Abstract
THE RESUSCITATION OF A PATIENT IN EXTREMIS is frequently characterized by chaos and disorganization, and is one of the most stressful situations in medicine. We reviewed selected studies from the fields of anesthesia, emergency medicine and critical care that address the process of responding to a critically ill patient. Individual clinicians can improve their performance by increased exposure to emergencies during training and by the incorporation of teamwork, communication and crisis resource management principles into existing critical care courses. Team performance may be enhanced by assessing personality factors when selecting personnel for high-stress areas, explicit assignment of roles, ensuring a common “culture” in the team and routine debriefings. Overreliance on technology and instinct at the expense of systematic responses should be avoided. Better training and teamwork may allow for clearer thinking in emergencies, so that knowledge can be translated into effective action and better patient outcomes.
Emergencies are among the most challenging situations in medicine. Consider, for example, what would happen if your next patient suddenly clutched her chest and stopped breathing while you were taking her history. The technical complexity of such situations may vary, but they almost always involve some anxiety for the physician. The need for immediate life-saving treatment not only places demands on clinical skills, but also challenges the physician's character. The combination creates a potent mix that can mark physicians indelibly.
The stress caused by emergencies is unavoidable and inevitable: life sometimes does hang in the balance. The outcome may depend on the cooperation of others and on swift decisions and actions, frequently in the absence of complete information. However, some of the stress may be related to the ways in which physicians and other team members work together. Optimizing teamwork might result in reduced stress and improved outcomes.1,2
Our goal is not to discuss the technical details of specific emergencies but, rather, to describe the process involved in an effective response to occasional, but spectacular, emergencies. Using selected articles from studies of emergency medicine, anesthesia and critical care, we will address the common pitfalls and highlight approaches and interventions that may help diminish the stress inherent in these challenging situations.
Pitfalls at the extremes of disease
Physicians are expected to manage a broad spectrum of disease presentations, from the obvious to the obscure, and from the common to the catastrophic. Yet, with the patient in extremis, the physician's response must be rapidly coordinated with those of other members of the health care team working simultaneously and side by side.2,3 Coordination is not simple and is further complicated because each team member must carry out many tasks simultaneously or in quick succession (Table 1).1,2,3
Table 1
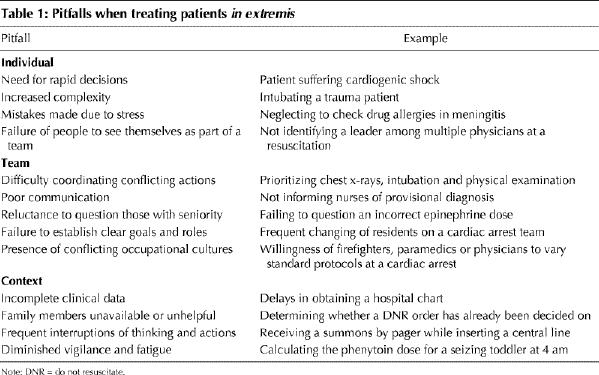
Moreover, a standard task is often more complex during an emergency than under normal circumstances. For example, in a study3 of endotracheal intubation in the setting of a trauma unit, very sick patients were more likely to require urgent intubations. In these situations, standard preparatory steps were omitted more often, monitoring was sacrificed more commonly, and suctioning and bag-valve-mask ventilation were more frequently needed. Urgent intubations were more likely to be classified as “very difficult,” there were more failed attempts and they were carried out in 40% less time than usual.3 The net result is a task that, when urgent, must be carried out faster despite greater technical difficulty and greater clinical uncertainty.
Apart from the increased technical difficulty of standard tasks, the stress inherent in medical crises may independently affect performance. Stress is a common element in emergencies, as shown by a study in which the only highly ranked source of stress resulting from residents' direct clinical duties was the treatment of life-threatening illnesses.4 Studies suggest that stress can impair motor and cognitive functioning,5 though the performance and judgement of physicians in emergencies has not been formally studied. However, among residents, stress has been associated with medical errors6 and inappropriate work behaviours such as absenteeism, mistakes and conflicts.7 Stress may not only affect short-term performance, but it may also have lasting consequences.
Poor communication between team members in the chaotic scene surrounding the critically ill patient only adds to stress.1,8,9 In one study of errors in the intensive care unit,8 communication between physicians and nurses accounted for only 2% of all the activities, yet was responsible for 37% of all the errors. Moreover, 29% of all the errors were judged to be serious enough to potentially cause significant deterioration or death. The situation during an emergency is probably worse, because exchanges of information are more likely to be misunderstood.2,8
Reluctance to question authority may also worsen strained communication between team members. For example, failures of communication account for over 75% of commercial airline accidents and are often attributed to hierarchical barriers that discourage subordinate crew members from giving crucial information to a crew member of higher rank and authority.10 Similar problems occur in operating rooms, where surveys show that surgeons are disinclined to allow the decisions of senior staff to be questioned.1 Given the hierarchical structure of most medical settings, these problems may also affect action and judgement during emergencies.2
Barriers to communicating crucial information may result, in part, from the failure of physicians and other staff to see themselves as part of a team with shared goals and prespecified roles. Instead, they may believe that they constitute an ad hoc collection of people with ill-defined responsibilities and expectations rather than with a common objective and specific tasks.11,12 Such ambiguity concerning professional roles is strongly linked to occupational stress, dissatisfaction and depression in emergency medicine residents.13 This ambiguity can be reduced by clearly defined responsibilities and better peer and work-group support, which are all components of a smoothly functioning team.13
Team support may be hindered, however, by the presence of different occupational cultures,1,9,14 that is, the collective programming of the minds of different professions.14 Different professional styles can exist within the same hospital, operating room or ambulance unit, despite the presence of similar patients. These differences become evident only when representatives of different occupations who are working together on the same task are carefully compared.1,14
One such study14 compared pilots, paramedics and physicians who make up emergency medical service aircrews in Norway. Pilots and paramedics were found to value rules and regulations significantly more highly than did physicians in the same aircrews. Physicians, in contrast, valued ambiguity and flexibility in their work and were significantly more likely than pilots to consider helping other people as their primary professional motivation. This suggests that physicians prefer to alter their approach and their decisions based on the task at hand, rather than to follow protocols, and that the individual motivations of team members may vary. Establishing the rapport necessary for supporting coworkers may be difficult when important differences exist between those coworkers.
Good rapport may be unnecessary when tasks are clearly separated, as in the case of a pilot flying an airplane (when rules are clearly important) and in the case of an anesthetist deciding on an intubation (when flexibility may be necessary). However, major cultural differences may be a hindrance when they affect attitudes toward shared responsibilities. Surveys of operating room physicians and nurses reveal significant differences in preferred styles of leadership and coordination.1 The absence of shared team attitudes may hamper critical care when, for example, the decision to call off an unsuccessful pediatric resuscitation generates tension in the team. Better training in effective teamwork and a common team culture would probably minimize these differences.1,2
The potential for cultural differences to hinder the response to crisis is best illustrated by disasters that require coordinated and rapid actions from hospitals, ambulance, fire and police services, and civil authorities. Many of the same problems that occur in a team attending to a single patient are seen in disasters affecting entire communities. Studies of disasters reveal recurring problems in establishing good communication, integrated command, prioritization of objectives and explicit delegation of tasks,15,16 all of which are relevant when a patient is in extremis.
Many other factors contribute to the stress inherent in emergencies. Clinical information is often incomplete and occasionally erroneous. Retrieval of old records may be delayed. Orders are called out into thin air, without any clearly assigned responsibility for carrying them out. Critical decisions may require the input of family members who are unavailable or overly distraught. Reasoning and action are frequently interrupted, and such interruptions are themselves stressful.17 Finally, the response to emergencies at night may be adversely affected by fatigue and diminished vigilance.18
Adequacy of preparation
Despite team members' technical proficiency, problems in both process and outcome occur during medical crises. Some probably reflect formal training in medical school (Table 2). The traditional academic approach to patients is linear, beginning with the history, which is followed in sequence by examination, testing, diagnosis and treatment. This approach is emphasized in textbooks19 and in bedside teaching, but it has little relevance when a patient is critically ill and all the elements must be carried out simultaneously or even in reverse order.
Table 2
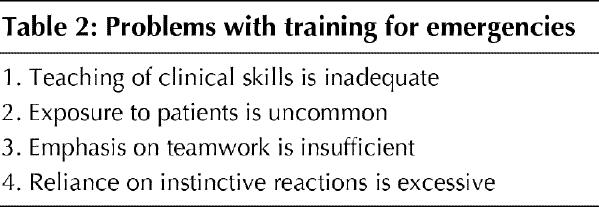
Traditional training may not prepare physicians adequately for emergencies. In one study20 of adverse outcomes in anesthesia, human error was responsible for over 95% of incidents that resulted in serious adverse outcomes; inadequate training was found to be the most commonly associated factor. The most common errors involved drug administration, use of medical machinery and airway management. Improved training and greater experience improved performance, but 28% of errors were associated with deficiencies in training even among experienced anesthetists.
In another study,21 investigators compared the responses of 3 groups of anesthetists of varying seniority to simulated intraoperative problems. A higher level of training was associated with more rapid detection and correction of clinical problems such as endobronchial intubation, acute atrial fibrillation and sudden equipment failure. However, the benefit of additional training was more evident for junior compared with senior residents than for senior residents compared with experienced anesthetists. Thus, relatively brief additional training and clinical exposure can result in improved performance.
Better training may also lessen stress. A study of residents during emergency department rotations found that the largest increases in their self-confidence were related to the management of pediatric emergencies, resuscitation and major trauma.22 Furthermore, greater confidence was associated with lower psychological distress scores. Additional experience and training may not only improve performance, but may also increase confidence and lessen stress.
Yet, even expert clinicians do not always react flawlessly to crises.2 Despite adequate skills and knowledge, problems occur because of overreliance on instinctive reactions at the expense of systematic protocols and coordinated team responses.9,20 These same problems have been encountered among pilots and, in both cases, reflect weaknesses in delegation, prioritization, monitoring, use of information, communication, leadership, problem assessment and avoidance of preoccupation, for example, becoming preoccupied by a persistent false alarm on a heart rate monitor may mean failing to notice that a patient has become cyanotic.9 Expert clinicians sometimes forget basic rules.
Such deficiencies are well known to physicians. In one survey, physicians preferred additional training in communication, coordination and leadership rather than in improved technical proficiency,1 whereas, in another study, 55% of physicians said that they had inadequate training in communication.23 Traditional protocol-based medical courses, such as Advanced Cardiac Life Support (ACLS), can improve performance in simulated crises24,25 and may be more effective than general clinical exposure at teaching specific procedural skills.22 However, these courses rarely incorporate training in the more subtle elements of effective teamwork and communication,2,9 despite the fact that those deficiencies are frequent sources of error in medical crises.8,9,26
Improving the process
Even with better courses, improving the process requires a formal means to evaluate it. Detecting errors in the response to medical crises relies largely on incident reports, or informal criticism following particularly poor performance.1 Such mechanisms rarely identify more than a small fraction of the problems that occur8,26 and, in any event, may not lead to any corrective measures. The usual approach to a serious incident is an intensive search for a human culprit, while ignoring the bias of hindsight.27,28
This approach is based on the assumption that human errors are behind most poor performance and that, by means of training, rules or sanctions, elimination is both possible and preferable. This strategy is not only inefficient, but it also fails to see a medical team for what it is — a dynamic system comprising people and technology, with resources and constraints. Inevitably, complex systems contain many latent, seemingly innocuous, faults (human or otherwise). The system will operate smoothly until several specific latent faults are combined in a particular manner. Therefore, corrective measures aimed at only the human elements present in one incident are unlikely to prevent future problems, because other unrecognized latent faults remain and the particular constellation of circumstances is unlikely to recur.27,29
Efforts directed at improving health care workers' responses to occasional, but spectacular, medical crises have typically relied largely on medical protocols and technical innovations. Yet, promising new technologies have often failed to improve outcomes. The introduction of intraoperative pulse oximetry monitoring has not reduced serious postoperative complications,30 and the monitoring of the intrapartum fetal heart rate has not resulted in fewer fetal catastrophes.31 No degree of technological sophistication is likely to result in a monitor that displays, for example, “tension pneumothorax” in response to a patient in crisis. For the foreseeable future, the judgement required to integrate complex data rapidly will continue to be confined to human beings.29 Nonetheless, many of the problems with process in the response to emergencies are human in origin and require solutions directed at human behaviour.1
Solutions should emphasize enhanced training in teamwork and systematic responses to medical crises (Table 3).2,29 Medical students and residents have been shown to gain confidence and proficiency from greater exposure to emergencies, either in emergency departments or elsewhere.22,24,25 In turn, improved confidence can diminish physicians' distress.22
Table 3
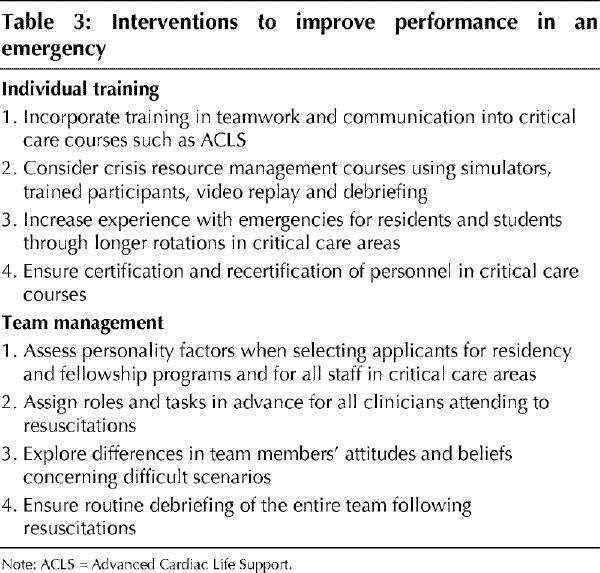
Newer protocol-based courses are evolving modelled on aircrew crisis resource management (CRM) training.2,9,11,32 These courses emphasize teamwork using sophisticated simulators, trained observers, video replay and debriefing, and they offer unique opportunities to simulate specific crises for the whole team.11,32 Although these courses were developed for anesthetists,9,32 they are now used to train other physicians, medical students and nurses in managing trauma, cardiac arrests and obstetric emergencies.33 Even without expensive simulators,34 existing courses in life support (such as ACLS or Advanced Trauma Life Support [ATLS]) can include training in communication, leadership, delegation, monitoring, use of information and other elements of CRM. Recertification may be even more important for physicians who treat patients in extremis infrequently.
Carrying out evaluations and feedback should be seen to be part of team leadership, with the focus on process and not outcome.2,27 This can occur during routine team debriefing sessions,1,2,12 especially following particularly unusual or stressful medical emergencies.9 Even following a successful resuscitation, debriefings offer an opportunity to praise good performance, or may uncover a negative process despite a positive outcome. Debriefing provides an opportunity to probe team members' attitudes, to clarify roles and responsibilities, and serves as a forum for finding local solutions.1,9,12 Debriefing reinforces team membership and, arguably, is one of the most effective methods for convincing and continuous quality improvement for individuals with substantial clinical experience.
Although human errors may be identified by debriefing, they should be seen as symptoms and not a cause.2 Focusing solely on an individual mistake may retard rather than advance the search for improvement and may lead to new rules, regulations or technology that serve only to make a system more brittle.2,27,29 Instead, errors can be viewed as important information about human performance in a complex system, and their investigation may lead to a better understanding of its function and malfunction.
Finally, careful attention should be paid to personnel selection for emergency departments, operating rooms or intensive care units, as well as for standing trauma or cardiac arrest teams, with the aim of choosing those who function best under stress and in a team.1,21 The same approach is probably appropriate for fellowships in critical care or residency programs in areas such as emergency medicine and anesthesia. Personality factors in medical personnel affect both the perception of stress and coping mechanisms,35 and may affect performance as well.36,37 As La Barre >stated,38 “it is not stress [of the external challenge] as such but the psychic reaction to it that is important.” Some people perceive little stress in situations that others find intolerable and their preferential selection for high-stress areas may lead to smoother functioning of a team.
Conclusion
The nature of the extremes of disease is such that no amount of training can entirely remove stress or ensure the smooth functioning of a team. Poor outcomes do occur, but what is perhaps surprising given the complex circumstances of medical emergencies is that good outcomes happen as often as they do.27 Nonetheless, increased clinical exposure, learned systematic responses and improved teamwork may result in diminished stress and improved care.
Physicians working in all areas may benefit from ongoing training, however, the clinical settings in which emergencies are rarest may be those in which such training is most necessary.39 Physicians who opt for the “it won't happen to me” posture are unlikely to avoid such situations forever, or to benefit the patient in extremis whom they eventually must treat. However, even in high-stress settings frequent team self-examination is important to ensure that ingrained habits are not masking important problems.
Thinking clearly in an emergency means knowing not only the right thing to do, but also how to translate that knowledge into effective action. Efforts to improve the response to patients in extremis must look beyond individual deeds to the actions and interactions of the whole team. A medical team that thinks clearly will function smoothly and perform beyond the sum of its individual capacities, with diminished stress and improved morale, and an enhanced likelihood of a successful outcome.
Articles to date in this series .
Redelmeier DA, Ferris LE, Tu JV, Hux JE, Schull MJ. Problems for clinical judgement: introducing cognitive psychology as one more basic science. CMAJ 2001;164(3):358-60.
Redelmeier DA, Schull MJ, Hux JE, Tu JV, Ferris LE. Problems for clinical judgement: 1. Eliciting an insightful history of present illness. CMAJ 2001;164(5):647-51.
Redelmeier DA, Tu JV, Schull MJ, Ferris LE, Hux JE. Problems for clinical judgement: 2. Obtaining a reliable past medical history. CMAJ 2001;164(6):809-13.
Footnotes
This article has been peer reviewed.
Competing interests: None declared.
Reprint requests to: Dr. Michael Schull, Clinical Epidemiology Unit, Sunnybrook & Women's College Health Sciences Centre, Rm. G147, 2075 Bayview Ave., Toronto ON M4N 3M5; fax 416 480-6048; mjs@ices.on.ca
References
- 1.Helmreich RL, Schaefer HG. Team performance in the operating room. In: Bogner MS, editor. Human error in medicine. 1st ed. Hillsdale (NJ): Lawrence Erlbaum Associates; 1994. p. 225-54.
- 2.Risser DT, Rice MM, Salisbury ML, Simon R, Jay GD, Berns SD. The potential for improved teamwork to reduce medical errors in the emergency department. Ann Emerg Med 1999;34:373-83. [DOI] [PubMed]
- 3.Xiao Y, Hunter WA, Mackenzie CF, Jefferies NJ. Task complexity in emergency medical care and its implications for team coordination. Hum Factors 1996;38:636-45. [DOI] [PubMed]
- 4.Chambers R, Wall D, Campbell I. Stresses, coping mechanisms and job satisfaction in general practitioner registrars. Br J Gen Pract 1996;46:343-8. [PMC free article] [PubMed]
- 5.Patil PG, Apfelbaum JL, Zacny JP. Effects of a cold-water stressor on psychomotor and cognitive functioning in humans. Physiol Behav 1995;58:1281-6. [DOI] [PubMed]
- 6.Houston DM, Allt SK. Psychological distress and error making among junior house officers. Br J Health Psychol 1997;2:141-51.
- 7.Jex SM, Hughes P, Storr C, Baldwin DC, Conard S. Behavioural consequences of job-related stress among resident physicians: the mediating role of psychological strain. Psychol Rep 1991;69:339-49. [DOI] [PubMed]
- 8.Donchin Y, Gopher D, Olin M, Badihi Y, Biesky M, Sprung CL. A look into the nature and causes of human errors in the intensive care unit. Crit Care Med 1995;23:294-300. [DOI] [PubMed]
- 9.Howard SK, Gaba DM, Fish KJ, Yang G, Sarnquist FH. Anaesthesia crisis resource management training: teaching anesthesiologists to handle critical incidents. Aviat Space Environ Med 1992;63:763-70. [PubMed]
- 10.Clemmer TP, Spuhler VJ, Berwick DM, Nolan TW. Cooperation: the foundation of improvement. Ann Intern Med 1998;128:1004-9. [DOI] [PubMed]
- 11.Gaba DM. Human error in dynamic medical domains. In: Bogner MS, editor. Human error in medicine. 1st ed. Hillsdale (NJ): Lawrence Erlbaum Associates; 1994. p. 197-224.
- 12.Felton JS. Burnout as a clinical entity — its importance in health care workers. Occup Med 1998;48:237-50. [DOI] [PubMed]
- 13.Revicki DA, Whitley TW, Gallery ME. Organizational characteristics, perceived work stress, and depression in emergency medicine residents. Behav Med 1993;19:74-81. [DOI] [PubMed]
- 14.Fonne VM, Myhre G. The effect of occupational culture on coordination of emergency medical service aircrew. Aviat Space Environ Med 1996;67:525-9. [PubMed]
- 15.Waeckerle JF. Disaster planning and response. N Engl J Med 1991;324:815-21. [DOI] [PubMed]
- 16.Auf der Heide E. Disaster planning, part II. Disaster problems, issues and challenges identified in the research literature. Emerg Med Clin North Am 1996;14:453-80. [DOI] [PubMed]
- 17.Paxton F, Howie JG, Porter AM. A study of interruption rates for practice nurses and GPs. Nurs Stand 1996;10(43):33-6. [DOI] [PubMed]
- 18.Krueger GP. Fatigue, performance and medical errors. In: Bogner MS, editor. Human error in medicine. 1st ed. Hillsdale: Lawrence Erlbaum Associates; 1994. p. 311-26.
- 19.Bates B. Clinical thinking: from data to plan. In: Bates B, editor. A guide to physical examination and history taking. 6th ed. Philadelphia: J.B. Lippincott; 1995. p. 635-48.
- 20.Cooper JB, Newbower RS, Kitz RJ. An analysis of major errors and equipment failures in anaesthesia management: considerations for prevention and detection. Anesthesiology 1984;60:34-42. [DOI] [PubMed]
- 21.De Anda A, Gaba DM. Role of experience in the response to simulated critical incidents. Anesth Analg 1991;72:308-15. [DOI] [PubMed]
- 22.Williams S, Dale J, Glucksman E, Wellesley A. Senior house officers' work related stressors, psychological distress and confidence in performing clinical tasks in accident and emergency: a questionnaire study. BMJ 1997;314:713-8. [DOI] [PMC free article] [PubMed]
- 23.Ramirez AJ, Graham J, Richards MA, Cull A, Gregory WM. Mental health of hospital consultants: the effects of stress and satisfaction at work. Lancet 1996;347:724-8. [DOI] [PubMed]
- 24.Ali J, Cohen R, Gana TJ, Al-Bedah KF. Effect of advanced trauma life support program on medical students' performance in simulated trauma patient management. J Trauma 1998;44:588-91. [DOI] [PubMed]
- 25.Ali J, Cohen R, Reznick R. Demonstration of acquisition of trauma management skills by senior medical students completing the ATLS program. J Trauma 1995;38:687-91. [DOI] [PubMed]
- 26.Mackenzie CF, Jefferies NJ, Hunter WA, Bernhard WN, Xiao Y, LOTAS group. Comparison of self-reporting of deficiencies in airway management with video analyses of actual performance. Hum Factors 1996;38:623-35. [DOI] [PubMed]
- 27.Cook RI, Woods DD. Operating at the sharp end: the complexity of human error. In: Bogner MS, editor. Human error in medicine. 1st ed. Hillsdale (NJ): Lawrence Erlbaum Associates; 1994. p. 255-310.
- 28.Caplan RA, Posner KL, Cheney FW. Effect of outcome on physician judgements of appropriateness of care. JAMA 1991;265:1957-60. [PubMed]
- 29.Gaba DM, Maxwell M, DeAnda A. Anesthetic mishaps: breaking the chain of accident evolution. Anesthesiology 1987;66:670-6. [PubMed]
- 30.Moller JT. Can we prove the benefits of monitoring? [editorial]. Acta Anaesthesiol Scand 1995;39(Suppl 107):287-9. [DOI] [PubMed]
- 31.Freeman R. Intrapartum fetal monitoring — a disappointing story [editorial]. N Engl J Med 1990;322:624-5. [DOI] [PubMed]
- 32.Kurrek MM, Fish KJ. Anaesthesia crisis resource management training: an intimidating concept, a rewarding experience. Can J Anaesth 1996;43:430-4. [DOI] [PubMed]
- 33.Wansbrough G. Doctors sharpen skills on blinking, breathing dummy. Medical Post [Toronto] 1999 March 2; 5.
- 34.Kurrek MM, Devitt JH. The cost for construction and operation of a simulation centre. Can J Anaesth 1997;44:1191-5. [DOI] [PubMed]
- 35.Deary IJ, Blenkin H, Agius RM, Endler NS, Zealley H, Wood R. Models of job-related stress and personal achievement among consultant doctors. Br J Psychol 1996;87:3-29. [DOI] [PubMed]
- 36.Risucci D, LaMantia J, Ryan J. Personality types and preferences of emergency medicine residents: correlation with clinical performance evaluations [abstract]. Ann Emerg Med 1999;34;4:S25.
- 37.Alagappan K, Steinberg M, Mancherje N, Pollack S, Carpenter K. The psychological effects of a four-week emergency medicine rotation on residents in training. Acad Emerg Med 1996;3:1131-5. [DOI] [PubMed]
- 38.Stein HF, Mold JW. Stress, anxiety and cascades in clinical decision-making. Stress Med 1988;4:41-8.
- 39.Sakellariou A, Lane RH, McDonald PJ. The trauma team concept and its implementation in a district general hospital. Ann R Coll Surg Engl 1995;77:45-52. [PMC free article] [PubMed]


