Abstract
Objectives
To investigate the utilisation of different treatment modalities for patients with laryngeal cancer (LC) during last decade in Poland.
Setting
Retrospective population-based study.
Participants
Patients with LC treated between January 2009 and December 2018.
Primary and secondary outcome measures
The contemporary utilisation of treatment modalities of LC: surgery with intent of radical resection (total or partial laryngectomy), radiotherapy (RT) and chemoradiotherapy (CRT).
Results
There was determined the overall number of 22 957 new diagnosis of LC from 2010 to 2018 and confirmed the steady decrease in the incidence rate of LC in the following years from 7.7 to 6.03. The mean age of patients with LC was raising by an average of 0.3832 of year per year. There was observed decrease in number of total laryngectomies (TLs) in subsequent years (from 1122 in 2009 to 776 in 2018). The number of procedures involving partial laryngeal resection was within stable ranges however the upward trend was observed separately for vocal cordectomy. There was established decreased involvement of surgery in LC treatment from 52.8% in 2009 to 24.3% in 2016 with the subsequent rise to 33.7% in 2018. The percentage of patients receiving RT increased from 23.8% in 2009 to 42.1% in 2013 with the next decrease to 25.7% in 2018. The utilisation of CRT in LC treatment was progressively increasing over analysed years from 23.4% in 2009 reaching 40.6% in 2018.
Conclusions
The presented data revealed an increase in total number of organs preserving treatment modality with CRT in subsequent years with decreasing number of TLs in Polish patients with LC.
Keywords: head & neck surgery, laryngology, adult radiotherapy, head & neck tumours
Strengths and limitations of the study.
This study is based on the national cohort of patients with laryngeal cancer.
It investigates the trends in treatment modalities during the last decade in the presence of the overall decline in outcomes.
Comparison of organs preserving treatment modality with chemoradiotherapy and surgical procedure of total laryngectomy was analysed in subsequent years.
The percentage of transoral laryngeal procedures and open partial laryngectomies was analysed.
Information concerning stage, locoregional control, metastatic disease, prior or concurrent cancer diagnosis, received radiation doses, data regarding CT administration with a number of cycles, specific agents, doses and long-term toxicities were not analysed.
Introduction
Approximately 177 422 new cases of laryngeal cancer (LC) were diagnosed worldwide in 2018 according to the estimation of the International Agency for Research on Cancer and the forecasts indicate an increasing trend in the future.1 In 2017, population-based studies prepared by the Polish National Cancer Registry confirmed 2224 new cases of LC and 1580 deaths due to this type of cancer.2 For comparison, the incidence and mortality due to LC reported in 2009 was 2413 and 1585, respectively.3 Although statistics show decreasing rates for new diagnoses in our country, survival rates are not improving. Recommendations for primary treatment of LC differ depending on the stage of the disease and the site of cancer within the organ but also follow certain trends that promote organ preservation methods and depend on the availability of equipment. Historically, total laryngectomy (TL) with postoperative radiation was standard treatment for advanced stage (T3, T4) LC. However, the results of the Department of Veterans Affairs4 Laryngeal Cancer Study from 1991 and the Radiation Therapy Oncology Group (RTOG) 91-11 Study from 2003 modified the treatment paradigm focusing on conservative laryngeal therapy with chemoradiation (CRT), primarily in the USA and subsequently in Europe.4 5 This approach has influenced the management of advanced LC and the number of primary laryngectomies, thus rendering the procedure rescue treatment. For T3 and T4 LC, current treatment protocols recommend concomitant or sequential radiotherapy (RT) with chemotherapy (CT) or TL. However, the radiological evidence of cartilage tumour infiltration is rather an indication for surgical resection.6 In contrast, the early stages of LC (T1 and T2) should always be treated with an initial intent of organ preservation. The recommendations include surgical resection or primary RT and both methods give comparable oncological outcomes. Both these treatment modalities have evolved significantly over the last two decades. The prevalence and advances in transoral endoscopic surgical methods have replaced the open laryngeal surgery in primary treatment of T1 and T2 LC. The improvements in radiation techniques have also reduced the contribution of upfront RT treatment and provided high-quality design and delivery with target volume determination and the use of intensity-modulated radiation therapy (IMRT).7 This increases the therapeutic dose within the tumour while optimally sparing normal tissue adjacent to the tumour, for example, the carotid arteries.
The purpose of this study was to investigate the trends in treatment modalities during the last decade in patients with LC in Poland, based on the national cohort of patients from the National Health Fund Database in order to evaluate the findings, compare them with global trends and assess the possibilities for improving survival rates.
Materials and Methods
Patients and public involvement statement
All data used in the study proposals were deidentified and therefore the approval of the Institutional Review Board was waived. Patients were not involved in the study.
The study design was a retrospective population-based study. The data concerned patients with LC and their treatment procedures between January 2009 and December 2018 and were obtained from the National Database of Hospitalized Patients maintained by the National Health Fund (NFZ) of Poland.8 The database compiles all data related to hospitalisations in public and private hospitals financed from public sources. The available database contains medical data (including diagnoses and procedures), identification numbers, dates of birth, area codes and patient genders. Diagnoses are coded according to the International Classification of Diseases, 10th Revision (ICD-10), while surgical procedures are coded using the International Classification of Diseases, 9th Revision (ICD-9).
Patients with laryngeal carcinoma were identified according to the ICD-10 classification with the following codes: C32—malignant neoplasm of larynx, C32.0—malignant neoplasm of glottis, C32.1—malignant neoplasm of supraglottis, C32.2—malignant neoplasm of subglottis, C32.3—malignant neoplasm of laryngeal cartilage, C32.8—malignant neoplasm of overlapping sites of larynx, C32.9—malignant neoplasm of larynx, unspecified, C10.1—malignant neoplasm of anterior surface of epiglottis and C13.1—malignant neoplasm of aryepiglottic fold, hypopharyngeal aspect. Procedures of interest included surgical resection of different extent according to the ICD-9 classification. All of the following procedures were included in the analysis: 30.1 hemilaryngectomy, 30.2 other partial laryngectomy, 30.21 epiglottidectomy, 30.22 vocal cordectomy, 30.23 partial laryngectomy with reconstruction, 30.24 laryngeal cartilage resection, 30.29 other partial laryngectomy, 30.3 complete laryngectomy, 30.31 en bloc laryngeal resection with thyroidectomy and tracheostomy, 30.32 laryngopharyngectomy, 30.39 other complete laryngectomy, 30.4 radical laryngectomy (with radical neck dissection), 30.41 radical laryngectomy (with radical neck dissection) and with thyroidectomy and tracheostomy, 30.49 other radical laryngectomy, 30.0 excision or destruction of lesion or tissue of larynx, 30.09 other excision or destruction of lesion or tissue of larynx, 31.5 local excision or destruction of larynx lesion or tissue of trachea. The RT and CT treatment was identified according to the ICD-10 classification (Z51.0—antineoplastic radiation therapy and Z51.1—antineoplastic CT).
Data on the population of Polish citizens were obtained from Statistics Poland (Główny Urząd Statystyczny).9
Taking into account different treatment modalities for LC, the following three options were analysed: surgery with intent of radical resection of LC (total or partial laryngectomy) including patients who received induction CRT or adjuvant RT/CRT; RT—including patients treated with RT alone or following induction CT and CRT—including patients treated with CRT alone or following induction CT.
Statistical analysis
Python V.3.3.6 and Microsoft Excel 2016 were used to separate and analyse patient data from datasets. For quantitative variables, basic statistics (mean and SD) were calculated. A linear regression model was used to analyse age variability of patients. The incidence rate is the number of new cases divided by 100 000 citizens.
Results
Considering the selected ICD-10 codes, the overall number of 61 571 hospitalisations related to LC from 2009 to 2018 in Poland was identified. The number of hospitalisations per year ranged from 5763 to 6674 without any specified trend. The highest numbers of hospital stays were recorded for C32.0—malignant neoplasm of glottis (24 208) as well as C32.8—malignant neoplasm of overlapping sites of larynx and C32.9—malignant neoplasm of larynx, unspecified (13 068 and 17 268, respectively). Taking into account only primary hospitalisation and the determination of the LC diagnosis, the overall number of 22 957 new diagnoses of LC from 2010 to 2018 was determined. This number could not be established for 2009 due to incomplete data in the register for previous years and the possibility of revaluation. A steady decrease in the incidence rate of LC was observed in the following years from 7.7 to 6.03 (mean incidence rate 6.63; 95% CI: 6.23 to 7.03). The trend was especially significant for male patients (the decrease in new diagnoses from 2577 in 2010 to 1987 in 2018) but was not as evident for female patients (from 388 in 2010 to 330 in 2018). In contrast to the incidence rate, the mean age of patients with diagnosed LC significantly increased, growing on average by 0.3832 (95% CI: 0.3381 to 0.4283) years per year. The trend was described by means of linear regression using the following formula: Y=0.3832*X+61.345, where X is the serial number of the year (ie, 2009-1, 2010-2, etc). The regression model was very well fitted to the data and explained 99% (R2=0.9909) of age variability of patients. Demographic data on population revealed that about 70% of the LC patients were urban dwellers. The percentage of urban dwellers has slightly decreased over the last 10 years (table 1).
Table 1.
The demographical characteristic of patients with new diagnosis of laryngeal cancer in Polish population from 2010 to 2018
| C32 patients | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | All |
| No of patients | 2965 | 2682 | 2653 | 2571 | 2520 | 2539 | 2360 | 2350 | 2317 | 22 957 |
| Population (in thousands) | 38 517 | 38 526 | 38 534 | 38 502 | 38 484 | 38 455 | 38 427 | 38 422 | 38 413 | — |
| Incidence rate* | 7.70 | 6.96 | 6.88 | 6.68 | 6.55 | 6.60 | 6.14 | 6.12 | 6.03 | — |
| Age mean±SE | 62.33±9.43 | 62.72±9.27 | 62.72±9.19 | 63.42±9.13 | 63.56±8.87 | 64.1±8.72 | 64.05±8.99 | 64.49±8.99 | 64.82±8.97 | 63.58±9.06 |
| Women (%) |
388 (13.09) | 336 (12.53) | 351 (13.23) | 364 (14.16) | 351 (13.93) | 353 (13.9) | 330 (13.98) | 308 (13.11) | 330 (14.24) | 3111 (13.57) |
| Men (%) |
2577 (86.91) | 2346 (87.47) | 2302 (86.77) | 2207 (85.84) | 2169 (86.07) | 2186 (86.10) | 2030 (86.02) | 2042 (86.89) | 1987 (85.76) | 19 846 (86.43) |
| Urban residence (%) | 2184 (73.66) | 1940 (72.33) | 1913 (72.11) | 1868 (72.66) | 1802 (71.51) | 1822 (71.76) | 1672 (70.85) | 1666 (70.89) | 1617 (69.79) | 16 484 (71.73) |
| Rural resistance (%) |
781 (26.34) | 742 (27.67) | 740 (27.89) | 703 (27.34) | 718 (28.49) | 717 (28.24) | 688 (29.15) | 684 (29.11) | 700 (30.21) | 6473 (28.27) |
*Incidence rate=no of all C32 new diagnoses/100 000 citizens
Analysing the number of individual ICD-10 codes related to newly diagnosed LC, the highest number of patients with C32.0—malignant neoplasm of glottis (12 566) was identified. A relatively high number of C32.9—malignant neoplasm of larynx, unspecified and C32—malignant neoplasm of larynx were found (5686 and 1118, respectively), however neither of them specifies laryngeal location or cancer stage. The new diagnosis of advanced cancer stages with cartilage infiltration C32.3 and extralaryngeal invasion C32.8 were recognised in 286 and 5279 patients, respectively. The calculated total hospitalisation coefficient (number of hospitalisations/number of new diagnoses) for LC patients was 2.04 during the analysed period. Patients with C32.9 were hospitalised most frequently, on average 2.74 hospitalisations.
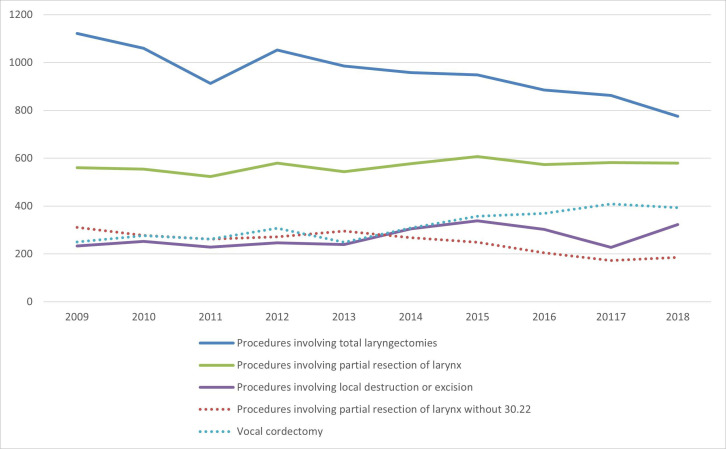
The surgical procedures applied to LC treatment were categorised according to the extent of the resection. Procedures involving TL (30.3, 30.31, 30.32, 30.39, 30.4, 30.41, 30.49) were performed in 9562 patients during the 10-year period. The most common procedure was 30.32 laryngopharyngectomy—5234 (54.7%) and the second in order 30.39. Other complete laryngectomy—2454 (25.7%). The partial resection of the larynx (30.1, 30.2, 30.21, 30.22, 30.23, 30.24, 30.29) was applied 5681 times as surgical treatment method over this time with significant advantage of the 30.22 vocal cordectomy procedure performed 3182 times (56%). The overall number of procedures restricted to local excision or destruction of the laryngeal lesion (30.0, 30.09, 31.5) was 2696 (table 2). The number of TLs decreased in subsequent analysed years (from 1122 in 2009 to 776 in 2018). Contrary to TL, the number of procedures involving partial laryngeal resection was quite stable in total count with 561 procedures in 2009 and 579 in 2018. However, the upward trend was observed separately for 30.22 vocal cordectomy procedure (from 250 in 2009 to 393 in 2018) at the cost of a downward trend for other procedures of partial laryngeal resection (figure 1; online supplemental file 1).
Table 2.
The number of surgical procedures applied to patients with laryngeal cancer with relation to extension of resection during the 10-year period
| Year/no (n) | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 20 117 | 2018 | Total |
| Surgical procedures involving total laryngectomy | |||||||||||
| (n) | 1122 | 1060 | 913 | 1052 | 985 | 958 | 948 | 885 | 863 | 776 | 9562 |
| Surgical procedures involving partial resection of larynx | |||||||||||
| (n) | 561 | 554 | 524 | 579 | 544 | 577 | 607 | 574 | 582 | 579 | 5681 |
| Surgical procedures involving local destruction or excision of laryngeal tissue | |||||||||||
| (n) | 233 | 253 | 229 | 247 | 239 | 305 | 338 | 302 | 227 | 323 | 2696 |
Figure 1.
Different surgical procedures involving total laryngectomy, partial resection of the larynx or local destruction or excision applied to patients with laryngeal cancer in 2009–2018.
bmjopen-2020-045308supp001.pdf (38.1KB, pdf)
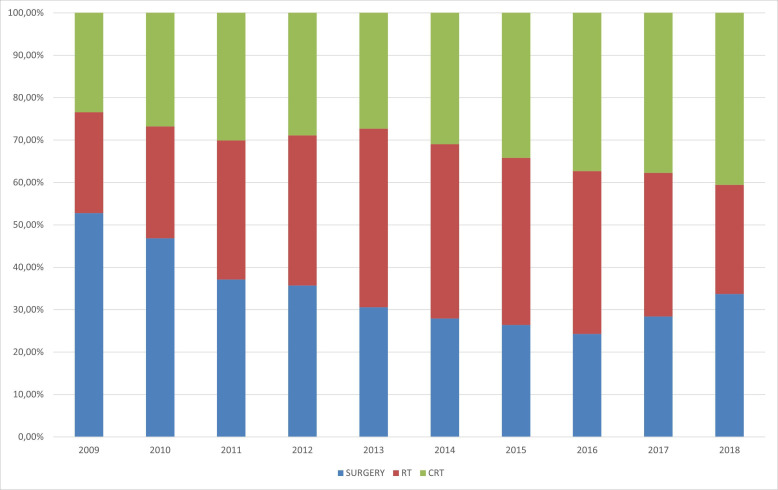
Considering the surgical procedures with the intent of radical resection of LC (total or partial laryngectomy), they were applied 15 243 times as a treatment modality over the analysed period. Among those cases, the additional treatment of RT or CRT was performed in 4250 patients. RT alone or with induction CT was applied over the same period for 16 308 patients, while concurrent or subsequent CRT was administered for treatment in 15 032 patients. There was observed a downward trend for surgical methods of LC treatment from 52.8% in 2009 to 24.3% in 2016 with the subsequent rise to 33.7% in 2018. The percentage of patients receiving RT was increasing from 23.8% in 2009 to 42.1% in 2013 and next it decreased to the level of 25.7% in 2018. The utilisation of CRT in LC treatment was progressively increasing over analysed years from 23.4% in 2009 reaching 40.6% in 2018 (table 3, figure 2).
Table 3.
The numbers of different treatment modalities for laryngeal cancer including surgery, radiotherapy (RT) and chemoradiotherapy (CRT) in 2009–2018 with the percentage share in following years
| Treatement/year | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | Total |
| Surgery | 1344 | 1278 | 1023 | 1109 | 998 | 1044 | 1073 | 1040 | 1005 | 1042 | 10 956 |
| Surgery_RT/CRT | 339 | 336 | 414 | 522 | 531 | 491 | 482 | 419 | 440 | 313 | 4287 |
| RT | 720 | 850 | 1181 | 1508 | 1929 | 2070 | 2095 | 2043 | 1568 | 960 | 14 924 |
| CT_RT | 39 | 60 | 92 | 110 | 180 | 191 | 223 | 261 | 152 | 76 | 1384 |
| CT_CRT | 76 | 118 | 174 | 219 | 240 | 301 | 392 | 477 | 352 | 304 | 2653 |
| CRT | 671 | 806 | 990 | 1102 | 1125 | 1401 | 1622 | 1766 | 1568 | 1328 | 12 379 |
| Surgery | 1683 | 1614 | 1437 | 1631 | 1529 | 1535 | 1555 | 1459 | 1445 | 1355 | 15 243 |
| RT | 759 | 910 | 1273 | 1618 | 2109 | 2261 | 2318 | 2304 | 1720 | 1036 | 16 308 |
| CRT | 747 | 924 | 1164 | 1321 | 1365 | 1702 | 2014 | 2243 | 1920 | 1632 | 15 032 |
| Surgery (%) | 52.78 | 46.81 | 37.09 | 35.69 | 30.56 | 27.92 | 26.41 | 24.29 | 28.42 | 33.68 | 32.72 |
| RT (%) | 23.80 | 26.39 | 32.86 | 35.40 | 42.15 | 41.12 | 39.37 | 38.36 | 33.82 | 25.75 | 35.01 |
| CRT (%) | 23.42 | 26.80 | 30.05 | 28.91 | 27.28 | 30.96 | 34.21 | 37.35 | 37.76 | 40.57 | 32.27 |
CRT, CT_CRT + CRT; RT, RT + CT_RT; SURGERY, SURGERY + SURGERY_RT/CRT.
Figure 2.
The proportional utilisation of surgery, radiotherapy (RT) and chemoradiotherapy (CRT) in treatment of laryngeal cancer in Poland in 2009–2018.
Discussion
The population-based analyses in the majority of developed countries show a decreasing incidence of LC, but paradoxically declining outcomes can be observed over the recent decade. This contradicts trends in survival for other cancer types. It was speculated that the overall decline in outcomes may reflect the consistent rise in larynx-preserving treatment methods with CRT, especially for T4 tumours or partial laryngectomies for T3.10 11 The extensive surgical treatment provided satisfactory survival results, however, it induced the deprivation of laryngeal phonation and permanent cervical stoma. The trend of organ-preserving treatment made the selection of treatment for the same tumour far more complex and the fact that it involved opposite strategies, has risen many controversies. The new directions are inevitable, however, their efficiency should be monitored.
The national cohort studies analysing the contemporary utilisation of treatment modalities of LC confronted to population-based studies are not so commonly performed. However, those expertise can update current trends in practice patterns and asses how the practice affects survival outcomes.
The presented study used the national cohort of patients who were diagnosed and treated between 2009 and 2018 in Poland to measure utilisation trends of LC treatment over that period. Initially, our data confirmed the decrease in the number of patients with LC observed worldwide. In the following years, a steady decrease was observed in the incidence rate from 7.77/1 00 000 in 2009 and 6.03/1 00 000 in 2018. The reports from Germany, the Netherlands, the USA and the Scandinavian countries present such downward trends, however the incidence rates in those countries are lower than in Poland.12–14 Another aspect to consider after our analysis is the gradual increase in the average age of patients with LC. We observed that the average age of the patients was almost 4 years higher in 2018 compared with 2009. This trend may result from changes in the structure of Polish society but also more effective methods of diagnosis and treatment in the last years. Similar results were presented in the study of Reizenstein et al 15 or Peller et al,16 although the increase of average age in German or Swedish patients was not as significant as in Polish ones. Considering the inhabitancy of LC patients almost 72% of them lived in cities, however the percentage decreased over 10 years. The results of the study by Włodarczyk et al 17 confirm the higher percentage of regular smokers in urban areas (30,3%) than in the countryside (25.4%).
Regarding the surgical treatment methods, a downward trend in TLs in the subsequent analysed years (from 1122 in 2009 down to 776 in 2018) could be observed and the declining trend was not only dependent on the decreasing incidence. Contrary to a TL, the number of procedures involving partial laryngeal resection remained stable. However an upward trend was observed for vocal cordectomy, performed as transoral laryngeal microsurgery. Hence the open partial laryngectomies rate has decreased. Summarising the overall number of surgical approaches in LC treatment, we observed a temporary downward trend from 52.8% in 2009 to 24.3% in 2016 and subsequent rise to 33.7% in 2018. Contrary to surgery, the percentage of patients receiving RT increased from 23.8% in 2009 to 42.1% in 2013 and then there was a decrease to the level of 25.7% in 2018. The utilisation of CRT in LC treatment was increasing progressively over the analysed period from 23.4% in 2009 to 40.6% in 2018. A quite comparable utility of treatment modalities in LC, additionally covering the earlier period is presented by Patel et al 18 in their analysis of the US National Cancer Database. Their study involved 8703 patients with stage III/IV LC treated between 2003 and 2011 and revealed the decline in TLs between 2003 and 2007 from 36.0% to 24.6%; in 2008, the utilisation of TLs increased to 27.8% and remained within the range of 26.6%–31.0%.18 The use of open partial laryngectomies decreased from a peak incidence of 17.1% in 2003 and remained stable in the range of 9.0%–10.4% up to 2011. The data presented show an evident rise in larynx-preserving CRT from 47% in 2003 to 61.5% in 2011.18 The review of García Lorenzo et al 19 presents another similar comparison of treatment options offered to patients with T3 and T4 LC over the last 30 years, however from single institution in Spain. They found out the surgery and RT were progressively substituted by CRT in chronological periods of 1985–1994, 1995–2004 and 2005–2014. The participation of surgery in treatment of LC patients declined from 62.5% to 52.2% and 50.5% respectively, while the percentages for RT were 33.5%, 39.7% and 16.8%, respectively. The contribution of CRT has risen from 0% to 8.1% and 32.7%, respectively. Moreover, the authors showed no significant differences in survival depending on treatment for T3 cancer patients, however, there was a significantly higher cancer-specific survival for T4 cancer patients treated surgically. The results of their report revealed the highest survival for patients from 1995 to 2004 period and the lowest survival for those treated in the period of 2005–2014.19 The results of a recent meta-analysis by Tang et al 20 that include controlled trials and compare long-term survival, support TL for patients with T4 LC and deny the advantage of primary organ preservation treatment for both T3 and T4 LC in increasing the overall survival rate. Therefore, a treatment modality for advanced stages of LC should be addressed especially for further prospective studies. The other reason responsible for declining outcomes of LC that needs to be considered is the increasing age of patients at the primary diagnosis. With the shift of the average age, the presence of other comorbidities is also inevitable and may not only influence the survival but make some patients susceptible to specific therapy options.
Regarding the treatment modality for T1 stage of LC in retrospective reports, there is a relative equivalence of RT and transoral endoscopic microsurgery and the rates of local control exceed 90%.7 However for T2 LC, the rates decrease significantly and range between 70% and 80%, regardless of treatment approach.21 Since the oncological benefits are comparable, both methods are verified in terms of voice and swallow outcomes, costs, side effects, time consumption and future options. The technological progress enabled the development of both methods in recent decades. The progress in visualisation techniques and widespread adoption of laser techniques in laryngeal microsurgery contribute to increased numbers of CO2 laser endoscopic laryngeal resections of cancer, especially vocal cordectomies. We did not found the data directly analysing the increase in the utility of transoral procedures performed with the laser compared with cold instruments and open partial laryngectomies in glottic cancer. However, Mendelsohn et al 22 identified a substantial annual growth rates and correct growth rates in original studies covering glottic cancer and LC in the time following the European Laryngological Society classification of cordectomies in 2000. Unfortunately, the ICD-9 classification does not include specification of the 30.22 procedure regarding involvement of laser vs cold instruments. However according to worldwide trends, we assume that the increase of vocal cordectomies in Poland is inevitably correlated with widespread CO2 laser endoscopic laryngeal microsurgery. The main advantages of laser-assisted LC treatment in comparison to RT are the short time of therapy, decreased costs, the possibility of revising endoscopic resection in case of persistence or recurrence and avoidance of the long-term side effects of RT.
In parallel to laser cordectomies, the new radiation techniques, including IMRT and stereotactic radiation therapy, are verified in studies dedicated to early stages of LC with analysis of sufficient doses (total dose and a single dose/fraction) and addition of sensitising CT.23
There are limitations to our analysis, resulting mainly from the fact that the National Foundation Database is unfortunately not combined with the National Cancer Registry. Therefore, the identification of LC stage with tumour, node, metastasis was not possible due to access to ICD-10 diagnosis solely. Information concerning locoregional control, metastatic disease, prior or concurrent cancer diagnosis, received radiation doses, data regarding CT administration with a number of cycles, specific agents, doses and long-term toxicities is also missing.
Conclusions
The presented data revealed an increase in the total number of organ-preserving treatment modality with CRT in the subsequent years and a decreasing number of TLs in Polish patients with LC. The progressing age of LC onset in Polish population may contribute to declining outcomes. The multicenter prospective randomised studies comparing treatment modalities should be planned to verify the oncological outcomes and to refer them to patients’ needs and cost-effectiveness.
Supplementary Material
Footnotes
Contributors: AR: methodology, writing, reviewing, editing and visualisation. MZ: methodology, data extraction, software and formal analysis, writing—draft, visualisation. KN: reviewing, editing.
Funding: This paper has been prepared within the project Maps of Health Needs—Database of Systemic and Implementation Analyses. The project is co-financed by the European Union from the European Social Fund under the Operational Programme Knowledge Education Development and it is being carried out by the Analyses and Strategies Department of the Polish Ministry of Health. Grant number: POWR 05.02.00-00.0149/15-01.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplemental information. Deidentified individual participant data that underlie the results are reported in the article (text, tables, figures and supplemental file)
Ethics statements
Patient consent for publication
Not required.
Ethics approval
All data used in the study were de-identified and therefore the approval of the Institutional Review Board was waived.
References
- 1. Globalcan . Global cancer Observatory. Available: http://globocan.iarc.fr/Default.aspx
- 2. Didkowska J, Wojciechowska U, Czaderny K. Nowotwory złośliwe W Polsce W 2017 roku, Polish National cancer registry, 2017. Available: http://onkologia.org.pl/wp-content/uploads/Nowotwory_2017.pdf
- 3. Didkowska J, Wojciechowska U, Zatoński W. Nowotwory złośliwe W Polsce W 2009 roku, Polish National cancer registry, 2009. Available: http://onkologia.org.pl/wp-content/uploads/Nowotwory_2009.pdf
- 4. Department of Veterans Affairs Laryngeal Cancer Study Group, Wolf GT, Fisher SG, et al. Induction chemotherapy plus radiation compared with surgery plus radiation in patients with advanced laryngeal cancer. N Engl J Med 1991;324:1685–90. 10.1056/NEJM199106133242402 [DOI] [PubMed] [Google Scholar]
- 5. Forastiere AA, Goepfert H, Maor M, et al. Concurrent chemotherapy and radiotherapy for organ preservation in advanced laryngeal cancer. N Engl J Med 2003;349:2091–8. 10.1056/NEJMoa031317 [DOI] [PubMed] [Google Scholar]
- 6. Wick CC, Rezaee RP, Wang T, et al. Use of concurrent chemoradiation in advanced staged (T4) laryngeal cancer. Am J Otolaryngol 2017;38:72–6. 10.1016/j.amjoto.2016.10.001 [DOI] [PubMed] [Google Scholar]
- 7. Baird BJ, Sung CK, Beadle BM, et al. Treatment of early-stage laryngeal cancer: a comparison of treatment options. Oral Oncol 2018;87:8–16. 10.1016/j.oraloncology.2018.09.012 [DOI] [PubMed] [Google Scholar]
- 8. Narodowy Fundusz Zdrowia . The National health fund data, 2018. Available: http://www.nfz.gov.pl [Accessed 20 Feb 2020].
- 9. Główny Urząd Statystyczny . Central statistical office of Poland data. Available: http://www.stat.gov.pl [Accessed 20 Feb 2020].
- 10. Olsen KD. Reexamining the treatment of advanced laryngeal cancer. Head Neck 2010;32:1–7. 10.1002/hed.21294 [DOI] [PubMed] [Google Scholar]
- 11. Cosetti M, Yu G-P, Schantz SP. Five-Year survival rates and time trends of laryngeal cancer in the US population. Arch Otolaryngol Head Neck Surg 2008;134:370–9. 10.1001/archotol.134.4.370 [DOI] [PubMed] [Google Scholar]
- 12. IKNL . Netherlands Cancer Registry [Internet]. Laryngeal cancer statistics, 2014. Available: http://www.dutchcancerfigures.nl/selecties/Dataset_3/img54d89aa75777a
- 13. Seer . Seer cancer statistics Factsheets: larynx cancer. National cancer Institute. Bethesda, MD. Available: http://seer.cancer.gov/statfacts/html/laryn.html
- 14. NORDCAN . Cancer incidence and mortality in the Nordic countries, 2014. Available: http://www-dep.iarc.fr/NORDCAN/english/frame.asp
- 15. Reizenstein JA, Bergström SN, Holmberg L, et al. Impact of age at diagnosis on prognosis and treatment in laryngeal cancer. Head Neck 2010;32:1062–8. 10.1002/hed.21292 [DOI] [PubMed] [Google Scholar]
- 16. Peller M, Katalinic A, Wollenberg B, et al. Epidemiology of laryngeal carcinoma in Germany, 1998-2011. Eur Arch Otorhinolaryngol 2016;273:1481–7. 10.1007/s00405-016-3922-8 [DOI] [PubMed] [Google Scholar]
- 17. Włodarczyk A, Raciborski F, Opoczyńska D, et al. Daily tobacco smoking patterns in rural and urban areas of Poland--the results of the GATS study. Ann Agric Environ Med 2013;20:588–94. [PubMed] [Google Scholar]
- 18. Patel SA, Qureshi MM, Dyer MA, et al. Comparing surgical and nonsurgical larynx-preserving treatments with total laryngectomy for locally advanced laryngeal cancer. Cancer 2019;125:3367–77. 10.1002/cncr.32292 [DOI] [PubMed] [Google Scholar]
- 19. García Lorenzo J, Montoro Martínez V, Rigo Quera A, et al. Modifications in the treatment of advanced laryngeal cancer throughout the last 30 years. Eur Arch Otorhinolaryngol 2017;274:3449–55. 10.1007/s00405-017-4639-z [DOI] [PubMed] [Google Scholar]
- 20. Tang Z-X, Gong J-L, Wang Y-H, et al. Efficacy comparison between primary total laryngectomy and nonsurgical organ-preservation strategies in treatment of advanced stage laryngeal cancer: a meta-analysis. Medicine 2018;97:e10625. 10.1097/MD.0000000000010625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Warner L, Lee K, Homer JJ. Transoral laser microsurgery versus radiotherapy for T2 glottic squamous cell carcinoma: a systematic review of local control outcomes. Clin Otolaryngol 2017;42:629–36. 10.1111/coa.12790 [DOI] [PubMed] [Google Scholar]
- 22. Mendelsohn AH, Remacle MJ. Vocal fold cancer transoral laser microsurgery following European Laryngological Society laser cordectomy classification. Front Oncol 2018;8:231. 10.3389/fonc.2018.00231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Stokes WA, Abbott D, Phan A, et al. Patterns of care for patients with early-stage glottic cancer undergoing definitive radiation therapy: a national cancer database analysis. Int J Radiat Oncol Biol Phys 2017;98:1014–21. 10.1016/j.ijrobp.2017.03.050 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-045308supp001.pdf (38.1KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplemental information. Deidentified individual participant data that underlie the results are reported in the article (text, tables, figures and supplemental file)