ABSTRACT
Background: Within the context of the COVID-19 pandemic, the WHO endorses facemask use to limit aerosol-spreading of the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). However, concerns have been raised regarding facemask-associated dyspnea, thermal distress and self-reported impairment of cognition. Accordingly, we tested how facemask-use affects motor-cognitive performances of relevance for occupational safety. We hypothesized that mask use would affect cognitively dominated performances and thermal discomfort, but not alter whole-body thermal balance.
Methods: Eight participants completed a facemask and a barefaced (control) trial, in a counterbalanced order, in 40°C and 20% humidity conditions. Motor-cognitive performance, physiological (rectal, mean skin and local facial temperatures) and perceptual (thermal comfort and dyspnea) measures were assessed at baseline and following 45 min of light work (100 W).
Results: Perceived dyspnea was aggravated with prolonged facemask use (p = 0.04), resulting in 36% greater breathlessness compared to control. However, no other differences were observed in motor-cognitive performance, physiological strain, or thermal discomfort.
Conclusions: Contradicting negative self-reported impacts of facemask-use, only dyspnea was aggravated in the present study, thereby reinforcing global recommendations of mask use, even in hot environments. (Funded by: European Union’s Horizon 2020 research and innovation program under the grant agreement No 668786).
KEYWORDS: COVID-19, occupational heat stress, occupational physiology, personal protective equipment, coronavirus
Introduction
In the context of the COVID-19 pandemic, facemask usage is endorsed by WHO [1] and mandatory by law across many countries to prevent aerosol-spreading of the virus [2,3]. This pertains not only to healthcare workers who require full-body personal protective equipment (PPE) [4], but even facemask use alone has been demonstrated to reduce transmission [5], and is often recommended for carrying out multiple activities outside the home (both outdoors and indoors) [6]. However, adverse effects from mask use, such as headaches [7], increased thermal discomfort [8], potential thermal physiological responses [9] and decreased work performance [7,10], have been reported in both healthcare workers and the general public [8]. In particular, cognition has been reported to be affected by ~25% of healthcare professionals [10] and concerns that PPE may aggravate heat stress and eventually jeopardize occupational safety [8]. To date, however, most of the data available have been recorded by self-reported questionnaires, completed days or weeks following heat exposure in PPE, thereby being highly vulnerable to the effects of recollection bias [11].
Accordingly, we conducted the present counterbalanced crossover study comparing the effect of mask use compared to a bare-faced control to test whether wearing a facemask would worsen thermal discomfort, perceived dyspnea, thermal physiological responses and impair task performance relying on concentration and motor-cognitive function when measured during (as opposed to days after) heat exposure. In particular, we employed a test battery that has been previously demonstrated to be highly sensitive and reliable for detecting the influence of heat-related factors that affect cognition [12-14]. It was hypothesized, based on the self-reported scores [7,10], that mask use would affect cognitively dominated performances and thermal discomfort, but not alter whole-body thermal balance.
Methods
Testing conditions were approved by the National Committee on Health Research Ethics (protocol number: 55907_v3_02012017). Following recruitment, participants underwent a familiarization trial, and then completed a control (uncovered face) and a facemask (KN95, Alchemy, Shenzhen, China) trial, in a counterbalanced order. All participants wore normal workwear during both trials with a clothing insulation factor of ~ 0.8). Resting measures were assessed following 30min of seated baseline. Subsequently, the participants completed 45 min of light exercise (100 W; equivalent to ~5 METs), simulating work in healthcare and related settings, and post-exercise measures were taken immediately upon the completion of exercise. All trials were completed in a climate chamber regulated at 40°C and 20% humidity.
Cognitive and fine-motor performances were assessed with an array of tests evaluating simple and complex motor, cognitively dominated (math calculation), and combined math-motor task performance [12]. This test battery has been previously demonstrated to be highly sensitive and reliable at detecting heat-related decrements in cognitive performance [12], including dehydration [14] and radiation [13].
Rectal temperature was measured by a thermistor probe (Ellab Copenhagen, CTD85) inserted at least 10 cm beyond the anal sphincter. Mean skin temperature was determined from a weighted average [15] of shoulder (0.3), chest (0.3), thigh (0.2) and calf (0.2) temperatures, measured using a thermistor probe (Ellab Copenhagen, CTD85). Additionally, skin temperature was measured at two sites on the face (in both trials), at locations representative of underneath (measured ~1 cm to the right of the right nostril) and outside (measured at the apex of the frontal facing zygoma) the mask when worn.
All perceptual measures were recorded on 200 mm visual-analog-scales and represented in the results as a percentage of max (by dividing the values by two). Dyspnea was measured using the Borg breathlessness scale (0 mm: nothing at all; 200 mm: maximal) [16]. Both facial and whole-body thermal discomfort were measured using a previously validated thermal comfort scale ranging from very comfortable (0 mm) to very uncomfortable (200 mm) [17].
All outcome variables were compared with two-way repeated measure ANOVA (test stage: at rest and following exercise; trial: control and facemask) using Graph Pad Prism (Version 8.0, Graph Pad Software, La Jolla, CA). Data are presented as means (±SD) with the risk of type-1 error set at 5%. Additionally, for ease of translation for clinical practitioners, the mean differences and 95% confidence intervals (95%CI) are provided for the comparisons of change from rest to baseline between the control and facemask trial, as recommended for clinical practice [18] and have been used for similar studies previously [19,20].
Results
Eight male participants (mean age: 35 ± 7 years; weight: 85.1 ± 26.2 kg) completed all trials. For ease of translation, Table 1 contains the global findings of the study; wherein resting values and the main effect for facemask use (i.e. mask use vs control) are displayed in the top section, the values immediately following exercise and the main effect of heat stress exposure (i.e. rest vs exercise) are displayed in the middle section and the comparisons between the change in outcome variables between facemask and control and the interaction p values are displayed in the bottom section.
Table 1.
Outcome variables at baseline (brief exposure with basal metabolic rate), following prolonged exposure (with exercise-induced hyperthermia) and intervention-control (interaction) comparisons
| |
Control |
Facemask |
Facemask main effect |
| Outcome variables at rest (SD) | |||
| Rectal temperature (ºC) | 37.5 (0.3) | 37.3 (0.2) | p = 0.04 |
| Skin temperature (ºC) | 34.9 (0.6) | 34.7 (0.6) | p = 0.50 |
| Under mask site temperature (ºC) | 36.0 (0.6) | 36.1 (0.5) | p = 0.59 |
| Outside mask site temperature (ºC) | 36.2 (0.7) | 36.3 (0.4) | p = 0.24 |
| Dyspnea (%) | 6.8 (13.2) | 8.5 (9.9) | p = 0.08 |
| Whole-body thermal discomfort (%) | 42.8 (21.2) | 39.8 (13.6) | p = 0.51 |
| Facial thermal discomfort (%) | 41.6 (18.6) | 49.4 (22.4) | p = 0.23 |
| Simple-motor performance (%) | 96.8 (1.5) | 98.0 (0.7) | p = 0.20 |
| Complex-motor performance (%) | 75.1 (5.8) | 74.9 (4.5) | p = 0.87 |
| Math calculation (%) | 97.9 (1.6) | 98.2 (2.7) | p = 0.75 |
| Math-motor task performance (%) | 94.5 (4.4) | 93.1 (4.9) | p = 0.16 |
| Combined cognitive score (%) | 91.1 (1.9) | 91.1 (1.7) | p = 0.58 |
| Outcome variables following exercise (SD) | |||
| Control | Facemask | Exposure main effect | |
| Rectal temperature (ºC) | 38.4 (0.6) | 38.2 (0.4) | p < 0.001 |
| Skin temperature (ºC) | 36.6 (0.5) | 36.6 (0.6) | p < 0.001 |
| Under mask site temperature (ºC) | 36.9 (0.7) | 36.6 (0.6) | p = 0.02 |
| Outside mask site temperature (ºC) | 37.2 (0.2) | 36.9 (0.6) | p < 0.001 |
| Dyspnea (%) | 21.4 (14.5) | 51.3 (27.6) | p < 0.001 |
| Whole-body thermal discomfort (%) | 66.8 (17.6) | 63.2 (19.2) | p < 0.01 |
| Facial thermal discomfort (%) | 64.3 (17.9) | 78.3 (17.3) | p < 0.001 |
| Simple-motor performance (%) | 96.9 (1.7) | 97.0 (1.7) | p = 0.22 |
| Complex-motor performance (%) | 74.8 (6.7) | 75.4 (4.1) | p = 0.89 |
| Math calculation (%) | 98.2 (1.8) | 97.4 (1.8) | p = 0.60 |
| Math-motor task performance (%) | 95.7 (2.0) | 93.4 (4.8) | p = 0.50 |
| Cognition (%) | 91.4 (1.8) | 90.8 (1.7) | p = 0.93 |
| Control-facemask comparisons [95%CI] | |||
| Mean difference | Facemask-exposure interaction | ||
| Rectal temperature (ºC) | −0.1 [−0.4, 0.2] | p = 0.55 | |
| Skin temperature (ºC) | 0.1 [−0.6, 0.8] | p = 0.77 | |
| Under mask site temperature (ºC) | −0.24 [−1.0, 0.6] | p = 0.50 | |
| Outside mask site temperature (ºC) | −0.5 [−1.4, 0.5] | p = 0.29 | |
| Dyspnea (%) | 28.3 [1.0, 55.5] | p = 0.04 | |
| Whole-body thermal discomfort (%) | −0.6 [−23.8, 22.5] | p = 0.95 | |
| Facial thermal discomfort (%) | 6.1 [−16.6, 28.9] | p = 0.54 | |
| Mean difference | Facemask-exposure interaction | ||
| Simple-motor performance (%) | −1.0 [−2.5, 0.4] | p = 0.14 | |
| Complex-motor performance (%) | 0.9 [−0.7, 2.5] | p = 0.23 | |
| Math calculation (%) | 1.1 [−3.7, 1.5] | p = 0.34 | |
| Math-motor task performance (%) | −1.0 [−7.9, 6.0] | p = 0.75 | |
| Cognition (%) | −0.6 [−2.7, 1.6] | p = 0.55 | |
N.B. p values provided in the top and middle sections of the table are for the ANOVA main effects of facemask use (control vs facemask) and exposure (rest vs exercise, respectively). Mean differences, 95% confidence interval (95%CI) and p values in the bottom section are representative of the comparisons of change from rest to exercise between the control and facemask trial, as recommended for clinical practice.
Perceived dyspnea was statistically worse with prolonged facemask use (p = 0.04), resulting in 36% greater breathlessness compared to control trials (Figure 1). Neither whole-body thermal discomfort (p = 0.95) nor facial thermal discomfort (p = 0.54) were affected by mask use (Figure 1). Both measures did, however, increase (worsen) following exercise (whole-body thermal comfort: p < 0.01, facial thermal discomfort: p < 0.001).
Figure 1.
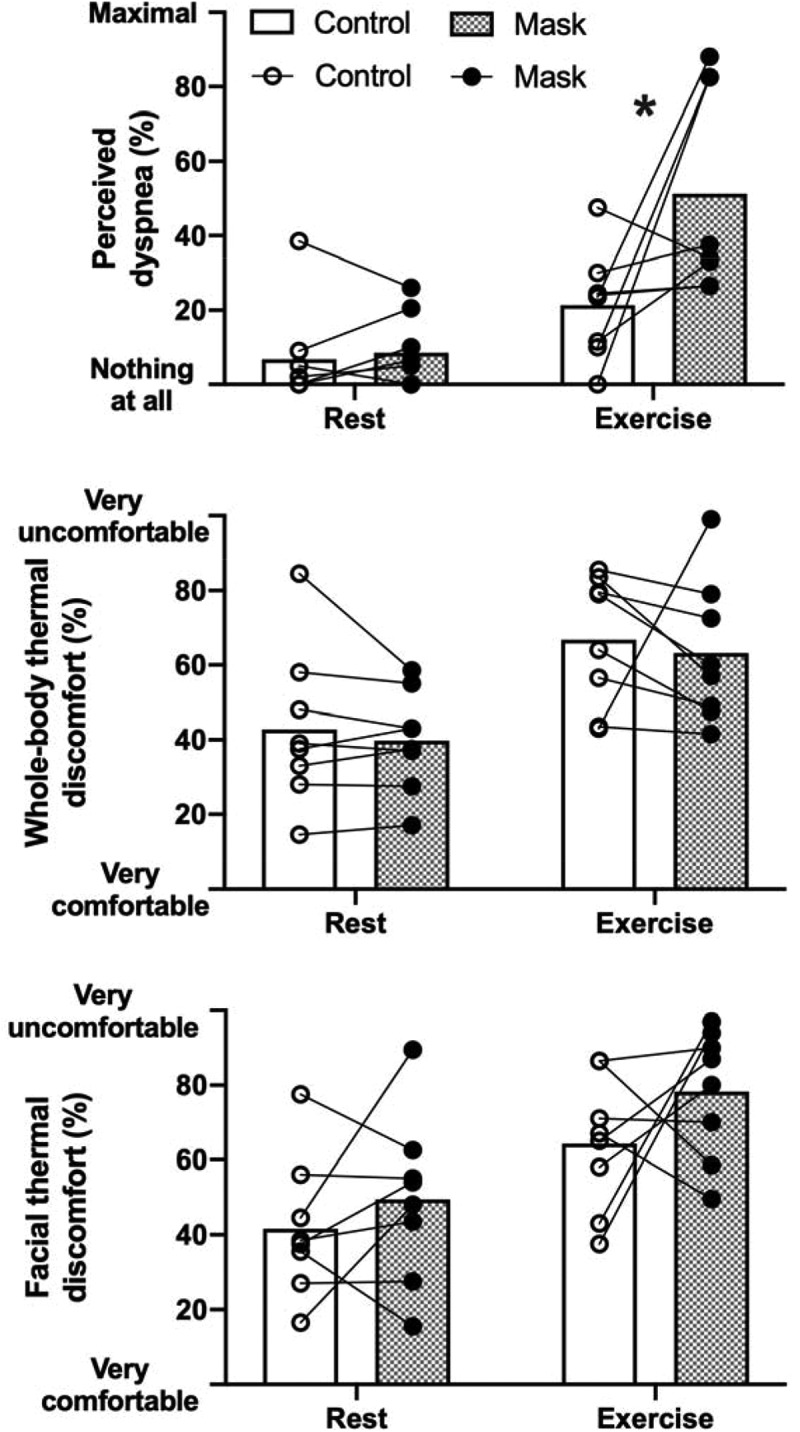
Individual scores superimposed onto group means (bars) during rest and exercise for the effect of mask use (closed circles and patterned bars) or no mask (open circles and bars) on perceptual responses. * denotes p < 0.05
The increase in dyspnea was not associated with impairments in cognitive performance indicators (Figure 2; all p > 0.05). Specifically, no statistical differences in simple (p = 0.14) or complex (p = 0.23) motor performance, math calculation (p = 0.34), math-motor performance (p = 0.75) and combined cognitive performance (p = 0.55) were observed. Nor did any of the cognitive values worsen following exercise (all p > 0.05).
Figure 2.
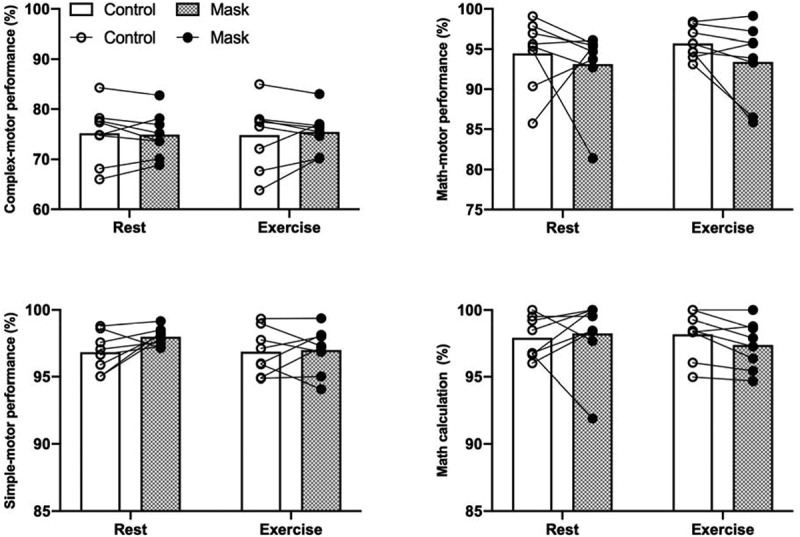
Individual scores superimposed onto group means (bars) during rest and exercise for the effect of mask use (closed circles and patterned bars) or no mask (open circles and bars) on motor-cognitive responses
Similarly, mask use did not statistically affect thermal physiological responses (Figure 3; all but rectal temperature p > 0.05) with the exception of rectal temperature, wherein core temperature was lower in the facemask trial (p = 0.04), however, there was no interaction between facemask use and time (p = 0.55). Additionally, as to be expected, all temperature measurements increased with exercise (exposure main effect: all p < 0.02).
Figure 3.
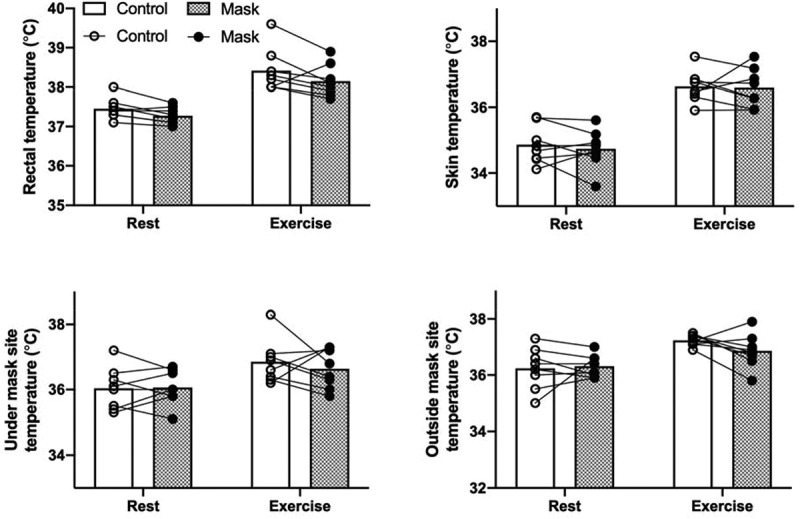
Individual scores superimposed onto group means (bars) during rest and exercise for the effect of mask use (closed circles and patterned bars) or no mask (open circles and bars) on physiological responses
Discussion
In contrast to concerns raised by occupational and thermal experts, as well as anecdotes of negative impact on cognition, the present study did not support that cognitively dominated performances or motor-control tasks are compromised by prolonged facemask use. Assessed with an experimental design and test array sufficiently sensitive to detect performance impairment due to dehydration [14] or solar radiation [13] (with similar sample sizes), the current conditions with aggravation of dyspnea and in combination with elevated thermal discomfort did not result in significant performance impairments that would jeopardize occupational safety.
The interference with respiration may be an area of concern, as heat exposure both at rest and during work may induce hyperventilation that subsequently lowers arterial CO2 and decreases cerebral blood flow [21]. Although, the set-up (wearing of facemask) excluded measures of pulmonary ventilation, we interpret changes as small, since neither the potential impact of altered ventilation on blood gas homeostasis nor the elevated perception of dyspnea affected any of the cognitively dominated performances as would be expected if cerebral oxygen delivery became a limiting factor. In terms of the perceived breathlessness, this was likely associated with the greater inhalation resistance which has been previously associated with breathlessness [22]. Indeed, anecdotal observations by the researchers as well as reports by the participants were that as exercise continued, sweat dripping down the forehead wetted the masks which increased the difficulty breathing (and the researchers observed greater puckering of the mask during inspiration toward the end of the trials). From this perspective, changing masks more regularly, or designing a mask specifically for working in hot conditions, which encourages sweat to be wicked away from the surface of the mask, rather than being absorbed by respirator materials, may help to reduce feelings of breathlessness.
Collectively, the present findings demonstrate, contrary to anecdotal reports of decreases in cognition and work performance while wearing face masks, indicators of cognitive-motor performance were not negatively affected by mask use. Moreover, thermal perception and physiological responses were similarly unaffected. Perceived breathlessness, however, was increased when masks were worn during prolonged periods of light work.
Funding Statement
This work was funded bythe European Commission Horizon 2020 Grant (668786 – Heat-Shield).
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- [1].When and how to use masks . [cited 2020 July15]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/when-and-how-to-use-masks
- [2].WHO . Infection prevention and control during health care when COVID-19 is suspected: interim guidance, 19 March 2020. Geneva: World Health Organization; 2020. [Google Scholar]
- [3].Organization WHO . Advice on the use of masks in the context of COVID-19: interim guidance, 5 June 2020. Geneva: World Health Organization; 2020. [Google Scholar]
- [4].Cao Y, Li Q, Chen J, et al. Hospital emergency management plan during the COVID-19 epidemic. Acad Emerg Med. 2020;27(4):309–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Chu DK, Akl EA, Duda S, et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395(10242):1973–1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Cheng VC, Wong S-C, Chuang VW, et al. The role of community-wide wearing of face mask for control of coronavirus disease 2019 (COVID-19) epidemic due to SARS-CoV-2. J Infect. 2020;81(1):107–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Ong JJY, Bharatendu C, Goh Y, et al. Headaches associated with personal protective equipment – a cross-sectional study among frontline healthcare workers during COVID-19. Headache J Head Face Pain. 2020;60(5):864–877. [DOI] [PubMed] [Google Scholar]
- [8].Shumake-Guillemot J, Amir S, Anwar N, et al. Protecting health from hot weather during the COVID-19 pandemic. Global heat health information network. [updated 2020 May 25; cited 2020 August14]. Available from: http://ghhin.org/heat-and-covid-19
- [9].Daanen HAM, Bose-O’Reilly S, Flouris AD, et al. COVID-19 and thermoregulation-related problems: practical recommendations. Temperature. 2021;8. (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Adverse RE. Effects of prolonged mask use among healthcare professionals during COVID-19. J Infect Dis Epidemiol. 2020;6. [Google Scholar]
- [11].Rhodes AE, Fung K. Self-reported use of mental health services versus administrative records: care to recall? Int J Methods Psychiatr Res. 2004;13(3):165–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Piil JF, Lundbye-Jensen J, Trangmar SJ, et al. Performance in complex motor tasks deteriorates in hyperthermic humans. Temperature. 2017;4(4):420–428. doi: 10.1080/23328940.2017.1368877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Piil JF, Christiansen L, Morris NB, et al. Direct exposure of the head to solar heat radiation impairs motor-cognitive performance. Sci Rep. 2020;10(1):7812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Piil JF, Lundbye-Jensen J, Christiansen L, et al. High prevalence of hypohydration in occupations with heat stress—Perspectives for performance in combined cognitive and motor tasks. PLoS One. 2018;13(10):e0205321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Ramanathan NL. A new weighting system for mean surface temperature of the human body. J Appl Physiol. 1964;19(3):531–533. [DOI] [PubMed] [Google Scholar]
- [16].Borg E, Borg G, Larsson K, et al. An index for breathlessness and leg fatigue. Scand J Med Sci Sports. 2010;20(4):644–650. [DOI] [PubMed] [Google Scholar]
- [17].Davey S, Reilly T, Newton M, et al. The reproducibility and validity of visual analogue scales (VAS) that assess thermal perceptions in stable and dynamic, asymmetric environments. Environ Ergon XII. 2007;117. [Google Scholar]
- [18].Shreffler J, Huecker MR. Hypothesis testing, P values, confidence intervals, and significance. StatPearls [Internet]. StatPearls Publishing; 2020. [PubMed] [Google Scholar]
- [19].Morris NB, Gruss F, Lempert S, et al. A preliminary study of the effect of dousing and foot immersion on cardiovascular and thermal responses to extreme heat. JAMA. 2019;322(14):1411–1413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Morris NB, English T, Hospers L, et al. The effects of electric fan use under differing resting heat index conditions: a clinical trial. Ann Intern Med. 2019;171(9):675–677. [DOI] [PubMed] [Google Scholar]
- [21].Nybo L, Møller K, Volianitis S, et al. Effects of hyperthermia on cerebral blood flow and metabolism during prolonged exercise in humans. J Appl Physiol. 2002;93(1):58–64. [DOI] [PubMed] [Google Scholar]
- [22].Warren DW, Mayo R, Zajac DJ, et al. Dyspnea following experimentally induced increased nasal airway resistance. Cleft Palate Craniofac J. 1996;33(3):231–235. [DOI] [PubMed] [Google Scholar]


