Abstract
Background
Transversus abdominis plane block with liposomal bupivacaine has been studied as an effective method of reducing the need for postoperative opioids and increasing same-day discharge rates. However, less is known about the cost-effectiveness of this strategy relative to opioids alone for hernia repair. We performed an economic evaluation of these strategies using a computer simulation model.
Methods
A decision tree was constructed to determine cost-effectiveness as measured by incremental cost-effectiveness ratios per quality-adjusted life-year. Base-case costs, quality-adjusted life-year values, and probabilities were derived from published studies and Medicare fee schedules. For input parameters for which we could not find values in the published literature, we used expert opinion. A 1-month time horizon was selected to focus on the immediate postoperative period. Finally, we performed 1-way, 2-way, and probabilistic sensitivity analyses.
Results
The liposomal bupivacaine transversus abdominis plane block was a dominant strategy yielding a $456.75 decrease in cost and an 0.1 increase in quality-adjusted life-years relative to opioids alone. In 1-way sensitivity analysis of cost incremental cost-effectiveness ratio, values were most sensitive to variations in the amount saved by same-day discharge and the cost of bupivacaine. In probabilistic sensitivity analyses, transversus abdominis plane strategy was cost-effective at a willingness-to-pay threshold of $50,000/quality-adjusted life-year in 94.5% of iterations and at a willingness-to-pay threshold of $100,000/quality-adjusted life-year in 97.1% of iterations.
Conclusion
The use of liposomal bupivacaine transversus abdominis plane block resulted in cost savings and improved quality-adjusted life-years in base-case analyses and was cost-effective at conventional willingness-to-pay thresholds in the majority of iterations in probabilistic sensitivity analyses.
Highlights
-
•
A decision tree was constructed to determine cost-effectiveness as measured by incremental cost-effectiveness ratios (ICER) per quality-adjusted life-year (QALY).
-
•
The liposomal bupivacaine TAP block was a dominant strategy yielding a $456.75 decrease in cost and an 0.1 increase in QALYs relative to opioids alone.
-
•
In 1-way sensitivity analysis of cost, ICER values were most sensitive to variations in the amount saved by SDD and the cost of bupivacaine.
-
•
In probabilistic sensitivity analyses, TAP strategy was cost-effective at a willingness-to-pay threshold of $50,000/QALY in 94.5% of iterations and pay threshold of $100,000/QALY in 97.1% of iterations.
1. BACKGROUND
Transversus abdominis plane (TAP) block with liposomal bupivacaine has been identified as an effective method of reducing the need for postoperative opioids and increasing same-day discharge (SDD) rates in conjunction with Enhanced Recovery After Surgery (ERAS) pathways [1,2]. Early discharge from the hospital after minimally invasive procedures has been shown to be safe in appendectomies, cholecystectomies, hysterectomies, and ventral hernia repairs [[3], [4], [5], [6]]. With this improvement in the safety of surgical procedures, the focus can shift toward a greater understanding of how to more efficiently perform them.
As part of the ERAS pathway, anesthesia techniques that emphasize adequate postoperative pain control while minimizing the use of narcotics have been developed. Adequate pain control maintains homeostasis by blunting the stress response, reducing postoperative ileus, and promoting early mobilization [2]. TAP blocks have been demonstrated to be a useful part of this strategy, in some cases reducing the need for opioids by up to 50% in laparoscopic surgery [1,[7], [8], [9], [10], [11], [12]].
The cost-effectiveness of TAP blocks in laparoscopic hysterectomy for gynecological cancers has been shown in previous studies [13]. The TAP block was cost-effective compared to an oral opioid alone strategy based on the reduced amount of opioids necessary to control pain and the increased rates of SDD. Although TAP block has been shown to be useful in laparoscopic ventral hernia repair, less is known about the cost-effectiveness of this strategy relative to opioids alone [11]. Using a computer simulation model, we estimated the cost-effectiveness at 30 days of TAP versus opioids alone for laparoscopic ventral hernia repair in a general surgery population from a health care system perspective.
2. METHODS
2.1. Decision model
We adapted a previously published decision analytic model by Seagle et al to determine the cost-effectiveness of TAP block with liposomal bupivacaine with routine oral opioids for postoperative pain management versus no TAP and oral opioids alone among patients who underwent a laparoscopic ventral hernia repair [13]. In decision analytic models, the downstream consequences of treatment decisions are simulated based on probability input parameters. Simulated patients then accumulate costs and health benefits or harms depending on the specific combination of clinical events they experience.
Like the previous model, we performed the analysis from a health care system perspective, which means we included only direct medical costs incurred by the health care system. We excluded indirect costs, such as lost days of work, patient time, caregiver time, transportation, and long-term costs, which are necessary for a societal perspective. The model estimated the average costs (in 2017 US $) and quality-adjusted life-years (QALYs) over a 30-day time horizon for simulated patients undergoing each treatment strategy. QALYs, an effectiveness outcome commonly used in cost-effectiveness analyses, accounts for both quality and quantity of life and is calculated by multiplying the sum of time spent in a health state by a utility weight for that health state. Utility weights represent an overall assessment of a patient's well-being and vary from 0 (death) to 1 (perfect health). We calculated the incremental costs and incremental QALYs as the difference in the average costs and QALYs, respectively, calculated from the model for TAP versus opioids alone. We considered one strategy dominant if it both costs less (ie, negative incremental costs) and was more effective (ie, positive incremental QALYs). In the case of both positive incremental costs and incremental QALYs, we determined cost-effectiveness by calculating the incremental cost-effectiveness ratio (ICER), which is the ratio of incremental costs to incremental QALYs. We considered an ICER <$50,000/QALY cost-effective. Our analysis adhered to current best practices for cost-effectiveness analysis (Appendix 1) [14].
In the model, patients were first simulated to receive TAP with liposomal bupivacaine and then simulated again without receiving TAP. In both arms, patients had a chance of SDD or hospital admission, a chance of readmission or no readmission within 30 days, and a chance of opioid use or no opioid use (Appendix 2). For patients receiving opioids, a complication subtree modeled the costs and risk for opioid-related ileus, aspiration, and perforation from Ogilvie syndrome. The TAP arm also included a subtree for complications related to the TAP procedure itself and adverse reactions to the liposomal bupivacaine. We assumed that having one of these complications would lead to a patient being admitted to the hospital. The chance of any complication (most commonly a surgical site infection) and 30-day mortality related to the surgery were included in both arms. Probabilities of death from a bupivacaine adverse reaction (anaphylaxis or arrhythmia), aspiration, and bowel perforation due to Ogilvie syndrome in the ileus group were also included. In patients that used opioids, the probability of mortality was a function of the probability of fatal opioid overdose in the overall population. Model creation, statistical analyses, and figure creation were performed with TreeAge Pro 2017 (TreeAge Software Inc, Williamstown, MA).
As with any simulation model, we made several assumptions in our model and analysis. First, TAP block had a higher rate of SDD than no TAP. This assumption was made based on published SDD rates, decreased pain scores, better 72-hour pain control, and decreased postoperative nausea and vomiting when liposomal bupivacaine is used for regional anesthesia [4,13,15,16]. Second, we assumed that there are no differences in surgical outcomes between the TAP and no-TAP groups because the choice of regional anesthetic should not affect the quality of general anesthesia or interfere with the surgical procedure itself. Third, we assumed that TAP blocks would be readily available and delivered in 1 of 2 fashions: ultrasound-guided block performed by qualified anesthesiologists or laparoscopically by qualified general surgeons. Either modality was assumed to not significantly change operating room time, time under general anesthesia, or overall length of stay as compared to patients not receiving the block; have equal analgesic effect; and not be significantly different in cost [11,12,17]. Finally, we modeled opioid use as a binary rather than a continuous variable because the literature is not specific enough to capture these differences in terms of outcomes.
2.2. Probabilities
Probability inputs for our model were generally derived from published literature and are listed in Table 1. We used study by Mason et al to estimate 30-day mortality after laparoscopic ventral hernia repair as 0.18% [18]. Aspiration with and without ileus were assumed to be 5 and 1%, with a range of 30%. Death from aspiration was assumed to be 1% with a standard variation of 30% [13]. Bowel perforation after ileus and Ogilvie syndrome was 7% with a 12.3% mortality from Ross et al [19]. Bupivacaine adverse events were low at 1.5% [20]; death from these was assumed to be rare at 0.1% [13]. Laparoscopic ventral hernia repair had a complication rate of 3.8% [18]. The chance of fatal opioid overdose was taken from overall population overdose rates [21]. We estimated the use of opioids for postoperative pain to be 95% in patients without TAP block compared to 50% with TAP [1,[7], [8], [9], [10],22]. Ileus after surgery with and without opioids was low and derived from Goestch et al at 1.43% and 0.17% [23]. SDD after TAP was estimated to be 80% for the base-case model. For those not receiving TAP, we estimated SDD rates at 65% of the probability of those receiving TAP based on the literature describing outpatient surgery for laparoscopic ventral hernia repair [4,15,16]. Readmission after SDD and admission in the TAP and no-TAP groups were 2.5% and 4% based on expert opinion and an American College of Surgeons National Surgical Quality Improvement Program study looking at discharge rates after laparoscopic hysterectomy [3]. Finally, TAP procedure complications were rare at 0.1%, and no deaths have been reported in the literature [20].
Table 1.
Probability estimates
| Probability | Base value (%) | Range (%) | Distribution | Reference |
|---|---|---|---|---|
| 30-d mortality | 0.0018 | 0.001–0.003 | β | [18] |
| Aspiration with ileus | 5.0 | 3.5–6.5 | β | Assumed [13] |
| Aspiration without ileus | 1 | 0.7–1.3 | β | Assumed [13] |
| Death by aspiration | 1 | 0.7–1.3 | β | Assumed [13, |
| Bowel perforation with ileus | 7 | 5–8 | β | 19] |
| Death by bowel perforation | 12.3 | 7–15 | β | [19] |
| Bupivacaine adverse event | 1.5 | 0–3 | β | [20] |
| Death by bupivacaine adverse event | 0.1 | 0–0.2 | β | Assumed [13] |
| Composite complication | 3.8 | 1–13 | β | [18] |
| Fatal opioid overdose | 0.001 | 0–0.002 | β | [21] |
| Opioid use without TAP block | 95 | 66.5–100 | β | Assumed [13] |
| Fraction opioid decrease with TAP | 50 | 30–100 | β | [1,5,[7], [8], [9], [10], [11], [12],22] |
| Postoperative ileus with opioids | 1.43 | 0.43–2.43 | β | [23] |
| Postoperative ileus without opioids | 0.17 | 0–0.34 | β | [23] |
| SDD, TAP | 80 | 20–99 | β | [4,15,16] |
| SDD decrease without TAP | 65 | 20–80 | β | [4,15,16] |
| Readmission after SDD, TAP | 2.5 | 0.5–5 | β | [3] |
| Readmission SDD, no TAP | 2.5 | 0.5–5 | β | [3] |
| Readmission after admission, TAP | 4 | 0.5–5 | β | [3] |
| Readmission after admission, no TAP | 4 | 0.5–5 | β | [3] |
| TAP procedure complication | 0.1 | 0–0.2 | β | [20] |
2.3. Costs
Cost data are shown in Table 2. Drug prices were obtained from monthly wholesale data from UpToDate. Liposomal bupivacaine was modeled as 1 vial of Exparel for $204. Treatment for uncomplicated aspiration was assumed to be ampicillin-clavulanate 875–125 mg orally twice a day for 3 days. Bilateral TAP injection (Current Procedural Terminology [CPT] code 64488) was priced using the online 2017 fee schedule from the Centers for Medicare and Medicaid Services (CMS). Cardiopulmonary resuscitation (CPT code 92950) was used as a proxy for the cost of a serious bupivacaine-related adverse event. Cost of composite complications was assumed to be the cost of a surgical site infection, the most common complication after laparoscopic ventral hernia repair, treated with 5 days of cephalexin 500 mg by mouth 4 times a day. Total cost of surgery and associated complications were from Ecker et al using a statewide claims database [24]. The cost reduction for SDD was derived from the average cost per day in the United States among nonprofit hospitals [25]. Cost of ileus was from Asgeirsson et al [26]. Costs for nonfatal bowel perforation due to Oglivie syndrome as a result of ileus was from Ross et al [19]. Cost for readmissions was from published data by Seagle et al [13,27]. Cost of a serious TAP block complications was assumed to be the cost of the abdomen and pelvis computed tomography scan necessary to diagnose it (CPT code 74177) [20].
Table 2.
Cost estimates
| Cost | Base Case ($) | Range ($) | Distribution | Reference |
|---|---|---|---|---|
| 30-d mortality | 5,000 | 3,500–6,500 | γ | Assumed [13] |
| Aspiration | 30 | 0–100 | γ | UpToDate |
| Composite complication | 209 | 100–300 | γ | UpToDate |
| Cost reduction for SDD | 2,271 | 1,000–4,000 | γ | [25] |
| Laparoscopic ventral hernia repair | 10,948 | 2,000–20,000 | γ | [24] |
| Liposomal bupivacaine | 204 | 50–350 | γ | UpToDate |
| Liposomal bupivacaine adverse event | 210 | 100–300 | γ | CMS |
| Nonfatal bowel perforation | 101,853 | 20,000–200,000 | γ | [26] |
| Oral opioids | 16 | 10–25 | γ | UpToDate |
| Postoperative ileus | 8,296 | 1,000–15,000 | γ | [26] |
| Readmission | 10,000 | 5,000–15,000 | γ | [13,27] |
| TAP complication | 316 | 200–450 | γ | CMS |
| TAP procedure | 84 | 75–100 | γ | CMS |
2.4. Effectiveness
Utility values used to estimate QALYs are listed in Table 3. The utility of being alive after a laparoscopic ventral hernia repair was 0.76. This was based on the analysis of the repair of a reducible ventral hernia by Stey et al [28]. Having a complication decreased utility during the 30-day time frame by 30%. Having a bowel perforation during this time frame was assumed to decrease utility by 80%. Based on patient satisfaction scores in a randomized trial of TAP blocks in laparoscopic hysterectomy, we used a 10% increase in utility with TAP [8,29].
Table 3.
Utility estimates
| Utility | Value | Range | Distribution | Source |
|---|---|---|---|---|
| Alive with ventral hernia repaired | 0.76 | 0.69–0.79 | β | [28] |
| Alive with complications | − 30%⁎ | [13] | ||
| Alive with perforation | − 80%⁎ | [13] | ||
| Utility addition after TAP | + 10%⁎ | 0.0–0.15 | β | [1,[7], [8], [9], [10], [11], [12]] |
Percentage that these conditions change the baseline.
2.5. Sensitivity analysis
We performed 1-way sensitivity analyses for all model inputs, which examine the impact on cost-effectiveness of independently varying each parameter over a plausible range while holding all others at their base-case values. The results from the 1-way sensitivity analyses are reported as tornado diagrams. The ranges in Table 1, Table 2 for costs and probabilities were used in 1-way sensitivity analyses. A 1-way sensitivity analysis was performed on the SDD probability in each arm. We performed probabilistic sensitivity analysis (PSA) by running 10,000 iterations of our model, each iteration with a different random draw of parameter values from distributions characterized by mean and standard deviations specific to each parameter. These PSAs were used to generate 95% uncertainty intervals for the base-case model ICER value estimate and results from the 10,000 iterations presented as cost-effectiveness acceptability curves (CEACs). CEACs depict the proportion of the 10,000 iterations for which each strategy was cost-effective for a range of willingness-to-pay thresholds for cost-effectiveness.
3. RESULTS
3.1. Base-case analysis
Liposomal bupivacaine TAP block dominated no TAP in the base-case analysis, costing $457 less and yielding 0.1 more QALY (Table 4). If the assumed that the 0.1 increase in QALY due to TAP was not present, the TAP strategy was still cost saving due to decreasing cost at the same effectiveness.
Table 4.
Cost-effectiveness of TAP with liposomal bupivacaine compared to no TAP
| Strategy | Cost ($) | Incremental cost ($) | 30-d QALY | Incremental | ICER($/QALY) |
|---|---|---|---|---|---|
| TAP | 9,877 | − 457 | 0.07 | 0.01 | − 54,632 (dominant) |
| No TAP | 10,333 | 0.06 |
3.2. Sensitivity analyses
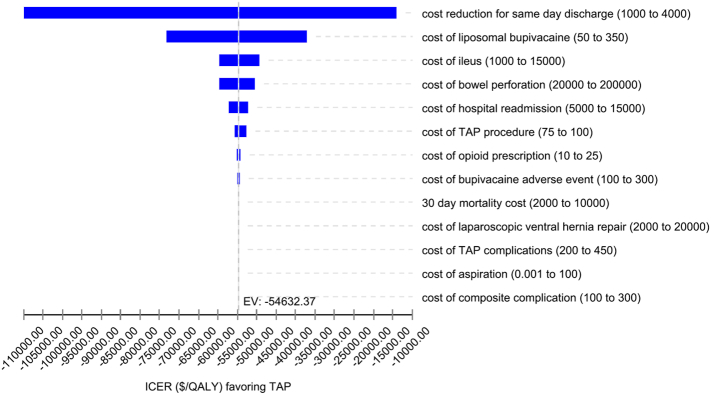
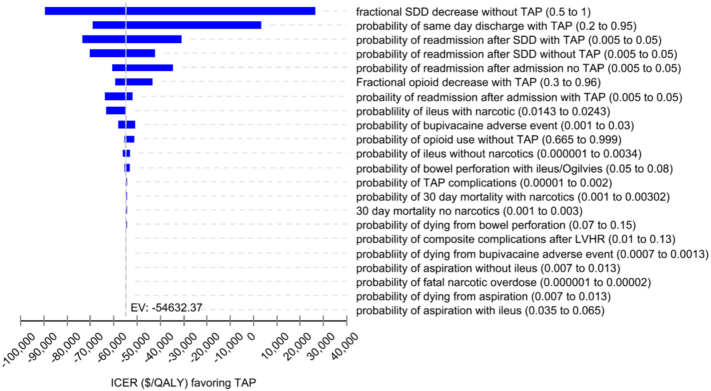
In 1-way sensitivity analysis, ICER values were most sensitive to variations in the amount saved by SDD compared to being admitted and the cost of bupivacaine (Fig. 1). For probabilities, ICER values were most sensitive to the fractional decrease in SDD without TAP and the probability of SDD with TAP (Fig. 2). When both strategies had an equal chance of SDD (90%), the TAP group was still cost-effective at a willingness to pay of $50,000/QALY.
Fig. 1.
One-way sensitivity analysis of cost estimates.
Fig. 2.
One-way sensitivity analysis of probability estimates.
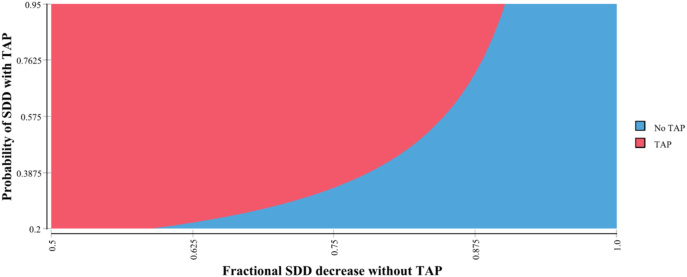
The threshold analysis for the probability of SDD in the TAP (range 20%–99%) and oral opioid arms (range 20%–80%), with willingness to pay set to $0/QALY to indicate the cost saving strategy, showed that at even at a low SDD probability in the TAP group, TAP was cost saving (Fig. 3). The no-TAP arm became more cost-effective if the chance of being discharged the same day approached zero.
Fig. 3.
Two-way sensitivity analysis for TAP versus no TAP.
Red area is when TAP strategy is cost saving, and blue area is when no-TAP strategy is cost saving.
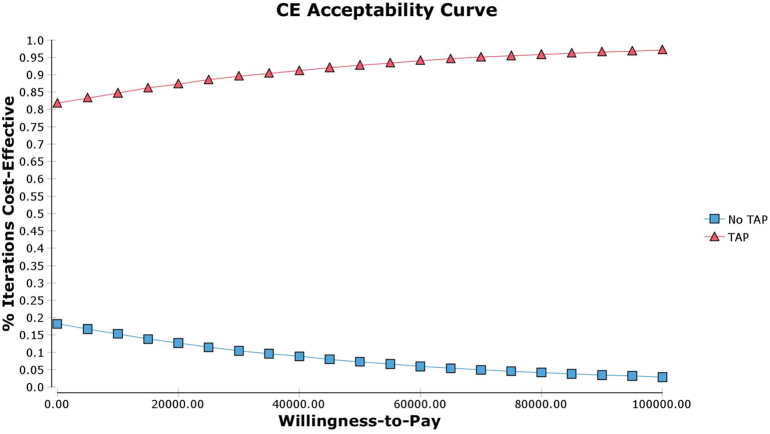
In PSA, TAP strategy was cost-effective at a willingness-to-pay threshold of $50,000/QALY in 94.5% of iterations and at a willingness-to-pay threshold of $100,000/QALY in 97.1% of iterations (Fig. 4). Additional PSAs were run with different major assumptions of the model and showed consistent results. If both groups were allowed to have the same chance of SDD, then the TAP group was cost-effective in 70.0% of iterations. Second, if the cost of liposomal bupivacaine was increased to $350, the high end of list costs, with a range of $250–$400, TAP strategy was still cost-effective 89.0% of the time. Third, if the utility benefit of the TAP block was removed, the TAP strategy was still cost-effective in 92.6% of simulations.
Fig. 4.
Cost-effectiveness acceptability curves for TAP versus no-TAP strategies from probabilistic sensitivity analyses.
4. DISCUSSION
In this computer simulation, the use of liposomal bupivacaine TAP block resulted in cost savings, improved QALYs in base-case analyses, and was cost-effective at conventional willingness-to-pay thresholds in the vast majority of iterations in probabilistic sensitivity analyses. This finding was robust to many variations in base-case parameters and in the probabilistic sensitivity analysis. The primary results of the model do not change even if major model assumptions and parameter inputs are varied, including varying SDD rates across a wide range of values. This is important because the analysis was most sensitive to changes in the SDD rate between patients that received TAP block versus those on an oral opioid only strategy. The 2-way sensitivity analysis also showed that the TAP strategy was cost-effective even at low SDD probabilities.
SDD after laparoscopic ventral hernia repair is quite variable nationally [3,15,18,24,30]. Minimizing unnecessary time spent in the hospital is a reasonable component of efficiency as long as it can be done without compromising patient care. This SDD approach has been shown to be effective in many laparoscopic procedures, including hysterectomy, appendectomy, cholecystectomy, and inguinal herniorrhaphy [3,4,15,16,18,24,30]. Laparoscopic ventral hernia repair can follow the same expedited recovery pathways as these other operations safely and thus save money without compromising quality [30]. Our group has shown in work relating to SDD protocols for appendectomy that it takes a coordinated effort by surgeons, anesthesiologists, and nursing staff to do this, but it is achievable.
Several limitations to our study are important to note. As with any simulation model, the input parameters from our model were determined by literature review and expert opinion. We have the benefit of basing this analysis on the work previously published by Seagle et al examining the benefit of TAP blocks for laparoscopic hysterectomy for endometrial cancer. They however based their SDD rates and opioid consumption on TAP blocks covering the T10 to L1 dermatomes. Fields et al showed that TAP block covering the T7 to T11 dermatome is effective in reducing pain scores and opioid use in ventral hernia repair using bupivacaine. There are currently no data directly comparing TAP block with bupivacaine to TAP block with liposomal bupivacaine in ventral hernia repair. As multiple studies have shown that TAP blocks are effective in other kinds of laparoscopic surgery with a similar number of port sites, it is reasonable to assume that this holds true in our simulations. We tried to account for this by having relatively large ranges in SDD rates and opioid consumption. Further clinical trials will be necessary to determine if this is true in clinical practice. Our model also did not account for all possible complications of having a ventral hernia repair, even when limited to the 30.5-day time horizon. Complications related to longer hospitalizations may increase costs for those admitted or readmitted. Major complications are however uncommon in this procedure. Furthermore, local variations of availability and expertise of anesthesiologists and surgeons with TAP block techniques may limit the applicability of these findings.
In conclusion, TAP block with liposomal bupivacaine is robustly cost-effective compared to an oral opioid-only strategy for patients receiving laparoscopic ventral hernia repair in our computer simulation. This research supports further studies examining remaining questions such as TAP block placement by anesthesiologists versus surgeons, type of local anesthetic used, and further refinement of the TAP block technique. This strategy could be incorporated into multimodal anesthesia protocols for ERAS and SDD protocols to fast track the appropriate postoperative patients.
Author contribution
Study conception and design: Colonna, Bellows, Nirula, Nelson.
Acquisition of data: Colonna, Bellows, Nelson.
Analysis and interpretation of data: Colonna, Bellows, Enniss, McCrum, Nunez, Young, Nirula, Nelson.
Drafting of manuscript: Colonna, Bellows, Enniss, McCrum, Nunez, Young, Nirula, Nelson.
Critical revision: Colonna, Bellows, Enniss, McCrum, Nunez, Young, Nirula, Nelson.
Conflict of interest
None.
Funding sources
The research reported in this publication was supported (in part or in full) by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR002538. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The following are the supplementary data related to this article.
Reporting checklist for cost-effectiveness analyses from the Second Panel on Cost-Effectiveness in Health and Medicine
Decision tree model
Contributor Information
Alexander L. Colonna, Email: alexander.colonna@hsc.utah.edu.
Brandon K. Bellows, Email: brandon.bellows@pharm.utah.edu.
Toby M. Enniss, Email: toby.enniss@hsc.utah.edu.
Jason B. Young, Email: jason.b.young@hsc.utah.edu.
Marta McCrum, Email: marta.mccrum@hsc.utah.edu.
Jade M. Nunez, Email: jade.nunez@hsc.utah.edu.
Raminder Nirula, Email: r.nirula@hsc.utah.edu.
Richard E. Nelson, Email: Richard.Nelson@utah.edu.
References
- 1.Keller D.S., Pedraza R., Tahilramani R.N., Flores-Gonzalez J.R., Ibarra S., Haas E.M. Impact of long-acting local anesthesia on clinical and financial outcomes in laparoscopic colorectal surgery. Am J Surg. 2017 Jul;214(1):53–58. doi: 10.1016/j.amjsurg.2015.10.035. [DOI] [PubMed] [Google Scholar]
- 2.Ljungqvist O., Scott M., Fearon K.C. Enhanced recovery after surgery: a review. JAMA Surg. 2017 Mar 1;152(3):292–298. doi: 10.1001/jamasurg.2016.4952. [DOI] [PubMed] [Google Scholar]
- 3.Lee J., Aphinyanaphongs Y., Curtin J.P., Chern J.Y., Frey M.K., Boyd L.R. The safety of same-day discharge after laparoscopic hysterectomy for endometrial cancer. Gynecol Oncol. 2016 Sep;142(3):508–513. doi: 10.1016/j.ygyno.2016.06.010. [DOI] [PubMed] [Google Scholar]
- 4.Shaikh I., Willder J.M., Kumar S. Same day discharge, surgical training and early complications after open and laparoscopic repair of primary paraumbilical hernia. Hernia. 2013 Aug;17(4):505–509. doi: 10.1007/s10029-013-1052-4. [DOI] [PubMed] [Google Scholar]
- 5.Elamin G., Waters P.S., Hamid H. Efficacy of a laparoscopically delivered transversus abdominis plane block technique during elective laparoscopic cholecystectomy: a prospective, double-blind randomized trial. J Am Coll Surg. 2015 Aug;221(2):335–344. doi: 10.1016/j.jamcollsurg.2015.03.030. [DOI] [PubMed] [Google Scholar]
- 6.Scott A., Shekherdimian S., Rouch J.D. Same-day discharge in laparoscopic acute non-perforated appendectomy. J Am Coll Surg. 2017 Jan;224(1):43–48. doi: 10.1016/j.jamcollsurg.2016.10.026. [DOI] [PubMed] [Google Scholar]
- 7.Fayezizadeh M., Majumder A., Neupane R., Elliott H.L., Novitsky Y.W. Efficacy of transversus abdominis plane block with liposomal bupivacaine during open abdominal wall reconstruction. Am J Surg. 2016 Sep;212(3):399–405. doi: 10.1016/j.amjsurg.2015.12.026. [DOI] [PubMed] [Google Scholar]
- 8.Hutchins J., Vogel R.I., Ghebre R. Ultrasound-guided subcostal transversus abdominis plane infiltration with liposomal bupivacaine for patients undergoing robotic-assisted hysterectomy: a retrospective study. Int J Gynecol Cancer. 2015 Jun;25(5):937–941. doi: 10.1097/IGC.0000000000000429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jablonka E.M., Lamelas A.M., Kim J.N. Transversus abdominis plane blocks with single-dose liposomal bupivacaine in conjunction with a nonnarcotic pain regimen help reduce length of stay following abdominally based microsurgical breast reconstruction. Plast Reconstr Surg. 2017 Aug;140(2):240–251. doi: 10.1097/PRS.0000000000003508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim A.J., Yong R.J., Urman R.D. The role of transversus abdominis plane blocks in enhanced recovery after surgery pathways for open and laparoscopic colorectal surgery. J Laparoendosc Adv Surg Tech A. 2017 Sep;27(9):909–914. doi: 10.1089/lap.2017.0337. [DOI] [PubMed] [Google Scholar]
- 11.Fields A.C., Gonzalez D.O., Chin E.H., Nguyen S.Q., Zhang L.P., Divino C.M. Laparoscopic-assisted transversus abdominis plane block for postoperative pain control in laparoscopic ventral hernia repair: a randomized controlled trial. J Am Coll Surg. 2015 Aug;221(2):462–469. doi: 10.1016/j.jamcollsurg.2015.04.007. [DOI] [PubMed] [Google Scholar]
- 12.Zaghiyan K.N., Mendelson B.J., Eng M.R., Ovsepyan G., Mirocha J.M., Fleshner P. Randomized clinical trial comparing laparoscopic versus ultrasound-guided transversus abdominis plane block in minimally invasive colorectal surgery. Dis Colon Rectum. 2019 Feb;62(2):203–210. doi: 10.1097/DCR.0000000000001292. [DOI] [PubMed] [Google Scholar]
- 13.Seagle B.L., Miller E.S., Strohl A.E., Hoekstra A., Shahabi S. Transversus abdominis plane block with liposomal bupivacaine compared to oral opioids alone for acute postoperative pain after laparoscopic hysterectomy for early endometrial cancer: a cost-effectiveness analysis. Gynecol Oncol Res Pract. 2017;4:12. doi: 10.1186/s40661-017-0048-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sanders G.D., Neumann P.J., Basu A. Recommendations for conduct, methodological practices, and reporting of cost-effectiveness analyses: second panel on cost-effectiveness in health and medicine. JAMA. 2016 Sep 13;316(10):1093–1103. doi: 10.1001/jama.2016.12195. [DOI] [PubMed] [Google Scholar]
- 15.Lorente-Herce J.M., Marin-Morales J., Jimenez-Vega F.J. Laparoscopic incisional hernia repair in an ambulatory surgery-extended recovery centre: a review of 259 consecutive cases. Hernia. 2015 Jun;19(3):487–492. doi: 10.1007/s10029-014-1229-5. [DOI] [PubMed] [Google Scholar]
- 16.Wright B.E., Beckerman J., Cohen M., Cumming J.K., Rodriguez J.L. Is laparoscopic umbilical hernia repair with mesh a reasonable alternative to conventional repair? Am J Surg. 2002 Dec;184(6):505–508. doi: 10.1016/s0002-9610(02)01071-1. [discussion 8-9] [DOI] [PubMed] [Google Scholar]
- 17.Park S.Y., Park J.S., Choi G.S., Kim H.J., Moon S., Yeo J. Comparison of analgesic efficacy of laparoscope-assisted and ultrasound-guided transversus abdominis plane block after laparoscopic colorectal operation: a randomized, single-blind, non-inferiority trial. J Am Coll Surg. 2017 Sep;225(3):403–410. doi: 10.1016/j.jamcollsurg.2017.05.017. [DOI] [PubMed] [Google Scholar]
- 18.Mason R.J., Moazzez A., Sohn H.J., Berne T.V., Katkhouda N. Laparoscopic versus open anterior abdominal wall hernia repair: 30-day morbidity and mortality using the ACS-NSQIP database. Ann Surg. 2011 Oct;254(4):641–652. doi: 10.1097/SLA.0b013e31823009e6. [DOI] [PubMed] [Google Scholar]
- 19.Ross S.W., Oommen B., Wormer B.A. Acute colonic pseudo-obstruction: defining the epidemiology, treatment, and adverse outcomes of Ogilvie’s syndrome. Am Surg. 2016 Feb;82(2):102–111. doi: 10.1177/000313481608200211. [DOI] [PubMed] [Google Scholar]
- 20.Young M.J., Gorlin A.W., Modest V.E., Quraishi S.A. Clinical implications of the transversus abdominis plane block in adults. Anesthesiol Res Pract. 2012;2012 doi: 10.1155/2012/731645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Paulozzi L.J., Budnitz D.S., Xi Y. Increasing deaths from opioid analgesics in the United States. Pharmacoepidemiol Drug Saf. 2006 Sep;15(9):618–627. doi: 10.1002/pds.1276. [DOI] [PubMed] [Google Scholar]
- 22.Malik O., Kaye A.D., Kaye A., Belani K., Urman R.D. Emerging roles of liposomal bupivacaine in anesthesia practice. J Anaesthesiol Clin Pharmacol. 2017 Apr-Jun;33(2):151–156. doi: 10.4103/joacp.JOACP_375_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goettsch W.G., Sukel M.P., van der Peet D.L., van Riemsdijk M.M., Herings R.M. In-hospital use of opioids increases rate of coded postoperative paralytic ileus. Pharmacoepidemiol Drug Saf. 2007 Jun;16(6):668–674. doi: 10.1002/pds.1338. [DOI] [PubMed] [Google Scholar]
- 24.Ecker B.L., Kuo L.E., Simmons K.D., Fischer J.P., Morris J.B., Kelz R.R. Laparoscopic versus open ventral hernia repair: longitudinal outcomes and cost analysis using statewide claims data. Surg Endosc. 2016 Mar;30(3):906–915. doi: 10.1007/s00464-015-4310-y. [DOI] [PubMed] [Google Scholar]
- 25.Kaiser state health facts. Available at: https://www.kff.org/health-costs/state-indicator/expenses-per-inpatient-day/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D. Accessed September 1st, 2017.
- 26.Asgeirsson T., El-Badawi K.I., Mahmood A., Barletta J., Luchtefeld M., Senagore A.J. Postoperative ileus: it costs more than you expect. J Am Coll Surg. 2010 Feb;210(2):228–231. doi: 10.1016/j.jamcollsurg.2009.09.028. [DOI] [PubMed] [Google Scholar]
- 27.Seagle B.L., Shahabi S. Cost-effectiveness analysis of dose-dense versus standard intravenous chemotherapy for ovarian cancer: an economic analysis of results from the gynecologic oncology group protocol 262 randomized controlled trial. Gynecol Oncol. 2017 Apr;145(1):9–14. doi: 10.1016/j.ygyno.2017.02.014. [DOI] [PubMed] [Google Scholar]
- 28.Stey A.M., Danzig M., Qiu S., Yin S., Divino C.M. Cost-utility analysis of repair of reducible ventral hernia. Surgery. 2014 Jun;155(6):1081–1089. doi: 10.1016/j.surg.2014.03.041. [DOI] [PubMed] [Google Scholar]
- 29.Hutchins J., Delaney D., Vogel R.I. Ultrasound guided subcostal transversus abdominis plane (TAP) infiltration with liposomal bupivacaine for patients undergoing robotic assisted hysterectomy: a prospective randomized controlled study. Gynecol Oncol. 2015 Sep;138(3):609–613. doi: 10.1016/j.ygyno.2015.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Franklin M.E., Jr., Gonzalez J.J., Jr., Glass J.L., Manjarrez A. Laparoscopic ventral and incisional hernia repair: an 11-year experience. Hernia. 2004 Feb;8(1):23–27. doi: 10.1007/s10029-003-0163-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Reporting checklist for cost-effectiveness analyses from the Second Panel on Cost-Effectiveness in Health and Medicine
Decision tree model