Abstract
Objective
The COVID-19 pandemic is expected to have a sustained psychological impact on healthcare workers. We assessed individual characteristics related to changes in emotional exhaustion and psychological distress over time.
Methods
A survey of diverse hospital staff measured emotional exhaustion (Maslach Burnout Inventory) and psychological distress (K6) in Fall 2020 (T1) and Winter 2021 (T2). Relationships between occupational, personal, and psychological variables were assessed using repeated measures ANOVA.
Results
Of 539 T1 participants, 484 (89.9%) completed T2. Emotional exhaustion differed by occupational role (F = 7.3, p < .001; greatest in nurses), with increases over time in those with children (F = 8.5, p = .004) or elders (F = 4.0, p = .047). Psychological distress was inversely related to pandemic self-efficacy (F = 110.0, p < .001), with increases over time in those with children (F = 7.0, p = .008). Severe emotional exhaustion occurred in 41.1% (95%CI 36.6–45.4) at T1 and 49.8% (95%CI 45.4–54.2) at T2 (McNemar test p < .001). Psychological distress occurred in 9.7% (95%CI 7.1–12.2) at T1 and 11.6% (95%CI 8.8–14.4) at T2 (McNemar test p = .33).
Conclusions
Healthcare workers' psychological burden is high and rising as the pandemic persists. Ongoing support is warranted, especially for nurses and those with children and elders at home. Modifiable protective factors, restorative sleep and self-efficacy, merit special attention.
Keywords: Healthcare workers, Covid-19, Burnout, Mental health, Occupational health, Nursing
1. Introduction
The stress of healthcare work during the COVID-19 pandemic adds to high pre-existing levels of burnout and psychological symptoms. Professional burnout in healthcare workers consists of emotional exhaustion, a sense of diminished personal connection to patients, and a diminished sense of personal accomplishment [1]. Prior to the pandemic, prevalence of severe emotional exhaustion was reported to range from 30% to as high as 50% in some settings [[2], [3], [4]]. The prevalence of depression and suicide was also higher than in the general population [5,6].
Occupational stressors in healthcare settings have potentially been amplified during the pandemic. These include working in circumstances of high-demand/low-control or high-effort/low-reward [7,8], shift work and long shifts [9,10], sleep deprivation [11], and challenges to work-life balance, including conflicts between work and home responsibilities [12]. Protective factors include social support and self-efficacy [13,14]. Self-efficacy is the belief in one's capacity to achieve specific performance goals, which is often induced and maintained by experiences of mastery [15]. Self-efficacy refers to specific goals (e.g. capacity to work in a hospital during a pandemic) rather than to a general self-appraisal. Higher self-efficacy is associated with lower occupational burnout in healthcare workers and in other professions [13].
As of this writing, COVID-19 has infected over 148 million people and killed over 3 million worldwide, with over 1,000,000 cases and 24,000 deaths in Canada [16]. Healthcare workers reported high levels of distress early in the pandemic [[17], [18], [19]]. Ongoing stress may have effects that last for months or years afterwards [20]. In previous outbreaks, predictors of outcomes included the type of work done within the hospital, with greater impact documented in nurses, in those who worked in higher-risk areas, and in those who had greater exposure to infected patients [21,22].
In our work to provide peer support during COVID-19 [23], healthcare workers report the dual impact of stressors at work and at home, including social disconnection and isolation. Parents have felt strained by having school-age children at home with little warning due to unpredictable transitions between virtual and in-school teaching, classes dismissed because of new cases, and children staying home for isolation or testing when symptomatic. Further, healthcare workers providing care for elderly relatives, who are at the highest risk of serious illness and mortality [24], have noted strain and a reduction in support resources for seniors.
The purpose of this study is to use data collected from hospital-based healthcare workers in the fall of 2020 (prior to the peak of the second wave in Ontario, Canada) and in the winter of 2021 (immediately after a peak in cases) to assess the relationship of occupational roles, care for children and elders at home, sleep quality, and self-efficacy with respect to the occupational challenges of the pandemic, on changes in emotional exhaustion and psychological distress over this time.
2. Methods
A survey of the psychological well-being and experiences of a cohort of hospital staff, learners (nursing students, medical students, residents), and volunteers during the pandemic was conducted at two sites of Sinai Health (a general hospital and a rehabilitation hospital, with >6000 employed staff) in Toronto, Canada at two time-points. Invitations to participate were distributed through hospital communications and unit/department managers. The first survey (T1) was conducted from Sept 21-Nov 15, 2020. During that interval, daily COVID-19 cases/100,000 rose in Toronto from 8.1 to 13.0 (peak: 17.1, Nov 9). Participants who provided data at T1 were invited to participate in T2. The T2 survey interval, Jan 25-Feb 15 2021, followed a peak of 34.8 cases/100,000 on Jan 4 and occurred during a period of decreasing case rates from 17.3 to 7.9 [25]. The study was approved by the Sinai Health Research Ethics Board.
The first survey was open to all hospital employees, physicians, learners, volunteers, retail employees, and contractors, whether or not they had regular patient contact. All surveys were completed online using PHIPA-compliant software (Alchemer, Louiseville, CO). To facilitate randomization to a longer or shorter version of the survey (not reported here), the baseline survey was conducted in two phases (T0 and T1) spaced by about two weeks. The T0 survey collected demographic data, personal circumstances including whether or not the participant lived with children under the age of 18 or adults over the age of 60, location and type of work, a checklist of COVID-19-related experiences, and an email address at which to receive the invitation link for subsequent surveys. The T1 survey included the measures of emotional exhaustion, psychological distress, sleep quality, and pandemic self-efficacy. The T2 survey used the same instruments to re-measure these constructs. Only emotional exhaustion and psychological distress at T2 are included in this analysis.
Burnout was measured with the widely used Maslach Burnout Inventory (MBI), which includes scales for emotional exhaustion, depersonalization, and personal achievement [1]. When the MBI is used to define burnout categorically, researchers employ various definitions which depend on the choice of high or severe cut-off scores, and the choice of using the emotional exhaustion scale alone or various combinations of the three scales [26]. In order to allow comparison to a broad range of pre-pandemic studies in healthcare settings, we used the emotional exhaustion scale (9 items scored from 0 to 6, yielding a score from 0 to 54) for analysis as a continuous measure of burnout, and defined burnout categorically using a cut-off of ≥27 to indicate severe emotional exhaustion.
Psychological distress is a composite of depressive and anxiety symptoms which is measured dimensionally as an indicator of severity of common mental disorders [27] and with a validated cut-off as a screening test for likely mental disorder. Psychological distress was measured with the Kessler K6, which has 6 items scored from 0 to 4, yielding a range of 0–24 [27]. The K6 strongly discriminates between community cases and non-cases of psychiatric disorders diagnosed by structured interview [27] and has acceptable sensitivity and specificity [28]. A cut-off of ≥13 indicates likely serious mental illness [29].
Sleep quality was measured with a single item (“During the past 7 days, how would you rate your sleep quality overall?”) rated on an 11-point visual analogue scale (0 “terrible” to 10 “excellent”). This measure has strong inverse correlations with validated multi-item measures of sleep quality, discriminates between groups whose sleep quality is known, and has adequate test-retest reliability [30].
Self-efficacy for COVID-19 prevention and control self-efficacy was measured with an instrument developed for the 2009 H1N1 pandemic, revised to change the instruction “How confident are you now that in the event of an influenza pandemic you will be able to…” by removing the word influenza. It has 23 items probing confidence in one's ability to meet pandemic-related challenges (e.g. “trust in the infection control procedures that are in place”, “perform duties that are outside your usual job”) scored on a 5-point scale, yielding a score from 23 to 115. In preparation for H1N1, self-efficacy scores measured with this scale increased after pandemic–related training [31]. In the current study internal reliability was high (Cronbach's alpha = 0.94).
A gift card (about US$15 value) was provided for each completed survey (T0, T1, T2). One hundred and twenty-one respondents who completed the T0/T1 survey more than once (possibly to collect extra reward cards) were identified by duplication of email address and/or IP address, timing of survey, and response patterns and eliminated from both the dataset and the retention rate denominator.
2.1. Analysis
In order to identify hospital workers with different types of stressful exposure and different training and expertise, participants were sorted into categories of occupational role based on (i) professional qualifications (e.g, whether their job is regulated by a professional college) and (ii) close patient contact (within two metres of a patient for more than 15 min in the previous month). The four roles were nurses, other healthcare professionals, other clinical staff (non-professionals who reported close patient contact), and non-clinical roles. Nurses were analyzed separately based on evidence from the SARS outbreak that nurses experienced a greater burden of stress than other professionals [21,22].
Participant characteristics and COVID-19-related experiences were summarized using descriptive statistics. Continuous measures were summarized using means and standard deviations (SD). Categorical measures were summarized using counts and percentages. Occurrence of COVID-19-related experiences associated with greater exposure to risk, or to extraordinary job stresses (yes/no), were compared between job categories with differences tested using χ2 tests or Fisher's exact tests for low expected cell counts. Proportions of participants of each occupational role with high scores for psychological outcomes were calculated using validated cut-offs. Differences in proportions of high scores in the same group at two time-points were tested using the McNemar test.
Changes over time in emotional exhaustion and psychological distress by occupational role were analyzed using repeated measures ANOVA. We included as covariates pandemic self-efficacy at T1 (divided into terciles), having children at home (none/any), having adults over 60 at home (none/any), and T1 sleep quality (as a continuous measure). Because poor sleep quality can be understood as both a provocative factor for poor psychological outcomes and as a consequence of psychological distress which may vary over time, sleep quality was compared at T1 and T2 using paired t-tests which revealed no significant difference between timepoints (Cohen's d effect size 95% confidence interval −0.09–0.09). Prior to analysis, the covariates were assessed for multicollinearity (tolerance statistic < 0.4). Multicollinearity was not found to be a concern and therefore all variables were retained for the multivariable model. All analyses were done with IBS SPSS Statistics 27 (Armonk, New York).
3. Results
Eight-hundred and eighty-four respondents provided consent. Of these, 539 (61.0%) completed a T1 survey to form the cohort for further follow-up. Respondents providing consent at T0 who did not provide data at T1 were more often male (25% vs 16% male, χ2 = 11.8, p = .003), of lower education (35% vs 17% with less than a professional or graduate degree, χ2 = 37.3, p < .001), and not healthcare professionals (55% vs 46% in non-professional role, χ2 = 6.6, p = .01). The T2 survey, including at least one of the emotional exhaustion or psychological distress scales, was completed by 484 participants (89.9% of the T1 cohort). The median time between the T1 and T2 surveys was 125 days (interquartile range 15, from 111 to 126 days).
The characteristics of the cohort at T1 are described in Table 1 . The prevalence of COVID-19-related experiences in the month before the T1 survey differed by occupational role. Healthcare professionals were more likely than non-professionals to have been in isolation for symptoms associated with COVID-19 (nurses 15.7%, other professionals 16.7%, other clinical positions 4.4%, non-clinical positions 8.2%; χ2 = 12.1, p = .007), to have been tested for the virus (nurses 50.7%, other professionals 49.4%, other clinical positions 39.6%, non-clinical positions 29.1%; χ2 = 18.7, p < .001), and to have been separated from family members that they usually live with because of the risk of contagion (nurses 15.7%, other professionals 7.7%, other clinical positions 7.7%, non-clinical positions 3.8%; χ2 = 13.5, p = .004). Non-professionals with close patient contact were more likely to have worked as a screener (nurses 15.7%, other professionals 12.2%, other clinical positions 33.3%, non-clinical positions 18.4%; χ2 = 17.6, p = .001) and to report a major change in work activities (nurses 11.2%, other professionals 20.5%, other clinical positions 25.3%, non-clinical positions 13.9%; χ2 = 10.0, p = .02). Nurses were most likely to have been in a situation in which insufficient personal protective equipment (PPE) was available (nurses 20.9%, other professionals 5.1%, other clinical positions 8.8%, non-clinical positions 0.0%; χ2 = 45.0, p < .001), to have experienced a breach in PPE (nurses 17.9%, other professionals 7.7%, other clinical positions 2.2%, non-clinical positions 0.0%; χ2 = 39.5, p < .001), and to have not had enough time to don PPE and provided patient care nonetheless (nurses 14.2%, other professionals 3.8%, other clinical positions 1.1%, non-clinical positions 0.0%; χ2 = 36.6, p < .001).
Table 1.
Characteristics of 539 participants at T1.
| N (%) | ||
|---|---|---|
| Role typea | Nursing | 134 (24.9) |
| Other clinical professionals | 156 (28.9) | |
| Other clinical positions | 91(16.9) | |
| Non-clinical position | 158 (29.3) | |
| Age (missing 5) | 18–30 | 174 (32.3) |
| 31–40 | 143 (26.5) | |
| 41–50 | 121 (22.4) | |
| Over 50 | 96 (17.8) | |
| Gender (missing 1) | Female | 422 (78.3) |
| Male | 86 (16.0) | |
| Other/prefer not to say | 30 (5.6) | |
| Education | High school or less | 13 (2.4) |
| College diploma | 79 (14.7) | |
| Undergraduate degree | 176 (32.7) | |
| Professional or graduate degree | 271 (50.3) | |
| Race/ethnicity (missing 1) | African/black | 30 (5.6) |
| Asian | 149 (27.6) | |
| East Indian | 35 (6.5) | |
| European/white | 278 (51.6) | |
| Hispanic | 15 (2.8) | |
| Other | 31 (5.8) | |
| Marital status | Married/common-law | 307 (57.0) |
| Single | 211 (39.1) | |
| Divorced/separated/widowed | 21 (3.9) | |
| Children under 18 living at home (missing 3) | None | 355 (65.9) |
| Any | 181 (33.6) | |
| Adults over 60 living at home (missing 8) | None | 412 (76.4) |
| Any | 119 (22.1) |
Other clinical professionals: Physician, resident, dietician, occupational therapist, social worker, physiotherapist, manager of clinical area, speech language pathologist, pharmacist, respiratory therapist, spiritual care practitioner.
Other clinical positions: Administrative assistant, medical imaging technologist, assistant to physician/occupational therapist/physiotherapist, retail employee, porter, clinical research staff, volunteer.
Non-clinical positions: Research scientist, research staff, laboratory technician, corporate and administrative staff, administrative assistant, volunteer, manager of non-clinical area, building services staff, clerk, laboratory technologist, housekeeper.
Specific job types, in descending order of number of participants. Groups with two or fewer members not listed. Some roles appear in both clinical and non-clinical lists as determined by patient contact as described by participant.
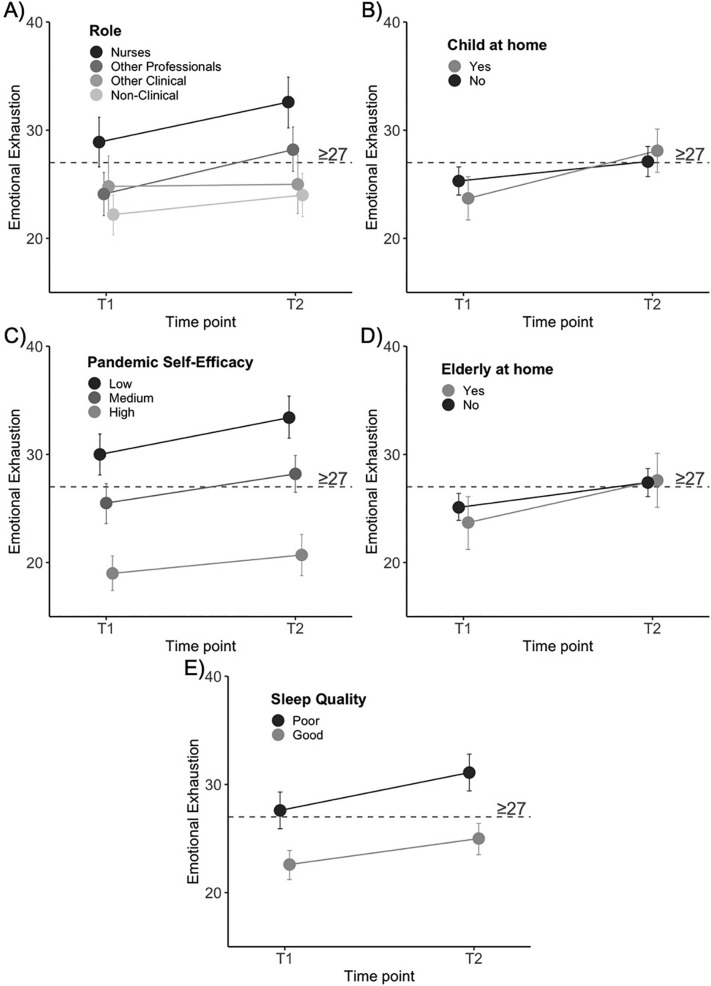
Mean levels of emotional exhaustion by occupational role were: nurses (T1: 28.9 [SD 12.4], T2: 32.6 [SD 12.6]); other professionals (T1: 24.1 [SD 11.8], T2: 28.2 [SD 11.9]); other clinical staff (T1: 24.8 [SD 13.0], T2: 25.0 [SD12.7]); and non-clinical staff (T1: 22.2 [SD 11.2], T2: 24.0 [SD 12.3]). The statistically significant relationships between personal and occupational characteristics and emotional exhaustion at T1 and T2 (identified in Table 2 ) are illustrated in Fig. 1 . Specifically, emotional exhaustion varied by occupational role (highest in nurses, lowest in non-clinical roles), and was greater in those with low pandemic self-efficacy and those with poor sleep quality at T1. The rate of increase in emotional exhaustion from T1 to T2 was greatest in nurses and other healthcare professionals, and in participants with children or elders at home.
Table 2.
Repeated measures analysis of variance in psychological outcomes at two time points.
| Emotional exhaustion |
Psychological distress |
|||
|---|---|---|---|---|
| F | P | F | p | |
| Time | 0.1 | 0.8 | 4.1 | 0.046 |
| Role | 7.3 | <0.001 | 1.9 | 0.1 |
| Role × Time | 3.8 | 0.01 | 1.0 | 0.4 |
| Pandemic Self-Efficacy (PSE) | 79.8 | <0.001 | 110.0 | <0.001 |
| PSE × Time | 0.4 | 0.6 | 0.3 | 0.6 |
| Child at home | 0.5 | 0.5 | 10.0 | 0.002 |
| Child at home × Time | 8.5 | 0.004 | 7.0 | 0.008 |
| Elderly adult at home | 0.0 | 1.0 | 0.1 | 0.8 |
| Elderly adult at home × Time | 4.0 | 0.047 | 0.3 | 0.6 |
| Sleep quality | 35.3 | <0.001 | 36.4 | <0.001 |
| Sleep quality × Time | 3.0 | 0.09 | 77.7 | <0.001 |
Fig. 1.
Significant relationships between emotional exhaustion in September–November 2020 (T1) and January–February 2021 (T2) and occupational or personal variables (as reported at T1).
The cut-off for severe burnout (≥27), measured using the emotional exhaustion scale of the Maslach Burnout Inventory, is indicated by a dashed line on each panel.
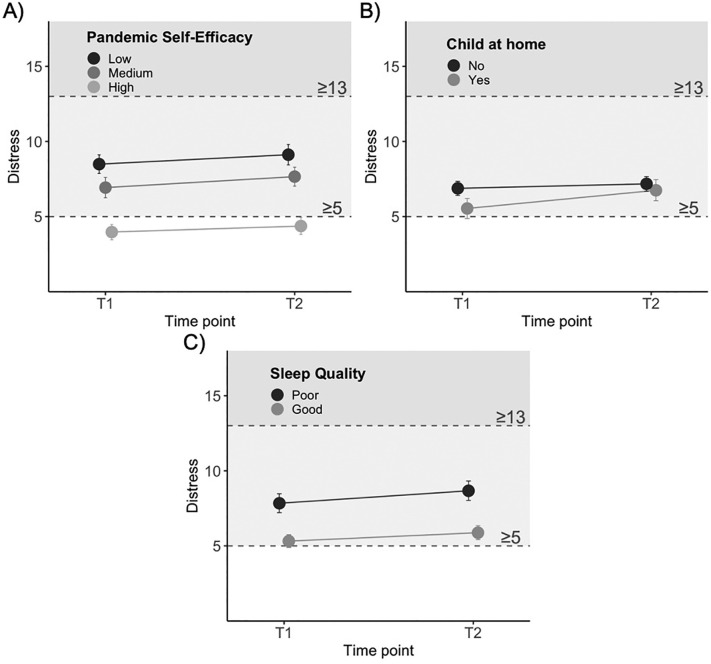
Mean levels of psychological distress by occupational role were: nurses (T1: 7.4 [SD 4.0], T2: 8.5 [SD 4.2]); other professionals (T1: 5.4 [SD 3.6], T2: 6.0 [SD 4.0]); other clinical staff (T1: 6.6 [SD 5.3], T2: 6.9 [SD 5.1]); and non-clinical staff (T1: 6.6 [SD 4.2], T2: 6.9 [SD 4.3]). The statistically significant relationships between personal and occupational characteristics and psychological distress at T1 and T2 (identified in Table 2) are illustrated in Fig. 2 . Psychological distress increased overall from T1 to T2. Participants with children at home had a greater increase from T1 to T2 (Fig. 2a). Participants with lower T1 sleep quality had higher overall levels of distress and a greater increase from T1 to T2 (Fig. 2b). Psychological distress was strongly and inversely related to pandemic self-efficacy (Fig. 2c).
Fig. 2.
Significant relationships between psychological distress in September–November 2020 (T1) and January–February 2021 (T2) and occupational or personal variables (as reported at T1).
The cut-off for severe psychological distress (≥13), as measured by the Kessler K6, is indicated by a dashed line and darker shaded region on each panel. The cut-off for medium distress (5 ≤ K6 < 13) is indicated by a dashed line and a lighter shaded region on each panel.
In order to aid interpretation, the proportion of survey participants whose scores indicated severe emotional exhaustion was 41.1% (95%CI 36.6–45.4) at T1 and 49.8% (95%CI 45.4–54.2) at T2 (McNemar test p < .001). Prevalence of severe emotional exhaustion by occupational role was: nurses, 54.3% at T1 (95%CI 45.9–62.7), 62.9% at T2 (95%CI 54.7–71.1); other healthcare professionals, 42.2% at T1 (95%CI 34.4–50.0), 55.6% at T2 (95%CI 47.8–63.4); clinical non-professionals, 38.4% at T1 (95%CI 28.4–48.4), 44.2% at T2 (95%CI 34.0–54.4); and non-clinical participants, 31.7% at T1 (95%CI 24.5–38.9), 37.9% at T2 (95%CI 30.4–45.4). The proportion of survey participants whose psychological distress scores indicated likely mental illness was 9.7% (95%CI 7.1–12.2) at T1 and 11.6% (95%CI 8.8–14.4) at T2 (McNemar test p = .33).
4. Discussion
There have been few reports of the psychological impact of the pandemic on healthcare workers at multiple time points [32], and this is the first that reports on the pandemic's second wave, to our knowledge. The value of this report is (i) to document levels of psychological distress and emotional exhaustion which are unsurprising but alarming (ii) to identify trends in these variables over time, (iii) to identify the groups of healthcare workers who are at greatest risk, and (iv) to identify potentially modifiable correlates of psychological distress and emotional exhaustion.
Prior to the pandemic, rates of severe emotional exhaustion in healthcare professionals were already high, typically reported in the range of 30% to 50%, with the highest rates in specialized settings such as critical care [[2], [3], [4]]. In the early months of the pandemic, rates of severe emotional exhaustion in healthcare settings ranged from 30 to 42% [18,19,33]. In this context, rates of severe emotional exhaustion in nurses of 54.3% in the fall of 2020, rising to 62.0% in early 2021 (and of 42.2% rising to 55.6% in other healthcare professionals) are both consistent with prior evidence and concerning. Despite fewer comparators for hospital staff who are not healthcare professionals, rates of severe emotional exhaustion above 30% at each measurement point also merit attention.
Rates of high psychological distress indicate likely mental illness [29]. For comparison to the rates found in this study (9.7% at T1 and 11.6% at T2), a study of over 60,000 employees of 58 large corporations found the prevalence of high K6 scores to be 4.5% [34], whereas a study of representative households directly impacted by Hurricane Katrina found a prevalence of high K6 scores of 10.9% 5–7 months after the hurricane and 14.0% one year later [35]. Thus, the range found in this study is similar to that found after a severe natural disaster.
Reports from other healthcare settings will provide context for these findings when they are available. Several factors suggest the impact might be higher elsewhere: (i) downtown Toronto has experienced a lesser impact of COVID-19 hospitalizations than other cities, (ii) the site of this study has implemented an extensive program of peer support for staff since early in the pandemic [23], and (iii) was recently re-designated with Magnet™ status from the American Nursing Credentialing Centre for having a professional work environment that yields positive outcomes for the nursing profession and excellence in patient care [36].
Although it is concerning that healthcare workers' burnout and psychological distress appear to be high and rising during the pandemic, it remains to be seen what the long-term psychological impact of the pandemic will be in this setting. On one hand, there is much evidence that the most common long-term response to exposure to highly aversive events is resilience [37]. On the other hand, evidence from longitudinal follow-up of healthcare workers in hospitals affected by the 2003 SARS outbreak, a much less severe and prolonged stressor than the COVID-19 pandemic at a societal level, demonstrated persistent meaningful effects of chronic stress 18 to 24 months after the resolution of the outbreak, including elevated burnout, psychological distress, posttraumatic stress symptoms, self-reported sick days, and self-reported decreases in patient contact and work hours [20]. Prospective, longitudinal research measuring a wide range of contextual protective and risk factors as the pandemic continues and resolves is needed to determine the prevalence of outcomes from chronic psychopathology to recovery and resilience and the contextual factors that favor different outcomes [37].
Increasing burnout and psychological distress associated with the ongoing pandemic emphasize the importance of identifying provocative and protective factors. In this study, significant correlations identify candidate provocative factors, extraordinary stresses related to caring for children and elders, and disrupted sleep, and a protective factor, self-efficacy. This study indicates that the challenge of balancing the extraordinary demands of parenting with hospital work contributes to the impact of stress, leading to increasing emotional exhaustion and psychological distress over time. The impact of parenting on outcomes was also observed in previous outbreaks [21]. Efforts to support work-home balance through flexible hours, support for daycare, or other supports for parents might mitigate this impact. This study also validates the impression that having elders at home during the COVID-19 pandemic has contributed to increases in healthcare workers' burnout and psychological distress. Flexibility and support for healthcare workers' who are challenged to balance work and home responsibilities should extend beyond those with parenting responsibilities.
The effect of pandemic self-efficacy, which was the strongest correlate of both psychological outcomes, is important because self-efficacy is modifiable through training in relevant tasks, role-modeling, and possibly organizational leadership [31,[38], [39], [40]]. The relationship of sleep quality with psychological outcomes was also substantial. This relationship may be bidirectional as it is consistent with both the known deleterious effects of nonrestorative sleep on professional burnout [41] and the sleep-disrupting effects of common psychiatric illnesses. Education about sleep hygiene, as well as organizational attention to the impact of shift work and shift length on sleep may support resilience, although this requires further research since the direction of causality cannot be determined in the current study.
This study's strengths include its use of validated measures of burnout and psychological distress at two time-points, relatively large sample size, high retention rate from T1 to T2, and representation of a wide variety of hospital roles. It also has limitations. The survey did not use a sampling strategy that ensures a representative population of hospital staff and the loss of 39% of consenting staff with demonstrated biases among drop-outs towards male gender, lower education and non-professional status indicates that non-represented staff differ from those who chose to participate. The survey question about having children under 18 at home did not distinguish between pre-school, elementary school-age children, and teenagers, which may affect pandemic-related parenting stresses. The survey question about having adults over 60 at home did not distinguish between elders who do or do not need care, or those who are able to help with childcare or other household activities. Further research to understand these aspects of personal circumstances is justified. The study is also limited by having not measured income or other factors that have resulted in greater impact of COVID-19 in marginalized communities.
Working in healthcare during the COVID-19 pandemic is contributing to both burnout and psychological distress for hospital workers and the psychological burden is rising as the pandemic persists. Our results indicate that the challenge is greater for healthcare workers with children and elders at home and is greatest in nurses. Substantive efforts to provide ongoing support to healthcare workers at both an organizational and individual level are needed. Further assessment of the psychological impact of this work over time is required to determine the long-term impact of the pandemic on healthcare providers.
Funding
This work was funded by a CIHR Canadian 2019 Novel Coronavirus (COVID-19) Rapid Research Grant (FRN 170642).
Declaration of Competing Interest
The authors of this paper have no competing interests to declare.
Acknowledgements
The authors gratefully acknowledge the contributions of Dr. Allison McGeer, Kate Wilkinson, and Jane Merkley to this work.
References
- 1.Maslach C., Jackson S.E., Leitner M.P. In: Evaluating stress: a book of resources. Zalaquett C.P., Woods R.J., editors. Scarecrow Press; Lanham, MD: 1997. Maslach burnout inventory: third edition; pp. 191–218. [Google Scholar]
- 2.Shanafelt T.D., Dyrbye L.N., Sinsky C., Hasan O., Satele D., Sloan J., et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc. 2016;91(7):836–848. doi: 10.1016/j.mayocp.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 3.Embriaco N., Papazian L., Kentish-Barnes N., Pochard F., Azoulay E. Burnout syndrome among critical care healthcare workers. Curr Opin Crit Care. 2007;13(5):482–488. doi: 10.1097/MCC.0b013e3282efd28a. [DOI] [PubMed] [Google Scholar]
- 4.Gomez-Urquiza J.L., De la Fuente-Solana E.I., Albendin-Garcia L., Vargas-Pecino C., Ortega-Campos E.M., Canadas-De la Fuente G.A. Prevalence of burnout syndrome in emergency nurses: a meta-analysis. Crit Care Nurse. 2017;37(5):e1–e9. doi: 10.4037/ccn2017508. [DOI] [PubMed] [Google Scholar]
- 5.Mata D.A., Ramos M.A., Bansal N., Khan R., Guille C., Di Angelantonio E., et al. Prevalence of depression and depressive symptoms among resident physicians: a systematic review and meta-analysis. JAMA. 2015;314(22):2373–2383. doi: 10.1001/jama.2015.15845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dutheil F., Aubert C., Pereira B., Dambrun M., Moustafa F., Mermillod M., et al. Suicide among physicians and health-care workers: a systematic review and meta-analysis. PLoS One. 2019;14(12) doi: 10.1371/journal.pone.0226361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Padilla Fortunatti C., Palmeiro-Silva Y.K. Effort-reward imbalance and burnout among ICU nursing staff: a cross-sectional study. Nurs Res. 2017;66(5):410–416. doi: 10.1097/NNR.0000000000000239. [DOI] [PubMed] [Google Scholar]
- 8.Murray C.J., Vos T., Lozano R., Naghavi M., Flaxman A.D., Michaud C., et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 9.Portoghese I., Galletta M., Coppola R.C., Finco G., Campagna M. Burnout and workload among health care workers: the moderating role of job control. Saf Health Work. 2014;5(3):152–157. doi: 10.1016/j.shaw.2014.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wisetborisut A., Angkurawaranon C., Jiraporncharoen W., Uaphanthasath R., Wiwatanadate P. Shift work and burnout among health care workers. Occup Med (Lond) 2014;64(4):279–286. doi: 10.1093/occmed/kqu009. [DOI] [PubMed] [Google Scholar]
- 11.Soderstrom M., Jeding K., Ekstedt M., Perski A., Akerstedt T. Insufficient sleep predicts clinical burnout. J Occup Health Psychol. 2012;17(2):175–183. doi: 10.1037/a0027518. [DOI] [PubMed] [Google Scholar]
- 12.Shanafelt T.D., Sloan J.A., Habermann T.M. The well-being of physicians. Am J Med. 2003;114(6):513–519. doi: 10.1016/s0002-9343(03)00117-7. [DOI] [PubMed] [Google Scholar]
- 13.Shoji K., Cieslak R., Smoktunowicz E., Rogala A., Benight C.C., Luszczynska A. Associations between job burnout and self-efficacy: a meta-analysis. Anxiety Stress Coping. 2016;29(4):367–386. doi: 10.1080/10615806.2015.1058369. [DOI] [PubMed] [Google Scholar]
- 14.Maunder R.G., Lancee W.J., Rourke S., Hunter J.J., Goldbloom D., Balderson K., et al. Factors associated with the psychological impact of severe acute respiratory syndrome on nurses and other hospital workers in Toronto. Psychosom Med. 2004;66(6):938–942. doi: 10.1097/01.psy.0000145673.84698.18. [DOI] [PubMed] [Google Scholar]
- 15.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 16.Worldometer Coronavirus update (live) 2021. https://www.worldometers.info/coronavirus/ Available from:
- 17.Luceno-Moreno L., Talavera-Velasco B., Garcia-Albuerne Y., Martin-Garcia J. Symptoms of posttraumatic stress, anxiety, depression, levels of resilience and burnout in Spanish health personnel during the COVID-19 pandemic. Int J Environ Res Public Health. 2020;17(15) doi: 10.3390/ijerph17155514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Naldi A., Vallelonga F., Di Liberto A., Cavallo R., Agnesone M., Gonella M., et al. COVID-19 pandemic-related anxiety, distress and burnout: prevalence and associated factors in healthcare workers of North-West Italy. BJPsych Open. 2021;7(1) doi: 10.1192/bjo.2020.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Orru G., Marzetti F., Conversano C., Vagheggini G., Miccoli M., Ciacchini R., et al. Secondary traumatic stress and burnout in healthcare workers during COVID-19 outbreak. Int J Environ Res Public Health. 2021;18(1) doi: 10.3390/ijerph18010337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maunder R.G., Lancee W.J., Balderson K.E., Bennett J.P., Borgundvaag B., Evans S., et al. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg Infect Dis. 2006;12:1924–1932. doi: 10.3201/eid1212.060584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kisely S., Warren N., McMahon L., Dalais C., Henry I., Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. 2020;369 doi: 10.1136/bmj.m1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brooks S.K., Dunn R., Amlot R., Rubin G.J., Greenberg N. A systematic, thematic review of social and occupational factors associated with psychological outcomes in healthcare employees during an infectious disease outbreak. J Occup Environ Med. 2018;60(3):248–257. doi: 10.1097/JOM.0000000000001235. [DOI] [PubMed] [Google Scholar]
- 23.Rosen B., Preisman M., Hunter J., Maunder R. Applying psychotherapeutic principles to bolster resilience among health care workers during the COVID-19 pandemic. Am J Psychother. 2020;73(4):144–148. doi: 10.1176/appi.psychotherapy.20200020. [DOI] [PubMed] [Google Scholar]
- 24.Nabors C., Sridhar A., Hooda U., Lobo S.A., Levine A., Frishman W.H., et al. Characteristics and outcomes of patients 80 years and older hospitalized with coronavirus disease 2019 (COVID-19) Cardiol Rev. 2021;29(1):39–42. doi: 10.1097/CRD.0000000000000368. [DOI] [PubMed] [Google Scholar]
- 25.Public Health Ontario ontario COVID-19 data tool. 2021. https://www.publichealthontario.ca/en/data-and-analysis/infectious-disease/covid-19-data-surveillance/covid-19-data-tool?tab=trends Available from:
- 26.Rotenstein L.S., Torre M., Ramos M.A., Rosales R.C., Guille C., Sen S., et al. Prevalence of burnout among physicians: a systematic review. JAMA. 2018;320(11):1131–1150. doi: 10.1001/jama.2018.12777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kessler R.C., Andrews G., Colpe L.J., Hiripi E., Mroczek D.K., Normand S.L., et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32(6):959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- 28.Staples L.G., Dear B.F., Gandy M., Fogliati V., Fogliati R., Karin E., et al. Psychometric properties and clinical utility of brief measures of depression, anxiety, and general distress: the PHQ-2, GAD-2, and K-6. Gen Hosp Psychiatry. 2019;56:13–18. doi: 10.1016/j.genhosppsych.2018.11.003. [DOI] [PubMed] [Google Scholar]
- 29.Kessler R.C., Barker P.R., Colpe L.J., Epstein J.F., Gfroerer J.C., Hiripi E., et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60(2):184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- 30.Snyder E., Cai B., DeMuro C., Morrison M.F., Ball W. A new single-item sleep quality scale: results of psychometric evaluation in patients with chronic primary insomnia and depression. J Clin Sleep Med. 2018;14(11):1849–1857. doi: 10.5664/jcsm.7478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Maunder R.G., Lancee W.J., Mae R., Vincent L., Peladeau N., Beduz M.A., et al. Computer-assisted resilience training to prepare healthcare workers for pandemic influenza: a randomized trial of the optimal dose of training. BMC Health Serv Res. 2010;10:72. doi: 10.1186/1472-6963-10-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hines S.E., Chin K.H., Glick D.R., Wickwire E.M. Trends in moral injury, distress, and resilience factors among healthcare workers at the beginning of the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18(2) doi: 10.3390/ijerph18020488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Giusti E.M., Pedroli E., D’Aniello G.E., Stramba Badiale C., Pietrabissa G., Manna C., et al. The psychological impact of the COVID-19 outbreak on health professionals: a cross-sectional study. Front Psychol. 2020;11:1684. doi: 10.3389/fpsyg.2020.01684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hilton M.F., Whiteford H.A., Sheridan J.S., Cleary C.M., Chant D.C., Wang P.S., et al. The prevalence of psychological distress in employees and associated occupational risk factors. J Occup Environ Med. 2008;50(7):746–757. doi: 10.1097/JOM.0b013e31817e9171. [DOI] [PubMed] [Google Scholar]
- 35.Kessler R.C., Galea S., Gruber M.J., Sampson N.A., Ursano R.J., Wessely S. Trends in mental illness and suicidality after Hurricane Katrina. Mol Psychiatry. 2008;13(4):374–384. doi: 10.1038/sj.mp.4002119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stone L., Arneil M., Coventry L., Casey V., Moss S., Cavadino A., et al. Benchmarking nurse outcomes in Australian Magnet(R) hospitals: cross-sectional survey. BMC Nurs. 2019;18:62. doi: 10.1186/s12912-019-0383-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chen S., Bonanno G.A. Psychological adjustment during the global outbreak of COVID-19: a resilience perspective. Psychol Trauma. 2020;12(S1):S51–S54. doi: 10.1037/tra0000685. [DOI] [PubMed] [Google Scholar]
- 38.Bartimote-Aufflick K., Bridgeman A., Walker R., Sharma M., Smith L. The study, evaluation, and improvement of university student self-efficacy. Stud High Educ. 2016;41(11):1918–1942. [Google Scholar]
- 39.Heslin P.A., Klehe U. In: Encyclopedia of industrial/organizational psychology. Rogelberg S.G., editor. Vol. 2. Sage; Thousand Oaks: 2006. Self-efficacy; pp. 705–708. [Google Scholar]
- 40.Slatten T. Determinants and effects of employee’s creative self-efficacy on innovative activities. Int J Qual Serv Sci. 2014;6(4):326–347. [Google Scholar]
- 41.Weaver M.D., Robbins R., Quan S.F., O’Brien C.S., Viyaran N.C., Czeisler C.A., et al. Association of sleep disorders with physician burnout. JAMA Netw Open. 2020;3(10) doi: 10.1001/jamanetworkopen.2020.23256. [DOI] [PMC free article] [PubMed] [Google Scholar]