Abstract
Objective
To assess rates of cardiovascular and haemostatic events in the first 28 days after vaccination with the Oxford-AstraZeneca vaccine ChAdOx1-S in Denmark and Norway and to compare them with rates observed in the general populations.
Design
Population based cohort study.
Setting
Nationwide healthcare registers in Denmark and Norway.
Participants
All people aged 18-65 years who received a first vaccination with ChAdOx1-S from 9 February 2021 to 11 March 2021. The general populations of Denmark (2016-18) and Norway (2018-19) served as comparator cohorts.
Main outcome measures
Observed 28 day rates of hospital contacts for incident arterial events, venous thromboembolism, thrombocytopenia/coagulation disorders, and bleeding among vaccinated people compared with expected rates, based on national age and sex specific background rates from the general populations of the two countries.
Results
The vaccinated cohorts comprised 148 792 people in Denmark (median age 45 years, 80% women) and 132 472 in Norway (median age 44 years, 78% women), who received their first dose of ChAdOx1-S. Among 281 264 people who received ChAdOx1-S, the standardised morbidity ratio for arterial events was 0.97 (95% confidence interval 0.77 to 1.20). 59 venous thromboembolic events were observed in the vaccinated cohort compared with 30 expected based on the incidence rates in the general population, corresponding to a standardised morbidity ratio of 1.97 (1.50 to 2.54) and 11 (5.6 to 17.0) excess events per 100 000 vaccinations. A higher than expected rate of cerebral venous thrombosis was observed: standardised morbidity ratio 20.25 (8.14 to 41.73); an excess of 2.5 (0.9 to 5.2) events per 100 000 vaccinations. The standardised morbidity ratio for any thrombocytopenia/coagulation disorders was 1.52 (0.97 to 2.25) and for any bleeding was 1.23 (0.97 to 1.55). 15 deaths were observed in the vaccine cohort compared with 44 expected.
Conclusions
Among recipients of ChAdOx1-S, increased rates of venous thromboembolic events, including cerebral venous thrombosis, were observed. For the remaining safety outcomes, results were largely reassuring, with slightly higher rates of thrombocytopenia/coagulation disorders and bleeding, which could be influenced by increased surveillance of vaccine recipients. The absolute risks of venous thromboembolic events were, however, small, and the findings should be interpreted in the light of the proven beneficial effects of the vaccine, the context of the given country, and the limitations to the generalisability of the study findings.
Introduction
As of early April 2021, the covid-19 pandemic has affected more than 130 million people worldwide and 2.8 million have died.1 Vaccines represent the most powerful tool for controlling the pandemic.2 Currently, four vaccines are approved for use against covid-19 in the European Union and these are manufactured by Pfizer-BioNTech (Comirnaty),3 Moderna,4 Oxford-AstraZeneca (Vaxzevria),5 6 and, most recently, Janssen.7 In large randomised controlled trials, these vaccines have shown 66% to 95% efficacy against symptomatic covid-19.3 4 5 6
During early to mid-March 2021, vaccination against covid-19 with the Oxford-AstraZeneca vaccine ChAdOx1-S was paused in several European countries because of spontaneous reports of severe and sometimes fatal thromboembolic events among vaccinated people.8 According to a statement from the European Medicines Agency, 30 cases of predominantly venous thromboembolic events had been reported by 10 March 2021 among the approximately five million recipients of ChAdOx1-S in Europe at the time.8
The EMA subsequently stated that “The number of thromboembolic events in vaccinated people is no higher than the number seen in the general population.”9 Adverse events might, however, be substantially underestimated if based only on spontaneous adverse event reporting. Moreover, since early March 2021, an increasing number of case reports from Austria, Norway, Denmark, Germany, the United Kingdom, and other countries has suggested a potentially distinct thrombotic syndrome associated with ChAdOx1-S.10 11 12 13 These reports have described severe thrombocytopenia, bleeding, arterial thrombosis, and venous thrombosis in unusual anatomical locations (cerebral venous sinus thrombosis, or thrombosis in the portal, splanchnic, or hepatic veins) but also lower limb venous thrombosis or pulmonary embolism in some patients, occurring within five to 24 days after vaccination.14 Whether these cases represent an excess over the expected rate is yet to be established. The risk of such adverse effects also remains unknown, as rare events are not identified in even large clinical trials and adverse effects are often underreported during post-marketing surveillance. Given the ongoing covid-19 pandemic and the current shortage of vaccines, it is crucially important to assess risks with covid-19 vaccines in real world settings.
The objective of the current collaboration between scientific centres in Denmark and Norway was to assess nationwide rates of cardiovascular and haemostatic events after vaccination with ChAdOx1-S and to compare these rates with corresponding age and sex standardised rates in the general populations of the two countries.
Methods
Data sources
We obtained data from Danish healthcare registries through an accelerated process involving registry agencies and national health and data protection authorities. The emergency preparedness register for covid-19 (Beredt C19) in Norway supplied Norwegian data.15 Beredt C19 includes information already collected by healthcare services, national health registries, and medical quality registers. Government funded healthcare systems in Scandinavian countries provide all legal residents with free access to healthcare.16 17 The national health registries of these countries contain prospectively collected health information on all residents, with civil personal registration numbers, permitting individual level data linkage among national registries.18
The study was conducted according to the ethical and legal requirements of each country.19 Owing to data privacy regulations, no cell counts below five could be reported.
Study cohorts
The vaccine cohorts consisted of all people aged 18-65 years in Denmark and Norway who received a first vaccination with ChAdOx1-S from 9 February 2021 to 11 March 2021 (the date the Danish and Norwegian vaccination programmes were halted owing to safety concerns). We excluded vaccine recipients younger than 18 years and older than 65 years and those who immigrated to the countries within 365 days before their first vaccination (ascertained from the civil registration systems in the two countries). The general populations aged 18-65 years in Denmark during 2016-18 and in Norway during 2018-19 served as prespecified comparator cohorts.
Vaccination against covid-19
The Danish vaccination register20 and the corresponding Norwegian immunisation registry SYSVAK21 provided the dates on which all members of the study cohorts received their first dose of ChAdOx1-S. The vaccine was authorised conditionally across the EU on 29 January 202122 and launched in Denmark, Norway, and other European countries shortly after. In Denmark, Norway, and many other European countries, ChAdOx1-S has been administered almost entirely to those younger than 65 years. In accordance with the Danish and Norwegian covid-19 vaccination strategies, the majority of ChAdOx1-S recipients were healthcare and social service workers.
Cardiovascular and haemostatic events
To obtain data on all inpatient stays and hospital outpatient clinic contacts (including emergency room visits), we accessed the national patient registers in Denmark and Norway (covering all hospitals). These registers contain doctor recorded diagnoses for each hospital contact according to ICD-10 (international classification of diseases, 10th revision).16 17 23 24 We assessed rates of hospital contacts for a range of prespecified cardiovascular and haemostatic diagnoses, grouped as arterial events, venous thromboembolism, thrombocytopenia/coagulation disorders, and bleeding events (see supplementary file for ICD-10 codes).
In analyses of individual outcomes, we excluded people from the vaccinated cohorts who had a history of that specific outcome during the 365 days before their first vaccination. For the general population cohorts, we similarly excluded people with a history of a given outcome during a one year fixed washout period from calculations of rates of specific outcomes. Individual outcomes were considered independently—for example, those with a recent history of stroke were not excluded from estimates of the age and sex specific rate of pulmonary embolism.
Statistical analyses
The observed number of incident events in the vaccinated cohorts was obtained by following the cohorts starting on the date of first vaccination for up to 28 days or until the date of death, emigration, the event of interest, or end of data availability (31 March 2021), whichever occurred first.
The expected number of events in the vaccinated cohorts was estimated based on the incidence rates of the given outcomes in the prespecified general population cohorts. These incidence rates were estimated from data for the general population aged 18-65 during 2016-18 in Denmark and during 2018-19 in Norway, with rates calculated stratified by sex and age in five year bands (18-24, 25-29, 30-34, 35-39, 40-44, 45-49, 50-54, 55-59, and 60-65, ascertained at the midpoints of the reference periods). The general population cohorts were followed for incident hospital contacts for the individual outcomes from 1 January 2016 to 31 December 2018 (Denmark) or 1 January 2018 to 31 December 2019 (Norway), emigration, death, or occurrence of the outcome in question, whichever came first. From these general population incidence rates, we estimated the expected number of events in the vaccinated cohort for each of the individual outcomes using indirect standardisation. Specifically, we multiplied the age, sex, and country specific general population incidence rate with the age, sex, and country specific follow-up time accumulated in the vaccinated cohorts for up to 28 days after vaccination. For each age, sex, and country specific stratum of the vaccine recipients, this yielded a count for the number of expected events, which we then summed across stratums. In this way, we obtained the expected number of outcomes that we would observe in the vaccinated cohort members if they had the same rate of outcomes as the general population, when taking into account age, sex, and country.
For each of the prespecified individual outcomes and for groups of outcomes, we calculated the Danish and Norwegian general population incidence rates, the observed and expected number of events, and the differences per 100 000 vaccine recipients followed for 28 days: excess events (standardised morbidity differences) per 100 000 vaccinations and standardised morbidity ratios. We obtained exact 95% confidence intervals for both from the Poisson distribution.25
Supplementary analyses
We conducted a range of prespecified supplementary analyses. Firstly, to investigate subgroup effects, we stratified the analyses by sex as well as by young versus middle aged adults (age categories 18-44 years and 45-65 years). Secondly, to focus specifically on early outcomes that could be more likely due to vaccination, we conducted an analysis with follow-up restricted to 14 days. Thirdly, to investigate the potential effect of heightened diagnostic awareness and thus inclusion of less serious events associated with brief hospital contacts among vaccine recipients, as well as the risk of incorrect coding or rule-out diagnoses from such brief contacts being counted as actual outcomes, we restricted the assessment of events to hospital contacts with a duration five hours or more. Finally, to assess whether use of a historical general population comparator cohort influenced the results, we used a general population cohort followed from 1 January 2020 to 15 March 2021 in both countries.
Public and patient involvement
No patients were involved in the design, execution, or interpretation of this study. Owing to both the urgency and the sensitivity of the study question, as well data privacy constraints, it was not possible to involve members of the public in the study.
Results
Among 282 572 people vaccinated against covid-19 with ChAdOx1-S in Denmark and Norway from February 2021 to 11 March 2021, 1308 (0.5%) were excluded owing to age (<18 years or >65 years) or recent immigration. The final vaccinated cohorts included 281 264 people: 148 792 in Denmark (median age 45 (interquartile range 33-55) years; 80.1% women), and 132 472 in Norway (44 (32-55); 77.6% women, table 1). Full 28 day follow-up was available for 206 894 people (73.6%) in the final cohorts. Among the remaining 74 370 people (26.4%) with fewer than 28 days of available follow-up, median available follow-up was 24 (interquartile range 23-26) days in Denmark and 23 (22-24) days in Norway.
Table 1.
Baseline characteristics of 281 264 study participants aged 18-65 years who received the Oxford-AstraZeneca vaccine against covid-19 (ChAdOx1) in Denmark and Norway
| Characteristics | Denmark (n=148 792) | Norway (n=132 472) |
|---|---|---|
| Women | 119 119 (80.1) | 102 848 (77.6) |
| Median (interquartile range) age (years): | 45 (33-55) | 44 (32-55) |
| 18-24 | 13 731 (9.2) | 13 092 (9.9) |
| 25-29 | 13 784 (9.3) | 12 704 (9.6) |
| 30-34 | 12 774 (8.6) | 13 002 (9.8) |
| 35-39 | 13 968 (9.4) | 13 199 (10.0) |
| 40-44 | 17 134 (11.5) | 14 365 (10.8) |
| 45-49 | 19 827 (13.3) | 15 582 (11.8) |
| 50-54 | 19 629 (13.2) | 15 916 (12.0) |
| 55-59 | 21 027 (14.1) | 17 630 (13.3) |
| 60-65 | 16 918 (11.4) | 16 982 (12.8) |
| Month vaccinated: | ||
| February 2021 | 84 359 (56.7) | 53 678 (40.5) |
| March 2021 | 64 433 (43.3) | 78 794 (59.5) |
Main analysis
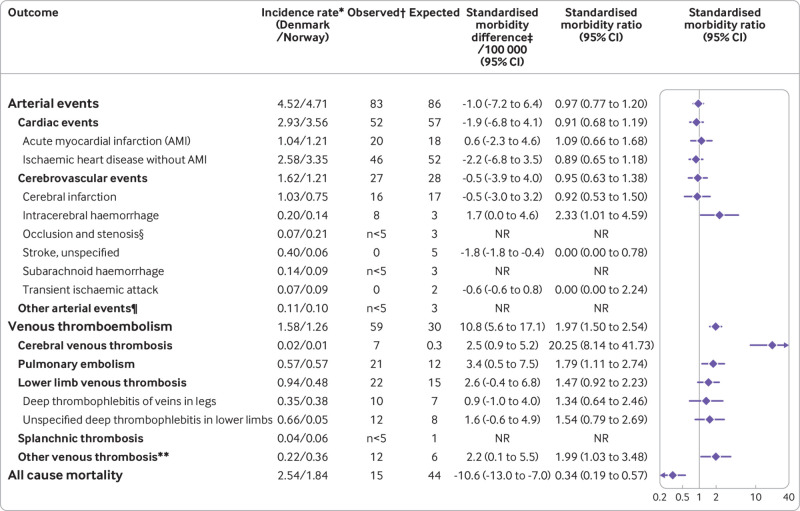
Arterial events—83 arterial events were observed versus 86 expected, corresponding to a standardised morbidity ratio of 0.97 (95% confidence interval 0.77 to 1.20, fig 1). Within the arterial events group, the rate of intracerebral haemorrhage was increased, with a standardised morbidity ratio of 2.33 (1.01 to 4.59), corresponding to 1.7 (95% confidence interval 0.0 to 4.6) excess events per 100 000 vaccinations.
Fig 1.
General population incidence rates, observed and expected counts of events, excess events per 100 000 vaccinations, and standardised morbidity ratios of arterial events, venous thromboembolism, and all cause mortality within 28 days of vaccination in a cohort of 18-65 year old Danish and Norwegian people (n=281 264) receiving their first dose of the Oxford-AstraZeneca vaccine (ChAdOx1-S). NR=not reported owing to privacy regulations. *Per 1000 person years in the general population. †Observed events are not mutually exclusive (ie, one patient can contribute to two different third level outcomes. However, two different third level outcomes would only count once towards a common second level outcome, and similarly only once in a first level outcome). ‡Expected events based on incidence rates in the general population. §Full name: Occlusion and stenosis of precerebral or cerebral arteries, not resulting in cerebral infarction. ¶Including angiitis hypersensitiva, angiitis hypersensitiva with Schönlein-Henochs purpura, Buerger’s syndrome, Goodpasture syndrome, microangiopathia thrombotica, other necrotising vasculitis, and thrombotic thrombocytopenic purpura. **Including embolism and thrombosis in non-specified veins, embolism and thrombosis in other specified veins, and embolism and thrombosis of caval vein
Venous thromboembolism—59 venous thromboembolic events were observed versus 30 expected, corresponding to a standardised morbidity ratio of 1.97 (1.50 to 2.54) and to 11 (5.6 to 17.0) excess events per 100 000 vaccinations (fig 1). An increase was also found for several subgroups, including pulmonary embolism (standardised morbidity ratio 1.79 (1.11 to 2.74); 3.4 (0.5 to 7.5) excess events per 100 000 vaccinations), lower limb venous thrombosis (1.47 (0.92 to 2.23); 2.6 (−0.4 to 6.8) excess events per 100 000 vaccinations), and other venous thrombosis (1.99 (1.03 to 3.48); 2.2 (0.1 to 5.5) excess events per 100 000 vaccinations). The standardised morbidity ratio for cerebral venous thrombosis was 20.25 (8.14 to 41.73) corresponding to 7 observed events versus 0.3 expected and an excess of 2.5 (0.9 to 5.2) events per 100 000 vaccinations.
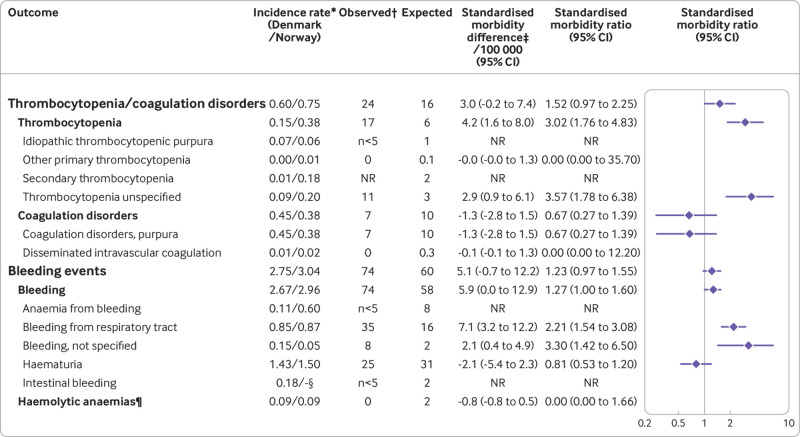
Any thrombocytopenia/coagulation disorder—the standardised morbidity ratio for any thrombocytopenia/coagulation disorder was 1.52 (0.97 to 2.25), corresponding to 3.0 (−0.2 to 7.4) excess events per 100 000 vaccinations (fig 2). This was driven by unspecified thrombocytopenia with a standardised morbidity ratio of 3.57 (1.78 to 6.38), corresponding to 2.9 (0.9 to 6.1) excess events per 100 000 vaccinations.
Fig 2.
General population incidence rates, observed and expected counts of events, excess events per 100 000 vaccinations, and standardised morbidity ratios of thrombocytopenia/coagulation disorders and bleeding events within 28 days of vaccination in a cohort of 18-65 year old Danish and Norwegian people (n=281 264) receiving their first dose of the Oxford-AstraZeneca covid-19 vaccine (ChAdOx1-S). NR=not reported owing to privacy regulations. *Per 1000 person years in the general population. †Observed events are not mutually exclusive (ie, one patient can contribute to two different third level outcomes. However, two different third level outcomes would only count once towards a common second level outcome, and similarly only once in a first level outcome). ‡Expected events based on incidence rates in the general population. §Not available in the Norwegian data source. ¶Including haemolytic anaemia, haemolytic uraemic syndrome, and paroxysmal nocturnal haemoglobinuria
Any bleeding—the standardised morbidity ratio for any bleeding was 1.23 (0.97 to 1.55), corresponding to 5.1 (−0.7 to 12.2) excess events per 100 000 vaccinations (fig 2). This included a standardised morbidity ratio of 2.21 (1.54 to 3.08) for bleeding from the respiratory tract (eg, epistaxis and haemoptysis), corresponding to 7.1 (3.2 to 12.2) excess events per 100 000 vaccinations; and 3.30 (1.42 to 6.50) for unspecified bleeding, corresponding to 2.1 (0.4 to 4.9) excess events per 100 000 vaccinations.
Deaths—15 deaths were observed in the vaccinated cohort compared with 44 expected deaths based on the general population mortality rates, corresponding to a standardised morbidity ratio of 0.34 (0.19 to 0.57).
Supplementary analyses
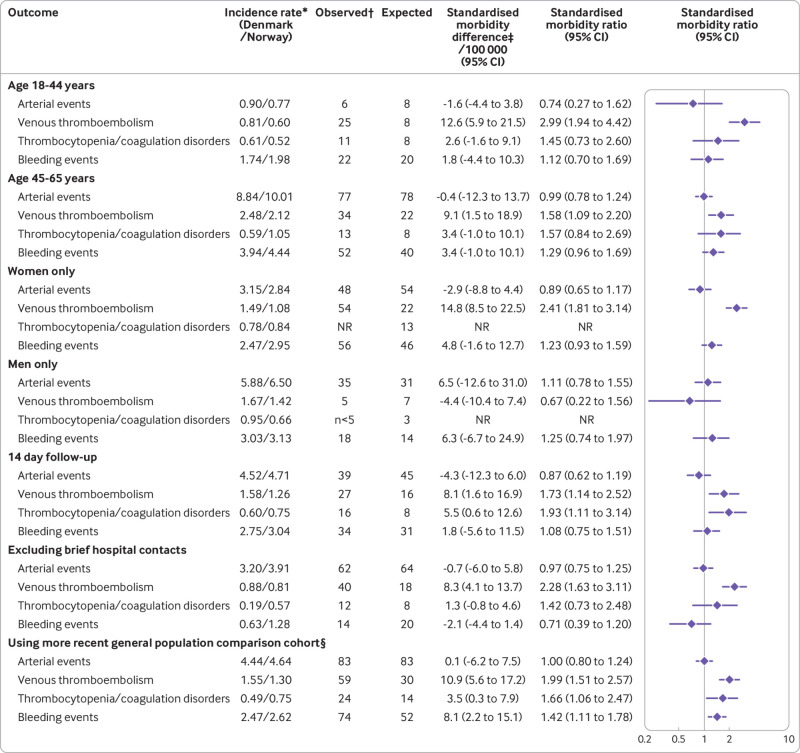
Figure 3 presents the results from the prespecified supplementary analyses. Standardised morbidity ratio estimates were generally similar among those aged 18-44 years compared with those aged 45-65 years, with the exception of venous thromboembolism: 2.99 (1.94 to 4.42) among those aged 18-44 years versus 1.58 (1.09 to 2.20) among those aged 45-65 years, corresponding to a slightly higher absolute excess rate of events in the younger group (13 excess events per 100 000 vaccinations among those aged 18-44 years v 9 excess events per 100 000 vaccinations among those aged 45-65 years). When the analysis was restricted to women, no excess rate of thrombocytopenia/coagulation disorders was observed, whereas other estimates were largely unaltered. When restricting to men, no excess rate of venous thromboembolism was observed: standardised morbidity ratio 0.67 (0.22 to 1.56); the results were, however, imprecise. When the analysis was restricted to 14 day follow-up, the standardised morbidity ratio for thrombocytopenia/coagulation disorders increased to 1.93 (1.11 to 3.14), whereas no excess rate of bleeding was observed. When hospital contacts of less than five hours were excluded from the analysis, results for venous thromboembolism remained unchanged, whereas no excess bleeding events were observed, and the excess events of thrombocytopenia/coagulation disorders was diminished (to 1.3 (−0.8 to 4.6) excess events per 100 000 vaccinations). Using the more recent general population comparison cohort (2020-21), nearly identical general population rates were found for all outcomes, and as such effect estimates remained virtually unchanged (for full results see supplementary tables 1 and 2).
Fig 3.
Results from supplementary analyses restricted to subgroups of patients on sex, and age, shorter follow-up, and excluding brief hospital contacts. NR=not reported owing to privacy regulations. *Per 1000 person years in the general population. †Observed events are not mutually exclusive (ie, one patient can contribute to two different third level outcomes. However, two different third level outcomes would only count once towards a common second level outcome, and similarly only once in a first level outcome). ‡Expected events based on incidence rates in the general population. §The general population comparison cohort was followed from January 2020 through March 2021 in both countries
Post hoc analyses
Firstly, to investigate whether signals for venous thromboembolism or cerebral venous thrombosis could be explained by unmeasured confounding from use of systemic hormone therapy, the proportion of women were quantified in the Danish vaccinated cohort who redeemed a prescription for systemic hormone therapy (oral contraceptives or estradiol) during the year before cohort entry as well as in the general population comparator cohort. This showed that women who received ChAdOx1-S were on average using systemic hormone therapy slightly less often than the background population (see supplementary table 3). Secondly, E-values were calculated for the outcomes of venous thromboembolism and cerebral venous thrombosis—these represent the minimum magnitude of association that an unmeasured confounder needs to have with both the exposure and the outcome to move the estimate so that the lower boundary of the 95% confidence interval includes unity.26 This yielded E-values of 2.37 for venous thromboembolism and 15.8 for cerebral venous thrombosis. Thirdly, to provide more clarity on the estimation of the expected counts and to investigate whether incidence rates in the background population were stable over time, yearly incidence rates were calculated for 2016-18 in Denmark, 2018-19 in Norway, and 2020-21 in both countries. This showed generally stable incidence rates over time in both countries for all outcomes (see supplementary tables 4-7). Fourthly, to investigate the potential influence from either previous or concomitant SARS-CoV-2 infection, the proportion of vaccine recipients with any positive test result for covid-19 before vaccination was identified (6.2% in Denmark and 1.4% in Norway). When these people were excluded from the analysis, the estimates for both overall venous thromboembolic events, and specifically cerebral venous thrombosis, remained virtually unchanged (data not shown owing to low counts conflicting with data privacy regulations). When the follow-up of vaccine recipients was further censored on a positive covid-19 test result after vaccination, which occurred for 0.24% (n=643) of the combined cohorts, results remained unchanged (data not shown). Finally, to contextualise the study findings of a cerebral venous thrombosis signal, the 28 day risk of cerebral venous thrombosis after a positive covid-19 test result was assessed for Denmark and Norway, using complete nationwide data on SARS-CoV-2 polymerase chain reaction results until 31 March 2021 from Danish and Norwegian microbiology databases.27 28 Among all 162 222 people with a positive test result between ages 18 and 65 years in Denmark, fewer than five cerebral venous thrombosis events were observed over a 28 day period (precise count not shown owing to data privacy regulations), whereas among 66 721 people aged 18-65 years with a positive test result in Norway, zero cerebral venous thrombosis events were observed.
Discussion
In this large binational cohort study of recipients of the Oxford-AstraZeneca covid 19 vaccine (ChAdOx1-S) aged 18-65 years, results were reassuring for most cardiovascular and haemostatic outcomes. We did, however, observe an increased rate of venous thromboembolic events, corresponding to 11 excess venous thromboembolic events per 100 000 vaccinations and including a clearly increased rate of cerebral venous thrombosis with 7 observed events versus 0.3 expected events among the 282 572 vaccine recipients (excess of 2.5 per 100 000 vaccinations, or one in 40 000 vaccine recipients). Conversely, we observed no increase in the rate of overall arterial events. We observed a slight increase in the rate of thrombocytopenia/coagulation disorders and bleeding, which was, however, attenuated after excluding brief hospital contacts (<5 hours) from the analysis.
Strengths and limitations of this study
The main strength of our study is its true population based approach, implemented in a setting with national health services providing free access to healthcare and with well defined and near complete follow-up based on computerised registries with full population coverage and daily updates.
The study also has potential weaknesses. The validity of our findings depends ultimately on the accurate coding of outcomes. The complex clinical syndrome reported with ChAdOx1-S is not captured completely by any single ICD-10 code. Instead, clinicians are likely to use the codes that reflect the dominant elements in individual patients’ presentation. A general lack of specificity of the outcome diagnoses would reduce the strength of any potential associations. However, from early March the increased focus on the adverse events being examined might have heightened clinical awareness, and therefore the level of reported diagnoses, above those documented in our reference populations. This is probably mainly a concern for less serious adverse events (eg, epistaxis, mild thrombocytopenia) that otherwise could have gone undetected, as these do not necessarily lead to a hospital contact. This finding is supported by the results of the supplementary analysis excluding brief hospital contacts, in which the signal for bleeding events was removed, and the association for thrombocytopenia/coagulation disorders was diminished (on an absolute scale), whereas the observed signal for venous thromboembolic events, which are generally more serious, remained largely unchanged. Another limitation is that our expected counts of outcomes were based on the general population of each country. Active healthcare and social services workers—the primary recipients of ChAdOx1-S in Denmark and Norway—are likely to be healthier than the average population of the same age.29 To the extent that better health decreases the risk of the studied outcomes, this will lead to falsely low estimated standardised morbidity ratios—that is, make the vaccine appear safer—and thus could not explain the safety signals observed in our study. A healthy vaccinee effect is expected to be particularly pronounced for all cause mortality,30 as people with severe comorbidity or known terminal illness in Denmark and Norway will generally not have received ChAdOx1-S. Moreover, the vaccine is not administered to people who report acute illness on the planned vaccination date. These bias mechanisms are the most likely explanation for the observed low count for deaths in our study and hinders meaningful interpretation of the reported all cause mortality effects of receiving the vaccine. Furthermore, if known risk factors for venous thromboembolism were more prevalent among vaccine recipients than in the general population this might have led to falsely increased standardised morbidity ratios. This could include risk factors such as female sex, use of oral contraceptives, use of menopausal hormone therapy, and recent surgery or trauma or other immobilisation.31 Our event rates were, however, standardised for any differences in sex and age, and use of systemic hormone therapy was not higher in our vaccine recipients than in the general population, and surgery or immobilisation is unlikely to be increased in members of the active work force. Similarly, as also observed in our post hoc analyses, any increase in observed venous thromboembolic events was unlikely to be explained by SARS-CoV-2 infections occurring in vaccinated people, as both the prevalence of covid-19 and the associated absolute risk of thromboembolic events was low in our setting.32 Our post hoc confounder analysis (E-values) suggested that our findings were unlikely to be explained by unmeasured confounders. Nevertheless, residual confounding from other factors cannot be ruled out owing to the non-randomised observational design of our study. Lastly, important boundaries exist as to the generalisability of our study findings. Firstly, as our study was restricted to people aged 18-65 years, it cannot inform evaluations of the safety of ChAdOx1-S in older people. Similarly, data were only available for those who received their first dose of the vaccine, and as such do not provide information on the safety of the second dose. Finally, the study was conducted in two Scandinavian countries and therefore the results might not be generalisable to populations of predominantly non-white ethnicities.
Comparison with other studies
Specific immune mediated mechanisms might contribute to the increased risk of venous thromboembolism after vaccination with ChAdOx1-S. This is currently under investigation. Reports in the New England Journal of Medicine by now have described three detailed case series of 39 patients (5 in Norway,10 11 in Germany and Austria,11 and 23 in the UK 12) who presented with thrombocytopenia and thrombosis beginning five to 24 days after vaccination with ChAdOx1-S. Another case was reviewed in Denmark.13 Among these 40 patients, 35 (88%) experienced any venous thrombosis, including a high proportion (26 patients, 65%) who experienced cerebral venous thrombosis, whereas 6 (15%) had splanchnic thrombosis and 7 (18%) pulmonary embolism, with multiple embolisms being common. This is now collectively referred to as vaccine induced thrombotic thrombocytopenia (VITT) or thrombosis with thrombocytopenia syndrome (TTS), with a suggested potential mechanism involving platelet activating antibodies directed against platelet factor 4, which are known to be triggered by heparin and sometimes other environmental factors.33 As of yet, no individual level risk factors for vaccine induced thrombotic thrombocytopenia or thrombosis with thrombocytopenia syndrome have been confirmed,14 with previously reported cases among both, for example, men and women and among users and non-users of hormone therapy.10 11 12 13 To the extent that the excess rate of venous thrombosis events reported in this manuscript is associated with vaccine induced thrombotic thrombocytopenia or thrombosis with thrombocytopenia syndrome, our study has insufficient data, and it is not designed to identify subgroups at particular risk, which constitutes an important area for further research.14 Importantly, whether this safety concern is specific to ChAdOx1-S or whether it is associated with either all adenovirus vector based covid-19 vaccines or even all covid-19 vaccines, is an important issue that remains to be elucidated. The European Medicines Agency recently raised “embolic and thrombotic events” as a new signal for the adenovirus vector based vaccine from Janssen,34 and its use was put on temporary hold by the Centers for Disease Control and Prevention and the Food and Drug Administration in the United States while further investigations were ongoing.14
Policy implications
The regulatory implications of our study findings are complex. Given ChAdOx1-S’s nearly 70% protection against a potentially lethal infection,5 6 the risk to benefit ratio of the vaccine in a pandemic scenario and on a population level is likely to remain favourable. From a public health perspective, multiple factors should be considered, including regional availability of other vaccines, capacity of the local healthcare system, delays in reaching the desired level of herd immunity, regional control of the epidemic through other measures, and the importance of trust in authorities and confidence in the vaccination programme. Many of these factors directly influence the benefit of receiving a covid-19 vaccine, at both the societal and the individual level. Furthermore, the applicability of our findings to a given context needs to consider the limitations to the study’s generalisability. Thus, vaccine recommendations must be context dependent and country specific. In any case, access to valid data on the magnitude of risk is essential. Such information must be made available and continuously updated for all covid-19 vaccines in the real world setting—ideally including studies that provide direct head-to-head comparisons of vaccines on both safety and efficacy, which constitutes an important area for further study.
Conclusions
Our study provides evidence of an excess rate of venous thromboembolism, including cerebral venous thrombosis, among recipients of the Oxford-AstraZeneca covid-19 vaccine ChAdOx1-S within 28 days of the first dose. The absolute risks of these events were, however, small. For the remaining safety outcomes, results were reassuring, with slightly higher rates of thrombocytopenia/coagulation disorders and bleeding, which could be influenced by heightened surveillance. The absolute risks described in this study are small in the context of the proven benefits of vaccination against covid-19, and the globally high incidence of serious cases of SARS-CoV-2 infection.
What is already known on this topic
Spontaneous adverse event reports and clinical case series have described thrombocytopenia, bleeding, and arterial and venous thromboses occurring within days to weeks after vaccination with the Oxford-AstraZeneca covid-19 vaccine (ChAdOx1-S)
Whether these cases represent excess events above expected rates is unknown
What this study adds
Increased rates for venous thromboembolism were observed within 28 days of vaccination with ChAdOx1-S in Denmark and Norway, corresponding to 11 excess events per 100 000 vaccinations, including 2.5 excess cerebral venous thrombosis events per 100 000 vaccinations
Results were largely reassuring for arterial events, whereas slightly increased rates of thrombocytopenia or coagulation disorders and bleeding in the vaccinated group could be influenced by heightened surveillance
Absolute risks of events were small and should be interpreted in the context of the benefits of covid-19 vaccination at both the societal and the individual level
Web extra.
Extra material supplied by authors
Web appendix: Supplementary material
Contributors: AP, LCL, MA, JH, ØL, AM, LP, HTS, RWT, and AH designed the study. AP, LCL, JD, ØK, GT, PLDR, and LP processed the collected data. AP and JH directed the analyses, which were carried out by LCL, GT, JD, ØK, and LP. All authors participated in the discussion and interpretation of the results. AP, JH, ØL, HTS, and RWT organised the writing and wrote the initial draft. All authors critically revised the manuscript for intellectual content and approved the final version. AP and AH are the guarantors. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: None.
Competing interests: All authors have completed the ICMJE uniform disclosure form at http://www.icmje.org/coi_disclosure.pdf and declare: no support from any organisation for the submitted work. The authors report no personal conflicts of interest pertaining to this work. The Department of Clinical Epidemiology, Aarhus University Hospital, receives funding for other studies from the European Medicines Agency and companies in the form of research grants to (and administered by) Aarhus University. None of these studies have any relation to the present study. AP, JH, and LCL report participation in research projects funded by Alcon, Almirall, Astellas, AstraZeneca, Boehringer-Ingelheim, Novo Nordisk, Servier, Menarini Pharmaceuticals, and LEO Pharma, all regulator mandated phase IV studies, all with funds paid to their institution (no personal fees) and with no relation to the work reported in this paper. ØK reports participation in research projects funded by Novo Nordisk and LEO Pharma, all regulator mandated phase IV studies, all with funds paid to his institution (no personal fees) and with no relation to the work reported in this paper. HLG reports previous participation in research projects and clinical trials funded by Novo Nordisk, GSK, AstraZeneca, and Boheringer-Ingelheim, all paid to her previous institution Oslo University Hospital (no personal fees). MA has previously participated in research projects funded by Pfizer, Janssen, AstraZeneca, H Lundbeck & Mertz, and Novartis with grants received by Karolinska Institutet (no personal fees). MA has personally received fees for teaching from Atrium, the Danish Association of the Pharmaceutical Industry. The Pharmacovigilance Research Center is supported by a grant from the Novo Nordisk Foundation (NNF15SA0018404) to the University of Copenhagen.
Ethical approval: According to Danish law, studies based entirely on registry data do not require approval from an ethics review board. However, the Danish analysis was registered at the repository of the University of Southern Denmark (11.346), and data access was approved by the Danish Health Data Authority (FSEID-00005646). In Norway, the emergency preparedness register was established according to the Health Preparedness Act §2-4 and the study also was approved by the Norwegian Regional Committee for Research Ethics (REK Sør-Øst A, ref 122745).
Data sharing: No additional data available. For legal and ethical reasons, individual level patient data cannot be shared by the authors and are only accessible to authorised researchers after application to the Danish Health Data Authority, or in Norway after ethical approval and application to helsedata.no administered by the Directorate of eHealth.
The lead author (AP) affirms the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Dissemination to participants and related patient and public communities: Dissemination to study participants is not possible. However, study findings will be disseminated to both Danish, Norwegian, and international regulators.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.World Health Organization. COVID-19 Weekly Epidemiological Update. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
- 2. Darby AC, Hiscox JA. Covid-19: variants and vaccination. BMJ 2021;372:n771. 10.1136/bmj.n771 [DOI] [PubMed] [Google Scholar]
- 3. Polack FP, Thomas SJ, Kitchin N, et al. C4591001 Clinical Trial Group . Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. N Engl J Med 2020;383:2603-15. 10.1056/NEJMoa2034577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Baden LR, El Sahly HM, Essink B, et al. COVE Study Group . Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine. N Engl J Med 2021;384:403-16. 10.1056/NEJMoa2035389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Voysey M, Clemens SAC, Madhi SA, et al. Oxford COVID Vaccine Trial Group . Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet 2021;397:99-111. 10.1016/S0140-6736(20)32661-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Voysey M, Costa Clemens SA, Madhi SA, et al. Oxford COVID Vaccine Trial Group . Single-dose administration and the influence of the timing of the booster dose on immunogenicity and efficacy of ChAdOx1 nCoV-19 (AZD1222) vaccine: a pooled analysis of four randomised trials. Lancet 2021;397:881-91. 10.1016/S0140-6736(21)00432-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.European Medicines Agency (EMA). EMA assessment report EMA/158424/2021. https://www.ema.europa.eu/en/documents/assessment-report/covid-19-vaccine-janssen-epar-public-assessment-report_en.pdf.
- 8. Wise J. Covid-19: European countries suspend use of Oxford-AstraZeneca vaccine after reports of blood clots. BMJ 2021;372:n699. 10.1136/bmj.n699 [DOI] [PubMed] [Google Scholar]
- 9.European Medicines Agency (EMA). COVID-19 Vaccine AstraZeneca: PRAC investigating cases of thromboembolic events - vaccine’s benefits currently still outweigh risks - Update. https://www.ema.europa.eu/en/news/covid-19-vaccine-astrazeneca-prac-investigating-cases-thromboembolic-events-vaccines-benefits.
- 10. Schultz NH, Sørvoll IH, Michelsen AE, et al. Thrombosis and Thrombocytopenia after ChAdOx1 nCoV-19 Vaccination. N Engl J Med 2021. 10.1056/NEJMoa2104882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Greinacher A, Thiele T, Warkentin TE, Weisser K, Kyrle PA, Eichinger S. Thrombotic Thrombocytopenia after ChAdOx1 nCov-19 Vaccination. N Engl J Med 2021. 10.1056/NEJMoa2104840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Scully M, Singh D, Lown R, et al. Pathologic Antibodies to Platelet Factor 4 after ChAdOx1 nCoV-19 Vaccination. N Engl J Med 2021. 10.1056/NEJMoa2105385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Blauenfeldt RA, Kristensen SR, Ernstsen SL, Kristensen CCH, Simonsen CZ, Hvas AM. Thrombocytopenia with acute ischemic stroke and bleeding in a patient newly vaccinated with an adenoviral vector-based COVID-19 vaccine. J Thromb Haemost 2021. 10.1111/jth.15347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cines DB, Bussel JB. SARS-CoV-2 Vaccine-Induced Immune Thrombotic Thrombocytopenia. N Engl J Med 2021. 10.1056/NEJMe2106315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Folkehelseinstituttet [Norwegian Institute of Public Health]. Emergency preparedness register for COVID-19 (Beredt C19). https://www.fhi.no/en/id/infectious-diseases/coronavirus/emergency-preparedness-register-for-covid-19/.
- 16. Furu K, Wettermark B, Andersen M, Martikainen JE, Almarsdottir AB, Sørensen HT. The Nordic countries as a cohort for pharmacoepidemiological research. Basic Clin Pharmacol Toxicol 2010;106:86-94. 10.1111/j.1742-7843.2009.00494.x [DOI] [PubMed] [Google Scholar]
- 17. Schmidt M, Schmidt SAJ, Adelborg K, et al. The Danish health care system and epidemiological research: from health care contacts to database records. Clin Epidemiol 2019;11:563-91. 10.2147/CLEP.S179083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Schmidt M, Pedersen L, Sørensen HT. The Danish Civil Registration System as a tool in epidemiology. Eur J Epidemiol 2014;29:541-9. 10.1007/s10654-014-9930-3 [DOI] [PubMed] [Google Scholar]
- 19. Ludvigsson JF, Håberg SE, Knudsen GP, et al. Ethical aspects of registry-based research in the Nordic countries. Clin Epidemiol 2015;7:491-508. 10.2147/CLEP.S90589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Grove Krause T, Jakobsen S, Haarh M, Mølbak K. The Danish vaccination register. Euro Surveill 2012;17:20155. 10.2807/ese.17.17.20155-en [DOI] [PubMed] [Google Scholar]
- 21. Trogstad L, Ung G, Hagerup-Jenssen M, Cappelen I, Haugen IL, Feiring B. The Norwegian immunisation register--SYSVAK. Euro Surveill 2012;17:17. 10.2807/ese.17.16.20147-en [DOI] [PubMed] [Google Scholar]
- 22.European Medicines Agency (EMA). EMA assessment report EMA/94907/2021. https://www.ema.europa.eu/en/documents/assessment-report/vaxzevria-previously-covid-19-vaccine-astrazeneca-epar-public-assessment-report_en.pdf.
- 23. Bakken IJ, Ariansen AMS, Knudsen GP, Johansen KI, Vollset SE. The Norwegian Patient Registry and the Norwegian Registry for Primary Health Care: Research potential of two nationwide health-care registries. Scand J Public Health 2020;48:49-55. 10.1177/1403494819859737 [DOI] [PubMed] [Google Scholar]
- 24. Schmidt M, Schmidt SAJ, Sandegaard JL, Ehrenstein V, Pedersen L, Sørensen HT. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol 2015;7:449-90. 10.2147/CLEP.S91125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Breslow NE, Day NE. Statistical methods in cancer research. Volume II--The design and analysis of cohort studies. IARC Sci Publ 1987;82:1-406. [PubMed] [Google Scholar]
- 26. VanderWeele TJ, Ding P. Sensitivity Analysis in Observational Research: Introducing the E-Value. Ann Intern Med 2017;167:268-74. 10.7326/M16-2607 [DOI] [PubMed] [Google Scholar]
- 27. Voldstedlund M, Haarh M, Mølbak K, MiBa Board of Representatives . The Danish Microbiology Database (MiBa) 2010 to 2013. Euro Surveill 2014;19:20667. 10.2807/1560-7917.ES2014.19.1.20667 [DOI] [PubMed] [Google Scholar]
- 28. National Microbiology Laboratory Database . https://www.fhi.no/nyheter/2020/nasjonal-laboratoriedatabase-for-covid-19-pa-plass/.
- 29. Thygesen LC, Hvidtfeldt UA, Mikkelsen S, Brønnum-Hansen H. Quantification of the healthy worker effect: a nationwide cohort study among electricians in Denmark. BMC Public Health 2011;11:571. 10.1186/1471-2458-11-571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Jackson LA, Jackson ML, Nelson JC, Neuzil KM, Weiss NS. Evidence of bias in estimates of influenza vaccine effectiveness in seniors. Int J Epidemiol 2006;35:337-44. 10.1093/ije/dyi274 [DOI] [PubMed] [Google Scholar]
- 31. Wolberg AS, Rosendaal FR, Weitz JI, et al. Venous thrombosis. Nat Rev Dis Primers 2015;1:15006. 10.1038/nrdp.2015.6 [DOI] [PubMed] [Google Scholar]
- 32. Dalager-Pedersen M, Lund LC, Mariager T, et al. Venous thromboembolism and major bleeding in patients with COVID-19: A nationwide population-based cohort study. Clin Infect Dis 2021;ciab003. 10.1093/cid/ciab003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Greinacher A, Thiele T, Warkentin TE, Weisser K, Kyrle P, Eichinger S. A Prothrombotic Thrombocytopenic Disorder Resembling Heparin-Induced Thrombocytopenia Following Coronavirus-19 Vaccination. [Preprint] 2021. 10.21203/rs.3.rs-362354/v1 [DOI]
- 34.European Medicines Agency. Pharmacovigilance Risk Assessment Committee (PRAC). Draft agenda for the meeting on 06-09 April 2021. https://www.ema.europa.eu/en/documents/agenda/agenda-prac-draft-agenda-meeting-6-9-april-2021_en.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Web appendix: Supplementary material