Abstract
Background:
Sick building syndrome (SBS) is defined as a condition occurring in people who live or work in a modern building and who suffer from complaints such as headache, fatigue, lack of concentration, and irritation of the skin and mucous membranes.
Objectives:
The aim of this study is to examine the complaints associated with SBS in the employees of our hospital and evaluate the relationship between the characteristics of the work environment and the complaints of SBS.
Methods:
890 workers participated in the study. The complaints of the participants were rated and the sum of all complaints was recorded as the Total Complaint Score (TCS). The mean TCS of the participants was compared according to demographic characteristics and work environment characteristics.
Results:
The most common complaints among the employees were fatigue (40%), and general muscle and joint pain (31.4%). There was a statistically significant difference in TCS according to the position (p < 0.001). The mean TCS was significantly higher in females [13 (0–81)] than in males [6 (0–59)] (p < 0.001). The mean TCS increased with the presence of odor, new wall paint, the presence of fungus/mold on walls, and the presence of rotting/mold smell (p < 0.001, for all). TCS positively correlated with stress level, social relationship, noise level, comfort, cleanliness, number of employees in the same room, presence of odor, new wall paint, presence of rotting/mold, and use of chemical materials for cleaning in the room (p < 0.001, for all), and negatively correlated with room size and number of windows (p = 0.006, p < 0.001, respectively).
Discussion:
The present study found that the female gender, a high level of education, a high level of stress, a low level of social relationships and work environment characteristics were associated with the complaints of SBS among the employees. Accordingly, we believe that hospital management should be informed in order for the managers to take precautions and make new regulations.
Keywords: Sick building syndrome, hospital employees, indoor environmental quality, hospital environment, complaints
Introduction
Sick building syndrome (SBS) is defined as a condition that occurs in people living or working in a modern building and suffering from complaints such as headache, fatigue, lack of concentration, and irritation of the skin and mucous membranes (1). The negative effects experienced by the residents of a building on their health and well-being are related to the time spent in that building. However, a specific disease or cause cannot be identified. The complaints may be related to a specific room or involve a certain region or the entire building (2). The most important feature of SBS, which was defined following the studies conducted by the World Health Organization in Northern Europe and the United States of America (USA), is that the complaints lessen when the affected person leaves the building (3). The complaints occurring in the employees can be associated with themselves, the materials or the technologies they use, or be caused by their duties in the buildings (e.g., stress) or a characteristic of the building (4). Factors that may cause SBS have been classified as follows: biological factors (molds, bacteria, microbial volatile organic compounds, house dust); chemical factors (construction and household products, formaldehyde, phthalates, man-made mineral fibers, volatile organic compounds, odors, environmental tobacco smoke, other indoor air pollutants); physical factors (environmental parameters of thermal comfort, parameters related to building ventilation, noise, vibrations, daylight, electromagnetic fields, ions, ergonomics, universal design); psychosocial factors (occupational stress, social status, loneliness, helplessness, work organization, communication, supervision); individual factors (gender, individual characteristics, health status); and other (location, geopathogenic zones; building characteristics, ownership, presence of insects, rodents, use of pesticides, disinfection, raticides) (5).
SBS is an issue of increasing importance among office workers worldwide (6, 7) and the most important cause of job loss and low performance (8). Good indoor air quality, favorable environmental factors, ergonomic features and the thermal comfort of the building improve employee satisfaction and comfort, and thereby increase productivity and reduce job loss (1). The main complaints of SBS are burning and watery eyes, nasal congestion, runny nose and sneezing, dry throat, fatigue, lethargy, headache, and occasionally asthma (4). Indoor air quality problems and insufficient ventilation in the working area can cause SBS and aggravate the complaints. In order to evaluate the indoor air quality as ‘good’, the temperature must be between 19 and 23°C, and the relative humidity rate must be 40–60%. Recently, there has been an increase in demand for buildings impervious to air, heat and moisture, in which novel insulation materials are used to save energy. However, this form of insulation has increased the possibility of keeping chemical compounds indoors (9).
Our hospital consists of three buildings, and the indoor environment measurements are carried out every year on a regular basis as required by law. The number of particles, noise level, temperature and relative humidity are all within legally permissible limits (10). The present study aims to examine the complaints of SBS in the employees of our hospital and evaluate the relationship between the characteristics of the work environment and SBS complaints.
Methods
The study was conducted in accordance with the recommendations of the Declaration of Helsinki and was approved by the Local Ethics Committee (2011-KAEK-25 2018/06-09).
Participants: All staff working in our hospital (No. = 1282) were evaluated. Those who worked in the hospital less than one month were excluded from the study (no. = 42, 3.3%), and all other employees were asked to complete the “Sick Building Syndrome Questionnaire” (no. = 1240, 96.7%). The questionnaire forms of 928 employees (74.8% of those who were asked to complete the questionnaire) who agreed to participate in the study were evaluated, and 38 of these employees (4.1% of those who agreed to participate in the questionnaire) were excluded from the study due to missing personal information or unanswered questions. The study continued with 890 questionnaires completed by the participants.
The Sick Building Syndrome Questionnaire: The study used the questionnaire MM 040 NA Hospital, which was developed by Andersson et al. (11) and the Turkish validation of which was conducted by Arikan et al. (1), and several items were added to the questionnaire to examine the physical characteristics of the work environment. The questionnaire consists of three sections. In the first section, the demographic data of the participants were evaluated. The questions included active and passive smoking, hours of working in the building, daily working hours, stress levels, social relationships with colleagues, hours of working with computers, and the noise level, comfort and cleanliness of the work environment. The second section inquired 29 complaints such as red-dry eye, nasal congestion, flu, dry throat, fatigue, tendency to sleep, headache, and dry-red skin on a 4-point scale (Never: 0, Sometimes: 1, Often: 2, Always: 3 points). The last section inquired the factors that may have caused these complaints in the work environment. These factors included the surface area of the work environment and the number of people working in the same environment, the number of windows, whether the windows are facing the main street, ventilation systems, filters, odor, mold, new wall paint in the room as well as the use of pesticides, the presence of new furniture, use of chemicals for cleaning, smoking status in the room, floor materials, and the number of computers.
Total Complaint Score (TCS): The volunteers evaluated each complaint as “none, rarely (once a week or less frequent), frequently (2-3 times a week) and constantly (at least 5 times a week). The scores were assessed as follows: none: 0, rarely: 1, frequently: 2, constantly: 3. The score obtained by the individual from all complaints was recorded as TCS.
Statistics: Statistical analyses were performed with IBM SPSS ver. 23.0 (IBM Corp. Released 2015. IBM SPSS Statistics for Windows, Version 23.0 Armonk, NY: IBM Corp.). The data was examined by the Shapiro Wilk test whether or not it presents normal distribution. Descriptive statistics were given as median (minimum-maximum) values for continuous variables and frequency with percentages for categorical variables. The continuous variables were compared using the Mann Whitney-U test. Spearman correlation coefficient was calculated for correlations between variables. Multiple regression analysis was performed for effects of the working environment variables on TCS values. p<0.05 was considered as significance levels.
Results
The study included 890 hospital employees. The demographic data, work time, and pre-existing diseases of the participants and their rates are presented in Table 1. The assessment of comfort, cleanliness and noise level in the work environment are shown in Table 2.
Table 1.
Demographic data, working times and current diseases of volunteers
| Age (years) | 37 (20-68) | |
| Gender (male) | 272 (30.6) | |
| Smoking | 288 (32.4) | |
| Working time (years) | 11 (0-43) | |
| Working time in the building (years) | 6 (0-18) | |
| Working time in the room (years) | 3 (0-18) | |
| Daily working time in the room (hours) | 8 (0-24) | |
| Daily working time indoors (hours) | 8 (0-24) | |
| Current Diseases | Rhinitis | 179 (20.1) |
| Chronic pharyngitis | 91 (10.2) | |
| Chronic sinusitis | 128 (14.4) | |
| Asthma | 64 (32.4) | |
Descriptive statistics were given as median(minimum-maximum) or frequency with percentage
Table 2.
Evaluation of the working environment
| Excellent | Well | Middle | Insufficient | Very inadequate | |
| Comfort no. (%) | 17 (1.9) | 138 (15.6) | 374 (42.4) | 256 (29) | 98 (11.1) |
| Cleaning no. (%) | 65 (7.4) | 286 (32.4) | 346 (39.2) | 142 (16.1) | 43 (4.9) |
| Noise level no. (%) | 32 (3.2) | 154 (17.4) | 310 (35) | 233 (26.3) | 156 (17.6) |
When the stress level of hospital staff was examined, 28.8% (no. = 254) had extreme stress, 30.9% had much stress (no. = 272), 32% (no. = 282) had moderate stress, 4.9% (no. = 43) had mild stress, and 3.3% (no. = 29) had no stress. Among the participants, 85% (no. = 751) had good or very good social relationships and 74.7% (no. = 660) were working with computers. The rate of those working in a room facing the main street was 11.2% (no. = 84), while 89.4% (no. = 648) were working in a room with air conditioning and central heating system. The characteristics of the workrooms are presented in Table 3.
Table 3.
Characteristics of the rooms
| Rooms with ventilation system | 565 (85.3) |
| Number of windows (units) | 1 (0-20) |
| Window size (m2) | 1.5 (0-2.5) |
| Room size (m2) | 20 (2-50) |
| Number of employees in the Room | 4 (1-15) |
| Presence of odor in the room | 239 (32.7) |
| Presence of mist and moisture in the room | 76 (11.4) |
| Presence of fungus and mold on the wall | 55 (7.5) |
| Presence of rotten and mold odor in the room | 62 (8.4) |
| Air freshener | 257 (34.2) |
| Daily cleaning | 670 (87.6) |
| New furniture | 258 (35.1) |
| Smoking in the room | 13 (1.7) |
| Recently dye-isolation | 160 (22.3) |
| Insecticide | 464 (65.4) |
Descriptive statistics were given as median (minimum-maximum) or frequency with percentage
The most common complaints among the employees were fatigue (40%), generalized muscle and joint pain (31.4%), burning eyes (28.3%), dry throat (27.6%), headache (26%), dry skin (26%) and watery eyes (23%) (Figure 1). The mean TCS was highest among the nurses [15 (0–81)]. This was followed by technicians [10 (0–61)], office workers [9 (0–73)], secretaries [7.5 (0–59)], physicians [7.5 (0–51)], cleaning personnel [3 (0–23)], and security personnel [2.5 (0–44)] in respective order. TTT significantly varied depending on the position (p < 0.001). Nurses had significantly higher TCS than physicians, office workers, secretaries, technicians, security and cleaning personnel (p = 0.006, p < 0.001, p < 0.001 p = 0.005, p = 0.001 and p = 0.001, respectively). There was no significant difference between technicians and office workers, and between technicians and physicians (p = 0.26, p = 0.39, respectively). There was no significant difference between secretaries and security personnel, secretaries and cleaning personnel, and cleaning and security personnel (p = 0.15, p = 0.11, p = 0.81, respectively). The mean TCS was significantly higher in females [13 (0–81)] than in males [6 (0–59)] (p < 0.001). There was no significant difference in mean TCS according to marital status (p = 0.33). The mean TCS differed significantly depending on the educational level (p <0.001). The mean TCS increased with increasing level of education (p < 0.001). The mean TCSs were compared according to the work environment characteristics (Table 4). The mean TCS positively correlated with gender, educational level, stress level, social relationship, noise level, comfort level, cleanliness, the number of employees in the room, the number of windows, the presence of odor, new wall paint, the presence of rotting/mold, the use of cleaning chemicals in the room (p < 0.001, for all) and room size (p = 0.006).
Figure 1.
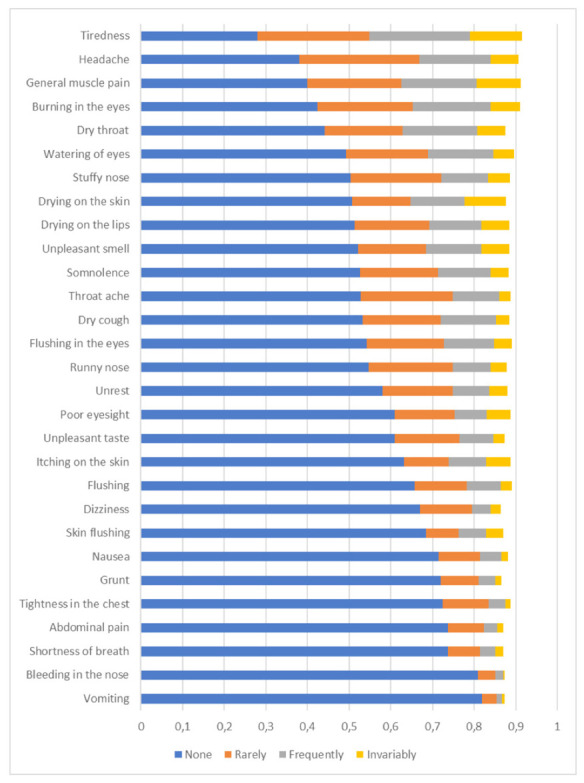
Rates of employee complaints
Table 4.
Comparison of variables of the working environment by the TCS average
| TCS, median (min-max) | p Value# | ||
| Gender | Female | 13 (0-81) | <0.001* |
| Male | 6 (0-59) | ||
| Room Type | Service room | 11 (0-81) | 0.510 |
| Study room | 11 (0-72) | ||
| Room overlooking the main street | (+) | 9 (0-51) | 0.297 |
| (-) | 11 (0-81) | ||
| Ventilation | (+) | 11 (0-81) | 0.410 |
| (-) | 12 (0-59) | ||
| Filter cleaning | (+) | 11 (0-81) | 0.237 |
| (-) | 12.5 (0-73) | ||
| Presence of odor | (+) | 16 (0-73) | <0.001* |
| (-) | 9 (0-81) | ||
| Presence of mist | (+) | 16 (0-67) | 0.139 |
| (-) | 11 (0-81) | ||
| New wall paint | (+) | 17 (0-81) | <0.001* |
| (-) | 10 (0-73) | ||
| Fungus and mold on the wall | (+) | 22 (0-65) | <0.001* |
| (-) | 11 (0-81) | ||
| Rotten and mold odor | (+) | 22.5 (0-73) | <0.001* |
| (-) | 11 (0-81) | ||
| Room spray | (+) | 9 (0-81) | 0.159 |
| (-) | 12 (0-73) | ||
| Daily cleaning in the room | (+) | 11 (0-81) | <0.001* |
| (-) | 8 (0-51) | ||
| New furniture in the room | (+) | 11 (0-81) | 0.459 |
| (-) | 11 (0-73) | ||
| Smoking in the room | (+) | 14 (0-47) | 0.403 |
| (-) | 11 (0-81) | ||
| Recent isolation in the room | (+) | 11 (0-54) | 0.830 |
| (-) | 11 (0-81) | ||
| Insecticide application in the room | (+) | 11 (0-81) | 0.519 |
| (-) | 11 (0-72) |
TCS: Total Complaint Score, #Mann Whitney-U Test, *p<0.05
When the variables in the regression model are examined, the variable new wall paint was found to have the greatest effect within the model. The least contributory variable was daily cleaning in the room. In the presence of variables in the model, an increase is observed in the TCS score (Table 5).
Table 5.
Multiple linear regression analysis results for TCS
| Unstandardized Coefficients B | Standardized Coefficients Beta | t | p | |
| Constant | 4.741 | 3.050 | 0.002 | |
| Gender (Female) | 5.150 | 0.164 | 4.522 | <0.001 |
| Presence of odor | 4.884 | 0.160 | 4.420 | <0.001 |
| New wall paint | 6.487 | 0.192 | 5.122 | <0.001 |
| Fungus and mold on the wall | 4.486 | 0.079 | 2.128 | 0.034 |
| Daily cleaning in the room | 3.523 | 0.083 | 2.302 | 0.022 |
TCS: Total Complaint Score
Discussion
This study is a comprehensive study that compare the frequency of SBS complaints among hospital staff according to environmental characteristics and working conditions such as educational status, level of stress, level of social relationships, level of comfort, cleanliness, number of employees in the room, room size, number of windows, presence of odor, presence of new wall paint, presence of rotting/mold, and frequent use of chemicals for cleaning in the room.
The present study found that the female gender, new wall paint, the presence of odor, the presence of fungus and mold on the wall, and daily cleaning of the room were associated with the complaints of SBS in the work environment of our hospital. Previous studies have examined topics such as the frequency of SBS complaints in non-hospital buildings (4), the relationship between environmental measurements and SBS (9, 12), or the comparison of the frequency of SBS complaints and environmental measurements between departments (5).
Daily cleaning using chemical substances, the presence of new wall paint, the decrease in room size and the number of windows increased TCS significantly. We could not identify any study examining the relationship between SBS complaints and the room size and number of windows, new wall paint, and everyday use of chemical cleaning agents. However, a previous study found good indoor ventilation, elimination of strong odors and cleaning at least once a week to be important. Although mechanical ventilation is beneficial, natural ventilation is promoted (13).
Since 1990s, there have been studies emphasizing the importance of age and gender in terms of work-related physical and psychosocial complaints (14–16). In the present study, the mean TCS was significantly higher in females than in males. This finding was supported by previous studies (12, 17–20). This was attributed to women’s stronger sense of smell and their greater perception of health (21, 22). Further reasons suggested include female physiology not being well understood, equipment dimensions not being suitable for women, and the work performed by women not being properly described (23). The mean age and gender distribution of the participants were similar to the findings of another study that was conducted in Slovenia on 258 healthcare workers (5). In the said study, 60.1% of the participants were non-smokers. In the present study, the rate of non-smokers was 67.6%.
Among the employees, nurses had the highest mean TCS. This was followed by technicians, physicians and secretaries. We could not identify any previous study comparing SBS complaints according to the job performed in the hospitals. However, we believe that this finding may be because nurses are mostly female, and nurses and technicians work for longer periods of time in the hospitals. New studies on this matter can provide us with more precise information.
We found increasing TCS with increasing level of stress and decreasing comfort of the work environment and level of social relationships. Redman et al. (24) and Runeson et al. (25) also mentioned that a decrease in the level of welfare and psychosocial status was associated with an increase in SBS complaints.
Variable complaints such as fatigue, headache, dizziness, nasal complaints or eye complaints are seen in SBS. In the study by Dhungana et al. on bank employees, the most common complaints were fatigue (37.3%), dizziness (16.2%) and headache (14.1%) (26). A study conducted with 126 hospital employees in Taiwan reported that nasal (66%) and eye complaints (53%) were the most frequent complaints. The authors also found dry facial skin in 33% and fatigue in 30% (27). In a study by Quoc et al. involving 207 hospital employees, the most frequent complaints were fatigue, headache, dizziness, cough and dry throat in respective order (20). Also in the present study, the most common complaint was fatigue (40%). This was followed by generalized muscle and joint pain (31.4%), burning eyes (28.3%), dry throat (27.6%), headache (26%), dry skin (26%) and watery eyes (23%). Building characteristics and working conditions can cause different complaints in different work areas.
TCS increased significantly with increasing level of education. On the other hand, a study by Karvala et al. examined 4,941 people from general population found that low level of education was associated with SBS complaints, especially in women (21). Since the participants of the present study were healthcare workers, we believe that they may have slightly better awareness of the effects of work environment conditions on health. The authors consider that people with higher level of education in the present study may have reported higher number of complaints.
Menteşe et al. indicated that dermatological complaints increased with increasing number of employees working in the same room (12). The present study found a correlation between the number of employees in the same room and TCS. We found that TCS significantly increased as the participants’ complaints about the noise level increased. Rashid et al. reported an increased risk of SBS with an increase in the noise level measurements (28). Arikan et al. (1) and Akova et al. (29) also agreed with this finding and indicated that the risk was 1.2 and 3.11 times higher, respectively. In the present study, we found that the presence of a rotting smell and mold in the environment significantly increased TCS. This finding was in support of previous studies. However, hospital settings were not examined in any of these studies (4, 30–32).
The limitation of the present study was conducted based on the subjective questionnaire responses of the participants. The participants who reported complaints did not undergo physical examination. Another limitation is the absence of examination of the differences between departments. Furthermore, environmental measurements were not included in the study. The periodic measurements of noise, moisture, temperature, and gas and particles in ambient air, which are a legal obligation, are carried out every year in our hospital and are found to be within normal limits.
Conclusion
The present study found that female gender, a high level of education, a high level of stress, a low level of social relationships, a high level of noise, a decreased level of comfort, a large number of employees in the room, room size, the number of windows, the presence of odor, the presence of new wall paint, the presence of rotting/mold, and the frequent use of chemicals for cleaning in the room were associated with SBS complaints among individuals working in the hospital setting. We believe that hospital management should be informed in order for the managements to take measures and make new regulations to improve indoor quality, and healthcare workers should be made aware of the relationship between the characteristics of their work environment and SBS. It would also appear to be important to arrange work environments in the light of these findings in the new hospital buildings in order to achieve high levels of employee productivity and to protect employee health.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. None declared
No potential conflict of interest relevant to this article was reported by the authors. Written informed consent for publication of their details was obtained from the patient.
References
- 1.Arikan I, Tekin OF, Erbas O. Relatıonshıp between sıck buıldıng syndrome and ındoor aır qualıty among hospıtal staff. Med Lav. 2018, 20;109(6):435–443. doi: 10.23749/mdl.v110i6.7628. doi: 10.23749/mdl.v110i6.7628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.United States Environmental Protection Agency. Indoor Air Facts No. 4 (revised). Sick Building Syndrome. Research and Development (MD-56), 1991 Feb. https://www.epa.gov/sites/production/files/2014–08/documents/sick_building_factsheet.pdf .
- 3.World Health Organisation (WHO) EURO Reports and Studies, No. 78. Copenhagen: WHO; 1983. Indoor air pollutants: exposure and health effects. https://www.euro.who.int/__data/assets/pdf_file/0010/156970/euro_series_78.pdf . [Google Scholar]
- 4.Burge PS, Hedge A, Wilson S, Bass JH, Robertson A. Sick building syndrome; a study of 4373 office workers. Ann Occup Hyg. 1987;31:493–504. doi: 10.1093/annhyg/31.4a.493. doi: 10.1093/annhyg/31.4a.493. [DOI] [PubMed] [Google Scholar]
- 5.Smajlović SK, Kukec A, Dovjak M. Association between Sick Building Syndrome and Indoor Environmental Quality in Slovenian Hospitals: A Cross-Sectional Study. Int J Environ Res Public Health. 2019;16:3224. doi: 10.3390/ijerph16173224. doi: 10.3390/ijerph16173224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abdel-Hamid MA, Elokda EE, Mostafa NS. Prevalence and risk factors of sick building syndrome among office workers. J Egypt Public Health Assoc. 2013 Aug;88(2):109–14. doi: 10.1097/01.EPX.0000431629.28378.c0. doi: 10.1097/01.EPX.0000431629.28378.c0. [DOI] [PubMed] [Google Scholar]
- 7.Wittczak T, Walusiak J, Pałczyński C. “Sick building syndrome”-a new problem of occupational medicine. Med Pr. 2001;52(5):369–73. [PubMed] [Google Scholar]
- 8.Crawford JO, Bolas SM. Sick building syndrome, work factors and occupational stress. Scand J Work Environ Health. 1996;22(4):243–250. doi: 10.5271/sjweh.138. doi: 10.5271/sjweh.138. [DOI] [PubMed] [Google Scholar]
- 9.Suzuki N, Nakaoka H, Hanazato M, et al. Indoor Air Quality Analysis of Newly Built Houses. Int J Environ Res Public Health. 2019;28(16)(21):4142. doi: 10.3390/ijerph16214142. doi: 10.3390/ijerph16214142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dovjak M, Kukec A. Springer, Switzerland: 2019. Creating Healthy and Sustainable Buildings: An Assessment of Health Risk Factors. doi: 10.1007/978-3-030-19412-3. [PubMed] [Google Scholar]
- 11.Andersson K, Stridh G. Levy F, , Maroni , editors. The use of standardized questionnaires in building related illness (BRI) and sick building syndrome (SBS) surveys. NATO/CCMS pilot study on indoor air quality. National Institute of Occupational Health, Oslo, 1992. pp. 47–64. Retrieved from http://www.mmquestionnaire.se/mmq/mm040_care.pdf .
- 12.Mentese S, Tasdibi D. Airborne bacteria levels in indoor urban environments: The influence of season and prevalence of sick building syndrome (SBS) Indoor and Built Environment. 2016;25(3):563–580. doi: 10.1177/1420326X14562454. [Google Scholar]
- 13.Nakayama Y, Nakaoka H, Suzuki N, et al. Prevalence and risk factors of pre-sick building syndrome: characteristics of indoor environmental and individual factors. Environ Health Prev Med. 2019;24(1):77. doi: 10.1186/s12199-019-0830-8. doi: 10.1186/s12199-019-0830-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Zwart BC, Broersen JP, Frings-Dresen MH, van Dijk FJ. Musculoskeletal complaints in the Netherlands in relation to age, gender and physically demanding work. Int Arch Occup Environ Health. 1997;70(5):352–60. doi: 10.1007/s004200050229. doi: 10.1007/s004200050229. [DOI] [PubMed] [Google Scholar]
- 15.Knez I, Enmarker I. Effects of office lighting on mood and cognitive performance and a gender effect in work-related judgment. Environ Behav. 1998;30(4):553–567. doi: 10.1177/001391659803000408. [Google Scholar]
- 16.Karlqvist L, Tornqvist EW, Hagberg M, Hagman M, Toomingas A. Self-reported working conditions of VDU operators and associations with musculoskeletal symptoms: a cross-sectional study focusing on gender differences. Int J Ind Ergon. 2002;30(4):277–294. doi: 10.1016/S0169-8141(02)00131-2. [Google Scholar]
- 17.Kim J, Jang M, Choi K, Kim K. Perception of indoor air quality (IAQ) by workers in underground shopping centers in relation to sick-building syndrome (SBS) and store type: a cross-sectional study in Korea. BMC Public Health. 2019;19(1):632. doi: 10.1186/s12889-019-6988-6. doi: 10.1186/s12889-019-6988-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Runeson R, Wahlstedt K, Wieslander G, Norback D. Personal and psychosocial factors and symptoms compatible with sick building syndrome in the Swedish workforce. Indoor Air. 2006;16(6):445–53. doi: 10.1111/j.1600-0668.2006.00438.x. doi: 10.1111/j.1600-0668.2006.00438.x. [DOI] [PubMed] [Google Scholar]
- 19.Lin Z, Wang T, Norback D, Kan H, Sundell J, Zhao Z. Sick building syndrome, perceived odors, sensation of air dryness and indoor environment in Urumqi, China. Chin Sci Bull. 2014;59(35):5153–60. doi: 10.1007/s11434-014-0647-1. [Google Scholar]
- 20.Quoc CH, Huong GV, Duc HN. Working Conditions and Sick Building Syndrome among Health Care Workers in Vietnam. Int J Environ Res Public Health. 2020 May 21;17(10):3635. doi: 10.3390/ijerph17103635. doi: 10.3390/ijerph17103635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Karvala K, Sainio M, Palmquist E, Claeson AS, Nyback MH, Nordin S. Building-Related Environmental Intolerance and Associated Health in the General Population. Int. J. Environ. Res. Public Health. 2018;15(9):2047. doi: 10.3390/ijerph15092047. doi: 10.3390/ijerph15092047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Johansson A, Brämerson A, Millqvist E, Nordin S, Bende M. Prevalence and risk factors for self-reported odour intolerance: the Skövde population-basedstudy. Int Arch Occup Environ Health. 2005;78(7):559–64. doi: 10.1007/s00420-005-0616-8. doi: 10.1007/s00420-005-0616-8. [DOI] [PubMed] [Google Scholar]
- 23.Lee S, Park MH, Jeong BY. Gender differences in public office workers’ satisfaction, subjective symptoms and musculoskeletal complaints in workplace and office environments. Int J Occup Saf Ergon. 2018;24(2):165–170. doi: 10.1080/10803548.2016.1272959. doi: 10.1080/10803548.2016.1272959. [DOI] [PubMed] [Google Scholar]
- 24.Redman T, Hamilton P, Malloch H, Kleymann B. Working here makes me sick! The consequences of sick building syndrome. Human Resource Manag J. 2011;21:14–27. doi: 10.1111/j.1748-8583.2010.00155.x. [Google Scholar]
- 25.Runeson R, Wahlstedt K, Wieslander G, Norback D. Personal and psychosocial factors and symptoms compatible with sick building syndrome in the Swedish workforce. Indoor Air. 2006;16(6):445–53. doi: 10.1111/j.1600-0668.2006.00438.x. doi: 10.1111/j.1600–0668.2006.00438.x. [DOI] [PubMed] [Google Scholar]
- 26.Dhungana P, Chalise M. Prevalence of Sick Building Syndrome Symptoms and its Associated Factors among Bank Employees in Pokhara Metropolitan, Nepal. Indoor Air. 2020;30(2):244–250. doi: 10.1111/ina.12635. doi: 10.1111/ina.12635. [DOI] [PubMed] [Google Scholar]
- 27.Chang CJ, Yang HH, Wang YF, Li MS. Prevalence of Sick Building Syndrome-Related Symptoms among Hospital Workers in Confined and Open Working Spaces. Aerosol Air Qual Res. 15:2378–2384. doi: 10.4209/aaqr.2015.01.0040. [Google Scholar]
- 28.Rashid M, Zimring CA. Review of the Empirical Literature on the Relationships between Indoor Environmental and Stress in Healthcare and Office Settings: Problems and Prospects of Sharing Evidence. Environ Behav. 2008;40(2):151–190. doi: 10.1177/0013916507311550. [Google Scholar]
- 29.Akova I, Kiliç E, Sümer H, Keklikçi T. Prevalence of sick building syndrome in hospital staff and its relationship with indoor environmental quality. Int J Environ Health Res. 2020;16:1–16. doi: 10.1080/09603123.2020.1862067. doi: 10.1080/09603123.2020.1862067. [DOI] [PubMed] [Google Scholar]
- 30.Straus DC. Molds, mycotoxins, and sick building syndrome. Toxicol Ind Health. 2009;25(9):617–35. doi: 10.1177/0748233709348287. doi: 10.1177/0748233709348287. [DOI] [PubMed] [Google Scholar]
- 31.Saijo Y, Kishi R, Sata F, et al. Symptoms in relation to chemicals and dampness in newly built dwellings. Int Arch Occup Environ Health. 2004;77(7):461–70. doi: 10.1007/s00420-004-0535-0. doi: 10.1007/s00420-004-0535-0. [DOI] [PubMed] [Google Scholar]
- 32.Fu X, Norbäck D, Yuan Q, et al. Association between indoor microbiome exposure and sick building syndrome (SBS) in junior high schools of Johor Bahru, Malaysia. Sci Total Environ. 2021;20:753–141904. doi: 10.1016/j.scitotenv.2020.141904. doi: 10.1016/j.scitotenv.2020.141904. [DOI] [PubMed] [Google Scholar]


