TCM) theory. Needles were inserted into classical meridian points, tender points, or trigger points in the skin. Manual stimulation, heating by moxa, or electrical current stimulation could be further administered to maximize the effectiveness.
The comparators were sham intervention, no treatment, usual care, or other therapies. We also included trials comparing acupuncture plus another intervention to the intervention alone, and trials comparing two acupuncture techniques. We excluded trials that did not use needles, such as acupressure or laser acupuncture.
Types of outcome measures
Primary outcomes
Pain intensity (measured with a visual analogue scale (VAS), numeric rating scale (NRS), Chronic Pain Grade Classification‐pain (CPGS‐pain), etc.)
Back‐specific functional status (measured with the Roland Morris Disability Questionnaire (RMDQ), Oswestry Disability Index (ODI), Hannover Functional Ability Questionnaire (HFAQ), etc.)
Quality of life (measured with the 36‐ or 12‐item Short Form Health Survey (SF‐36, SF‐12), etc.)
Secondary outcomes
Pain‐related disability (measured with the pain disability index (PDI), etc.). This included work‐relevant outcomes, such as sick leave days, work status, absenteeism, presenteeism, productivity, etc.
Global assessment of therapy effectiveness
Adverse events
Timing of follow‐up
Immediately after to up to seven days after the end of the sessions
Short term ‐ between the eighth day and three months after the end of the sessions
Intermediate term ‐ between the fourth month and one year after the end of the sessions
Long term ‐ more than one year after the end of the sessions
Search methods for identification of studies
Electronic searches
We searched the following databases to 30 August 2019.
Cochrane Back and Neck trials register (The Central Register of Contracts (CRS) web) (29 August 2019);
Cochrane Central Register of Controlled Trials (CENTRAL; CRS web) (29 August 2019);
MEDLINE(R) Ovid Epub Ahead of Print, In‐Process, and Other Non‐indexed Citations, MEDLINE(R) Ovid Daily and MEDLINE(R) Ovid (1946 to 29 August 2019);
Embase (Ovid, 1974 to 2019 Week 34);
Cumulative Index to Nursing and Allied Health Literature (CINAHLplus, EBSCO; 1937 to 29 August 2019);
China National Knowledge Infrastructure database (CNKI; 1995 to 30 August 2019);
WangFang database (1995 to 30 August 2019);
US National Institutes of Health (clinicaltrials.gov/; 29 August 2019);
World Health Organization (WHO) International Clinical Trials Registry Platform (apps.who.int/trialsearch/Default.aspx; 29 August 2019).
Search strategies for the English databases were developed in accordance with the CBN method guidelines (Furlan 2015) by a Cochrane information specialist. We developed the strategies for the Chinese databases in consultation with a medical librarian at the University of Hong Kong. The search strategies can be found in Appendix 1.
Searching other resources
We reviewed the references in included articles, systematic reviews, and LBP guidelines to find eligible studies.
Data collection and analysis
We followed the methods recommended by the Cochrane Handbook of Systematic Reviews of Interventions (Higgins 2019), and the Cochrane Back and Neck guidelines (Furlan 2015).
Selection of studies
Two review authors (JLM and ZPN) independently reviewed titles and abstracts of articles retrieved from the searches according to the Criteria for considering studies for this review. They conducted a pilot screening to ensure they were consistently following the criteria. We obtained the full text of potential articles and the two review authors independently assessed them further. They used consensus to resolve disagreements and consulted two other review authors (LXL and AF) if they could not reach consensus.
Adequacy of treatment
Two review authors, who are experienced acupuncturists (LXL and MH), conducted independent and blinded assessments of the adequacy of acupuncture treatment in the included trials. Reviewers were blinded to the author, journal, and trial site. They used eight assessment items, developed from the previous Cochrane review and the updated STRICTA recommendations to assess adequacy of treatment (Furlan 2005; MacPherson 2010):
Choice of acupoints,
Number of sessions,
Treatment duration,
Treatment frequency,
Needling technique,
Acupuncturist experience,
Adequacy of sham or placebo intervention, and
Adequate number of sessions or dose of the control group.
The two review authors resolved disagreements by consensus. When disagreements could not be resolved, a third review author (AF) joined the discussion.
Data extraction and management
A pair of review authors (JLM and WYL) independently extracted the data. If there were disagreements, they discussed them and reached consensus; if they still disagreed, the third review author (LLX) joined the discussion until consensus was reached.
We developed a data extraction from the version used in our previous review, and followed the recommendations by CBN (Furlan 2005; Furlan 2015). We conducted pilot data extraction to test the form's applicability and the consistency of data extraction between different review authors. We extracted data at the time points closest to our predefined time points. We extracted adjusted data rather than unadjusted data, if available. We used Review Manager 5.3 to manage the data (Review Manager 2014). The detailed information of methods, participants, interventions and outcomes for individual trials are shown in the 'Characteristics of included studies' table.
Assessment of risk of bias in included studies
The same pair of review authors (JLM and WYL) independently assessed the risk of bias using the 13 items shown in Table 4 and Table 5, as recommended by the CBN (Furlan 2015), which were developed in accordance with the 'risk of bias' criteria in the Cochrane Handbook of Systematic Reviews of Interventions (Higgins 2019). The 13 items examine selection bias, performance bias, detection bias, attrition bias, reporting bias, and other sources of bias. The risk of bias was summarized by these five domains.
1. Sources of risk of bias.
| Bias domain | Source of bias | Possible answers |
| Selection | (1) Was the method of randomization adequate? | yes/no/unsure |
| Selection | (2) Was the treatment allocation concealed? | yes/no/unsure |
| Performance | (3) Was the participant blinded to the intervention? | yes/no/unsure |
| Performance | (4) Was the care provider blinded to the intervention? | yes/no/unsure |
| Detection | (5) Was the outcome assessor blinded to the intervention? | yes/no/unsure |
| Attrition | (6) Was the dropout rate described and acceptable? | yes/no/unsure |
| Attrition | (7) Were all randomized participants analyzed in the group to which they were allocated? | yes/no/unsure |
| Reporting | (8) Are reports of the study free of suggestion of selective outcome reporting? | yes/no/unsure |
| Selection | (9) Were the groups similar at baseline regarding the most important prognostic indicators? | yes/no/unsure |
| Performance | (10) Were co‐interventions avoided or similar? | yes/no/unsure |
| Performance | (11) Was the compliance acceptable in all groups? | yes/no/unsure |
| Detection | (12) Was the timing of the outcome assessment similar in all groups? | yes/no/unsure |
| Other | (13) Are other sources of potential bias unlikely? | yes/no/unsure |
2. Criteria for a judgement of 'yes' for the sources of risk of bias.
| 1 | A random (unpredictable) assignment sequence. Examples of adequate methods are coin toss (for studies with 2 groups), rolling a dice (for studies with 2 or more groups), drawing of balls of different colours, drawing of ballots with the study group labels from a dark bag, computer‐generated random sequence, pre‐ordered sealed envelopes, sequentially ordered vials, telephone call to a central office, and pre‐ordered list of treatment assignments. Examples of inadequate methods are: alternation, birth date, social insurance/security number, date in which they are invited to participate in the study, and hospital registration number. |
| 2 | Assignment generated by an independent person not responsible for determining the eligibility of the patients. This person has no information about the persons included in the trial and has no influence on the assignment sequence or on the decision about eligibility of the patient. |
| 3 | Index and control groups are indistinguishable for the participants, or if the success of blinding was tested among the participants and it was successful. |
| 4 | Index and control groups are indistinguishable for the care providers, or if the success of blinding was tested among the care providers and it was successful. |
| 5 | Adequacy of blinding should be assessed for each primary outcome separately. This item should be scored 'yes' if the success of blinding was tested among the outcome assessors and it was successful, or:
|
| 6 | The number of participants who were included in the study but did not complete the observation period or were not included in the analysis must be described and reasons given. If the percentage of withdrawals and dropouts does not exceed 20% for short‐term follow‐up and 30% for long‐term follow‐up and does not lead to substantial bias, a 'yes' is scored (note: these percentages are arbitrary, not supported by literature). |
| 7 | All randomized participants are reported and analyzed in the group to which they were allocated by randomization for the most important moments of effect measurement (minus missing values), irrespective of non‐compliance and co‐interventions. |
| 8 | All the results from all prespecified outcomes have been adequately reported in the published report of the trial. This information is either obtained by comparing the protocol and the report, or in the absence of the protocol, assessing that the published report includes enough information to make this judgement. |
| 9 | Groups have to be similar at baseline regarding demographic factors, duration and severity of complaints, percentage of participants with neurological symptoms, and value of main outcome measure(s). |
| 10 | If there were no co‐interventions, or they were similar between the index and control groups. |
| 11 | The reviewer determines if the compliance with the interventions is acceptable, based on the reported intensity, duration, number and frequency of sessions for both the index intervention and control intervention(s). For example, physiotherapy treatment is usually administered for several sessions; therefore, it is necessary to assess how many sessions each participant attended. For single‐session interventions (e.g. surgery), this item is irrelevant. |
| 12 | Timing of outcome assessment should be identical for all intervention groups and for all primary outcome measures. |
| 13 | Other types of biases. For example:
|
COI: conflict of interest Furlan 2015
We rated individual items at low, high, or unclear risk of bias for each included trial. For blinding of the acupuncturists, we realize it is very difficult to blind the person delivering acupuncture, and we rated studies as being at high risk when this was not done, and unclear risk when it was not clear or not described in detail. For dropout rate, we considered the following situations as being at high risk of bias: in the short‐ or long‐term follow‐up when dropouts exceeded 20%, unequal dropout rates across groups, and dropouts due to no response to acupuncture, which could lead to substantial bias. Similarly, we rated the risk of bias on compliance as high if the trials reported unequal compliance rates, which could affect the credibility of the results. After each individual item was assessed, we determined the risk of bias for each domain considering the scores of each item in that domain. We conducted a pilot assessment to ensure the criteria were consistently followed. Disagreements on risk of bias were resolved by consensus. A third review author (LXL) joined in the discussion if the disagreement persisted.
Measures of treatment effect
For dichotomous outcomes, we calculated a risk ratio (RR) and its 95% confidence interval (CI). For continuous outcomes, we calculated a mean difference (MD) with 95% CI when all studies used the same scales, or standardized mean difference (SMD) with 95% CI if the studies used different scales. When judging the effect size of pain intensity, we adopted a clinically important difference of 15 points on a 0 to 100 scale, 2 points on a 0 to 10 scale, or 30% change of the scores between two comparison groups (Dworkin 2008). We defined a clinically important change in back‐specific functional status using the data reported by the included trials, which was 3.7 points on the RMDQ scale (0 to 24 (Zaringhalam 2010)), 4.2 points on the ODI scale (0 to 50 (Cho 2013)), and 12% on the HFAQ scale (0 to 100 (Haake 2007)). For quality of life, we defined 4 points on the SF‐36 scale (Cherkin 2009), 3.29 on the physical component summary and 3.77 on the mental component summary of Short Form SF‐12 (SF‐12) (Diaz‐Arribas 2017) as a clinically important change. For pain‐related disability, we considered a decrease of 8.2 points in PDI (0 to 70) as a clinically important change (Brinkhaus 2006). When continuous data were measured by two or more tools and were combined in a meta‐analysis, we used Cohen's classification of SMD to assess the effect as small (SMD < 0.5), medium (SMD 0.5 to 0.8), or large (SMD > 0.8) (Cohen 1988). We considered measures of treatment effect to be statistically significant when the 95% CI excluded one in a RR, or zero in a MD or SMD.
Unit of analysis issues
For clinical trials using a simple parallel group design, we collected data from each participant and analyzed a single measurement, or measurements, assessing the same outcome. We did not include any cluster‐randomized trials in this review. Multi‐arm acupuncture studies set different control groups compared to acupuncture; for example, Cherkin and colleagues (Cherkin 2009) compared standardized acupuncture to individualized acupuncture, sham, or usual care group. The data were extracted into the corresponding comparisons in this review based on the controls' category.
Dealing with missing data
We contacted the first or corresponding author of the study to obtain missing data. We estimated data from graphs and figures when data were not presented in tables or text. If any information regarding SDs was missing, we calculated them from the confidence intervals. Otherwise, we estimated them from the corresponding baseline SDs.
Assessment of heterogeneity
We assessed clinical heterogeneity (i.e. differences in comparators, interventions, and outcomes) between studies qualitatively. For studies that we judged to have sufficient clinical homogeneity to combine, we further assessed statistical heterogeneity using the I² statistic. We assessed statistical heterogeneity of the results as low (I² = 0 to 40%), moderate (I² = 30% to 60%), substantial (I² = 50% to 90%), or considerable (I² = 75% to 100% (Higgins 2019)).
Assessment of reporting biases
We had planned to assess publication bias by using a funnel plot for meta‐analyses in which we included data from at least 10 studies. However, no meta‐analyses enrolled 10 studies or more. We assessed the risk of selective outcome reporting bias for each study as part of the 'Risk of bias' assessment.
Data synthesis
We considered statistical pooling or meta‐analyses when there was homogeneity of comparison group, outcome, and timing of follow‐up. We defined the comparison groups, primary and secondary outcomes, and the timing of follow‐up in Criteria for considering studies for this review. We conducted meta‐analyses using Review Manager 5.3 (Review Manager 2014). As we expected statistical heterogeneity, we used a random‐effects model to synthesize the results. We reported other variable outcomes or trials qualitatively. We used the GRADE approach including five aspects (study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the certainty of evidence as it related to the studies which contributed data to the meta‐analyses for the prespecified outcomes, and we reported the certainty of evidence as high, moderate, low, or very low, according to the methods and recommendations described in section 8.5 and 8.7, and chapters 11 and 12, of the Cochrane Handbook for Systematic Reviews of Interventions and CBN guidelines (Appendix 2; Furlan 2015; Higgins 2019; Ryan 2016; Schünemann 2017a; Schünemann 2017b). We used GRADEpro software to prepare the SoF tables (GRADEpro GDT 2020). Two reviewers (JLM and ADF) independently assessed the certainty of the evidence and it was planned that a third author (LXL) would join in if consent was not reached.
Subgroup analysis and investigation of heterogeneity
We did not conduct any subgroup analysis to investigate heterogeneity, as sufficient data for main factors were not available. We had planned to conduct subgroup analyses such as different protocols of acupuncture, shorter (≤ 1 year) or longer (> 1 year) pain duration, and older (mean age 65 years or older) versus younger age.
Sensitivity analysis
We had planned to perform sensitivity analysis based on potential sources of heterogeneity, such as the duration of the intervention, and pain intensity at baseline. We did not conduct sensitivity analyses as these data was not available in all studies.
Summary of findings and assessment of the certainty of the evidence
We prepared 'Summary of findings' tables for the main comparisons: acupuncture versus sham intervention, acupuncture versus no treatment, and acupuncture versus usual care. All 'Summary of findings' tables reported the primary outcomes: pain, back‐specific function and quality of life, and the secondary outcome, adverse events. We selected the follow‐up time "immediately after" for the outcomes of pain, function and adverse events, and we selected the "short‐term" follow‐up timing for the quality of life outcome.
Results
Description of studies
The details of all studies are shown in the Characteristics of included studies, Characteristics of excluded studies, Characteristics of studies awaiting classification, and Characteristics of ongoing studies tables.
Results of the search
The screening flow chart is shown in Figure 1. The updated search retrieved 3643 records. The previous review offered 35 studies of acupuncture for acute (3 studies), chronic (24 studies) or unclear/mixed duration low back pain (8 studies) (Furlan 2005). Together, 2876 records were found after removing the duplicates. When reviewing the titles and abstracts, there were 105 articles that required further full‐text assessment. Through the screening, we finally included 33 studies (37 articles) in this update (32 in the meta‐analysis) and two studies among them came from the previous review (Grant 1999; Leibing 2002). The detailed reasons for exclusion are given in the 'Characteristics of excluded studies' tables. We identified six ongoing studies, details of which can be found in the 'Characteristics of ongoing studies' tables.
1.
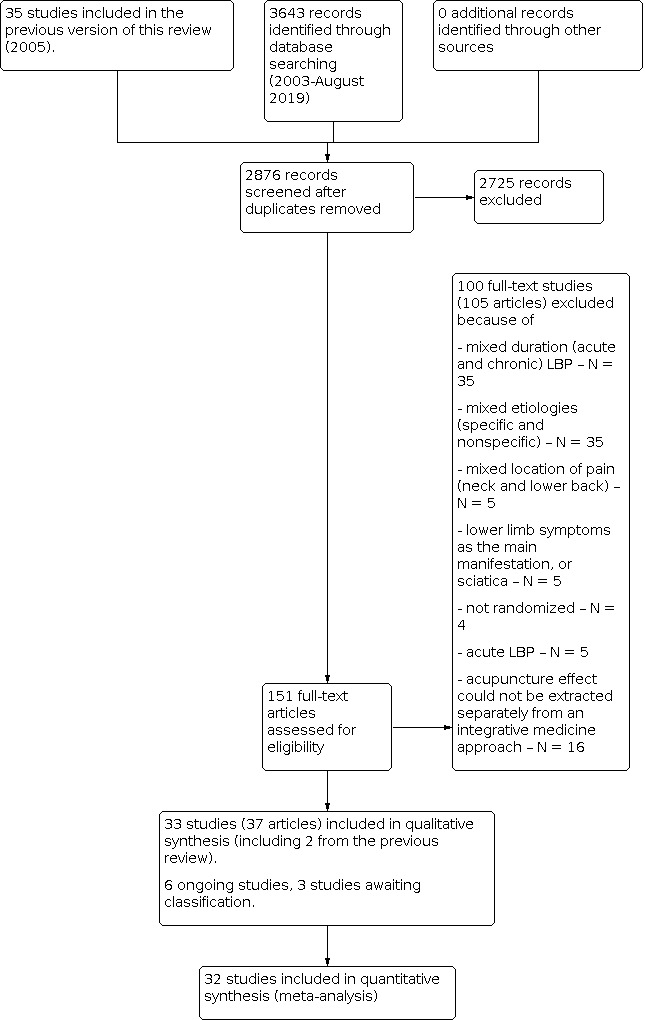
Flowchart of studies' screening
Three studies were found after this review was submitted for editorial review (Han 2018; Leite 2018; Tu 2019). Two studies would be included in the main comparison of acupuncture versus sham acupuncture (Leite 2018; Tu 2019), however the number of participants (35 in the acupuncture group and 34 in the sham group) would not make any meaningful difference to the main comparison of this review which included a total of 1483 participants. The other study (Han 2018) would not be included in any of the main comparisons. The details of these three studies are shown in the Studies awaiting classification tables. These studies will be included in the next update of this review.
Included studies
We included 33 studies (37 articles) with 8270 participants. Seven studies from Germany accounted for more than 67% of the overall population (5572 participants) (Brinkhaus 2006; Haake 2007; Leibing 2002; Molsberger 2002; Pach 2013; Weiss 2013; Witt 2006). The other studies were conducted in China (Chen 2010; Chen 2016; Li 2017; Lin 2010; Nie 2005; Pan 2005; Wang 2016a; Yuan 2016; Yun 2012a; Zhao 2012), the United Kingdom (Grant 1999; Hunter 2012; Kerr 2003; Yuan 2009), the United States (Cherkin 2009; Meng 2003), Japan (Itoh 2009; Tsukayama 2002), Spain (Pérez‐Palomares 2010), Sweden (Carlsson 2001), Italy (Cesare 2011), Korea (Cho 2013), India (Shankar 2010), Brazil (Ushinohama 2016), Lebanon (Yun 2012a), and Iran (Zaringhalam 2010). The mean age of the participants was 41.6 years, and the mean duration of LBP was 5.3 years (age and LBP duration based on 29 trials that reported the data). Females accounted for 58% of the participants (based on 31 trials that reported the data). Most trials were conducted in recruitment or outpatient clinics. Funding resources or grants from governments, institutions, or foundations were reported in 16 of 33 trials. Further details on these studies can be found in the 'Characteristics of included studies' tables. All of the participants in the included trials had chronic nonspecific LBP, without a clear and specific etiology.
The index interventions involved acupuncture and dry needling at trigger points or combined interventions involving acupuncture. Seventeen trials compared acupuncture with sham intervention, usual care, or no treatment (Brinkhaus 2006; Carlsson 2001; Cherkin 2009; Cho 2013; Haake 2007; Itoh 2009; Kerr 2003; Leibing 2002; Lin 2010; Molsberger 2002; Shankar 2010; Ushinohama 2016; Witt 2006; Yuan 2016; Yun 2012; Yun 2012a; Zaringhalam 2010). Seven trials compared acupuncture with other interventions: transcutaneous electrical nerve stimulation (TENS) (Chen 2010; Grant 1999; Itoh 2009; Tsukayama 2002; Zhao 2012), baclofen (Zaringhalam 2010), and pulsed radiofrequency therapy (Lin 2010).
Twelve trials compared two styles of acupuncture. Three trials investigated effects between acupuncture and dry needling on trigger points (Cesare 2011; Li 2017; Pérez‐Palomares 2010); two trials compared standardized acupuncture with individualized acupuncture (Cherkin 2009; Pach 2013); one trial studied the effect of high‐frequency acupuncture versus low‐frequency acupuncture (Yuan 2009); two trials studied acupuncture on local points versus acupuncture on local plus distant acupoints (Yun 2012; Yun 2012a); one trial compared rotation of the acupuncture needle versus fast‐in and fast‐out insertion of the acupuncture needle (Zhao 2012); one trial compared 0.25 mm diameter acupuncture needles with 0.9 mm diameter needles (Wang 2016a), and two trials compared acupuncture and acupuncture with heated needles (Nie 2005; Pan 2005). The four remaining trials compared acupuncture supplemented by interventions with the interventions alone. The interventions included standard therapy (Meng 2003; Weiss 2013), exercise (Hunter 2012), and botulinum toxin type A (Chen 2016). Twelve trials compared acupuncture with two controls (Brinkhaus 2006; Carlsson 2001; Haake 2007; Leibing 2002; Lin 2010; Molsberger 2002; Wang 2016a; Yuan 2016; Yun 2012; Yun 2012a; Zaringhalam 2010; Zhao 2012) and five trials (Chen 2010; Chen 2016; Cherkin 2009; Itoh 2009; Zaringhalam 2010) compared acupuncture with three controls. We extracted data into the corresponding five comparisons in the review based on what category the control belonged to.
Pain intensity was reported in 27 trials; six reported 'pain bothersomeness', a measure reflecting the annoyance caused by pain (Cherkin 2009; Nie 2005; Pan 2005; Witt 2006; Yun 2012; Yun 2012a). Back‐specific functional status was not reported in eight of the 33 trials, which instead assessed the effectiveness of therapy with regard to physical examination results, pain disability outcomes, etc. (Grant 1999; Kerr 2003; Leibing 2002; Nie 2005; Pan 2005; Shankar 2010; Ushinohama 2016; Wang 2016a). Most of the trials measured outcomes immediately after therapy sessions, or in the short or intermediate term. None of the trials measured long‐term outcomes. As baseline and absolute data on pain intensity were not provided in Ushinohama 2016, we did not incorporate the results of this study into our meta‐analysis, but described it separately. Information on the studies' participants, interventions, comparisons, and outcomes is shown in the 'Characteristics of included studies' tables.
We contacted authors of the studies to clarify information that was not reported adequately in the trials; only one author responded to our requests (Witt 2006a).
Excluded studies
We excluded a total of 100 full‐text studies (105 articles). The main reasons were studies of LBP with mixed duration of pain and LBP with various etiologies. We also excluded studies due to mixed locations of pain, lower limb symptoms as the participants' main complaints, sciatica, non‐randomisation, and acute LBP. Studies with both groups receiving acupuncture therapy were excluded because the effect of acupuncture could not be separated from the integrative approach. For example, Zhu and colleagues' study (Zhu 2016) was excluded as it compared acupuncture with acupuncture and core‐strength exercises for chronic LBP, from which the effect of acupuncture was impossible to be extracted separately. Further details can be found in the 'Characteristics of excluded studies' tables.
Risk of bias in included studies
The results of the 'Risk of bias' assessment by domain for each trial are shown in Figure 2; the results as percentages across all trials are shown in Figure 3. The specific reasons for the judgements are shown in Characteristics of included studies. Only two studies were judged as having low risk of bias (Cherkin 2009; Pach 2013), but they also had some domains with unclear risk of bias. The remaining studies had between one and three domains judged as being at high risk of bias. The main issue with the majority of the studies (29 studies, 88%) was high risk of performance bias due to lack of blinding (Brinkhaus 2006; Carlsson 2001; Cesare 2011; Chen 2010; Chen 2016; Grant 1999; Haake 2007; Hunter 2012; Itoh 2009; Kerr 2003; Leibing 2002; Li 2017; Lin 2010; Meng 2003; Nie 2005; Pan 2005; Pérez‐Palomares 2010; Shankar 2010; Tsukayama 2002; Ushinohama 2016; Wang 2016a; Weiss 2013; Witt 2006; Yuan 2009; Yuan 2016; Yun 2012; Yun 2012a; Zaringhalam 2010; Zhao 2012), or unclear risk of performance bias in the remaining four studies (Cherkin 2009; Cho 2013; Molsberger 2002; Pach 2013).
2.
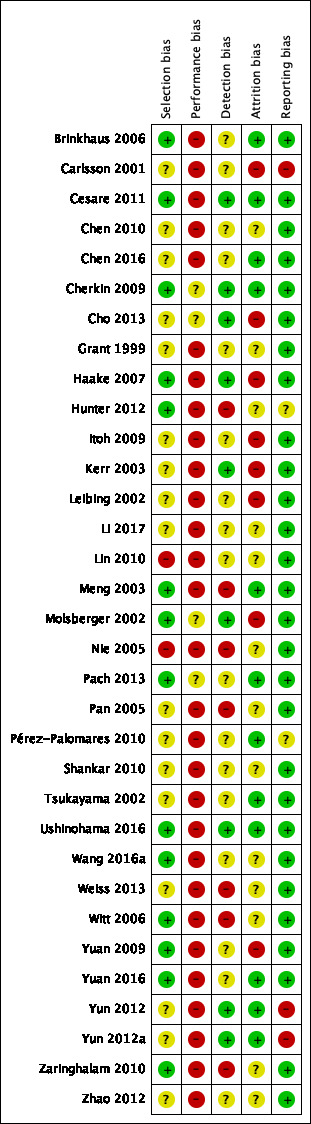
Risk of bias summary: review authors' judgements about each risk of bias item for each included study
3.
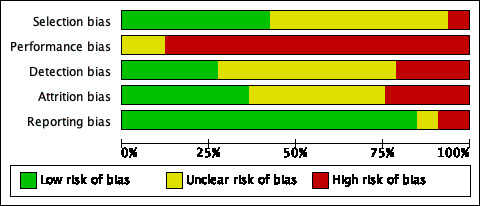
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
Allocation
We judged 14 trials to be at a low risk of selection bias because they had clear descriptions of random sequence generation and allocation concealment, and groups had similar baseline characteristics which confirmed random allocation (Brinkhaus 2006; Cesare 2011; Cherkin 2009; Haake 2007; Hunter 2012; Meng 2003; Molsberger 2002; Pach 2013; Ushinohama 2016; Wang 2016a; Witt 2006; Yuan 2009; Yuan 2016; Zaringhalam 2010). We judged 17 trials as being at unclear risk of selection bias due to not mentioning the ways for generation of the randomisation sequence and concealment methods for group allocation, or not reporting the baseline data of the groups studied (Carlsson 2001; Chen 2010; Chen 2016; Cho 2013; Grant 1999; Itoh 2009; Kerr 2003; Leibing 2002; Li 2017; Pan 2005; Pérez‐Palomares 2010; Shankar 2010; Tsukayama 2002; Weiss 2013; Yun 2012; Yun 2012a; Zhao 2012). The remaining studies we judged as being at high risk of selection bias because of baseline differences of age and gender (Lin 2010) and another trial claimed no difference in baseline data even though some key factors were found to be significantly different (Nie 2005). Overall, 40% or more of the trials had low risk of selection bias while about 50% had unclear risk, and fewer than 10% of trials had high risk of selection bias.
Blinding
None of the trials were judged as having low risk of performance bias because they all failed to use appropriate methods to mask the person delivering acupuncture. Four trials had unclear risk of performance bias (Cherkin 2009; Cho 2013; Molsberger 2002; Pach 2013). The reasons included: a certain degree of unblinding of the participants, unclear if acupuncturists were successfully blinded or not, and unclear risk in the unequal co‐interventions due to exact sessions or doses not given. Twenty‐nine trials were judged as having high risk of performance bias because the participants and care providers were not blinded and the co‐interventions were different (Brinkhaus 2006; Carlsson 2001; Cesare 2011; Chen 2010; Chen 2016; Grant 1999; Haake 2007; Hunter 2012; Itoh 2009; Kerr 2003; Leibing 2002; Li 2017; Lin 2010; Meng 2003; Nie 2005; Pan 2005; Pérez‐Palomares 2010; Shankar 2010; Tsukayama 2002; Ushinohama 2016; Wang 2016a; Weiss 2013; Witt 2006; Yuan 2009; Yuan 2016; Yun 2012; Yun 2012a; Zaringhalam 2010; Zhao 2012). The risk of performance bias across the studies was as high as 85%. The rest had unclear risk.
Nine trials were judged as having low risk of detection bias because the outcome assessors was blinded and they all used the same timing to collect the outcomes in the intervention and comparison groups (Cesare 2011; Cherkin 2009; Cho 2013; Haake 2007; Kerr 2003; Molsberger 2002; Ushinohama 2016; Yun 2012; Yun 2012a). Seventeen trials were judged as having unclear risk of detection bias as there was no clear indication of independent assessors or timing of outcomes assessment (Brinkhaus 2006; Carlsson 2001; Chen 2010; Chen 2016; Grant 1999; Itoh 2009; Leibing 2002; Li 2017; Lin 2010; Pach 2013; Pérez‐Palomares 2010; Shankar 2010; Tsukayama 2002; Wang 2016a; Yuan 2009; Yuan 2016; Zhao 2012). The remaining seven trials were judged as having high risk of detection bias due to unblinded outcome assessors (Hunter 2012; Meng 2003; Nie 2005; Pan 2005; Weiss 2013; Witt 2006; Zaringhalam 2010). The overall low risk of detection bias accounted for more than 25%, unclear risk was less than 50%, and high risk was less than 25% of studies.
Incomplete outcome data
We judged 12 trials as having low risk of attrition bias because they had acceptable dropout rates that were equal between the groups and conducted ITT (intention‐to‐treat) analyses (Brinkhaus 2006; Cesare 2011; Chen 2016; Cherkin 2009; Meng 2003; Pach 2013; Pérez‐Palomares 2010; Tsukayama 2002; Ushinohama 2016; Yuan 2016; Yun 2012; Yun 2012a). We judged 13 trials as having unclear risk of attrition bias, because of uncertainty if the dropouts were related to the treatment or if ITT analysis was properly used (Chen 2010; Grant 1999; Hunter 2012; Li 2017; Lin 2010; Nie 2005; Pan 2005; Shankar 2010; Wang 2016a; Weiss 2013; Witt 2006; Zaringhalam 2010; Zhao 2012). The remaining eight trials were judged as having high risk of detection bias because of large or unequal dropout rates between groups or ITT analysis was not used (Carlsson 2001; Cho 2013; Haake 2007; Itoh 2009; Kerr 2003; Leibing 2002; Molsberger 2002; Yuan 2009). Near equal percentages of studies had low or unclear risk of attrition bias and fewer than 25% of studies had high risk.
Selective reporting
Only seven trials had published protocols or registration records (Brinkhaus 2006; Cherkin 2009; Cho 2013; Haake 2007; Hunter 2012; Pach 2013; Zaringhalam 2010). We judged 28 trials as having low risk of reporting bias (Brinkhaus 2006; Cesare 2011; Chen 2010; Chen 2016; Cherkin 2009; Cho 2013; Grant 1999; Haake 2007; Itoh 2009; Kerr 2003; Leibing 2002; Li 2017; Lin 2010; Meng 2003; Molsberger 2002; Nie 2005; Pach 2013; Pan 2005; Shankar 2010; Tsukayama 2002; Ushinohama 2016; Wang 2016a; Weiss 2013; Witt 2006; Yuan 2009; Yuan 2016; Zaringhalam 2010; Zhao 2012). Two trials were judged as having unclear reporting bias: one did not report P values of some data (Hunter 2012) and the other did not present results for pain outcomes (Pérez‐Palomares 2010). The remaining three trials were judged as high risk because one trial reported pooling data for pain and function that broke the randomisation conditions (Carlsson 2001) and the others did not report on quality of life, but quality of life outcomes were described in the methods (Yun 2012; Yun 2012a). Around 80% of trials presented low risk of reporting bias. The remaining trials either had unclear or high risk of reporting bias
We did not assess publication bias using funnel plots as there were fewer than 10 trials pooled for each outcome.
Other potential sources of bias
We did not identify the other potential sources of bias.
Effects of interventions
See: Table 1; Table 2; Table 3
1. Acupuncture versus sham intervention
Nine trials, involving 1483 participants, examined the effect of acupuncture compared to sham intervention (Brinkhaus 2006; Carlsson 2001; Cho 2013; Haake 2007; Kerr 2003; Leibing 2002; Molsberger 2002; Ushinohama 2016; Yuan 2016). Sham interventions included superficial needling on sites next to acupoints without stimulation, non‐penetration needling on sites next to acupoints, and nonfunctioning TENS treatment on acupoints. See Table 1 for the findings for this comparison.
Primary outcomes
a. Pain intensity
1.1. Analysis.

Comparison 1: Acupuncture vs sham intervention, Outcome 1: Pain intensity (VAS)
Acupuncture decreased pain in the immediate term, but it was not clinically significant (mean difference (MD) ‐9.22, 95% confidence interval (CI) ‐13.82 to ‐4.61; 7 studies, 1403 participants; I² = 63%; low‐certainty evidence downgraded one level for risk of bias and for inconsistency, respectively). In the short term, acupuncture also decreased pain but the results were not clinically significant (MD ‐10.04, 95% CI ‐17.22 to ‐2.85; 5 studies, 1095 participants; I² = 76%; low‐certainty evidence downgraded one level for risk of bias and for inconsistency, respectively). In the intermediate term, acupuncture also decreased pain but did not have a clinically meaningful difference (MD ‐3.83, 95% CI ‐6.57 to ‐1.09; 4 studies, 1138 participants; I² = 0%; moderate‐certainty evidence downgraded one level for risk of bias). One study (Ushinohama 2016) only reported the change in pain intensity and was not included in the meta‐analyses. This study showed that ear acupuncture reduced pain more than sham at the immediate term: median change was 2, (interquartile range was 4) versus sham: median change was 1 (interquartile range was 4) (P = 0.032; 80 participants). None of the studies measured pain in the long‐term follow‐up.
b. Back‐specific functional status
1.2. Analysis.

Comparison 1: Acupuncture vs sham intervention, Outcome 2: Back‐specific function
No differences were found between acupuncture and sham acupuncture for functional improvement in the immediate term (standardized mean difference (SMD) ‐0.16, 95% CI ‐0.38 to 0.06; 5 studies, 1481 participants; I² = 72%; very low‐certainty evidence downgraded one level for risk of bias, for inconsistency, and for imprecision, respectively). A small functional improvement was found with acupuncture in the short term (SMD ‐0.38, 95% CI ‐0.69 to ‐0.07; 3 studies, 957 participants; I² = 67%; moderate‐certainty evidence downgraded one level for risk of bias), and in the intermediate term (SMD ‐0.16, 95% CI ‐0.27 to ‐0.05; 4 studies, 1373 participants; I² = 0%; moderate‐certainty evidence downgraded one level for risk of bias). When we transformed the SMD into a HFAQ score, we concluded that, in the immediate term, the sham and acupuncture groups had a score of 61.3 points (SD 20.8) and 3.33 points higher (1.25 lower to 7.90 higher); in the short term, the sham and acupuncture groups had a score of 61.3 points (SD 22.7) and 8.63 points higher (1.59 to 15.66 higher), and, in the intermediate term, the sham and acupuncture groups had a score of 62.2 points (SD 23) and 3.68 points higher (1.15 to 6.21 higher), respectively. None of the trials measured back‐related function in the long‐term follow‐up.
c. Quality of life
1.3. Analysis.

Comparison 1: Acupuncture vs sham intervention, Outcome 3: Quality of life
1.4. Analysis.

Comparison 1: Acupuncture vs sham intervention, Outcome 4: Quality of life
Due to different tools employed by the papers, the MD and SMD data were analyzed and shown separately. We found inconclusive results between acupuncture and sham acupuncture for quality of life in the immediate term (MD 4.42, 95% CI ‐1.34 to 10.18; 2 studies, 157 participants; I² = 0%; low‐certainty evidence downgraded one level for risk of bias and for imprecision, respectively). We found a small improvement in the acupuncture group in the short term (SMD 0.24, 95% CI 0.03 to 0.45; 3 studies, 1068 participants; I² = 51%; low‐certainty evidence downgraded one level for risk of bias and for inconsistency, respectively), and in the intermediate term (SMD 0.21, 95% CI 0.09 to 0.33; 3 studies, 1066 participants; I² = 0%; moderate‐certainty evidence downgraded one level for risk of bias), but the differences did not meet a clinically important change, based on the physical SF‐12 score in the representative study (Haake 2007). When we transformed the SMD into a physical SF‐12 score, we concluded that, in the short term, the sham and acupuncture groups had a score of 39.2 points (SD 9.7) and 2.33 points higher (0.29 to 4.37 higher), and, in the intermediate term, the sham and acupuncture groups had a score of 39.5 points (SD 10.1) and 2.12 points higher (0.91 to 3.33 higher). None of the trials measured quality of life in the long‐term follow‐up.
Secondary outcomes
a. Pain‐related disability
1.5. Analysis.

Comparison 1: Acupuncture vs sham intervention, Outcome 5: Pain‐related disability (PDI)
Acupuncture improved pain‐related disability in the immediate term, but the difference was not clinically important (MD ‐3.28, 95% CI ‐6.39 to ‐0.17; 2 studies, 285 participants; I² = 0%; low‐certainty evidence downgraded one level for risk of bias and for imprecision, respectively); the results were inconclusive in the intermediate term (MD ‐2.91, 95% CI ‐6.33 to 0.51; 2 studies, 269 participants; I² = 0%; very low‐certainty evidence downgraded one level for risk of bias and two levels for imprecision). No study looked at pain‐related disability for the other time points.
b. Global assessment of therapy effectiveness
1.6. Analysis.

Comparison 1: Acupuncture vs sham intervention, Outcome 6: Global assessment of therapy effectiveness (6‐point scale)
1.7. Analysis.

Comparison 1: Acupuncture vs sham intervention, Outcome 7: Global assessment of therapy effectiveness (effective number)
One study, evaluating global assessment on a 6‐point scale, found that the acupuncture group reported the therapy was more effective in the immediate term (MD ‐0.30, 95% CI ‐0.49 to ‐0.11; 1 study, 744 participants; moderate‐certainty evidence downgraded one level for risk of bias), in the short term (MD ‐0.30, 95% CI ‐0.49 to ‐0.11; 1 study, 747 participants; moderate‐certainty evidence downgraded one level for risk of bias), and in the intermediate term (MD ‐0.20, 95% CI ‐0.39 to ‐0.01; 751 participants; moderate‐certainty evidence downgraded one level for risk of bias).
Pooled results showed that acupuncture was 1.23 times more likely to improve the global assessment than sham acupuncture in the immediate term (risk ratio (RR) 1.23, 95% CI 1.04 to 1.46; 2 studies, 163 participants; I² = 0%; low‐certainty evidence downgraded one level for risk of bias and for imprecision, respectively), but not in the short term (RR 1.88, 95% CI 0.66 to 5.36; 2 studies, 141 participants; I² = 62%; very low‐certainty evidence downgraded one level for risk of bias and two levels for imprecision).
None of the studies measured global therapy effectiveness at long‐term follow‐up.
c. Adverse events
1.8. Analysis.

Comparison 1: Acupuncture vs sham intervention, Outcome 8: Adverse events
A similar incidence of adverse events was found between the acupuncture and sham acupuncture groups (RR 0.68, 95% CI 0.46 to 1.01; 4 studies, 465 participants; I² = 0%, low‐certainty evidence downgraded one level for risk of bias and for imprecision, respectively). The most common adverse events were pain at insertion points, hematoma, bleeding, worsening of LBP, and pain other than LBP (pain in leg and shoulder). No serious adverse events related to acupuncture were reported.
2. Acupuncture versus no treatment
Five trials, involving 2960 participants, examined the effect of acupuncture compared with no treatment (Brinkhaus 2006; Itoh 2009; Witt 2006; Yuan 2016; Zaringhalam 2010). No treatment included waiting lists, or participants who did not receive any specific treatment. (Table 2).
Primary outcomes
a. Pain intensity
2.1. Analysis.

Comparison 2: Acupuncture vs no treatment, Outcome 1: Pain intensity (VAS)
Acupuncture decreased pain intensity more than no treatment in the immediate term follow‐up, and this decrease was clinically relevant (MD ‐20.32, 95% CI ‐24.50 to ‐16.14; 4 studies, 366 participants; I² = 0%; moderate‐certainty evidence downgraded one level for risk of bias). At short‐term follow‐up, acupuncture also decreased pain more than no treatment; however, this difference was not clinically relevant (MD ‐10.11, 95% CI ‐16.80 to ‐3.43; 3 studies, 144 participants; I² = 0%; moderate‐certainty evidence downgraded one level for risk of bias). No study looked at pain intensity in the intermediate or long‐term follow‐up.
b. Back‐specific functional status
2.2. Analysis.

Comparison 2: Acupuncture vs no treatment, Outcome 2: Back‐specific function
Due to different tools employed by the papers, the data were analyzed in the form of MD and SMD and thus were shown separately. The acupuncture group showed a small improvement in back‐specific function in the immediate term (SMD ‐0.53, 95% CI ‐0.73 to ‐0.34; 5 studies, 2960 participants; I² = 41%; moderate‐certainty evidence downgraded one level for risk of bias), and in the short term (SMD ‐0.39, 95% CI ‐0.72 to ‐0.06; 3 studies; 144 participants; I² = 0%; moderate‐certainty evidence downgraded one level for risk of bias). When the SMD in the immediate term was transformed into a HFAQ score, the scores of the no treatment and acupuncture groups were 65.5 points (SD 21.7) and 11.50 points higher (7.38 lower to 15.84 higher); when the SMD in the short term was transformed into a ODI score, the scores of the no treatment and acupuncture groups were 40.1 points (SD 14.5) and 5.66 points lower (10.44 lower to 0.87 lower). No study looked at back‐specific function at intermediate or long‐term follow‐up.
c. Quality of life
2.3. Analysis.

Comparison 2: Acupuncture vs no treatment, Outcome 3: Quality of life
Compared with no treatment, acupuncture improved physical health‐related certainty of life more in the immediate term (MD 5.10, 95% CI 3.09 to 7.11; 2 studies, 2837 participants; I² = 58%; low‐certainty evidence downgraded one level for risk of bias and for inconsistency, respectively), and slightly improved mental health‐related quality of life in the immediate term, but the difference did not meet the predefined clinically important change (MD 1.85, 95% CI 1.06 to 2.64; 2 studies, 2837 participants; I² = 0%, moderate‐certainty evidence downgraded one level for risk of bias). No study looked at quality of life at other time points.
Secondary outcomes
a. Pain‐related disability
2.4. Analysis.

Comparison 2: Acupuncture vs no treatment, Outcome 4: Pain‐related disability (PDI, PRS)
Those in the acupuncture group had a medium improvement in pain‐related disability, compared with those in the no treatment group, in the immediate term (SMD ‐0.56, 95% CI ‐0.64 to ‐0.49; 2 studies, 2937 participants; I² = 0%; moderate‐certainty evidence downgraded one level for risk of bias). No study looked at pain‐related disability at any other time points.
b. Global assessment of therapy effectiveness
No study evaluated global assessment outcomes for this comparison.
c. Adverse events
No study reported adverse events for this comparison.
3. Acupuncture versus usual care
Eight trials, involving 1633 participants, examined the effect of acupuncture compared with usual care (Cherkin 2009; Haake 2007; Leibing 2002; Lin 2010; Molsberger 2002; Shankar 2010; Yun 2012; Yun 2012a). Usual care included treatment delivered by primary care healthcare providers using a variety of medications, physiotherapy, and exercises (Table 3).
Primary outcomes
a. Pain intensity
3.1. Analysis.

Comparison 3: Acupuncture vs usual care, Outcome 1: Pain intensity (VAS)
Those in the acupuncture group had a reduction in pain intensity in the immediate term, which was not clinically significant (MD ‐10.26, 95% CI ‐17.11 to ‐3.40; 5 studies, 1054 participants; I² = 77%; low‐certainty evidence downgraded one level for risk of bias and for inconsistency, respectively). In the short term, the results were inconclusive between the two groups (MD ‐18.78, 95% CI ‐37.97 to 0.41; 2 studies, 817 participants; I² = 95%; very low‐certainty evidence downgraded one level for risk of bias, for inconsistency, and for imprecision, respectively). In the intermediate term, the acupuncture group demonstrated a reduction in pain intensity, which was not clinically significant (MD ‐12.30, 95% CI ‐15.28 to ‐9.32; 2 studies, 804 participants; I² = 0%; moderate‐certainty evidence downgraded one level for risk of bias). None of the trials measured pain in the long‐term follow‐up (Table 3).
b. Back‐specific functional status
(Analysis 3.2 and Analysis 3.3)
3.2. Analysis.

Comparison 3: Acupuncture vs usual care, Outcome 2: Back‐specific function
3.3. Analysis.

Comparison 3: Acupuncture vs usual care, Outcome 3: Back‐specific function
As different tools were used, the data were analyzed in the form of MD and SMD and thus were shown in separate figures (Analysis 3.2 and Analysis 3.3). Those in the acupuncture group had a small improvement in back‐specific function in the immediate term (SMD ‐0.47, 95% CI ‐0.77 to ‐0.17; 5 studies, 1381 participants; I² = 83%; low‐certainty evidence downgraded one level for risk of bias and for inconsistency, respectively; Analysis 3.3). In the short term, those in the acupuncture group demonstrated improved back‐specific function (MD 9.40, 95% CI 6.15 CI to 12.65; 1 study, 734 participants; moderate‐certainty evidence downgraded one level for risk of bias; Analysis 3.2); and in the intermediate term (SMD ‐0.44, 95% CI ‐0.55 to ‐0.33; 4 studies, 1310 participants; I² = 0%; moderate‐certainty evidence downgraded one level for risk of bias; Analysis 3.3). When we transformed the immediate‐time SMD into a HFAQ score, we concluded that the usual care group had a score of 56.3 points (SD 20.8), and, in the acupuncture group, this score was 9.78 points higher (3.54 to 16.02 higher). At intermediate term, the usual care group had a score of 55.7 points (SD 22.7) and the acupuncture group score was 9.99 points higher (7.49 to 12.49 higher). None of the studies measured the effect in the long term.
c. Quality of life
3.4. Analysis.

Comparison 3: Acupuncture vs usual care, Outcome 4: Quality of life
The results were inconclusive for quality of life in the immediate term (MD 0.20, 95% CI ‐5.82 to 6.22; 1 study, 71 participants; low‐certainty evidence downgraded one level for risk of bias and for imprecision, respectively). Those in the acupuncture group demonstrated improved physical health‐related quality of life in the short term (MD 4.20, 95% CI 2.82 to 5.58; 1 study, 731 participants; moderate‐certainty evidence downgraded one level for risk of bias), and a smaller improvement in mental health‐related quality of life in the short term, which did not meet the predefined clinically important change (MD 1.90, 95% CI 0.25 to 3.55; 1 study, 731 participants; moderate‐certainty evidence downgraded one level for risk of bias). Those in the acupuncture group had more improvement in physical health‐related quality of life in the intermediate term (MD 5.80, 95% CI 4.36 to 7.24; 1 study, 737 participants; moderate‐certainty evidence downgraded one level for risk of bias), but results were inconclusive for mental health‐related quality of life in the intermediate term (MD 1.50, 95% CI ‐0.15 to 3.15; 1 study, 737 participants; moderate‐certainty evidence downgraded one level for risk of bias). None of the studies measured quality of life in the long‐term follow‐up.
Secondary outcomes
a. Pain‐related disability
3.5. Analysis.

Comparison 3: Acupuncture vs usual care, Outcome 5: Pain‐related disability (PDI)
Those in the acupuncture group demonstrated reduced pain‐related disability over usual care in the immediate term (MD ‐11.00, 95% CI ‐17.18 to ‐4.82; 1 study, 74 participants; low‐certainty evidence downgraded one level for risk of bias and for imprecision, respectively), but not in the intermediate term (MD ‐6.40, 95% CI ‐13.10 to 0.30; 1 study, 63 participants; very low‐certainty evidence downgraded one level for risk of bias and two levels for imprecision). No study looked at pain‐related disability in the short or long term.
b. Global assessment of therapy effectiveness
3.6. Analysis.

Comparison 3: Acupuncture vs usual care, Outcome 6: Global assessment of therapy effectiveness (6‐point scale)
3.7. Analysis.

Comparison 3: Acupuncture vs usual care, Outcome 7: Global assessment of therapy effectiveness (effective number)
One study, evaluating global assessment on a 6‐point scale, found that the acupuncture group reported the therapy more effective in the short term (MD ‐0.30, 95% CI ‐0.50 to ‐0.10; 1 study, 730 participants; moderate‐certainty evidence downgraded one level for risk of bias; Analysis 3.6), and in the intermediate term (MD ‐0.70, 95% CI ‐1.04 to ‐0.36; 1 study, 738 participants; moderate‐certainty evidence downgraded one level for risk of bias; Analysis 3.6).
Pooled results showed acupuncture was 1.41 times more likely to improve the global assessment than usual care in the immediate term (RR 1.41, 95% CI 1.18 to 1.67; 3 studies, 396 participants; I² = 0%; moderate‐certainty evidence downgraded one level for risk of bias; Analysis 3.7), 2.47 times more likely in the short term (RR 2.47, 95% CI 1.46 to 4.17; 1 study, 86 participants; low‐certainty evidence downgraded one level for risk of bias and for imprecision, respectively; Analysis 3.7), and 1.30 times more likely in the intermediate term (RR 1.30, 95% CI 1.08 to 1.55; 2 studies, 279 participants; I² = 0%; low‐certainty evidence downgraded one level for risk of bias and for imprecision, respectively; Analysis 3.7). None of the studies looked at therapy effectiveness in the long term.
c. Adverse events
3.8. Analysis.

Comparison 3: Acupuncture vs usual care, Outcome 8: Adverse events
One trial reported inconclusive results between groups for adverse events (RR 3.34, 95% CI 0.36 to 30.68; participants = 74; 1 study, 74 participants; low‐certainty evidence downgraded one level for risk of bias and for imprecision, respectively). The adverse events reported were pain (n = 2) and circulation problems (n = 1) in the acupuncture group, and persisting pain in the usual care group (n = 1).
4. Acupuncture versus another intervention
Seven trials, involving 475 participants, examined the effects of acupuncture compared with another intervention: TENS (Chen 2010; Grant 1999; Itoh 2009; Tsukayama 2002; Zhao 2012), baclofen (Zaringhalam 2010), and pulsed radiofrequency therapy (Lin 2010).
4.1 Acupuncture versus TENS
Primary outcomes
a. Pain intensity
4.1. Analysis.

Comparison 4: Acupuncture vs another intervention, Outcome 1: Acupuncture vs TENS
The results were inconclusive for reduction of pain intensity between the acupuncture and TENS groups in the immediate term (MD ‐8.26, 95% CI ‐19.03 to 2.51; participants = 196; 5 studies; I² = 61%, very low‐certainty evidence downgraded one level for risk of bias and for inconsistency, respectively, and two levels for imprecision). Acupuncture reduced pain intensity more than TENS in the short term, although the reduction was not clinically significant (MD ‐9.51, 95% CI ‐19.50 to 0.49; participants = 116; 3 studies; I² = 0%; low‐certainty evidence downgraded one level for risk of bias and imprecision, respectively). None of the studies looked at pain in the intermediate or long term.
b. Back‐specific functional status
4.2. Analysis.

Comparison 4: Acupuncture vs another intervention, Outcome 2: Acupuncture vs TENS
The MD and SMD data were analyzed and shown in separate figures.The results were inconclusive for back‐specific function between the acupuncture and TENS groups in the immediate term (SMD ‐0.83, 95% CI ‐1.91 to 0.24; 3 studies, 121 participants; I² = 85%; very low‐certainty evidence downgraded one level for risk of bias and for inconsistency, respectively, and two levels for imprecision; Analysis 4.2), and in the short term (MD ‐0.49, 95% CI ‐2.61 to 1.63; 2 studies, 61 participants; I² = 0%; very low‐certainty evidence downgraded one level for risk of bias and two levels for imprecision; Analysis 4.1). We then transformed this SMD into a RMDQ score in the immediate term, finding that the TENS group had a score of 6.6 points (SD 3.4) and the acupuncture group had a score 2.82 points lower (6.49 lower to 0.82 higher). None of the studies measured back‐specific function at intermediate or long term.
c. Quality of life
No study assessed quality of life for this comparison.
Secondary outcomes
a. Pain‐related disability
The results were inconclusive between the acupuncture and TENS groups for pain‐related disability in the immediate term (MD ‐2.80, 95% CI ‐5.81 to 0.21; 1 study, 19 participants; very low‐certainty evidence downgraded one level for risk of bias and two levels for imprecision; Analysis 4.1). None of the studies measured pain‐related disability at other time points.
b. Global assessment of therapy effectiveness
One trial (N = 60) measured global assessment at four levels (marked effective, effective, improved, no change). The acupuncture group reported therapy was more effective than the TENS (electroacupuncture) group in the immediate term (Table 6). None of the studies measured global assessment of therapy effectiveness at any other time points.
3. Comparison 4. Acupuncture versus another intervention. Outcome: global measurement.
| Study | Assessed term | Acupuncture | Another intervention | P value |
| Zhao 2012 | (N = 30) | TENS (N = 30) | ||
| Measured immediately after | Very effective | 9 | 5 | |
| Effective | 14 | 9 | ||
| Improved | 6 | 14 | ||
| No change | 1 | 2 | z = 4.57; P < 0.05 |
TENS = Electroacupuncture
c. Adverse events
The acupuncture group was found to have a similar incidence of adverse events to the TENS group (RR 1.22, 95% CI 0.48 to 3.13; 2 studies, 76 participants; I² = 0%; very low‐certainty evidence downgraded one level for risk of bias and two levels for imprecision; Analysis 4.3).
4.3. Analysis.

Comparison 4: Acupuncture vs another intervention, Outcome 3: Acupuncture vs TENS
4.2. Acupuncture versus baclofen
Primary outcomes
a. Pain intensity
A single trial (Zaringhalam 2010) reported that acupuncture reduced pain intensity more than baclofen in the immediate term (MD ‐14.90, 95% CI ‐27.77 to ‐2.03; 1 study, 40 participants; low‐certainty evidence downgraded one level for risk of bias and for imprecision, respectively; Analysis 4.4), and in the short term (MD ‐13.60, 95% CI ‐22.56 to ‐4.64; 1 study, 40 participants; low‐certainty evidence downgraded one level for risk of bias and for imprecision, respectively; Analysis 4.4); the results were not clinically significant. The trial did not measure pain intensity in the intermediate or long term.
4.4. Analysis.

Comparison 4: Acupuncture vs another intervention, Outcome 4: Acupuncture vs baclofen
b. Back‐specific functional status
Acupuncture improved back‐specific function more than baclofen in the immediate term (MD ‐2.40, 95% CI ‐4.49 to ‐0.31; 1 study, 40 participants; low‐certainty evidence downgraded one level for risk of bias and for imprecision, respectively; Analysis 4.4) and in the short term (MD ‐2.30, 95% CI ‐4.55 to ‐0.05; 1 study, 40 participants; low‐certainty evidence downgraded one level for risk of bias and for imprecision, respectively; Analysis 4.4); however, the results did not meet the criteria of clinically important change. The trial (Zaringhalam 2010) did not measure back‐specific function in the intermediate or long term.
c. Quality of life
The study did not measure quality of life.
Secondary outcomes
The only trial included in this comparison did not measure any of the secondary outcomes of interest for this review (pain‐related disability, global assessment of therapy effectiveness, adverse events).
4.3 Acupuncture versus pulsed radiofrequency therapy
Primary outcomes
a. Pain intensity
The results of one trial (Lin 2010) did not show differences for pain intensity in the immediate term between acupuncture and pulsed radiofrequency therapy (MD ‐0.30, 95% CI ‐1.97 to 1.37; 1 study, 65 participants; very low‐certainty evidence downgraded one level for risk of bias and two levels for imprecision; Analysis 4.5). The study did not measure pain intensity at other time points.
4.5. Analysis.

Comparison 4: Acupuncture vs another intervention, Outcome 5: Acupuncture vs pulsed radiofrequency therapy (PRT)
b. Back‐specific functional status
The trial did not find differences for back‐specific function in the immediate term between the two therapies (MD 3.40, 95% CI ‐11.82 to 18.62; 1 study, 65 participants; very low‐certainty evidence downgraded one level for risk of bias and two levels for imprecision; Analysis 4.5). The study (Lin 2010) did not measure function at other time points.
c. Quality of life
The trial did not find differences for quality of life in the immediate term between the two therapies (MD 4.20, 95% CI ‐1.91 to 10.31; 1 study, 65 participants; very low‐certainty evidence downgraded one level for risk of bias and two levels for imprecision; Analysis 4.5). The study (Lin 2010) did not measure quality of life at other time points.
Secondary outcomes
The study did not assess the secondary outcomes for this comparison.
5. Acupuncture versus another technique of acupuncture
Twelve trials, involving 1772 participants, examined the effects of one technique of acupuncture compared to another (Cesare 2011; Cherkin 2009; Li 2017; Nie 2005; Pach 2013; Pan 2005; Pérez‐Palomares 2010; Wang 2016a; Yuan 2009; Yun 2012; Yun 2012a; Zhao 2012). Three trials compared acupuncture with dry needling on trigger points (Cesare 2011; Li 2017; Pérez‐Palomares 2010), two trials compared standardized acupuncture with individualized acupuncture (Cherkin 2009; Pach 2013), one trial studied the effect of high‐frequency acupuncture versus low‐frequency acupuncture (Yuan 2009), two trials studied acupuncture on local points versus acupuncture on local plus distant acupoints (Yun 2012; Yun 2012a), one trial compared rotation of the acupuncture needle versus fast‐in and fast‐out insertion of the acupuncture needle (Zhao 2012), one trial compared 0.25 mm diameter acupuncture needles with 0.9 mm diameter needles (Wang 2016a), and two trials compared acupuncture and acupuncture with heated needles (Nie 2005; Pan 2005).
5.1. Acupuncture versus dry needling on trigger points
Primary outcomes
a. Pain intensity
Acupuncture did not have more pain reduction than drying needling on trigger points in the immediate term (MD 0.45, 95% CI ‐0.44 to 1.33; 3 studies, 246 participants; I² = 90%; very low‐certainty evidence downgraded one level for risk of bias and two levels for imprecision and inconsistency respectively; Analysis 5.1). The result did not change when we performed a subgroup analysis without Cesare 2011 which reported extremely small SDs of VAS pain intensity (MD 0.83, 95% CI ‐0.44 to 2.10; participants = 185; studies = 2; I² = 86%; very low‐certainty evidence downgraded two levels for imprecision and inconsistency respectively; Analysis 5.2). Acupuncture reduced pain in the short term, although it was not clinically significant comparing with drying needling on trigger points (MD ‐1.20, 95% CI ‐1.32 to ‐1.08; 1 study, 60 participants; low‐certainty evidence downgraded one level for risk of bias and for imprecision, respectively; Analysis 5.1). Acupuncture was less effective than dry needling in reducing pain in the intermediate term (MD 1.40, 95% CI 0.59 to 2.21; 1 study, 60 participants; very low‐certainty evidence; Analysis 5.1). No studies measured pain in the long term. We did sensitivity analysis by excluding one paper due to very small sd value, the heterogeneity is lower but still high. two papers had opposite conclusion.
5.1. Analysis.

Comparison 5: Acupuncture vs another acupuncture technique, Outcome 1: Acupuncture vs dry needling on trigger points
5.2. Analysis.

Comparison 5: Acupuncture vs another acupuncture technique, Outcome 2: Acupuncture vs dry needling on trigger points
b. Back‐specific functional status
The data were analyzed and shown separately for SMD (Analysis 5.1) and MD (Analysis 5.2). The results were inconclusive between the two interventions for back‐specific function in the immediate term (SMD 0.32, 95% CI ‐0.63 to 1.27; 2 studies, 121 participants; I² = 85%; very low‐certainty evidence downgraded one level for risk of bias and two levels for imprecision and inconsistency respectively; Analysis 5.2), and acupuncture improved back‐specific function in the short term, but it was not a clinically important difference (MD ‐1.08, 95% CI ‐1.34 to ‐0.82; 1 study, 60 participants; low‐certainty evidence downgraded one level for risk of bias and for imprecision, respectively; Analysis 5.1). However, acupuncture was less effective than dry needling in improving back‐specific function in the intermediate term (MD 5.02, 95% CI 2.05 to 7.99; 1 study, 60 participants; low‐certainty evidence; Analysis 5.1). When the SMD data in the immediate term was transformed into a RMDQ score, the dry needling group had a score of 7.68 points (SD 5.10) and the acupuncture group had 1.63 points lower (3.21 lower to 6.48 higher). No studies measured back‐specific function in the long term.
c. Quality of life
No study measured quality of life.
Secondary outcomes
a. Pain‐related disability
No study measured pain‐related disability.
b. Global assessment of therapy effectiveness
Those in the acupuncture group had less therapy effectiveness than those who received dry needling on trigger points immediately after the treatment, but not in the intermediate term (Table 7). None of the studies measured this outcome in the short or long term.
4. Comparison 5. Acupuncture versus another technique of acupuncture. Outcome: global measurement.
| Study | Assessed term | Acupuncture | Another technique of acupuncture | P value |
| Li 2017 | (N = 30) | Dry needling on trigger points (N = 30) | ||
| Measured immediately after | Cure | 7 | 8 | |
| Effective | 7 | 12 | ||
| Less effective | 13 | 8 | ||
| No change | 3 | 2 | P < 0.05 | |
| Measured in the intermediate term | Cure | 7 | 9 | |
| Effective | 8 | 11 | ||
| Less effective | 12 | 8 | ||
| No change | 3 | 2 | P > 0.05 | |
| Nie 2005 | (N = 30) | Heated needles (N = 30) | ||
| Measured immediately after | Cure | 13 | 18 | |
| Effective | 6 | 10 | ||
| No change | 11 | 2 | P < 0.05 | |
| Pan 2005 | (N = 38) | Heated needles (N = 35) | ||
| Measured immediately after | Cure | 8 | 16 | |
| Effective | 18 | 19 | ||
| No change | 6 | 4 | P > 0.05 (based on total rate of effectiveness) |
c. Adverse events
One study reported five adverse events of slight neck pain in the acupuncture group but none in the dry needling group (RR 9.71, 95% CI 0.56 to 168.32; 1 study, 62 participants; very low‐certainty evidence downgraded one level for risk of bias and two levels for imprecision; Analysis 5.3).
5.3. Analysis.

Comparison 5: Acupuncture vs another acupuncture technique, Outcome 3: Acupuncture vs dry needling on trigger points
5.2. Standardized acupuncture versus individualized acupuncture
Primary outcomes
a. Pain intensity
The results between the two acupuncture techniques were inconclusive for pain in the short term (MD ‐1.30, 95% CI ‐9.49 to 6.89; 1 study, 144 participants; low‐certainty evidence downgraded two levels for imprecision; Analysis 5.4), and in the intermediate term (MD ‐3.20, 95% CI ‐11.83 to 5.43; 1 study, 139 participants; low‐certainty evidence downgraded two levels for imprecision; Analysis 5.4). None of the studies measured pain in the immediate or long term.
5.4. Analysis.

Comparison 5: Acupuncture vs another acupuncture technique, Outcome 4: Standard acupuncture vs individualized acupuncture
b. Back‐specific functional status
The MD and SMD data were analyzed and shown in separate figures (Analysis 5.4 and .Analysis 5.5). The results between the two acupuncture techniques were inconclusive for back‐specific function in the immediate term (MD ‐0.10, 95% CI ‐1.35 to 1.15; 1 study, 299 participants; low‐certainty evidence downgraded two levels for imprecision; Analysis 5.4), in the short term (MD 1.70, 95% CI ‐4.34 to 7.74; 1 study, 144 participants; low‐certainty evidence downgraded two levels for imprecision; Analysis 5.4), and in the intermediate term (SMD 0.03, 95% CI ‐0.16 to 0.22; participants = 427; studies = 2; I2 = 0%; moderate‐certainty evidence downgraded one level for imprecision; Analysis 5.5). When the SMD data in the intermediate term was transformed into a RMDQ score, the dry needling group had a score of 6.00 points (SD 5.4) and the acupuncture group had 0.16 points lower (0.86 lower to 1.19 higher). None of the studies measured back‐specific function in the long term.
5.5. Analysis.

Comparison 5: Acupuncture vs another acupuncture technique, Outcome 5: Standard acupuncture vs individualized acupuncture
c. Quality of life
The results between the two acupuncture techniques were inconclusive in the short term for both physical health‐related quality of life (MD ‐0.60, 95% CI ‐3.72 to 2.52; 1 study, 144 participants; low‐certainty evidence downgraded two levels for imprecision; Analysis 5.4), and mental health‐related quality of life (MD 0.50, 95% CI ‐3.14 to 4.14; 1 study, 144 participants; low‐certainty evidence downgraded two levels for imprecision; Analysis 5.4), and in the intermediate term for physical health‐related quality of life (MD ‐1.40, 95% CI ‐4.62 to 1.82; 1 study, 139 participants; low‐certainty evidence downgraded two levels for imprecision; Analysis 5.4), and mental health‐related quality of life (MD 1.90, 95% CI ‐2.06 to 5.86; 1 study, 139 participants; low‐certainty evidence downgraded two levels for imprecision; Analysis 5.4). None of the studies measured quality of life in the immediate or long term.
Secondary outcomes
a. Pain‐related disability
The results between the two acupuncture techniques were inconclusive in the short term for the number of sick leave days (MD 0.30, 95% CI ‐3.96 to 4.56; 1 study, 144 participants; low‐certainty evidence downgraded two levels for imprecision; Analysis 5.4) and in the intermediate term (MD ‐0.70, 95% CI ‐8.49 to 7.09; 1 study, 139 participants; low‐certainty evidence downgraded two levels for imprecision; Analysis 5.4). None of the studies measured pain‐related disability in the immediate or long term.
b. Global assessment of therapy effectiveness
None of the studies measured this outcome.
c. Adverse events
Six adverse events, pain, dizziness and back spasms, were reported by each of the acupuncture technique groups (RR 0.97, 95% CI 0.32 to 2.93; 1 study, 299 participants; low‐certainty evidence downgraded two levels for imprecision; Analysis 5.6).
5.6. Analysis.

Comparison 5: Acupuncture vs another acupuncture technique, Outcome 6: Standard acupuncture vs individualized acupuncture
5.3. High‐frequency acupuncture versus low‐frequency acupuncture
Primary outcomes
a. Pain intensity
The results from one study (Cesare 2011) did not report differences between the high‐frequency and low‐frequency acupuncture groups for pain in the immediate term (MD ‐0.20, 95% CI ‐1.21 to 0.81; 1 study, 29 participants; very low‐certainty evidence downgraded one level for risk of bias and two levels for imprecision; Analysis 5.7), in the short term (MD 0.25, 95% CI ‐0.64 to 1.14; 1 study, 29 participants; very low‐certainty evidence downgraded one level for risk of bias and two levels for imprecision; Analysis 5.7), and in the intermediate term (MD 0.06, 95% CI ‐1.12 to 1.24; 1 study, 21 participants; very low‐certainty evidence downgraded one level for risk of bias and two levels for imprecision; Analysis 5.7). None of the studies measured pain in the long term.
5.7. Analysis.

Comparison 5: Acupuncture vs another acupuncture technique, Outcome 7: High‐frequency acupuncture vs low‐frequency acupuncture
b. Back‐specific functional status
The same study (Cesare 2011) did not report differences either for back‐specific function in the immediate term between the two therapies (MD ‐0.57, 95% CI ‐3.60 to 2.46; 1 study, 29 participants; very low‐certainty evidence downgraded one level for risk of bias and two levels for imprecision; Analysis 5.7), in the short term (MD 1.20, 95% CI ‐0.79 to 3.19; 1 study, 29 participants; very low‐certainty evidence downgraded one level for risk of bias and two levels for imprecision; Analysis 5.7), and in the intermediate term (MD 0.30, 95% CI ‐0.88 to 1.48; 1 study, 21 participants; very low‐certainty evidence downgraded one level for risk of bias and two levels for imprecision; Analysis 5.7). None of the studies measured back‐specific function in the long term.
c. Quality of life
This study did not measure quality of life.
Secondary outcomes
a. Pain‐related disability
The study did not measure this outcome.
b. Global assessment of therapy effectiveness
The study did not measure this outcome.
c. Adverse events
The results between techniques were inconclusive for adverse events (RR 1.47, 95% CI 0.80 to 2.69; 1 study, 29 participants; very low‐certainty evidence downgraded one level for risk of bias and two levels for imprecision; Analysis 5.8). The participants of both of the groups reported a similar number of minor bleeding, pain, tiredness, dizziness, twitch of muscle, stuck needle, headache, redness and dry mouth events.
5.8. Analysis.

Comparison 5: Acupuncture vs another acupuncture technique, Outcome 8: High‐frequency acupuncture vs low‐frequency acupuncture
5.4. Acupuncture (local acupoints) compared to acupuncture (local + distant acupoints)
Primary outcomes
a. Pain intensity
None of the studies measured pain.
b. Back‐specific functional status
Acupuncture in local acupoints provided less improvement in back‐specific function than acupuncture in both local and distant acupoints together in the immediate term (MD 0.90, 95% CI 0.44 to 1.36; 2 studies, 289 participants; I² = 0%; low‐certainty evidence downgraded one level for risk of bias and for imprecision, respectively; Analysis 5.9), and in the intermediate term (MD 1.15, 95% CI 0.74 to 1.57; 2 studies, 289 participants; I² = 0%; low‐certainty evidence downgraded one level for risk of bias and for imprecision, respectively;Analysis 5.9). No study measured function in the short and long term.
5.9. Analysis.

Comparison 5: Acupuncture vs another acupuncture technique, Outcome 9: Acupuncture (local acupoints) vs acupuncture (local + distant acupoints)
c. Quality of life
No study measured quality of life.
Secondary outcomes
a. Pain‐related disability
None of the studies measured this outcome.
b. Global assessment of therapy effectiveness
Results were inconclusive from two studies (Cherkin 2009; Pach 2013) between the two techniques for global assessment of therapy effectiveness in the immediate term (RR 0.92, 95% CI 0.77 to 1.10; 2 studies, 289 participants; I² = 0%, very low‐certainty evidence downgraded one level for risk of bias and two levels for imprecision; Analysis 5.10), and in the intermediate term (RR 0.89, 95% CI 0.78 to 1.01; 2 studies, 289 participants; I² = 0%; very low‐certainty evidence downgraded one level for risk of bias and two levels for imprecision; Analysis 5.10). None of the studies measured this outcome at the short and long term.
5.10. Analysis.

Comparison 5: Acupuncture vs another acupuncture technique, Outcome 10: Acupuncture (local acupoints) vs acupuncture (local + distant acupoints)
c. Adverse events
None of the studies measured adverse events.
5.5. Acupuncture (rotation of needle) versus acupuncture (fast‐in and fast‐out)
Primary outcomes
a. Pain intensity
One trial (Zhao 2012) found that rotation of acupuncture needles reduced pain more than a fast‐in and fast‐out technique in the immediate term, but it was not clinically significant (MD ‐1.00, 95% CI ‐1.94 to ‐0.06; 1 study, 60 participants; low‐certainty evidence downgraded one level for risk of bias and for imprecision, respectively; Analysis 5.11). The trial did not measure pain at other time points.
5.11. Analysis.

Comparison 5: Acupuncture vs another acupuncture technique, Outcome 11: Acupuncture (rotation) vs acupuncture (fast‐in & fast‐out)
b. Back‐specific functional status
The same study (Zhao 2012) showed that rotation of acupuncture needles improved back‐specific function more than a fast‐in and fast‐out technique in the immediate term (MD ‐3.50, 95% CI ‐4.82 to ‐2.18; 1 study, 60 participants; low‐certainty evidence downgraded one level for risk of bias and for imprecision, respectively; Analysis 5.11). The trial did not measure function at the short, intermediate, or long term.
c. Quality of life
The study did not measure quality of life.
Secondary outcomes
This study did not assess the secondary outcomes for this comparison.
5.6. Acupuncture using 0.25 mm diameter needles versus 0.9 mm diameter needles
Primary outcomes
a. Pain intensity
One trial (Wang 2016a) found that acupuncture using a needle of 0.25 mm diameter reduced pain more than acupuncture using a needle of 0.9 mm diameter in the immediate term, but it was not clinically significant (MD ‐1.46, 95% CI ‐2.81 to ‐0.11; 1 study, 31 participants; low‐certainty evidence downgraded one level for risk of bias and for imprecision, respectively; Analysis 5.12). The thinner needle resulted in more clinically meaningful pain relief in the short term (MD 1.99, 95% CI 0.56 to 3.42; 1 study, 31 participants; low‐certainty evidence downgraded one level for risk of bias and for imprecision, respectively; Analysis 5.12). No trial measured pain in the intermediate or long term.
5.12. Analysis.

Comparison 5: Acupuncture vs another acupuncture technique, Outcome 12: Acupuncture (0.25 mm diameter) vs. acupuncture (0.9 mm diameter)
b. Back‐specific functional status
No studies measured back‐specific function.
c. Quality of life
The results from acupuncture with different sized needles were inconclusive for quality of life in the immediate (MD 6.22, 95% CI ‐1.54 to 13.98; 1 study, 31 participants; very low‐certainty evidence downgraded one level for risk of bias and two levels for imprecision, respectively; Analysis 5.12), and short term (MD ‐5.27, 95% CI ‐11.27 to 0.73; 1 study, 31 participants; very low‐certainty evidence downgraded one level for risk of bias and two levels for imprecision, respectively; Analysis 5.12). The study (Wang 2016a) did not measure quality of life in the intermediate or long term.
Secondary outcomes
The study did not assess the secondary outcomes for this comparison.
5.7. Acupuncture versus acupuncture using heated needles
Two trials (Nie 2005; Pan 2005) examined the effects of acupuncture versus acupuncture with heated needles. They did not measure any of the primary outcomes of interest (i.e. pain intensity, back‐specific functional status), nor did they measure two of the three secondary outcomes of interest (pain‐related disability, adverse events).
One trial (Nie 2005) reported that those who received acupuncture with heated needles reported a higher global assessment of therapy effectiveness in the immediate term than those who received acupuncture alone. The other trial (Pan 2005) reported inconclusive results between the two groups in the immediate term (Table 7). Neither trial measured the outcome at other time points.
6. Acupuncture plus intervention versus intervention alone
Four trials, involving 277 participants, compared acupuncture supplemented by an intervention to the interventions alone. The interventions included standard therapy (Meng 2003; Weiss 2013), exercise (Hunter 2012), and botulinum toxin type A (Chen 2016).
6.1. Acupuncture plus standard therapy versus standard therapy
Primary outcomes
a. Pain intensity
There was a small improvement in pain intensity in those who received acupuncture plus standard therapy over those who received standard therapy alone in the immediate term (SMD ‐0.41, 95% CI ‐0.70 to ‐0.12; 2 studies, 187 participants; I² = 0%; low‐certainty evidence downgraded one level for risk of bias and for imprecision, respectively; Analysis 6.1), and in the short term (SMD ‐0.49, 95% CI ‐0.78 to ‐0.20; 2 studies, 187 participants; I² = 0%; low‐certainty evidence downgraded one level for risk of bias and for imprecision, respectively; Analysis 6.1). When we transformed the SMD data into a SF‐36 bodily pain score, we concluded that, in the immediate term, the standard therapy had a score of 58.60 points (SD 20) and the acupuncture plus standard therapy group had a score 8.20 points higher (14.00 higher to 2.40 higher). In the short term, the standard therapy had a score of 39.80 points (SD 20.00) and the acupuncture plus standard therapy group had a score 9.80 points higher (15.60 higher to 4.00 higher).
6.1. Analysis.

Comparison 6: Acupuncture plus intervention vs intervention alone, Outcome 1: Acupuncture + standard therapy vs standard therapy
b. Back‐specific functional status
There was a small improvement in back‐specific function in those who received acupuncture plus standard therapy over those who received standard therapy alone in the immediate term (SMD ‐0.34, 95% CI ‐0.63 to ‐0.05; 2 studies, 187 participants; I² = 0%, low‐certainty evidence downgraded one level for risk of bias and for imprecision, respectively; Analysis 6.1), and a moderate improvement in the short term (SMD ‐0.51, 95% CI ‐0.80 to ‐0.22; 2 studies, 187 participants; I² = 0%; low‐certainty evidence downgraded one level for risk of bias and for imprecision, respectively; Analysis 6.1). The SMD data was then transformed into a SF‐36 physical score. In the immediate term, the standard therapy had a score of 76.20 points (SD 19.00) and the acupuncture plus standard therapy group had a score 6.46 points higher (0.95 to 11.97 higher). In the short term, the standard therapy had a score of 58.00 points (SD 19.00) and the acupuncture plus standard therapy group had a score 9.69 points lower (15.20 lower to 4.18 higher).
c. Quality of life
Acupuncture plus standard therapy improved quality of life more than standard therapy alone in the immediate term (MD 8.20, 95% CI 3.09 to 13.31; 1 study, 143 participants; low‐certainty evidence downgraded one level for risk of bias and for imprecision, respectively; Analysis 6.2), and in the short term (MD 7.00, 95% CI 0.95 to 13.05; 1 study, 143 participants; low‐certainty evidence downgraded one level for risk of bias and for imprecision, respectively; Analysis 6.2).
6.2. Analysis.

Comparison 6: Acupuncture plus intervention vs intervention alone, Outcome 2: Acupuncture + standard therapy vs standard therapy
No study measured pain, back‐specific function, or quality of life in the intermediate or long term.
Secondary outcomes
a. Pain‐related disability
None of the studies measured this outcome.
b. Global assessment of therapy effectiveness
None of the studies measured this outcome.
c. Adverse events
The results for adverse events between groups were inconclusive (RR 1.64, 95% CI 0.70 to 3.83; 1 study, 44 participants; very low‐certainty evidence downgraded one level for risk of bias and two levels for imprecision; Analysis 6.3).
6.3. Analysis.

Comparison 6: Acupuncture plus intervention vs intervention alone, Outcome 3: Acupuncture + standard therapy vs standard therapy
6.2. Acupuncture plus exercise versus exercise alone
Primary outcomes
a. Pain intensity
One study (Hunter 2012) did not show differences for pain in the immediate term between the two groups (MD 0.49, 95% CI ‐2.38 to 3.36; 1 study, 45 participants; very low‐certainty evidence downgraded one level for risk of bias and two levels for imprecision; Analysis 6.4). No study measured pain in the short, intermediate, or long term.
6.4. Analysis.

Comparison 6: Acupuncture plus intervention vs intervention alone, Outcome 4: Acupuncture + exercise vs exercise
b. Back‐specific functional status
The same study (Hunter 2012) did not demonstrate differences for back‐specific function in the immediate term (MD 3.94, 95% CI ‐7.84 to 15.72; 1 study, 45 participants; very low‐certainty evidence downgraded one level for risk of bias and two levels for imprecision; Analysis 6.4), and in the intermediate term (MD ‐1.42, 95% CI ‐14.03 to 11.19; 1 study, 44 participants; very low‐certainty of evidence downgraded one level for risk of bias and two levels for imprecision; Analysis 6.4). The study (Hunter 2012) did not measure function in the short or long term.
c. Quality of life
The same study (Hunter 2012) did not find differences for quality of life in the immediate term (MD ‐0.05, 95% CI ‐0.26 to 0.16; 1 study, 45 participants; very low‐certainty evidence downgraded one level for risk of bias and two levels for imprecision; Analysis 6.4), and in the intermediate term (MD ‐0.10, 95% CI ‐0.32 to 0.12; 1 study, 44 participants; very low‐certainty evidence downgraded one level for risk of bias and two levels for imprecision; Analysis 6.4). The study (Hunter 2012) did not measure quality of life in the short or long term.
Secondary outcomes
a. Pain‐related disability
None of the studies measured this outcome.
b. Global assessment of therapy effectiveness
None of the studies measured this outcome.
c. Adverse events
The study (Weiss 2013) reported five adverse events in the acupuncture plus exercise group and none in the exercise group (RR 11.48, 95% CI 0.67 to 196.07; 1 study, 45 participants, very low‐certainty evidence downgraded one level for risk of bias and two levels for imprecision; Analysis 6.5). The five adverse events included pain, redness, minor bleeding and swelling around the needle insertion site.
6.5. Analysis.

Comparison 6: Acupuncture plus intervention vs intervention alone, Outcome 5: Acupuncture + exercise vs exercise
6.3. Acupuncture plus botulinum toxin type A versus botulinum toxin type A alone
Primary outcomes
a. Pain intensity
The results from a single study (Chen 2016) were inconclusive between groups for pain in the immediate term (MD ‐0.38, 95% CI ‐0.92 to 0.16; 1 study, 43 participants; very low‐certainty evidence downgraded one level for risk of bias and two levels for imprecision; Analysis 6.6). It did not measure pain in the short, intermediate, or long term.
6.6. Analysis.

Comparison 6: Acupuncture plus intervention vs intervention alone, Outcome 6: Acupuncture + botulinum toxin type A vs botulinum toxin type A
b. Back‐specific functional status
The group that received acupuncture plus botulinum toxin type A showed more back‐specific functional improvement than the group that received botulinum toxin type A alone in the immediate term (MD ‐11.91, 95% CI ‐19.02 to ‐4.80; 1 study, 43 participants; low‐certainty evidence downgraded one level for risk of bias and for imprecision, respectively; Analysis 6.6) (Chen 2016). The study did not measure back‐specific function in the short, intermediate, or long term.
c. Quality of life
The study did not measure quality of life.
Secondary outcomes
No study assessed the secondary outcomes for this comparison.
Adequacy of acupuncture
Our assessment of the adequacy of acupuncture treatment in the 33 trials reviewed is shown in Table 8.
5. Adequacy of acupuncture.
| Study | Choice of acupoints | Number of sessions | Treatment duration | Treatment frequency | Needling technique | Acupuncturist experience | Adequacy of sham or placebo intervention | Adequate number of sessions or dose of the control group |
| Brinkhaus 2006Brinkhaus 2006 | Adequate; but point selection at the discretion of different acupuncturists may introduce unexpected variables | Adequate | Adequate | Adequate | Adequate | Adequate | Probably adequate, as the needling insertion was away from the low back area; the best sham would be non‐insertion | Adequate |
| Carlsson 2001 | Adequate; however, point selection during the increase from 8 points to 14 to 18 should be clearly indicated | Don't know; no information provided on the total sessions | Adequate | Don't know; no information provided on the total sessions | Adequate | Adequate | Placebo intervention with mock TENS is a valid sham | Don't know. Sufficient information not given |
| Cesare 2011 | Inadequate; they did not use commonly used points BL23, BL25 | Inadequate; 4 sessions only | Don't know; no information provided | Inadequate; treatment once a week seems insufficient | Don't know; no mention of acupuncture techniques in the paper | Adequate | No sham or placebo | Don't know. Study comparing two acupuncture techniques |
| Chen 2010 | Adequate | Inadequate; 5 sessions may not be sufficient to provide adequate medical benefit | Inadequate; 15 minutes of intervention is not sufficient | Inadequate; once a week treatment for 5 weeks is not sufficient | Adequate | Don't know; no information provided | TENS without current induction is a good sham | Adequate |
| Chen 2016 | Adequate | Adequate | Adequate | Adequate | Adequate | Don't know; no information provided | No sham or placebo | Don't know. Botulinum toxin type A was the control |
| Cherkin 2009 | Adequate; standard acupuncture protocol is adequate. individualized acupuncture is possibly adequate, based on their training background | Adequate | Adequate | Adequate | Adequate; due to adequate training of acupuncturists | Adequate | Simulated acupuncture without actual needle insertion is a good sham | Adequate |
| Cho 2013 | Adequate | Don't know; no information provided | Adequate | Don't know; no information provided | Adequate | Adequate | Adequate; semi‐blunt needles were used without penetration | Don't know. No information given on control group's session |
| Grant 1999 | Don't know whether this protocol is adequate or not | Adequate | Adequate | Adequate | Don't know; no information on needling technique provided | Don't know; information on physiotherapist's experiences in acupuncture not provided | No sham or placebo control | Don't know. Parallel study comparing acupuncture and TENS |
| Haake 2007 | Don't know; list of acupuncture points not provided | Adequate | Adequate | Adequate | Adequate | Don't know; no mention of acupuncturist's training or experience | Not an adequate sham; acupuncture needle insertion avoiding non‐acupuncture points or meridians may still be considered Ashi points or trigger points | Adequate |
| Hunter 2012 | Adequate; used auricular acupuncture points | Adequate | Adequate | Adequate | Adequate | Don't know; no mention of acupuncture training | No sham for auricular acupuncture | Don't know. Exercise was the control |
| Itoh 2009 | Adequate | Don't know; no mention of numbers of sessions of treatment | Inadequate; 15‐minute treatment per session may provide insufficient benefit | Don't know; no mention of frequency of treatments | Adequate | Adequate | No sham | Adequate Non‐treatment group was control |
| Kerr 2003 | Adequate | Adequate; 6 sessions | Adequate | Inadequate; once a week treatment is insufficient | Adequate | Adequate; a chartered physiotherapist, trained in acupuncture, carried out all treatments |
Non‐functioning TENS intervention as placebo is viable | Adequate |
| Leibing 2002 | Don't know; no information provided | Adequate | Adequate | Adequate | Adequate | Don't know; only the institution where physician obtained his degrees provided; no mention of acupuncture training or background | Not an adequate sham; although needles were inserted superficially, at a distance from real acupuncture points, they may still provide some health benefit similar to needling Ashi points | Adequate |
| Li 2017 | Adequate | Adequate | Adequate | Adequate | Adequate | Don't know; no information provided on acupuncturist | No sham or placebo used | The study compared two styles of acupuncture |
| Lin 2010 | Adequate | Adequate | Adequate | Adequate | Adequate | Don't know; no information provided on acupuncturist | No sham or placebo used | Don't know. The study compared effects of different interventions |
| Meng 2003 | Adequate | Adequate | Adequate | Adequate | Adequate | Adequate; anesthetist certified in acupuncture carried out the treatments | No sham or placebo used | Don't know. Standard therapy as directed by primary physicians |
| Molsberger 2002 | Adequate | Adequate | Adequate | Adequate | Adequate | Don't know; no mention of the length of training in China | Needle insertion as a sham is not an optimal option; application of needles superficially, at non‐acupuncture points, may still produce local anesthetic effects | Adequate |
| Nie 2005 | Adequate | Don't know; only 5 sessions of the treatment were given | Don't know; no mention of treatment duration for each session | Adequate | Adequate | Don't know; no information provided | No sham or placebo control | Don't know. The study compared regular acupuncture and acupuncture + heated needles |
| Pach 2013 | Adequate | Adequate | Adequate | Adequate | Adequate | Adequate | No sham or placebo used | Don't know |
| Pan 2005 | Adequate | Adequate | Don't know; no mention of treatment duration | Adequate | Adequate | Don't know; no information provided | No sham or placebo control | Don't know. It is not applicable |
| Pérez‐Palomares 2010 | Adequate; acupuncture needle placement shown in picture corresponds to Huatuojiaji points from L2 to L5 | Adequate | Adequate | Adequate | Adequate | Don't know; no mention of acupuncturist | No sham or placebo used | Don't know. It is not applicable |
| Shankar 2010 | Adequate | Adequate | Adequate | Adequate | Adequate | Adequate | No sham or placebo | Don't know. The conventional therapy was the control |
| Tsukayama 2002 | Don't know; only 2 acupuncture points clearly mentioned; no explanation given on the choices of points | Inadequate; 4 treatments are not sufficient | Inadequate; 15‐minute treatment is not sufficient to produce satisfactory outcome | Adequate | Adequate | Don't know; no mention of practitioner's training | No sham or placebo | Don't know. The TENS intervention was the control |
| Ushinohama 2016 | Adequate | Inadequate; only 1 session was given | Adequate | Inadequate; only 1 session | Adequate | Adequate; "This therapist had 11 years of experience using EA as treatment for LBP". |
Simulated acupuncture without actual needle insertion is a good sham | Inadequate. The sham intervention contained only one session |
| Wang 2016a | Don't know; only tender points were needled | Inadequate; only 1 session was given | Inadequate; a 10‐minute session treatment is not enough | Inadequate; only 1 session was given | Adequate | Adequate; an experienced and licensed physician conducted the treatment | No sham or placebo | Don't know. The study compared the treatment effect of three diameters of needles for LBP |
| Weiss 2013 | Adequate; a pragmatic study that mimics daily practice; the protocol prescribed by the acupuncturist whose training is adequate | Don't know; total number of treatments not mentioned | Adequate | Adequate | Adequate; a qualified acupuncturist should be able to provide adequate needling technique | Adequate | No sham or placebo | Don't know. Standardized 21‐day inpatient rehabilitation program was control |
| Witt 2006 | Don't know; acupuncture protocols were not standardized; no mention of choice of acupuncture points | Adequate | Don't know; no information on duration | Adequate | Don't know; no information provided | Inadequate; 140 hours of training probably is not enough | No sham or placebo | Don't know. Routine care was control |
| Yuan 2009 | Adequate; prescribed by acupuncturist who had adequate training | Adequate | Adequate | Adequate | Adequate | Adequate | No sham or placebo | Don't know. Parallel study comparing different number of treatments per week |
| Yuan 2016 | Adequate | Adequate | Adequate | Adequate | Inadequate; no manipulation during the treatment | Don't know; no information provided | Simulated acupuncture without actual needle insertion is a good sham | Adequate |
| Yun 2012a | Adequate | Adequate | Adequate | Adequate | Adequate | Adequate | No sham or placebo | Don't know. Usual care was control |
| Yun 2012 | Adequate | Adequate | Adequate | Adequate | Adequate | Adequate | No sham or placebo | Don't know. Usual care was control |
| Zaringhalam 2010 | Adequate | Adequate | Adequate | Adequate | Adequate | Adequate | No sham or placebo | Don't know. It is not applicable |
| Zhao 2012 | Adequate | Inadequate; although total sessions are sufficient, 2 weeks of treatment seems too short |
Adequate | Adequate | Adequate | Don't know; no information provided | No sham or placebo | Don't know. Parallel study comparing two acupuncture techniques and medium frequency electrostimulation |
EA: electroacupuncture; LBP = low back pain; TENS: transcutaneous electrical nerve stimulation
The two experienced acupuncturists, who are also the review authors (LXL and MH), judged the majority of the trials to be adequate in their choice of acupoints. They judged Cesare 2011 inadequate because the acupoints most commonly used to treat low back pain (LBP), BL23 and BL25, were not chosen. They rated four studies as 'don't know' because these studies failed to provide information on the acupuncture points used.
The two assessors agreed that fewer than six sessions, sessions lasting 15 minutes or less, and sessions given at a frequency of one per 7 to 10 days or less often were insufficient and inadequate to treat chronic LBP. The assessors could not be certain whether one session per day was adequate, because this was a much higher session frequency than their own daily practice schedules. Based on the criteria specified above, they considered 16 studies to be adequate in terms of number of treatment sessions, treatment duration, and treatment frequency. They judged the others as inadequate or 'don't know'.
Three studies failed to report technique details, and 14 studies provided insufficient information on the participating acupuncturists' background and training. Therefore, the assessors could not identify either the needling techniques used in these studies or the backgrounds of the acupuncturists. They deemed the other studies adequate in both respects, with the exception of one trial, as they considered that the practitioner's 140 hours of training was probably insufficient (Witt 2006).
Of the 33 trials, 11 adopted sham acupuncture intervention as controls. The two assessors commented that "needle insertion as a sham was not an optimal option” because it may still have healthy benefits similar to those of needling Ashi points. The other 22 trials used a variety of comparators: no treatment, usual care, exercise, TENS, baclofen, and pulsed radiofrequency.
Subgroup and sensitivity analysis
We did not perform subgroup and sensitivity analysis because the maximum number of studies for each outcome was six, resulting in insufficient data to do these analyses. Meanwhile, the large variation in potential factors across the studies made it impossible to perform he analysis.
Discussion
Summary of main results
Low‐certainty evidence suggested that acupuncture may offer greater pain relief than sham acupuncture in the immediate term, but the difference was not clinically significant (Dworkin 2008). Very low‐certainty evidence suggested no difference in the immediate term that acupuncture improved back‐specific function than sham acupuncture but this finding was very uncertain. Low‐certainty evidence suggested a small improvement in quality of life with acupuncture in the short term, but which did not meet predefined clinical significance. The certainty of the evidence was downgraded due to high risk of bias, inconsistency, and severe imprecision. A similar incidence of adverse events was reported across four trials; however, the certainty of evidence was low due to imprecision and high risk of bias for lack of acupuncturist blinding.
Moderate‐certainty evidence showed that acupuncture provided greater clinically significant pain relief than no treatment in the immediate term. In addition, moderate‐certainty evidence showed that acupuncture improved back function more than no treatment immediately after the intervention, but this effect was not maintained in the short term. We downgraded the certainty of the evidence due to high risk of bias and inconsistency between studies. None of the studies comparing acupuncture with no treatment reported quality of life and adverse events related to acupuncture.
Low‐certainty evidence suggested that acupuncture did not reduce pain clinically in the immediate term compared with usual care. Low‐certainty evidence also showed that acupuncture may improve back‐specific function clinically in the immediate term. Usual care is a composition of primary care, medication, physiotherapy, and exercise. Moderate‐certainty evidence from one trial suggested that acupuncture had a clinically superior effect on physical health‐related but not mental health‐related quality of life in the short term. The certainty of evidence was moderate to low because of high risk of bias in blinding, dropouts, and inconsistency. One small trial reported four adverse events in the acupuncture group and one in the usual care group. The certainty of the evidence was low because of high risk of bias and imprecision from small sample sizes.
Overall completeness and applicability of evidence
The 33 included studies were carried out in various countries worldwide (Europe, Asia, and North America), therefore, the findings from our review are applicable worldwide. We did not separate dry needling results from acupuncture results, as very few studies investigated the use of dry needling alone to treat chronic low back pain (LBP). The primary effects studied were pain, back‐specific function, and quality of life, which are of the greatest interest or concern to patients, acupuncturists, and researchers. The secondary outcomes were pain‐related disability, global assessment of therapy effectiveness, and adverse events, which are also important outcomes of concern to people involved in acupuncture for treating chronic LBP. The mean age of the participants was 41.6 years, and the mean duration of LBP was 5.3 years. More than half of the participants reported moderate LBP (4 points on a 0 to 10 VAS) before receiving treatment. Therefore, our population was representative of the general population of people with chronic LBP, as the prevalence of LBP is highest between the ages of 40 and 69 years (Hoy 2012).
The trials reviewed assessed different techniques of acupuncture, such as dry needling at trigger points and standardized, semi‐standardized, and individualized styles of acupuncture. Our senior acupuncturist review authors (LXL and MH) found that the majority of the trials (28 RCTs) chose appropriate acupoints (common sites included Huatuojiaji points from L2 to L5, BL23, and BL25) as they are commonly used by trained practitioners. Half of the trials reported an adequate number of treatment sessions, adequate treatment duration, and treatment frequency. We defined sufficient treatment as consisting of six or more acupuncture sessions. In addition, 30 trials reported details of the acupuncture techniques used, and 19 trials provided sufficient information on the practitioners. This will enable the acupuncture practices reported to be repeated and continuously improved. Therefore, the results of this systematic review can be generalised across cultures, acupuncture practices, and people with chronic LBP in the real world, but not to LBP with a specific etiology.
Quality of the evidence
None of the included studies guaranteed that participants or acupuncturists had been blinded successfully, and all of the primary outcomes were self‐reported. Therefore, none of the evidence was high certainty. Quality was further compromised by a combination of a high risk of bias for co‐interventions (performance bias), unequal or high dropout rates (performance bias), the failure to use intention‐to‐treat analyses (attrition bias), inconsistency (heterogeneity), and imprecision (small samples, or results that included the null effect, or both). The certainty of the evidence provided for the comparisons of acupuncture versus other therapies, two acupuncture techniques, and acupuncture supplemented with an intervention versus the intervention alone, was generally poor, as some of the studies were at serious risk of bias. We often downgraded the certainties by two levels, either due to the use of small single studies (substantial imprecision) or high levels of inconsistency (substantial heterogeneity).
It is also difficult to totally blind the participants and providers, which may indicate a problem intrinsic to current clinical acupuncture randomized controlled trials (RCTs) that should be solved in the future. To determine whether heterogeneity was moderate or substantial, we considered conducting subgroup analyses based on differences in age (e.g. ≤ 65 versus > 65 years), LBP duration (e.g. ≤ 1 year versus > 1 year), patients' expectations of treatment effectiveness (high versus not high), etc. However, the large variation in those factors across the trials made it impossible to standardize the relevant factors. This is also reflected by the insufficient numbers of the studies enrolled for each outcome, with a maximum number of six and the majority of outcomes having data from one or two trials.
Reassuringly, the quality of studies of acupuncture to treat chronic LBP seems to have improved over the past 10 years. We classified many studies identified in our updated review as having low risk of bias in many areas, namely randomisation, allocation concealment, selective reporting, group similarity at baseline, compliance, and timing of outcome assessment.
Potential biases in the review process
Biases may have arisen from the literature search and review processes. We did not search grey literature (e.g. conference abstracts), and despite our best efforts, we were unable to gain access to some local databases (e.g. in Japan and Germany). Therefore, publication bias cannot be ruled out, although it was not detected, as only six trials or fewer were considered in each set of analyses.
Agreements and disagreements with other studies or reviews
The results of the updated review for true versus sham acupuncture differed from those of the previous review (Furlan 2005). We found that true acupuncture did not clinically outperform sham acupuncture for pain relief or functional improvement at any time point. The findings were based on 33 studies, two of which were retained from the previous review, and 31 of which were new. The interpretation of the findings was based on the Initiative for Maternal Mortality Programme Assessment's recommendation for a clinically important change in VAS pain score (Dworkin 2008), as adopted in the latest National Institute for Health and Care Excellence (NICE) guidelines (NICE 2016). The improvement threshold is a change of two points on a 0 to 10‐point visual analogue scale (VAS) or 30% on a 0 to 100‐point VAS, based on several big studies (Dworkin 2008). We adopted Haake’s criterion for a meaningful change in function (12% improvement on the Hannover Function Ability Questionnaire (HFAQ) because the trial placed the greatest weight on functional outcomes (Haake 2007)). However, we noticed that the conclusions of published reviews of studies comparing true with sham acupuncture were inconsistent; some favoured acupuncture over sham for pain relief but not functional improvement (Lam 2013; Rubinstein 2010; Xu 2013), whereas others concluded that the two had equivalent outcomes (Ammendolia 2008; NICE 2016). Similarly, our updated review found no clinically meaningful evidence that acupuncture was more effective than sham acupuncture in relieving pain or improving back‐specific function of people with chronic LBP.
Our results for acupuncture versus no treatment were consistent with those of the previous version of this review and other published reviews (Furlan 2005; Lam 2013; Xu 2013). We found that acupuncture relieved pain and improved function immediately, and in the short term. Also consistent with the results of most previous reviews, our findings indicated that acupuncture did not show a greater effect in relieving pain than usual care, but that acupuncture was slightly more effective in improving function in immediate, short‐term, and intermediate follow‐up (Ammendolia 2008; Lam 2013; Manheimer 2005; Rubinstein 2010; Xu 2013).
We obtained less, and lower certainty evidence of the relative effectiveness of acupuncture compared with other therapies (e.g. TENS, baclofen, pulsed radiofrequency therapy); no acupuncture technique was found to be appreciably better than another (acupuncture did not outperform dry needling at trigger points, standardized acupuncture did not surpass individualized acupuncture, etc.); and combining acupuncture with other interventions (e.g. exercise, botulinum toxin type A) resulted in little or no additional benefits, except for acupuncture with botulinum toxin type A improving the function more than botulinum toxin type A alone. Acupuncture plus standard therapy offered greater treatment than standard therapy alone, but this evidence was of low certainty. We noticed that neither our current nor the previous version of this review, nor other systematic reviews and guidelines, drew firm conclusions related to these three types of comparisons (Furlan 2005; Lam 2013; Liu 2015a; NICE 2016; Xu 2013). The most common reasons were low‐certainty evidence from single studies with small samples, conflicting results across studies, and uncertainty due to lack of clinically important differences of the outcomes assessed. In contrast, results for the insignificant incidence of adverse events related to acupuncture was consistent between our own and many other reviews, indicating that acupuncture may be a relatively safe treatment for people with chronic LBP (Ammendolia 2008; Lam 2013; Liu 2015a; Manheimer 2005; Rubinstein 2010; Xu 2013).
Authors' conclusions
Implications for practice.
The very low to low‐certainty evidence with sham controls provides evidence that acupuncture seems not to be more effective than sham in treating chronic nonspecific low back pain (LBP). In clinical practice, the decision to use acupuncture to treat chronic LBP may depend on treatment availability, cost, and, importantly, participant or provider preference. Moderate‐certainty evidence showed that acupuncture provided more immediate pain relief than no treatment for people with persistent pain. Very low to moderate‐certainty evidence provided no significant results between acupuncture and usual care. The majority of the evidence from the other three comparisons (acupuncture versus another intervention, one technique of acupuncture versus another, and acupuncture plus an intervention versus the same intervention alone) suggested that acupuncture brought no additional clinical benefits, and that no one acupuncture technique was clinically better than another. The certainty of this evidence was either very low or low, due to poor methodology and small samples.
Although there was low‐certainty evidence for adverse events in the main comparisons, the incidence of such events was generally similar between acupuncture and sham or usual care, consistent with the findings of many other systematic reviews. Therefore, we consider acupuncture might be a safe treatment for people with chronic LBP.
Implications for research.
Future studies should seek to minimize the risk of bias through appropriate blinding practices, co‐intervention strategies, and intention‐to‐treat (ITT) analyses. Finding a way to effectively mask acupuncturists and participants will reduce primary bias, and enable trials to differentiate the physiological (specific) and psychological (nonspecific) effects of acupuncture treatment. Overall, we highly recommend that future clinical trials follow the Consolidated Standards of Reporting Trials (CONSORT) checklist to improve research methodology in this field (Schulz 2010).
Many of the included trials did not fully meet the STRICTA guidelines, particularly in their failure to report the details of needling techniques (MacPherson 2010). Therefore, we strongly suggest that future researchers carefully consult the STRICTA checklist when designing and reporting acupuncture treatment protocols, as this will make their studies more informative.
Next, the trials reviewed did not investigate the types of people who would benefit most from the use of acupuncture to manage chronic LBP. Therefore, we recommend that future trials compare outcomes classified by pain duration and baseline pain intensity; for example, measuring LBP experienced for less than one year versus more than one year, or measuring baseline pain on a 10‐point visual analogue scale (VAS) between four and seven points and higher than seven. Additional methodological research in this field is also necessary, particularly to explore the potential influence of patients' preferences and expectations on outcomes. Finally, the included trials provided relatively little information on the effectiveness of combined interventions involving acupuncture in managing chronic nonspecific LBP. Future trials testing such interventions will provide very useful evidence for clinical practice.
What's new
| Date | Event | Description |
|---|---|---|
| 27 November 2020 | New search has been performed | We split our previous review into two reviews to address acute and chronic nonspecific LBP (Furlan 2005). This review used up‐to‐date methods, particularly the 13‐item risk of bias assessment tool and the GRADE approach to assess the quality of the evidence, as recommended in the Cochrane Handbook of Systematic Reviews of Interventions (Higgins 2019), and the Cochrane Back and Neck guidelines (Furlan 2015). |
| 27 November 2020 | New citation required and conclusions have changed | We included 33 trials in this update (8270 patients) with two trials from the previous review (132 patients) (Furlan 2005). The results for acupuncture versus sham acupuncture have changed since the previous review. The evidence indicates that acupuncture is not clinically better than sham acupuncture at relieving pain or improving function immediately post‐treatment. We added a new comparison of acupuncture versus usual care to reflect the development of research in this field. We found that acupuncture is more effective than usual care in relieving pain and improving function immediately after treatment. |
History
Review first published: Issue 12, 2020
| Date | Event | Description |
|---|---|---|
| 1 March 2016 | Amended | Converted to new review format. |
| 23 April 2010 | Amended | There was a decision that the previous review was split into acute and chronic non‐specific low back pain. |
Acknowledgements
We acknowledge the provision of unpublished trial data by Claudia Witt (Witt 2006). We thank Shireen Harbin, the Managing Editor of the Cochrane Back and Neck Group (CBN) for her help with the search strategies and efficient co‐ordination of the editorial process. We are grateful to the medical librarian, Lucinda Wong, of the University of Hong Kong, for her help in developing the search strategies for the Chinese databases. We thank Assistant Adminstrator Ms. Tan Xing, Secretary Ms. Xiao Jing‐Xin, and Dr. Zhang Fu, for their helps and supports in doing the review. Finally, we would like to thank all editors and peer review authors who provided excellent comments and help in edits to improve this review: Vicki Pennick, Janet Gunderson, Julie Fritz, Donna Urquhart, Ibrahem Hanafi, and Nicholas Henschke.
Appendices
Appendix 1. Search strategies
CBN register
Last searched on 29 August 2019
1 MESH DESCRIPTOR Back Pain EXPLODE ALL AND INREGISTER
2 dorsalgia AND INREGISTER
3 backache AND INREGISTER
4 MESH DESCRIPTOR Low Back Pain EXPLODE ALL AND INREGISTER
5 lumb* NEAR3 pain AND INREGISTER
6 lumbago or discitis or disc NEAR herniat* AND INREGISTER
7 spinal fusion AND INREGISTER
8 facet NEAR joint* AND INREGISTER
9 MESH DESCRIPTOR Intervertebral Disc EXPLODE ALL AND INREGISTER
10 arachnoiditis AND INREGISTER
11 failed NEAR back AND INREGISTER
12 MESH DESCRIPTOR Cauda Equina EXPLODE ALL AND INREGISTER
13 lumbar NEAR vertebra* AND INREGISTER
14 slipped NEAR (disc* or disk*) AND INREGISTER
15 degenerat* NEAR (disc* or disk*) AND INREGISTER
16 stenosis NEAR (spine or root or spinal) AND INREGISTER
17 displace* NEAR (disc* or disk*) AND INREGISTER
18 prolap* NEAR (disc* or disk*) AND INREGISTER
19 MESH DESCRIPTOR Sciatic Neuropathy EXPLODE ALL AND INREGISTER
20 sciatic* AND INREGISTER
21 back disorder* AND INREGISTER
22 back NEAR pain AND INREGISTER
23 #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 AND INREGISTER
24 MESH DESCRIPTOR Acupuncture EXPLODE ALL AND INREGISTER
25 MESH DESCRIPTOR Acupuncture Therapy EXPLODE ALL AND INREGISTER
26 Acupuncture AND INREGISTER
27 MESH DESCRIPTOR Trigger Points EXPLODE ALL AND INREGISTER
28 trigger point* AND INREGISTER
29 dry needl* AND INREGISTER
30 MESH DESCRIPTOR Meridians EXPLODE ALL AND INREGISTER
31 meridian* AND INREGISTER
32 #24 OR #25 OR #26 OR #27 OR #28 OR #29 OR #30 OR #31
33 #32 AND #23
34 (2018 OR 2019):YR AND INREGISTER
35 #33 AND #34
CENTRAL
Last searched 29 August 2019
1 MESH DESCRIPTOR Back Pain EXPLODE ALL AND CENTRAL
2 dorsalgia AND CENTRAL
3 backache AND CENTRAL
4 MESH DESCRIPTOR Low Back Pain EXPLODE ALL AND CENTRAL
5 lumb* NEAR3 pain AND CENTRAL
6 lumbago or discitis or disc NEAR herniat* AND CENTRAL
7 spinal fusion AND CENTRAL
8 facet NEAR joint* AND CENTRAL
9 MESH DESCRIPTOR Intervertebral Disc EXPLODE ALL AND CENTRAL
10 arachnoiditis AND CENTRAL
11 failed NEAR back AND CENTRAL
12 MESH DESCRIPTOR Cauda Equina EXPLODE ALL AND CENTRAL
13 lumbar NEAR vertebra* AND CENTRAL
14 slipped NEAR (disc* or disk*) AND CENTRAL
15 degenerat* NEAR (disc* or disk*) AND CENTRAL
16 stenosis NEAR (spine or root or spinal) AND CENTRAL
17 displace* NEAR (disc* or disk*) AND CENTRAL
18 prolap* NEAR (disc* or disk*) AND CENTRAL
19 MESH DESCRIPTOR Sciatic Neuropathy EXPLODE ALL AND CENTRAL
20 sciatic* AND CENTRAL
21 back disorder* AND CENTRAL
22 back NEAR pain AND CENTRAL:TARGET 12796
23 #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 AND CENTRAL
24 MESH DESCRIPTOR Acupuncture EXPLODE ALL AND CENTRAL
25 MESH DESCRIPTOR Acupuncture Therapy EXPLODE ALL AND CENTRAL
26 Acupuncture AND CENTRAL
27 MESH DESCRIPTOR Trigger Points EXPLODE ALL AND CENTRAL
28 trigger point* AND CENTRAL
29 dry needl* AND CENTRAL
30 MESH DESCRIPTOR Meridians EXPLODE ALL AND CENTRAL
31 meridian* AND CENTRAL
32 #31 OR #30 OR #29 OR #28 OR #27 OR #26 OR #25 OR #24 AND CENTRAL
33 #32 AND #23 AND CENTRAL
MEDLINE
Last searched on 29 August 2019
1 randomised controlled trial.pt.
2 controlled clinical trial.pt.
3 pragmatic clinical trial.pt.
4 random*.ti,ab.
5 placebo.ab,ti.
6 drug therapy.fs.
7 trial.ab,ti.
8 groups.ab,ti.
9 (animals not (humans and animals)).sh.
10 or/1‐8
11 10 not 9
12 dorsalgia.tw,kf.
13 exp Back Pain/
14 backache.tw,kf.
15 back pain.tw,kf.
16 (lumb* adj3 pain).tw,kf.
17 coccyx.tw,kf.
18 coccydynia.tw,kf.
19 sciatica.tw,kf.
20 sciatica/
21 spondylosis.tw,kf.
22 lumbago.tw,kf.
23 exp low back pain/
24 or/12‐23
25 exp Acupuncture Therapy/
26 exp Acupuncture/
27 exp Meridians/
28 meridian*.tw,kf.
29 Electroacupuncture.tw,kf.
30 dry needl*.tw,kf.
31 acupuncture.tw,kf.
32 trigger points/
33 trigger point*.tw,kf.
34 or/25‐33
35 11 and 24 and 34
Embase
Last searched on 29 August 2019
1 randomised Controlled Trial/
2 exp Controlled clinical trial/
3 Controlled Study/
4 Double Blind Procedure/
5 Single Blind Procedure/
6 crossover procedure/
7 placebo/
8 random*.ti,ab.
9 placebo?.ti,ab.
10 allocat*.ti,ab.
11 assign*.ti,ab.
12 blind*.ti,ab.
13 (compare or compared or comparing or comparison or comparative).ti,ab.
14 ((controlled adj7 study) or (controlled adj7 design)).ti,ab.
15 (cross‐over or crossover).ti,ab.
16 ((singl* adj7 mask*) or (doubl* adj7 mask*) or (trebl* adj7 mask*) or (tripl* adj7 mask*)).ti,ab.
17 trial.ti,ab.
18 or/1‐17
19 exp animals/ or exp invertebrate/ or animal experiment/ or animal model/ or animal tissue/ or animal cell/ or nonhuman/
20 human/ or normal human/ or human cell/
21 19 and 20
22 19 not 21
23 18 not 22
24 dorsalgia.tw,kw.
25 back pain.tw,kw.
26 exp BACKACHE/
27 (lumb* adj3 pain).tw,kw.
28 coccyx.tw,kw.
29 coccydynia.tw,kw.
30 sciatica.tw,kw.
31 sciatica/
32 exp ISCHIALGIA/
33 spondylosis.tw,kw.
34 lumbago.tw,kw.
35 exp Low back pain/
36 or/24‐35
37 exp Acupuncture/
38 Electroacupuncture.tw,kw.
39 Trigger points/
40 trigger point*.tw,kw.
41 meridian*.tw,kw.
42 dry needl*.tw,kw.
43 acupuncture.tw,kw.
44 or/37‐43
45 23 and 36 and 44
CINAHL plus
Last searched on 29 August 2019
S39 S29 AND S38 787
S38 S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37
S37 trigger point*
S36 "meridian*"
S35 MH Meridians+
S34 MH Dry Needling or dry needl*
S33 MH electroacupuncture or electroacupuncture
S32 MH trigger point
S31 "acupuncture"
S30 MH Acupuncture+
S29 S11 AND S28
S28 S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27
S27 "coccydynia"
S26 lumb* N3 pain
S25 "lumbago"
S24 MH Spondylolysis
S23 MH Spondylolisthesis
S22 MH Thoracic Vertebrae
S21 MH Lumbar Vertebrae
S20 MH sciatica
S19 MH coccyx
S18 "Sciatica"
S17 "Coccyx"
S16 "back pain"
S15 "backache"
S14 MH Low Back Pain
S13 MH Back Pain+
S12 dorsalgia
S11 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10
S10 TX random*
S9 MH Quantitative Studies
S8 MH Placebos
S7 TX placebo*
S6 TX control*
S5 MH Random Assignment
S4 TX (blind* or mask*)
S3 TX trial*
S2 PT Clinical trial
S1 MH Clinical Trials+
CNKI
Last searched on 30 August 2019
SU = (acupuncture and moxibustion+ electroacupuncture)*low back pain‐animal
TI = trial + observation + case (Searching in the results)
Wanfang Data
Last searched on 30 August 2019
(title: "acupuncture and moxibustion" or title: "acupuncture" or title: "electroacupuncture" or title: "auricular acupuncture") (title: "low back pain")
ClinicalTrials.gov
Last searched on 29 August 2019
((acupuncture OR electroacupuncture OR dry needling) AND (back pain OR lumbar pain OR sciatica OR lumbago))
ICTRP
Last searched on 29 August 2019
Acupuncture AND back pain OR acupuncture AND lumbar pain OR acupuncture AND sciatica OR acupuncture AND lumbago
electroacupuncture AND back pain OR electroacupuncture AND lumbar pain OR electroacupuncture AND sciatica OR electroacupuncture AND lumbago
Dry needling AND back pain OR dry needling AND lumbar pain OR dry needling AND sciatica OR dry needling and lumbago
Appendix 2. The GRADE approach to evidence synthesis
The certainty of evidence was assessed according to the GRADE Handbook (Schünemann 2017a; Schünemann 2017b)
High certainty (⊕⊕⊕⊕): further research is very unlikely to change our confidence in the estimate of effect.
Moderate certainty (⊕⊕⊕): further research is likely to have an important impact on our confidence in the estimate of effect.
Low certainty (⊕⊕): further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Very low certainty (⊕): any estimate of effect is very uncertain.
We graded the important evidence on the domains based on the criteria from Ryan 2016.
1. Risk of bias
Confidence in the certainty of the estimate decreases if studies have major limitations in design and conduct. We assessed five types of bias, classified in Table 4. The reasons to judge yes are described in Table 5.
selection bias (random sequence generation, allocation concealment, group similarities at baseline);
performance bias (blinding of participants, blinding of personnel or care providers, co‐interventions, compliance);
attrition bias (incomplete outcome data, intention‐to‐treat analysis);
detection bias (blinding of outcome assessors, timing of outcome assessments);
reporting bias (selective reporting), and other bias
If most of the information was from studies at low or unclear risk of bias, with no serious limitations in design, we did not downgrade the level of confidence. If there was a crucial limitation for one aspect of bias, or some limitations for multiple aspects, we downgraded the certainty of evidence by one level. If there was a crucial limitation for more than one aspect, we downgraded the certainty of evidence by two levels.
2. Inconsistency
Inconsistency refers to an unexplained heterogeneity of results. The I² statistic is an estimate of the percentage of the variability in effect estimates that is due to clinical or methodological heterogeneity rather than chance.
< 40% may be low
30% to 60% may be moderate
50% to 90% may be substantial
75% to 100% may be considerable
We downgraded the certainty of evidence by one level when heterogeneity was substantial (e.g. I² between 50% and 90%) but with a plausible clinical explanation, and by two levels when heterogeneity was considerable (e.g. I² between 75% to 100%), unless there was a plausible clinical explanation for the heterogeneity, then we downgraded by one level.
3. Indirectness
There are five sources of indirectness: differences in population, interventions, outcomes, and measures, and indirect comparisons. We downgraded the certainty of evidence by one level when there was indirectness for one element of the source (e.g. population), and by two levels when there was indirectness for two or more elements of the source.
4. Imprecision
In general, results are imprecise when studies include relatively few patients and few events, and thus have a wide confidence interval (CI) around the estimate of the effect. We used the following guidance in judging imprecision.
For continuous outcomes
We downgraded the certainty of the evidence by one level for imprecision if:
the total number of participants was less than 400; or
the 95% confidence interval around the estimate of effect covered both no effect and a minimally important difference for that outcome.
We calculated the optimal information size (OIS) if the total number of participants was fewer than 400. If the total number of patients was less than the calculated OIS, we downgraded one level for imprecision. We downgraded the certainty of the evidence by two levels for imprecision if both points above were true.
For dichotomous outcomes
We downgraded the certainty of the evidence by one level for imprecision if:
the total number of events was less than 300; or
the 95% confidence interval around the estimate of effect included both no effect and either appreciable benefit or appreciable harm. The threshold for appreciable benefit or appreciable harm was a relative risk reduction (RRR) or relative risk increase (RRI) greater than 25%.
We downgraded the certainty of the evidence by two levels for imprecision if both points above were true.
5. Publication bias
Publication bias is a systematic under‐estimation or an over‐estimation of the underlying beneficial or harmful effect due to the selective publication of studies. We downgraded the certainty of the evidence by one level if the funnel plot suggested the potential of publication bias, even when the included studies themselves had a low risk of bias.
Data and analyses
Comparison 1. Acupuncture vs sham intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Pain intensity (VAS) | 8 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1.1 Immediately after | 7 | 1403 | Mean Difference (IV, Random, 95% CI) | ‐9.22 [‐13.82, ‐4.61] |
| 1.1.2 Short term | 5 | 1095 | Mean Difference (IV, Random, 95% CI) | ‐10.04 [‐17.22, ‐2.85] |
| 1.1.3 Intermediate term | 4 | 1138 | Mean Difference (IV, Random, 95% CI) | ‐3.83 [‐6.57, ‐1.09] |
| 1.2 Back‐specific function | 5 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.2.1 Immediately after (RMDQ, ODI, HFAQ) | 5 | 1481 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.38, 0.06] |
| 1.2.2 Short term (ODI, HFAQ) | 3 | 957 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.69, ‐0.07] |
| 1.2.3 Intermediate term (RMDQ, ODI, HFAQ) | 4 | 1373 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.27, ‐0.05] |
| 1.3 Quality of life | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.3.1 Immediately after (SF‐36) | 2 | 157 | Mean Difference (IV, Random, 95% CI) | 4.42 [‐1.34, 10.18] |
| 1.4 Quality of life | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.4.1 Short term (SF‐36, SF‐12 physical) | 3 | 1068 | Std. Mean Difference (IV, Random, 95% CI) | 0.24 [0.03, 0.45] |
| 1.4.2 Intermediate term (SF‐36, SF‐12 physical) | 3 | 1066 | Std. Mean Difference (IV, Random, 95% CI) | 0.21 [0.09, 0.33] |
| 1.5 Pain‐related disability (PDI) | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.5.1 Immediately after | 2 | 285 | Mean Difference (IV, Random, 95% CI) | ‐3.28 [‐6.39, ‐0.17] |
| 1.5.2 Intermediate term | 2 | 269 | Mean Difference (IV, Random, 95% CI) | ‐2.91 [‐6.33, 0.51] |
| 1.6 Global assessment of therapy effectiveness (6‐point scale) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.6.1 Immediately after | 1 | 744 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.49, ‐0.11] |
| 1.6.2 Short term | 1 | 747 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.49, ‐0.11] |
| 1.6.3 Intermediate term | 1 | 751 | Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.39, ‐0.01] |
| 1.7 Global assessment of therapy effectiveness (effective number) | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.7.1 Immediately after | 2 | 163 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [1.04, 1.46] |
| 1.7.2 Short term | 2 | 141 | Risk Ratio (M‐H, Random, 95% CI) | 1.88 [0.66, 5.36] |
| 1.8 Adverse events | 4 | 465 | Risk Ratio (M‐H, Random, 95% CI) | 0.68 [0.46, 1.01] |
Comparison 2. Acupuncture vs no treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Pain intensity (VAS) | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1.1 Immediately after | 4 | 366 | Mean Difference (IV, Random, 95% CI) | ‐20.32 [‐24.50, ‐16.14] |
| 2.1.2 Short term | 3 | 144 | Mean Difference (IV, Random, 95% CI) | ‐10.11 [‐16.80, ‐3.43] |
| 2.2 Back‐specific function | 5 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.2.1 Immediately after (RMDQ, HFAQ, ODI) | 5 | 2960 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.53 [‐0.73, ‐0.34] |
| 2.2.2 Short term (RMDQ,ODI) | 3 | 144 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.39 [‐0.72, ‐0.06] |
| 2.3 Quality of life | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.3.1 Immediately after (SF‐36 physical) | 2 | 2837 | Mean Difference (IV, Random, 95% CI) | 5.10 [3.09, 7.11] |
| 2.3.2 Immediately after (SF‐36 mental) | 2 | 2837 | Mean Difference (IV, Random, 95% CI) | 1.85 [1.06, 2.64] |
| 2.4 Pain‐related disability (PDI, PRS) | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.4.1 Immediately after | 2 | 2837 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.56 [‐0.64, ‐0.49] |
Comparison 3. Acupuncture vs usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Pain intensity (VAS) | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1.1 Immediately after | 5 | 1054 | Mean Difference (IV, Random, 95% CI) | ‐10.26 [‐17.11, ‐3.40] |
| 3.1.2 Short term | 2 | 817 | Mean Difference (IV, Random, 95% CI) | ‐18.78 [‐37.97, 0.41] |
| 3.1.3 Intermediate term | 2 | 804 | Mean Difference (IV, Random, 95% CI) | ‐12.30 [‐15.28, ‐9.32] |
| 3.2 Back‐specific function | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.2.1 Short term (HFAQ) | 1 | 734 | Mean Difference (IV, Random, 95% CI) | 9.40 [6.15, 12.65] |
| 3.3 Back‐specific function | 5 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.3.1 Immediately after (RMDQ, ODI, HFAQ) | 5 | 1381 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.47 [‐0.77, ‐0.17] |
| 3.3.2 Intermediate term (RMDQ, HFAQ) | 4 | 1310 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.44 [‐0.55, ‐0.33] |
| 3.4 Quality of life | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.4.1 Immediately after (SF‐36) | 1 | 71 | Mean Difference (IV, Random, 95% CI) | 0.20 [‐5.82, 6.22] |
| 3.4.2 Short term (SF‐12 physical) | 1 | 731 | Mean Difference (IV, Random, 95% CI) | 4.20 [2.82, 5.58] |
| 3.4.3 Short term (SF‐12 mental) | 1 | 731 | Mean Difference (IV, Random, 95% CI) | 1.90 [0.25, 3.55] |
| 3.4.4 Intermediate term (SF‐12 physical) | 1 | 737 | Mean Difference (IV, Random, 95% CI) | 5.80 [4.36, 7.24] |
| 3.4.5 Intermediate term (SF‐12 mental) | 1 | 737 | Mean Difference (IV, Random, 95% CI) | 1.50 [‐0.15, 3.15] |
| 3.5 Pain‐related disability (PDI) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.5.1 Immediately after | 1 | 74 | Mean Difference (IV, Random, 95% CI) | ‐11.00 [‐17.18, ‐4.82] |
| 3.5.2 Intermediate term | 1 | 63 | Mean Difference (IV, Random, 95% CI) | ‐6.40 [‐13.10, 0.30] |
| 3.6 Global assessment of therapy effectiveness (6‐point scale) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.6.1 Short term | 1 | 730 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.50, ‐0.10] |
| 3.6.2 Intermediate term | 1 | 738 | Mean Difference (IV, Random, 95% CI) | ‐0.70 [‐1.04, ‐0.36] |
| 3.7 Global assessment of therapy effectiveness (effective number) | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.7.1 Immediately after | 3 | 396 | Risk Ratio (M‐H, Random, 95% CI) | 1.41 [1.18, 1.67] |
| 3.7.2 Short term | 1 | 86 | Risk Ratio (M‐H, Random, 95% CI) | 2.47 [1.46, 4.17] |
| 3.7.3 Intermediate term | 2 | 279 | Risk Ratio (M‐H, Random, 95% CI) | 1.30 [1.08, 1.55] |
| 3.8 Adverse events | 1 | 74 | Risk Ratio (M‐H, Random, 95% CI) | 3.34 [0.36, 30.68] |
Comparison 4. Acupuncture vs another intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Acupuncture vs TENS | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1.1 Pain intensity immediately after (VAS) | 5 | 196 | Mean Difference (IV, Random, 95% CI) | ‐8.26 [‐19.03, 2.51] |
| 4.1.2 Pain intensity short term (VAS) | 3 | 116 | Mean Difference (IV, Random, 95% CI) | ‐9.51 [‐19.50, 0.49] |
| 4.1.3 Back‐specific function short term (RMDQ) | 2 | 61 | Mean Difference (IV, Random, 95% CI) | ‐0.49 [‐2.61, 1.63] |
| 4.1.4 Pain‐related disability immediately after (JOA ‐ 2 aspects) | 1 | 19 | Mean Difference (IV, Random, 95% CI) | ‐2.80 [‐5.81, 0.21] |
| 4.2 Acupuncture vs TENS | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.2.1 Back‐specific function immediately after (RMDQ, ODI) | 3 | 121 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.83 [‐1.91, 0.24] |
| 4.3 Acupuncture vs TENS | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.3.1 Adverse events | 2 | 76 | Risk Ratio (M‐H, Random, 95% CI) | 1.22 [0.48, 3.13] |
| 4.4 Acupuncture vs baclofen | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.4.1 Pain intensity immediately after (VAS) | 1 | 40 | Mean Difference (IV, Random, 95% CI) | ‐14.90 [‐27.77, ‐2.03] |
| 4.4.2 Pain intensity short term (VAS) | 1 | 40 | Mean Difference (IV, Random, 95% CI) | ‐13.60 [‐22.56, ‐4.64] |
| 4.4.3 Back‐specific function immediately after (RMDQ) | 1 | 40 | Mean Difference (IV, Random, 95% CI) | ‐2.40 [‐4.49, ‐0.31] |
| 4.4.4 Back‐specific function short term (RMDQ) | 1 | 40 | Mean Difference (IV, Random, 95% CI) | ‐2.30 [‐4.55, ‐0.05] |
| 4.5 Acupuncture vs pulsed radiofrequency therapy (PRT) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.5.1 Pain intensity immediately after (VAS) | 1 | 65 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐1.97, 1.37] |
| 4.5.2 Back‐specific function immediately after (ODI) | 1 | 65 | Mean Difference (IV, Random, 95% CI) | 3.40 [‐11.82, 18.62] |
| 4.5.3 Quality of life immediately after (SF‐36) | 1 | 65 | Mean Difference (IV, Random, 95% CI) | 4.20 [‐1.91, 10.31] |
Comparison 5. Acupuncture vs another acupuncture technique.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Acupuncture vs dry needling on trigger points | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1.1 Pain intensity immediately after (VAS) | 3 | 246 | Mean Difference (IV, Random, 95% CI) | 0.45 [‐0.44, 1.33] |
| 5.1.2 Pain intensity immediately after (VAS) for subgroup analysis | 2 | 185 | Mean Difference (IV, Random, 95% CI) | 0.83 [‐0.44, 2.10] |
| 5.1.3 Back‐specific function short term (RMDQ) | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐1.08 [‐1.34, ‐0.82] |
| 5.1.4 Pain intensity intermediate term (VAS) | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 1.40 [0.59, 2.21] |
| 5.1.5 Back‐specific function intermediate after (ODI) | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 5.02 [2.05, 7.99] |
| 5.1.6 Pain intensity short term (VAS) | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐1.20 [‐1.32, ‐1.08] |
| 5.2 Acupuncture vs dry needling on trigger points | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.2.1 Back‐specific function immediately after (RMDQ, ODI) | 2 | 121 | Std. Mean Difference (IV, Random, 95% CI) | 0.32 [‐0.63, 1.27] |
| 5.3 Acupuncture vs dry needling on trigger points | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.3.1 Adverse events | 1 | 62 | Risk Ratio (M‐H, Random, 95% CI) | 9.71 [0.56, 168.32] |
| 5.4 Standard acupuncture vs individualized acupuncture | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.4.1 Pain intensity short term (VAS) | 1 | 144 | Mean Difference (IV, Random, 95% CI) | ‐1.30 [‐9.49, 6.89] |
| 5.4.2 Pain intensity intermediate term (VAS) | 1 | 139 | Mean Difference (IV, Random, 95% CI) | ‐3.20 [‐11.83, 5.43] |
| 5.4.3 Back‐specific function immediately after (RMDQ) | 1 | 299 | Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐1.35, 1.15] |
| 5.4.4 Back‐specific function short term (HFAQ) | 1 | 144 | Mean Difference (IV, Random, 95% CI) | 1.70 [‐4.34, 7.74] |
| 5.4.5 Quality of life short term (SF‐36 physical) | 1 | 144 | Mean Difference (IV, Random, 95% CI) | ‐0.60 [‐3.72, 2.52] |
| 5.4.6 Quality of life short term (SF‐36 mental) | 1 | 144 | Mean Difference (IV, Random, 95% CI) | 0.50 [‐3.14, 4.14] |
| 5.4.7 Quality of life intermediate term (SF‐36 physical) | 1 | 139 | Mean Difference (IV, Random, 95% CI) | ‐1.40 [‐4.62, 1.82] |
| 5.4.8 Quality of life intermediate term (SF‐36 mental) | 1 | 139 | Mean Difference (IV, Random, 95% CI) | 1.90 [‐2.06, 5.86] |
| 5.4.9 Pain‐related disability short term | 1 | 144 | Mean Difference (IV, Random, 95% CI) | 0.30 [‐3.96, 4.56] |
| 5.4.10 Pain‐related disability intermediate term | 1 | 139 | Mean Difference (IV, Random, 95% CI) | ‐0.70 [‐8.49, 7.09] |
| 5.5 Standard acupuncture vs individualized acupuncture | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.5.1 Back‐specific function intermediate term (RMDQ, HFAQ) | 2 | 427 | Std. Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.16, 0.22] |
| 5.6 Standard acupuncture vs individualized acupuncture | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.6.1 Adverse events | 1 | 299 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.32, 2.93] |
| 5.7 High‐frequency acupuncture vs low‐frequency acupuncture | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.7.1 Pain intensity immediately after (VAS) | 1 | 29 | Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐1.21, 0.81] |
| 5.7.2 Pain intensity short term (VAS) | 1 | 29 | Mean Difference (IV, Random, 95% CI) | 0.25 [‐0.64, 1.14] |
| 5.7.3 Pain intensity intermediate term (VAS) | 1 | 21 | Mean Difference (IV, Random, 95% CI) | 0.06 [‐1.12, 1.24] |
| 5.7.4 Back‐specific function immediately after (RMDQ) | 1 | 29 | Mean Difference (IV, Random, 95% CI) | ‐0.57 [‐3.60, 2.46] |
| 5.7.5 Back‐specific function short term (RMDQ) | 1 | 29 | Mean Difference (IV, Random, 95% CI) | 1.20 [‐0.79, 3.19] |
| 5.7.6 Back‐specific function intermediate term (RMDQ) | 1 | 21 | Mean Difference (IV, Random, 95% CI) | 0.30 [‐0.88, 1.48] |
| 5.8 High‐frequency acupuncture vs low‐frequency acupuncture | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.8.1 Adverse events | 1 | 29 | Risk Ratio (M‐H, Random, 95% CI) | 1.47 [0.80, 2.69] |
| 5.9 Acupuncture (local acupoints) vs acupuncture (local + distant acupoints) | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.9.1 Back‐specific function immediately after (RMDQ) | 2 | 289 | Mean Difference (IV, Random, 95% CI) | 0.90 [0.44, 1.36] |
| 5.9.2 Back‐specific function intermediate term (RMDQ) | 2 | 289 | Mean Difference (IV, Random, 95% CI) | 1.15 [0.74, 1.57] |
| 5.10 Acupuncture (local acupoints) vs acupuncture (local + distant acupoints) | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.10.1 Global assessment of therapy effectiveness immediately after (effective response) | 2 | 289 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.77, 1.10] |
| 5.10.2 Global assessment of therapy effectiveness intermediate term (effective response) | 2 | 289 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.78, 1.01] |
| 5.11 Acupuncture (rotation) vs acupuncture (fast‐in & fast‐out) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.11.1 Pain intensity immediately after (VAS) | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐1.00 [‐1.94, ‐0.06] |
| 5.11.2 Back‐specific function immediately after (ODI) | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐3.50 [‐4.82, ‐2.18] |
| 5.12 Acupuncture (0.25 mm diameter) vs. acupuncture (0.9 mm diameter) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.12.1 Pain intensity immediately after (VAS) | 1 | 31 | Mean Difference (IV, Random, 95% CI) | ‐1.46 [‐2.81, ‐0.11] |
| 5.12.2 Pain intensity short term (VAS) | 1 | 31 | Mean Difference (IV, Random, 95% CI) | 1.99 [0.56, 3.42] |
| 5.12.3 Quality of life immediately after (SF36) | 1 | 31 | Mean Difference (IV, Random, 95% CI) | 6.22 [‐1.54, 13.98] |
| 5.12.4 Quality of life short term (SF36) | 1 | 31 | Mean Difference (IV, Random, 95% CI) | ‐5.27 [‐11.27, 0.73] |
Comparison 6. Acupuncture plus intervention vs intervention alone.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 6.1 Acupuncture + standard therapy vs standard therapy | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1.1 Pain intensity immediately after (SF‐36 bodily pain, VAS (0 to 5)) | 2 | 187 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.70, ‐0.12] |
| 6.1.2 Pain intensity at short term (SF‐36 bodily pain, VAS (0 to 5)) | 2 | 187 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.49 [‐0.78, ‐0.20] |
| 6.1.3 Back‐specific function immediately after (SF‐36 physical, RMDQ) | 2 | 187 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.63, ‐0.05] |
| 6.1.4 Back‐specific function short term (SF‐ 36 physical, RMDQ) | 2 | 187 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.51 [‐0.80, ‐0.22] |
| 6.2 Acupuncture + standard therapy vs standard therapy | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.2.1 Quality of life immediately after (SF‐36 general health) | 1 | 143 | Mean Difference (IV, Random, 95% CI) | 8.20 [3.09, 13.31] |
| 6.2.2 Quality of life short term (SF‐ 36 general health) | 1 | 143 | Mean Difference (IV, Random, 95% CI) | 7.00 [0.95, 13.05] |
| 6.3 Acupuncture + standard therapy vs standard therapy | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 6.3.1 Adverse events | 1 | 44 | Risk Ratio (M‐H, Random, 95% CI) | 1.64 [0.70, 3.83] |
| 6.4 Acupuncture + exercise vs exercise | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.4.1 Pain intensity immediately after (VAS) | 1 | 45 | Mean Difference (IV, Random, 95% CI) | 0.49 [‐2.38, 3.36] |
| 6.4.2 Back‐specific function immediately after (ODI) | 1 | 45 | Mean Difference (IV, Random, 95% CI) | 3.94 [‐7.84, 15.72] |
| 6.4.3 Back‐specific function intermediate term (ODI) | 1 | 44 | Mean Difference (IV, Random, 95% CI) | ‐1.42 [‐14.03, 11.19] |
| 6.4.4 Quality of life immediately after (EQ‐5D) | 1 | 45 | Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.26, 0.16] |
| 6.4.5 Quality of life intermediate term (EQ‐5D) | 1 | 44 | Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.32, 0.12] |
| 6.5 Acupuncture + exercise vs exercise | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 6.5.1 Adverse events | 1 | 45 | Risk Ratio (M‐H, Random, 95% CI) | 11.48 [0.67, 196.07] |
| 6.6 Acupuncture + botulinum toxin type A vs botulinum toxin type A | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.6.1 Pain intensity immediately after (VAS 0 to10) | 1 | 43 | Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.92, 0.16] |
| 6.6.2 Back‐specific function immediately after (ODI) | 1 | 43 | Mean Difference (IV, Random, 95% CI) | ‐11.91 [‐19.02, ‐4.80] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Brinkhaus 2006.
| Study characteristics | ||
| Methods | Three‐arm RCT Number analyzed/randomized: 284/301 Statistical analysis: Intention‐to‐treat analysis (ITT); analysis of covariance (ANCOVA); power analysis Funding source: German social health insurance funds Ethical approval and informed consent obtained |
|
| Participants |
Participant recruitment: advertisement on local newspapers and by trial centers Setting: hospital outpatient units in Germany Inclusion criteria: 1) clinical diagnosis of chronic LBP lasting > 6 months; 2) aged 40 to 75; 3) average pain intensity of 40 or more (VAS, 0 to 100) in 7 days before acupuncture; 4) had taken only oral nonsteroidal anti‐inflammatory drugs (NSAIDs) for pain in the 4 weeks before the treatment Exclusion criteria: 1) protrusion or prolapse of one or more intervertebral discs with concurrent neurological symptoms; 2) radicular pain; prior vertebral column surgery; infectious spondylopathy; LBP caused by inflammatory, malignant, or autoimmune disease; 3) congenital deformation of the spine (except for slight lordosis or scoliosis); 4) compression fracture caused by osteoporosis, spinal stenosis, spondylolysis or spondylolisthesis; 5) patients with Chinese medicine diagnoses warranting treatment with moxibustion (determined by trial physicians); 6) any acupuncture treatment during the previous 12 months Age (mean ± SD): 58.8 ± 9.1 years Gender (female): 68% Pain duration (mean ± SD): 14.7 ± 11.1 years Pain intensity (mean ± SD): 64.8 ± 14.0 (VAS, 0 to 100) |
|
| Interventions |
1) GROUP 1: verum acupuncture (semi‐standardized) Acupuncture points: at least four bilateral local points (BL20 to 34, BL50 to 54, GB30, and GV3 to 6, Huatojiaji, and Shiqizhuixia); and at least two bilateral distant points (SI3, BL40, BL60, BL62, KI3, KI7, GB31, GB34, GB41, LV3, GV14, and GV20). If participants were experiencing local or pseudoradicular sensations, at least two local points were chosen. Other acupuncture points, including ear and trigger points, were chosen individually. Depth: not predefined De Qi: stimulated manually at least once Sessions: 12 sessions (30 min each, 2/week for 4 weeks + 1/week for 4 weeks) Acupuncturist experience: ≥ 140 hours of acupuncture training and ≥ 3 years of clinical practice 2) GROUP 2: minimal acupuncture Same treatment protocol as verum acupuncture, with exceptions for acupoints. At least 6 of 10 predefined non‐acupuncture points were needled bilaterally using a superficial insertion. These points were not in the lower back area. 3) GROUP 3: waiting list Participants received delayed verum acupuncture treatment after 8 weeks Co‐intervention: participants allowed to take oral NSAIDs during the treatment Duration of treatment: 8 wks Duration of follow‐up: 13 months after beginning of treatment |
|
| Outcomes |
1) Pain intensity: VAS (0 to 100); lower values better 2) Back‐specific function status: HFAQ; higher values better 3) Quality of life: SF‐36, higher values better 4) Pain‐related disability: pain disability index (PDI, 0 to 70), lower values better Assessment times: 8, 26, and 52 weeks after starting treatment Costs: NR Adverse effects: similar incidences between acupuncture groups; hematoma and bleeding most commonly reported |
|
| Notes |
Conclusion: "Acupuncture was more effective in improving pain than non‐acupuncture treatment in people with chronic LBP, whereas there were no significant differences between acupuncture and minimal acupuncture". Language: English For results, see comparisons 1 and 2. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation list generated by computer software |
| Allocation concealment (selection bias) | Low risk | Centralised telephone randomisation procedure used |
| Blinding of participants (performance bias) All outcomes | Unclear risk | Some degree of un‐blinding had arisen, based on testing, but not clear how much this affected outcomes. Testing suggested some degree of successful blinding of participants (P = 0.04). |
| Blinding of personnel /care providers (performance bias) All outcomes | Unclear risk | Did not describe the masking methods |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported whether the assessor was independent |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The dropout rate was 8% for each group and reasons were acceptable. |
| Intention‐to‐treat‐analysis (attrition bias) | Low risk | ITT analysis based on all available data; robustness analysis conducted |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Group similarity at baseline (selection bias) | Low risk | Similar baseline characteristics |
| Co‐interventions (performance bias) | High risk | Statistically significant differences for days with analgesics during last 3 weeks of acupuncture treatment |
| Compliance bias (performance bias) | Low risk | The compliance was acceptable and comparable across the groups. |
| Timing of outcome assessments (detection bias) | Low risk | Data on primary and secondary outcomes collected at the same time across groups |
| Other bias | Low risk | Not identified |
Carlsson 2001.
| Study characteristics | ||
| Methods | Three‐arm RCT Number analyzed/randomized: 27/50 Statistical analysis: Student's t test, Chi² test, Fisher exact test, Mann‐Whitney test, and Wilcoxon signed ranks test; power analysis not conducted Funding source: NR Ethical approval and informed consent obtained |
|
| Participants |
Participant recruitment: by referral Setting: Swedish university hospital Inclusion criteria: 1) lumbar or lumbosacral pain experienced for 6 months or longer; 2) no radiation of pain below knee; 3) normal neurological examination findings for lumbosacral nerve function, including deep tendon reflexes, plantar response, voluntary muscle activation, straight leg raising, and sensory function Exclusion criteria: 1) major trauma or systemic disease; 2) ongoing pregnancy; 3) history of acupuncture treatment Age (mean ± SD): 49.8 ± 15.4 years Gender (female): 66% Pain duration (mean ± SD): 9.5 ± 7.0 years Pain intensity: no significant difference in baseline pain intensity (VAS scale) |
|
| Interventions |
1) GROUP 1: manual acupuncture (semi‐standardized) Acupuncture points: some points on lower back (local points) and other points on lower limbs and forearms or hands (distal points; bilateral LI4, LI11, BL24, BL25, BL26, BL40, BL57, BL60, Yaoyan, and Jiaji) Depth: NR (30 to 70 mm needles) De Qi: stimulated three times during each treatment, usually at a depth of 2 to 3 cm Sessions: 10 (20 min; 1/week for 8 weeks; 9th at 6 months and 10th at 8 months). All three groups received same treatment schedule. Acupuncturist experience: board‐certified anesthesiologist with considerable acupuncture experience (> 10,000 treatments) 2) GROUP 2: electroacupuncture Two or three sessions of manual acupuncture administered, followed by treatments with electrical stimulation delivered by four needles (one pair on each side) to lower back. Stimulation frequency: 2 Hz every 2.5 seconds, interrupted by 15 Hz for 2.5 seconds (dense disperse) at perceptible but not painful stimulation intensity. Similar number of needles as used with the manual acupuncture group. Same schedule as Group 1. 3) GROUP 3: placebo Mock TENS administered by a disconnected stimulator attached to two large TENS electrodes. Electrodes placed on skin over most intensely painful area of low back. Flashing lamps visible to participant during stimulation. Same treatment schedule as Group 1 Co‐intervention: all participants permitted to take NSAIDs or weak opioids as needed Duration of treatment: 2 months for most of participants Duration of follow‐up: 6 months after the 8th session |
|
| Outcomes |
1) Pain intensity: VAS (0 to 100) recorded twice daily (morning and evening) 2) Global assessment of therapy effectiveness: classified as improved, unchanged, or worse, based on the results of clinical interviews on pain‐related disability and physical examination 3) Pain‐related disability: level of activity (at work or at home) recorded weekly. Change in workplace activity (at 6 months) Assessment times: 1, 3, and 6 months after the end of sessions Costs: NR Adverse effects: NR |
|
| Notes |
Conclusion: Compared with placebo, acupuncture had long‐term pain‐relieving effects for some people with chronic nonspecific LBP. Language: English Study not included in quantitative analysis for intermediate and long‐term follow‐up due to high dropout rates (44% at 3 months and 54% at 6 months) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation process was produced from a previously developed computer‐generated list. |
| Allocation concealment (selection bias) | Low risk | The randomized numbers were kept by a secretarial assistant who was not otherwise involved in the study. |
| Blinding of participants (performance bias) All outcomes | Low risk | Participants were told that they would receive three forms of stimulation, and were asked not to reveal to the independent observer what they were feeling. Blinding method not clearly described, but verification testing suggested some degree of successful blinding (P = 0.04) |
| Blinding of personnel /care providers (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Some outcomes measured by blinded assessor; other subjective outcomes recorded by participants, who may have been blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High dropout rate (44%) at second follow‐up due to subjects' failure to respond to treatment |
| Intention‐to‐treat‐analysis (attrition bias) | Unclear risk | Unclear whether ITT analysis was used; 44% (high) dropout rate |
| Selective reporting (reporting bias) | High risk | The outcomes were pooled from two acupuncture groups, which broke the randomisation and was unacceptable |
| Group similarity at baseline (selection bias) | Unclear risk | Doses of analgesic drug seemed not similar between the combined acupuncture groups and the placebo group. |
| Co‐interventions (performance bias) | Unclear risk | Could not be assessed because drugs were reported as pooled data of acupuncture groups |
| Compliance bias (performance bias) | Unclear risk | Most of the participants finished 8 of the 10 treatments; unclear if it was acceptable or comparable. |
| Timing of outcome assessments (detection bias) | Unclear risk | Global improvement at the third follow‐up was assessed between 6 and 48 months; others were assessed at the same time. |
| Other bias | Low risk | Not identified |
Cesare 2011.
| Study characteristics | ||
| Methods | Two‐arm RCT Number analyzed/randomized: 60/62 Statistical analysis: ITT analysis; ANCOVA; power analysis Funding source: NR Ethical approval and informed consent obtained |
|
| Participants |
Participant recruitment: at outpatient clinic directly Setting: outpatient clinic in Italy Inclusion criteria: 1) LBP > 6 months; 2) aged > 45 years; 3) no pharmacological therapy for other systemic pathologies; 4) no previous treatment with mesotherapy for chronic LBP Exclusion criteria: 1) presence of neurological pathologies; concomitant severe rheumatic disease; systemic pathologies (e.g. diabetes); 2) surgical intervention in 3 months prior to the study; 3) psychiatric pathologies or patients undergoing psychotherapeutic treatment or physical treatment in 5 weeks prior to the study Age (mean): 52.5 years Gender (female): 55% Pain duration (mean): 4.8 years Pain intensity (mean): 7.4 (VAS, 0 to 10) |
|
| Interventions |
1) GROUP 1: acupuncture mesotherapy (standardized) Local anesthetic (a drop of lidocaine, 2%) injected at 18 points for both groups before acupuncture. Acupuncture points: local bilateral points (GB30, BL31, BL52, GV3, Ashi points); bilateral distal points (GB34, GB41, BL60, KI4, TE5) Depth: NR De Qi: NR Sessions: 4 sessions (1/week for 4 weeks) Acupuncturist experience: 3 years of acupuncture training and 8 years of clinical experience 2) GROUP 2: trigger point mesotherapy A number of the 18 local superficial trigger points of the most important accessible muscles in lumbar tract and hip were treated (quadratus lumborum – 2 bilateral trigger points: one at the angle between the crest of the ilium and transverse processes of L4 and the other at the transverse processes of L1‐L2; iliopsoas muscle ‐ 2 paravertebral bilateral points: one on the D12 thoracic vertebrae and the other on L2 lumbar vertebrae; gluteus maximus – 3 bilateral trigger points: all on the medial superior portion of sacrum region; piriformis muscle – 2 bilateral points: one at the junction between the middle and the outer third of the piriformis line and the other one at medial end of piriformis line) Co‐intervention: none Duration of treatment: 4 weeks Duration of follow‐up: 12 weeks after starting treatment |
|
| Outcomes |
1) Pain intensity: VAS (0 to 10) and VRS (verbal rating scale, 0 to 6); lower values better 2) The quality and intensity of pain: McGill Pain Questionnaire (MPQ) Short Form, lower values better 3) Back‐specific function status: Roland Morris Disability Questionnaire (RMDQ, 0 to 24), and Oswestry Low Back Pain Disability Questionaire Index (ODI, 0 to 50); for both, lower values better Assessment times: 4 and 12 weeks after beginning of treatment Costs: NR Adverse effects: five participants in acupuncture group reported slight neck pain |
|
| Notes |
Conclusion: "Our results suggest that the response to ACP mesotherapy may be greater than the response to TRP mesotherapy in the short term follow‐up." Language: English For results, see comparison 5. Be cautious to the result related with the paper due to extremelly small SD values of pain reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used random numbers from a statistics textbook |
| Allocation concealment (selection bias) | Low risk | Used sealed, sequentially numbered, opaque envelopes |
| Blinding of participants (performance bias) All outcomes | Unclear risk | Authors claimed "blinding was maintained until the end of the study", but did not describe the details. |
| Blinding of personnel /care providers (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | VAS (pain) scores were recorded by participants reported to be blinded; other outcomes recorded by blinded assessor. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropout rate was low (< 5%) and the reasons were acceptable. |
| Intention‐to‐treat‐analysis (attrition bias) | Low risk | ITT analysis using last value carried forward for missing values |
| Selective reporting (reporting bias) | Low risk | All of the outcomes were reported. |
| Group similarity at baseline (selection bias) | Low risk | Similar baseline characteristics |
| Co‐interventions (performance bias) | Low risk | No co‐intervention was used. |
| Compliance bias (performance bias) | Low risk | All subjects completed the treatment. |
| Timing of outcome assessments (detection bias) | Low risk | The outcomes were collected at 4 and 12 weeks. |
| Other bias | Low risk | Not identified |
Chen 2010.
| Study characteristics | ||
| Methods | Four‐arm RCT Number analyzed/randomized: 100/100 Statistical analysis: did not mention ITT analysis; repeated measured Analysis of Variance (ANOVA); power analysis not conducted Funding source: NR Not reported if ethical approval and informed consent were obtained |
|
| Participants |
Participant recruitment: by referral Setting: an outpatient clinic at Department of Rehabilitation of a hospital in China Inclusion criteria: 1) LBP > 6 months; 2) negative response in straight‐leg raising test and intact on neurological examinations; 3) no findings in laboratory examination and X‐ray image; 4) not received acupuncture or TENS in previous 6 months Exclusion criteria: 1) LBP due to trauma or severe disease; 2) required analgesics during acupuncture treatment Age (mean ± SD): NR Gender (female): NR Pain duration (mean ± SD): NR Pain intensity (mean): 65.1 (VAS, 0 to 100) |
|
| Interventions |
1) GROUP 1: acupuncture (semi‐standardized) Acupuncture points: shenshu, dachangshu, yaoyangguan, shangjiao, jiaji, cijiao, weizhong, kunlun, huantiao, yanlingquan and Ashi point (4 to 6 points chosen) Depth: 32 gauge filiform needle inserted vertically to a depth of 1 to 1.2 inches De Qi: retention of needles for 1 min after De Qi sensation was elicited manually Sessions: 5 sessions (1/week for 5 weeks) Acupuncturist experience: NR 2) GROUP 2: TENS Equipment setting: frequency 1 to 160 Hz, wave width 2 to 500 μs, one phrase or biphasic wave; placing electrodes on trigger points or other locations in pain; adjusting current intensity at perceptible but not painful stimulation intensity during 15 min stimulation at each session; same schedule as Group 1 3) GROUP 3: acupuncture + TENS 15 min TENS + 15 min acupuncture at each session; same techniques and treatment schedule as Group 1 and 2 4) GROUP 4: sham TENS Same setting as TENS group, but no electrical current delivered when lights shining Co‐intervention: NR Duration of treatment: 5 weeks Duration of follow‐up: 10 weeks after beginning of treatment |
|
| Outcomes |
1) Pain intensity: VAS (0 to 100) 2) Back‐specific function status: Roland Morris Disability Questionnaire (RMDQ, 0 to 24) Assessment times: immediately after and 5 weeks after the end of sessions Costs: NR Adverse effects: NR |
|
| Notes |
Conclusion: acupuncture + TENS group provided better effect than the other two groups. Language: Chinese For results, see comparisons 4 and 5 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear how randomisation was conducted |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding of participants (performance bias) All outcomes | Unclear risk | Not mentioned if subjects were blinded. It was only possible to blind participants in the control and acupuncture + TENS groups. |
| Blinding of personnel /care providers (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Participants reported subjective outcomes; unclear if participants were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The dropout rate was 6%, but it was unclear if it related to the treatment. |
| Intention‐to‐treat‐analysis (attrition bias) | Unclear risk | Participants were analyzed according to group assignment, but the authors did not report how to deal with 6% missing data. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Group similarity at baseline (selection bias) | Unclear risk | The study claimed similar baselines but no P values were given. |
| Co‐interventions (performance bias) | Low risk | Not mentioned |
| Compliance bias (performance bias) | Unclear risk | The numbers of sessions received by groups or the compliance were not reported. |
| Timing of outcome assessments (detection bias) | Low risk | Similar |
| Other bias | Low risk | Not identified |
Chen 2016.
| Study characteristics | ||
| Methods | Two‐arm RCT Number analyzed/randomized: 43/43 Statistical analysis: ITT analysis; Student's t‐test and Chi² test; power analysis not conducted Funding source: NR Not reported if ethical approval, informed consent were obtained |
|
| Participants |
Participant recruitment: by referral Setting: an outpatient clinic at Department of Rehabilitation of a hospital at China Inclusion criteria: 1) LBP > 3 months without intermittent claudication; 2) no specific etiology found; 3) no findings in X‐ray image; 4) no history of surgery and trauma Exclusion criteria: 1) did not sign the consent; 2) had severe disease or mental illness; 3) pregnant or breastfeeding Age (mean): 40.3 years Gender (female): 35% Pain duration (mean): 30.1 months Pain intensity (mean): 5.47 (VAS, 0 to 10) |
|
| Interventions |
1) GROUP 1: electroacupuncture (standardized) + botulinum toxin type A Acupuncture points: 3 pairs of Jiaji acupoints around the tender points Depth: needles (0.35 mm × 50 mm) inserted to a depth of 10 to 15 mm toward the spine De Qi: electrical stimulation for 30 min after De Qi sensation elicited Sessions: 18 sessions (6/week for 3 weeks) Botulinum toxin type A injection is same as Group 2 Acupuncturist experience: NR 2) GROUP 2: botulinum toxin type A Inject with botulinum toxin type A at a dose of 5 IU/0.1 mL at 6 to 8 tender points on both sides of the spine 3) Co‐intervention: NR Duration of treatment: 3 weeks Duration of follow‐up: immediately after the end of sessions |
|
| Outcomes |
1) Pain intensity: VAS (0 to 10) 2) Back‐specific function status: Improved Oswestry Disability index (ODI, 0 to 100); lower values better Assessment times: immediately after the end of sessions Costs: NR Adverse effects: NR |
|
| Notes |
Conclusion: "Electroacupunture with botulinum toxin type A has a better treatment efficacy on chronic LBP than botulinum toxin type A alone." Language: Chinese For results, see comparisons 6. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used table of random number |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding of participants (performance bias) All outcomes | Unclear risk | Not mentioned |
| Blinding of personnel /care providers (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participant dropped out immediately after the treatment. |
| Intention‐to‐treat‐analysis (attrition bias) | Low risk | The analyses were conducted according to their randomisation group. |
| Selective reporting (reporting bias) | Low risk | Both pain and function outcomes were reported. |
| Group similarity at baseline (selection bias) | Low risk | Baseline characteristics were similar between two groups. |
| Co‐interventions (performance bias) | Low risk | The authors did not mention whether additional co‐interventions were given. |
| Compliance bias (performance bias) | Unclear risk | The authors did not report compliance. |
| Timing of outcome assessments (detection bias) | Low risk | Both groups had the outcomes measured in the immediate term. |
| Other bias | Low risk | Not identified |
Cherkin 2009.
| Study characteristics | ||
| Methods | Four‐arm RCT Number analyzed/randomized: 583/641 Statistical analysis: ITT analysis; Chi² and ANOVA test; power analysis Funding source: NIH Cooperative Agreement (U01 AT 001110) Ethical approval and informed consent obtained |
|
| Participants |
Participant recruitment: mail, advertisements, and newsletters Setting: two research clinics in western Washington and northern California in USA Inclusion criteria: 1) participants planned to continue enrolment in health plan; 2) 18 to 70 years; 3) at least one primary care visit for back pain within the past 3 to 12 months; 4) nonspecific and uncomplicated LBP; 5) physician was willing to have patients included in the study; 6) lived within 45 min travel time from study clinic Exclusion criteria: 1) specific causes of back pain (e.g. cancer, fractures, spinal stenosis, infections); 2) complicated back problems (e.g. sciatica, prior back surgery, medicolegal issues); 3) possible contraindications for acupuncture (e.g. coagulation disorders, cardiac pacemakers, pregnancy, seizure disorder); 4) conditions making treatment difficult (e.g. paralysis, psychoses); 5) conditions that might confound treatment effects or interpretation of results (e.g. severe fibromyalgia, rheumatoid arthritis, concurrent care from other providers) Age (mean): 47 Gender (female): 62% Pain duration (reported ≥ 1 yr): 2/3 participants Pain intensity (mean): NR |
|
| Interventions |
1) GROUP 1: acupuncture (standardized) Acupuncture points: bilateral BL23, BL40, KI3, Ashi point, and Du3 (8 points in total) Depth: NR De Qi: 20 min treatment with 10 min stimulation by twirling the needles just prior to needle removal to elicit De Qi Sessions: 10 sessions (20 min, 2/week for 3 weeks + 1/week for 4 weeks) Acupuncturist experience: six licensed acupuncturists with experience of 4 to 19 years 2) GROUP 2: individualized acupuncture The treatment was prescribed by an acupuncturist diagnostician at each visit. Average of 10.8 needles (range, 5 to 20) retained for a mean of 18 min (range, 15 to 20 min) were used. Seventy‐four distinct points were used, half on the bladder meridian, which includes points on the back and legs. No constraints on depth or manipulation. Treatment schedule and others were same as Group 1. 3) GROUP 3: sham acupuncture The acupuncturists simulated the insertion and the removal of needles at the eight standardized acupuncture points. A toothpick in a needle guide tube was used, which was found to be a credible acupuncture treatment by acupuncture‐naive participants with back pain. All acupuncture points were stimulated at 10 min with the tip of a toothpick and again at 20 min just before they were 'removed'. Participants were asked to wear eye masks and lie prone, with their heads in a face cradle. Same treatment schedule as Group 1 4) GROUP 4: usual care Participants received usual care that they and their physicians chose (mostly medications, primary care, and physical therapy visits). Co‐intervention: a self‐care book with information on managing flare‐ups, exercise, and lifestyle modifications Duration of treatment: 7 weeks Duration of follow‐up: 52 weeks after beginning of treatment |
|
| Outcomes |
1) Back‐specific function status: RMDQ (0 to 23), lower values better 2) Quality of life: sub‐scale of SF‐36 in physical health and mental health; higher values better 3) Pain‐related disability: cutting down on activities for more than 7 days in the past month (%); missed work or school for more than a day in the past month (%); no accurate data provided for sham and true acupuncture Assessment times: 8, 26, and 52 weeks after beginning of treatment Costs: NR (the reported total costs excluded acupuncture spending) Adverse effects: 12 of 477 participants in real acupuncture groups reported pain, dizziness, and back spasms. |
|
| Notes |
Conclusion: "Acupuncture was found effective for chronic LBP, tailoring needling sites to each participant and penetration of the skin appear to be unimportant in eliciting therapeutic benefits." Language: English For results, see comparisons 1, 3, and 5. The data for pain‐related disability were not extracted for meta‐analysis, because the study only reported a range of 5% to 10% in the acupuncture group. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A centrally generated variable‐sized block design |
| Allocation concealment (selection bias) | Low risk | "The random assignments cannot be viewed in advance and cannot be changed after randomisation.” |
| Blinding of participants (performance bias) All outcomes | Low risk | Participants in the three acupuncture groups were blinded, with credibility assessed. Participants were asked to wear eye masks and lie prone with their heads in a face cradle. Participants rated the acupuncture and simulated acupuncture treatments almost identically with regard to provider skills and caring. |
| Blinding of personnel /care providers (performance bias) All outcomes | Unclear risk | Although masking of acupuncturist is not possible, this design employed a diagnostician acupuncturist who made the diagnoses and determined which acupuncture points should be applied. An experienced therapist acupuncturist then delivered the assigned treatments, interacting minimally with participants and the diagnostician, who remained masked to treatment. The diagnostician acupuncturists rated the acupuncture and simulated acupuncture groups very similarly with regard to apparent efficacy and likelihood of receiving individualized treatment. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Assessor was blinded, and the subjective outcomes were reported by masked participants. Outcomes were measured using computer‐assisted telephone interviews by interviewers masked to treatment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropout rates (5% at 8 weeks and 9% at 52 weeks); the reasons were given and acceptable. |
| Intention‐to‐treat‐analysis (attrition bias) | Low risk | The analyses were conducted according to their randomisation allocation, regardless of treatment compliance. |
| Selective reporting (reporting bias) | Low risk | All outcomes in the protocol were reported. |
| Group similarity at baseline (selection bias) | Low risk | Similar baseline characteristics |
| Co‐interventions (performance bias) | Unclear risk | Participants in the usual care group were visited by a physical therapist twice compared to acupuncture groups. Unclear whether the co‐interventions were different across the groups |
| Compliance bias (performance bias) | Low risk | Comparable compliance rates were more than 80% across the groups. |
| Timing of outcome assessments (detection bias) | Low risk | Same assessment time |
| Other bias | Low risk | Not identified |
Cho 2013.
| Study characteristics | ||
| Methods | Two‐arm RCT Number analyzed/randomized: 116/130 Statistical analysis: per‐protocol analysis; Student's t‐test and mixed model; power analysis Funding source: Korea Health Industry Development Institute (B080048) Ethical approval and informed consent obtained |
|
| Participants |
Participant recruitment: local newspapers, hospital's magazine, website, and bulletin boards Setting: three medical hospitals in Korea Inclusion criteria: 1) chronic LBP ≥ 3 months before acupuncture treatment; 2) baseline VAS (bothersomeness, 0 to 10) > 5 points; 3) nonspecific and uncomplicated LBP that was intact on neurological examination Exclusion criteria: 1) sciatic pain; 2) pain mainly below knee; 3) serious spinal disorders including malignancy, vertebral fracture, spinal infection, inflammatory spondylitis, and cauda equine compression; 4) history of previous spinal surgery Age (mean ± SD): 42.1 ± 14.0 years Gender (female): 85% Pain duration (mean ± SD): NR Pain intensity (mean ± SD): 6.45 ± 1.30 (VAS, 0 to 10) |
|
| Interventions |
1) GROUP 1: verum acupuncture (semi‐standardized) Acupuncture points (according to the diagnosis): gallbladder meridian pattern ‐ GB12, GB26, GB30, GB34, GB41; bladder meridian pattern ‐ BL23, BL24, BL25, BL37, BL40; mixed pattern: ST4, ST36, SP13, SP14, GV3, GV4, GV5, GV24, and GV26 Depth: needles inserted vertically to a depth of 5 to 20 mm, depending on the site De Qi: needles left in situ for 15 to 20 min after De Qi sensation elicited by manual stimulation Sessions: 12 sessions (2/week for 6 weeks) Acupuncturist experience: licensed Korean Medicine Doctors with at least 3 years experience 2) GROUP 2: sham acupuncture Same technique and protocol as verum acupuncture except that semi‐blunt needles were used without penetration on 8 predefined non‐acupuncture points (1 cm below BL39, 1 cm lateral to BL18 and BL20, and 2 cm above GB30, all bilaterally) 3) Co‐intervention: participants were requested to do exercises every day according to the given manual; any additional therapy was prohibited. Duration of treatment: 6 weeks Duration of follow‐up: 24 weeks |
|
| Outcomes |
1) Pain intensity: VAS (0 to 10) 2) Back‐specific function status: Oswestry Disability Index (ODI, 0 to 50) 3) Quality of life: SF‐36, higher values better Assessment times: 6,8,12, and 24 weeks after beginning of treatment Costs: NR Adverse effects: 16/27 participants reported minor to moderate adverse events, none of which persisted longer than 1 weeks. |
|
| Notes |
Conclusion: “This randomised sham‐controlled trial suggests that acupuncture treatment shows better effect on the reduction of the bothersomeness and pain intensity than sham control in participants with chronic LBP.” Language: English Using the baseline SDs of SF‐36 and ODI as the corresponding SDs of the results in meta‐analysis For results, see comparison 1. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation code generated by computer |
| Allocation concealment (selection bias) | Low risk | The random code was kept by a clinician who did not contact participants. |
| Blinding of participants (performance bias) All outcomes | Low risk | Subjects were blinded and assessment showed adequate blinding. |
| Blinding of personnel /care providers (performance bias) All outcomes | Unclear risk | Unclear if acupuncturist was successfully blinded or not |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinded participants reported the outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Acceptable and balanced dropout rate (11%) across groups; the reasons were largely acceptable. |
| Intention‐to‐treat‐analysis (attrition bias) | High risk | The study used per protocol analysis. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Group similarity at baseline (selection bias) | Unclear risk | The baseline ODI scores in the acupuncture group were significantly higher. |
| Co‐interventions (performance bias) | Unclear risk | Unclear risk because the usual care group was visited by a physical therapist twice more than the acupuncture groups. |
| Compliance bias (performance bias) | Low risk | Subjects were asked to complete > 80% treatments, and they possibly did, according to the report. |
| Timing of outcome assessments (detection bias) | Low risk | Same assessment time |
| Other bias | Low risk | Not identified |
Grant 1999.
| Study characteristics | ||
| Methods | Two‐arm RCT Number analyzed/randomized: 56/60 Statistical analysis: unclear if ITT analyses were used; Wilcoxon signed ranks tests, Mann‐Whitney U‐tests, Student's t‐test; power analysis Funding source: Trustees of the Liberton Hospital Endowment Funds Ethical approvals were obtained, but the authors did not mention if participants consented. |
|
| Participants |
Participant recruitment: General practitioners referred suitable participants. Setting: at two hospitals or at home, according to participant's preference, Scotland, UK Inclusion criteria: people ≥ 60 years with back pain for at least 6 months Exclusion criteria: 1) treatment with anticoagulants, treatment with systemic corticosteroids; 2) dementia; 3) previous treatment with acupuncture or TENS; 4) cardiac pacemaker, other severe concomitant disease, inability of person to apply TENS machine Age (mean): 71.0 years Gender (female): 90% Pain duration (mean ± SD): NR Pain intensity (median): 120.5 (VAS, 0 to 200) |
|
| Interventions |
1) GROUP 1: acupuncture (individualized) Acupuncture points: points were chosen individually, but only on the back; 6 needles used on average (range 2 to 8) Depth: NR De Qi: NR Sessions: 8 sessions (20 min, 2/week for 4 weeks) Acupuncturist experience: physiotherapist conducted the treatment but the experience was not reported. 2) GROUP 2: TENS TENS treatment used 50 Hz stimulation and intensity was adjusted to suit the participant; participants were given the treatment daily at home for ≤ 30 min per session and ≤ 6 hours per day; participants seeing physiotherapist for 20 min twice weekly Co‐intervention: continue existing medication Duration of treatment: 4 weeks Duration of follow‐up: 3 months after the end of sessions |
|
| Outcomes |
1) Pain intensity: VAS (0 to 200) and pain subscale of the 38‐item Nottingham Health Profile Part 1 (NHP), lower values better Assessment times: 4 days and 3 months after the end of sessions Costs: NR Adverse effects: three participants receiving acupuncture reported dizziness; three participants having TENS developed skin reactions. |
|
| Notes |
Conclusion: "This trial cannot exclude the possibility that both treatments are placebos." Language: English For results, see comparison 4. The median (IQR) of VAS was transferred into 0‐100 scale by dividing 2; mean (SD) data of VAS was calculated from median (IQR) using the formula 'IQR = 1.35*SD'. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers were used. |
| Allocation concealment (selection bias) | Low risk | Sequenced and sealed envelopes were used. |
| Blinding of participants (performance bias) All outcomes | Unclear risk | Unclear if it was possible between two groups at two locations |
| Blinding of personnel /care providers (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Measurements were made by an independent observer; some subjective outcomes were reported by participants for whom it was unclear if they were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low dropout rate (7%) and reasons for withdrawal were acceptable |
| Intention‐to‐treat‐analysis (attrition bias) | Unclear risk | The subjects were analyzed according to groups assigned, but unclear how they dealt with the dropouts. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Group similarity at baseline (selection bias) | Unclear risk | Baselines NHP pain scores were of borderline statistical significance: P = 0.064. |
| Co‐interventions (performance bias) | Low risk | Baselines analgesics were similar, and the tablets were recorded as one of the outcomes. |
| Compliance bias (performance bias) | Unclear risk | The study did not report the number of sessions that the acupuncture and TENS groups really had, nor the attendance. |
| Timing of outcome assessments (detection bias) | Low risk | Same assessment time |
| Other bias | Low risk | Not identified |
Haake 2007.
| Study characteristics | ||
| Methods | Three‐arm RCT Number analyzed/randomized: 1117/1802 Statistical analysis: ITT analysis; Fisher exact test; power analysis Funding source: German public health insurance companies Ethical approval and informed consent obtained |
|
| Participants |
Participant recruitment: newspapers, magazines, radio, and television Setting: 340 outpatient practices in Germany Inclusion criteria: 1) clinical diagnosis of chronic LBP (≥ 6 months); 2) Van‐Korff Pain Score ≥ Grade I and HFAQ < 70%; 3) therapy‐free interval ≥ 7 days; 4) aged older than 18 years; ability to speak, read, and write German; 5) no previous treatment with needle‐acupuncture for chronic LBP Exclusion criteria: 1) previous treatment with acupuncture for any other indication in the last year; 2) sciatica or other neurologic disorders; 3) history of disc or spinal surgery; 4) history of fracture of the spine (e.g. osteoporosis, trauma); 5) infections or tumors of the spine; 6) systemic bone or joint disorders (e.g. rheumatoid arthritis); 7) scoliosis, kyphosis; 8) hemorrhagic disorders or anticoagulant therapy; 9) skin disease in the area of acupuncture; 10) chronic pain caused by other diseases; 11) abuse of drugs or pain medication; 12) pregnancy; 13) epilepsy; 14) person included in other studies Age (mean ± SD): 50 ± 15 years Gender (female): 60% Pain duration (mean): 8 years Pain intensity (mean): 67.8 (Von Korff Chronic Pain Grade Scale – 3 sub‐scales in pain, 0 to 100) |
|
| Interventions |
1) GROUP 1: verum acupuncture (semi‐standardized) Acupuncture points: fixed points and additional points (from a prescribed list) chosen individually on the basis of traditional Chinese medicine diagnosis Depth: 14 to 20 needles inserted to a depth of 5 to 40 mm, depending on the site De Qi: by manual stimulation Sessions: 10 sessions (30 min, 2/week for 5 weeks); 5 additional sessions if subjects experienced a 10% to 50% reduction in pain intensity after the 10th session Acupuncturist experience: physicians of various specialisations who had at least 140 hours of acupuncture training in Germany 2) GROUP 2: sham acupuncture Standardized points on either side of the lateral part of the back and on the lower limbs to avoid all known verum points or meridians; 14 to 20 needles inserted superficially (1 to 3 mm), without stimulation 3) GROUP 3: conventional therapy The treatment included 10 sessions with personal contact with a physiotherapist who administered physiotherapy, exercise, etc. Physiotherapy was supported by NSAIDs or pain medication up to the maximum daily dose during the therapy period. Co‐intervention: for acute episodes of pain, only rescue medication was permitted in all three groups (NSAIDs for ≤ 2 days per week, up to the maximum daily dose during the therapy period and only 1 day per week during follow‐up). Use of any additional therapies for pain during the entire study period was prohibited. Duration of treatment: 6 weeks Duration of follow‐up: 6 months after beginning of treatment |
|
| Outcomes |
1) Pain intensity: CPGC‐pain (0 to 100) and numbers of participants with 33% improvement of CPGC‐pain; lower values better 2) Back‐specific functional status: HFAQ (0 to 100) and numbers of participants with 12% improvement of HFAQ; higher values better 3) Quality of life: subscales of SF‐12 in physical and mental health component; higher values better 4) Global assessment: 6‐point scale, with 1 meaning very good and 6 meaning fail Assessment times: 6 weeks, 3 months, and 6 months after beginning of treatment Costs: NR Adverse effects: 476 clinically relevant adverse effects were reported by 257 participants (22.6%) with no difference between therapy groups (P = 0.81). |
|
| Notes |
Conclusion: "Low back pain was improved after acupuncture treatment for at least 6 months; effectiveness of acupuncture, either verum or sham, was almost twice that of conventional therapy". Language: English For results, see comparisons 1, 3 and 4. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Stratified randomisation was generated by computer program. |
| Allocation concealment (selection bias) | Low risk | Allocation was done by fax. |
| Blinding of participants (performance bias) All outcomes | Low risk | Participants were blinded between verum and sham acupuncture, and credibility was tested. |
| Blinding of personnel /care providers (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Assessors were blinded and blinded participants reported some outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Dropout rates at each time point were around twice higher in the conventional group than acupuncture groups. Reasons for missing were not reported. |
| Intention‐to‐treat‐analysis (attrition bias) | Low risk | The primary analysis used ITT. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Group similarity at baseline (selection bias) | Low risk | Baseline characteristics were similar. |
| Co‐interventions (performance bias) | High risk | Rescue medication was taken differently between acupuncture and conventional groups. |
| Compliance bias (performance bias) | Low risk | Similar average sessions were received by subjects among the 3 groups, which was acceptable. |
| Timing of outcome assessments (detection bias) | Low risk | Not identified |
| Other bias | Low risk | Not identified |
Hunter 2012.
| Study characteristics | ||
| Methods | Two‐arm RCT Number analyzed/randomized: 44/52 Statistical analysis: not conducted because it was a feasibility study (trial registration number ISRCTN94142364) Funding source: Research and Development Office, Northern Ireland, Strategic Priority Funding and Department for Employment and Learning, Northern Ireland, UK Ethical approval and informed consents obtained |
|
| Participants |
Participant recruitment: by general practitioner Setting: NR Inclusion criteria: 1) having chronic nonspecific LBP for at least 12 weeks; 2) if there was associated buttock and leg pain, back pain must be the chief complaint; 3) ≥ 60 years; 4) having an imaging check of the lumbar spine within the past year Exclusion criteria: 1) spinal tumor, infection or fracture; a bleeding diathesis; epilepsy; a cardiac arrhythmia or pacemaker; dementia; any serious, active medical condition that precluded safe participation (i.e. myocardial infarction within the past 3 months); 2) neurological involvement (loss of sensation, motor weakness or loss of reflexes); planned or scheduled lumbar surgery; a history of lumbar surgery; a significant psychiatric disability; inflammatory arthritis; 3) prior use of acupuncture for back pain; 4) uses of systemic corticosteroids, muscle relaxants, narcotic medications, anticoagulants, and epidural steroid injections within the past 3 months; the involvement in litigation related to back pain; 5) refusal to be randomized Mean age: 42.8 years Gender (female): 63 % Pain duration (mean ± SD): 9.9 ± 9 years Pain intensity (mean): 4.6 (VAS, 0 to 10) |
|
| Interventions |
1) GROUP 1: auricular acupuncture + exercise (standardized) Acupuncture points: Shen Men, Lumbar Spine, and Cushion Depth: NR De Qi: NR Sessions: used conventional auricular stud needles during the first 6 weeks before each exercise class, and left the needles in situ for 48 hours Acupuncturist experience: two chartered physiotherapists 2) GROUP 2: exercise The participants had exercises for 1 hour per week for 6 weeks: "The exercise program consisted of a 10 min warm‐up, a series of exercise stations involving core strengthening, flexibility, and cardiovascular exercise, a 10 min cool down, and a period of relaxation. Each exercise station consisted of three levels: easy, moderate, and hard". "This exercise program is underpinned by cognitive behavioural therapy principles designed to change participants behaviour by modifying their attitude to their LBP.” Co‐intervention: received a 12‐week intervention program consisting of 6 weeks of supervised exercise followed by 6 weeks of unsupervised exercise with telephone support Duration of treatment: 12 weeks Duration of follow‐up: 6 months |
|
| Outcomes |
1) Pain intensity: VAS (0 to 10) 2) Back‐specific function status: ODI (0 to 50) 3) Quality of life: EuroQol 5D (EQ‐5D, ‐0.59 to 1); higher values better 4) Others relevant: IPAQ‐MET, International Physical Activity Questionnaire‐MET/min/week; HHQ‐CAM, Holistic Complementary and Alternative Health Questionnaire‐Complementary and Alternative Medicine; HHQ‐HH, Holistic Complementary and Alternative Health Questionnaire‐Holistic Health subscale Assessment times: 13 weeks and 6 months after beginning of treatment Costs: NR Adverse effects: pain (14%), redness (2%), and minor bleeding (1%) at the site of needle insertion; swelling (n = 1) around the needle insertion site due to rheumatoid arthritis |
|
| Notes |
Conclusion: Auricular acupuncture was safe and demonstrated additional benefits when combined with exercise for people with chronic LBP, which requires confirmation in a fully powered RCT. Language: English For results, see comparison 6. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers were generated by computer. |
| Allocation concealment (selection bias) | Low risk | Kept in secured location and only accessible by an independent trial statistician |
| Blinding of participants (performance bias) All outcomes | High risk | Not possible between the studied groups |
| Blinding of personnel /care providers (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Unblinded participants reported the subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropout rates were < 20% and comparable between groups; the reasons were acceptable. |
| Intention‐to‐treat‐analysis (attrition bias) | Unclear risk | A feasibility RCT without statistical analysis |
| Selective reporting (reporting bias) | Unclear risk | No reported P value |
| Group similarity at baseline (selection bias) | Low risk | Similar baselines |
| Co‐interventions (performance bias) | High risk | Higher percentage of participants in the exercise group thought that the treatment received had changed the number of pain relieving tablets. |
| Compliance bias (performance bias) | Unclear risk | Exercise group had 8% higher attendance rate than AA + exercise group. |
| Timing of outcome assessments (detection bias) | Low risk | Same assessment time |
| Other bias | Low risk | Not identified |
Itoh 2009.
| Study characteristics | ||
| Methods | Four‐arm RCT Number analyzed/randomized: 26/32 Statistical analysis: did not mention ITT analysis; ANOVA with Bonferroni correction; power analysis not conducted Funding source: NR Ethical approval and informed consents obtained |
|
| Participants |
Participant recruitment: from outpatients at Meiji University of Oriental Medicine Hospital, Japan Setting: NR Inclusion criteria: 1) age ≥ 60 years; 2) lumbar or lumbosacral LBP ≥ 6 months; 3) no radiation of LBP; 4) normal neurological findings of lumbosacral nerve, including deep tendon reflexes, plantar response, voluntary muscle action, straight‐leg raising, and sensory function; 5) did not receive acupuncture treatment for past 6 months Exclusion criteria: 1) major trauma or systemic disease; 2) receiving conflicting or ongoing co‐interventions; 3) patients under drug treatment were included if there had been no change in medicine and the dosage for at least 1 month. Age (range): 61 to 80 years Gender (female): 62.5% Pain duration (mean ± SD): NR Pain intensity (mean ± SD): 62.4 (VAS, 0 to 100) |
|
| Interventions |
1) GROUP 1: acupuncture (standardized) Acupuncture points: BL23, BL25, BL32, BL40, BL60, GB30, GB34 Depth: 10 mm De Qi: needles inserted using "sparrow pecking" technique until De Qi achieved with 10 min needles' retention Sessions: 5 sessions (15 min, 1/week for 5 weeks) Acupuncturist experience: acupuncturists had 4 years of acupuncture training and 3 to 8 years of clinical experience. 2) GROUP 2: TENS Surface disposable electrodes of 809 mm² and 5688 mm² were placed on the points with the most tenderness and the near side of the points for 15 min, with frequency of 122 Hz. The intensity of TENS adjusted to subject's feedback. Same schedule as Group 1 3) GROUP 3: acupuncture + TENS 15 min TENS following 15 min acupuncture at affected lower back; same schedule as Group 1 4) GROUP 4: control (no treatment) Did not receive any specific treatment, but allowed to use topical poultice containing methylsalicylate acid when needed Co‐intervention: not taking any other co‐interventions during the study period Duration of treatment: 5 weeks Duration of follow‐up: 10 weeks |
|
| Outcomes |
1) Pain intensity: VAS (0 to 100) 2) Back‐specific function status: RMDQ (0 to 24) Assessment times: 5 weeks and 10 weeks after beginning of treatment Costs: NR Adverse effects: one participant in the acupuncture + TENS group dropped out due to deterioration of symptoms. |
|
| Notes |
Conclusion: Combined acupuncture and TENS treatment is effective for pain relief and function for people suffering from chronic LBP. Language: English For results, see comparisons 2, 4 and 5. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The random numbers were generated by computer software. |
| Allocation concealment (selection bias) | Unclear risk | Not reported whether the concealment was done or not |
| Blinding of participants (performance bias) All outcomes | High risk | Not possible |
| Blinding of personnel /care providers (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | It was not reported who assessed the outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Six subjects (18.8%) dropped out, five of them because they did not respond to treatment. |
| Intention‐to‐treat‐analysis (attrition bias) | High risk | Five subjects who did not respond to treatment were excluded in the data analysis. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Group similarity at baseline (selection bias) | Low risk | Similar baselines |
| Co‐interventions (performance bias) | Low risk | No co‐intervention |
| Compliance bias (performance bias) | Low risk | Acceptable and comparable compliance across the groups |
| Timing of outcome assessments (detection bias) | Low risk | Same assessment time |
| Other bias | Low risk | Not identified |
Kerr 2003.
| Study characteristics | ||
| Methods | Two‐arm RCT Number analyzed/randomized: 40/60 Statistical analysis: did not mention ITT analysis; Student's t test and Chi² test; power analysis Funding source: Department of Health and Social Services for Northern Ireland Ethical approval and informed consents obtained |
|
| Participants |
Participant recruitment: referred by general practitioners in local hospitals in Northern Ireland Setting: NR Inclusion criteria: 1) LBP > 6 months, with or without leg pain, and with no neurologic deficits; 2) happy to have acupuncture or another treatment, willing to participate in the trial and to undergo the assessment procedures Exclusion criteria: 1) contraindications to acupuncture therapy, age < 18 years, pregnancy, 2) underlying systemic disorders, diagnoses of rheumatoid arthritis, osteoarthritis of the spine, or cancer Age (mean ± SD): 41 ± 12.6 years Gender (female): 53.3% Pain duration (mean ± SD): 75.8 ± 75.2 months Pain intensity (mean ± SD): 77.9 (VAS, 0 to 100) |
|
| Interventions |
1) GROUP 1: acupuncture (standardized) Acupuncture points: BL23, BL25, BL40, GB30, KI3 (all bilateral), and GV4 Depth: NR De Qi: needles manually rotated to produce De Qi sensation initially, and at 10 and 20 min intervals, respectively Sessions: 6 sessions (30 min, 1/week for 6 weeks) Acupuncturist experience: chartered physiotherapist trained in acupuncture 2) GROUP 2: sham TENS A nonfunctioning TENS machine was attached to four electrodes and placed over the lumbar spine. The unit was switched on, but the circuit was broken between the unit and the participant. Same treatment schedule as Group 1 Co‐intervention: participants were given a leaflet regarding their LBP that included standardized advice and exercises Duration of treatment: 6 weeks Duration of follow‐up: 6 months |
|
| Outcomes |
1) Pain intensity: VAS (0 to 100) and Pain Rating Index (PRI) of McGill Pain Questionnaire (MPQ); lower values better 2) Quality of life: SF‐36 3) Global assessment: percentages of pain relief events at 6 months Assessment times: 6 weeks and 6 months after beginning of treatment Costs: NR Adverse effects: two participants (acupuncture group) reported other pain but not LBP becoming more manifest; one reported pain in legs and the other reported intensified pain (TENS group) |
|
| Notes |
Conclusion: "This study clearly shows that there was an improvement over time in both the acupuncture and placebo‐TENS groups." Language: English For results, see comparison 1. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The random numbers were generated by computer software. |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias) All outcomes | Low risk | Patents were informed that they would receive 1 of 2 different forms of treatment; possible blinding between acupuncture and TENS‐placebo groups |
| Blinding of personnel /care providers (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | A blinded assessor carried out assessments and some subjective outcomes were reported by participants. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | The short‐term dropout rates exceeded 20%. |
| Intention‐to‐treat‐analysis (attrition bias) | High risk | The authors did not report using ITT analysis; 14 subjects were excluded from the analyses, 5 of them due to no benefit from the treatment. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Group similarity at baseline (selection bias) | Unclear risk | Unable to verify similar baselines of age and duration of pain |
| Co‐interventions (performance bias) | Low risk | The authors did not report different co‐intervention used between groups. |
| Compliance bias (performance bias) | Unclear risk | The noncompliance rate was 23%; unclear whether it was comparable between the two groups, and the possible influence on the outcomes |
| Timing of outcome assessments (detection bias) | Low risk | Same assessment time |
| Other bias | Low risk | Not identified |
Leibing 2002.
| Study characteristics | ||
| Methods | Three‐arm RCT Number analyzed/randomized: 94/132 Statistical analysis: ITT analysis, using last‐observation‐carried‐forward (LOCF) strategy; ANOVA,Tukey studentized range test, power analysis Funding source: Trustees of the Liberton Hospital Endowment Funds Ethical approval and informed consents obtained |
|
| Participants |
Participant recruitment: NR Setting: at outpatient clinic at Department of Orthopedics, University Goettingen, Germany Inclusion criteria: 150 participants aged 18 to 65 years with non‐radiating LBP for at least 6 months Exclusion criteria: an abnormal neurological status, concomitant severe disease, psychiatric illness, current psychotherapy, pathological lumbosacral anterior‐posterior and lateral X‐rays (except for minor degenerative changes), rheumatic inflammation disease, planned hospitalization, and refusal to participate Mean age: 48.1 years Gender (female): 58% Pain duration (mean ± SD): 9.6 ± 8.2 years Pain intensity (mean ± SD): 5.2 (VAS, 0 to 10) |
|
| Interventions |
1) GROUP 1: acupuncture + standard therapy (standardized) All participants in three groups received active physiotherapy of 26 sessions (30 min each) over the 12 weeks, performed by trained physiotherapists. Acupuncture points: 20 body points – GV3, GV4 (single), BL40, BL60, BL23, BL25, BL32, GB34, SP6, and BL31 (all bilaterally), Yautungdien (extra meridian at the back of the hand); 6 points in ear – os sacrum (38), parasympathic (51), nervus ischiadicus (52), lumbosacrum (54), Shenmen (55), kidney (95) Depth: depth of body needling (10 to 30 mm) De Qi: elicited and lasted for 5 to 20 seconds; acupoints in ear not stimulated Sessions: 20 sessions (30 min, 4/week for 2 weeks + 1/week for 10 weeks); body needles retention for 30 min and ear needles retention for 1 week Acupuncturist experience: experienced Taiwanese physician 2) GROUP 2: sham acupuncture + standard therapy Needles were inserted superficially and outside the meridians (10 to 20 mm distant to the verum acupoints), and needles were not stimulated; others were same as Group 1. 3) GROUP 3: control group Received active physiotherapy with no other treatment over 12 weeks Co‐intervention: a plan of 26 sessions of standardized active physiotherapy at 30 min each over 12 weeks Duration of treatment: 12 weeks Duration of follow‐up: 9 months after the end of sessions |
|
| Outcomes |
1) Pain intensity: VAS (0 to 10) 2) Pain‐related disability: pain disability index (PDI, 0 to 70) Assessment times: 12 weeks (immediately post‐treatment) and 9 months after the end of sessions Costs: NR Adverse effects: painfulness of acupuncture (n = 2) and problems with circulation during acupuncture (n = 1); persisting pain at control group/usual care (n = 1) |
|
| Notes |
Conclusion: "We found a significant improvement by traditional acupuncture in chronic LBP compared to routine care (physiotherapy) but not compared to sham acupuncture. The trial demonstrated a placebo effect of traditional acupuncture in chronic LBP”. Language: English Using baseline SDs of VAS pain as the corresponding SDs of VAS results in the meta‐analysis For results, see comparisons 1 and 3. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐based randomisation process |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias) All outcomes | Unclear risk | Possibly participants were blinded between verum and sham acupuncture groups. |
| Blinding of personnel /care providers (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Authors did not report a blinded assessor; some subjective outcomes were reported by possibly blinded participants. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Dropout rates were obviously higher in sham and control groups than acupuncture group; the overall rate was 29% at nine months. |
| Intention‐to‐treat‐analysis (attrition bias) | Low risk | LOCF was used for dropouts; patents were analyzed according to group assigned. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Group similarity at baseline (selection bias) | Low risk | Although baseline psychological distress was different, it seemed not to be a prognostic factor. Other baselines were similar. |
| Co‐interventions (performance bias) | Low risk | Participants continued existing medication and physiotherapy. |
| Compliance bias (performance bias) | Unclear risk | Numbers of treatment sessions completed by subjects in each group were not reported. |
| Timing of outcome assessments (detection bias) | Low risk | Same assessment time |
| Other bias | Low risk | Not identified |
Li 2017.
| Study characteristics | ||
| Methods | Two‐arm RCT Number analyzed/randomized: 60/60 Statistical analysis: did not mention ITT analysis; Student's t‐test and Chi² test; power analysis not conducted Funding source: NR Not reported if ethical approval was obtained, but informed consent was obtained |
|
| Participants |
Participant recruitment: recruitment at clinic at Department of Rehabilitation of a hospital in China Setting: recruitment clinic Inclusion criteria: 1) LBP > 3 months; 2) pain located between lower rib and the inferior gluteal folds, not below the knee; 3) negative response in straight‐leg raising test and intact on neurological examinations; 3) no meaningful positive findings on X‐ray image Exclusion criteria: 1) severe cardiac, or brain disease and severe psychosis, or combination; 2) LBP due to specific etiology, including lumbar tuberculosis, disc protrusion, disc stenosis, ankylosing spondylitis, spondylolisthesis, or tumor Age (mean): 42 years Gender (female): 47% Pain duration (mean): 2.1 years Pain intensity (mean): 6.1 (VAS, 0 to 10) |
|
| Interventions |
1) GROUP 1: electroacupuncture (local + distance acupoints) Acupuncture points: shenshu, dachangshu, jiaji, cijiao, huantiao (all bilaterally) Depth: inserted vertically to a depth of 1 to 1.5 cm De Qi: elicited by manual stimulation and maintained for 30 min Sessions: 20 sessions (1/d for 20 d) Equipment setting: G6805‐1 equipment with continuous wave Acupuncturist experience: NR 2) GROUP 2: acupuncture (local acupoints) Acupuncture points: Ashi points Depth: inserting into the muscle De Qi: not mentioned Sessions: 10 sessions (1/d for 10 d) Co‐intervention: NR Duration of treatment: 10 to 20 days Duration of follow‐up: 6 months after the end of the sessions |
|
| Outcomes |
1) Pain intensity: VAS (0 to 10) 2) Back‐specific function status: Oswestry disability index (ODI, 0 to 100%), lower values better Assessment times: immediately after, and 6 months after the end of sessions Costs: NR Adverse effects: NR |
|
| Notes |
Conclusion: There was no difference between acupuncture at Ashi points and electroacupuncture for treatment of nonspecific LBP. Language: Chinese For results, see comparisons 5. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Table of random numbers was used. |
| Allocation concealment (selection bias) | Unclear risk | No mention of concealment methods |
| Blinding of participants (performance bias) All outcomes | Unclear risk | Not mentioned |
| Blinding of personnel /care providers (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No participant dropped out during the follow‐up period. |
| Intention‐to‐treat‐analysis (attrition bias) | Low risk | The analyses were conducted according to their randomisation group. |
| Selective reporting (reporting bias) | Low risk | Both pain and function outcomes were reported. |
| Group similarity at baseline (selection bias) | Low risk | Baseline characteristics were similar between two groups. |
| Co‐interventions (performance bias) | Low risk | Authors did not mention if additional co‐interventions were given. |
| Compliance bias (performance bias) | Unclear risk | Study did not report compliance. |
| Timing of outcome assessments (detection bias) | Low risk | The outcomes were measured at the same time in both groups. |
| Other bias | Low risk | Not identified |
Lin 2010.
| Study characteristics | ||
| Methods | Three‐arm RCT Number analyzed/randomized: 100/100 Statistical analysis: did not mention ITT analysis; ANOVA, power analysis not conducted Funding source: NR Ethical approval and informed consents: NR |
|
| Participants |
Participant recruitment: NR Setting: NR Inclusion criteria: chronic LBP for more than 6 months, with or without radiation pain Exclusion criteria: congenital deformities, tumors, infection, etc. Mean age: NR Gender (female): 69% Pain duration (mean): NR Pain intensity (mean): 5.5 (VAS, 0 to 10) |
|
| Interventions |
1) GROUP 1: electroacupuncture (EA, standardized) Acupuncture points: BL23, BL25, BL40, and SP6 Depth: NR (study only reported 0.3 mm diameter and 40 mm disposable needles used) De Qi: elicited by manual stimulation first; needles connected to the EA machine with a low pulse frequency 15 Hz stimulation for 30 min Sessions: 12 sessions (30 min, 3/week for 4 weeks) Acupuncturist experience: NR 2) GROUP 2: pulsed radiofrequency (PRF) therapy "Under local anaesthesia, 10 cm electrode needle (22 gauge, 5 mm active tip; SMK‐10, Radionics) was inserted into the skin of the lumbar transverse process tip and went on by 45 degrees until the dorsal cranial quadrant of the intervertebral foramen, and introduced with its tip between one‐third and about halfway the mid‐facetal column". The stylet of the cannula was replaced by a PRF probe connected to a PRF machine. When all tests were finished, the PRF lesion mode was started at 42 degrees centigrade for a duration of 120 seconds. Treatment schedule was not reported. 3) GROUP 3: conservation treatment; participants only used medicine 4) Co‐intervention: NR Duration of treatment: 4 weeks Duration of follow‐up: 1 month after treatment |
|
| Outcomes |
1) Pain intensity: VAS (0 to 10) 2) Back‐specific function status: ODI (0 to 50) 3) Quality of life: SF‐36 Assessment times: 1 month after treatment Costs: NR Adverse effects: NR |
|
| Notes |
Conclusion: “Acupuncture was highly accepted and had positive effects in people with chronic LBP.” Language: English For results, see comparison 3 and 4. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation method not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants (performance bias) All outcomes | High risk | It seems impossible |
| Blinding of personnel /care providers (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | The study claimed the assessors were blinded, but subjective outcomes were reported by participants who seemed not be blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not reported |
| Intention‐to‐treat‐analysis (attrition bias) | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Group similarity at baseline (selection bias) | High risk | The similarities of age and sex were not tested. |
| Co‐interventions (performance bias) | Low risk | No co‐interventions |
| Compliance bias (performance bias) | Unclear risk | Not reported |
| Timing of outcome assessments (detection bias) | Low risk | Same |
| Other bias | Low risk | Not identified |
Meng 2003.
| Study characteristics | ||
| Methods | Two‐arm RCT Number analyzed/randomized: 47/55 Statistical analysis: ITT analysis; ANOVA, repeated measures ANOVA, Mann–Whitney U‐test; power analysis not conducted Funding source: New York Chapter of the Arthritis Foundation Ethical approval and informed consents obtained |
|
| Participants |
Participant recruitment: private surgeries and clinics of the Hospital for Special Surgery, an orthopedic and rheumatic disease referral center, and at the New York Presbyterian Hospital Setting: Hospital for Special Surgery and New York Presbyterian Hospital, USA Inclusion criteria: 1) having chronic nonspecific LBP ≥ 12 weeks; if there was associated buttock and leg pain, back pain must be the chief complaint; 2) ≥ 60 years; 3) having an imaging study of the lumbar spine within the past year Exclusion criteria: 1) spinal tumor, infection, or fracture; 2) a bleeding diathesis, epilepsy, a cardiac arrhythmia or pacemaker, dementia, any serious, active medical condition that precluded safe participation; 3) neurological involvement, planned or scheduled lumbar surgery, a history of lumbar surgery, a significant psychiatric disability, inflammatory arthritis; 4) prior use of acupuncture for back pain, the current use of systemic corticosteroids, muscle relaxants, narcotic medications, anticoagulants, and the use of epidural steroid injections within the previous 3 months, involvement in litigation related to back pain; 5) refusal to be randomized Mean age: 71.1 years Gender (female): 60% Pain duration (mean ± SD): NR Pain intensity (mean): 1.6 (VAS, 0 to 5) |
|
| Interventions |
1) GROUP 1: electroacupuncture plus standard therapy (semi‐standardized) Same standard therapy as group 2 Acupuncture points: UB23, UB24, UB25, and UB28 (all bilaterally), and Du3 and Du4, plus maximum of 4 points from UB36, 54, 37, 40, and GB30, 31 Depth: NR De Qi: elicited at all points by manual stimulation first; electrical stimulation at 4 to 6 Hz with a pulse duration of 0.5 ms followed Sessions: 10 sessions (20 min, 2/week for 5 weeks) Acupuncturist experience: two anaesthetists certified in acupuncture 2) GROUP 2: standard therapy Participants' primary physician prescribed during the 5‐week intervention period, including NSAIDs, aspirin and non‐narcotic analgesic medications intakes, same medications maintained and new ones not started, and back exercises continued. Co‐intervention: prohibited therapies were narcotic medications, muscle relaxants, TENS, epidural steroid injections, and trigger point injections Duration of treatment: 5 weeks Duration of follow‐up: 9 weeks after beginning of treatment |
|
| Outcomes |
1) Pain intensity: VAS (0 to 5), lower values better 2) Back‐specific function status: RMDQ (0 to 24) 3) Global assessment of therapy effectiveness: global scale ranged from 'much worse' at 1 to 'much better' at 5 Assessment times: 6 weeks and 9 weeks after beginning of treatment Costs: NR Adverse effects: acupuncture subjects reported minor aching (n = 5), bruising (n = 3), and light‐headedness (n = 1), withdrew from the study because of pain (n = 5). Significantly fewer acupuncture subjects had medication‐related side effects compared with those in the control group. |
|
| Notes |
Conclusion: Acupuncture is an effective, safe adjunctive treatment for chronic LBP in the elder patient. Language: English For results, see comparison 6. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer software generated |
| Allocation concealment (selection bias) | Low risk | Serially numbered, sealed and opaque envelopes were used. |
| Blinding of participants (performance bias) All outcomes | High risk | Not possible in the study |
| Blinding of personnel /care providers (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Unblinded participants reported subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropout rate was < 10% and the reasons were acceptable. |
| Intention‐to‐treat‐analysis (attrition bias) | Low risk | "The data were analysed both as intention‐to‐treat (N = 55) and as completers only (N = 47)." |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Group similarity at baseline (selection bias) | Low risk | Similar baseline characteristics |
| Co‐interventions (performance bias) | Low risk | No significant difference between groups |
| Compliance bias (performance bias) | Low risk | Comparable and acceptable compliance |
| Timing of outcome assessments (detection bias) | Low risk | Same assessment time |
| Other bias | Low risk | Not identified |
Molsberger 2002.
| Study characteristics | ||
| Methods | Three‐arm RCT Number analyzed/randomized: 124/186 Statistical analysis: ITT analysis; Chi², exact Fisher test, Mann–Whitney–Wilcoxon rank test; power analysis Funding source: German Ministry of Education, Science and Research Ethical approval and informed consents obtained |
|
| Participants |
Participant recruitment: from consecutive inpatients of a rehabilitation hospital in Germany Setting: rehabilitation clinic in Germany Inclusion criteria: 1) LBP ≥ 6 weeks between the 12th rib and the gluteal fold; 2) with an average VAS (0 to 100) pain score of ≥ 50 points during the last week, aged 20 to 60 years; 3) the ability to communicate in German (all enrolled participants had a pain duration > 3 months actually) Exclusion criteria: 1) sciatica or other neurological disorders; 2) history of disc or spine surgery; 3) systemic bone and joint disorders (e.g. rheumatoid arthritis); 4) previous treatment with acupuncture; 4) overt psychiatric illness; pregnancy; dependent on regular intake of analgesics Age (mean ± SD): 50 ± 7 years Gender (female): 48% Pain duration (mean ± SD): 9.9 ± 7.8 years Pain intensity (mean ± SD): 66 ± 15 (VAS, 0 to 100) |
|
| Interventions |
1) GROUP 1: acupuncture + conventional orthopedic therapy (semi‐standardized) Participants received acupuncture treatment together with orthopedic therapy during 4 weeks Acupuncture points: BL23, BL25,GB30; distal points: BL40, BL60, GB34; up to 4 Ashi points Depth: depth ranged from 1 to 10 cm De Qi: achieved by manipulation Sessions: 12 sessions (30 min, 3/week for 4 weeks) Acupuncturist experience: experienced medical doctor who had studied acupuncture in China 2) GROUP 2: sham acupuncture + conventional orthopedic therapy Ten needles applied superficially (depth of needle insertion was less than 1 cm) at defined non‐acupuncture points of the lumbar region, and five needles on either side of the back; other treatment was identical to Group 1. 3) GROUP 3: conventional orthopedic therapy Received the conventional conservative orthopedic treatment only. It consisted of a standardized, daily session of physiotherapy, physical exercise, back school, mud packs, infrared heat therapy, and 50 mg diclofenac up to 3 times a day on demand. Injections or cortisone application of any kind were not allowed. Co‐intervention: conventional orthopedic therapy Duration of treatment: 4 weeks Duration of follow‐up: 3 months after treatment |
|
| Outcomes |
1) Pain intensity: average pain level during the last 7 days (VAS, 0 to 100) 2) Global assessment: excellent, good, satisfactory, fail, on a four‐point box scale (4‐PBS) Assessment times: immediately post‐treatment and 3 months after treatment Costs: NR Adverse effects: No important adverse events or side effects reported |
|
| Notes |
Conclusion: "Acupuncture can be an important supplement of conservative orthopaedic treatment in the management of chronic LBP.” Language: English For results, see comparison 1 and 3. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer software generated the numbers. |
| Allocation concealment (selection bias) | Low risk | Central telephone allocation was used. |
| Blinding of participants (performance bias) All outcomes | Low risk | Participants were blinded against verum and sham acupuncture. |
| Blinding of personnel /care providers (performance bias) All outcomes | Unclear risk | Study did not report the blinding process. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Independent assessors did the assessment; some subjective outcomes were reported by participants. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High dropout rate (33%) at the end of study (three months) |
| Intention‐to‐treat‐analysis (attrition bias) | Low risk | The ITT analyses were conducted using best‐case assumption and worst‐case assumption. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Group similarity at baseline (selection bias) | Low risk | Similar baseline characteristics |
| Co‐interventions (performance bias) | Low risk | Anti‐inflammation drug intakes were similar. |
| Compliance bias (performance bias) | Low risk | The compliance rate was 94%. |
| Timing of outcome assessments (detection bias) | Low risk | Same assessment time |
| Other bias | Low risk | Not identified |
Nie 2005.
| Study characteristics | ||
| Methods | Two‐arm RCT Number analyzed/randomized: 60/60 Statistical analysis: did not mention ITT analysis; did not report statistical methods and power analysis. Funding source: NR Ethical approval and informed consents: NR |
|
| Participants |
Participant recruitment: 60 subjects enrolled at acupuncture clinic, Hospital of Chinese Medicine, Jiang Xi, China Setting: recruitment clinic Inclusion criteria: met Chinese diagnosis of chronic LBP as defined in Dignosis of Disease in Traditional Medical Traumatologyand Orthopedics Exclusion criteria: lumbar fracture and clinical positive findings in radiological images Mean age: 40 years Gender (female): 45% Pain duration (mean): 24.1 months Pain intensity (mean ± SD): NR |
|
| Interventions |
1) GROUP 1: acupuncture (standardized) Acupuncture points: shenshu, weizhong (all bilaterally) and Ashi points Depth: NR (2.5 inch needles used) De Qi: by manual stimulation Sessions: 5 sessions in 10 days Acupuncturist experience: NR 2) GROUP 2: acupuncture using heated needles Using 1.5 inch needles; put needles in fire (alcohol burning) until the tips became red; sterilised skin, manipulated needle insertion and drew out very fast; needles should be inserted into muscle or fascia Co‐intervention: none Duration of treatment: 10 days Duration of follow‐up: immediately post‐treatment |
|
| Outcomes |
1) Global assessment: classified as very effective, effective, and no effect Assessment time: immediately post‐treatment Costs: NR Adverse effects: NR |
|
| Notes |
Conclusion: Acupuncture using heated tips of needles confirmed pain alleviation effect. Language: English For results, see Table 7. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not reported |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding of participants (performance bias) All outcomes | High risk | Not possible |
| Blinding of personnel /care providers (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Subjective outcomes were reported by unblinded participants. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No mention of dropout rate |
| Intention‐to‐treat‐analysis (attrition bias) | Unclear risk | Unclear if ITT protocol was properly used |
| Selective reporting (reporting bias) | Low risk | The outcomes were reported. |
| Group similarity at baseline (selection bias) | High risk | Study reported that P < 0.05 for baseline risks, but claimed there was no difference between the two groups. |
| Co‐interventions (performance bias) | Low risk | Not reported if any co‐intervention used |
| Compliance bias (performance bias) | Low risk | Not mentioned |
| Timing of outcome assessments (detection bias) | Low risk | Possibly immediately post‐treatment |
| Other bias | Low risk | Not identified |
Pach 2013.
| Study characteristics | ||
| Methods | Two‐arm RCT Number analyzed/randomized: 139/150 Statistical analysis: ITT analysis; ANCOVA and GEE model; power analysis Funding source: grant from the Chair of Complementary Medicine Research of the Carstens Foundation Ethical approval and informed consents obtained |
|
| Participants |
Participant recruitment: from regular patients of a general medicine practice in Berlin, Germany Setting: a site run by a Chinese‐born medical doctor trained in western and Chinese medicine in Berlin Inclusion criteria: 1) age ≥ 18 years, male or female, LBP ≥ 3 months; 2) clinical diagnosis of chronic LBP confirmed by a medical specialist and indication for treatment of LBP with acupuncture confirmed by a medical specialist; 3) average VAS pain intensity of the last 7 days ≥ 40 points; 4) intellectual and physical ability to participate in the study, and informed consent Exclusion criteria: 1) acupuncture during the last 6 months; 2) start of a new therapy for LBP within the last 4 weeks, 3) pregnancy, substance or drug abuse; 4) participation in another clinical trial Age (mean ± SD): 57.8 ± 12.5 years Gender (female): 58% Pain duration (mean ± SD): 16.3 ± 12.3 years Pain intensity (mean): 58.5 (VAS, 0 to 100) |
|
| Interventions |
1) GROUP 1: acupuncture (semi‐standardized) Acupuncture points: bilateral local points (BL 23‐25) and bilateral distal points (BL40, BL60, Gb34, K3); fewer than 14 needles applied Depth: needles were vertically inserted at 1 to 2 cm depth into the skin depending on the size of the muscle De Qi: elicited by rotation and lift‐thrusting technique Sessions: 10 to 15 sessions (25 min, 2/week) Acupuncturist experience: medical doctor specialized in Western general medicine (25 years of clinical practice) and trained in Chinese medicine; (s)he had 20 years experience using acupuncture to treat LBP. 2) GROUP 2: acupuncture (individualized) Individualized acupuncture was based on syndrome diagnosis, which was done before each treatment session. Others were same as Group 1. Co‐intervention: medication was allowed in both groups Duration of treatment: 7 weeks Duration of follow‐up: 26 weeks after beginning of treatment |
|
| Outcomes |
1) Pain intensity: VAS (0 to 10) average scores during the previous 7 days 2) Back‐specific function status: HFAQ 3) Quality of life: physical and mental component scores of SF‐36 4) Pain‐related disability: Sick leave days Assessment times: 8 weeks and 26 weeks after beginning of treatment Costs: NR Adverse effects: no acupuncture‐related side effects reported |
|
| Notes |
Conclusion: "Individualised acupuncture was not superior to standardized acupuncture for people suffering from chronic low back pain." Language: English For results, see comparison 5. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer software generated |
| Allocation concealment (selection bias) | Low risk | Secured database with limited access was used. |
| Blinding of participants (performance bias) All outcomes | Unclear risk | Participants guessed correctly their assignment treatment, suggesting a certain degree of unblinding. |
| Blinding of personnel /care providers (performance bias) All outcomes | Unclear risk | Unclear how credibly the blinding of the acupuncturists was done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Some outcomes were obtained by an unblinded assessor, while others were reported by participants. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropout rate was < 10% with acceptable reasons. |
| Intention‐to‐treat‐analysis (attrition bias) | Low risk | Subjects with available data included in analysis regardless of treatment adherence |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Group similarity at baseline (selection bias) | Low risk | Even though some of the baseline factors were not similar, the results were adjusted. |
| Co‐interventions (performance bias) | Low risk | Days with pain medication were similar between the two groups. |
| Compliance bias (performance bias) | Low risk | Similar and satisfactory compliance |
| Timing of outcome assessments (detection bias) | Low risk | Same assessment time |
| Other bias | Low risk | Not identified |
Pan 2005.
| Study characteristics | ||
| Methods | Two‐arm RCT Number analyzed/randomized: 73/73 Statistical analysis: did not mention ITT analysis; Chi² test; power analysis not conducted Funding source: NR Ethical approval and informed consents: NR |
|
| Participants |
Participant recruitment: from acupuncture outpatients clinic of Chinese Medicine Hospital at Guang Zhou, China Setting: recruitment clinic Inclusion criteria: 1) aged 20 to 30 years, had chronic lumbar muscle strain and pain mainly in lumbosacral region; 2) LBP became severe on a rainy or cold day; LPB was aggravated during working and alleviated after rest; 3) LBP of frequent recurrence; 4) no limitation in the movement of low back and legs Exclusion criteria: 1) positive clinical findings in radiological images, such as lumbar disc herniation and other deformity requiring operation; 2) severe brain and cardiac disease; 3) could not finish all the therapies and the follow‐up assessments Age (most): 40 to 60 years Gender (female): 44% Pain duration: most around 5 years Pain intensity: NR |
|
| Interventions |
1) GROUP 1: acupuncture (semi‐standardized) Acupuncture points: Ashi points, bladder meridian in lower back, yaoyang guan, jiaji L1‐L5, yanglingquan, zusanli, weizhong, all treated bilaterally except Ashi and weizhong; 8 points on average chosen Depth: NR (32 gauge and 1.5‐3 inch needles used) De Qi: manual stimulation conducted but not reported if De Qi was elicited Sessions: 18 sessions (6/week for 3 weeks) Acupuncturist experience: NR 2) GROUP 2: acupuncture (heating needles) The same acupuncture points as Group 1 chosen; put needles in fire (alcohol burning) until tips became red; sterilized skin, manipulated needles' insertion and drew out very fast; needles should be inserted into taut muscle and fascia; 6 sessions (2/week * 3 weeks) treatment Co‐intervention: none Duration of treatment: 3 weeks Duration of follow‐up: immediately post‐treatment |
|
| Outcomes |
1) Global assessment of therapy effectiveness: classified as very effective, effective, no effect Assessment time: immediately post‐treatment Costs: NR Adverse effects: NR |
|
| Notes |
Conclusion: Acupuncture using heated needles produced a better effect for chronic lumbar muscle strain than traditional acupuncture. Language: English For results, see Table 7. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Study did not report the methods. |
| Allocation concealment (selection bias) | Unclear risk | Envelopes were used; no further details were given. |
| Blinding of participants (performance bias) All outcomes | High risk | Not possible |
| Blinding of personnel /care providers (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Subjective outcomes were reported by unblinded participants. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Study did not mention the dropout rate. |
| Intention‐to‐treat‐analysis (attrition bias) | Unclear risk | Unclear if ITT was properly used |
| Selective reporting (reporting bias) | Low risk | Only one outcome was measured and was reported. |
| Group similarity at baseline (selection bias) | Unclear risk | Severity of LBP at baseline was not measured. |
| Co‐interventions (performance bias) | Low risk | Study did not mention if any co‐interventions used |
| Compliance bias (performance bias) | Unclear risk | Compliance not mentioned |
| Timing of outcome assessments (detection bias) | Unclear risk | Immediate post‐treatment assessment, possibly |
| Other bias | Low risk | Not identified |
Pérez‐Palomares 2010.
| Study characteristics | ||
| Methods | Two‐arm RCT Number analyzed/randomized: 125/135 Statistical analysis: ITT analysis; Student's t test and Mann–Whitney U test; power analysis not conducted Funding source: Aragonese Health Service (Spain) and Research Network on Preventive Activities and Health Promotion (Health Institute Carlos III) and Aragonese Health Science Institute Informed consents obtained; did not report ethical approval |
|
| Participants |
Participant recruitment: referred by primary physicians from four primary healthcare centers in Spain Setting: NR Inclusion criteria: patients > 18 years old, with chronic LBP lasting at least 4 months, or less if it was recurring Exclusion criteria: 1) suspected or diagnosed fibromyalgia syndrome, structural lesions in the lumbar column, either at the disc level or on any other structure; 2) concomitant non‐pharmacological treatments (acupuncture, homeopathy), and any medical conditions or circumstances that in researcher's judgment might interfere with the results Age (mean ± SD): 45.9 ± 14.4 years Gender (female): 75% Pain duration ( > 1 ): 39.9% Pain intensity (mean): 6.0 (VAS, 0 to 10) |
|
| Interventions |
1) GROUP 1: percutaneous electrical nerve stimulation therapy (PENS) Acupuncture points: eight acupuncture needles were inserted at the level of dermatomes from L2 to L5 bilaterally Depth: at a depth of 2 to 2.5 cm De Qi: NR Sessions: 9 sessions (30 min, 3/week for 3 weeks) Practitioner experience: NR 2) GROUP 2: Dry needling therapy Dry needling points: trigger points were diagnosed during the initial assessment and only those that remained active were treated in successive sessions. Depth: using needles of 0.30 × 40 mm with plastic guide tubes; did not report depth De Qi: elicited by fast‐in and fast‐out Hong's technique followed by spray and stretch technique. Each muscle was then passively stretched over three sequences, with vapocoolant spray applied. Treatment was carried out on the trigger points diagnosed during the initial assessment. Trigger points that remained active were treated in successive sessions. Sessions: 3 sessions in 3 weeks Practitioner experience: NR Co‐intervention: none reported Duration of treatment: 3 weeks Duration of follow‐up: immediately post‐treatment |
|
| Outcomes |
1) Pain intensity: VAS (0 to 10) 2) Back‐specific function status: ODI (0 to 50) Assessment time: immediately post‐treatment Costs: NR Adverse effects: NR |
|
| Notes |
Conclusion: The effectiveness of dry needling therapy was comparable to that of PENS. Language: English For results, see comparison 5. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers table was used. |
| Allocation concealment (selection bias) | Low risk | "A third‐party investigator carried out the randomised distribution of both the sequence and the assignment." |
| Blinding of participants (performance bias) All outcomes | High risk | A pragmatic study; didn't mask participants |
| Blinding of personnel /care providers (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Assessor was blinded, but some outcomes were subjective. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Acceptable dropout rates: 3/67 in PENS and 7/68 in dry needing groups |
| Intention‐to‐treat‐analysis (attrition bias) | Low risk | Subjects in their assigned group who completed the treatment were included in the analysis. |
| Selective reporting (reporting bias) | Unclear risk | Results of VAS (pain; sleep) at 2 weeks after treatment were not reported. |
| Group similarity at baseline (selection bias) | Unclear risk | ODI baseline results were not given. |
| Co‐interventions (performance bias) | Unclear risk | Dry needling on trigger points group used additional vapocoolant spray on the pain reference zone. |
| Compliance bias (performance bias) | Unclear risk | Compliance not reported |
| Timing of outcome assessments (detection bias) | Low risk | Both groups had intermediate and final outcomes measured within the same week. |
| Other bias | High risk | Different numbers of included participants reported in the study |
Shankar 2010.
| Study characteristics | ||
| Methods | Two‐arm RCT Number analyzed/randomized: 60/60 Statistical analysis: no mention of ITT analysis; repeated ANOVA with Tukey's test; power analysis not conducted Funding source: NR Informed consents obtained but no report of ethical approval |
|
| Participants |
Participant recruitment: from the Orthopedics Outpatient Department Setting: Department of Physiology and Anesthesiology of a hospital in India Inclusion criteria: 1) adult subjects of both sexes between 30 and 50 years, with a history of moderate to severe pain intensity; 2) non‐radiating LBP of 6 months or longer duration Exclusion criteria: apparent neurological deficit or any prior history of acupuncture therapy Age (mean ± SD): 35.5 ± 5.24 years Gender (female): 63% Pain duration (mean ± SD): 22.33 ± 13.88 months Pain intensity (mean ± SD): 6.80 ± 1.33 (acupuncture) versus 2.03 ± 0.65 (drug therapy) with VAS, 0 to 10 |
|
| Interventions |
1) GROUP 1: electroacupuncture (standardized) Acupuncture points: BL23, BL24, BL36, BL37, BL40, BL57 and BL60, GB30, GB34, and GV4 Depth: not reported; 30 gauge and 2 inch needles used De Qi: NR Sessions: 10 sessions delivered on alternate days in 3 weeks A rectangular wave pulse and a current of 0.5 mA and an output of 6 to 9 volts was delivered at 10 to 20 Hz for 20 min Acupuncturist experience: NR 2) GROUP 2: conventional therapy Valdecoxib 20 mg twice a day for 10 days, together with supervised physiotherapy by a qualified physiotherapist for 3 weeks Co‐intervention: not reported Duration of treatment: 3 weeks Duration of follow‐up: immediately post‐treatment |
|
| Outcomes |
1) Pain intensity: VAS (0 to 10) 2)Global assessment: scale (0 to 7) with 0 indicating worst pain, and 7 indicating best ever Assessment time: immediately post‐treatment Costs: NR Adverse effects: NR |
|
| Notes |
Conclusion: "Acupuncture effectively relieves pain and improves autonomic status, and hence, can be used as an alternative or additional treatment modality in these cases." Language: English For results, see comparison 3. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization list |
| Allocation concealment (selection bias) | Unclear risk | No details described |
| Blinding of participants (performance bias) All outcomes | High risk | Not possible |
| Blinding of personnel /care providers (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported who assessed the outcomes |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Study did not report dropout rate. |
| Intention‐to‐treat‐analysis (attrition bias) | Unclear risk | Data analyzed according to group assigned, but the number of subjects who completed the study was not given. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Group similarity at baseline (selection bias) | Low risk | No significant difference in baseline factors was found between the two groups. |
| Co‐interventions (performance bias) | Low risk | No co‐interventions were reported. |
| Compliance bias (performance bias) | Unclear risk | Not reported |
| Timing of outcome assessments (detection bias) | Low risk | Outcomes seemed to be assessed immediately post‐therapy. |
| Other bias | Low risk | Not identified |
Tsukayama 2002.
| Study characteristics | ||
| Methods | Two‐arm RCT Number analyzed/randomized: 19/20 Statistical analysis: analyzed as assigned group; repeated ANOVA; power analysis not conducted Funding source: grant from the Foundation for Training and Licensure Examination in Anma‐Massage‐Acupressure, Acupuncture and Moxibustion and the Tsukuba College of Technology Ethical approval and informed consents obtained |
|
| Participants |
Participant recruitment: by leaflets in Tsukuba, Japan Setting: at Tsukuba College of Technology Clinic, Japan Inclusion criteria: 1) LBP without sciatica; 2) at least a 2‐week history of LBP; (3) > 20 years old Exclusion criteria: 1) radiculopathy or neuropathy in the lower extremity; 2) fracture, tumor, infection, or internal disease; 3) other general health problems; 4) other conflicting or ongoing treatments Mean age: 44.9 years Gender (female): 84% Pain duration (mean): 8.3 years Pain intensity (mean ± SD): not reported |
|
| Interventions |
1) GROUP 1: electroacupuncture (EA, semi‐standardized) Acupuncture points: 8 points in total; BL23 and BL26 most frequently used Depth: the average insertion depth was approximately 20 mm De Qi: 15 min stimulation with a frequency of 1Hz Sessions: 4 sessions (2/week for 2 weeks) Acupuncturist experience: conservative physical therapy currently practiced in Japan After electroacupuncture treatment at each session, the press tack needles (Seirin Jr®: Seirin Kasei Co. Ltd., Japan) were inserted at four of the eight points chosen, left in situ for several days, and then removed. 2) GROUP 2: TENS Gel type disposable electrodes of size 20 x 30 mm were used for eight points. Electrostimulation was applied and muscle contraction was observed. After each session, a poultice containing methyl salicylic acid, menthol, and antihistamine was prescribed for home application between treatments to the low back region. Co‐intervention: not reported Duration of treatment: 2 weeks Duration of follow‐up: immediately post‐treatment |
|
| Outcomes |
1) Pain intensity: VAS (0 to 100) 2) Pain‐related disability: subjective symptoms and restriction of daily activities items of Japanese Orthopaedic Association (JOA) score, higher values = better Assessment time: immediately post‐treatment Costs: NR Adverse effects: 1) EA group: transient aggravation of LBP (n = 1), discomfort due to press tack needles (n = 1), pain on needle insertion (n = 1) and small subcutaneous bleeding (10 mm in diameter, n = 1); 2) TENS group: transient aggravation of back pain (n = 1), transient fatigue (n = 1), itching with electrode (n = 1) |
|
| Notes |
Conclusion: "In the present preliminary study, although some placebo effect may be included, EA showed more effectiveness than TENS in short‐term treatment of LBP." Language: English Mean and SD data of VAS and JOA score were obtained from Figures. For results, see comparison 4. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer software‐generated random numbers |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes were used. |
| Blinding of participants (performance bias) All outcomes | Unclear risk | Not reported |
| Blinding of personnel /care providers (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded assessor was mentioned; otherwise outcomes seemed to be participant‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There was a 5% dropout rate, and acceptable withdrawal reasons. |
| Intention‐to‐treat‐analysis (attrition bias) | Low risk | Subjects with available data were analyzed according to the assigned group. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Group similarity at baseline (selection bias) | Unclear risk | The risk factors were similar between the two groups except for VAS (pain). |
| Co‐interventions (performance bias) | Unclear risk | TENS group also used a poultice to the low back region. |
| Compliance bias (performance bias) | Low risk | Comparable compliance between groups |
| Timing of outcome assessments (detection bias) | Low risk | Same time |
| Other bias | Low risk | Not identified |
Ushinohama 2016.
| Study characteristics | ||
| Methods | Two‐arm RCT Number analyzed/randomized: 80/80 Statistical analysis: analyzed as assigned group; multivariate analysis of variance (MANOVA) and Mann‑Whitney U test; power analysis Funding source: NR Ethical approval and informed consents obtained |
|
| Participants |
Participant recruitment: personal invitation by the researchers Setting: university, fitness center, and cookie factory (three different places) in São Paulo, Brazil Inclusion criteria: 1) patients with nonspecific chronic LBP (≥ 12 weeks) and aged 18 to 50 years ; 2) VAS (0 to 10) pain ≥ 4 points Exclusion criteria: 1) other musculoskeletal or neurological conditions; 2) underwent spine surgery or had complaints of dizziness; 3) seeking other treatment to reduce LBP, and had taken painkillers and anti‐inflammatory medicine 24 hours prior to the test Mean age: 35 years Gender (female): 62.5% Pain duration (mean): 43 months Pain intensity (mean): 5.7 (VAS, 0 to 10) |
|
| Interventions |
1) GROUP 1: Ear Acupuncture (standardized) Acupuncture points: 29‐analgesic point, 40‐shenmen point, 55‐low back point Depth: NR; used disposable Dong Bang needles (0.15 × 30 mm) De Qi: NR Sessions: one sessions lasting 20 min Acupuncturist experience: therapist with 11 years of experience using ear acupuncture for LBP treatment 2) GROUP 2: placebo group Detuned ultrasound (Sonopulse III, Ibramed, Brazil) was turned on but not activated. The head of the ultrasound wand was placed in light contact with the skin of the painful lower back region and was kept in constant circular motion for minimal interference with the painful area. Co‐intervention: not reported Duration of treatment: 20 min Duration of follow‐up: immediately post‐treatment |
|
| Outcomes |
1) Pain intensity: numeric pain rating scale (NPRS, 0 to 11); lower values better Assessment time: immediately post‐treatment Costs: NR Adverse effects: dizziness |
|
| Notes |
Conclusion: "The findings indicated that ear acupuncture was better than placebo in reducing pain, but neither treatment had any effect on postural control." Language: English The studied was qualitatively described because the pain intensity scores were reported as the mean of the change from baseline score, while the baseline pain data were not reported in the paper as either a median (IQR) or mean ± SD. Therefore, the absolute pain data were unavailable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomized in a 1:1 ratio using a specific website by a person not involved in the study |
| Allocation concealment (selection bias) | Low risk | The randomization codes were placed in consecutively numbered, sealed, and opaque envelopes by a person not involved in the study, ensuring concealed allocation for the two groups. |
| Blinding of participants (performance bias) All outcomes | Unclear risk | It was not mentioned if participants were deceived about the nature of the placebo treatment with de‐tuned ultrasound. |
| Blinding of personnel /care providers (performance bias) All outcomes | High risk | Not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The assessor was blinded to the participants' group allocation and credibility was tested. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Intention‐to‐treat‐analysis (attrition bias) | Low risk | All participants randomized were analyzed. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Group similarity at baseline (selection bias) | Low risk | The groups were similar in sex, age, duration of pain, and functional levels. |
| Co‐interventions (performance bias) | Low risk | The intervention was very short (only 20 minutes), and there were no co‐interventions. |
| Compliance bias (performance bias) | Low risk | It was only a single session. |
| Timing of outcome assessments (detection bias) | Low risk | Was identical for everyone |
| Other bias | Low risk | No other biases |
Wang 2016a.
| Study characteristics | ||
| Methods | Three‐arm RCT Number analyzed/randomized: 46/48 Statistical analysis: analyzed as assigned group; repeated measures ANOVA; power analysis Funding source: NR Ethical approval and informed consents obtained |
|
| Participants |
Participant recruitment: recruited by the researchers at the hospital Setting: Chinese People's Liberation Army (PLA) General Hospital in China Inclusion criteria: 1) male or female patients, 20 to 60 years old; 2) myofascial pain syndrome (MPS) lasting longer than 12 months; 3) VAS (pain) between 5 and 10 points; 4) normal cognitive function; 5) BMI between 18 and 25 kg/m² Exclusion criteria: 1) previous dry needling therapy (including acupuncture) or trigger point injections within 6 months; 2) surgery history of lumbar area; central nervous system diseases; malignant diseases; skin diseases in the lumbar region; blood system diseases; mental disease or cognitive dysfunction; pregnancy; taking anticoagulant drugs; immune system disorders; history of fainting, alcoholism, or drug addiction; 3) patients receiving other treatment (including trigger point injections, medication, physical therapy, etc.) for the lumbar MPS within the time period, between dry needling therapy and the last follow‐up (3 months) Mean age: 42.6 years Gender (female): 52% Pain duration (mean): 49.1 months Pain intensity (mean): 6.69 (VAS, 0 to 10) |
|
| Interventions |
1) GROUP 1: electroacupuncture using dry needles of 0.25 mm diameter (standardized) Acupuncture points: tender points Depth: the needle reached the point of maximum tenderness De Qi: NR Sessions: 1 session lasting 10 min Acupuncturist experience: experienced and licensed physician 2) GROUP 2: electroacupuncture using dry needles of 0.5 mm diameter The protocol was the same as Group 1. 3) GROUP 3: electroacupuncture using dry needles of 0.9 mm diameter The protocol was the same as Group2 . Duration of treatment: 10 min Duration of follow‐up: 3 months after treatment |
|
| Outcomes |
1) Pain intensity: VAS (0 to 10) 2) Quality of life: SF‐36 Assessment times: 7 days post‐treatment and 3 months after treatment Costs: NR Adverse effects: NR |
|
| Notes |
Conclusion: Larger needles (0.9 mm) were better than smaller ones (0.5 mm) in the reduction of pain, but treatment with needles of varying diameters were all effective for quality of life. There was no difference in pain and quality of life between the three groups at three months. Language: English For results, see comparison 5. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization table was used. |
| Allocation concealment (selection bias) | Low risk | Relevant information was sealed. |
| Blinding of participants (performance bias) All outcomes | Low risk | The triage nurse knew the treatment allocation and only informed the physician, who didn't tell participants about the diameter of the needle. |
| Blinding of personnel /care providers (performance bias) All outcomes | High risk | The triage nurse informed the treating physician what the participant received. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Study did not provide any information about independent outcome assessor. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts were reported, and the number was acceptable. |
| Intention‐to‐treat‐analysis (attrition bias) | Unclear risk | Not mentioned |
| Selective reporting (reporting bias) | Low risk | All predefined outcomes were reported. |
| Group similarity at baseline (selection bias) | Low risk | No difference at baseline between groups |
| Co‐interventions (performance bias) | Low risk | No medication or physical therapy were received during treatment, or within the first three months after treatment. |
| Compliance bias (performance bias) | Low risk | There was only one session; all participants finished the treatment except for two dropouts. |
| Timing of outcome assessments (detection bias) | Low risk | Same time points reported |
| Other bias | Low risk | Not identified |
Weiss 2013.
| Study characteristics | ||
| Methods | Two‐arm RCT Number analyzed/randomized: 143/160 Statistical analysis: unclear if ITT analysis used; Chi² test and Student's t‐test; power analysis not conducted Funding source: NR Ethical approval and informed consents obtained |
|
| Participants |
Participant recruitment: by an inpatient rehabilitation program in Germany Setting: inpatient rehabilitation clinic in Germany Inclusion criteria: chronic LBP for ≥ 6 months, and aged 25 to 75 years Exclusion criteria: 1) contraindications to acupuncture (e.g. anticoagulation with phenprocoumon or warfarin; coagulation disorders or thrombocytopenia (platelet count < 150,000 cells/mm³)); 2) poor fluency in German language; insufficient adherence; recent surgical treatment; and herniated vertebral discs Mean age: 50.7 ± 7.7 years Gender (female): 32.9% Pain duration (mean ± SD): 11.3 ± 8.4 years Pain intensity (mean ± SD): NR |
|
| Interventions |
1) GROUP 1: acupuncture (individualized) + standard therapy Acupuncture points: each participant was treated individually according to the advice of the traditional Chinese Medicine (TCM) physician. Depth: NR De Qi: NR Sessions: 6 sessions (30 to 40 min, 2/week for 3 weeks) Acupuncturist experience: Chinese physicians who had completed education in TCM in China and had practiced in Germany for several years Tuina massage and a magnet lamp (TDP‐lamp CQ‐35, Chongqing Xinfeng Medical Instruments Co. Ltd., Chongqing, China) were used in addition, at the discretion of the TCM physicians. 2) GROUP 2: standard therapy All participants participated in a standardized 21‐day inpatient rehabilitation program, according to current German guidelines. Co‐intervention: not reported Duration of treatment: 3 weeks Duration of follow‐up: 3 months after treatment |
|
| Outcomes |
1) Pain intensity: bodily pain on SF‐36 (0 to 100); higher values better 2) Quality of life: SF‐36 (reported in 8 aspects); higher values better Assessment times: immediately post‐treatment, and 3 months after treatment Costs: NR Adverse effects: nausea in 2.7% of participants; dizziness in 13.5%; urgency in 20.3%; and pain at puncture site in 36.5% of participants |
|
| Notes |
Conclusion: "Acupuncture was highly accepted and had positive effects in people with chronic low back pain." Language: English We used baseline SDs as corresponding SDs for meta‐analysis. For results, see comparison 6. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A balanced block randomization was used. |
| Allocation concealment (selection bias) | Unclear risk | No details were provided. |
| Blinding of participants (performance bias) All outcomes | High risk | Not possible |
| Blinding of personnel /care providers (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Subjective outcomes were reported by unblinded participants. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropout rate was acceptable, though a little higher rate in the usual care group (8/77) than the acupuncture group (5/79); the reasons were given. |
| Intention‐to‐treat‐analysis (attrition bias) | Unclear risk | Data analysis excluded all dropped participants (8.1%). |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported except for some changes of pain intensity, which were not important. |
| Group similarity at baseline (selection bias) | Low risk | Baseline values were reported to be similar, but no P values were given. |
| Co‐interventions (performance bias) | Low risk | Study did not report using co‐interventions. |
| Compliance bias (performance bias) | Unclear risk | Not reported |
| Timing of outcome assessments (detection bias) | Low risk | Same time |
| Other bias | Low risk | Not identified |
Witt 2006.
| Study characteristics | ||
| Methods | Two‐arm RCT Number analyzed/randomized: 2594/2841 Statistical analysis: ITT analysis; covariance analysis; power analysis Funding source: a group of social health insurance funds in Germany Ethical approval and informed consents obtained |
|
| Participants |
Participant recruitment: referral by participating physician Setting: NR Inclusion criteria: 1) clinical diagnosis of chronic LBP > 6 months, and aged > 18 years; 2) provision of written consent Exclusion criteria: 1) protrusion or prolapse of 1+ intervertebral discs with concurrent neurologic symptoms; 2) prior vertebral column surgery and infectious spondylopathy; 3) LBP caused by inflammatory, malignant, or autoimmune disease; 4) congenital deformation of the spine, except for slight lordosis or scoliosis; 5) compression fracture caused by osteoporosis, spinal stenosis, spondylolysis, or spondylolisthesis Mean age: 52.9 years Gender (female): 57.3% Pain duration (mean): 7.2 years Pain intensity (mean ± SD): NR |
|
| Interventions |
1) GROUP 1: acupuncture (individualized) Acupuncture points: points treated and number of needles used were decided by acupuncturist Depth: NR De Qi: NR Sessions: a maximum of 15 sessions in 3 months Acupuncturist experience: physicians required to have at least a German diploma representing 140 hours of certified acupuncture education 2) GROUP 2: waiting list Received acupuncture treatment as Group 1 three months later Co‐intervention: other treatment was allowed, as needed Duration of treatment: 3 months Duration of follow‐up: immediately post‐treatment |
|
| Outcomes |
1) Pain disability: Low Back Pain Rating Scale (PRS, 0 to 100) consisting of back and leg pain (60 points), disability index (30 points), and physical impairment (10 points); lower values better 2) Back‐specific function status: HAFQ (0 to 100) 3) Quality of life: SF‐36 (mental and physical health component) Assessment time: immediately post‐treatment Costs: Quality‐adjusted life years utility values were higher in the acupuncture group than in the control group. Adverse effects: 1% incidence; cases such as minor local bleeding or hematoma, needling pain, and vegetative symptoms reported |
|
| Notes |
Conclusion: "People with chronic low back pain treated with acupuncture in addition to routine care showed significant improvements in symptoms and quality of life compared with those who received routine care alone. Acupuncture plus routine care was associated with higher costs but was estimated to be cost‐effective." Language: English We contacted the first author and obtained absolute data for HFAQ after treatment. For results, see comparison 2. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated software |
| Allocation concealment (selection bias) | Low risk | Central telephone allocation was used. |
| Blinding of participants (performance bias) All outcomes | High risk | Not possible in this study |
| Blinding of personnel /care providers (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Unblinded participants reported outcomes, which were subjective in nature. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Acceptable dropout rates, but it seemed they were not comparable between two groups: 6.1% versus 9.4% at three months; 9.0% versus 13.9% at six months |
| Intention‐to‐treat‐analysis (attrition bias) | Low risk | Subjects were analyzed according to the group allocated, and sensitivity analysis was performed. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Group similarity at baseline (selection bias) | Low risk | Similar baseline factors between acupuncture and control groups |
| Co‐interventions (performance bias) | Low risk | "The number of participants who used analgesic agents during the study were similar in the two randomised groups.” |
| Compliance bias (performance bias) | Low risk | Participants in the acupuncture groups received 10.4 ± 2.6 out of maximum 15 sessions, which is acceptable. |
| Timing of outcome assessments (detection bias) | Low risk | Same time |
| Other bias | Low risk | Not identified |
Yuan 2009.
| Study characteristics | ||
| Methods | Two‐arm RCT Number analyzed/randomized: 21/30 Statistical analysis: ITT analysis; repeated measures ANCOVA and Mann‐Whitney U test; power analysis Funding source: the Vice Chancellors Research Scholarship; the Strategic Priority Grant, Department for Employment and Learning, Northern Ireland Ethical approval and informed consents obtained |
|
| Participants |
Participant recruitment: email and poster advertisement at the University of Ulster clinic, UK Setting: University of Ulster clinic, UK Inclusion criteria: pain below the 12th costal margin and above the inferior gluteal folds, with or without radiating leg pain Exclusion criteria: 1) history of disc or spine surgery; 2) sciatica; 3) neurological disorders and possible serious pathological back problem; 4) systemic bone or joint disorders; pregnancy; dementia; overt psychiatric illness; severe clotting disorders or anticoagulant therapy; epilepsy; systemic or visceral disease; other acute orthopedic or medical problems; 5) current use of systemic corticosteroids, muscle relaxants, narcotic medications; 6) received acupuncture treatment within the past 6 months; 7) unemployed or having current or pending compensation claims Mean age: 43.7 years Gender (female): 40% Pain duration (mean): 12.5 years Pain intensity (mean): 4.1 (VAS, 0 to 10) |
|
| Interventions |
1) GROUP 1: low‐frequency acupuncture (individualized) Acupuncture points: points were chosen individually according to TCM principles or segmental or trigger point principles; average of 3 to 12 needles used at each session Depth: Not reported De Qi: elicited by rotation, thrust or twirling; re‐elicit De Qi if the sensation was not maintained at 10‐min intervals Sessions: 10 sessions (20‐30 min, 2/week for 5 weeks) Acupuncturist experience: acupuncturists with more than 5 years clinical experience 53% participants received cupping, and 20% received moxibustion as supplementary therapies 2) GROUP 2: high‐frequency acupuncture (individualized) 10 sessions (20 to 30 min, 5/week for 2 weeks); 47% participants received cupping, and 33% received moxibustion; others were same as Group 1. Co‐intervention:The Back Book recommended by the European guidelines was given to participants, which encouraged them to keep as active as possible. Duration of treatment: 5 weeks and 2 weeks, respectively Duration of follow‐up: 1 year after the end of sessions |
|
| Outcomes |
1) Pain intensity: VAS (0 to 10) 2) Back‐specific function status: RMDQ (0 to 24) 3) Others relevant: Measure Yourself Medical Outcome Profile 2 (MYMOP‐2) Assessment times: 2 weeks, 5 weeks, 3 months, and 1 year after the end of sessions Costs: NR Adverse effects: 1) high‐frequency group: minor bleeding (n = 7), tiredness (n = 3), minor dizziness, headache, redness, and dry mouth (n = 1 for each); 2) low‐frequency group: minor bleeding (n = 4), pain (n = 2), reported tiredness, minor dizziness, muscle twitching, and stuck needle (n = 1 for each) |
|
| Notes |
Conclusion: "No significant differences were found for any of the investigated outcomes at 2 weeks, 5 weeks, 3 months, 1 year, and at discharge between groups." Language: Chinese For results, see comparison 5. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random allocation sequence was used. |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes were used. |
| Blinding of participants (performance bias) All outcomes | Unclear risk | Acupuncture treatment with two different sessions were given to participants; no reports on masking process |
| Blinding of personnel /care providers (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | An independent outcome assessor; some subjective outcomes were reported by participants. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High risk of long‐term dropout rate (30%) |
| Intention‐to‐treat‐analysis (attrition bias) | Low risk | ITT analysis was used; and imputation was used for missing values. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Group similarity at baseline (selection bias) | Low risk | Balanced baselines |
| Co‐interventions (performance bias) | Low risk | All subjects received the same Back Book as co‐intervention. |
| Compliance bias (performance bias) | Low risk | High and comparable compliance |
| Timing of outcome assessments (detection bias) | Unclear risk | Immediate post‐treatment time was different in the two groups. |
| Other bias | Low risk | Not identified |
Yuan 2016.
| Study characteristics | ||
| Methods | Three‐arm RCT Number analyzed/randomized: 150/150 Statistical analysis: ITT analysis; ANOVA, repeated ANOVA and Chi²; power analysis Funding source: Chinese government grant Ethical approval and informed consents obtained |
|
| Participants |
Participant recruitment: study recruited the participants at outpatient clinics Setting: outpatient clinics of two different hospitals in China Inclusion criteria: 1) pain located in the lumbar and buttocks region, and the top of the legs; 2) chronic pain for more than 6 months, patients aged between 18 and 70 years; 3) had acute attack at least once in the recent two weeks; 4) VAS (pain, 0 to 100) ≥ 30 points; 5) no pain due to pressure; negative straight‐leg raising testing; negative nerve root involved; normal findings in image testing Exclusion criteria: 1) severe diseases; psychiatric illness; pregnancy; history of disc or spine surgery; 2) positive iodine allergy testing; anticoagulant therapy in previous 6 months; 3) history of acupuncture treatment Mean age: 45.5 years Gender (female %): 68% Pain duration (mean): 12.4 years Pain intensity (mean): 65.3 (VAS, 0 to 10) |
|
| Interventions |
1) GROUP 1: Acupunture (individualized) Acupuncture points: BL23, BL25, BL40, GV3, and GB30; SI4, GB26, GB34, GB41, ST4, ST36, GV4, GV5, GV24, GV26 (independent points) Depth: 5 to 20 mm De Qi: elicited and needles were retained for 20 min Sessions: 12 sessions (2/week for 6 weeks) Acupuncturist experience: NR 2) GROUP 2: Sham acupuncture Needling without skin penetration; the protocol was the same as Group 1. 3) Wait‐to‐treat group Participants did not receive any treatment until acupuncture group finished all of the sessions. Co‐intervention: all participants were permitted to take NSAIDs, if necessary. Duration of treatment: 6 weeks, respectively Duration of follow‐up: 12 weeks after the end of sessions |
|
| Outcomes |
1) Pain intensity: VAS (0 to 100) 2) Back‐specific function status: improved Oswestry Disability Index (IODI, 0 to 100), lower values better Assessment times: 1 week, 4 weeks, and 12 weeks Costs: NR Adverse effects: 1) acupuncture group: aggregated LBP (n = 4); insertion points pain (n = 2); bruise (n = 1); pain and numbness in leg (n = 2); pain in shoulder (n = 2); 2) sham acupuncture group: aggregated LBP (n = 8); insertion points pain (n = 2); pain and numbness in leg (n = 1); pain in shoulder (n = 1), pain in foot (n = 1) |
|
| Notes |
Conclusion: "Acupuncture therapy has specific therapeutic effects on chronic nonspecific low back pain; it can relieve low back pain and improve lumbar function in the short term (≤ 4 weeks), meanwhile it has a high safety profile." Language: Chinese For results, see comparison 1 and 2. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated software |
| Allocation concealment (selection bias) | Low risk | Sealed, opaque envelopes were used to conceal the allocation. |
| Blinding of participants (performance bias) All outcomes | Low risk | Sham group used non‐penetrating needles and details of the blinding method were described. |
| Blinding of personnel /care providers (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No mention |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 14 of 150 participants dropped out during the assessment. |
| Intention‐to‐treat‐analysis (attrition bias) | Low risk | ITT analysis was used. |
| Selective reporting (reporting bias) | Low risk | All VAS (pain) and ODI scores at designed time terms were reported. |
| Group similarity at baseline (selection bias) | Low risk | Similar baseline characteristics |
| Co‐interventions (performance bias) | Unclear risk | Participants were allowed to take NSAIDs, but the dose and how many participants took were not reported. |
| Compliance bias (performance bias) | Low risk | All participants completed the treatment. |
| Timing of outcome assessments (detection bias) | Low risk | Same timing of outcome assessments |
| Other bias | Low risk | Not identified |
Yun 2012.
| Study characteristics | ||
| Methods | Three‐arm RCT Number analyzed/randomized: 236/236 Statistical analysis: analyzed as assigned to randomized groups; repeated measures ANOVA; power analysis not conducted Funding source: NR Ethical approval and informed consents obtained |
|
| Participants |
Participant recruitment: by letters Setting: at the Chinese Level II Peacekeeping Hospital in Lebanon Inclusion criteria: 1) participants aged between 18 and 70 years who could continue enrolling in the health plan; 2) ≥ 1 primary care visit for back pain within the past 3 to 12 months; 3) nonspecific and uncomplicated LBP Exclusion criteria: 1) previous acupuncture for any reason; 2) LBP < 3 months and mild symptoms (VAS pain < 3); 3) specific diseases that could be the cause of back pain; 4) complicated back problems, such as sciatica, back surgery in prior 3 years; 5) other disabling chronic conditions that might confound treatment effects or the interpretation of data; 6) acupuncture contraindicated or safety not confirmed; 7) medicolegal issues; 8) conditions that could possibly make consent or treatment difficult Age (mean ± SD): 33 ± 11 years Gender (female %): 30% Pain duration (≥ 1 yr): 57% Pain intensity (mean ± SD): NR |
|
| Interventions |
1) GROUP 1: acupuncture (standardized) Acupuncture points: bilateral points (Du 3, BL23, BL40, and KI3l) and Ashi points Depth: generally 1 to 3 cm De Qi: manipulated needles to elicit the sensation at 10 min after the beginning of treatment and again before removal of needles Sessions: 14 sessions (20 min in 4 weeks) Acupuncturist experience: acupuncturists had at least 6 years clinical experience 2) GROUP 2: another style of acupuncture (back‐pain acupoints + standardized points) Same side of back‐pain acupuncture points were inserted in hands and stimulated to introduce De Qi sensation; acupuncture on body points and treatment schedule were same as Group 1. 3) GROUP 3: usual care Participants received care not related to the study, including massage, physical therapy visits, and continued use of medications (ibuprofen). Co‐intervention: massage and physical therapy prescribed for each participant; a self‐care book about management of chronic LBP given to participants Duration of treatment: 4 weeks Duration of follow‐up: 24 weeks after beginning of treatment |
|
| Outcomes |
1) Pain bothersomeness: VAS (0 to 10) 2) Back‐specific function status: RMDQ (0 to 24) 3) Quality of life: SF‐36 4) Global assessment: classified as effective or no change Assessment times: 4 weeks and 24 weeks after beginning of treatment Costs: NR Adverse effects: NR |
|
| Notes |
Conclusion: 1) Acupuncture had beneficial and persistent effects on chronic LBP compared with usual care, in clinically significant improvement in function and mental condition; 2) Acupuncture on same side of back‐pain points and body points was significantly more effective, especially in the long term. Language: English For results, see comparison 3 and 5. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A centrally generated variable‐sized block design was used. |
| Allocation concealment (selection bias) | Unclear risk | Specific details of allocation concealment were not mentioned. |
| Blinding of participants (performance bias) All outcomes | Low risk | The participants were not informed how the acupuncture treatments were different and the testing showed an identical masking effect. |
| Blinding of personnel /care providers (performance bias) All outcomes | Unclear risk | Details not described. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcomes were assessed by blinded telephone interviewers and subjective outcomes were reported by participants. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participant dropped out. |
| Intention‐to‐treat‐analysis (attrition bias) | Low risk | All subjects were analyzed according to their randomized group. |
| Selective reporting (reporting bias) | High risk | Physical scores of SF‐36 were not reported. |
| Group similarity at baseline (selection bias) | Low risk | Similar baselines |
| Co‐interventions (performance bias) | High risk | During treatment, doses of medicines were significantly different among the three groups. |
| Compliance bias (performance bias) | Unclear risk | Compliance not reported |
| Timing of outcome assessments (detection bias) | Low risk | Same time |
| Other bias | Unclear risk | Typing mistake on outcome figure; not clear if VAS scale was used for bothersomeness or pain intensity. |
Yun 2012a.
| Study characteristics | ||
| Methods | Three‐arm RCT Number analyzed/randomized: 187/187 Statistical analysis: analyzed as assigned to randomized groups; repeated measures ANOVA; power analysis not conducted Funding source: NR Ethical approval and informed consents obtained |
|
| Participants |
Participant recruitment: by letters and telephone Setting: Traditional Chinese Medicine Department of Chengdu General Military Hospital, China Inclusion criteria: patients aged 20 to 45 years with LBP ≥ 3 months; VAS (0 to 10) ≥ 3 points Exclusion criteria: 1) specific causes of back pain (e.g. cancer, fractures, spinal stenosis, and infections); 2) complicated back problems (e.g. sciatica, scoliosis > 40 degree curvature, chronic spondylitis, prior back surgery, medicolegal issues); 3) possible contraindications for acupuncture (e.g. coagulation disorders, cardiac pacemakers, pregnancy, seizure disorder); 4) conditions making treatment difficult (e.g. paralysis, psychoses); 5) conditions that might confound treatment effects or the interpretation of results (e.g. severe fibromyalgia, rheumatoid arthritis, concurrent care from other providers); 6) previous acupuncture treatment for any condition Mean age: 34 years Gender (female): 23% Pain duration (> 1 yr): 71% Pain intensity (mean ± SD): 6.2 ± 1.8 (VAS, 0 to 10) |
|
| Interventions |
1) GROUP 1: acupuncture (standardized) Acupuncture points: bilateral points (Du 3, BL23, BL40, and KI3l) and Ashi points Depth: generally 1 to 3 cm De Qi: manipulated needles to elicit the sensation at 10 min after the beginning of treatment and again before removal of needles Sessions: 18 sessions (20 min, 10/3 weeks + 2/week for 4 weeks) Acupuncturist experience: acupuncturists with at least 6 years clinical experience 2) GROUP 2: hegu acupuncture (hegu + body points) Three needles were inserted at hegu points in different directions and De Qi was introduced by repeating twirling and drawing back; acupuncture on body points and treatment schedule were same as Group 1. 3) GROUP 3: usual care Participants received care not related to the study, including massage, physical therapy visits, and continued use of medications (ibuprofen) Co‐intervention: massage and physical therapy prescribed for every participant; a self‐care book about management of chronic LBP given to participants Duration of treatment: 7 weeks Duration of follow‐up: 48 weeks after beginning of treatment |
|
| Outcomes |
1) Pain intensity: VAS (0 to 10) 2) Back‐specific function status: RMDQ (0 to 24) 3) Quality of life: SF‐36 4) Global assessment: classified as effective and no change Assessment times: 8 weeks and 48 weeks after beginning of treatment Costs: NR Adverse effects: NR |
|
| Notes |
Conclusion: 1) Acupuncture had beneficial and persistent effects on chronic LBP compared with usual care in clinically significant improvement in function and mental condition; 2) Acupuncture on hegu and body points was significantly more effective, especially in the long term Language: English For results, see comparison 3 and 5. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A centrally generated variable‐sized block design was used. |
| Allocation concealment (selection bias) | Unclear risk | Specific details of allocation concealment was not mentioned. |
| Blinding of participants (performance bias) All outcomes | Low risk | "The trial was described to participants only as an acupuncture points study without information about how treatments differed"; the testing showed identical masking effect. |
| Blinding of personnel /care providers (performance bias) All outcomes | Unclear risk | Not described in detail |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinded outcome assessors were used; some subjective outcomes were reported by blinded participants. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participant dropped out. |
| Intention‐to‐treat‐analysis (attrition bias) | Low risk | All subjects were analyzed according to their randomized group. |
| Selective reporting (reporting bias) | High risk | Physical scores of SF‐36 at two time points were not reported. |
| Group similarity at baseline (selection bias) | Low risk | Similar baselines |
| Co‐interventions (performance bias) | High risk | Doses of medicines were significantly different among the three groups. |
| Compliance bias (performance bias) | Unclear risk | Compliance was not reported. |
| Timing of outcome assessments (detection bias) | Low risk | Same time |
| Other bias | Low risk | Not identified |
Zaringhalam 2010.
| Study characteristics | ||
| Methods | Four‐arm RCT Number analyzed/randomized: 80/84 Statistical analysis: did not mention ITT analysis; ANOVA followed by Tukey's multiple comparison test and Student's t‐test; power analysis not conducted but estimated sample size based on a previous paper Funding source: NR Ethical approval and informed consents obtained |
|
| Participants |
Participant recruitment: by local newspapers and the trial research centers of the Tehran University of Medical Sciences, Iran Setting: recruitment center Inclusion criteria: 1) lumbar or lumbosacral pain for 6 months or longer; 2) LBP without radiation to other regions; 3) normal neurological signs of lumbosacral nerves including deep tendon and plantar reflexes, voluntary motor function, straight‐leg raise and sensory function; 4) no acupuncture treatment in the previous 6 months; 5) absence of significant pathology, such as bone fracture or severe psychiatric conditions; 6) stable health; 7) all participants experienced ongoing pain, the intensity of which did not change over the course of a day Exclusion criteria: 1) major trauma or systemic disorders; 2) conflicting or ongoing co‐interventions (drugs, alternative treatments, or both); 3) prior use of acupuncture for LBP in the previous 6 months; 4) refusal to be randomized; 5) protrusion or prolapse of one or more intervertebral discs with concurrent neurological symptoms; 6) prior vertebral column surgery; 7) infectious spondylopathy; 8) LBP secondary to an inflammatory, malignant, or autoimmune disease; 9) congenital deformation of the spine (except for slight lordosis or scoliosis); 10) compression fracture caused by osteoporosis, spinal stenosis, spondylolysis, or spondylolisthesis Mean age: 54.5 years Gender (female): NR Pain duration (mean): 6.9 years Pain intensity (mean): 64.5 (VAS, 0 to 100) |
|
| Interventions |
1) GROUP 1: acupuncture (semi‐standardized) Acupuncture points: bilateral points (BL23, BL25, BL28, BL32, BL60, GB30, and GB34); 10 to 12 needles were used Depth: NR De Qi: elicited by manual stimulation and electrical stimulation at 4 to 6 Hz with pulse duration of 0.5 ms followed Sessions: 10 sessions (20 to 25 min, 2/week for 5 weeks) Acupuncturist experience: certified acupuncturist 2) GROUP 2: baclofen (BA) Baclofen was administered orally 30 mg/day (15 mg twice a day). 3) GROUP 3: baclofen + acupuncture (BA + AC) Participants received both baclofen (30 mg/day) and acupuncture for five weeks. 4) GROUP 4: control group (no treatment) Participants did not receive any treatment for chronic pain Co‐intervention: all participants were advised to maintain their normal lifestyle and not to start any new medications. Duration of treatment: 5 weeks Duration of follow‐up: 10 weeks after beginning of treatment |
|
| Outcomes |
1) Pain intensity: VAS (0 to 10) 2) Back‐specific function status: RMDQ (0 to 24) Assessment times: 5 weeks and 10 weeks after beginning of treatment Costs: NR Adverse effects: NR |
|
| Notes |
Conclusion: "The present study indicates that the combined treatment of acupuncture and baclofen is more effective than baclofen treatment alone to reduce pain in people with nonspecific chronic LBP.” Language: English For results, see comparisons 2, 4 and 5. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Stratified block randomization was generated by computer software. |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes were used. |
| Blinding of participants (performance bias) All outcomes | High risk | Not possible between acupuncture and drug intake groups |
| Blinding of personnel /care providers (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | All outcomes were self‐reported by the unblinded participants. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low dropout rate (< 5%) |
| Intention‐to‐treat‐analysis (attrition bias) | Unclear risk | All randomized participants were included in analysis, except for four participants, who dropped out with rational reasons; ITT not mentioned |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Group similarity at baseline (selection bias) | Low risk | Baseline characteristics were similar. |
| Co‐interventions (performance bias) | Low risk | No co‐interventions |
| Compliance bias (performance bias) | Low risk | All four groups had one subject who discontinued the intervention. |
| Timing of outcome assessments (detection bias) | Low risk | Same time |
| Other bias | Low risk | Only men recruited, seemed not to be a risk factor; other risks were not identified. |
Zhao 2012.
| Study characteristics | ||
| Methods | Three‐arm RCT Number analyzed/randomized: 90/90 Statistical analysis: did not mention ITT analysis; Wilcoxon signed‐rank test and Student's t test; power analysis not conducted Funding source: NR Informed consents obtained; did not mention ethical approval |
|
| Participants |
Participant recruitment: outpatients and inpatients of Physiotherapy Department of Hospital, Hu Nan, China Setting: recruitment site Inclusion criteria: 1) meeting the criteria of chronic nonspecific LBP; 2) aged 20 to 70 years; 3) did not have any treatment or drugs in 2 weeks before the trial; 3) no organ dysfunction or drug allergies; 4) no pregnancy and no breastfeeding; 5) no severe diseases, such as cancer, stoke, and mental disease; 6) can finish all the treatments and assessments Exclusion criteria: 1) severe systematic disorders; 2) not suitable to be included in the study Mean age: 51.8 years Gender (female): 67% Pain duration (mean): 10.2 years Pain intensity (mean): 6.5 (VAS, 0 to 10) |
|
| Interventions |
1) GROUP 1: acupuncture using dragon‐tiger fighting simulation technique (standardized) Acupuncture points: 1) shenyu, dachangyu, weizhong, Ashi points; 2) qihaiyu, guanyuanyu, kunlun, yaoyangguan Depth: 25 to 55 mm De Qi: elicited using dragon‐tiger fighting simulation technique twice for 30 seconds at each session Sessions: 12 sessions (30 min, 1/d for 13 d with one day of rest after 6th session) Acupuncturist experience: NR Dragon‐tiger fighting simulation technique: using thumb to twirl the needles clockwise nine times and then counterclockwise six times 2) GROUP 2: acupuncture using lifting, thrusting, and twirling simulation technique (standardized) Same treatment protocol and schedule as Group 1. When De Qi was elicited, using lifting, thrusting, and twirling simulation technique for 30 seconds, twice at each session 3) GROUP 3: TENS Put the electrodes on the lower back area; adjusted electrical intensity to participants' response Co‐intervention: none Duration of treatment: 13 days Duration of follow‐up: immediately post‐treatment |
|
| Outcomes |
1) Pain intensity: VAS (0 to 10) 2) Back‐specific function status: ODI (0 to 50) Assessment time: immediately post‐treatment Costs: NR Adverse effects: NR |
|
| Notes |
Conclusion: Acupuncture treatment using the dragon‐tiger fighting simulation technique was more effective for LBP than another style of acupuncture. Language: Chinese For results, see comparisons 4 and 5. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table was used. |
| Allocation concealment (selection bias) | Unclear risk | No concealment information was provided. |
| Blinding of participants (performance bias) All outcomes | Unclear risk | Study did not report on blinding of participants. |
| Blinding of personnel /care providers (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Subjective outcomes were reported by the subjects who may not have been blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No reported dropouts |
| Intention‐to‐treat‐analysis (attrition bias) | Unclear risk | ITT not mentioned |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Group similarity at baseline (selection bias) | Low risk | Similar baselines |
| Co‐interventions (performance bias) | Low risk | Not allowed |
| Compliance bias (performance bias) | Unclear risk | Compliance not mentioned |
| Timing of outcome assessments (detection bias) | Low risk | Possibly immediately post‐treatment |
| Other bias | Low risk | Not identified |
4‐PBS: four‐point box scale; AA: auricular acupuncture; AC:acupuncture; ANCOVA: analysis of covariance; ANOVA: analysis of variance; BA: baclofen; BMI: Body Mass Index; CI: confidence interval; CPGC: Chronic Pain Grade Classification; EA: electroacupuncture; EQ‐5D: EuroQol‐ 5 Dimension; GEE: generalized estimating equation; HADS: Hospital Anxiety and Depression Scale; HFAQ: Hannover Function Ability Questionnaire; IPAQ‐MET: International Physical Activity Questionnaire‐MET/min/week; HHQ‐CAM: Holistic Complementary and Alternative Health Questionnaire‐Complementary and Alternative Medicine; HHQ‐HH: Holistic; Complementary and Alternative Health Questionnaire‐Holistic Health subscale; ODI: Oswestry disability index; IQR: interquartile range; ITT: intention to treat; JOA: Japanese Orthopaedic Association; LBP: low back pain: LOCF: last‐observation‐carried‐forward; m: month; d: day; min: minutes; MANOVA: multivariate analysis of variance; MD: mean difference; MPQ: McGill Pain Questionnaire; MPS: myofascial pain syndrome; MYMOP‐2: Measure Yourself Medical Outcome Profile 2; NHP: Nottingham Health Profile; NPRS: numeric pain rating scale; NR: not reported; NSAIDs: Nonsteroidal anti‐inflammatory drugs; PDI: pain disability index; PENS: percutaneous electrical nerve stimulation therapy; PRF: pulsed radiofrequency; PRI: Pain Rating Index; RCT: randomized controlled trial; RMDQ: Roland Morris Disability Questionnaire; RR: risk ratio; SD: standard deviation SF‐36 or SF‐12: Short Form Health Survey; SMD: standardized mean difference; TCM: Traditional Chinese Medicine; TENS: Transcutaneous electrical nerve stimulation; TRP: trigger point; VAS: Visual Analog Scale; VRS: Verbal Rating Scale; wk: week; y: year(s).
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Araki 2001 | Acute low back pain (less than three days) was studied. |
| Bahrami‐Taghanaki 2014 | Participants with diverse LBP etiologies were included. |
| Bo 2014 | Acute and chronic LBP were included; chronic LBP group could not be separated out. |
| Ceccherelli 2002 | The study included LBP due to specific and nonspecific etiologies. |
| Chang 2012 | The study did not define the duration of LBP in inclusion criteria; chronic pain could not be separated out. |
| Chen 2015 | The acupuncture effect could not be extracted separately from an integrative medicine approach. |
| Chen 2016a | Almost half of the participants had lumbar disc protrusion. |
| Cherkin 2001 | The trial included participants who had pain for six weeks (did not meet our criteria for chronic low back pain). |
| Chong 2019 | The study aimed to investigate LBP patients of different durations which did not meet our inclusion criteria. |
| Coan 1980 | More than half of the included participants had sciatica. |
| Ding 1998 | The study was designed for LBP of different durations and chronic data could not be separated out. |
| Dong 2014 | Participants with diverse LBP etiologies included |
| Edelist 1976 | Study did not report pain duration; disc disease was involved. |
| Fu 2006 | The study assessed LBP patients who had suffered for less than three months as well as longer; a chronic group could not be separated out. |
| Garvey 1989 | The trial studied acute non‐radiating low back pain. |
| Giles 1999 | Almost half of the participants had positive findings on radiological images, accounting for specific LBP; outcomes of LBP participants could not be extracted separately from those with spine pain. |
| Giles 2003 | Participants with LBP could not be separated from participants with spine pain. |
| Griswold 2019 | The trial was designed for studying common LBP with different months of duration; therefore, the data for a chronic group could not be separated out. |
| Gu 2010 | Participants with diverse LBP etiologies were included. |
| Gunn 1980 | The chronic LBP group included some specific pain, caused by diseases such as disc protrusion and prolapsed disc. |
| Guo 2016 | The trial was designed for investigating LBP of mixed duration. |
| Han 2018b | Specific pain related to the kidneys was included. |
| He 1997 | Mixed duration of LBP; from five days to six months |
| Hu 2015 | The study compared acupuncture and moxibustion with acupuncture and heating lamp. It did not meet the inclusion criteria of acupuncture versus another intervention. |
| Inoue 2000 | The study investigated LBP of mixed duration. |
| Inoue 2001 | The study was designed to investigate LBP ranging from days to months. |
| Inoue 2006 | The study assessed specific LBP caused by lumbar vertebral arthritis diagnosed by physicians. |
| Inoue 2008 | The study assessed LBP patients suffering from a few days to more than one year and cases with specific LBP were included. |
| Inoue 2009 | Mixed LBP participants with different duration and etiologies were included. |
| Itoh 2004 | Most included participants had specific LBP. |
| Itoh 2005 | Most of the participants had LBP because of sciatica. |
| Itoh 2006 | LBP participants with pathological changes in the lumbar spine accounted for half of the participants. |
| Jing 2011 | Lower limb symptoms were the main manifestations of LBP. |
| Kawase 2006 | The study was designed to investigate mixed durations of LBP. |
| Kim 2009 | Participants with diverse LBP etiologies were included. |
| Kittang 2001 | The trial investigated acute LBP. |
| Kumnerddee 2009 | The study assessed 17 LBP patients with mixed duration. Chronic pain could not be separated out. |
| Kurosu 1979 | LBP duration was not reported. |
| Lee 2011 | The study assessed LBP lasting from less than one month, not chronic LBP. |
| Lee 2018 | Patients had specific LBP. |
| Lehmann 1983 | Some LBP participants had sciatica and others underwent lumbar surgery. |
| Li 1997 | The trial was designed to investigate LBP of different durations. |
| Li 2005 | The study compared acupuncture and moxibustion with physiotherapy, which did not meet the inclusion criteria of this review. |
| Li 2012 | The study compared acupuncture with acupuncture and local muscle exercise, which did not meet the inclusion criteria of this review. |
| Li 2013 | The study compared acupuncture and massage with acupuncture and massage and muscle exercise, which did not meet the inclusion criteria for two styles of acupuncture. |
| Li 2013a | LBP patients with different days and weeks duration were enrolled for analysis; the chronic data could not be separated out. |
| Li 2016 | Participants with specific LBP of different duration were studied. |
| Li 2016a | LBP patients with a mixed duration and specific etiologies were investigated. |
| Li 2018 | The study did not report the duration of the pain. |
| Lian 2005 | The number of participants with specific LBP accounted for half of the sample size. |
| Liu 2015 | The study compared lumbar electroacupuncture with electroacupuncture and muscle exercise, which did not meet the inclusion criteria of this review. |
| Liu 2017 | Specific LBP suggested by positive images was included. |
| Lopacz 1979 | The study assessed LBP lasting more than one month. |
| Macdonald 1983 | Specific LBP was studied, such as pain due to a prolapsed intervertebral disc. |
| Marignan Michel 2014 | It was unclear whether the study assessed nonspecific LBP and the randomization of this small pilot study was not explicit. |
| McKee 2012 | Not an RCT as randomization was not mentioned. |
| Mendelson 1983 | Patients with chronic LBP with specific etiologies were included, for example, pain due to traumatic spondylopathy and disc lesions. |
| Meng 2019 | Study was designed for general pain of unclear duration and the characteristics of LBP were not given (meeting abstract). |
| Miyazaki 2009 | Patients with a mixed pain duration were enrolled and investigated. |
| Moura 2019 | The study investigated chronic back pain including upper back pain. |
| Muller 2005 | The data from LBP participants could not be separated from data of participants with neck and back pain. |
| Pan 2018 | Specific pain caused by spinal disc herniation was included. |
| Puetz 2019 | The study assessed general LPB based where the duration and characteristics of the pain was not given (meeting abstract). |
| Sakai 1998 | The trial studied LBP of various duration. |
| Sakai 2001 | The trial studied LBP lasting more than two weeks. |
| Sator‐Katzenschlager 2004 | LBP participants with severe skeletal changes in lumbar spine were included (40%). |
| Sha 2018 | The acupuncture effect could not be extracted from the effects of the combined therapies. |
| Song 2014 | Data from the chronic LBP group could not be separated out from data from the participants with mixed duration of back pain. |
| Sun 2010 | LBP participants had pain ranging from days to months with mixed duration. |
| Sundberg 2009 | The enrolled participants had lower back, or neck pain, or both, of mixed duration; chronic LBP could not be separated out. |
| Takeda 2001 | Pain with or without specific etiologies was not described and pain duration was not defined. The study was designed to investigate general LBP and data from chronic nonspecific LBP could not be separated out. |
| Tellez‐Garcia 2015 | The study compared dry needling with dry needling plus another intervention, which did not meet the inclusion criteria for two styles of acupuncture. |
| Thomas 1994 | Pain due to specific etiologies was studied, such as sciatica and intervertebral disc degeneration. |
| Thomas 2005 | Data from chronic LBP participants could not be separated out from data from participants with a mixed duration of pain; more than half of the participants had leg pain. |
| Thomas 2006 | Data from chronic LBP participants could not be separated out from data from participants with a mixed duration of pain; more than half the participants had leg pain. |
| Tian 2016 | LBP patients with different duration of pain were studied and analyzed together. |
| Tonev 2010 | The study investigated acupuncture effects for subacute and chronic LBP together. |
| Toroski 2018 | Not a randomized controlled trial |
| Tsui 2004 | Specific LBP was included. |
| Von Mencke 1988 | The study did not report the duration of LBP; pain with specific etiologies was included. |
| Wang 1996 | The trial studied general LBP; duration of pain was not reported. |
| Wang 2013 | We assumed that this was not an RCT as randomization was not mentioned. |
| Wang 2016 | Data from acute and chronic LBP were studied together; data from the chronic group could not be separated out. |
| Wasan 2010 | LBP participants with diverse etiologies were included. |
| Witt 2006a | Data from the chronic LBP group could not be separated out from patients with headache and pain due to osteoarthritis. |
| Wu 1991 | The trial studied acute low back pain. |
| Wu 2012 | Unclear the specific duration for the 40 patients it studied. |
| Xian 2018 | Specific pain caused by spinal disc herniation was included. |
| Xiao 2014 | We assumed that this was not an RCT as randomization was not mentioned. |
| Yang 2008 | Sciatica was reported in more than half of the participants. |
| Yeung 2003 | LBP participants with diverse etiologies were included. |
| Yu 2002 | Randomization was not reported; cases like disc protrusion were included. |
| Yu 2010 | The study compared electroacupuncture with electroacupuncture and the McKenzie method, which did not meet the inclusion criteria for acupuncture versus another intervention. |
| Yu 2019 | The study compared massage with acupuncture combined with infrared light therapy. The effects of acupuncture alone could not be extracted out. |
| Zeng 2005 | The study compared acupuncture and cupping with TENS, which did not meet the inclusion criteria for acupuncture versus another intervention. |
| Zeng 2016 | Acute and chronic LBP were studied and analyzed together; it was impossible to separate out the data for the chronic group. |
| Zhao 2014 | The study compared acupuncture and cupping with acupuncture and heating lamp, which did not meet the inclusion criteria for two styles of acupuncture. |
| Zhou 2010 | The study compared acupuncture with another style of acupuncture plus another intervention, which did not meet the inclusion criteria for two styles of acupuncture. |
| Zhu 2016 | Both the intervention and control group received electroacupuncture and thus the acupuncture effect could not be separated out. |
LBP: low back pain; RCT: randomized controlled trial
Characteristics of studies awaiting classification [ordered by study ID]
Han 2018.
| Methods | Two‐arm RCT Number analyzed/randomized: 200/205 Statistical analysis: ITT analysis not mentioned; Chi² test; power analysis not conducted Funding source: Not reported (NR) Informed consent obtained; did not mention ethical approval |
| Participants |
Participant recruitment: NR Setting: NR Inclusion criteria: 1) pain lasting more than 12 weeks without specific reasons; 2) the pain area is between bilateral midaxillary line and below the costal margin and above the hip transverse, with or without leg pain Exclusion criteria: 1) low back pain due to specific disease (e.g. spine, nerve roots, coagulation disorders, cancer, osteoporosis, tuberculosis, fractures, infections, fracture, rheumatism Mean Age (years): 40.5 Gender (female %): 55.1% Pain duration: 3 months to 5 years Pain intensity (mean ± SD): NR |
| Interventions |
1) GROUP 1: Acupuncture Acupuncture points: BL23, BL25, DU3, BL17, DU4, DU14, Ashi point Depth: NR De Qi: Sour, numb, swell up and painful feelings were elicited. Sessions: 28 sessions (once per day, three days rest per seven days) Acupuncturist experience: NR 2) GROUP 2: Shock wave treatment Acupuncture points: same as Group 1 Depth: NR De Qi: Sour, numb and swell up feelings were elicited Sessions: Four sessions (one time per week) Co‐intervention: NR Duration of treatment: four weeks Duration of follow‐up: three months |
| Outcomes |
1) Global assessment: classified as cure, very effective, effective, and no effect Assessment time: one week and three months Costs: NR Adverse effects: NR |
| Notes |
Conclusion: Shock wave therapy showed much better global effect than acupuncture for chronic nonspecific low back pain. Language: Chinese |
Leite 2018.
| Methods | Four‐arm RCT Number analyzed/randomized: 69/86 Statistical analysis: ITT analysis not mentioned; Chi² test, Wilcoxon text, ANOVA, and Kruskal‐Wallis test; power analysis Funding source: Brazil grant Ethical approval and informed consents obtained |
| Participants |
Participant recruitment: NR Setting: at the Ambulatory of Laboratory for Research in Neurosciences, Federal University of Sergipe, Brazil Inclusion criteria: 1) low back pain diagnosis made by orthopedics physician; 2) pain on the lumbar region for at least three months; 3) never received acupuncture or electroacupuncture treatment Exclusion criteria: 1) doing physiotherapy or other treatment for low back pain; 2) pregnant or postpartum women who had given birth in the past three months; 3) having deformities or important amputations on lower limbs; 4) low back pain due to infection, tumor, osteoporosis, rheumatoid arthritis, vertebrae fracture, or radiculopathy; 5) nervous or cutaneous tissue injury affecting lumbar region; 6) active infectious processes; 7) surgery or invasive exams on the spine for the past three months; 8) inability to understand instructions or consent to the study; 9) psychiatric or cognitive impairments; 10) neurological, pulmonary, or cardiac disease; 11) heart pacemaker; 12) auditory, visual, or communication disturbance Mean Age (years): 46.38 Gender (female %): 55.1% Pain duration: NR Pain intensity (mean ± SD): 3.61‐4.40 (McGill tool,range) |
| Interventions |
1) GROUP 1: Electroacupuncture (n = 21) Acupuncture points: B22, B26, B50, B53 Depth: 10 mm De Qi: NR Sessions: Ten sessions (three times a week) Acupuncturist experience: NR During the 30‐minute stimulation, frequency was alternated between high and low every five seconds. 2) GROUP 2: Control 1 (needles + device off) (n = 22) Needles kept inserted for 30 minutes, with electrical stimulus for 45 seconds only 3) GROUP 3: Control 2 (needle alone) (n = 22) Participants had a needle inserted, without electrical stimulus. 4) GROUP 4: Control 3 (withdrawn needles) (n = 21) Needles placed in the acupoints as group 1; needles were withdrawn immediately after puncture which was not seen by patients. Co‐intervention: No additional components of treatment (moxibustion, cupping, and herbs) were used. Duration of treatment: four weeks Duration of follow‐up: immediate time point |
| Outcomes |
1) Pain intensity: 11‐point numerical rating pain scale (0 to 10); McGill Pain Questionnaire Assessment time: immediate time point Costs: NR Adverse effects: NR |
| Notes |
Conclusion: Compared to the controls, electroacupuncture treatment could not change the pain intensity in patients with chronic nonspecific low back pain. Language: English |
Tu 2019.
| Methods | Four‐arm RCT Number analyzed/randomized: 50/54 Statistical analysis: ITT analysis not mentioned; t‐test; power analysis not conducted Funding source: NIH/NCCIH in USA Ethical approval and informed consents not mentioned |
| Participants |
Participant recruitment: NR Setting: hospitals in US Inclusion criteria: patients diagnosed with chronic LBP with a duration of at least six months were included. Exclusion criteria: not reported in the paper Mean Age (years): 39.52 Gender (female %): NR Pain duration: 6.42 years Pain intensity (mean ± SD): NR |
| Interventions |
1) GROUP 1: Augmented real acupuncture (n = 12) Acupuncture points: GV3, BL23, BL40, KI3, and 1–3 ahshi points bilaterally Depth: NR De Qi: elicit 'deqi' by twirling the needles at 10 min and again just prior to needle removal Sessions: six sessions (twice a week for two weeks and then once a week for two weeks) Acupuncturist experience: a licensed acupuncturist "Patients randomly assigned to the augmented context group experienced a structured interaction with the acupuncturist lasting around 30 minutes." 2) GROUP 2: Augmented sham acupuncture (n = 13) The 12 sham acupoints were selected for the placebo acupuncture treatment using a Streitberger placebo acupuncture needle. Others were similar to GROUP 1. 3) GROUP 3: Limited real acupuncture (n = 12) "The acupuncturist merely read study information to the patient and aimed to 'converse with patients as little as possible'.”The acupuncture protocol was similar to GROUP 1. 4) GROUP 4: Limited sham acupuncture (n = 13) The same 12 sham acupoints were used. Others were similar to GROUP 3. Co‐intervention: medication and non‐pharmacological methods Duration of treatment: four weeks Duration of follow‐up: immediate time point |
| Outcomes |
1) Pain intensity: Patient Reported Outcomes Measurement Information System (PROMIS) subscores (higher values worse). 2) Physical function: PROMIS subscores (higher values worse). Assessment time: immediate time point. Costs: NR Adverse effects: NR |
| Notes |
Conclusion: ANCOVA results showed no significant main effect for treatment (real and sham acupuncture), context (augment and limited), and their interaction. Language: English |
ANCOVA: analysis of covariance; ANOVA: analysis of variance; ITT: intention to treat; NR: not reported; PROMIS: Patient Reported Outcomes Measurement Information System.
Characteristics of ongoing studies [ordered by study ID]
ACTRN12615000534583.
| Study name | The effects of different number of sessions of acupuncture in addition to usual care on chronic LBP |
| Methods | RCT |
| Participants | Adults with chronic low back pain |
| Interventions | Four sessions, seven sessions or ten sessions of acupuncture in addition to usual care |
| Outcomes | Pain intensity and back‐specific function were set as secondary outcomes. |
| Starting date | June 2015 |
| Contact information | lizhou.liu@otago.ac.nz (Principal investigator Lizhou Liu) |
| Notes | ACTRN12615000534583 |
IRCT20150602022539N9.
| Study name | The effect of electroacupuncture in non specific low back pain patients with gluteus maximus trigger points |
| Methods | RCT |
| Participants | Patients with nonspecific chronic low back pain at least three months from the onset of their pain |
| Interventions | Electroacupancture or routine physiotherapy |
| Outcomes | Primary outcome(s): Functional disability, pain, size of gluteus maximus muscle |
| Starting date | April 2019 |
| Contact information | Ziaeddin Safavi Farokhi, Semnan University of Medical Sciences |
| Notes | IRCT20150602022539N9 |
IRCT2017090224149N37.
| Study name | Treatment of chronic low back pain using a method of manual therapy and dry needling |
| Methods | RCT |
| Participants | Nonspecific chronic low back pain |
| Interventions | Dry needle treatment for one week in 3 sessions in addition to the control group |
| Outcomes | Functional disability; pain |
| Starting date | September 2017 |
| Contact information | Sharifian.pt@gmail.com |
| Notes | IRCT2017090224149N37 |
NCT02039037.
| Study name | Efficacy of acupuncture and electroacupuncture in participants with chronic nonspecific low back pain: randomised clinical trial |
| Methods | RCT |
| Participants | Adults between 20 and 60 years, with chronic low back pain lasting longer than three months |
| Interventions | Acupuncture versus electroacupuncture |
| Outcomes | Pain intensity and back‐specific function were set as primary outcomes |
| Starting date | January 2014 |
| Contact information | josiellicomachio@usp.br (Principal investigator Josielli Comachio) |
| Notes | NCT02039037 |
NCT02468297.
| Study name | Efficacy of electronic acupuncture shoes: a clinical trial for chronic low back pain |
| Methods | RCT |
| Participants | Adults with chronic low back pain |
| Interventions | Electronicacupunture shoes + placebo versus pseudo‐electrotherapy + ibuprofen |
| Outcomes | Pain intensity was set as a primary outcome. |
| Starting date | April 2009 |
| Contact information | Responsible party: Chen Yu Sheng, Medical Doctor, Chang Gung Memorial Hospital |
| Notes | NCT02468297 |
NCT03794869.
| Study name | Short‐term effects of exercise program versus electropuncture in patients with chronic non‐specific low back pain: a randomised clinical trial |
| Methods | RCT |
| Participants | Chronic nonspecific low back pain persisting ≥ 3 months, age between 25 and 60 years |
| Interventions | Percutaneous electrostimulation treatment (EPS) + exercise program |
| Outcomes | Primary outcome: algometry [time frame: at baseline and immediate post‐treatment] |
| Starting date | April 15, 2018 |
| Contact information | Adelaida María Castro‐Sánchez, PhD(Lecturer), Universidad de Almeria |
| Notes | NCT03794869 |
EPS: percutaneous electrcostimulation treatment; RCT: randomized controlled trial.
Differences between protocol and review
The previous review had included both acute and chronic nonspecific LBP (Furlan 2005). This review included only chronic nonspecific LBP. A protocol was not published for this review.
Literature searches: We added some new databases: CINAHLplus, CNKI and WangFang (Chinese databases), ClinicalTrials and WHO ICTRP (trial register databases). We did not search the Japanese databases as no one in our team had access or expertise in those databases.
We expanded on the definition of participants. We included studies with a majority of participants (> 50%) who had chronic nonspecific LBP, and studies enrolling populations with spine pain, if we could separate data for those who had chronic LBP.
We used the 13‐item risk of bias assessment recommended by CBN for this update (Furlan 2015). We had previously used the assessment tools used in Jadad 1996 and Van Tulder 2003.
We used the updated STRICTA recommendations to develop the 8‐item assessment form for the assessment of the adequacy of acupuncture (MacPherson 2010).
We used the GRADE approach, which is recommended by both the Cochrane Handbook for Systematic Reviews of Interventions and CBN guidelines, to assess the quality of the evidence in the updated review (Higgins 2019;).
The primary and secondary outcomes changed. In the protocol for the 2005 review, primary outcomes were pain, global measure, function, and return to work. In the updated review, they were pain, function, and quality of life. Secondary outcomes in the protocol were the physiological outcomes of physical exam, generic functional status, and medication. In this version, they were pain‐related disability, global assessment, and adverse events.
Types of interventions: usual care was added.
The changes we made were based on the development of methods of conducting systematic reviews, and the clinical research on acupuncture treatment for chronic nonspecific LBP.
Contributions of authors
Study concept and design: ADF, LXL, JLM
Development of search strategy: ADF, JLM
Searching for studies: JLM, ZPN
Study selection: JLM, ZPN, LXL, ADF
Data extraction: JLM, WYL, ADF
Data analysis: JLM, ADF
Adequacy of acupuncture treatment assessment: LXL, MH
Drafting and editing the manuscript: JLM, ADF, WYL, LXL
Critically revising manuscript for important intellectual content and providing final approval of the version to be published: all authors.
Sources of support
Internal sources
No sources of support supplied
External sources
NIH NCCIH, Cochrane Collaboration CAM Field – Resource for Research, R24 AT001293, USA
Foundation of Direction of Nangfang Hospital, 2018B008, China
National Natural Science Foundation of China, 81902009, China
Declarations of interest
JLM has no conflicts of interest. JLM is funded by the Foundation of Direction of Nangfang Hospital (2018B008) and National Natural Science Foundation (81902009) from China. JLM was funded by Post‐doctoral Fellow (PDF) Research Assistant Professor (RAP) Scheme of the University of Hong Kong when she started the research work. The relevant overseas travel grant for the 27th European Society of Intensive Care Medicine (ESICM) Congress was offered by the Chinese University of Hong Kong.
ADF has no conflicts of interest
WYL has no conflicts of interest
MH has no conflicts of interest
ZPN has no conflicts of interest
LXL has no conflicts of interest. LXL was funded by USA NIH grant: Number R24 AT001293. LXL was partially funded by Grant Number R24 AT001293 from the National Center for Complementary and Alternative Medicine (NCCAM) of the US National Institutes of Health.
New
References
References to studies included in this review
Brinkhaus 2006 {published data only}
- Brinkhaus B, Witt CM, Jena S, Linde K, Streng A, Wagenpfeil S, et al. Acupuncture in patients with chronic low back pain: a randomized controlled trial. Archives of Internal Medicine 2006;166(4):450-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Carlsson 2001 {published data only}
- Carlsson CP, Sjölund BH. Acupuncture for chronic low back pain: a randomized placebo-controlled study with long-term follow-up. Clinical Journal of Pain 2001;17(4):296-305. [PMID: ] [DOI] [PubMed] [Google Scholar]
Cesare 2011 {published data only}
- Di Cesare A, Giombini A, Di Cesare M, Ripani M, Vulpiani MC, Saraceni VM. Comparison between the effects of trigger point mesotherapy versus acupuncture points mesotherapy in the treatment of chronic low back pain: a short term randomized controlled trial. Complementary Therapies in Medicine 2011;19(1):19-26. [PMID: ] [DOI] [PubMed] [Google Scholar]
Chen 2010 {published data only}
- Chen LX, Duan JF, Wang YQ, Ding XH, Long GH. Effects of acupuncture/TENS and the two therapies combined on the treatment of chronic low back pain: a randomised control trial. Journal of Cervicodynia and Lumbodynia 2010;31(2):137-8. [Google Scholar]
Chen 2016 {published data only}
- Chen J, Lei NW, Liu JF, Zhu LW. Therapeutic effect of Jiaji electroacupunture with botulinum toxin type A on chronic low back pain. Journal of Clinical Acupuncture and Moxibustion 2016;32(4):4-6. [Google Scholar]
Cherkin 2009 {published data only}
- *.Cherkin DC, Sherman KJ, Avins AL, Erro JH, Ichikawa L, Barlow WE, et al. A randomized trial comparing acupuncture, simulated acupuncture, and usual care for chronic low back pain. Archives of Internal Medicine 2009;169(9):858-66. [PMID: 19433697 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherkin DC, Sherman KJ, Hogeboom CJ, Erro JH, Barlow WE, Deyo RA, et al. Efficacy of acupuncture for chronic low back pain: protocol for a randomized controlled trial. Trials 2008;9:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cho 2013 {published data only}
- Cho YJ, Song YK, Cha YY, Shin BC, Shin IH, Park HJ, et al. Acupuncture for chronic low back pain: a multicenter, randomized, patient-assessor blind, sham-controlled clinical trial. Spine (Phila Pa 1976) 2013;38(7):549-57. [PMID: ] [DOI] [PubMed] [Google Scholar]
Grant 1999 {published data only}
- Grant DJ, Bishop-Miller J, Winchester DM, Anderson M, Faulkner S. A randomized comparative trial of acupuncture versus transcutaneous electrical nerve stimulation for chronic back pain in the elderly. Pain 1999;82(1):9-13. [PMID: ] [DOI] [PubMed] [Google Scholar]
Haake 2007 {published data only}
- *.Haake M, Müller HH, Schade-Brittinger C, Basler HD, Schäfer H, Maier C, et al. German acupuncture trials (GERAC) for chronic low back pain: randomized, multicenter, blinded, parallel-group trial with 3 groups. Archives of Internal Medicine 2007;167(17):1892-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Haake M, Muller HH, Schade-Brittinger C, Prinz H, Basler HD, Streitberger K, et al. The German multicenter, randomized, partially blinded, prospective trial of acupuncture for chronic low-back pain: a preliminary report on the rationale and design of the trial. Journal of Alternative and Complementary Medicine (New York) 2003;9(5):763-70. [PMID: ] [DOI] [PubMed] [Google Scholar]
Hunter 2012 {published data only}
- *.Hunter RF, McDonough SM, Bradbury I, Liddle SD, Walsh DM, Dhamija S, et al. Exercise and auricular acupuncture for chronic low-back pain: a feasibility randomized-controlled trial. Clinical Journal of Pain 2012;28(3):259-67. [PMID: 21753728 ] [DOI] [PubMed] [Google Scholar]
- McDonough SM, Liddle SD, Hunter R, Walsh DM, Glasgow P, Gormley G, et al. Exercise and manual auricular acupuncture: a pilot assessor-blind randomised controlled trial (the Acupuncture and Personalised Exercise Programme (APEP) trial). BMC Musculoskeletal Disorders 2008;9:31. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Itoh 2009 {published data only}
- Itoh K, Itoh S, Katsumi Y, Kitakoji H. A pilot study on using acupuncture and transcutaneous electrical nerve stimulation to treat chronic non-specific low back pain. Complementary Therapies in Clinical Practice 2009;15(1):22-5. [PMID: ] [DOI] [PubMed] [Google Scholar]
Kerr 2003 {published data only}
- Kerr DP, Walsh DM, Baxter D. Acupuncture in the management of chronic low back pain: a blinded randomized controlled trial. Clinical Journal of Pain 2003;19(6):364-70. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Leibing 2002 {published data only}
- Leibing E, Leonhardt U, Köster G, Goerlitz A, Rosenfeldt JA, Hilgers R, et al. Acupuncture treatment of chronic low-back pain – a randomized, blinded, placebo-controlled trial with 9-month follow-up. Pain 2002;96(1-2):189-96. [PMID: ] [DOI] [PubMed] [Google Scholar]
Li 2017 {published data only}
- Li JH. Clinical observation on chronic nonspecific low back pain treated with oblique acupuncture. Journal of Shanxi College of Traditional Chinese Medicine 2016;18(6):50-2. [Google Scholar]
Lin 2010 {published data only}
- Lin ML, Lin MH, Fen JJ, Lin WT, Lin CW, Chen PQ. A comparison between pulsed radiofrequency and electro-acupuncture for relieving pain in patients with chronic low back pain. Acupuncture & Electro-therapeutics Research 2010;35(3-4):133-46. [DOI] [PubMed] [Google Scholar]
Meng 2003 {published data only}
- Meng CF, Wang D, Ngeow J, Lao L, Peterson M, Paget S. Acupuncture for chronic low back pain in older patients: a randomized, controlled trial. Rheumatology (Oxford) 2003;42(12):1508-17. [PMID: ] [DOI] [PubMed] [Google Scholar]
Molsberger 2002 {published data only}
- Molsberger AF, Mau J, Pawelec DB, Winkler J. Does acupuncture improve the orthopedic management of chronic low back pain – a randomized, blinded, controlled trial with 3 months follow up. Pain 2002;99(3):579-87. [PMID: ] [DOI] [PubMed] [Google Scholar]
Nie 2005 {published data only}
- Nie B, Tang ZG, Nie T, Yang SY. Effects of heating acupuncture for chronic non-specific low back pain. Journal of Clinical Acupuncture and Moxibustion 2005;21(4):22-3. [Google Scholar]
Pach 2013 {published data only}
- Pach D, Yang-Strobel X, Lüdtke R, Roll S, Icke K, Brinkhaus B, et al. Standardized versus individualized acupuncture for chronic low back pain: a randomized controlled trial. Evidence-based Complementary and Alternative Medicine 2013;2013:1-8. [PMID: 24288556] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pan 2005 {published data only}
- Pan L, Meng CR, Mi JP, Fo WB, Li WX, Wen X, et al. Comparing effect between acupuncture and heating acupuncture for chronic low back pain. Hebei Journal of Traditional Chinese Medicine 2005;27(10):759-61. [Google Scholar]
Pérez‐Palomares 2010 {published data only}
- Perez-Palomares S, Olivan-Blazquez B, Magallon-Botaya R, De-La-Torre-Beldarrain ML, Gaspar-Calvo E, Romo-Calvo L, et al. Percutaneous electrical nerve stimulation versus dry needling: effectiveness in the treatment of chronic low back pain. Journal of Musculoskeletal Pain 2010;18(1):23-30. [Google Scholar]
Shankar 2010 {published data only}
- Shankar N, Thakur M, Tandon POM, Saxena AK, Arora S, Bhattacharya N. Autonomic status and pain profile in patients of chronic low back pain and following electro acupuncture therapy: a randomized control trial. Indian Journal of Physiology and Pharmacology 2011;55(1):25-36. [PubMed] [Google Scholar]
Tsukayama 2002 {published data only}
- Tsukayama H, Yamashita H, Amagai H, Tanno Y. Randomised controlled trial comparing the effectiveness of electroacupuncture and TENS for low back pain: a preliminary study for a pragmatic trial. Acupuncture in Medicine 2002;20(4):175-80. [PMID: ] [DOI] [PubMed] [Google Scholar]
Ushinohama 2016 {published data only}
- Ushinohama A, Cunha BP, Costa LO, Barela AM, Freitas PB. Effect of a single session of ear acupuncture on pain intensity and postural control in individuals with chronic low back pain: a randomized controlled trial. Brazilian Journal of Physical Therapy 2016;20(4):328-35. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2016a {published data only}
- Wang G, Gao Q, Li J, Tian Y, Hou J. Impact of needle diameter on long-term dry needling treatment of chronic lumbar myofascial pain syndrome. American Journal of Physical Medicine & Rehabilitation 2016;95(7):483-94. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Weiss 2013 {published data only}
- Weiss J, Quante S, Xue F, Muche R, Reuss-Borst M. Effectiveness and acceptance of acupuncture in patients with chronic low back pain: results of a prospective, randomized, controlled trial. Journal of Alternative and Complementary Medicine (New York) 2013;19(12):935-41. [PMID: ] [DOI] [PubMed] [Google Scholar]
Witt 2006 {published data only}
- *.Witt CM, Jena S, Selim D, Brinkhaus B, Reinhold T, Wruck K, et al. Pragmatic randomized trial evaluating the clinical and economic effectiveness of acupuncture for chronic low back pain. American Journal of Epidemiology 2006;164(5):487-96. [PMID: 16798792 ] [DOI] [PubMed] [Google Scholar]
- Witt CM, Schutzler L, Ludtke R, Wegscheider K, Willich SN. Patient characteristics and variation in treatment outcomes: which patients benefit most from acupuncture for chronic pain? Clinical Journal of Pain 2011;27(6):550-5. [PMID: ] [DOI] [PubMed] [Google Scholar]
Yuan 2009 {published data only}
- Yuan J, Purepong N, Hunter RF, Kerr DP, Park J, Bradbury I, et al. Different frequencies of acupuncture treatment for chronic low back pain: an assessor-blinded pilot randomised controlled trial. Complementary Therapies in Medicine 2009;17(3):131-40. [PMID: ] [DOI] [PubMed] [Google Scholar]
Yuan 2016 {published data only}
- Yuan QL, Liu L, Ma JT, Wu WT, Ye ML, Zhang YG. A clinical study of acupuncture for low back pain. The Journal of Traditional Chinese Orthopedics and Traumatolog 2016;28(6):12-7. [Google Scholar]
Yun 2012 {published data only}
- Yun M, Xiong N, Guo M, Zhang J, Liu D, Luo Y, et al. Acupuncture at the back pain-acupoints for chronic low back pain of peacekeepers in Lebanon: a randomized controlled trial. Journal of Musculoskeletal Pain 2012;20(2):107-15. [Google Scholar]
Yun 2012a {published data only}
- Yun M, Shao Y, Zhang Y, He S, Xiong N, Zhang J, et al. Hegu acupuncture for chronic low-back pain: a randomized controlled trial. Journal of Alternative and Complementary Medicine (New York) 2012;18(2):130-6. [DOI] [PubMed] [Google Scholar]
Zaringhalam 2010 {published data only}
- Zaringhalam J, Manaheji H, Rastqar A, Zaringhalam M. Reduction of chronic non-specific low back pain: a randomised controlled clinical trial on acupuncture and baclofen. Chinese Medicine 2010;5(15):1-7. [PMC2867967] [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhao 2012 {published data only}
- Zhao F, Cao DB, Yuan YQ, Luo J, Wen YY, Wang Y, et al. Efficacy observation of nonspecific low back pain treated with the dragon-tiger fighting needling method. Chinese Acupuncture & Moxibustion 2012;32(6):507-10. [PubMed] [Google Scholar]
References to studies excluded from this review
Araki 2001 {published data only}
- Araki S, Kawamura O, Mataka T, Fujioka H, Shiro K,Tomoyuki T. Randomized controlled trial comparing the effect of manual acupuncture with sham acupuncture for acute low back pain [RCT ni yoru kyuseiyotsu–sho ni taisuru shishin–gun to gishin–gun no tiryou koka]. Journal of the Japan Society of Acupuncture and Moxibustion 2001;51(3):382. [Google Scholar]
Bahrami‐Taghanaki 2014 {published data only}
- Bahrami-Taghanaki H, Liu Y, Azizi H, Khorsand A, Esmaily H, Bahrami A, et al. A randomized, controlled trial of acupuncture for chronic low-back pain. Alternative Therapies in Health & Medicine 2014;20(3):13-9. [PMID: ] [PubMed] [Google Scholar]
Bo 2014 {published data only}
- Bo LL, Chen LQ, Peng HY, Xu Q. Electroacupuncture and external application of Chinese medicine in treatment of cold and damp low back pain. Jiang Su Traditional Chinese Medicine Journal 2014;46(9):60-1. [Google Scholar]
Ceccherelli 2002 {published data only}
- Ceccherelli F, Rigoni MT, Gagliardi G, Ruzzante L. Comparison of superficial and deep acupuncture in the treatment of lumbar myofascial pain: a double-blind randomized controlled study. Clinical Journal of Pain 2002;18(3):149-53. [PMID: ] [DOI] [PubMed] [Google Scholar]
Chang 2012 {published data only}
- Chang DH, Bae UY, Jung JH, Lee IS. The effects of burning acupuncture therapy with Chuna therapy for low back pain patients. Journal of Oriental Rehabilitation Medicine 2011;21(3):21-32. [Google Scholar]
Chen 2015 {published data only}
- Chen J, Lei NW, Song WB, Zhu LW. Treatment of chronic non-specific low back pain with acupuncture and Mckenzie method. Acta Chinese Medicine and Pharmacology 2015;43(6):66-8. [Google Scholar]
Chen 2016a {published data only}
- Chen LD, Hou XP. Comparison of effect of warm acupuncture with conventional acupuncture for the treatment of cold dampness lumbago. China Modern Medicine 2016;25(23):150-2. [Google Scholar]
Cherkin 2001 {published data only}
- *.Cherkin DC, Eisenberg D, Sherman KJ, T J Kaptchuk, J Street, et al. Randomized trial comparing traditional Chinese medical acupuncture, therapeutic massage, and self-care education for chronic low back pain. Archives of Internal Medicine 2001 2001;161(8):1081-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Kalauokalani D, Cherkin DC, Sherman KJ, Koepsell TD, Deyo RA. Lessons from a trial of acupuncture and massage for low back pain: patient expectations and treatment effects. Spine 2001;26(13):1418-24. [PMID: ] [DOI] [PubMed] [Google Scholar]
Chong 2019 {published data only}
- Chong FF, Geng BL, Zhu PF, Zhao KP. The effect of acupuncture with or without Shen Tong Zhu Yu Tang for low back pain treatment. Chinese Primary Health Care 2019;33(3):58-60. [Google Scholar]
Coan 1980 {published data only}
- Coan RM, Wong G, Ku SL, Chan YC, Wang L, Ozer FT, et al. The acupuncture treatment of low back pain: a randomized controlled study. American Journal of Chinese Medicine 1980;8(1-2):181-9. [PMID: 6446852] [DOI] [PubMed] [Google Scholar]
Ding 1998 {published data only}
- Ding YD. Fly-probing-acupoint manipulation as a main treatment for lumbago. Shanghai Journal of Acupuncture and Moxibustion 1998;17(5):25–6. [MEDLINE: 4] [Google Scholar]
Dong 2014 {published data only}
- Dong G, Tian LQ, Zhu SF, Xu GF. Efficacy of laser acupuncture in treating cold-damp low back pain. Chinese Journal of Laser Medicine & Surgery 2014;23(6):354-7. [Google Scholar]
Edelist 1976 {published data only}
- Edelist G, Gross AE, Langer F. Treatment of low back pain with acupuncture. Canadian Anaesthetists Society Journal 1976;23:303–6. [DOI] [PubMed] [Google Scholar]
Fu 2006 {published data only}
- Fu ZH, Chen XY, Lu LJ, Lin J, Xu JG. Immediate effect of Fu's subcutaneous needling for low back pain. Chinese Medical Journal 2006;119(11):953-6. [PMID: ] [PubMed] [Google Scholar]
Garvey 1989 {published data only}
- Garvey TA, Marks MR, Wiesel SW. A prospective, randomized,double-blind evaluation of trigger-point injection therapy for low back pain. Spine 1989;14:962–4. [DOI] [PubMed] [Google Scholar]
Giles 1999 {published data only}
- Giles LG, Muller R. Chronic spinal pain syndromes: a clinical pilot trial comparing acupuncture, a nonsteroidal anti-inflammatory drug, and spinal manipulation. Journal of Manipulative and Physiological Therapeutics 1999;22(6):376-81. [PMID: ] [DOI] [PubMed] [Google Scholar]
Giles 2003 {published data only}
- Giles LG, Muller R. Chronic spinal pain: a randomized clinical trial comparing medication, acupuncture, and spinal manipulation. Spine 2003;28(14):1490-502; discussion 1502-3. [PMID: ] [DOI] [PubMed] [Google Scholar]
Griswold 2019 {published data only}
- Griswold D, Gargano F, Learman KE. A randomised clinical trial comparing non-thrust manipulation with segmental and distal dry needling on pain, disability, and rate of recovery for patients with non-specific low back pain. Journal of Manual & Manipulative Therapy 2019;27(3):141-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gu 2010 {published data only}
- Gu T. Effectiveness of acupuncture and exercise therapy in treating chronic low back pain. China Medical Herald 2010;7(28):84-5. [Google Scholar]
Gunn 1980 {published data only}
- Gunn CC, Milbrandt WE, Little AS, Mason KE. Dry needling of muscle motor points for chronic low-back pain: a randomized clinical trial with long-term follow-up. Spine 1980;5(3):279-91. [PMID: ] [DOI] [PubMed] [Google Scholar]
Guo 2016 {published data only}
- Guo YC. The Immediate Effect of Acupuncture Treatment for Nonspecific Low Back Pain with Zang Fu Bie Tong Theory [thesis]. Fujian University of Traditional Chinese Medicine, 2016. [Google Scholar]
Han 2018b {published data only}
- Han ZM, Liu Y, Luo YP, Peng XJ, Shen J, Zhan SQ, et al. A clinical trial comparing shock wave therapy with acupuncture for chronic low back pain. Guide of China Medicine 2018;16(31):169-70. [Google Scholar]
He 1997 {published data only}
- He RY. Clinical observation on treatment of lumbago due to cold-dampness by warm-acupuncture plus Chinese medicine. Chinese Acupuncture & Moxibustion 1997;17(5):279–80. [MEDLINE: ] [Google Scholar]
Hu 2015 {published data only}
- Hu B. A comparison between acupuncture plus moxibustion and acupuncture plus heating lamp for treatment of chronic low back pain. Hubei Journal of Traditional Chinese Medicine 2015;37(12):58-9. [Google Scholar]
Inoue 2000 {published data only}
- Inoue M, Kitakouji H, Ikeuchi R, Katayama K, Ochi H, Imakei. Randomized controlled pilot study comparing acupuncture with sham acupuncture for lumbago [Yotsu ni taisuru gishin womochiita randamuka hikaku–shiken no kokoromi]. Journal of the Japan Society of Acupuncture and Moxibustion 2000;50(2):356. [MEDLINE: ] [Google Scholar]
Inoue 2001 {published data only}
- Inoue M, Kitakouji H, Ikeuchi R, Katayama K, Ochi H, Nakanishi H. Randomized controlled pilot study comparing manual acupuncture with sham acupuncture for lumbago (2nd report) [Yotsu ni taisuru gishin wo mochiita randamuka hikaku–shiken nokokoromi]. Journal of The Japan Society of Acupuncture and Moxibustion 2001;51(3):412. [Google Scholar]
Inoue 2006 {published data only}
- Inoue M, Kitakoji H, Ishizaki N, Tawa M, Yano T, Katsumi Y, et al. Relief of low back pain immediately after acupuncture treatment - a randomised, placebo controlled trial. Acupuncture in Medicine 2006;24(3):103-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Inoue 2008 {published data only}
- Inoue M, Nakajima M, Itoi M, Ohashi S, Yano T. The comparison of the effectiveness between acupuncture treatment and local injection for low back pain - a randomized controlled trial. Journal of the Japanese Society of Balneology, Climatology and Physical Medicine 2008;71(4):211-20. [Google Scholar]
Inoue 2009 {published data only}
- Inoue M, Hojo T, Nakajima M, Kitakoji H, Itoi M. Comparison of the effectiveness of acupuncture treatment and local anaesthetic injection for low back pain: a randomised controlled clinical trial. Acupuncture in Medicine 2009;27(4):174-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Itoh 2004 {published data only}
- Itoh K, Katsumi Y, Kitakoji H. Trigger point acupuncture treatment of chronic low back pain in elderly patients - a blinded RCT. Acupuncture in Medicine 2004;22(4):170-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Itoh 2005 {published data only}
- Itoh K, Katsumi Y. Effect of acupuncture treatment on chronic low back pain with leg pain in aged patients. Journal of the Japan Society of Acupuncture and Moxibustion 2005;55(4):530-7. [Google Scholar]
Itoh 2006 {published data only}
- Itoh K, Katsumi Y, Hirota S, Kitakoji H. Effects of trigger point acupuncture on chronic low back pain in elderly patients - a sham-controlled randomised trial. Acupuncture in Medicine 2006;24(1):5-12. [PMID: ] [DOI] [PubMed] [Google Scholar]
Jing 2011 {published data only}
- Jing HT, Peng YY, Chen M, Huang YS. Clinical observation of lumbar spinal stenosis treated with deep puncture at Jiaji (EX-B2). Chinese Acupuncture & Moxibustion 2011;31(9):791-4. [PMID: ] [PubMed] [Google Scholar]
Kawase 2006 {published data only}
- Kawase Y, Ishigami T, Nakamura H, Hattori T, Minagawa M, Kouda H, et al. Acupuncture treatment for lower back pain: multi-center randomized controlled trial using sham acupuncture as a control. Journal of the Japan Scoiety of Acupuncture and Moxibustion 2006;56(2):140-9. [Google Scholar]
Kim 2009 {published data only}
- Kim SM, Kim HJ, Lee MJ, Shin YJ. Effects of local and Sa-am acupuncture on hypoadrenia and chronic low back pain. Journal of Korean Oriental Medicine, 2009;30(2):104-16. [Google Scholar]
Kittang 2001 {published data only}
- Kittang G, Melvaer T, Baerheim A. Acupuncture contra antiphlogistics in acute lumbago [Akupunktur kontra antiflogistika ved akutt lumbago]. Tidsskrift for den Norske Laegeforening: Tidsskrift for Praktisk Medicin, ny Raekke 2001;121(10):1207-10. [PMID: ] [PubMed] [Google Scholar]
Kumnerddee 2009 {published data only}
- Kumnerddee, W. Effectiveness comparison between Thai traditional massage and Chinese acupuncture for myofascial back pain in Thai military personnel: a preliminary report. Journal of the Medical Association of Thailand 2009.;92(Suppl 1):S117-23. [PMID: ] [PubMed] [Google Scholar]
Kurosu 1979 {published data only}
- Kurosu Y. Acupuncture and moxibustion for lumbago (II) - comparative experiment of the therapeutic effectiveness of acupuncture and garlic moxibustion. Journal of the Japan Acupuncture & Moxibustion Association 1979;28(2):31-4. [MEDLINE: ] [Google Scholar]
Lee 2011 {published data only}
- Lee JB, Im JG, Lee HG, Kim JU, Yook TH, Song BY. The comparison of effectiveness between acupuncture and its cotreatment with wan-gwa acupuncture on the treatment of low back pain. Journal of Korean Acupuncture & Moxibustion Society 2011;28(2):43-7. [Google Scholar]
Lee 2018 {published data only}
- Lee HJ, Choi BI, Jun S, Park MS, Oh SJ, Lee JH, et al. Efficacy and safety of thread embedding acupuncture for chronic low back pain: a randomised controlled pilot trial. Trials 2019;10(1):680. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lehmann 1983 {published data only}
- Lehmann TR, Russell DW, Spratt KF, Colby H, Liu YK, Fairchild ML, et al. Efficacy of electroacupuncture and TENS in the rehabilitation of chronic low back pain patients. Pain 1986;26(3):277-90. [PMID: ] [DOI] [PubMed] [Google Scholar]
- *.Lehmann TR, Russell DW, Spratt KF. The impact of patients with nonorganic physical findings on a controlled trial of transcutaneous electrical nerve stimulation and electroacupuncture. Spine 1983;8(6):625-34. [DOI] [PubMed] [Google Scholar]
Li 1997 {published data only}
- Li Q, Shang WM. The effect of acupuncture plus cupping on 78 cases with lumbago. Hebei Chinese Traditional Medicine 1997;19(5):28. [MEDLINE: ] [Google Scholar]
Li 2005 {published data only}
- Li N, Wu B, Wang CW. Comparison of acupuncture-moxibustion and physiotherapy in treating chronic non-specific low back pain. Chinese Journal of Clinical Rehabilitation 2005;9(2):186-7. [Google Scholar]
Li 2012 {published data only}
- Li L, Feng WW, Lu HF, Li C. Comparing the effect between acupuncture and combined acupuncture with local muscle exercise for chronic non-specific low back pain treatment. Chinese Journal of Rehabilitation Medicine 2012;27(5):475-6. [Google Scholar]
Li 2013 {published data only}
- Li CZ, Shu GJ, Chen Y, Tao HX, Xiang Y, Li J, et al. Effect of acupuncture and massage and Thera-Band physical exercise for chronic non-specific low back pain. Chinese Journal of Rehabilitation Medicine 2013;28(1):51-3. [Google Scholar]
Li 2013a {published data only}
- Li QT. Treatment of chronic lumbar muscle strain with acupuncture and bloodletting therapy. Modern Journal of Integrated Traditional Chinese and Western Medicine 2013;22(1):64-5. [Google Scholar]
Li 2016 {published data only}
- Li RQ, Wei NR, Sun LX, Xin HY, Zhang YL, Liu YS. The effectiveness of acupoint catgut embedding therapy and electroacupuncture treatment on chronic low back pain. Hainan Medical Journal 2016;27(1):125-8. [Google Scholar]
Li 2016a {published data only}
- Li WS, Yue XY, Xu JH, Wu DZ, Zhou YH, Sun SY, et al. Comparison of effect of electroacupuncture with warm needling for treatment of low back pain. Shanghai Journal of Acupuncture and Moxibustion 2016;35(7):866-9. [Google Scholar]
Li 2018 {published data only}
- Li HL, Zhang JS. The treatment of electroacupuncture for nonspecific low back pain.. Journal of New Chinese Medicine 2018;50(8):170-2. [Google Scholar]
Lian 2005 {published data only}
- Lian N, Liu JB, Francisco T, Yan QM, Edwin G. Improvement of dermal needle and body acupuncture on pain due to lumbar strain and hyperplastic spondylitis. Chinese Journal of Clinical Rehabilitation 2005;9(42):161-3. [Google Scholar]
Liu 2015 {published data only}
- Liu HJ, Zhu SG, Qiu YF, Dong L, Qin T, Fu YL. Effects of lumbar muscle exercise combined with electroacupuncture for chronic non-specific low back pain. Chinese Journal of Rehabilitation 2015;30(4):296-7. [Google Scholar]
Liu 2017 {published data only}
Lopacz 1979 {published data only}
- Lopacz S, Gralewski Z. A trial of assessment of the results of acupuncture or suggestion in the treatment of low back pain. Neurologia i Neurochirurgia Polska 1979;8:405-9. [PubMed] [Google Scholar]
Macdonald 1983 {published data only}
- Macdonald AJ, Macrae KD, Master BR, Rubin AP. Superficial acupuncture in the relief of chronic low back pain. Annals of The Royal College of Surgeons of England 1983;65(1):44-6. [PMC free article] [PubMed] [Google Scholar]
Marignan Michel 2014 {published data only}
- Marignan M. Auriculotherapy treatment protocol for low-back pain: a randomized trial. Medical Acupuncture 2014;26(3):154-60. [Google Scholar]
McKee 2012 {published data only}
- McKee MD, Kligler B, Blank AE, Fletcher J, Jeffres A, Casalaina W, et al. The ADDOPT study (Acupuncture to Decrease Disparities in Outcomes of Pain Treatment): feasibility of offering acupuncture in the community health centre setting. Journal of Alternative and Complementary Medicine (New York) 2012;18(9):839-43. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mendelson 1983 {published data only}
- Mendelson G, Kidson MA, Loh ST, Scott DF, Selwood TS, Kranz H. Acupuncture analgesia for chronic low back pain. Clinical Experimental Neurology 1978;15:182–5. [PubMed] [Google Scholar]
- *.Mendelson G, Selwood TS, Kranz H, Loh TS, Kidson MA, Scott DS. Acupuncture treatment of chronic back pain.: a double-blind placebo-controlled trial. American Journal of Medicine 1983;74:49–55. [DOI] [PubMed] [Google Scholar]
Meng 2019 {published data only}
- Meng Q, Wang Y, Yu C, Liu C. The clinical study of internal heat needling versus TCM acupuncture in the treatment of nonspecific low back pain (NLBP). Advances in Integrative Medicine 2019;6:S51.
Miyazaki 2009 {published data only}
- Miyazaki S, Hagihara A, Kanda R, Mukaino Y, Nobutomo K. Applicability of press needles to a double-blind trial: a randomized, double-blind, placebo-controlled trial. Clinical Journal of Pain 2009;25(5):438-44. [PMID: ] [DOI] [PubMed] [Google Scholar]
Moura 2019 {published data only}
- Moura CC, Chaves ECL, Chianca TCM, Ruginsk SG, Nogueira DA, Souza VHS, et al. Contribution of Chinese and French ear acupuncture for the management of chronic back pain: a randomised controlled trial. Journal of Clinical Nursing 2019;28(21-22):3796-806. [PMID: ] [DOI] [PubMed] [Google Scholar]
Muller 2005 {published data only}
- Muller R, Giles LG. Long-term follow-up of a randomized clinical trial assessing the efficacy of medication, acupuncture, and spinal manipulation for chronic mechanical spinal pain syndromes. Journal of Manipulative and Physiological Therapeutics 2005;28(1):3-11. [PMID: ] [DOI] [PubMed] [Google Scholar]
Pan 2018 {published data only}
- Pan XA, Wu XM, Chan J, Li P. Curative effect observation on acupuncture combined with you gui capsules for chronic low back pain with kidney-yang deficiency. Journal of New Chinese Medicine 2018;50(12):218-20. [Google Scholar]
Puetz 2019 {published data only}
- Puetz CL, Kong JT. Electro-acupuncture for the treatment of chronic low back pain: effectiveness and prediction. Pain Medicine 2019;20(3):642. [Google Scholar]
Sakai 1998 {published data only}
- Yamashita H, Kiichiro T, Tsukayama H, Nakamura T, Ikeuchi T, Kawamoto M. Are the effects of electro-acupuncture on low back pain equal to those of TENS? Focus on Alternative and Complementary Therapies 2001;6(4):254-5. [MEDLINE: ] [Google Scholar]
Sakai 2001 {published data only}
- Sakai T, Tsutani K, Tsukayama H, Nakamura T, Ikeuchi T, Kawamoto M, et al. Multi-center randomized controlled trial of acupuncture with electric stimulation and acupuncture-like transcutaneous electrical nerve stimulation for lumbago. Journal of the Japan Society of Acupuncture and Moxibustion 2001;51:175-84. [Google Scholar]
Sator‐Katzenschlager 2004 {published data only}
- Sator-Katzenschlager SM, Scharbert G, Kozek-Langenecker SA, Szeles JC, Finster G, Schiesser AW, et al. The short- and long-term benefit in chronic low back pain through adjuvant electrical versus manual auricular acupuncture. Anesthesia and Analgesia 2004;98(5):1359-64. [PMID: ] [DOI] [PubMed] [Google Scholar]
Sha 2018 {published data only}
- Sha SY, Zhang M, Meng QL. Clinical study on curative effects of nonspecific low back pain based on back-shu and front-mumatching acupoints method of acupuncture combined with rehabilitation treatment. World Chinese Medicine 2018;13(11):2847-50. [Google Scholar]
Song 2014 {published data only}
- Song WL, Zhang J, Qin YX, Wang DZ. The compound intervention of moxibustion box and floating acupuncture for chronic low back pain treatment. Journal of Guiyang College of Traditional Chinese Medicine 2014;36(1):91-2. [Google Scholar]
Sun 2010 {published data only}
- Sun YZ, Li DY. Observation on lower back myofascitis treated with penetration needling on yang meridians of the back and electroacupuncture as compared with Western medication. Zhongguo Zhen Jiu 2010;30(10):816-8. [PMID: ] [PubMed] [Google Scholar]
Sundberg 2009 {published data only}
- Sundberg T, Petzold M, Wandell P, Ryden A, Falkenberg T. Exploring integrative medicine for back and neck pain - a pragmatic randomised clinical pilot trial. BMC Complementary and Alternative Medicine 2009;9:33. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Takeda 2001 {published data only}
- Takeda H, Nabeta T. Randomized controlled trial comparing the effect of distal point needling with local point needling for low back pain [RCT ni yoru yotsu–sho ni taisuru enkakubu–sisin tokyokusho–sisin no koka hikaku]. Journal of the Japan Society of Acupuncture and Moxibustion 2001;51(3):411. [Google Scholar]
Tellez‐Garcia 2015 {published data only}
- Téllez-García M, De-la-Llave-Rincón AI, Salom-Moreno J, Palacios-Ceña M, Ortega-Santiago R, Fernández-de-Las-Peñas C. Neuroscience education in addition to trigger point dry needling for the management of patients with mechanical chronic low back pain: a preliminary clinical trial. Journal of Bodywork and Movement Therapies 2015;19(3):464-72. [PMID: ] [DOI] [PubMed] [Google Scholar]
Thomas 1994 {published data only}
- Thomas M, Lundberg T. Importance of modes of acupuncture in the treatment of chronic nociceptive low back pain. Acta Anaesthesiologica Scandinavica 1994;38(1):63-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Thomas 2005 {published data only}
- Thomas KJ, MacPherson H, Ratcliffe J, Thorpe L, Brazier J, Campbell M, et al. Longer term clinical and economic benefits of offering acupuncture care to patients with chronic low back pain. Health Technology Assessment (Winchester, England) 2005;9(32):iii-iv, ix-x, 1-109. [PMID: ] [DOI] [PubMed] [Google Scholar]
Thomas 2006 {published data only}
- Thomas KJ, MacPherson H, Thorpe L, Brazier J, Fitter M, Campbell MJ, et al. Randomised controlled trial of a short course of traditional acupuncture compared with usual care for persistent non-specific low back pain. BMJ (Clinical Research Ed) 2006;333(7569):623. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tian 2016 {published data only}
- Tian M, Zhong ZG. Intensive silver needle acupuncture therapy for treatment of chronic low back pain. Asia-Pacific Traditional Medicine 2016;12(8):93-4. [Google Scholar]
Tonev 2010 {published data only}
- Tonev D, Radeva S, Toncheva A. Non-pharmacological treatment of subacute and chronic low back pain without radiculopathy: acupuncture versus physiotherapy. Revmatologiia 2010;18(2):46-50. [Google Scholar]
Toroski 2018 {published data only}
Tsui 2004 {published data only}
- Tsui ML, Cheing GL. The effectiveness of electroacupuncture versus electrical heat acupuncture in the management of chronic low-back pain. Journal of Alternative and Complementary Medicine (New York) 2004;10(5):803-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Von Mencke 1988 {published data only}
- Von Mencke M, Wieden TE, Hoppe M, Porschke W, Hoffmann O, Herget HF. Akupunktur des schulter-arm-syndroms und de lumbagie/ischialgie - zwei prosepktive doppelblind-studien* (TeilII). Akupunktur 1989;5:5–13. [Google Scholar]
- *.Von Mencke M, Wieden TE, Hoppe M, Porschke W, HoffmannO, Herget HF. Akupunktur des schulter-arm-syndroms und der lumbagie/ischialgie - zwei prosepktive doppelblind-studien* (TeilI). Akupunktur 1988;4:204–15. [Google Scholar]
Wang 1996 {published data only}
- Wang JX. The effect of acupuncture on 492 cases with lumbago. Shanghai Acupuncture Journal 1996;15(5):8. [MEDLINE: ] [Google Scholar]
Wang 2013 {published data only}
- Wang YN, Zhao ZY. Treatment of thirty-two patients of low back pain with acupuncture on points in abdomen. Zhejing Journal of Traditional Chinese Medicine 2013;48(11):830-1. [Google Scholar]
Wang 2016 {published data only}
- Wang HW. The effect of integrative medicine for treatment of lumbar muscle strain. Journal of Clinical Medical Literature 2016;3(6):1132-4. [Google Scholar]
Wasan 2010 {published data only}
- Wasan AD, Kong J, Pham LD, Kaptchuk TJ, Edwards R, Gollub RL. The impact of placebo, psychopathology, and expectations on the response to acupuncture needling in patients with chronic low back pain. Journal of Pain 2010;11(6):555-63. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Witt 2006a {published data only}
- Witt CM, Brinkhaus B, Willich SN. Acupuncture. Clinical studies on efficacy and effectiveness in patients with chronic pain [Akupunktur: Klinische studien zur wirksamkeit bei patienten mit chronischen schmerzen]. Bundesgesundheitsblatt, Gesundheitsforschung, Gesundheitsschutz 2006;49(8):736-42. [PMID: ] [DOI] [PubMed] [Google Scholar]
Wu 1991 {published data only}
- Wu YC, Xu GG. Acupuncture for 150 cases of acute lumbago. Shanghai Journal of Acupuncture and Moxibustion 1991;10(2):18-9. [MEDLINE: ] [Google Scholar]
Wu 2012 {published data only}
- Wu CH. Treatment effect of acupuncture and angelica injection for low back pain in the elderly. China Healthcare and Nutrition 2012;9(10):335. [Google Scholar]
Xian 2018 {published data only}
- Xian SS, Jiang GL, Nie DF. Clinical observation of Tong Du spinal rotation massage in observation of 30 patients with backache. Medical & Pharmaceutical Journal of Chinese Peoples Liberation Army 2018;030(002):66-9. [Google Scholar]
Xiao 2014 {published data only}
- Xiao J, Zhu LG, Jin T, Chen JF, Yu J, Feng MS. Comparison of paravertebral soft tissue tension changes in patients with chronic lower back pain treated by sliver needle and traditional Chinese medicine fumigation. China Journal of Orthopaedics and Traumatology 2014;27(6):513-7. [PubMed] [Google Scholar]
Yang 2008 {published data only}
- Yang XX, Qiu F, Meng LX. Treatment of low back pain by acupuncture and Mckenzie method. Aerospace Medicine 2008;19(4):238-9. [Google Scholar]
Yeung 2003 {published data only}
- Yeung CK, Leung MC, Chow DH. The use of electro-acupuncture in conjunction with exercise for the treatment of chronic low-back pain. Journal of Alternative and Complementary Medicine (New York) 2003;9(4):479-90. [PMID: ] [DOI] [PubMed] [Google Scholar]
Yu 2002 {published data only}
- Yu LH, Wu NS, Zhang KP. An investigation of treatment with silver acupuncture for pain of chronic soft tissue lesions in low back. Chinese Journal of Clinical Rehabilitation 2002;6(14):2176-7. [Google Scholar]
Yu 2010 {published data only}
- Yu QJ, Liu B. Effects of McKenzie method with electroacupuncture treatment for chronic non-specific low back pain. Chronic Pathematology Journal 2010;12(9):1004. [Google Scholar]
Yu 2019 {published data only}
- Yu C, Jia D, Wan Y, Jiang H, Liu YC, Shang H, et al. The clinical study of Chinese Tuina versus acupuncture in the treatment of chronic nonspecific low back pain (CNLBP). Advances in Integrative Medicine 2019;6:S54-151.
Zeng 2005 {published data only}
- Zeng HH, Wu SL, Huang LR, Ma C, Xiao XH. Effect of acupuncture combined with cupping on the pain index in patients with chronic lumbar muscle strain. Chinese Journal of Clinical Rehabilitation 2005;9(26):46-7. [Google Scholar]
Zeng 2016 {published data only}
- Zeng Y. The Immediate Effect of Acupuncture Treatment for Nonspecific Low Back Pain with Qijingtiaoqi Manipulation (thesis). Fujian University of Traditional Chinese Medicine, 2016. [Google Scholar]
Zhao 2014 {published data only}
- Zhao H. Clinical observation on therapeutic effect of cupping combined with acupuncture stimulation at trigger points for lumbar myofascial pain syndrome. Acupuncture Research 2014;39(4):324-8. [PubMed] [Google Scholar]
Zhou 2010 {published data only}
- Zhou SM, Zhou XX. Effect of acupuncture for treatment of chronic non-specific low back pain. Journal of Changchun University of Traditional Chinese Medicine 2010;26(1):81-2. [Google Scholar]
Zhu 2016 {published data only}
- Zhu WL, Xu DM, Liu J, Wu WZ. The treatment effect of the combination of electroacupuncture and core-strength exercises for nonspecific low back pain. Chinese Journal of Rehabilitation 2016;31(4):283-5. [Google Scholar]
References to studies awaiting assessment
Han 2018 {published data only}
- Han ZM, Liu Y, Luo YP, Peng XJ, Shen J, Zhan SQ, et al. The comparison of shock wave therapy versus acupuncture for the treatment of chronic nonspecial low back pain. Guide of China Medicine 2018;16(31):169-70. [Google Scholar]
Leite 2018 {published data only}
- Leite PMS, Mendonca ARC, Maciel LYS, Poderoso-Neto ML, Araujo CCA, Gois HCJ, et al. Does electroacupuncture treatment reduce pain and change quantitative sensory testing responses in patients with chronic nonspecific low back pain? A randomized controlled clinical trial. Evidence-Based Complementary and Alternative Medicine 2018;2018:8586746. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tu 2019 {published data only}
- Tu Y, Ortiz A, Gollub RL, Cao J, Gerber J, Lang C, et al. Multivariate resting-state functional connectivity predicts responses to real and sham acupuncture treatment in chronic low back pain. NeuroImage: Clinical 2019;23:1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to ongoing studies
ACTRN12615000534583 {unpublished data only}
- ACTRN12615000534583. For adults with chronic low back pain, does the number of sessions of traditional Chinese Medicine acupuncture in addition to usual care affect back pain and function outcomes? A randomized controlled feasibility study. apps.who.int/trialsearch/Trial2.aspx?TrialID=ACTRN12615000534583 (first received 27 May 2014).
IRCT20150602022539N9 {unpublished data only}
- IRCT20150602022539N9. The effect of electroacupuncture in non specific low back pain patients with gluteus maximus trigger points. apps.who.int/trialsearch/Trial2.aspx?TrialID=IRCT20150602022539N9 (first received 28 March 2019).
IRCT2017090224149N37 {unpublished data only}
- IRCT2017090224149N37. Treatment of chronic low back pain using a method of manual therapy and dry needling. apps.who.int/trialsearch/Trial2.aspx?TrialID=IRCT2017090224149N37 (first received 21 Sep 2017).
NCT02039037 {unpublished data only}
- NCT02039037. Efficacy of acupuncture and electroacupuncture in patients with chronic nonspecific low back pain: randomized clinical trial. clinicaltrials.gov/ct2/show/NCT02039037 (first received 30 October 2013).
NCT02468297 {unpublished data only}
- NCT02468297. Efficacy of the electronic acupuncture shoes: a clinical trial for chronic low back pain. clinicaltrials.gov/ct2/show/NCT02468297 (first received 6 June 2015).
NCT03794869 {unpublished data only}
- NCT03794869. Short-term effects of exercise program versus electropuncture in patients with chronic non-specific low back pain: a randomized clinical trial. clinicaltrials.gov/ct2/show/study/NCT03794869 (first received January 7 2019).
Additional references
Ammendolia 2008
- Ammendolia C, Furlan AD, Imamura M, Irvin E, Tulder M. Evidence-informed management of chronic low back pain with needle acupuncture. Spine Journal: official journal of the North American Spine Society 2008;8(1):160-72. [PMID: ] [DOI] [PubMed] [Google Scholar]
Balague 2012
- Balague F, Mannion AF, Pellise F, Cedraschi C. Non-specific low back pain. Lancet (London, England) 2012;379(9814):482-91. [PMID: ] [DOI] [PubMed] [Google Scholar]
Berman 2010
- Berman BM, Langevin HM, Witt CM, Dubner R. Acupuncture for chronic low back pain. New England Journal of Medicine 2010;363(5):454-61. [PMID: ] [DOI] [PubMed] [Google Scholar]
Chou 2007
- Chou R, Qaseem A, Snow V, Casey D, Cross JT Jr, Shekelle P, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Annals of Internal Medicine 2007;147(7):478-91. [PMID: ] [DOI] [PubMed] [Google Scholar]
Cohen 1988
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd Edition. New Jersey (NJ): Lawrence Erlbaum Associates, 1988. [Google Scholar]
Dhond 2007
- Dhond RP, Kettner N, Napadow V. Neuroimaging acupuncture effects in the human brain. Journal of Alternative and Complementary Medicine (New York, N.Y.) 2007;13(6):603-16. [PMID: ] [DOI] [PubMed] [Google Scholar]
Diaz‐Arribas 2017
- Diaz-Arribas MJ, Fernandez-Serrano M, Royuela A, Kovacs FM, Gallego-Izquierdo T, Ramos-Sanchez M, et al. Minimal Clinically Important Difference in Quality of Life for Patients With Low Back Pain. Spine 2017;42(24):1908-16. [PMID: ] [DOI] [PubMed] [Google Scholar]
Dworkin 2008
- Dworkin RH, Turk DC, Wyrwich KW, Beaton D, Cleeland CS, Farrar JT, et al. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. Journal of Pain: official journal of the American Pain Society 2008;9(2):105-21. [PMID: ] [DOI] [PubMed] [Google Scholar]
Furlan 2012
- Furlan AD, Yazdi F, Tsertsvadze A, Gross A, Van Tulder M, Santaguida L, et al. A systematic review and meta-analysis of efficacy, cost-effectiveness, and safety of selected complementary and alternative medicine for neck and low-back pain. Evidence-Based Complementary and Alternative Medicine 2012;2012:953139. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Furlan 2015
- Furlan AD, Malmivaara A, Chou R, Maher CG, Deyo RA, Schoene M, et al. 2015 Updated Method Guideline for Systematic Reviews in the Cochrane Back and Neck Group. Spine 2015;40(21):1660-73. [PMID: ] [DOI] [PubMed] [Google Scholar]
Goldman 2010
- Goldman N, Chen M, Fujita T, Xu Q, Peng W, Liu W, et al. Adenosine A1 receptors mediate local anti-nociceptive effects of acupuncture. Nature Neuroscience 2010;13(7):883-8. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
GRADEpro GDT 2020
- GRADEpro GDT: GRADEpro Guideline Development Tool [Software]. McMaster University, 2020 (developed by Evidence Prime, Inc.). Available from gradepro.org.
Han 2003
- Han JS. Acupuncture: neuropeptide release produced by electrical stimulation of different frequencies. Trends in Neurosciences 2003;26(1):17-22. [PMID: ] [DOI] [PubMed] [Google Scholar]
Hartvigsen 2018
- Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, et al. What low back pain is and why we need to pay attention. Lancet (London, England) 2018;391(10137):2356-67. [PMID: ] [DOI] [PubMed] [Google Scholar]
Higgins 2019
- Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 6.0 [updated July 2019]. The Cochrane Collaboration, 2019. Available from handbook.cochrane.org.
Hoy 2012
- Hoy D, Bain C, Williams G, March L, Brooks P, Blyth F, et al. A systematic review of the global prevalence of low back pain. Arthritis and Rheumatism 2012;64(6):2028-37. [PMID: ] [DOI] [PubMed] [Google Scholar]
Jadad 1996
- Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Controlled Clinical Trials 1996;17(1):1-12. [PMID: ] [DOI] [PubMed] [Google Scholar]
Kim 2016
- Kim SY, Min S, Lee H, Cheon S, Zhang XY, Park JY, Song TJ, Park HJ. Changes of Local Blood Flow in Response to Acupuncture Stimulation: A Systematic Review. Evidence-Based Complementary and Alternative Medicine 2016;2016:1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lam 2013
- Lam M, Galvin R, Curry P. Effectiveness of acupuncture for nonspecific chronic low back pain: a systematic review and meta-analysis. Spine 2013;38(24):2124-38. [PMID: ] [DOI] [PubMed] [Google Scholar]
Langevin 2002
- Langevin HM, Yandow JA. Relationship of acupuncture points and meridians to connective tissue planes. The Anatomical Record. 2002;269(6):257-65. [PMID: ] [DOI] [PubMed] [Google Scholar]
Lao 1996
- Lao L. Acupuncture techniques and devices. Journal of Alternative and Complementary Medicine (New York, N.Y.) 1996;2(1):23-5. [PMID: ] [DOI] [PubMed] [Google Scholar]
Li 2008
- Li A, Lao L, Wang Y, Xin J, Ren K, Berman BM, et al. Electroacupuncture activates corticotrophin-releasing hormone-containing neurons in the paraventricular nucleus of the hypothalammus to alleviate edema in a rat model of inflammation. BMC Complementary and Alternative Medicine 2008;8:20. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Liu 2015a
- Liu L, Skinner M, McDonough S, Mabire L, Baxter GD. Acupuncture for low back pain: an overview of systematic reviews. Evidence-Based Complementary and Alternative Medicine. 2015;2015:328196. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
MacPherson 2010
- MacPherson H, Altman DG, Hammerschlag R, Youping L, Taixiang W, White A, Moher D. Revised STandards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): Extending the CONSORT Statement. PLoS Med 2010;7(6):e1000261. [DOI] [PMC free article] [PubMed] [Google Scholar]
Manheimer 2005
- Manheimer E, White A, Berman B, Forys K, Ernst E. Meta-analysis: acupuncture for low back pain. Annals of Internal Medicine 2005;142(8):651-63. [PMID: ] [DOI] [PubMed] [Google Scholar]
Melzack 1981
- Melzack R. Myofascial trigger points: relation to acupuncture and mechanisms of pain. Archives of Physical Medicine and Rehabilitation 1981;62(3):114-7. [PMID: ] [PubMed] [Google Scholar]
NICE 2016
- National Institute for Health and Care Excellence. Low back pain and sciatica in over 16s: assessment and management; Nov 2016. Available at www.nice.org.uk/guidance/NG59. [PubMed]
Pomeranz 1996
- Pomeranz B. Scientific research into acupuncture for the relief of pain. Journal of alternative and complementary medicine (New York, N.Y.) 1996;2(1):53-60. [PMID: ] [DOI] [PubMed] [Google Scholar]
Qaseem 2017
- Qaseem A, Wilt TJ, McLean RM, Forciea MA, Clinical Guidelines Committee of the American College of Physicians. Noninvasive treatments for acute, subacute, and chronic low back pain: A clinical practice guideline from the American college of physicians. Annals of Internal Medicine 2017;166(7):514-30. [DOI] [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rubinstein 2010
- Rubinstein Sidney M, van Middelkoop Marienke, Kuijpers Ton, Ostelo Raymond, Verhagen Arianne P, Boer Michiel R, et al. A systematic review on the effectiveness of complementary and alternative medicine for chronic non-specific low-back pain. European Spine Journal 2010;19(8):1213-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ryan 2016
- Ryan R, Hill S (2016). How to GRADE the quality of the evidence (Version 3.0). Cochrane Consumers and Communication Group, 2016. Available at cccrg.cochrane.org/author-resources..
Schulz 2010
- Schulz Kenneth F, Altman Douglas G, Moher David. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. British Medical Journal 2010;23(349):c332. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schünemann 2017a
- Schünemann HJ, Oxman AD, Higgins JP, Vist GE, Glasziou P, Akl E, et al, on behalf of the Cochrane GRADEing Methods Group and the Cochrane Statistical Methods Group. Chapter 11: Completing 'Summary of findings' tables and grading the confidence in or quality of the evidence. In: Higgins JP, Churchill R, Chandler J, Cumpston MS, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.2.0 (updated June 2017). The Cochrane Collaboration, 2017. Available from www.training.cochrane.org/handbook. [Google Scholar]
Schünemann 2017b
- Schünemann HJ, Oxman AD, Vist GE, Higgins JP, Deeks JJ, Glasziou P, et al, on behalf of the Cochrane GRADEing Methods Group and the Cochrane Statistical Methods Group. Chapter 12: Interpreting results and drawing conclusions. In: Higgins JP, Churchill R, Chandler J, Cumpston MS, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.2.0 (updated June 2017). The Cochrane Collaboration, 2017. Available from www.training.cochrane.org/handbook. [Google Scholar]
Van Tulder 2003
- Van Tulder M, Furlan A, Bombardier C, Bouter L. Updated method guidelines for systematic reviews in the cochrane collaboration back review group. Spine 2003;28(12):1290-1299. [PMID: ] [DOI] [PubMed] [Google Scholar]
Xu 2013
- Xu M, Yan S, Yin X, Li X, Gao S, Han R, et al. Acupuncture for chronic low back pain in long-term follow-up: a meta-analysis of 13 randomised controlled trials. The American journal of Chinese medicine 2013;41(1):1-19. [PMID: ] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Furlan 2005
- Furlan AD, Van Tulder MW, Cherkin DC, Tsukayama H, Lao L, Koes BW, et al. Acupuncture and dry-needling for low back pain. The Cochrane database of systematic reviews 2005;25(1):CD001351. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]


