Abstract
Background
Patients undergoing open-heart surgery frequently require one or more blood transfusions. Because of the risks of receiving blood from volunteer donors, some patients choose to donate their own blood before surgery. This reduces their risk of exposure to volunteer-donated blood, but it increases their chance of receiving any transfusion, either of self-donated or volunteer-donated blood. Also, preoperative hemoglobin levels tend to be lower in patients who donate their own blood, and surgeons may be more likely to give transfusions to patients with self-donated blood. To help patients decide whether to donate their blood before surgery, we designed a decision aid comprising a booklet and audiotape and assessed its effectiveness.
Methods
The 59 study subjects were a sample of consecutive patients referred to the Ottawa Heart Institute between Oct. 1, 1998, and Jan. 5, 1999, for future coronary artery bypass grafting, valve surgery or combined surgery. All were eligible to donate blood. Initial questionnaires were administered in the clinic by a physician or study nurse, and follow-up questionnaires were completed at home and mailed in after use of the decision aid. Outcome measures included patients' knowledge, values (importance ratings), preferences for transfusion methods, decisional conflict (the amount of uncertainty about the course of action to take), risk perception and acceptability of the decision aid.
Results
Mean knowledge scores on a 15-item test increased from 67% correct responses before the decision aid to 85% correct responses after use of the aid (p < 0.001); the effect was similar when the patients were divided into subgroups according to education level. The number of patients favouring donating their own blood increased from 41 (69%) before to 45 (76%) after use of the aid. Nine (64%) of 14 initially uncertain patients preferred autologous donation after use of the aid. The overall mean score for decisional conflict was unchanged, at 1.7, which indicated a low level of uncertainty. Risk perception improved, from 0%–14% correct responses on an 8-item test before the aid to 18%–60% correct responses after use of the aid. The decision aid was acceptable to the majority of patients, and 95% indicated that they would recommend it to others.
Interpretation
The decision aid improved knowledge and risk perceptions of blood donation and transfusion, and it helped uncertain patients to make choices.
In an effort to reduce their chance of receiving transfusions of blood from volunteer donors, patients facing open-heart surgery may choose to donate their own blood before surgery. Patients who choose to do so are less likely to receive volunteer-donated blood during surgery1 and therefore are at reduced risk of transfusion-transmitted viral infections such as HIV infection, hepatitis B and hepatitis C. In addition, because of their involvement in the process of donating their own blood, these patients may gain a sense of control over their care. However, they are at increased risk of receiving any transfusion (self-donated or volunteer-donated blood) during surgery.1 This increases their risk of acute hemolytic reaction due to human error and of infection due to bacterial contamination of blood during collection or storage. In addition, self-donation can be inconvenient for patients, requiring one or more trips to a blood clinic. Rarely, patients may experience symptoms such as chest pain or syncope while donating blood. Self-donation is not cost-effective according to conventional criteria because of the very low risk of viral transmission from volunteer-donated blood, the higher cost associated with self-donation and the considerable number of self-donated units that are not used.2,3
Decision aids are designed to help patients make informed choices by providing information on the options and relevant outcomes. The Ottawa Decision Support Framework identified some aspects of the decision-making process that may be improved by decision aids.4 These include perceptions of the decision (knowledge, expectations, values and decisional conflict [the amount of uncertainty about the course of action to take]), the perceptions of important others such as family members or the physician, and the resources needed to make and implement a decision. In this study we developed and evaluated a decision aid for patients considering the donation of their own blood before open-heart surgery. The formats of decision aids range from simple printed materials to complex devices such as interactive videodiscs.5 Our decision aid comprised a booklet and audiotape because this format is inexpensive, convenient, self-administered and easy to use.
Methods
The study was approved by the University of Ottawa Heart Institute Human Research Ethics Committee.
Subjects were recruited from a consecutive series of patients referred by their cardiologists to the 6 surgeons at the Ottawa Heart Institute for a preoperative consultation before elective coronary artery bypass grafting, valve surgery or combined surgery between Oct. 1, 1998, and Jan. 5, 1999. All patients were over 18 years of age, were able to speak and read English, and were eligible to donate their own blood. The decision for eligibility to donate blood was made by the patient's surgeon, according to predefined criteria. For example, patients with severe aortic stenosis, frequent angina on ordinary activity, anemia and heart failure were excluded from blood donation and were not entered in the study.
After the patients gave informed consent for study participation, the baseline questionnaire was administered in the clinic by one of us (F.C.G.) or by the study nurse. Eleven patients were interviewed before seeing the surgeon, and 48 were interviewed immediately afterward. The patients were given the decision aid and follow-up questionnaire to take home. After using the decision aid, each patient completed the follow-up questionnaire and mailed it to us. Those who delayed sending in the questionnaire were reminded by telephone.
A sample size of 60 patients was estimated using the method of Cohen for paired comparisons6 using an effect size for the decisional conflict scale of 0.4, a test–retest correlation coefficient as low as 0.4, an α value of 0.05 and a β value of 0.20. Recruitment was increased to 70 patients because of emergency admissions (7 patients), return of an incomplete questionnaire (2 patients), erroneous recruitment of 1 clinically unstable patient and loss of 1 patient to follow-up. Overall, 59 (95%) of 62 clinically stable patients returned completed questionnaires.
Decision aid
The decision aid comprised a 16-page booklet and a 22-minute audiotape. The topics covered included the role of blood in the body and the consequences of blood loss. It defined blood transfusion and clarified its role in heart surgery. It described the probabilities of receiving a blood transfusion and of complications associated with transfusions of volunteer-donated blood and self-donated blood. We estimated the probabilities of any perioperative transfusion by reviewing Ottawa Heart Institute records for February to November 1996: 35% for those who chose to receive volunteer-donated blood and 58% for those who opted to donate their own blood (50% received only self-donated blood and 8% received additional volunteer-donated blood). The probabilities of complications were estimated from the medical literature7,8 and were expressed as the number of patients out of a million expected to have the complication, as well as the number out of a million who were expected not to have the complication. The clinical consequences of each complication (e.g., hepatitis) were briefly described. A summary chart compared the risks and benefits of each transfusion method. Patients were instructed to read the booklet while listening to the audiotape. A sample page from the booklet, with the corresponding script from the audiotape, is included in Fig. 1.
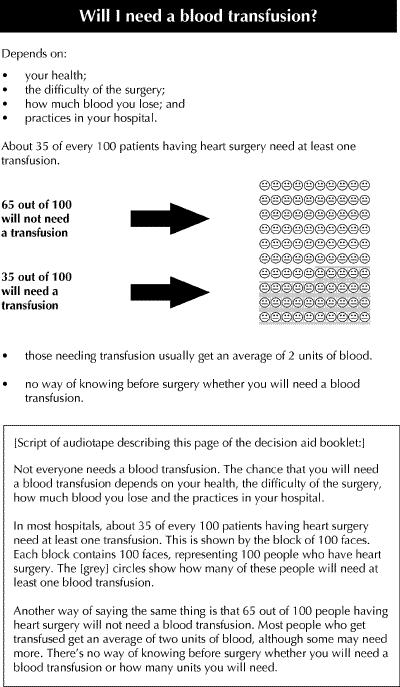
Fig. 1: Sample page from decision aid booklet, and script from accompanying audiotape, for patients considering donation of their own blood before open-heart surgery.
Measures
Knowledge: A 15-item portion of the questionnaire tested patients' knowledge of information covered in the decision aid. Potential answers were “true,” “false” and “unsure.” One point was given for each correct response and zero for unsure or incorrect responses; answers were expressed as percent correct. This format has been used successfully in other decision aid trials of hormone replacement therapy4,9 and antithrombotic therapy.10
Values (importance ratings): Patients rated the personal importance of 3 potential complications (AIDS, hepatitis B and C, and unknown infections), reducing the number of transfusions received (including self-donated blood) and the inconvenience of making extra trips to donate blood. Ratings were expressed on an 11-point scale (0 = not at all important and 10 = extremely important). For analysis, values were grouped as follows: unimportant (0–2), intermediate (3–7) and very important (8–10).
Preferences: Patients indicated their current choice of transfusion methods by placing a check mark on an 11-box scale (“volunteer-donated blood” was on the left end, “uncertain” in the centre and “self-donated blood” on the right end). For analysis, preferences were grouped as follows: volunteer-donated blood (boxes 1–3), uncertain (4–8) and self-donated blood (9–11).
Decisional conflict: The Decisional Conflict Scale measures a person's uncertainty about making a decision. It has been validated and used in a variety of studies.11,12 Uncertainty is greater when a person feels uninformed about the alternatives, benefits and risks, unclear about personal values, or feels unsupported by others. Four subscales were used: uncertain (3 questions), uninformed (5 questions), unclear values (3 questions) and unsupported (4 questions). Ratings were expressed on a 5-point Likert scale (1 = strongly agree, 3 = neither agree nor disagree and 5 = strongly disagree). Mean scores for each subscale and overall mean scores for 15 questions were calculated for each patient. According to scale norms, patients with a mean score of 2 or less tend to make decisions, and those with a mean score above 2.5 tend to delay decisions.11,12 For example, people with a mean score close to 1 will feel highly confident about their decision, whereas those with a mean score close to 5 will feel very uncertain about which course of action to take.
Risk perception: An 8-item portion of the questionnaire was used to determine risk perception. Patients estimated the number out of 100 patients having cardiac surgery who need at least one transfusion, both for those who accept volunteer-donated blood and for those who donate their own blood. They rated their chances of having complications (AIDS, hepatitis and immediate reactions) for both transfusion methods. Risks were stated in words and were compared to familiar local and regional populations. Responses were structured to assess comprehension rather than memory. Patients were given the options of stating an exact probability if known, checking a probability “closest to” their estimate on a list, or of indicating “I have no idea of the chance.” Exact probabilities were converted to the corresponding “closest-to” category for consistency in analysis.
Acceptability: Patients were asked to rate the length, clarity, fairness and helpfulness of the decision aid on a 4- or 5-box scale. They were asked if they would recommend the decision aid to others; the responses “I would definitely recommend it” and “I would probably recommend it” were grouped together.
Statistical analysis
Knowledge scores were compared using paired t-tests. Changes in values and preferences were evaluated using the Fleiss modification of the Stuart–Maxwell test.13 Decisional conflict scores were compared using both paired t-tests and Wilcoxon's signed-rank tests. Since the results were the same, only the t-test results are reported here. A sign test was used for subgroup analysis of the uncertainty subscale because of asymmetry of the difference scores. The McNemar test was used to assess the risk perception responses.
Results
Of the 59 participants 11 (19%) were women and 48 (81%) were men. The proportion of women was lower than the proportion of female surgical patients at the Ottawa Heart Institute (27%) over an 11-month period that included the 3-month study period. The median age was 70 years for the female participants and 60 for the male participants. The language spoken at home was English for 45 patients (76%), French for 13 (22%) and “other” for 1 patient (2%). Education levels varied widely: 37 (63%) had a high school diploma or less, 22 (37%) had at least some postsecondary education, and 10 (17%) had a university degree. Forty-eight patients (81%) were to have coronary artery bypass grafting, 8 (14%) valve surgery and 3 (5%) combined bypass and valve surgery. Fifty-three (90%) were undergoing heart surgery for the first time. None had ever donated blood for their own use.
Measures
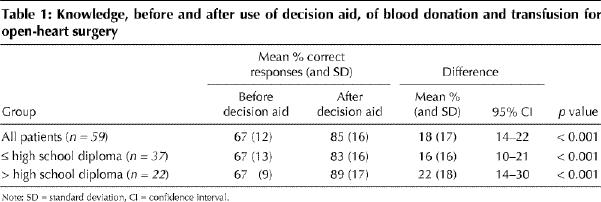
Knowledge: There was a significant improvement in knowledge after use of the decision aid (Table 1); the effect was similar when the patients were divided into subgroups according to education level. Several misconceptions about blood transfusion were identified. Before using the decision aid, 26 (44%) of the patients felt that all people undergoing open-heart surgery received transfusions; after using the aid 7 (12%) felt that this was true. The corresponding figures before and after use of the decision aid were 26 (44%) and 7 (12%) for the belief that AIDS is a frequent complication of volunteer-donated blood transfusion, 27 (46%) and 21 (36%) for the belief that self-donation lowers the chance of any transfusion, 28 (47%) and 13 (22%) for the belief that there is no chance of receiving the wrong blood with self-donation, and 19 (32%) and 9 (15%) for the belief that donating blood does not cause symptoms.
Table 1
Values: Transfusion-transmitted viral infections were rated as very important both before and after use of the decision aid: AIDS 90% (52/58) before and 91% (53/58) after, hepatitis 88% (51/58) before and 91% (53/58) after, and unknown infections 88% (51/58) before and after. Reducing the number of transfusions, including those of self-donated blood, during surgery was rated as very important by 42% (24/57) before and 54% (31/57) after use of the decision aid. The inconvenience of self-donation was rated as unimportant by 57% (33/58) before and 47% (27/58) after use of the decision aid. None of the changes was statistically significant.
Preferences: Most of the patients strongly preferred the option of donating their own blood before surgery: 69% (41/59) before and 76% (45/59) after use of the decision aid. Of the 14 patients who were uncertain about self-donation before using the decision aid, 9 strongly preferred it, 2 strongly preferred the choice of volunteer-donated blood and 3 remained uncertain after use of the aid. The overall changes in preferences were significant (p = 0.03). Eleven of the 14 initially uncertain patients had a high school diploma or less, 11 were men, and 10 spoke English at home.
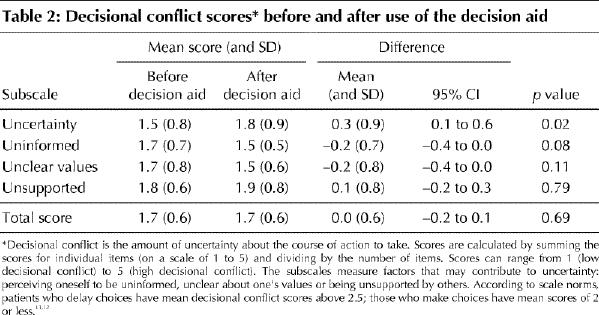
Decisional conflict: There was no significant difference in the mean overall decisional conflict score before and after use of the decision aid (Table 2), but there was a significant worsening in the mean uncertainty subscale score. The 45 patients who had made a choice at baseline had a small but statistically significant increase in median uncertainty scores, from 1.0 to 1.2 (p < 0.001), after use of the decision aid. The 14 patients who were uncertain at baseline had a nonsignificant reduction in median uncertainty scores, from 2.3 to 2.0 (p = 0.55), after using the aid.
Table 2
Risk perception: The results of the risk perception questions are shown in Table 3. Fig. 2 shows a typical example of the pattern of responses: although only 42% of the patients correctly estimated the risk of AIDS from volunteer-donated blood transfusion after using the decision aid, an additional 32% answered within one category of the correct answer. For each question, there was a marked reduction in the proportion of patients who did not know the risk estimate after using the aid.
Table 3
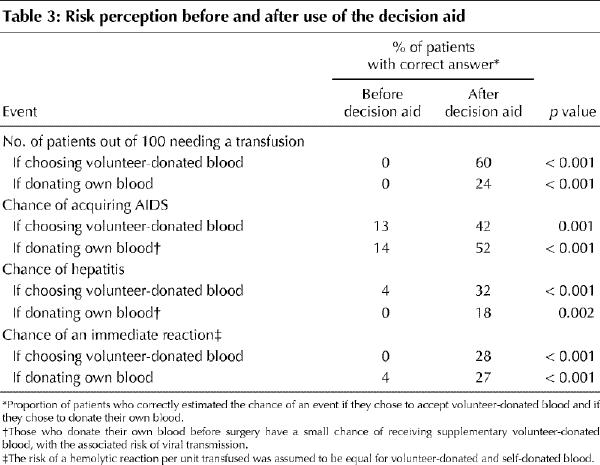
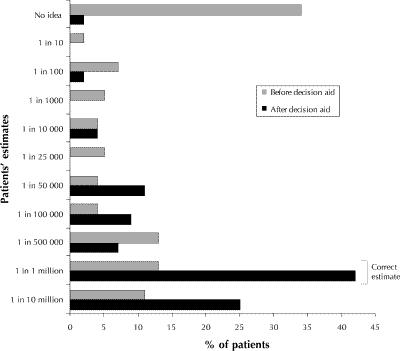
Fig. 2: Patients' estimates, before and after use of the decision aid, of the chance of AIDS from blood transfusions if they were to choose volunteer-donated blood. Correct estimate is 1 in 1 million.
Acceptability: The majority of patients felt that the decision aid was acceptable: 91% (48/53) felt that the length was “about right,” 88% (49/56) indicated that “most things were clear” or that “everything was clear,” 74% (40/54) felt that it was “balanced and fair,” 80% (45/56) indicated that it was “very” or “somewhat” helpful, and 95% (52/55) indicated that they would “definitely” or “probably” recommend it to others.
Interpretation
The greatest beneficial effects of the decision aid were improvements in the patients' knowledge and risk perception of blood donation and transfusion for open-heart surgery. The improvement in knowledge was seen both among those with a high school education or less and among those with higher levels of education. However, many of the patients did not understand 2 concepts. First, those who donate their own blood before surgery are at greater risk of receiving any transfusion (self-donated or volunteer-donated blood) than those who choose to receive volunteer-donated blood.1 This increased risk is likely due to patients who donate their own blood having lower preoperative hemoglobin levels and to their surgeons using more liberal transfusion criteria.14,15 Second, the greater frequency of transfusion increases the risk of receiving ABO incompatible blood or blood contaminated by bacteria. Future editions of the decision aid will need to be modified to help patients understand these concepts. Patients receiving the modified decision aid, who may be more aware of the limitations of self-donated blood transfusion, may be less enthusiastic to donate their own blood than the study patients were.
The decision aid had little effect on the choices of those who had strong preferences at baseline, but it did help those who were initially uncertain. Results from previous studies support our findings.4,9
In contrast to previous trials of decision aids that have shown a reduction in decisional conflict,4,9 our study, and a randomized controlled trial of a decision aid in antithrombotic therapy,10 showed no overall effect. However, there was a significant increase in the median uncertainty subscale score. This increased uncertainty may have been due to newly acquired knowledge of the complications associated with self-donated blood transfusion and is therefore not necessarily detrimental.
Potential selection bias may limit the generalizability of our findings. We were concerned that women were underrepresented and that the majority of patients strongly favoured self-donation. The male preponderance may be explained in part by the fact that men aged 65 to 74 years are 3 times as likely as women of the same age to undergo a coronary artery bypass procedure in Ontario.16 It would be important to examine more women's responses to the decision aid, because they are more likely than men to rate health hazards as “high risk.”17 The strong preferences for self-donation may be explained in part by regional enthusiasm. Self-donated units of blood comprise 9% of blood collections in Ottawa, as compared with the average of 2.4% at all Canadian transfusion centres.18
In summary, a decision aid in the form of a booklet and audiotape allows the use of verbal descriptions, numerical statements, charts and risk comparisons, and thus appeals to people with different educational backgrounds and learning abilities. The decision aid may potentially benefit patients by improving their knowledge and expectations, and by helping those who are uncertain to make choices. A randomized controlled trial of a modified decision aid is underway, and it will provide more information about its effect on decision-making.
Footnotes
This article has been peer reviewed.
Acknowledgments: We thank Lynda Hoey for her assistance with the patient interviews and data collection, and Jacqueline Tetroe, Liz Drake, Kim Robertson and Finlay McAlister for their help with developing the decision aid. We thank George Wells for statistical advice. We are grateful to the surgeons and their assistants at the Ottawa Heart Institute for encouraging their patients to participate in our study.
This research was supported in part by a grant from the Medical Research Council of Canada (grant no. 13304). Andreas Laupacis is a Senior Scientist of the Canadian Institute for Health Research. Annette O'Connor is the recipient of an Ontario Ministry of Health Career Scientist Award.
Competing interests: None declared.
Correspondence to: Dr. F. Curry Grant, Institute for Clinical Evaluative Sciences, 2075 Bayview Ave., Building G, Toronto ON M4N 3M5; fax 416 480-6048; curry.grant@ices.on.ca
References
- 1.Forgie MA, Wells PS, Laupacis A, Fergusson D. Preoperative autologous donation decreases allogeneic transfusion but increases exposure to all red blood cell transfusion: results of a meta-analysis. Arch Intern Med 1998;158:610-6. [DOI] [PubMed]
- 2.Etchason J, Petz L, Keeler E, Calhoun L, Kleinman S, Snider C, et al. The cost effectiveness of preoperative autologous blood donations. N Engl J Med 1995; 332(11):719-24. [DOI] [PubMed]
- 3.AuBuchon JP. Cost-effectiveness of preoperative autologous blood donation for orthopedic and cardiac surgeries. Am J Med 1996;101(Suppl 2A):38S-42S. [DOI] [PubMed]
- 4.O'Connor AM, Tugwell P, Wells GA, Elmslie T, Jolly E, Hollingworth G, et al. A decision aid for women considering hormone therapy after menopause: decision support framework and evaluation. Patient Educ Couns 1998;33(3):267-79. [DOI] [PubMed]
- 5.Consumer health informatics and patient decisionmaking: final report [AHCPR publication no. 98-N001]. Rockville (MD): Agency for Health Care Policy and Research; 1997. Summary available: www.ahrq.gov/research/rtisumm.htm (accessed 2001 Mar 20).
- 6.Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Mahwah (NJ): Lawrence Erlbaum Associates; 1988. p. 62-6.
- 7.Schreiber GB, Busch MP, Kleinman SH, Korelitz JJ. The risk of transfusion-transmitted viral infections. N Engl J Med 1996;334(26):1685-90. [DOI] [PubMed]
- 8.Linden JV, Paul B, Dressler KP. A report of 104 transfusion errors in New York State. Transfusion 1992;32(7):601-6. [DOI] [PubMed]
- 9.O'Connor AM, Tugwell P, Wells GA, Elmslie T, Jolly E, Hollingworth G, et al. Randomized trial of a portable, self-administered decision aid for post-menopausal women considering long-term preventive hormone therapy. Med Decis Making 1998;18:295-303. [DOI] [PubMed]
- 10.Man-Son-Hing M, Laupacis A, O'Connor AM, Biggs J, Drake E, Yetisir E, et al. A patient decision aid regarding antithrombotic therapy for stroke prevention in atrial fibrillation: a randomized controlled trial. JAMA 1999;282:737-43. [DOI] [PubMed]
- 11.O'Connor AM. Validation of a decision conflict scale. Med Decis Making 1995; 15:25-30. [DOI] [PubMed]
- 12.O'Connor AM. Decisional conflict scale. 3rd ed. Ottawa: Loeb Health Research Institute; 1998.
- 13.Fleiss JL. Statistical methods for rates and proportions. 2nd ed. New York: John Wiley & Sons; 1981. p. 119-23.
- 14.Dupuis JY, Bart B, Bryson G, Robblee J. Transfusion practices among patients who did and did not predonate autologous blood before elective cardiac surgery. CMAJ 1999;160(7):997-1002. Available: www.cma.ca/cmaj/vol-160/issue-7/0997.htm [PMC free article] [PubMed]
- 15.Graham I, Fergusson D, Dokainish H, Biggs J, McAuley L, Laupacis A. Autologous versus allogeneic transfusion: patients' perceptions and experiences. CMAJ 1999;160(7):989-95. Available: www.cma.ca/cmaj/vol-160/issue-7/0989.htm [PMC free article] [PubMed]
- 16.Shin AY, Jaglal S, Slaughter P, Iron K. Women and heart disease. In: Naylor CD, Slaughter PM, editors. Cardiovascular health and services in Ontario: an ICES atlas. Toronto: Institute for Clinical Evaluative Sciences; 1999. p. 335-54.
- 17.Krewski D, Slovic P, Bartlett S, Flynn J, Mertz CK. Health risk perception in Canada. 1: Rating hazards, sources of information and responsibility for health protection. Hum Ecol Risk Assess 1995;1(2):117-32.
- 18.Canadian Red Cross/Blood Services. 1997–1998 statistical report. Ottawa: Canadian Red Cross/Blood Services; 1998.


