Abstract
Using data from the German Ageing Survey (Deutscher Alterssurvey, DEAS; N = 4,712), this study examined age-related change in three dimensions of self-perceptions of aging (SPA): perceptions of physical losses, social losses, and ongoing development. Participants ranged in age from 40 to 85 years at study entry (1996, 2002, or 2008) and were followed for up to 21 years. Time-invariant, context-specific and time-varying, person-specific predictors of the observed age-related changes were examined. Findings from longitudinal multilevel regression analyses showed significant nonlinear age-related change for all three dimensions. Specifically, starting at about age 65, participants showed age-related increases in perceptions of physical and social losses, with increases getting steeper in old age. Starting at about age 55, participants reported increasingly fewer perceptions related to ongoing development. The decline in perceptions of ongoing development also became increasingly steeper after age 70. Region of residence was a significant context-specific predictor of the intercepts of the three SPA dimensions. Health-related variables (i.e., number of chronic diseases, self-rated health), affective well-being (i.e., positive and negative affect), and measures of social integration (i.e., loneliness) were significant person-specific predictors. Health-related variables had their strongest association with perceptions of physical losses, whereas negative affect and loneliness had their strongest association with perceptions of social losses. Positive affect had its strongest association with perceptions of ongoing development. This study is the first one to describe age-related change trajectories in multiple dimensions of SPA and significant predictors of these change trajectories.
Keywords: multidimensional self-perceptions of aging, age-related change trajectories, context-specific predictors, person-specific predictors
The concept of self-perceptions of aging (SPA) refers to the well-documented observation that individuals have perceptions of their own aging that they can articulate and reflect about (Diehl & Wahl, 2010; Steverink et al., 2001). SPA are based on individuals’ age-related experiences and expectations in different life domains and on age-related feedback from the social environment (Miche, Wahl, et al., 2014), and include perceptions of age-related losses and gains (Brothers et al., 2019; Steverink et al., 2001; Wurm et al., 2017). Loss-related SPA may refer to physical (e.g., having more wrinkles) or psychological changes (e.g., becoming more forgetful), social losses (e.g., death of close friends), or changes in personality (e.g., becoming more rigid). In contrast, gain- or growth-related SPA may refer to having fewer responsibilities and more liberties, having possibilities to learn new things, having become more generative, or having increased in competence and life experience. Importantly, SPA are significant predictors of a host of important developmental outcomes, including cognitive functioning (Robertson et al., 2016; Sargent-Cox et al., 2012a, 2014; Siebert et al., 2018; Stephan et al., 2014; Tovel et al., 2019), psychological well-being (Westerhof & Barrett, 2005; Wurm et al., 2008), social relations and social involvement (Menkin et al., 2017; Schwartz et al., 2020), and health and longevity (Kotter-Grühn et al., 2009; Levy et al., 2002; Sargent-Cox et al., 2014; Spuling et al., 2013; Uotinen et al., 2005; Westerhof et al., 2014; Wurm et al., 2007). Although these associations are well documented, very little is known about how SPA themselves change as individuals develop from midlife into later adulthood (for exceptions, see Jung et al., 2019; Wolff et al., 2018; Wurm et al., 2019).
The current study examined age-related change in three dimensions of SPA in a nationally representative sample of middle-aged and older adults who were followed for up to 21 years. The three dimensions included participants’ SPA regarding physical losses, social losses, and ongoing development. Furthermore, we examined time-invariant, context-specific and time-varying, person-specific predictors of the observed age-related changes. Investigation of such predictors of age-related changes in SPA is important, because SPA become increasingly self-relevant from midlife to early old age (Diehl & Wahl, 2010; Infurna et al., 2020; Levy, 2009) and influence how adults respond to the challenges of growing old(er) (Diehl et al., 2020; Kornadt, Kessler, et al., 2019).
Self-Perceptions of Aging: A Multidimensional View
To date, the overwhelming majority of studies have focused on adults’ perceptions of their own aging in a unidimensional way, either in the form of subjective age ratings (using the single question “How old do you feel most of the time?”) or in terms of attitudes toward own aging (ATOA; Lawton, 1975). Informed by lifespan developmental psychology (Baltes, 1987; Kornadt, Kessler, et al., 2019), this approach, however, has been criticized because it neglects the multidimensional and potentially multidirectional nature of adults’ SPA (Diehl et al., 2015; Hess et al., 2017; Wurm et al., 2017). That is, individuals’ SPA may differ not only in terms of their valence (i.e., positive vs. negative), but also by behavioral domain (Diehl & Wahl, 2010; Kornadt & Rothermund, 2011; Steverink et al., 2001). This assumption is consistent with findings showing that adults have well-defined expectations and beliefs about age-related gains and losses in different behavioral domains (Heckhausen et al., 1989) that may influence their reactions to perceived age-related changes and, hence, their SPA (Beyer, Wolff, et al., 2019; Diehl & Wahl, 2010; Levy & Myers, 2004; Wurm et al., 2013). Moreover, adopting a multidimensional perspective (Heckhausen et al., 1989; Hess et al., 2017) raises the question whether individuals’ age-related perceptions in different behavioral domains change in uniform or potentially different, multidirectional ways across the adult lifespan (Baltes, 1987; Kornadt, Kessler, et al., 2019). Although multidirectionality refers primarily to whether “the direction of change varies by categories of behavior” (Baltes, 1987, p. 613), it also refers to the timing, shape, and rate of change in different behavioral domains. In terms of timing of change, for example, individuals may already perceive age-related changes in some behavioral domains (e.g., physical appearance, health) in midlife, whereas changes in other domains (e.g., social relationships) may not be perceived until much later in life. Similarly, in terms of the shape and rate of change, some dimensions may change in a linear age-related way and show relatively gradual changes, whereas others may show nonlinear change trajectories and exhibit larger changes. Given these implications of a multidimensional and multidirectional conceptualization of adults’ SPA, the first study objective focused on the examination of the timing, shape, and rate of age-related change for three separate dimensions of SPA: perceptions of physical losses, social losses, and ongoing development.
This study objective extends past work which has mostly focused on adults’ SPA as predictors of outcomes (Kotter-Grühn et al., 2009; Levy et al., 2002; Robertson et al., 2016; Sargent-Cox et al., 2012a, 2012b; Westerhof et al., 2014). In contrast to this previous work, the current study conceptualizes adults’ SPA as the outcome variable and examines the predictors of the observed age-related changes. Furthermore, the present study extends past work by addressing questions related to the timing, shape, and rate of the observed age-related changes (Baltes, 1987; Kornadt, Kessler, et al., 2019).
Examination of Age-Related Change in Self-Perceptions of Aging
This study is the first to examine long-term age-related change in multiple dimensions of SPA, thus addressing the lifespan principles of multidimensionality and multidirectionality (Baltes, 1987; Kornadt, Kessler, et al., 2019). Given the importance of SPA for a host of important outcomes in later life (Kotter-Grühn et al., 2009; Levy et al., 2002; Menkin et al., 2017; Robertson et al., 2016; Sargent-Cox et al., 2012a; Schwartz et al., 2020; Siebert et al., 2018; Westerhof et al., 2014), it is critically important to understand how different dimensions of adults’ SPA develop and change over the course of the adult lifespan (Kornadt, Kessler, et al., 2019). Moreover, because there are substantial interindividual differences in the different dimensions of SPA (Jung et al., 2019; Spuling et al., 2019), it is also crucial to understand the correlates/predictors that account for interindividual differences in the change trajectories of adults’ SPA.
Research on changes in SPA has been very limited to date and has primarily focused on unidimensional measures. The findings from these studies with unidimensional measures (Kleinspehn-Ammerlahn et al., 2008; Kotter-Grühn et al., 2009; Miche, Elsässer, et al., 2014) document that age-related change in SPA occurs and is less steep in midlife than in later adulthood. To date, only one other study has examined longitudinal change in multiple dimensions of SPA. Jung et al. (2019) used four waves of the Deutscher Alterssurvey (DEAS) to examine time-related change in the dimensions of the Aging-Related Cognitions Scales (AgeCog; Wurm et al., 2007) over a 15-year period. These authors also examined predictors of interindividual differences in starting level but did not examine predictors of the change trajectories because they found only little interindividual variance in these trajectories. Findings from linear growth curve models showed that the average slope across time was only significant for the dimensions of social losses and ongoing development, indicating changes toward more negative SPA in these domains. Different sets of predictors accounted for the interindividual differences in the starting levels, with health-related (e.g., self-rated health and number of illnesses) and social network variables being the most consistent predictors. These findings were relevant for the current study for two reasons. First, instead of examining time-related change, we opted to examine age-related change in the different AgeCog dimensions. Second, this study provided guidance in the selection of the context- and person-specific predictors examined in the present study. Furthermore, in contrast to Jung et al. (2019), predictors of intercepts and slopes of the SPA dimensions were specified in the present study, and both time-invariant as well as time-varying predictors were tested.
Predictors of Age-Related Changes in Self-Perceptions of Aging
Although conceptual models have proposed a variety of correlates/predictors of adults’ SPA (Diehl & Wahl, 2010; Kornadt, Kessler, et al., 2019), actual studies examining the relevance of such predictors are scarce (Jung et al., 2019; Miche, Elsässer, et al., 2014; Wolff et al., 2018; Wurm et al., 2019; Wurm & Huxhold, 2012). Thus, the second objective of this study focused on testing predictors of the observed age-related changes in the different dimensions of the AgeCog scales. Specifically, we examined the effects of time-invariant, context-specific and time-varying, person-specific correlates/predictors based on three criteria: First, the chosen predictors were identified in conceptual models and relevant literature reviews (Diehl & Wahl, 2010; Kornadt, Kessler, et al., 2019). Second, the relevance of the predictors was supported by findings from previous studies (Jung et al., 2019; Miche, Elsässer, et al., 2014; Wolff et al., 2018; Wurm et al., 2019; Wurm & Huxhold, 2012). Third, the identified predictor variables were available for all measurement occasions of the German Ageing Survey.
Context-Specific Predictors
Geographical region of residence was included as a time-invariant, context-specific predictor because participants in the DEAS were sampled nationwide and were stratified by former West or East Germany. This distinction was important because individuals in these two regions grew into midlife and old age under very different political and social systems, which may have influenced how they perceived their own aging (Hess et al., 2017; Löckenhoff et al., 2009; North & Fiske, 2015). Moreover, the political unification in 1990 was accompanied by profound socio-political and economic changes in the regions of Eastern Germany. These changes resulted, among others, in unemployment, disrupted occupational careers, and involuntary early retirement, threatening middle-aged and older adults social and financial security. This may, in part, explain why adults in Eastern Germany hold more negative SPA compared to their counterparts in Western Germany, even two decades after the unification (Wurm & Huxhold, 2012). Furthermore, more regions in Eastern Germany show fast rising rates of population aging compared to regions in Western Germany. This may affect the availability of resources that may facilitate successful aging at the societal level and, hence, influence individuals’ SPA. For example, Wolff et al. (2018) showed that adults living in regions with a fast population aging rate held more negative SPA in terms of physical losses and ongoing development compared to adults living in regions with slow population aging.
Participants’ level of education was included as another time-invariant, context-specific predictor. Level of education was included as a proxy for participants’ socio-economic status (SES; see Kirsch et al., 2019; Miche, Elsässer, et al., 2014), because we expected that individuals with a higher SES (i.e., a higher level of education) may perceive age-related changes more favorably than individuals with a lower SES (Jung et al., 2019; Spuling et al., 2019).
Person-Specific Predictors
In terms of time-varying, person-specific predictors, we included variables from three domains: the health domain, the affective domain, and the social integration domain. Consistent with the findings from previous studies (Jung et al., 2019; Miche, Elsässer, et al., 2014), we included participants’ subjective health ratings and the number of chronic diseases as predictors of change in SPA. Although most previous studies have examined the effects of SPA on indicators of health and longevity (Levy et al., 2002; Kotter-Grühn et al., 2009; Sargent-Cox et al., 2012a; Westerhof et al., 2014), several studies have shown that adults’ health-related experiences are significant predictors of their SPA (e.g., Sargent-Cox et al., 2012b; Wurm et al., 2007, 2019).
In terms of indicators of affective well-being, we included the Positive and Negative Affect Schedule (PANAS; Watson et al., 1988). To the best of our knowledge, positive and negative affect have not been examined as predictors of age-related changes in multidimensional SPA. However, we expected that indicators of affective well-being would show significant associations with the three dimensions of the AgeCog scales because affective states influence how individuals perceive and evaluate their own aging process (Bryant et al., 2016; Dutt & Wahl, 2017). Moreover, Miche, Elsässer, et al. (2014) examined the effects of the personality traits extraversion (known as positive affectivity) and neuroticism (known as negative affectivity; McAdams, 2009) on middle-aged and older adults’ level and change in ATOA and found a positive association between neuroticism and more negative ATOA at the beginning of the study, but no association with change in ATOA over time.
Lastly, we also expected that participants’ social integration, as assessed in terms of the size of their social network and a measure of loneliness (De Jong Gierveld & Van Tilburg, 2006), may be associated with age-related changes in the AgeCog scales. This assumption was informed by a body of literature documenting the positive effects of social networks and social relationships on health and well-being in adulthood and old age (Antonucci, 2001; Rook & Charles, 2017). This literature suggests that being embedded into a supportive social network and not feeling lonely (Holt-Lunstad et al., 2015) serve as a protective buffer when age-related events (e.g., transition into retirement; loss of a loved person) challenge adults’ perceptions and evaluations of their own aging. Moreover, recent findings by Schwartz et al. (2020) showed that involvement in informal social activities predicted more positive change in SPA over a 6-year period.
The Present Study
Given the assumptions of theoretical models and findings from previous studies, we predicted the following age-related changes in the three AgeCog dimensions. For physical losses and social losses, we predicted that as individuals get older, they will report more SPA in both dimensions (i.e., positive association), with the possibility that the age-related trajectory may become steeper in very old age (i.e., nonlinear change). This prediction was based on evidence suggesting that health-related incidents (Baltes & Smith, 2003; Wolff et al., 2002) and social losses (Rook & Charles, 2017) increase with age and, therefore, may shape individuals’ SPA in these domains. In terms of ongoing development, we predicted negative age-related change that may possibly become steeper in very old age. This prediction was based on evidence suggesting that as individuals advance in age, they become more selective in the type of activities they pursue (Charles & Carstensen, 2010) and may therefore have more limited opportunities to experience ongoing development. Also, in very old age greater vulnerabilities in health (Baltes & Smith, 2003), cognitive functioning (Salthouse, 2019; Schaie, 2013), and self-regulatory processes (Diehl et al., 2014; Gerstorf & Ram, 2009) may constrain individuals’ opportunities to experience continued development. To test these predictions, we specified linear and quadratic effects of age-related change in longitudinal multilevel regression models.
The predictions regarding the effects of the time-invariant, context-specific predictors of the observed age-related changes were based on theoretical frameworks and findings from previous studies. In terms of region of residence, we expected that adults in the former region of East Germany would report higher perceptions of physical and social losses and lower perceptions of ongoing development than adults in the former region of West Germany. We did not specify any predictions in terms of regional differences in change trajectories because previous evidence in this regard has been very limited.
In terms of level of education, we predicted that individuals with a higher level of education would report less negative SPA in terms of physical and social losses, and more positive perceptions in terms of ongoing development (Beyer et al., 2017). We also expected that adults with a higher level of education would show more favorable age-related changes on these dimensions compared to individuals with a lower level of education.
In terms of the effects of the time-varying, person-specific predictors, we predicted that they would behave in a domain-specific way, similarly to what has been documented in terms of the stereotype-matching effect (Levy & Leifheit-Limson, 2009). That is, participants’ self-rated health and number of chronic diseases were expected to show their strongest time-varying associations with self-perceptions in the physical losses domain compared to the two other domains. For positive affect, we expected a positive time-varying association with perceptions of ongoing development and a negative association with perceptions of physical and social losses. Conversely, we predicted that negative affect would be negatively associated with participants’ perceptions of ongoing development and positively associated with perceptions of physical losses and social losses. Overall, we expected that positive affect would show the strongest association with the dimension of ongoing development, whereas negative affect would show the strongest association with the dimension of social losses.
Lastly, we predicted that the size of study participants’ social network would be negatively associated with their perceptions of physical and social losses, and positively associated with their perceptions of ongoing development. Regarding loneliness, we predicted a positive association with perceptions of physical and social losses and a negative association with perceptions of ongoing development. Overall, we expected that social network size and loneliness would show their strongest association with the dimension of social losses and a weaker association with the dimensions of physical losses and of ongoing development.
Method
Study Population and Sample Description
This study used a subsample of the DEAS, consisting of community-dwelling adults between age 40 and 85 years at study entry (for details on the study design and sampling, see Klaus et al., 2017). The survey is a cohort-sequential study and six waves of measurement have been completed to date (T1: 1996, T2: 2002, T3: 2008, T4: 2011, T5: 2014, T6: 2017). At each measurement point, except in 2011 and 2017, a new sample was drawn based on national probability sampling. All samples were stratified by age, gender, and region (i.e., former West or East Germany). Study participants who agreed were re-interviewed at the subsequent measurement points.
For the analyses presented here, we included only participants who provided three or more observations and who had at least one valid observation on the SPA outcomes and on each included predictor. This resulted in a study sample of 4,712 individuals. Individuals with fewer than three observations may not provide enough repeated data for a reliable estimation of the age-related change trajectories and their predictors, particularly if nonlinear trajectories and within-person predictor effects are estimated. Descriptive statistics for the socio-demographic and predictor variables are shown in Tables 1 and 2, respectively.
Table 1.
Sample Description (Time-Invariant Study Variables)
| Variable | n/% |
|---|---|
| Gender | |
| Women | 2,361 (50.1%) |
| Men | 2,351 (49.9%) |
| Region | |
| Eastern Germany | 1,574 (33.4%) |
| Western Germany | 3,138 (66.6%) |
| Education | |
| Low | 335 (7.1%) |
| Medium | 2,416 (51.3%) |
| High | 1,961 (41.6%) |
| Number of observations | |
| 3 | 1,457 (30.9%) |
| 4 | 2,242 (47.6%) |
| 5 | 703 (14.9%) |
| 6 | 310 (6.6%) |
| Study cohort: first participationa | |
| 1996 | 1,296 (27.5%) |
| 2002 | 1,002 (21.3%) |
| 2008 | 2,414 (51.2%) |
Note.
By including only individuals with three or more observations, all individuals who first participated in 2014 were dropped, because they had only 1 or 2 observations.
Table 2.
Comparison of the Study Sample and the Parent Sample
| Variable | Study sample | Parent sample | Effect size d |
|---|---|---|---|
| Gender | |||
| Women, n (%) | 2,361 (50.1%) | 7,884 (49.2%) | |
| Men, n (%) | 2,351 (49.9%) | 8,139 (50.8%) | |
| Region | |||
| Eastern Germany, n (%) | 1,574 (33.4%) | 5,423 (33.8%) | |
| Western Germany, n (%) | 3,138 (66.6%) | 10,600 (66.2%) | |
| Education | |||
| Low, n (%) | 335 (7.1%) | 1,715 (10.7%) | |
| Medium, n (%) | 2,416 (51.3%) | 8,714 (54.6%) | |
| High, n (%) | 1,961 (41.6%) | 5,567 (34.7%) | |
| Age at baseline, M (SD) | 57.45 (10.83) | 60.98 (11.92) | −.30 |
| AgeCog scales, M (SD) | |||
| Physical losses | 2.72 (0.58) | 2.81 (0.59) | −.15 |
| Social losses | 1.77 (0.56) | 1.84 (0.60) | −.12 |
| Ongoing development | 3.03 (0.55) | 2.88 (0.63) | .24 |
| Health, M (SD) | |||
| Self-rated health | 3.67 (0.78) | 3.51 (0.86) | .19 |
| Chronic conditions | 2.14 (1.68) | 2.41 (1.88) | −.14 |
| Affective well-being, M (SD) | |||
| Positive affect | 3.54 (0.54) | 3.46 (0.59) | .14 |
| Negative affect | 2.07 (0.53) | 2.06 (0.55) | .02 |
| Social integration, M (SD) | |||
| Social network size | 4.92 (2.71) | 4.67 (2.75) | .09 |
| Loneliness | 1.73 (0.54) | 1.76 (0.57) | −.05 |
Note. Effect size d computed according to Cohen (1992).
Because limiting the sample to those participants who were assessed at least three times may result in a selected sample, we performed several analyses to quantify potential selection effects. The findings from these analyses showed that the selection effects were small (e.g., d = .02 to d = −.30; see Table 2) and for all practical purposes negligible (for a detailed description, see Supplemental Materials).
Measures
Self-Perceptions of Aging
The Aging-Related Cognitions Scales (AgeCog; Steverink et al., 2001; Wurm et al., 2007) were used to assess participants’ SPA. These scales were established via exploratory (Steverink et al., 2001) and confirmatory factor analysis (Jung et al., 2019; Wurm et al., 2007) and consist of three dimensions: perceptions of physical losses, social losses, and ongoing development. Each scale has four items that are answered on a four-point scale (1 = strongly agree to 4 = strongly disagree). The exact wording of the items is shown in Table S1 in the Supplemental Materials. Sum scores were calculated for each scale so that greater values indicated higher perceptions of physical losses, social losses, and ongoing development, respectively. Reliability coefficients (Cronbach’s α) for the six occasions of measurement from 1996 to 2017 were for physical losses .78, .78, .77, .79, .78, and .79, respectively; for social losses .74, .67, .73, .71, .72, and .73, respectively; and for ongoing development .71, .72, .79, .79, .79, and .81, respectively. Evidence supporting the multidimensionality of the scales is provided in Table S2 in the Supplemental Materials. Specifically, across times of measurement the intercorrelations among the three scales (bolded and underlined coefficients in Table S2) indicated that the shared variance ranged from 8% to 20%. This suggests highly distinct dimensions.
Time-Invariant, Context-Specific Predictors
Region of residence (West vs. East Germany), and level of education were included as socio-demographic variables. Level of education was determined using the International Standard Classification of Education (ISCED) coding (UNESCO, 2012). This classification was based on school and professional education, differentiating between low (ISCED 0–2; high-school education or less), medium (ISCED 3–4; completed vocational training or college degree), and high education (ISCED 5–6; advanced professional training and graduate or professional degrees).
Time-Varying, Person-Specific Predictors
Health
Number of Chronic Diseases.
Study participants indicated on a list of 11 different chronic health conditions (e.g., diabetes, cancer, cardiovascular disease) which of these conditions they had. A sum score was computed as an indicator of chronic disease burden, with a higher score indicating greater chronic disease burden (see Wurm et al., 2007).
Self-Rated Health.
Participants rated their health based on a single item (How would you rate your current health?), which is a common approach to measuring subjective health (e.g., DeSalvo et al., 2006). Participants responded on a five-point scale, ranging from 1 (very good) to 5 (very poor). Participants’ ratings were recoded so that higher scores indicate better self-rated health.
Affective Well-Being
Affective well-being was measured using the PANAS (Watson et al., 1988). Each of the PANAS subscales consists of 10 adjectives describing either positive (e.g., excited, inspired) or negative (e.g., upset, hostile) affective states. Respondents rated on a five-point scale (1 = never to 5 = very often) how often they had experienced each affective state during the past month. Two mean scores were computed per individual, with higher mean scores indicating more positive and more negative affect. Reliability coefficients (Cronbach’s α) for the six occasions of measurement from 1996 to 2017 were for positive affect .86, .84, .86, .86, .87, and .86, respectively, and for negative affect .82, .86, .86, .86, .85, and .85, respectively.
Social Integration
Social network size was assessed by asking participants to name the individuals they considered important to them and with whom they had regular contact. Participants could name up to eight individuals. If their network was larger, all additional persons in the network were grouped into one aggregated category. A sum score was computed (ranging from 0 to 9), with higher scores indicating a larger social network.
A modified version of the six-item De Jong Gierveld loneliness scale (De Jong Gierveld & Van Tilburg, 2006) was used to assess participants’ lack of close relationships and emotional loneliness. The items of the scale (e.g., “There are enough people I feel close to.”—reverse coded) have a response format ranging from 1 (strongly agree) to 4 (strongly disagree), with a higher sum score indicating greater loneliness. Reliability coefficients (Cronbach’s α) for the six occasions of measurement from 1996 to 2017 were .83, .82, .83, .81, .83, and .84, respectively.
Control Variables
Gender and study cohort were included as control variables. Study cohort indicates the year when a participant entered the survey (i.e., 1996, 2002, or 2008).
Statistical Analyses
Longitudinal multilevel regression models (Hox & Kreft, 1994; Ram & Grimm, 2015) were estimated using Stata 15.0 (StataCorp, 2017). Age was specified as the time metric and grand-mean-centered based on all observations (included repeated ones) at 63.78 years to facilitate the interpretation of the intercept as well as all predictor effects on the intercept.
Time-varying predictors permit the examination of between-person (interindividual) differences as well as within-person (intraindividual) change (Curran & Bauer, 2011; Wang & Maxwell, 2015). For a separation of these two components, we specified a grand-mean-centered between-person component (i.e., an individual’s mean score across all their available measurement occasions) and a person-centered within-person component (i.e., the measurement-occasion-specific deviation of an individual from their overall mean) for each time-varying predictor. This approach has been recommended for the testing of time-varying predictor effects in a longitudinal multilevel regression framework (Hoffman & Stawski, 2009).
Following the guidelines by Kass and Raftery (1995), we also checked for nonlinear changes in the age-related trajectories of the AgeCog scales. Specifically, we compared the nonlinear model, which included a quadratic slope component in addition to a linear one, with the linear model in terms of model fit by comparing their values of the Bayesian Information Criterion (BIC). If the difference between the models was 2[ΔBIC] ≥ 6, then the nonlinear model was chosen as the more appropriate representation of the shape of the mean-level age-related trajectory. Additionally, we compared both models based on the Likelihood Ratio Test (LRT) for nested models.
Results
Age-Related Trajectories of Self-Perceptions of Aging
First, we specified random-intercept-only models without any predictors and computed the intraclass correlation (ICC) coefficient for each SPA to determine the proportions of total variance that were due to within-person variation. ICC coefficients for physical losses, social losses, and ongoing development were .51, .49, and .52, respectively, indicating that about 50% of the total variation in each SPA domain was due to within-person variability.
Next, we computed unadjusted models which additionally included age as the slope component, but no other predictors (see Table 3). For all three AgeCog dimensions, the unadjusted nonlinear change model containing a quadratic age component in addition to a linear one provided a better model fit, both in terms of the BIC and the LRT, compared to the linear change model. Therefore, quadratic change models were specified. The inclusion of the fixed and random slope (age) components resulted in proportional reductions of residual variance relative to a random-intercept-only model (R2; computed according to Xu, 2003) that were in a range between .05 (physical losses) and .12 (ongoing development). As shown by the solid lines in Figures 1-3, mean-level changes in all three AgeCog scales became more pronounced with advancing age. Specifically, Figures 1 and 2 show that with advancing age, participants reported increasingly more SPA related to physical losses and social losses, respectively. Furthermore, starting at about age 65, participants showed a steeper increase in SPA related to both physical and social losses (see Figures 1 and 2). Conversely, Figure 3 shows that with advancing age, and particularly in old and very old age, participants reported increasingly fewer SPA related to ongoing development. Although SPA regarding ongoing development already started to decline at age 55, about after age 70 this decline became increasingly steeper (see Figure 3).
Table 3.
Age-Related Trajectories of Self-Perceptions of Aging
| Physical losses |
Social losses |
Ongoing development |
|
|---|---|---|---|
| Fixed regression coefficients | |||
| Intercept [SE] | 2.72*** [0.01] | 1.77*** [0.01] | 2.99*** [0.01] |
| Linear slope [age] [SE] | 0.01*** [0.00] | 0.00*** [0.00] | −0.01*** [0.00] |
| Quadratic slope [age × age] [SE] | 0.00*** [0.00] | 0.00*** [0.00] | −0.00*** [0.00] |
| Random variances | |||
| Variance intercept [SE] | 0.14*** [0.00] | 0.14*** [0.00] | 0.15*** [0.00] |
| Variance slope [SE] | 0.00*** [0.00] | 0.00*** [0.00] | 0.00*** [0.00] |
| Covariance intercept—slope [SE] | −0.00 [0.00] | 0.00*** [0.00] | 0.00*** [0.00] |
| Residual variance [SE] | 0.14*** [0.00] | 0.14*** [0.00] | 0.14*** [0.00] |
| BIC | 22,277.3 | 22,008.79 | 21,417.41 |
| R2 | .05 | .08 | .12 |
Note. Time unit is age [in years], grand-mean-centered [0 corresponds to 63.78 years].
R2: relative reduction in residual variance compared to the residual variance of the unconditional model (Xu, 2003).
p < .05.
p < .01.
p < .001.
Figure 1. Mean-Level Age-Related Trajectories of Perceptions of Physical Losses.

Note. Unadjusted trajectories correspond to the age-related mean-level trajectories without control of any other variables as specified in Table 3. Adjusted trajectories correspond to the age-related mean-level trajectories controlling for all predictors as specified in Table 4.
Figure 3. Mean-Level Age-Related Trajectories of Perceptions of Ongoing Development.
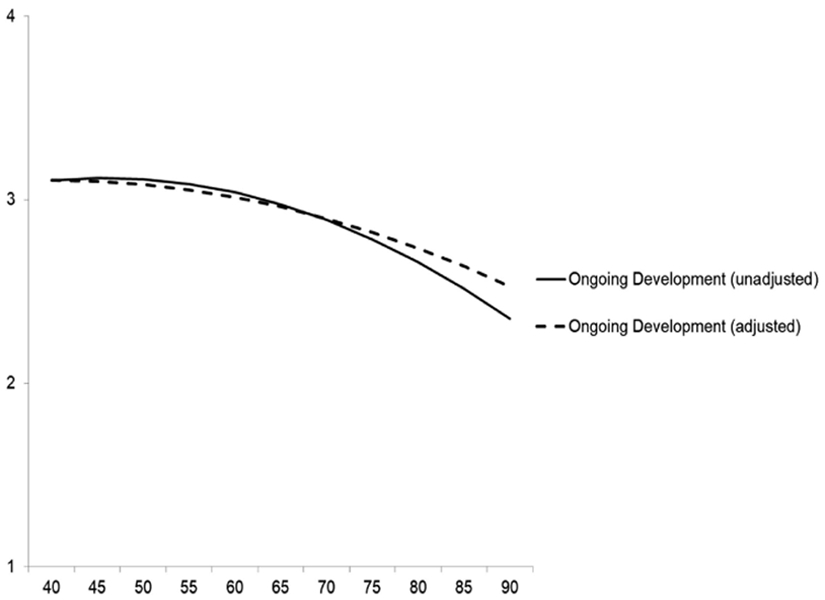
Note. Unadjusted trajectories correspond to the age-related mean-level trajectories without control of any other variables as specified in Table 3. Adjusted trajectories correspond to the age-related mean-level trajectories controlling for all predictors as specified in Table 4.
Figure 2. Mean-Level Age-Related Trajectories of Perceptions of Social Losses.

Note. Unadjusted trajectories correspond to the age-related mean-level trajectories without control of any other variables as specified in Table 3. Adjusted trajectories correspond to the age-related mean-level trajectories controlling for all predictors as specified in Table 4.
Comparing the models containing only age as predictor (solid line in Figures 1-3) with the full models including all time-invariant and time-varying predictors (Table 4; dashed line in Figures 1-3), mean-level increase in physical and social losses as well as mean-level decrease in ongoing development was less steep in the adjusted models containing all predictors. Thus, socio-demographic factors, health, affect, and social integration accounted for some amount of the age-related changes in participants’ SPA. When these predictors were added, the proportional reductions in residual variance (R2), again in reference to the random-intercept-only model, increased to .12 for self-perceptions of physical losses and to .21 for self-perceptions of both social losses and ongoing development. As Figures 1-3 show, although the unadjusted and adjusted trajectories were quite similar in the age range from 40 to about 80, they increasingly diverged after age 80. This divergence was rather small for perceptions of social losses as compared to perceptions of physical losses and ongoing development.
Table 4.
Predictors of Age-Related Change in Self-Perceptions of Aging
| Physical losses | Social losses | Ongoing development | |
|---|---|---|---|
| Fixed regression coefficients | |||
| Intercept [SE] | 2.73*** [0.03] | 1.81*** [0.02] | 2.93*** [0.03] |
| Linear slope [age] [SE] | 0.00 [0.00] | 0.00 [0.00] | −0.01*** [0.00] |
| Quadratic slope [age × age] [SE] | 0.00 [0.00] | 0.00* [0.00] | −0.00*** [0.00] |
| Time-invariant predictors | |||
| Regiona [SE] | 0.05*** [0.01] | 0.04** [0.01] | −0.10*** [0.01] |
| Genderb [SE] | −0.01 [0.01] | −0.00 [0.01] | −0.02 [0.01] |
| Study cohortc [SE] | −0.01 [0.01] | −0.01 [0.01] | −0.01 [0.01] |
| Education [low is reference] | |||
| Medium [SE] | 0.02 [0.03] | −0.02 [0.02] | 0.01 [0.02] |
| High [SE] | 0.08** [0.03] | −0.03 [0.03] | 0.05 [0.03] |
| Regiona × linear slope [SE] | 0.00* [0.00] | 0.00 [0.00] | −0.00* [0.00] |
| Genderb × linear slope [SE] | 0.00 [0.00] | 0.00 [0.00] | −0.00* [0.00] |
| Cohortc × linear slope [SE] | −0.00* [0.00] | −0.00*** [0.00] | 0.00*** [0.00] |
| Education [low is reference] × linear slope | |||
| Medium × linear slope [SE] | −0.00 [0.00] | −0.00 [0.00] | −0.00 [0.00] |
| High × linear slope [SE] | −0.00 [0.00] | −0.00 [0.00] | −0.00 [0.00] |
| Regiona × quadratic slope [SE] | −0.00* [0.00] | 0.00 [0.00] | 0.00** [0.00] |
| Genderb × quadratic slope [SE] | 0.00 [0.00] | 0.00 [0.00] | 0.00 [0.00] |
| Cohortc × quadratic slope [SE] | 0.00** [0.00] | 0.00*** [0.00] | 0.00 [0.00] |
| Education [low is reference] × quadratic slope | |||
| Medium × quadratic slope [SE] | 0.00 [0.00] | −0.00 [0.00] | 0.00 [0.00] |
| High × quadratic slope [SE] | 0.00 [0.00] | −0.00 [0.00] | 0.00 [0.00] |
| Time-varying predictors | |||
| Between-person predictor effects | |||
| Chronic diseases [SE] | 0.04*** [0.00] | 0.01 [0.00] | 0.00 [0.00] |
| Self-rated health [SE] | −0.23*** [0.01] | 0.00 [0.01] | 0.06*** [0.01] |
| Positive affect [SE] | −0.26*** [0.01] | −0.23*** [0.01] | 0.58*** [0.01] |
| Negative affect [SE] | 0.10*** [0.01] | 0.20*** [0.01] | −0.03* [0.01] |
| Loneliness [SE] | −0.02 [0.01] | 0.40*** [0.01] | −0.07*** [0.01] |
| Network size [SE] | −0.01* [0.00] | 0.00 [0.00] | −0.00 [0.00] |
| Within-person predictor effects | |||
| Chronic diseases [SE] | 0.02*** [0.00] | 0.00 [0.00] | −0.01** [0.00] |
| Self-rated health [SE] | −0.13*** [0.01] | −0.01* [0.01] | 0.06*** [0.01] |
| Positive affect [SE] | −0.17*** [0.01] | −0.19*** [0.01] | 0.30*** [0.01] |
| Negative affect [SE] | 0.04*** [0.01] | 0.17*** [0.01] | −0.04*** [0.01] |
| Loneliness [SE] | 0.00 [0.01] | 0.24*** [0.01] | −0.10*** [0.01] |
| Network size [SE] | −0.00 [0.00] | 0.00 [0.00] | 0.00 [0.00] |
| Random variances | |||
| Variance intercept [SE] | 0.08*** [0.00] | 0.06*** [0.00] | 0.06*** [0.00] |
| Variance slope [SE] | 0.00*** [0.00] | 0.00*** [0.00] | 0.00*** [0.00] |
| Covariance intercept—slope [SE] | −0.00*** [0.00] | −0.00 [0.00] | 0.00*** [0.00] |
| Residual variance [SE] | 0.13*** [0.00] | 0.12*** [0.00] | 0.12*** [0.00] |
| BIC | 18,966.92 | 17,229.81 | 17,121.22 |
| R2 | .12 | .21 | .21 |
Note. Time unit is age [in years], grand-mean-centered [0 corresponds to 63.78 years].
Between-person predictor effects: Each individual’s mean score across all available measurement occasions. Within-person predictor effects: Measurement-occasion-specific deviations of each individual’s score from their overall mean score (see Hoffman & Stawski, 2009). R2: relative reduction in residual variance compared to the residual variance of the unconditional model (Xu, 2003).
0 = Western Germany, 1 = Eastern Germany.
0 = man, 1 = woman.
First study participation in: 0 = 1996, 1 = 2002, 2 = 2008.
p < .05.
p < .01.
p < .001.
Predictors of Self-Perceptions of Aging
The results of the longitudinal models that included the predictors are presented in Table 4. The effects of the time-invariant, context-specific predictors are reported first, followed by the findings for the time-varying, person-specific predictors, separately for the between-person and within-person effects.
Time-Invariant, Context-Specific Predictors
In terms of intercept effects of the context-specific predictors, individuals from East Germany scored higher on perceptions of physical and social losses, and lower on perceptions of ongoing development than individuals from West Germany. However, these East–West differences were small, ranging from 0.04 (social losses) to 0.10 (ongoing development) on the SPA scales ranging from 1 to 4. Regarding education, individuals with high education had a 0.08 points higher score on perceptions of physical losses than individuals with low education.
In terms of predictors of the linear age-related change component in SPA, individuals from East Germany revealed a steeper linear age-related increase in perceptions of physical losses as well as a steeper linear age-related decrease in perceptions of ongoing development compared to individuals from West Germany. Educational level was not significantly associated with linear change in any of the AgeCog dimensions.
The quadratic age-related change components in perceptions of physical losses and ongoing development, indicating an accelerated late-life increase in the former dimension and an accelerated late-life decline in the latter, were attenuated in East Germans compared to West Germans. Given that the differences between East and West Germans in linear change were in the opposite direction, this pattern indicates that West Germans scored lower on perceptions of physical losses and higher on perceptions of ongoing development in early old age, but this difference got increasingly smaller with advancing age. Educational level was not significantly associated with quadratic change in any of the AgeCog scales (see Table 4).
Time-Varying, Person-Specific Predictors: Between-Person Effects
Regarding the between-person effects of the time-varying, person-specific predictors, individuals with a greater number of chronic diseases (computed as person-specific mean score across all measurement occasions) scored higher on physical losses. Each additional chronic disease was associated with a higher score on perceptions of physical losses by 0.04 points (on the scale ranging from 1 to 4). Also, individuals with overall poorer self-rated health scored higher on perceptions of physical losses and lower on perceptions of ongoing development. As expected, the effect of self-rated health was stronger on perceptions of physical losses than on perceptions of ongoing development, with each point lower on self-rated health being associated with a higher score on physical losses by about ¼ point. The corresponding regression coefficient was more than three times larger for perceptions of physical losses (β = −.23, p < .001) than for perceptions of ongoing development (β = .06, p < .001).
The between-person components of positive and negative affect were significantly associated with the intercepts of all three AgeCog dimensions. Specifically, higher positive affect and lower negative affect were associated with lower scores on perceptions of physical and social losses, and higher scores on perceptions of ongoing development. In line with our assumptions, positive affect showed the strongest association with perceptions of ongoing development, and weaker associations with both other SPA domains. Each additional point on the positive affect scale was associated with a higher score on perceptions of ongoing development by more than half a point (β = .58, p < .001). In contrast, the coefficient of positive affect was only about half the size for the other two SPA dimensions (physical losses: β = −.26, p < .001; social losses: β = −.23, p < .001). Negative affect showed the strongest association with perceptions of social losses.
Higher overall loneliness scores were significantly associated with lower scores on perceptions of ongoing development and with higher scores on perceptions of social losses. As expected, loneliness showed the strongest association with perceptions of social losses. The coefficient of loneliness was more than five times greater for social losses (β = .40, p < .001) than for ongoing development (β = −.07, p < .001) and indicated that each additional point on the loneliness scale was associated with a higher score on self-perceptions of social losses by 0.4 points. Finally, an overall larger network size was associated with lower perceptions of physical losses (β = −.01, p < .05).
Time-Varying, Person-Specific Predictors: Within-Person Effects
The within-person effects of the person-specific predictors describe the extent to which intraindividual, occasion-specific deviations from an individual’s personal mean for a given predictor variable were associated with the respective dimension of the AgeCog scales. As can be seen in Table 4, the within-person component of number of chronic diseases was positively associated with perceptions of physical losses and negatively associated with perceptions of ongoing development. This means that on measurement occasions when individuals reported more chronic diseases than their individual average, they also scored higher on perceptions of physical losses and lower on perceptions of ongoing development. When individuals reported better self-rated health than their personal average, then they scored lower on perceptions of physical and social losses and higher on perceptions of ongoing development. Consistent with the corresponding between-person effect of self-rated health and as shown in Figure 4, the within-person component of self-rated health was more strongly related with perceptions of physical losses (β = −.13, p < .001) than with perceptions of social losses (β = −.01, p < .05) and ongoing development (β = .06, p < .001).
Figure 4. Within-Person Effects of Self-Rated Health on Self-Perceptions of Aging.

Note. Analyses controlled for all other predictors by using the residualized SPA scores (i.e., residuals from multilevel models with all predictors except the within-person component of self-rated health were saved and then used as outcome in the figure). The figure illustrates that on measurement occasions when individuals scored higher on self-rated health (i.e., above their overall mean), they reported fewer negative perceptions related to physical and social losses, and more positive perceptions related to ongoing development. All within-person effects were significant, with the strongest effect for perceptions of physical losses.
The within-person components of positive and negative affect were also significantly associated with all three AgeCog dimensions. Specifically, on occasions when participants’ positive affect was higher and when their negative affect was lower than their personal mean, they scored lower on perceptions of physical and social losses and higher on perceptions of ongoing development. Similar to the pattern for the between-person effects, the within-person component of positive affect was more strongly associated with perceptions of ongoing development (β = .30, p < .001), compared to its association with perceptions of physical (β = −.17, p < .001) and social losses (β = −.19, p < .001; see Figure 5). Negative affect showed the strongest association with perceptions of social losses (β = .17, p < .001) and weaker associations with perceptions of physical losses (β = .04, p < .001) and ongoing development (β = −.04, p < .001).
Figure 5. Within-Person Effects of Positive Affect on Self-Perceptions of Aging.

Note. Analyses controlled for all other predictors by using the residualized SPA scores (i.e., residuals from multilevel models with all predictors except the within-person component of positive affect were saved and then used as outcome in the figure). The figure illustrates that on occasions when individuals reported higher positive affect (i.e., above their overall mean), they scored lower on perceptions of physical and social losses, and higher on perceptions of ongoing development. All within-person effects were significant, with the strongest effect for perceptions of ongoing development.
Finally, on occasions when individuals reported greater loneliness than their personal average, they scored lower on perceptions of ongoing development and higher on perceptions of social losses. As shown in Figure 6, this within-person effect of loneliness was strongest for perceptions of social losses (β = .24, p < .001), and weaker for perceptions of ongoing development (β = −.10, p < .001). There was no significant within-person effect of loneliness on perceptions of physical losses (β = .00, p > .05). The within-person component of social network size was not significantly associated with any of the AgeCog dimensions.
Figure 6. Within-Person Effects of Loneliness on Self-Perceptions of Aging.

Note. Analyses controlled for all other predictors by using the residualized SPA scores (i.e., residuals from multilevel models with all predictors except the within-person component of loneliness were saved and then used as outcome in the figure). The figure illustrates that on occasions when individuals reported greater loneliness (i.e., above their overall mean), they scored higher on perceptions of social losses and lower on perceptions of ongoing development, with the strongest effect on perceptions of social losses. The within-person effect of loneliness on perceptions of physical losses was not significant.
In terms of the random variances, all random intercept and random slope effects were significant (see Table 4). These significant effects indicated that there was considerable interindividual variability in both the individual levels of participants’ SPA and their age-related intraindividual changes, even after the time-invariant and time-varying predictors were included.
Additional Analyses
Two sets of secondary analyses were performed to explore additional questions. First, because there might be associations of the between-person components of the included time-varying predictors (i.e., corresponding to individuals’ mean scores across all available occasions on these predictors), with the linear and quadratic slopes of the three SPA domains, we computed models that included these effects in addition to all predictors listed in Table 4. Several effects reached significance, and effects were again highly specific for each SPA domain. The detailed findings from these analyses are presented in the online Supplemental Materials.
Second, because the effects of the within-person predictors may vary in size among individuals, we tested models that specified all within-person predictor effects as random effects. All other predictor effects were specified as in the original models shown in Table 4. Except for size of social network, there was indeed evidence for substantial interindividual variation in the effects of the within-person predictors on participants’ domain-specific SPA. The findings from these analyses are also presented in the Supplemental Materials.
Discussion
This study had two objectives. First, using a nationally representative sample of adults from the DEAS who were followed for up to 21 years, we examined the age-related change trajectories in SPA related to physical losses, social losses, and ongoing development (Wurm et al., 2007). We examined these change trajectories in terms of the timing, shape and rate of change, testing the developmental principles of multidimensionality and multidirectionality (Baltes, 1987; Kornadt, Kessler, et al., 2019). Second, because it is of critical importance to understand the developmental correlates and predictors of any observed age-related changes, we examined the effects of time-invariant, context-specific and time-varying, person-specific predictors on the age-related trajectories.
Age-Related Changes in Self-Perceptions of Aging
Consistent with our predictions, findings from longitudinal multilevel regression analyses showed that nonlinear change models provided a better fit to the observed data than linear models. Figures 1-3 show that mean levels in SPA related to physical losses, social losses, and ongoing development changed with age in a nonlinear fashion. Specifically, from age 40 to about age 65, participants’ perceptions of physical and social losses were, on average, mostly stable. However, starting at about age 65, participants showed age-related increases in perceptions of physical and social losses, with these increases getting steeper in old age (see Figures 1 and 2). Similarly, starting at about age 55, participants reported increasingly less positive SPA related to ongoing development. The decline in perceptions of ongoing development became increasingly steeper after age 70 (see Figure 3). Moreover, as indicated by the significant random variances for the slope effects of all three SPA dimensions, there was considerable interindividual variation around these mean-level change trajectories.
This is the first study describing age-related change in multiple dimensions of adults’ SPA over an extended time period (i.e., for up to 21 years). Previous studies only examined change trajectories for unidimensional measures (Miche, Elsässer, et al., 2014), over shorter periods of time (Kleinspehn-Ammerlahn et al., 2008), or in a non-age-related way (Jung et al., 2019). Given these limitations of previous studies and given that the DEAS is based on a nationally representative sample, the present study is the first one to describe the normative age-related change in SPA in three important domains. Moreover, although the findings indicate that adults’ SPA related to all three dimensions became overall more negative with age, the timing, shape, and rates of change support the lifespan developmental notion of multidirectionality (Baltes, 1987) as originally suspected by Steverink et al. (2001).
In terms of the timing of the age-related change, it was interesting to see that for perceived physical and social losses, there was mostly stability from age 40 to about age 65. At about age 65, perceptions of physical and social losses started to become more frequent and the rate of change accelerated after age 80 for both dimensions. This resulted in the nonlinear shape of the age-related trajectory. These findings may be interpreted in several ways. From a life course perspective (Barrett & Montepare, 2015; Macmillan, 2005), it seems plausible that this pattern of changes in SPA reflects existing age norms in the German society. According to these norms, the age of 65 is viewed as the official entry point into old age and several normative events (e.g., mandatory retirement; eligibility for pension benefits), are tied to this age and may influence adults’ SPA accordingly. Additionally, this finding may reflect one of the key propositions of Stereotype Embodiment Theory (Levy, 2009). That is, starting in the early and mid-sixties, the negative age stereotypes that individuals internalized earlier in their lives may become increasingly self-relevant and may influence their SPA in negative ways. Finally, around the age of 65, individuals commonly make the decision to retire and it has been documented that the transition into retirement is associated with declines in physical health and social interactions (Dhaval et al., 2008). The increase in the rate of change of self-perceived physical and social losses after the age of 80 may reflect the fact that in very old age vulnerabilities in health (Baltes & Smith, 2003) and the loss of important social roles and partners become increasingly normative events (Rook & Charles, 2017; Shaw et al., 2007).
Compared to perceptions of physical and social losses, adults’ SPA in terms of ongoing development started to decline already at age 55 and the rate of decline accelerated after the age of 75. This finding very likely reflects that in late midlife, individuals often engage in a process of midlife review (Stewart & Vandewater, 1999). This subjective process of stock-taking may increase individuals’ awareness that certain goals (e.g., professional goals) may not be achievable anymore or certain opportunities may not exist any longer (e.g., opportunity for job promotion). Overall, this may trigger the decline in perceptions of ongoing development and increase the awareness that certain developmental deadlines may have passed (Heckhausen et al., 2001). Furthermore, these subjective processes may be reinforced by “feedback” from the social environment (e.g., treatment as older employee in the workplace), experiences with age-based discrimination (Han & Richardson, 2015), or by the negative age stereotypes others may be expressing (Levy, 2009). The accelerated downturn of perceptions of ongoing development after the age of 75, on the other hand, very likely reflects the cumulative effects of (a) declining cognitive functions (Salthouse, 2019), (b) declining health and mobility (Baltes & Smith, 2003), and (c) growing constraints in terms of resources (Jopp & Smith, 2006). In very old age, these factors may combine in ways so that they may undo the well-documented positivity effect (Scheibe & Carstensen, 2010) and further question the observed paradox of well-being (Kunzmann et al., 2000; see also Diehl et al., 2014).
In summary, the findings related to the study’s first objective showed that adults’ SPA regarding physical losses, social losses, and ongoing development became more negative with age and this trend accelerated in later adulthood. Overall, these findings suggest that it may become psychologically more difficult to maintain positive SPA in very old age. Given the findings from studies showing that positive SPA have beneficial effects on adults’ psychological well-being and social relationships (Brothers et al., 2016; Menkin et al., 2017; Schwartz et al., 2020), future research should focus on the context- and person-specific conditions that minimize the development of negative SPA and maximize the maintenance of positive SPA.
The Role of Time-Invariant, Context-Specific Predictors
Findings related to the time-invariant, context-specific predictors of the age-related trajectories were mostly in support of the predicted effects. In terms of the intercepts of adults’ SPA, the effects were significant for region of residence and level of education. Regarding regional differences, East German adults scored higher on perceptions of physical and social losses and lower on perceptions of ongoing development than West German adults, which is in line with previous findings (Wurm & Huxhold, 2012). This suggests that East German participants had overall more negative SPA than their West German counterparts. In terms of the effect of education, individuals with a higher education scored higher on perceptions of physical losses than individuals with lower education. Although it might be possible that individuals with higher education could be more aware of physical losses for several reasons (e.g., higher health literacy), this counterintuitive finding should be interpreted with caution as it may reflect a potential bias in the sample due to some health-related selectivity, which is always present in longitudinal studies (Lindenberger et al., 2002). In addition, this finding may indicate that level of education may be less predictive than indicators of subjective social status (English et al., 2019).
Region of residence was also a significant predictor of linear and nonlinear age-related change in SPA. Specifically, East German adults showed steeper linear age-related increases in perceptions of physical losses and steeper linear age-related decreases in perceptions of ongoing development compared to their West German counterparts. In contrast, the quadratic change components in these two AgeCog dimensions were smaller in East Germans than in West Germans, suggesting that the effect of region of residence became less pronounced in old and very old age. These findings are consistent with results from studies showing that individuals’ SPA are associated with socio-political and societal variables (Löckenhoff et al., 2009), including wealth (e.g., gross-domestic product), primary care supply (Wurm et al., 2014), social aging policies, and indicators of regional population aging (North & Fiske, 2015; Wolff et al., 2018). Furthermore, the prevalence of societal age discrimination (Beyer et al., 2017; Han & Richardson, 2015) or the percentage of older adults engaged in paid and volunteer work have been shown to be associated with societal and individual views of aging (Bowen & Skirbekk, 2013). Taken together, these findings suggest that adults’ SPA are not only based on personal experiences but are also influenced by societal, macrolevel variables that may be subject to historical change (Diehl et al., 2021; Gerstorf et al., 2020).
The Role of Time-Varying, Person-Specific Predictors
Findings regarding the effects of the time-varying, person-specific predictors on the age-related change trajectories were mostly as predicted, both for effects at the between-person and the within-person level. At the between-person level, the effects of the health-related predictors (i.e., chronic disease burden and self-rated health) were significant for the dimensions of physical losses and ongoing development, with overall greater chronic disease burden and poorer self-rated health being associated with higher perceptions of physical losses and better self-rated health being also associated with lower perceptions of ongoing development. At the within-person level, the same pattern of associations was found, indicating that on measurement occasions when participants reported a greater than average number of chronic diseases and poorer than average self-rated health, they also showed higher perceptions of physical losses and lower perceptions of ongoing development (see Figure 4).
Both at the between- and the within-person level, greater positive affect was associated with lower perceptions of physical and social losses and higher perceptions of ongoing development (see Figure 5). Conversely, at both levels, greater negative affect was associated with higher perceptions of physical and social losses and lower perceptions of ongoing development. Loneliness showed the same pattern of associations with the dimensions of social losses and ongoing development. That is, greater between- and within-person loneliness was associated with higher perceptions of social losses and lower perceptions of ongoing development (see Figure 6). Social network size was a significant between-person predictor of perceptions of physical losses, with a larger social network being associated with lower perceptions of physical losses.
Interestingly, at both the between- and within-person level, positive affect showed the strongest association with perceptions of ongoing development, whereas negative affect and loneliness had their strongest association with perceptions of social losses. As expected, chronic disease burden and self-rated health had their strongest associations with perceptions of physical losses. These findings, showing the strongest associations of the time-varying predictors in a domain-specific way (e.g., health-related predictors having the strongest association with perceptions of physical losses), are consistent with the stereotype-matching effect (Levy & Leifheit-Limson, 2009). This effect describes the observation that age stereotypes have a greater impact on outcomes when they match the corresponding behavioral domain. For example, age stereotypes about adults’ cognitive functioning have a stronger effect on their cognitive performance than their physical performance and vice versa. The domain-specificity effect was also supported by the additional analyses showing that most of the between-person components of predictors were significantly associated with linear slopes in a domain-specific way (e.g., loneliness with change in perceptions of social losses).
Because recent studies have focused on middle-aged and older adults’ SPA as potential intervention targets (Beyer, Wiest, et al., 2019; Beyer, Wolff,et al., 2019; Brothers & Diehl, 2017; Wolff et al., 2014), these findings may also have important practical implications. Specifically, these findings point to physical health, affective states (e.g., positive and negative affect) and indicators of social integration (e.g., loneliness and social involvement) as potential underlying mechanisms that may over time “feed into” and shape specific SPA. For this reason, these predictors should be considered as potential intervention targets. Although most researchers focus on indicators of physical and mental health and the presence or absence of material resources as critical antecedents of adults’ SPA (Jopp & Smith, 2006; Jung et al., 2019; Wurm et al., 2019), these findings suggest that closer attention should be paid to affective processes and social relationships as developmental correlates and antecedents of adults’ SPA (Schwartz et al., 2020). Moreover, greater attention should be paid to adults’ SPA in very late life when increased physical and cognitive vulnerabilities tax individuals’ psychological resources in predictable ways (Baltes, 1997; Baltes & Smith, 2003).
Finally, additional analyses also yielded several noteworthy findings. For example, these analyses confirmed significant within-person random effects for most of the time-varying, person specific predictors, indicating that the effects of the within-person predictors varied significantly across individuals. Taken together, the findings from the additional analyses indicated that the examination of predictors of change in adults’ SPA needs to be an integral part of research on adults’ SPA (Diehl et al., 2021; Kornadt, Kessler, et al., 2019; Levy, 2009).
Limitations
Despite several notable strengths of the present study, there are also several noteworthy limitations. First, it is important to note that the included measures of physical health were both based on self-report. Objective measures of physical health, such as the results of a physical exam, would be desirable to complement these self-report measures.
Second, another limitation was that we were not able to include a measure of depressive symptoms as an indicator of mental health in our analyses. Although the DEAS administered a depression scale in 2002, this measure was not available in the 1996 wave, and we decided in favor of a larger sample and a longer observation period.
Third, we were also not able to examine the role of personality traits (e.g., neuroticism, extraversion, or agreeableness) as predictors of participants’ SPA because the DEAS did not include a personality inventory. However, personality traits are documented correlates and predictors of attitudes toward aging (Bryant et al., 2016; Kornadt, Siebert, et al., 2019; Miche, Elsässer, et al., 2014; Rupprecht et al., 2019). In the context of the present study, positive and negative affect may be considered approximations for the traits of extraversion and neuroticism as some authors have suggested (McAdams, 2009).
Finally, although the multilevel modeling approach provided flexibility in terms of separation of between- and within-person effects, a limitation is that the presented analyses do not permit causal conclusions as they are correlational in nature and describe time-varying associations between predictors and outcomes. In order to make causal conclusions, lagged or cross-correlational effects would need to be modeled to examine the directionality of effects over time (see Sargent-Cox et al., 2012b; Wurm et al., 2007). Moreover, the question when person-specific characteristics are treated as predictors or outcomes of individuals’ SPA, is the topic of an ongoing debate on the directionality/causality of effects (see Schwartz et al., 2020; Wurm et al., 2007). Whether person-specific characteristics are conceptualized as predictor or outcome variables depends first and foremost on the research questions to be addressed. In general, we subscribe to a conceptualization of SPA and person-specific variables as mutually influencing each other over time (i.e., bidirectional associations). Such a conceptualization is consistent with theoretical models (Diehl & Wahl, 2010; Kornadt, Kessler, et al., 2019) and findings from several studies on the bidirectional associations between SPA and outcomes (Schwartz et al., 2020; Wurm et al., 2007).
In summary, the present study extended past work on SPA in adulthood in two major ways. First, we conceptualized adults’ SPA as the outcome variable and examined age-related changes in multiple dimensions of SPA in a nationally representative sample of adults ranging in age from 40 to 85 years over a period of up to 21 years. Second, we examined both context- and person-specific predictors to gain a better understanding of the time-invariant and time-varying correlates of the observed age-related changes in the multiple dimensions of adults’ SPA.
Supplementary Material
Acknowledgments
The German Ageing Survey (DEAS) was funded by Grant 301-1720-2/2 from the German Federal Ministry for Family, Senior Citizens, Women, and Youth. Manfred Diehl’s work on this article was supported in part by a Humboldt Research Award from the Alexander von Humboldt Foundation, Germany, and by a grant from the National Institute on Aging, National Institutes of Health (R01 AG051723). Manfred Diehl would like to thank Clemens Tesch-Römer for the opportunity to spend time during his Humboldt Research Award at the German Centre of Gerontology in Berlin, Germany.
References
- Antonucci TC (2001). Social relations: An examination of social networks, social support, and sense of control. In Birren JE & Schaie KW (Eds.), Handbook of the psychology of aging (5th ed., pp. 427–453). Academic Press. [Google Scholar]
- Baltes PB (1987). Theoretical propositions of life-sapn developmental psychology: On the dynamics between growth and decline. Developmental Psychology, 23, 611–626. 10.1037/0012-1649.23.5.611 [DOI] [Google Scholar]
- Baltes PB (1997). On the incomplete architecture of human ontogeny: Selection, optimization, and compensation as foundation of developmental theory. American Psychologist, 52, 366–380. 10.1037/0003-066X.52.4.366 [DOI] [PubMed] [Google Scholar]
- Baltes PB, & Smith J (2003). New frontiers in the future of aging: From successful aging of the young old to the dilemmas of the fourth age. Gerontology, 49, 123–135. 10.1159/000067946 [DOI] [PubMed] [Google Scholar]
- Barrett AE, & Montepare JM (2015). “It’s about time”: Applying life span and life course perspectives to the study of subjective aging. Annual Review of Gerontology & Geriatrics, 35, 55–77. 10.1891/0198-8794.35.55 [DOI] [Google Scholar]
- Beyer A-K, Wiest M, & Wurm S (2019). There is still time to be active: Self-perceptions of aging, physical activity, and the role of perceived residual lifetime among older adults. Journal of Aging and Physical Activity, 27, 807–815. 10.1123/japa.2018-0380 [DOI] [PubMed] [Google Scholar]
- Beyer A-K, Wolff JK, Freiberger E, & Wurm S (2019). Are self-perceptions of ageing modifiable? Examination of an exercise programme with vs. without self-perceptions of ageing-intervention for older adults. Psychology & Health, 34, 661–676. 10.1080/08870446.2018.1556273 [DOI] [PubMed] [Google Scholar]
- Beyer A-K, Wurm S, & Wolff JK (2017). Älter werden—Gewinn oder Verlust? Individuelle Altersbilder und Altersdiskriminierung. [Aging—Gain or loss? Individual views of aging and age discrimination]. In Mahne K, Wolff JK, Simonson J, & Tesch-Römer C (Eds.), Altern im Wandel: Zwei Jahrzehnte Deutscher Alterssurvey (DEAS) [Aging in a changing world: Two decades of the German Aging Survey]. (pp. 329–343). Springer. 10.1007/978-3-658-12502-8_22 [DOI] [Google Scholar]
- Bowen CE, & Skirbekk V (2013). National stereotypes of older people’s competence are related to older adults’ participation in paid and volunteer work. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 68, 974–983. 10.1093/geronb/gbt101 [DOI] [PubMed] [Google Scholar]
- Brothers A, Gabrian M, Wahl H-W, & Diehl M (2016). Future time perspective and awareness of age-related change: Examining their role in predicting psychological well-being. Psychology and Aging, 31, 605–617. 10.1037/pag0000101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brothers AF, & Diehl M (2017). Feasibility and efficacy of the AgingPLUS program: Changing views on aging to increase engagement in physical activity. Journal of Aging and Physical Activity, 25, 402–411. 10.1123/japa.2016-0039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brothers AF, Gabrian M, Wahl H-W, & Diehl M (2019). A new multidimensional questionnaire to assess awareness of age-related change (AARC). The Gerontologist, 59, e141–e151. 10.1093/geront/gny006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant C, Bei B, Gilson K-M, Komiti A, Jackson H, & Judd F (2016). Antecedents of attitudes to aging: A study of the roles of personality and well-being. The Gerontologist, 56, 256–265. 10.1093/geront/gnu041 [DOI] [PubMed] [Google Scholar]
- Charles ST, & Carstensen LL (2010). Social and emotional aging. Annual Review of Psychology, 61, 383–409. 10.1146/annurev.psych.093008.100448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J (1992). A power primer. Psychological Bulletin, 112, 155–159. 10.1037/0033-2909.112.1.155 [DOI] [PubMed] [Google Scholar]
- Curran PJ, & Bauer DJ (2011). The disaggregation of within-person and between-person effects in longitudinal models of change. Annual Review of Psychology, 62, 583–619. 10.1146/annurev.psych.093008.100356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Jong Gierveld J, & Van Tilburg T (2006). A 6-item scale for overall, emotional, and social loneliness: Confirmatory tests on survey data. Research on Aging, 28, 582–598. 10.1177/0164027506289723 [DOI] [Google Scholar]
- DeSalvo KB, Bloser N, Reynolds K, He J, & Muntner P (2006). Mortality prediction with a single general self-rated health question. A meta-analysis. Journal of General Internal Medicine, 21(3), 267–275. 10.1111/j.1525-1497.2005.00291.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhaval D, Rashad I, & Spasojevic J (2008). The effects of retirement on physical and mental health outcomes. Southern Economic Journal, 75, 497–523. [Google Scholar]
- Diehl M, Brothers AF, & Wahl H-W (2021). Self-perceptions and awareness of aging: Past, present, and future. In Schaie KW & Willis SL (Eds.), Handbook of the Psychology of Aging (9th ed.). Academic Press. 10.1016/B978-0-12-816094-7.00001-5 [DOI] [Google Scholar]
- Diehl M, Chui H, Hay EL, Lumley MA, Grühn D, & Labouvie-Vief G (2014). Change in coping and defense mechanisms across adulthood: Longitudinal findings in a European American sample. Developmental Psychology, 50, 634–648. 10.1037/a0033619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diehl M, Smyer MA, & Mehrotra CM (2020). Optimizing aging: A call for a new narrative. American Psychologist, 75, 577–589. 10.1037/amp0000598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diehl M, & Wahl H-W (2010). Awareness of age-related change: Examination of a (mostly) unexplored concept. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 65B, 340–350. 10.1093/geronb/gbp110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diehl M, Wahl H-W, Brothers A, & Miche M (2015). Subjective aging and awareness of aging: Toward a new understanding of the aging self. Annual Review of Gerontology & Geriatrics, 35, 1–28. 10.1891/0198-8794.35.1 [DOI] [Google Scholar]
- Dutt AJ, & Wahl H-W (2017). Feeling sad makes us feel older: Effects of a sad-mood induction on subjective age. Psychology and Aging, 32, 412–418. 10.1037/pag0000179 [DOI] [PubMed] [Google Scholar]
- English AN, Bellingtier JA, & Neupert SD (2019). It’s “the Joneses”: The influence of objective and subjective socioeconomic status on subjective perceptions of aging. European Journal of Ageing, 16, 121–128. 10.1007/s10433-018-0475-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerstorf D, Hülür G, Drewelies J, Willis SL, Schaie KW, & Ram N (2020). Adult development and aging in historical context. American Psychologist, 75, 525–539. 10.1037/amp0000596 [DOI] [PubMed] [Google Scholar]
- Gerstorf D, & Ram N (2009). Limitations on the importance of self-regulation in old age. Human Development, 52, 38–43. 10.1159/000189214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han J, & Richardson VE (2015). The relationships among perceived discrimination, self-perceptions of aging, and depressive symptoms: A longitudinal examination of age discrimination. Aging & Mental Health, 19, 747–755. 10.1080/13607863.2014.962007 [DOI] [PubMed] [Google Scholar]
- Heckhausen J, Dixon RA, & Baltes PB (1989). Gains and losses in development throughout adulthood as perceived by different adult age groups. Developmental Psychology, 25, 109–121. 10.1037/0012-1649.25.1.109 [DOI] [Google Scholar]
- Heckhausen J, Wrosch C, & Fleeson W (2001). Developmental regulation before and after a developmental deadline: The sample case of “biological clock” for childbearing. Psychology and Aging, 16, 400–413. 10.1037/0882-7974.16.3.400 [DOI] [PubMed] [Google Scholar]
- Hess TM, O’Brien EL, Voss P, Kornadt AE, Rothermund K, Fung HH, & Popham LE (2017). Context influences on the relationship between views of aging and subjective age: The moderating role of culture and domain of functioning. Psychology and Aging, 32, 419–431. 10.1037/pag0000181 [DOI] [PubMed] [Google Scholar]
- Hoffman L, & Stawski RS (2009). Persons as contexts: Evaluating between-person and within-person effects in longitudinal analysis. Research in Human Development, 6, 97–120. 10.1080/15427600902911189 [DOI] [Google Scholar]
- Holt-Lunstad J, Smith TB, Baker M, Harris T, & Stephenson D (2015). Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspectives on Psychological Science, 10, 227–237. 10.1177/1745691614568352 [DOI] [PubMed] [Google Scholar]
- Hox JJ, & Kreft IGG (1994). Multilevel analysis methods. Sociological Methods & Research, 22, 283–299. 10.1177/0049124194022003001 [DOI] [Google Scholar]
- Infurna FJ, Gerstorf D, & Lachman ME (2020). Midlife in the 2020s: Opportunities and challenges. American Psychologist, 75, 470–485. 10.1037/amp0000591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jopp D, & Smith J (2006). Resources and life-management strategies as determinants of successful aging: On the protective effect of selection, optimization, and compensation. Psychology and Aging, 21, 253–265. 10.1037/0882-7974.21.2.253 [DOI] [PubMed] [Google Scholar]
- Jung S, Cham H, Siedlecki KL, & Jopp DS (2019). Measurement invariance and developmental trajectories of multidimensional self-perceptions of aging in middle-aged and older adults. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. Advance online publication. 10.1093/geronb/gbz099 [DOI] [PubMed] [Google Scholar]
- Kass RE, & Raftery AE (1995). Bayes factors. Journal of the American Statistical Association, 90, 773–795. 10.1080/01621459.1995.10476572 [DOI] [Google Scholar]
- Kastenbaum R, Derbin V, Sabatini P, & Artt S (1972). “The ages of me”: Toward personal and interpersonal definitions of functional aging. Aging & Human Development, 3, 197–211. 10.2190/TUJR-WTXK-866Q-8QU7 [DOI] [Google Scholar]
- Kirsch JA, Love GD, Radler BT, & Ryff CD (2019). Scientific imperatives vis-à-vis growing inequality in America. American Psychologist, 74, 764–777. 10.1037/amp0000481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klaus D, Engstler H, Mahne K, Wolff JK, Simonson J, Wurm S, & Tesch-Römer C (2017). Cohort profile: The German Ageing Survey (DEAS). International Journal of Epidemiology, 46, 1105–1105g. 10.1093/ije/dyw326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleinspehn-Ammerlahn A, Kotter-Grühn D, & Smith J (2008). Self-perceptions of aging: Do subjective age and satisfaction with aging change during old age? The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 63, P377–P385. 10.1093/geronb/63.6.P377 [DOI] [PubMed] [Google Scholar]
- Kornadt AE, Kessler E-M, Wurm S, Bowen CE, Gabrian M, & Klusmann V (2019). Views on aging: A lifespan perspective. European Journal of Ageing. Advance online publication. 10.1007/s10433-019-00535-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kornadt AE, & Rothermund K (2011). Contexts of aging: Assessing age stereotypes in different life domains. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 66B, 547–556. 10.1093/geronb/gbr036 [DOI] [PubMed] [Google Scholar]
- Kornadt AE, Siebert JS, & Wahl H-W (2019). The interplay of personality and attitudes toward own aging across two decades of later life. PLoS One, 14(10), Article e0223622. 10.1371/journal.pone.0223622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotter-Grühn D, Kleinspehn-Ammerlahn A, Gerstorf D, & Smith J (2009). Self-perceptions of aging predict mortality and change with approaching death: 16-year longitudinal results from the Berlin Aging Study. Psychology and Aging, 24, 654–667. 10.1037/a0016510 [DOI] [PubMed] [Google Scholar]
- Kunzmann U, Little TD, & Smith J (2000). Is age-related stability of subjective well-being a paradox? Cross-sectional and longitudinal evidence from the Berlin Aging Study. Psychology and Aging, 15, 511–526. 10.1037/0882-7974.15.3.511 [DOI] [PubMed] [Google Scholar]
- Lawton MP (1975). The philadelphia geriatric center morale scale: A revision. Journal of Gerontology, 30, 85–89. 10.1093/geronj/30.1.85 [DOI] [PubMed] [Google Scholar]
- Levy B (2009). Stereotype embodiment: A psychosocial approach to aging. Current Directions in Psychological Science, 18, 332–336. 10.1111/j.1467-8721.2009.01662.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy B, & Myers LM (2004). Preventive health behaviors influenced by self-perceptions of aging. Preventive Medicine, 39, 625–629. 10.1016/j.ypmed.2004.02.029 [DOI] [PubMed] [Google Scholar]
- Levy BR, & Leifheit-Limson E (2009). The stereotype-matching effect: Greater influence on functioning when age stereotypes correspond to outcomes. Psychology and Aging, 24, 230–233. 10.1037/a0014563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy BR, Slade MD, Kunkel SR, & Kasl SV (2002). Longevity increased by positive self-perceptions of aging. Journal of Personality and Social Psychology, 83, 261–270. 10.1037/0022-3514.83.2.261 [DOI] [PubMed] [Google Scholar]
- Lindenberger U, Singer T, & Baltes PB (2002). Longitudinal selectivity in aging populations: Separating mortality-associated versus experimental components in the Berlin Aging Study (BASE). The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 57, P474–P482. 10.1093/geronb/57.6.P474 [DOI] [PubMed] [Google Scholar]
- Löckenhoff CE, De Fruyt F, Terracciano A, McCrae RR, De Bolle M, Costa PT, Aguilar-Vafaie ME, Ahn C-K, Ahn H-N, Alcalay L, Allik J, Avdeyeva TV, Barbaranelli C, Benet-Martinez V, Blatný M, Bratko D, Brunner-Sciarra M, Cain TR, Crawford JT, … Yik M (2009). Perceptions of aging across 26 cultures and their culture-level associates. Psychology and Aging, 24, 941–954. 10.1037/a0016901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macmillan R (2005). The structure of the life course: Classic issues and current controversies. In Macmillan R (Ed.), Advances in life course research: Vol. 9. The structure of the life course: Standardized? Individualized? Differentiated? (pp. 3–24). Elsevier. [Google Scholar]
- McAdams DP (2009). The person: An introduction to the science of personality psychology (5th ed.). Wiley. [Google Scholar]
- Menkin JA, Robles TF, Gruenewald TL, Tanner EK, & Seeman TE (2017). Positive expectations regarding aging linked to more new friends in later life. The Journals of Gerontology, Series B. Psychological Science, 72, 771–781. 10.1093/geronb/gbv118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miche M, Elsässer VC, Schilling OK, & Wahl H-W (2014). Attitude toward own aging in midlife and early old age over a 12-year period: Examination of measurement equivalence and developmental trajectories. Psychology and Aging, 29, 588–600. 10.1037/a0037259 [DOI] [PubMed] [Google Scholar]
- Miche M, Wahl H-W, Diehl M, Oswald F, Kaspar R, & Kolb M (2014). Natural occurrence of subjective aging experiences in community-dwelling older adults. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 69, 174–187. 10.1093/geronb/gbs164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- North MS, & Fiske ST (2015). Modern attitudes toward older adults in the aging world: A cross-cultural meta-analysis. Psychological Bulletin, 141, 993–1021. 10.1037/a0039469 [DOI] [PubMed] [Google Scholar]
- Ram N, & Grimm KJ (2015). Growth curve modeling and longitudinal factor analysis. In Overton WF, Molenaar PCM, & Lerner RM (Eds.), Handbook of child psychology and developmental science: Volume 1. Theory and method (7th ed., pp. 758–788). Wiley. 10.1002/9781118963418.childpsy120 [DOI] [Google Scholar]
- Robertson DA, King-Kallimanis BL, & Kenny RA (2016). Negative perceptions of aging predict longitudinal decline in cognitive functioning. Psychology and Aging, 31, 71–81. 10.1037/pag0000061 [DOI] [PubMed] [Google Scholar]
- Rook KS, & Charles ST (2017). Close social ties and health in later life: Strengths and vulnerabilities. American Psychologist, 72, 567–577. 10.1037/amp0000104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rupprecht FS, Dutt AJ, Wahl H-W, & Diehl MK (2019). The role of personality in becoming aware of age-related changes. GeroPsych, 32, 57–67. 10.1024/1662-9647/a000204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salthouse TA (2019). Trajectories of normal cognitive aging. Psychology and Aging, 34, 17–24. 10.1037/pag0000288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sargent-Cox KA, Anstey KJ, & Luszcz MA (2012a). Change in health and self-perceptions of aging over 16 years: The role of psychological resources. Health Psychology, 31, 423–432. 10.1037/a0027464 [DOI] [PubMed] [Google Scholar]
- Sargent-Cox KA, Anstey KJ, & Luszcz MA (2012b). The relationship between change in self-perceptions of aging and physical functioning in older adults. Psychology and Aging, 27, 750–760. 10.1037/a0027578 [DOI] [PubMed] [Google Scholar]
- Sargent-Cox KA, Anstey KJ, & Luszcz MA (2014). Longitudinal change of self-perceptions of aging and mortality. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 69, 168–173. 10.1093/geronb/gbt005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaie KW (2013). Developmental influences on adult intelligence: The Seattle Longitudinal Study (2nd ed.). Oxford University Press. [Google Scholar]
- Scheibe S, & Carstensen LL (2010). Emotional aging: Recent findings and future trends. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 65B, 135–144. 10.1093/geronb/gbp132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz E, Ayalon L, & Huxhold O (2020, January 17). Exploring the reciprocal associations of perceptions of aging and social involvement. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. Advance online publication. 10.1093/geronb/gbaa008 [DOI] [PubMed] [Google Scholar]
- Shaw BA, Krause N, Liang J, & Bennett J (2007). Tracking changes in social relations throughout late life. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 62, S90–S99. 10.1093/geronb/62.2.S90 [DOI] [PubMed] [Google Scholar]
- Siebert JS, Wahl H-W, & Schröder J (2018). The role of attitude toward own aging for fluid and crystallized functioning: 12-year evidence from the ILSE study. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 73, 836–845. 10.1093/geronb/gbw050 [DOI] [PubMed] [Google Scholar]
- Spuling SM, Klusmann V, Bowen CE, Kornadt AE, & Kessler E-M (2019). The uniqueness of subjective aging: Convergent and discriminant validity. European Journal of Ageing. Advance online publication. 10.1007/s10433-019-00529-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spuling SM, Miche M, Wurm S, & Wahl H-W (2013). Exploring the causal interplay of subjective age and health dimensions in the second half of life: A cross-lagged panel analysis. Zeitschrift für Gesundheitspsychologie, 21, 5–15. 10.1026/0943-8149/a000084 [DOI] [Google Scholar]
- StataCorp. (2017). Stata Statistical Software: Release 15. [Google Scholar]
- Stephan Y, Caudroit J, Jaconelli A, & Terracciano A (2014). Subjective age and cognitive functioning: A 10-year prospective study. The American Journal of Geriatric Psychiatry, 22, 1180–1187. 10.1016/j.jagp.2013.03.007 [DOI] [PubMed] [Google Scholar]
- Steverink N, Westerhof GJ, Bode C, & Dittmann-Kohli F (2001). The personal experience of aging, individual resources, and subjective well-being. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 56, P364–P373. 10.1093/geronb/56.6.P364 [DOI] [PubMed] [Google Scholar]
- Stewart AJ, & Vandewater EA (1999). “If I had it to do over again…”: Midlife review, midcourse corrections, and women’s well-being in midlife. Journal of Personality and Social Psychology, 76, 270–283. 10.1037/0022-3514.76.2.270 [DOI] [PubMed] [Google Scholar]
- Tovel H, Carmel S, & Raveis VH (2019). Relationships among self-perception of aging, physical functioning, and self-efficacy in late life. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 74, 212–221. 10.1093/geronb/gbx056 [DOI] [PubMed] [Google Scholar]
- UNESCO. (2012). International standard classification of education ISCED 2011. UNESCO Institute for Statistics. [Google Scholar]
- Uotinen V, Rantanen T, & Suutama T (2005). Perceived age as a predictor of old age mortality: A 13-year prospective study. Age and Ageing, 34, 368–372. 10.1093/ageing/afi091 [DOI] [PubMed] [Google Scholar]
- Wang L, & Maxwell S (2015). On disaggregating between-person and within-person effects with longitudinal data using multilevel models. Psychological Methods, 20, 63–83. 10.1037/met0000030 [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54, 1063–1070. 10.1037/0022-3514.54.6.1063 [DOI] [PubMed] [Google Scholar]
- Westerhof GJ, & Barrett AE (2005). Age identity and subjective well-being: A comparison of the United States and Germany. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 60, S129–S136. 10.1093/geronb/60.3.S129 [DOI] [PubMed] [Google Scholar]
- Westerhof GJ, Miche M, Brothers AF, Barrett AE, Diehl M, Montepare JM, Wahl H-W, & Wurm S (2014). The influence of subjective aging on health and longevity: A meta-analysis of longitudinal data. Psychology and Aging, 29, 793–802. 10.1037/a0038016 [DOI] [PubMed] [Google Scholar]
- Wolff JK, Beyer A-K, Wurm S, Nowossadeck S, & Wiest M (2018). Regional impact of population aging on changes in individual self-perceptions of aging: Findings from the German Ageing Survey. The Gerontologist, 58, 47–56. 10.1093/geront/gnx127 [DOI] [PubMed] [Google Scholar]
- Wolff JK, Warner LM, Ziegelmann JP, & Wurm S (2014). What do targeting positive views on ageing add to a physical activity intervention in older adults? Results from a randomised controlled trial. Psychology & Health, 29, 915–932. 10.1080/08870446.2014.896464 [DOI] [PubMed] [Google Scholar]
- Wolff JL, Starfield B, & Anderson G (2002). Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Archives of Internal Medicine, 162, 2269–2276. 10.1001/archinte.162.20.2269 [DOI] [PubMed] [Google Scholar]
- Wurm S, Diehl M, Kornadt AE, Westerhof GJ, & Wahl H-W (2017). How do views on aging affect health outcomes in adulthood and late life? Explanations for an established connection. Developmental Review, 46, 27–43. 10.1016/j.dr.2017.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wurm S, & Huxhold O (2012). Sozialer Wandel und individuelle Entwicklung von Altersbildern [Social change and individual development of images of aging]. In Berner F, Rossow J, & Schwitzer K-P (Eds.), Individuelle und kulturelle Altersbilder. Expertisen zum Sechsten Altenbericht der Bundesregierung [Individual and cultural images of aging: Expert opinion for the sixth aging report of the federal government]. (Vol. 1, pp. 27–69). VS Verlag für Sozialwissenschaften. 10.1007/978-3-531-93286-6_2 [DOI] [Google Scholar]
- Wurm S, Tesch-Römer C, & Tomasik MJ (2007). Longitudinal findings on aging-related cognitions, control beliefs, and health in later life. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 62, P156–P164. 10.1093/geronb/62.3.P156 [DOI] [PubMed] [Google Scholar]
- Wurm S, Tomasik MJ, & Tesch-Römer C (2008). Serious health events and their impact on changes in subjective health and life satisfaction: The role of age and a positive view on ageing. European Journal of Ageing, 5, 117–127. 10.1007/s10433-008-0077-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wurm S, Warner LM, Ziegelmann JP, Wolff JK, & Schüz B (2013). How do negative self-perceptions of aging become a self-fulfilling prophecy? Psychology and Aging, 28, 1088–1097. 10.1037/a0032845 [DOI] [PubMed] [Google Scholar]
- Wurm S, Wiest M, Wolff JK, Beyer A-K, & Spuling SM (2019). Changes in views on aging in later adulthood: The role of cardiovascular events. European Journal of Ageing. Advance online publication. 10.1007/s10433-019-00547-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wurm S, Wolff JK, & Schüz B (2014). Primary care supply moderates the impact of diseases on self-perceptions of aging. Psychology and Aging, 29, 351–358. 10.1037/a0036248 [DOI] [PubMed] [Google Scholar]
- Xu R (2003). Measuring explained variation in linear mixed effects models. Statistics in Medicine, 22, 3527–3541. 10.1002/sim.1572 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


