Abstract
Aim
This study aimed to evaluate the patients' satisfaction with using store-and-forward voice and text messaging teleconsultation service to provide primary health care to patients during the COVID-19 pandemic.
Method
A cross-sectional survey was conducted between October 1 and December 1, 2020, in Iran. The study population consisted of patients who used the service. Three hundred-ninety-six patients were enrolled in the study by convenience sampling. Data were collected by a researcher-made questionnaire. The face, comprehensibility, and content validity of the questionnaire were tested and met. The reliability of this questionnaire was confirmed (r = 0.9). Descriptive statistics and multinomial logistic regression were conducted. Data were analyzed using STATA 14.0 software.
Results
In total, 396 patients responded to the online questionnaire. The mean age of patients was 37 ± 10.31 years. More than half of them had an academic degree (65.40 %). Teleconsultation was considered satisfactory by 172 patients (43.43 %), while more than half of the patients (56.57 %) were unsatisfied with teleconsultation. In terms of "quality of care provided" and "patient information privacy" components, around 41 % of patients were satisfied. However, the number of patients who feel satisfied with teleconsultation's similarity to a face-to-face encounter was lower (37.88 %). The results showed no significant relationship between age, gender, education, and overall satisfaction (p > 0.05). The association between overall satisfaction and health status was (AOR = 1.51, 95 % CI = 1.16–1.96).
Conclusion
More than half of patients from our study did not have a good experience with teleconsultation. This is also partially due to the use of existing communication platform, instead of custom-made solution. It is necessary to improve the services' quality and meet patients' needs to optimize patients' experience, particularly during a health crisis, resulting in better health outcomes and end-user satisfaction.
Keywords: Teleconsultation, Satisfaction, Telemedicine, Telehealth, COVID-19 pandemic
1. Introduction
On March 11, 2020, the World Health Organization declared Coronavirus Disease 2019 (COVID-19) as a pandemic [1]. COVID-19 has been spread to 220 countries and affected 85,027,813 patients worldwide by January 1, 2021 [2]. On February 19, 2020, Iran reported its first confirmed cases of infections in Qom. The disease spread rapidly in all 31 provinces of the country. To date (January 28, 2020), the total number of positive infected people has reached 1,405,414 with 57,807deaths [3].
The COVID-19 pandemic has resulted in many countries' complete lockout due to the virus's infectious nature and the lack of adequate care. Iran has concentrated on social distancing, rather than mandatory quarantine, since the early days of the COVID-19 epidemic to delay this virus's spread. Social distancing measurements, including closing public places such as schools and universities [4], canceling sports events, canceling or delaying face to face services, even some healthcare services [5]. Given that the entire healthcare system has been massively impacted to accommodate COVID-19 patients, there have been temporary delays in the access and delivery of regular and non-emergency medical services during the COVID-19 pandemic [6]. In other words, COVID-19 has resulted in disruptions in the provision of essential healthcare services across the world, including those provided at the primary health care (PHC) level. Delay or avoidance of PHC may increase the risk of morbidity and mortality associated with treatable and preventable health conditions. It may lead to recorded excess deaths linked directly or indirectly to COVID-19 [7].
A big concern that emerges is "How are we going to catch up with all the consultations canceled or delayed?" In this context, many healthcare organizations have urgently set up teleconsultation facilities to provide PHC for patients.
Teleconsultation can be defined as remote consultation or telehealth, which refers to interactions between a clinician and a patient to provide diagnostic or therapeutic advice through electronic means [7]. Teleconsultation can provide telecare, provide remote assistance, and assist with patient administrative supervision, triage, follow-up, meetings, and professional discussions among physicians in different locations [8]. It provides opportunities to enhance communication between patients and their healthcare teams [9]. Teleconsultation can use different platforms including, telephone, videoconference, chatbots, and text messaging [10,11]. Teleconsultation has evolved to deliver medical care while respecting social distance and reducing the virus's transmission within patients/physicians.
Several types of research on teleconsultation have been published. The findings of these studies have confirmed the use of teleconsultation as an accessible alternative solution. For example, in a systematic review study by Aashaka, the result showed that telemedicine approaches produced better outcomes than to control groups in symptom management, quality of life, satisfaction, medication adherence, visit completion rates, and disease progression [12]. The Sherif study also showed that text messaging and mobile phone apps are feasible and acceptable in improving preventive behavior [13,14]. Moreover, in pediatric and adult patients with sickle cell disease, eHealth interventions can improve various self-management outcomes [15]. Children, adolescents, and young adults undergoing cancer care may benefit from eHealth and mHealth to improve their mental and physical [16].
Some factors lead to teleconsultation effectiveness and efficiency, including improved outcomes, user-friendliness, low cost, and decreased travel time [17,18].
Teleconsultation, as a new tool, has rarely been tested for patients during a global pandemic. While some studies have been conducted on teleconsultation during the COVID-19 pandemic [[19], [20], [21], [22]], there has been limited research regarding patient satisfaction [23,24]. To address this gap, this study aims to examine the satisfaction of patients with teleconsultation during the COVID-19 pandemic.
2. Materials and methods
2.1. Study design
This cross-sectional descriptive study was carried out from September 2020 to January 2021 in Kerman, Iran. The primary outcome was patient satisfaction with teleconsultation using the validated questionnaire.
2.2. Study setting
Kerman University of Medical Sciences (KUMS) is one of the medical universities located in Kerman province, in southeastern Iran. KUMS started implementing the store-and-forward voice and text messaging teleconsultation service on March 14, about four weeks after the first patient with COVID-19 was diagnosed in Iran.
Individual clinics and outpatient departments in some Iranian provinces and cities were forced to close during the disease prevention and control period. Due to the difficulties of obtaining medical attention, treatment can be delayed, causing the disease to worsen. Certain illnesses, such as stroke, cancer, and respiratory illness, can be fatal if not treated promptly. Also, patients' psychological states may be affected by physical pain and epidemic fear, contributing to anxiety and frustration [25,26]. To meet patients' needs, using alternative methods to provide PHC services can be useful. These methods range from the Internet to social media and mobile apps. According to reports, there were 58.42 million Internet users and 33.40 million social media users in Iran in January 2020. So, it seems that using these platforms can be helpful during the pandemic.
Although it is critical to measure patients' need and input in the development of digital health interventions to maintain long-term and short-term commitment [[27], [28], [29]], KUMS decided to use free available social media to meet these challenges due to limited time and resources to design and implement teleconsultation service using other platforms. After reviewing different social media platforms and features, KUMS decided to provide teleconsultation using a popular instant messaging software called Telegram. Telegram is a freeware, cross-platform, cloud-based instant messaging (IM) software and application service. To implement teleconsultation through Telegram App, eight staffs at KUMS create a Telegram group and manage it. This Telegram group has some functionality such as sending text and voice messages, pinching a message, and restricting sending messages. Also, KUMS created a new Telegram bot that was linked to the Telegram group. The Telegram bot transmitted messages between the healthcare providers and the patients using the Telegram user ID to link the healthcare providers' answers to patients' questions.
During 9 PM and 11 PM, patients can ask their questions by sending a text message in the Telegram group. Then, the Telegram bot sends the patient message to a healthcare provider. Following that, the healthcare provider answers the question. After that, the Telegram bot sends back the healthcare provider’s answer to the Telegram group (reply on the patient message).
Teleconsultation was held every night for two consecutive hours. First, between 9 PM and 10 PM, healthcare providers answered patients' questions about COVID-19 disease. Then, patients with other diseases who need help regarding monitoring their disease or taking their medicine can ask their questions between 10 PM and 11 PM. This group of patients used teleconsultation for follow-up or further advice. Until today, teleconsultation had been held for 11 months (about 308 nights). Currently, about 91 healthcare providers are actively providing teleconsultation to the patients. Teleconsultation service was free of charge.
2.3. Sampling method and sample size
Convenience sampling was used in this study. A sample of 384 patients were selected using Cochran’s sample size formula (z = 1.96, p = 0.5, q = 0.5, d = 0.05). The sample size was increased to 400 patients to reduce sampling error.
2.4. Data collection tool (modified questionnaire, validity and reliability)
A researcher-constructed questionnaire based on a prior standard and validated questionnaire for teleconsultation named Teleconsultation Satisfaction Questionnaire (TSQ) and other items extracted from the literature was developed [[30], [31], [32]]. Overall, eighteen items were extracted from these sources. These items were read and discussed frequently among a panel consist of seven experts. These experts had one of two criteria: 1) having a research background in telemedicine or medical informatics, and 2) has experience as a manager of a teleconsultation system. This final questionnaire included satisfaction and demographic information questions. There were eight main questions about satisfaction with the teleconsultation and demographic questions (age, gender, education level and self-reported health status). Single-item self-reported health status was defined on a 5-point Likert scale (1=very bad, 2= bad, 3=moderate, and 4= good, 5=very good). The satisfaction items were categorized into three components adapted from the TSQ, including quality of care provided (n = 3 items), similarity to a face-to-face encounter (n = 3 items), and patient information privacy (n = 2 items).
For determining the necessity and relevance of the items, we used the content validity ratio (CVR) and content validity index (CVI). The results for CVI and CVR of final questionnaire are 0.98 and 1, respectively. Then, the questionnaire was pilot tested on 40 people who were not included in the study. No changes were needed due to piloting. The questionnaire's reliability assessment results showed good internal consistency with an acceptable Cronbach's alpha coefficient of 0.90.
2.5. Data collection
The self-administered questionnaire was designed on a platform of an online Internet-based survey. Several studies have shown that Internet-based surveys are effective enough for health surveys, especially satisfaction [33,34]. All the Telegram group members were included as the research population. The message consists of a brief description of the research and questionnaire's link. This message was sent daily after holding the online teleconsultation at 11:00 PM in the Telegram group. In order to increase the response rate, two reminders were sent daily. Data collection continued until the sample size was reached.
2.6. Data analysis
The demographic variables and single-item self-reported health status was described using descriptive statistics (i.e., mean, absolute, and relative frequency). A total questionnaire score > 32 was considered as a cut-off-point for the analysis so that the satisfaction scores higher than thirty-two were considered as desired satisfaction. The cut-off for a patient's desired satisfaction for the quality of care provided and similarity to a face-to-face encounter was considered > 12 because each of these two components consists of three items. In contrast, the cut-off for patient information privacy was considered > 8 as a desired satisfaction of patient who uses the system. The results of satisfied or unsatisfied were reported for each item and component of the questionnaire. For investigating the association between the demographic, single-item self-reported health status with the satisfied or unsatisfied of patients, the univariate and multivariate regression model was used. The goodness of fit of the models was assessed using the Hosmer-Lemeshow test. 2-tailed P < 0.05 or OR with 95 % CI, not including 1.0, were considered statistically significant. All data processes were conducted using STATA 14.0 software (STATA Corp, College Station, TX, USA)
2.7. Ethical considerations
The Ethics Committee of Kerman University of Medical Sciences (KUMS) approved this study (Code of Ethics: IR.KMU.REC.1399.599). The participants also participated with informed consent in the study and were assured about the confidentiality of their information.
3. Results
3.1. Patient demographics
In total, 396 patients (131 men and 265 women) responded to the online questionnaire. The response rate of patients was 50 %. The mean age of patients was 37.76 ± 10.31 years (Age range: 14-69). More than half of the patients (62.12 %) were aged 31–50. More than half of them had an academic degree (65.40 %), and about a quarter of them had a diploma degree. Of the participants, 260 (65.66 %) believed that their health status is good, and 30.56 % and 3.79 % reported their health status moderate and bad, respectively. The results obtained for the demographic data are listed in Table 1 .
Table 1.
Demographic characteristics of the respondents
| Characteristic | Total number of respondents (n = 396) |
|---|---|
| Age | Mean ± SD |
| 37.76 ± 10.31 | |
| Gender | N (%) |
| Female | 265 (66.92) |
| Male | 131 (33.08) |
| Education level | |
| Under diploma | 33 (8.33) |
| Diploma | 104 (26.26) |
| Academic | 259 (65.40) |
| Health status | |
| Bad | 15 (3.79) |
| Moderate | 121 (30.56) |
| Good | 260 (65.66) |
3.2. Satisfaction with teleconsultation
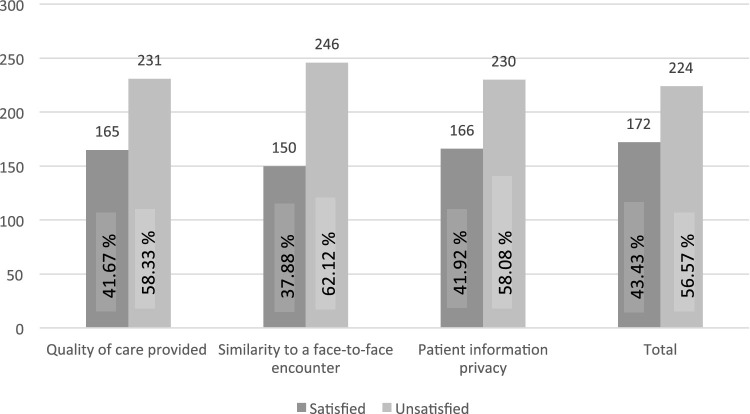
Fig. 1 shows the patients' satisfaction with the teleconsultation method. Teleconsultation was considered satisfactory for 172 patients (43.43 %), while more than half of the patients (56.57 %) were unsatisfied with teleconsultation. In all three components, the number of patients satisfied with the teleconsultation was lower than those who were unsatisfied. Regarding "quality of care provided" and "patient information privacy" components, about 41 % of patients were satisfied. However, the number of patients who feel satisfied with similarity to a face-to-face encounter was lower, with 37.88 %.
Fig. 1.
Satisfaction with teleconsultat.
Based on respondents to three components items, patients agreed that they could easily talk to their healthcare provider and received adequate attention during teleconsultation, with 71.72 % and 74.24 %, in turn. Meanwhile, about 87 % of patients believed that teleconsultation provides their healthcare needs. The agreement rate about "I see my healthcare provider as if we met in person" was lower with 59.34 %.
Independent factors (patients' age, gender, education, and health status) associated with satisfaction are shown in Table 2 . After adjustment for other covariates in the multivariable logistic regression model, satisfaction remained significantly associated with health status in all three components as follows: quality of care provided (AOR = 1.38, 95 % CI = 1.07–1.79), similarity to a face-to-face encounter (AOR = 1.49, 95 % CI = 1.14–1.95), and patient information privacy (AOR = 1.58, 95 % CI = 1.21–2.05). The association between overall satisfaction and health status was (AOR = 1.51, 95 % CI = 1.16–1.96). The results also showed no significant relationship between age, gender, education, and overall satisfaction scores (p > 0.05).
Table 2.
The variables associated with the participants' satisfaction using teleconsultation service.
| Variables | Quality of care provided |
Similarity to a face-to-face encounter |
Patient information privacy |
Total |
||||
|---|---|---|---|---|---|---|---|---|
| OR crud (95 % CI) | OR adjusted (95 % CI) | OR crude (95 % CI) | OR adjusted (95 % CI) | OR crude (95 % CI) | OR adjusted (95 % CI) | OR crude (95 % CI) | OR adjusted (95 % CI) | |
| Age | 1.00 (0.98, 1.02) | 1.00 (0.98, 1.02) | 1.02 (0.99, 1.04) | 1.02 (0.99, 1.04) | 1.00 (0.98, 1.02) | 1.00 (0.98, 1.03) | 1.01 (0.99, 1.03) | 1.01 (0.99, 1.03) |
| Gender | ||||||||
| Female | Ref. | Rff. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Male | 1.28 (0.84, 1.97) | 1.13 (0.73, 1.76) | 1.23 (0.80, 1.90) | 1.06 (0.68, 1.66) | 1.27 (0.83, 1.93) | 1.10 (0.71, 1.70) | 1.10 (0.72, 1.68) | 0.94 (0.61, 1.46) |
| Educationlevel | ||||||||
| Under Diploma | Ref. | Rff. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Diploma | 1.15 (0.52, 2.51) | 1.26 (0.57, 2.79) | 0.99 (0.45, 2.17) | 1.08 (0.48, 2.40) | 0.56 (0.26, 1.24) | 0.62 (0.28, 1.40) | 1.10 (0.50, 2.42) | 1.23 (0.55, 2.73) |
| Academic | 0.62 (0.30, 1.27) | 0.64 (0.31, 1.34) | 0.62 (0.30, 1.28) | 0.66 (0.31, 1.38) | 0.49 (0.23, 0.99) | 0.50 (0.24, 1.06) | 0.70 (0.34, 1.45) | 0.75 (0.36, 1.57) |
| Health status | 1.36 (1.06, 1.75)* | 1.38 (1.07, 1.79)* | 1.46 (1.12, 1.89)** | 1.49 (1.14, 1.95)** | 1.59 (1.23, 2.06)*** | 1.58 (1.21, 2.05)** | 1.46 (1.13, 1.88)** | 1.51 (1.16, 1.96)* |
P-value < 0.05
P-value <0.01
P-value < 0.001
4. Discussion
Our finding showed that less than half of the respondents were satisfied with teleconsultation. They believed that teleconsultation provides appropriate quality, reliable method, and trustworthy teleconsultation services. However, they did not feel teleconsultation is similar to a face-to-face encounter. Most of the patients did not worry about disclosing information related to their health problems.
Other studies have examined the satisfaction of individuals with teleconsultation during the COVID-19 pandemic. Many of these studies were conducted in developed countries [24,[35], [36], [37], [38], [39], [40], [41], [42]]. To the best of our knowledge, there is just one study in Saudi Arabia [43] and one study in India [44], which may have a similar research setting as Iran. In a study by Magadmi [45], the satisfaction of participants who used teleconsultation services was investigated. They were the least satisfied with sharing private or personal information. While in our study, participants did not feel worried about their information privacy and can trust teleconsultation. This difference may relate to the fact that patient information confidentiality was an essential issue for us that received special attention from the beginning of the teleconsultation service. To do so, we restricted patients to share their lab test images.
The present study found that most patients believed that they could easily talk to their healthcare provider and understand their condition and healthcare need. The same as our findings, the study of Magadmi's study [43] showed that participants agreed on their ability to explain their medical problems to the doctor, and then the doctor could provide an appropriate health care management plan via teleconsultation.
Many studies in developed countries assessed patient satisfaction with telemedicine services during the COVID-19 pandemic. For example, in the Pinar study [24], patient and physician satisfaction with teleconsultation in urology was investigated in Paris, France. Most of the patients and physicians had a good experience, and teleconsultation satisfaction level was high and was consistent with previous studies[18,46]. Also, satisfaction surveys in the Ramaswamy study [41] showed that patient satisfaction with telemedicine (video visits) was high, and video visits were considered a viable alternative to traditional in-person visits. Another study [42] investigated the satisfaction of participants in Australia regarding telehealth during the COVID-19 pandemic. It showed that participants believed their Telehealth experience was "just as good as" or "better than" their traditional in-person medical care experience, which was consistent with another survey in Australia [47]. Dobrusin’s study [36] also concluded that patients were incredibly satisfied with their telehealth appointments, with more than 80 % suggesting that they could engage in potential telehealth visits and the provider is able to answer their questions. In AmbrosIti's study [35], patients with genitourinary cancer who had weekly video-conference meetings through Zoom with healthcare professionals showed that most patients had a high level of satisfaction with their telehealth visits. In Gilbert's study [37], in the United Kingdom, virtual consultations (via telephone or video call) were described as a possible alternative to face-to-face consultations during the COVID-19 pandemic. In this study, satisfaction scores were high for phone and virtual consultations.
In a study done by Li [48] regarding vascular patients' satisfaction of using virtual telemedicine communications to provide remote healthcare, it was concluded that the overall experience of the video consultation, all of the patients were ”satisfied” or ”highly satisfied” with the video calls. In this study, video calls were performed between patients and vascular surgeons using WeChat tools. Whereas, in our study, patients experienced higher levels of unsatisfaction with teleconsultation service. Poorer infrastructure and lower Internet connections in Iran may be the explanation for this difference [32]. It seems that high-speed Internet access is the most critical factor in developing telemedicine services [49]. The second reason for this difference could be that teleconsultation was implemented using Telegram group. The Iranian government banned the Telegram on May 1, 2018, following street protests. After that, if people try to access Telegram, their only alternative is to log in via a Virtual Private Network (VPN), leading to a challenging connection. So, it seems that Telegram did not meet two important conditions for teleconsultation's sustainability [50]: high-quality service and better care access.
On the other hand, the economic evaluation of digital health interventions is limited [51,52]. Economic evaluation is required in addition to efficacy and effectiveness evidence. The impact of digital health interventions on healthcare expenses could be more significant than the direct cost benefits associated with drug adherence and related health outcomes. Therefore, to encourage the implementation of digital health interventions, studies are needed to prove their cost-effectiveness.
In our study, there was no significant relationship between participants' demographics and overall satisfaction. In agreement with our study, the study results by Wang [40] showed that 85 % of mean overall satisfaction for teleconsultation with no differences regarding age and gender.
This study had four limitations. First, the KUMS did not have the proper infrastructure to implement the teleconsultation service before the COVID-19 outbreak started. Due to the high prevalence of the disease, the fastest possible way to provide this service was to use free and available messaging applications such as Telegram, the most popular messaging application in Iran. It is recommended that countries establish long-term strategic plans to develop and implement eHealth services such as teleconsultation. Second, some fake Telegram users in the Telegram group caused losing the number of people using the teleconsultation service. To address this limitation, we recommend that future studies use the Telegram bot to identify and remove fake users. Third, patients in our study can send voice and text messages to the Telegram group. They could not send photos such as a lab test images or MRI scan or CT scan images. In some cases, this limitation made it difficult to make a decision by clinicians. Finally, the generalization of results to the whole population must be cautious
5. Conclusions
This study was the first time that teleconsultation was used to provide PHC in KUMS as a medical university in developing countries. Teleconsultation is a suitable method to provide primary health care to avoid unnecessary clinic visits or hospitalizations, which result in the prevention and control of infectious diseases such as COVID-19. Although teleconsultation is unlikely to replace face-to-face appointments completely, it is a reliable way to access PHC. This study's findings can provide health policymakers and managers with valuable insight into teleconsultation services. In this regard, it is recommended that medical university managers assess the universities' readiness in terms of the required technological infrastructure and implement a viable teleconsultation service before health crises such as COVID-19 when providing healthcare is challenging. Healthcare policymakers also need to invest in the Internet bandwidth and upgrading telecommunications equipment to improve communication lines' speed to benefit from teleconsultation service. While digital intervention is rapidly evolving, there are still several open questions and information gaps that should be investigated further. Future research should concentrate on enhancing digital health intervention delivery, access to healthcare, digital health interventions solution consistency, and integrating digital health interventions into in-person physician visits. Future research should focus on the cost-effectiveness of digital health interventions, the utilization of these interventions in remote areas, and the challenges to technology adoption to fully understand the true potential of digital health approaches for improving the health outcomes of people.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
All authors had substantial contributions to the research and written of the manuscript. NJ and VYF were responsible for the overall design of this study. NJ addressed ethical considerations. NJ and VYF collected data. NJ and VYF planned statistical analysis. NJ and VYF wrote the first draft manuscript. NJ, NN, VYF, and DT contributed to writing the final versions of the manuscript.
Declaration of Competing Interest
The authors report no declarations of interest.
Acknowledgment
The authors would like to thank Prof. Kambiz Bahaadinbeigy and Mr. Mohamad Samari and for helpful feedback and all Patients who participated in this study.
References
- 1.Organization WH . 2020. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19-11 March 2020. [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC). Coronavirus Disease . 2019. (COVID-19). Situation Summary.https://www.cdc.gov/coronavirus/2019-nCoV/%0Asummary.html [Internet]. [cited 2020 January 3]. Available from: [Google Scholar]
- 3.(MHME) M of H and ME The Most Recent Definitive Statistics of COVID-19 MHME2020. https://behdasht.gov.ir [Internet] Available from:
- 4.Serlachius A., Badawy S.M., Thabrew H. Psychosocial challenges and opportunities for youth with chronic health conditions during the COVID-19 pandemic. JMIR Pediatr Parent. 2020;3(October (2)):e23057. doi: 10.2196/23057. https://pubmed.ncbi.nlm.nih.gov/33001834 [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abdi M. Coronavirus disease 2019 (COVID-19) outbreak in Iran: actions and problems. Infect. Control Hosp. Epidemiol. 2020;41(June (6)):754–755. doi: 10.1017/ice.2020.86. https://pubmed.ncbi.nlm.nih.gov/32192541 [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Santoli J.M., Lindley M.C., DeSilva M.B., et al. Effects of the COVID-19 pandemic on routine pediatric vaccine ordering and administration — united States, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020;69:591–593. doi: 10.15585/mmwr.mm6919e2. [DOI] [PubMed] [Google Scholar]
- 7.CDC NC for HS . US Department of Health and Human Services, CDC, National Center for Health Statistics; Atlanta, GA: 2020. Excess Deaths Associated With COVID-19.https://www.cdc.gov/nchs/nvss/vsrr/covid19/excess_deaths.htm [Internet] Available from: [Google Scholar]
- 8.Nerlich Michael. 1st edition. IOS Press; US: 2003. Integration of Health Telematics Into Medical Practice. 159 pages. [Google Scholar]
- 9.Badawy S.M., Radovic A. Digital approaches to remote pediatric health care delivery during the COVID-19 pandemic: existing evidence and a call for further research. JMIR Pediatr Parent. 2020;3(June (1)):e20049. doi: 10.2196/20049. https://pubmed.ncbi.nlm.nih.gov/32540841 [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Organization PAH . 2021. Teleconsultations During a Pandemic. [Internet] Available from: https://www.paho.org/ish/images/docs/covid-19-teleconsultations-en.pdf?ua=1#:∼:text=Whatisteleconsultation%3F,therapeuticadvicethroughelectronicmeans. [Google Scholar]
- 11.Wootton R., Craig J.J., Patterson V. 2nd ed. Royal Society of Medicine Press; London: 2006. Introduction to Telemedicine. [Google Scholar]
- 12.Shah A.C., Badawy S.M. Telemedicine in pediatrics: systematic review of randomized controlled trials. JMIR Pediatr Parent. 2021;4(February (1)) doi: 10.2196/22696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Badawy S.M., Barrera L., Sinno M.G., Kaviany S., O’Dwyer L.C., Kuhns L.M. Text messaging and mobile phone apps as interventions to improve adherence in adolescents with chronic health conditions: a systematic review. JMIR mHealth uHealth. 2017;5(May (5)):e66. doi: 10.2196/mhealth.7798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Badawy S.M., Kuhns L.M. Texting and mobile phone app interventions for improving adherence to preventive behavior in adolescents: a systematic review. JMIR mHealth uHealth. 2017;5(April (4)):e50. doi: 10.2196/mhealth.6837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Badawy S.M., Cronin R.M., Hankins J., Crosby L., DeBaun M., Thompson A.A., et al. Patient-centered eHealth interventions for children, adolescents, and adults with sickle cell disease: systematic review. J. Med. Internet Res. 2018;20(7) doi: 10.2196/10940. 2018/07/22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ramsey W.A., Heidelberg R.E., Gilbert A.M., Heneghan M.B., Badawy S.M., Alberts N.M. eHealth and mHealth interventions in pediatric cancer: a systematic review of interventions across the cancer continuum. Psychooncology. 2020;29(January (1)):17–37. doi: 10.1002/pon.5280. [DOI] [PubMed] [Google Scholar]
- 17.de la Torre-Díez I., López-Coronado M., Vaca C., Aguado J.S., de Castro C. Cost-utility and cost-effectiveness studies of telemedicine, electronic, and mobile health systems in the literature: a systematic review. Telemed. J. e-Health. 2015;21(2):81–85. doi: 10.1089/tmj.2014.0053. 2014/12/05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kruse Cs, Krowski N., Rodriguez B., Tran L., Vela J., Brooks M. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. 2017;7(8) doi: 10.1136/bmjopen-2017-016242. 2017/08/05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vidal-Alaball J., Acosta-Roja R., Pastor Hernández N., Sanchez Luque U., Morrison D., Narejos Pérez S., et al. Telemedicine in the face of the COVID-19 pandemic. Aten. Primaria. 2020;52(6):418–422. doi: 10.1016/j.aprim.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu S., Yang L., Zhang C., Xiang Y.-T., Liu Z., Hu S., et al. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e17–8. doi: 10.1016/S2215-0366(20)30077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Latifi R., Doarn C.R. Perspective on COVID-19: finally, telemedicine at center stage. Telemed. J. e-Health. 2020;26(September (9)):1106–1109. doi: 10.1089/tmj.2020.0132. [DOI] [PubMed] [Google Scholar]
- 22.North S. Telemedicine in the time of COVID and beyond. J. Adolesc. Health. 2020;67(August (2)):145–146. doi: 10.1016/j.jadohealth.2020.05.024. https://pubmed.ncbi.nlm.nih.gov/32605827 [Internet]. 2020/06/27. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Layfield E., Triantafillou V., Prasad A., Deng J., Shanti Rm, Newman Jg, et al. Telemedicine for head and neck ambulatory visits during COVID-19: evaluating usability and patient satisfaction. Head Neck. 2020;42(July (7)):1681–1689. doi: 10.1002/hed.26285. [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pinar U., Anract J., Perrot O., Tabourin T., Chartier-Kastler E., Parra J., et al. Preliminary assessment of patient and physician satisfaction with the use of teleconsultation in urology during the COVID-19 pandemic. World J. Urol. 2020;(September (9)):1–6. doi: 10.1007/s00345-020-03432-4. https://pubmed.ncbi.nlm.nih.gov/32909174 [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xiang Y.-T., Yang Y., Li W., Zhang L., Zhang Q., Cheung T., et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7(Mar (3)):228–229. doi: 10.1016/S2215-0366(20)30046-8. https://pubmed.ncbi.nlm.nih.gov/32032543 [Internet] 2020/02/04. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kavanagh M.M., Erondu N.A., Tomori O., Dzau V.J., Okiro E.A., Maleche A., et al. Access to lifesaving medical resources for African countries: COVID-19 testing and response, ethics, and politics. Lancet (London, England) 2020;395(May (10238)):1735–1738. doi: 10.1016/S0140-6736(20)31093-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Perski O., Blandford A., West R., Michie S. Conceptualising engagement with digital behaviour change interventions: a systematic review using principles from critical interpretive synthesis. Transl. Behav. Med. 2017;7(2):254–267. doi: 10.1007/s13142-016-0453-1. 2016/12/15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Badawy S.M., Thompson A.A., Liem R.I. Technology access and smartphone app preferences for medication adherence in adolescents and young adults with sickle cell disease. Pediatr. Blood Cancer. 2016;63(5):848–852. doi: 10.1002/pbc.25905. https://www.scopus.com/inward/record.uri?eid=2-s2.0-84961214041&doi=10.1002%2Fpbc.25905&partnerID=40&md5=a992b1d36b1e70dc28136f6e121f7081 [Internet] Available from: [DOI] [PubMed] [Google Scholar]
- 29.Badawy S.M., Thompson A.A., Kuhns L.M. Medication adherence and technology-based interventions for adolescents with chronic health conditions: a few key considerations. JMIR mHealth uHealth. 2017;5(December (12)):e202. doi: 10.2196/mhealth.8310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yip Mp, Chang Am, Chan J., MacKenzie A.E. Development of the Telemedicine Satisfaction Questionnaire to evaluate patient satisfaction with telemedicine: a preliminary study. J. Telemed. Telecare. 2003;9(1):46–50. doi: 10.1258/135763303321159693. [DOI] [PubMed] [Google Scholar]
- 31.Allemann Iseli M., Kunz R., Blozik E. Instruments to assess patient satisfaction after teleconsultation and triage: a systematic review. Patient Prefer. Adherence. 2014;8(June (24)):893–907. doi: 10.2147/PPA.S56160. https://pubmed.ncbi.nlm.nih.gov/25028538 [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Eslami Jahromi M., Ahmadian L. Evaluating satisfaction of patients with stutter regarding the tele-speech therapy method and infrastructure. Int. J. Med. Inform. 2018;115(July):128–133. doi: 10.1016/j.ijmedinf.2018.03.004. [DOI] [PubMed] [Google Scholar]
- 33.Wyatt J.C. When to use web-based surveys. J. Am. Med. Inform. Assoc. 2000;7(4):426–429. doi: 10.1136/jamia.2000.0070426. https://pubmed.ncbi.nlm.nih.gov/10887170 [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.van Gelder M.M.H.J., Bretveld R.W., Roeleveld N. Web-based questionnaires: the future in epidemiology? Am. J. Epidemiol. 2010;172(Dec (11)):1292–1298. doi: 10.1093/aje/kwq291. [Internet] Available from: [DOI] [PubMed] [Google Scholar]
- 35.Ambrosini F., Di Stasio A., Mantica G., Cavallone B., Serao A. COVID-19 pandemic and uro-oncology follow-up: a “virtual” multidisciplinary team strategy and patients’ satisfaction assessment. Arch. Ital. Urol. Androl. 2020;92(June (2)) doi: 10.4081/aiua.2020.2.78. [DOI] [PubMed] [Google Scholar]
- 36.Dobrusin A., Hawa F., Gladshteyn M., Corsello P., Harlen K., Walsh C.X., et al. Gastroenterologists and patients report high satisfaction rates with telehealth services during the novel coronavirus 2019 pandemic. Clin. Gastroenterol. Hepatol. 2020;18(October (11)):2393–2397.e2. doi: 10.1016/j.cgh.2020.07.014. https://pubmed.ncbi.nlm.nih.gov/32663521 [Internet] 2020/07/11. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gilbert A.W., Billany J.C.T., Adam R., Martin L., Tobin R., Bagdai S., et al. Rapid implementation of virtual clinics due to COVID-19: report and early evaluation of a quality improvement initiative. BMJ Open Qual. 2020;9(2) doi: 10.1136/bmjoq-2020-000985. https://bmjopenquality.bmj.com/content/9/2/e000985 [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Holcomb D., Faucher Ma, Bouzid J., Quint-Bouzid M., Nelson Db, Duryea E. Patient perspectives on audio-only virtual prenatal visits amidst the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic. Obstet. Gynecol. 2020;136(August (2)):317–322. doi: 10.1097/AOG.0000000000004026. [DOI] [PubMed] [Google Scholar]
- 39.Holtz B.E. Patients perceptions of telemedicine visits before and after the coronavirus disease 2019 pandemic. Telemed. J. e-Health. 2021;27(January (1)):107–112. doi: 10.1089/tmj.2020.0168. [DOI] [PubMed] [Google Scholar]
- 40.Wang Y.-C., Ganzorig B., Wu C.-C., Iqbal U., Khan H.-A.-A., Hsieh W.-S., et al. Patient satisfaction with dermatology teleconsultation by using MedX. Comput. Methods Programs Biomed. 2018;167(December):37–42. doi: 10.1016/j.cmpb.2018.10.015. [DOI] [PubMed] [Google Scholar]
- 41.Ramaswamy A., Yu M., Drangsholt S., Ng E., Culligan Pj, Schlegel Pn, et al. Patient satisfaction with telemedicine during the COVID-19 pandemic: retrospective cohort study. J. Med. Internet Res. 2020;22(9):e20786. doi: 10.2196/20786. http://www.jmir.org/2020/9/e20786/ [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Isautier J.M.J., Copp T., Ayre J., Cvejic E., Meyerowitz-Katz G., Batcup C., et al. People’s experiences and satisfaction with telehealth during the COVID-19 pandemic in Australia: cross-sectional survey study. J. Med. Internet Res. 2020;22(12):e24531. doi: 10.2196/24531. http://www.jmir.org/2020/12/e24531/ [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Magadmi M., Kamel F., Magadmi R. Research Square; 2020. Patients’ Perceptions and Satisfaction Regarding Teleconsultations During the COVID-19 Pandemic in Jeddah, Saudi Arabia. [Google Scholar]
- 44.Shenoy P., Ahmed S., Paul A., Skaria Tg, Joby J., Alias B. Switching to teleconsultation for rheumatology in the wake of the COVID-19 pandemic: feasibility and patient response in India. Clin. Rheumatol. 2020;39(Sep (9)):2757–2762. doi: 10.1007/s10067-020-05200-6. https://pubmed.ncbi.nlm.nih.gov/32474883 [Internet] 2020/05/30. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Magadmi M., Kamel F., Magadmi R. Research Square; 2020. Patients’ Perceptions and Satisfaction Regarding Teleconsultations During the COVID-19 Pandemic in Jeddah, Saudi Arabia.https://europepmc.org/article/PPR/PPR206839 [Internet] Available from: [Google Scholar]
- 46.Georgsson M., Staggers N. Quantifying usability: an evaluation of a diabetes mHealth system on effectiveness, efficiency, and satisfaction metrics with associated user characteristics. J. Am. Med. Inform. Assoc. 2016;23(January (1)):5–11. doi: 10.1093/jamia/ocv099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ageing GC for M . 2020. Telehealth- Here To Stay? [Internet] Available from: https://static1.squarespace.com/static/5ae17ed32971146319f879ca/t/5f446c2012ef3956120b20df/1598319661535/Telehealth+Here+to+Stay+GCMA+research+report.pdf. [Google Scholar]
- 48.Li H.-L., Chan Y.C., Huang J.-X., Cheng S.W. Pilot study using telemedicine video consultation for vascular patients’ care during the COVID-19 period. Ann. Vasc. Surg. 2020;68(October):76–82. doi: 10.1016/j.avsg.2020.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Alizadeh A., Mohammadi A., Khademloo M., Hosaini H. Survey of views of medical students on telemedicine methods developed in the mazandaran university of medical sciences iran. Strides Dev. Med. Educ. 2013;10(2):247–259. http://sdme.kmu.ac.ir/article_90272.html [Internet] Available from: [Google Scholar]
- 50.Müller K.I., Alstadhaug K.B., Bekkelund S.I. Acceptability, feasibility, and cost of telemedicine for nonacute headaches: a randomized study comparing video and traditional consultations. J. Med. Internet Res. 2016;18(May (5):e140. doi: 10.2196/jmir.5221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Iribarren S.J., Cato K., Falzon L., Stone P.W. What is the economic evidence for mHealth? A systematic review of economic evaluations of mHealth solutions. PLoS One. 2017;12(2) doi: 10.1371/journal.pone.0170581. 2017/02/06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Badawy S.M., Kuhns L.M. Economic evaluation of text-messaging and smartphone-based interventions to improve medication adherence in adolescents with chronic health conditions: a systematic review. JMIR mHealth uHealth. 2016;4(October (4)):e121. doi: 10.2196/mhealth.6425. [DOI] [PMC free article] [PubMed] [Google Scholar]