Abstract
A projected shortage of hematopoietic cell transplantation (HCT) health professionals was identified as a major issue during the National Marrow Donor Program/Be The Match System Capacity Initiative. Work-related distress and work–life balance were noted to be potential barriers to recruitment/retention. This study examined these barriers and their association with career satisfaction across HCT disciplines. A cross-sectional, 90-item, web-based survey was administered to advanced practice providers, nurses, physicians, pharmacists, and social workers in 2015. Participants were recruited from membership lists of 6 professional groups. Burnout (measured with the Maslach Burnout Inventory subscales of emotional exhaustion and depersonalization) and moral distress (measured by Moral Distress Scale—Revised) were examined to identify work-related distress. Additional questions addressed demographics, work–life balance, and career satisfaction. Of 5759 HCT providers who received an individualized invitation to participate, 914 (16%) responded; 627 additional participants responded to an open link survey. Significant differences in demographic and practice characteristics existed across disciplines (P < .05). The prevalence of burnout differed across disciplines (P < .05) with an overall prevalence of 40%. Over one-half of pharmacists had burnout, whereas social workers had the lowest prevalence at less than one-third. Moral distress scores ranged from 0 to 336 and varied by discipline (P < .05); pharmacists had the highest mean score (62.9 ± 34.8) and social workers the lowest (42.7 ± 24.4). In multivariate and univariate analyses, variables contributing to burnout varied by discipline; however, moral distress was a significant contributing factor for all providers. Those with burnout were more likely to report inadequate work–life balance and a low level of career satisfaction; however, overall there was a high level of career satisfaction across disciplines. Burnout, moral distress, and inadequate work–life balance existed at a variable rate in all HCT disciplines, yet career satisfaction was high. These results suggest specific areas to address in the work environment for HCT health professionals, especially the need for relief of moral distress and a greater degree of personal time. As the creation of healthy work environments is increasingly emphasized to improve quality care and decrease costs, these findings should be used by HCT leadership to develop interventions that mitigate work-related distress and in turn foster recruitment and retention of HCT providers.
Keywords: Hematopoietic cell, transplantation, Burnout, Moral distress, Work–life balance, Career satisfaction
INTRODUCTION
There is a projected shortage of health professionals in hematopoietic cell transplantation (HCT) in the coming decade to care for the increasing number of transplant recipients [1]. To address challenges related to workforce and other needed resources for the anticipated future growth, the National Marrow Donor Program/Be the Match organized a national collaborative effort, the System Capacity Initiative. The System Capacity Initiative represented a diverse group of stakeholders including representatives of the multidisciplinary HCT team [1,2].
To better understand barriers to recruitment and retention, workforce-related working groups conducted surveys of their stakeholders. The Physician System Capacity Initiative Workforce Group identified high workload resulting in long working hours and poor work–life balance as well as the responsibility of care for complex patient populations as the primary reasons trainees were not attracted to the field of HCT [3]. A survey conducted by the Nursing System Capacity Initiative Workforce Group found that over 50% of the 148 nurses recognized their top 3 challenges as working in stressful environments, balancing work and personal lives, and addressing ethical moral issues [2].
Caring for patients in HCT demands that health professionals be competent in both rendering care and providing emotional comfort, especially in end-of-life situations. This leads to physical and mental exhaustion, with negative work-related corollaries [4–6] that have the potential to erode work engagement and professionalism and ultimately influence quality of care [4,7]. In addition, secondary traumatic stress from compassion fatigue and caring has been recognized as an adverse consequence that can lead to burnout and vicarious traumatization [4]. Burnout has been described as a psychological syndrome emerging as a prolonged response to chronic interpersonal stressors on the job. The 3 key dimensions of this response are an overwhelming exhaustion, feelings of cynicism and detachment from the job, and a sense of ineffectiveness and lack of accomplishment [8].
Several studies have measured the prevalence of burnout among physicians and nurses working in oncology [6,9–11]. A nationwide study of oncologists in the United States that evaluated burnout identified dissatisfaction with work–life balance as a common occurrence [12–14]. Small sample studies of transplant nursing in the 1990s reported burnout and stress emanating from intense patient–nurse relationships, reacting to death, attempting to find meaning in patient suffering, adapting to ongoing changing care protocols, and managing emergent and intensive clinical scenarios [11,15–17]. However, there are no recent studies on the prevalence of burnout in HCT nurses or other HCT disciplines.
HCT health professionals are frequently faced with challenges in recognizing the ethically appropriate decisions related to end-of-life care in this vulnerable patient population but being unable to carry out these decisions because of internal and/or external constraints [18]. This often results in moral distress: a “psychological disequilibrium” that occurs when the provider is able to make a moral judgment about the correct choice [11,15–17] but is not able to provide the care that is perceived to be “right” or “best” for the patient [19]. Moral distress can contribute to job dissatisfaction, burnout, and job attrition [20,21]. It is also known to result in decreased sensitivity to ethically difficult clinical issues and providers withdrawing from the patient care situation [20] or a form of conscientious objection to caring for a patient perceived as having no chance for meaningful recovery [20].
The primary aim of this study was to determine the prevalence of and factors contributing to work-related distress, namely burnout and moral distress, in HCT health professionals. The secondary aim was to examine perceptions of work–life balance and career satisfaction and their association with burnout. Recognizing that clinical care in HCT is provided collectively by a team of multidisciplinary health professionals, this study examined the variations in prevalence and associations of these issues across HCT disciplines.
METHODS
Study Design and Population
A 90-item, web-based survey was disseminated from January to March 2015 using the tailored-design survey method [22]. HCT health professionals, including advanced practice providers (APPs, which includes advanced practice nurses, clinical nurse specialists, physician assistants, and nurse practitioners), nurses, physicians, pharmacists, and social workers providing direct care to HCT patients in a US hospital or clinic-based program, were eligible to participate. Participants were recruited from membership lists provided by professional societies/associations (Figure 1). Duplicate memberships were eliminated. Pharmacists were recruited from an existing Google Group because no HCT-focused pharmacy group existed.
Figure 1.
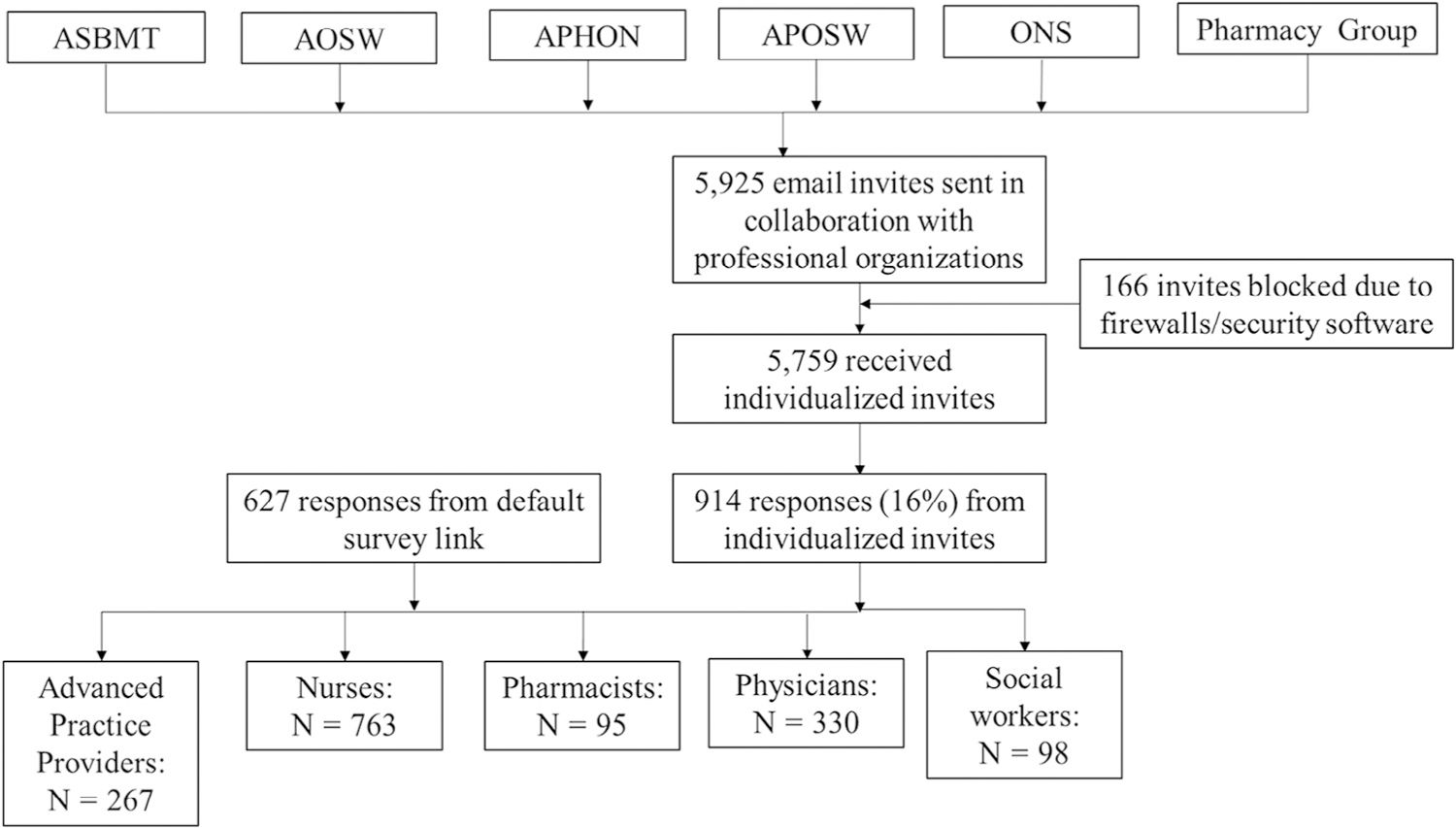
Recruitment from 6 professional groups. ASBMT indicates American Society for Blood and Marrow Transplant; AOSW, Association of Oncology Social Work; APHON, Association of Pediatric Hematology/Oncology Nurses; APOSW, Association of Pediatric Oncology Social Workers; ONS, Oncology Nursing Society.
Recruitment methods included an introductory e-mail from the relevant professional association or National Marrow Donor Program explaining the purpose of the study and providing background information, followed by an e-mail invitation to participate in the survey. Four targeted follow-up contacts were made to nonrespondents. Honoraria of twenty $100 Visa gift cards were offered through a lottery. The initial overall response rate from individualized invitations was low; therefore, in an effort to increase the response rate, the survey link was subsequently distributed as an open invitation, and invitees were asked to forward a default survey link to all those eligible and interested in participating.
Measurement: Instrument Content
The survey instrument is provided in the Supplementary Materials (Appendix A). The instrument focused on 4 measurement domains: burnout, moral distress, work–life balance, and career satisfaction. Burnout and moral distress were considered as major components of work-related distress that impact work–life balance and career satisfaction. The survey also asked about demographics and personal- and work-related factors. Questions to address compassion fatigue were also included (results are reported separately). Piloting revealed an average completion time of 20 minutes.
Burnout was measured using the Maslach Burnout Inventory (MBI), a frequently used, standardized, and well-validated 22-item self-administered questionnaire comprising 3 subscales: emotional exhaustion (EE; includes 9 items), depersonalization (DP; includes 5 items), and personal accomplishment (PA; includes 8 items) [8]. Each question received a Likert-scale score based on the respondent’s perceived frequency of experiencing the situation from 0 (never) to 6 (every day). The range of possible total scores were 0 to 54 for EE, 0 to 30 for DP, and 0 to 48 for PA; scores within these ranges were categorized per the MBI as low, medium, and high scores [8]. For the EE and DP subscales higher mean scores corresponded to higher degrees of perceived burnout, with burnout defined as an EE score ≥ 27 and/or DP score ≥ 10. Higher mean scores on the PA subscale corresponded to a higher sense of personal accomplishment [8].
Moral distress was measured using 3 versions of the validated Moral Distress Scale—Revised (MDS-R) [19,24], 1 for physicians, 1 for nurses, and 1 for all other health professionals because of question modification for practice differences between clinicians [24]. The MDS-R is a 21-item questionnaire that has been extensively used in nursing research to measure an individual’s perceptions of 21 hypothetical situations/scenarios causing moral distress. Each item has 2 parts: (1) frequency of the encountered situation in their work and (2) intensity of moral distress felt by the respondent. Scores ranged from 0 (never) to 4 (very frequently or very intense) for each part. The total score for each item was calculated by multiplying the frequency by the intensity of distress. Scores were divided by 33 and 67 percentiles and categorized as low, medium, and high.
Adequate work–life balance was defined by agreement (strongly agree, agree) to the statement, “My work leaves me enough time for my personal/family life” and inadequate by disagreement (disagree, strongly disagree) [7]. This single-item measure was adapted from a study on burnout and career satisfaction in US physicians relative to the general population [7].
A high level of career satisfaction was defined as agreement (strongly agree, agree) with the statement, “I am satisfied with my career in HCT” and low level by disagreement (disagree, strongly disagree) as adapted from a study of US oncologists [7,14]. Participants were also asked if they would recommend a career in HCT and their level of satisfaction with aspects of HCT work.
Statistical Analysis
Demographic characteristics of the groups of health professionals responding to the individual and open invitations were compared and were similar; therefore, the responses were combined for analysis. Responses from advanced practice nurses, nurse practitioners, and physician assistants were combined as APPs for analysis.
The distribution of personal and work-related characteristics was described by discipline. Mean scores were calculated for the 3 subscales of the MBI: EE, DP, and PA. The distributions of low, medium, and high MBI score ranges were described by percentage. The mean scores of MBI subscales and MDS-R scores were compared by discipline using analysis of variance; post hoc analyses by the Tukey-Kramer procedure were applied for examining the differences between professional groups. The associations of burnout, work–life balance, and career satisfaction were examined by chi-square tests. Multivariable linear regression models were developed to identify personal and work-related characteristics associated with the scores of EE and DP by discipline. Variables included in the regression models are included in Supplementary Tables S1 and S2. Predictors for the presence of burnout were examined by binary logistic regression. To adjust for the effects of personal characteristics on EE, DP, and burnout, multivariable linear regression and logistic regression models included all selected parameters, instead of using stepwise selection. Respondents working only in critical care or settings other than inpatient/outpatient units were excluded from multivariate analyses because of a small sample size (n = 24). Univariate logistic regression models were developed for pharmacists and social workers because of the relatively small size of respondents (<100). Variables included in the regression models are included in Supplementary Tables S1 and S2. Statistical significance was defined as P < .05.
RESULTS
Demographics and Work-Related Characteristics
A total of 1541 respondents completed the survey (Figure 1). The response rate to the initial distribution was 914 (16%); there were an additional 617 respondents from all disciplines to the open mailing invitation. Respondents’ characteristics varied by discipline as shown in Table 1. One-third were aged 30 to 39 years (the range with the highest percentage in every discipline except for physicians). Nurses had the highest percentage among disciplines in the youngest age range (20 to 29 years) and physicians in the oldest range (≥60 years). Most respondents were women (except in the physician group), married or partnered, and had 1 or more dependents.
Table 1.
Demographics and Work-Related Characteristics by Discipline (N = 1541)
| Characteristic | APPs (n = 255) | Nurses (n = 763) | Physicians (n = 330) | Pharmacists (n = 95) | Social Workers (n = 98) | Total (n = 1541) |
|---|---|---|---|---|---|---|
| Age, yr | ||||||
| 20–29 | 22 (9) | 150 (20) | 1 (<1) | 17 (18) | 12 (12) | 202 (13) |
| 30–39 | 95 (38) | 240 (32) | 94 (29) | 44 (46) | 39 (40) | 512 (33) |
| 40–49 | 59 (23) | 162 (21) | 96 (29) | 18 (19) | 17 (17) | 352 (23) |
| 50–59 | 55 (22) | 161 (21) | 82 (25) | 13 (14) | 22 (22) | 333 (22) |
| ≥60 | 22 (9) | 49 (6) | 57 (17) | 3 (3) | 8 (8) | 139 (9) |
| Gender | ||||||
| Female | 236 (94) | 729 (96) | 142 (43) | 65 (70) | 87 (89) | 1259 (82) |
| Male | 16 (6) | 27 (4) | 186 (57) | 28 (30) | 11 (11) | 268 (18) |
| Relationship status | ||||||
| Married or partnered | 180 (71) | 514 (83) | 285 (87) | 69 (73) | 75 (77) | 1123 (73) |
| Divorced/widowed/widower | 19 (8) | 52 (8) | 17 (5) | 1 (1) | 6 (6) | 95 (6) |
| Single | 54 (21) | 54 (9) | 27 (8) | 24 (26) | 17 (17) | 312 (20) |
| No. of dependents | ||||||
| 0 | 116 (47) | 373 (50) | 101 (32) | 43 (46) | 47 (49) | 680 (45) |
| 1–2 | 108 (43) | 277 (37) | 139 (43) | 40 (43) | 45 (47) | 609 (41) |
| ≥3 | 25 (10) | 93 (13) | 81 (25) | 10 (11) | 4 (4) | 21 (14) |
| Years in HCT | ||||||
| 0–2 | 34 (13) | 113 (15) | 62 (19) | 14 (15) | 29 (30) | 252 (16) |
| 3–5 | 69 (27) | 181 (24) | 76 (23) | 26 (27) | 29 (30) | 368 (24) |
| 6–10 | 39 (15) | 103 (14) | 99 (30) | 25 (26) | 16 (16) | 253 (16) |
| 11–20 | 45 (18) | 175 (23) | 47 (14) | 23 (24) | 19 (19) | 322 (21) |
| ≥21 | 67 (26) | 190 (25) | 46 (14) | 7 (7) | 5 (5) | 344 (22) |
| Work setting | ||||||
| Inpatient | 81 (32) | 394 (52) | 16 (5) | 34 (36) | 16 (16) | 541 (35) |
| Outpatient | 66 (26) | 245 (33) | 8 (2) | 13 (14) | 32 (33) | 364 (24) |
| Inpatient and outpatient | 100 (40) | 102 (14) | 302 (92) | 46 (48) | 49 (50) | 599 (39) |
| Critical care and other | 5 (2) | 13 (2) | 3 (1) | 2 (2) | 1 (1) | 24 (2) |
| Average hours worked/week | ||||||
| ≤40 | 29 (11) | 415 (55) | 7 (2) | 7 (7) | 22 (22) | 480 (31) |
| 41–50 | 143 (56) | 267 (35) | 35 (11) | 39 (41) | 69 (70) | 553 (36) |
| 51–60 | 61 (24) | 60 (8) | 100 (30) | 35 (37) | 6 (6) | 262 (17) |
| ≥61 | 21 (8) | 20 (3) | 188 (57) | 14 (15) | 1 (1) | 244 (16) |
| Nights/month on call | ||||||
| 0 | 220 (87) | 667 (88) | 46 (14) | 64 (67) | 82 (84) | 1079 (70) |
| 1–5 | 22 (9) | 60 (8) | 143 (43) | 14 (15) | 10 (10) | 249 (16) |
| ≥6 | 12 (5) | 35 (5) | 141 (43) | 17 (18) | 6 (6) | 211 (14) |
| Hours/week spent on patient care | ||||||
| 0–20 | 50 (20) | 153 (20) | 98 (30) | 8 (8) | 14 (14) | 323 (21) |
| 21–40 | 119 (47) | 510 (67) | 135 (41) | 61 (64) | 72 (74) | 897 (58) |
| ≥41 | 85 (34) | 99 (13) | 97 (30) | 26 (27) | 12 (12) | 319 (21) |
| Hours/week spent on administrative tasks | ||||||
| ≤20 | 202 (80) | 588 (77) | 273 (83) | 83 (87) | 90 (92) | 1236 (80) |
| >20 | 52 (21) | 174 (23) | 57 (17) | 12 (13) | 8 (8) | 303 (20) |
| Hours/week working at home | ||||||
| ≤10 | 190 (75) | 599 (79) | 188 (57) | 77 (81) | 80 (82) | 1334 (74) |
| >10 | 47 (19) | 62 (8) | 142 (43) | 15 (16) | 4 (4) | 270 (18) |
| N/A | 17 (7) | 101 (13) | 0 (0) | 3 (3) | 14 (14) | 135 (9) |
| Hours/week on research tasks at home | ||||||
| ≤10 | 187 (74) | 579 (76) | 197 (60) | 79 (83) | 77 (79) | 1119 (73) |
| >10 | 16 (6) | 40 (5) | 130 (39) | 7 (7) | 5 (5) | 198 (13) |
| N/A | 51 (20) | 143 (19) | 3 (1) | 9 (10) | 16 (16) | 222 (14) |
| Hours/week on certification or continuing medical education | ||||||
| ≤10 | 217 (85) | 620 (81) | 288 (87) | 84 (88) | 83 (85) | 1292 (84) |
| >10 | 32 (13) | 123 (16) | 41 (12) | 9 (10) | 10 (10) | 215 (14) |
| N/A | 5 (2) | 19 (3) | 1 (<1) | 2 (2) | 5 (5) | 32 (2) |
| Patient population | ||||||
| Adult | 179 (71) | 524 (69) | 202 (61) | 67 (71) | 74 (76) | 1046 (68) |
| Pediatric | 58 (23) | 148 (19) | 88 (27) | 13 (14) | 17 (17) | 169 (11) |
| Both | 17 (7) | 90 (12) | 40 (12) | 15 (16) | 7 (7) | 324 (21) |
| Total transplant volume | ||||||
| 0–50 | 49 (19) | 147 (19) | 66 (20) | 13 (14) | 18 (18) | 293 (19) |
| 51–150 | 67 (26) | 186 (24) | 98 (30) | 31 (33) | 25 (26) | 407 (27) |
| >150 | 123 (48) | 292 (38) | 162 (49) | 48 (51) | 38 (39) | 663 (43) |
| Unknown | 15 (6) | 137 (18) | 4 (1) | 3 (3) | 17 (17) | 176 (11) |
| Number of autologous transplants | ||||||
| 0–50 | 87 (34) | 248 (33) | 131 (40) | 36 (38) | 35 (36) | 537 (35) |
| 51–150 | 65 (26) | 184 (24) | 126 (39) | 30 (32) | 20 (20) | 425 (28) |
| >150 | 58 (23) | 111 (15) | 63 (19) | 23 (24) | 11 (11) | 266 (17) |
| Unknown | 44 (17) | 219 (29) | 10 (3) | 6 (6) | 32 (33) | 311 (20) |
| Number of allogeneic transplants | ||||||
| 0–50 | 95 (37) | 279 (37) | 143 (43) | 43 (45) | 40 (41) | 600 (39) |
| 51–150 | 64 (25) | 184 (24) | 126 (38) | 32 (34) | 20 (20) | 426 (28) |
| >150 | 49 (19) | 83 (11) | 52 (16) | 14 (15) | 6 (6) | 204 (13) |
| Unknown | 46 (18) | 216 (28) | 9 (3) | 6 (6) | 32 (33) | 309 (20) |
Values are n (%). N/A indicates not applicable.
Forty-three percent of all respondents had over 10 years of experience. Approximately one-fourth of APPs and nurses had worked more than 21 years in HCT; the largest percentage of physicians had worked 6 to 10 years in HCT. Interestingly, more than one-half of social workers had ≤5 years of experience in HCT. With the exception of nurses, of whom over half worked in the inpatient setting, most health professionals worked in both inpatient and outpatient settings. Across disciplines, over one-third reported working 41 to 50 hours weekly and most had no nights on call per month, although more than half of physicians worked ≥ 61 hours per week and most were on call 1 to 5 nights or more. The variation in hours spent on patient care, administrative tasks, working at home, research tasks, and maintaining certification was significantly different and associated with the distinct disciplines. Most respondents were providers for adult patients. The highest percentage of respondents in each discipline provided care at larger transplant programs (total number of autologous and allogeneic transplants > 150 per year).
MBI Subscales and Burnout
Subscale scores for EE, DP, and PA are shown in Table 2. Significant differences in EE and DP mean scores were observed across disciplines (P < .0001). Slightly over one-third of all respondents scored within the high range on the EE subscale. APPs and pharmacists had significantly higher mean EE scores (P < .05) and had the largest percentage (over 40%) of respondents in the high range than did the other disciplines. Seventy-nine percent of all respondents scored low (less depersonalized behavior) on the DP subscale. Physicians had significantly higher DP scores than APPs, nurses, and social workers (P < .05); pharmacists had significantly higher scores than social workers (P < .05); and APPs and nurses were not significantly different in DP scores. PA scores were also significantly different across disciplines (P < .001), with means scores in the high range for over half of respondents in all groups. Social workers and physicians had significantly higher scores than nurses and pharmacists (P < .05); APPs and nurses were not significantly different.
Table 2.
MBI Subscales Scores and Ranges
| MBI Subscale Scores (Range) and Mean (SD) | APPs (n = 255) | Nurses (n = 763) | Physicians (n = 330) | Pharmacists (n = 95) | Social Workers (n = 98) | Total (n = 1541) | |
|---|---|---|---|---|---|---|---|
| EE score* | Low (0–16) | 51 (20) | 241 (32) | 117 (35) | 15 (16) | 25 (26) | 449 (29) |
| Medium (17–26) | 93 (37) | 267 (35) | 105 (32) | 33 (35) | 45 (46) | 543 (35) | |
| High (27–54) | 111 (44) | 255 (33) | 108 (33) | 47 (49) | 28 (29) | 549 (36) | |
| Mean (SD) | 25.2 (10.9) | 22.8 (10.4) | 22.2 (11.6) | 26.9 (8.9) | 22.4 (9.3) | 23.3 (10.5) | |
| Range | 4–52 | 3–53 | 0–54 | 10–49 | 5–51 | 0–54 | |
| DP score* | Low (0–8) | 211 (83) | 605 (79) | 240 (73) | 70 (74) | 88 (91) | 1215 (79) |
| Medium (9–13) | 28 (11) | 104 (14) | 58 (18) | 17 (18) | 8 (8) | 215 (14) | |
| High (14–30) | 16 (6) | 54 (7) | 32 (10) | 8 (8) | 1 (1) | 111 (7) | |
| Mean (SD) | 4.8 (4.8) | 5.0 (4.9) | 6.1 (5.1) | 6.0 (5.1) | 3.8 (3.1) | 5.2 (4.9) | |
| Range | 0–26 | 0–26 | 0–24 | 0–24 | 0–14 | 0–26 | |
| PA score* | Low (0–30) | 30 (12) | 104 (14) | 40 (12) | 12 (13) | 9 (9) | 195 (13) |
| Medium (31–36) | 67 (26) | 211 (28) | 67 (20) | 34 (36) | 17 (17) | 396 (26) | |
| High (37–48) | 158 (62) | 448 (59) | 223 (68) | 49 (52) | 72 (73) | 950 (62) | |
| Mean (SD) | 37.6 (5.7) | 37.0 (6.3) | 38.4 (6.7) | 35.7 (6.0) | 39.0 (5.5) | 37.5 (6.3) | |
| Range | 19–48 | 6–48 | 0–48 | 16–47 | 22–48 | 0–48 | |
Values are n (%). The sum of percentages may be more than 100% due to rounding. SD indicates standard deviation.
Higher EE scores, DP scores, and PA scores indicate greater levels of emotional exhaustion, depersonalization, and personal accomplishment, respectively.
Overall, the prevalence of burnout, defined by EE mean ≥ 27 and/or DP mean ≥ 10, was 40% with significant differences across disciplines (P < .05) (Figure 2). Pharmacists had the highest prevalence, with over one-half meeting the threshold, whereas social workers had the lowest, at less than one-third.
Figure 2.
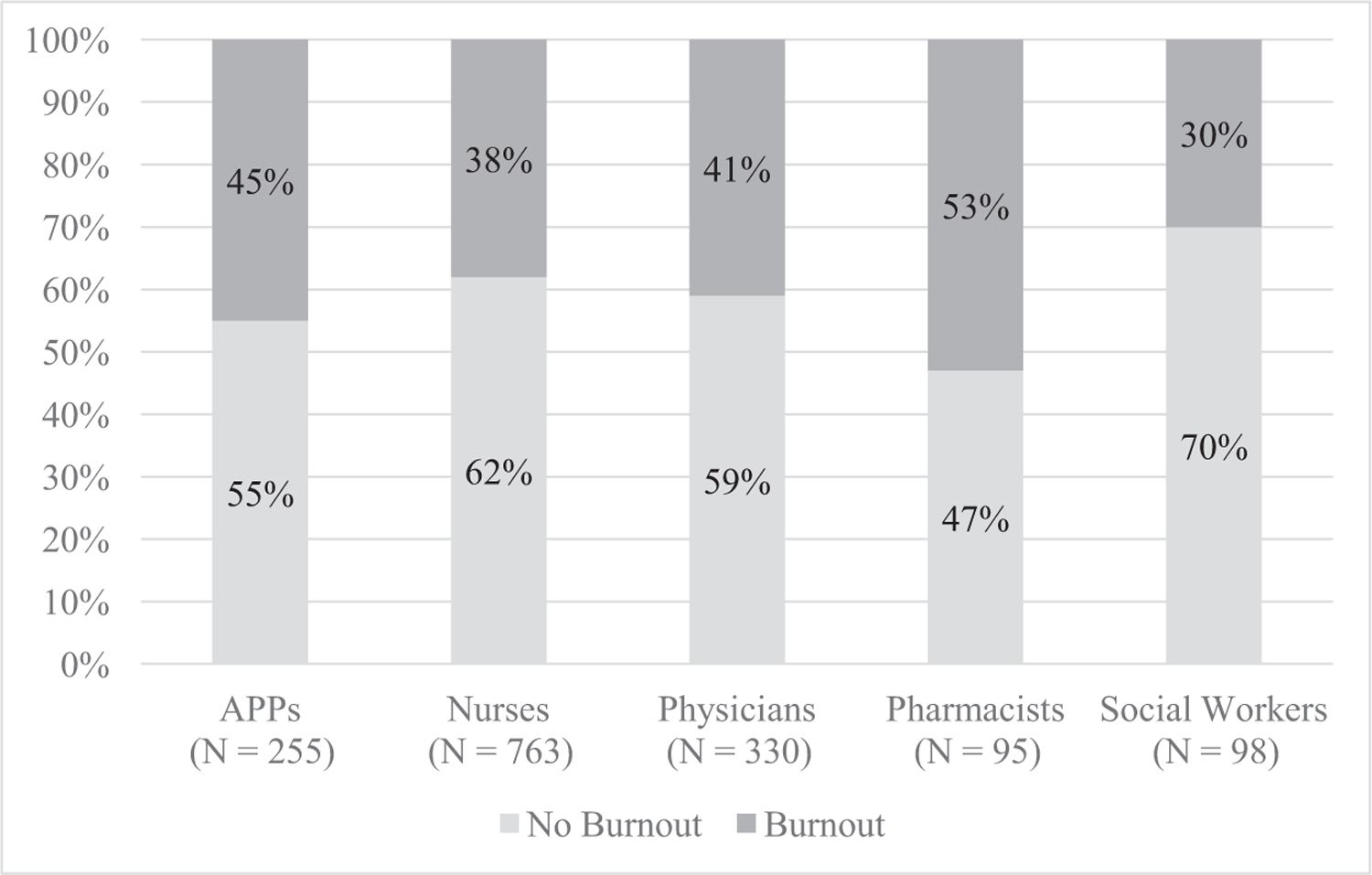
Prevalence of burnout by discipline,* defined as ≥27 on emotional exhaustion score and/or ≥10 on depersonalization score, by discipline. *Significant differences in prevalence of burnout existed across disciplines (P < .05).
Moral Distress
Scores for moral distress were significantly different across disciplines (P < .0001) (Table 3). Pharmacists had the largest percentage in the high score group followed by nurses, who also had the widest range of scores (0 to 231). Physicians and social workers had significantly lower scores than APPs, nurses, and pharmacists (P < .05); physicians had significantly higher scores than social workers (P < .05). Social workers had the largest percentage of low scores and the lowest mean and narrowest range of scores.
Table 3.
MDS-R Scores and Ranges by Discipline
| MDS Score | APPs (n = 255) | Nurses (n = 763) | Physicians (n = 330) | Pharmacists (n = 95) | Social Workers (n = 98) | Total (n = 1541) |
|---|---|---|---|---|---|---|
| Low (≤43) | 70 (27) | 241 (32) | 128 (39) | 31 (33) | 60 (61) | 530 (34) |
| Medium (44–63) | 94 (37) | 236 (31) | 116 (35) | 24 (25) | 20 (20) | 490 (32) |
| High (>63) | 91 (36) | 286 (37) | 86 (26) | 40 (42) | 18 (18) | 521 (34) |
| Mean (SD) | 61.2 (30.0) | 62.3 (37.2) | 52.0 (28.9) | 62.9 (34.8) | 42.7 (24.4) | 58.7 (34.0) |
| Range (0–336) | 1–172 | 0–231 | 0–195 | 5–192 | 5–121 | 0–231 |
Values are n (%). Low, medium, and high scores are based on 33% percentiles of scores of total respondents. Higher scores indicate higher degrees of moral distress.
Work–Life Balance, Career Satisfaction, and Burnout
When asked if their work schedule provided enough time for personal/family life, a greater percentage of respondents in all disciplines reported adequate work–life balance (strongly agreed or agreed with statement) versus inadequate (strongly disagreed or disagreed with statement) except physicians (Figure 3A). Only 31% of physicians reported adequate work–life balance. Burnout was significantly associated with work–life balance within each discipline (P < .05) (Figure 3B). Of the HCT professionals with burnout, 72% of physicians responded that their work schedule did not provide them enough time for personal or family life, followed by APPs (57%), pharmacists (50%), social workers (35%), and nurses (32%).
Figure 3.
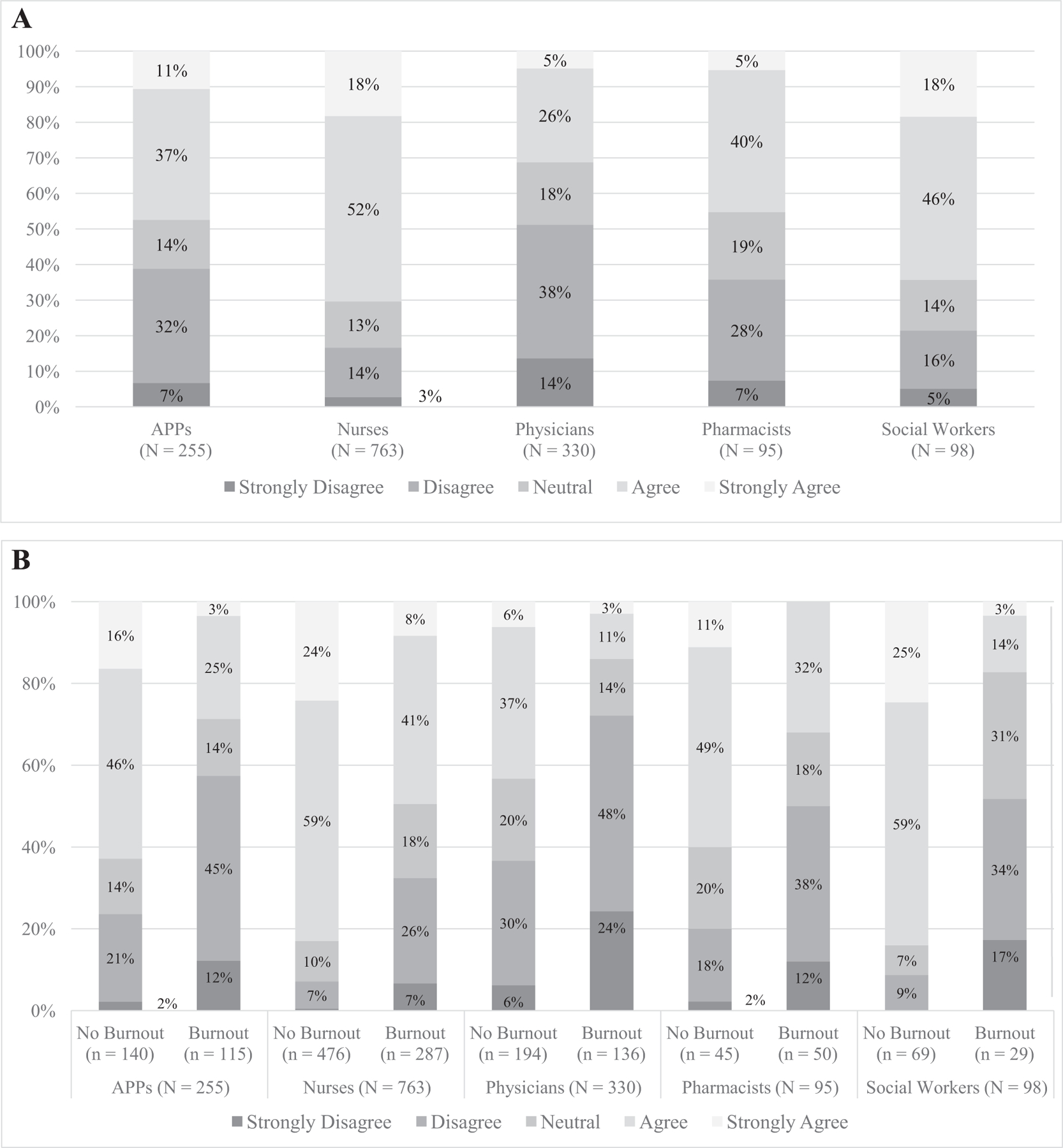
(A) Work–life balance (determined by level of agreement with statement, “My work schedule leaves me enough time for personal/family life”) by discipline. (B) Work–life balance (determined by level of agreement with statement, “My work schedule leaves me enough time for personal/family life”) by burnout* and discipline. *Burnout is significantly associated with work–life balance for all disciplines (P < .05).
The overwhelming majority of respondents (93% to 97%) across disciplines reported a high level of career satisfaction (Figure 4A). Burnout was also found to be significantly associated with career satisfaction within each discipline (P < .05) (Figure 4B). HCT professionals who had burnout reported relatively lower levels of agreement to the career satisfaction statement (ranging from 62% for social workers to 88% for pharmacists). Respondents across all disciplines indicated that emotional gratification and the hope and promise HCT treatment offered to patients were the 2 most important aspects of their work (data not shown).
Figure 4.
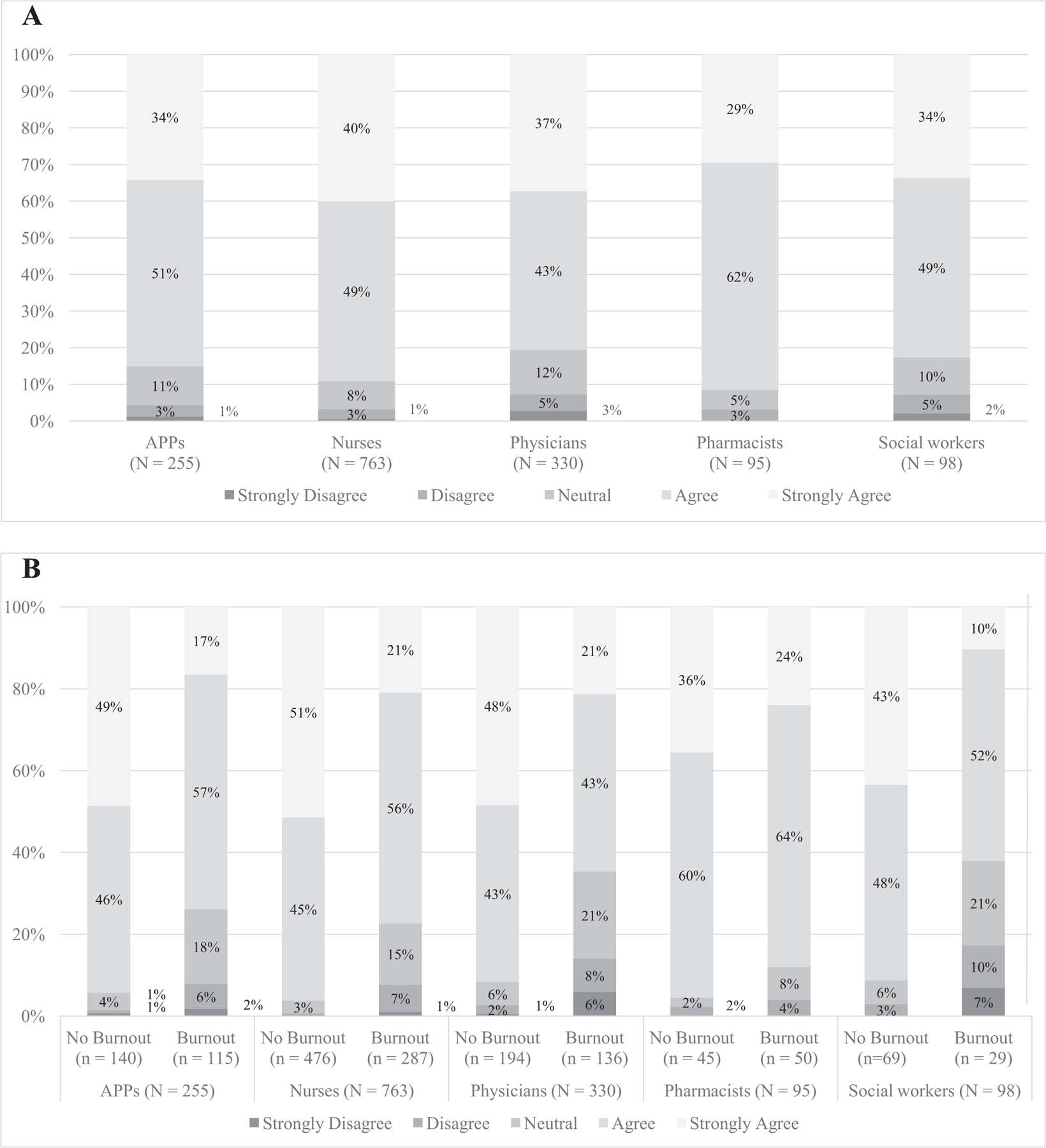
(A) Career satisfaction (determined by level of agreement to “I am satisfied with my career in hematopoietic cell transplantation”) by discipline. (B) Career satisfaction (determined by level of agreement to “I am satisfied with my career in hematopoietic cell transplantation”) by burnout* and discipline. *Burnout is significantly associated with career satisfaction for all disciplines (P < .05).
Predictors for EE, DP, and Burnout
Emotional exhaustion
Multivariable linear regression models on EE scores by discipline are presented in Supplementary Table S1. Female and single physicians had significantly higher EE scores than their comparison groups. Any number of nights on call per month and more than 10 hours spent per week working at home were significantly associated with higher levels of EE in physicians. In contrast, over 6 nights on call per month was associated with less EE than no call nights.
Multiple work-related variables were significantly associated with EE scores in the nurse respondents. Nurses working in the inpatient compared with outpatient setting had lower EE. Nurses who worked 51 to 60 hours per week (versus ≤40) and >10 working hours on research tasks at home (versus 0 to 10 hours) had significantly higher EE scores. Nurses who reported spending >10 hours per week on certification tasks reported less EE. Nurses who cared for both adult and pediatric patients had lower EE scores, compared with those who worked with adult patients only. Nurses who worked in centers with allogeneic transplantation volume >150 per year (versus 0 to 50) had higher EE. Significant variables for EE among pharmacists included working in the inpatient or both outpatient and inpatient settings compared with only the outpatient setting. Pharmacists who served pediatric patients had lower EE compared with pharmacists who served adult patients only. Higher total HCT volume of the transplant center (51 to 150 versus 0 to 50 transplants a year) was associated with lower levels of EE score in pharmacists.
Depersonalization
Overall, few variables were associated with DP in the linear regression model (Supplementary Table S2), and for physicians and pharmacists none reached statistical significance. APPs who worked >20 hours on patient care experienced or >20 hours per week on administrative tasks had higher DP. Higher number of working hours on research tasks at home and total allogeneic HCT volume (51 to 150, >150 versus 0 to 50) were associated with higher DP in nurses, whereas higher total autologous HCT volume (>150) was associated with lower level of DP. Compared with younger nurses (ages 20 to 29), nurses aged 40 years and older (40 to 49, 50 to 59, 60+) had lower DP scores. Social workers spending >41 hours per week on patient care had higher DP.
Burnout
Multivariable analysis for burnout in the APP, nurse, and physician disciplines is shown in Table 4. The only variable that impacted burnout for all disciplines was the moral distress score, with each additional point increasing the risk of burnout by 2%. Nurses working in an inpatient setting had a 42% lower probability of burnout than nurses working in an outpatient setting, and nurses working 51 to 60 hours weekly had a 2.37-fold increased burnout than those working ≤ 40 hours per week. Compared with having no nights on call per month, 1 to 5 nights on call per month was significantly associated with an increased burnout in nurses. Nurse respondents working at centers with higher volumes (51 to 150, 150+) had 86% and 96% increased risk of burnout compared with those working at centers with lower HCT volume (0 to 50), respectively. An increased burnout was also found in physicians who were on call 6 nights per month. More hours spent working at home per week (>10 hours) more than doubled the presence of burnout in physicians. Univariate analyses were conducted for the pharmacist and social worker groups because of the small numbers of respondents (Supplementary Table S3). The only significant variable for burnout was the moral distress scale score; each score point increased the incidence of burnout by 2% and 3% for pharmacists and social workers, respectively.
Table 4.
Multivariate Logistic Regression on Burnout by Discipline: APPS, Nurses, and Physicians
| Characteristic | APPS |
Nurses |
Physicians |
||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | |
| Age, yr (ref: 20–29) | |||||||||
| 30–39 | 1.18 | (.33–4.26) | .8016 | .86 | (.49–1.50) | 5881 | R | R | R |
| 40–49 | 2.73 | (.63–11.83) | 1800 | 1.06 | (.54–2.06) | .8674 | .69 | (.22–2.20) | .5332 |
| 50–59 | 2.18 | (.47–10.18) | .3233 | .79 | (.41–1.54) | .4856 | .48 | (.11–211) | 3301 |
| ≥60 | – | – | – | – | – | 1.39 | (.26–7.49) | .7040 | |
| Gender (ref: male) | |||||||||
| Female | .92 | (.27–3.19) | .8990 | .98 | (.37–2.62) | .9668 | 1.61 | (.88–2.97) | .1243 |
| Relationship status (ref: married/partnered) | |||||||||
| Divorced/widowed/widower | 1.91 | (.45–8.05) | .3767 | 1.09 | (.54–2.18) | .8188 | 1.96 | (.51–7.52) | .3290 |
| Single | 1.73 | (.69–4.34) | .2402 | 1.13 | (.70–1.82) | .6255 | .44 | (.14–1.41) | .1662 |
| Number of dependents (ref: 0) | |||||||||
| 1–2 | 1.16 | (.53–2.53) | .7079 | 1.15 | (.75–1.77) | .5206 | 1.10 | (.54–2.27) | .7908 |
| 3+ | .84 | (.24–2.91) | .7780 | .71 | (.37–1.35) | .2981 | 1.62 | (.71–3.67) | .2516 |
| Work setting (ref: outpatient) | |||||||||
| Inpatient | .65 | (.27–1.59) | .3455 | .58 | (.38-.89) | .0118 | .16 | (.01–1.84) | .1413 |
| Outpatient and inpatient both | .98 | (.44–2.18) | .9531 | .73 | (.41–1.28) | .2704 | 1.14 | (.22–6.02) | .8765 |
| Average hours worked/week (ref: ≤40) | |||||||||
| 41–50 | 1.60 | (.56–4.56) | .3802 | 1.07 | (.70–1.61) | .7653 | R | R | R |
| 51–60 | 3.15 | (.99–10.08) | .0528 | 2.37 | (1.15–4.89) | .0192 | 2.85 | (1.00–813) | .0510 |
| ≥61 | .99 | (.18–5.39) | .9931 | 2.08 | (.72–6.01) | .1773 | 2.24 | (.79–6.33) | .1301 |
| Nights/month on call (ref: 0 nights) | |||||||||
| 1–5 nights | .32 | (.09–1.11) | .0730 | 2.33 | (1.26–4.29) | .0069 | 3.32 | (1.24–8.88) | .0170 |
| ≥6 nights | 1.12 | (.22–5.74) | .8928 | 1.00 | (.40–2.46) | .9907 | 3.08 | (1.12–8.45) | .0288 |
| Hours/week spent on patient care (ref: 0–20) | |||||||||
| 21–40 | 1.71 | (.64–4.56) | .2855 | .94 | (.59–1.51) | .8006 | 1.91 | (.95–3.84) | .0713 |
| ≥41 | 1.41 | (.48–4.12) | .5307 | .96 | (.51–1.81) | .8946 | 1.30 | (.58–2.92) | .5266 |
| Hours/week on administration (ref: ≥20) | |||||||||
| >20 | 1.70 | (.68–4.22) | .2565 | 1.21 | (.76–1.94) | .4273 | 1.20 | (.59–2.43) | .6163 |
| Hours/week working at home (ref: 0–10) | |||||||||
| >10 | 1.67 | (.64–4.35) | .2941 | .56 | (.26–1.21) | .1385 | 2.54 | (1.32–4.89) | .0054 |
| Hours/week spent on research tasks at home (ref: 0–10) | |||||||||
| >10 | .32 | (.08–1.40) | .1319 | 2.21 | (.86–5.66) | .0982 | 1.28 | (.67–2.46) | .4514 |
| Hours/week spent on certification tasks (ref: 0–10) | |||||||||
| >10 | .98 | (.34–2.79) | .9683 | .61 | (.36–1.04) | .0678 | 1.33 | (.56–3.21) | .5199 |
| Patient population (ref: adult) | |||||||||
| Pediatric | .51 | (.19–1.42) | .1986 | .95 | (.57–1.59) | .8459 | 1.04 | (.47–2.29) | .9250 |
| Both | .69 | (.17–2.80) | .6022 | .59 | (.33–1.05) | .0704 | 2.33 | (.99–5.50) | .0537 |
| Total transplant volume (ref: 0–50) | |||||||||
| 51–150 | 2.28 | (.76–6.84) | .1425 | 1.86 | (1.06–3.27) | .0311 | .76 | (.33–1.73) | .5116 |
| >150 | 1.85 | (.60–5.70) | .2860 | 1.96 | (1.11–3.44) | .0200 | .71 | (.30–1.70) | .4388 |
| Unknown | NI | NI | NI | 1.70 | (.91–3.19) | .0981 | NI | NI | NI |
| MDS-R score | 1.02 | (1.01–1.04) | <.0001 | 1.02 | (1.02–1.03) | <.0001 | 1.02 | (1.01–1.04) | <.0001 |
Significant variables are in bold. OR indicates odds ratio; CI, confidence interval; ref, reference group; NI, not included in model because APPs and physicians had very few missing values for total transplant volume.
DISCUSSION
This is the first study published to date that specifically examines multidisciplinary HCT healthcare professionals’ experiences with burnout, moral distress, career satisfaction, and work–life balance. Work-related distress varied among the HCT disciplines but had significant prevalence for all. Burnout was associated with career satisfaction and work–life balance for all disciplines. Statistically significant differences between the disciplines in burnout, EE, and DP were expected because of the differences in roles and job functions. The overall burnout rate across disciplines of 40% in this study is comparable with that of other studies in the disciplines of medicine [7,14], nursing [23,25], and critical care [26]. We also found that pharmacists had the highest percentage of burnout, highest mean score on the EE subscale, and lowest PA score. Comparison studies are extremely limited or completely lacking for the disciplines of APPs, pharmacy, and social work, further emphasizing the contribution of this study to these fields.
Predictors for Burnout and Moral Distress by Discipline
Professional and work-related factors were associated with burnout and its corollaries EE and DP in all disciplines. Only physicians and nurses had personal demographic factors that were associated with EE or DP. APP and pharmacist respondents had the highest percentage of burnout and highest EE scores among all disciplines; although specific variables differed between the disciplines, they reflect work-related stressors in APP and pharmacist roles that have been confirmed in the few discipline-specific studies available [27–29].
The only significant variable for burnout in all disciplines was moral distress. Physicians’ scores on the MDS-R were lower than nurses, APPs, and pharmacists, which has been reported in other studies [24,30–32] and may be attributed in part because of the decision authority they possess [24]. Moral distress has been well studied in the nursing field, but few studies exist that include other healthcare professionals, and no previous multidisciplinary study has specifically examined the relationship between burnout and moral distress. Moral distress has not been noted in pharmacist professional literature in the United States; however, UK researchers recently reported on a moral distress instrument developed for pharmacy practice, perhaps reflecting an increased professional interest in this area [33]. A study [34] examining burnout and resilience of nurses in high acuity care settings did identify a correlation between moral distress and burnout (r = .49, P < .01).
Advanced Practice Professionals
The medical literature supports findings that a work schedule with a high demand for direct patient care and additional administrative tasks leaves little time for personal and professional development activities and increases the risk of burnout [7,35]. Administrative tasks, including expanded use of electronic medical records, have contributed to increased burnout [35]. An increased number of patient care hours per week and over 20 hours per week on administrative tasks resulted in increased EE and DP for APPs. APPs share responsibility with the physician for direct patient care at most HCT centers; these results, albeit not demonstrated in the physician group, may indicate the increased demand on APPs. A work schedule that includes nights on call was associated with less EE for APPs and may be explained by a preference of some to work off-shift, providing an alteration in workload and salary increase.
Nurses
Nurse respondents had the greatest number of predictors associated with burnout. Among nurses, age was significantly associated with DP, with progressive decrease in DP for every decade past 40, a finding reflected in an earlier study [23]. Inpatient nurses experienced less EE and burnout than nurses working outpatient, similar to the Davis et al. study [23]. This may be attributable to the fact that HCT nurses have numerous work opportunities (clinical inpatient or outpatient nursing, HCT coordinator, research nurse, working part-time), allowing for flexibility if 1 setting becomes too stressful, and outpatient HCT nurses experience increased demands with high acuity outpatients, expanded clinic hours, and longer-term relationships with patients and families. Nurses were the only group who reported increased EE and burnout when working 51 hours per week or performing research-related tasks at home. Most clinical nurses work shifts with full-time equivalents of 36 to 40 hours per week; these additional hours may be reflective of unusual workload (elective or mandatory undetermined) and an interference with work–life balance.
Interestingly, nurses who spent more time on certification tasks reported less EE, presumably because it may be time provided by employers and the fact that certification affords them an increased sense of personal accomplishment. Nurses who work on a combined pediatric and adult unit had a decrease in EE, perhaps because of the hope and promise HCT has for patients. Level of nursing experience was not associated with EE, unlike another study that reported an increase in EE with less experience in pediatric HCT nurses [36]; however we did not examine pediatric nurses separately from adult nurses in this cohort. Nurses who worked in larger HCT programs experienced increased burnout. Our findings support those of others in that high acuity work environments, which expose nurses to increased number of patients with complex treatment and subsequently more patient deaths, contributes to workplace stress, burnout, and depersonalization [25].
Physicians
Physicians were the only group in which personal factors significantly influenced EE. Being female and single were both associated with increased EE, similar to the findings of a study of US oncologists [7]. Physicians in this study had a higher mean score for DP than previously reported for oncologists [7,12]. Physicians who were 60 years or older had less DP, but this did not reach statistical significance (P = .0662); however, age was a significant variable in a previous mentioned study in which younger physicians were reported to experience increase burnout [7,37]. For HCT physicians, nights on call increased EE—likely representing an additional burden because of need to work the following day as well. Nights on call increased burnout for physicians and has been recognized to negatively affect work–life balance for physicians [12]. Working at home, which likely interferes with work–life balance, was another factor that resulted in increased EE and burnout for physicians.
Pharmacists
Personal factors have been reported to be associated with burnout for pharmacist in another study but were not revealed in this study [38]. Pharmacists who worked inpatient only or in combination with outpatient settings experienced higher EE, which may be due to the higher acuity and intensity of pharmacologic management in that setting. This could also reflect competing demands that pharmacists experience with medication distribution versus clinical roles. Job stress, role ambiguity, and role conflict has been reported in hospital pharmacists [29].
Pharmacists working exclusively in pediatrics and in larger size programs had a decrease in EE. This decrease may be because of the hope and promise HCT has for pediatric patients and the fact that larger size programs may allow pharmacists to focus solely on HCT versus multiple services and provides for better collaboration with interprofessional HCT team.
Social Workers
Increased number of patient care hours per week resulted in increased DP in social workers and was the only factor that illustrated any significant work-related or personal factors for social workers. Interestingly, in our study social workers had the lowest mean for moral distress, highest mean on PA subscale, the lowest percentage of burnout, in addition to high level of agreement with career satisfaction. Burnout has been correlated with compassion fatigue (r = .47, P < .05) in oncology social workers [39]. The lower prevalence of EE, DP, and burnout in the social worker group could be reflective of the nature of their training, expertise, and work that stresses coping skill development [40]. This is a novel finding, because there are no reported comparison studies in the United States.
Impact of Burnout on Career Satisfaction and Work–Life Balance
Burnout was associated with work–life balance and career satisfaction for all disciplines. Those respondents with burnout were more likely to report dissatisfaction with the amount of time for personal and family life or work–life balance, indicating the impact of highly demanding work in HCT. Most of these respondents expressed a high sense of personal accomplishment in their work, and despite burnout and dissatisfaction with work–life balance, most respondents in this study and in related medical [7] and nursing studies expressed agreement with satisfaction related to career. This may be reflective of the emotional gratification of the care they provide and the hope and promise HCT offers patients, as indicated by the survey question about satisfying aspects of HCT work. Being able to recognize the positive attributes of the work in HCT will help practitioners encourage and mentor trainees to enter the field.
Burnout in healthcare, including its impact on quality of care, has gained wide public recognition [27,28,41,42]. Research studies on the topic [7,12,13,41,43,44] have been discussed in the national public forum. The US Surgeon General has identified this as an urgent situation because of the increased demand for healthcare providers to meet the needs of an aging population [45]. The Critical Care Societies Collaborative, which represents 4 critical care professional associations, has published a call to action to deal with professional burnout. Professional organizations including the American Society of Clinical Oncology [42], American Medical Association, American Society of Blood and Marrow Transplantation, American Nurses Association, Oncology Nursing Society, and Hematology/Oncology Pharmacy Association developed web-based programs and presentations at national meetings addressing this issue.
Methods to intervene and mitigate burnout and moral distress have been suggested [7,12,13,41] and studied. Several studies examined the benefit of counseling or training programs for providers working in settings where burnout or moral distress is high [34,41,46]. Interventions focusing on clinicians’ personal well-being and professional satisfaction have stressed the importance of symptom recognition, professional advice, and planning and incorporating resiliency strategies [34,42,43,47]. Resiliency strategies have included mindfulness-based stress reduction, self-confidence building, communication skills, finding meaning, and physical exercise. Research, including this study, supports that work-related distress is influenced by the healthcare system and that solutions must also include an organizational approach to be successful [34,42,46–49].
Organizational interventions have focused on changes to improve practice environment, increase professional engagement, and team building. Medical practice interventions, such as altering length of direct care rotations and work hours, support for clerical responsibilities, built-in protected time, and senior leadership rounds [42,43,50,51], have been examined and successful in reducing factors associated with burnout. Team-building activities, such as serial discussion groups, have demonstrated increase interpersonal and interprofessional understanding and building of more cohesive teams with shared experiences [31,47,52].
Medical schools (and some nursing programs) have started to recognize the need to address issues of work-related stress. Curricula including content about maintaining personal well-being and professional satisfaction have been somewhat successful, although evidence suggests that programs are less beneficial when mandatory [53]. It is clear that to successfully address work-related distress, a multifaceted approach that incorporates actions of the individual provider, healthcare institutions, and support of professional organizations are needed.
LIMITATIONS
This study has several limitations. Although initial response rates were lower than expected, the addition of an open link invitation made it possible to achieve adequate numbers of participants to examine trends and correlations between and within professional groups. A disadvantage was the lack of an accurate number of potential respondents (total and discipline specific), thereby potentially skewing the response rate. The numbers of pharmacy and social work participants were particularly low, limiting the analysis and generalizability of the findings for those groups. Most respondents were from larger HCT centers and so may not reflect situations at smaller size centers. Inviting professionals who are members of professional organizations who may have a higher level of commitment may contribute bias to the results. Despite these limitations this research provides important data related to the prevalence of burnout and moral distress as well as the associated impact and perception of career satisfaction and work–life balance of HCT professionals, which ultimately impacts the delivery of quality care to HCT patients.
CONCLUSIONS
This study contributes significantly to a cross-sectional illustration of burnout and moral distress within and between diverse HCT healthcare professionals. Burnout and moral distress were experienced across HCT professional groups; however, the degree to which they occurred and the associated variables contributing to their occurrence varied greatly within and between groups. The data from this study may be used to highlight identifiable contributors to burnout and moral distress within the professional subgroups. As the creation of healthy work environments is increasingly emphasized to improve quality care and decrease costs, these findings should be used by HCT leadership to develop interventions that mitigate work-related distress and in turn promote recruitment and retention of HCT providers. Further work should address how to remediate these experiences, provide resources to ameliorate their consequences, and identify how to foster work environments in which professional and personal boundaries are well established to promote a healthy and flourishing workforce.
Supplementary Material
ACKNOWLEDGMENTS
The authors appreciate the enormous assistance of the National Marrow Donor Program/Be the Match. The authors thank the professional organizations that assisted in the recruitment of participants, namely the American Society for Blood and Marrow Transplant, Oncology Nursing Society, Association of Oncology Social Work, Association of Pediatric Hematology/Oncology Nurses, and Association of Pediatric Oncology Social Workers. The authors also want to thank the physicians, nurses, nurse practitioner, physician assistants, advanced practice nurses, pharmacists, and social workers who participated in our study and who work so diligently to care for our HCT patients and their families.
Footnotes
Financial disclosure: The authors have nothing to disclose.
Conflict of interest statement: There are no conflicts of interest to report.
SUPPLEMENTARY DATA
Supplementary data related to this article can be found online at doi:10.1016/j.bbmt.2017.11.015.
REFERENCES
- 1.Majhail NS, Murphy EA, Denzen EM, et al. The National Marrow Donor Program’s Symposium on Hematopoietic Cell Transplantation in 2020: a health care resource and infrastructure assessment. Biol Blood Marrow Transplant 2012;18:172–182. [DOI] [PubMed] [Google Scholar]
- 2.Denzen EM, Majhail NS, Stickney Ferguson S, et al. Hematopoietic cell transplantation in 2020: summary of year 2 recommendations of the National Marrow Donor Program’s System Capacity Initiative. Biol Blood Marrow Transplant 2013;19:4–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Burns LJ, Gajewski JL, Majhail NS, et al. Challenges and potential solutions for recruitment and retention of hematopoietic cell transplantation physicians: the National Marrow Donor Program’s System Capacity Initiative Physician Workforce Group report. Biol Blood Marrow Transplant 2014;20:617–621. [DOI] [PubMed] [Google Scholar]
- 4.Aycock N, Boyle D. Interventions to manage compassion fatigue in oncology nursing. Clin J Oncol Nurs 2009;13:183–191. [DOI] [PubMed] [Google Scholar]
- 5.Cooke L, Gemmill R, Kravits K, Grant M. Psychological issues of stem cell transplant. Semin Oncol Nurs 2009;25:139–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Demirci S, Yildirim YK, Ozsaran Z, Uslu R, Yalman D, Aras AB. Evaluation of burnout syndrome in oncology employees. Med Oncol 2010;27:968–974. [DOI] [PubMed] [Google Scholar]
- 7.Shanafelt TD, Gradishar WJ, Kosty M, et al. Burnout and career satisfaction among US oncologists. J Clin Oncol 2014;32:678–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maslach C, Jackson S, Leiter M. Burnout Inventory Manual 4th ed. Menlo Park, CA: Mind Garden, Inc.; 2014. [Google Scholar]
- 9.Kovacs M, Kovacs E, Hegedus K. Is emotional dissonance more prevalent in oncology care? Emotion work, burnout and coping. Psychooncology 2010;19:855–862. [DOI] [PubMed] [Google Scholar]
- 10.Lederer W, Kinzl JF, Traweger C, Dosch J, Sumann G. Fully developed burnout and burnout risk in intensive care personnel at a university hospital. Anaesth Intensive Care 2008;36:208–213. [DOI] [PubMed] [Google Scholar]
- 11.Sherman AC, Edwards D, Simonton S, Mehta P. Caregiver stress and burnout in an oncology unit. Palliat Support Care 2006;4:65–80. [DOI] [PubMed] [Google Scholar]
- 12.Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med 2012;172:1377–1385. [DOI] [PubMed] [Google Scholar]
- 13.Shanafelt TD, Raymond M, Kosty M, et al. Satisfaction with work-life balance and the career and retirement plans of US oncologists. J Clin Oncol 2014;32:1127–1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Whippen DA, Canellos GP. Burnout syndrome in the practice of oncology: results of a random survey of 1,000 oncologists. J Clin Oncol 1991;9:1916–1920. [DOI] [PubMed] [Google Scholar]
- 15.Leung D, Fillion L, Duval S, Brown J, Rodin G, Howell D. Meaning in bone marrow transplant nurses’ work: experiences before and after a “meaning-centered” intervention. Cancer Nurs 2012;35:374–381. [DOI] [PubMed] [Google Scholar]
- 16.Molassiotis A, Haberman M. Evaluation of burnout and job satisfaction in marrow transplant nurses. Cancer Nurs 1996;19:360–367. [DOI] [PubMed] [Google Scholar]
- 17.Molassiotis A, van den Akker OB, Boughton BJ. Psychological stress in nursing and medical staff on bone marrow transplant units. Bone Marrow Transplant 1995;15:449–454. [PubMed] [Google Scholar]
- 18.Houston S, Casanova MA, Leveille M, et al. The intensity and frequency of moral distress among different healthcare disciplines. J Clin Ethics 2013;24:98–112. [PubMed] [Google Scholar]
- 19.Corley MC. Nurse moral distress: a proposed theory and research agenda. Nurs Ethics 2002;9:636–650. [DOI] [PubMed] [Google Scholar]
- 20.Allen R, Judkins-Cohn T, de Velasco R, et al. Moral distress among healthcare professionals at a health system. JONAS Healthc Law Ethics Regul 2013;15:111–118, quiz 119–120. [DOI] [PubMed] [Google Scholar]
- 21.Hamric AB. Empirical research on moral distress: issues, challenges, and opportunities. HEC Forum 2012;24:39–49. [DOI] [PubMed] [Google Scholar]
- 22.Dillman DA, Smyth JD, Christian LM. Internet, Mail, and Mixed-Mode Surveys: the Tailored Design Method Hoboken, NJ: Wiley Publishing; 2008. [Google Scholar]
- 23.Davis S, Lind BK, Sorensen C. A comparison of burnout among oncology nurses working in adult and pediatric inpatient and outpatient settings. Oncol Nurs Forum 2013;40:E303–E311. [DOI] [PubMed] [Google Scholar]
- 24.Hamric AB, Epstein EG. Development and testing of an instrument to measure moral distress in healthcare professionals. AJOB Prim Res 2012;3:1–9.26137345 [Google Scholar]
- 25.Potter P, Deshields T, Divanbeigi J, et al. Compassion fatigue and burnout: prevalence among oncology nurses. Clin J Oncol Nurs 2010;14:E56–E62. [DOI] [PubMed] [Google Scholar]
- 26.Moss M, Good VS, Gozal D, Kleinpell R, Sessler CN. A critical care societies collaborative statement: burnout syndrome in critical care health-care professionals. A call for action. Am J Respir Crit Care Med 2016;194:106–113. [DOI] [PubMed] [Google Scholar]
- 27.Almost J, Laschinger HK. Workplace empowerment, collaborative work relationships, and job strain in nurse practitioners. J Am Acad Nurse Pract 2002;14:408–420. [DOI] [PubMed] [Google Scholar]
- 28.Gilles I, Burnand B, Peytremann-Bridevaux I. Factors associated with healthcare professionals’ intent to stay in hospital: a comparison across five occupational categories. Int J Qual Health Care 2014;26:158–166. [DOI] [PubMed] [Google Scholar]
- 29.Mott DA, Doucette WR, Gaither CA, Pedersen CA, Schommer JC. Pharmacists’ attitudes toward worklife: results from a national survey of pharmacists. J Am Pharm Assoc 2004;44:326–336. [DOI] [PubMed] [Google Scholar]
- 30.Dodek PM, Wong H, Norena M, et al. Moral distress in intensive care unit professionals is associated with profession, age, and years of experience. J Crit Care 2016;31:178–182. [DOI] [PubMed] [Google Scholar]
- 31.Lievrouw A, Vanheule S, Deveugele M, et al. Coping with moral distress in oncology practice: nurse and physician strategies. Oncol Nurs Forum 2016;43:505–512. [DOI] [PubMed] [Google Scholar]
- 32.Whitehead PB, Herbertson RK, Hamric AB, Epstein EG, Fisher JM. Moral distress among healthcare professionals: report of an institution-wide survey. J Nurs Scholarsh 2015;47:117–125. [DOI] [PubMed] [Google Scholar]
- 33.Astbury JL, Gallagher CT. Development and validation of a questionnaire to measure moral distress in community pharmacists. Int J Clin Pharm 2017;39:156–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rushton CH, Batcheller J, Schroeder K, Donohue P. Burnout and resilience among nurses practicing in high-intensity settings. Am J Crit Care 2015;24:412–420. [DOI] [PubMed] [Google Scholar]
- 35.Shanafelt TD, Dyrbye LN, Sinsky C, et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc 2016;91:836–848. [DOI] [PubMed] [Google Scholar]
- 36.Gallagher R, Gormley DK. Perceptions of stress, burnout, and support systems in pediatric bone marrow transplantation nursing. Clin J Oncol Nurs 2009;13:681–685. [DOI] [PubMed] [Google Scholar]
- 37.Banerjee S, Califano R, Corral J, et al. Professional burnout in European young oncologists: results of the European Society For Medical Oncology (ESMO) young oncologists committee burnout survey. Ann Oncol 2017;28:1590–1596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lahoz MR, Mason HL. Burnout among pharmacists. Am Pharm 1990; NS30:28–32. [DOI] [PubMed] [Google Scholar]
- 39.Simon CE, Pryce JG, Roff LL, Klemmack D. Secondary traumatic stress and oncology social work: protecting compassion from fatigue and compromising the worker’s worldview. J Psychosoc Oncol 2005;23:1–14. [DOI] [PubMed] [Google Scholar]
- 40.National Marrow Donor Program® /Be The Match® Social Work Workforce Group. BMT clinical social worker role description 2014. Available at: http://asbmt.org/sites/default/files/dkotheimer/media/BMT%20Clinical%20Social%20Worker%20Role%20Description_2017.pdf. Accessed July 26, 2017.
- 41.Shanafelt T, Dyrbye L. Oncologist burnout: causes, consequences, and responses. J Clin Oncol 2012;30:1235–1241. [DOI] [PubMed] [Google Scholar]
- 42.Hlubocky FJ, Back AL, Shanafelt TD. Addressing burnout in oncology: why cancer care clinicians are at risk, what individuals can do, and how organizations can respond. Am Soc Clin Oncol Educ Book 2016;35:271–279. [DOI] [PubMed] [Google Scholar]
- 43.Panagioti M, Panagopoulou E, Bower P, et al. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis. JAMA Intern Med 2017;177:195–205. [DOI] [PubMed] [Google Scholar]
- 44.Shanafelt T, Adjei A, Meyskens FL. When your favorite patient relapses: physician grief and well-being in the practice of oncology. J Clin Oncol 2003;21:2616–2619. [DOI] [PubMed] [Google Scholar]
- 45.Frieden J Surgeon General concerned about physician burnout—if physicians aren’t happy, they can’t heal others 2016. Available at: https://www.medpagetoday.com/publichealthpolicy/generalprofessionalissues/57280. Accessed August 28, 2017.
- 46.Rushton CH, Caldwell M, Kurtz M. CE: moral distress: a catalyst in building moral resilience. Am J Nurs 2016;116:40–49. [DOI] [PubMed] [Google Scholar]
- 47.West CP, Dyrbye LN, Rabatin JT, et al. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med 2014;174:527–533. [DOI] [PubMed] [Google Scholar]
- 48.Pavlish C, Brown-Saltzman K, So L, Wong J. SUPPORT: an evidence-based model for leaders addressing moral distress. J Nurs Adm 2016;46:313–320. [DOI] [PubMed] [Google Scholar]
- 49.Swensen S, Shanafelt T. An organizational framework to reduce professional burnout and bring back joy in practice. Jt Comm J Qual Patient Saf 2017;43:308–313. [DOI] [PubMed] [Google Scholar]
- 50.Sexton JB, Schwartz SP, Chadwick WA, et al. The associations between work-life balance behaviours, teamwork climate and safety climate: cross-sectional survey introducing the work-life climate scale, psychometric properties, benchmarking data and future directions. BMJ Qual Saf 2017;26(8):632–640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shanafelt TD, Noseworthy JH. Executive leadership and physician well-being: nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc 2017;92:129–146. [DOI] [PubMed] [Google Scholar]
- 52.Wu S, Singh-Carlson S, Odell A, Reynolds G, Su Y. Compassion fatigue, burnout, and compassion satisfaction among oncology nurses in the United States and Canada. Oncol Nurs Forum 2016;43:E161–E169. [DOI] [PubMed] [Google Scholar]
- 53.Drybye LN, Shanafelt TD, Werner L, et al. The impact of a required longitudinal stress management and resilience training course for first-year medical students. J Gen Intern Med 2017;32:1309–1314. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


