Abstract
Background and Objectives:
Quality indicators for the performance of EUS have been developed to monitor and improve service value and patient outcomes. To support the incorporation of these indicators and standardize EUS documentation, we propose standard EUS reporting elements for endosonographers and endoscopy units.
Methods:
A comprehensive literature search and review was performed to identify EUS quality indicators and key components of high-quality standardized EUS reporting. Guidance statements regarding standard EUS reporting elements were developed and reviewed at the Forum for Canadian Endoscopic Ultrasound (FOCUS) 2019 Annual Meeting.
Results:
EUS reporting elements can be divided into preprocedural, intraprocedural, and postprocedural items. Preprocedural components include the type, indication, and urgency of the procedure and patient clinical information and consent. Intraprocedural components include the adequacy and extent of examination, relevant landmarks, lesion characteristics, sampling method, specimen quality, and intraprocedural adverse events. Postprocedural components include a summary and synthesis of relevant findings as well as recommended management and follow-up.
Conclusions:
Standardizing reporting elements may help improve the care of patients undergoing EUS procedures. Our review provides a practical guide and compilation of recommended reporting elements to ensure ongoing best practices and quality improvement in EUS.
Keywords: EUS, reporting elements, standardization
INTRODUCTION
The quality of endoscopic reporting significantly impacts the provision of timely and appropriate patient care.[1,2] Large variations exist in the quality of endoscopic reporting among endoscopic procedures including EUS.[1,3,4,5,6] Improved patient outcomes and efficiency of care have been shown when procedural reporting is consistent.[3,7,8] Guidance regarding reporting elements is necessary to incorporate quality indicators into routine practice and to standardize documentation.[3,4,9] Currently, there is no formal guidance document outlining reporting standards for EUS. To drive quality in EUS documentation, statements regarding standardized diagnostic EUS reporting were developed and reviewed by experts at a national EUS meeting.
METHODS
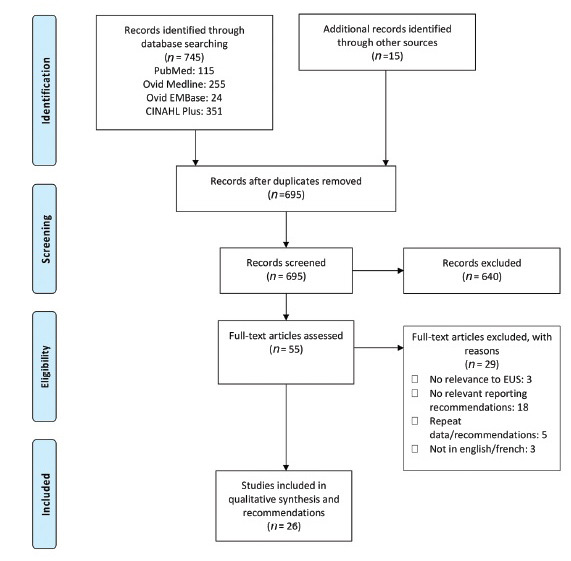
A comprehensive electronic search was conducted by two independent reviewers (SL and MM) of the databases PubMed, Ovid MEDLINE, and Embase from 1990 to December 2019. Search terms included the MeSH subheadings “Endoscopic Ultrasound” and/or “EUS” with “Quality Indicators” and/or “Quality Reporting,” with further sources obtained through review of reference lists of articles of interest. All human adult studies published in full manuscript form in English were reviewed. Details on the search strategy and article review are provided in Supplementary Appendices 1 and 2.
Preprocedural, intraprocedural, and postprocedural indicators as well as reporting recommendations common to all endoscopy procedures were considered, with emphasis placed on items specific to EUS. All relevant indicators were extracted to develop a list of standardized EUS reporting elements [Table 1]. Guidance statements were then developed and reviewed by experts at the Forum for Canadian Endoscopic Ultrasound (FOCUS) 2019 Annual Meeting based on the results of our literature review. Reporting details regarding specific therapeutic EUS procedures such as drainage procedures and celiac plexus blockade were out of the scope of our review.
Table 1.
Required elements of EUS reporting
| Preprocedural |
|---|
| Date and time of procedure |
| Type of procedure |
| Type of EUS probe |
| Linear or radial |
| Name of primary endoscopist |
| Name(s) of assistants/trainees |
| Patient demographics and comorbidities |
| Age |
| Sex |
| Past medical history |
| Relevant surgical, family, and social history |
| Patient home medications |
| Including modifications to medications for the procedure |
| Other preendoscopic medications |
| Need for antibiotic prophylaxis |
| Indication for the procedure |
| Relevant preprocedural investigations |
| Blood work, imaging, and prior endoscopy |
| Documentation of informed consent |
| Type and dose of sedation |
| Anesthetist |
| General or conscious sedation |
| Preprocedural preparation |
| Duration of NPO |
| Bowel preparation |
| Intraprocedural |
| Adequacy and extent of examination |
| Description |
| Relevant landmarks |
| Lesion(s) |
| Size |
| Sonographic characteristics |
| Pertinent positives/negatives |
| Tumor staging (TNM) |
| Sampling method and sample quality |
| Needle type and gauge |
| Number of passes |
| Tissue acquisition technique |
| Presence of rapid on-site evaluation |
| Sample characteristics |
| Patient comfort |
| Intraprocedural adverse events |
| Endoscopic Interventions |
| Postprocedural |
| Diagnosis and relevant findings |
| Management and follow-up recommendations |
| Clear list of action items with timing, responsible provider, and rationale |
| Recommendations regarding the resumption of antithrombotic |
| Indication of provision of postprocedural information to patient/family |
| Plan for sharing of pathology results when available |
TNM: Tumor, node, metastatic spread; NPO: Nil per os
RESULTS
Preprocedural elements
Type of procedure, date, and procedural personnel
The type of procedure and whether EUS was performed with a linear or radial echoendoscope, mini-probe, or other available echoendoscope should be documented at the beginning of the report. The date and time of the procedure as well as the names of the primary and any assisting endoscopist(s) should be included. Trainee involvement should also be indicated, as this may impact procedural duration and outcomes such as adverse events.[10,11]
Patient demographics and comorbidities
A summary of the patient's clinical history and active medical issues should be documented in the endoscopy report or reference made to easily available consultation or preprocedural notes containing this information. Specific patient factors relevant to the performance and potential adverse events of the procedure should be noted. An objective assessment of perioperative morbidity and mortality with a tool such as the American Society of Anesthesiologists classification should be conducted and documented.[3,12]
Medications, antithrombotics, and antibiotic prophylaxis
A list of the patient's current medications should be reviewed before the procedure. The endoscopy report should highlight all medications that may impact procedural success and/or safety, such as anticoagulants, benzodiazepines, and narcotics. All documented or reported allergies, including allergy to latex, should be noted to ensure patient safety.
All antithrombotic agents should be listed as well as whether they were held appropriately in preparation for the procedure. While the risk of bleeding after EUS-guided biopsies is considered to be <3%, this can increase with the use of antithrombotics.[13]
The use of preprocedural prophylactic antibiotics should be clearly stated. Most recent guidelines recommend antibiotic prophylaxis for EUS-guided biopsies of mediastinal/thoracic lesions and for pancreatic cystic lesions; however, this practice may be changing in light of new evidence.[14] A recent randomized controlled trial showed no advantage in using antibiotic prophylaxis before EUS-guided sampling of pancreatic cystic lesions.[15] The American Society of Gastrointestinal Endoscopy (ASGE) recommends against prophylactic antibiotics in EUS-guided fine-needle aspiration (FNA) transcolonic sampling of solid lesions as current data are conflicting, and individual assessment is required.[12] If prophylaxis is used during the procedure, the name, dosage, route of administration, and timing should be reported.
Procedure indication(s)
Accepted diagnostic and therapeutic indications for EUS have been published by the ASGE and European Society of Gastrointestinal Endoscopy (ESGE) and are summarized in Table 2.[12] These should be stated in all reports for accuracy of documentation among providers. Documenting the indication allows the endoscopist to justify the need for an EUS examination while serving as a means of auditing compliance with accepted guidelines. In addition, it could guide readers through reported landmark descriptions and pertinent findings. Relevant observations based on a properly stated indication can prompt accurate clinical impressions and management plans.
Table 2.
Appropriate indications for EUS
| Diagnostic indications |
| Evaluation of biliary tree abnormalities (obstruction, strictures, stones, and dilation) |
| Staging of localized tumors of the GI tract, pancreas, bile ducts, and mediastinum |
| Diagnostic evaluation of solid and cystic lesions of the pancreas |
| Evaluation of pancreatic abnormalities including pancreatic duct abnormalities, masses, and chronic pancreatitis |
| Evaluation of subepithelial lesions of the GI tract |
| Evaluation of perianal/perirectal lesions |
| Therapeutic indications |
| Guiding drainage of symptomatic pancreatic pseudocysts |
| Guiding access to biliary and/or pancreatic ducts |
| Placement of fiducial markers into tumors within/adjacent to the GI tract |
| Celiac plexus block/neurolysis |
GI: Gastrointestinal
Consent for the procedure
Documentation of the consent process, including whether the patient was advised of and reasonably understood all relevant information about the procedure, its risks, benefits, and alternatives, is essential in any endoscopy report. Moreover, it should be noted that the patient was given adequate opportunity to ask questions and that they received appropriate answers from the physician.[16] EUS and EUS-FNA/fine-needle biopsy present risks of unique adverse events apart from those associated with standard endoscopy, which should be carefully reviewed with the patient and documented.[17,18]
Sedation
EUS reports should indicate whether sedation was utilized, the agents used, dosages, routes, and if anesthesia or nursing staff were responsible for its administration. Studies have shown that overall patient satisfaction is directly associated with the degree of sedation, with deeper sedation anecdotally providing higher satisfaction scores.[19] Safety concerns regarding the use of agents such as propofol have been reported, but there are limited data to suggest a difference in the risk of adverse events based on the type of sedation used.[20,21,22]
Preprocedural preparation
Endoscopists should report whether the patient complied with all preprocedural instructions. Current guidelines recommend that patients planned for upper EUS procedures be nil per os for a minimum of 6 h before the procedure to facilitate visualization, as well as reduce the risk of aspiration.[3] Bowel preparation quality of the rectosigmoid colon should be noted in lower EUS procedures, as this can impact visualization, the technical ease of the procedure, and the potential increased risk of infection of EUS-FNA in areas of poor bowel preparation.[23,24] Reporting of bowel preparation quality should be done utilizing a validated scoring system such as the Boston Bowel Preparation Scale or the Ottawa Bowel Preparation Scale.[25] The type of bowel preparation and regiment used should be included in all lower EUS procedure reports.[9]
Intra-procedural elements
Adequacy and extent of examination
Various patient factors may impact the ability of an endoscopist to complete an EUS examination satisfactorily, and these should be clearly documented. The presence of abdominal ascites or anatomical abnormalities from prior surgeries may preclude adequate examination of all relevant structures.[3] In addition, the presence of obstructing luminal lesions or strictures may prevent a complete EUS examination or increase the risk of adverse events and should thus be carefully described in the report.[1,26] Intraprocedural adverse events or patient intolerance to the procedure that ultimately compromises the quality or the extent of the examination should be noted.[3,27]
Description of relevant anatomical landmarks and lesions
It is important to accurately and routinely document all relevant anatomic structures, landmarks, and lesion characteristics using established descriptors based on procedure indication to maximize the utility of EUS reports, particularly for subsequent treatment planning.[1,3] Given the diverse indications for EUS, the definition of a complete examination will vary based on the primary indications. Overall, there is a paucity of data regarding the reporting of specific landmarks based on indication; however, the appropriate selection of the most relevant landmarks and findings will maximize the clinical efficacy and reflect the overall quality of the report.[12,26] It is also important to ensure the use of minimal standard terminology in all reports to ensure consistency.[28,29,30]
Our recommendations for the standard reporting of relevant landmarks and lesions based on common indications are as follows [Table 3]:
Table 3.
Reporting standards of relevant landmarks and components by indication
| Indication | Relevant landmarks and components |
|---|---|
| Biliary tree abnormalities | Biliary anatomy |
| Common bile duct | |
| Common hepatic duct | |
| Intrahepatic ducts | |
| Cystic duct | |
| Gallbladder (when present) | |
| Pancreatic duct | |
| Gallstones | |
| Location | |
| Size | |
| Relevant vasculature | |
| Solid and cystic lesions of the pancreas | Number and size of the lesion(s) |
| Location in the pancreas (head, uncinate, neck, and body) | |
| Morphology | |
| Biliary or pancreatic duct dilation | |
| Relevant vasculature | |
| Lymph nodes | |
| Pancreatic parenchymal abnormalities | Parenchyma |
| Echogenicity | |
| Heterogeneity | |
| Atrophy | |
| Lobularity | |
| Stranding | |
| Cysts | |
| Atrophy | |
| Pancreatic duct | |
| Anatomy | |
| Contour | |
| Dilation | |
| Echogenicity | |
| Biliary tree | |
| Dilation | |
| Gallstones | |
| Biliary sludge | |
| Ampulla | |
| Subepithelial lesions | Luminal layers |
| Lesion characteristics | |
| Size | |
| Echogenicity | |
| Shape | |
| Borders | |
| Doppler flow | |
| Locoregional lymphadenopathy | |
| Local vasculature | |
| Perianal and rectal lesions | Rectal wall layers |
| Sphincter apparatus | |
| Internal anal sphincter | |
| External anal sphincter | |
| Levator ani | |
| Puborectalis | |
| Perineal body | |
| Perirectal structures | |
| Bladder | |
| Male: Seminal vesicles, prostate | |
| Female: Uterus, vagina | |
| Fistulas | |
| Length | |
| Location | |
| Penetration into muscle layers (Parks classification) | |
| Continuity of internal/external anal sphincters | |
| Localized staging of tumors | Location of tumor |
| Depth of tumor invasion | |
| Tumour extent | |
| Lymph nodes: Mediastinal, perigastric, celiac | |
| Vasculature: Celiac axis, azygos vein | |
| Metastatic spread: Lungs, liver, peritoneum, mediastinum | |
| Ascites and pleural effusions | |
Biliary tree abnormalities
In the evaluation of biliary disorders, all reports should include a complete description of biliary tree anatomy including the common bile duct, common hepatic duct, and cystic duct.[31] The maximal caliber of the common bile duct and any associated dilation of the biliary tree, in addition to the presence or absence of any intraductal abnormalities such as gallstones, should be clearly reported. In addition, visualization and description of the gallbladder (both in terms of luminal contents and wall thickness) should be noted in patients who have not undergone cholecystectomy. A description of the duodenum and ampulla should be provided for the examination of possible obstructing lesions.
In cases where the primary indication involves evaluation for a suspected biliary stricture or mass, a thorough description should be given of both the biliary and pancreatic ducts. If any lesion or abnormality is found, its location, shape, size, echoendoscopic features, and demarcation should be noted.[29] For cases of suspected malignancy, a description of the celiac axis and surrounding lymph nodes as involved vasculature should be provided. Features of invasion and infiltration should be clearly noted. An evaluation of the liver and assessment for intra-abdominal ascites should be noted as a part of the examination for metastatic spread.
Solid and cystic lesions of the pancreas
Given the high potential for malignancy, EUS evaluation and reporting of solid pancreatic lesions should include elements focusing on both lesion characteristics and on potential invasiveness, locoregional spread, and/or presence of metastatic disease.[32] Thorough endosonographic assessment can significantly impact treatment decisions on whether a lesion is resectable.[33] Important reporting elements include tumor characteristics such as size, echogenicity, and associated pancreatic and/or biliary duct obstruction. A report of relevant vasculature including the celiac artery, hepatic artery, superior mesenteric artery, splenic vein, portal vein, superior mesenteric vein, and portal confluence for evidence of invasion or encasement should be provided. Locoregional lymph nodes around the celiac axis and peripancreatic region should be examined and clearly reported for any abnormalities. Evidence of metastasis in the liver should also be reported in addition to the presence or absence of ascites.
EUS evaluation of pancreatic cystic lesions requires accurate and detailed reporting, as morphological features can significantly impact diagnosis and management. All reports should include information regarding the number, size, shape, and location of each lesion. Any solid components should be clearly noted. Features including thickened cyst walls and septations should be included. Communication of the cyst with the pancreatic duct should be noted, as well as the presence and extent of pancreatic duct dilation.[31,34] The ampulla should be examined endoscopically for the presence of mucin secretion.
Pancreatic parenchymal abnormalities
EUS is commonly utilized for evaluation of inflammatory pancreatic disorders including chronic pancreatitis (CP) and idiopathic acute pancreatitis (AP).[35] Required reporting elements relevant to CP include a description of parenchymal echogenicity, homogeneity, lobularity, and the presence of cystic lesions. In addition, pancreatic ductal features such as main or side-branch dilation, the presence of any pancreatic duct (PD) calculi, and echogenicity of the main PD walls should be described.[36]
In the assessment of idiopathic and/or recurrent AP, a description should be provided of the pancreatic and biliary ducts and any associated stones and sludge, if present. The anatomy of the dorsal and ventral pancreatic ducts should be noted in cases of suspected pancreatic divisum. The pancreatic parenchyma should be well described and atrophy noted if present.
Subepithelial lesions of the gastrointestinal tract
It is important to clearly report the layer from which the suspected subepithelial lesion arises. A description of the echogenicity, shape, borders, and size of the lesion should be provided as this has significant implications in the diagnosis, malignant risk assessment, and management of these lesions.[37,38] Supplementary Doppler assessment and elastography of the lesion should be noted if conducted by the endoscopist.[37,39] Any adjacent lymph nodes and vasculature should also be described for evidence of local spread or invasion.
Perianal and rectal lesions
EUS is a useful modality that is occasionally used for evaluation of perianal fistulas, anal sphincter abnormalities, and rectal cancer.[24] A digital rectal examination with subjective assessment of rectal tone and direct visualization of the anus should be conducted prior to scope insertion to add supplementary diagnostic information and ensure safe scope insertion in cases of potential anal strictures.[40] For each indication, the involved rectal wall layers should be well described. Adjacent perirectal structures should be reported including the bladder, seminal vesicles and prostate in men, and uterus and vagina in women. For perianal fistulas, the location, orientation, extent, and penetration of the fistula should be carefully noted in relation to the internal and external anal sphincters and levator ani muscle. In the assessment of anal sphincter abnormalities, a clear description of the anal sphincter anatomy is necessary including the internal and external anal sphincters, perineal body, and puborectalis muscle. Discontinuity of the internal or external sphincters should be noted as this may correspond to patients with complete tears that may benefit from surgical intervention.[40]
In the local staging of rectal cancer, the proximal and distal tumor extent in relation to the anal verge should be noted. A clear description of the depth of tumor invasion in relation to rectal wall layers is required. The iliac vessels and any associated lymph nodes should be described, and any abnormalities noted. A comment should be provided on whether there is any evidence of invasion of surrounding perirectal organs.[24]
Local staging of tumors
We recommend incorporation of the TNM staging systems when evaluating lesions suspicious for malignancy of the luminal gastrointestinal tract, pancreas, and biliary tree.[3] Key components include depth of luminal wall invasion, involvement of adjacent structures, and evidence of vascular infiltration. Local lymph node size, shape, and irregularity should be described, as well as the evaluation for metastatic spread and ascites.[3,26] The report should acknowledge the limitation of EUS for evaluation of distal metastatic disease.
Sampling method and sample quality
The performance of FNA/B significantly improves the diagnostic accuracy of EUS. Multiple factors have been shown to impact its diagnostic yield.[12] ASGE and ESGE both suggest minimum quality standards of >85% diagnostic sampling yield of all EUS-guided biopsy procedures of solid pancreatic lesions.[12,26] Procedural factors including the needle type, needle gauge, number of passes, and sampling have all been shown to potentially impact diagnostic yield and should thus be documented in EUS reports.[41] The presence of rapid on-site cytologic evaluation should be indicated, as well as the specimen medium used to process the sample. Proper documentation of sampling details may aid endoscopists and their institution in identifying modifiable factors that may contribute to diagnostic yield to inform future studies and institutional quality improvement/assessment initiatives.
Documentation of specimen adequacy should be conducted by the endoscopist.[41] Sample characteristics, phase (solid or liquid), viscosity, and the amount of blood in the aspirate should be noted by the endoscopist in all cases, as they may impact pathology evaluation, particularly in cases of FNA.[3,41]
Photo documentation
Appropriate photo documentation of all relevant lesions and anatomical landmarks should be included in EUS reports and stored for future reference.[16,42] Systematic photo documentation in EUS is an indicator of procedure quality according to the ASGE; however, there has not yet been a study to validate this recommendation. Systematic photo documentation can facilitate surveillance EUS evaluations. If available, video documentation of sonographic and/or endoscopic views may be helpful to document intraprocedural findings or to plan future procedures.[43]
Patient comfort
Patient comfort during the procedure should be reported via a validated comfort scoring system, and is a recommended quality metric for all endoscopy units.[44,45] Multiple validated patient comfort scoring systems are available that are applicable to general endoscopy and colonoscopy; however, to date, no scoring system specific to EUS has been developed.[45,46]
Adverse events
All intraprocedural adverse events should be documented, in addition to any interventions performed as a result of such occurrences. Intraprocedural adverse events more likely to occur during EUS evaluation that are associated with diagnostic EUS and EUS-FNA/B include perforation, infection, and bleeding.[47] Systematic reporting of EUS adverse events is a key quality indicator in endoscopy and has been shown to be suboptimal in prior studies.[48] Routine reporting of all intraprocedural adverse events can aid in identifying trends that can be used to predict future outcomes and thus create areas for improvement.[49,50]
Postprocedural elements
Diagnoses and relevant findings
Clinical impressions should be clearly expressed and understandable by the referring physicians. They should be based on a synthesis of relevant data from the patient's clinical characteristics, previous relevant investigations, and intraprocedural findings. All likely differential diagnoses should be outlined, and significant findings outside of the procedure indication should be noted.[3,8]
Management and follow-up recommendations
All appropriate recommendations and alarm features based on the indication and endoscopic findings should be listed in the report. Details should include the continuation of prophylactic antibiotics and recommendations on the resumption of previously held antithrombotic agents. Potential follow-up with the endoscopist, referring physician, and/or other relevant care providers should be clearly outlined. Each action plan item should be listed and should include the rationale, responsible provider, and suggested timing.[16]
The report should indicate that postprocedural information was provided to the patient and/or their caregivers. Quality standards from the Canadian Association of Gastroenterology have previously outlined key postprocedural information that should be provided to patients on the same day after endoscopy.[9,16] The provision of procedure information to patients immediately after endoscopy has been shown to reduce anxiety, improve patient recall and compliance, and increase referring provider satisfaction.[51,52,53]
Pathology reports
The EUS report should include a statement indicating the plan to share pathology reports to members of the patient's circle of care. The endoscopist should ensure timely dissemination of the pathology results to relevant stakeholders, including the referring physician and family physician, and clearly identify who will communicate the pathology report to the patient when it becomes available.[9,16]
DISCUSSION
Our review provides a summary of the available evidence and expert recommendations regarding reporting elements to be included in EUS procedures. With the ongoing drive to deliver high-quality EUS procedures, standardized reporting elements will be important for monitoring quality and promoting adherence to established targets.[54]
Overall, the implementation of effective quality reporting frameworks may involve short educational sessions to endoscopists and trainees, in addition to ease of access to standardized documentation templates (Supplementary Appendix 3), all of which have been shown to be effective.[55,56,57] Use of computer-based reporting systems may help in ensuring quality documentation.[6] With the increasing use of electronic reporting, it is important to ensure that platforms include mandatory fields for reporting elements that are built around quality indicators.
Supplementary Appendix 3.
Sample EUS report template
| Preprocedural | Patient name and medical record number |
| Patient date of birth | |
| Date of procedure | |
| Procedure type and indication | |
| Primary endoscopist name (and assistant/trainee if applicable): | |
| Preoperative diagnosis | |
| Postoperative diagnosis | |
| Clinical history | |
| Reason for referral | |
| Brief clinical summary of primary indication for EUS | |
| Summary of relevant preprocedural investigations | |
| List of pertinent comorbid conditions relevant to case and potentially impacting procedural success/yield | |
| Highlight key medications and date if held | |
| Anesthesia | |
| Type of agents (topical, intravenous) and dosage | |
| Practitioner administering anesthesia | |
| Preprocedural prophylaxis | |
| Type of antibiotic, dosage, and length of course if administered | |
| Pre-procedural preparation | |
| Duration of NPO prior to procedure | |
| Bowel preparation as appropriate for procedure | |
| Intra-procedural | Procedural description |
| Document the type and model of scope used | |
| Description of landmarks and relevant characteristics | |
| Clear characterization of principle finding for procedure | |
| If lesion present description of location, shape, size, invasion, echofeatures, and vascularity | |
| Any regional lymphadenopathy | |
| Type of equipment used and model for sampling if applicable | |
| Needle type and gauge, tissue acquisition technique, number of passes | |
| Impression on quality of sample | |
| Quality of bowel preparation if applicable | |
| Adverse events | |
| Any intraprocedural adverse events and subsequent management | |
| Patient comfort | |
| Postprocedural | Summary |
| Summary of the major findings during examination, sampling or therapeutic intervention if completed | |
| Overall impression and diagnosis | |
| Patients comfort and tolerance during the procedure | |
| Plan | |
| Timing for resuming anticoagulation if held | |
| Sharing of pathology results | |
| Next steps in management and follow-up providers listed | |
| Communicating the procedure and pathology results with the patient |
NPO: Nil per os
Adherence with quality endoscopic reporting may also be improved with the use of audit and feedback (A&F), which has been shown to improve the quality of other endoscopic procedures.[58] Possible mechanisms for this potential improvement include the Hawthorne effect, in which the behavior of subjects is improved simply as a result of their knowledge of being observed. In this context, the durability of A&F in maintaining a long-term improvement is unclear.[8,59,60] Nevertheless, it is crucial for all endoscopy units to achieve and maintain quality indicators in EUS that will require suitable monitoring practices and quality reporting.
Although we have provided guidance on key components to be included in all diagnostic EUS reports to ensure quality, a number of limitations exist with our review. Notably, standards for reporting of therapeutic EUS procedures were not addressed in our review. With the rapidly growing field of therapeutic EUS, future statements and guidelines are needed to guide endoscopists on key reporting elements. Finally, in any endoscopic procedure, incidental findings may occur that are outside the primary procedural indication. The extent to which incidental findings in EUS should be further evaluated is outside the scope of our review; however, it is important to note that incidental findings in EUS may represent significant pathology and should therefore be noted in the report to prompt future evaluation as necessary.[61]
CONCLUSIONS
Standardizing reporting elements is an important step toward improving the quality of care for patients undergoing EUS procedures. Our review and recommended reporting elements can be used to guide best practices and quality improvement in EUS.
Supplementary Materials
Supplementary information is linked to the online version of the paper on the Endoscopic Ultrasound website.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
SUPPLEMENTARY APPENDICES
Supplementary Appendix 1. Search Strategy
PubMed
((endoscopic ultrasonography[MeSH Terms]) OR EUS) AND (Quality Indicators OR Reporting)
Limit to: Humans
Ovid Medline
exp Endosonography/or EUS.mp.
Endoscopic Ultrasound.mp.
exp Quality Indicators, Health Care/or Quality Indicators. Mp.
Procedural Reporting.mp.
exp Quality Assurance, Health Care/
1 or 2
3 or 4 or 5
6 and 7
Limit 8 to huma
Ovid Embase
exp endoscopic ultrasonography/
EUS.mp.
Quality Indicators.mp.
Procedural Reporting.mp.
Quality Reporting.mp.
1 or 2
3 or 4 or 5
6 and 7
Limit 8 to human
CINAHL Plus
(Endoscopic ultrasound or EUS) AND Quality indicators OR Procedure reporting
Limiters: Human; Language: English, French
Expanders: Apply equivalent subjects
Supplementary Appendix 2.
PRISMA Diagram
REFERENCES
- 1.Barbetta A, Faraz S, Shah P, et al. Quality of endoscopy reports for esophageal cancer patients: Where do we stand? J Gastrointest Surg. 2018;22:778–84. doi: 10.1007/s11605-018-3710-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Raju G, Lum P, Ross W, et al. Quality of endoscopy reporting at index colonoscopy significantly impacts outcome of subsequent EMR in patients with >20 mm colon polyps. Endosc Int Open. 2019;7:E361–E366. doi: 10.1055/a-0746-3520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lachter J, Bluen B, Waxman I, Bellan W. Establishing a quality indicator format for endoscopic ultrasound. World J Gastrointest Endosc. 2013;5:574–80. doi: 10.4253/wjge.v5.i11.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Jonge V, Sint Nicolaas J, Cahen DL, et al. Quality evaluation of colonoscopy reporting and colonoscopy performance in daily clinical practice. Gastrointest Endosc. 2012;75:98–106. doi: 10.1016/j.gie.2011.06.032. [DOI] [PubMed] [Google Scholar]
- 5.Hadlock SD, Liu N, Bernstein M, et al. The quality of colonoscopy reporting in usual practice: Are endoscopists reporting key data elements? Can J Gastroenterol Hepatol. 2016 doi: 10.1155/2016/1929361. 2016:1929361. https://www.hindawi.com/journals/cjgh/2016/1929361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lieberman DA, Faigel DO, Logan JR, et al. Assessment of the quality of colonoscopy reports: Results from a multicenter consortium. Gastrointest Endosc. 2009;69:645–53. doi: 10.1016/j.gie.2008.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gardner TB, Taylor DJ, Gordon SR. Reported findings on endoscopic ultrasound examinations for chronic pancreatitis: Toward establishing an endoscopic ultrasound quality benchmark. Pancreas. 2014;43:37–40. doi: 10.1097/MPA.0b013e3182a85e1e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schwab R, Pahk E, Lachter J. Impact of endoscopic ultrasound quality assessment on improving endoscopic ultrasound reports and procedures. World J Gastrointest Endosc. 2016;8:362–7. doi: 10.4253/wjge.v8.i8.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beaulieu D, Barkun AN, Dubé C, et al. Endoscopy reporting standards. Can J Gastroenterol. 2013;27:286–92. doi: 10.1155/2013/145894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Coté GA, Hovis CE, Kohlmeier C, et al. Training in EUS-guided fine needle aspiration: Safety and diagnostic yield of attending supervised, trainee-directed FNA from the Onset of training. Diagn Ther Endosc. 2011 doi: 10.1155/2011/378540. 2011:378540. https://www.hindawi.com/journals/dte/2011/378540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khan U, Abunassar M, Chatterjee A, et al. Advanced endoscopy trainee involvement early in EUS training may be associated with an increased risk of adverse events. J Can Assoc Gastroenterol. 2020;3:83–90. doi: 10.1093/jcag/gwy066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wani S, Wallace MB, Cohen J, et al. Quality indicators for EUS. Gastrointest Endosc. 2015;81:67–80. doi: 10.1016/j.gie.2014.07.054. [DOI] [PubMed] [Google Scholar]
- 13.Anderson MA, Ben-Menachem T, Gan SI, et al. Management of antithrombotic agents for endoscopic procedures. Gastrointest Endosc. 2009;70:1060–70. doi: 10.1016/j.gie.2009.09.040. [DOI] [PubMed] [Google Scholar]
- 14.Khashab MA, Chithadi KV, Acosta RD, et al. Antibiotic prophylaxis for GI endoscopy. Gastrointest Endosci. 2015;81:81–9. doi: 10.1016/j.gie.2014.08.008. [DOI] [PubMed] [Google Scholar]
- 15.Colán-Hernández J, Sendino O, Loras C, et al. Antibiotic prophylaxis is not required for endoscopic ultrasonography-guided fine-needle aspiration of pancreatic cystic lesions, based on a randomized trial. Gastroenterology. 2020;158:1642–9.e1. doi: 10.1053/j.gastro.2020.01.025. [DOI] [PubMed] [Google Scholar]
- 16.Armstrong D, Barkun A, Bridges R, et al. Canadian Association of Gastroenterology consensus guidelines on safety and quality indicators in endoscopy. Can J Gastroenterol. 2012;26:17–31. doi: 10.1155/2012/173739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Facciorusso A, Buccino RV, Muscatiello N. How to measure quality in endoscopic ultrasound. Ann Transl Med. 2018;6:266. doi: 10.21037/atm.2018.03.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Polkowski M, Larghi A, Weynand B, et al. Learning, techniques, and complications of endoscopic ultrasound (EUS)-guided sampling in gastroenterology: European Society of Gastrointestinal Endoscopy (ESGE) Technical Guideline. Endoscopy. 2012;44:190–206. doi: 10.1055/s-0031-1291543. [DOI] [PubMed] [Google Scholar]
- 19.McQuaid KR, Laine L. A systematic review and meta-analysis of randomized, controlled trials of moderate sedation for routine endoscopic procedures. Gastrointest Endosc. 2008;67:910–23. doi: 10.1016/j.gie.2007.12.046. [DOI] [PubMed] [Google Scholar]
- 20.Campbell JA, Irvine AJ, Hopper AD. Endoscopic ultrasound sedation in the United Kingdom: Is life without propofol tolerable? World J Gastroenterol. 2017;23:560–2. doi: 10.3748/wjg.v23.i3.560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim MG, Park SW, Kim JH, et al. Etomidate versus propofol sedation for complex upper endoscopic procedures: A prospective double-blinded randomized controlled trial. Gastrointest Endosc. 2017;86:452–61. doi: 10.1016/j.gie.2017.02.033. [DOI] [PubMed] [Google Scholar]
- 22.Jensen JT, Hornslet P, Konge L, et al. High efficacy with deep nurse-administered propofol sedation for advanced gastroenterologic endoscopic procedures. Endosc Int Open. 2016;4:E107–11. doi: 10.1055/s-0041-107899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fujii LL, Levy MJ. Basic techniques in endoscopic ultrasound-guided fine needle aspiration for solid lesions: Adverse events and avoiding them. Endosc Ultrasound. 2014;3:35–45. doi: 10.4103/2303-9027.123006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schwartz DA, Harewood GC, Wiersema MJ. EUS for rectal disease. Gastrointest Endosc. 2002;56:100–9. doi: 10.1067/mge.2002.125233. [DOI] [PubMed] [Google Scholar]
- 25.Kastenberg D, Bertiger G, Brogadir S. Bowel preparation quality scales for colonoscopy. World J Gastroenterol. 2018;24:2833–43. doi: 10.3748/wjg.v24.i26.2833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Domagk D, Oppong KW, Aabakken L, et al. Performance measures for endoscopic retrograde cholangiopancreatography and endoscopic ultrasound: A European Society of Gastrointestinal Endoscopy (ESGE) Quality Improvement Initiative. United European Gastroenterol J. 2018;6:1448–60. doi: 10.1177/2050640618808157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ootaki C, Stevens T, Vargo J, et al. Does general anesthesia increase the diagnostic yield of endoscopic ultrasound-guided fine needle aspiration of pancreatic masses? Anesthesiology. 2012;117:1044–50. doi: 10.1097/ALN.0b013e31826e0590. [DOI] [PubMed] [Google Scholar]
- 28.Aabakken L, Rembacken B, Olivier LeMoine U, et al. Minimal standard terminology for gastrointestinal endoscopy. MST 3.0. Endoscopy. 2009;41:727–8. doi: 10.1055/s-0029-1214949. [DOI] [PubMed] [Google Scholar]
- 29.Aabakken L. Standardized terminology in endoscopic ultrasound. Eur J Ultrasound. 1999;10:179–83. doi: 10.1016/s0929-8266(99)00052-x. [DOI] [PubMed] [Google Scholar]
- 30.Delvaux M, Crespi M, Armengol-Miro JR, et al. Minimal standard terminology for digestive endoscopy: Results of prospective testing and validation in the GASTER project. Endoscopy. 2000;32:345–55. doi: 10.1055/s-2000-7384. [DOI] [PubMed] [Google Scholar]
- 31.Hawes RH, Fockens P, Varadarajulu S. Endosonography. 2018 [Google Scholar]
- 32.Santo E, Bar-Yishay I. Pancreatic solid incidentalomas. Endosc Ultrasound. 2017;6:S99–S103. doi: 10.4103/eus.eus_72_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tempero MA, Malafa MP, Behrman SW, et al. Pancreatic adenocarcinoma, version 2.2014: Featured updates to the NCCN guidelines. J Natl Compr Canc Netw. 2014;12:1083–93. doi: 10.6004/jnccn.2014.0106. [DOI] [PubMed] [Google Scholar]
- 34.ASGE Standards of Practice Committee, Muthusamy VR, Chandrasekhara V, et al. The role of endoscopy in the diagnosis and treatment of cystic pancreatic neoplasms. Gastrointest Endosc. 2016;84:1–9. doi: 10.1016/j.gie.2016.04.014. [DOI] [PubMed] [Google Scholar]
- 35.ASGE Standards of Practice Committee, Chandrasekhara V, Chathadi KV, et al. The role of endoscopy in benign pancreatic disease. Gastrointest Endosc. 2015;82:203–14. doi: 10.1016/j.gie.2015.04.022. [DOI] [PubMed] [Google Scholar]
- 36.Catalano MF, Sahai A, Levy M, et al. EUS-based criteria for the diagnosis of chronic pancreatitis: The Rosemont classification. Gastrointest Endosc. 2009;69:1251–61. doi: 10.1016/j.gie.2008.07.043. [DOI] [PubMed] [Google Scholar]
- 37.Standards of Practice Committee, Faulx AL, Kothari S, et al. The role of endoscopy in subepithelial lesions of the GI tract. Gastrointest Endosc. 2017;85:1117–32. doi: 10.1016/j.gie.2017.02.022. [DOI] [PubMed] [Google Scholar]
- 38.Alkhatib AA, Faigel DO. Endoscopic ultrasonography-guided diagnosis of subepithelial tumors. Gastrointest Endosc Clin N Am. 2012;22:187–205, vii. doi: 10.1016/j.giec.2012.04.006. [DOI] [PubMed] [Google Scholar]
- 39.Ignee A, Jenssen C, Hocke M, et al. Contrast-enhanced (endoscopic) ultrasound and endoscopic ultrasound elastography in gastrointestinal stromal tumors. Endosc Ultrasound. 2017;6:55–60. doi: 10.4103/2303-9027.200216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ciobanu L, Badea R. Endoluminal Ultrasonography of the Rectum and the Anal Canal. 2017 [Google Scholar]
- 41.Weston BR, Bhutani MS. Optimizing diagnostic yield for EUS-guided sampling of solid pancreatic lesions: A Technical Review. Gastroenterol Hepatol (N Y) 2013;9:352–63. [PMC free article] [PubMed] [Google Scholar]
- 42.AIUM Practice Parameter for Documentation of an Ultrasound Examination. Parameter for Documentation of an Ultrasound Examination. J Ultrasound Med. 2020:39–E1-4. doi: 10.1002/jum.15187. [DOI] [PubMed] [Google Scholar]
- 43.ASGE Technology Committee, Murad FM, Banerjee S, et al. Image management systems. Gastrointest Endosc. 2014;79:15–22. doi: 10.1016/j.gie.2013.07.048. [DOI] [PubMed] [Google Scholar]
- 44.ASGE Endoscopy Unit Quality Indicator Taskforce, Day LW, Cohen J, et al. Quality indicators for gastrointestinal endoscopy units. VideoGIE. 2017;2:119–40. doi: 10.1016/j.vgie.2017.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chan BP, Hussey A, Rubinger N, et al. Patient comfort scores do not affect endoscopist behavior during colonoscopy, while trainee involvement has negative effects on patient comfort. Endosc Int open. 2017;5:E1259–67. doi: 10.1055/s-0043-120828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Burtea D, Dimitriu A, Maloş A, et al. Assessment of the quality of outpatient endoscopic procedures by using a patient satisfaction questionnaire. Curr Health Sci J. 2019;45:52–8. doi: 10.12865/CHSJ.45.01.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.ASGE Standards of Practice Committee, Early DS, Acosta RD, et al. Adverse events associated with EUS and EUS with FNA. Gastrointest Endosc. 2013;77:839–43. doi: 10.1016/j.gie.2013.02.018. [DOI] [PubMed] [Google Scholar]
- 48.Amato A, Bianchi M, Fabbri C, et al. Quality indicators of endoscopic ultrasonography: A nationwide survey. Dig Liver Dis. 2018;50:E106. [Google Scholar]
- 49.Romagnuolo J, Cotton PB, Eisen G, et al. Identifying and reporting risk factors for adverse events in endoscopy.Part II: Noncardiopulmonary events. Gastrointest Endosc. 2011;73:586–97. doi: 10.1016/j.gie.2010.11.023. [DOI] [PubMed] [Google Scholar]
- 50.Romagnuolo J, Cotton PB, Eisen G, et al. Identifying and reporting risk factors for adverse events in endoscopy.Part I: Cardiopulmonary events. Gastrointest Endosc. 2011;73:579–85. doi: 10.1016/j.gie.2010.11.022. [DOI] [PubMed] [Google Scholar]
- 51.Spodik M, Goldman J, Merli K, et al. Providing an endoscopy report to patients after a procedure: A low-cost intervention with high returns. Gastrointest Endosc. 2008;67:103–11. doi: 10.1016/j.gie.2007.08.035. [DOI] [PubMed] [Google Scholar]
- 52.Lachter J, Feldman R, Krief I, et al. Satisfaction of the referring physician: A quality control study focusing on EUS. J Clin Gastroenterol. 2007;41:889–93. doi: 10.1097/01.mcg.0000225688.83206.2c. [DOI] [PubMed] [Google Scholar]
- 53.Siddiqui UD, Rossi F, Padda MS, et al. Patient preferences after endoscopic ultrasound with fine needle aspiration (EUS-FNA) diagnosis of pancreas cancer: Rapid communication valued over long-term relationships. Pancreas. 2011;40:680–1. doi: 10.1097/MPA.0b013e3182197359. [DOI] [PubMed] [Google Scholar]
- 54.Aabakken L, Barkun AN, Cotton PB, et al. Standardized endoscopic reporting. J Gastroenterol Hepatol. 2014;29:234–40. doi: 10.1111/jgh.12489. [DOI] [PubMed] [Google Scholar]
- 55.Coe SG, Panjala C, Heckman MG, et al. Quality in colonoscopy reporting: An assessment of compliance and performance improvement. Dig Liver Dis. 2012;44:660–4. doi: 10.1016/j.dld.2012.03.022. [DOI] [PubMed] [Google Scholar]
- 56.Harris N, Telford J, Yonge J, et al. Improvement of endoscopic reports with implementation of a dictation template. J Can Assoc Gastroenterol. 2019 doi: 10.1093/jcag/gwz033. doi:10.1093/jcag/gwz033.https://academic.oup.com/jcag/advancearticleldoi/10.1093/jcag/gwz033/5680684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Coe SG, Raimondo M, Woodward TA, et al. Quality in EUS: An assessment of baseline compliance and performance improvement by using the American Society for Gastrointestinal Endoscopy-American College of Gastroenterology quality indicators. Gastrointest Endosc. 2009;69:195–201. doi: 10.1016/j.gie.2008.04.032. [DOI] [PubMed] [Google Scholar]
- 58.Bishay K, Causada-Calo N, Scaffidi MA, et al. Associations between endoscopist feedback and improvements in colonoscopy quality indicators: A systematic review and meta-analysis. Gastrointest Endosc. 2020;92:1030–40. doi: 10.1016/j.gie.2020.03.3865. [DOI] [PubMed] [Google Scholar]
- 59.Lisboa-Gonçalves P, Libânio D, Marques-Antunes J, et al. Quality of reporting in upper gastrointestinal endoscopy: Effect of a simple audit intervention. GE Port J Gastroenterol. 2018;26:24–32. doi: 10.1159/000487145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hernandez LV, Deas TM, Catalano MF, et al. Longitudinal assessment of colonoscopy quality indicators: A report from the Gastroenterology Practice Management Group. Gastrointest Endosc. 2014;80:835–41. doi: 10.1016/j.gie.2014.02.1043. [DOI] [PubMed] [Google Scholar]
- 61.Sotoudehmanesh R, Arab P, Ali-Asgari A. Incidental findings on upper gastrointestinal endoscopic ultrasonography. J Diagnostic Med Sonogr. 2013;29:73–776. [Google Scholar]


