Abstract
Introduction
At all ages, randomised trials demonstrate lower mortality and cardiovascular disease incidence with blood pressure (BP) lowering. However, this may not generalise to older people with frailty. We aimed to determine the acceptability to clinicians of key aspects of trial designs using different BP targets and strategies to better manage hypertension in the context of frailty.
Methods
We conducted a multinational survey of clinicians managing hypertension in older people, distributed using an online survey link amongst professional societies and social networks. Questions described case histories of patients who were frail with different systolic blood pressures (SBP), treatment target, strategy and target trial population.
Results
In total, 114 responses were received (48 primary care, 66 secondary care). A majority would consider recruiting patients to a trial of relaxing treatment in those whose SBP < 130 mm Hg; a majority would consider recruiting to a trial intensifying treatment in patients with SBP > 150 mm Hg. Respondents elected to intensify treatment by: choosing the next step by NICE guidelines, adding a new treatment agent at full dose, or adding two agents at half dose.
Conclusion
A majority of clinicians surveyed would recruit older people to a trial intensifying treatment where SBP is more than 150 mm Hg and where patients have high cardiovascular risk or to a trial relaxing treatment where the SBP is below 130 mm Hg and where the patient has frailty.
Keywords: questionnaire, blood pressure, antihypertensive, multi-morbidity, treatment strategy, older people
Key Points
Blood pressure (BP) management in older people with competing co-morbidities is complex.
Trials of antihypertensive therapy in populations representative of most older people are now needed.
Frontline clinicians diverged on BP management at systolic measures between 130 and 150 mm Hg.
Older people with frailty and those with cardiovascular disease should be prioritised for future clinical trials.
Background
Hypertension increases the risk of future cardiovascular diseases [1]. Antihypertensive treatment can reduce this risk [2], and two recent large trials demonstrate treatment benefit extending to adults in later life [3,4]. However, patients with frailty, co-existing conditions and polypharmacy were less likely to be recruited to these trials [5]. Even when older people with frailty are targeted in trial recruitment, a minority of those invited are enrolled [6]. In the absence of trial evidence, clinical guidelines for the management of blood pressure (BP) in older adults with frailty and/or multi-morbidity are the subject of debate [7] so that clinicians are left with significant uncertainty on how best to manage BP in these patients.
We are designing a trial to best address clinical uncertainty of those who are regularly involved in these clinical decisions. We undertook a survey of clinicians to identify the target BPs, treatment strategies and patient populations where a trial is perceived potentially most useful.
Methods
We surveyed clinicians managing hypertension in older people through the British Geriatrics Society, European Society of Cardiology, social media and primary care and geriatrics networks in Ireland and the UK. The survey was open from September to November 2019 and comprised three sections:
Target BP
We first investigated the level of systolic BP at which the clinician would be willing to recruit a patient to a trial of BP treatment escalation or de-escalation. We presented seven clinical vignettes of older patients with frailty. Each vignette differed by the patient’s systolic blood pressure (SBP): 80–99, 100–119, 120–129, 130–139, 140–149, 150–159 and 160–179 mm Hg. At each SBP, the clinicians were asked whether they would recruit the patient to a trial that compared standard care with an intensifying treatment strategy, relaxing treatment strategy, either strategy or neither strategy.
Treatment strategy
The second section investigated the preferred treatment strategy the clinician would be willing to adopt. Options included adding/stopping one agent by half or full dose; escalating or de-escalating the type of agent according to the NICE stepped care for BP management or none of the above.
Target population
Lastly, clinicians were asked which subpopulations of older adults should be prioritised for either a trial relaxing or intensifying treatment. The clinicians could select multiple answers from a list of following patient characteristics: recovered from stroke or heart attack; using a Zimmer frame to walk with once a day package of care; requires a wheelchair to mobilise and has mild cognitive impairment; has recovered from delirium; none of the above; or others.
Results
A total of 114 responses were received from 48 general practitioners, 42 geriatricians, 9 stroke physicians, 2 cardiologists and 13 other secondary care clinicians.
Target BP
For patients with SBP < 130 mm Hg, most respondents (71% for 80–99; 80% for 100–119; 61% for 120–129) favoured a trial of relaxing treatment versus standard therapy (Figure 1). One-third of respondents reported they would recruit participants to either strategy where the SBP was between 130 and 150 mm Hg (33% for 130–140; 40% for 140–150, respectively). For patients with SBP > 150 mm Hg, most respondents (47% for 150–159; 75% for 160–179) favoured a trial of intensifying treatment versus standard therapy.
Figure 1.
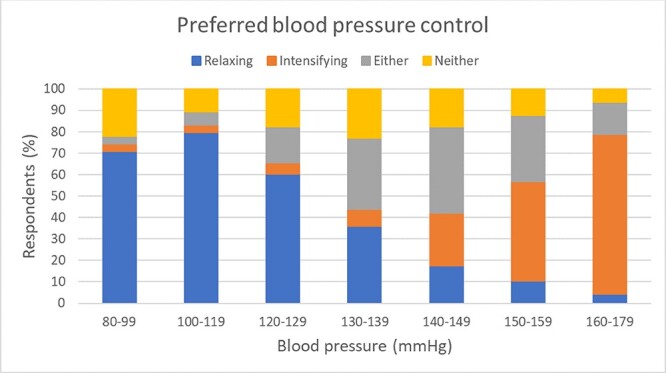
Summary of chosen options for BP control shows that: for a SBP < 130 mm Hg the majority favour a trial of relaxing control; for a SBP between 130 and 149 mm Hg many would recruit either strategy; for a SBP > 150 mm Hg the majority favour a trial of intensifying control.
Treatment strategy
Respondents elected to intensify treatment by either: choosing the next step of the NICE hypertension guidelines (70%); adding a new treatment agent at full dose (52%); or, adding two agents at half dose (53%). Three clinicians stated they would not consider intensifying BP control. Respondents elected to relax treatment by either: stopping one full dose of a BP agent (64%); going down one step in the NICE stepped care for BP (62%); or, stopping a half dose of a BP agent (57%). Only one clinician stated they would not consider relaxing BP control.
Target population
Most clinicians were willing to recruit otherwise well patients to a trial of treatment intensification (76%) or relaxation (85%) (Figure 2). A trial of treatment intensification was favoured (91%) over relaxation (33%) in those with known cardiovascular risk. In patients with different features of frailty, a trial of treatment relaxation (74–88%) was favoured over treatment intensification (42–55%).
Figure 2.
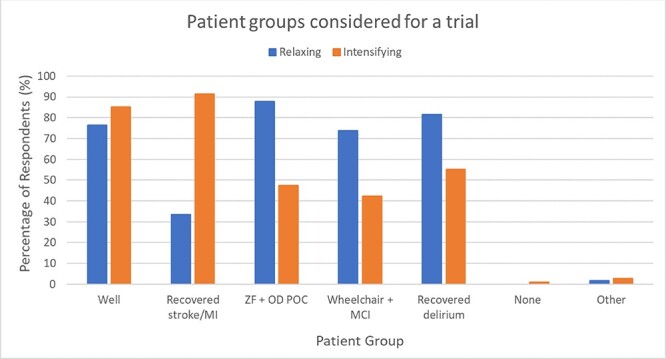
Clinicians were asked which of the following groups of patients over the age of 75 they would select for a randomised trial of intensifying (orange) or lowering (blue) BP control: is well, has recovered from stroke or myocardial infarction (MI), uses a Zimmer Frame (ZF) to walk and has a once daily (OD) package of care (POC), uses a wheelchair to mobilise and has mild cognitive impairment (MCI), has recovered from delirium, I would not randomise any patient into such a trial, other.
Discussion
In this survey, clinicians were most willing to recruit patients to a trial to relax therapy whose SBP was less than 130 mm Hg; and recruit to a trial to intensify therapy in patients whose SBP was more than 150 mm Hg. The favoured method of titrating therapy was stepping up or stepping down therapy according to the respective NICE guidelines. Patients with known cardiovascular risk were favoured for recruitment to a trial of treatment intensification, patients with frailty were favoured for recruitment to a trial of treatment relaxation.
Clinicians diverged on whether they would be willing to recruit a patient to a trial of treatment intensification or treatment withdrawal in patients with SBPs between 130 and 150 mm Hg. This may indicate clinical uncertainty or may reflect the differences amongst international guidelines on SBP targets in patients with known hypertension who are old or have other underlying health conditions [6]. For adults over the age of 80 years, the UK National Institute for Healthcare Excellence (NICE) guidelines [8], and the American Academy of Family Physicians [9] recommend treating SBP to less than 150 mm Hg; the American College of Cardiologists recommend treatment to a target of less than 130 mm Hg SBP [10]; and, the European Society of Cardiology recommend maintaining SBP below 140 mm Hg above 130 mm Hg [11].
There is uncertainty whether frail patients benefit from a lower BP [12]. A recent meta-analysis of observational studies demonstrated that whilst SBP lower than 140 mm Hg is associated with lower mortality in older people without frailty, there was no such association in older people with frailty, [13] but did not exclude reverse causality as an explanation. In contrast, older people with heightened cardiovascular risk were assessed by survey respondents as potentially benefiting from greater intervention. This is supported by the major trials undertaken to date, which have demonstrated benefit in older people in populations with established cardiovascular risk [5].
Strengths and limitations
This survey will inform the design of a trial in hypertension management of older people. Limitations of the survey include the convenience sampling methods therefore the respondents may not be representative of all geriatricians. The true complexity of clinical decision making in managing hypertension in older people was difficult to represent in a clinical vignette and in reality, many other considerations would be relevant, e.g. the recent trend of a patient’s BP and their overall cardiovascular risk status. The focus of this succinct survey was SBP alone, whereas any trial would necessarily also include diastolic BP targets [14].
Implications for future research
The design of any future trial would need to identify frail older people in electronic health records, although the best method to do so is uncertain. The method of treatment reduction or escalation strategy in older people is also a research question that remains unanswered.
Conclusion
Survey respondents across primary and secondary care in the UK and Ireland favoured the design of a trial targeting SBP between 130 and 150 mm Hg. Older people with high cardiovascular risk and those with clinical manifestations of frailty should be prioritised. A trial designed on these terms could address existing clinical uncertainty experienced by clinicians in the management of hypertension in older people.
Contributor Information
Miriam Veenhuizen, Edinburgh Medical School, University of Edinburgh, UK.
Oliver Todd, Academic Unit for Ageing and Stroke Research, University of Leeds, UK.
Atul Anand, BHF/University Centre for Cardiovascular Science, University of Edinburgh, UK; Edinburgh Delirium Research Group, Department of Geriatric Medicine, University of Edinburgh, UK.
Will Whiteley, Centre for Brain Sciences, University of Edinburgh, UK.
Declaration of Sources of Funding
This work was supported by Dunhill Medical Trust, UK [RTF107/0117 to OMT]; Dr Will Whiteley reports grants from Chief Scientist’s Office, during the conduct of the study; grants from Alzheimer’s Society, British Heart Foundation and the UK Stroke Association, outside the submitted work.
Acknowledgements
Thank you to all who responded to our survey.
Declaration of Conflicts of Interest
None.
References
- 1. Rapsomaniki E, Timmis A, George Jet al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1.25 million people. Lancet 2014; 383: 1899–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ettehad D, Emdin CA, Kiran Aet al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet 2016; 387: 957–67. [DOI] [PubMed] [Google Scholar]
- 3. Beckett NS, Peters R, Fletcher AEet al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med 2008; 358: 1887–98. [DOI] [PubMed] [Google Scholar]
- 4. Sprint Research Group, Wright JT Jr, Williamson JDet al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med 2015; 373: 2103–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sheppard JLM, Burt J, Temple Eet al. Generalisability of blood pressure lowering trials to older patients in primary care: a comparison of patient characteristics (in print). JAMA 2020. doi: 10.1111/jgs.16749. Online ahead of print. [DOI] [Google Scholar]
- 6. Sheppard JP, Burt J, Lown Met al. Effect of antihypertensive medication reduction vs usual care on short-term blood pressure control in patients aged ≥ 80 years with hypertension: the OPTiMISE randomized clinical trial. JAMA 2020; 323: 2039–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Conroy SP, Westendorp RGJ, Witham MD. Hypertension treatment for older people-navigating between Scylla and Charybdis. Age and Ageing 2018; 47: 505–8. [DOI] [PubMed] [Google Scholar]
- 8. National Institute for Health and Care Excellence, N . Clinical Guideline [CG136] Hypertension in adults: diagnosis and management, London, UK: Royal College of Physicians; 2019. [PubMed]
- 9. Qaseem A, Wilt TJ, Rich Ret al. Pharmacologic treatment of hypertension in adults aged 60 years or older to higher versus lower blood pressure targets: a clinical practice guideline from the American College of Physicians and the American Academy of family physicians. Ann Intern Med 2017; 166: 430–7. [DOI] [PubMed] [Google Scholar]
- 10. Whelton PK, Carey RM, Aronow WSet al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and Management of High Blood Pressure in adults: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol 2018; 71: e127–248. [DOI] [PubMed] [Google Scholar]
- 11. Williams B, Mancia G, Spiering Wet al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J 2018; 39: 3021–104. [DOI] [PubMed] [Google Scholar]
- 12. Masoli JAH, Delgado J, Pilling L, Strain D, Melzer D. Blood pressure in frail older adults: associations with cardiovascular outcomes and all-cause mortality. Age and Ageing 2020; 49: 807–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Todd OM, Wilkinson C, Hale Met al. Is the association between blood pressure and mortality in older adults different with frailty? A systematic review and meta-analysis. Age and Ageing 2019; 48: 627–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Spence JD. Risk from low blood pressure in frail older adults: diastolic pressure and pulse pressure are important. Age and Ageing 2020; afaa084. [DOI] [PubMed] [Google Scholar]


