Abstract
Background:
Every day, we see more patients present to hospitals and clinics seeking gender-affirmation care to ameliorate the symptoms of gender dysphoria. However, to provide a multidisciplinary approach, it is important to offer an integrated clinical program that provides mental health assessment, endocrine therapy, physical therapy, research, and the full spectrum of surgical services devoted to transgender patients. This article describes our experience on building a specialized, multidisciplinary, academic state-of-the-art gender-affirmation program.
Methods:
Herein, we describe the main and critical components on how to build a multidisciplinary academic gender-affirmation program. We share our lessons learned from this experience and describe how to overcome some of the obstacles during the process.
Results:
Building a multidisciplinary academic gender-affirmation program requires an invested team, as each and every member is essential for feedback, referrals, and to improve patient’s experience. Institutional support is essential and by far the most important component to overcome some of the obstacles during the process. Having all team members working under the same institution provides all the critical components needed to improve outcomes and patient satisfaction. In addition, the collection of prospective data with a well-structured research team will provide information needed to improve clinical services and standardize clinical protocols, while leaving space for innovation.
Conclusions:
This article describes the steps and experience needed to build a multidisciplinary holistic academic gender-affirmation program. We provide our lessons learned during the process that will help guide those who intend to start an academic gender-affirmation program.
Introduction
Based on the American Psychiatry Association and the World Professional Association for Transgender Health (WPATH), gender dysphoria involves a conflict between a person’s physical/assigned gender and the gender with which he/she identifies.1,2 This can lead patients to experience significant distress, affecting their quality of life.3–5 Gender dysphoria occurs in 1:30,000 male-assigned births and in 1:100,000 female-assigned births. It is estimated that about 0.005%–0.014% individuals assigned male at birth and that 0.002%–0.003% individuals assigned female at birth would be diagnosed with gender dysphoria.6,7
Over the last decade, the number of gender-affirmation surgeries (GAS) has increased exponentially.8–13 Based on the American Society for Plastic Surgeons, GAS was among the most rapidly increasing surgeries between 2016 and 2017, with a 289% increase for transmen and a 41% increase for transwomen.9,14,15 GAS aim to align patient’s gender identity with their sex assigned at birth, helping achieve personal comfort with their self and, consequently, decrease psychological distress, and improve quality of life and body image satisfaction.1,8,11,16–24
Healthcare in this population might be challenging because it depends not only on good clinical care, but also on social and political matters. However, as healthcare providers, it is our responsibility and priority to provide high-quality services with evidence-based medicine. This evidence-based article will provide a complete guide for building an academic surgical gender-affirmation program, and we will review the lessons learned and adaptations made based on our experience over the years.
Management of Patients with Gender Dysphoria
To build a multidisciplinary comprehensive gender-affirmation program, the assessment and feedback from multiple team members and subspecialties such as mental health specialists, endocrinologists, nursing staff, physical therapists, social workers, urologists, gynecologists, and plastic surgeons are a must.25
Team members should meet on a regular basis to discuss about patients who are and will be candidates for surgery and to make sure that each patient meets the criteria required by the WPATH.26 Certain institutions have their own screening mechanism, which is important to standardize to avoid multiple hospital visits. However, it is important to keep in mind that these steps are necessary, especially if there are medical comorbidities that need to be addressed and controlled before surgical intervention. Surgery, particularly genital or bottom surgery, is often the last and most considered step for patients with gender dysphoria.26
The role of surgery has shown to be essential and medically necessary to alleviate patient’s gender dysphoria.18,22,27–34 In several occasions, there are numerous procedures offered during surgical consultation, which include (but are not limited to) the following: facial feminization, breast augmentation, orchiectomy, penectomy, and vaginoplasty in transwomen; and facial masculinization, chest-wall masculinization, hysterectomy and oophorectomy, metoidioplasty, and phalloplasty in transmen.5,10 In Table 1, GAS options are presented. Genital (bottom surgery), breast/chest (top surgery), and facial surgery for gender dysphoria are not just another set of elective procedures. The overall concept of elective procedures involve only a private mutual contract between a patient and a surgeon.26
Table 1.
Gender-affirmation Surgery
| Facial Surgeries | Chest Surgeries | Genitalia | |
|---|---|---|---|
| Feminization surgery | Facial feminization | Breast augmentation | Orchiectomy |
| Thyroid chondroplasty | Lipofilling | Penectomy | |
| Hairline reconstruction | Vaginoplasty ± neurovascular O-flap + clitorolabiaplasty | ||
| Voice modification surgery | |||
| Vulvoplasty + clitorolabiaplasty | |||
| Waist lipoplasty | |||
| Masculinization surgery | Facial masculinization | Subcutaneous mastectomy | Hysterectomy |
| Liposuction | Salpingo-oophorectomy | ||
| Lipofilling | Chest-wall contouring | Vaginectomy | |
| Voice modification surgery | Pectoral implants | Clitoral release | |
| Metoidioplasty ± urethral lengthening | |||
| Phalloplasty ± urethral lengthening | |||
| Scrotoplasty | |||
| Testicular prosthesis placement | |||
| Penile prosthesis placement |
In addition, collaborative research to advance the field of GAS is much in need. Creating clinical databases, collecting prospective data regarding surgical and patient-reported outcomes, and analyzing surgical recovery pathways and surgical innovation are essential.35 Based on evidence-based medicine and the authors’ experience, this article will focus on the different aspects of how to build a state-of-the-art transgender practice.
Components of a Comprehensive Academic Gender-affirmation Surgical Program of Excellence
A successful academic gender-affirmation surgical practice requires a multidisciplinary team approach to offer a comprehensive evaluation and surgical state-of-the-art care. Figure 1 depicts an organizational chart of a gender-affirmation multidisciplinary program. The team members involved are nursing staff, social workers, physical therapists, mental health specialists, endocrinologists, gynecologists, urologists, and plastic surgeons.1 Team members develop coordinated medical care, bringing their own expertise in a collaborative manner. In addition, research should be focused on clinical outcomes, patient experience, and innovation. A strong, comprehensive, and prospectively collected database should be built to keep record of the patients. Additionally, clinical trials should be encouraged and conducted to advance the field and provide state-of-the-art care. Each patient who comes into the practice should ideally have a 1-day visit if possible, in which all the team consults and clinical recommendations are provided to the patient, thus avoiding multiple trips to the hospital and decreasing patient dissatisfaction.28
Fig. 1.
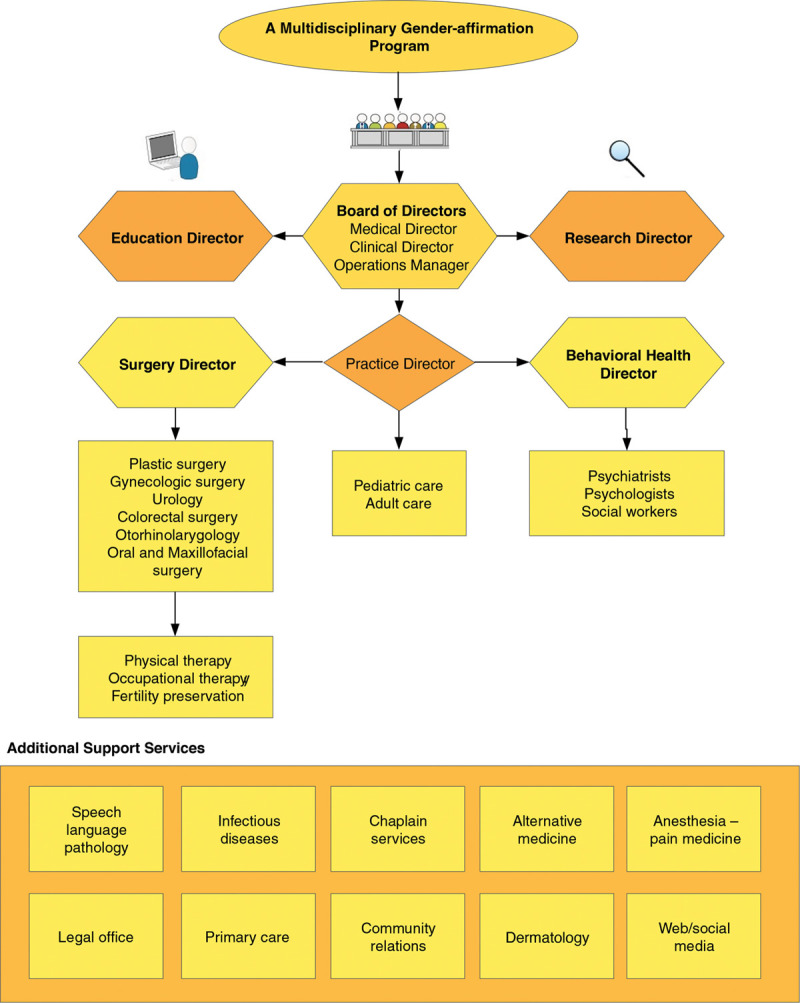
Organizational chart of a multidisciplinary gender-affirmation program.
The key components required to develop a multidisciplinary academic surgical gender-affirmation program are presented in Table 2.
Table 2.
Key Components of a Multidisciplinary Academic Surgical Gender-affirmation Program
| – Multidisciplinary team: nursing staff, social workers, physical therapists, mental health specialists, endocrinologists, gynecologists, urologists, and plastic surgeons. |
| – Team members must use their own expertise in a collaborative manner. |
| – Provide patients 1-day visit for all medical consults. |
| – Constant patient teaching and education by well-trained health care providers. |
| – Provide a comfortable environment and stimulate patients to feel confident in asking any question regarding the health care. |
| – The program should have a specific unit or clinical space. |
| – All patients should follow WPATH eligible criteria for transgender health care. |
| – Conjunction work with physical therapy. |
| – Provide fertility preservation options. |
| – The use of telemedicine increases patient’s follow-up adherence and improves patient-reported outcome data. |
| – Research program focused in on clinical outcomes, patient experience and innovation. |
| – Referrals have to be canalized through the same team of experts with experience in transgender care |
| – Open to feedback for constant improvement in the transgender program. |
Vision
Our vision is to build a multidisciplinary comprehensive academic gender-affirmation program with high-quality healthcare services and well-trained healthcare providers that positions patients’ objectives, desires, safety, and evidence-based medicine options first.
Infrastructure and Resources
Ideally, the program should have a specific unit or clinical space, in which all team members are able to provide clinical assessment in an expedited fashion.36 Figure 1 shows several services involved in gender-affirmation care. Each clinical subspecialty requires its own clinical space, clinical assessment tools, imaging sources for diagnosis and staging, and if surgical services are needed, intraoperative equipment must be available, among other specific requirements for each individual specialty.
Patients Eligible for GAS
Based on the WPATH1 selection criteria for surgery, most GAS require previous hormonal therapy and 1 or 2 referral letters provided by a mental health professional, which must include the following:
Patient’s general information,
Patient’s psychosocial assessment and diagnoses,
Duration of the physician–client relationship,
Surgical criteria explanation with a brief description of the clinical rationale that supports the patient’s request for the surgery,
Informed consent obtained from the patient, and
Statement of mental health professional that will be available for coordination of health care.
Each patient should be assessed to confirm if these requirements are met. From the surgical perspective, a dedicated area for preoperative and postoperative photography is ideal. This will help the patient understand the current anatomy and to follow-up over time any postoperative changes.36 The gender-affirmation postoperative unit should be equipped with medical staff who are familiar with current protocols. These protocols should be available to any staff in these units to answer questions related to patient care. In addition, these protocols should be updated and modified as needed.37
Endocrine Hormonal Therapy
Based on the WPATH guidelines,1 before GAS, the initiation of medical transition begins with hormone therapy.26,38,39 The goal of hormone therapy is to induce secondary sex characteristics but to suppress native biologic secondary sex characteristics.38,40–42 According to the clinical practice guidelines set forth by the American Endocrine Society in 2017, a multidisciplinary evaluation to confirm the diagnosis of gender dysphoria and address any medical or mental health issues is recommended before initiation of hormone therapy.40 In transgender adolescents, Gonadotropin Release Hormone (GnRH) analogs (leuprolide acetate and goserelin) may be started in early puberty to stop pubertal progression and delay the physical changes of the normal pubertal rise in testosterone until the patient is ready for feminizing hormone therapy.40
1Adequate hormonal management should be done by an experienced endocrinologist with expertise in gender-affirmation care. Information on hormonal therapy is key to disclose to the surgical team. There are some surgical groups that decide to stop hormonal therapy several weeks before surgery to decrease the risk of deep veonous thrombosis.43 However, one of the side effects of taking this approach is to reverse some of the hormonal effects of these medications that has been described as unpleasant by the patient.44 In our practice and after a careful discussion with the endocrinology team, we do not stop any hormonal therapy, but at the same time, surgical efficiency in the operating room, the use of compression boots intraoperatively, and postoperatively are a must to decrease the risk of deep venous thrombosis.44 In addition, our group has created an early ambulation protocol, engaging nursing staff to help the patient ambulate immediately after coming from surgery and during their hospital course. This vital information should be disclosed to the patient to make sure there is understanding of this approach, as patient engagement and cooperation is important during this process.
Fertility Preservation
Although hormonal therapies have been shown to increase self-esteem, alleviate depressive symptoms, and decrease symptoms of gender dysphoria, it can affect the individual’s reproductive potential.45–49 To pursue hormonal therapy, transgender individuals are required to live in their desired gender for at least 3 months or receive psychotherapy for 3 months.50 The team involved in the care of transgender patients during their gender-affirmation process should be aware of the fertility preservation options. The WPATH guidelines recommend a discussion of fertility preservation options before initiating gender-affirming therapies because the main purpose of this discussion is to find adequate window period before therapy and avoid possible complications.51
In the last decade, the incidence of transgender women seeking sperm cryopreservation has increased significantly.52 The age in which transgender patient presents to the physician has been trending down.52 Within our practice, fertility preservation options for transgender patients include sperm cryopreservation, surgical sperm extraction, and testicular tissue cryopreservation for transwomen, and oocyte cryopreservation, embryo cryopreservation, in vitro maturation, and ovarian tissue cryopreservation for transmen.46,49 These discussions are always started before the transition process and have to be well documented and further discussed with the team to provide all possible alternatives to patients seeking medical and surgical care.
Physical Therapy
Physical therapy has been shown to identify pelvic floor dysfunction in cis-female groups with high sensitivity and bring significant symptomatic improvement and quality of life.53–55 During the course of our practice, we had identified with high frequency these types of symptoms, the reason why we started evaluating pelvic floor dysfunction before surgery, and its progression using standardized questionnaires, and evaluated the role of physical therapy in the optimization of long-term outcomes.53 After years of looking into this problem, we concluded that pelvic floor dysfunction is commonly seen in patients with gender dysphoria even before surgery. Although the mechanism for this increased incidence is still unknown, preoperative assessment of pelvic floor dysfunction is vital to improve surgical outcomes.53 Physical therapy in patients with pelvic floor dysfunction can significantly improve symptoms both pre and post surgery; this is the reason behind why we always work in conjunction with a physical therapist at least three months before and after surgery. This protocol has changed significantly our clinical outcomes, as patients feel more comfortable with dilations, which extrapolates in the maintenance of the depth of the vaginal canal after surgery.
Patient Teaching and Education
To increase time efficiency before consultations and to improve education to medical personnel, having a formal education center is important.56 Here, the goals are to clarify patients’ questions before and after each healthcare visit.57 This unit should also provide material related to patient medical and surgical care, such as pamphlets, papers, videos, or books.57,58 At the end of each encounter, there should be a “checklist” that the patient must comply before surgery (supplies, dilators, pelvic therapy, etc.). When educating minors, parent involvement is mandatory.58
Based on our experience, there is inaccurate information on the Internet that can create false knowledge and unrealistic expectations.59 Clarification of any question helps not only the patients but also the health care provider because patients will be more familiar with the medical information, expectations, and surgical outcomes.
Patient Outcomes and Satisfaction
To have a state-of-the-art program, it is necessary to have defined metrics. This will allow the team to grow based on feedback from their own clinical outcomes. It is important to build and maintain prospective electronic databases; a designated research coordinator and/or personnel with focus and interest in these areas will help develop a database research program.35 In the last several years, websites and technological platforms with specific interest on patient outcomes and satisfaction have been driving further patient referrals, forum discussions, and group reputation.28
These prospective collected metrics will help assess any type of surgical outcomes, clinical volumes, patient referral sources and, more importantly, patient satisfaction. Using this information in a systematic fashion will allow the clinical team to grow; decrease medical costs; and allocate resources, infrastructure, and personnel. Constant reassessment of the practice will help the team to standardize protocols and improve efficiency while allowing surgical innovation.
One of the most challenging aspects when trying to obtain long-term data is patient compliance with postoperative follow-up visits. It is critical to develop a platform that allows for recurring patient-reported outcome with validated questionnaires that can be accessible through a mobile device or another electronic platform. Telemedicine, including virtual consultations, may play an important role in facilitating an adequate and long-term follow-up of these patients.60,61
Importance of Social Media
With the recent expansion in social media (including blogs and websites related to patient’s experience), we have experienced a growth of patients rating physicians on publicly accessible online websites and social media.28,62–67 The main purpose of Physician Rating Websites (PRWs) lies in using patient-reported information to rate surgeon’s quality online. However, these reviews not only encompass patient–physician interaction or surgical outcomes but also other domains such as office environment, waiting times, and staff friendliness. For these reasons, it is important that the gender-affirmation program understands why social media and PRWs are a powerful tool to understand patient impressions and overall satisfaction.28 In addition, these online platforms should provide information on the steps of the process for those who seek medical and surgical intervention and provide answers to some of the most commonly asked questions by patients. It is important to recognize that social media should be used not only to attract patients, but also to educate them on their options, realistic expectations, and complication management. Clarifying these points will help patients understand the process more clearly and set expectations before consultation.
Patient Referral
As new health insurance guidelines have adapted better policies for patients to access healthcare services related to transgender care, consultations for patients seeking surgical intervention have increased exponentially.15,68,69 Concomitantly, not many centers have the necessary infrastructure to offer these services, delaying the proper surgical care that the TGNB population need. Referrals have to be canalized through the same team of experts with experience in transgender care.70 Figure 2 illustrates the pathway when a patient is referred to the gender-affirmation clinic. This is important because it will provide feedback and close the loop starting from the first time the patient seeks medical care until the end of all the steps of the transition and follow-up visits. At the same time, creating mutual trust, positive feedback, and learning from the experiences of the patient and healthcare providers will improve the quality of care of the program. Creating online forums summarizing patients’ experience and steps required to complete the consultation process will strengthen the relationship of the healthcare provider/patients, improve referral sources, and provide feedback.70 On several occasions, even if the patient is seeking surgical care only, all specialties involved in the transition process are usually consulted, as a group consensus is key to provide adequate feedback to the patient and stimulate the referral pattern.
Fig. 2.
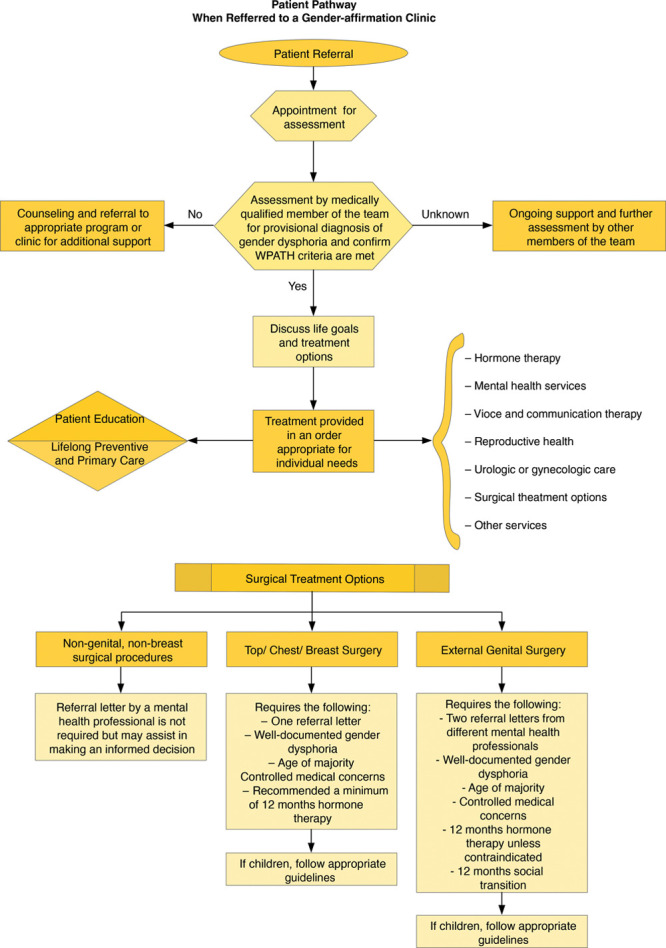
Patient pathway when referred to a gender-affirmation clinic.
Training
Hospitals with a comprehensive academic gender-affirmation program should continue to engage teaching trainees regarding an overall transgender health care approach, including psychological, medical, and surgical treatment.
Research Team
Research teams are an important component in the program, as they will provide and ensure constant improvement in healthcare services with evidence-based medicine toward their target population. Electronic databases collection of clinical outcomes would play an important role in clinical research. This will enrich not just your surgical gender-affirmation program, but also worldwide transgender health care.
Conclusions
Building a comprehensive, multidisciplinary academic program requires a clear vision and strategic planning from all members involved in the process. A triad of mental health and endocrinology, and the surgical team will provide the essential pillars to build a comprehensive, holistic, academic gender-affirmation program. In addition, WPATH guidelines are essential for screening and patient selection to offer the best medical care possible.
Footnotes
Published online 19 March 2021
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
References
- 1.Coleman E, Bockting W, Botzer M, et al. Standards of Care for the health of transsexual, transgender, and gender-nonconforming people, version 7. Int. J. Transgender Health. 2012; 13:165–232 [Google Scholar]
- 2.Turban J. What is gender dysphoria?. American Psychiatric Association website. 2020. Available at: https://www.psychiatry.org/patients-families/gender-dysphoria/what-is-gender-dysphoria. Accessed November 15, 2020
- 3.Schechter LS. Background. Surgical Management of the Transgender Patient. 2016, Philadelphia, Pa: Elsevier; 3–7. In Schecter LS (ed.) [Google Scholar]
- 4.Schechter LS. Gender confirmation surgery: an update for the primary care provider. Transgend Health. 2016; 1:32–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Safer JD, Tangpricha V. Care of transgender persons. N Engl J Med. 2019; 381:2451–2460 [DOI] [PubMed] [Google Scholar]
- 6.Marcovitch H. Gender identity disorders. Black’s Medical Dictionary. 2018; 290, 43rd ed. London: A&C Black. In Marcovitch H (Ed.) [Google Scholar]
- 7.American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders. 2013, Arlington, Va: American Psychiatric Publishing [Google Scholar]
- 8.Wernick JA, Busa S, Matouk K, et al. A systematic review of the psychological benefits of gender-affirming surgery. Urol Clin North Am. 2019; 46:475–486 [DOI] [PubMed] [Google Scholar]
- 9.Lane M, Ives GC, Sluiter EC, et al. Trends in gender-affirming surgery in insured patients in the United States. Plast Reconstr Surg Glob Open. 2018; 6:e1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nolan IT, Dy GW, Levitt N. Considerations in gender-affirming surgery: demographic trends. Urol Clin North Am. 2019; 46:459–465 [DOI] [PubMed] [Google Scholar]
- 11.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: Diagnostic and Statistical Manual of Mental Disorders. 2013, Fifth Edition. Arlington, Va: American Psychiatric Association [Google Scholar]
- 12.van de Grift TC, Kreukels BPC, Elfering L, et al. Body image in transmen: multidimensional measurement and the effects of mastectomy. J Sex Med. 2016; 13:1778–1786 [DOI] [PubMed] [Google Scholar]
- 13.van de Grift TC, Cohen-Kettenis PT, Steensma TD, et al. Body satisfaction and physical appearance in gender dysphoria. Arch Sex Behav. 2016; 45:575–585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.American Society of Plastic Surgeons Plastic surgery statistics report. 2017. Available at: https://www.plasticsurgery.org/documents/News/Statistics/2017/plastic-surgery-statistics-full-report-2017.pdf. Accessed May 12, 2020.
- 15.Nolan IT, Kuhner CJ, Dy GW. Demographic and temporal trends in transgender identities and gender confirming surgery. Transl Androl Urol. 2019; 8:184–190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Van De Grift TC, Elfering L, Greijdanus M, et al. Subcutaneous mastectomy improves satisfaction with body and psychosocial function in trans men: Findings of a cross-sectional study using the Body-Q chest module. Plast Reconstr Surg. 2018; 142:1125–1132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kühn S, Keval S, Sader R, et al. Mastectomy in female-to-male transgender patients: a single-center 24-year retrospective analysis. Arch Plast Surg. 2019; 46:433–440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Manrique OJ, Adabi K, Martinez-Jorge J, et al. Complications and patient-reported outcomes in male-to-female vaginoplasty-where we are today: a systematic review and meta-analysis. Ann Plast Surg. 2018; 80:684–691 [DOI] [PubMed] [Google Scholar]
- 19.van de Grift TC, Elaut E, Cerwenka SC, et al. Surgical satisfaction, quality of life, and their association after gender-affirming surgery: a follow-up study. J Sex Marital Ther. 2018; 44:138–148 [DOI] [PubMed] [Google Scholar]
- 20.Hadj-Moussa M, Ohl DA, Kuzon WM. Feminizing genital gender-confirmation surgery. Sex Med Rev. 2018; 6:457–468.e2 [DOI] [PubMed] [Google Scholar]
- 21.Barone M, Cogliandro A, Di Stefano N, et al. A systematic review of patient-reported outcome measures following transsexual surgery. Aesthetic Plast Surg. 2017; 41:700–713 [DOI] [PubMed] [Google Scholar]
- 22.Agarwal CA, Scheefer MF, Wright LN, et al. Quality of life improvement after chest wall masculinization in female-to-male transgender patients: a prospective study using the BREAST-Q and Body Uneasiness Test. J Plast Reconstr Aesthet Surg. 2018; 71:651–657 [DOI] [PubMed] [Google Scholar]
- 23.Nelson L, Whallett EJ, McGregor JC. Transgender patient satisfaction following reduction mammaplasty. J Plast Reconstr Aesthet Surg. 2009; 62:331–334 [DOI] [PubMed] [Google Scholar]
- 24.Papadopulos NA, Lellé JD, Zavlin D, et al. Quality of life and patient satisfaction following male-to-female sex reassignment surgery. J Sex Med. 2017; 14:721–730 [DOI] [PubMed] [Google Scholar]
- 25.Schechter LS, D’Arpa S, Cohen MN, et al. Gender confirmation surgery: guiding principles. J Sex Med. 2017; 14:852–856 [DOI] [PubMed] [Google Scholar]
- 26.Coleman E, Bockting W, Botzer M, et al. Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7. Int J Transgenderism. 2012; 13:165–232 [Google Scholar]
- 27.Oliver JD, Alsubaie SA, Vyas KS, et al. “Creation” rather than “reconstruction” in gender-affirming surgery. Plast Reconstr Surg. 2019; 144:341e–342e [DOI] [PubMed] [Google Scholar]
- 28.Bustos SS, Kapoor T, Schechter LS, et al. Impact of social media presence on online reviews among plastic surgeons who perform gender confirming surgeries. J Plast Reconstr Aesthet Surg. 2020; 73:783–808 [DOI] [PubMed] [Google Scholar]
- 29.Manrique OJ, Adabi K, Maldonado AA, et al. Cadaver study of combined neurovascular sensate flaps to create vaginal erogenous sensation during male-to-female genital confirmation surgery: the pedicle “O” flap. Ann Plast Surg. 2018; 81:571–575 [DOI] [PubMed] [Google Scholar]
- 30.Bustos SS, Forte AJ, Ciudad P, et al. The nipple split sharing vs. conventional nipple graft technique in chest wall masculinization surgery: can we improve patient satisfaction and aesthetic outcomes? Aesthetic Plast Surg. 2020; 44:1478–1486 [DOI] [PubMed] [Google Scholar]
- 31.Manrique OJ, Sabbagh MD, Ciudad P, et al. Gender-confirmation surgery using the pedicle transverse colon flap for vaginal reconstruction: a clinical outcome and sexual function evaluation study. Plast Reconstr Surg. 2018; 141:767–771 [DOI] [PubMed] [Google Scholar]
- 32.Black CK, Fan KL, Economides JM, et al. Analysis of chest masculinization surgery results in female-to-male transgender patients. Plast Reconstr Surg Glob Open. 2020; 8:e2356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bluebond-Langner R, Berli JU, Sabino J, et al. Top surgery in transgender men: how far can you push the envelope? Plast Reconstr Surg. 2017; 139:873e–882e [DOI] [PubMed] [Google Scholar]
- 34.Poudrier G, Nolan IT, Cook TE, et al. Assessing quality of life and patient-reported satisfaction with masculinizing top surgery: a mixed-methods descriptive survey study. Plast Reconstr Surg. 2019; 143:272–279 [DOI] [PubMed] [Google Scholar]
- 35.Streed CG, Lunn MR, Siegel J, et al. Meeting the patient care, education, and research missions. Acad Med. 2020 [DOI] [PubMed] [Google Scholar]
- 36.De Antonio IE, Gómez-Gil E. Coordination of healthcare for transsexual persons: a multidisciplinary approach. Curr Opin Endocrinol Diabetes Obes. 20:585–591 [DOI] [PubMed] [Google Scholar]
- 37.Esmonde N, Bluebond-Langner R, Berli JU. Phalloplasty flap-related complication. Clin Plast Surg. 2018; 45:415–424 [DOI] [PubMed] [Google Scholar]
- 38.Radix A, Sevelius J, Deutsch MB. Transgender women, hormonal therapy and HIV treatment: a comprehensive review of the literature and recommendations for best practices. J Int AIDS Soc. 2016; 193 Suppl 220810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sevelius JM. Gender affirmation: a framework for conceptualizing risk behavior among transgender women of color. Sex Roles. 2013; 68:675–689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hembree WC, Cohen-Kettenis PT, Gooren L, et al. Endocrine treatment of gender-dysphoric/gender-incongruent persons: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2017; 102:3869–3903 [DOI] [PubMed] [Google Scholar]
- 41.Kapoor T, Banuelos J, Nippoldt TB, et al. Effects of hormone therapy in patients who underwent male-to-female gender confirmation surgery. Eur J Plast Surg. 2019; 42:267–272 [Google Scholar]
- 42.White Hughto JM, Reisner SL. A systematic review of the effects of hormone therapy on psychological functioning and quality of life in transgender individuals. Transgend Health. 2016; 1:21–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Prince JCJ, Safer JD. Endocrine treatment of transgender individuals: current guidelines and strategies. Expert Rev Endocrinol Metab. 2020; 15:395–403 [DOI] [PubMed] [Google Scholar]
- 44.Haveles CS, Wang MM, Arjun A, et al. Effect of cross-sex hormone therapy on venous thromboembolism risk in male-to-female gender-affirming surgery. Ann Plast Surg. 2020; 86:109–114 [DOI] [PubMed] [Google Scholar]
- 45.Gorin-Lazard A, Baumstarck K, Boyer L, et al. Hormonal therapy is associated with better self-esteem, mood, and quality of life in transsexuals. J Nerv Ment Dis. 2013; 201:996–1000 [DOI] [PubMed] [Google Scholar]
- 46.De Roo C, Tilleman K, T’Sjoen G, et al. Fertility options in transgender people. Int Rev Psychiatry. 2016; 28:112–119 [DOI] [PubMed] [Google Scholar]
- 47.Jones CA, Reiter L, Greenblatt E. Fertility preservation in transgender patients. Int J Transgenderism. 2016; 17:76–82 [Google Scholar]
- 48.Barnard EP, Dhar CP, Rothenberg SS, et al. Fertility preservation outcomes in adolescent and young adult feminizing transgender patients. Pediatrics. 2019; 144:e20183943. [DOI] [PubMed] [Google Scholar]
- 49.Ainsworth AJ, Allyse M, Khan Z. Fertility preservation for transgender individuals: a review. Mayo Clin Proc. 2020; 95:784–792 [DOI] [PubMed] [Google Scholar]
- 50.Meyer W, Bockting WO, Cohen-Kettenis P, et al. The harry benjamin international gender dysphoria association’s standards of care for gender identity disorders, sixth version. J Psychol Human Sex. 2002; 13:1–30 [Google Scholar]
- 51.Caanen MR, Soleman RS, Kuijper EA, et al. Antimüllerian hormone levels decrease in female-to-male transsexuals using testosterone as cross-sex therapy. Fertil Steril. 2015; 103:1340–1345 [DOI] [PubMed] [Google Scholar]
- 52.Li K, Rodriguez D, Gabrielsen JS, et al. Sperm cryopreservation of transgender individuals: trends and findings in the past decade. Andrology. 2018; 6:860–864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Manrique OJ, Adabi K, Huang TC, et al. Assessment of pelvic floor anatomy for male-to-female vaginoplasty and the role of physical therapy on functional and patient-reported outcomes. Ann Plast Surg. 2019; 82:661–666 [DOI] [PubMed] [Google Scholar]
- 54.Adams SR, Dessie SG, Dodge LE, et al. Pelvic floor physical therapy as primary treatment of pelvic floor disorders with urinary urgency and frequency-predominant symptoms. Female Pelvic Med Reconstr Surg. 2015; 21:252–256 [DOI] [PubMed] [Google Scholar]
- 55.Pauls RN, Crisp CC, Novicki K, et al. Pelvic floor physical therapy: impact on quality of life 6 months after vaginal reconstructive surgery. Female Pelvic Med Reconstr Surg. 2014; 20:334–341 [DOI] [PubMed] [Google Scholar]
- 56.Stryker SD, Pallerla H, Pickle S. Considerations on medical training for gender-affirming care: motivations and perspectives. Int J Transgend Health. 2020; 21:79–88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hinrichs A, Link C, Seaquist L, et al. Transgender and gender nonconforming patient experiences at a family medicine clinic. Acad Med. 2018; 93:76–81 [DOI] [PubMed] [Google Scholar]
- 58.Poceta J, Cousins S, Wenzel C, et al. Effectiveness of a gender affirming surgery class for transgender and non-binary patients and their caregivers in an integrated healthcare setting. Int J Transgend. 2019; 20:81–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ayyala HS, Ward B, Mukherjee T, et al. Trends and techniques in gender affirmation surgery: is youtube an effective patient resource? Plast Reconstr Surg. 2020; 145:893e–894e [DOI] [PubMed] [Google Scholar]
- 60.Kauth MR, Shipherd JC, Lindsay JA, et al. Teleconsultation and training of VHA providers on transgender care: implementation of a multisite hub system. Telemed J E Health. 2015; 21:1012–1018 [DOI] [PubMed] [Google Scholar]
- 61.Shipherd JC, Kauth MR, Matza A. Nationwide interdisciplinary E-consultation on transgender care in the veterans health administration. Telemed J E Health. 2016; 22:1008–1012 [DOI] [PubMed] [Google Scholar]
- 62.Trehan SK, Daluiski A. Online patient ratings: why they matter and what they mean. J Hand Surg Am. 2016; 41:316–319 [DOI] [PubMed] [Google Scholar]
- 63.Gould DJ, Leland HA, Ho AL, et al. Emerging trends in social media and plastic surgery. Ann Transl Med. 2016; 4:455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Okike K, Peter-Bibb TK, Xie KC, et al. Association between physician online rating and quality of care. J Med Internet Res. 2016; 18:e324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Dorfman RG, Purnell C, Qiu C, et al. Happy and unhappy patients: a quantitative analysis of online plastic surgeon reviews for breast augmentation. Plast Reconstr Surg. 2018; 141:663e–673e [DOI] [PubMed] [Google Scholar]
- 66.Cohen JB, Myckatyn TM, Brandt K. The importance of patient satisfaction: a blessing, a curse, or simply irrelevant? Plast Reconstr Surg. 2017; 139:257–261 [DOI] [PubMed] [Google Scholar]
- 67.Hanauer DA, Zheng K, Singer DC, et al. Public awareness, perception, and use of online physician rating sites. JAMA. 2014; 311:734–735 [DOI] [PubMed] [Google Scholar]
- 68.Flores AR, Brown TNT, Herman JL. How many adults identify as transgender in the United States. The Williams Institute Website; 2016. Available at: https://williamsinstitute.law.ucla.edu/publications/trans-adults-united-states/. Accessed May 9, 2020 [Google Scholar]
- 69.Canner JK, Harfouch O, Kodadek LM, et al. Temporal trends in gender-affirming surgery among transgender patients in the United States. JAMA Surg. 2018; 153:609–616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Dietz E, Halem J. How should physicians refer when referral options are limited for transgender patients? AMA J Ethics. 2016; 18:1070–1078 [DOI] [PubMed] [Google Scholar]


