Abstract
Background
The COVID-19 pandemic continues to disrupt dental practice in the United States. Oral health care workers play an integral role in societal health, yet little is known about their willingness and ability to work during a pandemic.
Methods
Oral health care workers completed a survey distributed on dental-specific Facebook groups during an 8-week period (May 1-June 30, 2020) about their willingness and ability to work during the COVID-19 pandemic, barriers to working, and willingness to receive a COVID-19 vaccine.
Results
Four hundred and fifty-nine surveys were returned. Only 53% of dentists, 33% of dental hygienists, 29% of dental assistants, and 48% of nonclinical staff members would be able to work a normal shift during the pandemic, and even fewer (50%, 18%, 17%, and 38%, respectively) would be willing to work a normal shift. Barriers included caring for family, a second job, and personal obligations, and these were faced by dental assistants and hygienists. Dentists were more likely than hygienists (P < .001), assistants (P < .001), and nonclinical staff members (P = .014) to receive a COVID-19 vaccine.
Conclusions
Oral health care workers have a decreased ability and willingness to report to work during a pandemic, and dentists are significantly more able and willing to work than hygienists and assistants. Dentists are more likely than staff to receive a COVID-19 vaccine.
Practical Implications
The results of this study may help inform future initiatives of dental workforce readiness during a pandemic. Dentists should be prepared to discuss alterations to standard operating procedures to allay staff members’ fears and improve retention rates during pandemics, allowing for improved access to oral health care.
Key Words: Dental staff members, access to care, auxiliaries/dental personnel, practice management
Abbreviation Key: HCW, Health care worker; NA, Not applicable; OHCW, Oral health care worker; PPE, Personal protective equipment

The coronavirus pandemic began in the city of Wuhan in Hubei Province, China.1 The central disease of this pandemic, COVID-19, has affected the world in all realms of life. As of December 30, 2020, the John Hopkins Coronavirus Resource Center reported there were 19.5 million COVID-19 infections in the United States and 273,799 deaths due to the disease.2 Worldwide, health care workers (HCWs) are among the groups most likely to contract the virus.3 COVID-19 has put a tremendous amount of physical and mental stress on HCWs across the world.4 China’s National Health Commission reported more than 3,300 HCWs were infected in that country, and Italy reported that 20% of their HCWs had been infected with severe acute respiratory syndrome coronavirus 2, the virus that causes COVID-19.5 Damery and colleagues6 reported that a person’s sense of duty to work during a pandemic can often become conflicted with their sense of duty to protect their family from illness. Owing to the higher risk among HCWs of becoming infected during a pandemic, the factors affecting the ability and willingness of HCWs to work during a pandemic in the United States have been studied. Gershon and colleagues7 found that more than 50% of the participants in their study would have been absent from work due to non–illness-related factors.
Similarly, the effects of the COVID-19 pandemic on dentistry in the United States have been ongoing. Disruptions to the supply chain for pharmaceuticals, personal protective equipment (PPE), medical devices, medical supplies, and blood have caused stress on the health care system at large.8 After careful analysis in the month of March 2020, the American Dental Association recommended all dental procedures for patients be halted, other than emergency oral health care. Offices and clinics eventually reopened for routine dental procedures in all parts of the country. Spikes in COVID-19 infections continued to rise sporadically within regions, and different states reopened their dental offices at different times per local and state health department guidelines.
To meet the oral health needs of the public, US oral health care workers (OHCWs) must be available and willing to serve during a pandemic. After an extensive literature review, we found no literature about the ability and willingness of US OHCWs to work during a pandemic. The purpose of our research was to assess OHCWs’ ability and willingness to work during the COVID-19 pandemic and what factors are affecting that ability and willingness.
Methods
Design and sample
The Institutional Review Board of Indiana University, Indianapolis, Indiana, granted our cross-sectional study exempt status and consent was obtained from participants by means of their agreeing to participate after reading the study information sheet. Survey questions were adapted from previous research done by Gershon and colleagues7 on the ability and willingness of medical HCWs to work during a pandemic. The survey was open to OHCWs in the United States for completion during an 8-week period (May 1-June 30, 2020). A link to our survey was available via multiple US dental groups on Facebook, as it was posted to those groups’ Facebook pages with permission from the groups’ administrators. The groups were chosen to reach a wide range of OHCWs, including dentists, dental hygienists, dental assistants, and front-office personnel. Groups included “Dental Peeps Network,” “Nifty Thrifty Dentist,” “Dental Hygienist, Business Specialist & Dentist in Indiana,” and “The Collaborative Pediatric Dentist (iPEDO).” Each Facebook group has administrators that have vetted its members and their affiliation with dentistry.
Variables
Ability of OHCWs to Work During a Pandemic
The ability of OHCWs to work during a pandemic was measured using a Likert scale of whether the OHCW would be able to report for their usual shift, would be able to report for a condensed shift, would be able to report for emergency oral health care only, or would not be able to report.
Willingness of OHCWs to Work During a Pandemic
The willingness of OHCWs to work during a pandemic was measured using a Likert scale of whether the OHCW would be willing to report for their usual shift, would be willing to report for a condensed shift, would be willing to report for emergency oral health care only, or would not be willing to report at all.
Self-Perceived Barriers for OHCWs to Ability or Willingness to Work During the Pandemic
To determine the self-perceived barriers that might impede an OHCW’s ability or willingness to work during a pandemic, the respondents were prompted to check all of the items that might apply. Items were adapted from a previous survey by Gershon and colleagues.7 The list of items (or barriers) can be found in Box 1 .
Box 1.
Self-perceived barriers and factors that would affect oral health care workers’ ability and willingness to work during the pandemic.
| BARRIERS TO REPORTING TO WORK |
|---|
| ▪ I am responsible for other family members (or pets) who live with me |
| ▪ I have obligations to a second employer or volunteer commitments |
| ▪ I have a personal chronic health problem that would prohibit extra duty |
| ▪ I have other personal obligations that would prohibit my ability to work in an emergency situation |
| ▪ I have no obligations or restrictions |
| FACTORS THAT WOULD INCREASE ABILITY AND WILLINGNESS TO REPORT TO WORK |
| ▪ A vaccine was available |
| ▪ I knew I would be safe from infection |
| ▪ I could stay in touch with my family |
| ▪ I had child care available |
| ▪ I had care for elders or other family members available |
| ▪ I had pet care available |
| ▪ I could leave work when I needed to |
| ▪ My coworkers also came to work |
| ▪ I thought no one else was going to report |
| ▪ I felt It was my duty to report |
| ▪ I received hazard duty pay |
| ▪ My employer gave me an N95-type respirator |
| ▪ I was trained properly to use an N95-type respirator |
| ▪ I had a constant, steady stream of information during the pandemic |
| ▪ I had more knowledge about the pandemic (how it is spread, how to protect myself) |
| ▪ Knowing no aerosols would be created during the emergency appointment |
| Other |
Self-Perceived Items for OHCWs That Would Increase Their Ability or Willingness to Work During the Pandemic
To determine the self-perceived items that might increase the ability or willingness to work during a pandemic, the respondents were prompted to check all of the items that might apply. Items were adapted from a previous survey.7 The list of items can be found in Box 1.
Statistical analysis
Summary statistics were calculated and summarized using number and percentage. Associations between provider characteristics and outcomes were evaluated using Pearson χ2 tests when both variables were nominal and Mantel-Haenszel χ2 tests for ordered categorical responses when at least 1 variable had ordered response categories. A 5% significance level was used for all tests. Analyses were performed using SAS, Version 9.4 (SAS Institute).
Results
Survey responses were received from 459 respondents, for an estimated response rate of 1%. Eighty-eight percent of respondents were women, 12% were men, and 9% were younger than 30 years, 39% were aged 30 through 39 years, 29% were aged 40 through 49 years, and 24% were 50 years or older. Respondents races included White (87%), Asian (4%), Black (2%), multiracial (2%), and 1% or fewer were American Indian or Alaska Native, other, and not reported. Three percent reported that they were Hispanic or Latino. Most respondents were from the Great Lakes and Midwest region (59%), 14% were from the Pacific Coast, 9% were from the South, and 5% or fewer were from the Rocky Mountain (5%), Northeast (5%), Mid-Atlantic (4%), and Southwest (3%) regions.
Responses were received from dentists (30%), dental hygienists (49%), dental assistants (14%), midlevel providers (1%), and nonclinical staff members (7%). Ninety-five percent of respondents could not work from home. For the purpose of analyses, midlevel provider data were not considered owing to the low response rate (n = 4).
Bivariate analysis
Association With Job Title and Ability to Work
Fifty-three percent of dentists, 33% of dental hygienists, 29% of dental assistants, and 48% of nonclinical staff members reported that they would be able to report for their usual shift. Only 7% of dentists reported that they would not be able to report to work at all, and 27% of hygienists, 31% of assistants, and 34% of nonclinical staff members reported that they would not be able to report to work (Table ). Although from 7% through 34% of participants answered that they would not be able to report to work at all, positive responses to specific reasons were limited.
Table.
Ability and willingness to work during the COVID-19 pandemic according to job title.
| VARIABLE | DENTIST | DENTAL HYGIENIST | DENTAL ASSISTANT | NONCLINICAL STAFF MEMBER | P VALUE∗ |
|---|---|---|---|---|---|
| Ability to Work | .001 | ||||
| Report for my usual shift, no. (%) | 71 (53) | 73 (33) | 19 (29) | 14 (48) | NA† |
| Report for a condensed shift, no. (%) | 10 (7) | 54 (25) | 5 (8) | 2 (7) | NA |
| Report for emergency oral health care only, no. (%) | 44 (33) | 32 (15) | 21 (32) | 3 (10) | NA |
| Not report at all, no. (%) | 9 (7) | 59 (27) | 20 (31) | 10 (34) | NA |
| Versus dentist, odds ratio (95% CI) | NA | 0.50 (0.34 to 0.75) | 0.33 (0.19 to 0.57) | 0.56 (0.27 to 1.17) | NA |
| Willing to Work | < .001 | ||||
| Report for my usual shift, no. (%) | 66 (50) | 40 (18) | 11 (17) | 11 (38) | NA |
| Report for a condensed shift, no. (%) | 15 (11) | 47 (22) | 6 (9) | 3 (10) | NA |
| Report for emergency oral health care only, no. (%) | 43 (32) | 46 (21) | 25 (39) | 10 (34) | NA |
| Not report at all, no. (%) | 9 (7) | 85 (39) | 22 (34) | 5 (17) | NA |
| Versus dentist, odds ratio (95% CI) | NA | 0.25 (0.17 to 0.38) | 0.23 (0.13 to 0.39) | 0.57 (0.28 to 1.19) | NA |
Mantel-Haenszel χ2 test used to calculate P values.
NA: Not applicable.
Association With Job Title and Willingness to Work
The percentage of respondents who would be willing to work during a pandemic was lower than the number who were able to work during a pandemic, with 50% of dentists', 18% of hygienists', 17% of assistants', and 38% of nonclinical staff members' being willing to work their normal shift. Only 7% of dentists reported that they would not be willing to report to work at all, and 39% of hygienists, 34% of assistants, and 17% of nonclinical staff members said they would not be willing to report (Table). The survey results also showed that dentists were significantly less concerned than dental hygienists (odds ratio [OR], 0.23; 95% CI, 0.15 to 0.35; P < .001) and dental assistants (OR, 0.27; 95% CI, 0.15 to 0.49; P < .001) that they would contract COVID-19 at work.
Association With Job Title and Self-Perceived Barriers to Reporting to Work
Reasons for inability to work are found in Figure 1 . The most cited self-perceived barriers to reporting work was responsibility for other family members and pets, with 53% of total respondents agreeing. Dentists were significantly less likely than dental hygienists (OR 0.41; 95% CI, 0.26 to 0.63; P < .001) and dental assistants (OR, 0.40; 95% CI, 0.22 to 0.73; P = .003) to agree that caring for family members was a barrier. Hygienists were more likely to have obligations to a second employer or volunteering than dentists (OR, 12.90; 95% CI, 3.05 to 54.50; P < .001) and assistants (OR, 12.32; 95% CI, 1.66 to 91.69; P = .002) and were more likely than dentists (OR, 5.10; 95% CI, 1.50 to 17.32; P = .004) to have other personal obligations that would prohibit their ability to report to work in an emergency situation. Nonclinical staff members were significantly more likely to have a personal chronic health problem that would prohibit extra duty than were dentists (OR, 4.43; 95% CI, 1.66 to 11.80; P = .002), dental hygienists (OR, 2.76; 95% CI, 1.15 to 6.58; P = .018), and dental assistants (OR, 4.21; 95% CI, 1.34 to 13.27; P = .010).
Figure 1.
Self-perceived barriers to reporting to work during the COVID-19 pandemic by job title. P values were calculated using Pearson χ2 tests. ∗ Significant difference from dentists. † Significant difference from dental hygienists. ‡ Significant difference from dental assistants. § Significant difference from nonclinical staff members.
Association With Job Title and Items That Would Increase Willingness to Work
Items that would increase OHCWs willingness to work are provided in Figure 2 . Receiving hazard duty pay would increase the willingness to work of hygienists (OR, 4.33; 95% CI, 2.33 to 8.04; P < .001), dental assistants (OR, 14.89; 95% CI, 7.05 to 31.46; P < .001), and nonclinical staff members (OR, 3.17; 95% CI, 1.19 to 8.44; P = .017) significantly more than dentists. Having a steady stream of information during the pandemic would also increase dental hygienists’ (OR, 3.55; 95% CI, 2.27 to 5.55; P < .001) and dental assistants’ (OR, 2.58; 95% CI, 1.41 to 4.73; P = .002) willingness to report significantly more than dentists’ willingness to report. Knowing that no aerosols would be produced during treatment would also increase the willingness of both dental hygienists (OR, 2.50; 95% CI, 1.61 to 3.87; P < .001) and dental assistants (OR, 2.31; 95% CI, 1.26 to 4.26; P = .007) significantly more than dentists.
Figure 2.
Items that would increase the willingness of oral health care workers to report to work during the COVID-19 pandemic by job title. P values were calculated using Pearson χ2 tests. ∗ Significant difference from dentists. † Significant difference from dental hygienists. ‡ Significant difference from dental assistants. § Significant difference from nonclinical staff members.
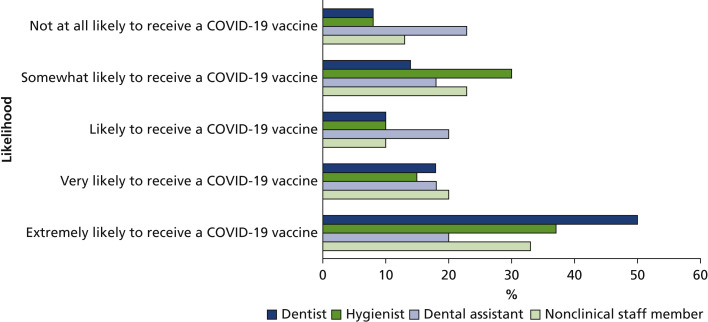
Survey participants were asked whether they would receive a vaccine against COVID-19 if one became available, and 78% of dentists were likely to extremely likely to receive the vaccine, and only 62% of hygienists and 58% of dental assistants were likely or extremely likely to receive the vaccine. This difference was significantly different, with dentists more willing than dental hygienists (OR, 1.79; 95% CI, 1.21 to 2.66; P = .004) and dental assistants (OR, 3.32; 95% CI, 1.93 to 5.71 P < .001) (Figure 3 ).
Figure 3.
Likelihood to receive a COVID-19 vaccine if a safe and effective vaccine becomes available during the pandemic. P values were calculated using Mantel-Haenszel χ2 tests. Dentists were significantly more likely than both dental hygienists and dental assistants to receive a COVID-19 vaccine.
Survey participants were also asked whether they would consider quitting their jobs or retiring during a pandemic, and dentists were significantly less likely to agree than all other groups (dental hygienists [OR, 0.23; 95% CI, 0.14 to 0.37; P < .001], dental assistants [OR, 0.28; 95% CI, 0.15 to 0.52; P < .001], and nonclinical staff members [OR, 0.36; 95% CI, 0.16 to 0.83; P = .014]).
Discussion
In our study, we assessed US OHCWs’ ability and willingness to work during a pandemic and, to our knowledge, we are the first to do so. One of the goals of Healthy People 2020 is to increase access to therapeutic and preventive services.9 Achieving this goal depends largely on patients having access to trained OHCWs. At the time of the publication of this article, COVID-19 infections were increasing daily in the United States with all areas of the country affected by the virus.
Our study results suggest that dental hygienists and dental assistants are more concerned about contracting COVID-19 at work than dentists. Bakaeen and colleagues10 reported that dentists are neither uncomfortable nor comfortable with the guidance they have received from dental organizations and are somewhat uncomfortable with the availability of PPE, the patient screening process, and measures to ensure patient safety. Those investigators surveyed dentists only, and did not ask about their willingness to treat patients; however, those data combined with the findings from our study suggest that dental hygienists and dental assistants might be even more uncomfortable with the availability of PPE, patient screening process, and measures to ensure patient safety. These responses are likely affected by the timing of the survey (May 1-June 30, 2020), during which time many dental offices in the United States were still seeing emergency patients only or were just starting to open for routine care. Follow-up studies are needed for investigators to assess how attitudes have changed as coronavirus became better understood and treatments and vaccines became available throughout the course of the pandemic.
When the availability and willingness of OHCWs to work during a pandemic is lower, access to therapeutic and preventive services could potentially decrease and impede the preventive goals set forth by the dental profession. As Damery and colleagues6 reported, HCWs are often conflicted with a “sense of duty to work” when it puts their family in harm’s way. With hygienists performing many important preventive services in the United States, this conflict could cause problems for the overall oral health of the public during a pandemic. In addition, Moraes and colleagues11 found that 90% of dentists in Brazil feared contracting COVID-19 at work, with approximately 70% being moderately or highly concerned. This is consistent with the 76% of US dentists in our study who were concerned to extremely concerned about contracting COVID-19 at work. We also found that dental hygienists and dental assistants were more concerned than dentists about contracting the disease.
Per our study results, hygienists found it harder to report to work for emergency oral health care during a pandemic than dentists, owing to obligations to a second employer or voluntary commitments. Hygienists also had other personal obligations that would prohibit their ability to work in an emergency situation. The Health Resources and Services Administration reported that before the pandemic there were 6,782 oral health care professional shortage areas in the United States.12 The impact of the COVID-19 pandemic on availability of OHCWs during and after the pandemic, especially in underserved areas, should be a potential topic of research in the future. The results of our study show that dentists were able and willing to work more during a pandemic than all other OHCWs; this highlights a potential challenge for practices throughout the country. Most dental practices rely on team members from all categories of OHCWs to function effectively. If there is a mismatch among ability, willingness, and barriers to reporting to work, or concern about risk and safety at work, then there might be a shortage of certain categories of OHCWs reporting to work. This can lead to a decrease in appointment availability due to lack of OHCWs working. We also found that dentists were less likely than all other OHCWs to quit their jobs during a pandemic, which would further exacerbate a shortage of OHCWs, particularly dental hygienists, dental assistants, and nonclinical staff members. Dentists should be aware that the concerns and barriers of their team members might be perceived by those team members as more severe than the dentists’ concerns and barriers, and dentists should be prepared to discuss alterations to standard operating procedures that have been made to ensure staff safety.
Dentists were also more likely to receive an available vaccine against COVID-19 than all other OHCWs. To our knowledge, there is no other literature available about the likelihood of different OHCWs being vaccinated. Investigators in a French study found that physicians were more likely to be vaccinated against COVID-19 than nurses or assistant nurses, which is similar to our findings in regard to dentists versus other OHCWs.13
Damery and colleagues6 reported that nearly 25% of physicians in their study did not consider it their duty to work if it would pose a risk to themselves or their families. Similarly, 83% of respondents in our study stated that they would be more willing to report for work if they knew they would be safe from infection. The American Dental Association has made many recommendations to increase the safety of providing oral health care during the COVID-19 pandemic, including screening patients for symptoms and increasing use of PPE.14 Providing adequate PPE for dentistry is essential for the protection of the overall oral health of the country. Increased costs and pent-up demand for PPE due to the pandemic might hinder some dental practices from functioning during this time. Specifically, practices that see a higher volume of patients per day or accept lower reimbursement insurance plans, such as Medicaid, might not be able to continue “normal” practice owing to lack of PPE. With oral health care already having the highest level of financial barrier compared with other health services,15 this could be detrimental to the care provided for our most vulnerable and underserved populations who often use these practices as their dental home.
Of the respondents in our survey, 95% could not work from home. This posed a considerable challenge to their ability to work if a dependent required care from them at home due to illness during the pandemic.
A major limitation of our study was the low estimated response rate. The response rate can only be estimated due to the dynamic nature of social media and social media groups and people joining and leaving those groups. It is also not possible to know how many of the members of each group are also part of another group that was sent the survey, or how many members are actually active in the groups and viewed the call for surveys.
The use of Facebook also limited our study because only those OHCWs that had access and ability to navigate to Facebook were able to participate in our study; however, use of social media to distribute surveys during the pandemic is not unprecedented and has had similarly low response rates.10 , 11 Owing to the quickly evolving nature of the pandemic, social media offered a unique opportunity to gather data quickly. In addition, although the survey had respondents from throughout the country, the proportion of respondents was higher from the Midwest region. This might have affected our findings in correlation with the timing of the survey (May 1-June 30, 2020), when COVID-19 cases were increasing in that region of the country. The timing of the survey might also have affected responses. The American Dental Association released guidance before the survey window; however, some states were still restricting oral health care to emergencies only, and dental offices were facing shortages of PPE. In our study, we provided a “snapshot” of OHCWs’ attitudes at that specific time during the pandemic. In a 1-year follow-up study, we will assess whether more information, access to PPE, and actual vaccine availability have changed these attitudes.
In our study, we set the groundwork for future research into the oral health care workforce during and after the coronavirus pandemic and future pandemics. Different sectors of the workforce can have different viewpoints that must be explored in future studies. Strategies must be implemented to ensure continued access to care for patients’ oral health from the entire oral health care team.
Conclusions
Within the limitations of our study, we arrived at the following conclusions:
-
▪
OHCWs have a decreased ability to report to work during a pandemic, with dentists being significantly more able to work than dental hygienists and dental assistants.
-
▪
OHCWs have a decreased willingness to report to work during a pandemic, with dentists being significantly more willing to report to work than dental hygienists and dental assistants.
-
▪
The most frequently reported barrier to report to work was the obligation to care for a family member, which was cited more frequently by dental hygienists and dental assistants than dentists.
-
▪
Dentists are more likely than hygienists and assistants, and hygienists are more likely than assistants, to receive a COVID-19 vaccine.
-
▪
Dentists are the least likely OHCW group to consider quitting their jobs or retiring during a pandemic.
-
▪
Dentists should be aware of the differences in ability and willingness to report to work and perceived barriers and concerns between dentists and staff members and be prepared to discuss alterations to standard operating procedures to allay staff members’ fears and improve retention rate during pandemics (Box 2 ).
Box 2.
| The American Dental Association and the Centers for Disease Control and Prevention have published recommendations related to practice staff member and patient safety during the COVID-19 pandemic. These recommendations can be found at |
| Practitioners are also encouraged to stay updated with recommendations of their state and local health departments. The Centers for Disease Control and Prevention Health Department Directory can be found at |
| The American Dental Association has provided and summarized resources related to the COVID-19 vaccine. They can be found at the following links: |
Biographies
Dr. Scully is a clinical assistant professor, School of Dentistry, Indiana University, Indianapolis, IN.
Dr. Joshi is a dentist in private practice, Fishers, IN; and an adjunct clinical assistant professor, School of Dentistry, Indiana University, Indianapolis, IN.
Dr. Rector is a pediatric dental resident, Riley Hospital for Children, Indianapolis, IN; and a pediatric dental resident, School of Dentistry, Indiana University, Indianapolis, IN.
Mr. Eckert is a biostatistician, Department of Biostatistics, School of Medicine, Indiana University, Indianapolis, IN.
This article has an accompanying online continuing education activity available at: http://jada.ada.org/ce/home.
Footnotes
Disclosure. None of the authors reported any disclosures.
References
- 1.Wu F., Zhao S., Yu B. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579(7798):265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.John Hopkins University and Medicine Coronavirus Resource Center. https://coronavirus.jhu.edu/ Available at:
- 3.Koh D. Occupational risks for COVID-19 infection. Occup Med (Lond) 2020;70(1):3–5. doi: 10.1093/occmed/kqaa036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Greenberg N., Docherty M., Gnanapragasam S., Wessely S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ. 2020;368:m1211. doi: 10.1136/bmj.m1211. [DOI] [PubMed] [Google Scholar]
- 5.COVID-19: protecting health-care workers. Lancet. 2020;395(10228):922. doi: 10.1016/S0140-6736(20)30644-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Damery S., Draper H., Wilson S. Healthcare workers' perceptions of the duty to work during an influenza pandemic. J Med Ethics. 2010;36(1):12–18. doi: 10.1136/jme.2009.032821. [DOI] [PubMed] [Google Scholar]
- 7.Gershon R.R., Magda L.A., Qureshi K.A. Factors associated with the ability and willingness of essential workers to report to duty during a pandemic. J Occup Environ Med. 2010;52(10):995–1003. doi: 10.1097/JOM.0b013e3181f43872. [DOI] [PubMed] [Google Scholar]
- 8.Mirchandani P. Health care supply chains: COVID-19 challenges and pressing actions. Ann Intern Med. 2020;173(4):300–301. doi: 10.7326/M20-1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.US Department of Health and Human Services Healthy People 2020: topics and objectives. http://www.healthypeople.gov/2020/topicsobjectives2020/ Available at:
- 10.Bakaeen L.G., Masri R., AlTarawneh S. Dentists’ knowledge, attitudes, and professional behavior toward the COVID-19 pandemic: a multisite survey of dentists’ perspectives. JADA. 2021;152(1):16–24. doi: 10.1016/j.adaj.2020.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moraes R.R., Correa M.B., Queiroz A.B. COVID-19 challenges to dentistry in the new pandemic epicenter: Brazil. PLoS One. 2020;15(11) doi: 10.1371/journal.pone.0242251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Surdu S., Mertz E., Langelier M., Moore J. Dental workforce trends: a national study of gender diversity and practice patterns. Med Care Res Rev. 2021;78(1 suppl):30S–39S. doi: 10.1177/1077558720952667. [DOI] [PubMed] [Google Scholar]
- 13.Gagneux-Brunon A., Detoc M., Bruel S. Intention to get vaccinations against COVID-19 in French healthcare workers during the first pandemic wave: a cross sectional survey. J Hosp Infect. 2021;108:168–173. doi: 10.1016/j.jhin.2020.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Solana K. ADA develops guidance on dental emergency, nonemergency care: recommendations part of dentists' response over COVID-19 concerns. ADA News. March 18, 2020.
- 15.Vujicic M., Buchmueller T., Klein R. Dental care presents the highest level of financial barriers, compared to other types of health care services. Health Aff (Millwood) 2016;35(12):2176–2182. doi: 10.1377/hlthaff.2016.0800. [DOI] [PubMed] [Google Scholar]