Abstract
THIS ARTICLE DESCRIBES THE MANITOBA CATARACT WAITING LIST PROGRAM. This program uses a centralized database to track and prioritize all patients waiting for cataract surgery. It provides an objective and reliable measure of the length of the wait, and patients on the waiting list are treated in a more equitable fashion through application of a uniform method of prioritization. The program will allow for long-term tracking of quality of care through monitoring of the average length of wait for patients with comparable functional impairment. It will also allow for long-term monitoring of thresholds for surgery. It has brought to light previously undocumented issues, such as the simultaneous booking of both eyes for cataract surgery and variations in waiting time between surgeons.
The rate of cataract surgery has increased significantly in Western countries in the last 2 decades.1 Presumed causes include lowered thresholds for surgery as surgical techniques and corresponding outcomes have improved, and, to a lesser extent, changes in demographic features.2 In countries with a socialized medical system this has led to significant waiting times for this procedure.3 As waiting times have grown longer, the need to prioritize patients has become more important. Several different models for prioritization have been developed.4,5,6,7,8,9 In this article we describe the Manitoba Cataract Waiting List Program (MCWLP), developed at the Misericordia Health Centre, Winnipeg. The MCWLP is the first Canadian provincial program for monitoring cataract surgery waiting lists and prioritizing patients.
Program description
The MCWLP was created as part of the contractual agreement between the Misericordia Health Centre and Manitoba Health when all adult ophthalmologic surgical services were consolidated at the centre, in 1993. It was decided that the list would record all patients waiting for cataract surgery in Winnipeg (representing over 90% of all cataract cases done in the province) and prioritize them. All members of the Department of Ophthalmology were invited to a series of planning meetings in 1997. A medical ethicist was invited at that time to give departmental rounds on the ethics of waiting lists and their management. There was consensus that the scoring system should be heavily weighted by the degree of functional impairment related to the cataract. This is consistent with other Canadian models for prioritizing elective surgery.10 The 14-item Visual Functioning Index (VF-14),11 a questionnaire based on common patient symptoms and their severity, was selected to measure the severity of functional impairment. Manitoba had been involved in the International Cataract Surgery Outcomes Study,12,13,14,15 which developed the VF-14, and thus there was some local familiarity with the instrument. Also, the VF-14 score had been shown to be the best preoperative predictor of gain in patient satisfaction11 and to have a high degree of reliability and interobserver scoring consistency.16,17 Finally, the use of this independently measured assessment of functional impairment was felt to eliminate possible manipulation by physicians to enhance the appearance of their waiting list.
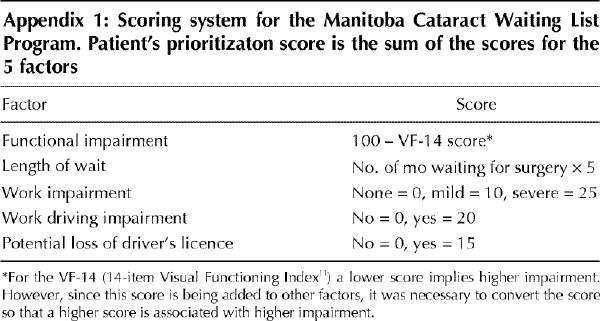
There was also consensus that difficulty at work due to visual impairment and potential loss of one's driver's licence should be factored into prioritization for cataract surgery. Precedent for incorporating social factors into a cataract surgery prioritization system comes from New Zealand, where, after public hearings, it was decided to take into account whether a patient's clinical condition threatened his or her ability to work, care for dependants or live independently.9
There was a strong feeling that spending a longer time on the waiting list constituted a burden to the patient, and so length of wait needed to be included. It was recognized that advanced age has been linked with a reduced likelihood of gain from cataract surgery,18 but it was felt that it would be socially unacceptable to penalize older patients. The department then agreed on the points to be awarded for all the scoring factors, and the final questionnaire with the final scoring formula was developed (Appendix 1).
A new computer program was created early in 1998 to maintain the waiting list. This program was divided into an active component, tracking all patients who had been booked to undergo surgery and were waiting, and an archive component, containing the records of all completed cataract procedures and bookings that were cancelled. Before this system was introduced, ophthalmologists kept their own waiting lists and, at a time of their choosing (no later than 2 weeks before their intended surgery date), would then send in a booking request form to the hospital specifying the time and date for surgery. Under the new system they are instructed to send in a booking request form to the hospital at the time when the decision to proceed with surgery is made. The hospital then contacts each patient by telephone to administer the questionnaire. Translators are used when necessary. The results are entered into the database to create the prioritization score. If both eyes are booked at the same time, the interview is conducted once, and the VF-14 score is used for both eyes.
Each ophthalmologist receives a monthly report listing his or her patients in order of priority as determined by the scoring system. Using this report, the doctors indicate which patients they wish to operate on and in what order for their month of surgical slates 3 months hence. The report is also used to transmit information in case there has been a change in patient status. Cancellations are transferred to the archive, but postponements remain in the active waiting list. The ophthalmologist can also revise or override the VF-14 score if a patient's condition deteriorates or if the physician believes that coexisting disease causes the functional impairment score to overestimate the potential gain from cataract surgery. The ophthalmologist is also asked to provide a VF-14 score for patients who could not be reached or who could not answer the questionnaire (e.g., because of mental handicap or deafness). Each day a record of completed operations is sent from the operating room to the MCWLP staff; this list is used to transfer records from the active database to the archive. The data from the entire waiting list are produced monthly and are examined in depth twice yearly.
The costs of developing and running the program were paid by the Misericordia Health Centre.
Preliminary evaluation
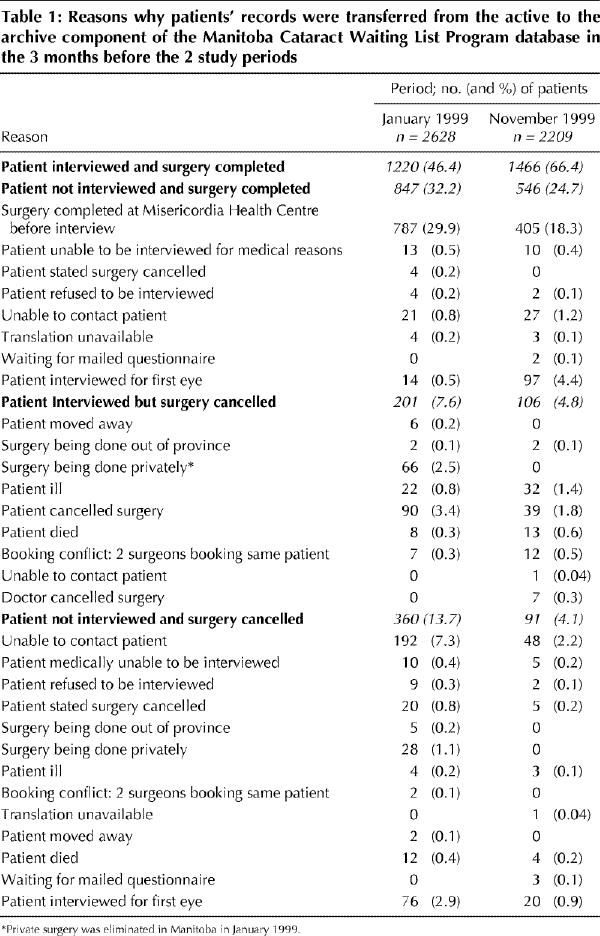
During the transition period, because of the unexpectedly large number of patients waiting, there was a backlog to get on the waiting list. The initial assessment of the database was conducted in January 1999 once the backlog had been eliminated. In January 1999 there were 5372 bookings on the active waiting list; by November the number had grown to 5481. Comparisons of VF-14 distribution curves were similar for all surgeons except for retina specialists, whose patients presumably had higher rates of coexisting disease. The reasons for transfer to the archive portion of the database during the 3 months preceding the 2 study periods are shown in Table 1. For patients who were interviewed and had surgery, there was no statistically significant difference in age, VF-14 score or patient's assessment of the degree of work impairment between the 2 study periods. The mean length of time waiting for surgery fell from 34.7 weeks in January to 28.9 weeks in November. Between January and November the number of cases fully insured by Manitoba Health increased from 6600 to 8600 per year (in January Manitoba Health agreed to pay the facility fee for 2000 cases performed at private surgery centres [these cases are tracked in the database]).
Table 1
There was significant variation in waiting times between physicians. In January, for the ophthalmologists with more than 300 patients on the active waiting list (surgeons operating both at the Misericordia Health Centre and at the private centres), the individual mean waiting time ranged from 13.3 to 65.2 weeks (group average 31.6 weeks). The subspecialists who performed some cataract surgery had individual mean waiting times ranging from 10.0 to 23.7 weeks (group average 12.2 weeks). The mean waiting times in November were similar.
For surgery completed in the 3 months before January 1999, no statistically significant correlation for variation in time spent waiting for cataract surgery could be attributed to differences in VF-14 score or patients' response to questions about work impairment, driving difficulties at work or potential loss of driver's licence in analysis of variance. The same analysis for the 3 months preceding November 1999 showed that all of these factors correlated with waiting time.
Comments
The creation of the MCWLP involved a significant degree of upheaval. During the transition period, there was a backlog to get on the waiting list. Initially it was forecast that 1.5 staff would be needed to run the program. For a 2-month period 8 temporary staff were needed to catch up on the backlog, and, ultimately, 2.0 staff have been required to run the program.
The program was designed to provide a standard scoring system to be used as a guide, but the actual slating of dates was still left in the hands of the individual ophthalmologists. This was done so that the surgeons would not lose control and could factor in any issues the system did not measure that they felt were important. In the first few months of the program, however, several surgeons told patients enquiring about their surgery date to call the hospital because it was now making all decisions. This was ultimately resolved after greater familiarization with the program. Also, one surgeon suggested that he would try to sabotage the program by instructing his patients to give inappropriate answers to all the questions; subsequent analysis showed that this did not occur.
Surgeons have complained that there is more paperwork for private offices. Computerization of data transfer between the offices and the hospital could significantly reduce the amount of paperwork, but this has not yet been accomplished. Surgeons have also complained that they can no longer give patients a fixed date when the decision to proceed with surgery is made, but can give them only a rough estimate of the expected waiting time. A surgery date can be confirmed only about 3 months in advance.
The scoring system has been criticized for overemphasizing driving, not giving extra credit for people who have dependants for whom they are the sole caregiver, and giving too many points for time waiting. At departmental meetings the consensus has been to leave the model unchanged for now.
The introduction of the MCWLP provides an accurate system to determine the number of patients waiting, their need for cataract surgery and waiting times. Prior estimates of waiting time for cataract surgery in Manitoba (18 weeks by the Fraser Institute19 and 23 weeks [for high-volume cataract surgeons] by the Manitoba Centre for Health Policy and Evaluation20) have been too low.
This program has introduced a greater degree of equality, since all patients are now prioritized by the same criteria. The data for November 1999 show that these factors are now influencing patients' position on their surgeon's waiting list in a significant way; thus, the system is achieving its goal.
The introduction of the MCWLP has brought to light the previously unrecognized issue of the simultaneous booking of both eyes for surgery. It had been assumed when the system was established that the waiting list would reflect the number of patients waiting rather than the number of eyes waiting. However, since in about 10% of cases surgeons are submitting booking requests for both eyes at the same time, the active waiting list records a number waiting that is 10% larger than the number of patients waiting. It is well established that there is benefit equal to that of the first eye for cataract surgery on symptomatic second eyes.21,22
The MCWLP has also brought to light the enormous variation that exists in waiting time between surgeons. Much of this variation arises because of the substantially shorter waiting times for subspecialists. This shorter waiting time is somewhat misleading because subspecialists do substantially lower volumes of cataract surgery than primary cataract surgeons and devote most of their operating room time to cases involving their own subspecialty.
Discussions have commenced with the Regional Health Authority about publishing surgeons' mean waiting times so that patients unhappy with their long wait would have the option of transferring to a surgeon with a shorter wait, but so far no action has been taken. Data from the MCWLP have recently been sent to the Regional Health Authority to petition for increased operating room time to reduce the average waiting time.
Appendix 1.
Footnotes
This article has been peer reviewed.
Acknowledgements: We thank Betty Holunga, Sharon McMichael, Nadine Bain and all the members of the Department of Ophthalmology, Misericordia Health Centre, for assistance in development of the Manitoba Cataract Waiting List Program. We are grateful to Dr. Bonnie Cham for helpful suggestions on an earlier version of the manuscript.
Competing interests: None declared.
Reprint requests to: Dr. Lorne Bellan, Rm. 271, Misericordia Health Centre, 99 Cornish Ave., Winnipeg MB R3C 1A2; fax 204 786-0978; lbellan@miseri.winnipeg.mb.ca
References
- 1.Taylor HR. Cataract: How much surgery do we have to do? [editorial]. Br J Ophthalmol 2000;84(1):1-2. [DOI] [PMC free article] [PubMed]
- 2.Norregaard JC, Bernth-Petersen P, Andersen TF. Changing threshold for cataract surgery in Denmark between 1980 and 1992. Results from the Danish Cataract Surgery Outcomes Study. II. Acta Ophthalmol Scand 1996;74(6):604-8. [DOI] [PubMed]
- 3.Dunn E, Black C, Alonso J, Norregaard JC, Anderson GF. Patients' acceptance of waiting for cataract surgery: What makes a wait too long? Soc Sci Med 1997; 44(11):1603-10. [DOI] [PubMed]
- 4.Lundstrom M, Stenevi U, Thorburn W. Assessment of waiting time and priority setting by means of a national register. Int J Technol Assess Health Care 1996; 12(1):136-40. [DOI] [PubMed]
- 5.Crabtree HL, Hildreth AJ, O'Connell JE, Phelan PS, Allen D, Gray CS. Measuring visual symptoms in British cataract patients: the cataract symptom scale. Br J Ophthalmol 1999;83(5):519-23. [DOI] [PMC free article] [PubMed]
- 6.Uusitalo RJ, Brans T, Pessi T, Tarkkanen A. Evaluating cataract surgery gains by assessing patients' quality of life using the VF-7. J Cataract Refract Surg 1999; 25(7):989-94. [DOI] [PubMed]
- 7.Mangione CM, Lee PP, Pitts J, Gutierrez P, Berry S, Hays RD. Psychometric properties of the National Eye Institute Visual Function Questionnaire (NEI-VFQ). NEI-VFQ Field Test Investigators. Arch Ophthalmol 1998;116 (11):1496-504. [DOI] [PubMed]
- 8.Lundstrom M, Stenevi U, Thorburn W, Roos P. Catquest questionnaire for use in cataract surgery care: assessment of surgical outcomes. J Cataract Refract Surg 1998;24(7):968-74. [DOI] [PubMed]
- 9.Hadorn DC, Holmes AC. The New Zealand priority criteria project. Part 1: Overview [see comments]. BMJ 1997;314:131-4. Comments in: BMJ 1997; 314:1130-1, 1997;314:86-7 and 1999;318:1699. [DOI] [PMC free article] [PubMed]
- 10.Naylor CD, Baigrie RS, Goldman BS, Cairns JA, Beanlands DS, Berman N, et al. Assigning priority to patients requiring coronary revascularization: consensus principles from a panel of cardiologists and cardiac surgeons. Can J Cardiol 1991;7(5):207-13. [PubMed]
- 11.Steinberg EP, Tielsch JM, Schein OD, Javitt JC, Sharkey P, Cassard SD, et al. The VF-14. An index of functional impairment in patients with cataract. Arch Ophthalmol 1994;112(5):630-8. [DOI] [PubMed]
- 12.Norregaard JC, Schein OD, Bellan L, Black C, Alonso J, Bernth-Petersen P, et al. International variation in anesthesia care during cataract surgery: results from the International Cataract Surgery Outcomes Study. Arch Ophthalmol 1997;115(10):1304-8. [DOI] [PubMed]
- 13.Norregaard JC, Schein OD, Anderson GF, Alonso J, Dunn E, Black C, et al. International variation in ophthalmologic management of patients with cataracts. Results from the International Cataract Surgery Outcomes Study. Arch Ophthalmol 1997;115(3):399-403. [DOI] [PubMed]
- 14.Norregaard JC. Cataract surgery. International comparisons of clinical practice. Acta Ophthalmol Scand 1997;75(5):605-6. [DOI] [PubMed]
- 15.Norregaard JC, Bernth-Petersen P, Alonso J, Dunn E, Black C, Andersen TF, et al. Variation in indications for cataract surgery in the United States, Denmark, Canada, and Spain: results from the International Cataract Surgery Outcomes Study [see comment]. Br J Ophthalmol 1998;82(10):1107-11. Comment in: Br J Ophthalmol 1998;82(10):1101-2. [DOI] [PMC free article] [PubMed]
- 16.Cassard SD, Patrick DL, Damiano AM, Legro MW, Tielsch JM, Diener-West M, et al. Reproducibility and responsiveness of the VF-14. An index of functional impairment in patients with cataracts. Arch Ophthalmol 1995;113(12): 1508-13. [DOI] [PubMed]
- 17.Alonso J, Espallargues M, Andersen TF, Cassard SD, Dunn E, Bernth-Petersen P, et al. International applicability of the VF-14. An index of visual function in patients with cataracts. Ophthalmology 1997;104(5):799-807. [DOI] [PubMed]
- 18.Norregaard JC, Hindsberger C, Alonso J, Bellan L, Bernth-Petersen P, Black C, et al. Visual outcomes of cataract surgery in the United States, Canada, Denmark, and Spain. Report from the International Cataract Surgery Outcomes Study. Arch Ophthalmol 1998;116(8):1095-100. [DOI] [PubMed]
- 19.Walker M, Zelder M. Waiting your turn: hospital waiting lists in Canada. In: Critical Issues Bulletin. Vancouver: Fraser Institute; 1999. Available: www.fraserinstitute.ca/publications/critical_issues/1999/waiting_your_turn (accessed 2001 Mar 13).
- 20.DeCoster CA, Carriere KC, Peterson S, Walld R, MacWilliam L. Surgical waiting times in Manitoba. Winnipeg: Centre for Health Policy and Evaluation; 1998. p. 18-23.
- 21.Castells X, Alonso J, Ribo C, Nara D, Teixido A, Castilla M. Factors associated with second eye cataract surgery. Br J Ophthalmol 2000;84(1):9-12. [DOI] [PMC free article] [PubMed]
- 22.Javitt JC, Steinberg EP, Sharkey P, Schein OD, Tielsch JM, Diener M, et al. Cataract surgery in one eye or both. A billion dollar per year issue. Ophthalmology 1995;102(11):1583-92. [DOI] [PubMed]


