Abstract
Background
Group B Streptococcus (GBS) infection is the leading cause of septicemia, meningitis, and pneumonia in neonates. Aberrant gut colonization in early life may predispose children to various diseases in adulthood. However, the associations between gut microbial changes and GBS colonization is still unclear.
Results
The composition and diversity of meconium microbiota in GBS group were similar to that of healthy controls. However, we identified several specific taxa that were differentially abundant between the two groups (linear discriminant analysis (LDA) effect size (LEfSe): p < 0.05, LDA > 2.0). Particularly, the relative abundance of Lactobacillus paracasei was significantly reduced, indicating a role in GBS colonization.
Conclusions
Our study presented a series of bacterial species colonized by GBS, thus providing novel evidence in support of initial intestinal microbiota dysbiosis in the neonates with mother’s GBS colonization.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12866-021-02204-3.
Keywords: Group B Streptococcus (GBS) colonization, Gut microbiota, Microarray-based technique
Background
Group B Streptococcus (GBS) are β-hemolytic and Gram-positive bacteria, which are recognized as a leading cause of neonatal early-onset sepsis (EOS), meningitis, and pneumonia [1, 2]. The mother-to-child vertical transmission is the major GBS infection route in neonatal periods. Previous studies have shown that the prevalence of GBS colonization in vagina during pregnancy is approximately 10–30% [3, 4] and the neonatal morbidity rate for acquiring GBS through birth canal is 60% [5]. The implementation of intrapartum antibiotic prophylaxis (IAP) in pregnant women with GBS colonization is a preventive treatment for reducing the risk of GBS-induced neonatal EOS [6]. However, IAP might also disrupt the balance between microbial members of the gut microbiota [7–9].
Recent evidences indicated that the disturbance of gut microbiome has been involved in potential prenatal and early life of infant [10, 11]. For example, Cassidy-Bushrow et al. observed that Clostridiaceae, Ruminococcoceae, and Enterococcaceae were significantly enriched in infants of GBS positive (GBS+) mothers compared to infants of GBS negative (GBS-) ones [12]. Rosen et al. reported 18 taxa that were found to be significantly associated with GBS carriage [13].
Meconium, as the first stool of infant, is made up of materials ingested in utero and considered as a good source for studying the microbiome of the maternal-fetal interface [14]. Based on the advancement in the technologies and methodologies to identify the microbiota, a number of studies have highlighted the possible microbial presence in the meconium which is partially similar to adult gut microbiome [15] and the microbiome of placenta/amniotic fluid [16]. These studies support the colonization of the fetal gut that may begin in utero due to contact with the placenta and/or amniotic fluid.
Although these aforementioned studies provided clues about the origin of microbiome of meconium and how GBS alter the vaginal microbiome of pregnant women, the origin of prenatal microbiome, expecially the placental microbiome, is still a lively debated focus in the recent year [17]. A study by de Goffau MC and his colleagues showed that human placenta has no microbiome except for potential pathogens such as GBS colonization [18]. Regarding the relationship between the gut microbiota of infants and maternal GBS colonization remains also largely unknown. In this study, we adopted a new microarray-based technique [19] to characterize the fecal samples of the neonates in GBS+ group as compared with control group. The study aimed to investigate the influence of maternal GBS colonization on the gut microbiome of newborns, with the intention of improving perinatal infant care.
Results
The clinical information in the study
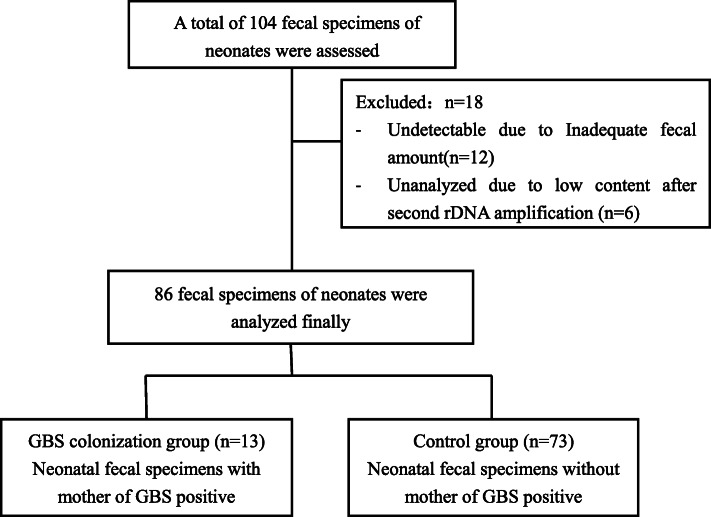
A total of 104 neonatal fecal specimens were collected during the study period. Of these, 12 fecal samples were undetectable due to inadequate amount of total DNA after extraction and 6 fecal samples were further excluded due to low content of 16S rDNA after amplification. Finally, 86 fecal samples from neonates were analyzed. The flowchart of the study is shown in Fig. 1.
Fig. 1.
The flowchart of this study
The clinical characteristics of the 86 neonates are shown in Table 1. There were no difference between two groups except in the term of gestational age and antibiotics exposure after birth.
Table 1.
The clinical information between GBS+ and control groups
| Parameters | GBS + group (n = 13) |
Control group (n = 73) |
OR (95%CI) | P value |
|---|---|---|---|---|
| Neonatal features | ||||
| Gestational age, W | 39.5 ± 0.6 | 38.8 ± 1.9 | – | 0.009 |
| Birth weight, g | 3192 ± 218 | 3121 ± 515 | – | 0.4 |
| Male, (n, %) | 8 (61.5) | 39 (53.4) | 1.4 (0.4 ~ 4.7) | 0.6 |
| Cesarean section (n, %) | 2 (15.4) | 30 (41.1) | 0.3 (0.05 ~ 1.3) | 0.1 |
| Antibiotics exposure | 10 (76.9) | 30 (41.1) | 4.8 (1.2 ~ 18.8) | 0.017 |
| Mother complication | ||||
| PROM (n, %) | 2 (15.4) | 17 (23.3) | 0.6 (0.1 ~ 2.9) | 0.8 |
| Intrapartum fever history | 0 (0) | 7 (9.6) | 0.8 (0.8 ~ 0.9) | 0.5 |
| GDM (n, %) | 1 (7.7) | 27 (37.0) | 0.1 (0.02 ~ 1.15) | 0.07 |
| Placental abruption | 0 (0) | 1 (1.4) | – | 1.0# |
| MSAF (n, %) | 1 (7.7) | 23 (31.5) | 0.2 (0.02 ~ 1.44) | 0.1 |
| IAP exposure | 11 (84.6) | 44 (60.3) | 3.6 (0.7 ~ 17.6) | 0.17 |
PROM Prelabor rupture of the membranes, GDM Gestational diabetes mellitus, MSAF Meconium- stained amniotic fluid, IPA Intrapartum antibiotics prophylaxis
#Fisher exact test
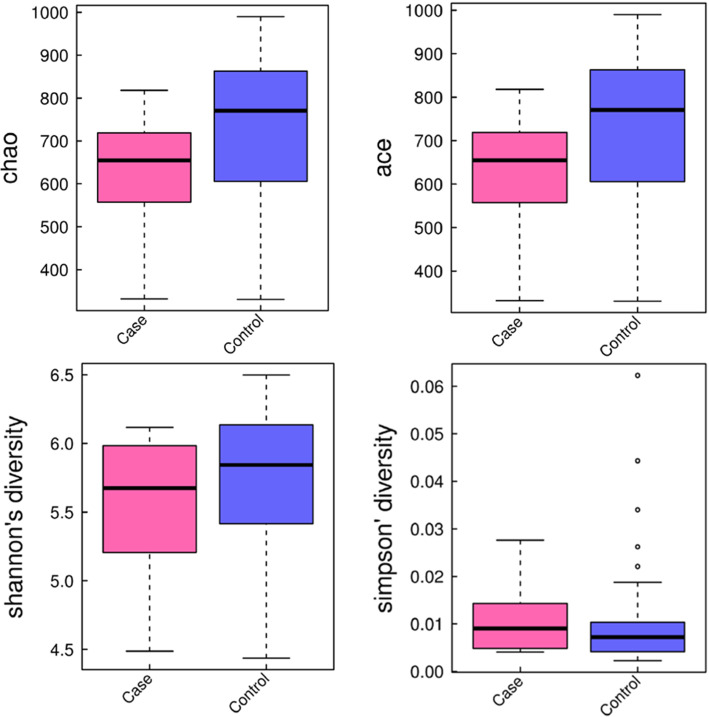
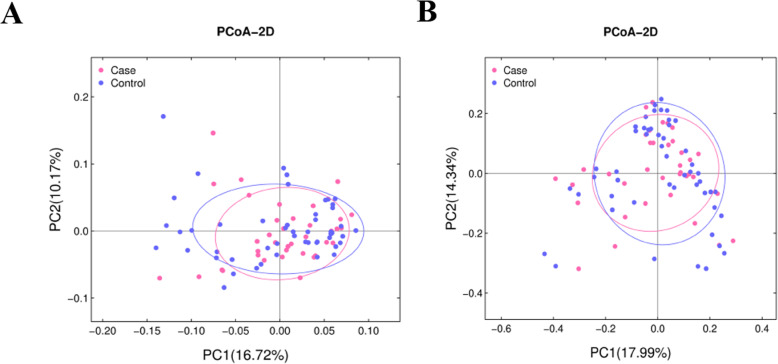
Comparison of α- and β-diversity between two groups
To evaluate the differences in composition of gut microbiota, we performed α- and β-diversity analyses. Several α-diversity indexes including Chao, Ace, Shannon and Simpson (Fig. 2) indicated no significant difference in species richness and diversity between GBS+ and control groups. As to β-diversity, as β-diversity indicators, were applied to estimate the dissimilarity between samples. PCoA plots based on weighted Unifrac distance and Bray Curtis distance showed that the controls clustered more tightly than the infants in GBS+ group (Fig. 3), indicating similar bacterial compositions in the controls. Furthermore, the exposure to infants to antibiotics did not significantly change the gut microbiota in infants of GBS infected group and control group (Figure S1).
Fig. 2.
Box plot of Chao, Ace, Shannon and Simpson indexes
Fig. 3.
Gut bacterial community analysis of infants in GBS+ and control groups. Principal coordinates analysis (PCoA) plots based on weighted Unifrac distance (a) and Bray Curtis distance (b)
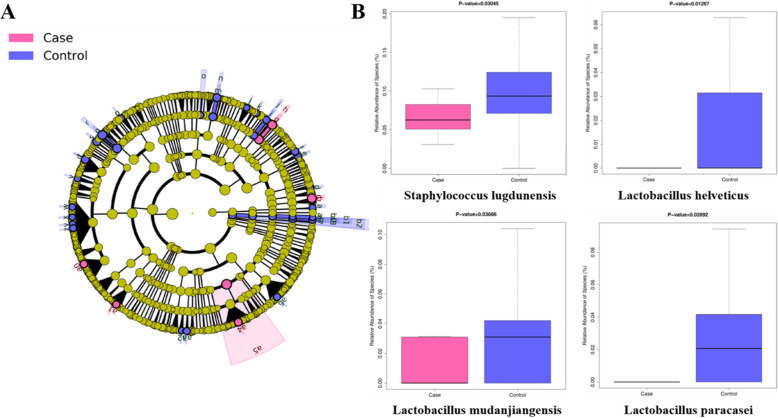
Alteration of taxa in the GBS+ and control groups
To identify the specific taxa associated with GBS infection, a comparison of the microbiota between the infants in GBS+ and control groups was conducted by the Linear discriminant (LDA) and effect size (LEfSe) approach. A cladogram represented the significant structure of the gut microbiota from phylum level to species level (Fig. 4a), which listed a collection of the differential abundant bacteria between two groups. Particularly, the abundance of Staphylococcus lugdunensis, Lactobacillus helveticus, Lactobacillus mudanjiangensis, Lactobacillus paracasei in the infants with GBS + group were reduced as compared to the controls.
Fig. 4.
Different profiles of gut microbiota in meconium between infants in GBS+ and control groups. a Cladogram of differentially abundant taxa, from the phylum level down to the species level. b The relative abundance of certain taxa associated with GBS infection
Discussion
The imbalance of bacterial communities in infants has a profound impact on host’s health, but there is insufficient evidence to suggest the associations between dysbiosis in meconium and bacterial colonization such as GBS colonization. In this context, identification of the factors affecting the morbidity for gestational GBS-related colonization is an important issue that needs to be addressed.
In this study, bacterial composition and diversity showed no significant differences between infants in GBS+ and control groups. However, we found a lower abundance of Staphylococcus and Lactobacillus in the infants with GBS+ mothers, which was in line with previous studies. Staphylococcus lugdunensis is a coagulase-negative Staphylococcus [20], which has been implicated as the main pathogen in various infections, including central nervous system infections, urinary tract infections, and systemic infections [20–23]. A study from Japan reported that the GBS detection was correlated with significantly lower probability of coagulase-negative Staphylococcus [24]. Furthermore, Altoparlak et al. reported that the decreased level of Lactobacillus species was associated with detection of GBS colonization [25]. Kubota et al. demonstrated that GBS positive women had lower percentages of Lactobacillus than GBS negative women [24]. It should be noted that certain Lactobacillus such as Lactobacillus paracasei had the capabilities to prevent GBS adherence to vaginal epithelial cells [26], and antimicrobial activity of Lactobacillus against GBS had been documented in vitro [27]. Moreover, this lower Lactobacillus species had been detected in the neonatal EOS recently [28]. Thus, the reduced abundance of above genera might limit the protective role of microbiome so as to increase susceptibility to infection.
Although intrapartum antibiotics prophylaxis (IAP) is the most effective measurement to reduce the risk of GBS-induced neonatal EOS [6], it can impact neonatal gut microbiota [29] and until the first 3 months after birth, thus increasing the prevalence of antibiotic resistance genes [30]. In our study, infants exposed to antibiotics after birth were significant higher in GBS group (76.9%) than control group (41.1%) due to GBS colonization (Table 1), but meconium microbiota of infants exposed or unexposed to antibiotics were no difference in GBS infected group and control group (Figure S1). Hence, this imbalance of bacterial communities within 24 h of life in our study might be closely correlated with mother’s GBS colonization in vaginal tract, which was in line with previous studies [12].
There were also certain limitations of our results. First, this study was conducted in a single center with a relatively small sample set. Second, potential influence of nutrition intakes during pregnancy was not taken into consideration. Third, the confound influence of antibiotic exposure on meconium microbiota prior to labor or operative period for C-section and immediately after birth couldn’t address completely due to the shortage of study design and relatively small sample size. Furthermore, we do not have access to the matched maternal microbiome samples, thus evidence tracing the origin of meconium microbiome is required in further study.
Conclusion
In summary, our findings add to a growing body of knowledge about the association between GBS colonization and neonatal meconium. Our results demonstrated the potential features of gut microbiota in neonatal early life born to mother with GBS colonization, which may lead to new biomarkers and innovative therapeutic approaches for perinatal infant care.
Methods
Study design and sample collection
The Ethics Committee of Shenzhen Luohu Maternity and Child Health Hospital has approved all of the research procedures. Under the procedure approved by the Institutional Review Board (registry number: LL201804007), informed consent was given by the parents of the newborns.
The high-risk neonates admitted to the department of neonatology from May, 2018 to Jul, 2019 were enrolled after receiving informed consent from the parents. Preterm infants with extreme asphyxia (stage III), fetal chromosomal abnormalities, cyanotic congenital cardiac failure, congenital intestinal atresia, gastroschisis, omphalocele, excessive upper gastric intestinal bleeding, or parental permission deficiency/refusal were excluded from the study.
The fecal samples were collected in 30 ~ 50 g from a sterilized diaper by using the sterile container having an equal volume of sterile cryoprotectant within 24 h after birth and transported immediately to lab on ice and stored at − 80 °C for further studies. The specialized senior nurses were responsible for this work and the small sample spoon could not touch other neonatal body sites when collecting.
The GBS culture from mother’s vaginal swab were conducted at 36 week gestational age for term labor or prior to delivery for premature labor. The clinical information, treatment and lab data of mothers and neonates were extracted from medical records.
DNA extraction and labeling
Bacterial DNA from the stool samples was processed following a previously published protocol [19]. In brief, DNA was collected using the Stool DNA Extraction Kit (Halgen, Ltd., Zhongshan, China) and amplified in a PCR with standardized primers that covered the 16S rRNA gene V1-V9 regions. The PCR products were explicitly labeled without purification for array hybridization.
Microarray hybridization
Previous protocols were followed to perform microarray hybridization [19]. In general, Cy5- and Cy3-labeled sample DNA were combined and loaded into a hybridization tank. After 3.5 h incubation, the slides were manually washed and automatically screened using a dual-channel (Genepix 4000B) scanner to calculation the mean signal strength of Cy5/Cy3 ratio, by which the relative abundance of each bacterial species is given.
Data analysis
Alpha-diversity was measured using default parameters and QIIME tools (version 1.9.0, http://qiime.org/) [31]. Wilcoxon rank-sum test was used to measure the disparities in alpha-diversities between classes. Analyzes of principal coordinates analysis (PCoA) and non-metric multidimensional scaling (NMDS) were performed using QIIME modules and visualized with the “ggplot2” package of R software (version 3.5.2). PERMANOVA test determines whether groups of samples are significantly different from one another using the ADONIS permutation-based statistical test in ‘Vegan’ package of R software. Linear Discriminant Analysis (LDA) Impact Size (LEfSe) tool [32] was adopted to analyze the disparity between classes of bacterial organisms. A threshold of > 2.0 was set for the logarithmic LDA score in order to take into account discriminant features [32].
Supplementary Information
Acknowledgements
Not applicable.
Authors’ contributions
Conceived and designed experiments: YFL and YHJ. Collected fecal samples: SXC. Collected and analyzed clinical data: XLG and YFL. Performed fecal DNA extraction and microarray hybridization: KJW. Analyzed and interpreted results: YHJ, YFL, KJW. Drafted the manuscript: YHJ, KJW, YFL and XLG. All authors read and approved the final manuscript.
Funding
This work was supported by the Department of Luohu Science and Technology [grant No. 2018006] and Key Discipline of Luohu Neonatal Department [grant No. 2019006]. Funding bodies had no role in study design, data collection, analysis, and writing manuscript.
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article and additional files. All these data are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
All procedures were approved by the Ethics Committee of Shenzhen Luohu Maternity and Child Health Hospital. Under the procedure approved by the Institutional Review Board (registry number: LL201804007), written informed consent was given and approved by the parents of the newborns.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yue-feng Li and Xue-lei Gong contributed equally to this work.
Contributor Information
Kejian Wang, Email: kejian-wang@foxmail.com.
Yan-hua Jiang, Email: 1453751387@qq.com.
References
- 1.Koenig JM, Keenan WJ. Group B streptococcus and early-onset sepsis in the era of maternal prophylaxis. Pediatr Clin. 2009;56(3):689–708. doi: 10.1016/j.pcl.2009.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vornhagen J, Waldorf KMA, Rajagopal L. Perinatal group B streptococcal infections: virulence factors, immunity, and prevention strategies. Trends Microbiol. 2017;25(11):919–931. doi: 10.1016/j.tim.2017.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.El Beitune P, Duarte G, Maffei CML. Colonization by Streptococcus agalactiae during pregnancy: maternal and perinatal prognosis. Braz J Infect Dis. 2005;9(4):276–282. doi: 10.1590/s1413-86702005000400002. [DOI] [PubMed] [Google Scholar]
- 4.El Aila NA, Tency I, Claeys G, Saerens B, Cools P, Verstraelen H, Temmerman M, Verhelst R, Vaneechoutte M. Comparison of different sampling techniques and of different culture methods for detection of group B streptococcus carriage in pregnant women. BMC Infect Dis. 2010;10(1):285. doi: 10.1186/1471-2334-10-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Matee MI, Massawe FA, Lyamuya EF. Maternal and neonatal colonisation of group B streptococcus at Muhimbili National Hospital in Dar Es Salaam, Tanzania: prevalence, risk factors and antimicrobial resistance. BMC Public Health. 2009;9(1):437. doi: 10.1186/1471-2458-9-437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hasperhoven G, Al-Nasiry S, Bekker V, Villamor E, Kramer B. Universal screening versus risk-based protocols for antibiotic prophylaxis during childbirth to prevent early-onset group B streptococcal disease: a systematic review and meta-analysis. BJOG Int J Obstet Gynaecol. 2020;127(6):680–691. doi: 10.1111/1471-0528.16085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zou Z-H, Liu D, Li H-D, Zhu D-P, He Y, Hou T, Yu J-L. Prenatal and postnatal antibiotic exposure influences the gut microbiota of preterm infants in neonatal intensive care units. Ann Clin Microbiol Antimicrob. 2018;17(1):9. doi: 10.1186/s12941-018-0264-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marshall BM, Levy SB. Food animals and antimicrobials: impacts on human health. Clin Microbiol Rev. 2011;24(4):718–733. doi: 10.1128/CMR.00002-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ouwehand AC, Forssten S, Hibberd AA, Lyra A, Stahl B. Probiotic approach to prevent antibiotic resistance. Ann Med. 2016;48(4):246–255. doi: 10.3109/07853890.2016.1161232. [DOI] [PubMed] [Google Scholar]
- 10.Azad MB, Konya T, Maughan H, Guttman DS, Field CJ, Chari RS, Sears MR, Becker AB, Scott JA, Kozyrskyj AL. Gut microbiota of healthy Canadian infants: profiles by mode of delivery and infant diet at 4 months. Cmaj. 2013;185(5):385–394. doi: 10.1503/cmaj.121189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gschwendtner S, Kang H, Thiering E, Kublik S, Fösel B, Schulz H, Krauss-Etschmann S, Heinrich J, Schöler A, Schloter M. Early life determinants induce sustainable changes in the gut microbiome of six-year-old children. Sci Rep. 2019;9(1):1–9. doi: 10.1038/s41598-019-49160-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cassidy-Bushrow AE, Sitarik A, Levin AM, Lynch SV, Havstad S, Ownby DR, Johnson CC, Wegienka G. Maternal group B Streptococcus and the infant gut microbiota. J Dev Orig Health Dis. 2016;7(1):45. doi: 10.1017/S2040174415001361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rosen GH, Randis TM, Desai PV, Sapra KJ, Ma B, Gajer P, Humphrys MS, Ravel J, Gelber SE, Ratner AJ. Group B Streptococcus and the vaginal microbiota. J Infect Dis. 2017;216(6):744–751. doi: 10.1093/infdis/jix395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wilczyńska P, Skarżyńska E, Lisowska-Myjak B. Meconium microbiome as a new source of information about long-term health and disease: questions and answers. J Matern Fetal Neonatal Med. 2019;32(4):681–686. doi: 10.1080/14767058.2017.1387888. [DOI] [PubMed] [Google Scholar]
- 15.Hu J, Nomura Y, Bashir A, Fernandez-Hernandez H, Itzkowitz S, Pei Z, Stone J, Loudon H, Peter I. Diversified microbiota of meconium is affected by maternal diabetes status. PLoS One. 2013;8(11):e78257. doi: 10.1371/journal.pone.0078257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Collado MC, Rautava S, Aakko J, Isolauri E, Salminen S. Human gut colonisation may be initiated in utero by distinct microbial communities in the placenta and amniotic fluid. Sci Rep. 2016;6:23129. doi: 10.1038/srep23129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Blaser MJ, Devkota S, McCoy KD, Relman DA, Yassour M, Young VB. Lessons learned from the prenatal microbiome controversy. Microbiome. 2021;9:8. doi: 10.1186/s40168-020-00946-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.de Goffau MC, Lager S, Sovio U, Gaccioli F, Cook E, Peacock SJ, Parkhill J, Charnock-Jones DS, Smith GCS. Human placenta has no microbiome but can contain potential pathogens. Nature. 2019;572:329–334. doi: 10.1038/s41586-019-1451-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu X, Zou Y, Ruan M, Chang L, Chen X, Wang S, Yang W, Zhang L, Guo Y, Chen Y. Pediatric acute lymphoblastic leukemia patients exhibit distinctive alterations in the gut microbiota. Front Cell Infect Microbiol. 2020;10:558799. doi: 10.3389/fcimb.2020.558799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Babu E, Oropello J. Staphylococcus lugdunensis: the coagulase-negative staphylococcus you don’t want to ignore. Expert Rev Anti-Infect Ther. 2011;9(10):901–907. doi: 10.1586/eri.11.110. [DOI] [PubMed] [Google Scholar]
- 21.Böcher S, Tønning B, Skov RL, Prag J. Staphylococcus lugdunensis, a common cause of skin and soft tissue infections in the community. J Clin Microbiol. 2009;47(4):946–950. doi: 10.1128/JCM.01024-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Haile D, Hughes J, Vetter E, Kohner P, Snyder R, Patel R, Cockerill F., III Frequency of isolation of Staphylococcus lugdunensis in consecutive urine cultures and relationship to urinary tract infection. J Clin Microbiol. 2002;40(2):654–656. doi: 10.1128/JCM.40.2.654-656.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Frank KL, Del Pozo JL, Patel R. From clinical microbiology to infection pathogenesis: how daring to be different works for Staphylococcus lugdunensis. Clin Microbiol Rev. 2008;21(1):111–133. doi: 10.1128/CMR.00036-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kubota T, Nojima M, Itoh S. Vaginal bacterial flora of pregnant women colonized with group B streptococcus. J Infect Chemother. 2002;8(4):326–330. doi: 10.1007/s10156-002-0190-x. [DOI] [PubMed] [Google Scholar]
- 25.Altoparlak U, Kadanali A, Kadanali S. Genital flora in pregnancy and its association with group B streptococcal colonization. Int J Gynecol Obstet. 2004;87(3):245–246. doi: 10.1016/j.ijgo.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 26.Zarate G, Nader-Macias M. Influence of probiotic vaginal lactobacilli on in vitro adhesion of urogenital pathogens to vaginal epithelial cells. Lett Appl Microbiol. 2006;43(2):174–180. doi: 10.1111/j.1472-765X.2006.01934.x. [DOI] [PubMed] [Google Scholar]
- 27.De Gregorio PR, Tomás MSJ, Terraf MCL, Nader-Macías MEF. In vitro and in vivo effects of beneficial vaginal lactobacilli on pathogens responsible for urogenital tract infections. J Med Microbiol. 2014;63(5):685–696. doi: 10.1099/jmm.0.069401-0. [DOI] [PubMed] [Google Scholar]
- 28.Shane A, Sánchez P, Stoll B. Sepsis neonatal. Lancet. 2017;390(10104):1770–1780. doi: 10.1016/S0140-6736(17)31002-4. [DOI] [PubMed] [Google Scholar]
- 29.Mazzola G, Murphy K, Ross RP, Di Gioia D, Biavati B, Corvaglia LT, Faldella G, Stanton C. Early gut microbiota perturbations following intrapartum antibiotic prophylaxis to prevent group B streptococcal disease. PLoS One. 2016;11(6):e0157527. doi: 10.1371/journal.pone.0157527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nogacka A, Salazar N, Suárez M, Milani C, Arboleya S, Solís G, Fernández N, Alaez L, Hernández-Barranco AM, Clara G. Impact of intrapartum antimicrobial prophylaxis upon the intestinal microbiota and the prevalence of antibiotic resistance genes in vaginally delivered full-term neonates. Microbiome. 2017;5(1):93. doi: 10.1186/s40168-017-0313-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kuczynski J, Stombaugh J, Walters WA, González A, Caporaso JG, Knight R. Using QIIME to analyze 16S rRNA gene sequences from microbial communities. Curr Protoc Bioinform. 2011;10:10.7. doi: 10.1002/0471250953.bi1007s36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Segata N, Izard J, Waldron L, Gevers D, Miropolsky L, Garrett WS, Huttenhower C. Metagenomic biomarker discovery and explanation. Genome Biol. 2011;12(6):1–18. doi: 10.1186/gb-2011-12-6-r60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets supporting the conclusions of this article are included within the article and additional files. All these data are available from the corresponding author on reasonable request.