To the Editor,
In the COVID-19 pandemic, the provision of adequate health care to patients is fundamental to keep mortality low. Medical stuff, in particular emergency medical service personnel, who represent the first line of the fight against COVID-19 [1]. It is in the pre-hospital setting that each patient should be treated as a potentially infectious patient, and it particularly exposed medical stuff working on front line to the risk of SARS-CoV-2 infection [2]. In a systematic review, Bandyopadhyay et al. examine data of 152,888 HCWs infections show mortality at 0.9% level [3]. However, they also calculate mortality at level 37.2 death per 100 infections for HCWs over 70 years. Rivett et al. study 3% of tested in the HCW asymptomatic screening group were SARS-CoV-2 positive [4]. Accurate testing allows identification of people who might need treatment, or who need to isolate themselves to prevent the spread of infection. In connection with the above, screening of emergency medicine stuff with minimal or no symptoms is approach which will be critical for protecting patients and all medical staff.
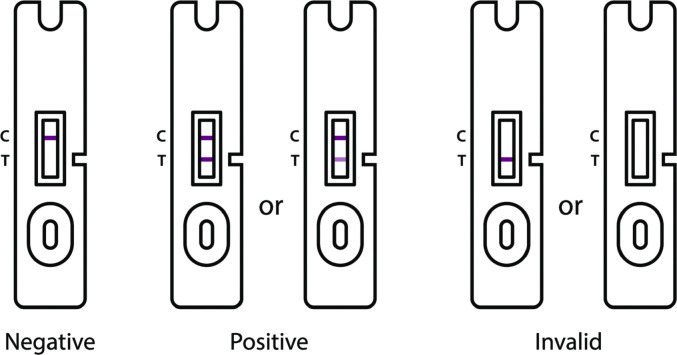
The increasing availability of antigen tests allows their use in hospital, pre-hospital and home settings. The specificity of immunological tests detecting AG antigens prove the current infection with SARS-CoV-2 virus [5]. Currently, antigen tests have been recognized as equivalent to genetic tests performed by RT-qPCR. Some tests require a nasal specimen that can be collected using an anterior nasal swab or a nasal mid-turbinate swab, other require a saliva specimen. The next step after collecting the biological material is mixing it with the buffer fluid. Then, after applying a few drops (depending on the test manufacturer) of the got sample to the test, the gold-antibody conjugate is hydrated and the COVID-19 antigen, if present in the sample, will interact with the gold-conjugated antibodies. The antigen-antibody-gold complex will migrate towards the test window as far as the Test Zone, where it will be captured by the immobilized antibodies, creating a visible pink line (Assay Band) showing a positive result. The advantage of rapid antigen tests, based on lateral flow immunochromatographic assays (LFIA), is short-term of detection, while their disadvantages are lower sensitivity than RT-qPCR and the possibility of obtaining a negative result in a person infected with SARS-CoV-2. The studies published at the beginning of the COVID-19 pandemic indicated that the sensitivity of first generation of rapid tests detecting SARS-CoV-2 antigens in the tested sample ranged from 34% to 80% [6]. Thanks to the possibility of obtaining the result in just a few or several minutes, the second generation of antigen test a quick and proper diagnostic tool, and nowadays its effectiveness is as high as sensitivity ≥90% and specificity ≥97%. An example of such a test is the COVID-19 antigen rapid test (SG Diagnostics, Singapore), the instructions for results interpretation was presented in Fig. 1 .
Fig. 1.
How to read the test results.
The antigen tests also gained recognition for assessing patients already in the pre-hospital stage. An example of the use of COVID-19 antigen tests at the prehospital care stage can be Emergency Medical Services in Warsaw (Poland), where every patient suspected of COVID-19 or having contact with the patient is subject to quick diagnosis using the test, thanks to which paramedics know whether it should be transported to a hospital dedicated to COVID-19 patients or a normal hospital [7]. Rapid antigen tests should be used to diagnose SARS-CoV-2 infections mostly in symptomatic patients during the first 5-7 days after symptom onset. Symptomatic individuals with a positive SARS-CoV-2 antigen test result should be treated as infected. The negative result of this test requires verification if the clinical picture or significant epidemiological premises suggest COVID-19 infection, because a negative result of the antigen test does not exclude infection with the virus.
In summary, screening of emergency medicine stuff and EMS patients with minimal or no symptoms is an approach which will be critical for protecting patients and all medical staff.
References
- 1.Dzieciatkowski T., Szarpak L., Filipiak K.J., Jaguszewski M., Ladny J.R., Smereka J. COVID-19 challenge for modern medicine. Cardiol J. 2020;27(2):175–183. doi: 10.5603/CJ.a2020.0055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Klosiewicz T., Ziemak P., Zalewski R., Tobola N., Antoszczuk M., Puslecki M. Paramedics’ safety during transportation of the patient under ongoing nebulization in the context of COVID-19 outbreak. Disaster Emerg Med J. 2020;5(4):218–220. doi: 10.5603/DEMJ.a2020.0036. [DOI] [Google Scholar]
- 3.Bandyopadhyay S., Baticulon R.E., Kadhum M., et al. Infection and mortality of healthcare workers worldwide from COVID-19: a systematic review. BMJ Glob Health. 2020;5(12) doi: 10.1136/bmjgh-2020-003097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rivett L., Sridhar S., Sparkes D., et al. Screening of healthcare workers for SARS-CoV-2 highlights the role of asymptomatic carriage in COVID-19 transmission. Elife. 2020 May 11;9 doi: 10.7554/eLife.58728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Greenky D., Wiltrakis S. COVID-19 testing for providers: Leading by example. Am J Emerg Med. 2021 Jan 11;S0735–6757(21):00013–00019. doi: 10.1016/j.ajem.2021.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brochot E., Demey B., Handala L., et al. Comparison of different serological assays for SARS-CoV-2 in real life. J Clin Virol. 2020;130:104569. doi: 10.1016/j.jcv.2020.104569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Greenky D., Wiltrakis S. COVID-19 testing for providers: Leading by example. Am J Emerg Med. 2021 Jan 11;S0735–6757(21):00013–00019. doi: 10.1016/j.ajem.2021.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]