Abstract
Obesity increases the risk of developing cardiovascular disease and other metabolic diseases. We intended to compare three different anthropometric indicators of obesity, in predicting the incidence of cardiovascular events in Chinese type 2 diabetes. Beijing Community Diabetes Study was a prospective multi-center study conducted in Beijing community health centers. Type 2 diabetes patients from fourteen community health centers were enrolled at baseline. The primary endpoint was cardiovascular events. The upper quartile of neck circumference (NC) was set as greater NC. A total of 3299 diabetes patients were enrolled. In which, 941 (28.52%) had cardiovascular disease at baseline. Logistic analysis showed that central obesity (waist circumference (WC) above 90 cm in men and 85 cm in women) and greater NC were all related to baseline cardiovascular disease (adjusted OR = 1.49, and 1.55). After 10-year follow-up, 340 (10.31%) had cardiovascular events. Compared with patients without cardiovascular events, those having cardiovascular events had higher BMI, larger WC and NC. Cox regression analysis showed that greater WC and NC were all associated with the occurrence of cardiovascular events (adjusted HR = 1.41, and 1.38). A higher NC and WC might increase the risk of cardiovascular events by about 40% in type 2 diabetes patients in Beijing communities.
Subject terms: Cardiology, Endocrinology, Risk factors
Introduction
Obesity is a major public health problem worldwide1. Multiple studies have shown the association of obesity with increased risk of developing type 2 diabetes mellitus (T2DM), coronary heart disease, stroke and other metabolic syndrome2–5. Obesity has been evaluated using several anthropometric indexes, such as body mass Index (BMI), waist circumference (WC), and neck circumference (NC). NC, as an index for upper-body subcutaneous fat distribution, was reported by Sjostrom et al. in 19956, and independently associated with cardiovascular risk factors in obese individuals. There were several studies to explore the association between NC and cardiovascular disease (CVD)7–9. In the Framingham heart study, it was found that NC was associated with CVD risk factors, however, not with the incidence of CVD events7. In a prospective cohort study, a greater NC was associated with a higher incidence of CVD events and mortality in high-risk population8. A cross-sectional study conducted on people with stable angina showed that NC was better in predicting the risk of coronary artery disease than BMI9. A report from the Beijing Community Diabetes Study (BCDS) baseline data found that NC was positively associated with central obesity and overweight in Chinese T2DM people10. The analysis from the BCDS 8-year follow-up data showed that NC was related to the incidence of CVD events following an 8-year management in T2DM11. CVD is one of macrovascular complications of T2DM and the leading cause of mortality in T2DM in China12. Several studies have reported the association of obesity indexes with CVD risk factors and CVD11,13,14. However, there is lack of prospective studies comparing the effects of BMI, WC, and NC on predicting the future CVD events in the Chinese T2DM patients. The aim of the present study was to evaluate the association between NC, WC, BMI and the occurrence of CVD events in T2DM following a 10-year management in Beijing communities.
Results
Baseline demographic characteristics
At baseline, a total of 3299 participants with T2DM were enrolled, in which, 1316 (39.89%) were males and 1983 (60.11%) were females. The mean age was 62.40 ± 10.48 years. The mean NC was 36.49 ± 3.73 cm. Higher NC (NC above the upper quartile) was observed among 671 (20.34%) participants, 670 (20.31%) were obese and 1978 (59.96%) had central obesity (WC ≥ 90 cm in men and ≥ 85 cm in women).
A total of 941 (28.52%) had a history of CVD at baseline. On comparing two BMI groups (BMI < 28 kg/m2 and BMI ≥ 28 kg/m2) with the prevalence of CVD, no statistically significant difference was observed (27.92% vs 30.90%, P = 0.128). With WC, participants with central obesity showed higher prevalence of CVD compared with those without central obesity (31.09 vs 24.68%, P < 0.001) and the association was found to be statistically significant. Also, participants with higher NC (NC above the upper quartile) showed statistically significant difference with the prevalence of CVD compared with those without high NC (27.17% vs 33.83%, P = 0.001).
Logistic analysis showed participants with central obesity and high NC were all associated with the baseline CVD (Crude OR = 1.38 (95% CI 1.18–1.61), 1.37 (95% CI 1.14–1.64), respectively, all P < 0.01). After adjusting age, diabetic duration, HbA1c, LDL, hypertension, gender, smoking, serum creatinine and aspirin treatment, these associations persisted (Adjusted OR = 1.49 (95% CI 1.12–1.97), 1.55 (95% CI 1.14–2.10), all P < 0.01). Obesity (BMI ≥ 28 kg/m2) was also associated with the baseline CVD (Adjusted OR = 1.47 (95% CI 1.08–2.00), P = 0.014).
The occurrence of CVD events after 10-year follow-up
After 10-year follow-up, 340 participants experienced CVD events and the total incidence of CVD events was 10.31%. In men, the incidence of CVD events was 12.61%, whereas, among women it was 8.77% (P < 0.001). The total incidence of coronary events and cerebral events was 6.24% and 4.06% respectively.
Compare with participants without CVD events, people with CVD events were older and had greater BMI, WC and NC. However, no statistically significant difference was observed in NC between participants with and without CVD events. A statistically significant difference in SBP and HbA1c was observed (P < 0.05). People with CVD events had higher prevalence of baseline CVD (Table 1).
Table 1.
Baseline characteristics in people with and without cardiovascular events.
| Total (n = 3299) | Without CVD group (n = 2959) | CVD group (n = 340) | t value | P value | |
|---|---|---|---|---|---|
| Age (year) | 62.40 ± 10.48 | 62.05 ± 10.63 | 65.40 ± 8.48 | − 6.69 | < 0.001 |
| Men (n, %) | 1316 (39.89) | 1150 (38.86) | 166 (48.82) | 12.61# (x2) | < 0.001 |
| Women (n, %) | 1983 (60.11) | 1809 (61.14) | 174 (51.18) | ||
| Diabetic duration (year) | 11.80 ± 98.31 | 12.16 ± 103.46 | 8.43 ± 9.77 | 1.73 | 0.083 |
| BMI (kg/m2) | 25.37 ± 3.47 | 25.32 ± 3.45 | 25.82 ± 3.56 | − 2.49 | 0.013 |
| WC (cm) | 89.23 ± 9.43 | 89.00 ± 9.38 | 91.22 ± 9.69 | − 4.13 | < 0.001 |
| NC (cm) | 36.49 ± 3.73 | 36.45 ± 3.69 | 36.85 ± 4.02 | − 1.77 | 0.077 |
| SBP (mmHg) | 129.36 ± 14.81 | 128.95 ± 14.61 | 132.96 ± 16.01 | − 4.38 | < 0.001 |
| DBP (mmHg) | 77.89 ± 8.96 | 77.92 ± 8.88 | 77.64 ± 9.64 | 0.50 | 0.615 |
| FPG (mmol/L) | 7.95 ± 2.65 | 7.94 ± 2.67 | 7.95 ± 2.42 | − 0.04 | 0.967 |
| PPG (mmol/L) | 10.70 ± 5.01 | 10.66 ± 5.09 | 11.09 ± 4.26 | − 1.67 | 0.095 |
| HbA1c (%) | 7.36 ± 1.64 | 7.34 ± 1.65 | 7.57 ± 1.56 | − 2.44 | 0.015 |
| TG (mmol/L) | 1.84 ± 1.31 | 1.83 ± 1.31 | 1.90 ± 1.36 | − 0.89 | 0.371 |
| TC (mmol/L) | 5.23 ± 1.24 | 5.22 ± 1.24 | 5.35 ± 1.23 | − 1.81 | 0.070 |
| LDL (mmol/L) | 3.04 ± 0.94 | 3.03 ± 0.94 | 3.10 ± 0.88 | − 1.18 | 0.237 |
| HDL (mmol/L) | 1.34 ± 0.47 | 1.35 ± 0.45 | 1.31 ± 0.61 | 0.94 | 0.350 |
| Smoking (n, %) | 543 (16.46) | 487 (16.46) | 56 (16.47) | 0.00# (x2) | 0.995 |
| Baseline CVD diseases (n, %) | 941 (28.52) | 785 (26.53) | 156 (45.88) | 56.02# (x2) | < 0.001 |
| Aspirin Treatment (n, %) | 1694 (51.35) | 1470 (49.68) | 224 (65.88) | 32.05# (x2) | < 0.001 |
| Lipid lowering treatment (n, %) | 2185 (66.23) | 1959 (66.20) | 226 (66.47) | 0.01# (x2) | 0.928 |
CVD cardiovascular disease, BMI body mass index, WC waist circumference, NC neck circumference, SBP systolic blood pressure, DBP diastolic blood pressure, FPG, fasting plasma glucose, HbA1c hemoglobin A1c, TG triglyceride, TC total cholesterol, HDL high-density lipoprotein cholesterol, LDL low-density lipoprotein cholesterol.
#Chi-square was used.
Association of BMI, WC and NC with the occurrence of CVD events
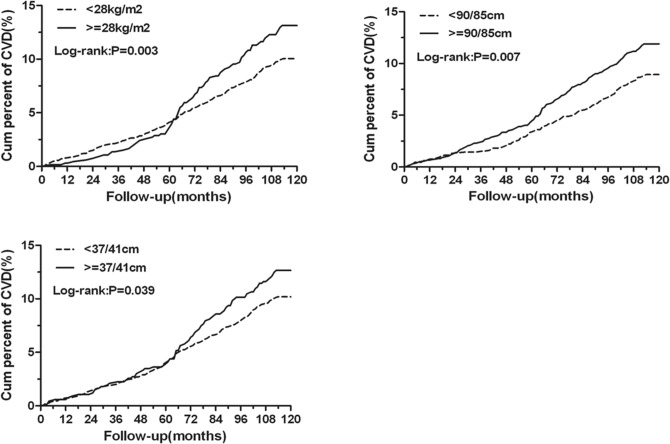
Kaplan–Meier analysis showed that obesity, central obesity and high NC were associated with the cumulative incidence of CVD events, log-rank test confirmed these associations (P < 0.05, Fig. 1).
Figure 1.
Kaplan–Meier estimates for body mass index, waist circumference, neck circumference with cardiovascular events during 10-year management. CVD cardiovascular diseases. This figure was drawn by using SAS for Windows version 9.2
Cox regression analysis showed that central obesity and high NC were associated with the occurrence of CVD events after adjusting age, diabetic duration, HbA1c, LDL and hypertension (Adjusted HR = 1.39 (95% CI 1.07–1.82), 1.42 (95% CI 1.08–1.88), P < 0.05). Further adjusting baseline CVD, gender, smoking, serum creatinine and aspirin treatment, these associations persisted (Adjusted HR = 1.41 (95% CI 1.08–1.84), 1.38 (95% CI 1.04–1.83), P < 0.05). However, obesity was not associated with the occurrence of CVD events when obesity was diagnosed by measuring participant’s BMI (Adjusted HR = 1.31 (95% CI 0.98–1.75)).
Discussion
In this study, the cumulative prevalence of CVD events increased with the BMI, WC and NC enlargement. Higher WC and NC were associated not only with the baseline CVD, but also with the incidence of CVD events during the 10-year management. Our study results showed that higher NC and WC might increase the risk of CVD and CVD events by about 40% in T2DM patients in Beijing communities. However, no association was found between higher BMI and the incidence of CVD events.
NC, a new indicator of upper body subcutaneous fat, is a reliable tool to screen obesity15. And NC was reported to be associated positively with central obesity and overweight in diabetes population10,16. Studies have shown positive correlation of NC measurement with multiple CVD risk factors, such as lipid profile, blood pressure and insulin resistance7,17–19. NC was also found to be related to metabolic syndrome in diabetes20. The relationship between NC and CVD was explored in different population9,13,21. A cross-sectional study showed that NC was associated with coronary artery disease in people with stable angina9. Another cross-sectional study in diabetes people found that NC was associated with the prevalence of CVD21. A meta-analysis including eight observation studies found that NC was related to CVD, especially when CVD was diagnosed by coronary angiography13. There were prospective studies to explore the association between NC and CVD events8,11. In a prospective cohort study involving high-risk CVD patients, higher NC was related to increased incidence of future fatal and non-fatal CVD events8. NC was also found to be associated with the incidence of CVD events in T2DM11.
WC has been used to measure abdominal adiposity and it is one of the indicators of obesity in clinical practice as recommended by the Chinese guideline for type 2 diabetes22. WC was associated with CVD risk factors23,24. A study conducted by Yang Liu et al. among the Chinese population suggested that WC was the predictor of multiple metabolic risk factors such as blood pressure, glucose, and triglyceride23. WC was found to be associated with blood pressure, glucose and total cholesterol in Vietnam subjects24. WC was reported to be related to the prevalence of CVD in an international study conducted in primary care25. In a prospective study conducted in Japanese diabetes people, WC was not a predictive indicator for future CVD events despite WC was associated with CVD risk factors26. However, In ADVANCE (Action in Diabetes and Vascular disease: preterAx and diamicroN-MR Controlled Evaluation) trial, an international cohort study, WC was related to CVD events in subjects with T2DM27.A meta-regression analysis showed WC was positively associated with the risk of CVD events, i.e. for 1 cm increase in WC, there would be 2% increase in the relative risk of CVD events28.
Though BMI was widely used in clinical practice to measure obesity, BMI could not reflect the body fat distribution. Also, BMI has been sub-optimally correlated with obesity in CVD patients due to variation in body fat distribution and metabolic risk factors associated29,30. Meta-analysis showed that increase in BMI was associated with the risk of CVD events31–33. However, Previous studies have found that high BMI was associated with lower mortality among patients with CVD and in other population as well29.
There were studies comparing the effects of different indicators of obesity on CVD25,34. An international cross-sectional study showed that WC had a stronger relationship with CVD compared with BMI25. A study conducted by Canoy et al.34 assessing distribution of body fat and risk of CVD found that abdominal obesity was the stronger predictor of CVD compared with BMI. Evaluation of different anthropometric indicators to assess CVD events among diabetes patients is limited. A prospective study conducted by Cho et al.35 showed a strong association of BMI with increased risk of CVD events in diabetes women with no history of CVD. However, in ADVANCE trial, WC, not BMI was related to CVD events in subjects with T2DM27. This finding is in line with our study result. In our study, WC, not BMI was associated with the increased risk of CVD events in T2DM people. There is lack of prospective cohort studies in T2DM comparing NC, WC and BMI on predicting the future CVD events. Our study reported the effects of BMI, WC, and NC on the incidence of CVD events in T2DM. In our study, NC and WC were found to have comparable association with the occurrence of CVD events in Chinese T2DM. The measurement of WC is not always practical in clinical practice, especially in winter. And it may differ between and after meal, especially in obese people. Our results indicated that NC might be used as a simple test for identifying obesity in predicting CVD events in future clinical practice, especially when the measurement of WC was inconvenient.
This study had some limitations. Initially, all the people with T2DM were managed by general practitioners according to the Chinese guideline for type 2 diabetes. The antiglycemic, antihypertensive and statin medication might have changed during the 10-year follow-up to result in HbA1c, blood pressure and LDL levels under control according to the Chinese guideline for type 2 diabetes. This might affect the incidence of CVD events compared with T2DM patients without management. Secondly, T2DM itself is a risk factor for CVD events36. T2DM people had higher prevalence of CVD. In our study, 28.52% people had CVD when enrollment, which may increase the risk of CVD events. Thirdly, about 16% of the patients in our study did not participate in the last visit in 2018, which may affect the incidence of CVD events reported in this study. The incidence of CVD events in this study may be underestimated.
In conclusion, in this prospective multi-center study, during the 10-year follow-up, greater NC and WC were associated not only with the prevalence of CVD, but also with the occurrence of CVD events in Chinese T2DM population. Moreover, NC and WC had comparable association with the occurrence of CVD events in Chinese T2DM. Greater NC and WC might increase the risk of CVD events by about 40%. Further large-scale prospective studies are needed to confirm this relationship.
Methods
This prospective, multi-center study (Beijing Community Diabetes Study, BCDS) was conducted at fourteen community health centers such as, Cuigezhuang, Jinsong, Xinjiekou, Yuetan, Donggaodi, Yongdinglu, Sanlitun, Jiangtai, Shazikou, Balizhuang, Zuojiazhuang, Dongfeng, Sijiqing and Majiapu community health center associated with Beijing Tongren Hospital. Multistage random sampling method was used to recruit T2DM patients at baseline in 2008 and the patients were followed up for next 10 years. T2DM patients aged 20 to 80 years and those who residing in the same community for at least 5 years were included in the study. Patient with hepatic failure, renal failure, severe disabilities, schizophrenia or goiter were excluded. Details of study design, methods and population of BCDS had been reported elsewhere10,37. A total of 140 participants with incomplete baseline data such as height, weight, neck circumference, waist circumference and lab values were excluded. There were 3299 DM participants were included in the analysis and 84% participants participated in the last visit in 2018.
The ethical approval was obtained from the Ethics Committee of Beijing Tongren Hospital, Capital Medical University. The study was conducted in accordance with the provisions of the Declaration of Helsinki and its subsequent revisions. Written informed consent was obtained from all the participants.
A physical examination including anthropometric parameters like BMI, WC and NC was performed according to the study protocol at baseline and subsequent follow-up visits. BMI was calculated by dividing body weight (kg) with the height squared (m2) along with light clothing and without shoes. WC (cm) was measured horizontally between the lower rib margin and the iliac crest in the mid-axillary line, with the subject in standing position and fasting. NC (cm) was measured horizontally at the upper margin of the laryngeal prominence (Adam’s apple) with people standing, head erecting and eye facing forward according to the protocol10,37. Patients with BMI ≥ 28 kg/m2 was diagnosed obese and WC ≥ 90 cm in men and 85 cm in women was set as the criteria of diagnosing central obesity according to the Chinese guidelines for Type 2 Diabetes22. NC above the upper quartile was defined as high NC. CVD was defined if the patients had been diagnosed in a top tier hospital having coronary heart disease, myocardial infarction, angina pectoris, stroke, or other clinical manifestations of CVD.
Over the follow-up period of 10 years, all the T2DM patients were seen by a collaborative team at least four times each year32. The study outcome was the occurrence of CVD events including coronary events (cardiac death, myocardial infarction, unstable angina pectoris, hospitalization for heart failure and coronary revascularization) and cerebral events (stroke, transient ischemic attack). Stroke was confirmed by cranial Computed Tomography or Magnetic Resonance Imaging.
Statistical analysis
The database was established using Epi-Data software (version 3.0). SAS software (SAS Institute Inc., Cary, NC) was used in statistical analysis. All the T2DM patients were categorized into the CVD group and without CVD group. An unpaired student t-test and chi-square test was used to compare the continuous and categorical data respectively at baseline and follow-up. The association between BMI, WC, NC and baseline CVD was assessed using Logistic regression to estimate the odds ratio (OR) and 95% confidence interval (CI). Kaplan–Meier analysis and log-rank test were used to assess the associations between BMI, WC, NC and the cumulative percentage of CVD events. The proportional hazards assumption of the Cox model was tested (Supplementary Table S1, Fig. S1). The proportional hazards Cox regression analysis was used to estimate the effects of BMI, WC and NC on CVD events risk and hazard ratio (HR) with 95% CI was reported. Last Observation Carry Forward (LOCF) was used for missing data during the 10-year follow-up. The physical and lab examination values were imputed by using the data of the most recent previous visit. The study outcome was imputed by the most recent reported outcome. The time of dropout was the time of the most recent previous visit. A P value < 0.05 in 2-tailed tests was considered to be statistically significant.
Supplementary Information
Acknowledgements
We thank Jian-Ping Feng (Department of Endocrinology, Beijing Tongren Hospital, Capital Medical University), Su-Fang Pan (Department of Endocrinology, Beijing Tongren Hospital, Capital Medical University) and general practitioners who took part in the study. Zong-Xue Lu, Shu-Xian Ma, Shu-Qin Yang, and Wei Bai are thanked as members of the Supervisory committee. This work was supported by Capital’s Funds for Health Improvement and Research (2016-1-2057, 2016-2-2054, 2020-1-1181), Beijing Municipal Science &Technology Commission (Z151100004015021) and the Beijing Municipal Training Foundation for Highly-qualified and Technological Talents of Health System (2014-3-013).
Author contributions
G.R.Y. researched data, wrote manuscript and took responsibility for the contents of the article. S.Y.Y and R.R.H. reviewed manuscript and took responsibility for the contents of the article. G.W. analyzed the data. H.J.F., M.X.Y., X.L.Z., L.X.Z., R.R.X., J.D.Z., Y.L.L., Y.H.S., Q.F.D., D.Y.G., X.L. C., J.Q.G., Z.M.W., Y.J.C., Y.J.L., D.M.H., J.G., Y.G., J. M. and Y.J.C. researched data.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Guang-Ran Yang, Email: gr.yang@ccmu.edu.cn.
Shen-Yuan Yuan, Email: fulvic@126.com.
Rury. R. Holman, Email: rury.holman@dtu.ox.ac.uk
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-88927-9.
References
- 1.Finucane MM, et al. National, regional, and global trends in body-mass index since 1980: Systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet. 2011;377:557–567. doi: 10.1016/S0140-6736(10)62037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Logue J, et al. Obesity is associated with fatal coronary heart disease independently of traditional risk factors and deprivation. Heart. 2011;97:564–568. doi: 10.1136/hrt.2010.211201. [DOI] [PubMed] [Google Scholar]
- 3.Wang Y, Rimm EB, Stampfer MJ, Willett WC, Hu FB. Comparison of abdominal adiposity and overall obesity in predicting risk of type 2 diabetes among men. Am. J. Clin. Nutr. 2005;81:555–563. doi: 10.1093/ajcn/81.3.555. [DOI] [PubMed] [Google Scholar]
- 4.Donahue RP, Abbott RD. Central obesity and coronary heart disease in men. Lancet. 1987;2:1215. doi: 10.1016/s0140-6736(87)91357-2. [DOI] [PubMed] [Google Scholar]
- 5.Prospective Studies Consortium Body-mass index and cause-specific mortality in 900,000 adults: Collaborative analyses of 57 prospective studies. Lancet. 2009;373:1083–1096. doi: 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sjostrom CD, Hakangard AC, Lissner L, Sjostrom L. Body compartment and subcutaneous adipose tissue distribution–risk factor patterns in obese subjects. Obes. Res. 1995;3:9–22. doi: 10.1002/j.1550-8528.1995.tb00116.x. [DOI] [PubMed] [Google Scholar]
- 7.Preis SR, et al. Neck circumference as a novel measure of cardiometabolic risk: The Framingham Heart Study. J. Clin. Endocrinol. Metab. 2010;95:3701–3710. doi: 10.1210/jc.2009-1779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dai Y, Wan X, Li X, Jin E, Li X. Neck circumference and future cardiovascular events in a high-risk population—A prospective cohort study. Lipids Health Dis. 2016;15:46. doi: 10.1186/s12944-016-0218-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arjmand G, Shidfar F, Molavi Nojoomi M, Amirfarhangi A. Anthropometric indices and their relationship with coronary artery diseases. Health Scope. 2015;4:e25120. doi: 10.17795/jhealthscope-25120. [DOI] [Google Scholar]
- 10.Yang GR, et al. Neck circumference positively related with central obesity, overweight, and metabolic syndrome in Chinese subjects with type 2 diabetes: Beijing Community Diabetes Study 4. Diabetes Care. 2010;33:2465–2467. doi: 10.2337/dc10-0798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang G-R, et al. Association between neck circumference and the occurrence of cardiovascular events in type 2 diabetes: Beijing Community Diabetes Study 20 (BCDS-20) Biomed. Res. Int. 2019;2019:6. doi: 10.1155/2019/4242304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lyu Y, et al. Regional differences in the prevalence of coronary heart disease and stroke in patients with type 2 diabetes in China. J. Clin. Endocrinol. Metab. 2018;103:3319–3330. doi: 10.1210/jc.2018-00422. [DOI] [PubMed] [Google Scholar]
- 13.Yang GR, et al. Association between neck circumference and coronary heart disease: A meta-analysis. Asian/Pac. Island Nurs. J. 2019;4:34–46. doi: 10.31372/20190401.1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ping Zhong DS, Wu D, Li T, Wu Y, Xu L. Neck circumference can be used as a valuable tool to screen the cardiovascular risk factors in Chinese elderly: A community based study. Int. J. Clin. Exp. Med. 2017;10:3685–3691. [Google Scholar]
- 15.Ben-Noun L, Sohar E, Laor A. Neck circumference as a simple screening measure for identifying overweight and obese patients. Obes. Res. 2001;9:470–477. doi: 10.1038/oby.2001.61. [DOI] [PubMed] [Google Scholar]
- 16.Papazafiropoulou A, Anagnostopoulou K, Papanas N, Petropoulou K, Melidonis A. Neck circumference as a simple tool for assessing central obesity in patients with type 2 diabetes mellitus in Greece—A descriptive study. Rev. Diabetic Stud. 2016;13:215–216. doi: 10.1900/RDS.2016.13.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ben-Noun L, Laor A. Relationship of neck circumference to cardiovascular risk factors. Obes. Res. 2003;11:226–231. doi: 10.1038/oby.2003.35. [DOI] [PubMed] [Google Scholar]
- 18.Zhou JY, et al. Neck circumference as an independent predictive contributor to cardio-metabolic syndrome. Cardiovasc. Diabetol. 2013;12:76. doi: 10.1186/1475-2840-12-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liang J, et al. neck circumference and insulin resistance in Chinese adults: The Cardiometabolic Risk in Chinese (CRC) Study. Diabetes Care. 2013;36:e145–e146. doi: 10.2337/dc13-1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ozkaya I, Yardimci B, Tunckale A. Appropriate neck circumference cut-off points for metabolic syndrome in Turkish patients with type 2 diabetes. Endocrinol. Diabetes y Nutr. 2017;64:517–523. doi: 10.1016/j.endinu.2017.07.006. [DOI] [PubMed] [Google Scholar]
- 21.Wan H, et al. Associations between abdominal obesity indices and diabetic complications: Chinese visceral adiposity index and neck circumference. Cardiovasc. Diabetol. 2020;19:118. doi: 10.1186/s12933-020-01095-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Weng J, et al. Standards of care for type 2 diabetes in China. Diabetes Metab. Res. Rev. 2016;32:442–458. doi: 10.1002/dmrr.2827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu Y, Tong G, Tong W, Lu L, Qin X. Can body mass index, waist circumference, waist-hip ratio and waist-height ratio predict the presence of multiple metabolic risk factors in Chinese subjects? BMC Public Health. 2011;11:35. doi: 10.1186/1471-2458-11-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tran NTT, et al. The importance of waist circumference and body mass index in cross-sectional relationships with risk of cardiovascular disease in Vietnam. PLoS ONE. 2018;13:e0198202. doi: 10.1371/journal.pone.0198202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Balkau B, et al. International Day for the Evaluation of Abdominal Obesity (IDEA): A study of waist circumference, cardiovascular disease, and diabetes mellitus in 168,000 primary care patients in 63 countries. Circulation. 2007;116:1942–1951. doi: 10.1161/CIRCULATIONAHA.106.676379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sone H, et al. Waist circumference as a cardiovascular and metabolic risk in Japanese patients with type 2 diabetes. Obesity. 2009;17:585–592. doi: 10.1038/oby.2008.481. [DOI] [PubMed] [Google Scholar]
- 27.Czernichow S, et al. Comparison of waist-to-hip ratio and other obesity indices as predictors of cardiovascular disease risk in people with type-2 diabetes: A prospective cohort study from ADVANCE. Eur. J. Cardiovasc. Prev. Rehabil. 2011;18:312–319. doi: 10.1097/HJR.0b013e32833c1aa3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.de Koning L, Merchant AT, Pogue J, Anand SS. Waist circumference and waist-to-hip ratio as predictors of cardiovascular events: Meta-regression analysis of prospective studies. Eur. Heart J. 2007;28:850–856. doi: 10.1093/eurheartj/ehm026. [DOI] [PubMed] [Google Scholar]
- 29.Romero-Corral A, et al. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: A systematic review of cohort studies. Lancet. 2006;368:666–678. doi: 10.1016/S0140-6736(06)69251-9. [DOI] [PubMed] [Google Scholar]
- 30.Lim S. Ectopic fat assessment focusing on cardiometabolic and renal risk. Endocrinol. Metab. 2014;29:1–4. doi: 10.3803/EnM.2014.29.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bogers RP, et al. Association of overweight with increased risk of coronary heart disease partly independent of blood pressure and cholesterol levels: A meta-analysis of 21 cohort studies including more than 300 000 persons. Arch. Intern. Med. 2007;167:1720–1728. doi: 10.1001/archinte.167.16.1720. [DOI] [PubMed] [Google Scholar]
- 32.Zhou BF. Effect of body mass index on all-cause mortality and incidence of cardiovascular diseases—Report for meta-analysis of prospective studies open optimal cut-off points of body mass index in Chinese adults. Biomed. Environ. Sci. 2002;15:245–252. [PubMed] [Google Scholar]
- 33.Ni Mhurchu C, et al. Body mass index and cardiovascular disease in the Asia-Pacific Region: An overview of 33 cohorts involving 310,000 participants. Int. J. Epidemiol. 2014;33:751–758. doi: 10.1093/ije/dyh163. [DOI] [PubMed] [Google Scholar]
- 34.Canoy D, et al. Body fat distribution and risk of coronary heart disease in men and women in the European Prospective Investigation Into Cancer and Nutrition in Norfolk cohort: A population-based prospective study. Circulation. 2007;116:2933–2943. doi: 10.1161/CIRCULATIONAHA.106.673756. [DOI] [PubMed] [Google Scholar]
- 35.Cho E, et al. A prospective study of obesity and risk of coronary heart disease among diabetic women. Diabetes Care. 2002;25:1142–1148. doi: 10.2337/diacare.25.7.1142. [DOI] [PubMed] [Google Scholar]
- 36.Haffner SM, Lehto S, Ronnemaa T, Pyorala K, Laakso M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N. Engl. J. Med. 1998;339:229–234. doi: 10.1056/NEJM199807233390404. [DOI] [PubMed] [Google Scholar]
- 37.Yang GR, et al. Influence of educational attainments on long term glucose control and morbid events in patients with type 2 diabetes receiving integrated care from 15 China urban communities: The Beijing Community Diabetes Study 11. Prim. Care Diabetes. 2015;9:473–481. doi: 10.1016/j.pcd.2015.03.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.