Abstract
Introduction
The aim of this study was to investigate the effect of 50 mg mirabegron once daily in relieving ureteral double-J (DJ) stent-related discomfort after ureteroscopy (URS) or retrograde intrarenal surgery (RIRS).
Material and methods
A total of 210 patients who underwent DJ ureteral stent insertion after URS or RIRS were randomized 1:1 to receive either no treatment (Group B) or mirabegron 50 mg once daily (Group A) during the stenting period. At time of stent removal, all patients were evaluated for stent-related symptoms using the Arabic translated and validated ureteral stent symptom questionnaire (USSQ). The severity of stent-related symptoms (SRS) was compared between the two groups.
Results
The mean age was 46.6 ±8.2 years in Group A and 44.7 ±9.4 (26–64) years in the control group (p = 0.13). The stone characteristics, stent size, and position were similar in both groups. Compared to the control group, the mirabegron group had significantly lower daytime frequency, nocturia and urgency (p = 0.028, p = 0.008 and p = 0.012, respectively). As for stent-related pain, Group A had significantly less flank and abdominal pain (p = 0.007 and p = 0.001, respectively). The mirabegron versus control group showed significant difference in mean analgesics use and quality of life (QoL) scores during the stenting period (p = 0.005 and p = 0.003, respectively). Three patients (2.9%) in Group A encountered minor adverse effects (two experienced dry mouth and one presented with constipation).
Conclusions
For patients with indwelling DJ stent, postoperative mirabegron 50 mg use was effective and well-tolerated for the treatment of lower urinary tract symptoms and stent-related pain.
Keywords: mirabegron, DJ stent, randomized trial
INTRODUCTION
Double-J (DJ) stent insertion is one of the most common procedures in endourological practice and a necessary component of many minimally invasive surgeries [1]. However, besides the known benefits, stent placement results in bothersome urinary symptoms and pain in approximately 80% of patients [2]. The stent-related symptoms (SRS) are attributed to lower ureter and bladder spasm and are due to bladder irritation [3]. In addition to the strategies such as accurate stent insertion indications, stenting maneuvers and using alternative stents; oral medication therapy remains one of the solutions used to alleviate these symptoms [4]. Some researchers continue to investigate the effect of several medical therapies on reducing the SRS, which affect the quality of life, however, the efficacy of these drugs is still controversial [5, 6]. Mirabegron is the first and only selective β3-adrenergic receptor agonist agent currently available and it is one of the treatment options for overactive bladder (OAB). Hence, many urologists have been introducing mirabegron therapy for OAB in recent years and because the SRS are similar to OAB symptoms, it may be another treatment option for reducing bladder irritability in patients indwelling DJ stent [7]. Thus, in the present randomized controlled study we aim to investigate the effect of 50 mg mirabegron once daily in relieving ureteral DJ stent-related discomfort after ureteroscopy (URS) or retrograde intrarenal surgery (RIRS) using the Arabic translated and validated ureteral stent symptom questionnaire (USSQ) [8].
MATERIAL AND METHODS
This study was conducted with approval from the Research Ethics Committee of the Minia University, Egypt (Reference No. 692:6/18). From June 2018 to March 2019, patients with unilateral DJ stent after URS or RIRS were accepted for enrollment in the study. After documentation of informed consent, patients were randomized (using a table with a random number) 1:1 to receive either no treatment (Group B) or mirabegron 50 mg once daily (Group A) during the stenting period. Patients were excluded if they metany of the following criteria: (1) age less than 18 years, (2) pregnant women, (3) history of previous ureteral stenting, (4) bilateral stents, (5) long-term stenting (on regular exchange), (6) bladder pathology, (7) symptomatic benign prostatic hyperplasia, (8) overactive bladder, (9) urinary tract infection, (10) moderate or severe cardiovascular disease, (11) hepatic dysfunction, (12) previous use of selective alpha-1-blocker and/or antimuscarinic agent.
Routine preoperative evaluation was done for the planned procedures. A 6 Fr polyurethane DJ stent (Inlay Optima®, Bard Medical, Covington, GA) was inserted under fluoroscopic and cystoscopic guidance. Appropriate length was adjusted according to patient’s height. Routine X-ray of the kidneys, ureter and bladder (KUB) was done for all patients before home discharge to confirm the proper stent positioning.
Patients in Group A received mirabegron 50 mg starting from the day after stent placement to the day of stent removal, while the control Group B received only the standardized discharge medication in the form of analgesic in case of pain plus antibiotic if indicated. The outcomes were obtained at stent removal after 2 weeks and not more than 20 days. We excluded patients who visited the hospital to remove the stent after 20 days, and classified them as loss to follow-up. To assess urinary symptoms and pain associated with DJ stent, patients were asked to complete the brief-form Arabic version USSQ at time of stent removal.
Statistical analysis
A sample size of 210 patients was calculated based on a power of 80% and a significance level of 0.05 to detect 30% difference in flank pain scores and 26% difference in frequency scores in the first 2 weeks with the stent in situ. Descriptive statistics included mean ±SD for continuous variables, number and percentage for categorical variables. Student t test, chi-square test and non-parameter Wilcoxon test were used, as appropriate. Analyses were performed on full per-protocol set population as it was determined more appropriate to exclude those who failed to complete the study. A p value <0.05 was considered significant. Statistical analyses were conducted using computer software (Package for SocialScience 19.0, SPSS Inc., Chicago, IL).
RESULTS
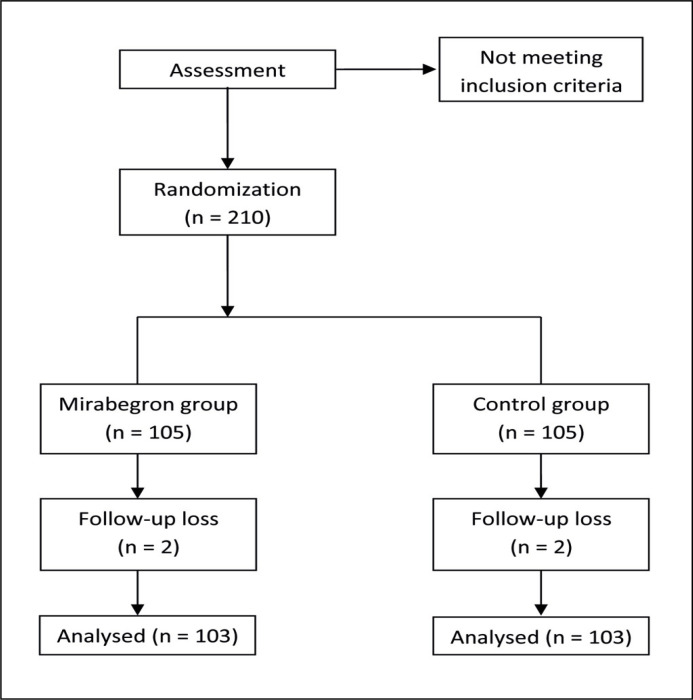
A total of 210 patients who underwent DJ ureteral stent insertion were randomly assigned to the treatment and control groups. Four patients were excluded from the final analysis due to loss during follow-up. Finally, 103 patients remained in the mirabegron group and 103 patients in the control group. Overall, a total of 206 treated patients were analyzed. The CONSORT diagram of this study is shown in Figure 1. Patient demographics are listed in Table 1. Average patient age was 45.7 years (range 26 to 66), and the overall distribution of males and females was 71% and 29%, respectively. There was no significant difference in age, gender, stone size, stone location and length of stent between the two groups. The main indication of ureteral DJ stent placement was URS and RIRS. The overall study results are presented in Table 2. Patients receiving mirabegron 50 mg presented with significantly lower daytime frequency, nocturia and urgency (p = 0.028, p = 0.008 and p = 0.012, respectively) when compared to Group B. Similarly, there were marked decreases in flank pain and abdominal pain that were associated with mirabegron use (p = 0.007 and p = 0.001, respectively). Mean analgesics use and quality of life (QoL) scores were also significantly lower in Group A during the stenting period (p = 0.005 and p = 0.003, respectively). There were no significant differences between the two groups (P = 0.227) regarding the adverse events. Three patients (2.9%) in Group A encountered minor adverse effects, 2 had dry mouth and one had constipation. No patients complained of acute urinary retention or tachycardia.
Figure 1.
CONSORT diagram of this study.
Table 1.
Patient demographics
| Variable | Group A | Group B | P value |
|---|---|---|---|
| No. of patients | 103 | 103 | NA |
| Age | 44.7 ±9.4 (26-64) | 46.6 ±8.2 (30-66) | 0.12* |
| Gender Male Female |
68 (66%) 35 (34%) |
78 (75.7%) 25 (24.3%) |
0.45† |
| Stone side Rt. Lt. |
53 (51.4%) 50 (48.5%) |
65 (63%) 38 (37%) |
0.12† |
| Stone site Pelvis Calyceal Upper ureter Mid ureter Lower ureter |
7 (6.8%) 4 (3.8%) 20 (19.4%) 16 (15.5%) 56 (54.3%) |
8 (7.7%) 3 (3%) 24 (23%) 13 (12.6%) 55 (53.3%) |
0.8† |
| Stone size (mm), Mean ±SD |
7.6 ±2.5 |
8.2 ±3.5 |
0.26* |
| Length of stent 26 cm 24 cm |
51 (49.5%) 52 (50.5%) |
54 (52.4%) 49 (47.5%) |
0.34† |
NA – not applicable;
Student t test;
Chi-square test
Table 2.
Overall study results
| Variable | Group A | Group B | P value |
|---|---|---|---|
| Daytime frequency | 2.18 ±1.80 | 2.68 ±2.00 | 0.028 |
| Nocturia | 1.05 ±1.18 | 1.66 ±1.62 | 0.008 |
| Urgency | 1.33 ±1.67 | 1.93 ±1.74 | 0.012 |
| Flank pain | 1.13 ±1.46 | 1.83 ±1.92 | 0.007 |
| Abdominal pain | 0.80 ±1.08 | 1.50 ±1.55 | 0.001 |
| Analgesics use | 0.30 ±0.79 | 0.74 ±1.29 | 0.005 |
| QoL | 2.79 ±1.05 | 3.27 ±1.32 | 0.003 |
| Drug related adverse events | 3 (2.9%) | 2 | 0.227 |
| Constipation | 2 (1.9) | 1 (0.9%) | |
| Dry mouth | 1 (2.1) | 0 (0) | |
| Acute urinary retention | 0 (0) | 0 (0) |
DISCUSSION
Indwelling DJ stent is a common urological intervention and its indications for use have continued to expand in the era of minimally invasive surgeries. It plays a major role in a wide range of situations to prevent or relieve ureteral obstruction [9]. However, this procedure is commonly associated with SRS responsible for patients’ discomfort with a negative effect on QoL during the stenting period [10]. A number of modern stents incorporate extraction strings made of fine suture material. Stent indwelling time was reported to be significantly lower in patients with these type of stents which positively impacts patients’QoL [11]. The exact pathophysiology of stent-related symptoms remains unknown; however, it is mostly attributed to lower ureter and bladder spasm due to bladder irritation [3].
In an attempt to alleviate these symptoms, some investigators reported that stent length, girth adjustment and avoiding distal end crossing the midline are essential and significantly decrease SRS [12]. Others showed no significant effect of length and girth on stent symptoms [13]. The effectiveness of different therapeutic protocols aiming to improve ureteral SRS is under investigation. Analgesics, anticholinergics and alpha-blockers, are among the most effective options to manage SRS. The rationale behind using alpha-blockers in overcoming SRS is that, the inhibition of α-1adrenergic receptors in the bladder body and ureter result in smooth muscle relaxation of lower ureter and trigone and this will decrease bladder overactivity and ureteral spasm [14]. Results of some studies have shown that using anticholinergic agents like solifenacin and tolterodine are also effective in reducing SRS through inhibition of involuntary bladder contractions induced by the distal end of DJ stent [5, 15]. Shalaby et al. strongly suggested using combination therapy of anticholinergics and alpha-blockers to improve the SRS [16]. However, because of the potential side effects of the above medications, it may be inappropriate to be used in patients with some comorbidities or this will decrease treatment compliance. Our proposal of the selective β-3 adrenergic receptor agonist, mirabegron 50 mg, may play a significant role to overcome these limitations. Beta-3 adrenergic receptors are distributed at various sites in the bladder including the smooth muscle and urothelium and also expressed in mucosa and muscular layers of the human ureter. So, use of highly selective β-3 agonists, relax the detrusor smooth muscle, and result in increased bladder capacity without any changes in micturition pressure, post-void residual urine volume, or voiding contractions [17]. Mirabegron demonstrated significant dose dependent improvements in OAB symptoms in a phase III study [18]. In consideration of these findings, we assumed that mirabegron would be more effective for voiding symptoms caused by DJ stent placement. Our findings showed that patients receiving mirabegron 50 mg expressed significant lower daytime frequency, nocturia and urgency. These results are found to be comparable with a prospective study performedon 76 patients and showed significant improvement of overactive bladder symptom scores and urinary urgency scores. Also, the postoperative USSQ and the overall pain score were lower in the mirabegron group compared to the no-treatment group, however, the QoL scores were lower in the mirabegron group, but in contrast to our study, the differences were not significant and this might be due to the small sample size [19]. In another study, the results were not statistically significant especially for frequency and nocturia, and urgency scores in the USSQ urinary symptom subscore were not significantly decreased in the mirabegron group as compared with the control group. They suggest that encouraging water intake for patients undergoing ureteroscopy and with an indwelling ureteric stent may have had an effect and that the resulting polyuria reduced the response to the drug [20]. Sahen et al. [21] confirmed mirabegron as a single therapy with better results in treating OAB symptoms related with DJ stents than other therapies. In a recent placebo controlled study comparing mirabegron with tamsulosin, it wasreported that tamsulosin improves only urinary symptoms due to the ureteral stent and decreases the need for analgesics, while mirabegron has no effect on ureteral stent-related symptoms, but it decreases analgesic need [22]. These findings that are in contrast to our study could be explained by lack of comparison with another drug in our study. We encountered minor adverse effects in the form of dry mouth and constipation in only 2.9% of our patients. Mirabegron was well tolerated for 12 weeks of treatment in patients with OAB with only 2% reported dry mouth and constipation [23]. This study has some limitations, being conducted at a single center with the used method of randomization, potentially subject it to selection bias. The favourable outcome provides clinical evidence for future placebo-controlled studies or combination studies with other agents (e.g. alpha-blockers, antimuscarinic agents).
CONCLUSIONS
For patients with indwelling DJ stent, postoperative mirabegron 50 mg use was effective and well-tolerated for the treatment of lower urinary tract symptoms, stent-related body pain and has positive impact on QoL.
CONFLICTS OF INTEREST
None of the contributing authors has any conflict of interest, including specific financial interests or relationships and affiliations relevant to the subject matter or materials discussed in the manuscript.
References
- 1.Knudsen BE, Beiko DT, Denstedt JD. Stenting after ureteroscopy: pros and cons. Urol Clin North Am. 2004;31:173–180. doi: 10.1016/S0094-0143(03)00091-0. [DOI] [PubMed] [Google Scholar]
- 2.Sighinolfi MC, Micali S, De Stefani S, et al. Indwelling ureteral stents and sexual health: a prospective, multivariate analysis. J Urol. 2007;178:229–231. doi: 10.1016/j.juro.2007.03.039. [DOI] [PubMed] [Google Scholar]
- 3.Thomas R. Indwelling ureteral stents: impact of material and shape on patient comfort. J Endourol. 1993;7:137–140. doi: 10.1089/end.1993.7.137. [DOI] [PubMed] [Google Scholar]
- 4.Miyaoka R, Monga M. Ureteral stent discomfort: Etiology and management. Indian J Urol. 2009;25:455–460. doi: 10.4103/0970-1591.57910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee YJ, Huang KH, Yang HJ, Chang H-C, Chen J, Yang T-K. Solifenacin improves double-J stent-related symptoms in both genders following uncomplicated ureteroscopic lithotripsy. Urolithiasis. 2013;41:247–252. doi: 10.1007/s00240-013-0554-y. [DOI] [PubMed] [Google Scholar]
- 6.Kuyumcuoglu U, Eryildirim B, Tuncer M, Faydaci G, Tarhan F, Ozgül A. Effectiveness of medical treatment in overcoming the ureteral double-J stent related symptoms. Can UrolAssoc J. 2012;6:E234–E237. doi: 10.5489/cuaj.10143.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khullar V, Amarenco G, Angulo JC, et al. Efficacy and tolerability of mirabegron, a beta-3 adrenoceptor agonist, in patients with overactive bladder: results from a randomised European-Australian phase 3 trial. Eur Urol. 2013;63:283–295. doi: 10.1016/j.eururo.2012.10.016. [DOI] [PubMed] [Google Scholar]
- 8.El-Nahas AR, Elsaadany MM, Tharwat M, et al. Validation of the Arabic linguistic version of the Ureteral Stent Symptoms Questionnaire. Arab J Urol. 2014;12:290–293. doi: 10.1016/j.aju.2014.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chew BH, Knudsen BE, Denstedt JD. The use of stents in contemporary urology. Curr Opin Urol. 2004;14:111–115. doi: 10.1097/00042307-200403000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Joshi HB, Stainthorpe A, MacDonagh RP, Keeley FX, Jr, Timoney AG, Barry MJ. Indwelling ureteral stents. Evaluation of symptoms, quality of life and utility. J Urol. 2003;169:1065–1069. doi: 10.1097/01.ju.0000048980.33855.90. [DOI] [PubMed] [Google Scholar]
- 11.Oliver R, Wells H, Traxer O, et al. Ureteric stents on extraction strings: a systematic review of literature. Urolithiasis. 2018;46:129–136. doi: 10.1007/s00240-016-0898-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rane A, Saleemi A, Cahill D, Sriprasad S, Shrotri N, Tiptaft R. Have stent-related symptoms anything to do with placement technique? J Endourol. 2001;7:741–745. doi: 10.1089/08927790152596352. [DOI] [PubMed] [Google Scholar]
- 13.Damiano R, Autorino R, De Sio M, et al. Does the size of ureteral stent impact urinary symptoms and quality of life? A prospective randomized study. Eur Urol. 2005;48:673–678. doi: 10.1016/j.eururo.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 14.Wang CJ, Huang SW, Chang CH. Effects of tamsulosin on lower urinary tract symptoms due to double-j stent: a prospective study. Urol Int. 2009;83:66–69. doi: 10.1159/000224871. [DOI] [PubMed] [Google Scholar]
- 15.Park SC, Jung SW, Lee JW, Rim JS. The effects of tolterodine extended release and alfuzosin for the treatment of double-j stent-related symptoms. J Endourol. 2009;23:1913–1917. doi: 10.1089/end.2009.0173. [DOI] [PubMed] [Google Scholar]
- 16.Shalaby E, Ahmed AF, Maarouf A, Yahia I, Ali M, Ghobish A. Randomized Controlled Trial to Compare the Safety and Efficacy of Tamsulosin, Solifenacin, and Combination of Both in Treatment of Double-J Stent-Related Lower Urinary Symptoms. Adv Urol. 2013;2013:752382. doi: 10.1155/2013/752382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leon LA, Hoffman BE, Gardner SD, et al. Effects of the b3-adrenergic receptor agonist disodium 5-[(2R)-2-[[(2R)-2-(3-chlorophenyl)-2hydroxyethyl] amino] propyl]-1, 3-benzodioxole-2, 2-dicarboxylate (CL316243) on bladder micturition reflex in spontaneously hypertensive rats. J Pharmacol Exp Ther. 2008;326:178–185. doi: 10.1124/jpet.108.138651. [DOI] [PubMed] [Google Scholar]
- 18.Nitti VW, Chapple CR, Walters C, et al. Safety and tolerability of the beta-3 adrenoceptor agonist mirabegron, for the treatment of overactive bladder: results of a prospective pooled analysis of three 12-week randomised Phase III trials and of a 1-year randomised Phase III trial. Int J ClinPract. 2014;68:972–685. doi: 10.1111/ijcp.12433. [DOI] [PubMed] [Google Scholar]
- 19.Tae BS, Cho S, Jeon BJ, et al. Does mirabegron relieve ureteric stent-related discomfort? A prospective, randomized, multicentre study. BJU Int. 2018;122:866–872. doi: 10.1111/bju.14416. [DOI] [PubMed] [Google Scholar]
- 20.Hideo O, Tomoya Y, Shunsuke H, et al. The Efficacy of Mirabegron for the Relief of Ureteral Stent-Related Symptoms. Acta Med. Okayama. 2020;74:145–150. doi: 10.18926/AMO/58273. [DOI] [PubMed] [Google Scholar]
- 21.Sahin A, Yildirim C, Yuksel OH, Urkmez A. Treatment of ureteral catheter related symptoms; mirabegron versus tamsulosin/solifenacin combination: A randomized controlled trial. Arch Esp Urol. 2020;73:54–59. [PubMed] [Google Scholar]
- 22.Yavuz A, Kilinc MF, Aydin M, Ofluoglu Y, Bayar G. Does tamsulosin or Mirabegron improve ureteral stent-related symptoms? A prospective placebo-controlled study. Low Urin Tract Symptoms. 2021;13:17–21. doi: 10.1111/luts.12320. [DOI] [PubMed] [Google Scholar]
- 23.Nitti VW, Auerbach S, Martin N, Calhoun A, Lee M, Herschorn S. Results of a Randomized Phase III Trial of Mirabegron in Patients with Overactive Bladder. J Urol. 2013;189:1388–1395. doi: 10.1016/j.juro.2012.10.017. [DOI] [PubMed] [Google Scholar]