Abstract
This article will discuss accidental head injuries in infants and young children. The first category of injury is the crushing head injury. Static forces applied slowly to the head result in multiple fractures of the skull and contusions and lacerations of the brain resulting from the bone fragments striking the brain.
This article will discuss the subject of short falls in young children and the resulting head injuries. Because falls are frequent events in early life, many cases have been collected and many papers written on the subject. Study of these cases is informative about the injuries likely to occur in these falls. Most often, only a minor contact injury such as scalp bruise or laceration results. In a 2 to 3% of falls, a simple linear skull fracture occurs and the majority of these are uneventful in terms of neurological deficit or intracranial bleeding. In about 1% of the fractures, an epidural or subdural hemorrhage occurs. Each of these forms of contact hemorrhages will be discussed and illustrated. While these are relatively rare injuries, it is essential that they can be identified as consistent with an accidental mechanism so that an erroneous diagnosis of inflicted injury is not made.
Keywords: epidural hemorrhage, head injury, short falls, subdural hemorrhage
INTRODUCTION
A study carried out to demonstrate the differences between accidental and inflicted injuries in children in the St. Louis Metropolitan area—with a population base of 2 million from 1975 to 1985—found 160 cases of which 63 (39%) died from accidents, 70 (43%) died from homicides and 27(16%) died from undetermined manners (4). The accidents excluded cases in which children died from gunshot wounds, drowning that occurred out of the home, fires, and vehicular accidents either as passenger or pedestrian. Of the 63 accidents, 39% were under 1 year old, 28% were between 1 and 2 years old, 8% were 2 to 3 years old and 22% were 3 years or older. Thirty‐seven (58%) of the accidental deaths were asphyxial deaths, 10 (16%) were head injuries, seven (11%) were intoxications, three (4%) were in‐home drowning, two (3%) were burns, three (4%) were electrocutions and one child died from lightning. Circumstances by which the head injuries were sustained included four children who were struck by an object (one each by a metal spear, tornado damage, rotary lawn mower and a heavy pole) and six children who fell (three from the second story, one from the ninth story, one down 13 basement stairs inside a baby walker and one child, holding onto a toy cart, down 10 basement stairs). The head injuries sustained by these children included two children with fractures with acute subdural hemorrhages, two children with penetrating wounds of the head and six children (70%) sustained massive crushing injuries with fractures and brain lacerations.
An identical study of the same population base from 1986 to 1999 found 72 cases of child injuries, of which 29% were accidents, 44% were homicides and 26% were undetermined. Forty‐three percent of the accidents were of children under 1 year old. The circumstances of injuries were similar to the study mentioned earlier, and head injuries accounted for 2 (10%) of the deaths. These head‐injury deaths—with crushing of the head—resulted from a dog attack and an event wherein child climbed into a vehicle and as the vehicle began to move the child fell out, and the vehicle ran over the head.
These studies and others have shown that most accidental deaths in and around the home—which excludes deaths from house fires, drowning outside the home, gunshot wounds and vehicular accidents—are caused by various asphyxial events. Injuries resulting from the excluded categories mentioned are usually easily identified as accidental. Difficulties arise when head trauma occurs in the home, far from the presence of an unbiased witness to provide an accurate account of what caused the injury. The neuropathology resulting from inflicted trauma has been described in an accompanying article. This article will describe the neuropathological findings in accidental head injuries in young children. In the Introduction section of this symposium, the mechanisms of head trauma were discussed and will not be described further here.
PATHOLOGY OF ACCIDENTAL HEAD INJURY
Crushing head injury
The category of crushing head injury is particularly pertinent to accidental pediatric neurotrauma. In the studies detailed previously, crushing head injuries are relatively common in the pediatric age group. Crushing head injuries are static injuries and are caused by the application of force over time periods greater than 200 ms. In a crushing head injury, the head is stationary, or at least the primary components of the injury occur in the stationary head. Massive forces literally crush the head causing fractures of the facial skeleton, calvarium and skull base. Examples of crushing injuries include: a vehicular wheel passing over the head of a pedestrian; a heavy object falling onto the head; and the head becoming fastened within a mechanical device that compresses the head. The brain injuries in a crushing head injury consist of contusions and lacerations of the brain caused by fractured bone striking and penetrating the brain. (Figure 1) There are neither coup or contrecoup contusions of the brain, but the contusions and lacerations caused by the bony fragments should be labeled as fracture contusions to properly denote their mechanism. Because there is no acceleration‐deceleration component of the injury, consciousness may not be lost initially as the head is being crushed, but unconsciousness may occur following the development of brain swelling and complications of raised intracranial pressure. Despite the extensive injury caused by this type of accident, a few studies have found that some children survive these massive injuries, and the outcome of the survivors is surprisingly good 9, 22. Some of the crushing head injuries in these studies were children who were run over by a vehicle where the wheel passed over the head, and children who pulled a heavy object—like a television—onto their heads. These cases provide evidence that dynamic injuries from impulsive forces are much more damaging than the actual physical disruption created by the crushing forces of a static injury.
Figure 1.
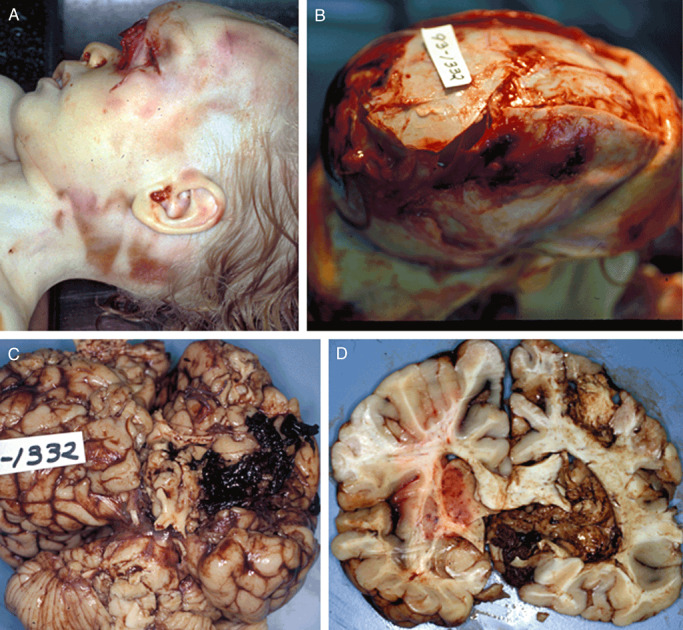
A. A 21‐month‐old male with a crushing head injury after a vehicle ran over the child in a driveway. Head of child showing abrasions from wheel and skull deformity. B. Skull showing multiple fractures and deformities from crushing injury. C. Brain showing lacerations and contusions from crushing injury. D. Coronal section of brain showing fracture lacerations and fracture contusions of brain.
Short falls
Falling is a common occurrence in children and probably every child experiences one or more falls from infancy throughout childhood. The great majority of childhood falls result in no significant head injury. Whether a particular head injury in a child has been caused by a fall is a common dilemma faced by a variety of physicians, because the history of a fall is a common scenario falsely provided by caregivers in cases where the head injury is actually an inflicted injury. A large literature on short falls in young children has accumulated to assist in understanding what injuries occur in the common household falls during childhood 5, 6, 12, 13, 15, 16, 20, 26. The short falls that occur in and around the home from distances of less than 6 ft are associated primarily with focal contact injuries such as a scalp laceration or contusion although the great majority of patients demonstrate no injury at all. About 1% to 3% of short falls in young children cause a skull fracture. These fractures are generally simple linear fractures without any associated intracranial hemorrhage or neurological deficit. Approximately less than 1% of these fractures cause an epidural hemorrhage or, even more rarely, a subdural hemorrhage; and if these hemorrhages enlarge sufficiently to become a mass lesion, death may result from increased intracranial pressure (8). In these rare incidences, either the epidural or the subdural hemorrhage is a focal injury located near or adjacent to the region of the fracture. Because fracture of the skull may arise at the point of the outbending of the bone, the fracture and hemorrhage may arise at a point different than the point of impact. A biomechanical study of bed falls using a test dummy demonstrated that rolling from a 27‐in.‐high bed onto a surface presented a low risk of contact‐type head injury (3). In short falls, even in those associated with a skull fracture, the period over which energy is delivered to the head is so short that there is little deformation of the brain substance distant to the point of impact such that there is no diffuse brain injury. Although there may be point of contact focal injury in the form of a skull fracture or fracture contusion of the brain, there is no potential for traumatic diffuse axonal injury 17, 18. A divergent view is presented in a paper by Ommaya et al proposing that in fact contact injury may distribute injury widely throughout the brain of a young child (21). However, this view is not supported by the literature noted earlier that looked at hundreds of cases of short falls and found that the great majority produced no loss of consciousness or neurological deficit 5, 6, 12, 13, 15, 16, 20, 26.
Falls from great heights
Falls from a height are a major cause of accidental injury and death especially in urban children where they are vulnerable to falling from tall buildings. One study of 61 children under 16 years of age who were admitted to a hospital after falling from a height found that all of the children who fell from three stories or less survived, and a 50% mortality rate occurred for those who fell from the fifth to sixth story (1). Twenty‐three percent of the children died and the cause of death in 11 of the 14 children (78%) who died was lethal head injury. The head injuries consisted of skull fractures and brain contusions identical to those seen in crushing head injuries. Of 70 children—from 10 months to 15 years old—admitted to the hospital after sustaining a fall from a height greater than 10 feet and up to 17 stories all survived their injuries (19). Fifty percent were under 3 years of age and most of the falls were from a height of one to three stories. The most common injury in these children was head injury, seen in 54% of the cases, and consisted of skull fractures and intracranial hemorrhages.
Epidural hemorrhage
Epidural hemorrhage occurs in about 3% of all head injuries with the highest incidence between 10 and 30 years of age (2). Epidural hemorrhages are uncommon under 2 years of age and after 60 years because the dura is very firmly adherent to the inner table of the skull (14). Of 738 head injuries in children under 16 years of age, Hahn found that epidural hemorrhages accounted for 44% of the intracranial hemorrhages, and that 75% of these hemorrhages occurred in children under 3 years old (11). In about 85% of cases, epidural hemorrhage is associated with skull fracture (23). Children under 15 years old are less likely to have a fracture associated with development of an epidural hemorrhage. Bleeding in an epidural hemorrhage usually arises from laceration of a branch of the middle meningeal artery when the dura is separated away from the inner table of the skull. Fracture of the skull may lacerate small branches of the middle meningeal artery where these vessels lie in grooves on the inner table of the skull. In children, an impact to the head may cause deformity of the skull without causing a fracture, but this is sufficient to separate the dura from the inner table and tear the small vessels. The grooves on the inner table of the skull in which the small vessels lie do not develop until 4 years of age when the diploe of the skull develops (10). In some cases, epidural bleeding arises from tears of a dural sinus or diploic vein rather than arterial vessels. Variations in whether the source of bleeding is arterial or venous determine how rapidly the hemorrhage enlarges.
Epidural hemorrhage is a contact injury and requires an impact to the head. Epidural hemorrhages in young children arise most commonly from falls. These are much less common from an inflicted blow to the head that is more likely to produce acceleration of the head with diffuse brain injuries. However, it is possible to inflict blows to the stationary head and cause an epidural hemorrhage.
Epidural hemorrhages occur most commonly over the cerebral convexities most often in the parietal and temporal regions, although they may occur in the frontal region or the occipital‐posterior fossa. Epidural hemorrhages in the posterior fossa tend to be of venous origin and even small amounts may be significant as mass lesions. Epidural hemorrhages over the cerebral convexities are usually limited to one side by the firm attachment of the dura at the sagittal suture. Epidural bleeding into the lifted‐out dura creates a lens‐shaped configuration of the hematoma and markedly flattens out the underlying gyral surfaces (Figure 2). The gyral surface beneath an epidural hemorrhage will frequently have contusions and subarachnoid hemorrhage caused by the adjacent skull fracture. The volume of epidural blood needed to act as a mass lesion is about 100 mL in an adult and much less in children (23). Epidural hemorrhages over the cranial fossae may create problems with increased intracranial pressure in much smaller volumes than those over the convexity (Figure 3). The evolution of an epidural hemorrhage may be observed by serial computed tomography (CT) scans;. not all hemorrhages continue to bleed but may stop and then be resorbed.
Figure 2.
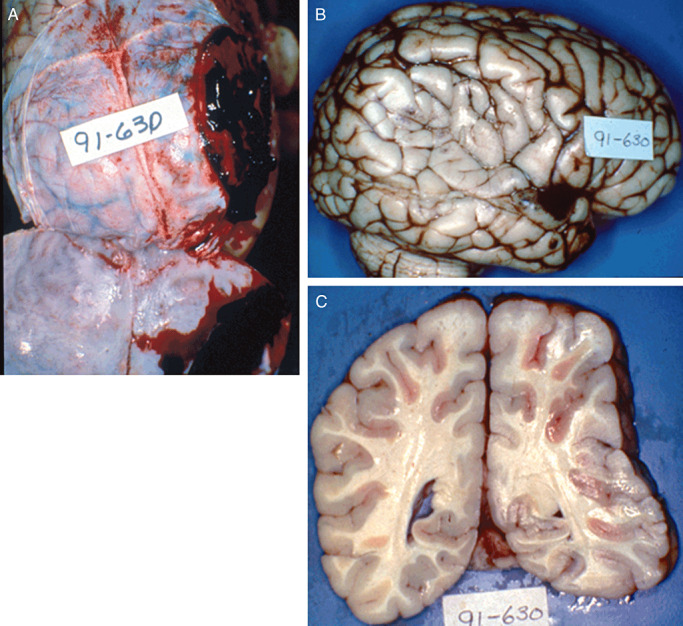
A. A 2‐year‐old child struck on head with object, with a fracture of right parietal bone and an 80‐mL epidural hemorrhage over the right temporoparietal convexity. B. Marked flattening of right parietal lateral convexity with fracture contusions of right superior and middle temporal gyri. C. Coronal section of brain showing marked flattening of right parietal lobe.
Figure 3.
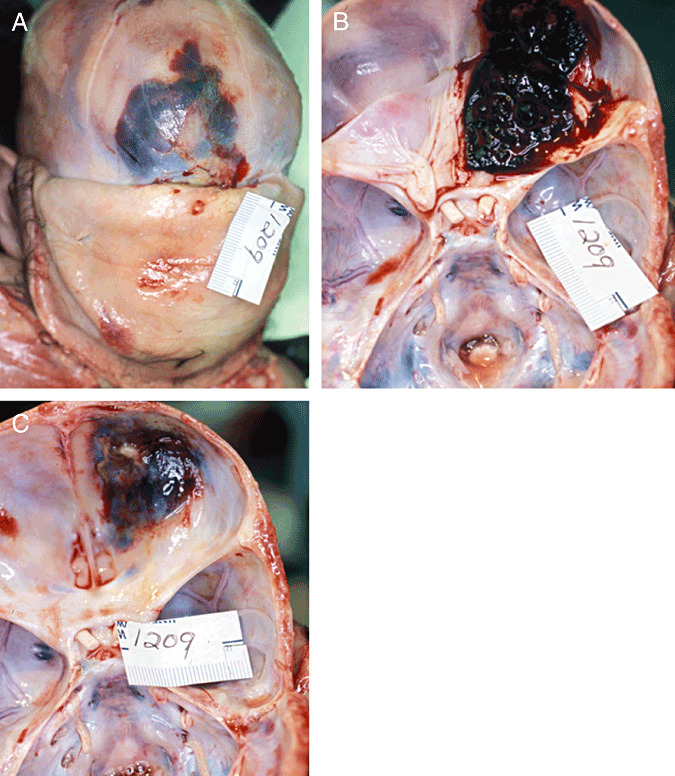
A. A 4‐month‐old male (Case 1 in Table 1), who fell from bed and struck a table, with fractures of the right frontal bone and the right orbital plate. B. Epidural hemorrhage over right anterior cranial fossa. C. Fracture of right orbital plate.
The dura is the periosteum of the skull and is adherent to the inner table of the skull and more firmly adherent during the younger and older ages. Microscopically, the epidural surface of the dura in young children has a layer of cells comprised of osteoclasts and fibroblastic cells. Pigment resembling hemosiderin is often present in the osteoclastic cells. Sometimes, the epidural surface is mistakenly interpreted as an organizing subdural membrane because of the cellular elements that resemble macrophages bearing hemosiderin. The epidural surface may have actual spicules of osteoid tissue. The younger the child, the more reactive the dural osteoblastic activity appears.
The clinical significance of an epidural hemorrhage depends upon its association with other brain injuries and with the size and rate of development of the hemorrhage. Cases of epidural hemorrhages that are the only head injury have a near 0% mortality rate with prompt diagnosis and treatment (25). Those epidural hemorrhages that are associated with diffuse brain injury have much greater mortality. Despite the near 0% mortality, in the last 10 years the author has seen four children die from epidural hemorrhages. In the two studies described previously in this section covering the years 1975 to 1999 in the St. Louis metropolitan region, there were no cases of accidental head injury with epidural hemorrhages. Since that time period, the author has seen four cases of children dying from accidental head injuries with epidural hemorrhages (Table 1). In Cases 2 and 3, the children were not taken to medical care because the parents did not recognize that the symptoms they observed in the children needed medical attention. In Case 1, after falling out of bed, the infant was seen in the emergency department of a children's hospital and had a CT scan that was read as negative despite a fracture. Case 4 was taken to a community hospital and had a CT scan that showed an epidural hemorrhage but it was thought not to be causing a mass lesion. He was treated supportively without surgical intervention and died.
Table 1.
Epidural hemorrhages in accidental falls in young children.
| Case number | Case history | Age | Sex | How accident occurred | Findings |
|---|---|---|---|---|---|
| 1 | Taken to a children's hospital and had a CT scan that was read as normal; would not eat or sleep well; survived for 2 days; taken to pediatrician and died on way to the office. | 4 months | Male | Fell out of adult bed and struck edge of bedside table. | Right forehead contusion; fracture of right frontal bone and right orbital plate; epidural hemorrhage over right anterior cranial fossa. |
| 2 | Complained of headache and vomited several times over next 12 h; found dead in morning. | 7 years | Female | Fell off tree stump about 3‐ft high and hit the back of the head. | Right frontal subgaleal hemorrhage; fracture of right frontal bone extending to coronal suture posteriorly; epidural hemorrhage over left frontal; small contusions of left superior and middle temporal gyri. |
| 3 | Cried after fall; able to be comforted; vomited but then put back to bed; found dead in bed in morning. | 21 months | Male | Fell out of bed. | Left temporal subgaleal hemorrhage; left temporal linear fracture; large epidural hemorrhage over left lateral temporoparietal convexity. |
| 4 | Found on ground with an overturned bike; combative; became somnolent in emergency room; CT showed fracture of right temporal; became unresponsive; neurosurgery consulted and recommended observation; died 2 days later. | 10 years | Male | Riding bike and fell off; not wearing a helmet. | Right temporal scalp contusion; fracture of right temporal skull; epidural hemorrhage over right perital; contrecoup contusions of left temporal lobe. |
Subdural hemorrhage
Unlike epidural hemorrhage that requires an impact and is most commonly associated with a skull fracture, subdural hemorrhage does not require impact but may result from inertial forces alone. Most subdural hemorrhages are in the class described in the Introduction of this symposium as diffuse injuries, but subdural hemorrhages may also be a focal injury and the result of impact to the head. Although experimental forms of subdural bleeding can be produced by inertial forces alone, in reality in most circumstances of injury impact occurs either as the initiator of accelerating the head into motion or occurs when the head is decelerated by striking an object or surface. The common causes of subdural hemorrhages at other ages—vehicular accidents, falls and sporting events—are not common causes of subdural hemorrhage in infants and young children. Infants and young children spend most of their time in the home and not in activities that cause head injuries in older groups. The most common cause of subdural hemorhage in the young age group is abusive head injury.
Subdural hemorrhage in certain circumstances deserves mention. Accidental circumstances that might produce inertial acceleration deceleration forces to the head to of a child have been studied as possible causes of inertial subdural hemorrhages in young children. A report of a playground rocking toy—described as a motorcycle‐shaped toy mounted on a large spring—caused a head injury with subdural hemorrhage in a 2‐year‐old boy (24). The child was in the care of a 12‐year‐old caretaker and was accompanied by his 3‐year‐old and 6‐year‐old brothers. The 2‐year‐old boy sat on the rocking toy as the 6‐year‐old was shaking it from behind and the 12‐year‐old was holding the handlebars and pushing the toy back. After 4 to 5 minutes of intense violent rocking, the 2‐year‐old lost his grip and his head struck the handlebars. He cried and a bruise appeared on his forehead but he then returned to play. The boys went home shortly afterwards and the child seemed fine and was put to bed about 1 1/2 h later. During the night, it was noticed that the child was breathing irregularly and he was taken to the hospital. He died as the subdural hemorrhage was being evacuated. Autopsy demonstrated a 10 × 9‐cm bruise on the forehead. There was evidence of surgical drainage of a left subdural hemorrhage and a residual right subdural hemorrhage, bilateral subarachnoid hemorrhages, diffuse cerebral swelling and multiple bilateral retinal hemorrhages extending out to the ora serrata. After investigation, it did appear that the stories of the three children were consistent and that the details of the rocking incident were truthful. In this incident, there was an impact to the handle bars that terminated the intense rocking. Occasionally, rocking chairs have been implicated as causes of diffuse subdural hemorrhages in young children. The author has seen two such cases where such a mechanism was alleged in over 30 years of forensic practice. Both cases involved toddler‐aged children standing up on a rocking chair, facing the back and holding on to the chair and rocking the chair. The child then lost his grip and catapulted from the chair and fell to the ground striking the head. The head injuries sustained were lethal and consisted of a thin layer of subdural blood over the cerebral convexities and a few retinal hemorrhages. These cases were placed into the category of “undetermined” manner of death because although the rocking chair scenario was a possible mechanism for creating inertial brain injury, the only witness is each case was the caretaker and the veracity of the account may not be truthful.
Contact mechanisms can also produce subdural hemorrhage. Of the 1% to 3% of short falls that caused a skull fracture, in a very rare number of cases, the skull fracture is accompanied by a contact subdural hemorrhage. These cases result from skull deformation and the subdural hemorrhage is localized to the area of contact. Denton and Milueusnic reported such a case (8). A 9‐month‐old male fell backwards off the edge of a queen‐sized bed elevated 30 in. to a concrete floor, an event witnessed by the grandmother. In falling, he rotated off the bed from a sitting position striking the back of his head. He immediately cried and the grandmother placed ice on his bump. He then appeared fine. He was taken to a babysitter's residence and the babysitter was told about the fall and was asked to watch for any change in behavior. The mother picked up the child later in the day and the child still appeared fine. Approximately 72 h after the fall, the child was found in bed unresponsive and was pronounced dead shortly thereafter on arrival in the emergency department. At autopsy, there was right parietal subgaleal hemorrhage and a linear fracture of the right parietal skull 3 in. long extending to the right parieto‐occipital suture and causing mild diastasis. There was a thin, adherent clotted 2 × 2 × 0.1 cm subdural hemorrhage underlying the fracture. The brain showed severe edema with herniation. Coronal sections of the cerebrum showed a focal 1‐mm tear of the midsuperior corpus callosum surrounded by 2 mm of hemorrhage. Microscopically, the tear showed hemorrhage with intact red blood cells, focal axonal injury and microglial activation without inflammation. The brain showed no evidence of diffuse axonal injury. The subgaleal hemorrhage showed hemorrhage with neutrophilic inflammation. The eyes were examined by an ophthalmic pathologist and were found to be normal. The authors analyzed the fall and autopsy findings and felt that the rotational component of the fall could account for the injuries found at autopsy. The several caretakers of the child had consistent accounts. So although a rare occurrence, this case appears to represent an example of a low‐level fall causing a fracture and a focal contact, subdural hemorrhage with delayed deterioration and resulting in death from brain swelling.
Brain contusions
Contusions of the brain in young children are commonly seen adjacent to skull fractures and these contusions should be labeled fracture contusions. Coup and contrecoup contusions do not or only rarely occur in children under about 4 years of age. Several reasons account for this lack of brain contusions. The very soft consistency of the young brain makes the brain less likely to contuse than to tear when significant force is applied to the head. Lesions described as contusion tears were discussed in the accompanying article on inflicted traumatic injury in infants and young children. On rare occasions, coup contusions may occur in young children but appear more like a faint blush on the cortical surface rather than a fully developed hemorrhagic contusion. Cross‐sections of these blush contusions reveal little hemorrhagic component within the cortical lamina. There is little or no associated subarachnoid hemorrhage. Contrecoup contusions occur when a moving head is accelerated by falling from a standing position to produce a torque action on the body, and then the head strikes a hard surface (7). A young child does not fall in a manner similar to a rigid body—which is needed to produce head acceleration. A young child is already near the surface as they strike on falling, and their fall does not accelerate the head. After about 4 years of age, children falling from a standing height will show the typical pattern of contrecoup contusions.
REFERENCES
- 1. Barlow B, Niemirska M, Rajindar P, Gandi RP, Leblanc W (1983) Ten years pf experience with falls from a height in children. J Pediatr Surg 18:509–511. [DOI] [PubMed] [Google Scholar]
- 2. Baykaner K, Alp H, Ceviker N, Keskil S, Seckin Z (1988) Observation of 95 patients with extradural hematoma and review of the literature. Surg Neurol 30:339–341. [DOI] [PubMed] [Google Scholar]
- 3. Bertocci GE, Pierce MC, Deemer E, Aguel F, Janosky JE, Vogeley E (2003) Using test dummy experiments to investigate pediatric injury risk in simulated short‐distance falls. Arch Pediatr Adolesc Med 157:480–486. [DOI] [PubMed] [Google Scholar]
- 4. Case MES (1994) Head injury in child abuse. Chapter 5. In: Child Maltreatment. Broduer AE, Monteleone JA (eds), pp. 75–87. GW Medical: St. Louis, MO. [Google Scholar]
- 5. Chadwick DL, Salerno C (1993) Likelihood of the death of an infant or young child in a short fall of less than 6 vertical feet. J Trauma 35:968. [PubMed] [Google Scholar]
- 6. Chadwick DL, Chin S, Salerno CS, Landsverk J, Kitchen L (1991) Deaths from falls in children: how far is fatal? J Trauma 13:1353–1355. [DOI] [PubMed] [Google Scholar]
- 7. Dawson SL, Hirsch CS, Lucas FV, Sebek BA (1980) The contrecoup phenomenon: reappraisal of a classic problem. Hum Pathol 11:155–166. [DOI] [PubMed] [Google Scholar]
- 8. Denton S, Miluesnic D (2003) Delayed sudden death in an infant following an accidental fall: a case report with review of the literature. J Forensic Med Pathol 24:371–376. [DOI] [PubMed] [Google Scholar]
- 9. Duhaime AC, Eppley M, Margulies S, Heher K, Scott P (1995) Crush injuries to the head of children. Neurosurgery 37:401–407. [DOI] [PubMed] [Google Scholar]
- 10. Freytag E (1963) Autopsy findings in head injuries from blunt forces. Arch Pathol 75:402–413. [PubMed] [Google Scholar]
- 11. Hahn YS, Chung C, Barthel MJ, Balies J, Flannery AM, McLone DG (1988) Head injuries in children under 36 months of age. Childs Nerv Syst 4:34–40. [DOI] [PubMed] [Google Scholar]
- 12. Helfer RE, Slovis TL, Black M (1977) Injuries resulting when small children fall out of bed. Pediatrics 60:533–535. [PubMed] [Google Scholar]
- 13. Hymel KP, Bandak FA, Portington MD, Winston KR (1998) Abusive head trauma? A biomechanics‐based approach. Child Maltreat 3:116–128. [Google Scholar]
- 14. Jamieson KG, Yellan JD (1968) Extradural hematoma: report of 167 cases. J Neurosurg 29:13–23. [DOI] [PubMed] [Google Scholar]
- 15. Kravitz H, Driessen F, Gomberg R, Korach A (1969) Accidental falls from elevated surfaces in infants from birth to one year of age. Pediatrics 44(Suppl.):869–876. [PubMed] [Google Scholar]
- 16. Lyons JL, Oates RK (1993) Falling out of bed: a relatively benign occurrence. Pediatrics 92:125–127. [PubMed] [Google Scholar]
- 17. Maxwell WL, Povlishock JT, Graham DL (1997) A mechanistic analysis of nondisruptive axonal injury: a review. J Neurotruma 14:419–440. [DOI] [PubMed] [Google Scholar]
- 18. Meythaler JM, Peduzzi JD, Eleftheriou E, Novak TA (2001) Current concepts: diffuse axonal injury—associated traumatic brain injury. Arch Phys Med Rehabil 82:1461–1471. [DOI] [PubMed] [Google Scholar]
- 19. Musemeche CA, Barthel M, Cosentino C, Reynolds M (1991) Pediatric falls from heights. J Trauma 31:1347–1349. [DOI] [PubMed] [Google Scholar]
- 20. Nimitiyongskul DL, Anderson L (1987) The likelihood of injuries when children fall out of bed. J Pediatr Orthop 7: 184–186. [DOI] [PubMed] [Google Scholar]
- 21. Ommaya A, Goldsmith W, Thibault L (2003) Biomechanics and neuropathology of adult and paediatric head injury. Br J Neurosurg 16:220–242. [DOI] [PubMed] [Google Scholar]
- 22. Prasad M (1999) Crush head injuries in infants and young children: neurologic and neuropsychiatric sequelae. J Child Neurol 14:496–501. [DOI] [PubMed] [Google Scholar]
- 23. Rivas JJ, Lobato RD, Sarabia R, Cordobes F, Cabrera A, Gomez P (1988) Extradural hematoma: analysis of factors influencing the courses of 161 patients. Neurosurgery 23:44–51. [DOI] [PubMed] [Google Scholar]
- 24. Sauvageau A, Bourgault A, Racette S (2008) Cerebral traumatism with a playground rocking toy mimicking shaken baby syndrome. J Forensic Sci 53:479–482. [DOI] [PubMed] [Google Scholar]
- 25. Servadei F (1997) Prognostic factors in severely head injured patients with epidural hemtomas. Acta Neurochir 139:273–278. [DOI] [PubMed] [Google Scholar]
- 26. Williams RA (1991) Injuries in infants and small children resulting from witnessed and corroborated free falls. J Trauma 31:1350–1352. [DOI] [PubMed] [Google Scholar]


