To the Editor:
We enjoyed reading the systematic review recently published in CHEST (November 2020) by Adams et al.1 Based on 28 studies that included 3,466 patients, the authors analyzed known CT findings and structured the disease’s imaging signature. Expectedly, the most frequent pattern was ground glass opacity (81.0%), but more interesting was the high prevalence of “vascular thickening” (72.9%). Although vascular abnormalities have escaped the attention of early reports, they are described increasingly and recently gained interest regarding both pathophysiologic condition and prognosis.2 We regret that this review did not include more insights into those critical changes. In the current knowledge, vascular signs can be subdivided into two groups: thromboembolic-related abnormalities and nonthrombotic vascular changes. We believe that both should receive more attention, be identified, and reported in coronavirus disease 2019 (COVID-19) CT imaging.
From this perspective, we are intrigued by the fact that the potential incremental value of pulmonary CT angiography was not reported in this article nor discussed as a limitation. The use of IV contrast material may not be indicated in all individuals with known or suspected COVID-19; however, simultaneous severe acute respiratory syndrome coronavirus 2 pneumonia and acute pulmonary embolism is a common association that leads to specific therapeutic decisions.3 High incidence of thromboembolic disease is a hallmark of severe COVID-19 disease and should prompt pulmonary CT angiography in selected patients.4 Furthermore, the role of severe acute respiratory syndrome coronavirus 2-induced inflammation and thromboembolic events has been debated extensively.5
Additionally, we would like to comment that Adams et al1 classified vascular abnormalities as “bronchovascular abnormalities.” This classification scheme suggests two assumptions: (a) the dilated vessel is not independent of bronchial abnormalities and (b) the dilated vessel is part of the bronchovascular anatomy complex, therefore necessarily an artery. Actually, dilated vessels are mostly veins running at a distance from the bronchi. When examining Figure 5 in their article, the dilated vessel is more likely to be a vein. The connection of the dilated vein with the left atrium is better seen on adjusted multiplanar reformation, as shown in Figure 1 .
Figure 1.
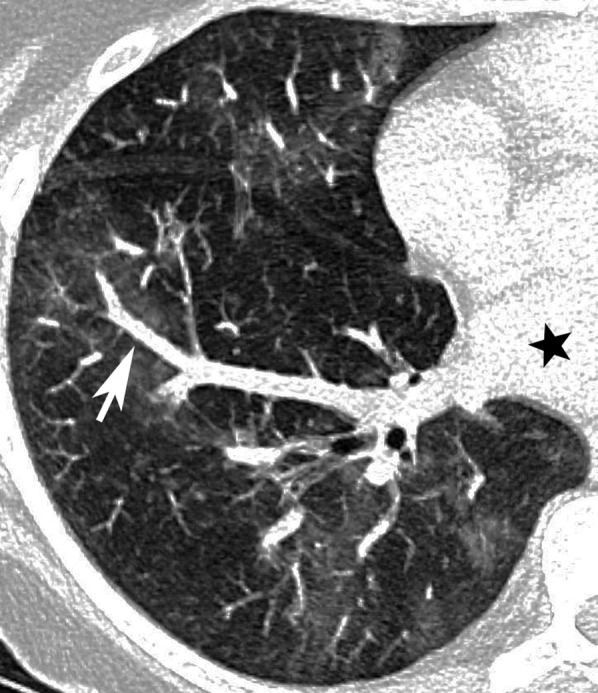
Axial oblique CT pulmonary angiography in a patient with severe acute respiratory syndrome coronavirus 2 pneumonia shows ground-glass opacity in the right lower lobe and dilation of a blood vessel draining the affected lung segment (arrow). The dilated blood vessel is connected to the left atrium (star), demonstrating its venous nature.
For those reasons, we believe that vascular changes are independent of bronchoalveolar damage and should be integrated into the signature of the COVID-19. Furthermore, we think that CT angiography should be considered part of the imaging findings and might have a crucial impact on the decision-making process and patient treatment.
Footnotes
FINANCIAL/NONFINANCIAL DISCLOSURES: None declared.
References
- 1.Adams H.J.A., Kwee T.C., Yakar D., Hope M.D., Kwee R.M. Chest CT imaging signature of coronavirus disease 2019 infection: in pursuit of the scientific evidence. Chest. 2020;158(5):1885–1895. doi: 10.1016/j.chest.2020.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tekcan Şanlı D.E., Yıldırım D. A new imaging sign in COVID-19 pneumonia: vascular changes and their correlation with clinical severity of the disease. Diagn Interv Radiol. 2021;27(2):172–180. doi: 10.5152/dir.2020.20346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moores L., Tritschler T., Brosnahan S. Prevention, diagnosis, and treatment of VTE in patients with coronavirus disease 2019: CHEST Guideline and Expert Panel report. Chest. 2020;158(3):1143–1163. doi: 10.1016/j.chest.2020.05.559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hauguel-Moreau M, Hajjam ME, De Baynast Q, et al. Occurrence of pulmonary embolism related to COVID-19 [published online ahead of print October 6, 2020]. J Thromb Thrombolysis. 10.1007/s11239-020-02292-4. [DOI] [PMC free article] [PubMed]
- 5.Wells P. Hypercoagulability in COVID-19. Journal of the South African Heart Association. 2020;17(3):266–274. [Google Scholar]


