Abstract
Between national unification and World War I, Germany was preeminent in many areas of science and medicine. Alois Alzheimer, who lived during this period, was one of the founders of the field of neuropathology. His name will always be linked with the form of dementia that he described 100 years ago. Here we mark this anniversary by discussing Alzheimer’s contributions to dementia research in the context of his life and times.
Alois Alzheimer (Figure 1) was born on 14 June 1864 in Marktbreit‐am‐Main, a small town in Franconia. Following secondary studies in Aschaffenburg, he studied medicine at the Universities of Berlin, Tübingen and Würzburg, where he obtained his MD degree in 1888 (31, 50). His dissertation “On the Ceruminal Glands of the Ear” was carried out under the supervision of the influential histologist Albert von Koelliker (1817–1905).
Figure 1.
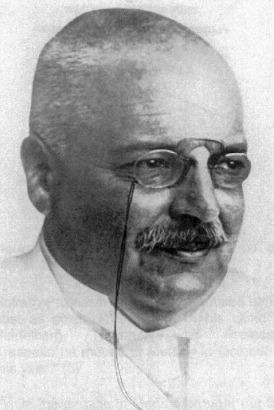
Alois Alzheimer (1864–1915).
FRANKFURT: THE BEGINNING
In December 1888, Alzheimer began to work at the Municipal Asylum for the Mentally Ill and Epileptics in Frankfurt‐am‐Main, where he stayed for the next 14 years (50). Its founder was Heinrich Hoffmann (1809–1894), who is mainly remembered today as the author of “Der Struwwelpeter” (Slovenly Peter), one of the best‐known children’s books in German. Hoffmann retired in 1888 at the age of 79 years and Emil Sioli (1852–1922) became his successor. He reorganized and modernized the Frankfurt asylum by introducing no‐restraint policies, hydrotherapy and occupational therapy. Sioli, who believed that progress in psychiatry depended on scientific investigation, adhered to Wilhelm Griesinger’s (1817–1868) dictum that “mental diseases are brain diseases” (71).
In 1889, Franz Nissl (Figure 2) (1860–1919) became assistant medical director of the Frankfurt asylum (67). The 7 years that he spent in Frankfurt had a profound influence on Alzheimer’s career. Despite his young age, Nissl was already a leading histopathologist, having invented the “Nissl stain”, an entirely new method for staining nerve cell bodies, when still a medical student at the University of Munich (44, 47, 53). Nissl was a pupil of Bernhard von Gudden (1824–1886) (22, 34), Professor of Psychiatry at the University of Munich and, like him, psychiatrist to members of the Bavarian Royal family, especially Prince Otto, who suffered from schizophrenia, and his elder brother King Ludwig II, whose behavior became increasingly erratic over the years. Gudden played a major part in the forced abdication of Ludwig II on grounds of insanity. On 13 June 1886, both king and psychiatrist were found dead in lake Starnberg near Munich. It seems that Gudden had run after Ludwig II, who had walked into the lake. In the ensuing struggle, Ludwig II probably strangled Gudden, before drowning himself. These dramatic events, which left Nissl without a mentor, led to his departure from Munich in February 1888. From October 1888 until March 1889, he worked at the Blankenheim State Mental Asylum in Weimar, before moving to Frankfurt in April 1889 (Nissl, unpublished, Courtesy of G. Kreutzberg).
Figure 2.

Franz Nissl (1860–1919).
Nissl and Alzheimer became close collaborators and lifelong friends. They were clinicians by day and histopathologists by night (45, 55, 67). In other areas of medicine, histopathology had already succeeded in correlating disease symptoms with organic causes. Nissl and Alzheimer wanted to achieve the same in psychiatry through the use of microscopic analysis of the brain, with a major focus on the cerebral cortex (29, 68). They were convinced that only if mental disorders could be clearly defined, would it become possible to understand and treat them. Nissl was mostly interested in developing novel methods and performing experimental studies, whereas Alzheimer’s focus was on correlating psychiatric symptoms with histological results obtained from brain autopsies. He published a case report on progressive spinal muscular atrophy in 1891 (1). Studies on cerebral arteriosclerosis and progressive paralysis, the two major research topics of Alzheimer’s career, followed in 1894 and 1896 (2, 3). The collaboration between Nissl and Alzheimer lasted until 1895, when Nissl accepted a position at the University of Heidelberg with Emil Kraepelin (Figure 3) (1856–1926), perhaps the most influential psychiatrist of his time. Kraepelin, who was one of the founders of modern psychiatry, is best known for his seminal work on the nosology of schizophrenia (he called it dementia praecox) and manic‐depressive illness (42). Many years later, in his obituary of Alzheimer, Nissl described his time in Frankfurt as “the seven wonderful years that I spent working with Alzheimer. They were years of hard work, of learning and of striving, underpinned by an ideal friendship” (55).
Figure 3.

Emil Kraepelin (1856–1926).
The story of Alzheimer’s disease began on 25 November 1901, when Alzheimer admitted the 51‐year‐old Auguste D. as a patient (50, 51). He was now assistant medical director of the Frankfurt asylum. Hermann Paul Nitsche (1876–1948) was the junior physician in charge of Auguste D. (19, 50). Over the previous year, she had experienced a marked decline in her ability to form new memories. She had developed a fear of people who were well known to her; she had also become paranoid and unduly jealous of her husband. Alzheimer followed Auguste D. until March 1903, when he, like Nissl 7 years earlier, heeded the call from Kraepelin and moved to Heidelberg (31, 50). Alzheimer and Nissl could now resume their collaboration. Alzheimer’s stay in Heidelberg, however, was only short‐lived. In October 1903, Kraepelin became head of the Royal Psychiatric Clinic at the University of Munich (46). Alzheimer moved with him to direct the clinic’s anatomical laboratory. He stayed in Munich for the next 9 years.
Karl Bonhoeffer (1868–1948) succeeded Kraepelin in Heidelberg (70). Six months into the job, he left to become Professor of Psychiatry at the University of Breslau in Silesia (now Wroclaw in Poland). Nissl, who had planned to move with Kraepelin and Alzheimer, was offered and accepted the chair of Psychiatry at the University of Heidelberg (67). As a result, Alzheimer and Nissl were not able to continue their collaboration. Nissl was a successful head of the Psychiatric Clinic and exerted a major influence on a number of young psychiatrists, among them Karl Jaspers (1883–1969) and Hugo Spatz (1888–1969). Jaspers, who was to become a major philosopher of existentialism, wrote his influential book Allgemeine Psychopathologie (General Psychopathology) (36), while an unpaid assistant at the Heidelberg Clinic. He later described the congenial atmosphere Nissl had created there (35).
MUNICH: THE MIDDLE PERIOD
Alzheimer was now at the height of his powers. Shortly after his move to Munich, he published his habilitation thesis on the histopathology of progressive paralysis (297 pages in length) in the Journal he and Nissl were editing (5). At the time, progressive paralysis was a major problem, with close to 10% of psychiatric patients being affected. Alzheimer described findings based on 170 autopsy cases. This was going to be his best‐known work during his lifetime. In Munich, Alzheimer assembled an impressive international group of researchers, which included F. Bonfiglio, U. Cerletti, H.G. Creutzfeldt, A. Farworsky, S.C. Fuller, A. Jakob, F.H. Lewy, F. Lotmar. L. Merzbacher, G. Perusini and T. Simchowicz. Friedrich Lewy (1885–1950) described the defining pathological features of Parkinson’s disease (Lewy bodies and Lewy neurites) while at the Munich Institute (48). Alzheimer’s clinical duties were now less onerous, but they continued to form an important part of his daily work. Following the move of Robert Gaupp (1870–1953) to Tübingen in 1906, he was second‐in‐command at the Munich Clinic; however, after 18 months, he asked to be relieved of this duty, because he had too little time for research. His place was taken by Ernst Rüdin (1874–1952). In 1908, the medical faculty of the University of Munich awarded Alzheimer an Associate Professorship.
Auguste D. died at the Frankfurt asylum on 8 April 1906. Alzheimer asked for her brain to be sent to Munich for analysis, where it arrived on 28 April. The work he carried out over the next 6 months was to make medical history. Alzheimer described his findings at the 37th meeting of the Society of Southwest German Psychiatrists in Tübingen on 3 November 1906. They were published in the short paper of 1907, which is essentially a transcript of the Tübingen talk, and in the more extensive article of 1911 (6, 7). The 1907 paper gives the clinicopathological description of Auguste D.’s illness (6). In her cerebral cortex, Alzheimer saw abundant plaques and neurofibrillary tangles using the reduced silver staining methods described by Max Bielschowsky (Figure 4) (1869–1940) over the previous 4 years (13, 14, 15). The clinical file and histological sections of Auguste D. were recovered a few years ago (33, 51).
Figure 4.

Max Bielschowsky (1869–1940).
Bielschowsky trained with Ludwig Edinger (1855–1918) and Carl Weigert (1845–1904) at the Senckenberg Institute of Pathology and Anatomy of the University of Frankfurt, at a time (1893–1896) when Nissl and Alzheimer were both working at the local municipal asylum (21). He then moved to Berlin, where he worked in the Neurological Clinic of Emanuel Mendel (1839–1907). It was here that Bielschowsky developed the silver staining techniques based on the use of ammoniacal silver and mild reducing agents (13, 14, 15). In 1904, he moved to the Neurobiological Laboratory directed by Oskar Vogt (1870–1959), which was to become the Kaiser‐Wilhelm‐Institute for Brain Research (57). Bielschowsky lost his position in 1933 and died in exile in London 7 years later.
In normal brain, the Bielschowsky method visualizes what were named “neurofibrils” at the end of the 19th century (12), a network of fine filaments that traverses the nerve cell and corresponds most closely to what we now know as the neuronal cytoskeleton. Santiago Ramón y Cajal (1852–1934) also referred to the “neurofibrillar cytoskeleton” (62). The ability to visualize neurofibrils provided some of the evidence in favor of the Neuron Doctrine, for which Ramón y Cajal was awarded the Nobel Prize in Physiology or Medicine in 1906 (together with C. Golgi) (61). It is interesting to note that at this time the Neuron Doctrine had its supporters (such as Bielschowsky), but also its fair share of detractors (Golgi and Nissl among them) (30, 54).
Alzheimer saw increased silver staining in many nerve cells of the cerebral cortex of Auguste D., which he attributed to an abnormal thickening of neurofibrils and their alignment into bundles (the term “neurofibril” survives to this day in the expression “neurofibrillary tangle”). Indeed, they were found to survive the degeneration of nerve cells (as extracellular or ghost tangles). Alzheimer states that he could also stain these bundles with dyes that did not label normal neurofibrils, thus underscoring their pathological nature (6).
In April 1907, the American psychiatrist Solomon Carter Fuller (1872–1953), a former collaborator of Alzheimer, reported on neurofibrils in a number of conditions, including three cases of senile dementia [he had presented his findings at the June 1906 meeting of the American Medico‐Psychological Association (26, 37)]. It has been suggested that Fuller may have been the first to describe the tangle (11). However, unlike Alzheimer, he did not describe “the abnormal thickening of neurofibrils”, nor did he mention their accumulation inside nerve cells and the ensuing demise of these cells. He observed instead a reduction in neurofibrils in senile dementia and a number of unrelated conditions, probably as a result of the process of nerve cell degeneration. It thus seems clear that Alzheimer described the tangle for the first time. Fuller was of the same opinion, as he referred to the tangle as “the type of intracellular degeneration of neurofibrils to which Alzheimer was the first to call attention” (27).
Plaques were first described in 1892 by Paul Blocq (1860–1896) and Georges Marinesco (1863–1938), who were working at the Salpêtrière Clinic in Paris, in the brain of an elderly patient with epilepsy (18). Emil Redlich (1866–1930), who worked at the Psychiatric‐Neurological Hospital of the University of Vienna, described them in two cases of senile dementia in 1898 (63). This was followed by Oskar Fischer’s description of neuritic plaques in senile dementia and their absence in controls and cases of progressive paralysis and functional psychosis (24, 25). He concluded that they are a specific feature of senile dementia; they were subsequently often referred to as Redlich’s or Fischer’s plaques. Like plaques, the clinical characteristics of dementia had been described before Alzheimer, most notably by the French psychiatrist Jean‐Etienne Esquirol (1772–1840) (23).
Kraepelin separated the disease from senile dementia and named it after Alzheimer in the second volume of the 8th edition of his textbook of psychiatry (43). By this time, additional cases had been described by F. Bonfiglio (1908, one case) (20), U. Sarteschi (1909, one case) (65) and G. Perusini (1909, two cases) (58). The ages of hospital admission of the five cases published by the end of 1909 were 51, 63, 67, 45 and 65 years. It remains unclear why Kraepelin made the distinction between Alzheimer’s disease and senile dementia. His introduction of the term senium praecox proved highly influential and led to the view that Alzheimer’s disease is always a presenile condition. This assumption was overturned later, when it had become apparent that Alzheimer’s disease and most cases of senile dementia are similar, both clinically and neuropathologically (17). It is possible that the early ages of disease onset and the clinical pictures of Auguste D. and Johann F. (Alzheimer’s “second patient”, who was hospitalized in Munich from 1907 until his death in 1910 at the age of 59 years), together with the striking cortical pathology of Auguste D., convinced Kraepelin that Alzheimer’s disease was altogether different from senile dementia (10, 74). He strongly believed that observable pathological processes in the brain cause specific psychopathologies. It has also been suggested (albeit without documentary evidence) that Kraepelin’s motivation for distinguishing between Alzheimer’s disease and senile dementia may have been in part opportunistic, as this made it easier to name the disease after his collaborator (9). It would otherwise have been difficult to ignore Fischer, who worked at the Psychiatric Clinic of the German University of Prague, headed by Arnold Pick (1851–1924).
Alzheimer’s article of 1911 is devoted to the nosology of the disease (7). He presents the case of Johann F. (with plaques, but no neurofibrillary pathology in cortex) and provides additional information on Auguste D. The histological preparations of Johann F. have been recovered (32), and it has been suggested that he may have suffered from a familial form of Alzheimer’s disease (41). Towards the end of the article, Alzheimer also describes the microscopic pathology of two cases with circumscribed lobar atrophy that he had recently examined. Similar cases of what we now know as “frontotemporal lobar degeneration” (FTLD) had been described clinically and from post‐mortem inspection of the brain by Pick (59). Alzheimer reported on the absence of plaques and the presence of neurofibrillary changes with a characteristic round shape, which distinguished them from the tangles of Alzheimer’s disease (Figure 5). They are now called Pick bodies (despite the fact that they were first described by Alzheimer) and the clinicopathological entity is known as Pick’s disease (following a suggestion by A. Gans, a pupil of Pick) (28). Alzheimer did not provide much information about the two cases of lobar atrophy. Subsequently, the clinical features of one case (Therese M.) were described in more detail by Georg Stertz (1878–1959) (69), who was Alzheimer’s son‐in‐law. K. Onari and Spatz provided a neuropathological description of this case (56). They reported a severe temporal lobe atrophy and the presence of abundant Pick bodies.
Figure 5.

The abnormal deposits that Alzheimer described. A. Neurofibrillary tangles (brown) and neuritic plaques (dark blue) in Alzheimer’s disease. Tangles were stained with an antibody against tau protein and plaques with an antibody against β‐amyloid. B. Pick bodies (brown) in Pick’s disease. They were stained with an antibody against tau protein.
By all accounts, Alzheimer was a gentle and considerate man. Nissl described him as fortiter in re, suaviter in modo (resolute in deed, gentle in manner) (55). In his 1920 article about the lives of Alzheimer, Korbinian Brodmann (1868–1918) and Nissl, who all died young, Kraepelin provided a vivid portrait of Alzheimer as a very dedicated individual who worked without pay and only rarely took a break (45). In 1894, Alzheimer had married Cäcilie Geisenheimer (née Wallerstein), the widow of a wealthy industrialist, with whom he had three children. Following his wife’s early death in 1901, he became financially independent. In Munich, Alzheimer lived with his children and his sister in an apartment near the Clinic (50). Kraepelin, who used his article to advocate the creation of full‐time research positions in psychiatry, believed that Alzheimer’s heavy workload contributed to his early death. Only little appears to be known about Alzheimer’s views on the causes of mental illness and the general atmosphere at the Munich Clinic in the period preceding World War I.
From the 1880s onwards, the medical establishment in Germany (and several other countries) became increasingly preoccupied with social Darwinism, monism, theories of degeneration and racial hygiene. Psychiatrists played an important part in this movement. Racial hygiene was considered an applied science based on the laws of genetics (Gregor Mendel’s work was rediscovered by Correns, Tschermak and de Vries in 1900), which was necessary for improving the health of the population by preventing genetic defects (75, 77). It was believed to be complementary to personal hygiene. At the root of racial hygiene lay a strong belief in biological determinism (64). The inherited nature of some disorders was already well known. In addition, more diffuse ideas of inheritance and degeneration gained in popularity, especially following the publication of the influential book Traité des dégénérescences physiques, intellectuelles et morales de l’espèce humaine (Treatise of the physical, intellectual and moral degeneration of the human species) by the French psychiatrist Bénédict Augustin Morel (1809–1873) in 1857 (52). He believed that mental disorders were inherited in such a way that degeneracy was cumulative and that as a result a worsening of symptoms occurred in subsequent generations. What was present as nervousness in the first generation could manifest itself as neurosis in the second generation, psychosis in the third generation and mental retardation, physical deformity and sterility in the fourth generation. Over‐consumption of alcohol, tobacco and opium was thought to weaken the genetic material and lead to degeneration. These ideas had a strong influence on the Italian psychiatrist Cesare Lombroso (1835–1909), who linked organic disease with social deviancy and put forward the concept of the “delinquente nato” (born criminal) (49, 60, 78). Moral decadence, social deviancy, tuberculosis and venereal diseases were all seen as symptoms of hereditary degeneration. Alzheimer appears to have shared many of these views (4, 8). They were also held in other walks of life and influenced some of the major literary works of the period, such as Henrik Ibsen’s “Ghosts”, Emile Zola’s cycle of novels “Les Rougon‐Macquart”, Robert Louis Stevenson’s “The Strange Case of Dr Jekyll and Mr Hyde”, Gerhart Hauptmann’s “Vor Sonnenaufgang” (Before Sunrise) and Thomas Mann’s “Buddenbrooks”.
It is against this background that one probably has to view Alzheimer’s membership of the “Deutsche Gesellschaft für Rassenhygiene” (German Racial Hygiene Society). His name appears on the list of members for 1913, at a time when the Society was still in its infancy (74). On 9 January 1912, he lectured on the brain to an audience of 300 people for the Munich chapter of the Racial Hygiene Society (75). Alzheimer’s colleague Rüdin was a founding member of the Society (72, 73, 75, 77). Gaupp and Nitsche were two colleagues at the Munich Clinic who also belonged to the Society. Kraepelin, by contrast, was not a member. The Munich branch of the Racial Hygiene Society was constituted in 1907 and recruited its members from the higher echelons of Society (72, 75, 77). They included Wilhelm von Bestelmeyer, chief physician of the Bavarian army, Johannes Ranke, chairman of the German Society for Anthropology, Karl von Frisch, the zoologist and recipient of the 1973 Nobel Prize in Physiology or Medicine (with K. Lorenz and N. Tinbergen), Julius Lehmann, publisher of the medical weekly “Muenchener Medizinische Wochenschrift” (MMW) and Bernhard Spatz, editor‐in‐chief of the MMW, and the father of Hugo Spatz. Although the German Racial Hygiene Society was the first of its kind (it began in Berlin in 1905), by 1912 similar societies also existed in the US, the UK and Sweden (38).
Many years after Alzheimer’s death, the views espoused by the Racial Hygiene Society had a significant impact on Nazi ideology and a number of psychiatrists helped to prepare and implement some of the terrible events of the 1930s and 1940s (39, 75, 76, 77). Alfred Hoche (1865–1943), Professor of Psychiatry at the University of Freiburg, co‐authored (with K. Binding) the book Die Freigabe der Vernichtung lebensunwerten Lebens (Allowing the extermination of life not worth living), which was published in 1920 (16). Rüdin co‐authored (with A. Gütt and F. Ruttke) the official commentary on the Gesetz zur Verhütung erbkranken Nachwuchses (Law for the Prevention of Genetically Diseased Offspring) of 1933 (72, 73). Around 400 000 people were sterilized under this law until 1939, when it was replaced by the wartime “euthanasia” program, which led to the killing of some 80 000 psychiatric patients (39). In his capacity as chief adjudicator of the “T4‐Aktion” (the “euthanasia” program, named after the location of its administrative headquarters in Berlin’s Tiergartenstrasse 4), Nitsche sent thousands of mental patients to their deaths (19, 39, 76). After the war, he was tried, sentenced to death and executed in Dresden (in the Soviet sector) in 1948 for his role in the implementation of the “euthanasia” program.
BRESLAU: THE FINAL YEARS
In 1912, Alzheimer was appointed to the chair of Psychiatry and the Directorship of the Psychiatric Institute at the University of Breslau, where he succeeded Bonhoeffer who had moved to Berlin (50). Alzheimer’s place in Munich was taken by Walther Spielmeyer (1879–1935). Spielmeyer’s successor was Willibald Scholz (1889–1971), who described the blood vessel‐associated amyloid deposits in Alzheimer’s disease (66). At the time, Breslau was the seventh largest city in Germany. Its Psychiatric Clinic was put on the map by Carl Wernicke (1848–1905) who directed it from 1890 to 1903 (40).
By all accounts, Alzheimer wanted to try his hand at directing a large Psychiatric Clinic, while continuing to do research in histopathology. In Munich, he felt that his position did not fully reflect his true value (45). Lewy moved with him to take charge of the anatomical laboratory. In the event, Alzheimer’s years in Breslau were overshadowed by the sequels of a bacterial infection that he contracted during the move from Munich. It developed into a subacute endocarditis, which weakened him physically and forced him to take lengthy breaks from work. In 1913, he organized the annual meeting of the German Society of Psychiatry in Breslau. Kraepelin, who saw Alzheimer there for the last time, noted that he no longer was the tower of strength he had been in Munich (46). By now, he was suffering from chronic heart and kidney problems. Alzheimer’s physical decline coincided with the beginning of World War I, with ensuing deprivations, an increased workload and personal worries (both his son and son‐in‐law were drafted into the army). His condition worsened markedly during the second half of 1915. Alzheimer died in Breslau on December 19, 1915, aged 51 years. He was laid to rest next to this wife in Frankfurt’s main cemetery.
ACKNOWLEDGMENTS
We wish to thank Heiko Braak, Manuel Graeber, Georg Kreutzberg, Volker Roelcke and Matthias Weber for photographs, documents and helpful discussions.
REFERENCES
- 1. Alzheimer A (1891) Über einen Fall von spinaler progressiver Muskelatrophie mit hinzutretender Erkrankung bulbärer Kerne und der Rinde. Arch Psychiat Nervenkrankh 23:459–485. [Google Scholar]
- 2. Alzheimer A (1894) Die arteriosklerotische Atrophie des Gehirns. Neurol Centralbl 13:765–767. [Google Scholar]
- 3. Alzheimer A (1896) Die Frühform der allgemeinen progressiven Paralyse. Allg Z Psychiat 52:533–595. [Google Scholar]
- 4. Alzheimer A (1896) Ein “geborener Verbrecher”. Arch Psychiat Nervenkrankh 28:327–353. [Google Scholar]
- 5. Alzheimer A (1904) Histologische Studien zur Differentialdiagnose der progressiven Paralyse. In: Histologische und histopathologische Arbeiten. Nissl F, Alzheimer A (eds), 1, pp. 1–297. Fischer Verlag: Jena. [Google Scholar]
- 6. Alzheimer A (1907) Über eine eigenartige Erkrankung der Hirnrinde. Allg Z Psychiat 64:146–148. [Google Scholar]
- 7. Alzheimer A (1911) Über eigenartige Krankheitsfälle des späteren Alters. Z ges Neurol Psychiat 4:356–385. [Google Scholar]
- 8. Alzheimer A (1913) 25 Jahre Psychiatrie. Ein Rückblick anlässlich des 25jährigen Jubiläums von Professor Dr. Emil Sioli als Direktor der Frankfurter Irrenanstalt. Arch Psychiat Nervenkrankh 52:853–866. [Google Scholar]
- 9. Amaducci LA, Rocca WA, Schoenberg BS (1986) Origin of the distinction between Alzheimer’s disease and senile dementia. Neurology 36:1497–1499. [DOI] [PubMed] [Google Scholar]
- 10. Beach TG (1987) The history of Alzheimer’s disease: three debates. J Hist Med Allied Sci 42:327–349. [DOI] [PubMed] [Google Scholar]
- 11. Berrios GE (1990) Alzheimer’s disease: a conceptual history. Int J Geriat Psychiat 5:355–365. [Google Scholar]
- 12. Bethe A (1900) Über die Neurofibrillen in den Ganglienzellen von Wirbeltieren und ihre Beziehungen zu Golginetzen. Arch mikr Anat 55:513–558. [Google Scholar]
- 13. Bielschowsky M (1902) Die Silberimprägnation der Achsenzylinder. Neurol Centralbl 21:579–584. [Google Scholar]
- 14. Bielschowsky M (1903) Die Silberimprägnation der Neurofibrillen. Neurol Centralbl 22:997–1006. [Google Scholar]
- 15. Bielschowsky M (1904) Die Silberimprägnation der Neurofibrillen: einige Bemerkungen zu der von mir angegebenen Methode und den von mir gelieferten Bildern. J Psychol Neurol 3:169–189. [Google Scholar]
- 16. Binding K, Hoche A (1920) Die Freigabe der Vernichtung lebensunwerten Lebens. Ihr Mass und ihre Form. Felix Meiner Verlag: Leipzig. [Google Scholar]
- 17. Blessed G, Tomlinson BE, Roth M (1968) The association between quantitative measures of dementia and of senile change in the cerebral grey matter of elderly subjects. Br J Psychiatry 114:797–811. [DOI] [PubMed] [Google Scholar]
- 18. Blocq P, Marinesco G (1892) Sur les lésions et la pathogénie de l’épilepsie dite essentielle. Sem Méd 12:445–446. [Google Scholar]
- 19. Böhm B, Markwardt H (2004) Hermann Paul Nitsche. (1876–1948). Zur Biografie eines Reformpsychiaters und Hauptakteurs der NS‐“Euthanasie”. In: Nationalsozialistische Euthanasieverbrechen. Gedenkstätten SS (ed.), pp. 71–104. Michel Sandstein Verlag: Dresden. [Google Scholar]
- 20. Bonfiglio F (1908) Di speciali reperti in uno caso di probabile sifilide cerebrale. Riv Sper Freniatr 34:196–206. [Google Scholar]
- 21. Braak H, Braak E (2000) Neurofibrillary changes. The hallmark of Alzheimer’s disease. In: Concepts of Alzheimer Disease. Whitehouse PJ, Maurer K, Ballenger JF, (eds), pp. 53–71. Johns Hopkins University Press: Baltimore. [Google Scholar]
- 22. Danek A, Gudden W, Distel H (1989) The dream king’s psychiatrist Bernhard von Gudden. Arch Neurol 46:1349–1353. [DOI] [PubMed] [Google Scholar]
- 23. Esquirol J (1838) Des Maladies Mentales. Baillière: Paris. [Google Scholar]
- 24. Fischer O (1907) Miliare Nekrosen mit drusigen Wucherungen der Neurofibrillen, eine regelmässige Veränderung der Hirnrinde bei seniler Demenz. Monatsschr Psychiat Neurol 22:361–372. [Google Scholar]
- 25. Fischer O (1910) Die presbyophrene Demenz, deren anatomische Grundlage und klinische Abgrenzung. Z ges Neurol Psychiat 3:371–471. [Google Scholar]
- 26. Fuller SC (1907) A study of the neurofibrils in dementia paralytica, dementia senilis, chronic alcoholism, cerebral lues and microcephalic idiocy. Am J Insan 63:415–468. [Google Scholar]
- 27. Fuller SC (1911) A study of the miliary plaques found in brains of the aged. Am J Insan 68:147–219. [Google Scholar]
- 28. Gans A (1922) Betrachtungen über Art und Ausbreitung des krankhaften Prozesses in einem Fall von Pickscher Atrophie des Stirnhirns. Z ges Neurol Psychiat 80:10–28. [Google Scholar]
- 29. Gaupp. R (1916) Alois Alzheimer. Muenchener Med Wochenschr 6:195–196. [Google Scholar]
- 30. Golgi C (1906) The Neuron Doctrine—Theory and Facts. In: Nobel Lectures in Physiology or Medicine, 1901–1921. pp. 189–217. World Scientific Publishing: Singapore (1999). [Google Scholar]
- 31. Graeber MB (2006) Alois Alzheimer. Available at: http://www.ibro.info (accessed 08.04.06).
- 32. Graeber MB, Kösel S, Egensperger R, Banati RB, Müller U, Bise K, Hoff P, Möller HJ, Fujisawa K, Mehraein P (1997) Rediscovery of the case described by Alois Alzheimer in 1911: historical, histological and molecular genetic analysis. Neurogenetics 1:73–80. [DOI] [PubMed] [Google Scholar]
- 33. Graeber MB, Kösel S, Grasbon‐Frodl E, Möller HJ, Mehraein P (1998) Histopathology and APOE genotype of the first Alzheimer disease patient Auguste D. Neurogenetics 1:223–228. [DOI] [PubMed] [Google Scholar]
- 34. Grünthal E (1956) Bernhard von Gudden. In: Grosse Nervenärzte, Band I. Kolle K (ed.), pp. 127–134. Thieme Verlag: Stuttgart. [Google Scholar]
- 35. Jaspers K (1958) Philosophie und Welt. Piper Verlag: München. [Google Scholar]
- 36. Jaspers K (1973) Allgemeine Psychopathologie. Neunte unveränderte Auflage. Springer Verlag: Berlin. [Google Scholar]
- 37. Kaplan M (2005) Solomon Carter Fuller. Where My Caravan Rested. University Press of America: Lanham, MD. [Google Scholar]
- 38. Kevles DJ (1995) In the Name of Eugenics. Genetics and the Uses of Human Heredity. Harvard University Press: Cambridge, MA. [Google Scholar]
- 39. Klee E (1985) “Euthanasie” im SS Staat. Fischer Verlag: Frankfurt‐am‐Main. [Google Scholar]
- 40. Kleist K (1959) Carl Wernicke. In: Grosse Nervenärzte, Band II. Kolle K (ed.), pp. 106–128. Thieme Verlag: Stuttgart. [Google Scholar]
- 41. Klünemann HH, Fronhöfer W, Wurster H, Fischer W, Ibach B, Klein HE (2002) Alzheimer’s second patient: Johann F and his family. Ann Neurol 52:520–523. [DOI] [PubMed] [Google Scholar]
- 42. Kraepelin E (1899) Psychiatrie. Ein Lehrbuch für Studierende und Ärzte, 6. Auflage. Barth Verlag: Leipzig. [Google Scholar]
- 43. Kraepelin E (1910) Psychiatrie. Ein Lehrbuch für Studierende und Ärzte, 8. Auflage, Band II: Klinische Psychiatrie. Barth Verlag: Leipzig. [Google Scholar]
- 44. Kraepelin E (1919) Franz Nissl. Muenchener Med Wochenschr 66:1058–1060. [Google Scholar]
- 45. Kraepelin E (1920) Lebensschicksale deutscher Forscher (Alzheimer, Brodmann, Nissl). Muenchener Med Wochenschr 67:75–78. [Google Scholar]
- 46. Kraepelin E (1983) Lebenserinnerungen. Hippius H, Peters G, Ploog D (eds). Springer Verlag: Berlin. [Google Scholar]
- 47. Kreutzberg GW (1984) 100 years of Nissl staining. Trends Neurosci 7:236–237. [Google Scholar]
- 48. Lewy FH (1912) Paralysis agitans. In: Handbuch der Neurologie, Vol. 3. Lewandowsky M, Abelsdorff G (eds), pp. 920–933. Springer Verlag: Berlin. [Google Scholar]
- 49. Lombroso C (1876) L’uomo delinquente studiato in rapporto alla antropologia, alla medicina legale ed alle discipline carcerarie. Hoepli: Milan. [Google Scholar]
- 50. Maurer K, Maurer U (1998) Alois Alzheimer. Das Leben eines Arztes und die Karriere einer Krankheit. Piper Verlag: München. [Google Scholar]
- 51. Maurer K, Volk S, Gerbaldo H (1997) Auguste D and Alzheimer’s disease. Lancet 349:1546–1549. [DOI] [PubMed] [Google Scholar]
- 52. Morel BA (1857) Traité des dégénérescences physiques, intellectuelles et morales de l’espèce humaine. Baillière: Paris [Google Scholar]
- 53. Nissl F (1884) Die pathologischen Veränderungen der Nervenzellen der Grosshirnrinde. Inauguraldissertation, Universität München: München. [Google Scholar]
- 54. Nissl F (1903) Die Neuronentheorie und ihre. Anhänger. Fischer Verlag: Jena. [Google Scholar]
- 55. Nissl F (1916) Alois Alzheimer. Deutsche Med Wochenschr 42:426–427. [Google Scholar]
- 56. Onari K, Spatz H (1926) Anatomische Beiträge zur Lehre von der Pickschen umschriebenen Grosshirnrinden‐Atrophie (“Picksche Krankheit”). Z ges Neurol Psychiat 101:470–511. [Google Scholar]
- 57. Ostertag B (1963) Max Bielschowsky. In: Grosse Nervenärzte, Band III. Kolle K (ed.), pp. 3–8. Thieme Verlag: Stuttgart. [Google Scholar]
- 58. Perusini G (1909) Über klinisch und histologisch eigenartige psychische Erkrankungen des späteren Lebensalters. In: Histologische und Histopathologische Arbeiten. Nissl F, Alzheimer A (eds), 3:297–351. Fischer Verlag: Jena. [Google Scholar]
- 59. Pick A (1892) Über die Beziehungen der senilen Atrophie zur Aphasie. Prager Med Wochenschr 17:165–167. [Google Scholar]
- 60. Pick D (1989) Faces of Degeneration. A European Disorder, c.1848–c.1918. Cambridge University Press: Cambridge. [Google Scholar]
- 61. Ramón y Cajal S (1906) The structure and connexions of neurons. In: Nobel Lectures in Physiology or Medicine 1901–1921. pp. 220–253. World Scientific Publishing: Singapore (1999). [Google Scholar]
- 62. Ramón y Cajal S (1917) Recuerdos de mi vida. Moya Madrid [Translated as: Recollections of My Life]. MIT Press: Cambridge, MA (1989). [Google Scholar]
- 63. Redlich E (1898) Über miliare Sklerose der Hirnrinde bei seniler Atrophie. Jahrb Psychiat Neurol 17:208–216. [Google Scholar]
- 64. Roelcke V (2004) Nazi medicine and research on human beings. Lancet 364:6–7. [DOI] [PubMed] [Google Scholar]
- 65. Sarteschi U (1909) Contributo all’istologia patologica della presbiofrenia. Riv Sper Freniatr 35:464–484. [Google Scholar]
- 66. Scholz W (1938) Studien zur Pathologie der Hirngefässe II. Die drusige Entartung der Hirnarterien und –capillaren. Z ges Neurol Psychiat 162:694–715. [Google Scholar]
- 67. Spatz H (1959) Franz Nissl. In: Grosse Nervenärzte, Band II. Kolle K (ed.), pp. 13–31. Thieme Verlag: Stuttgart. [Google Scholar]
- 68. Spielmeyer W (1916) Alzheimer’s Lebenswerk. Z ges Neurol Psychiat 33:1–44. [Google Scholar]
- 69. Stertz G (1926) Über die Picksche Atrophie. Z ges Neurol Psychiat 101:729–749. [Google Scholar]
- 70. Stertz G (1956) Karl Bonhoeffer. In: Grosse Nervenärzte, Band I. Kolle K (ed.), pp. 17–26. Thieme Verlag: Stuttgart. [Google Scholar]
- 71. Thiele R (1956) Wilhelm Griesinger. In: Grosse Nervenärzte, Band I. Kolle K (ed.), pp. 115–127. Thieme Verlag: Stuttgart. [Google Scholar]
- 72. Weber MM (1993) Ernst Rüdin. Eine kritische Biographie. Springer Verlag: Berlin. [Google Scholar]
- 73. Weber MM (1996) Ernst Rüdin, 1874–1952: A German Psychiatrist and Geneticist. Am J Hum Genet 67: 323–331. [DOI] [PubMed] [Google Scholar]
- 74. Weber MM (1997) Aloys Alzheimer, a coworker of Emil Kraepelin. J Psychiat Res 31:635–643. [DOI] [PubMed] [Google Scholar]
- 75. Weindling P (1989) Health, Race and German Politics between National Unification and Nazism 1870–1945. Cambridge University Press: Cambridge. [Google Scholar]
- 76. Weindling P (2004) Nazi Medicine and the Nuremberg Trials: from Medical War Crimes to Informed Consent. Palgrave Macmillan: London. [Google Scholar]
- 77. Weingart P, Kroll P, Bayertz K (1992) Rasse, Blut und Gene. Geschichte der Eugenik und Rassenhygiene in Deutschland. Suhrkamp Verlag: Frankfurt‐am‐Main. [Google Scholar]
- 78. Zambianchi A (1963) Cesare Lombroso. In: Grosse Nervenärzte, Band III. Kolle K (ed.), pp. 95–100. Thieme Verlag: Stuttgart. [Google Scholar]


