Since the global spread of Sars-Cov-2 in early 2020, the healthcare systems in many countries have been in a constant state of preparedness to deal with the burden of critically ill infected patients. In April 2020, the Swedish National Registry for Vascular Surgery (Swedvasc) introduced three Covid-19 specific variables in the registry, to monitor the effects of the disease on vascular surgical care, as previously suggested in this journal.1 These mandatory variables register if the patient is tested (to identify possible infection in patients with or without respiratory symptoms), if the patient is infected, and if the procedure has been postponed due to the pandemic. Swedvasc covers all vascular units and procedures for peripheral arterial occlusive disease (PAOD), carotid artery stenosis, aortic aneurysms and dissections, popliteal artery aneurysms, venous obstructions, and most units register treating varicose veins. The registry is under continuous assessment with external and internal validities of > 95% for arterial procedures.
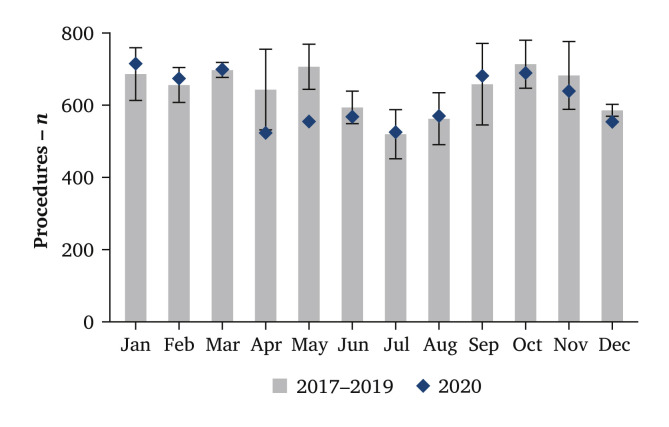
According to data for 1 January 2020 to 31 December 2020 there was no significant decrease in the total number of procedures compared with 2017 – 2019. Despite a reduced number of interventions during the first wave of the pandemic in April and May, the rest of 2020 was similar to previous years (Fig. 1 ).
Figure 1.
Mean number of registrations of arterial procedures (carotid, aortic and peripheral arterial occlusive disease) per month in the Swedvasc registry 2017 – 2019 (grey bars, with 95% confidence interval) vs. 2020 (diamonds).
The registered number of procedures in 2020 compared with 2017 – 2019 (mean) was 5 286 vs. 5 544 for PAOD, 778 vs. 795 for carotid, and 1 326 vs. 1 339 for the aorta. The only significant decrease was in venous procedures 9 316 vs. 11 019.
Although the proportions of operations for acute and chronic limb ischaemia (13% vs. 87%) were unchanged in 2020 compared with 2017 – 2019, fewer procedures for claudication were registered: 27% in 2020, and 35% in 2017 – 2019. Considering reports of thromboembolic complications of Covid-19, an increase in treatments of acute limb ischaemia was expected, but no significant difference compared with previous years was observed. Neither was there any significant increase in the treatment of acute proximal venous thrombosis, and none of the patients who underwent venous thrombolysis had a verified Covid-19 infection.
Operation for symptomatic carotid stenosis was a prioritised procedure, 86% were performed within 14 days from symptom onset vs. 83% (2017 – 2019). Stroke or death within 30 days was similar (3.9% vs. 3.5%). Only 3.9% of the carotid procedures performed were for asymptomatic stenoses (vs. 4.6% in 2017 – 2019, p = .49), which is the lowest reported number in Swedvasc to date.
An increase in operations for symptomatic thoracic and thoraco-abdominal aneurysm was observed but not in aneurysm rupture, thus the total number of aneurysm repairs was not affected. The mean diameter of elective infrarenal aneurysms was 6.1 cm (2019: 6.2 cm). Endovascular repair of aneurysms increased from 64% to 71%. This trend towards increasing use of endovascular aneurysm repair is not new, however.
Although interventions for varicose veins decreased, there was considerable regional variation. In regions with mainly private care providers for venous interventions, there was no decrease at all.
No differences in age or risk factors were found in the registered cohort of patients treated in 2020 compared with previous years, either in terms of post-operative complications, or 30 day mortality. Forty-nine patients (0.4%) were treated with active verified Covid-19 infection, with the following indications for intervention: symptomatic carotid stenosis (n = 4), aortic aneurysm (n = 3), aortic dissection (n = 1), acute limb ischaemia (n = 11), chronic limb ischaemia (n = 15), varicose veins (n = 15). Of note, some of these operations may have been performed in asymptomatic patients with a positive test identified post-operatively, and only 18% of all the patients during the studied time period underwent testing. The frequency of tested patients varied widely across the country from 85% in one unit to 4% in another. This is because the testing strategy for Covid-19 was managed independently in all healthcare regions in the country, and because the spread of disease varied considerably between regions. In total, 10% of all operated patients had their procedures postponed, the majority for more than one month.
The effect of the pandemic on vascular surgical practice has varied in different countries and regions.2, 3, 4, 5 While a study from Italy reported that it was possible to safely maintain vascular surgical practice during the first wave of the pandemic,3 others reported a considerable drop in the number of procedures, as well as increased rates of post-operative complications and death.4 , 5 The decrease in vascular procedures in Sweden is much less pronounced compared with a national analysis of data in the UK.5 The Swedish strategy for management of Covid-19 differed from many other countries, with no formal lockdowns during 2020. From a healthcare perspective, the national ambition was to not reduce the provision of imperative (life or limb threatening) care. The current analysis suggests that this strategy was implemented in vascular surgery during 2020 despite the first and second wave of the pandemic. Of note, surgery for asymptomatic carotid stenosis and claudication constitute a smaller proportion of cases in Sweden (irrespective of the pandemic) compared with many other countries.6 Thus the effect of the pandemic on the total number of procedures is less marked in this context. With the continued expansion of Covid-19 in Sweden from December 2020 and onwards, it will be interesting to monitor further effects of the pandemic.
ACKNOWLEDGEMENTS
This report was authored by the steering committee of the Swedvasc registry. Joachim Starck, accountable for the registry to the health authorities, is acknowledged for contributing to this paper, as well as all vascular surgeons in Sweden contributing to the registry.
References
- 1.Björck M., Boyle J.R., Dick F. The need of research initiatives amidst and after the covid-19 pandemic: a message from the editors of the EJVES. Eur J Vasc Endovasc Surg. 2020;59:695–696. doi: 10.1016/j.ejvs.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kahlberg A., Mascia D., Bellosta R., Attisani L., Pegorer M., Socrate A.M. Vascular surgery during COVID-19 emergency in hub hospitals of Lombardy: experience on 305 patients. Eur J Vasc Endovasc Surg. 2021;61:306–315. doi: 10.1016/j.ejvs.2020.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pini R., Faggioli G., Vacirca A., Gallitto E., Mascoli C., Attard L., Viale P., Gargiulo M. Is it possible to safely maintain a regular vascular practice during the COVID-19 pandemic? Eur J Vasc Endovasc Surg. 2020;60:127–134. doi: 10.1016/j.ejvs.2020.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Benson R.A., Nandhra S. Outcomes of vascular and endovascular interventions performed during the coronavirus disease 2019 (COVID-19) pandemic. Ann Surg. 2021;273:630–635. doi: 10.1097/SLA.0000000000004722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Impact of the Covid-19 pandemic on the provision of vascular surgery in the UK National Health Service. November 2020. https://www.vsqip.org.uk/content/uploads/2020/11/NVR-Short-Report-Covid-19.pdf National Vascular Registry Short Report. Available at: [Google Scholar]
- 6.Venermo M., Wang G., Sedrakyan A., Mao J., Eldrup N., DeMartino R. Editor's Choice – Carotid stenosis treatment: variation in international practice patterns. Eur J Vasc Endovasc Surg. 2017;53:511–519. doi: 10.1016/j.ejvs.2017.01.012. [DOI] [PubMed] [Google Scholar]