Abstract
Streptomycin is considered to be one of the effective antibiotics for the treatment of plague. In order to investigate the streptomycin resistance of Y. pestis in China, we evaluated streptomycin susceptibility of 536 Y. pestis strains in China in vitro using the minimal inhibitory concentration (MIC) and screened streptomycin resistance-associated genes (strA and strB) by PCR method. A clinical Y. pestis isolate (S19960127) exhibited high-level resistance to streptomycin (the MIC was 4,096 mg/L). The strain (biovar antiqua) was isolated from a pneumonic plague outbreak in 1996 in Tibet Autonomous Region, China, belonging to the Marmota himalayana Qinghai–Tibet Plateau plague focus. In contrast to previously reported streptomycin resistance mediated by conjugative plasmids, the genome sequencing and allelic replacement experiments demonstrated that an rpsL gene (ribosomal protein S12) mutation with substitution of amino-acid 43 (K43R) was responsible for the high-level resistance to streptomycin in strain S19960127, which is consistent with the mutation reported in some streptomycin-resistant Mycobacterium tuberculosis strains. Streptomycin is used as the first-line treatment against plague in many countries. The emergence of streptomycin resistance in Y. pestis represents a critical public health problem. So streptomycin susceptibility monitoring of Y. pestis isolates should not only include plasmid-mediated resistance but also include the ribosomal protein S12 gene (rpsL) mutation, especially when treatment failure is suspected due to antibiotic resistance.
Author summary
The plague natural foci are widely distributed in the world, and correspondingly, the plague still poses a significant threat to human health in some countries with endemic plague foci. Streptomycin is used as the first-line treatment against plague in many countries for the antibiotic is considered to be one of the effective antibiotics, particularly for the treatment of pneumonic plague. The resistance to streptomycin had been reported in Y. pestis strains from Madagascar in previous studies. In this study, we reported the high-level resistance to streptomycin in a clinical isolate of Y. pestis from a pneumonic patient in Tibet Autonomous Region, China, and a novel mechanism of streptomycin resistance, i.e. mutation in the rpsL gene were identified. The knowledge acquired about streptomycin resistance in Y. pestis will remain of great practical value. For the emergence of resistance to streptomycin in Y. pestis would render the treatment failure, thus corresponding antibiotic monitoring should be routinely carried out in countries threatened by plague. In addition, based on our further understanding about streptomycin resistance of Y. pestis isolates, such monitoring should not only include plasmid-mediated resistance but also include the ribosomal protein S12 gene (rpsL) mutation in Y. pestis isolates.
Background
Plague is an acute infectious disease caused by Yersinia pestis; it is primarily a disease of wild rodents and their parasitic fleas are considered to be the transmitting vectors. Three major types of plague occur in human beings: bubonic, pneumonic, and septicemic plague. Pneumonic plague is the most threatening clinical form as person-to-person transmission typically occurs. So far, five biovars of Y. pestis have been recognized on the basis of their biochemical properties: Y. pestis antiqua, mediaevalis, orientalis, pestoides (microtus), and intermedium [1–3].
Streptomycin is the most effective antibiotic agent against Y. pestis [4]. However, resistance to streptomycin has been reported in Y. pestis strains from Madagascar in two studies [5,6]. In 1995, an isolate named 17/95 was isolated from a 16-year-old boy in the Ambalavao district of Madagascar and this strain exhibited multidrug-resistant traits to eight antimicrobial agents (streptomycin, chloramphenicol, tetracycline, sulfonamides, ampicillin, kanamycin, spectinomycin, and minocycline) [5]. The biovar of the strain 17/95 was orientalis and it carried the conjugative multidrug-resistant plasmid pIP1202 (a member of the IncA/C plasmid family), in which the high level of streptomycin resistance (MICs>2,048 mg/L) was due to the presence of streptomycin phosphotransferase activity induced by streptomycin resistance-associated genes (strA and strB) [5]. Another isolate named 16/95 (orientalis), only exhibiting streptomycin resistance, was obtained in 1995 in the Ampitana district of Madagascar from an axillary bubo puncture from a 14-year-old boy before antibiotic treatment [6]. The resistance determinant of 16/95 was carried by a self-transferable plasmid (pIP1203, a member of the IncP group) and the MIC of streptomycin for 16/95 was 1,024 mg/L. Recently, a paper reported plasmid-mediated doxycycline resistance in a Y. pestis strain in Madagascar (isolated from a rat in 1998) [7]. In addition, another multidrug-resistant Y. pestis strain was isolated in Mongolia in 2000 from a marmot, but the genetic basis and transferability of the resistance were not investigated [7,8].
Public health measures and effective antibiotic treatments led to a drastic decrease in plague worldwide. However, the disease has not yet been eradicated, and endemic plague foci are widely distributed in Africa, Asia, and North and South America [9]. In this study, we report high-level resistance to streptomycin in a clinical isolate of Y. pestis named S19960127 from a pneumonic patient occurred in 1996 in Shannan Prefecture, Tibet Autonomous Region, China. Different from the mechanism of conjugative plasmids that carry phosphoryltransferase encoded by strA or strB to inactivate streptomycin[5,6], we found that the high-level streptomycin resistance originated from a mutation in rpsL (ribosomal protein S12).
Methods
Ethics statement
The ethical aspect of this study was approved by the Qinghai Institute for Endemic Disease Control and Prevention, Xining, China. All procedures were in accordance with the ethical standards of the National Research Committee.
Antibiotic resistance evaluation
A total of 536 Y. pestis isolates from 1946 to 2012 in 12 natural plague foci in China were used to evaluate the susceptibility to streptomycin. Susceptibility testing for Y. pestis and corresponding quality control referenced standard Clinical and Laboratory Standards Institute (CLSI) methods [10]. Minimal inhibitory concentrations (MICs) were determined by the agar dilution method following National Committee for Clinical Laboratory Standards guidelines [11] and previous literatures [12,13]. Quality control strains (Escherichia coli ATCC 25922 and Pseudomonas aeruginosa ATCC27853) were tested periodically with each batch of Y. pestis isolates to validate the accuracy of the procedure. All the experiments associated with Y. pestis were conducted in the Bio-safety Level 3 (BSL-3) laboratory in Qinghai Institute for Endemic Disease Control and Prevention.
PCR for screening the streptomycin resistance-associated genes strA and strB
We scanned for the streptomycin resistance-associated genes (strA and strB) using the PCR method in 536 Y. pestis strains, in which the strA and strB genes targeted the enzymes that phosphorylated streptomycin in the conjugative plasmids pIP1202 (Y. pestis strain 17/95) and pIP1203 (Y. pestis strain 16/95) (EMBL data bank under accession number AJ249779) [5,6]. The primers used to amplify strA and strB are listed in S1 Table. PCR was performed using Taq DNA polymerase (Takara) with the following cycling protocol: denaturing step for 5 min at 95°C, followed by 30 cycles of the amplification step at 95°C for 50 s, 58°C for 50 s, and 72°C for 1 min, and the final extension step for 5 min at 72°C.
Y. pestis and DNA preparation for genome sequencing
A total of 15 Y. pestis isolates from Shannan Prefecture (natural plague focus) in Tibet Autonomous Region were used for genome sequencing, including seven Y. pestis strains isolated from human and eight strains isolated from Marmota himalayana or hare in various years (S2 Table). The 15 strains were also included in the 536 Y. pestis isolates used for evaluation of antibiotic resistance. Genomic DNA from each bacterium was extracted using the QIAamp DNA Mini Kit (Qiagen Shanghai, China) according to the manufacturer’s instructions. The complete genome of streptomycin resistance Y. pestis strain S19960127 was sequenced using PacBio RS II sequencers and assembled de novo using SMRT Link v5.1.0 software [14]. The draft genomes of the other 14 strains were sequenced on the Illumina HiSeq 2500-PE125 platform with massively parallel sequencing Illumina technology and assembled using SOAP software [15]. The PlasmidFinder was used to identify the characteristics of plasmids in sequenced strains [16].
Identification of mutated genes in Y. pestis strain S19960127 and alignment of rpsL genes
The genes in the complete genome of the streptomycin-resistant Y. pestis strain S19960127 was predicted by Glimmer software using the default parameters [17]. Compared with the streptomycin-sensitive Y. pestis strains in the Genbank database, those genes with point mutations in S19960127 were blasted and an rpsL gene (ribosomal protein S12) mutation was finally found. This SNP point mutation was confirmed by PCR (primers: rpsL-F/rpsL-R in S2 Table) and Sanger sequencing. MEGA6.0 software [18] was used to align the mutated rpsL gene in Y. pestis S19960127 with its counterparts in M. tuberculosis [19], E. coli, and Salmonella. Another gene rrs, also responsible for streptomycin-resistance in M. tuberculosis [20], was examined in S19960127.
Gene replacement of rpsL
Allele exchange was carried out as described previously [21,22]. The primers used in this study are listed in S1 Table. The chloramphenicol acetyltransferase (cat) gene was amplified from the pKD3 plasmid with the primers Dcat-F/Dcat-R. The tool plasmids were constructed as follows. The primers YPO0199-DF1/YPO0199-DR1 and YPO0199-DF2/YPO0199-DR2 were used to amplify 507 bp upstream and 495 bp downstream of the rpsL gene from Y. pestis EV76 genomic DNA (note: EV76 is a vaccine strain and streptomycin sensitive, MIC: 4mg/L). The overlapping PCR fragment was cleaved with XhoI and SpeI enzymes then ligated to the suicide plasmid pWM91 digested with the same enzymes. In order to delete the locus of rpsL gene in S19960127, the recombinant plasmid (pWM△YPO0199::cat) was transferred from SM10λpir to S19960127 by conjugation, and selection of transformants were performed on ampicillin (100 μg/ml) plates and chloramphenicol (20μg/ml) plates overnight at 37°C. In order to re-introduce the locus of rpsL gene with rpsL-128A, the primers YPO0199-DF1/YPO0199-DR2 were used to amplify a 1281-bp region that contained the rpsL gene from Y. pestis strain EV76 genomic DNA. The PCR fragment was ligated to the Pwm91 plasmid. The recombinant plasmids were transformed into E. coli SM10λpir and then combined with S19960127△YPO0199::cat. The mixtures were transferred to gentian violet agar plates at 37°C to select Y. pestis. The rpsL mutant (Y. pestis S19960127:: rpsL-128A) was transferred to 10% sucrose (W/V) plates at 22°C for 36–48 h to remove the plasmid backbone Pwm91.The replacement of the rpsL gene with the mutant allele (G128-A) was confirmed by PCR (primers: rpsL-F/rpsL-R) and DNA sequencing. Meanwhile the caf1 gene was screened by PCR to guarantee the target bacterium was Y. pestis. In addition, the streptomycin resistance was evaluated by MIC method. In order to intuitively display the diminishment of streptomycin resistance by allele gene mutation, the disk diffusion method were used to illustrate the streptomycin resistance according to reference protocols [23].
Results
Streptomycin Resistance in Y. pestis
A clinical isolate of Y. pestis named S19960127 was highly resistant to streptomycin and the MIC was 4,096 mg/L, while the MIC breakpoint of streptomycin resistance stipulated by CLSI is ≥16 mg/L. Apart from Y. pestis strain S19960127, all the other 535 strains in this study were susceptible to streptomycin, and the ranges of MICs were 2–4 mg/L with the 50% and 90% MIC values all were 4 mg/L. Moreover, the streptomycin resistance genes strA and strB in the 536 strains were screened using PCR assays. None of them, including S19960127, carried these genes. Such results suggested that the high level of streptomycin resistance exhibited in strain S19960127 is not due to the presence of conjugative plasmids or self-transferable plasmids like the isolates from Madagascar [5], [6].
Pneumonic plague outbreak associated with streptomycin-resistant strain S19960127 in 1996 in Tibet, China
The strain S19960127 isolated from a pneumonic patient’s organs at necropsy during a plague outbreak that occurred in 1996 in Qayü village (Latitude: 28.17; Logitude: 92.44), Lhünze County, Shannan Prefecture in Tibet, China. On 2 August 1996, a 21-year-old herdsman (Patient A) caught and skinned a diseased hare. On 4 August, Patient A suffered a fever with left axillary lymphadenopathy (bubonic plague) and the next day had the onset of headache, shivering, chest pain, and a productive cough with bloody sputum, and the patient died on 9 August without any treatment. On 11August, Patient B (a veterinarian) who once took care of Patient A without any personal protection became ill and showed corresponding symptoms with primary pneumonic plague. Patient B was given unified combination treatment intramuscular injection streptomycin (1 g, twice daily), oral trimethoprim/sulfamethoxazole (1 g, three times daily); oral tetracycline (0.5 g, three times daily), Such treatment lasted eight days and the patient died on 19 August. Patient B’s wife (Patient C) suffered primary pneumonic plague on 16 August. Even although she was administrated above combination treatment, she died on 19 August. A Y. pestis strain (S19960127) was isolated from necropsy organ samples from Patient C, and the strain was identified with streptomycin resistance in this study. A village doctor (Patient D) who close contacted with Patients C during the course of her illness suffered fever and coughing with blood-tinged sputum on 17 August. Patient D was given same treatment on 17 August but still died on 22 August.
General feature of streptomycin resistance strain S19960127
The whole genome of Y. pestis S19960127 (sequence accession number CP045636) consists of a 4.63-megabase chromosome and four plasmids, besides three common virulence plasmid pCD1/pYV, pPCP1/pPst, pMT1/ Fra [24,25], a novel 33.9-kb plasmid (named pS96127) in the Y. pestis S19960127 genome was discovered. The novel plasmid pS96127 shared 99.95% identity and 99.98 coverage with the pTP33 plasmid in Y. pestis strain I-2638 (KT020860.1). Apart from S19960127, another 14 strains sensitive to streptomycin isolated in Shannan Prefecture also carried the pS96127 plasmid.
Mutation in the rpsL gene are involved in high-level streptomycin resistance in S19960127
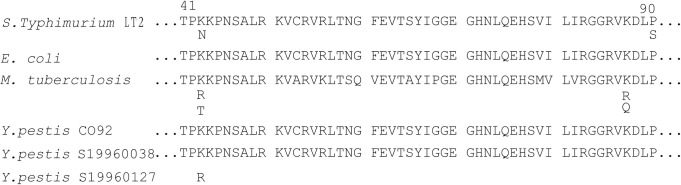
The whole genome of Y. pestis strain S19960127 was analyzed to find the genetic differences for streptomycin resistance. In these alignment results, the rpsL gene that encodes ribosomal S12 protein was mutated at 128 bp in S19960127, corresponding to amino-acid substitution of Lys to Arg at site 43 (K43R) in the RpsL protein (Fig 1). Such streptomycin-resistant mutation is consistent with the ribosomal S12 mutation in M. tuberculosis [20,26]. However, those Y. pestis strains sensitive to streptomycin in this study, including Y. pestis S19960038 and S19960156 (isolated from a county adjacent to Lhünze County in 1996), as well as other strains in Shannan Prefecture, did not exhibit any mutation in the rpsL gene. In addition, no amino-acid alteration at position 88 of ribosomal protein S12 or rrs gene mutations in S19960127 were found (Figs 1 and S1), which also confer streptomycin resistance in M. tuberculosis [26].
Fig 1. Sequence comparisons of RpsL protein.
The relevant streptomycin resistance determinants in S19960127 compared with CO92 and a local susceptible isolate S19960038, as well as M. tuberculosis, E.coli, and S.Typhimurium. Each singly conferring streptomycin resistance are listed below the relevant positions. The numbering is based on reference sequences of the E. coli K-12 substrain MG1655 RpsL (accession number NP_417801). Amino acid substitutions in RpsL were observed at positions 43 in Y.pestis S19960127.
Allelic gene replacement experiments demonstrated the mechanism that the rpsL mutation at 128 bp is the cause of streptomycin resistance in S19960127
To confirm the role of the observed mutations in streptomycin resistance, allelic exchanges experiments were carried out in S19960127, leading to the replacement of rpsL-128G in S19960127 with rpsL-128A from Y.pestis strain EV76 (MIC of streptomycin: 4 mg/L). As indicated in Fig 2, such genetic manipulations caused a substantial decrease in streptomycin resistance. The Arg 43 codon of rpsL gene in Y.pestis S19960127 is AGG. Once this codon altered to AAG would result in amino acid exchange from arginine to lysine (Fig 1), and corresponding streptomycin resistance would diminish greatly, i.e. the MIC of streptomycin was 4,096 mg/L for S19960127 (rpsL-128G), while the MIC decreased to 4 mg/L in strain S19960127:: rpsL-128A (Table 1 and Fig 2). This result indicates that rpsL mutation at 128 bp in the rpsL gene is responsible for the streptomycin resistance in strain S19960127.
Fig 2. Antimicrobial susceptibility test using the disk diffusion method.
Y. pestis strains were streaked on cation-adjusted Mueller-Hinton agar plates with streptomycin disc (300 μg/disc), incubated plates at 35°Cfor 48 h. 1: Y.pestis vaccine strain EV76 (Vaccine strain, MIC: 4 mg/L); 2: Y.pestis S19960127 (rpsL-128G, MIC 4,096 mg/L); 3: Y.pestis S19960127:: rpsL-128A (MIC 4 mg/L); 4: Escherichia coli ATCC 25922.
Table 1. The Strains and Plasmids Used in this Study.
| Strains or Plasmids | Relevant Properties | Source or Reference |
|---|---|---|
| Y. pestis strains | ||
| EV76 | Vaccine strain; pCD1; pPCP1; pMT1; SMS (MIC: 4mg/L), rpsL:128-A | Madagascar(1922); |
| S1996127 | Wild strain, pCD1; pPCP1; pMT1; pS96127; SM r (MIC:4,096 mg/L), rpsL:128-G, | This study |
| S1996127△YPO0199::cat | S1996127 delete YPO0199, SM r(MIC:4,096 mg/L), with cat gene | This study |
| S1996127:: rpsL-128A | S1996127 replacement:rpsL:G128-A; SMS(MIC: 4mg/L) | This study |
| E. coli strains | ||
| DH5α | F—, M(lacZYA-argF) U169, hsdR17 (rk—mk +), recA1, endA1, relA1 | Laboratory stock |
| SM10λpir | thi recA thr leu tonA lacY supE RP4-2-Tc::Mu_::pir; Kan r | Laboratory stock |
| SMS(MIC: 4mg/L) | ||
| Plasmids | ||
| pkd3 | Cloning vector; lacZ Amp r | Laboratory stock |
| pWM91 | Suicide vector containing R6K ori, sacB, lacZα; Ampr | Laboratory stock |
| pWM△YPO0199::cat | 2.137kb, containing the flanking sequence of rpsL, with cat gene | This study |
| pWMDF1-DR2 | 1.281 kb, EV76 fragment containing the sequence of the rpsL | This study |
Discussion
Streptomycin resistance worldwide and underlying mechanism
Traditional antimicrobials used for treatment and/or prophylaxis of plague patients include aminoglycosides (streptomycin and gentamicin), tetracyclines (doxycycline and tetracycline), chloramphenicol, and trimethoprim/sulfamethoxazole [4]. Generally, Y. pestis isolates are uniformly susceptible to the dominant antibiotics against Gram-negative bacteria [27,28]. Recently, a paper reported plasmid-mediated doxycycline resistance in a Y. pestis strain in Madagascar (isolated from a rat in 1998) [7].
Resistance to streptomycin conferred by resistance plasmids encoding streptomycin phosphotransferase enzymes had been documented in two studies from Madagascar [5,6], in which strain 17/95 (orientalis) carried the conjugative plasmid pIP1202 (a member of the IncA/C plasmid family) and the MIC of streptomycin for strain 17/95 was >2,048 mg/L [5]. Meanwhile, another Y. pestis strain 16/95 (orientalis) only resistant to streptomycin, whose resistance determinant was carried by a self-transferable plasmid (pIP1203, a member of the IncP group). The MIC of streptomycin for 16/95 was 1,024 mg/L [6].
Another mechanism for streptomycin resistance is conferred via chromosomal mutations which alter the ribosomal binding site of streptomycin [20,26]. Streptomycin binds to the aminoacyl-tRNA recognition site (A-site) of 16S rRNA, interferes with a proofreading step in translation, and inhibits the initiation of translation, thereby perturbing polypeptide synthesis and subsequent cell death. Two gene mutations, encoding ribosomal protein S12 (rpsL gene) and the 16S rRNA gene (rrs), have been associated with streptomycin resistance in M. tuberculosis [29] and other species of bacteria such as Salmonella typhimurium [30]. Streptomycin resistance in M. tuberculosis is associated with substitution of amino-acid 43 or 88 in rpsL mutations in streptomycin-resistant isolates [26]. Highly-resistant strains are those that tolerate streptomycin concentrations >500 mg/L [20], and this phenotype has only been found in isolates with an altered rpsL in M. tuberculosis, while mutations in rrs are associated with a low or intermediate level of resistance (tolerating streptomycin at concentrations between 50 and 500 mg/L) in M. tuberculosis [20]. In this study, the high level of streptomycin resistance (the MIC was 4,096 mg/L) exhibited in Y. pestis S19960127 was identified as being due to a rpsL mutation associated with substitution of amino-acid 43 of ribosomal protein S12. Sequence comparison showed no amino-acid alteration at position 88 of ribosomal protein S12 or rrs gene mutations in S19960127 (Figs 1 and S1).
Reasons for streptomycin resistance
The epidemiological investigation indicated that the Patient C took care of Patient B (primary pneumonic plague) and unfortunately got infection. Considering their clinical symptoms and treatment, as well as the genomic phylogenetic relationship in associated strains (molecular subpopulation designations see in S2 Table), we inferred that the high level of resistance by a mutation did not originate from the local reservoir of M. himalayana or previous plague outbreaks, because no such mutation in rpsL occurred in strains isolated from M. himalayana or human cases in adjacent counties, even though the phylogenetic lineage of these strains was same with the streptomycin-resistant strain S19960127, i.e.2.ANT2d. Such strains included S19960038 (2.ANT2d, isolated from a pneumonic plague outbreak at the end of July in 1996 in Cona County) and S19960156 (2.ANT2d, isolated from local reservoir M. himalayana in Cona County in 1996); In addition, S19910050 (2.ANT2d) was involved in a pneumonic plague outbreak (six-patients with five deaths) in Lhünze county in September 1991, and the strain S19910056 (2.ANT2d) was associated with a pneumonic plague outbreak (15 cases with five deaths) occurred in Qusug County (Xiajiang village, adjacent to Lhünze county) in 1991. All these strains did not exhibited substitution mutation in rpsL gene.
Streptomycin is the most effective antibiotic against Y. pestis and the drug of choice for treatment of plague, particularly for the pneumonic form[4]. The Patient C got infection from her husband (Patient B). She was given united combination treatment including streptomycin, tetracycline and trimethoprim/sulfamethoxazole for three days but still ended in death, and streptomycin resistance strain S19960127 was isolated from her necropsy organ. So the emergence of streptomycin resistance was suspected due to the streptomycin application in Patient C or her predecessor (Patient B). In addition, on one hand, the treatment failures maybe associated with such streptomycin resistance, even they were also administrated the trimethoprim/sulfamethoxazole and the tetracycline besides the streptomycin. For the former two antibiotics, comparatively, are not effective as streptomycin, especially for the treatment of pneumonic plague[4]. For the other hand, we can’t completely rule out the possibility that the treatment failure was associated with the severity of pneumonic plague disease. Because no strain was obtained from Patient B, so, for Patient B, no sufficient evidence to confirm that the pathogen had developed corresponding streptomycin resistance because of streptomycin application, even though Patient B was given streptomycin treatment for 8 days. Of course, Additional studies investigating the origination of streptomycin resistance are still needed in vitro or in vivo to prove such selective function.
Risk of streptomycin-resistant Y. pestis in M. himalayana plague focus on the Qinghai-Tibet plateau
In history, plague once killed millions of people in Europe in the 14th century and tens of thousands in China in the 19th century [9]. To date, at least 12 plague foci had been identified in China[31], in which the Marmota himalayana plague focus on the Qinghai-Tibet plateau is the largest and highest risk focus in China [31]. In this natural plague focus, human plague infection is always associated with hunting or skinning diseased or dead M. himalayana or Tibetan sheep (Ovis aries) [32] and the pathogen Y. pestis (biovar antiqua) frequently causes pneumonic or septicemic plague with high mortality [32]. So even though Y.pestis resistance to streptomycin is not widespread in this plague focus, we should not ignore the possibility of spread due to overuse of streptomycin, for once the streptomycin-resistant Y. pestis spreads in humans or in hosts and vectors in natural plague foci, a significant public health threat will have to be confronted. What’s more, we can’t completely rule out such a possibility that clinician attributed the treatment failure on plague to severity of the disease while ignored streptomycin resistance in the case of the antibiotic was administrated. So, from the clinical and public health point of view, antimicrobial susceptibility monitoring of Y. pestis isolates should be routinely carried out in countries threatened by plague.
The significance of this research
Streptomycin is the preferred choice for therapy of plague in China and other countries. This is the first report that streptomycin resistance is present in Y. pestis in China. To the best of our knowledge, this is the first report of a high level of streptomycin resistance associated with an rpsL mutation in Y. pestis. So streptomycin susceptibility monitoring of Y. pestis isolates should not only include plasmid-mediated resistance but also include the ribosomal protein S12 gene (rpsL) mutation, especially when treatment failure is suspected due to antibiotic resistance. Currently, Genome sequencing became significantly easier with the advance of next generation sequencing technologies [23]. On one hand, the genome-wide SNP analysis could be used to illustrate the phylogenetic relationship or the microevolution of Y. pestis [33], including used for source-tracking in plague outbreaks. On the other hand, whole genome sequencing and associated analysis methods could greatly facilitate the detection of known or potentially novel mutations associated with antibiotics resistance in Y. pestis. Ultimately, such insights will greatly assist with patient treatment, management, and the disease control.
Supporting information
(DOC)
(XLS)
(TIF)
Acknowledgments
We thank all the professionals for natural plague foci surveillance in Shannan Prefecture and in Tibet Autonomous Region CDCs.
Data Availability
The sequencing data of Y. pestis strain S19960127 are available in GenBank under accession numbers CP045636–CP045640, and the genome sequences of Y. pestis strains sequenced in this study have been deposited in GenBank with accession numbers WHKG00000000–WHLN00000000.
Funding Statement
RD received support from National Natural Science Foundation of China (81660349), WL from National Important Scientific and Technology Project (2018ZX10101002-002), RD from Science and Technology Plan Project in Qinghai Province (2019-ZJ-7074) and XZ from National Health Commission Project for Key Laboratory of Plague Prevention and Control (2019PT310004). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Anisimov AP, Lindler LE, Pier GB. Intraspecific diversity of Yersinia pestis. Clin Microbiol Rev. 2004;17(2):434–64. Epub 2004/04/16. 10.1128/cmr.17.2.434-464.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou D, Tong Z, Song Y, Han Y, Pei D, Pang X, et al. Genetics of metabolic variations between Yersinia pestis biovars and the proposal of a new biovar, microtus. J Bacteriol. 2004;186(15):5147–52. Epub 2004/07/21. 10.1128/JB.186.15.5147-5152.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li Y, Cui Y, Hauck Y, Platonov ME, Dai E, Song Y, et al. Genotyping and phylogenetic analysis of Yersinia pestis by MLVA: insights into the worldwide expansion of Central Asia plague foci. PLoS One. 2009;4(6):e6000. Epub 2009/06/23. 10.1371/journal.pone.0006000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Plague manual—epidemiology, distribution, surveillance and control. Wkly Epidemiol Rec. 1999;74(51–52):447. Epub 2000/01/15. . [PubMed] [Google Scholar]
- 5.Galimand M, Guiyoule A, Gerbaud G, Rasoamanana B, Chanteau S, Carniel E, et al. Multidrug resistance in Yersinia pestis mediated by a transferable plasmid. N Engl J Med. 1997;337(10):677–80. Epub 1997/09/04. 10.1056/NEJM199709043371004 . [DOI] [PubMed] [Google Scholar]
- 6.Guiyoule A, Gerbaud G, Buchrieser C, Galimand M, Rahalison L, Chanteau S, et al. Transferable plasmid-mediated resistance to streptomycin in a clinical isolate of Yersinia pestis. Emerg Infect Dis. 2001;7(1):43–8. Epub 2001/03/27. 10.3201/eid0701.010106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cabanel N, Bouchier C, Rajerison M, Carniel E. Plasmid-mediated doxycycline resistance in a Yersinia pestis strain isolated from a rat. Int J Antimicrob Agents. 2018;51(2):249–54. Epub 2017/10/17. 10.1016/j.ijantimicag.2017.09.015 . [DOI] [PubMed] [Google Scholar]
- 8.Kiefer D, Dalantai G, Damdindorj T, Riehm JM, Tomaso H, Zoller L, et al. Phenotypical characterization of Mongolian Yersinia pestis strains. Vector Borne Zoonotic Dis. 2012;12(3):183–8. Epub 2011/10/26. 10.1089/vbz.2011.0748 . [DOI] [PubMed] [Google Scholar]
- 9.Morelli G, Song Y, Mazzoni CJ, Eppinger M, Roumagnac P, Wagner DM, et al. Yersinia pestis genome sequencing identifies patterns of global phylogenetic diversity. Nat Genet. 2010;42(12):1140–3. Epub 2010/11/03. 10.1038/ng.705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Heine HS, Hershfield J, Marchand C, Miller L, Halasohoris S, Purcell BK, et al. In vitro antibiotic susceptibilities of Yersinia pestis determined by broth microdilution following CLSI methods. Antimicrob Agents Chemother. 2015;59(4):1919–21. Epub 2015/01/15. 10.1128/AAC.04548-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.CLSI. Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically. Approved standard-Ninth Edition: Wayne,PA: Clinical and Laboratory standards institute; 2012. [Google Scholar]
- 12.Smith MD, Vinh DX, Nguyen TT, Wain J, Thung D, White NJ. In vitro antimicrobial susceptibilities of strains of Yersinia pestis. Antimicrob Agents Chemother. 1995;39(9):2153–4. Epub 1995/09/01. 10.1128/aac.39.9.2153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hernandez E, Girardet M, Ramisse F, Vidal D, Cavallo JD. Antibiotic susceptibilities of 94 isolates of Yersinia pestis to 24 antimicrobial agents. J Antimicrob Chemother. 2003;52(6):1029–31. Epub 2003/11/14. 10.1093/jac/dkg484 . [DOI] [PubMed] [Google Scholar]
- 14.Ardui S, Ameur A, Vermeesch JR, Hestand MS. Single molecule real-time (SMRT) sequencing comes of age: applications and utilities for medical diagnostics. Nucleic Acids Res. 2018;46(5):2159–68. Epub 2018/02/06. 10.1093/nar/gky066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Luo R, Liu B, Xie Y, Li Z, Huang W, Yuan J, et al. SOAPdenovo2: an empirically improved memory-efficient short-read de novo assembler. Gigascience. 2012;1(1):18. Epub 2012/01/01. 10.1186/2047-217X-1-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carattoli A, Hasman H. PlasmidFinder and In Silico pMLST: Identification and Typing of Plasmid Replicons in Whole-Genome Sequencing (WGS). Methods Mol Biol. 2020;2075:285–94. Epub 2019/10/05. 10.1007/978-1-4939-9877-7_20 . [DOI] [PubMed] [Google Scholar]
- 17.Delcher AL, Bratke KA, Powers EC, Salzberg SL. Identifying bacterial genes and endosymbiont DNA with Glimmer. Bioinformatics. 2007;23(6):673–9. Epub 2007/01/24. 10.1093/bioinformatics/btm009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tamura K, Stecher G, Peterson D, Filipski A, Kumar S. MEGA6: Molecular Evolutionary Genetics Analysis version 6.0. Mol Biol Evol. 2013;30(12):2725–9. Epub 2013/10/18. 10.1093/molbev/mst197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dal Molin M, Gut M, Rominski A, Haldimann K, Becker K, Sander P. Molecular Mechanisms of Intrinsic Streptomycin Resistance in Mycobacterium abscessus. Antimicrob Agents Chemother. 2018;62(1). Epub 2017/10/25. 10.1128/AAC.01427-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Meier A, Sander P, Schaper KJ, Scholz M, Bottger EC. Correlation of molecular resistance mechanisms and phenotypic resistance levels in streptomycin-resistant Mycobacterium tuberculosis. Antimicrob Agents Chemother. 1996;40(11):2452–4. Epub 1996/11/01. 10.1128/AAC.40.11.2452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang G, Inaoka T, Okamoto S, Ochi K. A novel insertion mutation in Streptomyces coelicolor ribosomal S12 protein results in paromomycin resistance and antibiotic overproduction. Antimicrob Agents Chemother. 2009;53(3):1019–26. Epub 2008/12/24. 10.1128/AAC.00388-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhou YY, Zhang HZ, Liang WL, Zhang LJ, Zhu J, Kan B. Plasticity of regulation of mannitol phosphotransferase system operon by CRP-cAMP complex in Vibrio cholerae. Biomed Environ Sci. 2013;26(10):831–40. Epub 2013/11/13. 10.3967/bes2013.006 . [DOI] [PubMed] [Google Scholar]
- 23.Yang R. Yersinia Pestis Protocols: Springer Nature Singapore Pte Ltd; 2018. [Google Scholar]
- 24.Parkhill J, Wren BW, Thomson NR, Titball RW, Holden MT, Prentice MB, et al. Genome sequence of Yersinia pestis, the causative agent of plague. Nature. 2001;413(6855):523–7. Epub 2001/10/05. 10.1038/35097083 . [DOI] [PubMed] [Google Scholar]
- 25.Deng W, Burland V, Plunkett G 3rd, Boutin A, Mayhew GF, Liss P, et al. Genome sequence of Yersinia pestis KIM. J Bacteriol. 2002;184(16):4601–11. Epub 2002/07/27. 10.1128/jb.184.16.4601-4611.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sreevatsan S, Pan X, Stockbauer KE, Williams DL, Kreiswirth BN, Musser JM. Characterization of rpsL and rrs mutations in streptomycin-resistant Mycobacterium tuberculosis isolates from diverse geographic localities. Antimicrob Agents Chemother. 1996;40(4):1024–6. Epub 1996/04/01. 10.1128/AAC.40.4.1024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Urich SK, Chalcraft L, Schriefer ME, Yockey BM, Petersen JM. Lack of antimicrobial resistance in Yersinia pestis isolates from 17 countries in the Americas, Africa, and Asia. Antimicrob Agents Chemother. 2012;56(1):555–8. Epub 2011/10/26. 10.1128/AAC.05043-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wagner DM, Runberg J, Vogler AJ, Lee J, Driebe E, Price LB, et al. No resistance plasmid in Yersinia pestis, North America. Emerg Infect Dis. 2010;16(5):885–7. Epub 2010/04/23. 10.3201/eid1605.090892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nair J, Rouse DA, Bai GH, Morris SL. The rpsL gene and streptomycin resistance in single and multiple drug-resistant strains of Mycobacterium tuberculosis. Mol Microbiol. 1993;10(3):521–7. Epub 1993/11/01. 10.1111/j.1365-2958.1993.tb00924.x . [DOI] [PubMed] [Google Scholar]
- 30.Bjorkman J, Hughes D, Andersson DI. Virulence of antibiotic-resistant Salmonella typhimurium. Proc Natl Acad Sci U S A. 1998;95(7):3949–53. Epub 1998/05/09. 10.1073/pnas.95.7.3949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cui Y, Li Y, Gorge O, Platonov ME, Yan Y, Guo Z, et al. Insight into microevolution of Yersinia pestis by clustered regularly interspaced short palindromic repeats. PLoS One. 2008;3(7):e2652. Epub 2008/07/10. 10.1371/journal.pone.0002652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dai R, Wei B, Xiong H, Yang X, Peng Y, He J, et al. Human plague associated with Tibetan sheep originates in marmots. PLoS Negl Trop Dis. 2018;12(8):e0006635. Epub 2018/08/17. 10.1371/journal.pntd.0006635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cui Y, Yu C, Yan Y, Li D, Li Y, Jombart T, et al. Historical variations in mutation rate in an epidemic pathogen, Yersinia pestis. Proc Natl Acad Sci U S A. 2013;110(2):577–82. Epub 2012/12/29. 10.1073/pnas.1205750110 [DOI] [PMC free article] [PubMed] [Google Scholar]