Abstract
Aim:
The purpose of this study is to evaluate and compare the effect of different access cavity designs on root canal instrumentation efficacy using micro-computed tomography (CT) scan and resistance to fracture evaluated using the universal testing machine on maxillary central incisor.
Materials and Methodology:
Forty extracted human permanent maxillary central incisors were divided into four groups for each access cavity. The access cavities were prepared according to predefined criteria and were further assessed under Micro-CT to evaluate pre and postoperative instrumentation efficacy. After biomechanical preparation and obturation, the teeth were wrapped with tin foil to maintain a thickness of 0.2–0.3 mm as periodontal ligament. Then, the silicon impression material was applied in the acrylic alveolus, to maintain and simulate the thickness of periodontal ligament and fracture resistance was checked using the universal testing machine.
Statistical Analysis:
Data were analyzed using one-way analysis of variance test. Pair-wise comparison was made using post hoc multiple comparison (Tukey) test.
Results:
Fracture resistance was highest (1272 N) for the control group followed by the Lingual Conventional Access Group (1153.90 N). Fracture resistance for Lingual Cingulum Access Group was 1130.70 N and least for the Lingual Incisal Straight-Line Access Group (1022.80 N). This difference in fracture resistance among all the groups was significant (P = 0.001). Overall comparison showed that dentin volume reduction (DVR) for Group II was 22.45 mm3, for Group III was 17.37 mm3 and for Group IV was 28. 41 mm3. This difference in DVR among the three groups was significant (P = 0.001).
Conclusion:
The most effective instrumentation efficacy was obtained in lingual incisal straight-line access group, followed by lingual cingulum access group, followed by lingual conventional access group. The most effective fracture resistance was obtained in the lingual conventional access group, followed by the lingual cingulum access group, followed by the lingual incisal straight-line access group.
Keywords: Access cavity design, instrumented canal surface, pericervical dentin
INTRODUCTION
The ultimate aim of endodontic treatment is functional healing and retention of teeth. Failure of root canal treated teeth occurs due to structural and microbiological reasons.[1] Although the role of caries removal and disinfection of root canal cannot be overemphasized, there have been controversies regarding the size of the access cavity preparation and various root canal preparation parameters.[1,2]
A minimal invasive access cavity can be prepared only if there is a direct visualization of the entire floor of the pulp chamber, ability to localize all anticipated canal orifices and if complete removal of any present calcifications on the pulp chamber floor can be done. Traditional endodontic cavities (TECs), emphasize that straight-line access into the root canal is a pathway for better preparation efficacy.[2] However, gaining straight-line access for anterior teeth is difficult with TEC's. Increased flexural forces may lead to increased strain at the junction of crown and root surface which in turn increases the susceptibility of teeth to fracture with TEC designs as a lot of dentin is removed from pericervical region, therefore there is a need for minimal access cavity preparation.[3]
The most common access is located at the cingulum in lingual cingulum access which has the shortest distance from the pulp chamber; however, instrumentation may be less effective because a straight-line access is not allowed to the apex.[3] To overcome this, the lingual cingulum access cavity was modified and shifted slightly lingual incisally to obtain a straight-line access known as lingual conventional access cavity design. However, both the designs could not preserve the pericervical dentin.[4,5]
Loss of pericervical dentin is the most common reason for fracture of root canal treated tooth.[6] The position and design of access cavities affect the debridement, disinfection, and resistance to fracture of anterior teeth under functional load. Hence, excavation at coronal one third should be minimally conservative.[7] In addition, thicker dentin at the lingual surface of Lingual Cingulum Access Cavities and Traditional Lingual Access Cavities could lead to an enlarged preparation weakening the clinical crown.[8] However, the confined outline of TEC restricts the biomechanical preparation and filling of root canals, increasing the risk of inefficient canal instrumentation and the occurrence of procedural errors. Instrumented canal disrupts the biofilm mechanically exposing deeper layers of bacteria. Whereas the noninstrumented canals are only debrided by chemical irrigants or medicaments reaching it, which may leave areas of dentinal walls untouched, leading to poor disinfection and incomplete disruption of the root canal shavings.[9] To overcome these drawbacks, a modification was introduced in the access cavity design known as Incisal access cavity design.[10] This cavity design allows straight-line access to the apex which would facilitate the efficient instrumentation of the root canal wall and helped in the preservation of the pericervical dentin, thereby improving the fracture resistance in anterior teeth.
Fracture resistance of teeth is routinely assessed by simulated functional loading in the Universal Testing machine until fracture occurs. Loading point, force, and direction can be controlled and the load at fracture is recorded. Micro-computed tomography (CT) Analysis of pre-and postoperative images enables measurements of changes in root canal morphology including volume of dentin removed and canal wall areas untouched by instruments. Micro-CT provides high-resolution images of internal structures.[10] Hence, the purpose of this study is to evaluate and compare the effect of different access cavity designs on root canal instrumentation efficacy using micro-CT scan and resistance to fracture evaluated using the universal testing machine on maxillary central incisor.
MATERIALS AND METHODOLOGY
Forty intact permanent maxillary central incisor teeth with Vertucci Class I Root Canal configuration with fully formed apices were collected and stored in 4% phosphate-buffered saline (Fresenius Kabi, India Pvt., Ltd.,). Teeth with cracks, root caries, fractured root, extensive restorations, and immature apex were excluded from the study.
Forty sample teeth were then radiographically (VATECH Korea) exposed from 2 perpendicular views; mesio-distal and bucco-lingual dimensions, length, and degree of canal curvature were used to match teeth within each type when allocated into groups. The study was conducted in the department of conservative dentistry and endodontics of a dental college with the permission of the institutional ethical committee.
Teeth were mounted in a custom-made device and imaged with micro-CT at an isotropic resolution of [Figure 1] 30 μm (pretreatment scan) [Figure 2]. They were randomly divided into four groups (one control and three experimental groups):
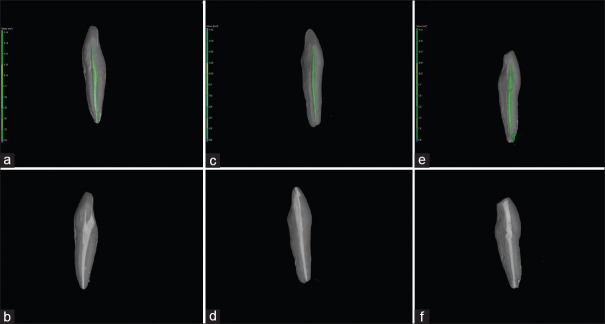
Figure 1.
(a) Preoperative micro-computed tomography scan of lingual cingulum access group (b) Postoperative micro-computed tomography scan of lingual cingulum access group (c) Preoperative micro-computed tomography scan of lingual conventional access group (d) Post operative micro-computed tomography scan of lingual conventional access group (e) Preoperative microcomputed tomography scan of lingual incisal straight-line access group. (f) Post-operative micro-computed tomography scan of lingual incisal straight-line access group
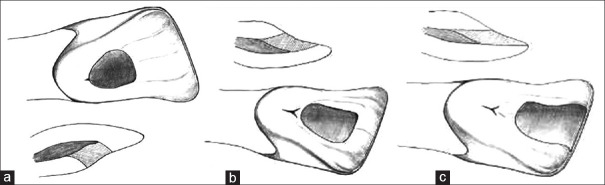
Figure 2.
(a) Diagrammatic view of lingual conventional access (b) Diagrammatic view of lingual cingulum access. (c) Diagrammatic view of lingual incisal straight-line access.
Group I (n = 10): Control group
Group II (n = 10): Lingual cingulum access
Group III (n = 10): Lingual conventional access
Group IV (n = 10): Lingual Incisal straight-line access.
Sample preparation
Teeth in all the experimental groups were cleaned of debris and mounted in a custom made device and imaged with micro-CT. Scans were used to plan the access cavity outlines by projecting the access trajectory to each canal orifice according to the respective groups. The access cavity was prepared using tungsten carbide burs (Mani, Inc., Tochigi Japan) no. 2 surgical length carbide round burs since they provide extended reach and improved vision during the entry into the pulp chamber. The #2 round bur is appropriately sized for bicuspid and anterior teeth:
Group I: Control group
No endodontic access cavity was prepared on samples of this group.
Group II: Lingual cingulum access [Figure 1a, 1b, 2b]
The initial point of entry was the lingual surface of crown, just coronal to the cingulum with bur at the right angle to the long axis of the tooth. The opening was enlarged until the cavity wall extended minimally to remove the entire pulp chamber roof cervico-incisally and mesiodistally.
Group III: Lingual conventional access [Figure 1a, 2a]
The initial point of entry was the center of the lingual surface of crown with the bur at the right angle to the long axis of teeth. The opening was enlarged holding the bur at the right angle to the long axis to teeth until the cavity extended cervically to a point just above the cingulum incisally to within 2 mm of the incisal edge and mesiodistally to remove the entire pulp chamber roof.
Group IV: Lingual incisal straight-line access [Figure 1b, 2c]
The initial point of entry was just short of the incisal edge on the lingual surface of the crown, with the bur held parallel to the long axis of teeth. The opening was enlarged holding the bur parallel to the long axis until the cavity extended cervically to enter the center of the lingual surface, incisally to involve half the bucco-lingual width of the incisal edge and mesiodistally to include the entire pulp chamber roof.
The canal working length was calculated using no. 20K file (Mani, Inc., Tochigi Japan) passed through the canal until just visible apically. The working length was estimated by reducing 0.5 mm from that measured length. The teeth were radiographed from two aspects (buccolingually and palatal) using standardized parallel technique [Table 1].
Table 1.
Comparison of fracture resistance (Newton) among four groups
| Groups | n | Mean | P | 1 versus 2 | 1 versus 3 | 1 versus 4 | 2 versus 3 | 2 versus 4 | 3 versus 4 |
|---|---|---|---|---|---|---|---|---|---|
| Group 1 | 10 | 1272.00±25.33 | 0.001* | 0.001* | 0.001* | 0.001* | 0.228 | 0.001* | 0.001* |
| Group 2 | 10 | 1130.70±31.44 | |||||||
| Group 3 | 10 | 1153.90±21.54 | |||||||
| Group 4 | 10 | 1022.80±27.49 |
One-way ANOVA test; *Significant at P≤0.05. Group 1: Control group, Group 2: Lingual cingulum access, Group 3: Lingual conventional access, Group 4: Lingual incisal straight line access, ANOVA: Analysis of variance
Biomechanical preparation was done using rotary protaper file system (Denstply Mallefer, Switzerland) that were used sequentially at the speed of 300 rpm to prepare the canals. Sx file was used to enlarge the coronal portion of the canal, and then, all files were used till the WL: S1-S2-F1-F2-F3-F4. The first two shaping files were used with a torque of 1.5 N cm in a brushing motion along the root canal walls away from the root concavities before light resistance was encountered. The last four finishing files were used until the WL was reached with a torque of 2.5 N cm. The last file used was F4, which corresponds to file 40 with a taper 0.06 at the apical area and teeth were irrigated with 5 ml of 3% sodium hypochlorite (Photon-RPC Pvt., Ltd.) followed by normal saline.
After complete cleaning shaping, all teeth were scanned in the μ-CT machine (Phoenix v|tome|x s) to capture the instrumented canal shape. Pre and posttreatment scans were precisely repositioned through a software-controlled iterative superimposition algorithm. Canal and crown boundaries were demarcated at the buccolingual level of the cementoenamel junction in incisors.
The obturation was done with gutta percha (Sure Endo) and AH plus sealer (Denstply Mallefer, Swizerland) by lateral compaction technique and was restored using composite resin material (IVOCLAR).
After restoration, teeth were wrapped in tin foil maintaining the thickness of 0.2–0.3 mm as periodontal ligament <2 mm from the cervical line. The spacer was removed from the root surface and the acrylic resin block alveolus. Then, the silicon impression material was applied in the acrylic alveolus, to maintain and simulate the thickness of periodontal ligament. The block was held in a jig at 130° angulation and fracture resistance was checked using the universal testing machine (HYTECH; Mumbai) at a crosshead speed of 1 mm/min.
Statistical analysis
SPSS 17 SPSS IBM, Chicago for windows program was used for the statistical analysis of the data [Figure 1b]. One-way analysis of variance test was used for the comparison of groups and Tukey's Honestly significant test (HSD) test was used for the determination of the group leading to significance.
RESULTS
Fracture resistance was highest (1272N) for the control group followed by lingual Conventional Access Group (1153.90N). Fracture resistance for Lingual Cingulum Access Group was 1130.70N and least for the Lingual Incisal Straight-Line Access Group (1022.80 N). This difference in fracture resistance among all the groups was significant (P = 0.001)
Overall comparison showed that Dentin volume reduction (DVR) for Group II was 22.45 mm3, for Group III was 17.37 mm3 and for Group IV was 28. 41 mm3. This difference in DVR among the three groups was significant (P = 0.001) [Table 2].
Table 2.
Comparison of dentin volume reduction among three test groups
| Groups | n | Mean | P | Group 2 versus Group 3 | Group 2 versus Group 4 | Group 3 versus Group 4 |
|---|---|---|---|---|---|---|
| Overall | ||||||
| Group 2 | 10 | 22.45±1.79 | 0.001* | 0.001* | 0.001* | 0.001* |
| Group 3 | 10 | 17.37±1.57 | ||||
| Group 4 | 10 | 28.41±3.06 | ||||
| Crown | ||||||
| Group 2 | 10 | 20.27±1.25 | 0.001* | 0.001* | 0.001* | 0.001* |
| Group 3 | 10 | 15.88±1.20 | ||||
| Group 4 | 10 | 25.39±2.13 | ||||
| Coronal | ||||||
| Group 2 | 10 | 1.55±0.45 | 0.001* | 0.001* | 0.001* | 0.001* |
| Group 3 | 10 | 1.01±0.24 | ||||
| Group 4 | 10 | 1.99±0.58 | ||||
| Middle | ||||||
| Group 2 | 10 | 0.52±0.15 | 0.001* | 0.011* | 0.169 | 0.001* |
| Group 3 | 10 | 0.25±0.10 | ||||
| Group 4 | 10 | 0.68±0.28 | ||||
| Apical | ||||||
| Group 2 | 10 | 0.18±0.08 | 0.009* | 0.469 | 0.100 | 0.007* |
| Group 3 | 10 | 0.13±0.05 | ||||
| Group 4 | 10 | 0.27±0.13 |
One-way ANOVA test; *Significant at P≤0.05. ANOVA: Analysis of variance
DISCUSSION
The advanced imaging technology and resolution led to the evolution in access cavity preparation, starting from the Traditional endodontic cavity (TEC's) to Conservative Endodontic Access Cavity (CECs), Ninja endodontic access cavity, orifice-directed dentin conservation access cavity, incisal access to Cala Lilly enamel preparation.[11] Additional alterations to the tooth anatomy, such as preflaring the coronal aspect of the root canal, are usually recommended to facilitate cleaning, shaping, and filling of the root canals.[12] One of the most important causes of fractures in root-filled teeth is the loss of tooth structure.[13] The preparation of the endodontic access cavity, following the TEC principals, were reported to be the second-largest cause of tooth structure loss. Thus, a conservative endodontic access design could improve the endodontic prognosis of a treated tooth.[4]
An alternative to TEC are the contracted endodontic cavities which maintain mechanical stability while emphasizing the importance of preserving the pericervical dentin (located 4 mm above and 4 mm below the crestal bone).[12] This regional dentin is significant for the distribution of functional stresses along the root.[14] The effectiveness of succeeding steps in endodontic treatment is inevitably linked to the endodontic cavity. Therefore, it is normal for changes to be judiciously assessed before being accepted into routine clinical practice.[15] Thus, this study evaluated and compared the effects of different access cavity designs on root canal instrumentation efficacy using micro-CT scan and resistance to fracture evaluated using the universal testing machine on maxillary central incisor.[16] Experiments conformed to previously established protocols.
Samples were embedded in the elastic impression material. Soares and others concluded that the method of root embedment to simulate the periodontal ligament has a significant effect on fracture resistance and the artificial periodontal ligament may modify the fracture modes.[17] Simulation of the periodontal ligament should be done with an elastomeric material since it undergoes elastic deformation and reproduces the accommodation of tooth in the alveolus, providing nonconcentration of stresses in the cervical region of tooth. Moreover, it has been believed that the use of a rigid material (acrylic resin) to embed extracted teeth may lead to distorted load values and possibly affect the mode of failure of the specimens. Therefore, in the current study, roots were coated with a polyvinyl siloxane to simulate the periodontal ligament and surrounding anatomical structures, and the roots were then embedded in acrylic resin.[17]
Fracture resistance was assessed using the ubiquitous Instron testing machine. DVR was registered with micro-CT imaging at adequate resolution. Micro-CT systems developed in the early 1980s had much better spatial resolution, producing voxels in the range of 5–50 μm or approximately 1,000,000 times smaller in volume than CT voxels.[18] Micro-CT system using micro-focal spot X-ray source and high-resolution detectors allows projection rotated through multiple viewing directions to produce three dimensional (3D) reconstructed images of samples. The images represent spatial distribution maps. The best endodontic treatment outcome is based on a thorough knowledge of the internal anatomy of teeth. Conventional clinical radiography produces a two-dimensional record rather than 3D information of teeth. Traditional in-vitro methods of studying morphologic characteristics of root canal systems are generally destructive and produce irreversible changes to the specimen, such as tooth serial sections, transparent tooth and dye penetration, etc.[19] CT provides a noninvasive method to study root canal morphology. Since the imaging process is nondestructive, the internal features of the same sample may be examined many times and samples remain available after scanning additional biological and mechanical testing.[20]
The results of the present study showed that all types of access cavity preparation reduced the fracture-resistance of tooth compared to the control group which showed, highest load to fracture which was statistically highly significant. Among the experimental groups, the lingual conventional access group and lingual cingulum access group showed better fracture resistance, compared to lingual incisal straight-line assess group. Values of which were highly statistically significant (P = 0.001). The lingual conventional access cavity provides a design which leaves the incisal edge intact but allowing reasonably good contact of the file with the canal walls.[18,21] To facilitate disinfection and complete debridement, straight-line access to the root canal orifice is recommended (Mannan et al. 2001[9] Rhodes,[10] Johnson 2009) along with improving the fracture resistance of endodontically treated tooth.[22] In incisal access cavity preparation the remaining tooth structure was devoid of dentinal support in the incisal region. This was concluded based on the type of fractures that involved the incisal edge of the tooth in Group IV samples. The results of the present study are in agreement with previous study conducted by Krishan et al.[15] in which the fracture resistance of traditional endodontic access cavity preparation was better than the conservative endodontic access preparation.[23] However, there was no statistical difference in the fracture resistance values between Group II and Group III (P = 0.228).
The canal instrumentation efficacy as represented by DVR was best achieved with lingual incisal straight-line access in comparison to lingual conventional access group and lingual cingulum access group which was highly statistically significant at all levels of root canal.[24] The lingual cingulum group showed increased DVR as compared to the conventional lingual access group the result being highly significant. However, increased amount of untouched canal wall was seen in the lingual cingulum access group with more dentin reduction on buccal surface of root canal as shown in the micro-CT images. Interference by the lingual shoulder lead to failure in achieving a straight-line access and directing the file to cut more on the buccal surface of the root canal wall could be the possible reason for the increased DVR.[24,25,26]
Within the limitation of the present study, the lingual incisal straight cavity design facilitated better instrumentation of root canal, allowing the endodontic files to reach and shape all the areas of the root canal. However, lingual incisal group showed a lesser fracture resistance to functional load resulting in fractures which were favorable to the tooth to be easily restored.
However, questions on long-term clinical performance of tooth with lingual straight-line access cavity design need to be evaluated in clinical trials in near future.
CONCLUSION
Within the limitation of the present study, it is concluded that,
The most effective instrumentation efficacy was obtained in the lingual incisal straight-line access group, followed by the lingual cingulum access group, followed by lingual conventional access group
The most effective fracture resistance was obtained in the lingual conventional access group, followed by the lingual cingulum access group, followed by the lingual incisal straight-line access group. However, the lingual incisal access cavity showed the favorable type of fracture compared to the other groups which showed unfavorable fractures.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Alovisi M, Pasqualini D, Musso E, Bobbio E, Giuliano C, Mancino D, et al. Influence of contracted endodontic access on root canal geometry: An in vitro study. J Endod. 2018;44:614–20. doi: 10.1016/j.joen.2017.11.010. [DOI] [PubMed] [Google Scholar]
- 2.Neelakantan P, Khan K, Hei Ng GP, Yip CY, Zhang C, Pan Cheung GS. Does the orifice-directed dentin conservation access design debride pulp chamber and mesial root canal systems of mandibular molars similar to a traditional access design? J Endod. 2018;44:274–9. doi: 10.1016/j.joen.2017.10.010. [DOI] [PubMed] [Google Scholar]
- 3.Moore B, Verdelis K, Kishen A, Dao T, Friedman S. Impacts of contracted endodontic cavities on instrumentation efficacy and biomechanical responses in maxillary molars. J Endod. 2016;42:1779–83. doi: 10.1016/j.joen.2016.08.028. [DOI] [PubMed] [Google Scholar]
- 4.Clark D, Khademi J. Modern molar endodontic access and directed dentin conservation. Dent Clin North Am. 2010;54:249–73. doi: 10.1016/j.cden.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 5.Clark D, Khademi JA. Case studies in modern molar endodontic access and directed dentin conservation. Dent Clin North Am. 2010;54:275–89. doi: 10.1016/j.cden.2010.01.003. [DOI] [PubMed] [Google Scholar]
- 6.Ahmed HM. Thoughts on conventional and modern access cavity preparation techniques. Endo (lond engl) 2015;9:287–8. [Google Scholar]
- 7.Ahmed A, Mohamed H, Gutmann JL. Education for prevention: A viable pathway for minimal endodontic treatment intervention. Endo Pract Today. 2015;9:283–5. [Google Scholar]
- 8.Kayahan MB. Fracture resistance of prepared maxillary incisor teeth after different endodontic access cavity location. Biomed Res. 2016;27:191–4. [Google Scholar]
- 9.Mannan G, Smallwood ER, Gulabivala K. Effect of access cavity location and design on degree and distribution of instrumented root canal surface in maxillary anterior teeth. Int Endod J. 2001;34:176–83. doi: 10.1046/j.1365-2591.2001.00359.x. [DOI] [PubMed] [Google Scholar]
- 10.Rhodes JS, Ford TP, Lynch JA, Liepins PJ, Curtis RV. Micro-computed tomography: A new tool for experimental endodontology. Int Endod J. 1999;32:165–70. doi: 10.1046/j.1365-2591.1999.00204.x. [DOI] [PubMed] [Google Scholar]
- 11.Clark D, Khademi J. Modern endodontic access and dentin conservation, part 2. Dent Today. 2009;28:86–8. [PubMed] [Google Scholar]
- 12.Bóveda C, Kishen A. Contracted endodontic cavities: The foundation for less invasive alternatives in the management of apical periodontitis. Endodontic Top. 2015;33:169–86. [Google Scholar]
- 13.Clark D, Khademi J, Herbranson E. The new science of strong endo teeth. Dent Today. 2013;32:112. [PubMed] [Google Scholar]
- 14.Plotino G, Grande NM, Isufi A, Ioppolo P, Pedullà E, Bedini R, et al. Fracture strength of endodontically treated teeth with different access cavity designs. J Endod. 2017;43:995–1000. doi: 10.1016/j.joen.2017.01.022. [DOI] [PubMed] [Google Scholar]
- 15.Krishan R, Paqué F, Ossareh A, Kishen A, Dao T, Friedman S. Impacts of conservative endodontic cavity on root canal instrumentation efficacy and resistance to fracture assessed in incisors, premolars, and molars. J Endod. 2014;40:1160–6. doi: 10.1016/j.joen.2013.12.012. [DOI] [PubMed] [Google Scholar]
- 16.Zehnder MS, Connert T, Weiger R, Krastl G, Kühl S. Guided endodontics: Accuracy of a novel method for guided access cavity preparation and root canal location. Int Endod J. 2016;49:966–72. doi: 10.1111/iej.12544. [DOI] [PubMed] [Google Scholar]
- 17.Marchesan MA, Lloyd A, Clement DJ, McFarland JD, Friedman S. Impacts of contracted endodontic cavities on primary root canal curvature parameters in mandibular molars. J Endod. 2018;44:1558–62. doi: 10.1016/j.joen.2018.07.008. [DOI] [PubMed] [Google Scholar]
- 18.Cobankara FK, Unlu N, Cetin AR, Ozkan HB. The effect of different restoration techniques on the fracture resistance of endodontically-treated molars. Oper Dent. 2008;33:526–33. doi: 10.2341/07-132. [DOI] [PubMed] [Google Scholar]
- 19.Swain MV, Xue J. State of the art of micro-CT applications in dental research. Int J oral Sci. 2009;1:177. doi: 10.4248/IJOS09031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peters OA, Peters CI, Schönenberger K, Barbakow F. ProTaper rotary root canal preparation: Effects of canal anatomy on final shape analysed by micro CT. Int Endod J. 2003;36:86–92. doi: 10.1046/j.1365-2591.2003.00626.x. [DOI] [PubMed] [Google Scholar]
- 21.LaTurno SA, Zillich RM. Straight-line endodontic access to anterior teeth. Oral Surg Oral Med Oral Pathol. 1985;59:418–9. doi: 10.1016/0030-4220(85)90069-6. [DOI] [PubMed] [Google Scholar]
- 22.Rajasingham R, Ng YL, Knowles JC, Gulabivala K. The effect of sodium hypochlorite and ethylenediaminetetraacetic acid irrigation, individually and in alternation, on tooth surface strain. Int Endod J. 2010;43:31–40. doi: 10.1111/j.1365-2591.2009.01625.x. [DOI] [PubMed] [Google Scholar]
- 23.Özyürek T, Ülker Ö, Demiryürek EÖ, Yilmaz F. The effects of endodontic access cavity preparation design on the fracture strength of endodontically treated teeth: Traditional Versus Conservative preparation. J Endod. 2018;44:800–5. doi: 10.1016/j.joen.2018.01.020. [DOI] [PubMed] [Google Scholar]
- 24.Corsentino G, Pedullà E, Castelli L, Liguori M, Spicciarelli V, Martignoni M, et al. Influence of access cavity preparation and remaining tooth substance on fracture strength of endodontically treated teeth. J Endod. 2018;44:1416–21. doi: 10.1016/j.joen.2018.05.012. [DOI] [PubMed] [Google Scholar]
- 25.Varghese VS, George JV, Mathew S, Nagaraja S, Indiresha HN, Madhu KS. Cone beam computed tomographic evaluation of two access cavity designs and instrumentation on the thickness of peri-cervical dentin in mandibular anterior teeth. J Conserv Dent. 2016;19:450–4. doi: 10.4103/0972-0707.190018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Allen C, Meyer CA, Yoo E, Vargas JA, Liu Y, Jalali P. Stress distribution in a tooth treated through minimally invasive access compared to one treated through traditional access: A finite element analysis study. J Conserv Dent. 2018;21:505–9. doi: 10.4103/JCD.JCD_260_18. [DOI] [PMC free article] [PubMed] [Google Scholar]