Abstract
Aims:
This protocol describes a study aiming to: (1) describe pathways and experiences of women’s symptom recognition, appraisal and management of endometriosis; and (2) identify differences in pathways and experiences among a socioeconomically and racially diverse group of women.
Design:
Descriptive qualitative study with stratified purposeful sampling
Methods:
Data will be collected from a minimum of 24 women with provider-presumed or surgically confirmed diagnoses across two time points. The study will recruit across socioeconomic status (SES) and race/ethnicity (non-Hispanic White, non-Hispanic Black and Hispanic/Latina) to ensure diversity of the sample. Recruitment will occur at a large public hospital in the southeastern United States (US). Participants will be interviewed using semi-structured interview guides informed by Elder and Giele’s Life Course perspective approaching women as active beings in dynamic systems shaped by: 1) their location in time and space; 2) linked lives; and 3) human agency and 4) the time of their lives. Each woman’s experiences, symptoms and contacts with health care systems will be mapped to trace their diagnostic pathways. Coded interviews and data will undergo within- and across-case analysis to identify similarities and differences in their experiences. Institutional review board approval was obtained June 2019.
Discussion:
The participants’ diagnostic maps will enable us to distinguish the differences in pathways and experiences between and across groups. Findings will inform the development of interventions aimed at shortening the time to diagnosis.
Impact:
This will be the first study to compare pathways to diagnosis of endometriosis in a socioeconomically and racially diverse sample of U.S. women using the life course perspective. The results from this research stand to inform future interventions aimed at helping women achieve more timely diagnoses.
Keywords: endometriosis, pathway, diagnosis, delay, qualitative interview, protocol, life course, disparities, equity, nurses, midwives, nursing
Introduction
Endometriosis, the proliferation of endometrial cells exterior to the uterus, is a debilitating chronic illness associated with chronic pelvic pain and poor health-related quality of life (Fuldeore & Soliman, 2017; Giudice & Kao, 2004; Zondervan, Becker, & Missmer, 2020). Endometriosis affects approximately 10% of reproductive age women, with global estimates suggesting prevalence of approximately 200 million women (Adamson, Kennedy, & Hummelshoj, 2010; As-Sanie et al., 2019). While a common disease, barriers in diagnosis and treatment are associated with endometriosis being under researched, with limited funding available for interventions with impact (As-Sanie et al., 2019; National Institutes of Health, 2020).
Diverse samples in endometriosis research are also lacking, with minimal data on race, ethnicity and socioeconomic status (SES). Historically, endometriosis study samples are largely White and SES data is lacking or confounded with race/ethnicity (Bougie, Healey, & Singh, 2019). Studies lack diversified information from broad diverse racial and/or ethnic groups. Largely homogeneous samples have biased our current knowledge of the disease, supporting stereotypes of women who suffer from the disease, with potential harm to clinical practice (Bougie et al., 2019). Bougie, Healey and Singh (2019) recently highlighted the need for more inclusive samples in endometriosis research, with a focus on ethnically sensitive symptomatology:
Until we are able to examine the patients’ diagnostic journey in an ethnically/culturally sensitive manner, accounting for the potential variation in the pattern of seeking medical attention, we will be unable to make relevant conclusions based on the diagnosis of endometriosis alone (Bougie et al., 2019, p. 2).
In response, this protocol describes a study to investigate the pathways to diagnosis of endometriosis in non-Hispanic White, non-Hispanic Black and Hispanic/Latina women across SES in the southeastern United States (U.S.). The final sample will include women with surgically confirmed and provider-presumed diagnoses to increase the inclusion of women with limited access to care. This study uses a life course perspective which will strengthen our insight into symptom appraisal, recognition and management as related to lifestyle, social and environmental factors contributing to diagnosis among missed populations.
Background
Worldwide, women and adolescents experience extended times to diagnosis. Delays in diagnosis, measured from the onset of symptoms to a diagnosis of endometriosis, have had averages reported as great as nearly 12 years in the US (Hadfield, Mardon, Barlow, & Kennedy, 1996), 10.4 years in Austria and Germany (Hudelist et al., 2012), nearly 8 years in the UK (Hadfield et al., 1996), 3.8 years in Brazil,(T. M. Santos, Pereira, Lopes, & Depes Dde, 2012) and 7.4 years in the Netherlands (Staal, van der Zanden, & Nap, 2016). A broad study across 10 countries showed a mean delay of 6.7 years with a range from 3.3 years in China to 10.7 years in Italy (Nnoaham et al., 2011).
The largest barrier in the diagnostic pathway is the required surgical pathology of endometriosis. Despite treatment largely targeted at symptom management and clinical symptoms used to provisionally diagnose endometriosis, the surgical evaluation with adjunct histologic review is the only way to make a definitive diagnosis (Giudice & Kao, 2004; Kinkel, Brosens, & Brosens, 2006). This standard can represent an obstacle to diagnosis, and we see that access to care can influence health care use among women with endometriosis. Recently, a study in Puerto Rico reported that women with private health insurance were more likely to have surgery, be prescribed opioids and use emergency services compared with women with public coverage (Fourquet et al., 2019). Worldwide, women with reduced access to resources or less comprehensive health coverage may experience significant barriers to diagnosis.
Since most studies and prevalence calculations typically sample patients with a confirmed diagnosis, the understanding of the pre-diagnosis period is limited, and study samples systematically exclude women with limited access to healthcare. As a result, little is known about the significance of the length in diagnostic delay of endometriosis or the potential outcomes of delayed diagnosis, particularly in populations of lower SES or Women of Color.
Women face social, environmental, informational and system barriers to diagnosis during the pre-diagnostic period. On the patient level, the period from symptom recognition to help-seeking can be the source of significant delay in diagnosis (Andersen & Cacioppo, 1995; Ballard, Lowton, & Wright, 2006). Women frequently normalize their pain, interpreting symptoms as ‘normal menstruation’. This coping behavior extends the period of appraisal and lengthens time to diagnosis (Culley et al., 2013; Denny, 2004b; Young, Fisher, & Kirkman, 2015). Family and social relationships may contribute to this misinformation and prolong the delay in help-seeking when others minimize or normalize the significance of symptoms (Culley et al., 2013; Denny, 2004b).
Several factors can influence a woman’s path. Age of diagnosis may stratify the care of women with endometriosis as dysmenorrhea is the most common menstrual symptom reported by adolescents and young women and women with endometriosis (American College of Obstetricians and Gynecologists, 2018). Early diagnosis is important in adolescent patients, as untreated disease can have a lasting impact on quality of life measures and treatment with a medical and/or surgical intervention may be warranted based on symptoms (Mama, 2018). A survey of over 4,000 women found that women who first experienced symptoms in their adolescence waited on average three times longer to seek help and had longer intervals from the time of seeking help to getting a diagnosis than those who experienced first symptoms as adults (Greene, Stratton, Cleary, Ballweg, & Sinaii, 2009). These delays are consistent with other findings (Soliman, Fuldeore, & Snabes, 2017). Type of provider also has a role in timing of diagnosis. Women who seek help from a primary provider or general practitioner have shown longer times to diagnosis (Greene et al., 2009). Another study found that obstetricians/gynecologists are more likely to diagnose patients earlier than non-obstetrician/gynecologists (Soliman et al., 2017). Most research in this area focuses on averages of time to diagnosis, but do not compare times to diagnosis across race, ethnicity, or SES.
Delays in diagnosis have potentially harmful results. Prolonging the time to diagnosis may increase the period of suffering as women search for a diagnosis of endometriosis. Treatment delays may also affect the progression of pain over time. Neurogenesis occurring within the highly vascularized endometriotic lesions are recognized as a contributor to endometriosis pain. An increased burden of nerve pain fibers may activate accelerated pain pathways in the peripheral and central nervous system (Stratton & Berkley, 2011). This nervous system ‘sensitization’ combined with a protracted time to diagnosis may increase the risk of developing chronic pelvic pain (CPP) and abnormal pain referral patterns (Aredo, Heyrana, Karp, Shah, & Stratton, 2017; Bajaj, Bajaj, Madsen, & Arendt-Nielsen, 2003; Stratton & Berkley, 2011; Vuontisjarvi et al., 2018)
There are also financial implications with a reduction of work productivity when women are symptomatic and direct healthcare costs that accumulate as they seek professional help. In 2018, one study estimated the mean adjusted direct healthcare costs of those with endometriosis to be approximately $10,000 per year (Soliman, Surrey, Bonafede, Nelson, & Castelli-Haley, 2018). Nnoaham et al. (2011) found an average loss of work productivity of 10.8 hours per week across 10 countries. To our knowledge, no studies have mapped how delay in diagnosis impacts women’s symptom progression or the effect on their symptom management and help-seeking on the path to diagnosis. This protocol presents a study focused on the timing of diagnosis with symptom progression and how personal financial costs influence a woman’s decision and resources to seek help.
On the medical and system levels, unanswered questions surrounding pathogenesis, pathology and progression of endometriosis persist and create confusion for women and health care providers. The complexity and ambiguity of symptom presentation, with many symptoms shared with other chronic conditions, makes symptom reporting and diagnosis challenging. Diagnosis is further complicated by high rates of comorbidities among women with endometriosis such as pelvic inflammatory disorder, interstitial cystitis, irritable bowel syndrome, autoimmune and endocrine disorders, fibromyalgia and chronic fatigue syndrome (Sinaii, Cleary, Ballweg, Nieman, & Stratton, 2002; Surrey et al., 2018). These barriers, a representative few, contribute to misdiagnoses and delayed diagnoses resulting in repetitive cycling through symptom recognition, assessment and help-seeking. The research in this protocol, grounded in the life course perspective (G. H. Elder & Giele, 2009), will help better understand the pre-diagnostic period among women with endometriosis—including social and environmental influences—and identify barriers to diagnosis of a diverse group of women.
Theoretical Framework
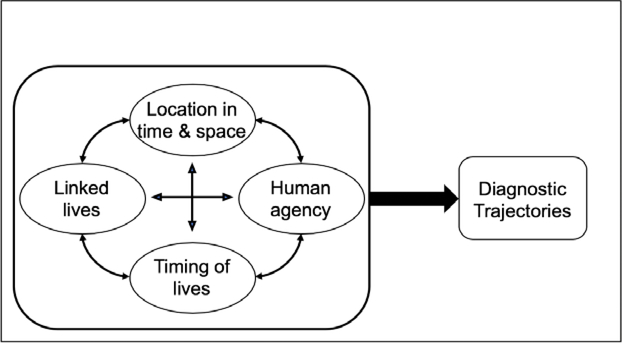
The long-term struggle and impact of endometriosis has implications across the lifespan. As a result, this protocol applies a life course approach. The life course perspective views women as active beings in dynamic systems where they are shaped by: 1) their location in time and space (culture); 2) linked lives (social integration); 3) human agency (individual goals); and 4) the time of their lives (intersection of age, period and cohort) (G. H. Elder & Giele, 2009; G. H. Elder, Johnson, & Crosnoe, 2003; G. H. Elder, Jr., 1998; Giele & Elder, 1998; Mortimer & Shanahan, 2003; Wethington, 2005). First, the woman’s location in time and space sets the context and culture of their development (Giele & Elder, 1998). This is heavily influenced by factors such as SES, race, gender, and social norms (Wethington, 2005). This design considers how women’s perceptions of the influence of culture and context through the continua of their lives influenced their symptom recognition, assessment and management and help-seeking. The linked lives concept speaks to the socialization and interactions of the women on every level (e.g., work, networks, family and friends) (Giele & Elder, 1998). For example, qualitative studies have found that mothers, family and friends influenced how the women assessed their symptoms by normalizing their experiences or stigmatizing the women and leading to delays in help-seeking and diagnosis (Denny, 2004a; Seear, 2009). The human agency element involves the goals of the individual as seen through decision-making and life pursuits (Giele & Elder, 1998). The women’s goals can motivate their decision-making and help-seeking (e.g., career and fertility). Finally, the timing of their lives is a dynamic concept where the women’s decisions are influenced by the timing of events in their lives and the time when they live (Giele & Elder, 1998). A woman’s development, health outcomes and pathway to diagnosis are shaped by these four concepts and the interplay in the woman’s life course. Furthermore, time plays its own part in the accumulation of challenges influencing the life course. The life course perspective suggests that the accrual of adverse events (environment, conditions, behaviors) increases the risk of chronic illness (Kuh & Ben-Shlomo, 2004). Figure 1 presents the proposed modified life course framework specific to endometriosis diagnosis grounded in Giele & Elder’s (1998) work. This framework guides the interviews and qualitative analysis to map the diagnostic trajectories experienced by a diverse sample of women in this protocol.
Figure 1.
Proposed modified life course framework for delayed diagnosis of endometriosis
The Study
Aims
The primary purpose of the study is to examine the pre-diagnostic period of a diverse sample of women diagnosed with endometriosis through a life course perspective. This is accomplished by mapping participant pathways to diagnosis using qualitative interviews and analysis informed by a life course perspective. The study will do this by (1) describing pathways and experiences of the women’s symptom recognition, appraisal and management; and (2) identifying differences in pathways and experiences among a socioeconomically and racially diverse groups of women.
Design and Methodology
This project will map the pathways to diagnosis of endometriosis for a socioeconomically and racially/ethnically diverse group of women using qualitative interviews and analysis informed by a life course perspective. Using a descriptive qualitative design, the investigators will purposefully sample a minimum of 24 women diagnosed with endometriosis. The study will oversample Black and Hispanic/Latina women and lower SES women of all three race/ethnic groups to achieve a diverse sample. Furthermore, we provide interviews in English and Spanish to increase inclusiveness of Hispanic/Latina participants.
Sample and Setting
The investigators will use stratified purposeful sampling to recruit a minimum of 24 adult women who have received diagnoses of endometriosis—surgically confirmed or provider-presumed (Patton, 2002; Sandelowski, 1995b, 2000). We defined provider-presumed as when a participant did not have a surgery to confirm the diagnosis, but their provider provisionally diagnosed them with endometriosis based on symptom history and response to treatment. The base sample size was estimated to fit the defined strata goals while achieving information saturation (Sandelowski, 1995b, 2000). The sample size will be expanded if we do not achieve information saturation. The goal of the stratification is to achieve even distribution across diverse SES and race/ethnicity groups to describe previously unrevealed differences among women’s pathways to diagnosis. The participants will be sampled in equal numbers across six groups making up the race/ethnicity and SES categories. The sample size and numbers across the races/ethnicities will be a foundation for hypotheses building and further research. The inclusion criteria are: (a) female; (b) age ≥18 years; (c) able to speak and understand English or Spanish; (d) diagnosed with endometriosis (surgically confirmed or provider-presumed); and (e) non-Hispanic Black, non-Hispanic White or Hispanic/Latina. There are no additional exclusion criteria.
Women will be recruited from secondary (ob/gyn clinic) and tertiary care (gynecologic surgical clinic) facilities at a large public hospital in the southeastern U.S. The medical center offers an assistance program for patients at or below 250% of the Federal Poverty Guidelines. The interviews will occur in-person or via telephone depending on participant preference and safety guidelines in light of the pandemic.
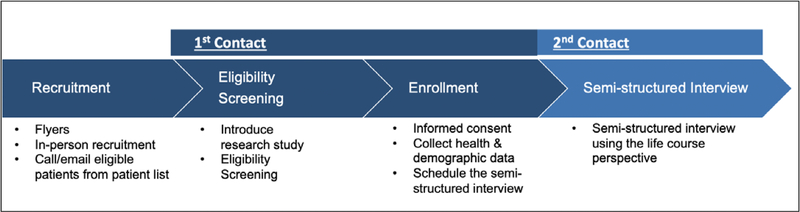
Data collection
Data will be collected in two points of contact with the participants (see Figure 2) and are grouped as four types of data: (1) eligibility screening; (2) demographic data; (3) background/health data; and (4) semi-structured interview. The eligibility screening will consist of questions to satisfy the inclusion criteria and the stratified sampling plan: (a) sex; (b) age; (c) speaks and understands English or Spanish; (d) diagnosed with endometriosis (surgically confirmed or presumed by doctor); (e) SES (education attainment); and (f) self-declared race and ethnicity. The participants will be asked to identify diagnosis (surgically confirmed or presumed by doctor) and diagnosis will be confirmed with their medical record. For eligibility screening, SES will be determined by highest education level attained. Those with some college or more will be categorized as “Higher SES” and those with less than college will be categorized as “Lower SES.” Educational attainment, as a proxy for SES, reflects early life circumstances, life transitions and adult resources making it ideal for life course grounded research (B. Galobardes, Lynch, & Smith, 2007; Bruna Galobardes, Shaw, Lawlor, Smith, & Lynch, 2006). The women will also be asked to self-identify race and ethnicity. Non-Hispanic Whites make up about 63% of the local population according to the 2010 U.S. Census. However, this study will oversample non-Hispanic Black and Hispanic/Latina women since they have been underrepresented in previous qualitative endometriosis studies. People of Hispanic ethnicity may self-identify with any racial group and sometimes identify their Hispanic or Latina ethnicity as a race (Parker, Horowitz, Morin, & Lopez, 2015). For the purposes of this study, anyone self-identifying as Hispanic or Latina, regardless of race chosen, will be categorized as Hispanic/Latina for sampling stratification. If the participant fulfills the eligibility requirements, the first contact will progress to enrollment and collection of demographic and health information.
Figure 2.
Study procedure
The demographic data will include the information gathered in the screening (i.e., sex, age, race, ethnicity, education) and expand in detail. The investigators will inquire about income, health coverage, employment status, marital status and family structure from the participants’ past and present. For example, questions regarding health coverage will span from childhood to the present, emphasizing points of change in coverage. The health history will focus on menstruation history, symptoms (e.g., timing and progression), healthcare providers, different diagnoses, date of diagnosis of endometriosis and treatments.
The semi-structured interview will follow an interview guide ensuring central issues identified in the literature will be addressed consistently using a life course perspective. The life course perspective provides the conceptual underpinning of the interview guide (see Theoretical Framework). The four life course concepts with their operational definition and example interview questions for the semi-structured interviews can be seen in Table 1. The interview questions will elicit data about the life course of the participant as it relates to endometriosis. The interview will start with an introductory question: “Tell me when you noticed the first sign that something might be different or wrong.” The interviewer and participant will work backwards and forwards from that point to fill in the participant’s life course in relationship to their menstruation, symptom development, health management and help seeking. The questions will start more generally, and probing questions will be posed to gain more detail.
Table 1.
Modified Life course model variables and Interview Questions.
| Life Course Concepts | Definition of Life Course Concept applied to Endometriosis | Example Interview Questions |
|---|---|---|
| Location in Time and Space | Culture and context (including gender, SES and race) impacting women’s symptom recognition, assessment and management and help-seeking. | • Tell me when you noticed the first sign that something might be different or wrong. • What was the first time you remember anyone talking to you about your periods or your female health? • Were you aware of others experiencing similar symptoms? • Did you talk to anyone about your early symptoms and what do you remember them saying about your symptoms or how you should manage them? |
| Linked Lives | The interaction of women with others and socialization influencing their symptom recognition, assessment and management and help-seeking. | • How did others influence the way you assessed your symptoms? • Who was most influential to how you saw your symptoms? • Have your symptoms had an effect on personal relationships? |
| Human Agency | The goals of the individual and the effect on their decision-making and life pursuits as they relate to their symptom recognition, assessment and management and help-seeking. | Think about what you wanted for yourself as a child, teenager, and adult. • How did your symptoms impact your goals for your life? • How did your goals impact what you did about your symptoms? • How did your goals factor into whether you went to see a doctor about your symptoms? |
| Time of their Lives | Choices made in their lives regarding symptom recognition, assessment, management and help-seeking are influenced by the time in which they live and the timing of events in their lives as they relate to their goals. | • Tell me how your symptoms have changed over time. • How has the way you manage your symptoms changed throughout your life? • What did you think about the timing of your diagnosis and the amount of time it took to get a diagnosis? |
It is the priority of the research team to include Spanish-speaking participants in this study. As a result, all of the recruitment materials, consent forms, scripts, questionnaires and interview guides will be translated to Spanish using forward and backward translation by independent, professional translators (Beaton, Bombardier, Guillemin, & Ferraz, 2000) and a Spanish-speaking researcher will be available for participants preferring Spanish.
Procedures
Figure 2 outlines the proposed study’s progression and participant contacts. Data will be collected across two contacts with participants: (1) first contact with eligibility screening and enrollment (demographic and health information); and (2) individual, semi-structured qualitative interview using an interview guide. All elements of data collection can occur via telephone or in-person to increase participant choice. All participant contact can occur in Spanish or English.
Recruitment will use three means of contact: flyers, in-person and identifying potentially eligible participants from clinic patient lists. The first author will search the EMR for women at least 18 years with an endometriosis diagnosis (surgically confirmed or provider-presumed). Potentially eligible participants identified in the patient list will be contacted via email or phone with an Institutional Review Board (IRB)-approved email/script. Second, the first author will be at the recruitment sites on predetermined days to recruit in-person. Finally, IRB-approved study flyers will be posted in the exam rooms and nurses will be asked to distribute additional flyers to patients. The flyers will provide basic information about the study including the purpose, process, participant time investment and study contact information. The flyers will be provided in Spanish and English and the email addresses and phone numbers on the respective flyers will lead to a Spanish- or English-speaking researcher. Interested potential participants can contact the researchers by phone or email. Potential participants who were identified from the EMR or who indicated interest will be called to screen for eligibility.
In the first contact, the recruiters will introduce the study with an IRB-approved script, answer the individual’s questions and ask if the individual is still interested in participating. If they are, the eligibility screening will be performed (see Data collection). If the potential participants meet the screening criteria and agree to participate in all phases of the proposed study, they will be asked for verbal informed consent. The informed consent and HIPAA release forms will be mailed with duplicate copies for the participant and a stamped return envelope to return signed copies.
After verbal informed consent is obtained during the first contact, data collection will focus on demographic and health information. The questions to acquire demographic and health information will be structured and closed-ended. They will follow a predetermined questionnaire. Once these data are gathered, the investigators will schedule the semi-structured interview with the participant. The time and location will be determined to maximize safety and convenience for the participant and minimize burden.
Interviews will concentrate on the participants’ experiences during their pathways to diagnoses through the course of their lives and will elicit the data needed to address the research aims. The first author will review the participants’ answers to the eligibility screening, demographic questions and background questions prior to the first interviews to familiarize herself with the participants’ situations. The semi-structured interview guide (see Data Collection) will ensure the investigator obtains key data pertinent to the study aims. The interviews will be conversational in approach and the interviewer will encourage participants to follow trains of thought, elaborate on their experiences and introduce topics not in the guide. Audio recordings of the interviews will be transcribed verbatim by a professional transcriptionist and checked for accuracy. Transcribed interviews in Spanish will be professionally translated to English in the data preparation phase, prior to coding or analysis (Lopez, Figueroa, Connor, & Maliski, 2008; H. P. Santos, Jr., Black, & Sandelowski, 2015).
Data Analysis
The demographic questions will be analyzed using descriptive statistics to characterize the sample. The interview transcripts will be imported into Atlas.ti after verification, where they will be coded and analyzed for common themes and distinctions using directed content analysis. Coding will be completed by two independent coders who will discuss differences in their applications of codes to reach consensus. Analysis will entail inspection of all data related to single codes or subsets of codes using constant comparison (Patton, 2002; Sandelowski & Barroso, 2007). The semi-structured interview guide and the life course perspective on which it is based (see Theoretical Framework), will provide the initial organizing structure for coding interviews (Sandelowski, 1995a). The coders will code the interviews independently using the codebook (Creswell, 2013). Intercoder reliability will be checked by having the coders code the same selected portions of interviews (Creswell, 2013). A life course/diagnosis pathway case summary will be created for each woman to avoid the reductionist quality of coding, foster intimacy with the data, assist with analytic insight and provide context for the women’s pathways (Knafl & Ayres, 1996). The investigators will complete within- and across-case analyses addressing the four life course concepts to provide a thorough mapping of participant pathways to diagnosis of endometriosis (Ayres, Kavanaugh, & Knafl, 2003). The data collected in the health questionnaire and the semi-structured interview will combine to form the diagnosis map. The maps of the pathways to diagnosis will reconstruct the participants’ life courses in relationship to their endometriosis.
Ethical considerations
Institutional Review Board (IRB) approval was obtained from the host university in June 2019 and subsequently from the hospital’s Nursing Research Council. Data collection will occur November 2019-December 2020. To reduce burden, the study plans to recruit and data-collect over the telephone and in-person. If the participant is recruited in person at a clinic, they will be approached in a private exam room. They will have adequate time to ask questions and review the material. They can agree to participate then or take the material with them to consider. If they are interested in participating, they will be asked to sign written copies of the informed consent form and HIPAA authorization. They will receive copies of the consent form and HIPAA authorization. If the participant is recruited over the phone, the women will be encouraged to find a location to speak in private. We will complete an IRB pre-approved verbal consent procedure prior to completing the questionnaires. Again, they will be encouraged to ask questions and voice concerns. If they are willing to share their mailing address, we can mail the consent form and HIPAA authorization forms with a copy for their records and a pre-stamped envelope to return a signed copy. They will be encouraged to call the recruiter with questions. In all cases, the consent will be affirmed at the beginning of the interviews. An email option is also available with an IRB-approved electronic consent at the beginning of the online questionnaires. Participants will have several options to provide consent and complete the study to maximize safety and privacy. The researchers will offer incentives in the form of prepaid gift cards to compensate participants for their time.
The investigators will take measures to protect the participants’ anonymity and data. Participants will be randomly assigned a unique participant identification number (PIN) using a computer-generated list of random numbers. All sources of material and data collected will be identified by the participant’s unique PIN, not by their name or other personal identifier. The list linking participant names and IDs will be securely stored separately from the study data. The computerized data will not include any personal identifiers and will only be identified by the PIN. All digital records will be downloaded from the recording device immediately after the data collection, named by the PIN and stored in the university’s secure network drive (Secure NAS). Once the download is determined to be audible and saved, the digital recording will be erased from the recording device. The interviews will be transcribed verbatim with the transcript file named by PIN. Once the transcription has been verified, the audio file will be destroyed.
Since this study is accessing a small sample and asking intimate life details, extra effort will be made to protect the privacy and confidentiality during dissemination. This includes, but is not limited to, using only de-identified data, reporting generalized demographics when using a direct quote and cleaning examples or reports of any information that might identify an individual.
Rigour
Rigor and reproducibility are addressed in the proposed study through its design described in the above narrative sections. First, the questionnaire and interview questions will be tested and refined with the first four participants to ensure their acceptability and relevance for participants. Second, the Spanish-translated recruitment flyers, emails, script and interview guide will undergo forward and backward translation by independent translators and will be IRB approved. Third, the data analysis procedure was established before the data collection and includes checks on the coding process and use of well-established analytic techniques. Finally, the results will be reported consistent with the Standards for Reporting Qualitative Research (O’Brien, Harris, Beckman, Reed, & Cook, 2014).
Discussion
The purpose of the study described in this protocol is to better understand women’s pathways to diagnosis of endometriosis. Other research has studied timing and delay in the diagnosing of endometriosis. Quantitative studies typically focus on the amount of time from first symptoms to diagnosis or contributing factors to the timing such as specialty of the first provider seen or age at the time of the first symptom (Dmowski, Lesniewicz, Rana, Pepping, & Noursalehi, 1997; Greene et al., 2009; Hadfield et al., 1996; Hudelist et al., 2012; Husby, Haugen, & Moen, 2003; T. M. Santos et al., 2012; Soliman et al., 2017; Staal et al., 2016). Qualitative studies have interviewed women about their experiences getting a diagnosis, identifying themes such as contributing factors, provider interactions, diagnosis meaning, help-seeking and family or social interactions (Ballard et al., 2006; Denny, 2004b; Manderson, Warren, & Markovic, 2008; Riazi et al., 2014). These works have furthered knowledge surrounding women’s pathways to diagnosis with unique information.
The study described in this protocol will undoubtedly share themes with the above works, but it stands to fill in gaps through its unique approach. The variety of subjects in the described study means a more robust understanding of women’s experiences in their search for a diagnosis. Additionally, we will speak with the women about their experiences across their life courses and consider how their pathways are influenced by their environments, relationships and communities (among other factors). Framing the women as dynamic beings in complex systems will help create a more complete picture of influencing factors on pathways to diagnosis. This study answers the call by Bougie, Healey and Singh (2019) for endometriosis research with a more diverse sample focused on women’s experiences with help-seeking and their pathway to diagnosis. The results of this work will outline an agenda for future research and identify points of intervention to streamline pathways to diagnosis of endometriosis.
The 2020 coronavirus pandemic began shortly after recruitment and data collection for this study commenced. Its spread to the U.S. caused in-person recruitment and data collection to stop and an adjustment in the means of contact to protect the participants and the researchers. Under the guidance of the IRB, all recruitment and data collection have transitioned to email and telephone methods. We maintain the original aims and procedures previously described, but the changes are lengthening the original timeline. It might also impact the pathways of women seeking help during the pandemic and raise new themes in the interviews.
Limitations
This proposed project’s sampling requires endometriosis diagnosis—surgically confirmed or provider-presumed. Diagnosis criteria for sample inclusion proves challenging when researching endometriosis due to inherent difficulties of diagnosis. By including the provider-presumed diagnoses, this project will sample from a broader base and include those who do not have access to surgical confirmation. Although there is a potential for including women who do not have a confirmed diagnosis of endometriosis, this risk is lessened by the fact that recruitment occurs at tertiary and secondary treatment facilities.
There are populations this study will not sample such as those not under medical care, women who do not self-identify as White, Black or Hispanic/Latina and those who do not speak English or Spanish. The race/ethnicity groups and languages were chosen to achieve representation of the most common racial/ethnic groups in the catchment area based on data from the U.S. census. Including women in endometriosis research who have not presented for medical care continues to be a challenge and their experiences would greatly further research in pathways to diagnosis of endometriosis. However, this study focuses on the pathway through diagnosis, which requires presentation for medical care. A future study focused on symptom assessment and help-seeking among women who have not sought medical care would be valuable.
Conclusion
Globally, women face overwhelming obstacles to receiving a diagnosis of endometriosis. These barriers contribute to misdiagnoses and delayed diagnoses resulting in repetitive cycling through symptom recognition, assessment and help-seeking. The study described in this protocol, grounded in the life course perspective, will help better understand the pre-diagnostic period among women with endometriosis—including social and environmental influences—and identify barriers to diagnosis of a diverse group of women. It will greatly advance the limited knowledge of the pathways to diagnosis of endometriosis among under-represented populations and identify areas for future research and intervention with the goal to reduce women’s times to diagnosis.
Acknowledgments
Funding Statement: This research is supported by the National Institute of Nursing Research of the National Institutes of Health under award number F31NR018786 (Cromeens, PI), a UNC Dissertation Completion Fellowship, and a 2019 Sigma Small Grant by Sigma Theta Tau International (STTI #19–2191). Ms. Cromeens is also a Virginia Kelley Scholar of the American Nurses Foundation, a Linda Waring Matthews Research Scholar, 2019–2020, and a Hillman Scholar in Nursing Innovation at the School of Nursing at the University of North Carolina at Chapel Hill. This study also received funding from the Hillman Scholars Program in Nursing Innovation through the “Interdisciplinary Inquiry” and the “Advancing Early Research Opportunities” grants. Dr. Robinson’s research, “Racial differences in treatment with hysterectomy: A multilevel investigation,” is supported by the National Institute on Minority Health and Health Disparities of the National Institutes of Health under award number R01MD011680 (Robinson, PI).
Footnotes
Anonymised Conflict of Interest Statement
“No conflict of interest has been declared by the authors”
References
- Adamson GD, Kennedy S, & Hummelshoj L (2010). Creating Solutions in Endometriosis: Global Collaboration through the World Endometriosis Research Foundation. Journal of Endometriosis, 2(1), 3–6. doi: 10.1177/228402651000200102 [DOI] [Google Scholar]
- American College of Obstetricians and Gynecologists. (2018). ACOG Committee Opinion No. 760 Summary: Dysmenorrhea and Endometriosis in the Adolescent. Obstet Gynecol, 132(6), 1517–1518. doi: 10.1097/aog.0000000000002981 [DOI] [PubMed] [Google Scholar]
- Andersen BL, & Cacioppo JT (1995). Delay in seeking a cancer diagnosis: delay stages and psychophysiological comparison processes. Br J Soc Psychol, 34 (Pt 1), 33–52. [DOI] [PubMed] [Google Scholar]
- Aredo JV, Heyrana KJ, Karp BI, Shah JP, & Stratton P (2017). Relating Chronic Pelvic Pain and Endometriosis to Signs of Sensitization and Myofascial Pain and Dysfunction. Semin Reprod Med, 35(1), 88–97. doi: 10.1055/s-0036-1597123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- As-Sanie S, Black R, Giudice LC, Gray Valbrun T, Gupta J, Jones B, … Nebel RA (2019). Assessing research gaps and unmet needs in endometriosis. Am J Obstet Gynecol, 221(2), 86–94. doi: 10.1016/j.ajog.2019.02.033 [DOI] [PubMed] [Google Scholar]
- Ayres L, Kavanaugh K, & Knafl KA (2003). Within-case and across-case approaches to qualitative data analysis. Qual Health Res, 13(6), 871–883. doi: 10.1177/1049732303013006008 [DOI] [PubMed] [Google Scholar]
- Bajaj P, Bajaj P, Madsen H, & Arendt-Nielsen L (2003). Endometriosis is associated with central sensitization: a psychophysical controlled study. J Pain, 4(7), 372–380. [DOI] [PubMed] [Google Scholar]
- Ballard K, Lowton K, & Wright J (2006). What’s the delay? A qualitative study of women’s experiences of reaching a diagnosis of endometriosis. Fertil Steril, 86(5), 1296–1301. doi: 10.1016/j.fertnstert.2006.04.054 [DOI] [PubMed] [Google Scholar]
- Beaton DE, Bombardier C, Guillemin F, & Ferraz MB (2000). Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976), 25(24), 3186–3191. [DOI] [PubMed] [Google Scholar]
- Bougie O, Healey J, & Singh SS (2019). Behind the Times: Revisiting Endometriosis and Race. Am J Obstet Gynecol. doi: 10.1016/j.ajog.2019.01.238 [DOI] [PubMed] [Google Scholar]
- Creswell JW (2013). Qualitative inquiry & research design : choosing among five approaches (3rd ed.). Los Angeles: SAGE Publications. [Google Scholar]
- Culley L, Law C, Hudson N, Denny E, Mitchell H, Baumgarten M, & Raine-Fenning N (2013). The social and psychological impact of endometriosis on women’s lives: a critical narrative review. Hum Reprod Update, 19(6), 625–639. doi: 10.1093/humupd/dmt027 [DOI] [PubMed] [Google Scholar]
- Denny E (2004a). Women’s experience of endometriosis. J Adv Nurs, 46(6), 641–648. doi: 10.1111/j.1365-2648.2004.03055.x [DOI] [PubMed] [Google Scholar]
- Denny E (2004b). ‘You are one of the unlucky ones’: delay in the diagnosis of endometriosis. Diversity in Health & Social Care, 1(1), 39–44. Retrieved from https://auth.lib.unc.edu/ezproxy_auth.php?url=http://search.ebscohost.com/login.aspx?direct=true&db=rzh&AN=106377962&site=ehost-live&scope=site [Google Scholar]
- Dmowski WP, Lesniewicz R, Rana N, Pepping P, & Noursalehi M (1997). Changing trends in the diagnosis of endometriosis: a comparative study of women with pelvic endometriosis presenting with chronic pelvic pain or infertility. Fertil Steril, 67(2), 238–243. doi: 10.1016/s0015-0282(97)81904-8 [DOI] [PubMed] [Google Scholar]
- Elder GH, & Giele JZ (2009). Life course studies: An evolving field. In Elder GH & Giele JZ (Eds.), The Craft of Life Course Research. New York, NY: The Guilford Press. [Google Scholar]
- Elder GH, Johnson MK, & Crosnoe R (2003). The emergence and development of life course theory. In Mortimer JT & Shanahan MJ (Eds.), Handbook of the Life Course (pp. 3–22). New York, NY: Kluwer Academic/Plenum Publishers. [Google Scholar]
- Elder GH Jr. (1998). The life course as developmental theory. Child Dev, 69(1), 1–12. [PubMed] [Google Scholar]
- Fourquet J, Zavala DE, Missmer S, Bracero N, Romaguera J, & Flores I (2019). Disparities in healthcare services in women with endometriosis with public vs private health insurance. Am J Obstet Gynecol, 221(6), 623.e621–623.e611. doi: 10.1016/j.ajog.2019.06.020 [DOI] [PubMed] [Google Scholar]
- Fuldeore MJ, & Soliman AM (2017). Prevalence and Symptomatic Burden of Diagnosed Endometriosis in the United States: National Estimates from a Cross-Sectional Survey of 59,411 Women. Gynecol Obstet Invest, 82(5), 453–461. doi: 10.1159/000452660 [DOI] [PubMed] [Google Scholar]
- Galobardes B, Lynch J, & Smith GD (2007). Measuring socioeconomic position in health research. Br Med Bull, 81–82, 21–37. doi: 10.1093/bmb/ldm001 [DOI] [PubMed] [Google Scholar]
- Galobardes B, Shaw M, Lawlor DA, Smith GD, & Lynch J (2006). Indicators of socioeconomic position. In Oakes JM & Kaufman JS (Eds.), Methods in Social Epidemiology (1st ed., pp. 47–85). San Francisco: Jossey-Bass. [Google Scholar]
- Giele JZ, & Elder GH (1998). Life course research: Development of a field. In Giele JZ & Elder GH (Eds.), Methods of Life Course Research: Qualitative and Quantitative Approaches (pp. 5–27). London: Sage Publications. [Google Scholar]
- Giudice LC, & Kao LC (2004). Endometriosis. Lancet, 364(9447), 1789–1799. doi: 10.1016/s0140-6736(04)17403-5 [DOI] [PubMed] [Google Scholar]
- Greene R, Stratton P, Cleary SD, Ballweg ML, & Sinaii N (2009). Diagnostic experience among 4,334 women reporting surgically diagnosed endometriosis. Fertil Steril, 91(1), 32–39. doi: 10.1016/j.fertnstert.2007.11.020 [DOI] [PubMed] [Google Scholar]
- Hadfield R, Mardon H, Barlow D, & Kennedy S (1996). Delay in the diagnosis of endometriosis: a survey of women from the USA and the UK. Hum Reprod, 11(4), 878–880. [DOI] [PubMed] [Google Scholar]
- Hudelist G, Fritzer N, Thomas A, Niehues C, Oppelt P, Haas D, … Salzer, H. (2012). Diagnostic delay for endometriosis in Austria and Germany: causes and possible consequences. Hum Reprod, 27(12), 3412–3416. doi: 10.1093/humrep/des316 [DOI] [PubMed] [Google Scholar]
- Husby GK, Haugen RS, & Moen MH (2003). Diagnostic delay in women with pain and endometriosis. Acta Obstet Gynecol Scand, 82(7), 649–653. [DOI] [PubMed] [Google Scholar]
- Kinkel K, Brosens J, & Brosens I (2006). Preoperative Investigations. In Sutton C, Jones K, & Adamson GD (Eds.), Modern Management of Endometriosis (pp. 71–85). London, England: Taylor and Francis Group. [Google Scholar]
- Knafl KA, & Ayres L (1996). Managing large qualitative data sets in family research. Journal of Family Nursing, 2(4), 350–364. Retrieved from https://auth.lib.unc.edu/ezproxy_auth.php?url=http://search.ebscohost.com/login.aspx?direct=true&db=rzh&AN=107321795&site=ehost-live&scope=site [Google Scholar]
- Kuh D, & Ben-Shlomo Y (2004). Introduction. In Kuh D & Ben-Shlomo Y (Eds.), A life course approach to chronic disease epidemiology (Second ed.). Oxford: Oxford University Press. [Google Scholar]
- Lopez GI, Figueroa M, Connor SE, & Maliski SL (2008). Translation barriers in conducting qualitative research with Spanish speakers. Qual Health Res, 18(12), 1729–1737. doi: 10.1177/1049732308325857 [DOI] [PubMed] [Google Scholar]
- Mama ST (2018). Advances in the management of endometriosis in the adolescent. Curr Opin Obstet Gynecol, 30(5), 326–330. doi: 10.1097/gco.0000000000000483 [DOI] [PubMed] [Google Scholar]
- Manderson L, Warren N, & Markovic M (2008). Circuit breaking: pathways of treatment seeking for women with endometriosis in Australia. Qual Health Res, 18(4), 522–534. doi: 10.1177/1049732308315432 [DOI] [PubMed] [Google Scholar]
- Mortimer JT, & Shanahan MJ (Eds.). (2003). Handbook of the Life Course. New York, NY: Kluwer Academic/Plenum Publishers. [Google Scholar]
- National Institutes of Health. (2020). Estimates of Funding for Various Research, Condition and Disease Categories (RCDC). Retrieved from https://report.nih.gov/categorical_spending.aspx
- Nnoaham KE, Hummelshoj L, Webster P, d’Hooghe T, de Cicco Nardone F, de Cicco Nardone C, … Zondervan KT (2011). Impact of endometriosis on quality of life and work productivity: a multicenter study across ten countries. Fertil Steril, 96(2), 366–373.e368. doi: 10.1016/j.fertnstert.2011.05.090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Brien BC, Harris IB, Beckman TJ, Reed DA, & Cook DA (2014). Standards for reporting qualitative research: a synthesis of recommendations. Acad Med, 89(9), 1245–1251. doi: 10.1097/acm.0000000000000388 [DOI] [PubMed] [Google Scholar]
- Parker K, Horowitz JM, Morin R, & Lopez MH (2015). Chapter 7: The Many Dimensions of Hispanic Racial Identity Pew Research Center: Social & Demographic Trends. Retrieved from http://www.pewsocialtrends.org/2015/06/11/chapter-7-the-many-dimensions-of-hispanic-racial-identity/
- Patton MQ (2002). Qualitative research and evaluation methods. Thousand Oaks, Calif.: Sage Publications. [Google Scholar]
- Riazi H, Tehranian N, Ziaei S, Mohammadi E, Hajizadeh E, & Montazeri A (2014). Patients’ and physicians’ descriptions of occurrence and diagnosis of endometriosis: a qualitative study from Iran. BMC Womens Health, 14, 103. doi: 10.1186/1472-6874-14-103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandelowski M (1995a). Qualitative analysis: what it is and how to begin. Res Nurs Health, 18(4), 371–375. [DOI] [PubMed] [Google Scholar]
- Sandelowski M (1995b). Sample size in qualitative research. Res Nurs Health, 18(2), 179–183. [DOI] [PubMed] [Google Scholar]
- Sandelowski M (2000). Combining qualitative and quantitative sampling, data collection and analysis techniques in mixed-method studies. Res Nurs Health, 23(3), 246–255. [DOI] [PubMed] [Google Scholar]
- Sandelowski M, & Barroso J (2007). Constant Targeted Comparison. In Handbook for Synthesizing Qualitative Research (pp. 201–204). New York, NY: Springer Publishing Company. [Google Scholar]
- Santos HP Jr., Black AM, & Sandelowski M (2015). Timing of translation in cross-language qualitative research. Qual Health Res, 25(1), 134–144. doi: 10.1177/1049732314549603 [DOI] [PubMed] [Google Scholar]
- Santos TM, Pereira AM, Lopes RG, & Depes Dde B (2012). Lag time between onset of symptoms and diagnosis of endometriosis. Einstein (Sao Paulo), 10(1), 39–43. [DOI] [PubMed] [Google Scholar]
- Seear K (2009). The etiquette of endometriosis: stigmatisation, menstrual concealment and the diagnostic delay. Soc Sci Med, 69(8), 1220–1227. doi: 10.1016/j.socscimed.2009.07.023 [DOI] [PubMed] [Google Scholar]
- Sinaii N, Cleary SD, Ballweg ML, Nieman LK, & Stratton P (2002). High rates of autoimmune and endocrine disorders, fibromyalgia, chronic fatigue syndrome and atopic diseases among women with endometriosis: a survey analysis. Hum Reprod, 17(10), 2715–2724. [DOI] [PubMed] [Google Scholar]
- Soliman AM, Fuldeore M, & Snabes MC (2017). Factors Associated with Time to Endometriosis Diagnosis in the United States. J Womens Health (Larchmt), 26(7), 788–797. doi: 10.1089/jwh.2016.6003 [DOI] [PubMed] [Google Scholar]
- Soliman AM, Surrey E, Bonafede M, Nelson JK, & Castelli-Haley J (2018). Real-World Evaluation of Direct and Indirect Economic Burden Among Endometriosis Patients in the United States. Adv Ther, 35(3), 408–423. doi: 10.1007/s12325-018-0667-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staal AH, van der Zanden M, & Nap AW (2016). Diagnostic Delay of Endometriosis in the Netherlands. Gynecol Obstet Invest, 81(4), 321–324. doi: 10.1159/000441911 [DOI] [PubMed] [Google Scholar]
- Stratton P, & Berkley KJ (2011). Chronic pelvic pain and endometriosis: translational evidence of the relationship and implications. Hum Reprod Update, 17(3), 327–346. doi: 10.1093/humupd/dmq050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surrey ES, Soliman AM, Johnson SJ, Davis M, Castelli-Haley J, & Snabes MC (2018). Risk of Developing Comorbidities Among Women with Endometriosis: A Retrospective Matched Cohort Study. J Womens Health (Larchmt), 27(9), 1114–1123. doi: 10.1089/jwh.2017.6432 [DOI] [PubMed] [Google Scholar]
- Vuontisjarvi S, Rossi HR, Herrala S, Morin-Papunen L, Tapanainen JS, Karjula S, … Piltonen TT (2018). The Long-Term Footprint of Endometriosis: Population-Based Cohort Analysis Reveals Increased Pain Symptoms and Decreased Pain Tolerance at Age 46 Years. J Pain, 19(7), 754–763. doi: 10.1016/j.jpain.2018.02.005 [DOI] [PubMed] [Google Scholar]
- Wethington E (2005). An overview of the life course perspective: implications for health and nutrition. J Nutr Educ Behav, 37(3), 115–120. [DOI] [PubMed] [Google Scholar]
- Young K, Fisher J, & Kirkman M (2015). Women’s experiences of endometriosis: a systematic review and synthesis of qualitative research. J Fam Plann Reprod Health Care, 41(3), 225–234. doi: 10.1136/jfprhc-2013-100853 [DOI] [PubMed] [Google Scholar]
- Zondervan KT, Becker CM, & Missmer SA (2020). Endometriosis. N Engl J Med, 382(13), 1244–1256. doi: 10.1056/NEJMra1810764 [DOI] [PubMed] [Google Scholar]