Abstract
Objective:
We sought to assess the frequency, content, and quality of shared decision making (SDM) in the emergency department (ED), from patients’ perspectives.
Methods:
Utilizing a cross-sectional, multisite approach, we administered an instrument, consisting of two validated SDM assessment tools—the CollaboRATE and the SDM-Q-9—and one newly developed tool to a sample of ED patients. Our primary outcome was the occurrence of SDM in the clinical encounter, as defined by participants giving “top-box” scores on the CollaboRATE measure, and the ability of patients to identify the topic of their SDM conversation. Secondary outcomes included the content of the SDM conversations, as judged by patients, and whether patients were able to complete each of the two validated scales included in the instrument.
Results:
After exclusions, 285 participants from two sites completed the composite instrument. Just under half identified as female (47%) or as white (47%). Roughly half gave top-box scores (i.e., indicating optimal SDM) on the CollaboRATE scale (49%). Less than half of the participants were able to indicate a decision they were involved in (44%), although those who did gave high scores for such conversations (73/100 via the SDM-Q-9 tool). The most frequently identified decisions discussed were admission versus discharge (19%), medication options (17%), and options for follow-up care (15%).
Conclusions:
Fewer than half of ED patients surveyed reported they were involved in SDM. The most common decision for which SDM was used was around ED disposition (admission vs. discharge). When SDM was employed, patients generally rated the discussion highly.
Many emergency department (ED) patients want to be part of medical decision making when multiple, reasonable options are available.1,2 Shared decision making (SDM)—the conversation between patients and clinicians where clinicians describe options and share their expertise and patients contribute their values and preferences—has been gaining increased recognition in emergency medicine.3 Emergency physicians (EPs) report using SDM in about half of the encounters where they believe it appropriate, but cite multiple barriers to widespread use.4 A framework exists to encourage physicians to recognize opportunities to use this patient-centered method of decision making, but little is known about the actual frequency, content, or quality of SDM in the ED from the patient perspective.3
Shared decision making has the potential to decrease resource utilization and improve patients’ knowledge, understanding of risk, trust in physician, and experience of care.5–7 Despite increased attention to SDM in the ED, few rigorously tested decision aids exist for use in the ED.6 It is likely that the majority of SDM in the ED takes place without the use of a formal decision aid,4,8 and measuring the frequency and quality of these interactions is challenging. To increase adoption of SDM, a better understanding of the current usage of SDM is needed.9 To facilitate the widespread implementation of SDM in the ED, we need a better understanding of how SDM is currently being used and whether existing scales are feasible for assessing SDM in the ED.10–12
We sought to use currently available, validated scales to measure the content, frequency, and quality of SDM in ED encounters from the patient perspective and to determine if patient-and visit-level factors were associated with the use of SDM. Additionally, we sought to assess the feasibility of two commonly used scales (the CollaboRATE scale and the SDM-Q-9) in the ED setting, to guide future SDM implementation efforts.11,12 Finally, we hypothesized that a newly developed question about “choice awareness” and involvement in decision making would be feasible and would correlate with other markers of patient experience.
METHODS
Study Design and Setting
We administered an instrument that included three different SDM-related scales (two validated and one newly developed) to a cross-section of alert, stable adult patients at two academic EDs. The composite instrument described here was the 17-item second section of a two-part (total 36-item) instrument regarding patient’s preferences in decision making.2 The entire instrument is available in the Data Supplement S1 (Appendix S1, available as supporting information in the online version of this paper, which is available at http://onlinelibrary.wiley.com/doi/10.1111/acem.13850/full). Patients only received this second section, evaluating the occurrence of SDM, if the ED portion of the care was complete (i.e., the decision regarding admission or discharge had been made, and the patient was aware of the plan). Instrument design and testing are described below. The study was approved by each hospital’s institutional review board.
The two hospitals are both urban, teaching, safety-net hospitals and level one trauma centers with 80,000 to 115,000 annual visits. One hospital is in New England and the other in California.
Selection of Participants
Participants were eligible for inclusion if they were English-speaking ED patients, age 18 and older, alert, oriented, and hemodynamically stable. Exclusion criteria were altered mental status; intoxication; presenting for hallucinations or suicidal or homicidal ideation; or other cognitive, hearing, or linguistic barriers to the administration of an English-language survey. To assess whether SDM happened during the visit, only subjects whose ED care was considered completed were included—that is, patients only received the instrument when they were aware of their disposition (admission vs. discharge). Patients awaiting discharge paperwork from their nurse, or awaiting inpatient bed placement, were approached. Once a patient had been admitted for over 4 hours, they were not eligible for the study both to avoid oversampling admitted patients and because patients may have difficulty distinguishing ED care from inpatient care provided in the ED. Verbal informed consent was used to maintain confidentiality, and trained research assistants (RAs) administered the survey either in verbal or in written form. Screening logs were maintained to record reasons for exclusions and refusals and to ensure that patients with multiple ED visits were only enrolled once; these data have been published previously.2 Overall sampling was based on RA availability (i.e., convenience sampling,) but RAs attempted to enroll a consecutive sample of patients available during their shifts across various days and time spans.
Methods and Measurements
To determine the best tool to measure the occurrence of SDM from the patients’ perspectives, the research team assessed several validated options.13 We determined that two published and publicly available scales were potentially appropriate for general use in the ED setting: the CollaboRATE scale (Data Supplement S1, Box 1) and the SDM-Q-9 (Data Supplement S1, Box 2).11,12
CollaboRATE (Data Supplement S1, Box 1)
The CollaboRATE scale was developed to guide SDM implementation efforts.12 It was meant to be not only valid but practical, having only three questions, and the original development showed concurrent validity with the SDM-Q-9. (The concurrent validity with the SDM-Q-9, as measured by Pearson product moment correlation was (r) = 0.80 [95% CI = 0.78 to 0.82], p < 0.001; relationship: strong, positive) for mean scores and as measured by point-biserial correlation was (rpb) = 0.50 [95% CI = 0.46 to 0.54, p < 0.001; relationship: strong, positive) for top-box scores.)12 CollaboRATE has been used as a general measure across several settings—primary care, surgery, anesthesia, and others.14–16
SDM-Q-9 (Data Supplement S1, Box 2)
The SDM-Q-9 was developed by taking the theoretical key steps of SDM and translating them into actionable items.11 Considerable refinements led to the final nine-item tool, which has since undergone psychometric testing in different populations, such as oncology, neurology, and behavioral health, with generally favorable properties (for example, in the oncology population, total sum scores derived from the general factor showed good reliability in terms of omega coefficient = 0.90).17–20
We used cognitive interviewing prior to survey deployment to assess the understandability and feasibility of using these scales in the ED. For cognitive interviewing, we approached stable ED patients and explored both scales with open-ended questions regarding their interpretation of the questions.21 We discovered that patients were willing to give favorable responses to questions like, “My doctor precisely explained the advantages and disadvantages of the options” (item from SDM-Q-9) even in scenarios when no decisions had been discussed with the patient. We decided that prior to presenting the SDM-Q-9 questions we would ask about choice awareness. Choice awareness is the understanding that more than one reasonable option exists and thus that a decision needed to be made. This concept does not currently have a validated patient-reported metric.22 The use of a choice awareness question prior to the use of the SDM-Q-9 forced respondents to report what decision conversation they were rating—as was also suggested by the original SDM-Q-9 scale development team.11 To assess choice awareness, we asked two additional questions. The first question was to categorize any decision-making conversations participants had with their clinician (e.g., admission vs. discharge, one medication vs. another), including a response option for “We did not discuss any decisions.” Second, we asked whether respondents were “as involved in today’s decisions as you would have liked to be” with three response options “Yes, I was as involved as I wanted to be,” “No, I would have liked to be more involved,” and “Not applicable, there were no decisions for me to be involved in today.” These questions were developed from the study team’s qualitative work and were subject to multiple rounds of cognitive interviewing and piloting (Data Supplement S1, Box 3).1,2
Additionally, two Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) ratings were included to assess the patients’ experience of overall care.23
The final instrument contained 17 items, 15 of which were drawn from validated scales. It was administered as a section of a 36-item instrument assessing preferences (Control Preferences Scale), experiences of care, and demographics (see Data Supplement S1, Appendix S1).2 Some patients responded to both sections at the same time, if their ED care was complete, while others responded to the longer first section (that included 10 demographics items) while waiting for tests and then completed the instrument described here only when a disposition decision had been made and communicated.
Outcomes
Our primary outcome was the degree to which SDM occurred, from the patients’ perspective, as measured by the CollaboRATE scale, the SDM-Q-9 scale, and the final choice awareness question derived from the qualitative work: “Were you as involved as you wanted to be?” We measured the association between choice awareness (i.e., being able to recognize that decisions were being made) on the primary outcomes and other measures of patient experience. Secondary outcomes included the proportion of patients willing and able to answer each scale (feasibility). We also reported findings from an exploratory analysis of whether any of the collected covariates were associated with the occurrence of SDM.
Data Analysis
Data were compiled using REDCap electronic data capture tools. Based on physician-reported estimates that SDM is appropriate about 50% of the time, and used in 50% of those instances,4 we sought to determine if patients reported the use of SDM approximately 25% of the time. A sample size of 300 would give a power of 0.80, with an alpha of 0.05, to detect reported SDM at 25%, with a 95% CI of ±2%. Our study was not powered to detect which covariates (such as demographics) were significantly associated with the occurrence of SDM; therefore, our regression analyses should be considered exploratory and hypothesis generating only and is not intended to be generalizable. Factors used for adjustment in the regression models were selected based on clinical relevance. Descriptive statistics were expressed as means and proportions. Differences in measures were presented with 95% CIs.
As per the authors’ suggestions in the original article, we dichotomized CollaboRATE responses using the “top-box” scoring approach, which means that respondents are categorized by whether or not they rated all three statements as “10 out of 10,” as this is considered to represent optimum SDM. We report SDM-Q-9 scores after rescaling from 0 to 100.11 Feasibility is reported as the proportion of patients able to fill out individual scales.
For our exploratory analysis, we used logistic regression to assess whether collected patient-and visit-characteristics were associated with a top-box score.24 We used linear regression to evaluate associations between these covariates and the CollaboRATE and SDM-Q-9 numerical scores, scaled to 0 to 100. We also modeled the response to our one developed question, “Were you as involved as you wanted to be?” We used logistic regression with the 0/1 outcome, 1 = yes and 0 combining “no” and “not applicable—there were no decisions for me to be involved with today.”
Regarding covariates examined, we included demographics, a summary score of 15 items on “barriers to SDM,” and the Control Preferences Scale, to assess whether any of these were associated with the occurrence of SDM from the patients’ perspectives.25 Additional details on the scaling of these covariates is available in Data Supplement S1, Appendix S2. No clinical covariates (i.e., variables regarding testing, results, or provider) were collected.
For our newly developed measure, “Were you as involved in today’s decisions as you would have liked to be?” we examined the association of the three response options with the other measures of SDM and patient experience measured by HCAHPS overall ratings. All analyses were performed with R version 3.5.
RESULTS
Participant Characteristics
Of the participants who completed the first section of the instrument (response rate = 83%),2 were asked to complete the second section of the instrument that included the measures described above, and 285 were included (eight excluded because of incomplete CollaboRATE scores; Figure 1). The mean age of participants was 49 years old with 47% (n = 135) female (Table 1). The mean (±SD) CollaboRATE score was 84 (±23)/100 and 49% of participants had a top-box score (i.e., the highest response option for all three questions). Table 2 shows patient experience scores. Ninety-nine patients completed the SDM-Q-9 items with a rescaled mean score of 73/100.
Figure 1.
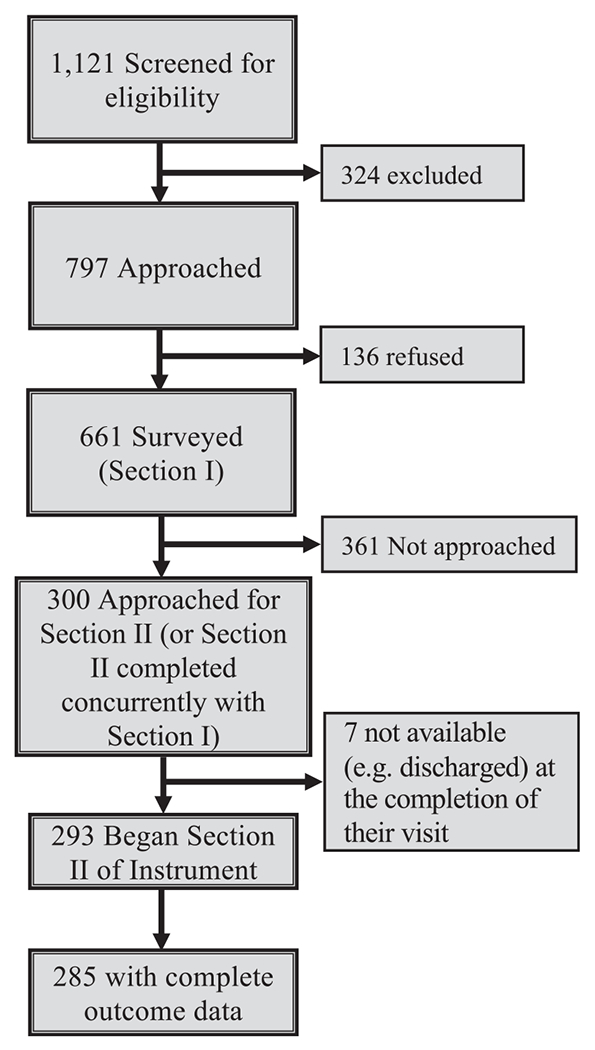
Patients screened, approached, and consented for Sections I and II of the instrument.
Table 1.
Patient and Visit Characteristics
| Characteristics | Number (%) |
|---|---|
| N | 285 |
| Site (%) | |
| New England ED | 143 (50.2) |
| California ED | 142 (49.8) |
| Age (years), mean (±SD) | 48.7 (±17.6) |
| Sex (%) | |
| Female | 135 (47.4) |
| Male | 148 (51.9) |
| Other | 0 (0.0) |
| Missing | 2 (0.7) |
| Race (%) | |
| Black | 54 (18.9) |
| White | 134 (47.0) |
| Other | 97 (34.0) |
| Ethnicity (%) | |
| Not Hispanic | 215 (75.4) |
| Hispanic | 70 (24.6) |
| Education (%) | |
| Not a high school graduate | 44 (15.4) |
| High school graduate or GED | 86 (30.2) |
| Some college or 2-year degree | 86 (30.2) |
| 4-year college degree or more | 67 (23.5) |
| Missing | 2 (0.7) |
| Primary insurance (%) | |
| Commercial | 89 (31.2) |
| Medicaid | 93 (32.6) |
| Medicare | 55 (19.3) |
| None | 15 (5.3) |
| Other | 31 (10.9) |
| Missing | 2 (0.7) |
| Primary language at home (%) | |
| English | 241 (84.6) |
| Not English | 43 (15.1) |
| Missing | 1 (0.4) |
| ED arrival time (%) | |
| 6 A.M. to 11:59 A.M. | 160 (56.1) |
| 12 noon to 5:59 P.M. | 69 (24.2) |
| 6 P.M. to 11:59 P.M. | 30 (10.5) |
| 12 midnight to 5:59 A.M. | 22 (7.7) |
| Missing | 4 (1.4) |
| Emergency Severity Index (%) | |
| 1 (most severe) | 12 (4.2) |
| 2 | 92 (32.3) |
| 3 | 108 (37.9) |
| 4 | 65 (22.8) |
| 5 (least severe) | 5 (1.8) |
| Unknown | 1 (0.4) |
| Missing | 2 (0.7) |
| Admitted to the hospital (%) | |
| No | 181 (63.5) |
| Yes | 104 (36.5) |
| Barriers to SDM score, range 15–75, mean (±SD) | 30.5 (±6.1) |
GED = general education development; SDM = shared decision making.
Table 2.
Primary Outcome and Patient Experience Measures
| Measure | Number (%) |
|---|---|
| N | 285 |
| Completed all three parts of CollaboRATE (%) | |
| Yes | 285 (97% of 293) |
| No (excluded from further analysis) | 8 (3% of 293) |
| CollaboRATE top-box score (%) | |
| Yes | 139 (48.8) |
| No | 146 (51.2) |
| CollaboRATE score, mean (±SD) | 84.5 (±22.8) |
| SDM-Q-9 completed (%) | |
| Yes | 99 (34.7) |
| No | 186 (65.3) |
| SDM-Q-9, mean (±SD) (n = 99) | 73.23 (±21.7) |
| Were you as involved in today’s decisions as you would have liked to be? (%) | |
| Yes, I was as involved as I wanted to be. | 133 (46.7) |
| No, I would have liked to be more involved. | 18 (6.3) |
| Not applicable, there were no decisions for me to be involved in today. | 131 (46.0) |
| Missing | 3 (1.1) |
| Would you recommend this ED to friends/family (%) | |
| Definitely no | 2 (0.7) |
| Probably no | 7 (2.5) |
| Probably yes | 52 (18.2) |
| Definitely yes | 223 (78.2) |
| Missing | 1 (0.4) |
| Overall rating of care received (%) | |
| 0 (worst) | 0 (0.0) |
| 1 | 0 (0.0) |
| 2 | 2 (0.7) |
| 3 | 2 (0.7) |
| 4 | 3 (1.1) |
| 5 | 7 (2.5) |
| 6 | 8 (2.8) |
| 7 | 23 (8.1) |
| 8 | 38 (13.3) |
| 9 | 46 (16.1) |
| 10 (best) | 155 (54.4) |
| Missing | 1 (0.4) |
| Overall rating of care received from 1 to 10, mean (±SD) | 8.92 (±1.6) |
SDM = shared decision making.
When asked explicitly about involvement in decision making, the most frequently discussed decision was regarding “admission versus discharge” (19%), followed by “treatment options like medications” (17%), “different options for follow-up care after you leave the ED” (15%), and “one test versus another test or no test” (13%). The majority of participants, 56% (n = 159) reported that they “did not discuss any decisions” (Table 3). When queried regarding “were you as involved as you wanted to be,” results reflected a similar trend: 47% (n = 133) reported “yes,” 6% (n = 18) reported “no,” and the remaining 46% (n = 131) reported “Not applicable, there were no decisions for me to be involved in today,” with 1% (n = 3) not responding.
Table 3.
Participants’ Responses to “Did You and Your Doctor Discuss Any of the Following Decisions Today?” a
| Response Options | |
|---|---|
| Being admitted to the hospital versus going home | 54 (19.1) |
| Medications (one medication vs. another or vs. no medication) | 47 (16.6) |
| Different options for follow-up care after you leave the ED | 43 (15.2) |
| One test versus another test or no test (like CT scan, blood tests, or ultrasound) | 38 (13.4) |
| Surgery or a procedure | 16 (5.7) |
| Going to an observation unit or physical rehabilitation versus going home or being admitted | 15 (5.3) |
| Antibiotics versus no antibiotics or another option | 13 (4.6) |
| Breathing tubes, ventilators, or life support (e.g., “What would you want done if you stopped breathing on your own?”) | 8 (2.8) |
| CPR and aggressive care versus comfort care | 6 (2.1) |
| No, I did not discuss any decisions with my ED doctors today. | 159 (56.2) |
Data are reported as total n (%). Percentages do not equal 100 as participants could select more than one response, unless “No, I did not discuss any decisions with my emergency department doctors today” was selected.
To assess the association between patient and visit characteristics and the frequency and quality of SDM, we modeled the outcome of SDM using the different instruments. Our four models examined top-box CollaboRATE scores, raw CollaboRATE scores, scaled SDM-Q-9 scores, and our newly developed question. We examined the same set of explanatory factors across all four outcomes. The final models are found in Data Supplement S1, Appendix S3. The following characteristics were associated with a lower likelihood of giving a top-box CollaboRATE score: higher agreement with barriers, being admitted, younger age, and identifying as white. When the score was modeled based on its raw numeric value using linear regression, no covariates were statistically significant. The model of the SDM-Q-9 scores showed an association only between being male and a higher SDM-Q-9 score. Finally, when we modeled “were you as involved in today’s decisions as you wanted to be” (using a 0/1 outcomes with “yes” vs. both “no” and “not applicable”), no covariate factors were significantly associated with a “yes” answer (i.e., “Yes, I was involved in today’s decisions as I wanted to be”).
Regarding feasibility, of the initial 293 participants, 285 (97%) answered all three of the CollaboRATE questions. However, after the addition of the question asking about choice awareness, only 99 (34%) completed the SDM-Q-9 questions. This is because, based on piloting and the original SDM-9 publication, we asked patients to explicitly identify the specific conversation/decision they were rating before they answered the SDM-Q-9 questions. If a patient was unable to identify a specific conversation/decision, they were not asked to complete the questions about SDM in the SDM-Q-9.
Regarding associations between whether participants could identify a decision being made (i.e., choice awareness) and measures of quality of SDM and patient experience, those who were unable to identify a decision they were involved in, had only a 6 points lower mean CollaboRATE score compared to those who were able to identify a decision (82 vs. 88, 95% CI of difference = 1 to 11). For participants who reported “Yes, I was as involved as I wanted to be” (n = 133), the mean CollaboRATE score was 32 points higher than for those (n = 18) who said “No, I would have liked to be more involved” (90 vs. 58, 95% CI of difference = 22 to 42). These two groups also showed significant differences in ratings of overall patient experience of care, using a 0 to 10 rating with 0 as the worst care possible and 10 as the best care possible. Those reporting adequate involvement rated their overall experience of care higher than those who reported wanting more involvement, with a median (IQR) of 10 (9–10) versus 7 (6–8; Table 4).
Table 4.
Differences in Validated Measures Based on Newly Developed Question, “Were You as Involved in Today’s Decisions as You Would Have Liked to Be?” (Statistical Comparison Is Between “Yes” and “No” Groups)
| “Yes, I Was as Involved as I Wanted to Be” | “No, I Would Have Liked to Be More Involved” | “Not Applicable—There Were No Decisions for Me to Be Involved in Today” |
|
|---|---|---|---|
| Total | 133 | 18 | 131 |
| CollaboRATE top-box score (%) | |||
| Yes | 69 (51.9) | 1 (5.6) | 69 (52.7) |
| No | 64 (48.1) | 17 (94.4) | 62 (47.3) |
| CollaboRATE score, mean (±SD) | 90.4 (±15.2) | 58.0 (±19.4) | 82.33 (±26.8) |
| Overall rating of ED, mean (±SD) | 9.1 (±1.5) | 7.1 (±1.8) | 9.02 (±1.6) |
| Willingness to recommend (%) | |||
| Definitely no | 0 (0.0) | 0 (0.0) | 2 (1.5) |
| Probably no | 1 (0.8) | 3 (16.7) | 3 (2.3) |
| Probably yes | 23 (17.3) | 8 (44.4) | 20 (15.3) |
| Definitely yes | 109 (82.0) | 6 (33.3) | 106 (80.9) |
| Missing | 0 (0.0) | 1 (5.6) | 0 (0.0) |
DISCUSSION
To our knowledge, this is the first study to assess the occurrence of SDM in the ED from the patient perspective. Our results suggest that the areas where SDM is being used most frequently include admission/discharge, treatments/medications, follow-up planning, and testing. Future efforts aimed at increasing SDM should focus on the development of decision aids and clinician training around discussing the disposition decision (i.e., admission vs. discharge) with patients, when clinically appropriate. For example, SDM is potentially appropriate for conditions such as intermediate-risk chest pain, pneumonia, pyelonephritis, cellulitis, and intermediate-risk syncope, among others. Supporting physicians in how best to engage in SDM for these clinical scenarios would have the highest potential for impact.
Although approximately half of patients were able to report a decision they discussed, it is notable that 46% of participants felt that “there were no decisions for me to be involved with today.” Being “as involved as I would like to be” was associated with better overall experiences of care, as measured by HCAHPS ratings; however, it was less clear how failing to recognize an opportunity for involvement influenced patients’ overall experience of care. This is consistent with our prior research that found that ED patients often do not expect SDM and are not aware of decisions being made with or without their involvement.1
Our results mirrored prior patient experience research—that involvement in decision making, as a component of communication, is clearly correlated with overall ratings of the patient experience of care.2 When we compared those who responded “yes” to “Were you as involved as you wanted to be?” to those who responded with a “no” (i.e., omitting those who did not see opportunities for involvement), we found very large differences across all measures: CollaboRATE top-box scores decreased from 52% to 6% and “definitely yes” on the “would recommend” question decreased from 82% to 33%. This provides evidence for the importance of helping patients feel involved in decision making: patients who feel involved in clinical decisions report a better overall experience of care.
Regarding the feasibility of the two previously validated measures, a number of important questions are clarified by our results. The CollaboRATE was, as advertised, “fast and frugal:” 97% of participants provided answers to all three questions. However, those who reported “there were no decisions for me to be involved in” had similar CollaboRATE scores to those who reported they were “as involved as they wanted to be” in a decision, raising the question of whether patients may offer high scores on the CollaboRATE scale without actually experiencing SDM, as defined for research purposes. This has been seen in other studies as well: Bakhit et al.27 found that the use of a decision aid increased OPTION scores (a SDM measure scored by a third-party observers) but that CollaboRATE scores were unchanged. Stubenrouch et al.14 sought to determine current levels of SDM within preoperative visits with anesthesiology and found that while third-party observers, again using the OPTION score, gave conversations low marks for the presence of SDM, patients gave these same conversations high scores on the CollaboRATE and SDM-Q-9 scales. It appears that patients often do not recognize that there are decisions that they could be involved in and, as a result, provide high scores for good communication, without actual involvement in decision making. Nonetheless, the concepts CollaboRATE attempts to assess are valid measures of patient-centered communication and may be more appropriate, from patients’ perspectives, than whether SDM, as defined by a researcher or clinician, has actually happened. Additionally, with an overall top-box score of 49%, this metric may be appropriate for measuring implementation of SDM interventions aimed at improving patient experience, as our study suggests that there is room for improvement, at least in the studied EDs.
A potential shortcoming of the SDM-Q-9 scale emerged during cognitive testing, as patients were often willing to give positive ratings to SDM when in fact no discussion of a decision had taken place. Patients would check “agree” to “The doctor made clear to me that a decision needed to be made;” however, when research staff would ask for more detail about that decision, patients would clarify that they were not thinking about anything specifically. The SDM-Q-9 is clearly only meant for use when the participant can reflect on a specific conversation about a decision, and we found that in the evaluation of ED clinical decision making, this did not happen most of the time. The SDM-Q-9 did have the distinct advantage of giving specific feedback regarding aspects of SDM. From our data, we could easily note which of the nine domains were rated best and worst. For example, while only 7% disagreed with, “My doctor made clear that a decision needs to be made,” 24% disagreed with, “My doctor told me that there are different options for my medical condition.”
Despite the respective advantages of these two scales, as noted, patients usually rate interactions higher than third-party observers do.14,27 Based on previous studies, we should assume that the actual number of decisions discussed was lower than these scores suggest. For example, in the analogous study by Stubenrouch et al. in anesthesiology, when all scores were rescaled to 0 to 100, mean scores were 92/100 for both CollaboRATE and SDM-9, but only 31/100 as judged by a third party (as measured by the OPTION score).14 Therefore, while CollaboRATE and SDM-Q-9 are intended to be patient-centered measures of SDM, they may be simply measuring the general interpersonal and communication skills of the clinician.
LIMITATIONS
Our study has several limitations. The current tools measuring SDM are new, inexact, and evolving, and SDM can be measured (inexactly) from multiple perspectives. No current measurement tools have been developed specifically for the context of ED care, although the tools we employed were created to be implemented in a variety of clinical scenarios. The tool that is most commonly used in SDM research, the OPTION scale, is time- and resource-intensive, as it requires audio or video recording of the patient-provider conversation and an adequately trained third-party observer(s) to rate the conversation. We instead chose two easy-to-score, patient-centered tools to incorporate the patients’ perspectives. However, most patients are not familiar with the concept of SDM and do not expect it.1,2 Therefore, patients may be judging provider-patient communication in general and not specifically SDM.1,2
Our study is also limited in generalizability for two main reasons. First, the instruments were only available in English. Second, we included only two locations, both of which were urban, academic, safety-net hospitals. It is unknown if we would find similar results with non-English speakers or at different types of EDs. Finally, as the instrument followed earlier questions about the desirability of involvement with decisions, we may have influenced responses by asking about preferences and barriers, and survey fatigue may have affected the responses to the final questions.
CONCLUSIONS
In conclusion, fewer than half of stable, cognitively intact, English-speaking adult ED patients recognized that decisions were being made that they could have been involved in. The most frequent decision discussed was admission versus discharge, but fewer than half of participants reported that they were involved to the degree they wanted. While in the context of busy ED care this could be considered reasonable, there is certainly room for improvement. The appropriate use of shared decision making could be increased by providing training and education for clinicians, by the development of more evidence-based decision aids for commonly encountered clinical scenarios, and by the development of patient experience measures related to shared decision making. Further research on the implementation of shared decision making in this setting is warranted since even a small degree of involvement in decision making appears to be quite meaningful to ED patients.
Supplementary Material
Acknowledgments
The project described was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, awards UL1TR001064 and UL1 RR025752. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. Dr. Probst was supported by a career development grant from the National Heart, Lung, and Blood Institute of the National Institutes of Health under award 1K23HL132052-02. Dr. Schoenfeld was supported by a career development grant from AHRQ, award 1K08HS025701-01A1.
The authors acknowledge the assistance of the research associates program at Baystate Medical Center as well as Athena Sofides, Shelby Mader, Kye Poronsky, Kyle Gress, and Daniela Garcia.
Footnotes
Presented at the American College of Emergency Physicians Scientific Assembly, Washington, DC, October 2017.
HK reports being an unpaid Clinical Advisory Board member for Collective Medical and has received reimbursement for travel and accommodation related expenses. He has also been a paid consultant for RAND Health and Castlight Health in the past 36 months.
Supporting Information
The following supporting information is available in the online version of this paper available at http://onlinelibrary.wiley.com/doi/10.1111/acem.13850/full Data Supplement S1. Supplemental material.
References
- 1.Schoenfeld EM, Goff SL, Downs G, et al. A qualitative analysis of patients’ perceptions of shared decision making in the emergency department: “let me know I have a choice.”. Acad Emerg Med 2018;25:716–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schoenfeld EM, Kanzaria HK, Quigley DD, et al. Patient preferences regarding shared decision making in the emergency department: findings from a multisite survey. Acad Emerg Med 2018;25:1118–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Probst MA, Kanzaria HK, Schoenfeld EM, et al. Shared decisionmaking in the emergency department: a guiding framework for clinicians. Ann Emerg Med 2017;70:688–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kanzaria HK, Brook RH, Probst MA, et al. Emergency physician perceptions of shared decision-making. Acad Emerg Med 2015;22:399–405. [DOI] [PubMed] [Google Scholar]
- 5.Wilson SR, Strub P, Buist AS, et al. Shared treatment decision making improves adherence and outcomes in poorly controlled asthma. Am J Respir Crit Care Med 2010;181:566–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hess EP, Hollander JE, Schaffer JT, et al. Shared decision making in patients with low risk chest pain: prospective randomized pragmatic trial. BMJ 2016;355:i6165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schoenfeld EM, Mader S, Houghton C, et al. The effect of shared decisionmaking on patients’ likelihood of filing a complaint or lawsuit: a simulation study. Ann Emerg Med 2019;74:126–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schoenfeld EM, Goff SL, Elia TR, et al. The physician-as-stakeholder: an exploratory qualitative analysis of physicians’ motivations for using shared decision making in the emergency department. Acad Emerg Med 2016; 23:1417–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sepucha KR, Breslin M, Graffeo C, et al. State of the science: tools and measurement for shared decision making. Acad Emerg Med 2016;23:1325–31. [DOI] [PubMed] [Google Scholar]
- 10.Elwyn G, Hutchings H, Edwards A, et al. The OPTION scale: measuring the extent that clinicians involve patients in decision-making tasks. Health Expect 2005;8:34–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kriston L, Scholl I, lzel LH, et al. The 9-item shared decision making questionnaire (SDM-Q-9). Development and psychometric properties in a primary care sample. Patient Educ Couns 2010;80:94–9. [DOI] [PubMed] [Google Scholar]
- 12.Barr PJ, Thompson R, Walsh T, et al. The psychometric properties of CollaboRATE: a fast and frugal patient-reported measure of the shared decision-making process. J Med Internet Res 2014;16:e2–e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bouniols N, Leclère B, Moret L. Evaluating the quality of shared decision making during the patient-carer encounter: a systematic review of tools. BMC Res Notes 2016;9:382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stubenrouch FE, Mus EM, Lut JW, et al. The current level of shared decision-making in anesthesiology: an exploratory study. BMC Anesthesiol 2017;17:95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Forcino RC, Barr PJ, O'Malley AJ, et al. Using CollaboRATE, a brief patient-reported measure of shared decision making: results from three clinical settings in the United States. Health Expect 2017;260:1743–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Manning AM, Duggins AL, Tiemeyer KA, et al. Characterizing decisional conflict for caregivers of children with obstructive sleep apnea without tonsillar hypertrophy. J Clin Sleep Med 2018;14:849–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Calderon C, Jiménez-Fonseca P, Ferrando PJ, et al. Psychometric properties of the shared decision-making questionnaire (SDM-Q-9) in oncology practice. Int J Clin Health Psychol 2018;18:143–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alvarez K, Wang Y, Alegria M, et al. Psychometrics of shared decision making and communication as patient centered measures for two language groups. Psychol Assess 2016;28:1074–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ballesteros J, Moral E, Brieva L, et al. Psychometric properties of the SDM-Q-9 questionnaire for shared decisionmaking in multiple sclerosis: item response theory modelling and confirmatory factor analysis. Health Qual Life Outcomes 2017;15:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Green SB, Yang Y. Evaluation of dimensionality in the assessment of internal consistency reliability: coefficient alpha and omega coefficients. Educ Measure Issues Pract 2015;34:14–20. [Google Scholar]
- 21.Willis GB, Artino AR Jr. What do our respondents think we’re asking? Using cognitive interviewing to improve medical education surveys. J Grad Med Educ 2013;5:353–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kunneman M, Branda ME, Hargraves I, Pieterse AH, Montori VM. Fostering choice awareness for shared decision making: a secondary analysis of video-recorded clinical encounters. Mayo Clin Proc Innov Qual Outcomes 2018;2:60–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hospital Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey. Health Services Advisory Group. 2017. “Facts” Available at: http://www.hcahpsonline.org/en/facts/. Accessed June 1, 2019.
- 24.Giordano LA, Elliott MN, Goldstein E, et al. Development, implementation, and public reporting of the HCAHPS survey. Med Care Res Rev 2010;67:27–37. [DOI] [PubMed] [Google Scholar]
- 25.Degner LF, Sloan JA, Venkatesh P. The Control Preferences Scale. Can J Nurs Res 1997;29:21–43. [PubMed] [Google Scholar]
- 26.Sonis JD, Aaronson EL, Lee RY, Philpotts LL, White BA. Emergency department patient experience. J Patient Exp 2017;5:101–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bakhit M, Del Mar C, Gibson E, Hoffmann T. Shared decision making and antibiotic benefit-harm conversations: an observational study of consultations between general practitioners and patients with acute respiratory infections. BMC Fam Pract 2018;19:165. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


