Abstract
Background
Asthma affects 350 million people worldwide including 45% to 70% with mild disease. Treatment is mainly with inhalers containing beta₂‐agonists, typically taken as required to relieve bronchospasm, and inhaled corticosteroids (ICS) as regular preventive therapy. Poor adherence to regular therapy is common and increases the risk of exacerbations, morbidity and mortality. Fixed‐dose combination inhalers containing both a steroid and a fast‐acting beta₂‐agonist (FABA) in the same device simplify inhalers regimens and ensure symptomatic relief is accompanied by preventative therapy. Their use is established in moderate asthma, but they may also have potential utility in mild asthma.
Objectives
To evaluate the efficacy and safety of single combined (fast‐onset beta₂‐agonist plus an inhaled corticosteroid (ICS)) inhaler only used as needed in people with mild asthma.
Search methods
We searched the Cochrane Airways Trials Register, Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE and Embase, ClinicalTrials.gov and the World Health Organization (WHO) trials portal. We contacted trial authors for further information and requested details regarding the possibility of unpublished trials. The most recent search was conducted on 19 March 2021.
Selection criteria
We included randomised controlled trials (RCTs) and cross‐over trials with at least one week washout period. We included studies of a single fixed‐dose FABA/ICS inhaler used as required compared with no treatment, placebo, short‐acting beta agonist (SABA) as required, regular ICS with SABA as required, regular fixed‐dose combination ICS/long‐acting beta agonist (LABA), or regular fixed‐dose combination ICS/FABA with as required ICS/FABA. We planned to include cluster‐randomised trials if the data had been or could be adjusted for clustering. We excluded trials shorter than 12 weeks. We included full texts, abstracts and unpublished data.
Data collection and analysis
Two review authors independently extracted data. We analysed dichotomous data as odds ratios (OR) or rate ratios (RR) and continuous data as mean difference (MD). We reported 95% confidence intervals (CIs). We used Cochrane's standard methodological procedures of meta‐analysis. We applied the GRADE approach to summarise results and to assess the overall certainty of evidence. Primary outcomes were exacerbations requiring systemic steroids, hospital admissions/emergency department or urgent care visits for asthma, and measures of asthma control.
Main results
We included six studies of which five contributed results to the meta‐analyses. All five used budesonide 200 μg and formoterol 6 μg in a dry powder formulation as the combination inhaler. Comparator fast‐acting bronchodilators included terbutaline and formoterol. Two studies included children aged 12+ and adults; two studies were open‐label. A total of 9657 participants were included, with a mean age of 36 to 43 years. 2.3% to 11% were current smokers.
FABA / ICS as required versus FABA as required
Compared with as‐required FABA alone, as‐required FABA/ICS reduced exacerbations requiring systemic steroids (OR 0.45, 95% CI 0.34 to 0.60, 2 RCTs, 2997 participants, high‐certainty evidence), equivalent to 109 people out of 1000 in the FABA alone group experiencing an exacerbation requiring systemic steroids, compared to 52 (95% CI 40 to 68) out of 1000 in the FABA/ICS as‐required group. FABA/ICS as required may also reduce the odds of an asthma‐related hospital admission or emergency department or urgent care visit (OR 0.35, 95% CI 0.20 to 0.60, 2 RCTs, 2997 participants, low‐certainty evidence).
Compared with as‐required FABA alone, any changes in asthma control or spirometry, though favouring as‐required FABA/ICS, were small and less than the minimal clinically‐important differences. We did not find evidence of differences in asthma‐associated quality of life or mortality. For other secondary outcomes FABA/ICS as required was associated with reductions in fractional exhaled nitric oxide, probably reduces the odds of an adverse event (OR 0.82, 95% CI 0.71 to 0.95, 2 RCTs, 3002 participants, moderate‐certainty evidence) and may reduce total systemic steroid dose (MD ‐9.90, 95% CI ‐19.38 to ‐0.42, 1 RCT, 443 participants, low‐certainty evidence), and with an increase in the daily inhaled steroid dose (MD 77 μg beclomethasone equiv./day, 95% CI 69 to 84, 2 RCTs, 2554 participants, moderate‐certainty evidence).
FABA/ICS as required versus regular ICS plus FABA as required
There may be little or no difference in the number of people with asthma exacerbations requiring systemic steroid with FABA/ICS as required compared with regular ICS (OR 0.79, 95% CI 0.59 to 1.07, 4 RCTs, 8065 participants, low‐certainty evidence), equivalent to 81 people out of 1000 in the regular ICS plus FABA group experiencing an exacerbation requiring systemic steroids, compared to 65 (95% CI 49 to 86) out of 1000 FABA/ICS as required group. The odds of an asthma‐related hospital admission or emergency department or urgent care visit may be reduced in those taking FABA/ICS as required (OR 0.63, 95% CI 0.44 to 0.91, 4 RCTs, 8065 participants, low‐certainty evidence).
Compared with regular ICS, any changes in asthma control, spirometry, peak flow rates (PFR), or asthma‐associated quality of life, though favouring regular ICS, were small and less than the minimal clinically important differences (MCID). Adverse events, serious adverse events, total systemic corticosteroid dose and mortality were similar between groups, although deaths were rare, so confidence intervals for this analysis were wide. We found moderate‐certainty evidence from four trials involving 7180 participants that FABA/ICS as required was likely associated with less average daily exposure to inhaled corticosteroids than those on regular ICS (MD ‐154.51 μg/day, 95% CI ‐207.94 to ‐101.09).
Authors' conclusions
We found FABA/ICS as required is clinically effective in adults and adolescents with mild asthma. Their use instead of FABA as required alone reduced exacerbations, hospital admissions or unscheduled healthcare visits and exposure to systemic corticosteroids and probably reduces adverse events. FABA/ICS as required is as effective as regular ICS and reduced asthma‐related hospital admissions or unscheduled healthcare visits, and average exposure to ICS, and is unlikely to be associated with an increase in adverse events.
Further research is needed to explore use of FABA/ICS as required in children under 12 years of age, use of other FABA/ICS preparations, and long‐term outcomes beyond 52 weeks.
Keywords: Adolescent, Adult, Child, Humans, Adrenal Cortex Hormones, Adrenal Cortex Hormones/administration & dosage, Adrenergic beta-2 Receptor Agonists, Adrenergic beta-2 Receptor Agonists/administration & dosage, Anti-Asthmatic Agents, Anti-Asthmatic Agents/administration & dosage, Asthma, Asthma/drug therapy, Beclomethasone, Beclomethasone/administration & dosage, Budesonide, Budesonide/administration & dosage, Disease Progression, Drug Combinations, Formoterol Fumarate, Formoterol Fumarate/administration & dosage, Hospitalization, Hospitalization/statistics & numerical data, Nebulizers and Vaporizers, Prednisolone, Prednisolone/administration & dosage, Quality of Life, Randomized Controlled Trials as Topic, Terbutaline, Terbutaline/administration & dosage
Plain language summary
Combination fixed‐dose beta agonist and steroid inhaler as required for adults or children with mild asthma
Background
Asthma is the most common respiratory illness. Many people with asthma have mild asthma, but still remain at risk of severe asthma exacerbations, which often result in the use of oral steroids. Mild asthma is commonly treated with preventative inhalers, which contain a steroid used to reduce inflammation in the airways, and with reliever inhalers, which relax the muscles of the airways causing quick relief of asthma symptoms. Combination inhalers contain both the preventative steroid and the reliever, simplifying treatment and ensuring steroids are always given alongside the immediate relief of symptoms.
Review question
We examined the findings of clinical trials to assess the use of combination inhalers in the treatment of mild asthma when taken on an as‐needed, symptom‐driven basis.
Study characteristics
We searched for studies up to March 2021. Results were collected from six studies which compared use of a combination inhaler used on an as‐needed basis with either as‐needed reliever‐only therapy or daily treatment with a low dose preventative inhaler.
Key findings
We found that combination inhalers used as‐needed when compared with reliever‐only treatment reduced severe exacerbations requiring tablet steroids and rates of emergency admission to hospital with asthma symptoms. Differences in other measures relating to symptom control and lung function were too small to be clinically important. Rates of severe exacerbations were similar between patients on daily preventative steroid inhalers and those using combination inhalers as‐needed. People using combination inhalers had lower rates of hospital admission and lower total inhaled steroid dose, whilst the differences in lung function and asthma symptom control were not clinically significant.
This review found the use of combination inhalers used when the patient experiences asthma symptoms was beneficial in reducing severe exacerbations when compared to stand‐alone reliever therapy in mild asthma. In addition to this the use of combination inhalers used on an as‐needed basis was associated with a reduction in hospital admissions and total inhaled steroid dose when compared with regularly‐taken low dose preventative inhaler therapy.
Quality of the evidence
The studies which contributed data were well‐designed and robust, although two were open‐label (participants knew which treatment they were getting), with some potential for bias, so the evidence was generally of moderate‐to‐high quality.
Summary of findings
Summary of findings 1. As‐required FABA/ICS inhalers compared to as‐required FABA inhalers for mild asthma.
| As‐required FABA/ICS inhalers compared to as‐required FABA inhalers for mild asthma | ||||||
| Patient or population: mild asthma Setting: community Intervention: as‐required FABA/ICS inhalers Comparison: as‐required FABA inhalers | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with as required FABA inhalers | Risk with as required FABA / ICS inhalers | |||||
| Asthma exacerbation requiring systemic steroid follow‐up: 52 weeks | 109 per 1,000 | 52 per 1,000 (40 to 68) | OR 0.45, 95% CI 0.34 to 0.60 | 2997 (2 RCTs) | ⊕⊕⊕⊕ HIGH 1 2 | People with mild asthma treated with combined inhalers have substantially fewer exacerbations requiring systemic steroid than those treated with FABA alone. |
| Hospital admission, ED and urgent care visits follow‐up: 52 weeks | 34 per 1,000 | 12 per 1,000 (7 to 21) | OR 0.35, 95% CI 0.20 to 0.60 | 2997 (2 RCTs) | ⊕⊕⊝⊝ LOW 2 3 | People with mild asthma treated with combined inhalers probably have substantially fewer exacerbations requiring hospital admission, ED attendance or urgent care visit than those treated with FABA alone. |
| Asthma control
follow‐up: 52 weeks Lower scores = better control. |
Mean baseline ACQ‐5 ranged from 1.1 to 1.61 | MD ‐0.15, 95% CI ‐0.20 to ‐0.10 | ‐ | 2859 (2 RCTs) | ⊕⊕⊕⊝ MODERATE 2 | MCID for ACQ‐5 is 0.5. A third study reported no difference in asthma symptom scores between the two arms. |
| Inhaled steroid dose assessed with: Mean daily inhaled steroid dose, μg beclomethasone equivalent follow‐up: 52 weeks | The mean inhaled steroid dose was 18.7 μg beclomethasone | MD 76.50 μg beclomethasone higher (69.40 higher to 83.60 higher) | ‐ | 2554 (2 RCTs) | ⊕⊕⊕⊝ MODERATE 2 | People with mild asthma treated with a combined inhaler have a higher daily inhaled steroid dose than those treated with a FABA alone. |
| Total systemic steroid dose assessed with: mg prednisolone total over 52 weeks follow‐up: 52 weeks | The mean total systemic steroid dose was 17.4 mg prednisolone | MD 9.90 mg prednisolone lower (19.38 lower to 0.42 lower); participants = 443) | ‐ | 443 (1 RCT) | ⊕⊕⊝⊝ LOW 2 4 | Total systemic steroid dose was similar and small in both those given combined inhalers and those given FABA alone. |
| Adverse events follow‐up: 52 weeks | 486 per 1,000 | 437 per 1,000 (402 to 473) | OR 0.82 (0.71 to 0.95) | 3002 (2 RCTs) | ⊕⊕⊕⊝ MODERATE 2 | Slightly fewer adverse events occurred in those taking combination inhalers compared with those taking FABA alone. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ACQ‐5: asthma control questionnaire ‐5; CI: Confidence interval; ED: emergency department; FABA: fast‐acting beta₂‐agonist; ICS: inhaled corticosteroids; MCID: minimum clinically important difference; MD: mean difference; OR: Odds ratio; RCT: randomised controlled trial. | ||||||
|
GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
1 Upgraded as large effect (OR < 0.5) with fairly tight confidence intervals.
2 Downgraded as included an open label study.
3 Downgraded as based on a small number of events
4 Downgraded as based on one study with a relatively small number of participants.
Summary of findings 2. As‐required FABA/ICS inhalers compared to regular inhaled steroid for mild asthma.
| As‐required FABA/ICS inhalers compared to regular inhaled steroid for mild asthma | ||||||
| Patient or population: mild asthma Setting: community Intervention: as‐required FABA/ICS inhalers Comparison: regular inhaled steroid | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with regular inhaled steroid | Risk with as required FABA / ICS inhalers | |||||
| Exacerbations requiring systemic steroid follow‐up: 52 weeks | 81 per 1,000 | 65 per 1,000 (49 to 86) | OR 0.79 (0.59 to 1.07) | 8065 (4 RCTs) | ⊕⊕⊝⊝ LOW 1 2 | Exacerbations requiring systemic steroid occurred less frequently in those treated with as required combination inhalers than those treated with regular inhaled steroid, but the 95%CI includes no difference. |
| Hospital admission, ED and urgent care visits follow‐up: 52 weeks | 19 per 1,000 | 12 per 1,000 (8 to 17) | OR 0.63 (0.44 to 0.91) | 8065 (4 RCTs) | ⊕⊕⊝⊝ LOW 1 3 | Fewer hospital admissions, ED attendances and urgent care visits occurred in those treated with as required combination inhalers compared with regular inhaled steroid. |
| Asthma control
assessed with: ACQ‐5,
follow‐up: 52 weeks Lower scores indicate better asthma control. |
The mean asthma control was ‐0.467 points, change from baseline | MD 0.12 points higher (0.09 higher to 0.15 higher) | ‐ | 7382 (4 RCTs) | ⊕⊕⊕⊕ HIGH | ACQ‐5 fell slightly more compared with baseline in those treated with regular inhaled steroid than those treated with combination inhalers. MCID for ACQ‐5 is 0.5 points. |
| Inhaled steroid dose assessed with: Mean daily dose in μg, beclomethasone equivalent follow‐up: 52 weeks | The mean inhaled steroid dose was 257.8 μg beclomethasone equivalent per day | (MD 154.51 μg/day lower (207.94 lower to 101.09 lower) | ‐ | 7180 (4 RCTs) | ⊕⊕⊕⊝ MODERATE 1 | Those treated with as required combination inhalers had a lower average daily inhaled steroid dose than those treated with a regular inhaled steroid. |
| Total systemic steroid dose assessed with: Mean cumulative dose of prednisolone over the course of the trial in mg follow up: 52 weeks | The mean total systemic steroid dose was 20.97 mg prednisolone | MD 7 mg prednisolone lower (13.97 lower to 0.03 lower) | ‐ | 1330 (2 RCTs) | ⊕⊕⊕⊝ MODERATE 1 | Total systemic steroid exposure was similar and low in those treated with regular inhaled steroid and those treated with as required combination inhalers. |
| Adverse events assessed with: Participants experiencing at least one adverse event follow‐up: 52 weeks | 493 per 1,000 | 482 per 1,000 (443 to 525) | OR 0.96 (0.82 to 1.14) | 8072 (4 RCTs) | ⊕⊕⊕⊝ MODERATE 1 | The proportion of participants experiencing at least one adverse event was similar in those treated with combination inhalers and those with regular inhaled steroid. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ACQ‐5: asthma control questionnaire‐5; CI: Confidence interval; ED: emergency department; FABA: fast‐acting beta₂‐agonist; ICS: inhaled corticosteroids; MCID: minimum clinically important difference; MD: mean difference; RCT: randomised controlled trial; OR: Odds ratio. | ||||||
|
GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
1 Downgraded as included open label studies
2 Downgraded as heterogeneity between trials at low risk of bias in all domains and those at high risk in at least one domain
3 Downgraded as based on a relatively small number of events
Background
Description of the condition
Asthma is the most common chronic respiratory disease, affecting 350 million people worldwide; and it is potentially serious, claiming 400,000 lives per year (GBD Study 2017; GINA 2019). Asthma is recognised as a heterogeneous disease, but common symptoms include wheezing, shortness of breath, chest tightness and cough; these vary over time in their occurrence, frequency and intensity (GINA 2019). Asthma is a clinical diagnosis defined by the history of a constellation of respiratory symptoms that vary over time and in intensity, together with variable expiratory airflow limitation (GINA 2019). Asthma treatment broadly focusses on maintaining daily symptom control and preventing acute worsening of symptoms known as asthma attacks or 'exacerbations'.
The seriousness of asthma varies greatly and severe asthma has attracted significant interest from researchers. Asthma control is the extent to which features of asthma are observed in an individual or have been reduced by treatment. Asthma severity is assessed retrospectively from the level of treatment required to control symptoms and exacerbations (GINA 2019). Globally, prevalence of mild asthma is estimated to be between 45% and 70% of all patients diagnosed with the condition (Rabe 2004; Dusser 2007; Sadatsafavi 2010). Despite being labelled as having mild asthma, this group continues to have severe asthma attacks requiring oral steroids or hospital admission (Bloom 2018), and suffer asthma‐related deaths (Bergström 2008; RCP 2014). Inhaled corticosteroids (ICS) are the most effective preventer drug for adults in achieving overall treatment goals and reducing mortality (Suissa 2000). Intermittence of symptoms in this population often leads to poor inhaler adherence (Taylor 2014). Up to 90% of people with asthma do not take ICS regularly as prescribed (AIHW 2007). Poor adherence to preventer ICS is thought to be a main cause for an increase in risk of exacerbations in people with mild asthma (Engelkes 2015).
Description of the intervention
Preventers and relievers
There are over 30 different inhalers now approved for use in asthma. They are usually classified as preventers or relievers. Short‐acting beta‐agonists (SABA) have been used since the 1970s for rapid relief of asthma symptoms from bronchoconstriction. They lead to rapid improvement of symptoms but do not affect the underlying pathological process (Barnes 1999).
Taking daily preventer steroid inhalers should lead to better asthma control (Chauhan 2013). Adherence to ICS is often poor, however, for a variety of reasons including fear of side effects, costs and perceptions of asthma severity (Bender 2005). Increasing the daily dose of the preventer ICS therapy during the early phase of an acute exacerbation has also been studied as a way to treat the exacerbation without the need for systemic corticosteroids (Kew 2016), though a benefit from this approach has not been shown. These regimens still depend on the use of a preventer even when the patient feels well; and they are still affected by poor adherence rates (Beasley 2019).
Longer‐acting beta₂ agonists (LABA) are also available. They are generally used as preventer medication and are co‐prescribed with an ICS. Some LABAs have a rapid onset of action and will also rapidly relieve symptoms (Wallin 1993). In this review, we refer to any beta agonist (SABA or LABA) that has a quick onset of action as a fast‐acting beta₂‐agonist (FABA).
Fixed‐dose combination inhalers
A number of combination inhalers exist. These contain both a steroid and a beta₂ agonist in the same device, thus delivering both treatments at the same time. This has the advantages of simplifying an inhaler regimen and ensuring LABA therapy is not taken without ICS. This is important because use of a LABA without an ICS is associated with a significantly increased risk of asthma death (Nelson 2006). In some, but not all, combination inhalers, the LABA is also a FABA, making the inhaler potentially suitable for as‐required use.
Exacerbations or 'attacks' are thought to be precipitated by external triggers (viral, bacterial, allergen or irritants) leading to an enhanced type 2 inflammatory response in the asthmatic airways (Papi 2018). The prodrome preceding an attack would be a logical time to intervene, especially if these are infrequent. The rapid‐acting beta₂ agonist will act immediately on the smooth muscle to relieve airway narrowing and resultant symptoms. ICS are thought to work by suppressing the type 2 inflammation at the epithelial level (Barnes 2010). Pairing the ICS with the beta₂ agonist therapy, specifically at the time of increased symptoms, could lead to both symptomatic improvement and suppression of the underlying pathological process, and importantly decrease the risk of severe or life‐threatening events (Beasley 2019). In patients with moderate asthma not controlled on medium‐dose ICS or ICS/LABA, fixed‐dose ICS/FABA inhalers used as both maintenance and reliever therapy (MART) is effective in reducing risk of asthma attacks (Cates 2013), but these data cannot necessarily be extrapolated to mild asthma or to use of the combination inhaler as‐required, without its use also as regular maintenance therapy.
How the intervention might work
This review focuses on fixed‐dose combination ICS/fast‐acting beta₂ agonist taken as needed — i.e. both treatments in the same inhaler. This is now being considered as a replacement for prescribing people either a SABA or SABA and a separate ICS. The idea is that when people's symptoms are worse they will take their inhaler more often to get symptom relief from the bronchodilator (Wallin 1993); and they will also get more steroid to treat the underlying inflammation (Barnes 2010). This also has the possible benefit of simplification due to the use of a single inhaler as well as reduced issues with adherence, and may in effect titrate the amount of ICS delivered to the individual's symptomatology.
Why it is important to do this review
Several clinical trials of as‐required fixed‐dose combination inhalers have been reported in recent years, and have led to a significant change in an international guideline (GINA 2019), which now recommends fixed‐dose ICS/FABA as first‐line therapy for mild asthma, where the previous guideline recommended use of SABA only. As the majority of economic costs of asthma are related to regular prescribing of preventer medications in primary care (Mukherjee 2016), this recommendation has major cost implications, particularly for public health systems in low‐ to middle‐income countries. There is also the potential for important benefits in improving symptom control, reducing exposure to systemic corticosteroids and reducing admissions; the last of which is a major contributor to the economic burden of asthma (Mukherjee 2016). Therefore, an accurate assessment of these benefits using all available randomised clinical trial data is timely, with implications for millions of people with asthma worldwide.
Objectives
To evaluate the efficacy and safety of single combined (fast‐acting beta₂‐agonist (FABA) plus an inhaled corticosteroid (ICS)) inhaler only used as needed in people with mild asthma.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) as well as cross‐over designs provided they included an appropriate washout period (a week or more) between interventions. We planned to include cluster‐randomised trials if the data had been or could be adjusted for clustering. We excluded trials of very short duration (an intervention of less than 12 weeks). We included studies reported in full text, those published as an abstract only and unpublished data.
Types of participants
We included adults and children (age 6 years and older) with a diagnosis of mild asthma as defined by GINA 2019: asthma that is well‐controlled with as‐needed controller medication alone, or with low‐intensity maintenance controller treatment. Where GINA definitions were not specified, review authors judged severity using baseline characteristics; an Asthma Control Questionnaire (ACQ) score less than or equal to 1.5 or an Asthma Control Test (ACT) score equal to or more than 16. We did not exclude participants based on non‐respiratory co‐morbidities, provided they also met the required definition for a diagnosis of asthma. We excluded participants with chronic obstructive pulmonary disease (COPD), defined by GOLD 2020; and any physician diagnosis of pulmonary fibrosis, bronchiectasis, lung cancer or other respiratory co‐morbidity. To ensure that we only investigated patients with mild asthma, we excluded patients taking moderate‐dose ICS daily (defined as greater than or equal to 300 μg per day of beclomethasone equivalent) or higher‐dose ICS daily (defined as greater than or equal to 600 μg per day of beclomethasone equivalent for adults and children aged 12 years or older).
Types of interventions
We included studies comparing a single fixed‐dose ICS/FABA inhaler used as needed with at least one of the following comparators.
No treatment
Placebo
As‐required SABA
Regular ICS with as‐required SABA
Regular fixed‐dose combination ICS/LABA, with or without as‐required SABA
Regular fixed‐dose combination ICS/LABA with as‐required ICS/FABA
Separate comparisons were done comparing single fixed‐dose ICS/FABA against each of the comparators listed above. Fast‐acting beta₂ agonists include salbutamol (albuterol), terbutaline, and formoterol.
We did not consider studies investigating other asthma treatments: if required, they would suggest severe asthma. Including systemic corticosteroids, leukotriene inhibitors, inhaled long‐acting anti‐cholinergics, methylxanthines and monoclonal antibodies.
Types of outcome measures
We analysed the following outcomes in the review, but did not use them as a basis for including or excluding studies. Where possible we analysed outcomes at the 12‐month time point.
Primary outcomes
Exacerbations requiring systemic steroids.
Hospital admissions/emergency department or urgent care visits for asthma.
Measures of asthma control: in order of preference Asthma Control Questionnaire (ACQ), Asthma Control Test (ACT), symptom‐free days.
Secondary outcomes
Measures of lung physiology: in order of preference post‐bronchodilator FEV₁, post‐bronchodilator peak expiratory flow rate (PEFR), FeNO, then other measures.
Quality of life measures, preferably Asthma Quality of Life Questionnaire (AQLQ), then the Short Form 36 (SF‐36).
Adverse events/side effects.
Total inhaled steroid dose. We converted inhaled steroid doses to beclomethasone equivalents using the conversion described in Table 3.
Total systemic corticosteroid dose.
Mortality.
1. Inhaled steroid equivalents.
| Drug | Dose considered equivalent to 100 μg beclomethasone dipropionate | Conversion factor |
| Beclometasone | 100 | 1.0 |
| Beclometasone (extra fine particles) | 50 | 2.0 |
| Budesonide | 100 | 1.0 |
| Fluticasone propionate | 50 | 2.0 |
| Fluticasone furoate | 12.5 | 8.0 |
| Mometasone | 50 | 2.0 |
| Ciclesonide | 62.5 | 1.6 |
Search methods for identification of studies
Electronic searches
We identified studies from searches of the following databases and trial registries.
Cochrane Airways Trials Register (Cochrane Airways 2019), via the Cochrane Register of Studies, all years to 19 March 2021.
Cochrane Central Register of Controlled Trials (CENTRAL) in the Cochrane Library, via the Cochrane Register of Studies, all years to 19 March 2021.
MEDLINE Ovid SP 1946 to 18 March 2021 (searched 19 March 2021).
Embase Ovid SP 1974 to week 10 2021 (searched 19 March 2021).
US National Institutes of Health Ongoing Trials Register (www.ClinicalTrials.gov).
World Health Organization International Clinical Trials Registry Platform (apps.who.int/trialsearch).
We present the database search strategies in Appendix 1. The search strategy was developed in MEDLINE by the Cochrane Airways Information Specialist in collaboration with the authors, and then adapted for use in the other databases.
We searched all databases and trials registries from their inception to 19 March 2021, and we imposed no restriction regarding language or type of publication. We identified hand searched conference abstracts and grey literature through the Cochrane Airways Trials Register and the CENTRAL database.
Searching other resources
We checked the reference lists of all primary studies and review articles for additional references. We searched relevant manufacturers' websites for study information.
We searched on PubMed for errata or retractions from included studies published in full text on 30 March 2021.
Data collection and analysis
Selection of studies
We used Cochrane's Screen4Me workflow to help assess the search results. Screen4Me comprises three components: known assessments – a service that matches records in the search results to records that have already been screened in Cochrane Crowd and have been labelled as 'RCT' or 'Not an RCT'; the RCT classifier – a machine learning model that distinguishes RCTs from non‐RCTs; and, if appropriate, Cochrane Crowd (crowd.cochrane.org) – Cochrane's citizen science platform where 'the crowd' help to identify and describe health evidence. More detailed information about the Screen4Me components can be found in the following publications: McDonald 2017; Thomas 2017; Marshall 2018; Noel‐Storr 2018.
Following this initial assessment, four review authors (ST, FY, MG, AF) screened the titles and abstracts of the remaining search results independently using Rayyan (Ouzzani 2016), and coded them as 'retrieve' (eligible or potentially eligible/unclear) or 'do not retrieve', with each abstract being screened by at least two review authors. We retrieved the full‐text study reports of all potentially eligible studies and two review authors (two of ST, FY, RR, MG and AF) independently screened them for inclusion, recording the reasons for exclusion of ineligible studies. We resolved any disagreement through discussion or, if required, consulted a third person/review author (IC or TSCH). We identified and excluded duplicates and collated multiple reports of the same study so that each study, rather than each report, was the unit of interest in the review. We recorded the selection process in sufficient detail to complete a PRISMA flow diagram and 'Characteristics of excluded studies' table (Moher 2009). Ouzzani 2016.
Data extraction and management
We used a data collection form which had been piloted on at least one study in the review for study characteristics and outcome data. Two review authors out of FY, RR, PW, EOB, SR and MG extracted the following study characteristics from each included study.
Methods: study design, total duration of study, details of any 'run‐in' period, number of study centres and location, study setting, withdrawals and date of study.
Participants: N, mean age, age range, gender, severity of condition, diagnostic criteria, baseline lung function, smoking history, inclusion criteria and exclusion criteria.
Interventions: intervention, comparison (including types and doses of beta agonist and corticosteroid), concomitant medications, prior medications and excluded medications.
Outcomes: primary and secondary outcomes specified and collected, and time points reported.
Notes: funding for studies and notable conflicts of interest of trial authors.
Two review authors (out of FY, RR, PW, EOB, SR and MG) independently extracted outcome data from included studies. We noted in the 'Characteristics of included studies' table if outcome data were not reported in a usable way. We resolved disagreements by discussion or by involving a third person/review author (IC or TSCH) to reach consensus. One review author (IC) transferred data into the Review Manager 5 file (Review Manager 2014). We double‐checked that data were entered correctly by comparing the data presented in the systematic review with the study reports. A second review author (TSCH) spot‐checked study characteristics for accuracy against the study report.
Assessment of risk of bias in included studies
Two review authors (SR, GH) assessed risk of bias independently for each study using the criteria outlined in version 5.1 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We resolved any disagreements by discussion or by involving another author (IC or TSCH). We assessed the risk of bias according to the following domains.
Random sequence generation
Allocation concealment
Blinding of participants and personnel
Blinding of outcome assessment
Incomplete outcome data
Selective outcome reporting
Other bias
We judged each potential source of bias as high, low or unclear risk and provide a quote from the study report together with a justification for our judgement in the 'Risk of bias' table. We summarised the 'Risk of bias' judgements across different studies for each of the domains listed. We considered blinding separately for different key outcomes where necessary (e.g. for unblinded outcome assessment, risk of bias for all‐cause mortality may be very different than for a patient‐reported pain scale). Where information on risk of bias related to unpublished data or correspondence with a trialist, we noted this in the 'Risk of bias' table.
When considering treatment effects, we took into account the risk of bias for the studies that contribute to that outcome.
Assessment of bias in conducting the systematic review
We conducted the review according to this published protocol and justified any deviations from it in the 'Differences between protocol and review' section of the review.
Measures of treatment effect
We analysed dichotomous data as odds ratios (OR) or (where appropriate) rate ratios (RR) and continuous data as the mean difference (MD).We planned to use the standardised mean difference (SMD) to combine trials that measured the same outcome but used different methods. If data from rating scales were combined in a meta‐analysis, we ensured they were entered with a consistent direction of effect (e.g. lower scores always indicate improvement).
We undertook meta‐analyses only where this is meaningful: that is, if the treatments, participants and the underlying clinical question were similar enough for pooling to make sense.
We described skewed data narratively (for example, as medians and interquartile ranges for each group).
Where multiple trial arms were reported in a single study, we included only the relevant arms. If two comparisons (e.g. drug A versus placebo and drug B versus placebo) were combined in the same meta‐analysis, we either combined the active arms or halved the control group to avoid double‐counting.
If adjusted analyses were available (ANOVA or ANCOVA), we used these as a preference in our meta‐analyses. If both change from baseline and endpoint scores were available for continuous data, we used change from baseline unless there was low correlation between measurements in individuals. If a study reported outcomes at multiple time points, we used 12 months preferentially, with three months as a 'second choice'.
We used intention‐to‐treat (ITT) or 'full analysis set' analyses where they were reported (i.e. those where data had been imputed for participants who were randomly assigned but did not complete the study) instead of completer or per protocol analyses
Unit of analysis issues
For outcomes involving event counts where participants may have had multiple events (exacerbations, hospitalisations) and three or 12 month incidence rates were available, we used events primarily as the unit of analysis rather than participants. For other dichotomous outcomes and where incidence rate ratios were not available, we used participants, rather than events, as the unit of analysis (i.e. number of children admitted to hospital, rather than number of admissions per child).
Dealing with missing data
We contacted investigators or study sponsors in order to verify key study characteristics and obtain missing numerical outcome data where possible (e.g. when a study was identified as an abstract only). When this was not possible, and the missing data were thought to introduce serious bias, we took this into consideration in the GRADE rating for affected outcomes.
Assessment of heterogeneity
We used the I² statistic to measure heterogeneity among the studies in each analysis. When we identified substantial heterogeneity we reported it and planned to explore the possible causes by prespecified subgroup analysis.
We defined substantial heterogeneity using the following ranges from Higgins 2019:
0% to 40%: might not be important;
30% to 60%: may represent moderate heterogeneity;
50% to 90%: may represent substantial heterogeneity;
75% to 100%: considerable heterogeneity
Assessment of reporting biases
Had we been able to pool more than 10 studies, we planned to create and examine a funnel plot to explore possible small‐study and publication biases.
Data synthesis
We performed meta‐analysis using RevMan Web. We used a random‐effects model and performed a sensitivity analysis with a fixed‐effect model.
Subgroup analysis and investigation of heterogeneity
We planned to carry out the following subgroup analyses.
Adults and adolescents versus children (i.e. 12 years and over versus under 12 years) in keeping with GINA 2019 definitions
High versus low eosinophil counts (for trials where this was reported, using the trialists' definition of high and low)
High versus low FeNO (where reported, using the trialists' definition of high and low)
By inhaler component drugs (i.e. by each inhaled steroid drug and by short‐ or long‐acting beta agonist)
We planned to use the following outcomes in subgroup analyses.
Exacerbations requiring oral steroid
Hospital admissions/emergency department or urgent care visits for asthma
Measures of asthma control
For this review, we did not identify studies that would allow such subgroup analyses.
Sensitivity analysis
We planned to carry out sensitivity analyses, removing the following from the primary outcome analyses.
Trials deemed at high risk of bias in at least one domain
Cross‐over (as opposed to parallel group) trials
Trials in which asthma severity is not explicitly stated, but only derived from baseline characteristics
For this review, only the first sensitivity analysis was possible. We compared the results from a fixed‐effect model with the random‐effects model.
Summary of findings and assessment of the certainty of the evidence
We created 'Summary of findings' tables using the following outcomes.
Exacerbations requiring systemic steroids
Hospital admissions/emergency department or urgent care visits for asthma
Asthma control, preferably measured by the Asthma Control Questionnaire
Inhaled steroid dose
Total systemic steroid dose
Adverse events
We used the five GRADE considerations (risk of bias; consistency of effect; imprecision; indirectness; and publication bias) to assess the certainty of a body of evidence as it relates to the studies that contributed data for the prespecified outcomes. We used the methods and recommendations described in Section 8.5 and Chapter 12 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2019), using GRADEpro software (GRADEpro GDT). We justified all decisions to downgrade the certainty of studies using footnotes and we made comments to aid the reader's understanding of the review where necessary.
Results
Description of studies
Results of the search
We identified 14,045 records in our literature search conducted in December 2019: 6597 records were removed as duplicates; 108 were excluded by Cochrane Crowd Known Assessments; and 1490 by the Cochrane RCT classifier. We excluded a further 5526 records on the basis of title and abstract. An additional search in March 2021 identified a further 612 records, 257 of which were removed as duplicates. A further 17 were removed by Cochrane Crowd Known Assessments and 78 by the RCT classifier. From the remaining 260 records, two new ongoing studies were identified as well as 10 new references to studies that had already been included. The literature search is summarised in Figure 1.
1.

Included studies
Six studies met our inclusion criteria (Characteristics of included studies). Four of those (Novel START, PRACTICAL, SYGMA 1 and SYGMA 2) were large studies from the same research group and we identified multiple records referring to each of these studies.There was one record for Haahtela 2006, a peer‐reviewed journal article. A further study (Tanaka 2017) was only mentioned in a brief conference abstract. The authors of this abstract did not respond to requests for further information.
Two studies (SYGMA 1 and SYGMA 2) included children aged 12 and over as well as adults. The other four studies included adults only. We did not identify any trial that accepted participants under the age of 12. A total of 9657 participants were included in the five trials included in the meta analysis. There were a further 28 participants in Tanaka 2017.
No trials compared as‐required combination inhalers with no treatment, placebo or regular combination inhalers.
As‐required combination inhaler compared with as‐required fast‐acting beta agonist (FABA)
Three studies (SYGMA 1, Novel START and Haahtela 2006) compared an as‐required combined inhaled corticosteroid (ICS) and fast‐acting beta‐agonist (FABA) inhaler with an as required beta‐agonist. Both SYGMA 1 and Novel START used budesonide 200 μg with formoterol 6 μg as the combination inhaler. The beta‐agonist was terbutaline (0.5 mg per puff) in SYGMA 1 and salbutamol (2 puffs of 100 μg each) in Novel START. Haahtela 2006 compared as‐required combined budesonide (160 μg) and formoterol (4.5 μg) with as‐required formoterol (4.5 μg).
As‐required combination inhaler compared with regular inhaled steroid plus as required fast‐acting beta agonist (FABA)
Five studies compared an as‐required FABA/ICS combination inhaler versus regular inhaled steroid plus an as‐required beta‐agonist. SYGMA 1, SYGMA 2, Novel START and PRACTICAL all compared the combination of budesonide 200 μg and formoterol 6 μg with regular budesonide 200 μg twice daily. The as‐required beta‐agonist given with the regular budesonide was salbutamol (200 μg) in Novel START and terbutaline (500 μg) in the other three studies. Tanaka 2017 compared budesonide 320 μg with formoterol 9 μg as required with regular budesonide 160 μg once daily. It was not stated whether or not those receiving regular budesonide in this study also got an as‐required beta‐agonist.
Excluded studies
We examined a large number (N = 293) of full‐text records as our initial search identified many records with a title but no abstract (see Characteristics of excluded studies). The main reason for excluding records at this stage was that the study did not include an arm with participants treated on a purely as‐required basis with a combination inhaled steroid and rapid acting beta‐agonist inhaler. Such studies often included a regular dose of the combination inhaler in addition to as‐required doses in the intervention arm or delivered the beta‐agonist and inhaled steroid using separate devices. Thirty‐eight records were excluded as the study enrolled participants with moderate or severe asthma and we were not able to identify a subgroup with mild asthma from the study. Twenty‐seven studies looked at interventions lasting less than 12 weeks. Many of these studies would also have been excluded for lack of an appropriate intervention arm. Seventeen studies were excluded as the only combination inhaler used contained a beta‐agonist that was not fast‐acting, for example, salmeterol. All of these studies also lacked an appropriate intervention arm. Other records were excluded because they were review articles or correspondence to journals, not describing original studies (21 records), or because they described studies without randomisation (three records).
We identified two ongoing studies that would potentially meet our inclusion criteria (see Characteristics of ongoing studies). ACTRN12620001091998 2020 will compare as‐required salbutamol with as‐required budesonide‐formoterol in children aged 5 to 15 years, but as of October 2020, had yet to start recruiting. NCT04215848 2020 is comparing budesonide‐formoterol with regular budesonide in adults and scheduled to complete in late 2021.
Risk of bias in included studies
We assessed risk of bias using the Cochrane 'Rrisk of bias' tool from Higgins 2011. The revised 'RoB 2' tool from Higgins 2019 was not in widespread use at the time our protocol was written. The 'Risk of bias' assessments are summarised in Figure 2.
2.

'Risk of bias' summary review
Allocation
We did not have enough information to assess the allocation and randomisation procedures in Tanaka 2017, and therefore marked it at uncertain risk of bias in this domain. The other studies were felt to be at low risk.
Blinding
Novel START ,PRACTICAL and Tanaka 2017 were all open‐label studies and were therefore judged at high risk of bias in these domains. The other studies were judged at low risk of bias.
Incomplete outcome data
Tanaka 2017 had an 18% dropout rate with a suspicion that dropout was related to treatment allocation, so was judged at high risk of attrition bias. We felt we had insufficient information on dropout in Haahtela 2006 and so rated it as at unclear risk of attrition bias. The other studies were felt to be low risk in this domain.
Selective reporting
We judged Tanaka 2017 to be at high risk of selective reporting bias on the limited and vague details in the conference abstract. Without an identified published protocol, it was unclear whether there was any selective reporting in the Haahtela 2006 study. The other studies all had published protocols and we were able to confirm that the reported outcomes matched the protocols.
Other potential sources of bias
We did not identify any other potential sources of bias in the included studies. It should be noted that four of the RCTs contributing data were funded by AstraZeneca.
Effects of interventions
All outcomes discussed are at 52 weeks unless otherwise stated. For an overview of the data and judgements on the certainty see Table 1 and Table 2.
As‐required combination inhalers compared with as‐required fast‐acting beta‐agonists (FABA)
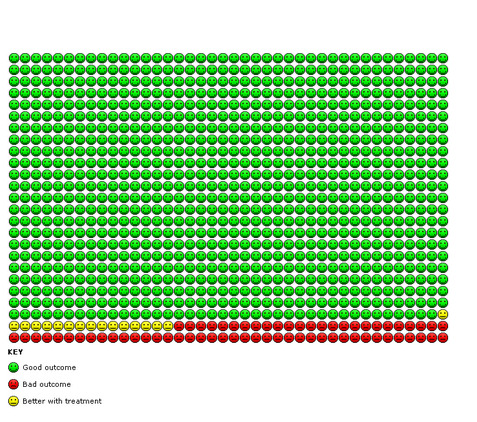
Exacerbations requiring systemic steroids
We found evidence from two trials (Novel START, SYGMA 1) that compared with as‐required beta‐agonists alone, as‐required FABA/ICS significantly reduced the number of asthma exacerbations requiring systemic steroid over a 52‐week period (odds ratio (OR) 0.45, 95% confidence interval (CI) 0.34 to 0.60; participants = 2997, high‐certainty evidence, Figure 3Analysis 1.1). In the control group 109 people out of 1000 had exacerbations requiring systemic steroids over 52 weeks, compared to 52 (95% CI 40 to 68) out of 1000 for the active treatment group (Figure 4).
3.

1.1. Analysis.

Comparison 1: As required fixed dose combination inhaler versus as required short acting beta agonist, Outcome 1: Asthma exacerbations requiring systemic steroid
4.

In the FABA as required group, 109 people out of 1000 had exacerbations requiring systemic steroids over 52 weeks, compared to 52 (95% CI 40 to 68) out of 1000 for the FABA/ICS as required group.
Data from the same two studies showed an overall reduction in the annual exacerbation rate (Rate ratio 0.41, 95% CI 0.30 to 0.55; participants = 2997, Analysis 1.2). The third study that looked at this comparison (Haahtela 2006) did not record exacerbation rates or numbers.
1.2. Analysis.

Comparison 1: As required fixed dose combination inhaler versus as required short acting beta agonist, Outcome 2: Annual exacerbation rate
Hospital admissions/emergency department or urgent care visits for asthma
We found a reduction in the odds of hospital admission or emergency department or urgent care visit for asthma in participants given as‐required FABA/ICS compared with as‐required short‐acting beta‐agonists (SABA) alone (OR 0.35, 95% CI 0.20 to 0.60; participants = 2997, low‐certainty evidence, Analysis 1.3).
1.3. Analysis.

Comparison 1: As required fixed dose combination inhaler versus as required short acting beta agonist, Outcome 3: Exacerbations requiring hospital admission or emergency department / urgent care visit
Measures of asthma control
Three studies in this area reported measures of asthma control. Haahtela 2006 reported no difference in asthma symptom scores between the two arms. Novel START reported slightly lower ACQ‐5 scores (with lower scores indicating better asthma control) at some, but not all time points in the study and the differences were less than the typical minimal clinically important difference (MCID) of 0.5. SYGMA 1 reported slightly better improvements from baseline in ACQ‐5 in the as‐required FABA/ICS group compared with the as‐required SABA alone group, but again not reaching the point of clinical significance. The combined change from baseline scores and endpoint scores at longest follow‐up favoured as‐required FABA/ICS, but did not exceed the MCID (MD ‐0.15, 95% CI ‐0.20 to ‐0.10; participants = 2859, moderate‐certainty evidence, Analysis 1.4). The number of "electronically recorded weeks with well controlled asthma" were slightly higher in the as‐required FABA/ICS group in SYGMA 1 compared with as‐required SABA.
1.4. Analysis.

Comparison 1: As required fixed dose combination inhaler versus as required short acting beta agonist, Outcome 4: ACQ‐5
Measures of lung function
The three studies captured data on pre bronchodilator FEV1 (rather than post bronchodilator). In two studies (Haahtela 2006 and SYGMA 1), there was a larger increase in FEV1 on treatment compared with baseline on as‐required FABA/ICS compared with as‐required SABA (MD 64.03 mL, 95% CI 27.49 to 100.57; participants = 2596, Analysis 1.5). This difference is less than the MCID for FEV1 of about 100 mL. Novel START reported no statistically significant difference in FEV1 between as‐required FABA/ICS and as‐required SABA at any time point.
1.5. Analysis.

Comparison 1: As required fixed dose combination inhaler versus as required short acting beta agonist, Outcome 5: FEV1 change from baseline
SYGMA 1 found a smaller drop in both morning and evening peak expiratory flow rate (PEFR) in the as‐required FABA/ICS group compared with the as‐required SABA group. The magnitude of the differences was small at around 10 to 12 L/minute. The other studies did not report PEFR.
Novel START reported a 17% reduction in mean FeNO at 52 weeks in the as‐required FABA/ICS group compared to as‐required SABA using a ratio of geometric means due to skew (ratio of geometric means 0.83, 95% CI 0.75 to 0.92; participants = 387, Analysis 1.6). Similarly, Haahtela 2006 showed a bigger decrease in FeNO from baseline to treatment in those treated with as‐required FABA/ICS compared with as‐required SABA (MD ‐15.50 parts per billion (ppb), 95% CI ‐23.39 to ‐7.61; participants = 93, Analysis 1.7). SYGMA 1 did not collect FeNO data.
1.6. Analysis.

Comparison 1: As required fixed dose combination inhaler versus as required short acting beta agonist, Outcome 6: FeNO [ppb]
1.7. Analysis.

Comparison 1: As required fixed dose combination inhaler versus as required short acting beta agonist, Outcome 7: FeNO change from baseline
Quality of life measures
Asthma quality of life questionnaire (AQLQ) scores were reported in SYGMA 1, but only available in graphical form. AQLQ did not differ between any of the arms by a clinically significant amount at any time point. The other two trials did not report quality of life data.
Adverse events
We did not find a clear difference in serious adverse events in the three trials reporting this outcome, although events were infrequent and confidence intervals wide (OR 1.31, 95% CI 0.50 to 3.46; participants = 3095, Analysis 1.8). In the two trials reporting all adverse events, the odds of an adverse event were about 18% lower in the as‐required FABA/ICS group compared with as‐required SABA (OR 0.82, 95% CI 0.71 to 0.95; participants = 3002,moderate‐certainty evidence, Analysis 1.9).
1.8. Analysis.

Comparison 1: As required fixed dose combination inhaler versus as required short acting beta agonist, Outcome 8: Serious adverse events
1.9. Analysis.

Comparison 1: As required fixed dose combination inhaler versus as required short acting beta agonist, Outcome 9: All adverse events
Total inhaled steroid dose
The daily inhaled steroid dose was unsurprisingly higher in the as‐required FABA/ICS group than the as‐required SABA group. It appears that some participants in the as‐required SABA arm of SYGMA 1 did receive inhaled steroids and data were provided that is displayed in Analysis 1.10 (MD 77 μg beclomethasone equivalent/day, 95% CI 69 to 84; participants = 2554). Haahtela 2006 did not report daily inhaled steroid doses but we estimate these to be around 130 μg beclomethasone equivalent in the as‐required FABA/ICS group based on the average weekly number of as required medication doses. It does not appear that the as‐required SABA arm in Haahtela 2006 or Novel START had any inhaled steroid exposure.
1.10. Analysis.

Comparison 1: As required fixed dose combination inhaler versus as required short acting beta agonist, Outcome 10: Daily inhaled steroid dose
Total systemic corticosteroid dose
Only Novel START reported systemic corticosteroid doses. These did not differ between the as‐required FABA/ICS and as required SABA arms (Analysis 1.11). The majority of participants in both arms did not receive systemic steroids.
1.11. Analysis.

Comparison 1: As required fixed dose combination inhaler versus as required short acting beta agonist, Outcome 11: Total systemic corticosteroid dose
Mortality
We found no difference in mortality between as required FABA/ICS and as required SABA (Analysis 1.12), however this is based on a single death in the three studies (in an as‐required FABA/ICS arm) so we have very low confidence in the precision of this result.
1.12. Analysis.

Comparison 1: As required fixed dose combination inhaler versus as required short acting beta agonist, Outcome 12: Mortality
As‐required combination inhalers compared with regular inhaled steroids
Exacerbations requiring systemic steroids
We found evidence based on four studies (Novel START, PRACTICAL, SYGMA 1 and SYGMA 2) that the odds of an asthma exacerbation requiring systemic steroids were reduced in participants treated with as‐required FABA/ICS compared with regular ICS, but confidence intervals include no difference (OR 0.79, 95% CI 0.59 to 1.07; participants = 8065, low‐certainty evidence, Figure 5, Analysis 2.1). In the control group 81 people out of 1000 had exacerbations requiring systemic steroids over 52 weeks, compared to 65 (95% CI 49 to 86) out of 1000 for the active treatment group (Figure 6).
5.

2.1. Analysis.

Comparison 2: Fixed dose combination inhaler as required versus regular inhaled steroid plus as required short acting beta agonist, Outcome 1: Number of exacerbations requiring systemic steroid
6.
In the regular ICS group 81 people out of 1000 had exacerbations requiring systemic steroids over 52 weeks, compared to 65 (95% CI 49 to 86) out of 1000 for the FABA/ICS as required group.
The annual rate of asthma exacerbations requiring systemic steroid was similar in both groups (rate ratio 0.90, 95% CIs 0.76 to 1.06, participants = 8065, Analysis 2.2). Tanaka 2017 reported that one participant discontinued the study because of an asthma exacerbation but otherwise does not give further information on exacerbation rates.
2.2. Analysis.

Comparison 2: Fixed dose combination inhaler as required versus regular inhaled steroid plus as required short acting beta agonist, Outcome 2: Annual severe exacerbation rate
Hospital admissions/emergency department or urgent care visits for asthma
There were fewer exacerbations of asthma requiring either hospital admission or a visit to an emergency department or urgent care clinic in participants taking as‐required FABA/ICS compared with regular ICS (OR 0.63, 95% CI 0.44 to 0.91; participants = 8065,low‐certainty evidence, Analysis 2.3).
2.3. Analysis.

Comparison 2: Fixed dose combination inhaler as required versus regular inhaled steroid plus as required short acting beta agonist, Outcome 3: Exacerbations requiring hospital admission or emergency department / urgent care visit
Measures of asthma control
Two studies (Novel START and PRACTICAL) reported ACQ‐5 at last trial visit and two studies (SYGMA 1 and SYGMA 2) reported change in ACQ‐5 from baseline. We combined these scores in Analysis 2.4. We found that analyses of these data showed a statistical advantage to regular ICS compared with as‐required FABA/ICS but the absolute differences were small and probably not clinically significant (MD 0.12, 95% CI 0.09 to 0.15; participants = 7382). The MCID in ACQ‐5 is around 0.5 points.
2.4. Analysis.

Comparison 2: Fixed dose combination inhaler as required versus regular inhaled steroid plus as required short acting beta agonist, Outcome 4: ACQ‐5
Tanaka 2017 reported no difference in mean ACQ‐5 scores at 4, 8, 16 and 24 weeks between regular ICS and as‐required FABA/ICS without giving values for mean ACQ‐5 score.
Measures of lung function
Two studies (PRACTICAL and Novel START) reported (probably pre‐bronchodilator) FEV1 at 52 weeks. We found no difference between as‐required FABA/ICS and regular ICS for this outcome (MD ‐0.01 L 95% CIs ‐0.11 to 0.09, participants = 1199, Analysis 2.5). SYGMA 1 and SYGMA 2 reported the change in FEV1 from baseline. FEV1 was 38 mL lower in the as‐required FABA/ICS group compared with regular ICS (MD ‐37.68 mL, 95% CIs ‐68.19 to ‐7.17; participants = 6287, Analysis 2.6). This finding is below the MCID in FEV1 of around 100 mL. Tanaka 2017 reported no difference in mean change in FEV1 and FVC from baseline without giving absolute values or specifying whether they were pre or post bronchodilator.
2.5. Analysis.

Comparison 2: Fixed dose combination inhaler as required versus regular inhaled steroid plus as required short acting beta agonist, Outcome 5: FEV1
2.6. Analysis.

Comparison 2: Fixed dose combination inhaler as required versus regular inhaled steroid plus as required short acting beta agonist, Outcome 6: FEV1 change from baseline
SYGMA 1 found that morning and evening PEFR increased slightly in the regular ICS group compared with baseline and fell slightly compared with baseline in the as‐required FABA/ICS group. The absolute differences between as‐required FABA/ICS and regular ICS in change in peak flow from baseline were small, less than 10 L/minute. The other studies did not report PEFR data.
Two studies (PRACTICAL and Novel START) reported data on FeNO. Both studies reported the ratio of geometric means due to skew in this outcome, which indicated that mean FeNO levels at 52 weeks were 13% higher in the as‐required FABA/ICS arm compared to the regular ICS arm (OR 1.13, 95% CI 1.06 to 1.20; participants = 1197, Analysis 2.7) .
2.7. Analysis.

Comparison 2: Fixed dose combination inhaler as required versus regular inhaled steroid plus as required short acting beta agonist, Outcome 7: FeNO [ppb]
Quality of life measures
Both SYGMA 1 and SYGMA 2 collected data on AQLQ but the findings were only available in graphical form. AQLQ scores were generally higher in the regular ICS arms compared with as‐required FABA/ICS but by less than the minimal clinically important difference of 0.5 points.
Tanaka 2017, Novel START and PRACTICAL did not report quality of life measures.
Adverse events
Serious adverse events occurred at similar rates in the as‐required FABA/ICS and regular ICS arms across four trials, although confidence intervals are wide (OR 1.14, 95% CI 0.82 to 1.57; participants = 8072, Analysis 2.8). We found similar odds of experiencing any adverse event in the two groups (OR 0.96, 95% CIs 0.82 to 1.14; participants = 8072, moderate‐certainty evidence, Analysis 2.9). Other than reporting a discontinuation due to an asthma exacerbation, Tanaka 2017 did not report adverse events.
2.8. Analysis.

Comparison 2: Fixed dose combination inhaler as required versus regular inhaled steroid plus as required short acting beta agonist, Outcome 8: Serious adverse events
2.9. Analysis.

Comparison 2: Fixed dose combination inhaler as required versus regular inhaled steroid plus as required short acting beta agonist, Outcome 9: All adverse events
Total inhaled steroid dose
We found that participants randomised to as‐required FABA/ICS received about 150 μg less ICS (beclomethasone equivalent) per day than those on regular ICS (MD ‐154.51 μg/day, 95% CI ‐207.94 to ‐101.09; participants = 7180; moderate‐certainty evidence, Analysis 2.10). Tanaka 2017 did not report data on ICS usage.
2.10. Analysis.

Comparison 2: Fixed dose combination inhaler as required versus regular inhaled steroid plus as required short acting beta agonist, Outcome 10: Daily inhaled steroid dose
Total systemic corticosteroid dose
Using data from two studies (PRACTICAL; Novel START), we found similar total systemic steroid exposure in the as‐required FABA/ICS and regular ICS groups (MD ‐7.00 mg prednisolone, 95% CI ‐13.97 to ‐0.03; participants = 1330, moderate‐certainty evidence, Analysis 2.11) The other three studies did not report systemic steroid doses. There were numerically fewer total days on systemic steroid in the as‐required FABA/ICS group compared with regular ICS in SYGMA 1 (465 versus 500 days). SYGMA 2 reported that those in the as‐required FABA/ICS and the regular ICS groups had the same median number of days on systemic steroids (six days). Tanaka 2017 did not report data on systemic steroid usage.
2.11. Analysis.

Comparison 2: Fixed dose combination inhaler as required versus regular inhaled steroid plus as required short acting beta agonist, Outcome 11: Total systemic corticosteroid dose
Mortality
There was no clear difference in the risk of death between as‐required FABA/ICS and regular ICS four studies (OR 0.63, 95% CI 0.12 to 3.25; participants = 8070, Analysis 2.12). This analysis is based on a small number of events and consequently has very broad confidence intervals. Tanaka 2017 didn't report information on mortality.
2.12. Analysis.

Comparison 2: Fixed dose combination inhaler as required versus regular inhaled steroid plus as required short acting beta agonist, Outcome 12: Mortality
Subgroup analyses
Our preplanned subgroup analyses were not possible, given the lack of studies covering these areas. In particular, we found no studies recruiting children (under 12 years) and included studies used the combination of formoterol and budesonide rather than other combination inhalers. We found little evidence of heterogeneity across the majority of outcomes studied. This is perhaps unsurprising as the bulk of the data came from studies carried out using similar methodology, led by one research group.
Sensitivity analyses
No cross‐over trials were identified, nor were there any included studies where the baseline asthma severity had to be implied from the baseline characteristics. Excluding the open‐label studies (Novel START and PRACTICAL, judged at high risk of bias due to lack of blinding) did not alter the direction of effect in any of the primary outcomes. Using a fixed‐effect model as opposed to a random‐effects one made no meaningful difference to the point estimates of the primary outcomes.
Discussion
Summary of main results
Of the six studies which met our inclusion criteria, four (Novel START, PRACTICAL, SYGMA 1 and SYGMA 2) dominated the results of the meta‐analyses. These were large randomised controlled trials from the same research group and included 9565 participants in total. Two studies (SYGMA 1 and SYGMA 2) included children aged 12 and over as well as adults. Two studies were open‐label (Novel START and PRACTICAL) and judged as high risk of bias in this domain, but all studies were otherwise of low risk of bias in other domains. In all four of these trials the fixed‐dose combination as‐required fast‐acting beta₂‐agonist/inhaled corticosteroids (FABA/ICS) was budesonide 200 μg and formoterol 6 μg in a dry powder formulation. Haahtela 2006 is a smaller study with 93 participants, conducted by a different research group. It also used budesonide/formoterol as the combination inhaler, again as dry powder formulation.
When compared with as‐required short‐acting beta2‐agonists (SABA) alone, as‐required fixed‐dose combination inhalers significantly reduced the number of asthma exacerbations requiring systemic steroids (odds ratio (OR) 0.45, 95% confidence interval (CI) 0.34 to 0.60, Analysis 1.1), and reduced the annual exacerbation rate (rate ratio 0.41, 95% CI 0.30 to 0.55, Analysis 1.2), and the odds of an asthma‐related hospital admission or emergency department or urgent care visit (OR 0.35, 95% CI 0.20 to 0.60, Analysis 1.3). The reduction in exacerbations requiring systemic steroid is based on high‐certainty evidence from two clinical trials including 2997 participants. The certainty of the other outcomes is lower, particularly as they are based on relatively few events.
Compared with SABA alone, any changes in asthma control or spirometry, though favouring as required FABA/ICS, were small and less than the minimal clinically‐important differences. We did not find evidence of differences in asthma‐associated quality of life, total systemic corticosteroid dose or mortality. For other secondary outcomes as‐required FABA/ICS was associated with significant reductions in FeNO, a marker of exacerbation risk (Petsky 2016), by ‐11 to ‐15.5 ppb and of the odds of an adverse event (OR 0.82, 95% CI 0.71 to 0.95, Analysis 1.9), and with an increase in the daily inhaled steroid dose (mean difference (MD) 76.50 μg beclomethasone equivalent per day, 95% CI 69.40 to 83.60, Analysis 1.10).
When compared with regular maintenance use of inhaled corticosteroids, as‐required fixed‐dose combination inhalers did not lead to a significant difference in the odds ratio (OR 0.79, 95% CI 0.59 to 1.07, Analysis 2.1) or annual rate (rate ratio 0.90, 95% CIs 0.76 to 1.06, Analysis 2.2) of severe asthma exacerbations requiring systemic steroids, but did reduce the odds of an asthma‐related hospital admission or emergency department or urgent care visit (OR 0.63, 95% CI 0.44 to 0.91, Analysis 2.3). We have relatively low certainty in the precision of these estimates.
Compared with regular maintenance use of inhaled corticosteroids, any changes in asthma control, spirometry, peak flow rates, or asthma‐associated quality of life, though favouring regular ICS, were small and less than the minimal clinically‐important differences. As this review was limited to mild asthma, study participants generally had good asthma control and normal lung function and so it is not surprising that we found no major between intervention effects. We found evidence that adverse events, serious adverse events, total systemic corticosteroid dose and mortality were similar between groups, although deaths were rare, so confidence intervals for this analysis were wide. We found moderate‐certainty evidence from four trials involving 7180 participants that as‐required FABA/ICS was associated with less average daily exposure to inhaled corticosteroids than those on regular ICS (MD ‐154.51 μg/day, 95% CI ‐207.94 to ‐101.09, Analysis 2.10).
Overall completeness and applicability of evidence
We believe these studies are representative of adults with mild asthma in the real world, with broad inclusion criteria, with only two of the studies that contributed data requiring reversibility as an inclusion criterion, the others depending on self‐report of physician‐diagnosed asthma. Participants had mean age 36 to 43 years, a mild deficit in baseline lung function (pre‐bronchodilator FEV1 84% to 90%) and including current smokers (2.3% to 11% of participants), and those with a range of preceding annual exacerbation rates (5.5% to 22%). These results are therefore likely to be generalisable to populations with mild asthma in primary care.
Whilst numbers of exacerbations, annual severe exacerbation rates and severe adverse events were reported consistently between studies, other outcome measures including symptom scores, FeNO and lung function were not, and none of the included studies reported on quality of life outcomes. As we were unable to obtain single‐patient data we were unable to include a large randomised controlled trial (RCT) (Papi 2007), which included participants with a mixture of mild and moderate asthma. We also identified an unpublished trial presented only in a conference abstract, although this trial was small so unlikely to influence significantly the findings of the meta‐analyses.
There are a number of different preparations of fixed‐dose FABA/ICS, including pressurised meter dose inhaler formulations, but our search identified studies which used dry powder formulations of budesonide and formoterol only. The majority of studies which contributed data are produced by a single group of investigators, albeit as part of a multinational collaboration, and three of these are funded by a single pharmaceutical company.
Quality of the evidence
Using the GRADE system, we judged the certainty of the evidence per outcome for main comparisons – those related to rates of exacerbations – to be low (with the exception of exacerbations requiring systemic steroid in the as‐required FABA/ICS versus as‐required FABA comparison). This judgement may be a little harsh, as the results are based solely on relevant, well‐designed randomised clinical trials. Of the five trials that contributed data, two were open‐label, which has the potential to introduce biases in participant behaviour, such as seeking urgent care, and treatment outcomes such as reducing the threshold for prescribing systemic steroids, or affecting the reporting of adverse events. However, the methodological quality was otherwise good for the included trials, they were conducted in applicable populations, examining outcomes of direct relevance to participants, with low‐moderate heterogeneity across studies, and with consistent findings between studies, including between blinded and unblinded studies. It is unlikely that lack of blinding would be sufficient to explain the large magnitude of the observed differences on exacerbation rates between as‐required FABA/ICS and FABA alone. This is particularly so as the effect size observed was larger for reduction in exacerbations requiring hospital admission or urgent care visit, than for exacerbations requiring systemic corticosteroids, both in comparisons with SABA alone and in comparisons with maintenance steroids. Blinding would be unlikely to have a sizeable effect on other markers of lung function, though knowledge of treatment allocation is likely to affect symptom scores, which could be rated higher in those aware they are not receiving combination therapies.
Several of the outcomes, particularly in comparisons against as‐required SABA alone, were based on only one or two studies. Given the large trial sizes, good methodological quality and large effect size, we have a high degree of confidence in the benefits of as‐required FABA/ICS in reducing exacerbations compared with SABA alone, and in the evidence suggesting no difference between as‐required FABA/ICS and maintenance ICS in rates of exacerbations or adverse events. We have less confidence in comparative effects of as‐required FABA/ICS and SABA alone on FeNO or Asthma Control Questionnaire (ACQ‐5) as these are dependent on a single open‐label RCT. Due to the small number of included studies, a funnel plot was not feasible as a formal assessment of publication bias. However, our search strategy was comprehensive and rigorous, and our searches included conference abstracts and ongoing trials to find unpublished studies.
Potential biases in the review process
Our review adhered closely to the published protocol (Crossingham 2020). We were unable to identify data on quality of life or meta‐analyse lung function due to differences in data presentation between studies, and for the same reason we could analyse only severe adverse events rather than all adverse events for the comparison of as required FABA/ICS with regular ICS.
There remains the possibility that we may have failed to identify unpublished trials contributing positive or negative results, although we have searched available trial registries, and most relevant trials will have been conducted since the introduction of mandatory trial registration. We are aware of the potential for publication bias. We identified six trials meeting our prespecified inclusion criteria through comprehensive, systematic database searches, and all identified studies were reviewed independently by two review authors to minimise study selection bias or errors.
Agreements and disagreements with other studies or reviews
Our findings are in broad agreement with one previous meta‐analysis (Hatter 2021), which was conducted by the authors of the Novel START and PRACTICAL studies. The authors assessed their open‐label trials as of lower risk of bias than did our assessments, and their meta‐analysis considered only the comparison of as‐required FABA/ICS with regular ICS, and not the comparison against SABA alone. Both meta‐analyses found similar results, and similar magnitudes of effects for a range of outcomes including reduction in inhaled steroid dose and a slight increase in ACQ‐5, which was less than the: minimum clinically important difference (MCID), and no evidence of differences in rates of severe adverse events and mortality.
Both meta‐analyses found some evidence of a reduction in urgent care visits associated with as‐required FABA/ICS, though, due to differences in methodology and the statistical analysis selected, the two meta‐analyses differed in the detail. The current meta‐analysis found fewer exacerbations requiring hospital admission or urgent care visit with as‐required FABA/ICS compared with maintenance ICS, whilst Hatter 2021, using Peto Odds Ratios, reported no difference in this outcome or in hospitalisation rates. However the upper limits of their confidence intervals were close to unity and their findings would be compatible with significant decrease in these outcomes. Moreover Hatter 2021 reported a significant reduction in emergency department visits with as‐required FABA/ICS (Peto OR 0.65, 95%CI 0.43 to 0.98), consistent with evidence of a reduction in urgent care visits.
In the current review, we did not find evidence of a reduction in the odds or annual rates of asthma exacerbations requiring systemic steroids with as‐required FABA/ICS compared with maintenance ICS. By contrast, the Hatter 2021 study reported moderate evidence that as‐required FABA/ICS was associated with a prolonged time to first severe exacerbation, with a confidence interval including the possibility of no effect, for a prolonged time to first severe exacerbation with as‐required FABA/ICS (hazard ratio (HR) 0.85, 95%CI 0.73 to 1.00, P = 0.048). They report similar reductions in the rate ratios of severe exacerbations and of the risk of at least one exacerbation, though again the statistical significance of these findings is borderline (P = 0.044 and P = 0.064, respectively, with confidence intervals including the possibility of no effect) and so there is low certainty in these findings.
Our findings are also in accord with data from a 2007 double‐blind RCT which showed beclomethasone‐salbutamol 250/100 μg in a single inhaler, administered as‐required, was as effective as regular use of inhaled beclomethasone 250 μg twice daily and more effective than as‐required salbutamol alone in preventing exacerbations and improving morning peak expiratory flow rate (PEFR) (Papi 2007). We judged this study to be at low risk of bias, but it was excluded from the meta‐analysis because the population studied included a proportion with moderate asthma, with 31.6% receiving regular ICS, with a mean dose of 460 μg/day, and we were unable to obtain individual patient data to determine the effects in the subgroup with mild asthma alone.
Authors' conclusions
Implications for practice.
This review has provided moderate‐to‐high certainty evidence that as‐required use of fast‐acting beta₂‐agonist/inhaled corticosteroids (FABA/ICS) in a fixed‐dose combination inhaler is clinically effective in adults and adolescents with mild asthma. The use of FABA/ICS instead of as‐required short‐acting beta2‐agonists (SABA) alone would be expected to reduce important patient‐relevant outcomes including use of systemic corticosteroids, rates of exacerbations and of hospital admissions or unscheduled healthcare visits, and may reduce adverse events. As exacerbations are responsible for the majority of morbidity, mortality and the economic costs of asthma, this would support recent changes in international guidelines (GINA 2019) away from the use of SABA‐alone in mild asthma.
Furthermore, use of as‐required FABA/ICS is as effective as regular use of ICS, and is associated with a reduction of asthma‐related hospital admissions or unscheduled healthcare visits, whilst reducing the average daily exposure to ICS, without any evidence of an increase in adverse events. As mild asthma is heterogeneous, with eosinophilic airway inflammation – linked to the greatest benefit from ICS – present in only one quarter of individuals (Lazarus 2019), these dual benefits are likely to be achieved by a symptom‐driven therapy reducing intentional and unintentional use of SABA in monotherapy in these individuals.
These findings support as‐required use of FABA/ICS in a fixed‐dose combination inhaler as superior to SABA‐alone, and as a therapeutic alternative to maintenance ICS in mild asthma. All the data are derived from studies of dry powder formulations and may not necessarily apply to pressurised meter dose inhalers. The implementation of these findings may depend on differing health economic assessments, differing healthcare infrastructures, and population‐specific factors in different settings globally. The findings of this meta‐analysis are only relevant to adults and adolescents aged 12 years or above.
Implications for research.
In all five trials in the meta analyses fixed‐dose combination as‐required FABA/ICS was budesonide 200 μg and formoterol 6 μg in a dry powder formulation. There would be value in further trials which assessed other fixed‐dose combinations including formulations with pressurised meter dose inhalers, ultra‐fine particle preparations, and other ICS such as beclomethasone or other FABAs such as salbutamol (albuterol).
Although our protocol allowed inclusion of children aged SIX years and older, we did not identify trials which included children under 12 years of age. The utility of as‐required FABA/ICS remains to be assessed in this age group (and hopefully will be in the one study, yet to commence recruitment, ACTRN12620001091998 2020).
Outcome data from as‐required FABA/ICS are not available beyond 52‐week trials. Asthma is associated with accelerated decline in lung function over the life course (Lange 1998), which may in part be related to recurrent episodes of bronchospasm (Grainge 2011), and may be fastest in early disease (Ulrik 1994), whilst there is evidence that regular ICS may provide protection against this decline (Domingo 2019; Haahtela 1994). Therefore, it will be important to assess long‐term outcomes in prospective long‐term cohort studies to determine whether there are differences between as‐required FABA/ICS and regular maintenance ICS, particularly in measures of lung function.
Whilst asthma is responsible for an estimated 400,000 deaths per year globally (GBD Study 2017), of which the majority occur in mild or moderate asthma (RCP 2014), analysis of very large observational datasets will be required to determine whether as‐required FABA/ICS use is associated with a reduction in asthma‐related mortality. FABA/ICS are regularly unaffordable in low‐ and middle‐income countries. These studies were conducted in > 25 countries across six continents, though populations in Africa and the Indian Subcontinent were under represented and should be addressed in future studies using a more inclusive global health approach.
Our review did not include health economic assessments, which will be of value to guide implementation of these findings in different healthcare settings globally. Application of findings will also be affected by other local factors including geography, access to health care, and differing healthcare beliefs within each population, thus further research will be required within each potential healthcare setting.
What's new
| Date | Event | Description |
|---|---|---|
| 4 May 2021 | Amended | We updated the legend for figure 6. |
History
Protocol first published: Issue 1, 2020 Review first published: Issue 5, 2021
Acknowledgements
The authors would like to thank the Cochrane Airways Editorial team, particularly Rebecca Fortescue, Emma Dennett and Emma Jackson for their help defining the clinical question and methods and Liz Stovold for the search strategy. We are grateful to Adnan Chaudhry, Gareth Hynes and Hannah Bruguier for contributions to screening abstracts and data extraction.
The authors and Airways' Editorial Team are grateful to the following peer‐ and patient‐reviewers for their time and comments: Kevin Mortimer (UK), Refiloe Masekala (South Africa), Hebatullah Abdulazeem (Germany), Chen‐Yuan Chiang (France), Amnuayporn Apiraksakorn (Thailand) and Sarah Hodgkinson (UK).
The Background and Methods sections of this review were based on a standard template used by Cochrane Airways.
This project is funded by the National Institute for Health Research (NIHR) [NIHR Incentive Awards 2019 (NIHR130687)]. The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
This project was supported by the National Institute for Health Research (NIHR), via Cochrane Infrastructure funding to the Cochrane Airways Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the NIHR or the Department of Health and Social Care.
Appendices
Appendix 1. Database search strategies
| Database/search date | Search strategy | Results retrieved |
|
Airways Register (via Cochrane Register of Studies) Date of most recent search: 19 March 2021 |
1 AST:MISC1 AND INSEGMENT 2 MeSH DESCRIPTOR Asthma Explode All AND INSEGMENT 3 asthma*:ti,ab AND INSEGMENT 4 #1 or #2 or #3 AND INSEGMENT 5 MESH DESCRIPTOR Fluticasone AND INSEGMENT 6 MESH DESCRIPTOR Budesonide AND INSEGMENT 7 MESH DESCRIPTOR Beclomethasone AND INSEGMENT 8 MESH DESCRIPTOR Triamcinolone EXPLODE ALL AND INSEGMENT 9 fluticasone AND INSEGMENT 10 budesonide AND INSEGMENT 11 triamcinolone AND INSEGMENT 12 flunisolide AND INSEGMENT 13 ciclesonide AND INSEGMENT 14 flixotide or flovent AND INSEGMENT 15 becotide or beclofort or becodisk or QVAR or vanceril AND INSEGMENT 16 pulmicort AND INSEGMENT 17 kenalog or azmacort AND INSEGMENT 18 bronalide AND INSEGMENT 19 Alvesco AND INSEGMENT 20 MESH DESCRIPTOR Mometasone Furoate AND INSEGMENT 21 mometasone AND INSEGMENT 22 (inhal* NEAR3 (steroid* or corticosteroid* or glucocorticoid*)) AND INSEGMENT 23 #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 24 MESH DESCRIPTOR Adrenergic beta‐2 Receptor Agonists EXPLODE ALL AND INSEGMENT 25 MESH DESCRIPTOR Albuterol EXPLODE ALL AND INSEGMENT 26 MESH DESCRIPTOR Terbutaline AND INSEGMENT 27 MESH DESCRIPTOR Formoterol Fumarate AND INSEGMENT 28 MESH DESCRIPTOR Salmeterol Xinafoate AND INSEGMENT 29 Salbutamol or albuterol AND INSEGMENT 30 Terbutaline AND INSEGMENT 31 Bambuterol AND INSEGMENT 32 formoterol or eformoterol AND INSEGMENT 33 Indacaterol AND INSEGMENT 34 Olodaterol AND INSEGMENT 35 salmeterol AND INSEGMENT 36 #24 OR #25 OR #26 OR #28 OR #27 OR #29 OR #30 OR #31 OR #32 OR #33 OR #34 OR #35 37 MESH DESCRIPTOR Fluticasone‐Salmeterol Drug Combination AND INSEGMENT 38 MESH DESCRIPTOR Budesonide, Formoterol Fumarate Drug Combination AND INSEGMENT 39 MESH DESCRIPTOR Mometasone Furoate, Formoterol Fumarate Drug Combination AND INSEGMENT 40 Fostair AND INSEGMENT 41 Symbicort AND INSEGMENT 42 DuoResp Spiromax AND INSEGMENT 43 Fobumix AND INSEGMENT 44 Seretide AND INSEGMENT 45 Relvar AND INSEGMENT 46 Ventide AND INSEGMENT 47 Aerocort AND INSEGMENT 48 Salbair AND INSEGMENT 49 #48 OR #47 OR #46 OR #45 OR #44 OR #43 OR #42 OR #41 OR #39 OR #40 OR #38 OR #37 50 #23 AND #36 51 #4 AND (#49 or #50) 52 INREGISTER 53 #51 AND #52 |
|
|
CENTRAL (via Cochrane Register of Studies) Date of most recent search: 19 March 2021 |
1 AST:MISC1 AND CENTRAL:TARGET 2 MeSH DESCRIPTOR Asthma Explode All AND CENTRAL:TARGET 3 asthma*:ti,ab AND CENTRAL:TARGET 4 #1 or #2 or #3 AND CENTRAL:TARGET 5 MESH DESCRIPTOR Fluticasone AND CENTRAL:TARGET 6 MESH DESCRIPTOR Budesonide AND CENTRAL:TARGET 7 MESH DESCRIPTOR Beclomethasone AND CENTRAL:TARGET 8 MESH DESCRIPTOR Triamcinolone EXPLODE ALL AND CENTRAL:TARGET 9 fluticasone AND CENTRAL:TARGET 10 budesonide AND CENTRAL:TARGET 11 triamcinolone AND CENTRAL:TARGET 12 flunisolide AND CENTRAL:TARGET 13 ciclesonide AND CENTRAL:TARGET 14 flixotide or flovent AND CENTRAL:TARGET 15 becotide or beclofort or becodisk or QVAR or vanceril AND CENTRAL:TARGET 16 pulmicort AND CENTRAL:TARGET 17 kenalog or azmacort AND CENTRAL:TARGET 18 bronalide AND CENTRAL:TARGET 19 Alvesco AND CENTRAL:TARGET 20 MESH DESCRIPTOR Mometasone Furoate AND CENTRAL:TARGET 21 mometasone AND CENTRAL:TARGET 22 (inhal* NEAR3 (steroid* or corticosteroid* or glucocorticoid*)) AND CENTRAL:TARGET 23 #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 AND CENTRAL:TARGET 24 MESH DESCRIPTOR Adrenergic beta‐2 Receptor Agonists EXPLODE ALL AND CENTRAL:TARGET 25 MESH DESCRIPTOR Albuterol EXPLODE ALL AND CENTRAL:TARGET 26 MESH DESCRIPTOR Terbutaline AND CENTRAL:TARGET 27 MESH DESCRIPTOR Formoterol Fumarate AND CENTRAL:TARGET 28 MESH DESCRIPTOR Salmeterol Xinafoate AND CENTRAL:TARGET 29 Salbutamol or albuterol AND CENTRAL:TARGET 30 Terbutaline AND CENTRAL:TARGET 31 Bambuterol AND CENTRAL:TARGET 32 formoterol or eformoterol AND CENTRAL:TARGET 33 Indacaterol AND CENTRAL:TARGET 34 Olodaterol AND CENTRAL:TARGET 35 salmeterol AND CENTRAL:TARGET 36 #24 OR #25 OR #26 OR #28 OR #27 OR #29 OR #30 OR #31 OR #32 OR #33 OR #34 OR #35 AND CENTRAL:TARGET 37 MESH DESCRIPTOR Fluticasone‐Salmeterol Drug Combination AND CENTRAL:TARGET 38 MESH DESCRIPTOR Budesonide, Formoterol Fumarate Drug Combination AND CENTRAL:TARGET 39 MESH DESCRIPTOR Mometasone Furoate, Formoterol Fumarate Drug Combination AND CENTRAL:TARGET 40 Fostair AND CENTRAL:TARGET 41 Symbicort AND CENTRAL:TARGET 42 DuoResp Spiromax AND CENTRAL:TARGET 43 Fobumix AND CENTRAL:TARGET 44 Seretide AND CENTRAL:TARGET 45 Relvar AND CENTRAL:TARGET 46 Ventide AND CENTRAL:TARGET 47 Aerocort AND CENTRAL:TARGET 48 Salbair AND CENTRAL:TARGET 49 #48 OR #47 OR #46 OR #45 OR #44 OR #43 OR #42 OR #41 OR #39 OR #40 OR #38 OR #37 AND CENTRAL:TARGET 50 #23 AND #36 AND CENTRAL:TARGET 51 #4 AND (#49 or #50) AND CENTRAL:TARGET |
|
|
MEDLINE (Ovid) ALL Date of most recent search: 19 March 2021 |
1 exp Asthma/ 2 asthma$.ti,ab. 3 1 or 2 4 Fluticasone/ 5 Budesonide/ 6 Beclomethasone/ 7 exp Triamcinolone/ 8 fluticasone.tw. 9 beclomethasone.tw. 10 budesonide.tw. 11 triamcinolone.tw. 12 flunisolide.tw. 13 ciclesonide.tw. 14 (flixotide or flovent).tw. 15 (becotide or beclofort or becodisk or QVAR or vanceril).tw. 16 pulmicort.tw. 17 (kenalog or azmacort).tw. 18 bronalide.tw. 19 Alvesco.tw. 20 Mometasone Furoate/ 21 mometasone.tw. 22 (inhal$ adj3 (steroid$ or corticosteroid$ or glucocorticoid$)).tw. 23 or/4‐22 24 exp Adrenergic beta‐2 Receptor Agonists/ 25 exp Albuterol/ 26 Terbutaline/ 27 Formoterol Fumarate/ 28 Salmeterol Xinafoate/ 29 (Salbutamol or albuterol).tw. 30 Terbutaline.tw. 31 Bambuterol.tw. 32 (formoterol or eformoterol).tw. 33 Indacaterol.tw. 34 Olodaterol.tw. 35 salmeterol.tw. 36 or/24‐35 37 Fluticasone‐Salmeterol Drug Combination/ 38 Budesonide, Formoterol Fumarate Drug Combination/ 39 Mometasone Furoate, Formoterol Fumarate Drug Combination/ 40 Fostair.tw. 41 Symbicort.tw. 42 DuoResp Spiromax.tw. 43 Fobumix.tw. 44 Seretide.tw. 45 Relvar.tw. 46 Ventide.tw. 47 Aerocort.tw. 48 Salbair.tw. 49 or/37‐48 50 23 and 36 51 3 and (49 or 50) 52 (controlled clinical trial or randomized controlled trial).pt. 53 (randomized or randomised).ab,ti. 54 placebo.ab,ti. 55 dt.fs. 56 randomly.ab,ti. 57 trial.ab,ti. 58 groups.ab,ti. 59 or/52‐58 60 Animals/ 61 Humans/ 62 60 not (60 and 61) 63 59 not 62 64 51 and 63 |
|
|
Embase (Ovid) Date of most recent search: 19 March 2021 |
1 exp asthma/ 2 asthma$.ti,ab. 3 1 or 2 4 fluticasone/ or fluticasone furoate/ 5 budesonide/ 6 beclometasone/ 7 triamcinolone/ 8 fluticasone.tw. 9 beclomethasone.tw. 10 budesonide.tw. 11 triamcinolone.tw. 12 flunisolide.tw. 13 ciclesonide.tw. 14 (flixotide or flovent).tw. 15 (becotide or beclofort or becodisk or QVAR or vanceril).tw. 16 pulmicort.tw. 17 (kenalog or azmacort).tw. 18 bronalide.tw. 19 Alvesco.tw. 20 mometasone furoate/ 21 mometasone.tw. 22 (inhal$ adj3 (steroid$ or corticosteroid$ or glucocorticoid$)).tw. 23 or/4‐22 24 exp beta 2 adrenergic receptor stimulating agent/ 25 (Salbutamol or albuterol).tw. 26 Terbutaline.tw. 27 Bambuterol.tw. 28 (formoterol or eformoterol).tw. 29 Indacaterol.tw. 30 Olodaterol.tw. 31 salmeterol.tw. 32 or/24‐31 33 budesonide plus formoterol/ 34 formoterol fumarate plus mometasone furoate/ 35 exp fluticasone propionate plus salmeterol/ 36 Fostair.tw. 37 Symbicort.tw. 38 DuoResp Spiromax.tw. 39 Fobumix.tw. 40 Seretide.tw. 41 Relvar.tw. 42 Ventide.tw. 43 Aerocort.tw. 44 Salbair.tw. 45 or/33‐44 46 23 and 32 47 3 and (45 or 46) 48 Randomized Controlled Trial/ 49 randomization/ 50 controlled clinical trial/ 51 Double Blind Procedure/ 52 Single Blind Procedure/ 53 Crossover Procedure/ 54 (clinica$ adj3 trial$).tw. 55 ((singl$ or doubl$ or trebl$ or tripl$) adj3 (mask$ or blind$ or method$)).tw. 56 exp Placebo/ 57 placebo$.ti,ab. 58 random$.ti,ab. 59 ((control$ or prospectiv$) adj3 (trial$ or method$ or stud$)).tw. 60 (crossover$ or cross‐over$).ti,ab. 61 or/48‐60 62 exp animals/ or exp invertebrate/ or animal experiment/ or animal model/ or animal tissue/ or animal cell/ or nonhuman/ 63 human/ or normal human/ or human cell/ 64 62 and 63 65 62 not 64 66 61 not 65 67 47 and 66 |
|
|
ClinicalTrials.gov Date of most recent search: 19 March 2021 |
Study type: Interventional Condition: asthma Intervention: Fixed dose OR combination inhaler |
|
|
WHO trials portal Date of most recent search: 19 March 2021 |
Condition: asthma Intervention: Fixed dose OR combination inhaler |
|
Data and analyses
Comparison 1. As required fixed dose combination inhaler versus as required short acting beta agonist.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Asthma exacerbations requiring systemic steroid | 2 | 2997 | Odds Ratio (M‐H, Random, 95% CI) | 0.45 [0.34, 0.60] |
| 1.2 Annual exacerbation rate | 2 | 2997 | Exacerbation rate (IV, Random, 95% CI) | 0.41 [0.30, 0.55] |
| 1.3 Exacerbations requiring hospital admission or emergency department / urgent care visit | 2 | 2997 | Odds Ratio (M‐H, Random, 95% CI) | 0.35 [0.20, 0.60] |
| 1.4 ACQ‐5 | 2 | 2859 | Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.20, ‐0.10] |
| 1.5 FEV1 change from baseline | 2 | 2596 | Mean Difference (IV, Random, 95% CI) | 64.03 [27.49, 100.57] |
| 1.6 FeNO [ppb] | 1 | Geometric mean (IV, Random, 95% CI) | Totals not selected | |
| 1.7 FeNO change from baseline | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.8 Serious adverse events | 3 | 3095 | Odds Ratio (M‐H, Random, 95% CI) | 1.31 [0.50, 3.46] |
| 1.9 All adverse events | 2 | 3002 | Odds Ratio (M‐H, Random, 95% CI) | 0.82 [0.71, 0.95] |
| 1.10 Daily inhaled steroid dose | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.11 Total systemic corticosteroid dose | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.12 Mortality | 3 | 3089 | Odds Ratio (M‐H, Random, 95% CI) | 3.07 [0.12, 75.71] |
Comparison 2. Fixed dose combination inhaler as required versus regular inhaled steroid plus as required short acting beta agonist.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Number of exacerbations requiring systemic steroid | 4 | 8065 | Odds Ratio (M‐H, Random, 95% CI) | 0.79 [0.59, 1.07] |
| 2.2 Annual severe exacerbation rate | 4 | 8065 | Exacerbation rate ratio (IV, Random, 95% CI) | 0.90 [0.76, 1.06] |
| 2.3 Exacerbations requiring hospital admission or emergency department / urgent care visit | 4 | 8065 | Odds Ratio (M‐H, Random, 95% CI) | 0.63 [0.44, 0.91] |
| 2.4 ACQ‐5 | 4 | 7382 | Mean Difference (IV, Random, 95% CI) | 0.12 [0.09, 0.15] |
| 2.5 FEV1 | 2 | 1199 | Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.11, 0.09] |
| 2.6 FEV1 change from baseline | 2 | 6287 | Mean Difference (IV, Random, 95% CI) | ‐37.68 [‐68.19, ‐7.17] |
| 2.7 FeNO [ppb] | 2 | 1197 | Geometric mean (IV, Random, 95% CI) | 1.13 [1.06, 1.20] |
| 2.8 Serious adverse events | 4 | 8072 | Odds Ratio (IV, Random, 95% CI) | 1.14 [0.82, 1.57] |
| 2.9 All adverse events | 4 | 8072 | Odds Ratio (M‐H, Random, 95% CI) | 0.96 [0.82, 1.14] |
| 2.10 Daily inhaled steroid dose | 4 | 7180 | Mean Difference (IV, Random, 95% CI) | ‐154.51 [‐207.94, ‐101.09] |
| 2.11 Total systemic corticosteroid dose | 2 | 1330 | Mean Difference (IV, Random, 95% CI) | ‐7.00 [‐13.97, ‐0.03] |
| 2.12 Mortality | 4 | 8070 | Odds Ratio (M‐H, Random, 95% CI) | 0.63 [0.12, 3.25] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Haahtela 2006.
| Study characteristics | ||
| Methods | Double‐blind parallel group randomised controlled trial | |
| Participants | 93 current non smoking adults using only as required beta agonists for asthma. Mean age was 37 years and 70% were female. Mean pre bronchodilator FEV1 was 99.5% ‐ 102.4% of predicted. | |
| Interventions | Budesonide / formoterol 160 μg/4.5 μg as required versus formoterol 4.5 μg as required (delivered doses) | |
| Outcomes | Change in FeNO, asthma symptom scores, asthma free days, morning and evening PEFR, number of inhalations of study drug, FEV1 | |
| Notes | Outcomes reported as baseline and on treatment, combining different time points | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Separate randomisation at each study centre using balanced blocks generated by a computer programme |
| Allocation concealment (selection bias) | Low risk | Not specifically described, but likely done |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, identical devices |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind, identical devices |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Double‐blind, identical devices |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Reasons for withdrawal not stated |
| Selective reporting (reporting bias) | Unclear risk | No published protocol identified |
Novel START.
| Study characteristics | ||
| Methods | Randomised, open‐label, parallel trial | |
| Participants | Adults (18‐75 years old) with self‐reported diagnosis of asthma. Short‐acting beta‐agonist use in the last four weeks but not using inhaled or oral steroid or other asthma medication (e.g. leukotriene receptor antagonist, theophylline). Average age was between 34.9 to 36 years across the three intervention groups with 50.7% to 57.3% female. 8.2% to 10.8% were current smokers. On treatment FEV1 was around 90% on average. 91% ‐ 94.5% had had no severe exacerbations in the preceding 12 months. | |
| Interventions | As required budesonide‐formoterol (200 μg/6 μg) 1 puff via a turbohaler versus salbutamol 100 μg 2 puffs as required via metered dose inhaler versus budesonide 200 μg (turbohaler) one puff twice day plus as required salbutamol 100 μg 2 puffs via metered dose inhaler. | |
| Outcomes | Annualised asthma exacerbation rate, number of exacerbations, time to first exacerbation, withdrawals for treatment failure, ACQ‐5, FEV1, FeNO, daily budesonide dose, oral prednisolone use, number of beta agonist actuations per day, adverse events | |
| Notes | Funded by AstraZeneca and the Health Research Council of New Zealand | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised with computer‐generated sequence, stratified to country |
| Allocation concealment (selection bias) | Low risk | Electronic clinical record system concealed treatment assignments at the time of randomisation |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open‐label |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Open‐label, however blinding of study statistician. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 98.9% follow‐up |
| Selective reporting (reporting bias) | Low risk | All protocol outcomes reported |
PRACTICAL.
| Study characteristics | ||
| Methods | Open‐label, parallel group, multicentre, randomised controlled trial | |
| Participants | Adults (18‐75 years) with self‐reported doctor's diagnosis of asthma with either no or low‐dose inhaled steroid in the past 12 weeks. Mean age was 43 years. 5% ‐ 9% were current smokers with more current smokers in the as require FABA/ICS arm. 55% were female. FEV1 was 87% predicted. 88% had not had a severe asthma exacerbation in the previous 12 months. | |
| Interventions | Budesonide‐formoterol (200 μg/6 μg) as required versus budesonide 200 μg twice daily plus as required terbutaline 250 μg. | |
| Outcomes | Annualised number of severe asthma exacerbations per patient, time to first severe exacerbation, ACQ‐5, FEV1, FeNO, mean daily inhaled steroid dose, proportion of participants with at least one day of no inhaled steroid use, longest duration of no steroid use, systemic steroid exposure, days of high beta agonist use | |
| Notes | Funded by the Health Research Council of New Zealand | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated block randomisation |
| Allocation concealment (selection bias) | Low risk | Central system to ensure allocation concealment |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open‐label |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Open‐label |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Perhaps slightly higher loss to follow up in maintenance treatment arm but no major concerns. |
| Selective reporting (reporting bias) | Low risk | Good adherence with published protocol |
SYGMA 1.
| Study characteristics | ||
| Methods | Double‐blind, parallel, randomised controlled trial | |
| Participants | 12 years old or over from 18 countries worldwide with a least a six‐month history of asthma on GINA step 2 treatment. Average age was 39.6 years and 61.1% were female. Pre bronchodilator FEV1 was 84% predicted on average and 80.3% had had no severe asthma exacerbation in the previous 12 months. | |
| Interventions | Budesonide‐formoterol 200 μg/6 μg as required plus twice daily placebo versus terbutaline 500 μg as required plus twice daily placebo versus budesonide 200 μg twice daily plus terbutaline 500 μg as required | |
| Outcomes | Electronically recorded weeks with well‐controlled asthma, moderate and severe exacerbation rates, ACQ5, AQL, mean ICS score, time to additional steroid for asthma, asthma‐related discontinuations, adverse events, deaths, change in FEV1 and peak flow, night time awakenings, asthma control days, as required drug‐free days, high as required drug use. | |
| Notes | Funded by AstraZeneca | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised randomisation system |
| Allocation concealment (selection bias) | Low risk | Centralised system to ensure allocation concealment |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Multiple measures to ensure blinding |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Multiple measures to ensure blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Multiple measures to ensure blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 10% loss to follow‐up, balanced across groups |
| Selective reporting (reporting bias) | Low risk | Analysis matches pre published protocol |
SYGMA 2.
| Study characteristics | ||
| Methods | Double‐blind, randomised, parallel group controlled trial | |
| Participants | Adults and children 12 years and over with at least six month history of asthma, needing GINA step 1 or 2. Mean age was 41 years and 2.5% were current smokers. 62% were female. Mean pre bronchodilator FEV1 was 84% predicted. 78% had had no severe asthma exacerbations in the prior 12 months. | |
| Interventions | Budesonide/formoterol 200 μg / 6 μg turbohaler as required (with twice daily placebo) versus budesonide 200 μg twice per day plus terbutaline 500 μg as required. | |
| Outcomes | Annual severe asthma exacerbation rate, time to first severe exacerbation, asthma related discontinuation, change from baseline FEV1, as needed drug use, ACQ‐5, AQLQ(S), percentage of controller use days. | |
| Notes | Funded by AstraZeneca | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation codes |
| Allocation concealment (selection bias) | Low risk | Multiple allocation concealment measures |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Multiple measures to preserve blinding |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Multiple measures to preserve blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Multiple measures to preserve blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 9% loss to follow up, appears balanced across groups |
| Selective reporting (reporting bias) | Low risk | Final report matches published protocol |
Tanaka 2017.
| Study characteristics | ||
| Methods | Open‐label cross‐over trial | |
| Participants | Adults (22‐77 years) probably from a single secondary care centre (Japan), asthma for at least 3 months on GINA step 1‐2 | |
| Interventions | Budesonide 320 μg/formoterol 9 μg as required versus 160 μg budesonide daily | |
| Outcomes | ACT, ACQ5, FeNO, FEV1, FVC, blood eosinophils | |
| Notes | Single conference abstract only. No other reports identified and the authors have not responded to requests for information. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make any other judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make any other judgement |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open‐label |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Open‐label |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 18% dropout. At least one discontinuation due to exacerbation therefore likely non randomly related to allocation. |
| Selective reporting (reporting bias) | High risk | No protocol. Limited description of results. |
ACQ: Asthma Control Questionnaire; FABA: fast‐acting beta₂‐agonist; GINA: Global Initiative for Asthma; ICS: inhaled corticosteroid; PEFR: peak expiratory flow rate.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aalbers 2003 | Participants with moderate or severe asthma |
| Aalbers 2004 | Regular daily use of beta agonist /inhaled steroid |
| Aalbers 2005 | Regular daily use of beta agonist /inhaled steroid |
| Agarwal 2010 | Wrong population ‐ acute asthma |
| Aggarwal 2003 | Wrong drug ‐ not rapid acting beta agonist |
| Aldrey 1995 | Not as‐required inhaled steroid |
| Aldridge 2000 | Not as‐required inhaled steroid/beta agonist |
| Aldridge 2002 | Intervention lasted less than 12 weeks |
| Ankerst 2000 | Regular daily use of beta agonis/inhaled steroid |
| Ankerst 2001 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| Ankerst 2002 | Wrong intervention ‐ does not include a beta agonist inhaled steroid as‐required only arm |
| Anonymous 1999 | Wrong drug ‐ not rapid‐acting beta agonist |
| Anonymous 2003 | Review article |
| Anonymous 2007 | Review article |
| Arun 2012 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| AstraZeneca 2005 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| AstraZeneca 2006 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| AstraZeneca 2006a | Participants with moderate or severe asthma |
| AstraZeneca 2006b | Regular daily use of beta agonist/inhaled steroid |
| AstraZeneca 2009 | Regular daily use of beta agonist/inhaled steroid |
| AstraZeneca 2012 | Regular daily use of beta agonist/inhaled steroid |
| AstraZeneca 2012a | Regular daily use of beta agonist/inhaled steroid |
| AstraZeneca 2012b | Regular daily use of beta agonist/inhaled steroid |
| Atienza 2013 | Regular daily use of beta agonist/inhaled steroid |
| Balanag 2003 | Intervention lasted less than 12 weeks |
| Balanag 2004 | Intervention lasted less than 12 weeks |
| Balanzat 2004 | Not a primary study ‐ aggregate of other trials |
| Barnes 1995 | Intervention lasted less than 12 weeks |
| Barnes 2000 | Regular daily use of beta agonist/inhaled steroid |
| Barnes 2007 | Review article |
| Bateman 2001 | Regular daily use of beta agonist/inhaled steroid |
| Bateman 2004 | Regular daily use of beta agonist/inhaled steroid |
| Bateman 2004a | Regular daily use of beta agonist/inhaled steroid |
| Bateman 2007 | Wrong drug ‐ not rapid‐acting beta agonist |
| Bateman 2018 | Correspondence about another (primary) article |
| Beasley 2013 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| Beeh 2002 | Wrong drug ‐ not rapid‐acting beta agonist |
| Benbow 1994 | Review article |
| Bennati 1989 | Participants with moderate or severe asthma |
| Bisgaard 2016 | Combination of data from other studies, not primary research |
| Bodzenta‐Lukaszyk 2010 | Regular daily use of beta agonist/inhaled steroid |
| Bodzenta‐Lukaszyk 2010a | Regular daily use of beta agonist/inhaled steroid |
| Bodzenta‐Lukaszyk 2013 | Participants with moderate or severe asthma |
| Bousquet 2007 | Regular daily use of beta agonist/inhaled steroid |
| Braido 2010 | Regular daily use of beta agonist/inhaled steroid |
| Bruce 2005 | Regular daily use of beta agonist/inhaled steroid |
| Buhl 2001 | Regular daily use of beta agonist/inhaled steroid |
| Buhl 2004 | Regular daily use of beta agonist/inhaled steroid |
| Buhl 2007 | Regular daily use of beta agonist/inhaled steroid |
| Buhl 2007a | Review article |
| Buhl 2010 | Regular daily use of beta agonist/inhaled steroid |
| Busse 2007 | Participants with moderate or severe asthma |
| Canonica 2004 | Regular daily use of beta agonist/inhaled steroid |
| Carnimeo 1979 | Not randomised |
| Chandra 2013 | Participants with moderate asthma |
| Chew 2012 | Intervention duration too short |
| ChiCTR1800019852 2018 | Regular daily use of beta agonist/inhaled steroid |
| ChiCTR1800020279 2018 | Included participants with moderate asthma |
| Chuchalin 2002 | Regular maintenance inhaled steroid |
| Creticos 1999 | Regular daily use of beta agonist/inhaled steroid |
| D'Urzo 2005 | Regular daily use of beta agonist/inhaled steroid |
| Dahl 2005 | Regular daily use of beta agonist/inhaled steroid |
| Dal Negro 2001 | Wrong drug ‐ not rapid‐acting beta agonist |
| Del Bufalo1989 | Participants with moderate or severe asthma |
| Dente 2001 | Wrong drug ‐ not rapid‐acting beta agonist |
| Didier 1994 | Regular daily use of beta agonist/inhaled steroid |
| Dorinsky 2000 | Wrong drug ‐ not rapid‐acting beta agonist |
| Eliraz 2002 | Intervention lasted less than 12 weeks |
| Ericsson 2001 | Not a randomised controlled trial |
| Estrada 2005 | Participants with moderate or severe asthma |
| EUCTR2004‐000211‐26‐SE 2004 | Regular daily use of beta agonist/inhaled steroid |
| EUCTR2004‐000679‐32‐FI 2004 | Regular daily use of beta agonist/inhaled steroid |
| EUCTR2004‐001107‐36‐BE 2005 | Regular daily use of beta agonist/inhaled steroid |
| EUCTR2004‐004042‐41‐SE 2005 | Regular daily use of beta agonist/inhaled steroid |
| EUCTR2004‐004905‐11‐DE 2005 | Regular daily use of beta agonist/inhaled steroid |
| EUCTR2005‐000372‐41‐GB 2005 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| EUCTR2005‐000532‐25‐CZ 2006 | Regular daily use of beta agonist/inhaled steroid |
| EUCTR2005‐000532‐25‐IS 2005 | Regular daily use of beta agonist/inhaled steroid |
| EUCTR2005‐000836‐25‐SE 2005 | Regular daily use of beta agonist/inhaled steroid |
| EUCTR2005‐002950‐23‐SE 2005 | Regular daily use of beta agonist/inhaled steroid |
| EUCTR2005‐003518‐14‐HU 2005 | Regular daily use of beta agonist/inhaled steroid |
| EUCTR2005‐005305‐32‐GB 2005 | Regular daily use of beta agonist/inhaled steroid |
| EUCTR2006‐005349‐13‐ES 2008 | Regular daily use of beta agonist/inhaled steroid |
| EUCTR2006‐006512‐30‐DE 2007 | Regular daily use of beta agonist/inhaled steroid |
| EUCTR2007‐001634‐13‐GB 2007 | Regular daily use of beta agonist/inhaled steroid |
| EUCTR2007‐002816‐25‐IT 2007 | Regular daily use of beta agonist/inhaled steroid |
| EUCTR2008‐004671‐22‐IT 2008 | Regular daily use of beta agonist/inhaled steroid |
| EUCTR2008‐006869‐86‐HU 2008 | Regular daily use of beta agonist/inhaled steroid |
| EUCTR2009‐012805‐20‐SE 2009 | Intervention lasted less than 12 weeks |
| EUCTR2018‐003467‐64‐GB 2018 | Daily use of controller medication |
| FAS40008 2005 | Regular daily use of beta agonist/inhaled steroid |
| Faurschou 1997 | Regular daily use of beta agonist/inhaled steroid |
| Finiguerra 1989 | Intervention lasted less than 12 weeks |
| FitzGerald 2003 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| Fitzgerald 2005 | Regular daily use of beta agonist/inhaled steroid |
| FitzGerald 2005 | Regular daily use of beta agonist/inhaled steroid |
| Fitzgerald 2005a | Regular daily use of beta agonist/inhaled steroid |
| FitzGerland 2004 | Regular daily use of beta agonist/inhaled steroid |
| Gauthier 2019 | Commentary, not original research |
| Geppe 2008 | Regular daily use of beta agonist/inhaled steroid |
| Gerald 2012 | Not a combined ICS/beta agonist inhaler |
| Gerald 2012a | Not a combined IC beta agonist inhaler |
| Gillissen 2001 | Review article |
| Goseva 2005 | Regular daily use of beta agonist/inhaled steroid |
| Greefhorst 1992 | Regular daily use of beta agonist/inhaled steroid |
| Gross 1998 | Wrong drug ‐ not rapid‐acting beta agonist |
| Guarnaccia 1990 | Intervention lasted less than 12 weeks |
| Haahtela 1990 | Not a combination inhaler |
| Haahtela 1991 | Not as needed inhaled steroid/beta agonist |
| Handslip 1978 | Review article |
| Haughney 2002 | Regular daily use of beta agonist/inhaled steroid |
| Haughney 2002a | Regular daily use of beta agonist/inhaled steroid |
| Haughney 2004 | Regular daily use of beta agonist/inhaled steroid |
| Henriksen 1993 | Intervention lasted less than 12 weeks |
| Holt 2004 | Regular daily use of beta agonist/inhaled steroid |
| Holt 2004a | Wrong drug ‐ not rapid‐acting beta agonist |
| Ige 2010 | Regular daily use of beta agonist/inhaled steroid |
| Ind 2002 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| Ind 2002a | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| Ind 2002b | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| Ind 2003 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| Ind 2004 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| Joseph 2001 | Letter, not original research |
| Kaik 2002 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| Kalberg 1998 | Not a rapid‐acting beta agonist |
| Kardos 2001 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| Kardos 2002 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| Kardos 2003 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| Kim 1998 | Not a combined ICS and beta agonist inhaler |
| Kim 2009 | Participants with moderate or severe asthma |
| Kips 1997 | Participants with moderate or severe asthma |
| Kovesi 2011 | Review article |
| Kraemer 1993 | Review article |
| Kuna 2010 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| La 1991 | Regular maintenance inhaled steroid |
| LaForce 1994 | Not a rapid‐acting beta agonist |
| Lalloo 2000 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| Lalloo 2001 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| La Rosa 1991a | Intervention lasted less than 12 weeks |
| Lazarinis 2011 | Intervention lasted less than 12 weeks |
| Lazarinis 2014 | Intervention lasted less than 12 weeks |
| Lazzaro 2009 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| Lee 2003 | Participants with moderate or severe asthma |
| Lemiere 2002 | Commentary, not original research |
| Leuppi 2003 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| Lin 2015 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| Lipworth 2004 | Review article |
| Loukides 2005 | Participants with moderate or severe asthma |
| Lumry 1999 | Participants with moderate or severe asthma |
| Magnussen 1995 | Intervention lasted less than 12 weeks |
| Malozowski 1998 | Letter, not original research |
| Martinez 2011 | Not a combined ICS and beta agonist inhaler ‐ separate inhalers |
| Maspero 2009 | Participants with moderate or severe asthma |
| Matsunaga 2013 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| McCarthy 2001 | Not a rapid‐acting beta agonist |
| McCarthy 2001a | Not a rapid‐acting beta agonist |
| McIver 2012 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| McIver 2012a | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| Michillis 2003 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| Miller 2007 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| Miller 2008 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| Montani 2007 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| Moretti 2003 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| Morice 2005 | Participants with moderate or severe asthma |
| Morice 2005a | Participants with moderate or severe asthma |
| Morjaria 2019 | Regular maintenance inhaled steroid |
| Nakazawa 1994 | Intervention lasted less than 12 weeks |
| Nathan 2010 | Participants with moderate or severe asthma |
| NCT00118690 2005 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| NCT00118716 2005 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| NCT00169546 2005 | Not a rapid‐acting beta agonist |
| NCT00197106 2005 | Not a rapid‐acting beta agonist |
| NCT00235911 2005 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| NCT00238784 2005 | Participants with moderate or severe asthma |
| NCT00242411 2005 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| NCT00244608 2005 | Regular (not simply as‐required) ICS/ beta agonist inhaler use |
| NCT00252824 2005 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| NCT00259792 2005 | Participants with moderate or severe asthma |
| NCT00273026 2006 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| NCT00288379 2006 | Participants with moderate or severe asthma |
| NCT00291382 2006 | Not a rapid‐acting beta agonist |
| NCT00319306 2006 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| NCT00326053 2006 | Regular (not simply prn as‐required) ICS/beta agonist inhaler use |
| NCT00381485 2006 | Regular maintenance inhaled steroid |
| NCT00382889 2006 | Includes participants with moderate asthma (> 400 mcg inhaled steroid per day) |
| NCT00385593 2012 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| NCT00394121 2006 | Not randomised |
| NCT00419757 2007 | Participants with moderate or severe asthma |
| NCT00424008 2007 | Participants with moderate or severe asthma |
| NCT00441441 2007 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| NCT00461812 2007 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| NCT00475813 2007 | Participants with moderate or severe asthma |
| NCT00479739 2007 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| NCT00497237 2007 | Participants with moderate or severe asthma |
| NCT00528723 2007 | Regular (not simply prn as‐required) ICS/beta agonist inhaler use |
| NCT00628758 2008 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| NCT00646529 2008 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| NCT00651547 2008 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| NCT00651651 2008 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| NCT00651768 2008 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| NCT00652002 2008 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| NCT00658255 2008 | Intervention lasted less than 12 weeks |
| NCT00861926 2009 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| NCT00901368 2009 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| NCT01070888 2010 | Intervention lasted less than 12 weeks |
| NCT01444430 2011 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| NCT01471340 2011 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| NCT01566149 2012 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| NCT01676987 2012 | Regular (not simply prn as‐required) ICS/beta agonist inhaler use |
| NCT02491970 2015 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| NCT02741271 2016 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| NCT03015259 2017 | Intervention lasted less than 12 weeks |
| NCT03924635 2019 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| NCT04171180 2019 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| Nelson 2000 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| Nelson 2007 | Regular (not simply prn as‐required) ICS/beta agonist inhaler use |
| Ness 1993 | Review article |
| O'Brien 2007 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| O'Byrne 2001 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| O'Byrne 2004 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| O'Byrne 2005 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| O'Connor 2010 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| Obodo 2009 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid a‐ required only arm |
| Olsson 2002 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| Papi 2013 | Regular (not simply prn) ICS/beta agonist inhaler use |
| Patel 2013 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| Pauwels 1996 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| Pauwels 1998 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| Pauwels 2004 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| Pearlman 2000 | Wrong intervention ‐ doe not include a beta agonist/inhaled steroid as‐required only arm |
| Pedersen 2006 | Editorial, not primary research |
| Peters 2007 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| Pieters 1998 | Participants with moderate or severe asthma |
| Pilcher 2013 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| Pilcher 2016 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| Plit 1984 | Participants with moderate or severe asthma |
| Pohl 2004 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| Pover 1986 | Intervention lasted less than 12 weeks |
| Prenner 2007 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| Price 2003 | Participants with moderate or severe asthma |
| Price 2005 | Participants with moderate or severe asthma |
| Rabe 2004a | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| Rabe 2006 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| Remington 2002 | Review article |
| Riemersma 2012 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| Rooklin 2001 | Participants with moderate or severe asthma |
| Rosenhall 2001 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| Rosenhall 2001a | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| Saito 2012 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| SAM40027 2004 | Wrong intervention ‐ doe not include a beta agonist/inhaled steroid as‐required only arm |
| Sanguinetti 2003 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| SAS30013 2004 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| Schmidtmann 2005 | Intervention lasted less than 12 weeks |
| Schreurs 1998 | Regular daily use of beta agonist/inhaled steroid |
| Scicchitano 2004 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| SD‐039‐0349 1999 | Participants with moderate or severe asthma |
| SD‐039‐0618 2005 | Regular daily use of beta agonist/inhaled steroid |
| SD‐039‐0667 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| Sears 2003 | Regular daily use of beta agonist/inhaled steroid |
| Sergio 2012 | Intervention lasted less than 12 weeks |
| Serrier 2003 | Intervention lasted less than 12 weeks |
| Shah 2007 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| Shah 2009 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| Somerville 2007 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| Sovani 2004 | Regular daily use of beta agonist inhaled steroid |
| Stallberg 2003 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| Stoloff 2002 | Review article |
| Sudarshan 2012 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| Sumino 2018 | Not a combination inhaler |
| Sumino 2019 | Not a combination inhaler |
| Syed 2008 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| Søes‐Petersen 2011 | Wrong intervention ‐ does not include a beta agonist/inhaled steroid as‐required only arm |
| Tal 2001 | Participants with moderate or severe asthma |
| Tschopp 1984 | Not a combination inhaler |
| Tsoi 2006 | Regular daily use of beta agonist/inhaled steroid |
| UMIN000010825 2013 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| van Dalen 2009 | Intervention lasted less than 12 weeks |
| Van Der Woude 2004 | Intervention lasted less than 12 weeks |
| van Essen‐Zandvliet 1988 | Not a combined ICS and beta agonist inhaler |
| van Schayck 2012 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| Vermeulen 2001 | Participants with moderate or severe asthma |
| Vogelmeier 2005 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| Vogelmeier 2005a | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| Vogelmeier 2012 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| Wallin 1998 | Intervention lasted less than 12 weeks |
| Weinstein 2001 | Not a rapid‐acting beta agonist |
| Welte 2004 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| Worth 2005 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
| Yi 2003 | Intervention lasted less than 12 weeks |
| Zetterstrom 2000 | Participants with moderate or severe asthma |
| Zetterstrom 2000a | Participants with moderate or severe asthma |
| Zetterstrom 2001 | Participants with moderate or severe asthma |
| Zhong 2013 | Regular (not simply as‐required) ICS/beta agonist inhaler use |
Characteristics of ongoing studies [ordered by study ID]
ACTRN12620001091998 2020.
| Study name | A randomised controlled trial of the efficacy and safety of an inhaled corticosteroid and long acting beta agonist reliever therapy regimen in children with mild asthma‐ CARE: Children's Anti‐inflammatory REliever |
| Methods | Randomised controlled trial |
| Participants | Children aged 5‐15 with a doctor diagnosis of asthma (parent/participant‐reported) using an SABA reliever as sole asthma medication in the previous three months |
| Interventions | Budesonide‐formoterol PMI 50 mcg/3 mcg, two puffs via spacer as required. Comparator‐ salbutamol PMI 100mcg as required via spacer |
| Outcomes | Asthma attacks, severe asthma attacks as rate per participant per year,least one asthma attack (moderate and severe) and severe attack, time to first asthma attack (moderate and severe) and severe attack. Days in Hospital, FeNo, FEV1, ACQ‐5, lost school days, lost work days (parents/guardians), total systemic corticosteroid dose, growth |
| Starting date | |
| Contact information | Dr Lee Hatter Address Medical Research Institute of New Zealand Level 7 CSB Building Wellington Hospital Riddiford Street Newtown Wellington 6021 lee.hatter@mrinz.ac.nz (public and scientific enquiries) |
| Notes |
NCT04215848 2020.
| Study name | Efficacy of as‐needed budesonide/formoterol turbuhaler during stepping down period from step‐3 in adult patients with adequately controlled asthma |
| Methods | Randomised, parallel |
| Participants | Adults ages 18‐75 with a diagnosis of asthma of more than 6 months that is well‐controlled |
| Interventions | Budesonide/formoterol 160/4.5 mcg as required. Comparator‐ budesonide 200 mcg two puffs twice daily |
| Outcomes | Time and rate to first moderate/severe asthma exacerbation rate or loss of asthma controlled, ratio of asthma controlled, FEV1, FeNo, PEF, blood eosinophils, mean inhaled steroid dose. |
| Starting date | 01/02/2020 |
| Contact information | Naongwit Nakwan, M.D. naronak@hotmail.com |
| Notes |
ACQ: Asthma Control Questionnaire; SABA: short‐acting beta‐agonists
Differences between protocol and review
Three new review authors joined the team, PW, RR and EO'B, and two review authors stepped down, A Chaudhry and G Hynes.
Contributions of authors
SR and TSCH wrote the protocol Background. IC wrote the Methods section based on a standard Cochrane template with contributions from all the authors. IC, ST, SR, MG, FY, AF and TH screened abstracts and full texts. IC, ST, SR, MG, FY, AF, TH, RR, PW and EO’B performed data extraction. RR and TH wrote the lay summary. IC performed the meta‐analysis and TH wrote the discussion with contributions from all authors.
Contributions of editorial team
Rebecca Fortescue (Co‐ordinating Editor): edited the protocol; advised on methodology.
Chris Cates (Co‐ordinating Editor): checked the planned methods, approved the protocol prior to publication.
Emma Dennett (Managing Editor): co‐ordinated the editorial process; advised on content; edited the protocol.
Emma Jackson (Assistant Managing Editor): conducted peer review;edited the references and other sections of the review.
Elizabeth Stovold (Information Specialist): designed the search strategy; conducted the database searches.
Sources of support
Internal sources
-
National Institute for Health Research, UK
TSC Hinks, S Ramakrishnan and G Hynes were supported by the NIHR Oxford Biomedical Research Centre
-
NIHR Cochrane Incentive Award, UK
This work was supported by an NIHR Cochrane Incentive Awards Scheme 2019: NIHR130687 to I Crossingham
External sources
-
Wellcome Trust, UK
TSC Hinks was supported by a Wellcome Trust Career Development Fellowship 211050/Z/18/Z
Declarations of interest
I Crossingham works in a clinically‐relevant speciality. He has been involved in recruitment for a GlaxoSmithKline‐sponsored trial of inhaled nemiralisib for COPD, but did not directly receive funding for this.
S Turner reports money for travel from Novartis in 2019 for an educational event.
S Ramakrishnan is undertaking a PhD supported by an unrestricted research grant from AstraZeneca. He has attended educational events sponsored by AstraZeneca (2019). He also works in a clinically relevant specialty.
A Fries works in a clinically relevant speciality (respiratory medicine).
M Gowell: none known.
F Yasmin: none known.
R Richardson: none known.
P Webb works in a clinically relevant speciality (respiratory medicine)
E O'Boyle: none known.
TSC Hinks has received research funding from the Wellcome Trust (4 February 2015 to 31 July 2018, 3 December 2018 ‒ ongoing), NIHR (1 May 2019 ‒ ongoing), and the Beit Guardians (3 December 2018 ‒ ongoing). He has received speaker fees from AstraZeneca in June 2019, Boehringer Ingelheim (March 2019) and his research team have received funding from Sanofi (September 2019 ‒ ongoing).
Edited (no change to conclusions)
References
References to studies included in this review
Haahtela 2006 {published data only}
- Haahtela T, Tamminen K, Malmberg LP, Zetterstrom O, Karjalainen J, Yla-Outinen H, et al. Formoterol as needed with or without budesonide in patients with intermittent asthma and raised NO levels in exhaled air: A SOMA study. European FRespiratory Journal 2006;28(4):748-55. [DOI] [PubMed] [Google Scholar]
- Haahtela T, Tamminen K, Malmberg P, Karjalainen J, Yia-Outinen H, Zetterstrom O, et al. As-needed treatment with a b2-agonist/ corticosteroid combination in mild intermittent asthma (SOMA) [Abstract]. European Respiratory Journal 2005;26:1722. [Google Scholar]
Novel START {published data only}
- Beasley R, Holliday M, Reddel HK, Braithwaite I, Ebmeier S, Hancox RJ, et al. Controlled trial of budesonide-formoterol as needed for mild asthma. New England Journal of Medicine 2019;380(21):2020-30. [DOI] [PubMed] [Google Scholar]
- Beasley R, Pavord I, Papi A, Reddel HK, Harrison T, Marks GB, et al. Description of a randomised controlled trial of inhaled corticosteroid/fast-onset LABA reliever therapy in mild asthma. European Respiratory Journal 2016;47(3):981-4. [DOI] [PubMed] [Google Scholar]
- Beasley RW, Holliday M, Reddel HK, Braithwaite I, Ebmeier S, Hancox R, et al. Pragmatic randomized controlled trial of budesonide/formoterol reliever therapy in adults with mild asthma. American Journal of Respiratory and Critical Care Medicine 2019;199:A7477. [Google Scholar]
- EUCTR2015-002384-42-GB. Randomised controlled trial of the efficacy and safety of an ICS (Inhaled Corticosteroid)/LABA (long-acting beta agonist) reliever therapy regimen in asthma. www.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2015-002384-42-GB (first received 6 October 2016).
- Pavord ID, Holliday M, Reddel HK, Braithwaite I, Ebmeier S, Hancox RJ, et al. Predictive value of blood eosinophils and exhaled nitric oxide in adults with mild asthma: a prespecified subgroup analysis of an open-label, parallel-group, randomised controlled trial. Lancet Respiratory Medicine 2020;8(7):671-80. [DOI] [PubMed] [Google Scholar]
PRACTICAL {published data only}
- ACTRN12616000377437. Randomised controlled trial of the efficacy and safety of an inhaled corticosteroid and long acting beta agonist reliever therapy regimen in asthma [A 52-week, open label, parallel group, multicentre, phase III, randomised controlled trial to compare the efficacy and safety of Budesonide/formoterol turbuhaler taken as required for relief of symptoms and Budesonide turbuhaler as maintenance and terbutaline turbuhaler as required for relief of symptoms of asthma in adults]. www.who.int/trialsearch/Trial2.aspx?TrialID=ACTRN12616000377437 (first received 23 March 2016).
- Anonymous. Erratum: department of Error (The Lancet (2019) 394(10202) (919-928), (S0140673619319488), (10.1016/S0140-6736(19)31948-8)). Lancet 2020;395(10234):1422. [Google Scholar]
- Baggott C, Hardy J, Sparks J, Holliday M, Hall D, Vohlidkova A, et al. Self-titration of inhaled corticosteroid and beta2-agonist in response to symptoms in mild asthma: a pre-specified analysis from the PRACTICAL randomised controlled trial. European Respiratory Journal 2020;56(4):2000170. [DOI] [PubMed] [Google Scholar]
- Hardy J, Baggott C, Fingleton J, Reddel HK, Hancox RJ, Harwood M, et al. Budesonide-formoterol reliever therapy versus maintenance budesonide plus terbutaline reliever therapy in adults with mild to moderate asthma (PRACTICAL): a 52-week, open-label, multicentre, superiority, randomised controlled trial. Lancet 2019;394(10202):919-28. [DOI] [PubMed] [Google Scholar]
- Hardy J, Baggott C, Fingleton J, Reddel HK, Hancox RJ, Harwood M, et al. Open-label trial of budesonide/formoterol reliever therapy in mild asthma. European Respiratory Journal 2019;54:OA5332. [Google Scholar]
- Hardy J, Tewhaiti-Smith J, Baggott C, Fingleton J, Semprini A, Holliday M, et al. Combination budesonide/formoterol inhaler as sole reliever therapy in Maori and Pacific people with mild and moderate asthma. New Zealand Medical Journal 2020;133(1520):61-72. [PubMed] [Google Scholar]
SYGMA 1 {published data only}
- EUCTR2013-004474-96-RO. A 52-week, double-blind, randomised, multi-centre, parallel-group,Phase III study in patients 12 years and older with asthma, evaluating the efficacy and safety of Symbicort® (budesonide/formoterol) Turbuhaler® 160/4.5 µg ‘as needed’ compared with terbutaline Turbuhaler® 0.4 mg ‘as needed’ and with Pulmicort® (budesonide) Turbuhaler® 200 µg twice daily plus terbutaline Turbuhaler® 0.4 mg ‘as needed’. www.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2013-004474-96-RO (first received 23 April 2014).
- Fitzgerald M, O'Byrne PM, Bateman ED, Barnes PJ, Zhong N, Alagappan V, et al. Number needed to treat (NNT) to have an additional patient free from a severe or moderate/severe exacerbation: post-hoc analysis of SYGMA 1 in mild asthma. European Respiratory Journal 2019;54:PA3716. [Google Scholar]
- O'Byrne PM, FitzGerald JM, Bateman ED, Barnes PJ, Zheng J, Gustafson P, et al. Effect of a single day of increased as-needed budesonide-formoterol use on short-term risk of severe exacerbations in patients with mild asthma: a post-hoc analysis of the SYGMA 1 study. Lancet Respiratory Medicine 2020;9(2):149-58. [DOI] [PubMed] [Google Scholar]
- O'Byrne PM, FitzGerald JM, Bateman ED, Barnes PJ, Zhong N, Keen C, et al. Inhaled combined budesonide-formoterol AS needed in mild asthma. New England Journal of Medicine 2018;378(20):1865-76. [DOI] [PubMed] [Google Scholar]
- O'Byrne PM, FitzGerald JM, Zhong N, Bateman E, Barnes PJ, Keen C, et al. The SYGMA programme of phase 3 trials to evaluate the efficacy and safety of budesonide/formoterol given 'as needed' in mild asthma: study protocols for two randomised controlled trials. Trials 2017;18(1):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OByrne P, Fitzgerald JM, Bateman E, Barnes PJ, Zhong N, Gustafson P, et al. Risk of a severe exacerbation following higher reliever use: post-hoc analysis of SYGMA 1 in mild asthma. Pneumologie 2019;73:P05. [Google Scholar]
- PER-035-14. A 52-week, double-blind, randomised, multi-centre, parallel-group,phase iii study in patients 12 years and older with asthma, evaluating the efficacy and safety of symbicort® (budesonide/formoterol) turbuhaler® 160/4.5μg ‘as needed’ compared with terbutaline turbuhaler® 0.4 mg ‘as needed’ and with pulmicort® (budesonide) turbuhaler® 200μg twice daily plus terbutaline turbuhaler® 0.4 mg ‘as needed’. www.who.int/trialsearch/Trial2.aspx?TrialID=PER-035-14 (first received 24 October 2014).
- Reddel H, Bateman ED, Fitzgerald JM, Barnes PJ, Zhong N, Lamarca R, et al. Exacerbation risk after night-time waking due to asthma in SYGMA 1. European Respiratory Journal 2019;54:PA3715. [Google Scholar]
- Reddel H, O'Byrne P, D Bateman E, Barnes P, Zheng J, Lamarca R, et al. Number needed to treat with as-needed budesonide/formoterol or budesonide maintenance to have an additional patient free from a severe or moderate/severe exacerbation: post-hoc analysis of sygma 1 in mild asthma. Respirology 2020;25:TO155. [Google Scholar]
SYGMA 2 {published data only}
- Bateman ED, Reddel HK, O'Byrne PM, Barnes PJ, Zhong N, Keen C, et al. As-needed budesonide-formoterol versus maintenance budesonide in mild asthma. New England Journal of Medicine 2018;378(20):1877-87. [DOI] [PubMed] [Google Scholar]
- ChiCTR-TRC-09000566. Mild asthma--as-needed Symbicort Turbuhaler clinical study. www.who.int/trialsearch/Trial2.aspx?TrialID=ChiCTR-TRC-09000566 (first received 18 October 2009).
- EUCTR2013-004473-28-SE. A 52-week, double-blind, randomised, multi-centre, phase III, parallel-group study in patients 12 years and older with asthma, evaluating the efficacy and safety of Symbicort (budesonide/formoterol) Turbuhaler 160/4.5 µg ‘as needed’ compared with Pulmicort (budesonide) Turbuhaler 200 µg twice daily plus terbutaline Turbuhaler 0.4 mg ‘as needed’. www.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2013-004473-28-SE (first received 27 August 2014).
- NCT02224157. A clinical study to evaluate symbicort turbuhaler used 'as needed' in adults and adolescents with asthma (SYGMA2) [A clinical study comparing Symbicort 'as needed' with Pulmicort twice daily plus Terbutaline 'as needed' in adult and adolescent patients with asthma]. clinicaltrials.gov/show/NCT02224157 (first received 25 August 2014).
Tanaka 2017 {published data only}
- Tanaka A, Ohta S, Yamamoto M, Jinno M, Miyata Y, Hirai K, et al. Tolerability of as-needed treatment with budesonide and formoterol combination in adult patients with mild asthma. American Journal of Respiratory and Critical Care Medicine 2017;195:A3199. [Google Scholar]
References to studies excluded from this review
Aalbers 2003 {published data only}
- Aalbers R, Backer V, Kava TT, Welte T, Omenaas ER, Bergqvist PB, et al. Adjustable dosing with budesonide/formoterol reduces the rate of asthma exacerbations compared with fixed dosing salmeterol/fluticasone. European Respiratory Journal 2003;22:2-20. [Google Scholar]
Aalbers 2004 {published data only}
- Aalbers R, Welte T, Jorup C. Adjustable maintenance dosing (AMD) with budesonide /formoterol (B/F) meets guideline-defined management goals more effectively than fixed dosing (FD) with B/F or salmeterol/fluticasone (S/FL). European Respiratory Journal 2004;24:311s. [Google Scholar]
Aalbers 2005 {published data only}
- Aalbers R, Harris A, Naya I. Adjustable dosing with budesonide/formoterol achieves sustained guideline ‘well-controlled asthma‘ following step down in treatment. European Respiratory Journal 2005;26:50s. [Google Scholar]
Agarwal 2010 {published data only}
- Agarwal SK, Sharma S. Utility of inhaled corticosteroids (fluticasone/formoterol) by pressurized metered-dose inhaler for the early management of acute exacerbations of asthma. In: European Respiratory Society Annual Congress; 2010 Sep 18-22; Barcelona. 2010:[E5476].
Aggarwal 2003 {published data only}
- Aggarwal SK, Frith LJ, Ho M, Weeks T, Ho SY. Fluticasone propionate/salmeterol delivered from a single inhaler demonstrates synergistic benefits in asthma. Amercian Journal of Respiratory and Critical Care Medicine 2003;167(7):A890. [Google Scholar]
Aldrey 1995 {published data only}
- Aldrey OE, Anez H, Deibis L, Tassinari P, Isturiz G, Bianco NE. A double-blind, cross-over study using salbutamol, beclomethasone, and a combination of both in bronchial asthma. Journal of Asthma 1995;32(1):21-8. [DOI] [PubMed] [Google Scholar]
Aldridge 2000 {published data only}
- Aldridge RE, Town GI, Hancox RJ, Cowan JO, Winn MC, Chan T, et al. Eosinophilis and eosinophil cationic protein in induced sputum compared to blood: effects of budesonide and terbutaline treatment. European Respiratory Journal 2000;16:101s. [Google Scholar]
Aldridge 2002 {published data only}
- Aldridge RE, Hancox RJ, Cowant JO, Frampton CM, Town GI, Taylor DR. Eosinophils and eosinophilic cationic protein in induced sputum and blood: effects of budesonide and terbutaline treatment. Annals of Allergy, Asthma and Immunology 2002;89(5):492-7. [DOI] [PubMed] [Google Scholar]
Ankerst 2000 {published data only}
- Ankerst J, Persson G, Weibull E. A high dose of budesonide/formoterol in a single inhaler was well tolerated by asthmatic patients. European Respiratory Journal 2000;16:33s. [Google Scholar]
Ankerst 2001 {published data only}
- Ankerst J, Persson G, Weibull E. Symbicort® (budesonide and formoterol in a single inhaler) was well tolerated by asthmatic patients. In: Annual Thoracic Society 97th International Conference; 2001 May 18-23; San Francisco. 2001:D31.
Ankerst 2002 {published data only}
- Ankerst J, Malolepszy J, Eliraz A. Budesonide/formoterol in a single inhaler is more effective than a higher dose of inhaled corticosteroids in patients with persistent asthma. European Respiratory Journal 2002;20:387s. [Google Scholar]
Anonymous 1999 {published data only}
- No authors listed. Salmeterol/fluticasone propionate combination product in asthma. An evaluation of its cost effectiveness vs fluticasone propionate. Pharmacoeconomics 1999;16:i-viii, 1-34. [PubMed] [Google Scholar]
Anonymous 2003 {published data only}
- No authors listed. Flexible dosing of combination inhaler cuts asthma exacerbations. Pharmaceutical Journal 2003;271(7271):535. [Google Scholar]
Anonymous 2007 {published data only}
- No authors listed. PRN steroids are as good as - or better than - daily dosing for asthma. Journal of Family Practice 2007;56(8):620. [PubMed] [Google Scholar]
Arun 2012 {published data only}
- Arun JJ, Lodha R, Kabra SK. Bronchodilatory effect of inhaled budesonide/formoterol and budesonide/salbutamol in acute asthma: a double-blind, randomized controlled trial. BMC Pediatrics 2012;12:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
AstraZeneca 2005 {published data only}
- NCT00288379. SMILDA - Symbicort Turbuhaler allergen challenge study in allergic patients with mild asthma [A comparative, placebo-controlled, double blind, double dummy, cross-over, single centre, phase IIIb study between formoterol alone (Oxis® Turbuhaler® 4.5 µg) and the fixed combination of formoterol and budesonide (Symbicort® Turbuhaler®160/4.5 µg) on airway responsiveness and airway inflammation induced by repeatedlLow-dose allergen challenge in allergic patients with mild asthma]. www.clinicaltrials.gov/ct2/show/NCT00288379 (first received 8 February 2006).
AstraZeneca 2006 {published data only}
- D5890C00002. Efficacy and safety of Symbicort® Turbuhaler® 160/4.5 mcg/inhalation, two inhalations twice daily plus as-needed compared with Seretide Diskus 50/500 mcg/inhalation, one inhalation twice daily plus terbutaline Turbuhaler 0.4 mg/inhalation as-needed - a 6-month, randomised, double-blind, parallel-group, active controlled, multinational phase IIIB study in adult and adolescent patients with persistent asthma (AHEAD). astrazenecagrouptrials.pharmacm.com/ST/Submission/View?id=1511 (first received 1 May 2005).
AstraZeneca 2006a {published data only}
- NCT00290264. SALTO - symbicort single inhaler therapy use in adolescent adults and adults with persistent asthma. clinicaltrials.gov/ct2/history/NCT00290264?V_7=View#StudyPageTop (first received 9 February 2006).
AstraZeneca 2006b {published data only}
- NCT00244608. A comparison of the control of asthma inflammation provided by Symbicort turbuhaler 160/4.5 mcg/inhalation bid plus as-needed versus Symbicort turbuhaler 320/9 ug/inhalation bid plus Pulmicort turbuhaler 400mcg/dose bid plus Terbutaline turbuhaler 0.4mg/inhalation as-needed [A comparison of the inflammatory control of asthma provided by one inhalation of Symbicort® Turbuhaler® 160/4.5 µg/inhalation b.i.d. plus as-needed versus one inhalation of Symbicort® Turbuhaler® 320/9 µg/inhalation b.i.d. + one inhalation of Pulmicort® Turbuhaler® 400 µg/Dose b.i.d. plus Terbutaline Turbuhaler® 0.4 mg/inhalation as-needed. A 12-month, randomised, double-blind, parallel-group, active controlled, multinational, phase IIIB study in adult patients with asthma, EOS]. clinicaltrials.gov/ct2/show/NCT00244608 (first received 27 October 2005).
AstraZeneca 2009 {published data only}
- AstraZeneca SD-039-0735. Comparison of the efficacy and safety of one inhalation of Symbicort® Turbuhaler® 160/4.5 µg bid plus as-needed with two inhalations of SeretideTM EvohalerTM 25/125 µg bid plus Terbutaline Turbuhaler® 0.4 mg as-needed, and one inhalation of Symbicort® Turbuhaler® 320/9 µg bid plus Terbutaline Turbuhaler® 0.4 mg as-needed. A 6-month, randomised, double-blind, double-dummy, parallel-group, active-controlled, multi-centre, phase IIIB study in adult and adolescent asthmatic patients. astrazenecagrouptrials.pharmacm.com/ST/Submission/View?id=1999 (first received 27 June 2009).
AstraZeneca 2012 {published data only}
- AstraZeneca D5890L00011. A comparison of symbicort® single inhaler therapy (symbicort® turbuhaler® 160/4.5 mcg, 1 inhalation b.i.d. plus as-needed) and conventional best practice for the treatment of persistent asthma in adults - a 26-week, randomised, open-label, parallel-group, multicentre study. http://www.astrazenecaclinicaltrials.com/_mshost800325/content/clinical-trials/resources/pdf/D5890L00011 2012.
AstraZeneca 2012a {published data only}
- AstraZeneca. STYLE - a comparison of Symbicort SMART (symbicort turbuhaler160/4,5 mcg, 1 inhalation b.i.d. plus as needed) and conventional best practice for the treatment of persistent asthma in adolescents and adults – a 26-week, open-labelled, parallel-group, multicentre study. Http://www.astrazenecaclinicaltrials.com/_mshost800325/content/clinical-trials/resources/pdf/8610702 2012.
AstraZeneca 2012b {published data only}
- AstraZeneca. A comparison of Symbicort single inhaler therapy (Symbicort Turbuhaler160/4.5 mg, 1 inhalation b.i.d. plus as needed) and conventional best practice for the treatment of persistent asthma in adults - a 26-week, randomised, open-label, parallel-group, multicentre study – PASSION Study. Http://www.astrazenecaclinicaltrials.com/_mshost800325/content/clinical-trials/resources/pdf/8610675 2012.
Atienza 2013 {published data only}
- Atienza T, Aquino T, Fernandez M, Boonsawat W, Kawai M, Kudo T, et al. Budesonide/formoterol maintenance and reliever therapy via Turbuhaler versus fixed-dose budesonide/formoterol plus terbutaline in patients with asthma: phase III study results. Respirology 2013;18(2):354-63. [DOI] [PubMed] [Google Scholar]
Balanag 2003 {published data only}
- Balanag VM, Yunus F, Yang PC, Jorup C. Budesonide/formeterol in a single inhaler is as effective and well tolerated as salbutamol in relieving acute asthma in adults and adolescents. European Respiratory Journal 2003;22:P2836. [Google Scholar]
Balanag 2004 {published data only}
- Balanag M, Boonsawat W, Rubinfeld A, Selroos O. Formoterol and budesonide/formoterol are both equally as fast and effective as salbutamol in relieving severe acute bronchospasm. European Respiratory Journal 2004;24:541s. [Google Scholar]
Balanzat 2004 {published data only}
- Balanzat A, Centanni S, Palmqvist M, Rabe K. Budesonide/formoterol single inhaler therapy reduces over reliance on rapid acting reliever medication. European Respiratory Journal 2004;24:344s. [Google Scholar]
Barnes 1995 {published data only}
- Barnes PJ, O'Connor BJ. Use of a fixed combination beta 2-agonist and steroid dry powder inhaler in asthma. American Journal of Respiratory and Critical Care Medicine 1995;151(4):1053-7. [DOI] [PubMed] [Google Scholar]
Barnes 2000 {published data only}
- Barnes PJ, O'Byrne PM, Rodriguez-Roisin R, Runnerstrom E, Sandstrom T, Svensson K, et al. Treatment of mild persistent asthma with low doses of inhaled budesonide alone or in combination with formoterol. Thorax 2000;55:s5. [Google Scholar]
Barnes 2007 {published data only}
- Barnes PJ. Using a combination inhaler (budesonide plus formoterol) as rescue therapy improves asthma control. BMJ 2007;335(7618):513. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bateman 2001 {published data only}
- Bateman ED, Bantje TA, Joao Gomes M, Toumbis M, Huber R, Eliraz A, et al. Symbicort® (budesonide and formoterol in a single inhaler) is a more effective treatment than fluticasone in asthma patients. In: Annual Thoracic Society 97th International Conference; 2001 May 18-23; San Francisco. 2001:D31.
Bateman 2004 {published data only}
- Bateman ED, Boushey HA, Bousquet J, Busse WW, Clark TJ, Pauwels RA, et al. Can guideline-defined asthma control be achieved? The Gaining Optimal Asthma ControL study. American Journal of Respiratory and Critical Care Medicine 2004;170(8):836-44. [DOI] [PubMed] [Google Scholar]
Bateman 2004a {published data only}
- Bateman ED, Palmqvist M, Juniper EF, Zhu Y, Ekstrom T. Single inhaler therapy with budesonside/formoterol has superior efficacy to fixed-dose budesonide/formoterol or a higher dose of budesonide alone. In: American Thoracic Society 100th International Conference; 2004 May 21-26; Orlando. 2004:A37 Poster J75.
Bateman 2007 {published data only}
- Bateman ED, Bousquet J, Keech ML, Busse WW, Clark TJ, Pedersen SE. The correlation between asthma control and health status: the GOAL study. European Respiratory Journal 2007;29(1):56-62. [DOI] [PubMed] [Google Scholar]
Bateman 2018 {published data only}
- Bateman ED, Reddel HK, FitzGerald JM. As-needed budesonide-formoterol in mild asthma. New England Journal of Medicine 2018;379(9):898. [DOI] [PubMed] [Google Scholar]
Beasley 2013 {published data only}
- Beasley R, Patel M, Pilcher J, Weatherall M, Black P. Maintenance and reliever budesonide/formoterol therapy has a favourable risk/benefit profile in real-world asthma. Respirology 2013;18:13 [O013]. [Google Scholar]
Beeh 2002 {published data only}
- Beeh KM, Beier J, Kornmann O, Wiewrodt R, Buhl R. Efficacy and safety of salmeterol (50 mcg) and fluticasone (250 mcg) in a single inhaler device (Diskus(R)) in patients with mild to moderate asthma. Pneumologie 2002;56(2):91-7. [DOI] [PubMed] [Google Scholar]
Benbow 1994 {published data only}
- Benbow AG, Naya IP. Patient compliance with inhaled medication: does combining beta-agonists with corticosteroids improve compliance? European Respiratory Journal 1994;7(8):1554. [DOI] [PubMed] [Google Scholar]
Bennati 1989 {published data only}
- Bennati D, Piacentini GL, Peroni DG, Sette L, Testi R, Boner AL. Changes in bronchial reactivity in asthmatic children after treatment with beclomethasone alone or in association with salbutamol. Journal of Asthma 1989;26(6):359-64. [DOI] [PubMed] [Google Scholar]
Bisgaard 2016 {published data only}
- Bisgaard H, Lythgoe D, Jorup C. Budesonide/formoterol maintenance and reliever therapy in adolescent patients with asthma. European Respiratory Journal 2016;48(Suppl 60):PA4903. [DOI] [PubMed] [Google Scholar]
Bodzenta‐Lukaszyk 2010 {published data only}
- Bodzenta-Lukaszyk A, Pulka G, Dymek A, Mansikka H. Fluticasone propionate/formoterol fumarate combination therapy has an efficacy and safety profile similar to that of its individual components administered concurrently in the treatment of asthma. In: European Respiratory Society Annual Congress; 2010 18-12 Sep; Barcelona. 2010:P1207.
Bodzenta‐Lukaszyk 2010a {published data only}
- Bodzenta-Lukaszyk A, Dymek A, Mansikka H. Fluticasone propionate/formoterol fumarate combination therapy is as effective as fluticasone propionate/salmeterol xinafoate, but has a more rapid onset of action in the treatment of asthma. In: European Respiratory Society Annual Congress; 2010 18-22 Sep; Barcelona. 2010:P1205.
Bodzenta‐Lukaszyk 2013 {published data only}
- Bodzenta-Lukaszyk A, Noord J, Schröder-Babo W, McAulay K, McIver T. Efficacy and safety profile of fluticasone/formoterol combination therapy compared to its individual components administered concurrently in asthma: a randomised controlled trial. Current Medical Research and Opinion 2013;29(5):579-88. [DOI] [PubMed] [Google Scholar]
Bousquet 2007 {published data only}
- Bousquet J, Miravitlles M, Wiren A. Budesonide /formoterol provides better efficacy at a lower or similar cost as compared to high dose salmeterol fluticasone treatment. European Respiratory Journal 2007;30:193s [P1185]. [Google Scholar]
Braido 2010 {published data only}
- Braido F, Troise C, Canonica GW, Paggiaro P, Voltolini S, Aubier M, et al. Budesonide/formoterol maintenance and reliever therapy, comparison between two different maintenance doses and predictive factors for the choice of the most appropriate maintenance dose. European Annals of Allergy and Clinical Immunology 2010;42(6):228. [Google Scholar]
Bruce 2005 {published data only}
- Bruce SA, Scherer YK. Maintenance and symptom relief with budesonide plus formoterol reduced severe asthma exacerbations. Evidence-Based Nursing 2005;8(3):78. [DOI] [PubMed] [Google Scholar]
Buhl 2001 {published data only}
- Buhl R, Creemers JP, Vondra V, Martelli NA. Symbicort ® (budesonide and formoterol in a single inhaler) administered once daily is effective in mild to moderate asthma. In: Annual Thoracic Society 97th International Conference; 2001 May 18-23 ; San Francisco. 2001:D31.
Buhl 2004 {published data only}
- Buhl R, Kardos P, Richter K, Meyer-Sabellek W, Bruggenjurgen B, Willich SN, et al. The effect of adjustable dosing with budesonide/formoterol on health-related quality of life and asthma control compared with fixed dosing. Current Medical Research and Opinion 2004;20(8):1209-220. [DOI] [PubMed] [Google Scholar]
Buhl 2007 {published data only}
- Buhl R, Kuna P. Does the choice of ICS/LABA regimen influence exacerbation rates in asthma patients with high as needed use? European Respiratory Journal 2007;30:617s [P3620]. [Google Scholar]
Buhl 2007a {published data only}
- Buhl R, Vogelmeier C. Budesonide/formoterol maintenance and reliever therapy: a new treatment approach for adult patients with asthma. Current Medical Research and Opinion 2007;23(8):1867-78. [DOI] [PubMed] [Google Scholar]
Buhl 2010 {published data only}
- Buhl R, O'Byrne PM, Humbert MJ, Peterson S, Eriksson GS. Patient baseline characteristics predict an increased risk of future asthma exacerbations. American Journal of Respiratory and Critical Care Medicine 2010;181(1 MeetingAbstracts):A5094. [Google Scholar]
Busse 2007 {published data only}
- Busse WW, Shah SR, Somerville L, Martin P, Goldman M. Comparison of asthma exacerbations and lung function with adjustable-dose budesonide/formoterol pressurized metered-dose inhaler (BUD/FM pmdi), fixed-dose BUD/FM pmdi, and fixed-dose fluticasone/salmeterol dry powder inhaler (FP/SM DPI). In: American Thoracic Society International Conference; 2007 May 18-23; San Francisco. 2007:A191.
Canonica 2004 {published data only}
- Canonica GW, Castellani P, Cazzola M, Fabbri LM, Fogliani V, Mangrella M, et al. Adjustable maintenance dosing with budesonide/formoterol in a single inhaler provides effective asthma symptom control at a lower dose than fixed maintenance dosing. Pulmonary Pharmacology and Therapeutics 2004;17(4):239-47. [DOI] [PubMed] [Google Scholar]
Carnimeo 1979 {published data only}
- Carnimeo N, Resta O, Valerio G, Foschino MP. Physiopathological evaluation of the combined beclomethasone-salbutamol therapy. Archivio Monaldi per la tisiologia e le malattie dell'apparato respiratorio 1979;34(1):49-54. [PubMed] [Google Scholar]
Chandra 2013 {published data only}
- Chandra S. Randomized, double blind comparative study to assess safety, efficacy with mometasone & formoterol versus fluticasone & formoterol dry powder inhaler (DPI) in the treatment of mild to moderate persistent asthma. World Allergy Organization Journal 2013;6:P225. [Google Scholar]
Chew 2012 {published data only}
- Chew KS, Kamarudin H, Hashim CW. A randomized open-label trial on the use of budesonide/formoterol (Symbicort ) as an alternative reliever medication for mild to moderate asthmatic attacks. International Journal of Emergency Medicine 2012;5(1):16. [DOI] [PMC free article] [PubMed] [Google Scholar]
ChiCTR1800019852 2018 {published data only}
- ChiCTR1800019852. The efficacy of budesonide/formoterol in cough variant asthma: a multi-center randomized, controlled clinical trial. www.chictr.org.cn/showproj.aspx?proj=33552 (first received 12 December 2018).
ChiCTR1800020279 2018 {published data only}
- ChiCTR1800020279. Clinical trial for step-down therapy in patients with mild to moderate asthma. ictrptest.azurewebsites.net/Trial2.aspx?TrialID=ChiCTR1800020279 (first received 22 December 2018).
Chuchalin 2002 {published data only}
- Chuchalin AG, Ovcharenko SI, Goriachkina LA, Sidorenko IV, Tsoi AN, Epoch Study Group. The safety and efficacy of formoterol (Oxis) turbuhaler plus budesonide (Pulmicort) turbuhaler in mild to moderate asthma: a comparison with budesonide Turbuhaler alone and current non-corticosteroid therapy in Russia. International Journal of Clinical Practice 2002;56(1):15-20. [PubMed] [Google Scholar]
Creticos 1999 {published data only}
- Creticos PS, Friedhoff LR, Bernstein DI, Chu T, Khattignavong AP, Pasatiempo AM, et al. Placebo comparison of an inhaled corticosteroid (triamcinolone acetonide) to a long-acting bronchodilator (salmeterol), the combination, and placebo in mild-moderate adult asthmatic patients. International Archives of Allergy and Immunology 1999;1181(2):345-6. [DOI] [PubMed] [Google Scholar]
D'Urzo 2005 {published data only}
- D'Urzo A, Vogeimeier C, Jaspal M, Merino JM, Boulet S. Symbicort (budesonide/formeterol) for both maintenance and relief reduces the exacerbation burden compared with titration of seretide (salmeterol/fluticasone) in patients with asthma, a real life study. In: American Thoracic Society International Conference; 2005 May 20-25; San Diego. 2005:[B35] [Poster: G24].
Dahl 2005 {published data only}
- Dahl R, Chuchalin A, Ringdal N, Gor D, Jones M. Salmeterol/fluticasone (SFC) reduces moderate/severe exacerbations more effectively than formoterol/budesonide 9FBC) with sustained maintenance therapy EXCEL. In: American Thoracic Society International Conference; 2005 May 20-25; San Diego. 2005:[C33] [Poster: F68].
Dal Negro 2001 {published data only}
- Dal Negro R, Micheletto C, Tognella S, Trevisan F, Pomari C. Short-term bronchodilation following salmeterol 50mcg and combined salmeterol + fluticasone p. (50/250 mcg) via diskus: a randomized, double-blind cross-over study in reversible airway obstruction. American Journal of Respiratory and Critical Care Medicine 2001;163(5):A866. [Google Scholar]
Del Bufalo1989 {published data only}
- Del Bufalo C, Impullitti S, Miniero R, Gunella G. Clinical controlled study on high doses of beclomethasone dipropionate associated with salbutamol in long term treatment of asthmatic subjects. Rivista di Patologia e Clinica della Tubercolosi e di Pneumologia 1989;60(2):137-55. [Google Scholar]
Dente 2001 {published data only}
- Dente FL, Scuotri L, Bacci E, Di Franco A, Giannini D, Taccola M, et al. Effects of combined treatment - fluticasone plus salmeterol - on allergen-induced asthmatic responses. American Journal of Respiratory and Critical Care Medicine 2001;463:A419. [Google Scholar]
Didier 1994 {published data only}
- Didier A, Desfougeres JL, Groupe de 28 Pneumologues Francais. Comparative study of salmeterol beclomethasona and terbutaline-budesonide. In deep treatment of adult asthma. Revue des Maladies Respiratoires 1994;11:R68. [Google Scholar]
Dorinsky 2000 {published data only}
- Dorinsky P, Yancey S, Kral K, Emmett A, House K, Prillaman B, et al. Asthma control with salmeterol/fluticasone propionate (50/250mcg) dry powder combination Diskus has a faster onset of effect compared with salmeterol or fluticasone propionate in patients with asthma. Journal Allergy and Clinical Immunology 2000;161:A195. [Google Scholar]
Eliraz 2002 {published data only}
- Eliraz A, Fritscher CC, Perez CM, Boonsawat W, Nang AN, Bardin P, et al. Symbicort® (Budesonide/Formoterol) achieves more rapid control of asthma that fluticasone in patients with mild asthma. American Journal of Respiratory and Critical Care Medicine 2002;165:A567. [Google Scholar]
Ericsson 2001 {published data only}
- Ericsson K, Bantje TA, Huber H, Borg S. Symbicort® turbuhaler® is more cost effective than fluticasone diskus™ in the treatment of asthma. In: Annual Thoracic Society 97th International Conference; 2001 May 18-23; San Francisco. 2001:D31.
Estrada 2005 {published data only}
- Estrada E, Nava-Ocampo A, Rosas-Vargas M, Del Rio-Navarro B. Co-administration of fluticasone and salbutamol for children with moderate acute asthma. In: XIX World Allergy Organization Congress; 2005 Jun 26-July 1; Munich. 2005:Abstract 851.
EUCTR2004‐000211‐26‐SE 2004 {published data only}
- EUCTR2004-000211-26-SE. A comparative, placebo-controlled, double blind, double dummy, cross over, single center phase IIIb study between formoterol alone and the fixed combination of formoterol and budesonide on airway responsiveness and airway inflammation induced by repeated low-dose allergen challenge. - SMILDA. ictrptest.azurewebsites.net/Trial2.aspx?TrialID=EUCTR2004-000211-26-SE (first received 4 August 2004).
EUCTR2004‐000679‐32‐FI 2004 {published data only}
- EUCTR2004-000679-32-FI. A comparison of the efficacy of symbicort single inhaler therapy (symbicort turbuhaler 160/4.5 microg, one inhalation twice a day plus as-needed) and conventional best standard treatment for the treatment of persistent asthma in adolescents and adults. A randomised, open, parallel-group, multicentre, 26 weeks study - MONO. www.clinicaltrialsregister.eu/ctr-search/search?query=EUCTR2004-000679-32-FI (first received 4 May 2005).
EUCTR2004‐001107‐36‐BE 2005 {published data only}
- EUCTR2004-001107-36-BE. A comparison of Symbicort Single inhaler Therapy (Symbicort Turbohaler 160/4.5 mg, 1 inhalation b.i.d. plus as needed) and conventional best practice for the treatment of persistent asthma in adolescents and adults - a 26-week, randomised, open-label, parallel-group, multi-centre study (SALTO) - SALTO. www.clinicaltrialsregister.eu/ctr-search/search? Query=eudract_number:2004-001107-36 (first received 19 November 2004).
EUCTR2004‐004042‐41‐SE 2005 {published data only}
- EUCTR2004-004042-41-SE. A comparison of the inflammatory control of asthma provided by one inhalation of Symbicort® Turbuhaler® 160/4.5 µg/inhalation b.i.d. plus as-needed versus one inhalation of Symbicort® Turbuhaler® 320/9 µg/inhalation b.i.d. + one inhalation of Pulmicort® Turbuhaler® 400 µg/dose b.i.d. plus Terbutaline Turbuhaler® 0.4 mg/inhalation as-needed. A 12-month, randomised, double-blind, parallel-group, active controlled, multinational, phase III B study in adult patients with asthma. - EOS. ictrptest.azurewebsites.net/Trial2.aspx?TrialID=EUCTR2004-004042-41-DE (first received 28 February 2005).
EUCTR2004‐004905‐11‐DE 2005 {published data only}
- EUCTR2004-004905-11-DE. Efficacy and safety of Symbicort® Turbuhaler® 160/4.5 µg/inhalation, two inhalations twice daily plus as-needed compared with Seretide™ Diskus™ 50/500 µg/inhalation, one inhalation twice daily plus terbutaline Turbuhaler 0.4 mg/inhalation as-needed - a 6-month randomised, double-blind, parallel-group, active controlled, multinational phase IIIB study in adult and adolescent patients with persistent asthma. - AHEAD. www.clinicaltrialsregister.eu/ctr-search/search?query=2004-004905-11 (first received 21 June 2005).
EUCTR2005‐000372‐41‐GB 2005 {published data only}
- EUCTR2005-000372-41-GB TN. Real life effectiveness in asthma of symbicort® single inhaler therapy (RELEASE) - RELEASE. www.clinicaltrialsregister.eu/ctr-search/search? Query=eudract_number:2005-000372-41 (first received 19 June 2005).
EUCTR2005‐000532‐25‐CZ 2006 {published data only}
- EUCTR2005-000532-25-CZ. A comparison of Symbicort Single inhaler Therapy (Symbicort Turbuhaler 160/4.5 mcg, 1 inhalation b.i.d. plus as needed) and conventional best practice for the treatment of persistent asthma in adolescents and adults - a 26-week, randomised, open-label, parallel-group, multicentre study - STYLE. ictrptest.azurewebsites.net/Trial2.aspx?TrialID=EUCTR2005-000532-25-IS (first received 12 May 2005).
EUCTR2005‐000532‐25‐IS 2005 {published data only}
- EUCTR2005-000532-25-IS. A comparison of symbicort single inhaler therapy (symbicort turbuhaler 160/4.5 mg, 1 inhalation b.i.d. plus AS needed) and conventional best practice for the treatment of persistent asthma in adolescents and adults - a 26-week, randomised, open-label, parallel-group, multicentre study - STYLE. www.clinicaltrialsregister.eu/ctr-search/search?query=2005-000532-25 (first received 15 June 2005).
EUCTR2005‐000836‐25‐SE 2005 {published data only}
- EUCTR2005-000836-25-SE. Seretide vs Flixotide in mild persistent asthma (GINAII). ictrptest.azurewebsites.net/Trial2.aspx?TrialID=EUCTR2005-000836-25-SE (first received 24 February 2005).
EUCTR2005‐002950‐23‐SE 2005 {published data only}
- EUCTR2005-002950-23-SE. A multi-centre, randomised, double blind, stratified, and parallel group study to evaluate whether a treatment strategy based on aiming for ‘Total control’ results in better airway hyper-responsiveness than a treatment strategy based on maintaining the treatment level at which ‘Well-controlled’ asthma was achieved. ictrptest.azurewebsites.net/Trial2.aspx?TrialID=EUCTR2005-002950-23-ES (first received 19 March 2005).
EUCTR2005‐003518‐14‐HU 2005 {published data only}
- EUCTR2005-003518-14-HU. Long-term open-label safety study with skp flutiform hfa pmdi (100/10µg and 250/10µg) in adult and adolescent patients with asthma. ictrptest.azurewebsites.net/Trial2.aspx?TrialID=EUCTR2005-003518-14-GB (first received 27 October 2005).
EUCTR2005‐005305‐32‐GB 2005 {published data only}
- EUCTR2005-005305-32-GB. A phase ii, randomised, double-blind, double-dummy crossover study to determine the superiority of hfa-propelled combination fluticasone propionate 125 mcg and salmeterol xinafoate 25 mcg pressurised metered dose inhalers over hfa-propelled fluticasone propionate 125 mcg pressurised metered dose inhalers alone in patients with mild to moderate asthma. ictrptest.azurewebsites.net/Trial2.aspx?TrialID=EUCTR2005-005305-32-GB (first received 11 November 2005).
EUCTR2006‐005349‐13‐ES 2008 {published data only}
- EUCTR2006-005349-13-ES. Ensayo clinico prospectivo, aleatorizado, abierto, multicentrico, controlado con farmaco activo, de grupos paralelos para evaluar la eficacia y la seguridad de dipropionato de beclometasona 400 µg + formoterol 24 µg pmdi a traves de hfa-134a (foster™) frente a propionato de fluticasona 500 µg + xinafoato de salmeterol 100 µg dpi (seretide diskus®) en el tratamiento con reduccion progresiva de la dosis durante 6 meses en pacientes adultos con asma controlado - forte. ictrptest.azurewebsites.net/Trial2.aspx?TrialID=EUCTR2006-005349-13-IT (first received 12 April 2007).
EUCTR2006‐006512‐30‐DE 2007 {published data only}
- EUCTR2006-006512-30-DE. A Pan-European, open label, randomised study comparing the efficacy and cost-effectiveness of Symbicort Maintenance and Reliever Therapy (Symbicort SMART) using a maintenance dose of Symbicort 160/4.5 micrograms of 1 or 2 inhalations twice daily in the treatment of persistent asthma. EUROSMART - EUROSMART. ictrptest.azurewebsites.net/Trial2.aspx?TrialID=EUCTR2006-006512-30-SE (first received 22 December 2006).
EUCTR2007‐001634‐13‐GB 2007 {published data only}
- EUCTR2007-001634-13-GB. An open, randomised, parallel group, multicentre study to compare the efficacy and safety of FlutiFormTM pMDI vs Fluticasone pMDI plus Formoterol DPI in adolescent and adult subjects with mild to moderate-severe persistent, reversible asthma. ictrptest.azurewebsites.net/Trial2.aspx?TrialID=EUCTR2007-001634-13-DE (first received 6 July 2007).
EUCTR2007‐002816‐25‐IT 2007 {published data only}
- EUCTR2007-002816-25-IT. Multicentre, multinational, randomised, double blind, double dummy, active drug controlled, parallel group study design clinical trial of the efficacy and tolerability of beclomethasone dipropionate 250 mcg plus salbutamol 100 mcg in HFA pMDI fixed combination vs. beclomethasone dipropionate 250 mcg plus salbutamol 100 mcg in CFC pMDI (Clenil Compositum 250) fixed combination in a 12-week treatment period of adult patients with uncontrolled asthma - ND. www.clinicaltrialsregister.eu/ctr-search/search?query=2007-002816-25 (first received 18 September 2007).
EUCTR2008‐004671‐22‐IT 2008 {published data only}
- EUCTR2008-004671-22-IT. A 48-week, multicentre, multinational, randomized, double-blind, 2-arm parallel group study, comparing the efficacy of FOSTERTM for maintenance and reliever versus fixed-dose FOSTERTM for maintenance + salbutamol as reliever in asthmatics >12 years of age. ictrptest.azurewebsites.net/Trial2.aspx?TrialID=EUCTR2008-004671-22-FR (first received 23 October 2008).
EUCTR2008‐006869‐86‐HU 2008 {published data only}
- EUCTR2008-006869-86-HU. A comparison of Symbicort® Maintenance and Reliever Therapy (Symbicort Turbuhaler® 160/4.5 mg, one inhalation bid plus as-needed) and Symbicort Turbuhaler 160/4.5 mg, one inhalation bid plus terbutaline Turbuhaler 0.4 mg/inhalation as needed, for treatment of asthma – a 12-month, randomized, double-blind, parallel group, active-controlled, multinational phase III study in asthmatic patients aged 16 years and above. - SAKURA. ictrptest.azurewebsites.net/Trial2.aspx?TrialID=EUCTR2008-006869-86-HU (first received 29 December 2008).
EUCTR2009‐012805‐20‐SE 2009 {published data only}
- EUCTR2009-012805-20-SE. A randomised, double blind, placebo controlled, parallel-group study with use of budesonide/formoterol “as-needed”, or terbutaline “as-needed” or regular use of budesonide + terbutaline “as-needed”, in patients with mild intermittent asthma. ictrptest.azurewebsites.net/Trial2.aspx?TrialID=EUCTR2009-012805-20-SE (first received 29 May 2009).
EUCTR2018‐003467‐64‐GB 2018 {published data only}
- EUCTR2018-003467-64-GB. A 24-week Study aiming to characterise changes in airway inflammation, symptoms, lung function, and reliever use in asthma patients using Salbutamol or AntiInflammatory Reliever (Symbicort® ) as rescue medication in addition to Symbicort® as daily asthma controller. www.clinicaltrialsregister.eu/ctr-search/search?query=2018-003467-64 (first received 30 Jan 2019).
FAS40008 2005 {published data only}
- FAS40008. An interventional three year study for asthma control - In what way and in what kind of population is it possible to get asthmatic patients free from symptoms, keep the patients in work, restore a normal lung function, diminish hyperreactivity and normalise quality of life? www.gsk-studyregister.com/en/trial-details/?id=FAS40008 (first received 1 July 2005).
Faurschou 1997 {published data only}
- Faurschou P, Dahl R, Jeffery P, Venge P, Egerod I. Comparison of the anti-inflammatory effects of fluticasone and salmeterol in asthma: a placebo controlled, double blind, cross-over study with bronchoscopy, bronchial methacholine provocation and lavage. European Respiratory Journal 1997;10:243S. [Google Scholar]
Finiguerra 1989 {published data only}
- Finiguerra M, Conti P, Rubini F, Biraghi M, Morandini GC. Flunisolide + salbutamol (VAL 679/A) inhaled in flogistic-obstructive respiratory disease. Controlled trial vs salbutamol. Minerva Pneumologica 1989;28(3):139-48. [Google Scholar]
FitzGerald 2003 {published data only}
- FitzGerald JM, Sears MR, Boulet LP, Becker AB, McIvor AR, Ernst P, et al. Adjustable maintenance dosing with budesonide/formoterol reduces asthma exacerbations compared with traditional fixed dosing: a five-month multicentre Canadian study. Canadian Respiratory Journal 2003;10(8):427-34. [DOI] [PubMed] [Google Scholar]
Fitzgerald 2005 {published data only}
- Fitzgerald JM, Boulet LP, Follows R. Improved control of symptoms, exacerbations and quality of life with stable dose treatment with salmeterol/fluticasone (SFC) compared with adjustable maintenance dosing with formoterol/budesonide. In: XIX World Allergy Organization Congress; 2005 June 26-July 1; Munich. 2005:Abstract 289.
FitzGerald 2005 {published data only}
- FitzGerald JM, Boulet LP, Follows RM. The CONCEPT trial: a 1-year, multicenter, randomized,double-blind, double-dummy comparison of a stable dosing regimen of salmeterol/fluticasone propionate with an adjustable maintenance dosing regimen of formoterol/budesonide in adults with persistent asthma. Clinical Therapeutics 2005;27(4):393-406. [DOI] [PubMed] [Google Scholar]
Fitzgerald 2005a {published data only}
- Fitzgerald M, Boulet LP, Pieters WR. Improved control of symptoms and exacerbations with stable dose treatment with salmeterol/fluticasone propionate (SFC) compared with adjustable maintenance dosing with formoterol/budesonide (FBC). European Respiratory Journal 2005;26:Abstract No. 2765. [Google Scholar]
FitzGerland 2004 {published data only}
- FitzGerland JM, Sears MR, Boulet LP, Becker AB. Erratum: Adjustable maintenance dosing with budesonide/formoterol reduces asthma exacerbations compared with traditional fixed dosing: A five month multicentre Canadian study [Canadian Respiratory Journal (2003) vol. 10 (8) (427-434)]. Canadian Respiratory Journal 2004;11(1):20. [DOI] [PubMed] [Google Scholar]
Gauthier 2019 {published data only}
- Gauthier M, Wenzel SE. As-needed beta agonist-inhaled corticosteroid in mild asthma. Lancet 2019;394(10202):897-8. [DOI] [PubMed] [Google Scholar]
Geppe 2008 {published data only}
- Geppe N, Denisova A, Sokolova N, Kirdakov F. Variation of regular maintenance therapy with budesonide/formoterol of children with asthma. In: European Respiratory Society Annual Congress; 2008 Oct 4-8; Berlin. 2008:E3067.
Gerald 2012 {published data only}
- Gerald JK, Gerald LB, Chinchilli VM, Bioty N, Martinez FD. Adherence to rescue inhaled corticosteroid use during the TREXA trial. American Journal of Respiratory and Critical Care Medicine 2012;185:A2200. [Google Scholar]
Gerald 2012a {published data only}
- Gerald LB, Gerald JK, Graber N, Chinchilli V, Martinez FD. Predictors of response to inhaled corticosteroids: Stratified results from the TREXA trial. American Journal of Respiratory and Critical Care Medicine 2012;185:A4071. [Google Scholar]
Gillissen 2001 {published data only}
- Gillissen A, Buhl R, Magnussen H, Menz G, Rabe K, Vogelmeier C, et al. Solid combination of budesonide and formoterol in the treatment of bronchial asthma. Pneumologie 2001;55(3):159-62. [DOI] [PubMed] [Google Scholar]
Goseva 2005 {published data only}
- Goseva Z, Dokic D, Gjorcev A, Nikolau M, Arsovski Z. Asthma control with inhaled corticosteroids (ICS) and beta2-agonists. In: XIX World Allergy Organization Congress; 2005 June 26-July 1; Munich. 2005:Abstract 282.
Greefhorst 1992 {published data only}
- Greefhorst AP. Budesonide and terbutaline delivered via turbuhaler compared to BDP and salbutamol delivered via rotahaler. European Respiratory Journal 1992;5:360s. [Google Scholar]
Gross 1998 {published data only}
- Gross G, Woodring A, Prillaman B, House K, Shah T. Efficacy and safety of the salmeterol/fluticasone propionate (50/100 µg) dry powder combination inhaler in patients with asthma. European Respiratory Journal 1998;12:156S. [Google Scholar]
Guarnaccia 1990 {published data only}
- Guarnaccia S, Pasquali M, Acerbis F, Pedrali M, Duse M, Ugazio AG. Clinico-functional evaluation of flunisolide + salbutamol combination (VAL 679/A) vs salbutamol in pediatric patients. Minerva Pediatrica 1990;42(6):237-42. [PubMed] [Google Scholar]
Haahtela 1990 {published data only}
- Haahtela T, Alanko K, Muittari A, Lahdensuo A, Sahlstrom K, Vilkka V. The superiority of the combination beclometasone-salbutamol over standard doses of salbutamol in at the treatment of chronic asthma. Comptes Rendus de Therapeutique et de Pharmacologie Clinique 1990;8(85):23-9. [Google Scholar]
Haahtela 1991 {published data only}
- Haahtela T, Jarvinen M, Kava T. Comparison of a beta2-agonist, terbutaline, with an inhaled corticosteroid, budesonide, in newly detected asthma. Annals of Internal Medicine 1991;115:82. [DOI] [PubMed] [Google Scholar]
Handslip 1978 {published data only}
- Handslip PD, Hartley JP. Salbutamol and beclomethasone in chronic asthma. Lancet 1978;2(8087):481. [DOI] [PubMed] [Google Scholar]
Haughney 2002 {published data only}
- Haughney J, Price D, Rosen JP, Morrison K. Symbicort used in a guided self management plan provides additional enablement to asthma patients compared with fixed dosing. Thorax 2002;57:iii88. [Google Scholar]
Haughney 2002a {published data only}
- Haughney J, Price D, Rosen JP, Kennelly J. Adjustable maintenance treatment with budesonide/formoterol combination rapidly improves and maintains quality of life in asthma patients. In: European Respiratory Society 12th Annual Congress; 2002 Sep 14-18; Stockholm. 2002:P379.
Haughney 2004 {published data only}
- Haughney J, Buhl R. Adjustable maintenance dosing with budesonide/formoterol (symbicort) is as well tolerated as fixed dosing: data from over 10,000 asthma patients. In: American Thoracic Society 100th International Conference; 2004 May 21-26; Orlando. 2004:A37 Poster J91.
Henriksen 1993 {published data only}
- Henriksen JM, Dahl R. Effects of inhaled budesonide alone and in combination with low-dose terbutaline in children with exercise-induced asthma. American Review of Respiratory Disease 1993;128(6):993-7. [DOI] [PubMed] [Google Scholar]
Holt 2004 {published data only}
- Holt S, Ryder-Lewis S, Masoli M, Weatherall M, Beasley R. The use of novel fixed and adjustable dose symbicort self-management plans in asthma. In: American Thoracic Society 100th International Conference; 2004 May 21-26; Orlando. 2004:B39 Poster C11.
Holt 2004a {published data only}
- Holt S, Masoli M, Beasley R. Increasing compliance with inhaled corticosteroids through the use of combination therapy. Journal of Allergy and Clinical Immunology 2004;113(2):219-20. [DOI] [PubMed] [Google Scholar]
Ige 2010 {published data only}
- Ige OM, Ohaju-Obodo JO, Chukwu C, Peters EJ, Okpapi J, Chukwuka C. Effectiveness and safety of adjustable maintenance dosing with budesonide/formoterol turbuhaler compared with traditional fixed doses in bronchial asthma: a multi-centre Nigerian study. African Journal of Medicine and Medical Sciences 2010;39(3):165-72. [PubMed] [Google Scholar]
Ind 2002 {published data only}
- Ind P, Haughney J, Price D, Rosen JP, Kennelly J, Rosen J-P. Four months adjustable or fixed BD dosing with budesonide /Formoterol in a single inhaler reduces symptom severity. Thorax 2002;57:iii 88. [Google Scholar]
Ind 2002a {published data only}
- Ind P, Haughney J, Price D, Rosen JP, Kennelly J. Managed adjustable dosing of budesonide/formoterol combination provides equivalent asthma control to fixed dosing at a lower overall dose. In: European Respiratory Society 12th Annual Congress; 2002 Sep 14-18; Stockholm. 2002:abstract P2450.
Ind 2002b {published data only}
- Ind P, Haughney J, Price D, Rosen J P, Kennelly J. 4-month adjustable or fixed maintenance treatment with budesonide/formoterol in a single inhaler reduces symptoms severity. European Respiratory Journal 2002;20:41s. [Google Scholar]
Ind 2003 {published data only}
- Ind PW, Price D, Haughney J, Rosen JP. Adjustable dosing with budesonide/formoterol in a single inhaler (symbicortA®) provides similarly effective treatment of asthma compared with fixed dosing but at a lower overall dose. In: American Thoracic Society 99th International Conference; 2003 May 16-21; Seattle. 2003:D034 Poster C38.
Ind 2004 {published data only}
- Ind PW, Haughney J, Price D, Rosen JP, Kennelly J. Adjustable and fixed dosing with budesonide/ formoterol via a single inhaler in asthma patients: the ASSURE study. Respiratory Medicine 2004;98(5):464-75. [DOI] [PubMed] [Google Scholar]
Joseph 2001 {published data only}
- Joseph J, Badrinath P. On-demand relief treatment for asthma. Lancet 2001;357(9271):1882-3. [DOI] [PubMed] [Google Scholar]
Kaik 2002 {published data only}
- Kaik G, Kottakis I, Anagnostopoulou O, Sichletidis L, Bachlitzanakis N, D'Amato M, et al. Sequential flexible therapy with formoterol (Foradil®) plus budesonide (Miflonide®) versus a fixed combination of salmeterol and fluticasone (Seretide®) in asthma self-management. In: European Respiratory Society 12th Annual Congress; 2002 Sep 14-18; Stockholm. 2002:P2407.
Kalberg 1998 {published data only}
- Kalberg CJ, Nelson H, Yancey S, Petrocella V, Emmett AH, Rickard KA. A comparison of added salmeterol versus increased-dose fluticasone in patients symptomatic on low-dose fluticasone. Journal of Allergy and Clinical Immunology 1998;101:S6. [Google Scholar]
Kardos 2001 {published data only}
- Kardos P, Bruggenjurgen B, Martin A, Meyer-Sabellek W, Richter K, Vogelmeier C, et al. Treatment of bronchial asthma using a new adjustable combination treatment plan: asthma Control Plan (ATACO). Pneumologie 2001;55(5):253-7. [DOI] [PubMed] [Google Scholar]
Kardos 2002 {published data only}
- Kardos P, Brueggenjuergen B, Baare A, Meyer-Sabellek W, Richter K, Voelmeier C, et al. The ATACO study: adjustable maintenance therapy with budesonide and formoterol in a single inhaler. European Respiratory Journal 2002;20:41s. [Google Scholar]
Kardos 2003 {published data only}
- Kardos P, Richter K, Vogelmeier C, Bruggenjurgen B, Willich SN, Baare A, et al. Adjustable dosing with budesonide/formoterol in a single inhaler maintains improvement in health-related quality of life at a lower drug load than fixed dosing - the ATACO study. European Respiratory Journal 2003;22:P1696. [Google Scholar]
Kim 1998 {published data only}
- Kim JH, Oh JW, Lee HB. Beneficial effects of inhaled budesonide on elevated circulating levels of serum ecp, icam-1, vcam-1, il-6 and il-6r in children with asthma. Pediatric Allergy and Respiratory Disease 1998;8(1):37-46. [Google Scholar]
Kim 2009 {published data only}
- Kim KT, Lanier BQ, Goldman M, Martin P, Zangrilli J. Effect of adjustable-dose (AD) budesonide/formoterol pressurized metered-dose inhaler (pMDI), fixed-dose (FD) budesonide/formoterol pMDI, and FD fluticasone/salmeterol dry powder inhaler (DPI) on predose FEF25-75%. American Thoracic Society International Conference; 2009 May 15-20 San Diego 2009;179:A2788 [Poster #J57]. [Google Scholar]
Kips 1997 {published data only}
- Kips JC, O'Connor BJ, Svensson K, Pauwels RA, O'Byrne PM. Low dose budesonide plus formoterol versus high dose budesonide in asthma therapy: effects on markers of airway inflammation. European Respiratory Journal 1997;10:1S. [DOI] [PubMed] [Google Scholar]
Kovesi 2011 {published data only}
- Kovesi T. In children and adolescents with mild persistent asthma, daily beclomethasone reduces treatment failure compared with rescue beclomethasone plus albuterol. Evidence-Based Medicine 2011;16(6):183-4. [DOI] [PubMed] [Google Scholar]
Kraemer 1993 {published data only}
- Kraemer R, Modelska K, Casaulta Aebischer CC, Schoni MH. Comparison of different inhalation schedules to control childhood asthma. Agents and Actions 1993;40:211-21. [DOI] [PubMed] [Google Scholar]
Kuna 2010 {published data only}
- Kuna P. Treatment comparison of budesonideformoterol with salmeterolfluticasone propionate in adults aged >16 years with asthma: post hoc analysis of a randomized, double-blind study. Clinical Drug Investigation 2010;30(9):565-79. [DOI] [PubMed] [Google Scholar]
La 1991 {published data only}
- La Rosa M, Francesco G, Musarra I, Biraghi M. Double-blind comparative study of inhaled flunisolide and flunisolide plus salbutamol in bronchial asthma in children. Current Therapeutic Research 1991;50(1):56-61. [Google Scholar]
LaForce 1994 {published data only}
- LaForce C, Liddle RF, Yancey SW. Salmeterol response in asthmatic patients using inhaled corticosteroids and in those not using inhaled corticosteroids. Annals of Allergy 1994;72:100. [Google Scholar]
Lalloo 2000 {published data only}
- Lalloo UG, Bantje TA, Kozma D, Krofta K, Ankerst J, Johansen B, et al. Low-dose symbicort (budesonide/formoterol) is more effective than double-dose inhaled corticosteroid in mild asthma. Allergy and Clinical Immunology International 2000;4:122. [Google Scholar]
Lalloo 2001 {published data only}
- Lalloo UG, Malolepszy J, Kozma D, Krofta K, Ankerst J, Johansen B, et al. Symbicort® (budesonide and formoterol in a single inhaler) is more effective than increasing the dose of inhaled corticosteroid in mild asthma. American Journal of Respiratory and Critical Care Medicine 2001;163(5):A863. [Google Scholar]
La Rosa 1991a {published data only}
- La Rosa M, Guglielmo F, Musarra I, Biraghi M. Double-blind comparative study of inhaled Flunisolide and Flunisolide + Salbutamol in childhood bronchial asthma. Pediatria Oggi 1991;11(6):176-80. [Google Scholar]
Lazarinis 2011 {published data only}
- Lazarinis N, Bjermer L, Carlsen K-H, Dahlen B, Ekstrom T, Hedlin G, et al. Effect of budesonide/formoterol, budesonide and terbutaline on exercise-induced bronchoconstriction in mild intermittent asthma. In: European Respiratory Society 21st Annual Congress; 2011 Sep 24-28; Amsterdam. Vol. 38. 2011:720s [P3957].
Lazarinis 2014 {published data only}
- Lazarinis N, Jorgensen L, Ekstrom T, Bjermer L, Dahlen B, Pullerits T, et al. Combination of budesonide/formoterol on demand improves asthma control by reducing exercise-induced bronchoconstriction. Thorax 2014;69(2):130-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lazzaro 2009 {published data only}
- Lazzaro C, Ruffo P, Gozzo M. Cost-effectiveness analysis of budesonide/formoterol combination for both maintenance and reliever therapy in the management of asthma. An Italian evaluation. Pharmacoeconomics 2009;11(1):39-53. [Google Scholar]
Lee 2003 {published data only}
- Lee DK, Currie GP, Cockburtn WJ, Lipworth BJ. Comparison of budesonide/formoterol versus fluticasone/salmeterol combination inhalers in moderate persistent asthma. In: American Thoracic Society 99th International Conference; 2003 May 16-21; Seattle. 2003:D094 Poster 613.
Lemiere 2002 {published data only}
- Lemiere C, Becker A, Boulet LP, Bowie D, Cartier A, Cockroft D, et al. Should combination therapy with inhaled corticosteroids and long-acting beta2-agonists be prescribed as initial maintenance treatment for asthma? Canadian Medical Association Journal 2002;167(9):1008-9. [PMC free article] [PubMed] [Google Scholar]
Leuppi 2003 {published data only}
- Leuppi JD, Salzberg M, Meyer L, Bucher SE, Nief M, Brutsche MH, et al. Benefits of adjustable vs fixed maintenance dosing of budesonide/formoterol: a Swiss study in asthma. European Respiratory Journal 2003;22:P1694. [Google Scholar]
Lin 2015 {published data only}
- Lin J, Tang Y, Xiu Q, Kang J, Cai S, Huang K, et al. Real-life effectiveness of budesonide/formoterol therapy in asthma: a Chinese sub-analysis of the smartasia study. Respirology 2015;20:16. [Google Scholar]
Lipworth 2004 {published data only}
- Lipworth BJ, Fardon TC. Enhanced synergy between fluticasone propionate and salmeterol inhaled from a single inhaler versus separate inhalers. Journal of Allergy and Clinical Immunology 2004;113(1):178; author reply 178-9. [DOI] [PubMed] [Google Scholar]
Loukides 2005 {published data only}
- Loukides S, Papageorgiou M, Karokis A, Zervas E, Christodoulopoulou A, Papageorgiou N, et al. Single inhaler therapy (SiT) with budesonide/formoterol (BUD/FUM) is effective in asthma control. European Respiratory Journal 2005;26:848. [Google Scholar]
Lumry 1999 {published data only}
- Lumry W, Windhom H, Mendelson L, Pedinoff A, Prillaman B, Baitinger L, et al. The salmeterol/fluticasone propionate (50/250mcg) dry powder combination Diskus has a faster onset of effect compared with salmeterol or fluticasone propionate in patients with asthma. Journal Allergy and Clinical Immunology 1999;103(1):S132. [Google Scholar]
Magnussen 1995 {published data only}
- Magnussen H, Willenbrock U, Jorres R. Duration of the effect of inhaled corticosteroids on lung function and sensitivity of the respiratory tract in patients with bronchial asthma. Medizinische Klinik 1995;90(4):214-9. [PubMed] [Google Scholar]
Malozowski 1998 {published data only}
- Malozowski S, Stadel BV, Pian LP. Comparison of beclomethasone, salmeterol, and placebo in children with asthma. New England Journal of Medicine 1998;339(10):704-5. [DOI] [PubMed] [Google Scholar]
Martinez 2011 {published data only}
- Gerald JK, Gerald LB, Vasquez MM, Morgan WJ, Boehmer SJ, Lemanske RF Jr, et al. Markers of differential response to inhaled corticosteroid treatment among children with mild persistent asthma [erratum appears in j allergy clin immunol pract. 2015 sep-oct;3(5):793]. Journal of Allergy and Clinical Immunology 2015;3(4):540-6.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez FD, Chinchilli VM, Morgan WJ, Boehmer SJ, Lemanske RFJr, Mauger DT, et al. Use of beclomethasone dipropionate as rescue treatment for children with mild persistent asthma (TREXA): a randomised, double-blind, placebo-controlled trial. Lancet 2011;377(9766):650-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Maspero 2009 {published data only}
- Maspero JF, Cherrez I, Nolte H. Mometasone furoate and formoterol (MF/F) combination administered via a metered-dose inhaler (MDI) for the treatment of asthma: results from a 1-yr safety study. In: American Thoracic Society International Conference; 2009 May 15-20; San Diego. 2009:A2768 [Poster #J37].
Matsunaga 2013 {published data only}
- Matsunaga K, Hirano T, Ichinose M. Difference in time-course of improvement in asthma control measures between budesonide and budesonide/formoterol. American Journal of Respiratory and Critical Care Medicine 2013;187:None. [CENTRAL: CN-01107670] [DOI] [PubMed] [Google Scholar]
McCarthy 2001 {published data only}
- McCarthy TP, Edin HM, House K, Vandermeer AK. Quality of life and asthma control assessment in patients previously treated with inhaled corticosteroids (ICS), treated with salmeterol/fluticasone combination (SFC) metered dose inhaler (MDI). Thorax 2001;56:iii64. [Google Scholar]
McCarthy 2001a {published data only}
- McCarthy TP, Edin HM, House K, Yan SK, Vandermeer AK, Vandermeer AK. The effects of salmeterol/fluticasone combination (SFC) dry powder inhaler (DPI) on asthma control and quality of life in patients previously treated with inhaled corticosteroids (ICS). Thorax 2001;56:iii 63. [Google Scholar]
McIver 2012 {published data only}
- McIver T, Grothe B, Jain M, Dissanayake S. Fluticasone propionate/formoterol fumarate combination therapy: treatment effects in patients by baseline asthma severity across the dose range. Thorax 2012;67:A68 [P12]. [Google Scholar]
McIver 2012a {published data only}
- McIver T, Grothe B, Jain M, S Dissanayake. Fluticasone propionate/formoterol fumarate combination therapy has an efficacy profile similar to that of its individual components administered concurrently. Thorax 2012;67:A66. [Google Scholar]
Michillis 2003 {published data only}
- Michillis A, Peche RV, Verbraeken JA, Vandenhoven G, Wollaert L, Duquenne V. SURF study: real-life effectiveness of budesonide/formoterol (B/F) adjustable maintenance dosing. Allergy and Clinical Immunology International 2003;1:P-2-39. [Google Scholar]
Miller 2007 {published data only}
- Miller E, Sears MR, McIvor A, Liovas A. Canadian economic evaluation of budesonide-formoterol as maintenance and reliever treatment in patients with moderate to severe asthma. Canadian Respiratory Journal 2007;14(5):269-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
Miller 2008 {published data only}
- Miller E, FitzGerald JM. Budesonide / formoterol as maintenance and reliever treatment compared to fixed dose combination strategies - A Canadian economic evaluation. Canadian Journal of Clinical Pharmacology 2008;15(2):e165-e76. [PubMed] [Google Scholar]
Montani 2007 {published data only}
- Montani D. Randomized comparison of strategies for reducing treatment in mild persistent asthma. Revue de Pneumologie Clinique 2007;63(6):390. [Google Scholar]
Moretti 2003 {published data only}
- Moretti A, Canonica GW, Sanguinetti CM, Mangrella M, Stabilini M. Adjustable maintenance dosing with budesonide/formoterol controls asthma symptom severity and maintains lung function with a lower overall dose than fixed dosing: results of an Italian study. European Respiratory Journal 2003;22:P1703. [Google Scholar]
Morice 2005 {published data only}
- Morice AH, Hochmuth L, Puterman A, Artheden L, Beckman O. Comparable safety of a novel budesonide/formoterol pMDI versus budesonide/formoterol Turbuhaler in adolescents and adults with asthma. Journal of Allergy and Clinical Immunology 2005;115(2):S3. [Google Scholar]
Morice 2005a {published data only}
- Morice AH, Osmanliev D, Arheden L, Beckman O. Therapeutic equivalence of a novel budesonide/formoterol pMDI versus budesonide/formoterol Turbuhaler in adolescents and adults with asthma. Journal of Allergy and Clinical Immunology 2005;115(2):S2. [Google Scholar]
Morjaria 2019 {published data only}
- Morjaria JB, Rigby AS, Morice AH. Symptoms and exacerbations in asthma: an apparent paradox? Therapeutic Advances in Chronic Disease 2019;10:2040622319884387. [DOI: 10.1177/2040622319884387] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nakazawa 1994 {published data only}
- Nakazawa T, Kobayashi S, Kondoh A. Clinical usefulness of combined inhalation method using SLI and BDI in the treatment of adults asthma. Japanese Journal of Chest Diseases 1994;53(9):801-8. [Google Scholar]
Nathan 2010 {published data only}
- Nathan R, Pearlman D, Nolte H, Nayak A. Efficacy and safety of combined mometasone furoate/formoterol 200/10?g in persistent asthmatics. In: European Respiratory Society Annual Congress, Barcelona, Spain, September 18-22. 2010:[E5489].
NCT00118690 2005 {published data only}
- NCT00118690. A study measuring asthma control in pediatric and adolescent subjects whose asthma is worsened by activity or exercise [A stratified, multicenter, randomized, double-blind, parallel group, 4-week comparison of fluticasone propionate/salmeterol DISKUS combination product 100/50mcg bid versus fluticasone propionate DISKUS 100mcg bid in pediatric and adolescent subjects with activity-induced bronchospasm]. clinicaltrials.gov/show/NCT00118690 (first received 12 July 2005).
NCT00118716 2005 {published data only}
- NCT00118716. A study measuring asthma control in pediatric and adolescent subjects whose asthma is worsened by activity or exercise [A stratified, multicenter, randomized, double-blind, parallel group, 4-week comparison of fluticasone propionate/salmeterol DISKUS combination product 100/50 mcg bid versus fluticasone propionate DISKUS 100 mcg bid in pediatric and adolescent subjects with activity-induced bronchospasm]. clinicaltrials.gov/show/NCT00118716 (first received 12 July 2005).
NCT00169546 2005 {published data only}
- NCT00169546. Study in airway physiology in children seretide diskus ® inhaler and flixotide® inhaler are trademarks of gsk group of companies [Randomised, double-blind parallel group study to assess the bronchodilative and bronchoprotective properties of SERETIDE DISKUS ® inhlaer 50/100mcg twice daily vs. FLIXOTIDE® inhaler 200mcg twice daily.]. clinicaltrials.gov/show/NCT00169546 (first received 15 September 2005).
NCT00197106 2005 {published data only}
- NCT00197106. Treatment of symptomatic asthma in children [A multicentre, randomised, double-blind, parallel group study to compare the efficacy and safety of salmeterol/fluticasone propionate combination product (Seretide®) 50/100 mcg with fluticasone propionate (Flixotide® ) 200 mcg, both delivered twice daily via the DISKUS inhaler, in the treatment of children aged 6-12 years with symptomatic asthma]. clinicaltrials.gov/show/nct00197106 (first received 20 September 2005).
NCT00235911 2005 {published data only}
- NCT00235911. Symbicort single inhaler therapy for asthma in a general practice setting [Effects of symbicort single inhaler therapy on bronchial hyper responsiveness, asthma control and safety in Mild to Moderate asthmatics in general practice, compared to usual care therapy]. clinicaltrials.gov/show/nct00235911 (first received 12 October 2005).
NCT00238784 2005 {published data only}
- NCT00238784. SOLO-Symbicort® in the treatment of persistent asthma in adolescents & adults [A comparison of Symbicort® single inhaler therapy (Symbicort® 200 Turbuhaler® 1 inhalation b.i.d. plus as needed) & conventional best practice for the treatment of persistent asthma in adolescents & adults-a 26-week, randomised, open-label, parallel group, multicentre study]. clinicaltrials.gov/show/nct00238784 (first received 14 October 2005).
NCT00242411 2005 {published data only}
- NCT00242411. MONO: symbicort® single inhaler therapy and conventional best standard treatment for the treatment of persistent asthma in adolescents and adults [A comparison of the efficacy of Symbicort® single inhaler therapy (Symbicort Turbuhaler® 160/4.5 mg 1 inhalation b.i.d. plus as-needed) and conventional best standard treatment for the treatment of persistent asthma in adolescents and adults. A randomized, open, parallel-group, multicentre 26-weeks study]. clinicaltrials.gov/show/NCT00242411 (first received 20 October 2005).
NCT00244608 2005 {published data only}
- NCT00244608. A comparison of the control of asthma provided by symbicort® turbuhaler® versus symbicort® turbuhaler® plus pulmicort® turbuhaler® plus terbutaline turbuhaler® [A comparison of the inflammatory control of asthma provided by one inhalation of Symbicort® Turbuhaler® 160/4.5 µg/inhalation b.i.d. plus as-needed versus one inhalation of Symbicort® Turbuhaler® 320/9 µg/inhalation b.i.d. + one inhalation of Pulmicort® Turbuhaler® 400 µg/dose b.i.d. plus terbutaline Turbuhaler® 0.4 mg/Inhalation As-needed. A 12-month, randomised, double-blind, parallel-group, active controlled, multinational, phase IIIB study in adult patients with asthma, EOS]. clinicaltrials.gov/show/NCT00244608 (first received 27 October 2005).
NCT00252824 2005 {published data only}
- NCT00252824. STYLE - symbicort single inhaler therapy vs. conventional therapy in treatment of persistent asthma [A comparison of the efficacy of Symbicort® single inhaler therapy (Symbicort Turbuhaler® 160/4.5 mg 1 inhalation b.i.d. plus as-needed) and conventional best practice for the treatment of persistent asthma in adolescents and adults - a 26 weeks, randomised, open-label, parallel-group, multicentre study]. www.clinicaltrials.gov/ct/show/nct00252824 (first received 15 November 2005).
NCT00259792 2005 {published data only}
- NCT00259792. SYMPHONIE - a comparison of symbicort single inhaler and conventional best practice for the treatment of persistent asthma in adolescents and adults [A comparison of Symbicort single inhaler and conventional best practice for the treatment of persistent asthma in adolescents and adults - a 26-week, randomised, open, parallel group multicentre study]. clinicaltrials.gov/show/nct00259792 (first received 1 December 2005).
NCT00273026 2006 {published data only}
- NCT00273026. Study In asthma control [An open-label, multi-centre, randomized, parallel group clinical effectiveness study to determine the level of asthma control in adolescent and adult patients with ADVAIR versus usual care for 24 weeks]. clinicaltrials.gov/show/NCT00273026 (first received 9 January 2006).
NCT00288379 2006 {published data only}
- NCT00288379. SMILDA - Symbicort®Turbuhaler® allergan challenge study in allergic patients with mild asthma [A comparative, placebo-controlled, double blind, double dummy, cross-over, single centre, phase IIIb study between formoterol alone (Oxis® Turbuhaler® 4.5 µg) and the fixed combination of formoterol and budesonide (Symbicort® Turbuhaler®160/4.5 µg) on airway responsiveness and airway inflammation induced by repeated low-dose allergen challenge in allergic patients with mild asthma]. clinicaltrials.gov/show/NCT00288379 (first received 8 February 2006).
NCT00291382 2006 {published data only}
- NCT00291382. Airway hyper-responsiveness study in asthma using salmeterol/fluticasone propionate combination product [A multicentre, stratified, randomised, double blind, parallel group trial to evaluate whether a treatment strategy based on aiming for total control results in better AHR than a treatment strategy based on maintaining well control]. clinicaltrials.gov/show/NCT00291382 (first received 14 February 2006).
NCT00319306 2006 {published data only}
- NCT00319306. Real life effectiveness in asthma of symbicort single inhaler therapy (RELEASE) [Real life effectiveness in asthma of Symbicort single inhaler therapy]. Https://clinicaltrials.gov/show/nct00319306 (first received 27 April 2006).
NCT00326053 2006 {published data only}
- NCT00326053. Prevention of asthma relapse after discharge from emergency (PARADE) [A comparison of budesonide/formoterol Turbuhaler® 160/4.5 µg 2 inhalations bid plus as needed to budesonide Turbuhaler® 320 µg 2 inhalations bid plus Terbutaline Turbuhaler® 0.4 mg as needed for the prevention of asthma relapse]. clinicaltrials.gov/show/NCT00326053 (first received 16 May 2006).
NCT00381485 2006 {published data only}
- NCT00381485. Effects of mometasone furoate/formoterol combination versus mometasone furoate alone in persistent asthmatics (study P04431AM2)(COMPLETED) [A 12-week efficacy and safety study of two doses of mometasone furoate/formoterol combination formulation compared with mometasone furoate monotherapy, in persistent asthmatics previously treated with high-dose inhaled glucocorticosteroids]. clinicaltrials.gov/show/nct00381485 (first received 27 September 2006).
NCT00382889 2006 {published data only}
- NCT00382889. As needed beclomethasone/salbutamol combination in single inhaler for mild persistent asthma [Multinational, double blind, randomised, parallel group study on the therapeutic efficacy and safety of beclomethasone dipropionate 250 mg combined with salbutamol 100 mg in the treatment of patients with mild persistent asthma]. clinicaltrials.gov/show/nct00382889 (first received 2 October 2006).
NCT00385593 2012 {published data only}
- NCT00385593. Symbicort single inhaler therapy vs conventional best practice for the treatment of persistent asthma in adults [A comparison of Symbicort single inhaler therapy (Symbicort Turbuhaler 160/4.5 micrograms, 1 inhalation b.i.d. plus as needed) and conventional best practice for the treatment of persistent asthma in adults - a 26-week, randomised, open-label, parallel-group, multicentre study. Study SPAIN]. clinicaltrials.gov/ct2/show/nct00385593 (first received 9 October 2006).
NCT00394121 2006 {published data only}
- NCT00394121. New combination inhaler (flutiform hfa mdi 100/10 µg and 250/10 µg) in patients with asthma [Long-term open-label safety study with SkyePharma FlutiForm HFA pMDI (100/10 µg and 250/10 µg) in adult and adolescent patients with asthma]. clinicaltrials.gov/show/nct00394121 (first received 31 October 2006).
NCT00419757 2007 {published data only}
- NCT00419757. An efficacy study comparing SYMBICORT® pressurised metered dose inhaler (pMDI) with budesonide hydrofluoroalkanes (HFA) pMDI, in Hispanic subjects with ICS dependent asthma [A 12-week, randomised, double blind, active-controlled, multi-centre, phase IIIB study comparing the efficacy and safety of SYMBICORT® pMDI 160/4.5 mg x 2 actuations twice daily versus budesonide HFA pMDI 160 mg x 2 actuations twice daily, in adult/adolescent (> 12 Yrs) Hispanic subjects with asthma]. clinicaltrials.gov/ct2/show/study/nct00419757 (first received 9 January 2007).
NCT00424008 2007 {published data only}
- NCT00424008. Study of inhaled glucocorticosteroids/long-acting bronchodilator drugs in subjects with asthma that have been taking inhaled glucocorticosteroids (study p04705am1) [A 52-week efficacy and safety non-inferiority study of fluticasone propionate/salmeterol 250/50mcg bid delivered by dry powder inhaler (Diskus) versus mometasone furoate/formoterol fumarate 200/10mcg bid delivered by pressurized metered-dose inhaler in persistent asthmatics previously treated with medium doses of inhaled glucocorticosteroids]. clinicaltrials.gov/show/NCT00424008 (first received 18 January 2007).
NCT00441441 2007 {published data only}
- NCT00441441. A 12-week study to assess the safety of fluticasone propionate/salmeterol 100/50 hydrofluoroalkane (hfa) versus fluticasone propionate 100 hfa in children with asthma [A randomized, double-blind, parallel group study evaluating the safety of fluticasone propionate/salmeterol 100/50mcg hfa (2 inhalations of 50/25mcg) twice daily compared with fluticasone propionate 100mcg hfa (2 inhalations of 50mcg) twice daily in subjects 4-11 years of age with persistent asthma]. clinicaltrials.gov/show/nct00441441 (first received 1 March 2007).
NCT00461812 2007 {published data only}
- NCT00461812. A comparison of mometasone to advair in patients with milder persistent asthma [A single-blind, randomized, positive-controlled study to compare monotherapy with an inhaled corticosteroid (mometasone) to combination therapy with an inhaled corticosteroid + a long-acting bronchodilator (Advair) in patients with milder persistent asthma]. clinicaltrials.gov/show/NCT00461812 (first received 18 April 2007).
NCT00475813 2007 {published data only}
- NCT00475813. Study of FLUTIFORM® VS Seretide® in paediatric subjects with asthma. clinicaltrials.gov/show/NCT00475813 (first received 21 May 2007).
NCT00479739 2007 {published data only}
- NCT00479739. CONCEPT: a 1-year comparison of a stable dose of seretide® inhaler with an adjustable maintenance dose of symbicort® inhaler. seretide® inhaler is a trademark of gsk group of companies. symbicort® inhaler is a trademark of astra zeneca [Randomised, double-blind, double-dummy, 52-week, parallel group study of a standard dosing regimen with salmeterol/fluticasone propionate50/250 twice daily diskus versus a symptom-driven, variable dosing regimen with formoterol/budesonide combination 4.5/160 in adult asthmatics]. clinicaltrials.gov/show/nct00479739 (first received 28 May 2007).
NCT00497237 2007 {published data only}
- NCT00497237. Clinical trial of the efficacy and safety of beclomethasone dipropionate plus formoterol vs fluticasone propionate plus salmeterol in the 6 months step down treatment of asthma (FORTE). [Prospective, randomised, open-label, multicentre, active drug controlled, parallel group design clinical trial of the efficacy and safety of beclomethasone dipropionate 400 mcg + formoterol 24 mcg pmdi via hfa-134a (foster™) vs. fluticasone propionate 500 mcg + salmeterol xinafoate 100 mcg dpi (seretide diskus®) in the 6 months stepdown treatment of adult patients with controlled asthma]. clinicaltrials.gov/ct2/show/NCT00497237 (first received 6 July 2007).
NCT00528723 2007 {published data only}
- NCT00528723. Efficacy and tolerability of beclomethasone plus salbutamol in hfa pmdi fixed combination vs beclomethasone plus salbutamol in cfc pmdi fixed combination in a 12-week treatment period of adult patients with uncontrolled asthma [Multicentre, multinational, randomised, double blind, double dummy, active drug controlled, parallel group study design clinical trial of the efficacy and tolerability of beclomethasone dipropionate 250 mcg plus salbutamol 100 mcg in hfa pMDI fixed combination vs. beclomethasone dipropionate 250 mcg plus salbutamol 100 mcg in CFC pMDI (Clenil® Compositum 250) fixed combination in a 12-week treatment period of adult patients with uncontrolled asthma]. clinicaltrials.gov/show/NCT00528723 (first received 12 September 2007).
NCT00628758 2008 {published data only}
- NCT00628758. A comparison of symbicort® single inhaler therapy and conventional best practice for the treatment of persistent asthma (PASSION) [A comparison of Symbicort® single inhaler therapy (Symbicort Turbuhaler® 160/4.5mg, 1 inhalation two times a day (b.i.d.) plus as needed) and conventional best practice for the treatment of persistent asthma in adults a -26-week, randomized, open-label, parallel-group, multicentre Study]. clinicaltrials.gov/show/NCT00628758 (first received 5 March 2008).
NCT00646529 2008 {published data only}
- NCT00646529. Long-term safety of symbicort in asthmatic children - SAPLING [A six month, randomized, open-label, safety study of Symbicort (160/4.5mcg) compared to pulmicort turbuhaler in asthmatic children aged six to eleven years - SAPLING]. https://clinicaltrials.gov/show/NCT00646529 (first received 28 March 2008).
NCT00651547 2008 {published data only}
- NCT00651547. Symbicort in asthmatic children - SEEDLING [A 12 week randomized, double-blind, double-dummy, placebo-controlled trial of Symbicort TM (40/4.5 Mcg) versus its mono-products (budesonide and formoterol) in asthmatic children aged six to eleven years - SEEDLING 40/4.5]. clinicaltrials.gov/show/NCT00651547 (first received 3 April 2008).
NCT00651651 2008 {published data only}
- NCT00651651. Efficacy of symbicort versus Its monocomponents - SPRUCE 80/4.5 [A 12 week randomized, double-blind, double-dummy, placebo-controlled trial of Symbicort TM (160/4.5mcg) versus its mono-products (budesonide and formoterol) in children (at least 6 years of age) and adults with asthma-SPRUCE 80/4.5]. clinicaltrials.gov/show/NCT00651651 (first received 3 April 2008).
NCT00651768 2008 {published data only}
- NCT00651768. Titratable dosing in moderate to severe asthmatics [A 52 wk randomized, doubleb lind, single dummy, parallel group multicenter phase 3 study comparing the long term safety of Symbicort pMDI 4x160/4.5mcg bid to SymbicortpMDI 2x160/4.5mcg bid & budesonide HFA pMDI 4x160mcg bid in adult and adolescent subjects with asthma]. clinicaltrials.gov/show/NCT00651768 (first received 3 April 2008).
NCT00652002 2008 {published data only}
- NCT00652002. Efficacy of symbicort versus its monocomponents - SPRUCE 160/4.5 [A 12 week, randomized, double-blind, double-dummy, placebo-controlled trial of Symbicort TM (160/4.5mcg) versus its mono-products (budesonide and formoterol) in adolescents (at least 12 years of age) and adults with asthma - SPRUCE 160/4.5]. clinicaltrials.gov/show/NCT00652002 (first received 3 April 2008).
NCT00658255 2008 {published data only}
- NCT00658255. Relative bronchodilating effects of formoterol when administered via symbicort pressurized metered-dose inhaler (pmdi) or oxis turbuhaler [A randomized, multicenter, open-label, active-controlled, single-dose, 5-period, incomplete block, cross-over study to evaluate the relative bronchodilating effects of formoterol when administered via Symbicort pMDI or Oxis Turbuhaler to adults with stable asthma]. clinicaltrials.gov/show/NCT00658255 (first received 14 April 2008).
NCT00861926 2009 {published data only}
- NCT00861926. Study comparing foster efficacy maintenance and reliever versus foster maintenance + salbutamol reliever in asthmatics [48-week,multinational,randomized,double-blind,2-parallel groups,comparing the efficacy of foster for maintenance and reliever versus fixed-dose foster for maintenance plus salbutamol as reliever in asthmatics >=18 years of age]. clinicaltrials.gov/show/nct00861926 (first received 16 March 2009).
NCT00901368 2009 {published data only}
- NCT00901368. FACTO study (Foster® As Complete Treatment Option) (FACTO) [A phase 4, multinational, multicentre, double blind, double dummy, randomized, parallel group, controlled clinical study of fixed combination beclomethasone dipropionate 100 µg plus formoterol fumarate 6 µg pmdi with hfa-134a propellant (chf1535, foster®) versus fluticasone 250 µg plus salmeterol 50 µg dpi (seretide® diskus®) as maintenance treatment in controlled asthmatic patients.]. clinicaltrials.gov/show/NCT00901368 (first received 13 May 2009).
NCT01070888 2010 {published data only}
- NCT01070888. Trial on the effect of budesonide/formoterol and inhaled budesonide alone on exercise-induced asthma [A randomized, double-blind, double dummy crossover trial on the effect of budesonide/formoterol and inhaled budesonide alone on exercise-induced asthma in patients with persistent asthma]. clinicaltrials.gov/show/nct01070888 (first received 18 Feb 2010).
NCT01444430 2011 {published data only}
- NCT01444430. A 6 month safety study comparing symbicort with inhaled corticosteroid only in asthmatic adults and adolescents [A 26 week, randomized, double-blind, parallel-group, active controlled, multicenter, multinational safety study evaluating the risk of serious asthma-related events during treatment With Symbicort®, a fixed combination of inhaled corticosteroid (ICS) (budesonide) and a long acting β2-agonist (LABA) (formoterol) as compared to treatment with ICS (budesonide) alone in adult and adolescent (≥12 years of age) patients with asthma]. clinicaltrials.gov/show/nct01444430 (first received 30 September 2011).
NCT01471340 2011 {published data only}
- NCT01471340. A serious asthma outcome study with mometasone furoate/formoterol versus mometasone furoate in asthmatics 12 years and over (P06241 AM3) (SPIRO) [A 26-week randomized, double-blinded, active controlled study comparing the safety of mometasone furoate/formoterol fumarate mdi fixed dose combination versus mometasone furoate mdi monotherapy in adolescents and adults with persistent asthma (protocol no. P06241 also known as P202)]. clinicaltrials.gov/show/nct01471340 (first received 16 November 2011).
NCT01566149 2012 {published data only}
- NCT01566149. Study of mometasone furoate/formoterol fumarate (MF/F) metered dose inhaler (MDI) in adolescents & adults with persistent asthma (P08212) [An open-label study to assess the safety and tolerability of Zenhale® (a fixed-dose combination of mometasone furoate/formoterol fumarate delivered by metered dose Inhaler) in 40 subjects with persistent asthma (protocol no. 206-00 [P08212])]. clinicaltrials.gov/show/NCT01566149 (first received 29 March 2012).
NCT01676987 2012 {published data only}
- NCT01676987. Evaluation of the efficacy and safety of a fixed-dose, single-capsule budesonide-formoterol combination in uncontrolled asthma (Ach-ALN) [Evaluation of the efficacy and safety of a fixed-dose, single-capsule budesonide-formoterol combination in uncontrolled asthma: a randomized, double-blind, multicenter, controlled clinical trial]. clinicaltrials.gov/show/nct01676987 (first received 31 August 2012). [DOI] [PubMed]
NCT02491970 2015 {published data only}
- NCT02491970. Small airway function of fluticasone/formoterol (flutiform®) and fluticasone/salmeterol (RECONFFIRM) [A single-blind, randomized, active-controlled, multi-center and phase IV study to evaluate the small airway parameters of fluticasone/formoterol (Flutiform®) compared to fluticasone/salmeterol in asthma patients]. clinicaltrials.gov/show/NCT02491970 (first received 8 July 2015).
NCT02741271 2016 {published data only}
- NCT02741271. Study of efficacy and long-term safety of mometasone furoate in combination with formoterol fumarate versus mometasone furoate in children (5 to 11 years of age) with persistent asthma (MK-0887A-087) [A phase III, randomized, active-controlled, parallel-group clinical trial to study the efficacy and long-term safety of mometasone furoate/formoterol fumarate (MF/F, MK-0887A [SCH418131]), compared with mometasone furoate (MF, MK-0887 [SCH032088]), in children with persistent asthma]. clinicaltrials.gov/show/NCT02741271 (first received 18 April 2016).
NCT03015259 2017 {published data only}
- NCT03015259. Randomized, placebo-controlled, multi-dose, study comparing budesonide/formoterol to symbicort® in asthmatic patients [Randomized, single blind, parallel group, placebo controlled, multidose study comparing the therapeutic equivalence of a 3M budesonide/formoterol fumarate inhaler and a Symbicort® reference inhaler in adult subjects with asthma]. clinicaltrials.gov/show/nct03015259 (first received 10 January 2017).
NCT03924635 2019 {published data only}
- NCT03924635. An exploratory study to characterise changes in airway inflammation, symptoms, lung function and reliever use in adult asthma patients [A 24-week randomised exploratory open-label study aiming to characterise changes in airway inflammation, symptoms, lung function, and reliever use in asthma patients using SABA (aalbutamol) or anti-inflammatory reliever (SYMBICORT®) as rescue medication in addition to SYMBICORT as daily asthma controller]. clinicaltrials.gov/show/nct03924635 (first received 23 April 2019).
NCT04171180 2019 {published data only}
- NCT04171180. The efficacy of budesonide/formoterol in cough variant asthma [The efficacy of budesonide/formoterol in cough variant asthma -- a multi-center randomized, controlled clinical trial]. clinicaltrials.gov/show/NCT04171180 (first received 20 November 2019).
Nelson 2000 {published data only}
- Nelson HS, Baitinger L, Scott C, House K, Payne E, Shah T. Salmeterol/fluticasone propionate (50/100µg dose) non-CFC metered dose inhaler is safe and effective in patients with asthma using short-acting a²-agonists alone. European Respiratory Journal 2000;16:53s. [Google Scholar]
Nelson 2007 {published data only}
- Nelson H, Murphy K, Parasuraman B, Boggs R, Miller C, O' Dowd L. Budesonide and formoterol in one metered dose inhaled improves health related quality of life in adults with mild to moderate persistent asthma previously treated with inhaled corticosteroids. Journal of Allergy and Clinical Immunology 2007;119(1):S246 [964]. [Google Scholar]
Ness 1993 {published data only}
- Ness RB. Bronchodilators added to inhaled corticosteroids. Annals of Internal Medicine 1993;118(6):48. [Google Scholar]
O'Brien 2007 {published data only}
- O'Brien CD, Peters SP, Prenner BM, Martin P. Long-term safety of budesonide/formoterol pressurized metered-dose inhaler (BUD/FM pMDI) in asthma patients: adverse events and asthma exacerbations. In: American Thoracic Society International Conference; 2007 May 18-23; San Francisco. 2007:Poster #L57.
O'Byrne 2001 {published data only}
- O'Byrne P, Barnes P, Rodriguez-Roisin R, Runnerstrom E, Standstrom T, Svensson K, et al. Low dose inhaled budesonide with and without formoterol in steroid free patients with mild persistent asthma. American Journal of Respiratory and Critical Care Medicine 2001;163(5):A862. [DOI] [PubMed] [Google Scholar]
- O'Byrne PM, Barnes PJ, Rodriguez-Roisin R, Sandtrom T, Tattersfield AE, Runnerstrom EM, et al. Addition of formoterol Turbuhaler® to budesonide Tubuhaler® is safe and well tolerated in the long-term treatment of mild asthma: results from the OPTIMA trial. European Respiratory Journal 2001;18:330s. [Google Scholar]
O'Byrne 2004 {published data only}
- O'Byrne PM, Godard P, Pistolesi M, Ekstrom T. Single inhaler therapy with budesonide/formoterol improves asthma control compared with fixed dosing with budesonide/formoterol or a higher dose of budesonide alone. In: American Thoracic Society 100th international conference; 2004 May 21-26; Orlando. 2004:A37 Poster J93.
O'Byrne 2005 {published data only}
- O'Byrne PM, Bisgaard H, Godard PP, Pistolesi M, Palmqvist M, Zhu Y, et al. Budesonide/formoterol combination therapy as both maintenance and reliever medication in asthma. American Journal of Respiratory and Critical Care Medicine 2005;171(2):129-36. [DOI] [PubMed] [Google Scholar]
O'Connor 2010 {published data only}
- O'Connor RD, Patrick DL, Parasuraman B, Martin P, Goldman M. Comparison of patient-reported outcomes during treatment with adjustable- and fixed-dose budesonide/formoterol pressurized metered-dose inhaler versus fixed-dose fluticasone propionate/salmeterol dry powder inhaler in patients with asthma. Journal of Asthma 2010;47(2):217-23. [DOI] [PubMed] [Google Scholar]
Obodo 2009 {published data only}
- Obodo O, Ige O, Chukwu C. Scientific rationale for using a single inhaler for asthma control by comparison of the effectiveness and safety of formoterol/budesonide turbuhaler as physician-guided adjustable maintenance dosing regimen versus formoterol/budesonide given as fixed dose of twice daily therapy in the management of bronchial asthma. In: European Respiratory Society 19th Annual Congress; 2009 Sep 12-15; Vienna. 2009:[1968].
Olsson 2002 {published data only}
- Olsson P, Stallberg B, Ekstrom T, Lindarck N, Jorgensen LA. Adjustable maintenance treatment of asthma with budesonide and formoterol in a single inhaler. In: European Respiratory Society 12th Annual Congress; 2002 Sep 14-18; Stockholm. 2002:P2451.
Papi 2013 {published data only}
- Papi A, Corradi M, Pigeon-Francisco C, Baronio R, Siergiejko Z, Petruzzelli S, et al. Beclometasone-formoterol as maintenance and reliever treatment in patients with asthma: a double-blind, randomised controlled trial. The Lancet Respiratory Medicine 2013;1(1):23-31. [DOI] [PubMed] [Google Scholar]
Patel 2013 {published data only}
- Patel M, Pilcher J, Pritchard A, Perrin K, Travers J, Shaw D, et al. Efficacy and safety of maintenance and reliever combination budesonide-formoterol inhaler in patients with asthma at risk of severe exacerbations: a randomised controlled trial. The Lancet Respiratory Medicine 2013;1(1):32-42. [DOI] [PubMed] [Google Scholar]
Pauwels 1996 {published data only}
- Pauwels RA, Hargreave FE, Camus P, Bukoski M, Stahl E. A 1-year comparison of turbuhaler vs pressurized metered-dose inhaler in asthmatic patients. Chest 1996;110(1):53-7. [DOI] [PubMed] [Google Scholar]
Pauwels 1998 {published data only}
- Pauwels R. Additive effects of inhaled formoterol and budesonide in reducing asthma exacerbations. Allergy 1998;53(42):20-3. [DOI] [PubMed] [Google Scholar]
Pauwels 2004 {published data only}
- Pauwels R, Bateman E, Boushey H, Bousquet J, Busse W, Clark T, et al. Can total control of asthma be achieved?: the results of the GOAL study. Journal of Allergy and Clinical Immunology 2004;113(2):114s. [Google Scholar]
Pearlman 2000 {published data only}
- Pearlman D, Baitinger L, Woodring A, Prillaman B, House K, Shah T. Salmeterol 50mcg/fluticasone propionate 250mcg diskus combination product demonstrates improvements in lung function regardless of baseline corticosteroid therapy. American Journal of Respiratory and Critical Care Medicine 2000;161:A196. [DOI] [PubMed] [Google Scholar]
Pedersen 2006 {published data only}
- Pedersen S. Budesonide plus formoterol for reliever therapy in asthma. Lancet 2006;368:707-8. [DOI] [PubMed] [Google Scholar]
Peters 2007 {published data only}
- Peters M, Bousquet J. Episodic high reliever use with budesonide/formoterol; maintenance and reliever therapy confers added protection against asthma exacerbations. European Respiratory Journal 2007;30:615s [P3613]. [Google Scholar]
Pieters 1998 {published data only}
- Pieters WR, Steinmetz KO, Aubier M, Johnson L, Gomez E, Bogolubov M. Effectiveness of a new salmeterol/fluticasone propionate (50/500µg) combination inhaler in patients with reversible airways obstruction. European Respiratory Journal 1998;12:35S. [Google Scholar]
Pilcher 2013 {published data only}
- Pilcher J, Patel M, Smith A, Davies C, Harwood M, Weatherall M, et al. Single budesonide/formoterol inhaler as maintenance and reliever therapy is beneficial in Maori asthma. Respirology 2013;18:44 [P027]. [Google Scholar]
Pilcher 2016 {published data only}
- Pilcher J, Patel M, Reddel HK, Pritchard A, Black P, Shaw D, et al. Effect of smoking status on the efficacy of the SMART regimen in high risk asthma. Respirology 2016;21(5):858-66. [DOI] [PubMed] [Google Scholar]
Plit 1984 {published data only}
- Plit M, Pover GM. Assessment of a new combination inhaler containing salbutamol and beclomethasone dipropionate in the management of asthmatic patients. South African Medical Journal 1984;65(19):758-62. [PubMed] [Google Scholar]
Pohl 2004 {published data only}
- Pohl W, Vetter N, Zwick H, Hrubbs W. Budesonide/formoterol adjustable maintenance dosing (AMD) improves health related quality of life (HRQL) compared with high dose budesonide (AMD). European Respiratory Journal 2004;24:311s. [Google Scholar]
Pover 1986 {published data only}
- Pover GM, Greger G, Kaspar P. Comparison of the effects of sequential or simultaneous administration of salbutamol and beclomethasone dipropionate. Respiration 1986;50(2):83-7. [DOI] [PubMed] [Google Scholar]
Prenner 2007 {published data only}
- Prenner BM, Peters SP, Martin P, O'Brien CD. Long-term control of asthma symptoms with budesonide/formoterol pressurized metered-dose inhaler (BUD/FM pMDI) versus BUD pMDI. In: American Thoracic Society International Conference; 2007 May 18-23; San Francisco. 2007:Poster #L67.
Price 2003 {published data only}
- Price D, Haughney J, Rosen JP, Morrison K. Switching to symbicort® from beclomethasone dipropionate (BDP) with or without salmeterol significantly improved symptom severity in patients with moderate asthma. In: American Thoracic Society 99th International Conference; 2003 May 16-21; Seattle. 2003:D034 Poster C40.
Price 2005 {published data only}
- Price D, Williams A, Yoxall S, Gauthier A. Quality of life of stable dose treatment with salmeterol/fluticasone (SFC) compared with adjustable maintenance dosing (AMD) with formoterol/budesonide (FBC). European Respiratory Journal 2005;26:1720. [Google Scholar]
Rabe 2004a {published data only}
- Rabe KF, Pizzichini E, Stalberg B, Romero S, Balanzat A, Soerensen T, et al. Single inhaler therapy with budesonide/formeterol provides superior asthma control compared with fixed dosing with budesonide plus terbutaline as needed. Journal of Allergy and Clinical Immunology 2004;113(2):S116. [Google Scholar]
Rabe 2006 {published data only}
- Rabe KF, Pizzichini E, Stallberg B, Romero S, Balanzat AM, Atienza T, et al. Budesonide/formoterol in a single inhaler for maintenance and relief in mild-to-moderate asthma: a randomized, double-blind trial. Chest 2006;129(2):246-56. [DOI] [PubMed] [Google Scholar]
Remington 2002 {published data only}
- Remington TL, Heaberlin A, DiGiovine B. Combined budesonide/formoterol turbuhaler treatment of asthma. Annals of Pharmacotherapy 2002;36(12):1918-28. [DOI] [PubMed] [Google Scholar]
Riemersma 2012 {published data only}
- Riemersma Roland A, Postma D, Molen T. Budesonide/formoterol maintenance and reliever therapy in primary care asthma management: effects on bronchial hyperresponsiveness and asthma control. Primary Care Respiratory Journal 2012;21(1):50-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rooklin 2001 {published data only}
- Rooklin A, Elkayam D, Weiler J, Windom H, Schoaf L, Scott C, et al. The fluticasone propionate/salmeterol HFA MDI is significantly more efficacious in treating asthma than placebo HFA MDI, fluticasone propionate CFC MDI or salmeterol CFC MDI. Journal of Allergy and Clinicial Immunology 2001;107(2):S100. [Google Scholar]
Rosenhall 2001 {published data only}
- Rosenhall L, Stahl E, Heinig JH, Lindqvist A, Leegard J, Bergqvist PB. Health-related quality of life and asthma control in patients treated with budesonide and formoterol in a single inhaler. European Respiratory Journal 2001;18:46s. [Google Scholar]
Rosenhall 2001a {published data only}
- Rosenhall L, Heinig JH, Lindqvist A, Leegard J, Bergqvist PB. Budesonide and formoterol in a single inhaler is safe and effective in the treatment of asthma. European Respiratory Journal 2001;18:159s. [Google Scholar]
Saito 2012 {published data only}
- Saito T, Hasunuma T. Safety and tolerability of high-dose budesonide/formoterol via Turbuhaler in Japanese patients with asthma: a randomized, double-blind, crossover, active comparator-controlled, phase III study. Clinical Drug Investigation 2012;32(1):51-61. [DOI] [PubMed] [Google Scholar]
SAM40027 2004 {published data only}
- SAM40027. Gaining optimal asthma controL (GOAL): a multi-centre, stratified, randomised, double-blind, parallel-group, step-up comparison of the level of asthma control achieved with salmeterol/fluticasone propionate combination DISKUS (ACCUHALER) dry powder inhaler compared with fluticasone propionate DISKUS (ACCUHALER) alone in adults and adolescents. www.gsk-clinicalstudyregister.com/study/SAM40027#rs (first received 21 December 2000).
Sanguinetti 2003 {published data only}
- Sanguinetti CM, Canonica GW, Moretti AM, Mangrella M. Adjustable maintenance dosing with budesonide/formoterol provides effective asthma symptom control at a lower than average dose than fixed dosing: results of a study in Italy [Abstract]. European Respiratory Journal 2003;22:P2641. [Google Scholar]
SAS30013 2004 {published data only}
- SAS30013. A study to compare the long term effects on airway inflammation of Seretide versus Flixotide in adult subjects with asthma. www.gsk-clinicalstudyregister.com/study/SAS30013 (first received 1 March 2004).
Schmidtmann 2005 {published data only}
- Schmidtmann S, Malek R, Trautmann M, SAM30020 Study Group. Once daily inhalation of salmeterol-fluticasone (50/100Aµg) Diskus for mild asthma - a randomised study in comparison with as-needed inhalation of reproterol-DNCG combination. Pneumologie 2005;59:S1, Poster 184. [Google Scholar]
Schreurs 1998 {published data only}
- Schreurs AJ, Noord JA, Mulder PG. Fluticasone propionate and salmeterol xinafoate in patients with mild to moderate asthma. European Respiratory Journal 1998;12:19s. [Google Scholar]
Scicchitano 2004 {published data only}
- Scicchitano R, Aalbers R, Ukena D, Manjra AI, Fouquet L, Centanni S, et al. Single inhaler therapy with budesonide/formeterol reduces the risk of severe exacerbations compared with budesonide plus terbutaline as needed in patients with asthma. Journal of Allergy and Clinical Immunology 2004;113(2):S116. [Google Scholar]
SD‐039‐0349 1999 {published data only}
- SD-039-0349. Efficacy and safety of a fixed combination of budesonide/formoterol Turbuhaler® in inhaled steroid-using asthmatic adults. astrazenecagrouptrials.pharmacm.com/ST/Submission/View?id=1020 (first received 1 October 1998).
SD‐039‐0618 2005 {published data only}
- SD-039-0618. Efficacy of symbicort turbuhaler® compared with fluticasone diskus in asthmatic patients. https://astrazenecagrouptrials.pharmacm.com/ST/Submission/View?id=1017 (first received 1 October 1999).
SD‐039‐0667 {published data only}
- SD-039-0667. Efficacy and safety of symbicort® turbuhaler® AS single therapy in patients with mild to moderate asthma - STEAM (SD-039-0667). astrazenecagrouptrials.pharmacm.com/ST/Submission/View?id=1011 (first received 1 January 200 1 ).
Sears 2003 {published data only}
- Sears MR, McIvor A, Becker A, Fitzgerald M, Boulet LP, Ernst P, et al. Budesonide/formoterol adjustable maintenance dosing effectively improves asthma symptom severity: a multicentre Canadian study. European Respiratory Journal 2003;22:P1695. [DOI] [PubMed] [Google Scholar]
Sergio 2012 {published data only}
- Sergio F, Francisco C, Muraro A, Kanniess F. Beclometasone/formoterol administered via extrafine dry powder inhaler in controlled asthmatic patients: Comparison with pMDI and beclometasone monotherapy [Abstract]. European Respiratory Journal 2012;40:314s. [Google Scholar]
Serrier 2003 {published data only}
- Serrier P, Roche N, Pello J Y, Larguier J S, Mezzi K. Control of asthma by treatment with inhaled corticosteroids and prolonged action beta 2-agonists in free or fixed combination. Results of the ALISE study. Presse Medicale 2003;32(11):493-7. [PubMed] [Google Scholar]
Shah 2007 {published data only}
- Shah SR, Busse WW, Somerville L, Martin P, Goldman M. Asthma control with adjustable-and fixed-dose budesonide/formoterol pressurized metered-dose inhaler (BUD/FM pMDI) and fixed-dose fluticasone/salmeterol dry powder inhaler (FP/SM DPI. In: American Thoracic Society International Conference; 2007 May 18-23; San Francisco. 2007:Poster #K4.
Shah 2009 {published data only}
- Shah SR, Busse WW, McElhattan J, O'Brien CD, Goldman M. Efficacy and tolerability of fixed-dose (fd) and adjustable-dose (ad) budesonide/formoterol pressurized metered-dose inhaler (bud/fm pmdi) and fd fluticasone propionate/salmeterol dry powder inhaler (fp/sal dpi) within racial groups. Journal of Allergy and Clinical Immunology 2009;123(2):S80. [Google Scholar]
Somerville 2007 {published data only}
- Somerville L, Busse WW, Shah SR, Martin P, Goldman M. Safety of adjustable-dose budesonide (BUD)/formoterol (FM) pressurized metered-dose inhaler (pMDI), fixed-dose (BUD/FM pMDI and fixed-dose fluticasone (FP)/salmeterol (SM) dry powder inhaler (DPI) in asthma patients. In: American Thoracic Society International Conference; 2007 May 18-23; San Francisco. 2007:Poster #K3.
Sovani 2004 {published data only}
- Sovani MP, Whale CI, Oborne J, Cooper S, Mortimer K, Harrison TW. The effect of providing a single inhaler containing formoterol and budesonide to be used once daily and as required on inhaled budesonide use and asthma control in poorly compliant patients. Thorax 2004;59:ii11. [Google Scholar]
Stallberg 2003 {published data only}
- Stallberg B, Olsson P, Ekstrom T, Lindark N. Fewer asthma patients experience exacerbations with budesonide/formoterol in a single inhaler using adjustable versus fixed dosing. European Respiratory Journal 2003;22:P2798. [Google Scholar]
- Stallberg B, Olsson P, Jorgensen LA, Lindarck N, Ekstrom T. Budesonide/formoterol adjustable maintenance dosing reduces asthma exacerbations versus fixed dosing. International Journal of Clinical Practice 2003;57(8):656-61. [PubMed] [Google Scholar]
Stoloff 2002 {published data only}
- Stoloff S, Poinsett-Holmes K, Dorinsky PM. Combination therapy with inhaled long-acting beta(2)-agonists and inhaled corticosteroids: a paradigm shift in asthma management. Pharmacotherapy 2002;22(2):212-6. [DOI] [PubMed] [Google Scholar]
Sudarshan 2012 {published data only}
- Sudarshan S. Monotherapy vs. combination therapy for the management of mild asthma. American Family Physician 2012;85(6):652. [Google Scholar]
Sumino 2018 {published data only}
- Sumino K, Bacharier LB, Taylor J, Kelley C, Curtis V, Nash A, et al. The real-world effectiveness of symptom-based, intermittent inhaled corticosteroid adjustment in African American children with asthma. American Journal of Respiratory and Critical Care Medicine 2018;197:A1426. [Google Scholar]
Sumino 2019 {published data only}
- Sumino K, Bacharier LB, Taylor J, Chadwick-Mansker K, Curtis V, Nash A, et al. A pragmatic trial of symptom-based inhaled corticosteroid use in African-American children with mild asthma. Journal of Allergy and Clinical Immunology 2019;8(1):176-85.e2. [DOI: 10.1016/j.jaip.2019.06.030.] [DOI] [PubMed] [Google Scholar]
Syed 2008 {published data only}
- Syed QK, Shah NN, Bachh AA, Bhargava R, Ahmed Z, Pandey DK, et al. Can beta-2 agonists substitute inhaled corticosteroids in stable persistent asthma? Chest 2008;134(4):94003s. [Google Scholar]
Søes‐Petersen 2011 {published data only}
- Søes-Petersen U, Kava T, Dahle R, Lei Y, Dam N. Budesonide/formoterol maintenance and reliever therapy versus conventional best standard treatment in asthma in an attempted 'real life' setting. Clinical Respiratory Journal 2011;5(3):173-82. [DOI] [PubMed] [Google Scholar]
Tal 2001 {published data only}
- Tal A, Simon G, Vermeulen JH, Petru V, Cobos N, Everard ML, et al. Symbicort (budesonide and formoterol in a single inhaler) is more effective that budesonide alone in children with asthma. In: International Paediatric Respiratory and Allergy Congress; 2001 April 1-4; Prague. 2001:84-5.
Tschopp 1984 {published data only}
- Tschopp JM, Turner-Warwick M. Persisting airflow limitation in asthmatics receiving routine self-adjusted medication. European Journal of Respiratory Diseases 1984;65(5):346-53. [PubMed] [Google Scholar]
Tsoi 2006 {published data only}
- Tsoi AN, Gavrishina EA, Lazareva NB, Akhipov VV. Efficacy of the using budesonide formoterol in patients with bronchial asthma (BA): the study of routine clinical practice. European Respiratory Journal 2006;28:499s. [Google Scholar]
UMIN000010825 2013 {published data only}
- UMIN000010825. Study of evaluation for efficacy and safety of SMART(Symbicort Maintenance and Reliever Therapy) in poorly controlled asthmatics [Study of evaluation for efficacy and safety of SMART(Symbicort maintenance and reliever therapy) in poorly controlled asthmatics - SMART(Symbicort Maintenance and Reliever Therapy) in poorly controlled asthmatics]. ictrptest.azurewebsites.net/Trial2.aspx?TrialID=JPRN-UMIN000010825 (first received 29 May 2013).
van Dalen 2009 {published data only}
- Dalen CJ, Aldridge RE, Chan T, Senthilmohan R, Hancox RJ, Cowan JO, et al. Bromotyrosines in sputum proteins and treatment effects of terbutaline and budesonide in asthma. Annals of Allergy, Asthma and Immunology 2009;103(4):348-53. [DOI] [PubMed] [Google Scholar]
Van Der Woude 2004 {published data only}
- Van Der Woude HJ, Boorsma M, Bergqvist PB F, Winter TH, Aalbers R. Budesonide/formoterol in a single inhaler rapidly relieves methacholine-induced moderate-to-severe bronchoconstriction. Pulmonary Pharmacology and Therapeutics 2004;17(2):89-95. [DOI] [PubMed] [Google Scholar]
van Essen‐Zandvliet 1988 {published data only}
- Essen-Zandvliet EE, Neijens HJ, Kerrebijn KF. The effect of inhalation treatment with corticosteroids and beta-sympathicomimetics on bronchial responsiveness in children. Nederlands Tijdschrift voor Geneeskunde 1988;132(6):257-61. [PubMed] [Google Scholar]
van Schayck 2012 {published data only}
- Schayck OC, Haughney J, Aubier M, Selroos O, Ekstrom T, Ostinelli J, et al. Do asthmatic smokers benefit as much as non-smokers on budesonide/formoterol maintenance and reliever therapy? Results of an open label study. Respiratory Medicine 2012;106(2):189-96. [DOI] [PubMed] [Google Scholar]
Vermeulen 2001 {published data only}
- Vermeulen JH, Simon G, Tal A. Symbicort® (budesonide and formoterol in a single inhaler) improves lung function in asthmatic children aged 4-17 years. In: Annual Thoracic Society 97th International Conference; 2001 May 18-23; San Francisco. 2001:D29.
Vogelmeier 2005 {published data only}
- Vogelmeier C, D'Urzo A, Jaspal M, Merino JM, Johansson G, Boulet S. Symbicort for both maintenance and relief reduces exacerbations compared with a titration of Seretide (Advair) in patients with asthma: a real life study. In: American Thoracic Society International Conference; 2005 May 20-25; San Diego. 2005:[C33] [Poster: F67].
Vogelmeier 2005a {published data only}
- Vogelmeier C, D'Urzo A. Maintenance plus as-needed budesonide/formoterol vs salmeterol/fluticasone in a real-life setting. European Respiratory Journal 2005;26:2770. [Google Scholar]
Vogelmeier 2012 {published data only}
- Vogelmeier C, Naya I, Ekelund J. Budesonide/formoterol maintenance and reliever therapy in Asian patients (aged ≥16 years) with asthma: a sub-analysis of the COSMOS study. Clinical Drug Investigation 2012;32(7):439-49. [DOI] [PubMed] [Google Scholar]
Wallin 1998 {published data only}
- Wallin A, Sandstrom T, Soderberg M, Howarth P, Djukanovic R, Wilson S, et al. Effects of formoterol, budesonide and placebo treatment on asthmatic airway inflammation. Annals of Allergy, Asthma and Immunology 1998;80:88. [Google Scholar]
Weinstein 2001 {published data only}
- Weinstein SF, Pearlman DS, Condemi JJ, Herrle MR, Scott CA, Payne JE, et al. Superior efficacy of the fluticasone propionate/salmeterol 88/42mcg HFA-MDI combination product versus the individual components in asthmatics previously treated with either short- or long-acting beta2-agonists or inhaled corticosteroids. Journal of Allergy and Clinical Immunology 2001;107(2):S102. [Google Scholar]
Welte 2004 {published data only}
- Welte T, Aalbers R, Naya I. Budesonide/formoterol adjustable maintenance dosing (B/F AMD) reduces the burden of asthma more effectively than fixed dosing (FD) with B/F or salmeterol/fluticasone (S/FL). European Respiratory Journal 2004;24:508s. [Google Scholar]
Worth 2005 {published data only}
- Worth H. DESOLO - SiT Peri-Launch: a comparison of symbicort single inhaler therapy and conventional best practice for the treatment of persistent asthma in adults [A comparison of Symbicort single inhaler therapy (Symbicort Turbuhaler 160/4.5 µg, 1 inhalation b.i.d. plus as needed) and conventional best practice for the treatment of persistent asthma in adults - a 26-week, randomised, open-label, parallel-group, multicentre study]. clinicaltrials.gov/ct2/show/NCT00252863 (first received 15 November 2005).
Yi 2003 {published data only}
- Yi TY, Li JM, Li QL, Zhi AI, Yi J. Budesonide in combination with salbutamol in the treatment of 61 cases of childhood bronchial asthma during acute episodes. Herald of Medicine 2003;22(8):540-1. [Google Scholar]
Zetterstrom 2000 {published data only}
- Zetterstrom O, Buhl R, Mellem H, Perpina M, Hedman J, O'Neill S, et al. Efficacy and safety of a new single inhaler product containing both budesonide and formoterol in adult asthma. European Respiratory Journal 2000;16:455s. [DOI] [PubMed] [Google Scholar]
Zetterstrom 2000a {published data only}
- Zetterstrom O, Buhl R, Mellem H, Perpina M, Hedman J, O'Neill S, et al. The new single inhaler product containing both budesonide/formoterol improves asthma control in adults. European Respiratory Journal 2000;16:455s. [DOI] [PubMed] [Google Scholar]
Zetterstrom 2001 {published data only}
- Zetterstrom O, Buhl R, Mellem H. Efficacy and safety of symbicort® (budesonide and formoterol in a single inhaler) in adults with asthma. In: Annual Thoracic Society 97th International Conference; 2001 May 18-23; San Francisco. 2001:D31.
Zhong 2013 {published data only}
- Zhong NS, Lin JT, Mehta P, Ngamjanyaporn P, Wu TC, Yunus F. Real-life effectiveness of budesonide/formoterol maintenance and reliever therapy in asthma patients across Asia: SMARTASIA study. BMC Pulmonary Medicine 2013;13:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to ongoing studies
ACTRN12620001091998 2020 {published data only}
- ACTRN12620001091998. A randomised controlled trial of the efficacy and safety of an inhaled corticosteroid and long acting beta agonist reliever therapy regimen in children with mild asthma [An open-label randomised controlled trial of the efficacy and safety of as-needed budesonide-formoterol vs salbutamol reliever therapy in mild childhood asthma]. ictrptest.azurewebsites.net/Trial2.aspx?TrialID=ACTRN12620001091998 (first received 20 October 2020).
NCT04215848 2020 {published data only}
- NCT04215848. As-needed budesonide/formoterol turbuhaler in stepping down period [Efficacy of as-needed budesonide/formoterol turbuhaler during stepping down period from step-3 in adult patients with adequately controlled asthma]. clinicaltrials.gov/show/NCT04215848 (first received 2 January 2020).
Additional references
AIHW 2007
- Australian Institute of Health and Welfare. Asthma in Australia with a focus chapter on chronic obstructive pulmonary disease. www.aihw.gov.au/getmedia/8d7e130c-876f-41e3-b581-6ba62399fb24/11774.pdf.aspx?inline=true (accessed prior to 20 September 2019).
Barnes 1999
- Barnes PJ. Effect of beta-agonists on inflammatory cells. Journal of Allergy and Clinical Immunology 1999;104(2 Pt 2):S10-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Barnes 2010
- Barnes PJ. Inhaled corticosteroids. Pharmaceuticals 2010;8(3):514-40. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Beasley 2019
- Beasley R, Holliday M, Reddel HK, Braithwaite I, Ebmeier S, Hancox RJ, et al. Controlled trial of budesonide-formoterol as needed for mild asthma. New England Journal of Medicine 2019;380(21):2020-30. [PMID: ] [DOI] [PubMed] [Google Scholar]
Bender 2005
- Bender BG, Bender SE. Patient-identified barriers to asthma treatment adherence: responses to interviews, focus groups, and questionnaires. Immunology and Allergy Clinics of North America 2005;25(1):107-30. [PMID: ] [DOI] [PubMed] [Google Scholar]
Bergström 2008
- Bergström SE, Boman G, Eriksson L, Formgren H, Foucard T, Hörte LG, et al. Asthma mortality among Swedish children and young adults, a 10-year study. Respiratory Medicine 2008;102(9):1335-41. [PMID: ] [DOI] [PubMed] [Google Scholar]
Bloom 2018
- Bloom CI, Nissen F, Douglas IJ, Smeeth L, Cullinan P, Quint JK. Exacerbation risk and characterisation of the UK’s asthma population from infants to old age. Thorax 2018;73(4):313. [PMID: ] [DOI] [PubMed] [Google Scholar]
Cates 2013
- Cates CJ, Karner C. Combination formoterol and budesonide as maintenance and reliever therapy versus current best practice (including inhaled steroid maintenance), for chronic asthma in adults and children. Cochrane Database of Systematic Reviews 2013, Issue 4. Art. No: CD007313. [DOI: 10.1002/14651858.CD007313.pub3] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chauhan 2013
- Chauhan BF, Chartrand C, Ducharme FM. Intermittent versus daily inhaled corticosteroids for persistent asthma in children and adults. Cochrane Database of Systematic Reviews 2013, Issue 2. Art. No: CD009611. [DOI: 10.1002/14651858.CD009611.pub3] [CD009611] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cochrane Airways 2019
- Cochrane Airways Trials Register. airways.cochrane.org/trials-register (accessed 7 May 2019).
Domingo 2019
- Domingo C, Rello J, Sogo A. As‑needed ICS‑LABA in mild asthma: what does the evidence say? Drugs 2019;79(16):1729-37. [PMID: ] [DOI] [PubMed] [Google Scholar]
Dusser 2007
- Dusser D, Montani D, Chanez P, Blic J, Delacourt C, Deschildre A, et al. Mild asthma: an expert review on epidemiology, clinical characteristics and treatment recommendations. Allergy 2007;62(6):591-604. [PMID: ] [DOI] [PubMed] [Google Scholar]
Engelkes 2015
- Engelkes M, Janssens HM, Jongste JC, Sturkenboom MC, Verhamme KM. Medication adherence and the risk of severe asthma exacerbations: a systematic review. European Respiratory Journal 2015;45(2):396. [PMID: ] [DOI] [PubMed] [Google Scholar]
GBD Study 2017
- Global Burden of Disease Study. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Respiratory Medicine 2017;5(9):691-706. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
GINA 2019
- Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention (2019 update). ginasthma.org/reports/ (accessed prior to 20 September 2019).
GOLD 2020
- Global Strategy for Prevention, Diagnosis and Management of COPD 2020 Report. goldcopd.org/wp-content/uploads/2019/11/GOLD-2020-REPORT-ver1.1wms.pdf (accessed 4th December 2019).
GRADEpro GDT [Computer program]
- GRADEpro GDT. Version accessed 16 October 2019. Hamilton (ON): McMaster University (developed by Evidence Prime), 2015. Available at gradepro.org.
Grainge 2011
- Grainge CL, Lau LC, Ward JA, Dulay V, Lahiff G, Wilson S, et al. Effect of bronchoconstriction on airway remodeling in asthma. New England Journal of Medicine 2011;364(21):2006-15. [PMID: ] [DOI] [PubMed] [Google Scholar]
Haahtela 1994
- Haahtela T, Marvinen M, Kava T, Kiviranta K, Koskinen S, Lehtonen K, et al. Effects of reducing or discontinuing inhaled budesonide in patients with mild asthma. New England Journal of Medicine 1994;331(11):700-5. [DOI: 10.1056/NEJM199409153311103] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hatter 2021
- Hatter L, Bruce P, Braithwaite I, Holliday M, Fingleton J, Weatherall M, et al. ICS-formoterol reliever versus ICS and short-acting β 2-agonist reliever in asthma: a systematic review and meta-analysis. European Respiratory Journal Open Research 2021;7(1):00701-2020. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Altman DG, Sterne JA (editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011.. Available from www.handbook.cochrane.org.
Higgins 2019
- Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.. [DOI] [PMC free article] [PubMed]
Kew 2016
- Kew KM, Quinn M, Quon BS, Ducharme FM. Increased versus stable doses of inhaled corticosteroids for exacerbations of chronic asthma in adults and children. Cochrane Database of Systematic Reviews 2016, Issue 6. Art. No: CD007524. [DOI: 10.1002/14651858.CD007524.pub4] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lange 1998
- Lange P, Parner J, Vestbo J, Schnohr P, Jensen G. A 15-year follow-up study of ventilatory function in adults with asthma. New England Journal of Medicine 1998;339(17):1194-200. [DOI: 10.1056/NEJM199810223391703] [PMID: ] [DOI] [PubMed] [Google Scholar]
Lazarus 2019
- Lazarus SC, Krishnan JA, King TS, Lang JE, Blake KV, Covar R, et al. Mometasone or tiotropium in mild asthma with a low sputum eosinophil level. New England Journal of Medicine 2019;380(21):2009-19. [DOI: 10.1056/NEJMoa1814917] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Marshall 2018
- Marshall IJ, Noel-Storr AH, Kuiper J, Thomas J, Wallace BC. Machine learning for identifying randomized controlled trials: an evaluation and practitioner’s guide. Research Synthesis Methods 2018;9(4):602-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
McDonald 2017
- McDonald S, Noel-Storr AH, Thomas J. Harnessing the efficiencies of machine learning and Cochrane Crowd to identify randomised trials for individual Cochrane reviews. In: Global Evidence Summit; 2017 September 13-16; Cape Town, South Africa. 2017.
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman D. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Medicine 2009;6(7):e1000097. [DOI: 10.1371/journal.pmed.1000097] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mukherjee 2016
- Mukherjee M, Stoddart A, Gupta RP, Nwaru BI, Farr A, Heaven M, et al. The epidemiology, healthcare and societal burden and costs of asthma in the UK and its member nations: analyses of standalone and linked national databases. BMC Medicine 2016;14(1):113. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nelson 2006
- Nelson HS, Weiss ST, Bleecker ER, Yancey SW, Dorinsky PM, SMART Study Group. The Salmeterol Multicenter Asthma Research Trial: a comparison of usual pharmacotherapy for asthma or usual pharmacotherapy plus salmeterol. Chest 2006;129(1):15-26. [DOI] [PubMed] [Google Scholar]
Noel‐Storr 2018
- Noel-Storr AH, Project Transform team. Cochrane Crowd: new ways of working together to produce health evidence. In: Evidence Live; 2018 June 18-20; Oxford, UK. 2018.
Ouzzani 2016 [Computer program]
- Rayyan — a web and mobile app for systematic reviews. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan Systems Inc, 2016. [DOI: 10.1186/s13643-016-0384-4] [PMID: ] [DOI] [PMC free article] [PubMed]
Papi 2007
- Papi A, Canonica GW, Maestrelli P, Paggiaro P, Olivieri D, Pozzi E, et al. Rescue use of beclomethasone and albuterol in a single inhaler for mild asthma. New England Journal of Medicine 2007;356(20):2040-52. [PMID: ] [DOI] [PubMed] [Google Scholar]
Papi 2018
- Papi A, Brightling C, Pedersen SE, Reddel HK. Asthma. Lancet 2018;391(10122):783-800. [PMID: ] [DOI] [PubMed] [Google Scholar]
Petsky 2016
- Petsky HL, Kew KM, Turner C, Chang AB. Exhaled nitric oxide levels to guide treatment for adults with asthma. Cochrane Database of Systematic Reviews 2016, Issue 9. Art. No: CD011440. [DOI: 10.1002/14651858.CD011440.pub2] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rabe 2004
- Rabe KF, Adachi M, Lai CK, Soriano JB, Vermeire PA, Weiss KB, et al. Worldwide severity and control of asthma in children and adults: the global asthma insights and reality surveys. Journal of Allergy and Clinical Immunology 2004;114(1):40-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
RCP 2014
- Royal College of Physicians. The National Review of Asthma Deaths. www.rcplondon.ac.uk/projects/national-review-asthma-deaths (accessed prior to 20 September 2019).
Review Manager 2014 [Computer program]
- Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Sadatsafavi 2010
- Sadatsafavi M, Lynd L, Marra C, Carleton B, Tan WC, Sullivan S, et al. Direct health care costs associated with asthma in British Columbia. Canadian Respiratory Journal [Revue Canadienne de Pneumologie] 2010;17(2):74-80. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Suissa 2000
- Suissa S, Ernst P, Benayoun S, Baltzan M, Cai B. Low-dose inhaled corticosteroids and the prevention of death from asthma. New English Journal of Medicine 2000;343(5):332-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Taylor 2014
- Taylor A, Chen LC, Smith MD. Adherence to inhaled corticosteroids by asthmatic patients: measurement and modelling. International Journal of Clinical Pharmacy 2014;36(1):112-9. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Thomas 2017
- Thomas J, Noel-Storr AH, Marshall I, Wallace B, McDonald S, Mavergames C, et al. Living systematic review network. Living systematic reviews: 2. Combining human and machine effort. Journal of Clinical Epidemiology 2017;91:31-7. [DOI] [PubMed] [Google Scholar]
Ulrik 1994
- Ulrik CS, Lange P. Decline of lung function in adults with bronchial asthma. American Journal of Respiratory and Critical Care Medicine 1994;150(3):629-34. [PMID: ] [DOI] [PubMed] [Google Scholar]
Wallin 1993
- Wallin A, Sandström T, Rosenhall L, Melander B. Time course and duration of bronchodilatation with formoterol dry powder in patients with stable asthma. Thorax 1993;48(6):611-4. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Crossingham 2020
- Crossingham I, Turner S, Ramakrishnan S, Hynes G, Gowell M, Yasmin F, et al. Combination fixed-dose beta agonist and steroid inhaler as required for adults or children with mild asthma. Cochrane Database of Systematic Reviews 2020, Issue 1. Art. No: CD013518. [DOI: 10.1002/14651858.CD013518] [DOI] [PMC free article] [PubMed] [Google Scholar]


