Abstract
When patients lack suitable superficial veins in the upper extremity to create an arteriovenous fistula, surgeons are faced with a decision between a synthetic graft or autologous fistula using deep veins, such as a brachial artery to brachial vein arteriovenous fistula. In patients with a high radial artery origin (or brachioradial artery) and inadequate superficial veins, arteriovenous fistula creation will be even more challenging. In the present report, we describe a technique used in three such patients who underwent successful staged brachioradial artery to brachioradial vein arteriovenous fistula creation.
Keywords: Arteriovenous fistula, AV access, Hemodialysis access, Proximal radial artery, Radial vein, Vascular surgery
A radiocephalic fistula is the preferred choice for first-time hemodialysis access creation.1, 2, 3 However, the reported rates of primary failure of autologous arteriovenous fistulas (AVFs) are high.4 Synthetic grafts have been reported to have greater rates of all-cause mortality, infection, thrombosis, and steal syndrome compared with autologous AVFs.3,5 When superficial veins are inadequate, deep veins can be used to create autologous dialysis access. The use of the radial vein for hemodialysis access has been previously reported.6
The variable anatomy of the upper extremity arteries poses an additional challenge. A high origin of the radial artery, or brachioradial artery, occurs in 9.2% to 20.3% of people.7,8 Two-stage brachioradial artery to brachioradial vein (BR-BR) AVF is an autologous option for an AVF, which we used in three patients at our institution. All three patients provided written informed consent for the report of their clinical details and images.
Case report
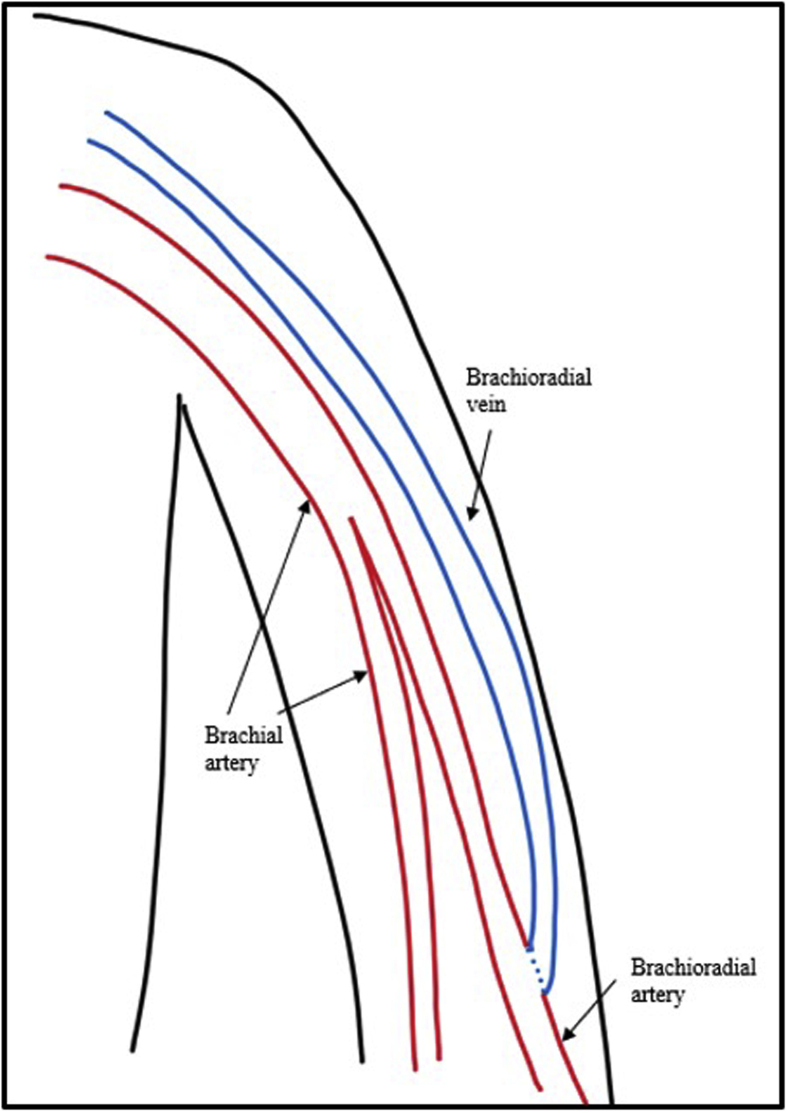
Three patients with end-stage renal disease (ESRD) had undergone BR-BR AVF creation within a 3-year period. No suitable superficial veins were identified in any of the three patients on preoperative vessel mapping ultrasound scans, and a high origin of the radial artery was present. The brachioradial veins measured >3 mm in diameter. Each first-stage operation consisted of an end to side arteriovenous anastomosis, and each second-stage operation consisted of superficialization underneath a flap of skin and subcutaneous fat. A schematic diagram of the BR-BR AVF is shown in Fig 1. Postoperatively, each patient had normal wound healing, palpable distal pulses at the wrist, and no sensorimotor changes during follow-up.
Fig 1.
Diagram of brachioradial artery to brachioradial vein (BR-BR) arteriovenous fistula (AVF).
Our first patient was a 64-year-old man with diabetes, hypertension, obesity, hepatitis C, a history of intravenous drug use, and ESRD. A first-stage, BR-BR AVF was created at the antecubital fossa. Three months later, the second-stage operation was performed. The brachioradial vein from the antecubital fossa to the mid-arm, in continuity with the brachial vein in the proximal arm, was exposed, and all tributary veins were ligated. A lateral subcutaneous flap was created, and the vein was secured within the flap using absorbable sutures. The fistula was used for 2 months after superficialization. The patient required percutaneous angioplasty >18 months after the initiation of use. At last follow-up, his fistula had a primary assisted functional patency of >2 years.
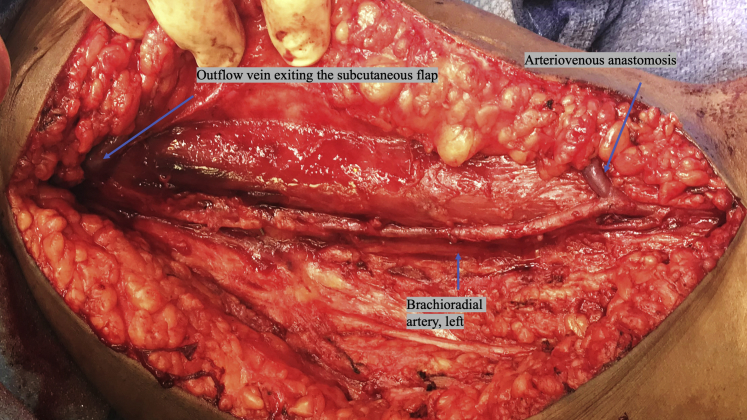
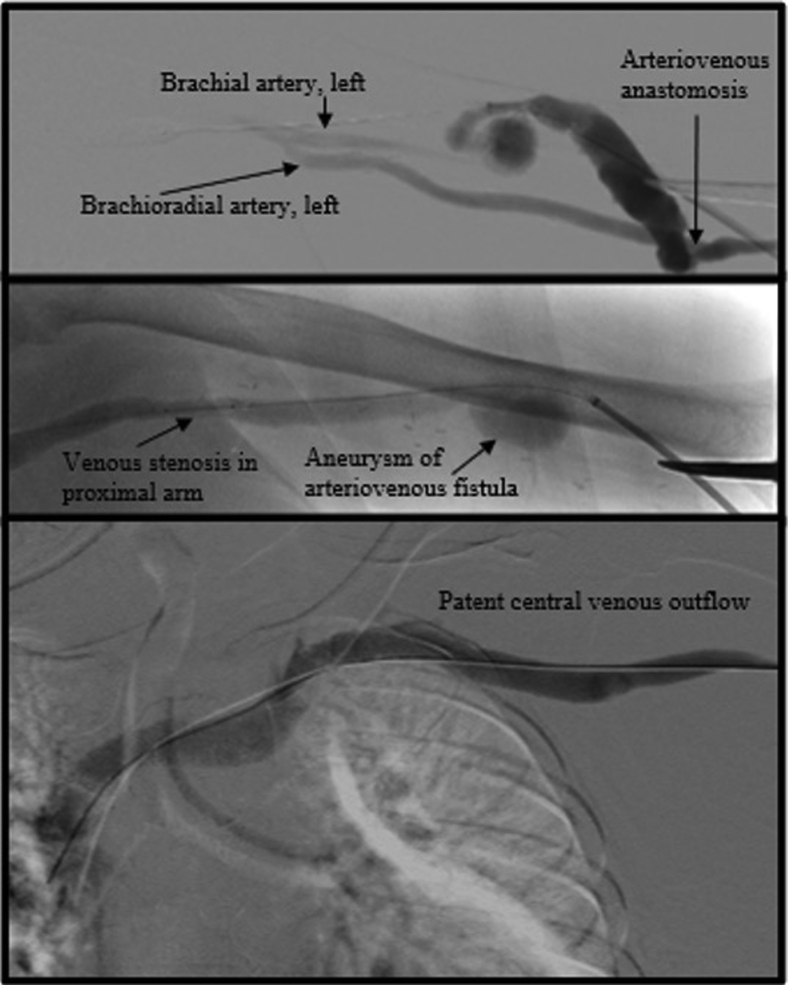
The second patient was a 38-year-old woman with diabetes, hypertension, and ESRD. A first-stage BR-BR AVF was created at the antecubital fossa. The second-stage revision was performed 3.5 months later. The brachioradial vein was 4 mm in diameter, without focal stenosis. The basilic vein was identified and dissected free. It entered the deep venous system in the mid-arm. The basilic vein measured <2.5 mm and had an early entry into the deep venous system. Although the basilic vein was not independently adequate in length and diameter, we believed we could use it to create a larger venous outflow. The brachioradial vein and basilic vein were opened longitudinally and syndactylized up to their point of confluence in the arm. The resultant arteriovenous fistula was >5 mm in diameter, with its main outflow via the brachial vein. The vein was superficialized. An intraoperative photograph of the second operation is shown in Fig 2. Four weeks later, the fistula was successfully cannulated. At 4 months after the initiation of use, the patient required percutaneous angioplasty for stenosis in the arm. At 3.5 months later, angioplasty was repeated. A stable aneurysm was present in the mid-arm. Images from the fistulogram are shown in Fig 3. At the last follow-up, her fistula had a primary assisted functional patency of 10 months.
Fig 2.
Intraoperative image of left upper extremity brachioradial arteriovenous fistula (AVF) superficialization.
Fig 3.
Fistulogram of patient 2 with an aneurysm in the mid-arm and stenosis in the proximal arm.
The third patient was a 60-year-old woman with human immunodeficiency virus, chronic obstructive pulmonary disease, and ESRD. A first-stage BR-BR AVF was created in the proximal forearm and superficialized 4 months later. Eight weeks postoperatively, the fistula was authorized for use. However, she died of an unknown cause 2 months after initiation of use of the fistula. She was still using her fistula at that time.
Discussion
The creation and maintenance of autologous access in patients without suitable superficial veins poses a significant challenge to access surgeons. The brachial vein transposition, or brachiobrachial AVF, is a well-described autologous alternative using the deep veins. The BR-BR AVF is analogous to a brachiobrachial AVF. Jennings et al9 reported primary patency of 46.2%, primary assisted patency of 75.5% and secondary patency of 92.4% at 24 months. Pham et al10 described higher primary patency but similar functional assisted patency of brachiobrachial AVFs compared with prosthetic grafts. The factors associated with successful brachiobrachial AVFs include early referral and no previous failed AV access.10,11 Generally, the brachial artery and veins will be larger in caliber than the radial artery and veins.
Brachial artery-based AVFs have been associated with a greater risk of steal syndrome than radial artery-based AVFs, likely related to the higher flow.9,12 Furthermore, cardiac risks, such as left ventricular hypertrophy and congestive heart failure, have been attributed to the greater flow rate of proximal AVFs.2,12 The data are insufficient to conclude whether the brachioradial artery would have clinical performance more consistent with the typical brachial or radial arteries.
It has been our practice to use the most peripheral point in the upper extremity where the brachioradial vein and its outflow is large enough for AVF creation. Accordingly, one of our patients had had her fistula created in the forearm, and the other two had had the arteriovenous anastomosis created at the antecubital fossa. Limited data are available to indicate the venous diameter at which the vessels can be deemed “adequate.” Extrapolating from the data reported by studies on brachiobrachial AVFs, we have used 3 mm as a minimum threshold for the brachioradial vein.13
Most brachioradial arteries course superficially to the true brachial artery in the arm. The median nerve is typically found with the true brachial artery, and a major nerve is not usually found with the brachioradial artery.8 It can be advantageous to use the brachioradial artery and vein, instead of the true brachial artery and vein to protect the median nerve. In our three patients, no median nerve injuries or steal syndrome were noted. One patient developed an aneurysm of her access. Secondary interventions were required in two of our three patients.
The present study had some limitations. The success of these AVFs was measured by the functional status at the follow-up examination. Consideration is warranted for other metrics not easily obtainable in the setting of an urban safety-net hospital. Another limitation was that the BR-BR AVF procedure is performed infrequently. Further experience will inform us about the long-term functionality of BR-BR AVFs. It would be interesting to compare percutaneous AVFs using the brachioradial artery and vein with surgical staged BR-BR AVFs.
Conclusions
The BR-BR AVF is an effective solution for establishing autologous arteriovenous access in patients with a high origin of the radial artery whose superficial upper extremity veins are inadequate. In patients with brachioradial veins >3 mm, it is reasonable to perform staged BR-BR AVF at the most peripheral point in the extremity where the vessels are adequate.
From the Midwestern Vascular Surgical Society
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Martinez L.I., Esteve V., Yeste M., Artigas V., Llagostera S. Clinical utility of a new predicting score for radiocephalic arteriovenous fistula survival. Ann Vasc Surg. 2017;41:56–61. doi: 10.1016/j.avsg.2016.09.022. [DOI] [PubMed] [Google Scholar]
- 2.Pisoni R.L., Zepel L., Fluck R., Lok C.E., Kawanishi H., Suleymanlar G. International differences in the location and use of arteriovenous accesses created for hemodialysis: results from the Dialysis Outcomes and Practice Patterns Study (DOPPS) Am J Kidney Dis. 2018;71:469–478. doi: 10.1053/j.ajkd.2017.09.012. [DOI] [PubMed] [Google Scholar]
- 3.Thomas M., Nesbitt C., Ghouri M., Hansrani M. Maintenance of hemodialysis vascular access and prevention of access dysfunction: a review. Ann Vasc Surg. 2017;43:318–327. doi: 10.1016/j.avsg.2017.02.014. [DOI] [PubMed] [Google Scholar]
- 4.Shenoy S. Surgical technique determines the outcome of the Brescia/Cimino AVF. J Vasc Access. 2017;18(Suppl 1):1–4. doi: 10.5301/jva.5000698. [DOI] [PubMed] [Google Scholar]
- 5.Ravani P., Palmer S.C., Oliver M.J., Quinn R.R., MacRae J.M., Tai D.J. Associations between hemodialysis access type and clinical outcomes: a systematic review. J Am Soc Nephrol. 2013;24:465–473. doi: 10.1681/ASN.2012070643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arroyo M.R., Sideman M.J., Spergel L., Jennings W.C. Primary and staged transposition arteriovenous fistulas. J Vasc Surg. 2008;47:1279–1283. doi: 10.1016/j.jvs.2008.01.047. [DOI] [PubMed] [Google Scholar]
- 7.Haładaj R., Wysiadecki G., Dudkiewicz Z., Polguj M., Topol M. The high origin of the radial artery (brachioradial artery): its anatomical variations, clinical significance, and contribution to the blood supply of the hand. BioMed Res Int. 2018;2018:1520929. doi: 10.1155/2018/1520929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rodriguez-Niedenfuhr M., Vazquez T., Nearn L., Ferreira B., Parkin I., Sanudo J.R. Variations of the arterial patter in the upper limb revisited: a morphological and statistical study, with a review of the literature. J Anat. 2001;199:547–566. doi: 10.1046/j.1469-7580.2001.19950547.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jennings W.C., Sideman M.J., Taubman K.E., Broughan T.A. Brachial vein transposition arteriovenous fistulas for hemodialysis access. J Vasc Surg. 2009;50:1121–1126. doi: 10.1016/j.jvs.2009.07.077. [DOI] [PubMed] [Google Scholar]
- 10.Pham X.D., Kim J.J., Ihenachor E.J., Parrish A.B., Bleck J.D., Kaji A.H. A comparison of brachial artery-brachial vein arteriovenous fistulas with arteriovenous grafts in patients with poor superficial venous anatomy. J Vasc Surg. 2017;65:444–451. doi: 10.1016/j.jvs.2016.09.037. [DOI] [PubMed] [Google Scholar]
- 11.Greenberg J.I., May S., Suliman A., Angle N. The brachial artery-brachial vein fistula: expanding the possibilities for autogenous fistulae. J Vasc Surg. 2008;48:1245–1250.e2. doi: 10.1016/j.jvs.2008.06.038. [DOI] [PubMed] [Google Scholar]
- 12.Gerrickens M.W.M., Vaes R.H.D., Govaert B., van Loon M., Tordoir J.H.M., van Hoek F. Three year patency and recurrence Rates of revision using distal inflow with a venous interposition graft for high flow brachial artery based arteriovenous fistula. Eur J Vasc Endovasc Surg. 2018;55:874–881. doi: 10.1016/j.ejvs.2018.03.014. [DOI] [PubMed] [Google Scholar]
- 13.de Castro-Santos G., Salles A.G., dos Anjos G.S., Procópio R.J., Navarro T.P. Brachial vein transposition: an alternative to hemodialysis arteriovenous graft. J Vasc Bras. 2019;18:e20190077. doi: 10.1590/1677-5449.190077. [DOI] [PMC free article] [PubMed] [Google Scholar]