Abstract
Objectives
Black adults in the United States have shorter sleep durations and poorer sleep efficiency relative to White adults, yet reasons for these disparities are not well explicated. The objective of this study was to examine neighborhood safety in childhood as a mediator of subsequent racial disparities in sleep.
Methods
Data were from Black and White young adults attending a large, predominantly White university in the Southeastern United States (N = 263; 52% Black, 53% female; Mean age = 19.21 years, SD = 1.01). Sleep parameters were assessed from 8 nights of wrist actigraphy (time in bed, sleep duration, and efficiency) and an established self-report measure of daytime sleepiness. Residential histories from birth through age 18 were documented, and retrospective self-reports of neighborhood safety in childhood were assessed.
Results
Black participants had less time in bed (p < 0.001), shorter sleep duration (p < 0.001), poorer sleep efficiency (p < 0.001), and more daytime sleepiness (p = 0.009) than White participants. Neighborhood safety mediated race differences in time in bed (p = 0.028), sleep duration (p = 0.033), and daytime sleepiness (p = 0.048), but not sleep efficiency. Findings were substantively unchanged after adjustment for family socioeconomic status, BMI, and substance use.
Conclusions
Findings support the hypothesis that neighborhood safety in childhood may partially account for race differences in subsequent sleep duration and daytime sleepiness. Addressing racial inequities in childhood neighborhood safety may be an important step toward reducing racial disparities in sleep health.
Keywords: Health inequalities, Race, Sleep disparities, Sleep duration, Actigraphy, Neighborhood disadvantage
1. Introduction
Several studies have documented an association between neighborhood safety and sleep outcomes [1]. However, few if any have examined the degree to which neighborhood safety in childhood may play a role in explaining race differences in sleep between Black and White Americans. This topic is highly relevant to current scientific and policy debates, and its significance is underscored by three established literatures.
First, neighborhood environments differ substantially by race. Black Americans live in more disadvantaged neighborhoods than White Americans, and are exposed to higher levels of poverty and crime [2–4]. The historical factors underlying race differences in neighborhood quality, such as housing discrimination, redlining, and predatory lending, are well documented [5], as are contemporary forms of racism that both create and sustain racial residential segregation [6]. Stemming from a history of segregation and inequality in residential opportunity, alongside inadequate enforcement of fair housing policies, race differences in neighborhood environments remain substantial even after adjusting for family socioeconomic status [4,7]. The deleterious consequences of neighborhood inequities for sleep health disparities are important to illuminate.
Second, Black Americans have shorter sleep durations, poorer sleep efficiency, greater daytime sleepiness, and worse overall sleep quality relative to White Americans [8–11]. Race disparities in sleep are well documented and have been linked to inequities in mortality and cardiometabolic disease [12,13]. Growing evidence demonstrates that racial inequities in sleep are also consequential factor in broader racial health disparities [12]. Although fewer studies have examined race differences in sleep earlier in the life span, some evidence suggests that Black-White sleep disparities are evident among young adults [14], and even among children [15]. Understanding the social determinants of Black-White disparities in sleep is a salient topic for health equity research.
Third, neighborhood environments are known to impact sleep outcomes among children, adolescents, and adults [1,16]. Among children and adolescents, higher levels of neighborhood violence and more concern about community safety have been associated with a range of sleep problems including shorter, more disrupted sleep, more self-reported sleep problems, and more daytime sleepiness [17–19]. Evidence also supports a longitudinal association between exposure to violence or safety concerns and sleep problems and disordered sleep among adolescents [20–22]. Similar associations between neighborhood safety and sleep outcomes have also been documented in diverse samples of adults [23–26]. This emerging literature is not surprising, given deeply engrained links between perceived safety and arousal processes, which have established associations with sleep physiology [27–30]. Based on these lines of research, perceived neighborhood safety is a likely candidate mechanism for racial inequities in sleep among young adults. Thus, our overarching hypotheses are that childhood neighborhood safety will: (1) be associated with sleep duration, sleep efficiency, and daytime sleepiness; and (2) that differences in childhood neighborhood safety will partially mediate racial disparities in sleep outcomes. More specifically, we postulate that, in a young adult sample, Black participants will have experienced lower levels of neighborhood safety in childhood than White participants, and that adjusting for neighborhood safety will attenuate race differences in sleep outcomes.
2. Methods
Participants were undergraduate college students at a large four-year university in the Southeastern United States. The student body was 86% White, 4% Black, 3% Hispanic, 2% Asian, and 5% other or multiracial at the time of recruitment. Using student records to identify demographic characteristics, equal numbers of first and second year African American (Black) and European American (White) students were invited to participate. White students who were first generation (did not have a parent who had graduated from a four-year college) were over-sampled to reduce potential confounding by socioeconomic status. Inclusion criteria was age between 18 and 25, and race of Black/African American or White in student records. In total, 468 Black and 608 White students (33% first generation in both groups) were sent information (pamphlet and letter) about the study via mail (to their local and permanent addresses) and emails (to their university email address). The study was described as seeking to understanding factors in students’ lives that influence their sleep and health. Responding students (26%; n = 284; 51% Black) were screened for sleep disorders during a lab visit using established measures of apnea [31], narcolepsy [32], restless leg syndrome [33], or severe insomnia [34]. Response rates were similar among the White males, White females, and Black males (25%). However, Black females were slightly more likely to participate (35%). No differences in response rates were observed by age or first generation college student status. Exclusion criteria were (1) reporting a sleep disorder, (2) screening above threshold values on sleep disorder screening measures, or (3) having a serious medical condition that interferes with sleep or precludes wearing an actigraph. Twenty-one students (9 Black, 12 White) were excluded due to having been previously diagnosed with a sleep disorder, or screening above threshold values for a sleep disorder. The final sample therefore consisted of 263 students (52% Black, 53% female; Mean age = 19.2, SD = 1.0). The study protocol involved a lab visit followed by an 8-day sleep actigraphy and sleep diary assessment. Participants provided written informed consent and were compensated $70. All study procedures complied with ethical guidelines for human subject’s research and received approval from an institutional review board.
2.1. Measures
2.1.1. Sleep
Participants wore an Actiwatch 2 (Philips Respironics) wrist actigraph for 8 consecutive days and nights. Philips Respironics devices use a solid-state piezo-electric sensor with a sampling rate of 32 Hz, and have been widely used and validated in sleep research, including against polysomnography [35]. On average, participants had actigraphy data for 7.6 nights (SD = 0.76). Consistent with best practices [36,37], rest intervals were coded through visual inspection of the plotted data in Actiware software and using information from event markers and daily diary reports. To assess agreement between three coders, intra-class correlations (ICCs) and their 95% confidence intervals were calculated based on single-rater (k = 3), absolute-agreement, 2-way mixed-effects models [38]. ICC estimates for each of the sleep actigraphy parameters ranged from 0.84 to 0.99 with 95% confidence intervals from 0.73 to 0.99, suggesting good to excellent reliability. Each actigraphy-assessed sleep parameter was averaged across all nights of available data to derive measures of time in bed, sleep duration, and sleep efficiency. Time in bed (also referred to as the rest interval) was scored using actigraphy (as described above) and is defined as the total length of the sleep interval from onset to final waking plus the morning and evening latency periods (Cronbach’s α for the 8-day average = 0.68). Sleep duration (also referred to as sleep time) is defined as the actual, actigraphy-assessed number of sleep minutes from sleep onset to wake time, excluding periods of wakefulness (α = 0.69). Sleep efficiency is the percentage of the rest interval spent asleep, from the time started trying to go to sleep to the time got out of bed (α = 0.83). During the laboratory visit (prior to actigraphy assessment), participants also completed the Epworth Sleepiness Scale to assess self-reports of recent daytime sleepiness [39]. Possible scores range from 0–24 with higher scores indicating greater daytime sleepiness. Scores were in the normal range for healthy adults (M = 6.4, SD = 3.9).
Time in bed and sleep duration were continuously coded in primary analyses (minutes/night). Additional analyses were conducted to consider nonlinear effects of neighborhood safety on sleep duration, and differential effects of neighborhood safety on short and long sleep. Results of these analyses indicated no nonlinear effects of neighborhood safety on sleep duration, and suggested that a continuous coding for sleep duration measures was appropriate to characterize the association with neighborhood safety in this study. Relatively few participants in our study (zero for sleep duration and thirty-five for time in bed) were long sleepers (>9 hours per night).
2.1.2. Neighborhood Safety
In an interview format, using interactive maps, residential histories from birth through age 18 were documented for each participant. From the interview, primary residential address during three periods of their childhood were recorded: early childhood (ages 0–5), middle childhood, (6–12), and adolescence (13–18). If participants had more than one address in a particular developmental period, they were asked to provide the location where they spent the most time. If they had trouble deciding between two locations (e.g., where they spent a similar amount of time), they were prompted to choose the one that they thought was most reflection of their experience during that developmental period. Building on prior work [40,41], perceived neighborhood safety was assessed with four self-report items for each developmental period’s primary residence: “How often was there a burglary or mugging in your neighborhood?”, “How often was there a violent argument between people in the neighborhood?”, “How often did you see people using drugs or drinking alcohol on your street?“, and “How often did you observe violent acts (for example, fist fights, beatings or use of weapons such as knives or guns) on your street?” To reduce self-report bias and potential confounding effects of personality, items focused on frequency of event occurrence rather than general perceptions of safety [42–44]. Response options were on a four point scale: never (1), occasionally (2), often (3), all the time (4). Items were reverse coded and a mean score was calculated such that higher scores indicated greater neighborhood safety. The Cronbach’s alphas were 0.81 for early childhood, 0.84 for middle childhood, and 0.58 for adolescence. Correlations between developmental periods ranged from 0.72 (between early childhood and middle childhood, p < 0.001), to 0.31 (between early childhood and adolescence, p < 0.001). Reports across the three developmental periods were averaged as an overall index of neighborhood safety in childhood. To facilitate clear interpretation of results, this measure was z-scored by subtracting the mean and dividing by the standard deviation. An alternative version of this measure, scored as the mean of the early and middle childhood safety measures (excluding adolescence), was also created. Sensitivity analyses with this measure, shown in the Appendix (Tables A1–A4), indicated a similar pattern of findings.
2.1.3. Demographic and Control Measures
Race was coded from student records (White=0; Black=1) and confirmed via self-reports. Age at time of data collection was coded in years. Highest level of parent education was coded from participant reports of each parent’s highest level of completing schooling. Parent’s combined total income was assessed from student self-reports and coded as an income-to-needs ratio, which is adjusted for family size using federal poverty guidelines [45]. Student employment status, and shift work, were measured using two items with response options of yes (1) and no (0): “Do you have a part-time or full-time job?”; and “Does your job involve working late nights?”
Substance use was assessed by averaging daily reports across the 8-day assessment period. Alcohol use was coded on a four point scale following USDA guidelines [46]: no use (coded as zero); 1 drink/day for females and 1–2 drinks/day for males (coded as 1); 2–3 drinks per day for females and 3–4 drinks for males (coded as 2); >3 drinks/day for females and >4 drinks/day for males (coded as 3). Caffeine use was converted into milligrams (mg) and coded on the following scale: no caffeine use (coded as 0), 1–50mg (coded as 1), and 51–100mg (coded as 2), 101–150mg (coded as 3), 151–200mg (coded as 4), >200mg (coded as 5). Marijuana use, converted into grams (g), was coded as follows: no use (coded as 0), .1–.25g (coded as 1), .26–.50g (coded as 2), .51–.75g (coded as 3), .76–1.0g (coded as 4), >.1.0g (coded as 5). Over-the-counter and prescription medications and the reasons for their use were recorded. National Sleep Foundation guidelines (2019) were used to identify medications known to influence sleep. In the sleep diary, a variable indicating sleep medication use was coded as 1 if participant reported taking a medication known to affect sleep, and otherwise coded as 0. A mean score was then taken across the eight nights to index frequency of sleep medication use. Depressive symptoms were assessed using the Beck Depression Inventory-II (BDI) [47,48]. Consistent with prior research, items relating specifically to sleep problems were excluded to avoid conceptual overlap with sleep outcomes [14]. Body mass index (BMI; kg/m2) was calculated from measures of height (using Seca 213 stadiometer) and body mass (using a Seca 874 digital scale), assessed during the lab visit.
2.2. Analysis Plan
For each sleep outcome, a series of regression models was estimated in Mplus Version 8.3. Model 1 examined race differences in sleep adjusting for age, sex, and medication use. Due to known effects of shift work on sleep [49], Model 1 also adjusted for whether students were employed, and whether employment involved working late nights. Model 2 added neighborhood safety. Model 3 added parent income, scored as an income-to-needs ratio. This model allowed for consideration of whether neighborhood effects were attenuated after adjusting for family socioeconomic status [4]. Model 4 added BMI, depressive symptoms, and substance use (alcohol, caffeine, nicotine, marijuana). Each of these variables has established associations with sleep [50,51] and neighborhood disadvantage [52], and were included in Model 4 to examine whether effects of neighborhood safety persisted after adjusting for their effects. Indirect effects were then estimated in the fully adjusted model to test mediation hypotheses [53,54]. In primary analyses, sleep outcomes were unstandardized so that findings could be interpreted in original units. These estimates are shown in Figures and Tables. Where relevant, standardized estimates are also reported in the text to elucidate the magnitude of associations in standard deviation (SD) units. Missing data were dealt with using full-information maximum likelihood estimation (FIML). This allowed for a consistent sample size across models irrespective of missing data on individual covariates [55]. Of the 263 individuals included analyses, 8% had missing data on sleep actigraphy parameters and 4% had missing data on parent income. All other variables had less than 2% missing data. An alternative model progression in which neighborhood safety was added in a final model after all other covariates was also considered and is shown in the Appendix (Tables A5–A8). Substantive findings in these models were equivalent to those reported in the main manuscript.
3. Results
Our analytic sample consisted of 52% Black, and 48% White students, and was 53% female. The mean income-to-needs ratio was 4.54 (SD = 3.03) and the mean level of parent education was between some college and graduating with a bachelor’s degree (M = 7.43, SD = 2.04). Participants averaged 480.55 minutes (8.0 hours) of time in bed (SD = 62.62 minutes) and 380.26 minutes (6.3 hours) of time asleep (SD = 54.08 minutes). Mean actigraphy assessed sleep efficiency was 79.0% (SD = 6.46%) and participants average self-reported daytime sleepiness was 6.41 on a scale from 0 to 22 (SD = 3.94). Time in bed was positively correlated with actual sleep duration (r = 0.86, p < 0.001), negatively correlated with daytime sleepiness (r = −0.19, p = 0.002), and not associated with sleep efficiency (r = −0.02, p = 0.803). Sleep duration was positively correlated with sleep efficiency (r = 0.48, p < 0.001) and negatively correlated with daytime sleepiness (r = −0.22, p = 0.001). Sleep efficiency was not correlated with daytime sleepiness (r = −0.08, p = 0.214).
Race differences in study variables are shown in Table 1. Black participants had significantly less time in bed (d = 0.39, p = 0.003), shorter sleep duration (d = 0.67, p < 0.001), lower sleep efficiency (d = 0.50, p < 0.001) and more daytime sleepiness (d = 0.37, p = 0.005) than White participants. Black participants also reported growing up in neighborhoods with lower levels of safety (d = 0.36, p = 0.003), had more depressive symptoms (d = 0.31, p = 0.015), and higher BMI (d = 0.48, p < 0.001) than White participants. White participants reported higher levels of caffeine use (d = 1.02, p < 0.001), alcohol use (d = 0.48, p < 0.001), and nicotine use (d = 0.33, p = 0.010) than Black participants. No race differences were found in sleep medication use (p = 0.109), marijuana use (p = 0.706), employment (p = 0.058), or working late nights (p = .083).
Table 1.
Descriptive Statistics by Racial Groups
| Variables | White (N = 126) M ± SD (or %) | Black (N = 137) M ± SD (or %) | p |
|---|---|---|---|
| Age (years) | 19.15 ± 0.96 | 19.26 ± 1.06 | 0.370 |
| Biological sex (female) | (48.4) | (58.4) | 0.105 |
| Sleep Medication | 0.04 ± 0.14 | 0.02 ± 0.10 | 0.109 |
| Employment Status | (27.0) | (38.0) | 0.058 |
| Shift Work | (14.3) | (22.6) | 0.083 |
| Parent Education (highest) | 7.39 ± 2.06 | 7.47 ± 2.03 | 0.752 |
| Income to Needs Ratio | 5.37 ± 3.66 | 3.81 ± 2.12 | < 0.001 |
| Body Mass Index | 24.24 ± 3.55 | 26.60 ± 5.95 | < 0.001 |
| Depressive Symptoms | 5.17 ± 5.08 | 7.10 ± 7.33 | 0.015 |
| Caffeine | 1.54 ± 1.42 | 0.40 ± 0.72 | < 0.001 |
| Alcohol | 0.31 ± 0.44 | 0.13 ± 0.30 | < 0.001 |
| Nicotine | 0.14 ± 0.33 | 0.05 ± 0.18 | 0.010 |
| Marijuana | 0.13 ± 0.51 | 0.11 ± 0.49 | 0.706 |
| Neighborhood Safety Composite | 3.82 ± 0.25 | 3.70 ± 0.40 | 0.003 |
| Early Childhood | 3.85 ± 0.26 | 3.64 ± 0.57 | < 0.001 |
| Middle Childhood | 3.78 ± 0.39 | 3.66 ± 0.54 | 0.037 |
| Adolescence | 3.83 ± 0.24 | 3.79 ± 0.32 | 0.246 |
| Sleep Measures | |||
| Time in Bed (actigraphy) | 492.69 ± 52.37 | 468.50 ± 69.32 | < 0.001 |
| Sleep Duration (actigraphy) | 397.51 ± 41.09 | 363.15 ± 59.85 | < 0.001 |
| Sleep Efficiency (actigraphy) | 80.56 ± 5.33 | 77.45 ± 7.10 | < 0.001 |
| Epworth Sleepiness Scale | 5.71 ± 3.72 | 7.07 ± 4.06 | 0.005 |
Note. Parent Education is scored from 1 (less than 8th grade) to 11 (professional degree). The neighborhood safety composite index is scored as the mean of neighborhood safety in early childhood, middle childhood, and adolescent. Independent sample t-tests and chi-squared tests were used to determine the statistical significance of differences between the Black and White samples.
3.1. Time in Bed (Rest Duration)
Results from models examining predictors of actigraphy-assessed time in bed are shown in Table 2. Model 1 estimates showed that Black participants spent 22.15 minutes/night (SE = 7.49) less time in bed than White participants (equivalent to 0.35 SD units, SE = 0.13, p = 0.005). Model 2 estimates indicated each SD unit increase in participant’s reports of neighborhood safety was associated with an additional 25.81 minutes/night (SE = 11.63) in bed (equivalent to 0.41 SD units, SE = 0.19, p = 0.026), and explained 14% of the race difference in sleep duration. Estimates from Models 3 and 4 showed the association between neighborhood safety and sleep duration was not attenuated after adjusting for family socioeconomic indicators (Model 3) or BMI, depressive symptoms, and substance use (Model 4). However, participants with higher alcohol use and higher BMI averaged significantly less time in bed (p = 0.048 and p = 0.012), while participants with higher marijuana use averaged significantly more time in bed (p = 0.003). In the fully adjusted model (Model 4), each SD unit increase in neighborhood safety was associated with 37.66 minutes/night (SE = 11.88) more sleep (equivalent to 0.60 SD units, SE = 0.19, p = 0.002). Path analyses revealed that 4.75 minutes (18%) of the race difference in sleep duration (SE = 2.16, p = 0.028) was mediated by neighborhood safety (Figure 1, Panel A).
Table 2.
Model results showing predictors of actigraphy-assessed time in bed.
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
|---|---|---|---|---|---|---|---|---|
| B | SE | B | SE | B | SE | B | SE | |
| Race (Black = 1) | −22.15** | 7.90 | −19.09* | 7.94 | −18.70* | 8.25 | −21.22* | 9.35 |
| Sex (Female = 1) | 10.28 | 7.94 | 9.29 | 7.89 | 9.15 | 7.88 | 12.57 | 7.74 |
| Age (years) | 1.84 | 4.06 | 2.55 | 4.03 | 2.44 | 4.06 | 1.10 | 4.01 |
| Parent Education | −0.77 | 2.11 | −0.81 | 2.03 | ||||
| Income to Needs | 0.15 | 1.51 | 0.19 | 1.45 | ||||
| BMI | −1.92 | 0.77 | ||||||
| Depressive Symptoms | 0.10 | 0.61 | ||||||
| Caffeine | −4.41 | 3.47 | ||||||
| Alcohol | −21.60 | 10.91 | ||||||
| Nicotine | 16.05 | 16.62 | ||||||
| Marijuana | 25.06** | 8.34 | ||||||
| Neighborhood Safety | 25.81* | 11.63 | 26.09* | 11.67 | 37.66** | 11.88 | ||
| R2 | 6.7% | 8.5% | 8.5% | 18.0% | ||||
Note. N = 263. All models also adjust for medication use, employment status, and shift work. Neighborhood safety is scored as the mean of neighborhood safety in early childhood, middle childhood, and adolescent. Parent Education is scored from 1 (less than 8th grade) to 11 (professional degree or higher).
p < 0.05.
p < 0.01.
p < 0.001.
Figure 1.
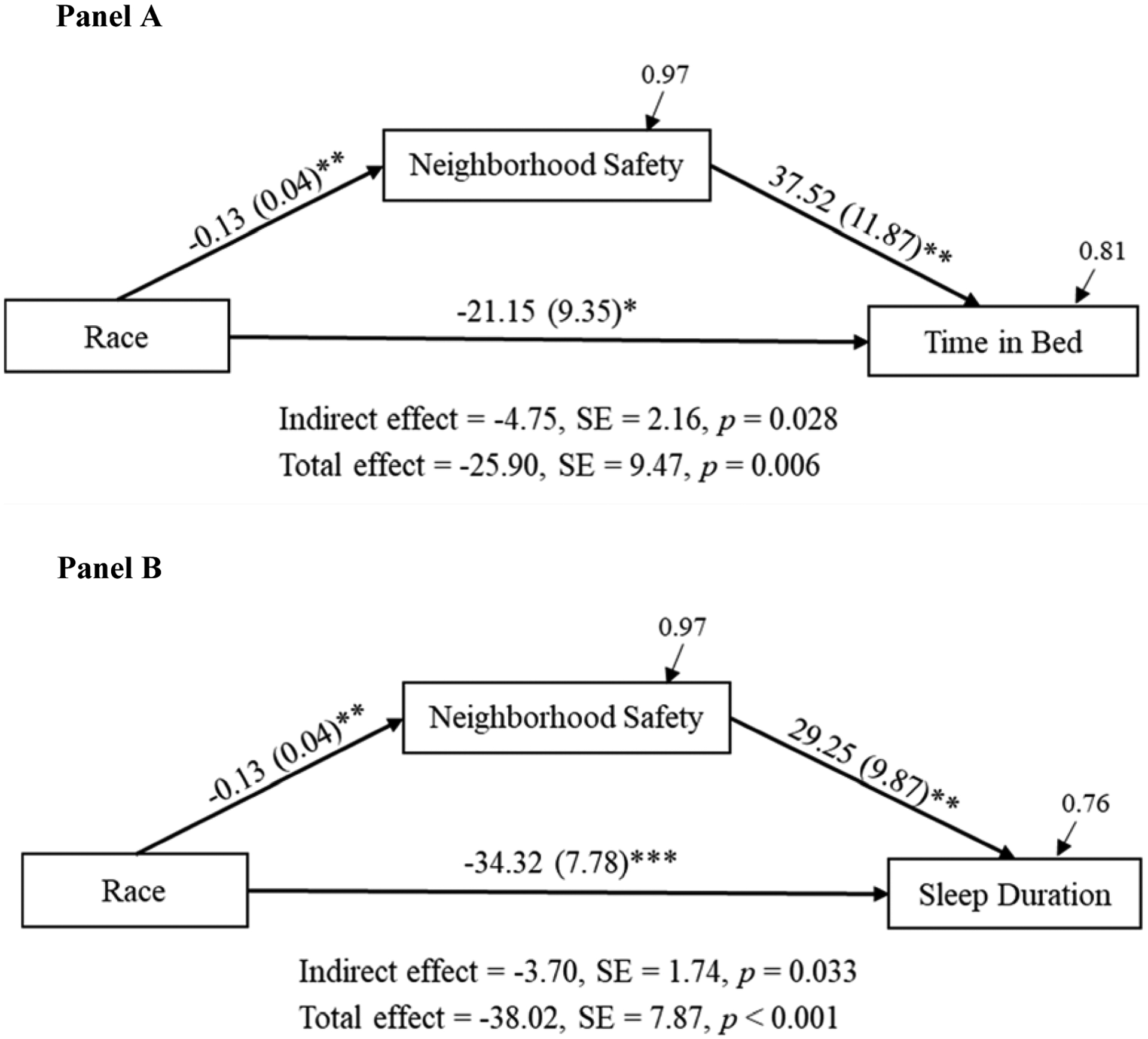
Path model showing indirect effects of race on time in bed (Panel A) and sleep duration (Panel B) via neighborhood safety. Note. N = 263. Coefficients are from a fully adjusted model with Model 4 covariates. Path coefficients are unstandardized. Residual variances are standardized. Race is coded as White = 0, Black = 1. *p < 0.05. **p < 0.01. ***p < 0.001.
3.2. Sleep Duration
A similar pattern of findings was evident for actigraphy-assessed sleep duration (shown in Table 3). Model 1 estimates indicated that Black participants had 33.31 less minutes/night (SE = 6.51) than White participants (equivalent to 0.62 SD units, SE = 0.12, p < 0.001). Model 2 estimates indicated each SD unit increase in neighborhood safety was associated with an additional 21.11 minutes/night (SE =9.59) of sleep (equivalent to 0.39 SD units, SE = 0.18, p = 0.028) and attenuated 8% of the race difference. Estimates from Models 3 and 4 showed that the association between neighborhood safety and sleep duration was not attenuated after adjusting for family socioeconomic indicators (Model 3), or BMI, depressive symptoms, and substance use (Model 4). As was the case for time in bed, alcohol use was associated with shorter sleep duration (p = 0.032) and marijuana use was associated with longer sleep duration (p = 0.003). In the fully adjusted model (Model 4), each SD unit increase in childhood neighborhood safety was associated with 29.34 minutes/night (SE = 9.88) more sleep (equivalent to 0.54 SD units, SE = 0.18, p = 0.003). Path analyses revealed 3.70 minutes (10%) of the race difference in sleep duration (SE = 1.74, p = 0.033) was mediated by neighborhood safety (Figure 1, Panel B).
Table 3.
Model results showing predictors of actigraphy-assessed sleep duration.
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
|---|---|---|---|---|---|---|---|---|
| B | SE | B | SE | B | SE | B | SE | |
| Race (Black = 1) | −33.31*** | 6.51 | −30.80*** | 6.55 | −31.94*** | 6.80 | −34.36*** | 7.79 |
| Sex (Female = 1) | 18.59** | 6.55 | 17.79** | 6.49 | 17.72** | 6.50 | 19.58** | 6.44 |
| Age (years) | −1.67 | 3.35 | −1.09 | 3.33 | −0.85 | 3.35 | −2.18 | 3.34 |
| Parent Education | 0.57 | 1.75 | 0.47 | 1.70 | ||||
| Income to Needs | −0.77 | 1.26 | −0.71 | 1.22 | ||||
| BMI | −1.03 | 0.64 | ||||||
| Depressive Symptoms | −0.15 | 0.51 | ||||||
| Caffeine | −2.33 | 2.90 | ||||||
| Alcohol | −19.49* | 9.10 | ||||||
| Nicotine | 1.99 | 13.86 | ||||||
| Marijuana | 20.91** | 6.95 | ||||||
| Neighborhood Safety | 21.11* | 9.59 | 21.24* | 9.62 | 29.34** | 9.88 | ||
| R2 | 15.0% | 16.6% | 16.8% | 23.0% | ||||
Note. N = 263. All models control for sleep medication, employment status, and shift work. Neighborhood safety is scored as the mean of neighborhood safety in early childhood, middle childhood, and adolescent. Parent Education is scored from 1 (less than 8th grade) to 11 (professional degree).
p < 0.05.
p < 0.01.
p < 0.001.
3.3. Sleep Efficiency
Model 1 estimates showed that Black participants sleep efficiency was 3.32 percent (SE = 0.80) lower than White participants (equivalent to 0.52 SD units, SE = 0.12, p < 0.001). Model 2 indicated neighborhood safety was not a significant predictor of sleep efficiency (p =0.715) and only attenuated 2% of the race difference. Lastly, Models 3 and 4 showed that adjustment for additional covariates did not explain any of the race difference in sleep efficiency and did not substantially change the effects of neighborhood safety. Full model results are shown in Appendix (Table A9).
3.4. Daytime Sleepiness
Results from regression models examining daytime sleepiness are shown in Table 4. Model 1 estimates indicated Black participants had 1.27 units (SE = 0.49) higher daytime sleepiness than white participants (equivalent to 0.32 SD units, SE = 0.12, p = 0.009). Model 2 estimates showed each SD increase in neighborhood safety was associated with a 2.61 units (SE = 0.72) reduction in daytime sleepiness (equivalent to 0.66 SD units, SE = 0.18, p < 0.001) and explained 24% of the race difference in daytime sleepiness. Estimates from Model 3 showed the association between neighborhood safety and sleepiness was not attenuated after adjusting for family socioeconomic indicators. In Model 4, depressive symptoms was significantly associated with daytime sleepiness. After adjusting for Model 4 covariates, the association between neighborhood safety and sleepiness remained significant (p = 0.009) but was attenuated by 30%. In the fully adjusted model (Model 4), each SD unit increase in neighborhood safety was associated with 1.88 reduction (SE = 0.73) in daytime sleepiness (equivalent to 0.48 SD units, SE = 0.18, p = 0.009). Path analyses revealed that neighborhood safety explained 0.24 (23%) of the race differences in self-reported daytime sleepiness through indirect effects (SE = 0.12; p = 0.048). Figure 2 shows the full path analyses with neighborhood safety mediating race differences in daytime sleepiness.
Table 4.
Model results showing predictors of daytime sleepiness.
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
|---|---|---|---|---|---|---|---|---|
| B | SE | B | SE | B | SE | B | SE | |
| Race (Black = 1) | 1.27** | 0.49 | 0.96* | 0.48 | 1.00* | 0.50 | 0.78 | 0.56 |
| Sex (Female = 1) | 0.16 | 0.49 | 0.27 | 0.48 | 0.29 | 0.48 | 0.01 | 0.47 |
| Age (years) | 0.07 | 0.25 | 0.01 | 0.25 | 0.02 | 0.25 | −0.03 | 0.24 |
| Parent Education | 0.09 | 0.12 | 0.09 | 0.12 | ||||
| Income to Needs | 0.05 | 0.09 | 0.03 | 0.08 | ||||
| BMI | −0.02 | 0.05 | ||||||
| Depressive Symptoms | 0.18*** | 0.04 | ||||||
| Caffeine | −0.01 | 0.21 | ||||||
| Alcohol | 0.47 | 0.67 | ||||||
| Nicotine | −1.35 | 0.99 | ||||||
| Marijuana | 0.37 | 0.51 | ||||||
| Neighborhood Safety | −2.61*** | 0.72 | −2.68*** | 0.72 | −1.88** | 0.73 | ||
| R2 | 3.8% | 8.5% | 8.90% | 17.6% | ||||
Note. N = 263. All models also adjust for medication use, employment status, and shift work. Neighborhood safety is scored as the mean of neighborhood safety in early childhood, middle childhood, and adolescent. Parent Education is scored from 1 (less than 8th grade) to 11 (professional degree or higher).
p < 0.05.
p < 0.01.
p < 0.001.
Figure 2.
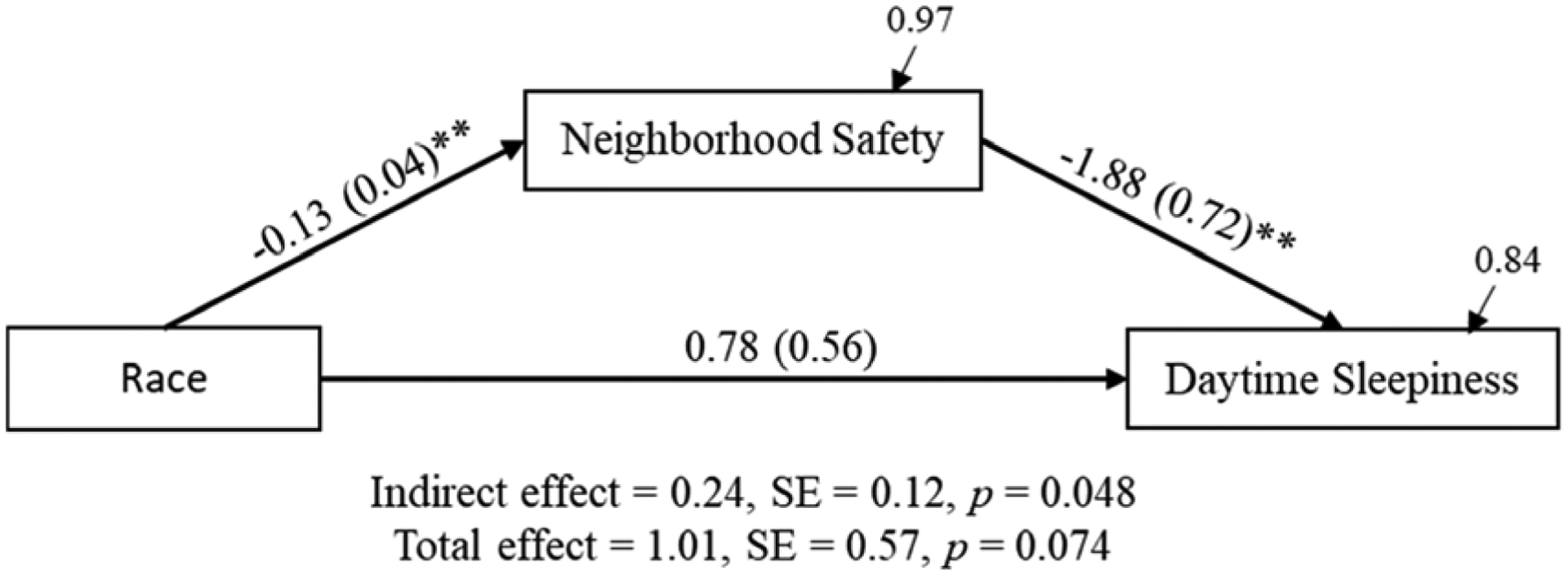
Path model showing indirect effects of race on daytime sleepiness via neighborhood safety and depressive symptoms. Note. N = 263. Coefficients are from a fully adjusted model with Model 4 covariates. Path coefficients are unstandardized. Residual variances are standardized. Race is coded as White = 0, Black = 1. *p < 0.05. **p < 0.01. ***p < 0.001.
4. Discussion
Understanding the social determinants of disparities in sleep between Black and White Americans is an understudied topic with important public health implications [13,56,57]. The significance of this topic is underscored by established research showing that short sleep duration and poor sleep quality are risk factors for psychological distress [58] and cardiometabolic disease [59,60], and that racial disparities in sleep partially explain race differences in health outcomes [12]. The current study is among the first (if not the first) to examine neighborhood safety as an explanation for the association between race and sleep outcomes. Results indicated that neighborhood safety in childhood mediated a portion of race differences in actigraphy-assessed time in bed and sleep duration, but not sleep efficiency. Indirect effects of race on sleep through neighborhood safety were also evident for daytime sleepiness. The main findings were largely unchanged after adjusting for family SES, depressive symptoms, BMI, and health behaviors.
Overall, the findings are consistent with studies showing that neighborhood safety and exposure to violence are associated with various sleep parameters among adolescents and adults [1,61]. The findings also extend this work in two key ways. First, our study shows that neighborhood safety in childhood mediates a portion of race differences in sleep among young adults. This result suggests that established associations between neighborhood safety and sleep may play an important role in racial health disparities, and that research examining interventions to reduce the adverse consequences of low neighborhood safety could be an important step toward addressing racial health disparities.
Second, our study shows that reports of neighborhood safety in childhood are associated with subsequent actigraphy-assessed sleep duration in young adulthood. This result is significant because it suggests that previously documented associations between neighborhood safety and sleep in childhood may have an enduring association with sleep into young adulthood. To probe whether early and middle childhood neighborhood contexts, as opposed to more proximal adolescent neighborhood contexts, were driving associations in this study, sensitivity analyses were conducted using an alternative measure of neighborhood safety that combined early and middle childhood neighborhood safety (excluding the adolescent period). Results (shown in Appendix) indicated that mediation findings were just as strong using the combined early and middle childhood neighborhood safety measure and thus support our conclusion that childhood contexts are likely to be consequential for subsequent sleep outcomes among young adults. The relatively homogenous context of college students at the same institution also makes it unlikely that childhood neighborhood effects are entirely operating through effects of more proximal neighborhood conditions. However, additional research is needed to examine the combined effects of childhood and adult neighborhood exposures.
Our null findings for sleep efficiency are in contrast to prior research, which has reported associations between neighborhood safety and sleep efficiency among middle-aged African American adults [26]. Although not expected, this difference is not entirely surprising when context and developmental timing are considered. That is, the effects of current neighborhood safety on the sleep outcomes of middle-aged adults may be quite different than effects of childhood neighborhood safety on young adults. More work will be needed to examine the timing and duration of neighborhood exposures, the extent to which the impact of childhood neighborhood safety persists, and their associations with sleep outcomes at different points in the life span.
Few prior studies have considered race differences in sleep among college students, and to our knowledge all of these studies are based on self-report measures [14,62–64]. The results of this study are therefore among the first to show racial disparities in actigraphy-assessed sleep duration between Black and White college students. Moreover, compared to other studies using self-report measures in similar populations, our results suggest larger racial disparities in sleep duration [65]. This is not entirely surprising given prior research suggesting that self-report measures may underestimate objective measures of Black-White differences in sleep [66]. Lastly, our findings also build on prior research demonstrating racial disparities in actigraphy-assessed sleep among adolescents and adults [9,13,67–70] by showing that sleep disparities are also evident in the college context. Substantial racial disparities in sleep evident in our data and in prior research underscore the urgent need for research elucidating reasons for these differences.
Results were largely unchanged after adjusting for family SES, BMI, and substance use. However, depressive symptoms significantly attenuated the effects of neighborhood safety on self-reported but not actigraphy assessed sleep outcomes. This finding is consistent with some prior work. For example, a study focusing on Black adults found that the association between neighborhood disadvantage and sleep duration and quality was attenuated after adjusting for depression [71]. Our results add to this research by showing that depression may be one important mechanism by which lower levels of neighborhood safety in childhood may impact sleep among young adults, thus highlighting the salience of both of these variables in understanding disparities in sleep.
Limitations of this research are important to note. One limitation was that neighborhood safety measures were self-reported and retrospective. However, retrospective reports of childhood neighborhood conditions have shown adequate reliability and validity in prior research [72]. Furthermore, self-report measures of safety have been consistently predictive of health outcomes [1], and as compared to objective measures, may yield conservative estimates of the magnitude of the association between neighborhood safety and sleep [73]. Nonetheless, research examining the role of objective or concurrent self-report measures of neighborhood safety in racial health disparities will be a useful addition to research on this topic.
A second limitation was that sleep measures were assessed via actigraphy and self-report methods. While these measures have various strengths and are well validated, polysomnography sleep assessments could provide important insight into the specific aspects of sleep architecture that may be affected by neighborhood safety, and therefore may be useful to consider in future research on this topic. Because our study was observational, we were not able to rule out third variable explanations for associations between neighborhoods and sleep. Studies examining changes in neighborhood environments and their associations with changes in sleep would therefore be one useful extension of this research. The findings of this study cannot be generalized to other racial/ethnic groups or to university students in other contexts (e.g., other geographic regions or different types of colleges). However, a key strength of our focus on a college sample, and oversampling of first-generation White students, was that it allowed us to reduce confounding of race and class. In particular, we were able to estimate the role of neighborhood safety in a sample with relatively similar levels of parent education within each racial group. That neighborhood safety was still a significant predictor of race differences in sleep in this sample is alarming and suggests the likely insidious nature of childhood neighborhood factors as a determinant of racial health disparities. It should be noted that due to the relatively homogenous socioeconomic composition of our college student sample, reported effects sizes are likely to be conservative. That is, within a broader population sample containing more socioeconomic diversity, neighborhood measures are likely to be more predictive of sleep and sleep disparities. Thus, because Black and White participants in our sample were more similar socioeconomically than Black and White young adults in the general population, our findings likely underestimate the role of neighborhood factors in racial sleep disparities.
Overall, the results provide evidence in support of the hypothesis that childhood neighborhood safety is linked to race differences in sleep duration and quality, which subsequently contribute to racial inequities in health [12]. The findings therefore suggest that studies examining the causal effects of neighborhood safety in childhood on disparities in more distal clinical health outcomes are warranted (e.g., using longitudinal or natural experimental designs). Eliminating race differences in neighborhood safety may be an important step toward addressing racial inequities in health.
Supplementary Material
Highlights.
Disparities in sleep outcomes between Black and White young adults are substantial
Black young adults had poorer objectively-assessed sleep outcomes than White participants
Black young adults had more daytime sleepiness than White young adults
Black young adults grew up in neighborhoods that were less safe than White young adults
Neighborhood safety in childhood partially explained race differences in sleep
Acknowledgements
This work was supported by the National Heart, Lung, and Blood Institute (grant number 1R15HL140504-01A1); and the USDA National Institute of Food and Agriculture (Hatch project 1003947).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].Hale L, James S, Xiao Q, Billings ME, Johnson DA. Chapter 7 - Neighborhood factors associated with sleep health. In: Grandner MA, editor. Sleep Health, Academic Press; 2019, p. 77–84. 10.1016/B978-0-12-815373-4.00007-1. [DOI] [Google Scholar]
- [2].Fuller-Rowell TE, Curtis DS, Klebanov PK, Brooks-Gunn J, Evans GW. Racial Disparities in Blood Pressure Trajectories of Preterm Children: The Role of Family and Neighborhood Socioeconomic Status. Am J Epidemiol 2017;185:888–97. 10.1093/aje/kww198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Osypuk TL, Galea S, McArdle N, Acevedo-Garcia D. Quantifying Separate and Unequal: Racial-Ethnic Distributions of Neighborhood Poverty in Metropolitan America. Urban Aff Rev Thousand Oaks Calif 2009;45:25–65. 10.1177/1078087408331119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Roux AVD, Kiefe CI, Jacobs DR Jr, Haan M, Jackson SA, Nieto FJ, et al. Area Characteristics and Individual-Level Socioeconomic Position Indicators in Three Population-Based Epidemiologic Studies. Ann Epidemiol 2001;11:395–405. 10.1016/S1047-2797(01)00221-6. [DOI] [PubMed] [Google Scholar]
- [5].Rothstein R The Color of Law: A Forgotten History of How Our Government Segregated America. New York, NY: Liveright Publishing; 2017. [Google Scholar]
- [6].Massey DS. Categorically unequal: The American stratification system. Russell Sage Foundation; 2007. [Google Scholar]
- [7].Sharkey P Spatial segmentation and the black middle class. AJS 2014;119:903–54. [DOI] [PubMed] [Google Scholar]
- [8].Petrov ME, Lichstein KL. Differences in sleep between black and white adults: an update and future directions. Sleep Med 2016;18:74–81. 10.1016/j.sleep.2015.01.011. [DOI] [PubMed] [Google Scholar]
- [9].Ruiter ME, DeCoster J, Jacobs L, Lichstein KL. Normal sleep in African-Americans and Caucasian-Americans: A meta-analysis. Sleep Med 2011;12:209–14. 10.1016/j.sleep.2010.12.010. [DOI] [PubMed] [Google Scholar]
- [10].Carnethon MR, De Chavez PJ, Zee PC, Kim K-YA, Liu K, Goldberger JJ, et al. Disparities in sleep characteristics by race/ethnicity in a population-based sample: Chicago Area Sleep Study. Sleep Med 2016;18:50–5. 10.1016/j.sleep.2015.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Shimizu M, Gillis BT, Buckhalt JA, El-Sheikh M. Linear and Nonlinear Associations between Sleep and Adjustment in Adolescence. Behav Sleep Med 2020;18:690–704. 10.1080/15402002.2019.1665049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Curtis DS, Fuller-Rowell TE, El-Sheikh M, Carnethon MR, Ryff CD. Habitual sleep as a contributor to racial differences in cardiometabolic risk. Proc Natl Acad Sci U S A 2017;114:8889–94. 10.1073/pnas.1618167114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Grandner MA, Williams NJ, Knutson KL, Roberts D, Jean-Louis G. Sleep disparity, race/ethnicity, and socioeconomic position. Sleep Med 2016;18:7–18. 10.1016/j.sleep.2015.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Fuller-Rowell TE, Curtis DS, El-Sheikh M, Duke AM, Ryff CD, Zgierska AE. Racial discrimination mediates race differences in sleep problems: A longitudinal analysis. Cultur Divers Ethnic Minor Psychol 2017;23:165–73. 10.1037/cdp0000104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Yip T, Cheon YM, Wang Y, Cham H, Tryon W, El-Sheikh M. Racial Disparities in Sleep: Associations With Discrimination Among Ethnic/Racial Minority Adolescents. Child Dev 2020;91:914–31. 10.1111/cdev.13234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Troxel WM, Shih RA, Ewing B, Tucker JS, Nugroho A, D’Amico EJ. Examination of neighborhood disadvantage and sleep in a multi-ethnic cohort of adolescents. Health Place 2017;45:39–45. 10.1016/j.healthplace.2017.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Bagley EJ, Tu KM, Buckhalt JA, El-Sheikh M. Community violence concerns and adolescent sleep. Sleep Health 2016;2:57–62. 10.1016/j.sleh.2015.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Kliewer W, Lepore SJ. Exposure to Violence, Social Cognitive Processing, and Sleep Problems in Urban Adolescents. J Youth Adolesc 2015;44:507–17. 10.1007/s10964-014-0184-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Rubens SL, Fite PJ, Cooley JL, Canter KS. The Role of Sleep in the Relation Between Community Violence Exposure and Delinquency Among Latino Adolescents. J Community Psychol 2014;42:723–34. 10.1002/jcop.21648. [DOI] [Google Scholar]
- [20].Heissel JA, Sharkey PT, Torrats-Espinosa G, Grant K, Adam EK. Violence and Vigilance: The Acute Effects of Community Violent Crime on Sleep and Cortisol. Child Dev 2018;89:e323–31. 10.1111/cdev.12889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Umlauf MG, Bolland JM, Lian BE. Sleep Disturbance and Risk Behaviors among Inner-City African-American Adolescents. J Urban Health Bull N Y Acad Med 2011;88:1130–42. 10.1007/s11524-011-9591-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Umlauf MG, Bolland AC, Bolland KA, Tomek S, Bolland JM. The effects of age, gender, hopelessness, and exposure to violence on sleep disorder symptoms and daytime sleepiness among adolescents in impoverished neighborhoods. J Youth Adolesc 2015;44:518–42. 10.1007/s10964-014-0160-5. [DOI] [PubMed] [Google Scholar]
- [23].Hill TD, Trinh HN, Wen M, Hale L. Perceived neighborhood safety and sleep quality: a global analysis of six countries. Sleep Med 2016;18:56–60. 10.1016/j.sleep.2014.12.003. [DOI] [PubMed] [Google Scholar]
- [24].Johnson DA, Brown DL, Morgenstern LB, Meurer WJ, Lisabeth LD. The association of neighborhood characteristics with sleep duration and daytime sleepiness. Sleep Health 2015;1:148–55. 10.1016/j.sleh.2015.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Steptoe A, O’Donnell K, Marmot M, Wardle J. Positive affect, psychological well-being, and good sleep. J Psychosom Res 2008;64:409–15. 10.1016/j.jpsychores.2007.11.008. [DOI] [PubMed] [Google Scholar]
- [26].Troxel WM, DeSantis A, Richardson AS, Beckman R, Ghosh-Dastidar B, Nugroho A, et al. Neighborhood disadvantage is associated with actigraphy-assessed sleep continuity and short sleep duration. Sleep 2018;41. 10.1093/sleep/zsy140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Dahl RE. The regulation of sleep and arousal. Dev Psychopathol 1996;8:3–27. 10.1017/S0954579400006945. [DOI] [Google Scholar]
- [28].Dahl RE, Lewin DS. Pathways to adolescent health sleep regulation and behavior. J Adolesc Health 2002;31:175–84. 10.1016/S1054-139X(02)00506-2. [DOI] [PubMed] [Google Scholar]
- [29].El-Sheikh M, Buckhalt JA, Mize J, Acebo C. Marital Conflict and Disruption of Children’s Sleep. Child Dev 2006;77:31–43. 10.1111/j.1467-8624.2006.00854.x. [DOI] [PubMed] [Google Scholar]
- [30].Philbrook LE, Buckhalt JA, El-Sheikh M. Community violence concerns and adolescent sleep: Physiological regulation and race as moderators. J Sleep Res 2020;29:e12897. 10.1111/jsr.12897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med 1999;131:485–91. [DOI] [PubMed] [Google Scholar]
- [32].Hublin C, Partinen M, Kaprio J, Koskenvuo M, Guilleminault C. Epidemiology of Narcolepsy. Sleep 1994;17:S7–12. 10.1093/sleep/17.suppl_8.S7. [DOI] [PubMed] [Google Scholar]
- [33].Garcia-Borreguero D, Stillman P, Benes H, Buschmann H, Chaudhuri KR, Gonzalez Rodríguez VM, et al. Algorithms for the diagnosis and treatment of restless legs syndrome in primary care. BMC Neurol 2011;11:28. 10.1186/1471-2377-11-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Morin CM, Belleville G, Bélanger L, Ivers H. The Insomnia Severity Index: Psychometric Indicators to Detect Insomnia Cases and Evaluate Treatment Response. Sleep 2011;34:601–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Marino M, Li Y, Rueschman MN, Winkelman JW, Ellenbogen JM, Solet JM, et al. Measuring Sleep: Accuracy, Sensitivity, and Specificity of Wrist Actigraphy Compared to Polysomnography. Sleep 2013;36:1747–55. 10.5665/sleep.3142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Chow CM, Wong SN, Shin M, Maddox RG, Feilds K-L, Paxton K, et al. Defining the rest interval associated with the main sleep period in actigraph scoring. Nat Sci Sleep 2016;8:321–8. 10.2147/NSS.S114969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].El-Sheikh M, Sadeh A. I. Sleep and Development: Introduction to the Monograph. Monogr Soc Res Child Dev 2015;80:1–14. 10.1111/mono.12141. [DOI] [PubMed] [Google Scholar]
- [38].Koo TK, Li MY. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J Chiropr Med 2016;15:155–63. 10.1016/j.jcm.2016.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Johns MW. Reliability and Factor Analysis of the Epworth Sleepiness Scale. Sleep 1992;15:376–81. 10.1093/sleep/15.4.376. [DOI] [PubMed] [Google Scholar]
- [40].Janicki-Deverts D, Cohen S, Doyle WJ, Marsland AL, Bosch J. Childhood environments and cytomegalovirus serostatus and reactivation in adults. Brain Behav Immun 2014;40:174–81. 10.1016/j.bbi.2014.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Mujahid MS, Diez Roux AV, Morenoff JD, Raghunathan T. Assessing the Measurement Properties of Neighborhood Scales: From Psychometrics to Ecometrics. Am J Epidemiol 2007;165:858–67. 10.1093/aje/kwm040. [DOI] [PubMed] [Google Scholar]
- [42].Compas BE, Davis GE, Forsythe CJ, Wagner BM. Assessment of major and daily stressful events during adolescence: The Adolescent Perceived Events Scale. J Consult Clin Psychol 1987;55:534–41. 10.1037/0022-006X.55.4.534. [DOI] [PubMed] [Google Scholar]
- [43].Podsakoff PM, MacKenzie SB, Lee J-Y, Podsakoff NP. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol 2003;88:879–903. 10.1037/0021-9010.88.5.879. [DOI] [PubMed] [Google Scholar]
- [44].Zimmerman M Methodological issues in the assessment of life events: A review of issues and research. Clin Psychol Rev 1983;3:339–70. 10.1016/0272-7358(83)90019-3. [DOI] [Google Scholar]
- [45].U.S. Census Bureau. How the Census Bureau measures poverty 2012.
- [46].DeSalvo KB, Olson R, Casavale KO. Dietary Guidelines for Americans. JAMA 2016;315:457–8. 10.1001/jama.2015.18396. [DOI] [PubMed] [Google Scholar]
- [47].Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. 1996. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- [48].Dozois DJA, Dobson KS, Ahnberg JL. A psychometric evaluation of the Beck Depression inventory-II. Psychol Assess 1998;10:83–9. [Google Scholar]
- [49].Åkerstedt T, Wright KP. Sleep Loss and Fatigue in Shift Work and Shift Work Disorder. Sleep Med Clin 2009;4:257–71. 10.1016/j.jsmc.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Mezick EJ, Wing RR, McCaffery JM. Associations of self-reported and actigraphy-assessed sleep characteristics with body mass index and waist circumference in adults: Moderation by gender. Sleep Med 2014;15:64–70. 10.1016/j.sleep.2013.08.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Taylor DJ, Bramoweth AD, Grieser EA, Tatum JI, Roane BM. Epidemiology of Insomnia in College Students: Relationship With Mental Health, Quality of Life, and Substance Use Difficulties. Behav Ther 2013;44:339–48. 10.1016/j.beth.2012.12.001. [DOI] [PubMed] [Google Scholar]
- [52].Roux AVD, Mair C. Neighborhoods and health. Ann N Y Acad Sci 2010;1186:125–45. [DOI] [PubMed] [Google Scholar]
- [53].Bollen KA. Structural Equations with Latent Variables. New York: Wiley; 1989. [Google Scholar]
- [54].Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychol Methods 2002;7:422–45. [PubMed] [Google Scholar]
- [55].Enders CK. Dealing with missing data in developmental research. Child Dev Perspect 2013;7:27–31. 10.1111/cdep.12008. [DOI] [Google Scholar]
- [56].Jackson CL, Redline S, Emmons KM. Sleep as a potential fundamental contributor to disparities in cardiovascular health. Annu Rev Public Health 2015;36:417–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Koh HK. A 2020 Vision for Healthy People. N Engl J Med 2010;362:1653–6. 10.1056/NEJMp1001601. [DOI] [PubMed] [Google Scholar]
- [58].Griggs S, Conley S, Batten J, Grey M. A systematic review and meta-analysis of behavioral sleep interventions for adolescents and emerging adults. Sleep Med Rev 2020;54:101356. 10.1016/j.smrv.2020.101356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Knutson KL. Sleep duration and cardiometabolic risk: A review of the epidemiologic evidence. Best Pract Res Clin Endocrinol Metab 2010;24:731–43. 10.1016/j.beem.2010.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Troxel WM, Buysse DJ, Matthews KA, Kip KE, Strollo PJ, Hall M, et al. Sleep Symptoms Predict the Development of the Metabolic Syndrome. Sleep 2010;33:1633–40. 10.1093/sleep/33.12.1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].DeSantis AS, Diez Roux AV, Moore K, Baron KG, Mujahid MS, Nieto FJ. Associations of Neighborhood Characteristics with Sleep Timing and Quality: The Multi-Ethnic Study of Atherosclerosis. Sleep 2013;36:1543–51. 10.5665/sleep.3054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Billings T, Berg-Cross L. Sleep Competing Activities and Sleep Problems in Minority College Students. J Racial Ethn Health Disparities 2014;1:300–8. 10.1007/s40615-014-0037-z. [DOI] [Google Scholar]
- [63].Clarke PJ, O’Malley PM, Johnston LD, Schulenberg JE, Lantz P. Differential Trends in Weight-Related Health Behaviors Among American Young Adults by Gender, Race/Ethnicity, and Socioeconomic Status: 1984–2006. Am J Public Health 2009;99:1893–901. 10.2105/AJPH.2008.141317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Walsemann KM, Ailshire JA, Gee GC. Student loans and racial disparities in self-reported sleep duration: evidence from a nationally representative sample of US young adults. J Epidemiol Community Health 2016;70:42–8. [DOI] [PubMed] [Google Scholar]
- [65].Jones RD, Jackson WB, Mazzei A, Chang A-M, Buxton OM, Jackson CL. Ethnoracial sleep disparities among college students living in dormitories in the United States: a nationally representative study. Sleep Health 2020;6:40–7. 10.1016/j.sleh.2019.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Petrov ME, Lichstein KL. Differences in sleep between black and white adults: An update and future directions. Sleep Med 2015. doi: 10.1016/j.sleep.2015.01.011. [DOI] [PubMed] [Google Scholar]
- [67].Fuller-Rowell TE, Curtis DS, El-Sheikh M, Chae DH, Boylan JM, Ryff CD. Racial disparities in sleep: The role of neighborhood disadvantage. Sleep Med 2016;27–28:1–8. 10.1016/j.sleep.2016.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Lauderdale DS, Knutson KL, Yan LL, Rathouz PJ, Hulley SB, Sidney S, et al. Objectively Measured Sleep Characteristics among Early-Middle-Aged Adults The CARDIA Study. Am J Epidemiol 2006;164:5–16. 10.1093/aje/kwj199. [DOI] [PubMed] [Google Scholar]
- [69].Matthews KA, Hall M, Dahl RE. Sleep in Healthy Black and White Adolescents. Pediatrics 2014;133:e1189–96. 10.1542/peds.2013-2399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Whinnery J, Jackson N, Rattanaumpawan P, Grandner MA. Short and long sleep duration associated with race/ethnicity, sociodemographics, and socioeconomic position. Sleep 2014;37:601–11. 10.5665/sleep.3508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Johnson DA, Lisabeth L, Hickson D, Johnson-Lawrence V, Samdarshi T, Taylor H, et al. The Social Patterning of Sleep in African Americans: Associations of Socioeconomic Position and Neighborhood Characteristics with Sleep in the Jackson Heart Study. Sleep 2016;39:1749–59. 10.5665/sleep.6106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Osypuk TL, Kehm R, Misra DP. Where We Used to Live: Validating Retrospective Measures of Childhood Neighborhood Context for Life Course Epidemiologic Studies. PLOS ONE 2015;10:e0124635. 10.1371/journal.pone.0124635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73].Johnson DA, Simonelli G, Moore K, Billings M, Mujahid MS, Rueschman M, et al. The Neighborhood Social Environment and Objective Measures of Sleep in the Multi-Ethnic Study of Atherosclerosis. Sleep 2017;40. 10.1093/sleep/zsw016. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


