Abstract
Objective:
The aim of the study was to evaluate the prevalence of root canal isthmus (RCI) and measure the interorifice distance (IOD) between the root canals. Additionally to correlate IOD with the RCI in human permanent teeth using conebeam computed tomography (CBCT) in an Indian sub-population (Chennai).
Materials and Methods:
A total of 5881 teeth from 280 CBCT full mouth scans were analyzed. The presence or absence of complete and incomplete RCI of each tooth was identified using the map-reading strategy. IOD was calculated by measuring the distance between the center of each root canal orifice to that of the center of the adjacent orifice at the level of the cementoenamel junction using the axial and sagittal sections. Chi-square analysis and correlation statistics using Spearman's rank-order test was done (P < 0.05).
Results:
High prevalence of RCI was found in maxillary first premolars, mesial root of mandibular molars, and mesiobuccal root of maxillary first molars, while its prevalence was low in maxillary canines and mandibular premolars and absent in maxillary incisors. RCI was predominantly seen in the cervical and middle third of the root canal in all the teeth evaluated. A weak negative correlation was established between the IOD and RCI for maxillary premolars, whereas a weak positive correlation was seen in maxillary first molars and mandibular second molars.
Conclusion:
The prevalence of RCI was high in the posterior teeth in comparison to the anterior teeth in the present study. There was no strong correlation between IOD and RCI in all the teeth evaluated.
Keywords: Cone-beam computed tomography, dental anatomy, human permanent teeth, isthmus, root canal system
INTRODUCTION
The human root canal system (RCS) is highly complex and variable.[1] Disinfection of the entire RCS is essential for the success of root canal therapy.[2,3] Certain parts of the RCS such as canal isthmus, lateral canals, and accessory canals are difficult to disinfect.[4] Root canal isthmus (RCI) is defined as a channel/corridor of communication between two canals that contain pulp/pulpally derived tissue.[5] Weller et al.[2] described RCI into two types; complete or incomplete. Hsu and Kim et al.[3] classified it into five different types, however both these studies had used sectioning to identify and classify the RCI. Microcomputed tomography (micro-CT) studies describe RCI to be a highly complex network that branches and extends longitudinally. Fan et al.[6] using micro-CT classified RCI into four types, namely: Type I-sheet connection, Type II-separate, Type III-mixed, and Type IV-cannular.
Recent cone-beam computed tomography (CBCT) and micro-CT studies have reported a high prevalence of RCI.[7,8,9] In CBCT images, RCI can be identified using the map reading strategy suggested by Pécora et al.[10] So far, these studies have mostly been done in the Brazilian,[10] Iranian,[11] and Chinese populations.[12] It is a well-established fact that the root canal anatomy varies in different populations and similarly, the prevalence of RCI might also vary among different populations.[11] To the best of our knowledge, there have been no published studies on the frequency of RCI in an Indian population.
RCI is commonly seen in single roots with two canals, such as the mesial root of the mandibular molars. It has been reported that when the distance between two orifices in a single root having two canals is <3 mm, these root canals often merge before their exit.[13] However, if the interorifice distance (IOD) is more than 3 mm, the canals remain separate. Similarly, it can be speculated that if the root canals are closer together, the chances of RCI being present could also be very high.
The aim and purpose of this retrospective study was to evaluate the frequency of RCI in human permanent teeth using a sample of CBCT images obtained from an Indian subpopulation (Chennai). The secondary objective of this study was to determine the IOD between the root canals and their correlation with RCI.
MATERIALS AND METHODS
Cone-beam computed tomography image selection
The study was conducted after obtaining approval from the Institutional Review Board of Meenakshi Academy of Higher Education and Research (MADC/IRB-XVIII/2018/330). A total of 5881 CBCT images of teeth (272 mandibular first molars, 246 mandibular second molars, 406 mandibular first premolars, 396 mandibular second premolars, 472 mandibular central incisors, 486 lateral incisors, 521 mandibular canines, 379 maxillary first molars, 335 maxillary second molars, 439 maxillary first premolars, 436 maxillary second premolars, 481 maxillary central incisors, 505 maxillary lateral incisors, and 507 maxillary canines) from 280 full mouth scans were taken up for analysis. Patients (age group: 16–78 years; gender: 156 males, 152 females) were referred for CBCT imaging by private clinics for purposes not related to this study between 2018 and 2019. Only adult human teeth with fully matured roots were included in the study. Teeth with dental caries, resorption, calcification, root fractures, crowned, and previously root canal treated teeth were excluded from the study.
Cone-beam computed tomography imaging method
All images were taken by Kodak 9500 CB3D scan system (Onex Corporation, Toronto, Canada), using the following settings: thickness 0.200 mm; field of view 18 cm × 20 cm; tube voltage 90 kVp; tube current, 10 mA; and exposure time 10.8 s. Images were examined using the Horos software (Version 3.1.2, Nimble Co LLC d/b/a Purview in Annapolis, Maryland, USA).
Root canal isthmus detection (map reading strategy)
The presence or absence of RCI was determined using the map reading strategy suggested by Pécora et al.[10] The involved teeth were viewed in sagittal, coronal, and axial planes from the cementoenamel junction (CEJ) till the apical foramen, and the RCI was classified into six different categories, namely CT-CT (beginning and ending in the cervical third), CT-MT (beginning in the cervical and ending in the middle third), CT-AT (beginning in the cervical third and ending in the apical third), MT-MT (beginning and ending in the middle third), MT-AT (beginning in the middle and ending in the apical third), and AT-AT (beginning and ending in the apical third).[10] Analysis of both complete and incomplete RCI was also done. The interpretation was done by two precalibrated endodontists having more than 5 years of experience (N. V, S. P). The interexaminer reliability was calculated using the Cohen kappa test, by comparing the interpretation of two investigators (N. V, S. P), who independently assessed 30 CBCT scans. Intraexaminer reliability was assessed by asking the investigators (N. V, S. P) to interpret the same CBCT scans after a period of 15 days.
Interorifice distance
IOD was measured by viewing the sagittal and axial sections of the roots containing more than one canal at the CEJ level. The IOD was calculated by measuring the distance between the center of each root canal orifice to that of the center of the adjacent orifice using the CBCT software.
Root canal pattern
The type of root canal pattern was classified using the Vertucci's classification.[1] In addition, any canal pattern that could not be classified under this classification was grouped using the Sert and Bayirli classification.[14]
Statistical analysis
The data obtained were subjected to statistical analysis using the SPSS software (v. 19, IBM, USA). The difference in the IOD with and without RCI and the difference in the prevalence of RCI between males and females were assessed for statistical significance using the Chi-square test for proportion. Correlation between the prevalence of RCI with age and IOD was checked using the Spearman's rank-order test. P < 0.05 was considered as the significance limit.
RESULTS
Cohen's Kappa test value for interexaminer reliability was 0.837 and for intraexaminer reliability was 0.920 and 0.911. Among the 5881 teeth assessed, the prevalence of RCI was seen to be highest in the maxillary first premolars (94%) and lowest in the maxillary canine teeth (3%). The prevalence of RCI of all other remaining teeth is given in Table 1.
Table 1.
Prevalence of root canal isthmus
| Teeth | Root | Prevalence of teeth with RCI (%) | Region-wise occurrence | Total number of RCI present | |||||
|---|---|---|---|---|---|---|---|---|---|
| CT-CT | CT-MT | CT-AT | MT-MT | MT-AT | AT-AT | ||||
| First mandibular molar (n=272) | Mesial | 224 (82.3) | 157 | 37 | 16 | 71 | 10 | 16 | 307 |
| Distal | 53 (19.5) | 16 | 26 | 5 | 18 | 4 | 1 | 70 | |
| Second mandibular molar (n=246) | Mesial | 209 (85) | 100 | 66 | 16 | 68 | 18 | 6 | 209 |
| Distal | 5 (2) | 1 | 3 | 0 | 2 | 0 | 0 | 5 | |
| First mandibular premolar (n=406) | Single/double root | 47 (11.5) | 4 | 9 | 0 | 25 | 9 | 4 | 51 |
| Second mandibular premolar (n=396) | Single root | 13 (3) | 7 | 3 | 0 | 3 | 0 | 0 | 13 |
| First maxillary molar (n=379) | Mesiobuccal | 290 (76.5) | 94 | 123 | 28 | 60 | 0 | 40 | 345 |
| Distobuccal | 2 (0.5) | 0 | 1 | 0 | 1 | 0 | 0 | 2 | |
| Second maxillary molar (n=335) | Mesiobuccal | 145 (43.2) | 27 | 36 | 12 | 28 | 4 | 3 | 110 |
| First maxillary premolar (n=439) | Single/double root | 413 (94) | 306 | 41 | 18 | 79 | 3 | 15 | 462 |
| Second maxillary premolar (n=436) | Single/double root | 275 (63) | 131 | 44 | 20 | 96 | 5 | 24 | 320 |
| Mandibular lateral incisor (n=486) | Single root | 153 (31) | 7 | -/- | -/- | 143 | 3 | -/- | 153 |
| Mandibular central incisor (n=472) | Single root | 107 (23) | 8 | -/- | -/- | 98 | 1 | -/- | 107 |
| Mandibular canine (n=521) | Single root | 60 (11) | 4 | -/- | -/- | 54 | 1 | 1 | 60 |
| Maxillary canine (n=507) | Single root | 15 (3) | -/- | -/- | -/- | 15 | -/- | -/- | 15 |
RCI: Root canal isthmus, CT: Cervical third, MT: Middle third, AT: Apical third
Mandibular posterior teeth
Among the mandibular posteriors assessed, first molars showed the highest prevalence of RCI, followed by second molars, first premolars, and second premolars.
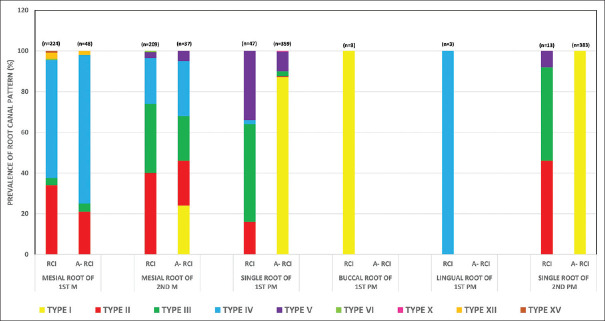
In the 272 first molars assessed, 82.3% of mesial roots and 19.5% of distal roots had the presence of RCI, while 15.1% showed the presence of RCI in both mesial and distal roots. In the mesial roots, majority of RCI were seen in the CT-CT region (51%) [Table 1]. Vertucci's Type IV root canal pattern (58.4%) was most prevalent in teeth with RCI [Figure 1]. In the distal roots, majority of RCI were seen in the CT-MT region (37%) [Table 1]. Type II root canal pattern (49%) was most prevalent in teeth with RCI [Figure 1].
Figure 1.
Prevalence of root canal pattern in mandibular posterior teeth. RCI: Root canal isthmus, A-RCI: Absence of root canal isthmus, M: Molar, PM: Premolar
In the 246 second molars assessed, 85% of mesial roots and 2% of distal roots revealed the presence of RCI. Another 2% had RCI in both the mesial and distal root. In the mesial roots, RCI was predominantly seen in the CT-CT region (36.4%) [Table 1]. Type II root canal pattern was most prevalent in teeth with RCI in both mesial (40.1%) and distal roots (60%) [Figure 1].
In the 406 first premolars assessed, 11.5% of teeth revealed the presence of RCI. The incidence of RCI was most commonly seen in the MT-MT region (49%) [Table 1]. Among the teeth with RCI (11.5%), 94% had a single root with type III root canal pattern (48%) being the most common, while 6% of teeth had two roots and showed type I root canal pattern (100%) in all of them [Figure 1].
In the 396 second premolars assessed, only 3% of teeth revealed the presence of RCI. The incidence of RCI was most commonly seen in the CT-CT region (54%) [Table 1], with type II and type III root canal patterns (46%) being equally predominant [Figure 1].
Maxillary posterior teeth
Among the maxillary posteriors assessed, maxillary first premolars showed the highest prevalence of RCI, followed by the first molars, second premolars, and molars, respectively.
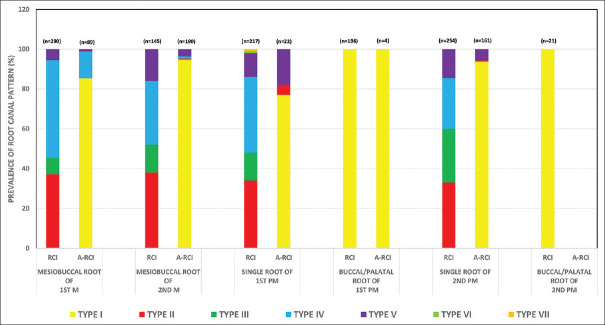
In the 379 first molars assessed, 76.5% of mesiobuccal roots, 0.5% of distobuccal roots, and none of the palatal roots showed the presence of RCI. In the mesiobuccal roots, RCI was predominantly seen in the CT-MT region (35.5%) [Table 1]. Type IV root canal pattern was most commonly seen in the mesiobuccal roots (49%) and type III root canal pattern in the distobuccal roots (100%) of teeth with RCI [Figure 2]. The prevalence of a second mesiobuccal (MB2) canal was 80%.
Figure 2.
Prevalence of root canal pattern in maxillary posterior teeth. RCI: Root canal isthmus, A-RCI: Absence of root canal isthmus, M: Molar, PM: Premolar
In the 335 second molars assessed, 43.2% of mesiobuccal roots showed the presence of RCI. RCI was not present in any of the distobuccal and palatal roots assessed. RCI was most commonly seen in the CT-MT region (33%) [Table 1]. Type II root canal pattern was predominant in the mesiobuccal roots (37.9%) of teeth with RCI [Figure 2]. The prevalence of the MB2 canal was 46.2%.
In the 439 first premolars assessed, 94% of teeth showed the presence of RCI. RCI was most commonly seen in the CT-CT region (66.2%) [Table 1]. In teeth with RCI, 52.5% had a single root and type IV root canal pattern was most prevalent (38.2%). About 47.5% had two roots and type I root canal pattern (100%) was seen in all teeth [Figure 2].
In the 436 second premolars assessed, 63% of teeth showed the presence of RCI. RCI was predominantly seen in the CT-CT region (41%) [Table 1]. In teeth with RCI, 92.3% had a single root and type II root canal pattern (33%) was predominant. 7.6% had two roots and type I root canal pattern (100%) was seen in all teeth [Figure 2].
Mandibular and maxillary anterior teeth
The prevalence of RCI in mandibular laterals, centrals, and canines was 31%, 23%, 11%, respectively. Among the maxillary teeth, only canines (3%) showed the presence of RCI. Majority of the RCI (>90%) were seen in the MT-MT region in all these teeth [Table 1]. Type III root canal pattern was most commonly seen in the mandibular incisors (97%), mandibular canines (83%), and maxillary canines (87%) with RCI. The remaining anterior teeth displayed a type I root canal pattern without the presence of RCI.
Prevalence of root canal isthmus in relation to interorifice distance, gender, and root canal pattern
The average IOD for the mandibular and maxillary posterior teeth is given in Tables 2a and b, respectively. There was no significant difference in IOD between the teeth with and without RCI. With regard to gender, there was no significant difference seen in all the posterior teeth, excepting the maxillary second premolars wherein, males had a significantly higher prevalence of RCI compared to females (P < 0.001). The prevalence of root canal pattern in mandibular and maxillary posteriors in teeth with and without RCI is given in Figures 1 and 2, respectively.
Table 2a.
Mean interorifice distance in mandibular molars (mm)
| Mandibular teeth | M-D | MB-ML | MB-D | ML-D | MB-DB | ML-DL | DB-DL | M-DB | M-DL | MM-MB | MM-ML |
|---|---|---|---|---|---|---|---|---|---|---|---|
| First molar (with RCI) | 3.1 | 2.6 | 3.5 | 3.3 | 3.5 | 3.6 | 2.3 | 3.4 | -/- | 1.6 | 1.5 |
| First molar (without RCI) | 3.8 | 2.7 | 3.7 | 3.5 | 3.5 | 3.4 | 3 | 3.4 | 3.8 | 1.2 | 1.2 |
| Second molar (with RCI) | 4.8 | 1.7 | 3.8 | 3.8 | 3.7 | 3.7 | 1.7 | -/- | -/- | -/- | -/- |
| Second molar (without RCI) | 3.7 | 1.4 | 3.9 | 3.9 | -/- | -/- | -/- | -/- | -/- | -/- | -/- |
RCI: Root canal isthmus, M: Mesial, D: Distal, MB: Mesiobuccal, ML: Mesiolingual, DB: Distobuccal, DL: Distolingual, MM: Middle mesial
Table 2b.
Mean interorifice distance for maxillary molars (in mm)
| Maxillary teeth | MB-DB | MB-MB2 | MB-P | MB2-P | DB-P |
|---|---|---|---|---|---|
| First molar (with RCI) | 2.7 | 2.1 | 5.3 | 3.7 | 3.8 |
| First molar (without RCI) | 2.6 | 2.2 | 5.3 | 3.9 | 3.8 |
| Second molar (with RCI) | 2.4 | 2.1 | 5 | 3.6 | 3.9 |
| Second molar (without RCI) | 2.3 | 2.3 | 5 | 3.5 | 3.9 |
RCI: Root canal isthmus, MB: Mesiobuccal, DB: Distobuccal, MB2: Second mesiobuccal, P: Palatal
Correlation statistics
Age and root canal isthmus
A statistically weak negative correlation was found between age and RCI in the mesiobuccal roots of maxillary first molars (ρ: -0.122; P: 0.018), whereas a statistically weak and moderate positive correlation was found in the maxillary first and second premolars (ρ: 0.113, 0.557; P: 0.017, <0.001), respectively. In all the remaining posterior teeth, no correlation was found.
Interorifice distance and root canal isthmus
A weak positive correlation was found between the IOD and RCI in the mesial roots of mandibular second molars and mesiobuccal roots of maxillary first molars (ρ: 0.206, 0.244; P: 0.001, <0.000), respectively. Contrastingly, a statistically weak negative correlation was found in the maxillary first and second premolars (ρ: -0.197, -0.189; P: 0.000, 0.014), respectively. No correlation was found in the remaining posterior teeth [Table 3].
Table 3.
Correlation between interorifice distance and isthmus
| Teeth | Root | Correlation coefficient | P |
|---|---|---|---|
| First mandibular molar (n=272) | Mesial | −0.110 | 0.071 |
| Second mandibular molar (n=244) | Mesial | 0.206 | 0.001* |
| First maxillary molar (n=266) | Mesiobuccal | 0.244 | 0.000* |
| Second maxillary molar (n=104) | Mesiobuccal | −0.048 | 0.627 |
| First maxillary premolar (n=359) | Single/double root | −0.197 | 0.000* |
| Second maxillary premolar (n=168) | Single/double root | −0.189 | 0.014* |
*Statistical significance was determined at P<0.05
DISCUSSION
The present study evaluated the RCI, IOD, and root canal pattern using CBCT images from an Indian subpopulation (Chennai) retrospectively. CBCT allows three-dimensional visualization of the tooth and surrounding structures in thin slices in all the three anatomic planes; axial, sagittal, and coronal, unlike the periapical radiographs. Pécora et al.[10] demonstrated that CBCT images constitute an in vivo accurate method to detect RCI. Similar to other anatomical characteristics such as root morphology, number of root canals, the prevalence and site of RCI is known to vary among different populations depending on elements such as age, gender, and geographical region.[11] In addition, the methodology of the study and sample size could also influence the prevalence rate.[11] So far, studies have not evaluated the prevalence of RCI in an Indian population. Moreover, no studies have reported a correlation between the IOD and RCI. Studies have only measured the IOD using CBCT in various teeth.[15,16] The current study is the first of its kind as it evaluated the prevalence of RCI in an Indian subpopulation, assessed the most common root canal pattern in teeth with and without RCI, measured the IOD, and correlated it with the presence of RCI.
Among all the teeth, maxillary first premolars (94%) showed the highest prevalence of RCI. The high prevalence of RCI could be due to increased presence of two root canals in a single root, thus increasing the intercommunications.[9] In contrast, Estrela et al.[17] (18.8%) and Haghanifar et al.[11] (5.4%) reported a lower prevalence of RCI in the maxillary first premolars. This variation in the incidence of RCI could be accounted to ethnic differences.
The second highest prevalence of RCI was seen in the mesial roots of mandibular molars (first molars –82.3%, second molars – 85%). With regard to the mesial roots of mandibular first molars, the present study was similar to the results reported in Iranian[18] (83%) and Brazilian[17] (87.9%) study populations, but contrast to the results reported in an American population[19] (64.7%).
In the present study, the incidence of RCI in the mesiobuccal roots of maxillary first and second molars was 76.5% and 43.5%, respectively. Estrela et al.[17] (Brazilian population) reported a similar prevalence of RCI in the maxillary second molars (46.5%). However, they found a lower prevalence of RCI in the maxillary first molars (60.8%).[17] Pécora et al.[10] (Brazilian population) reported that the incidence of RCI in the maxillary molars was 86% and 62% in ex vivo and in vivo assays, respectively.
In the present study, the prevalence of RCI in the mandibular second premolars (3.2%) was similar to the studies reported in the Iranian[11] and Brazilian[17] population; however, with respect to mandibular first premolars (11%), the frequency was higher than that reported in the Iranian[11] (3%) population and lower compared to the Brazilian[17] (18.8%) population.
In the current study among the posterior teeth, majority of the RCI were seen in the cervical and middle third of the root canal. A higher frequency of RCI was confined to the cervical third (51%) in comparison to the other thirds in the mesial roots of mandibular first molars. This is in accordance with Estrela et al.,[17] who also reported a high frequency of RCI confined to the cervical third (25%). However, a few earlier CBCT studies have reported an increased prevalence of RCI which were confined to the apical third (21%–34%).[10,19] In the present study, the mesiobuccal root of maxillary first molars showed an increased presence of RCI in the cervical to middle third regions (35.5%) and only 11.5% RCI were seen in the apical third of the root canal. This is similar to the results reported by Liu et al.[20] (cervical to middle third – 35%, apical third – 12.5%) in the Chinese population.
In contrast to the posterior teeth, the anterior teeth reported a lower prevalence of RCI in all teeth excepting the mandibular lateral incisors, wherein the prevalence was 31%. Similar findings were reported by Estrela et al.[17] (mandibular lateral incisors – 47.6%); however, this is in contrast to the values reported by Haghanifer et al.[11] (mandibular lateral incisors – 4.3%). In addition, more than 90% of the RCI began and ended in the middle third, which is similar to the previous studies.[11,17]
None of the previous studies compared the presence or absence of RCI with the root canal pattern in all the teeth. Type I Vertucci's root canal pattern was seen predominantly in all the teeth without RCI except for the mesial root of mandibular molars, in which type IV pattern was predominant. In teeth with RCI, Vertucci's type IV and II root canal pattern were predominant in the maxillary molars, maxillary premolars, and mandibular molars, whereas type III pattern was predominant in the mandibular premolars and anterior teeth. The probability of RCI to occur increased with the presence of Vertucci's type II and type IV root canal patterns in the mesial and mesiobuccal roots of mandibular and maxillary first molars, respectively. These results were in accordance with the studies reported by Hu et al.[21] and Liu et al.[20]
About 80% of maxillary first molars possessed a second mesiobuccal canal (MB2). Shetty et al.[22] (86%) and Kashyap et al.[23] (76.5%) reported similar results in a retrospective study done using CBCT in an Indian population. However, Kewalramani et al.[24] (61.9%) and Neelakantan et al.[25] (48.2%) reported a lower incidence of MB2 canal.
In the present study, only 46.2% of the maxillary second molars possessed a second mesiobuccal canal (MB2). This is in agreement with previous CBCT studies reported by Betancourt et al.[26] (Chile, 46%) and Lee et al.[27] (Korean, 42.2%), although being higher than that reported by Silva et al.[28] (Brazilian, 34.3%).
Knowledge about the IOD helps the clinicians in detecting and locating missed root canals, preparing a conservative access cavity, and avoiding iatrogenic perforation of the pulpal floor. To the best of our knowledge, this is the only study that has measured the IOD in all the maxillary and mandibular teeth with regard to the presence and absence of RCI. Hu et al.[21] reported the IOD between mesiobuccal and mesiolingual canal in mandibular first molars with RCI to be 2.8 mm; this is comparable to the present study result (2.6 mm).
The average IOD between MB1 and MB2 in maxillary first and second molars was found to be 2.1 mm. This value lies in the range reported by several studies done using CBCT.[15,24] However, these studies have not taken the RCI into consideration while reporting the IOD. In the present study, maxillary premolars reported a weak negative correlation between RCI and IOD, i.e., as the IOD increased, the number of RCI decreased and vice versa, whereas maxillary first molars and mandibular second molars reported a weak positive correlation of the same.
CBCT has a lower resolution and sensitivity in comparison to micro-CT for the visualization of small structures.[29] However, the latter can be used only for laboratory-based studies. At present, CBCT is the only imaging system that provides a good resolution for the three-dimensional assessment of the root canal anatomy in clinical studies.[29] The knowledge regarding RCI prevalence, IOD, and root canal pattern is essential before starting an endodontic procedure.
Clinical relevance
RCI was a commonly occurring phenomenon in the examined Indian subpopulation (Chennai) and hence, the clinician needs to adopt additional steps to clean this part of the RCS. Irrigant activation techniques such as the passive ultrasonic irrigation, modified Endovac technique, and the use of gentle wave system can help to debride these areas to a limited extent.[30,31,32]
CONCLUSION
Within the limitations of this study done in an Indian subpopulation, it can be concluded that:
High prevalence of RCI was found in maxillary first premolars, mesial root of mandibular molars, and mesiobuccal root of maxillary first molars, while its prevalence was low in maxillary canines and mandibular premolars and absent in maxillary incisors.
RCI was seen predominantly in the cervical and middle third of the root canal in all the teeth evaluated.
Vertucci's types IV, II, and III root canal patterns were seen predominantly in teeth with RCI.
A weak negative correlation was established between the IOD and RCI for maxillary premolars, whereas a weak positive correlation was seen in maxillary first molars and mandibular second molar.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Vertucci FJ. Root canal anatomy of the human permanent teeth. Oral Surg Oral Med Oral Pathol. 1984;58:589–99. doi: 10.1016/0030-4220(84)90085-9. [DOI] [PubMed] [Google Scholar]
- 2.Weller RN, Niemczyk SP, Kim S. Incidence and position of the canal isthmus. Part 1. Mesiobuccal root of the maxillary first molar. J Endod. 1995;21:380–3. doi: 10.1016/s0099-2399(06)80975-1. [DOI] [PubMed] [Google Scholar]
- 3.Hsu YY, Kim S. The resected root surfaces. The issue of canal isthmuses. Dent Clin North Am. 1997;41:529–40. [PubMed] [Google Scholar]
- 4.Vertucci FJ. Root canal morphology and its relationship to endodontic procedures. Endod Topics. 2005;10:3–29. [Google Scholar]
- 5.Cambruzzi JV, Marshall FJ. Molar endodontic surgery. J Can Dent Assoc. 1983;49:61–5. [PubMed] [Google Scholar]
- 6.Fan B, Pan Y, Gao Y, Fang F, Wu Q, Gutmann J. Three-dimensional morphologic analysis of isthmuses in the mesial roots of mandibular molars. J Endod. 2010;36:1866–9. doi: 10.1016/j.joen.2010.08.030. [DOI] [PubMed] [Google Scholar]
- 7.Marceliano-Alves MF, Lima CO, Bastos LG, Bruno AM, Vidaurre F, Coutinho TM, et al. Mandibular mesial root canal morphology using micro-computed tomography in a brazilian population. Aust Endod J. 2019;45:51–6. doi: 10.1111/aej.12265. [DOI] [PubMed] [Google Scholar]
- 8.Sun CW, Liu Y, Yang YM, Liao Q. Micro-CT study of root canal morphology of mandibular first premolars with multi-canals. Shanghai Kou Qiang Yi Xue. 2018;27:6–10. [PubMed] [Google Scholar]
- 9.Kang S, Yu HW, Shin Y, Karabucak B, Kim S, Kim E, et al. Topographic analysis of the isthmus in mesiobuccal and mesial roots of first molars in a South Korean population. Sci Rep. 2020;10:1247. doi: 10.1038/s41598-020-58364-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pécora JD, Estrela C, Bueno MR, Porto OC, Alencar AH, Sousa-Neto MD, et al. Detection of root canal isthmuses in molars by map-reading dynamic using CBCT images. Braz Dent J. 2013;24:569–74. doi: 10.1590/0103-6440201302380. [DOI] [PubMed] [Google Scholar]
- 11.Haghanifar S, Moudi E, Madani Z, Farahbod F, Bijani A. Evaluation of the prevalence of complete isthmi in permanent teeth using cone-beam computed tomography. Iran Endod J. 2017;12:426–31. doi: 10.22037/iej.v12i4.17175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang Y, Zheng QH, Zhou XD, Tang L, Wang Q, Zheng GN, et al. Evaluation of the root and canal morphology of mandibular first permanent molars in a western Chinese population by cone-beam computed tomography. J Endod. 2010;36:1786–9. doi: 10.1016/j.joen.2010.08.016. [DOI] [PubMed] [Google Scholar]
- 13.Cimilli H, Mumcu G, Cimilli T, Kartal N, Wesselink P. The correlation between root canal patterns and interorificial distance in mandibular first molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:e16–21. doi: 10.1016/j.tripleo.2005.11.015. [DOI] [PubMed] [Google Scholar]
- 14.Sert S, Bayirli GS. Evaluation of the root canal configurations of the mandibular and maxillary permanent teeth by gender in the Turkish population. J Endod. 2004;30:391–8. doi: 10.1097/00004770-200406000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Su CC, Wu YC, Chung MP, Huang RY, Cheng WC, Cathy Tsai YW, et al. Geometric features of second mesiobuccal canal in permanent maxillary first molars: A cone-beam computed tomography study. J Dent Sci. 2017;12:241–8. doi: 10.1016/j.jds.2017.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weinberg EM, Pereda AE, Khurana S, Lotlikar PP, Falcon C, Hirschberg C, et al. Incidence of middle mesial canals based on distance between mesial canal orifices in mandibular molars: A clinical and cone-beam computed tomographic analysis. J Endod. 2020;46:40–3. doi: 10.1016/j.joen.2019.10.017. [DOI] [PubMed] [Google Scholar]
- 17.Estrela C, Rabelo LE, de Souza JB, Alencar AH, Estrela CR, Sousa Neto MD, et al. Frequency of root canal isthmi in human permanent teeth determined by cone-beam computed tomography. J Endod. 2015;41:1535–9. doi: 10.1016/j.joen.2015.05.016. [DOI] [PubMed] [Google Scholar]
- 18.Mehrvarzfar P, Akhlagi NM, Khodaei F, Shojaee G, Shirazi S. Evaluation of isthmus prevalence, location, and types in mesial roots of mandibular molars in the Iranian population. Dent Res J (Isfahan) 2014;11:251–6. [PMC free article] [PubMed] [Google Scholar]
- 19.Tahmasbi M, Jalali P, Nair MK, Barghan S, Nair UP. Prevalence of middle mesial canals and isthmi in the mesial root of mandibular molars: An in vivo cone-beam computed tomographic study. J Endod. 2017;43:1080–3. doi: 10.1016/j.joen.2017.02.008. [DOI] [PubMed] [Google Scholar]
- 20.Liu YJ, Yang WD, Wang WM, Zhu YN, Lin ZT, Zhu M, et al. Relationship between canal morphology and isthmus in mesio-buccal roots of maxillary first molars in 9- to 12-year-old children: An in vivo cone-beam computed tomography analysis. Arch Oral Biol. 2020;112:104645. doi: 10.1016/j.archoralbio.2019.104645. [DOI] [PubMed] [Google Scholar]
- 21.Hu X, Huang Z, Huang Z, Lei L, Cui M, Zhang X, et al. Presence of isthmi in mandibular mesial roots and associated factors: An in vivo analysis. Surg Radiol Anat. 2019;41:815–22. doi: 10.1007/s00276-019-02231-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shetty H, Sontakke S, Karjodkar F, Gupta P, Mandwe A, Banga KS, et al. A cone beam computed tomography (CBCT) evaluation of MB2 canals in endodontically treated permanent maxillary molars. A retrospective study in Indian population. J Clin Exp Dent. 2017;9:e51–5. doi: 10.4317/jced.52716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kashyap RR, Beedubail SP, Kini R, Rao PK. Assessment of the number of root canals in the maxillary and mandibular molars: A radiographic study using cone beam computed tomography. J Conserv Dent. 2017;20:288–91. doi: 10.4103/JCD.JCD_73_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kewalramani R, Murthy CS, Gupta R. The second mesiobuccal canal in three-rooted maxillary first molar of Karnataka Indian sub-populations: A cone-beam computed tomography study. J Oral Biol Craniofac Res. 2019;9:347–51. doi: 10.1016/j.jobcr.2019.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Neelakantan P, Subbarao C, Ahuja R, Subbarao CV, Gutmann JL. Cone-beam computed tomography study of root and canal morphology of maxillary first and second molars in an Indian population. J Endod. 2010;36:1622–7. doi: 10.1016/j.joen.2010.07.006. [DOI] [PubMed] [Google Scholar]
- 26.Betancourt P, Navarro P, Muñoz G, Fuentes R. Prevalence and location of the secondary mesiobuccal canal in 1,100 maxillary molars using cone beam computed tomography. BMC Med Imaging. 2016;16:66. doi: 10.1186/s12880-016-0168-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee JH, Kim KD, Lee JK, Park W, Jeong JS, Lee Y, et al. Mesiobuccal root canal anatomy of Korean maxillary first and second molars by cone-beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:785–91. doi: 10.1016/j.tripleo.2010.11.026. [DOI] [PubMed] [Google Scholar]
- 28.Silva EJ, Nejaim Y, Silva AI, Haiter-Neto F, Zaia AA, Cohenca N. Evaluation of root canal configuration of maxillary molars in a Brazilian population using cone-beam computed tomographic imaging: An in vivo study. J Endod. 2014;40:173–6. doi: 10.1016/j.joen.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 29.Acar B, Kamburoglu K, Tatar I, Arikan V, Çelik HH, Yüksel S, et al. Comparison of micro-computerized tomography and cone-beam computerized tomography in the detection of accessory canals in primary molars. Imaging Sci Dent. 2015;45:205–11. doi: 10.5624/isd.2015.45.4.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Freire LG, Iglecias EF, Cunha RS, Dos Santos M, Gavini G. Micro-computed tomographic evaluation of hard tissue debris removal after different irrigation methods and Its Influence on the filling of curved canals. J Endod. 2015;41:1660–6. doi: 10.1016/j.joen.2015.05.001. [DOI] [PubMed] [Google Scholar]
- 31.Thomas AR, Velmurugan N, Smita S, Jothilatha S. Comparative evaluation of canal isthmus debridement efficacy of modified endoVac technique with different irrigation systems. J Endod. 2014;40:1676–80. doi: 10.1016/j.joen.2014.05.014. [DOI] [PubMed] [Google Scholar]
- 32.Chan R, Versiani MA, Friedman S, Malkhassian G, Sousa-Neto MD, Leoni GB, et al. Efficacy of 3 supplementary irrigation protocols in the removal of hard tissue debris from the mesial root canal system of mandibular molars. J Endod. 2019;45:923–9. doi: 10.1016/j.joen.2019.03.013. [DOI] [PubMed] [Google Scholar]