Abstract
Background
The increasing shift toward a more generalized medical undergraduate curriculum has led to limited exposure to subspecialties, including neurosurgery. The lack of standardized teaching may result in insufficient coverage of core learning outcomes. Social media (SoMe) in medical education are becoming an increasingly accepted and popular way for students to meet learning objectives outside formal medical school teaching. We delivered a series of case-based discussions (CbDs) over SoMe to attempt to meet core learning needs in neurosurgery and determine whether SoMe-based CbDs were an acceptable method of education.
Methods
Twitter was used as a medium to host 9 CbDs pertaining to common neurosurgical conditions in practice. A sequence of informative and interactive tweets were formulated before live CbDs and tweeted in progressive order. Demographic data and participant feedback were collected.
Results
A total of 277 participants were recorded across 9 CbDs, with 654,584 impressions generated. Feedback responses were received from 135 participants (48.7%). Participants indicated an increase of 77% in their level of knowledge after participating. Of participants, 57% (n = 77) had previous CbD experience as part of traditional medical education, with 62% (n = 84) receiving a form of medical education previously through SoMe. All participants believed that the CbDs objectives were met and would attend future sessions. Of participants, 99% (n = 134) indicated that their expectations were met.
Conclusions
SoMe has been shown to be a favorable and feasible medium to host live, text-based interactive CbDs. SoMe is a useful tool for teaching undergraduate neurosurgery and is easily translatable to all domains of medicine and surgery.
Key words: Brainbook, Medical education, Neurosurgery, Public engagement, Science dissemination, Social media
Abbreviations and Acronyms: CbD, Case-based discussion; CES, Cauda equina syndrome; CM, Cervical myelopathy; COVID-19, Coronavirus disease 2019; EDH, Extradural hematoma; GBM, Glioblastoma; HCP, Hydrocephalus; LMICs, Low- and middle-income countries; SAH, Subarachnoid hemorrhage; SDH, Subdural hematoma; SoMe, Social media; TBI, Traumatic brain injury; TBI-CM, Traumatic brain injury–clinical management; TBI-P, Traumatic brain injury–pathophysiology
Introduction
In recent years, there has been a shift toward a more generalized undergraduate medical curriculum in the United Kingdom. This shift has meant that there is less exposure to several specialties, including neurosurgery. As a result, some specialties have developed specialty-specific core curricula to ensure accurate, standardized teaching occurs.1 However, there are no national guidelines for undergraduate neurosurgery teaching, albeit with some recommendations from the Royal College of Surgeons and the Association of Surgeons in Training.2,3
An increasing body of literature has highlighted the disparities in neurosurgical teaching among medical schools.4,5 A United Kingdom survey examining teaching practice found that in some institutions, neurosurgery was not taught as part of the curriculum, and in others, not all students received formal teaching. Significant variations in the content were also reported and teaching was often undertaken by nonspecialist clinicians.4 Since the United Kingdom moved toward more streamlined residency programs through nationalized selection into specialties in 2005, postgraduate experience in neurosurgery has also dwindled; this experience would previously have been invaluable for doctors subsequently moving into other specialties.
There is evidence to suggest that teaching neurosurgery in the undergraduate and postgraduate curricula has beneficial advantages, including broadening the understanding of clinical neurosciences and reducing students' fear of neurologic practice.5 Approximately 20% of all acute medical admissions are for neurologic conditions,6 with headaches and back pain representing many of these presentations.7 Being able to identify red flag symptoms and the need for urgent referral and to arrange appropriate investigations are important for modern clinicians because the implications of missing or delaying time-critical neurosurgical diagnoses can be devastating for the patient. Conditions such as cauda equina syndrome (CES) are a prime example of this need, with more than half of referrals to United Kingdom specialist centers made without any previous imaging.8 Recognizing the diverse presentation of neurosurgical conditions can be challenging.
Furthermore, it has been recognized that providing low-cost, accessible, professionally curated digital content for neurosurgery trainees in low- and middle-income countries (LMICs) can provide a long-term benefit.9 The ability to transfer knowledge and decision-making skills among colleagues from Western countries and LMICs is an important aspect of the use of social media (SoMe) as a tool. This collaboration has traditionally been performed through passive webinars or e-learning platforms, which do not often promote discussion of concepts or allow time for questions.
One way to discuss the approach to these neurosurgical conditions is through the use of case-based discussions (CbDs). CbDs are a structured discussion of a clinical case, which links theory to practice using inquiry-based learning methods.10 CbDs have been widely used in both undergraduate and postgraduate medical curricula to develop clinical reasoning. A recent study examining surgical trainee perceptions of CbDs found them to be a positive feature in the curriculum and a powerful tool to encourage discussion, higher thinking, and reflection.11
Traditionally, these discussions have taken place in a work-based environment between the trainee and trainer. However, over recent years, SoMe have become an increasingly accepted and popular way to deliver medical education and enable students and surgical trainees to meet learning objectives outside the clinical setting. This situation is especially pertinent in the context of LMICs, where the ratio of neurosurgeons to the general population can be almost 1:10 million. Teaching over SoMe enables global engagement, facilitates collaborative learning, and provides several practical advantages for the user. The widespread integration of SoMe into medical education has meant that many institutions have now adopted SoMe as an educational tool in the classroom.12
We have previously reported that neurosurgery science communication over the Brainbook Twitter platform was successful in disseminating neurosurgical knowledge and enhancing public engagement.13 Brainbook is a neurosurgical charity (not-for-profit organization) dedicated to public engagement, science communication, and medical education. Therefore, in an attempt to bridge the gap in undergraduate neurosurgical teaching, CbDs were delivered over the Brainbook Twitter platform in an attempt to meet core learning needs in neurosurgery and determine whether SoMe-based CbDs were an efficient and acceptable method of education. These CbDs were also delivered during the coronavirus disease 2019 (COVID-19) pandemic, at a time when face-to-face teaching was not possible. This situation provided an opportunity to continue delivering neurosurgery medical education to a global audience, during a global pandemic. To our knowledge, this is the first resource to deliver live, structured neurosurgery CbDs over Twitter.
Methods
Host Medium
Twitter was used as a medium to host 9 CbDs pertaining to the common neurosurgical conditions in practice. The 9 CbDs consisted of subarachnoid hemorrhage (SAH), traumatic brain injury–pathophysiology (TBI-P) and traumatic brain injury–clinical management (TBI-CM), glioblastoma (GBM), hydrocephalus (HCP), subdural hematoma (SDH), extradural hematoma (EDH), cervical myelopathy (CM) and CES. Content was shared through the Brainbook account (@realbrainbook). A sequence of informative and interactive tweets were formulated before the live CbDs and were tweeted in progressive order. Each session was moderated by a United Kingdom neurosurgery trainee. Users interacted in the discussions by replying to the tweets to answer questions and raise discussions, as well as liking and retweeting. Tweets were numbered and categorized using the clinical abbreviations along with a hashtag (e.g., #BBSAH) to enable easy recognition and following of the discussions.
Qualitative and Quantitative Data Collection
Qualitative and quantitative data were collected before and after CbD using a unique link on Twitter to the online survey platform QualtricsXM (Qualtrics International Inc., Seattle, Washington, USA). The data were exported onto Microsoft Excel (Microsoft Corp., Redmond, Washington, USA) for further analysis.
Data collected consisted of a pre-CbD and post-CbD questionnaire. The pre-CbD questionnaire consisted of participant demographics (Appendix 1). The post-CbD questionnaire consisted of previous experience of CbDs and SoMe learning, CbD content and delivery, and participants' overall experience (Appendix 2). Free-text responses were also included in the post-CbD questionnaire. Using a 5-point interval ranking scale, participants were asked to evaluate their level of knowledge before and after CbD at the end of each CbD. The change in participants' level of knowledge was measured subjectively. They were further asked to rank their level of understanding of 6 key learning outcomes using a 5-point Likert scale (Appendix 3). SoMe impressions and engagements for each CbD were also collected using Twitter analytics. The engagements and impressions for only the educational tweets generated were collected.
Data were analyzed using descriptive statistics. Statistical analysis was performed on the quantitative data using GraphPad Prism (GraphPad Software, San Diego, California, USA). A 2-tailed paired t test was used to determine the difference in the level of knowledge before and after CbD. The level of knowledge data for each CbD was combined to ascertain any difference between the pre-CbD and post-CbD level of knowledge. For the open-ended questions, key themes were extracted from the participants' responses using simple thematic analysis. All quantitative data were plotted using GraphPad Prism. Level of knowledge data were plotted using column error plots with mean and 95% confidence interval.
Results
Demographics
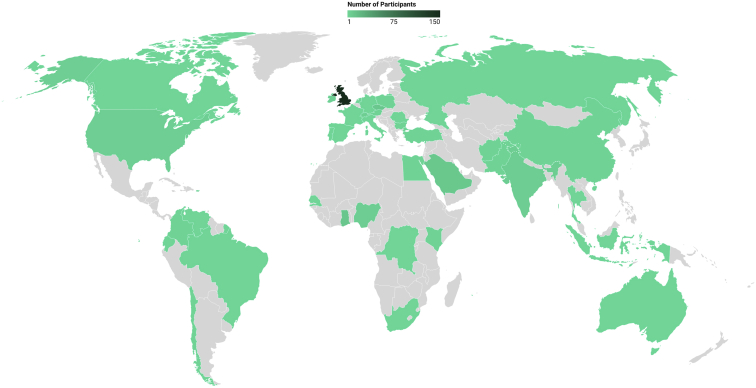
A total of 277 participants were recorded from the pre-CbD questionnaire across the 9 CbDs undertaken from February to April 2020. Of the participants, 189 (68%) were medical students. Of all medical students, the participants were predominantly year 4 level (n = 67, 24%). The remaining participants were specialist trainee doctors (n = 46, 17%), foundation year doctors (n = 22, 8%) and other health care practitioners (n = 8, 3%). The roles of 12 participants were unspecified (4%). Widespread global participation was also recorded. Participants came from 39 different countries, with most from the United Kingdom (54.2%) followed by Singapore (7.6%), Ghana (4%) and the Czech Republic (3.6%). Twenty participating countries (51.2%) were LMICs, represented by 49 participants (18%) (Table 1). Figure 1 highlights the reach of the CbDs as well as the representation from participating countries.
Table 1.
The Number of Participants from Each Participating Country
| Participating Country | Number of Participants |
|---|---|
| United Kingdom | 150 |
| Singapore | 21 |
| Ghana | 11 |
| Czech Republic | 10 |
| Saudi Arabia | 9 |
| Not specified | 7 |
| India | 6 |
| Nigeria | 6 |
| Switzerland | 5 |
| United States | 5 |
| Ireland | 4 |
| Austria | 3 |
| Bulgaria | 3 |
| Afghanistan | 2 |
| Chile | 2 |
| China | 2 |
| Colombia | 2 |
| Egypt | 2 |
| Kenya | 2 |
| Netherlands | 2 |
| Pakistan | 2 |
| Poland | 2 |
| Turkey | 2 |
| Australia | 1 |
| Brazil | 1 |
| Canada | 1 |
| Democratic Republic of Congo | 1 |
| Ecuador | 1 |
| France | 1 |
| Germany | 1 |
| Indonesia | 1 |
| Italy | 1 |
| Portugal | 1 |
| Romania | 1 |
| Russia | 1 |
| Senegal | 1 |
| South Africa | 1 |
| Spain | 1 |
| Thailand | 1 |
| Venezuela | 1 |
| Total | 277 |
Figure 1.
Participating countries.
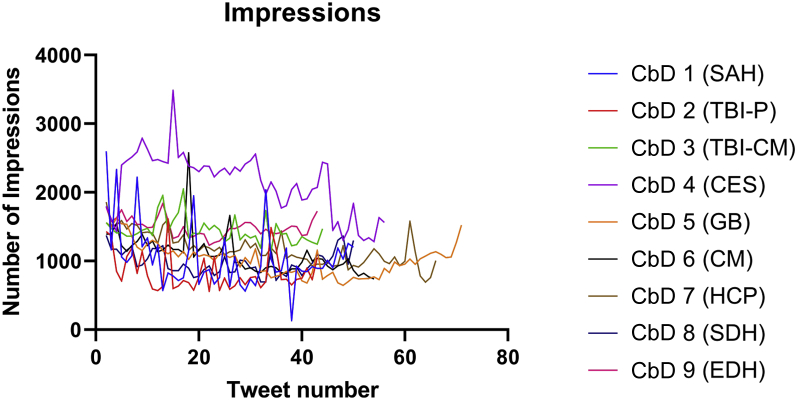
The CbDs were undertaken at either 1:30 pm or 7:30 pm (Greenwich Mean Time +1) and lasted from 1 to 2 hours. Each CbD had on average 53 tweets (range, 43–71). A total of 423 tweets were recorded across the 9 CbDs. Tweets comprised statements and questions, including differential diagnosis, investigations, treatments, and pathophysiology. An example of a CbD can be seen in Appendix 4. Across 9 CbDs, 24,376 engagements were generated, as defined by the total number of times users interacted with the tweets. A combined 654,584 impressions (defined as penetrance onto individual media feeds and total views of the content) were generated (Figure 2). In Figure 2, the first tweet has been removed because of its higher penetrance on the Twitter timeline; this removal helps to highlight the change in impressions throughout and among the CbDs over time. Of the 9 CbDs, 6 took place after the beginning of the United Kingdom COVID-19 lockdown.
Figure 2.
Impressions. CbD, case-based discussion; CES, cauda equina syndrome; CM, cervical myelopathy; EDH, extradural hematoma; GBM, glioblastoma; HCP, hydrocephalus; SAH, subarachnoid hemorrhage; SDH, subdural hematoma; TBI-CM, traumatic brain injury–clinical management; TBI-P, traumatic brain injury–pathophysiology.
The most popular case was GBM with 58 participants signing up for the CbD. GBM was followed by SAH (n = 43), SDH (n = 40), CM (n = 39), TBI-P (n = 27), EDH (n = 23), and TBI-CM (n = 19). The lowest number of recorded participants were in the CES and HCP CbDs (n = 14). However, the CbD with the greatest impact on SoMe was CES, which generated 126,435 impressions. CES was followed by HCP (n = 85,299) and GBM (n = 74,148). HCP received the greatest number of engagements across all CbDs (n = 4180).
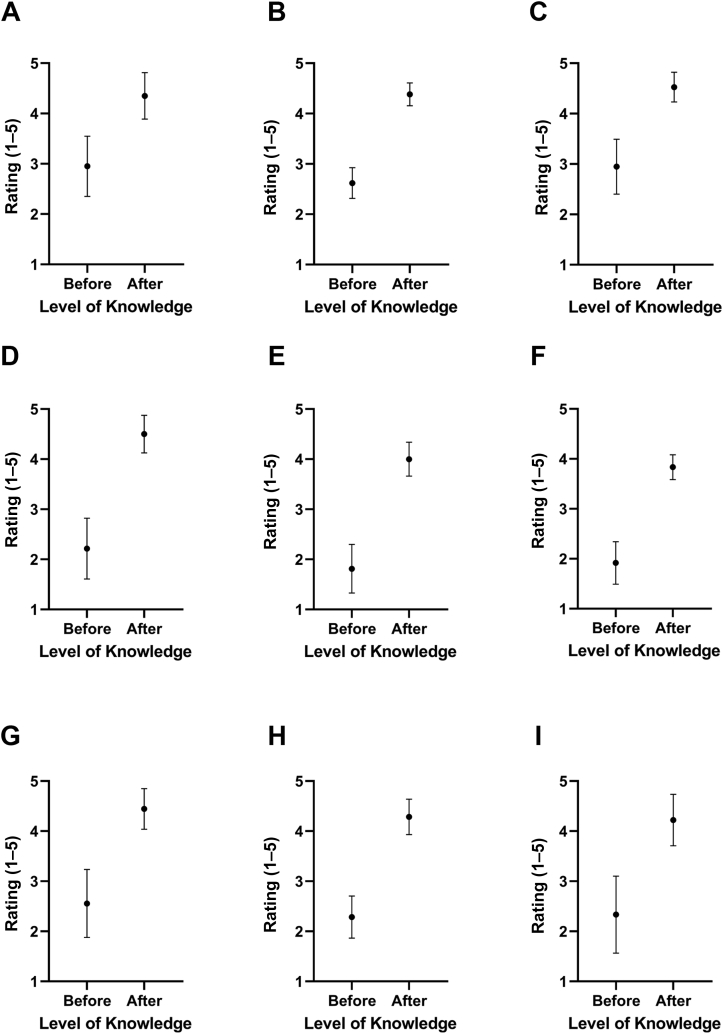
Feedback Analysis
Feedback was received from 135 participants (48.7%). The SAH CbD received 21 feedback forms (49%), TBI-P 21 (78%), TBI-CM 19 (100%), CES 14 (100%), GBM 16 (28%), CM 12 (31%), HCP 9 (64%), SDH 14 (35%), and EDH 9 (39%). Pre-CbD and post-CbD level of knowledge was scored subjectively using a 5-point interval ranking scale (Appendix 3). The mean pre-CbD score was 2.4, whereas the post-CbD mean score was 4.29 (Figure 3). The mean overall improvement in level of knowledge was 1.84 ± 0.9 (+77%). Of all CbDs, GBM showed the greatest improvement in level of knowledge with a 2.19 ± 0.98 (+121%) increase (Table 2). GBM was followed by CES (2.29 ± 0.83, +103%) and CM (1.92 ± 0.51, +100%). The lowest improvement in the level of knowledge was observed in the SAH CbD (1.4 ± 0.99, +48%) (Figure 4).
Figure 3.
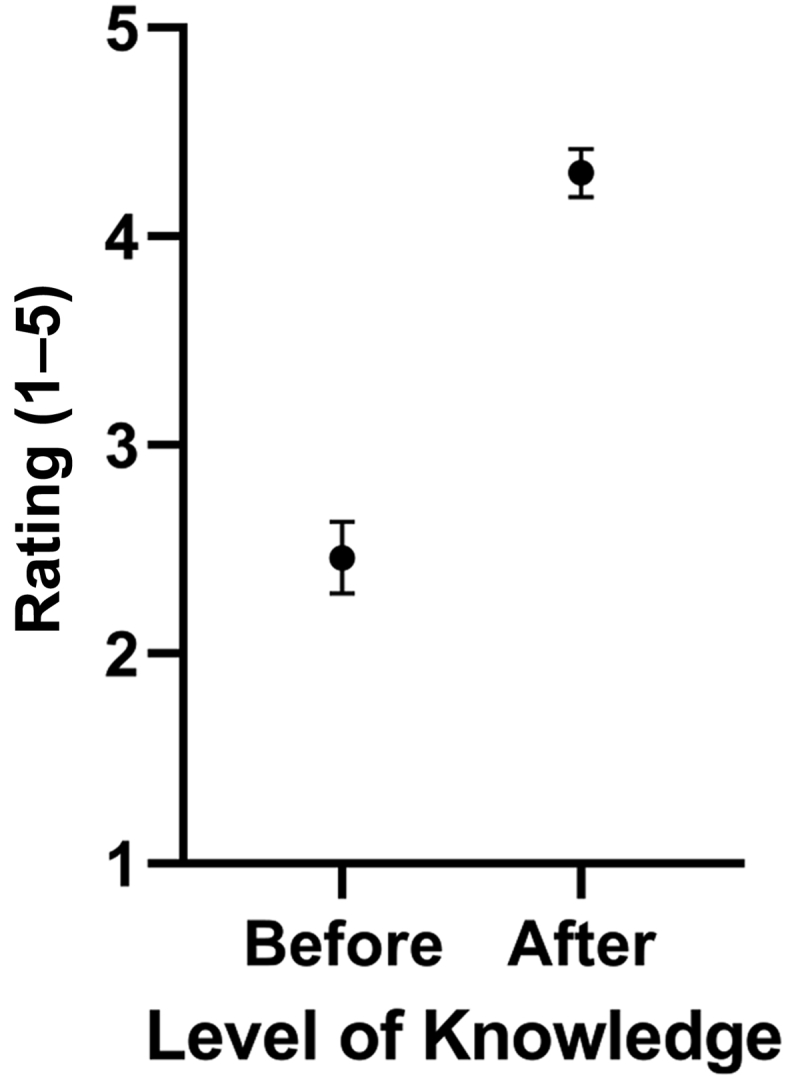
Overall change in Level of Knowledge for all Case-based discussions combined.
Table 2.
Pre–Case-Based Discussion and Post–Case-Based Discussion Level of Knowledge and Overall Change in Level of Knowledge After the Case-Based Discussions
| CbD | Average Level of Knowledge Before CbD | Average Level of Knowledge After CbD | Level of Knowledge Change After CbD | % Change in Level of Knowledge After CbD | P Value | Number of Participants | Number of Responses |
|---|---|---|---|---|---|---|---|
| Subarachnoid hemorrhage | 2.95 | 4.38 | +1.4 ± 0.99 | +48 | <0.0001 | 43 | 21 |
| Traumatic brain injury–pathophysiology | 2.62 | 4.38 | +1.76 ± 0.54 | +67 | <0.0001 | 27 | 21 |
| Traumatic brain injury–clinical management | 2.95 | 4.53 | +1.58 ± 1.07 | +54 | <0.0001 | 19 | 19 |
| Cauda equina syndrome | 2.21 | 4.5 | +2.29 ± 0.83 | +103 | <0.0001 | 14 | 14 |
| Glioblastoma | 1.81 | 4.00 | +2.19 ±0.98 | +121 | <0.0001 | 58 | 16 |
| Cervical myelopathy | 1.92 | 3.83 | +1.92 ± 0.51 | +100 | <0.0001 | 39 | 12 |
| Hydrocephalus | 2.56 | 4.44 | +1.89 ± 0.78 | +74 | <0.0001 | 14 | 9 |
| Subdural hematoma | 2.29 | 4.29 | +2.0 ± 0.96 | +88 | <0.0001 | 40 | 14 |
| Extradural hematoma | 2.33 | 4.22 | +1.89 ± 1.05 | +81 | <0.0007 | 23 | 9 |
CbD, case-based discussion.
Figure 4.
Improvement in the level of knowledge: (A) subarachnoid hemorrhage; (B) traumatic brain injury–pathophysiology; (C) traumatic brain injury–clinical management; (D) cauda equina syndrome; (E) glioblastoma; (F) cervical myelopathy; (G) hydrocephalus; (H) subdural hematoma; (I) extradural hematoma.
Participants were asked to rate their level of understanding of 6 key learning outcomes after CbD. Level of understanding was scored using a 5-point Likert scale (Appendix 3). Learning outcomes assessed were uniform across 7 of 9 CbDs. Two CbDs focused on neuropathophysiology and thus required the assessment of different learning outcomes. Table 3 shows the mean scores of the learning outcomes assessed. All learning outcomes achieved a mean score of ≥4.5. The question on the ability to recognize the presenting features of the neurosurgical condition discussed ranked the highest, with a post-CbD mean score of 4.78. Understanding the most common complications had the lowest post-CbD mean score of 4.51.
Table 3.
Average Level of Understanding in 6 Key Learning Outcomes After the Case-Based Discussions
| This CbD Has Improved My Ability to Recognise the Presenting Features | This CbD Has Improved My Ability to Recognise the Main Causes | This CbD Has Improved by Ability to Understand the Investigations Performed to Aid Diagnosis | This CbD Has Improved My Ability to Understand the Different Treatments | This CbD Has Improved My Ability to Understand the Common Complications | This CbD Has Improved My Ability to Understand the Type of Questions to Ask in the History | |
|---|---|---|---|---|---|---|
| Subarachnoid hemorrhage | 4.62 | 4.48 | 4.62 | 4.43 | 4.38 | 4.33 |
| Cauda equina syndrome | 4.71 | 4.79 | 4.93 | 4.71 | 4.43 | 4.86 |
| Glioblastoma | 4.63 | 4.31 | 4.63 | 4.56 | 4.19 | 4.69 |
| Cervical myelopathy | 4.92 | 4.67 | 4.83 | 4.75 | 4.58 | 4.83 |
| Hydrocephalus | 4.89 | 4.89 | 4.78 | 4.89 | 4.89 | 4.89 |
| Subdural hematoma | 4.93 | 4.86 | 4.86 | 4.79 | 4.43 | 4.86 |
| Extradural hematoma | 4.78 | 4.78 | 4.78 | 4.89 | 4.67 | 4.67 |
CbD, case-based discussion.
As part of the feedback form, participants were asked to comment on their experience with our CbDs and provide their opinions on the role of CbDs in neurosurgical education (Appendix 2). Of the 135 feedback forms received, all respondents (100%) would recommend the Twitter CbDs to colleagues and believed that CbD objectives were met and 99% (n = 134) believed that their expectations were met. The CbDs were clear and easy to follow for 98% (n = 132) of respondents and all respondents (100%, n = 135) would attend any future CbDs. Fifty-seven percent of respondents (n = 77) had previous experience of CbDs as part of the undergraduate medical degree and 62% (n = 84) had taken part in SoMe medical education previously.
Free-text responses were included in the feedback form. Most responses focused on the interactive nature of the CbD, the friendly learning environment, and the clear and succinct descriptions in the CbD. Participants particularly enjoyed the instant feedback and use of diagrams for explanation and found the feedback useful at identifying gaps in knowledge (Table 4).
Table 4.
Examples of Free-Text Responses to the Question “What Aspects of the CbD Did You Like?”
| Learning Environment | Usefulness | Engagement |
|---|---|---|
| It is very inspiring, and a great peer-to-peer learning opportunity | Very logical format, realistic to a clinical scenario | Very engaging, chance to interact with other interested students and health professionals |
| I really enjoyed the fact that there was a moderator, almost simulating a tutorial! | Easy to follow, good breakdown of questions following structure like history etc, visual aids also helpful | The interaction was swift and alive! |
| It's a very supportive environment. Very encouraging | Easily digestible and focused learning points | Interactive, highlighted the knowledge that I knew. Engaging questions |
| Loved the fast responses, the interactive nature makes you think on your feet, a really creative use of social media to stimulate critical thinking | The step-by-step, logical nature of the CbD massively helped me more clearly and comprehensively understand the concepts discussed | Enjoyed the engagement with participants and the case scenario |
| The community aspect of it was enjoyable | The interactive nature makes you think on your feet, a really creative use of social media to stimulate critical thinking | The feedback was useful in identifying gaps in my learning |
CbD, case-based discussion.
With respect to feedback on how the CbDs could be improved, participants recommended undertaking the CbDs at a time to suit different time zones. Some participants found the CbD pacing quick and recommended performing them at a slower rate. Furthermore, some participants were unable to join from the beginning and recommended a downloadable thread after CbD. A few participants would have liked the CbDs to be of a more challenging level with respect to the clinical anatomy and management options as well as more feedback in response to some of the questions asked. This feedback was recorded and will be used to improve future CbD content as well as the development of a more specific curriculum.
Discussion
SoMe have proved to be an invaluable tool in delivering medical education because of their practical advantages and their ability to engage a global audience. SoMe enable learning outside timetabled teaching and facilitate collaborative communication and online discussion.14 To our knowledge, delivering live, structured Twitter CbDs has never been reported previously in the literature.
Our study set out to evaluate the effectiveness of teaching core neurosurgical learning outcomes in the form of CbDs over SoMe. Overall, our CbDs were well received, with 98% of respondents reporting that they were clear and easy to follow and 100% reporting that they would attend future CbDs. Across the 9 CbDs, 654,584 impressions were generated, and 24,376 engagements were recorded. This result is encouraging and confirms that teaching CbDs over SoMe provides an engaging learning experience for participants.
The importance of teaching neurosurgery as part of the undergraduate curriculum is becoming increasingly recognized as vital in increasing the knowledge and confidence to promptly recognize and initially manage neurosurgical patients.15 However, the amount of neurosurgery teaching in the undergraduate curriculum varies considerably across medical schools in the United Kingdom.4 Previous literature has suggested the use of clinical electives and student-selected components as a method for increasing medical student exposure in neurosurgery.16 However, not all students are able to undertake such an opportunity. This disadvantage is particularly relevant to students in LMICs, where exposure to neurosurgery in high-income countries can present with several logistical and financial barriers.
In an attempt to standardize neurosurgery teaching, Whitehouse et al.4 have previously recommended the development of national undergraduate learning outcomes to ensure accurate, high-quality teaching. There remains a lack of specific neurosurgical learning outcomes. Over recent years, the Royal College of Surgeons of England has developed a National Undergraduate Curriculum in Surgery as a guide for medical students to identify the learning outcomes expected before graduation.2 Although these outcomes are not extensive and specific to neurosurgery, we modeled our CbDs according to this curriculum and expanded on it to ensure that key neurosurgical learning objectives could be met. All CbDs were open access, which enabled the free dissemination of knowledge and the exchange of ideas among participants from a wide range of countries.
To ascertain the effectiveness of our CbDs at meeting core neurosurgical learning outcomes, we assessed the before and after level of knowledge and the level of understanding of key neurosurgical concepts. Our results showed an improvement in the level of knowledge in all CbDs. This result, coupled with the fact 100% of respondents would attend future CbDs, highlights that delivering our CbDs over SoMe is an effective way of teaching and disseminating neurosurgical knowledge. This finding supports the idea that there is potential for SoMe CbDs to be used alongside the undergraduate neurosurgery curriculum, or any other curriculum, to maximize educational opportunities in neurosurgery.
To investigate further which of the neurosurgical conditions the participants performed well in, the before and after level of knowledge scores were compared for all CbDs. The GBM CbD had the greatest improvement in the level of knowledge followed by CES and CM, whereas the SAH and the TBI-CM CbDs showed the lowest improvement in the level of knowledge. This difference may be because neuro-oncology is not well covered in undergraduate curricula but there is a heavy focus on neurotrauma and intracerebral bleeds. This situation is because of their proportional workload in both neurosurgery and emergency medicine in general. CES is also intricately linked to spine anatomy, which is difficult to understand conceptually, both at an undergraduate and postgraduate level, which may account for why it received one of the greatest increases in knowledge attainment. However, further analysis regarding the structure of the medical school neurosurgery curriculum is required to draw any specific conclusion.
To determine user experience with our CbDs, we asked the participants to provide feedback at the end of each CbD. With respect to the structure of the CbDs, the responses stated that the CbDs were concise, in an orderly manner, and easy to follow, with focused learning points. Participants further reported that the CbDs were realistic to a clinical scenario and were an engaging and memorable way to learn. Regarding the CbD learning environment, participants commented on the supportive, collaborative nature of the CbDs and the instant, detailed feedback that they received. These results further suggest that the delivery of CbDs over SoMe is an effective method of delivering medical education and in increasing medical student exposure to neurosurgery.
Online CbDs have been widely used in medicine in an attempt to deliver interactive, engaging learning. Examples of this learning include the interactive clinical cases provided by New England Journal of Medicine and Lancet. Both these online platforms use illustrative videos, graphics, and radiologic imaging to review clinical scenarios and facilitate clinical decision making.17,18 As well as disseminating clinical information, online CbDs have been used to teach professionalism and engage doctors in reflective writing. Nadeau et al. used the online virtual learning platform, Blackboard, to create threaded discussions to encourage clinical conversations and enhance professional growth.19
Twitter provides several benefits for the user and may be a useful addition to a medical educator's repertoire of teaching tools (Table 5). First, it is an easily accessible, open-access, and user-friendly platform. The ability to host live Twitter discussions allows for engaging conversations with instant feedback and creates a supportive learning environment for the user. Twitter's 280-character limit means that the tweets are concise and memorable. The hashtag feature on Twitter enables content to be searched for easily, allowing participants to quickly search for other related responses in the discussion. Although the CbDs are live, the threads are embedded in the Twitter profile, meaning that users can customize their learning and revisit certain ideas and topics discussed easily. However, because of the structure and chronicity of the Twitter platform, the tweets may be difficult to find in the future. A workaround to this will be the ability to save such threads for future reference as Twitter “Moments.”
Table 5.
Benefits of Twitter as a Tool for the Dissemination of Neurosurgical Knowledge Through the Use of Live Case-Based Discussions
| Open-access, easily accessible platform |
| Wide audience outreach |
| Ability to integrate questions to reinforce engagement and enhance learning |
| Supportive learning environment |
| Instant feedback to aid understanding of topic |
| Opportunity to network with students and colleagues |
| Potential to join and revisit cases at any point |
| Concise information delivered through limited Twitter word count |
| Easily searchable content through the use of hashtag feature |
| Ability to share videos, images and links to aid learning |
| Encourage free discussion and conversation around topics |
| Ability to follow the CbD anonymously |
CbD, case-based discussion.
Instagram is another SoMe platform that has been used in medical education. Instagram is tailored toward sharing photos and videos and is an effective tool in conveying visual topics, particularly clinical images, and in integrating multiple choice questions to enhance interaction and reinforce learning. This tool is inherently useful for anatomy, which relies on the individual being able to identify structures.20 Like Twitter, Instagram uses the hashtag feature to enable a greater audience reach.
Facebook is another platform that is becoming increasingly used in delivering medical education. Because of its ease of use, Facebook is effective at encouraging collaboration and engagement among users through likes and comments. One study that explored the use of a dedicated Facebook page for human anatomy education21 found that it was a useful tool in providing opportunities for peer assessment and feedback. However, privacy and professionalism remained a concern for students, given that they had to use their personal profile to interact. This situation prevents anonymity, which can be a barrier to engagement in discussion. Although participants were logged in via their personal Twitter for the CbDs, the use of Twitter handles enables users to make their profile identifiable or anonymous as they wish. Although some participants had identifiable profiles, the data collected were not identifiable and completion of the survey was deemed to be providing consent.
Video-streaming platforms such as YouTube are a successful tool for teaching. The benefit of YouTube is that it allows users to pause, rewind, and replay content, enabling users to customize their learning to fit their needs. Compared with Twitter, Facebook, and Instagram, YouTube is less focused on user interaction and responses and is regarded as a passive learning experience. Despite this factor, 1 study showed that 78% of medical students use YouTube as their main source of anatomy education.22 Zoom, a video-conference application, is a relatively new addition to the classroom in the delivery of remote teaching sessions. Compared with the other SoMe platforms, Zoom allows face-to-face virtual teaching and provides a more personal approach to delivering medical education.
Although SoMe platforms have been widely used in delivering medical education, pitfalls surrounding their effectiveness compared with face-to-face teaching exist.23,24 One factor commonly encountered is the technical challenges associated with online platforms. Another important consideration is the varying degree of student participation. Several studies have reported that this factor is a challenge to teaching and have found some students tended to be more active than others, whereas others read SoMe posts without making any contributions.25 This is not a phenomenon that is exclusive to SoMe, but part of the normal classroom dynamics. By reinforcing ground rules and providing a safe environment for discussion, it is possible to garner more engagement from students who might not typically volunteer their thoughts in a discussion.
SoMe-based education often lacks the quality control that traditional in-person teaching has, and the use of informed consent and ethics.20 To address this pitfall, our CbDs were moderated by neurosurgical residents and any comments to the thread were reviewed and answered, to ensure that any inaccurate information submitted by the participants were corrected. Although privacy breaches and patient consent are a concern over SoMe, our CbDs were not based on real patients, and all images were taken from online radiologic databases or journals and appropriately referenced within the CbD thread, precluding the need for patient consent.
Exposure to neurosurgical teaching at an undergraduate level provides students with the skills and confidence to approach a neurosurgical patient and helps to promote interest in the specialty.26 Given this knowledge, we therefore recommend further similarly structured CbDs to be delivered over SoMe to enhance undergraduate neurosurgery teaching and increase medical student engagement and exposure in neurosurgery. The CbDs described were conducted before and during the current COVID-19 pandemic, when face-to-face tutorials were still possible in selected centers as well as when all educational institutions were closed. This factor therefore shows a powerful tool in medical education during mandated social distancing. We propose Twitter SoMe CbDs to be used alongside the traditional undergraduate neurosurgery curriculum to maximize educational opportunities in neurosurgery and enable students to identify gaps in their knowledge. Although we have shown the use of Twitter to be an effective form of delivering neurosurgical education, face-to-face teaching provides a more personal approach to education, encourages discussion, collaboration and role play live from a facilitator at hand, and provides a more social element to teaching.
The objective for the future is disseminate the CbDs to a wider audience. Although much of the Brainbook Charity Twitter following is those interested in the neurosciences, we hope to engage a larger audience by promoting the CbDs within universities through our Brainbook university ambassador scheme. This strategy will help advertise the CbDs to more medical students at all levels of training. We further hope to increase the participation of both health care practitioners and postgraduate trainees. One way that we can achieve this goal is through collaboration with the national surgical societies, such as the Royal College of Surgeons of Edinburgh and the Society of British Neurological Surgeons.
In addition, we hope to deliver future CbDs over a variety of SoMe platforms. Given the advantages of each platform, CbDs can be tailored to suit the purpose and audience of each platform. In addition, question polls can be used to enhance participation and engagement across our CbDs.
Future CbDs will also have neurosurgery residents and consultants invited from each of the subspecialties to curate and moderate cases. This strategy will give an insight into their specific practices and research in their subspecialty and enable the discussion of any innovations in the field. Furthermore, inviting neurosurgeons from a variety of global units will enable surgeons to share their practices and discuss common diseases in their country.
More conditions in neurosurgery and common neurologic diseases will be included in subsequent cases as well as current research pertaining to the case. This strategy will aid conversation and discussion surrounding innovation, new practices, or evidence-based knowledge. Given the increasing number of charities dedicated to neurosurgical conditions and research, collaborations with these charities to further raise awareness of neurologic conditions and highlight the resources and support available within the CbDs can be considered.
A perspective that has not been formally assessed here is the impact for the moderating neurosurgical resident. The moderators, 2 of whom are authors of this article, note that there are multiple benefits, including refreshing and consolidating knowledge, SoMe, and teaching skills and the ability to distill pearls of wisdom succinctly (into the length of a single tweet).
The limitations of this study were that although there was a high feedback response rate, not all participants who took part in the CbDs or followed the thread submitted feedback. This is a particularly difficult issue to work around given the lack of a physical space for discussion. In reality, participants are often asked to complete feedback before leaving a session, something that cannot happen online. To remedy this situation, certificates of participation were provided for those who completed feedback. Brainbook is a well-recognized educational resource and involvement with the charity has been referenced previously in United Kingdom National Selection applications. The certificates provided could therefore be used as evidence of commitment to the specialty for those keen to pursue a career in neurosurgery.
Given the nature of SoMe, we were unable to track the unique number of participants across all 9 CbDs. For future sessions, we may alter the way that we collect data by assigning participants a unique study identification beforehand on a separate system to input at the start of the session.
Overall change in the participants' level of knowledge was assessed using a 5-point interval ranking scale. The pre-CbD and post-CbD level of knowledge scores were both assessed in the post-CbD questionnaire. An alternative method would have been to assess the pre-CbD and post-CbD level of knowledge independently to ensure a more accurate assessment of the participants' understanding of each topic. Although learning outcomes for each CbD were assessed using a 5-point Likert scale, specific topic questions would have provided a more accurate way of assessing the participants' understanding of each of the key learning outcomes after each CbD. In addition, although participants reported that the CbDs were a useful way of learning, and their knowledge of particular topics was increased after each CbD, response bias should be taken into consideration. One way of addressing this situation would be to objectively test the change in the level of knowledge through a pre-CbD and post-CbD test.
Participants' interest in pursuing neurosurgery as a career was also not assessed. This subject may have been relevant in ascertaining the impact of the CbDs on such aspirations. In addition, it would help guide future CbDs in terms of tailoring content; it may be possible to run sessions tailored to a general medical student population with generic management pearls and tips for when to refer to neurosurgery, whereas other sessions could be tailored to aspiring neurosurgeons with more detail about anatomic and surgical considerations. Managing the level of detail in the latter is an important consideration. It would be ideal to cross-collaborate with postgraduate platforms such as The Neurosurgical Atlas to merge resources and prevent reiteration of material online.27
Another important consideration is time zone differences. Our CbDs were delivered at either 1:30 pm or 7:30 pm (Greenwich Mean Time +1), and therefore, this excluded many participants or meant that participants in different time zones ended the CbD early. Because Twitter was used as the medium to deliver our CbDs, the format of the discussion meant that participants had to engage with the CbD from the beginning to fully benefit. Nonetheless, our results show that participants highly valued our CbDs and found these to be an engaging and effective way to learn neurosurgery.
Conclusions
We report our experience of teaching live Twitter CbDs over SoMe. This study has shown that delivering CbDs over SoMe is an effective, easy-to-access way of disseminating neurosurgical knowledge to a global audience. We propose that a curriculum-based approach of teaching CbDs over SoMe can be an engaging and enjoyable learning experience for participants, which can enhance undergraduate neurosurgery teaching and increase medical student exposure to neurosurgery. Furthermore, providing free global access to the CbDs enables the dissemination of knowledge and exchange of ideas between high-income countries and LMICs.
Declaration of Competing interest
P.J.H. is supported by a Research Professorship from the National Institute for Health Research (NIHR), the NIHR Cambridge Biomedical Research Centre, an NIHR Senior Investigator award, a European Union Seventh Framework Program grant (CENTER-TBI; grant number 602150), and the Royal College of Surgeons of England. A.G.K. is supported by a Clinical Lectureship, School of Clinical Medicine, University of Cambridge and the Royal College of Surgeons of England. A.C. is supported by a Great Ormond Street Hospital (GOSH) Children's Charity Surgeon Scientist Fellowship and the GOSH–National Institute of Health Research Biomedical Research Centre. Brainbook is a United Kingdom charity, registered with the United Kingdom Charities Commission to operate in England and Wales (charity number 1181711).
CRediT Authorship Contribution Statement
Nicola Newall: Conceptualization, Writing - original draft, Writing - review & editing, Methodology. Brandon G. Smith: Formal analysis, Data curation, Visualization, Writing - review & editing. Oliver Burton: Formal analysis, Data curation, Visualization, Writing - review & editing. Aswin Chari: Writing - review & editing, Supervision. Angelos G Kolias: Writing - review & editing, Supervision. Peter J Hutchinson: Writing - review & editing, Supervision. Alex Alamri: Conceptualization, Methodology, Resources, Writing - review & editing, Supervision, Project administration. Chris Uff: Writing - review & editing, Supervision.
Acknowledgments
With thanks to Mr. Michael Cearns and Dr. Laura Lippa for their support and help in moderating CbDs.
Footnotes
Conflict of interest statement: This research was commissioned by the National Institute for Health Research (NIHR) Global Health Research Group on Neurotrauma (project 16/137/105) using UK aid from the UK Government. The views expressed in this publication are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Contributor Information
Brandon G. Smith, Email: bgs30@cam.ac.uk.
Brainbook:
Gideon Adegboyega, Meedie Ali, Sacha Chiuta, Gwenllian Evans, Patrick Hurley, Orla Mantle, Chidera Ota, Duranka Perera, Camilla Siig, and Staša Tumpa
Appendix 1. Demographics
-
1.What is your role?
- 1st year medical student
- 2nd year medical student
- 3rd year medical student
- 4th year medical student
- 5th year medical student
- 6th year medical student Foundation Doctor/Intern Specialist trainee/Resident Nurse Physician Associate Other (comment)
-
2.
University/Hospital attending?
-
3.
Country of residence?
Appendix 2. Case-Based Discussion–Specific Feedback
Each of the following questions were answered with Yes/No
-
1.
I would recommend this CbD experience to a colleague/friends
-
2.
I have previously attended social media-based learning experiences
-
3.
I have experience of CbDs as part of my undergraduate
-
4.
Do you feel this CbD met your expectations?
-
5.
Were the objectives of this CbD met?
-
6.
Was the CbD clear and easy to follow?
-
7.
Would you attend future CbDs?
Free-Text Responses
-
1.
What aspects of the CbD did you like?
-
2.
What aspects of the CbD did you not like
-
3.
How did you hear about us?
-
4.
Any further comments?
Appendix 3. Post-CbD Questionnaire
Each of the following was assessed using a 5-point Likert scale from 1 to 5 (1, poor; 5, excellent).
Level of Knowledge
-
1.
My level of knowledge of (CbD delivered) before the CbD was:
-
2.
My level of knowledge of (CbD delivered) after the CbD was:
Learning Outcomes
Each of the following was assessed using a 5-point Likert scale from 1 to 5. (1, poor; 5, excellent).
-
1.
This CbD has improved my ability to recognise the presenting features of (CbD delivered)
-
2.
This CbD has improved my ability to recognise the main causes of (CbD delivered)
-
3.
This CbD has improved by ability to understanding the investigations performed to aid diagnosis of (CbD delivered)
-
4.
This CbD has improved my ability to understand the different treatments of (CbD delivered)
-
5.
This CbD has improved my ability to understand the common complications of (CbD delivered)
-
6.
This CbD has improved my ability to understand the type of questions to ask in the history of (CbD delivered)
Appendix 4. Cerebellar Metastasis CbD
-
1.
A 54 year old female with a history of breast cancer presents with a 3 week history of worsening headache, trouble walking and visual impairment. Her breast cancer was treated 2 years ago with wide local excision followed by radiotherapy.
-
2.
Based on the history so far what are your thoughts on a differential diagnosis?
-
3.
Neoplastic: metastasis, meningioma, primary glial tumour. Infectious: abscess. Vascular: intracerebral haemorrhage, AVM. Other: hydrocephalus secondary to neoplasm.
-
4.
You begin to take a further history from the patient. She's become increasingly drowsy and seems to be deteriorating rapidly since being in the emergency department.
-
5.
What approach would you like to do to access the patient?
-
6.
ABCDE. An ABCDE approach is the most appropriate in this situation.
-
7.
On assessment: A: Airway is patent. B:RR is 18/min. Equal breath sounds bilaterally with no added noises. C: HR is 64 beats per minute and regular. BP is 136/86 mmHg. Capillary refill is <2 seconds. FBC, U+E, clotting screen and group and save taken.
-
8.
D: Capillary glucose is 5.2mmol/l. She opens her eyes to pain; she flexes to pain and she mutters incomprehensible sounds in response to your questions. Based on your assessment what is her GCS?
-
9.
8. This can be written as E2V2M4.
-
10.
What does this make you worry about?
-
11.
Who do you need to call for help?
-
12.
The anaesthetists come and review the patient with a plan to intubate and mechanically ventilate.
-
13.
How would you like to investigate the cause of our patients deteriorating condition further?
-
14.
An urgent CT head. The results of the CT head are shown. What do you notice?
-
15.
The CT demonstrates a solitary cerebellar metastasis (likely from our patient's history of breast cancer) and hydrocephalus.
-
16.
What features from a history or examination would make you consider the lesion is in the cerebellum?
-
17.
DANISH is a great way to remember the signs. D-Dysdiadochokinesis, A-Ataxia, N-nystagmus, I-intentional tremor, S-slurred speech, H-hypotonia.
-
18.
Signs and symptoms may vary depending on the location of the lesion in the cerebellum. If the lesion involves the cerebellar vermis there may be truncal ataxia with a broad-based gait.
-
19.
A cerebellar hemispheric lesion causes loss of co-ordination ipsilaterally, intentional tremor, past pointing, dysdiadochokinesis and nystagmus.
-
20.
Before we consider the cause of hydrocephalus lets firstly go through the circulation and absorption of CSF. This will help us understand what happens when the circulation or the absorption is disrupted in some way.
-
21.
CSF is a clear, proteinaceous fluid that bathes the CNS. CSF has a number of functions. It protects the brain from damage by “buffering” the brain, it excretes waste products e.g. harmful metabolites or drugs and it transports hormones to areas of the brain.
-
22.
How much CSF is circulating at any given moment?
-
23.
There is around 150 ml of CSF circulating at any given moment. ~17% of this volume is located in the ventricles and the remaining in the cisterns and subarachnoid space.
-
24.
CSF forms at a rate of 0.3–0.4 ml per min, this equates to 18–25 ml per hour and 430–530 ml per day. Where is CSF produced?
-
25.
CSF is produced by specialised vascular tissue called choroid plexuses. The choroid plexuses are located in the lateral ventricles, third ventricle and fourth ventricle.
-
26.
From the lateral ventricles, CSF flows through the right and left foramen of Munro (interventricular foramen) into the third ventricle. Next, it flows through the aqueduct of Sylvius into the fourth ventricle. The 4th ventricle is anterior to the cerebellum.
-
27.
From the fourth ventricle, where does the CSF exit?
-
28.
CSF may exit the foramen of Luschka laterally or the foramen of Magendie medially into the subarachnoid space. When CSF passes through the foramen of Magendie this results in filling of the spinal subarachnoid space.
-
29.
When CSF passes through the foramen of Luschka this results in filling of the subarachnoid space of the cisterns and the cerebral cortex. The level at which CSF enters the subarachnoid space is called the cerebellomedullary cistern.
-
30.
CSF flow is largely dependent on the cardiac cycle. During systole, the brain vasculature expands and compresses the lateral and third ventricle. This forces CSF to flow down the cerebral aqueduct. During diastole, flow through the aqueduct reverses.
-
31.
Does anyone know how CSF is then reabsorbed into our bloodstream?
-
32.
CSF is reabsorbed through outpouchings into the superior sagittal sinus called arachnoid granulations. This occurs through a pressure dependent gradient. This means that when the CSF pressure is greater than the venous pressure, CSF will flow into the superior sagittal sinus.
-
33.
However, the arachnoid villi provides a valvular mechanism for flow of CSF into the bloodstream. This means that even if the CSF pressure is lower than the venous pressure, the arachnoid villi will not let blood pass into the venous system.
-
34.
From the superior sagittal sinus, CSF flows into the transverse sinus via the confluence of sinuses. From here, CSF enters the sigmoid sinus followed by the internal jugular vein.
-
35.
Now we understand CSF flow let's go onto understanding the types of hydrocephalus. Does anyone know what are the two main types of hydrocephalus are?
-
36.
Communicating (non-obstructive) versus non-communicating (obstructive). Who knows the difference between the two?
-
37.
Non-communicating occurs when there is structural blockage within the ventricular system; whereas communicating (non-obstructive) is due to impaired CSF absorption.
-
38.
Who can give us some examples of the causes of communicating and non-communicating?
-
39.
Non-communicating: congenital (congenital aqueduct stenosis), obstructing lesion.
-
40.
Communicating: subarachnoid haemorrhage, infective meningitis, normal pressure hydrocephalus, congenital (Dandy Walker syndrome).
-
41.
Does anyone know any other type of hydrocephalus?
-
42.
Normal Pressure Hydrocephalus classically presents with a triad of symptoms. Who can name this triad for us?
-
43.
Dementia, gait disturbances and urinary incontinence.
-
44.
In the case of our patient what do you think the cause of hydrocephalus is?
-
45.
Non-communicating (obstructive hydrocephalus) secondary to cerebellar metastasis. As we mentioned before, the 4th ventricle is anterior to the cerebellum. This means that lesions in the cerebellum, if large enough, can compress the 4th ventricle and affect the CSF flow.
-
46.
If left untreated acute hydrocephalus can be fatal so emergency treatment is required. Do you know of any ways we can treat the hydrocephalus surgically?
-
47.
An external ventricular drain (EVD). An EVD is a thin drainage tube that sits outside the patient's head, with its tip in the ventricular system. The end of the drain is connected to a measurement system and can be used to monitor the ICP.
-
48.
The external drainage system is comprised of a collection chamber connected to a drainage bag, pressure scale and pressure transducer. The amount of CSF drainage can be controlled by raising or lowering the external drainage system to different pressures on the pressure scale.
-
49.
To find out more about what an EVD, click this link here: https://brainbookcharity.org/external-ventricular-drain/
-
50.
If you want to see how an EVD is inserted click on this link here: https://www.youtube.com/watch?v=XaL8AElw79o&feature=emb_title
-
51.
Our patient is taken to theatre and an EVD is placed. Then she is proned and undergoes a debulking of the cerebellar metastasis.
-
52.
She returns to the neuro-observations unit post-operatively. On assessment her GCS is E3V4M5. She remains on the ward and is showing good recovery.
-
53.
On day 3 the EVD is challenged. This can be done by rapid or gradual weaning. This is done in order to see the effectiveness of the EVD or to see whether any other intervention is required.
-
54.
One way of challenging the EVD rapidly is to clamp the EVD and observe for any signs of raised ICP. It's also important to examine for any CSF leak at the dressing site. This may take place over 24 hours.
-
55.
Gradual weaning is done by gradually changing the pressures on the EVD followed by clamping. Again, it's important to monitor for changes in ICP on the monitor and any clinical signs of raised ICP.
-
56.
Our patient's EVD was clamped for 24 hours. Her ICP was monitored and she showed no clinical signs of raised ICP. A follow-up CT head was performed which showed persistent hydrocephalus.
-
57.
Do you know what we could do if there was persisting communicating hydrocephalus and we needed a permanent treatment?
-
58.
In the long term, hydrocephalus can be treated by a CSF diversion procedure. A ventriculoperitoneal (VP) shunt is typically the procedure of choice. Who knows any other types of shunts we can use?
-
59.
Lumboperitoneal (LPS), ventriculopleural (VPS) or ventriculoatrial (VAS). Often these shunts may be required if the patient has had extensive intra-abdominal surgery or high intraperitoneal pressure.
-
60.
So what is a shunt? A shunt allows excess CSF to drain to other parts of the body. Shunts generally consist of 3 components: (1) An inflow catheter (this drains the CSF from the ventricles. It leaves the brain through a small hole in the skull, which then runs under the skin).
-
61.
(2) A valve mechanism (this regulates the pressure control through the shunt tubing. It is connected to the catheter and lies between the skin and the skull, usually on top of the head or behind the ear).
-
62.
(3) An outflow catheter (this runs under the skin and moves the CSF from the valve to the peritoneal cavity, heart or other drainage site).
-
63.
What does a VP shunting involve then? In a VP shunt a catheter is inserted into the ventricle with tubing tunnelled subcutaneously down the thorax and then further tunnelled into the peritoneal cavity where the CSF is absorbed.
-
64.
Here is a video showing you how a VP shunt is inserted: https://www.youtube.com/watch?time_continue=122&v=SDsBr6sXkH4&feature=emb_title. If you want any further information on VP shunts then clink this link here: https://brainbookcharity.org/ventriculo-peritoneal-shunt/
-
65.
Do you know any complications of shunting?
-
66.
Over-drainage (low pressure headaches, subdural haematoma), under-drainage, blockage, infection, disconnection, seizures, distal end problems (abdominal hernias [VPS], cardiac arrhythmias [VAS]).
-
67.
Back to our patient. Our patient is doing well on the ward. An MRI head is arranged and a CT chest, abdomen, pelvis to exclude any further metastatic disease and aid staging.
-
68.
The MRI head confirms a good debulk of the metastasis but residual remains. The CT chest, abdomen pelvis shows reoccurrence of her breast cancer.
-
69.
She is commenced on high dose steroids (Dexamethasone) with a PPI. The plan is for her to be discussed at the upcoming MDT to decide on the best management and plan for any further treatment options.
References
- 1.The Royal College of Obstetricians and Gynecologists (UK) RCOG Press; 2009. Working Party Report on the National Undergraduate Curriculum in Obstetrics and Gynaecology; pp. 1–31.https://www.rcog.org.uk/globalassets/documents/careers-and-training/academic-training/ndergraduate-curriculum-working-party-report.pdf Available at: [Google Scholar]
- 2.The Royal College of Surgeons England, (RCSENG) RCSENG - Professional Standards and Regulation; 2015. National undergraduate curriculum in surgery 2015.https://www.rcseng.ac.uk/-/media/files/rcs/library-and-publications/non-journal-publications/undergraduate_curriculum_2015-web.pdf Available at: [Google Scholar]
- 3.Baker D., Deekonda P., Glasbey J. Core content of the medical school surgical curriculum: consensus report from the Association of Surgeons in Training (ASIT) Int J Surg. 2020;84:186–193. doi: 10.1016/j.ijsu.2019.12.036. [DOI] [PubMed] [Google Scholar]
- 4.Whitehouse K.J., Moore A.J. Undergraduate teaching of neurosurgery–what is the current practice in the UK and is there a need for improvement? Br J Neurosurg. 2015;29:753–757. doi: 10.3109/02688697.2015.1054361. [DOI] [PubMed] [Google Scholar]
- 5.Resnick D.K. Neuroscience education of undergraduate medical students. Part I: Role of neurosurgeons as educators. J Neurosurg. 2000;92:637–641. doi: 10.3171/jns.2000.92.4.0637. [DOI] [PubMed] [Google Scholar]
- 6.Chowdhury R.N., Hasan A.T.M.H., Rahman Y.U., Khan S.I., Hussain A.R., Ahsan S. Pattern of neurological disease seen among patients admitted in tertiary care hospital. BMC Res Notes. 2014;7:20. doi: 10.1186/1756-0500-7-202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. James S.L., Abate D., Abate K.H. Global, regional, and national incidence, prevalence, and years lived with disability for 354 Diseases and Injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–1858. doi: 10.1016/S0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fountain D.M., Davies S.C.L., Woodfield J. Evaluation of nationwide referral pathways, investigation and treatment of suspected cauda equina syndrome in the United Kingdom. https://doi.org/10.1080/02688697.2019.1648757 [e-pub ahead of print]. Br J Neurosurg. [DOI] [PubMed]
- 9.Nicolosi F., Rossini Z., Zaed I., Kolias A.G., Fornari M., Servadei F. Neurosurgical digital teaching in low-middle income countries: beyond the frontiers of traditional education. Neurosurg Focus. 2018;45(4):E17. doi: 10.3171/2018.7.FOCUS18288. [DOI] [PubMed] [Google Scholar]
- 10.Williamson J.M.L., Osborne A.J. Critical analysis of case based discussions. Br J Med Pract. 2012;5:5–8. [Google Scholar]
- 11.Phillips A., Lim J., Madhavan A., Macafee D. Case-based discussions: UK surgical trainee perceptions. Clin Teach. 2016;13:207–212. doi: 10.1111/tct.12411. [DOI] [PubMed] [Google Scholar]
- 12.Keenan I.D., Slater J.D., Matthan J. Social media: Insights for medical education from instructor perceptions and usage. Med Ed Publish. 2018 doi: 10.15694/mep.2018.0000027.1. accessed April 19, 2021. [DOI] [Google Scholar]
- 13.Alamri A., Rogers P., Kearns C. Social media for dissemination and public engagement in neurosurgery–the example of Brainbook. Acta Neurochir (Wien) 2019;161:5–9. doi: 10.1007/s00701-018-3757-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ansari J.A.N., Khan N.A. Exploring the role of social media in collaborative learning the new domain of learning. Smart Learn Environ. 2020;7:9. [Google Scholar]
- 15.Hanrahan J., Burford C., Ansaripour A. Undergraduate neurosurgical conferences–what role do they play? Br J Neurosurg. 2019;33:76–78. doi: 10.1080/02688697.2018.1527288. [DOI] [PubMed] [Google Scholar]
- 16.Kolias A.G., Trivedi R.A. Enhancing the exposure of medical students to neurosurgery. Br J Neurosurg. 2013;27:706. doi: 10.3109/02688697.2013.833166. [DOI] [PubMed] [Google Scholar]
- 17.McMahon G.T., Solomon C.G., Ross J.J., Loscalzo J., Campion E.W. Interactive medical cases–a new journal feature. N Engl J Med. 2009;361:1113. [Google Scholar]
- 18.Stanley D., Grainger E. Introducing interactive grand rounds. Lancet Respir Med. 2015;3:271. [Google Scholar]
- 19.Nadeau M.T., Tysinger J., Wiemers M. A case-based approach for teaching professionalism to residents with online discussions. J Adv Med Educ Prof. 2016;4:1–7. [PMC free article] [PubMed] [Google Scholar]
- 20.Douglas N.K.M., Scholz M., Myers M.A. Reviewing the role of Instagram in education: can a photo sharing application deliver benefits to medical and dental anatomy education? Med Sci Educ. 2019;29:1117–1128. doi: 10.1007/s40670-019-00767-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jaffar A.A. Exploring the use of a facebook page in anatomy education. Anat Sci Educ. 2014;7:199–208. doi: 10.1002/ase.1404. [DOI] [PubMed] [Google Scholar]
- 22.Barry D.S., Marzouk F., Chulak-Oglu K., Bennett D., Tierney P., O’Keeffe G.W. Anatomy education for the YouTube generation. Anat Sci Educ. 2016;9:90–96. doi: 10.1002/ase.1550. [DOI] [PubMed] [Google Scholar]
- 23.El Bialy S., Jalali A. Go Where the students are: a comparison of the use of social networking sites between medical students and medical educators. JMIR Med Educ. 2015;1:e7. doi: 10.2196/mededu.4908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gholami-Kordkheili F., Wild V., Strech D. The impact of social media on medical professionalism: a systematic qualitative review of challenges and opportunities. J Med Internet Res. 2013;15:e184. doi: 10.2196/jmir.2708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Varga-Atkins T., Dangerfield P., Brigden D. Developing professionalism through the use of wikis: a study with first-year undergraduate medical students. Med Teach. 2010;32:824–829. doi: 10.3109/01421591003686245. [DOI] [PubMed] [Google Scholar]
- 26.Knight J., Stroud L., Geyton T., Stead A., Cock H.R. Medical student perceptions of clinical neurosurgery teaching in an undergraduate medical school curriculum. Br J Neurosurg. 2017;31:727–730. doi: 10.1080/02688697.2017.1335856. [DOI] [PubMed] [Google Scholar]
- 27.Neurosurgical Atlas Inc. The Neurosurgical Atlas by Aaron Cohen-Gadol M.D. Available at: https://https://www.neurosurgicalatlas.com/. Accessed December 2, 2020.