Abstract
Background
Our objective is to examine whether residential racial segregation may be constraining capacities for social distancing thus leaving African Americans potentially more exposed to contracting COVID-19. We hypothesized that residential racial segregation constrains African Americans’ spatial mobility when the whole population is locked down but increases their need for moving under reopening orders.
Methods
We employ a Black/White dissimilarity index as our independent variable and county-level mobility ratios as our dependent variable. Using generalized estimating equations for longitudinal data, we analyzed the effects of Black/White segregation on population mobility by counties across the United States from March 8 to August 7, 2020 under two different COVID-19 related policy conditions: lockdown and reopening.
Findings
While higher county-wide levels of segregation were significantly associated with decreased mobility under lockdown and stay-at-home orders, we found that this relationship between segregation and mobility dissipated under reopening orders.
Interpretations
Investigating the effects of health policy without considering differing effects due to structural racism will likely ignore complexities that may create unintended consequences of health policy. Our conclusions suggest African Americans may face structural limitations to effective social distancing as evidenced by higher rates of mobility after reopening policies go into effect.
PANEL: Research in context.
Evidence before this study
Research on responses to COVID-19 from China and recent studies from the United States demonstrate that lower mobility reduces COVID-19 incidence rates. However, little published research has examined what factors influence mobility. Racial segregation has prohibited the movement of Black populations into certain residential areas and operates as a persistent cause of health inequities and illness but we know very little about the effect of racial segregation on mobility under lockdown and reopen policies during a pandemic.
Added value of this study
Our research capitalizes on daily US county-level data to examine the impact of structural racism in the form of racial segregation across counties and its interaction with state policy shifts during the COVID-19 pandemic yielding important findings that underpins those relationships. Along with other studies that have demonstrated the disparate effects of racism on COVID-19 cases and mortality, this study suggests that racist structures such as residential segregation may play a role in the capacity of Black Americans in segregated areas to successfully carry out the distancing required to prevent COVID 19 spread.
Implications of all the available evidence
Our findings underscore the need to consider the legacies and the complex influence of structural racism on social distancing for COVID-19 in the United States. Moreover, persistent racial inequalities in housing and residential segregation suggest that one-size-fits-all interventions such as lockdowns and their relaxation may exhibit varying effects based upon the intensities of structural racism.
Alt-text: Unlabelled box
1. Introduction
The current COVID-19 pandemic has infected over 23 million people and claimed over 400,000 lives in the United States as of January 22, 2021 [1]. As the pandemic continues to evolve, significant racial disparities in confirmed cases and deaths have become apparent. Black Americans die from COVID-19 at 2.5 times the rates of the White population [2,3]. Since June 2020, the CDC has found that within counties with elevated COVID-19 prevalence or ‘hotspots’, racial disparities in COVID-19 persist with Hispanic and Black populations being disproportionately represented in case counts across most hotspots measured [4]. There has been an increasing awareness in the research community and the public at large that social factors, particularly racism, may drive racial disparities in pandemic outcomes and exacerbate the pandemic itself in the United States.
Residential segregation of racial groups has been a central component of racism in the United States. The legal segregation between black and white dates back to the late 19th century in the rural South and has sustained during the Great Migration. It is achieved through different mechanisms, ranging from targeted violence to overt discrimination and institutionalized practices of federal policies in real estate and banking [5] Though laws enforcing this separation have largely been repealed by 1977, levels of residential racial segregation remain high as do the negative effects of the persistent separate and unequal distribution of services and resources [6]. Segregation has been shown to have a disproportionately negative impact on the health of Black Americans, affecting life expectancy and the prevalence of certain infectious and chronic diseases [[7], [8], [9]]. While residential racial segregation has been documented as a fundamental cause of health disparities along racial lines [9,10,12], segregation also affects access and utilization of health services [11]. Much research shows evidence to support the lingering effects of residential racial segregation on limited access to employment and essential services within segregated areas that require significant travel from home to work and childcare facilities [12,13].
The social determinants of health framework in the public health literature [14] and the mechanisms by which racial stratification affects life chances in the social science literature [15,16] demonstrate that racism and its health consequences are a fundamental cause of illness [9]. Yet the mechanisms by which racial/ethnic stratification exacerbates the effects of the COVID-19 pandemic require further investigation. While there may be complex ways by which racism affects pandemic outcomes, this paper seeks to identify one such mechanism by which racism, a key social determinant of health, influences social distancing, a necessary practice curbing virus spread. Specifically, we ask whether and how the relationship between residential racial segregation and social distancing operates along the course of the US COVID-19 pandemic from periods of lockdown to reopening under state-specific policy responses.
The purpose of this study is to examine the relation between residential racial segregation and social distancing during the current COVID-19 epidemic at county level across the United States. Social distancing practices are closely related to the timing of state policy responses to COVID-19 – mandated during the lockdown period and relaxed during the reopening period [17,18]. Longer mobility distances increase the risk of coming in contact with other people [18] and breaching the guideline of social distance from the Centers for Disease Control and Prevention (CDC), elevating the risk of exposure to the virus. While in general racism induces spatial segregation and constrains the mobility among blacks, this relationship may disappear under reopening orders during the ongoing COVID-19 epidemic. In counties with high residential racial segregation, state reopening policy disproportionately places Black populations at the forefront of the reopening economy and undermines capacity for social distancing. At the county aggregate level, we hypothesize that the association between Black/White residential segregation and human geographic mobility is negative during lockdown and this association dissipates during reopening. Our analysis intervenes on existing research on the relationships between residential racial segregation and COVID-19 by examining how residential segregation affects capacity to social distance. In conducting this analysis we expose segregation as an important mechanism in affecting health seeking behaviors during a pandemic.
2. Methods
We draw county-day data from the COVID-19 Data Hub of the Hopkins Population Center (https://github.com/QFL2020/COVID_DataHub). Lingxin Hao and Xiao Yu were responsible for collecting these data. The Data Hub collects timely and effective data on 3142 counties from January 22, 2020 to present and ongoing for social science research on COVID-19. Drawing from trusted sources (Hopkins CSSE COVID-19 tracking system, Census Bureau, CDC, Bureau of Labor Statistics (BLS), Bureau of Economic Analysis, Internal Revenue Service, etc.), the data and documentation are updated weekly and publicly accessible.
Lingxin Hao, Xiao Yu, Roland Thorpe Jr. and Alexandre White designed the sampling method. Hao and Yu developed the models for this research. Residential racial segregation is commonly measured with Black/White dissimilarity index (herein Black-White Dissimilarity index, between 0 and 1) with a higher value indicating a higher level of segregation [15]. Social distancing can be measured with the inverse of human geographic mobility [17]. Our analytic sample includes all counties with valid data on mobility and Black-White Dissimilarity index. Of the 3142 counties, 541 (17%) were dropped due to no mobility data, yielding 2601 counties. Moreover, 9 county-day observations are also excluded, due to their extremely large values of mobility ratio, which are likely data errors. A further 629 counties were dropped as their populations comprised fewer than 100 Black people to create reliable Black-White Dissimilarity index. Our final analytic sample comprises 1972 counties with 283,097 county-day observations.
In addition, a separate analysis was conducted on ‘hotspot’ counties. Our criteria for hotspots are based on the metrics of trends of new daily cases rates [19]. Rather than daily case rates, we identify hotspots with county-level cumulative confirmed cases per 100,000 residents in two periods: January 22 – April 12, 2020 and April 13 – July 24, 2020. The cutoff points for the two periods are based on the highest 7-day average new cases from the CDC [20]. This choice is based on the emerging pattern from the empirical data and the contexts where the policy measures unfolded. This time period also reflects the period during which protocols first began and were relaxed. This allowed us to examine the effects of these policies without also considering how later additional policies may have intervened on existing regulations or how pandemic fatigue might affect behaviors. We ranked counties on these two cumulative measures and picked the top 200 counties in either period as the pool of hotspots. The unique number of hotspots with valid mobility ratio and Black-White Dissimilarity index data is 135, of which 50 counties in the first period, 58 in the second period, and 27 in both periods. The number of county-day observations of hotspots is 19,256.
The dependent variable is mobility ratio (MR), the median daily travel distance normalized by a baseline in order to capture the change of mobility levels over the pandemic course. We modified the method in Badr et al. [17] based on the work of Warren and Skillman [21]. Badr et al. demonstrated in their research that human mobility is strongly correlated to COVID-19 case rates with high rates of mobility correlating to increased incidence of COVD-19 and concluded that mobility is an effective proxy metric for social distancing [17]. The original data were collected from mobile device locations by Descartes Labs. A statistic, M50, represents the distance a typical resident of a given county moves in a day. MR is the ratio of daily M50 from March 8 to August 7 relative to the baseline, the average of daily M50 between March 1 and March 7. A higher mobility ratio may pose a challenge for practicing social distancing as evidenced by recent research on mobility constraints and COVID-19 [17,22].1
Our key explanatory variable is Black-White Dissimilarity index, which is a measure of the evenness within counties Black and White residents are distributed across Census tracts [15,23]. The original data source is the Robert Wood Johnson Foundation County Health Rankings based on American Community Survey data from 2014 to 2018 [23]. The index is only available for counties with a population having at least 100 Black people. The spatial distribution between Black and White within each county serves as the condition for group interaction and contact.
Policy responses to COVID-19 are the policy environment in which we examine the influence of residential racial segregation on mobility. We used two state policy timing variables. Five counties do not have the statewide stay-at-home order, including Arkansas, Iowa, Nebraska, North Dakota, South Dakota. We translated the policy timing variables into two time-varying dummy variables. “Stay-at-home” takes the value of 1 for days under the stay-at-home order and 0 otherwise, which indicates all specific days under lockdown; “Reopen” is 1 for days under the reopen order and 0 otherwise, which indicates all specific days under reopen. Counties with no stay-at-home order have a value of 0 for “Stay-at-home”, i.e., no days under stay-at-home, and a value of 1 for “Reopen”, i.e., all days under “Open”.
Our analysis includes three sets of control variables: geographic, demographic, and socioeconomic status (SES). The geographic covariates include metropolitan areas and three dummy variables indicating the Midwest, South and West regions with Northeast as the reference. The demographic covariates focus on racial compositions (Black, Hispanic and Asian) and population density (in thousands per square kilometers), the original source of which is the Census Bureau. The SES covariates include a 1-month lagged time-varying monthly unemployment rates from the BLS [24] and socioeconomic vulnerability index from the CDC [25]. Specifically, the index is a composite measure for individuals below poverty, unemployed, with lower income and no high school diploma.
3. Role of funding sources
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
4. Analytic approach
Given the panel data structure of county-level data and our goal of modeling is to obtain parameter estimates for the population, we employ the generalized estimating equations (GEE) model for longitudinal data, which estimates the parameters of a generalized linear model with an unknown exchangeable correlation on mobility ratio among counties over 153 days. The model error structure allows for consistent population-average estimates of the parameters of interest, the differential effects of Black-White Dissimilarity index on MR. We estimate the model separately for the analytic sample and the hotspot sample. All the analyses are analyzed using STATA 15 and visualized using the “ggplot2” package in R.
5. Results
Table 1 shows the descriptive statistics of all variables included in our analysis for the total population of 3142 counties, the analytic sample of 1972 counties, and the hotspot sample of 135 counties. The mobility ratio (MR) and Black-White Dissimilarity index are not fully available for all counties. The MR is slightly higher for the analytic sample (0.67) than the hotspot sample (0.61), and the baseline mobility is similar between the two samples, which is about 10 km for a typical resident to travel in a day. The mean Black-White Dissimilarity index is 0.46 for both samples, meaning that 46% of Black people (and Whites) must change their residence across census tracts in order to reach even distribution within the county. For the entire 3142 counties (column “All Counties”), 28% of the 153 days are under the stay-at-home order, this percentage is smaller (26%) for the Analytic Sample and slightly longer for the Hotspot Sample (30%). We examine the distributions of control variables to spot large differences across samples for potential sample selection problems. We note that the analytic and hotspot samples are more in metropolitan areas, in the Northeast region, with higher proportions for people of color, especially Black populations, and with higher population densities, especially in hotspots. These identified differences are relatively smaller between the analytic sample and the full sample, suggesting a relatively less concern over potential sample selection of the analytic sample. We do not generalize the results from the hotspot sample to the general population.
Table 1.
Descriptive statistics of variables in the analysis of mobility ratio over the COVID-19 Course (March 8th to August 7th): US county level analysis.
| All counties | Analytic sample | Hotspot sample | |
|---|---|---|---|
| Dependent variable | |||
| Mobility ratio | 0.67 | 0.61 | |
| Baseline mobility | 10.55 | 10.02 | |
| Black-White Dissimilarity index | 0.46 | 0.46 | |
| State policy | |||
| Stay-at-homea | 0.28 | 0.26 | 0.30 |
| Reopenb | 0.60 | 0.61 | 0.58 |
| Geographic | |||
| Metropolitan | 0.37 | 0.49 | 0.55 |
| Northeast | 0.07 | 0.09 | 0.28 |
| Midwest | 0.34 | 0.24 | 0.16 |
| South | 0.45 | 0.57 | 0.45 |
| West | 0.14 | 0.11 | 0.10 |
| Demographic | |||
| Prop. Blackc | 0.09 | 0.12 | 0.20 |
| Prop. Hispanicd | 0.10 | 0.10 | 0.16 |
| Prop. Asiane | 0.01 | 0.02 | 0.03 |
| Pop. Density (in 1000)f | 0.11 | 0.13 | 0.53 |
| SES | |||
| Vulnerability indexg | 0.55 | 0.57 | 0.59 |
| Unemployment (1-month lagged)h | 8.28 | 8.69 | 9.53 |
| No. counties | 3142 | 1972 | 135 |
| No. county-days | 480,573 | 283,097 | 19,256 |
Notes:
the proportion of days under stay-at-home order.
the proportion of days under reopening policy.
Proportion of the county population that identifies as Black in census records.
Proportion of the county population that identifies as Hispanic in census records.
Proportion of the county population that identifies as Asian in census records.
Population in thousands per square kilometers in 2018.
this is a composite measure for individuals below poverty, unemployed, with lower income, and with no high school diploma.
one-month lagged, time-varying monthly unemployment rates at the county level
Black-White Dissimilarity index is a measure of the evenness within counties Black and White residents are distributed across Census tracts. The index is only available for counties with a population having at least 100 Black people.
Mobility ratio is the median daily travel distance normalized by a baseline in order to capture the change of mobility levels over the pandemic course. It is calculated as the ratio of daily M50 from March 8 to August 7 relative to the baseline, the average of daily M50 between March 1 and March 7, obtained from mobile device locations by Descartes Labs.
Data: Hopkins Population Center COVID-19 Data Hub.
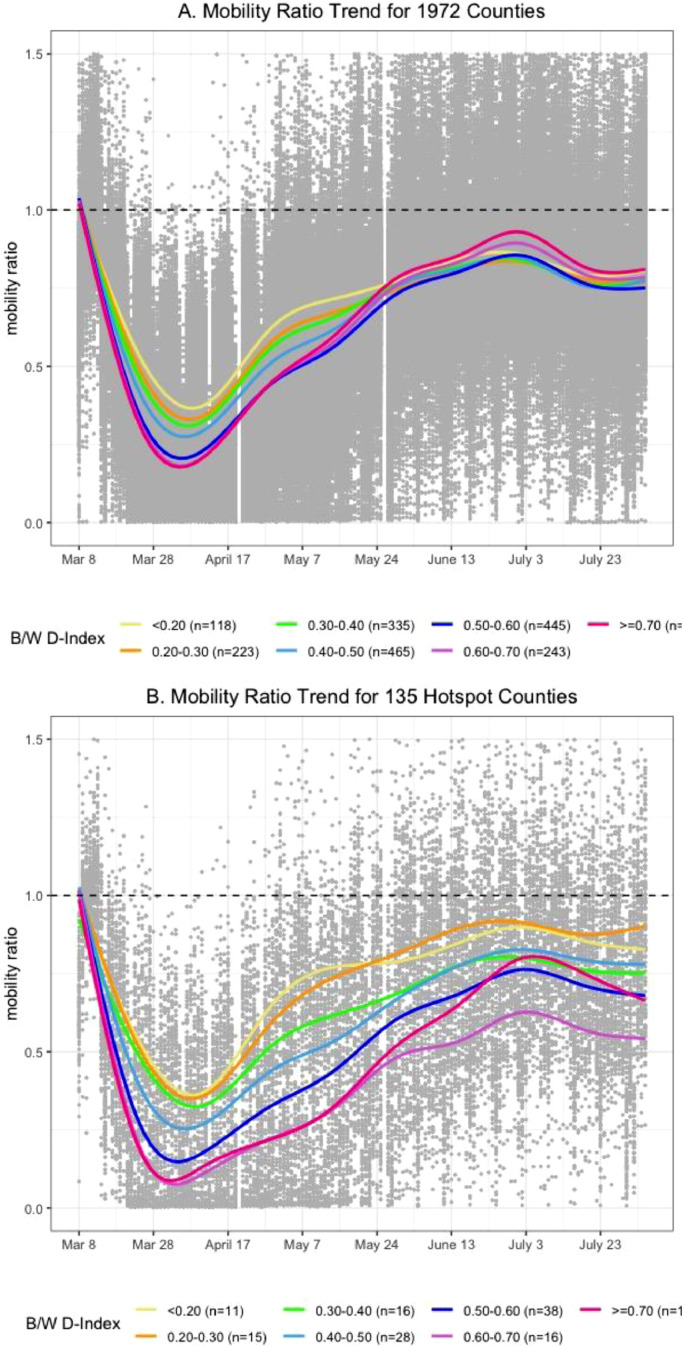
Fig. 1 depicts MR trends for the 1972 counties in figure A and 135 hotspot counties in 174 figure B for seven categories of Black-White Dissimilarity index. The choice of cut-off points ensures sufficient cell size for each category to compare between the analytic and hotspot samples. These categories also cover the dissimilarity index in previous studies ranging from 0.20 to 0.90 with a median close to 0.5 [15]. Both A and B show that the seven MR curves for the Black-White Dissimilarity index categories decline sharply from March 8 to early April, and the trends start to rise steadily to a near-baseline level around July 3 and then level off. There are two noticeable differences between the two figures. First, the seven curves cluster closely in A whereas they diverge in B, implying that MR varies less by Black-White Dissimilarity index in the 1972 sample than it does in the hotspot sample. Second, and more interestingly, the curve for the highest Black-White Dissimilarity index category (> = 0.7, in red) crosses all four lower Black-White Dissimilarity index curves from April 17 to May 24 and remains at the top since then. This cross-over by the red curve is less pronounced in figure B. Together, these bypassing patterns are consistent with our hypothesis that residential racial segregation constrains spatial mobility when the whole population is locked down but increases the need for moving under the reopen order. The test of the hypothesis will be conducted in the modeling analysis.
Fig. 1.
Mobility Ratio Trends over the COVID-19 Course (March 8th to August 7th).
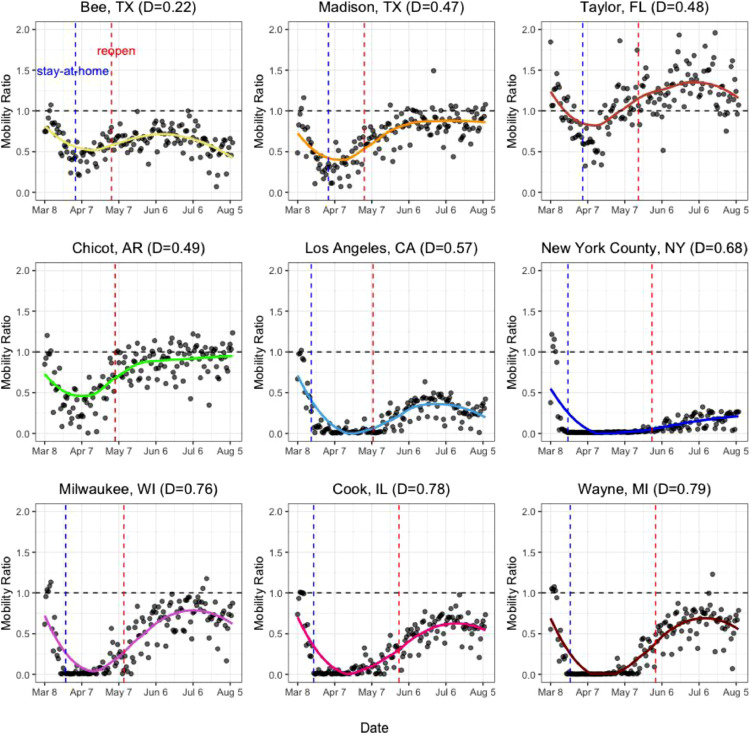
We selected nine hotspot counties reflecting both current and historical hotspots and visualize their profiles of MR over the COVID-19 course demarcated by stay-at-home and reopen policy timings in Fig. 2. These counties have various levels of Black-White Dissimilarity index (0.22–0.79 from top-left to bottom-right row-wise). Each curve follows the general trend shown in Fig. 1. The initial MR are similar around 0.7 in seven counties, the dip position is close to 0 in five counties, and the rebound to about the initial level occurs in seven counties. It is clear that Black-White Dissimilarity index alone does not determine the initial, dip and rebound positions and we must look at geographic, demographic and SES factors. We include a Supplementary Table to list the statistics of the same variables in Table 1 for each of the nine counties.
Fig. 2.
Mobility Ratio Profiles of 9 Selected Counties over the COVID-19 Course (March 8th to August 7th).
Fig. 2 depicts the relationship between mobility and policy for the nine selected counties. The continuing downward shift in mobility after lockdowns was introduced and the marked, but differential rise in mobility rates across the counties after reopen suggests a relationship between mobility and policy and a need to consider the policy environment in analysis. The divergence in curves for similarly segregated counties such as Milwaukee (a Dissimilarity index of 0.76) and New York (a Dissimilarity index of 0.68), but also of similar sizes such as Los Angeles County and New York County may be a reflection of how varying policy timings affect mobility rates, given that New York has longer lockdown period (reopened on May 29) than Los Angeles and Milwaukee (reopened on May 8 and May 11, respectively). Conversely as well, counties such as Cook County Illinois (Chicago) and Wayne County Michigan (Detroit) share very similar segregation rates (Dissimilarity indexes of 0.78 and 0.79, respectively) and two policy timings. They exhibit similar curves in the figure, despite of their large differences in population density, unemployment rates and demographic conditions. The steady decrease in mobility during lockdown periods in all counties and increase in mobility ratios after reopening orders in more segregated counties like Milwaukee versus New York and others supports the rationale of our hypothesis that segregation may not constrain mobility under reopening policies and other relevant social factors. One thing worth noting is the policy lag compared to human behavioral changes, such as the increase of mobility ratio was already underway before reopening policies. However, the degree of increase is larger in more segregated areas than less segregated areas, consistent with our rationale. We also observe a decrease of mobility ratio in early July, which may stem from the slow-down of job recovery during that period [26].
To test our hypothesis that Black-White Dissimilarity index constrains mobility under a stay-at-home order but increases mobility under a reopen order, we estimate an additive model and an interactive model with respect to Black-White Dissimilarity index and policy variables for the sample of 1972 counties and the 135 hotspots over the two policy periods of COVID-19. The trends in Figs. 1 and 2 suggest a cubic time function for the GEE model for longitudinal data. We specify a restricted cubit spline inspired by the empirical patterns.2 This time function serves the purpose of better fitting the non-linear nature of the time function. We focus on the substantive results from the model estimation presented in Table 2. The model comparisons at the bottom of the table (chi2 and degree of freedom) suggest that the interactive model significantly improves the model fit over the additive model. This improvement is true for both samples so we focus our interpretation of the interactive model results.
Table 2.
Estimates for mobility ratio over the COVID-19 course (March 8 to August 7th): US county level analysis.
| Variable | Analytic sample additive | Analytic sample interactive | Hotspot sample additive | Hotspot sample interactive |
|---|---|---|---|---|
| Time function | ||||
| linear | −0.007⁎⁎⁎ | −0.007⁎⁎⁎ | −0.007⁎⁎⁎ | −0.006⁎⁎⁎ |
| quadratic | 0.030⁎⁎⁎ | 0.030⁎⁎⁎ | 0.029⁎⁎⁎ | 0.029⁎⁎⁎ |
| cubic | −0.088⁎⁎⁎ | −0.088⁎⁎⁎ | −0.085⁎⁎⁎ | −0.084⁎⁎⁎ |
| Base mobility | −0.008⁎⁎⁎ | −0.008⁎⁎⁎ | −0.007* | −0.007* |
| Racial segregation | ||||
| Black-White Dissimilarity index | −0.104⁎⁎ | −0.141⁎⁎⁎ | −0.220* | 0.110 |
| *Stay-at-home | −0.213⁎⁎⁎ | −0.425⁎⁎⁎ | ||
| *Reopen | 0.154⁎⁎⁎ | −0.359⁎⁎⁎ | ||
| State policy | ||||
| Stay-at-home | −0.185⁎⁎⁎ | −0.082⁎⁎⁎ | −0.226⁎⁎⁎ | −0.040 |
| Reopen | −0.048⁎⁎⁎ | −0.114⁎⁎⁎ | −0.048⁎⁎ | 0.098⁎⁎⁎ |
| Geographic | ||||
| Metropolitan | −0.103⁎⁎⁎ | −0.103⁎⁎⁎ | −0.142⁎⁎⁎ | −0.143⁎⁎⁎ |
| Midwest | 0.154⁎⁎⁎ | 0.152⁎⁎⁎ | 0.338⁎⁎⁎ | 0.342⁎⁎⁎ |
| South | 0.134⁎⁎⁎ | 0.129⁎⁎⁎ | 0.285⁎⁎⁎ | 0.289⁎⁎⁎ |
| West | 0.164⁎⁎⁎ | 0.161⁎⁎⁎ | 0.097 | 0.097 |
| Demographic | ||||
| Prop. Black | −0.038 | −0.032 | −0.112 | −0.113 |
| Prop. Hispanic | −0.297⁎⁎⁎ | −0.297⁎⁎⁎ | 0.070 | 0.069 |
| Prop. Asian | −1.352⁎⁎⁎ | −1.346⁎⁎⁎ | −1.082⁎⁎ | −1.075⁎⁎ |
| Pop. Density (in 1000) | −0.019⁎⁎ | −0.018⁎⁎ | −0.007 | −0.007 |
| SES | ||||
| Vulnerability index | 0.170⁎⁎⁎ | 0.175⁎⁎⁎ | −0.149 | −0.153 |
| Unemployment (1-month lagged)a | 0.009⁎⁎⁎ | 0.008⁎⁎⁎ | 0.002* | 0.002⁎⁎⁎ |
| Constant | 1.025⁎⁎⁎ | 1.041⁎⁎⁎ | 1.198⁎⁎⁎ | 1.044⁎⁎⁎ |
| No. county-days | 296,901 | 296,901 | 20,201 | 20,201 |
| No. counties | 1972 | 1972 | 135 | 135 |
| chi2(df) | 120,222(17) | 122,856(29) | 11,159(17) | 11,323(19) |
Notes:
this is the one-month lagged time-varying unemployment rates at the county level.
Black-White Dissimilarity index is a measure of the evenness within counties Black and White residents are distributed across Census tracts. The index is only available for counties with a population having at least 100 Black people.
Mobility ratio is the median daily travel distance normalized by a baseline in order to capture the change of mobility levels over the pandemic course. It is calculated as the ratio of daily M50 from March 8 to August 7 relative to the baseline, the average of daily M50 between March 1 and March 7, obtained from mobile device locations by Descartes Labs.
Data:
Hopkins Population Center COVID-19 Data Hub.
* p < .05, ** p < .01, *** p < .001.
We start with the results for the analytic sample of 1972 counties by examining the coefficient for Black-White Dissimilarity index and its interaction with the two policy variables while holding other covariates constant. The main effect of Black-White Dissimilarity index is negative, significant (−0.141, p < .001), meaning that an increase of 0.1 in Black-White Dissimilarity index reduces MR by 0.141. The marginal effects under the stay-at-home order is (−0.141) + (−0.213) = −0.354, i.e., an increase of 0.1 in Black-White Dissimilarity index reduces MR by 0.354 under stay-at-home. The marginal effect under the reopen policy is (−0.141) + (0.154) = 0.013, revealing a positive segregation influence on MR under the reopen policy. We have tested and found that the difference between the two marginal effects is statistically significant (p < .001). Substantively, residents in spatially segregated counties become slightly more mobile compared to those in spatially integrated counties under the reopen order. Turning to the hotspot sample estimates, the estimate for the main effect is non-significant (p = .290), mostly due to the small sample size (135 counties) and fewer days before the stay-at-home order. The marginal effect of Black-White Dissimilarity index on MR under stay-at-home is (0.110) + (−0.425) = −0.315 and the corresponding value is −0.249 under the reopen order. A test of the equivalence of the two marginal effects is again statistically significant (p = .023). These results from both the analytic sample and the hotspot sample point to the significant decline of residential racial segregation influence on mobility from the stay-at-home period to the reopen period. These tests provide evidence to support our hypothesis, while holding other covariates constant.
The coefficients of control variables are robust between the additive and interactive models. Residents in metropolitan areas have lower MR than those in non-metro areas (e.g., −0.103 in additive model and −0.142 in interactive model, analytic sample, p < .001). Northeast region sees a greater reduction of movement than all other regions do. This may result from the immediate state response in issuing stay-at-home order to limit travel and curtail the spread of COVID-19, such as New York and New Jersey with high incidences of confirmed cases. Higher proportions of people of color lower the mobility ratio in general, but we find that the proportion Black is non-significant. This is perhaps due to its confounding effect with Black-White Dissimilarity index, given that the proportion Black is a proxy for residential racial segregation. Counties with higher population densities see a lower mobility ratio (−0.019 in the analytic sample, additive model, p = .005) . Socioeconomic conditions also matter. Counties with a higher socioeconomic vulnerability index (e.g. below poverty, unemployed, lower income and no high school diploma) have greater difficulty in practicing social distancing (0.170 in the analytic sample, additive model, p < .001). Moreover, high unemployment rates in the previous month create a large pool of unemployed individuals who may not be able to maintain the same level of social distancing (0.009 in the analytic sample, additive model, p < .001). For the hotspot sample, about half of the coefficients for the control variates are non-significant due to the small sample size and the significant coefficients have the same sign as those for the analytic sample.
6. Discussion
Like other studies that have demonstrated the disparate effects of racism on COVID-19 cases and mortality [3,27,28], this study suggests that racist structures such as residential segregation may play a role in the capacity of Blacks in segregated areas to successfully carry out the distancing required to prevent COVID-19 spread. Our research particularly demonstrates that segregation may have an effect on mobility and contribute to rates of exposure to and the incidence of COVID-19. Explanations from COVID-19 studies suggest that racial and ethnic minorities’ higher exposure may result from longer durations of commutes via public transport for work as well as demonstrated limitations to working from home [27]. For example, reporting on employment behaviors between 2018 and 2019 from the BLS shows that in comparison to roughly 30% of White workers who could work from home if necessary, only 19.7% of Black and 16.2% of Latinx workers could do so [29]. This deficit in home-based employment opportunities, along with an over-representation of Black populations in essential work fields as well as hospitality and service industries [28] may explain why, during and after the relaxation of COVID-19 restrictions and the return of employment in these fields, we witnessed an elevated mobility increase in segregated counties, as longer commutes from segregated areas were required to perform work outside of segregated living areas. As segregated areas are often deprived of needed resources such as staple good providers [15], further explanations for the effects presented in this study may relate to resources outside of segregated areas becoming available again once stay-at-home requirements lessened. This might reflect the increase in mobility rates in heavily segregated counties. These findings are consistent with surveys conducted on capacities to physically distance and isolate under episodes of pandemic influenza which reflected similar limitations to distance along racial lines [[30], [31], [32], [33]].
Our research has certain limitations. First, our measure of mobility is the median daily travel distance. Similar to other mobility measures such as the number of trips and the purpose of trips, our distance measure captures the risk of violating social distancing while it does not directly measure the compliance with the 6-feet rule. Information on the means of transportation would be more useful for gauging the real risks of mobility to social distancing as public transit, walking, and private car present differing risks. However, given the social interaction nature of human mobility and the positive relationship between human mobility and transmission of COVID-19 [21,34], mobility ratio captures a dimension of the multifaceted social distancing and we have adjusted for population density in our modeling. Second, our residential racial segregation measure is for county areas while past research usually measured segregation for metropolitan statistical areas (MSAs) that are economic and social integrated areas, larger than counties [35,36]. Given the importance of state and county policies during the pandemic, residential racial segregation at the county level allows us to analyze the differential influence of residential racial segregation on mobility and social distancing. It would be ideal for us to examine additional insights using other segregation measures (e.g., isolation index) but required data at tract or individual level are unavailable.
With these caveats, our research employs the daily county-level data to examine the impact of structural racism in the form of residential racial segregation across counties and its interaction with state policy shifts. This strategy yields important findings that underpins the relationship among structural racism, state policy, and the COVID-19 pandemic.
Declaration of Competing Interest
The authors declare no other competing interest.
Acknowledgments
Contributors
Alexandre White is the Primary Investigator of this article. He conducted the literature search, developed the design and assisted in data collection, interpretation and authored the final manuscript. Lingxin Hao is the Co-PI of this article and led the development for the quantitative data analysis and assisted in data interpretation, data collection and editing of the final manuscript. Xiao Yu assisted in the study design and conducted the data analysis, producing all figures and tables for the article. Yu assisted in the interpretation and writing of this article. Roland Thorpe Jr. Assisted in the study design and the interpretation of the data and findings. Thorpe Jr. also assisted in the editing and framing of the final manuscript.
Acknowledgments
The authors wish to thank the anonymous reviewers for their aid in strengthening this article. The authors would also like to thank the funding support of the National Institute of Child Health and Human Development, the National Institute on Aging and the National Institute on Minority Health and Health Disparities.
Funding
Funding was provided by The National Institute of Child Health and Human Development (R24HD042854), the National Institute on Aging (K02AG059140; R01AG054363) and the Eunice Kennedy Shriver National Institute on Minority Health and Health Disparities (U54MD000214).
Data sharing statement
All data are available publicly. We draw county-day data from the COVID-19 Data Hub of the Hopkins Population Center (https://github.com/QFL2020/COVID_DataHub). The Data Hub includes publicly available data from The Johns Hopkins CSSE COVID-19 tracking system, Census Bureau, CDC, Bureau of Labor Statistics (BLS), Bureau of Economic Analysis and the Internal Revenue Service which were employed in this study. Mobility data from Descartes Labs are available at: https://github.com/descarteslabs/DL-COVID-19
Strobe adherence statement
The reporting of this study conforms to the STROBE Statement.
Footnotes
While some studies such as Badr et al. 2020 have suggested producing mobility ratios based on the average number of total trips taken per day instead of average total distance traveled, we tested both approaches and found similar trends. Specifically, our mobility ratio also decreased from a value of 1 since March 8th and started to increase in late March and early April, although from a lower ratio.
A cubic spline is a spline constructed of piecewise third-order polynomials which pass through a set of control points. A restricted cubic spline is a cubic spline in which the splines are constrained to be linear in the two tails, which is natural to many phenomena including physical mobility studied in this paper. We use Stata -mkspline- which determine knot locations based on well-adopted percentiles.
References
- 1.Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20(5):533–4. doi:10.1016/S1473-3099(20)30120-1 [DOI] [PMC free article] [PubMed]
- 2.Garg S. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019 — COVID-NET, 14 states, March 1–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69 doi: 10.15585/mmwr.mm6915e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Price-Haywood E.G., Burton J., Fort D., Seoane L. Hospitalization and mortality among black patients and white patients with Covid-19. N Engl J Med. 2020;382(26):2534–2543. doi: 10.1056/NEJMsa2011686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moore J.T., Ricaldi J.N., Rose C.E. Disparities in incidence of COVID-19 among underrepresented racial/ethnic groups in counties identified as hotspots during June 5–18, 2020 — 22 states, February–June 2020. MMWR Morb Mortal Wkly Rep. 2020;69(33) doi: 10.15585/mmwr.mm6933e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Massey D.S. Still the linchpin: segregation and stratification in the USA. Race Soc Probl. 2020;12(1):1–12. doi: 10.1007/s12552-019-09280-1. [DOI] [Google Scholar]
- 6.Williams D.R., Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116(5):404–416. doi: 10.1016/S0033-3549(04)50068-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Williams D.R., Sternthal M. Understanding racial-ethnic disparities in health sociological contributions. J Health Soc Behav. 2010;51(1 suppl):S15–S27. doi: 10.1177/0022146510383838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hill J., Nielsen M., Fox M.H. Understanding the social factors that contribute to diabetes: a means to informing health care and social policies for the chronically Ill. Perm J. 2013;17(2):67–72. doi: 10.7812/TPP/12-099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Phelan J.C., Link B.G. Is racism a fundamental cause of inequalities in health? Annu Rev Sociol. 2015;41(1):311–330. doi: 10.1146/annurev-soc-073014-112305. [DOI] [Google Scholar]
- 10.Schulz A.J., Williams D.R., Israel B.A., Lempert L.B. Racial and spatial relations as fundamental determinants of health in detroit. Milbank Q. 2002;80(4):677–707. doi: 10.1111/1468-0009.00028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.White K., Haas J.S., Williams D.R. Elucidating the role of place in health care disparities: the example of racial/ethnic residential segregation. Health Serv Res. 2012;47(3pt2):1278–1299. doi: 10.1111/j.1475-6773.2012.01410.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Farber S., O'Kelly M., Miller H.J., Neutens T. Measuring segregation using patterns of daily travel behavior: a social interaction based model of exposure. J Transp Geogr. 2015;49:26–38. doi: 10.1016/j.jtrangeo.2015.10.009. [DOI] [Google Scholar]
- 13.Kain J.F. Housing segregation, negro employment, and metropolitan decentralization. Q J Econ. 1968;82(2):175. doi: 10.2307/1885893. [DOI] [Google Scholar]
- 14.Kronenfeld J.J. Vol. 31. Emerald Group Publishing Limited; 2013. (Social determinants, health disparities and linkages to health and health care). [DOI] [Google Scholar]
- 15.Massey D.S., Denton N.A. The Dimensions of Residential Segregation. Soc Forces. 1988;67(2):281–315. doi: 10.2307/2579183. [DOI] [Google Scholar]
- 16.Tilly C. University of California Press; 1998. Durable inequality. [Google Scholar]
- 17.Badr H.S., Du H., Marshall M., Dong E., Squire M.M., Gardner L.M. Association between mobility patterns and COVID-19 transmission in the USA: a mathematical modelling study. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30553-3. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kraemer M.U.G., Yang C.H., Gutierrez B. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science. 2020;368(6490):493–497. doi: 10.1126/science.abb4218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.The Harvard Global Health Institute . The Harvard Global Health Institute; 2020. Key metrics for covid suppression: a framework for policy makers and the public.https://globalepidemics.org/wp-content/uploads/2020/06/key_metrics_and_indicators_v4.pdf Harvard's edmond J. safra center for ethics. Published online. [Google Scholar]
- 20.Cases in the U.S. | CDC. Accessed 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html
- 21.Warren M.S., Skillman S.W. Mobility changes in response to COVID-19. arXiv:200314228 [cs]. Published online March 31, 2020. Accessed August 11, 2020. http://arxiv.org/abs/2003.14228
- 22.Kraemer M.U., Sinka M.E., Duda K.A. The global distribution of the arbovirus vectors Aedes aegypti and Ae. albopictus. Elife. 2015;4 doi: 10.7554/eLife.08347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Residential segregation - black/white*. County Health Rankings & Roadmaps. Accessed August 11, 2020. https://www.countyhealthrankings.org/explore-health-rankings/measures-data-sources/county-health-rankings-model/health-factors/social-and-economic-factors/family-social-support/residential-segregation-blackwhite
- 24.Tables and Maps Created by BLS. Accessed August 11, 2020. https://www.bls.gov/lau/tables.htm
- 25.Flanagan B.E., Hallisey E.J., Adams E., Lavery A. Measuring community vulnerability to natural and anthropogenic hazards: the centers for disease control and prevention's social vulnerability index. J Environ Health. 2018;80(10):34–36. [PMC free article] [PubMed] [Google Scholar]
- 26.Bureau of Labor Statistics. The employment situation — July 2020. Published online August 7, 2020:42.
- 27.Yaya S., Yeboah H., Charles C.H., Otu A., Labonte R. Ethnic and racial disparities in COVID-19-related deaths: counting the trees, hiding the forest. BMJ Glob Health. 2020;5(6) doi: 10.1136/bmjgh-2020-002913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.CDC . Centers for Disease Control and Prevention; 2020. Coronavirus disease 2019 (COVID-19): COVID-19 in racial and ethnic minority groups.https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/racial-ethnic-minorities.html Published February 11. [Google Scholar]
- 29.Table 1. Workers who could work at home, did work at home, and were paid for work at home, by selected characteristics, averages for the period 2017-2018. Accessed August 12, 2020. https://www.bls.gov/news.release/flex2.t01.htm
- 30.Quinn S.C., Kumar S., Freimuth V.S., Musa D., Casteneda-Angarita N., Kidwell K. Racial disparities in exposure, susceptibility, and access to health care in the US H1N1 influenza pandemic. Am J Public Health. 2011;101(2):285–293. doi: 10.2105/AJPH.2009.188029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dee D.L., Bensyl D.M., Gindler J. Racial and ethnic disparities in hospitalizations and deaths associated with 2009 pandemic influenza A (H1N1) virus infections in the United States. Ann Epidemiol. 2011;21(8):623–630. doi: 10.1016/j.annepidem.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 32.Lowcock E.C., Rosella L.C., Foisy J., McGeer A., Crowcroft N. The social determinants of health and pandemic H1N1 2009 influenza severity. Am J Public Health. 2012;102(8):e51–e58. doi: 10.2105/AJPH.2012.300814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Blendon R.J., Koonin L.M., Benson J.M. Public response to community mitigation measures for pandemic influenza. Emerg Infect Dis. 2008;14(5):778–786. doi: 10.3201/eid1405.071437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhao S., Zhuang Z., Cao P. Quantifying the association between domestic travel and the exportation of novel coronavirus (2019-nCoV) cases from Wuhan, China in 2020: a correlational analysis. J Travel Med. 2020;27(2):taaa022. doi: 10.1093/jtm/taaa022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Corral I., Landrine H., Hao Y., Zhao L., Mellerson J.L., Cooper D.L. Residential segregation, health behavior and overweight/obesity among a national sample of African American adults. J Health Psychol. 2012;17(3):371–378. doi: 10.1177/1359105311417191. [DOI] [PubMed] [Google Scholar]
- 36.Do D.P., Frank R., Zheng C., Iceland J. Hispanic segregation and poor health: it's not just black and white. Am J Epidemiol. 2017;186(8):990–999. doi: 10.1093/aje/kwx172. [DOI] [PubMed] [Google Scholar]