Abstract
The high prevalence and psychological impact of childhood exposure to potentially traumatic events (PTE) is a major public health concern in the United States. Considerable evidence has demonstrated the significant racial disparities that exist with respect to PTE exposure, indicating that Black youth are particularly burdened by these harmful experiences. Racism may serve a unique role in explaining why Black youth are disproportionately exposed to PTEs, and why mental health disparities are more likely to occur following such experiences. Despite clear evidence acknowledging racism as a major life stressor for Black youth, theoretical models of early childhood adversity have largely neglected the multifaceted influence of racism on mental health outcomes. Inspired by bourgeoning literature highlighting the potentially traumatic nature of racism-related experiences for Black youth, we present a culturally-informed Adverse Childhood Experiences (ACEs) model, or “C-ACE”, to understand the pervasive and deleterious mental health impact of racism on Black youth. This model extends the ACE framework by noting the significance of racism as an ACE exposure risk factor, a distinct ACE category, and a determinant of post-ACE mental health outcomes among Black youth. The model acknowledges and supports the advancement of ACEs research that takes a culturally informed approach to understanding the intergenerational and multilevel impact of racism on the mental health of Black youth. Future research utilizing the proposed C-ACE model is essential for informing clinical and public health initiatives centered on reducing the mental health impact of racism-related experiences and health disparities in the United States.
Keywords: Racism, Racial trauma, Adverse childhood experiences, Black youth, Traumatic stress
California’s first Surgeon General, Dr. Nadine Burke Harris, made national headlines in October 2019 for her recommendation that every child in school be screened for trauma. Although this may seem like a radical suggestion, approximately two-thirds of youth in the U.S. experience at least one potentially traumatic event (PTE) before age 16 (Copeland et al. 2007; Substance Abuse and Mental Health Services Administration 2017), with approximately 50% of youth experiencing serious interpersonal trauma before age 18 (Finkelhor et al. 2013; Kilpatrick et al. 2003b). Exposure to PTEs is greatest among youth from socially disadvantaged backgrounds, with Black1 youth reporting the highest rates (López et al. 2017). These disparities may be explained, in part, due to the overrepresentation of Black youth in contexts where PTEs are more likely to occur, such as low-income communities, juvenile detention centers, and foster care placements (Andrews et al. 2015; Wamser-Nanney et al. 2018).
Although exposure to PTEs are detrimental to the well-being of all youth, their effects may be particularly harmful among Black youth given the relevance and impact of racism and racial discrimination. Racism is defined as “the exercise of power against a racial group defined as inferior by individuals and institutions with the intentional or unintentional support of the entire culture” (Jones 1972, p. 117), whereas experiences of racial discrimination (i.e., individual racism) represent behavioral enactments of racism that reinforce beliefs that one racial group is inferior to another (Jones 1972). Racial discrimination is nearly ubiquitous, with recent data indicating that Black youth average five experiences of racial discrimination per day (English et al. 2020). This is concerning given the myriad of adverse consequences linked to racial discrimination among Black youth including decreased psychological, physical, behavioral, and emotional functioning (Cave et al. 2020; Priest et al. 2013). The harmful indirect effects of racial discrimination are equally potent (Jones et al. 2016), with research illustrating that the deleterious effects of other stressors may be amplified for Black youth who have experienced racial discrimination, thereby compounding risk for negative mental health outcomes (De Coster and Thompson 2017).
A growing body of research has demonstrated that the profound effects of racial discrimination on health may be best understood through a traumatic stress perspective (i.e., racial trauma). However, the majority of extant work detailing the traumatic implications of racial discrimination has been conducted among Black adults (Bryant-Davis and Ocampo 2005; Carter 2007; Williams et al. 2018), with considerably few studies taking steps to consider racial discrimination as a PTE for Black youth (Anderson and Stevenson 2019; Jernigan and Daniel 2011; Saleem et al. 2019). As such, there is a shortage of comprehensive conceptual models that forecast how racial discrimination can be conceptualized as a PTE to inform mental health trajectories among Black youth. Thus, the goal of the current paper is to propose a culturally-informed adaptation of the Adverse Childhood Experiences (ACEs) conceptual framework – a well-known and highly referenced framework for understanding the mental and behavioral health consequences of PTEs among youth (Felitti et al. 1998). The proposed model integrates childhood models of racial trauma into the ACEs framework, detailing how manifestations of racism (e.g., racial discrimination) can simultaneously serve as an ACE exposure risk factor, a discrete ACE category, and a determinant of post-ACE mental health outcomes. Subsequently, we discuss how the present adaptation of the ACEs model provides direction for future research that can inform public health efforts centered on clarifying and addressing the impact of racism on Black youth.
The ACEs Conceptual Framework
Several theoretical frameworks highlight the increased health risk conferred by childhood traumatic stress and exposure to PTEs (Ford and Greene 2017), with the ACEs framework representing perhaps one of the most widely-acknowledged among them. Based on the seminal work of Felitti et al. (1998), the ACEs model provides a risk-based framework in which childhood exposure to PTEs are theorized to have a dose-dependent effect on health risk behaviors, developmental disruptions, and mental and physical illness during childhood that extends well into adulthood (Felitti et al. 1998; Hughes et al. 2017; Kalmakis and Chandler 2015). According to the Centers for Disease Control and Prevention (CDC), ACEs represent any individual or environmental experience that disrupts a child’s sense of safety, stability, or bonding (CDC 2020a). Though broadly defined, ACEs literature has generally examined the implications of exposure to the following adverse events: childhood abuse (sexual, physical, emotional), household substance abuse and mental illness, neglect, parental separation or divorce, and household criminality (Hughes et al. 2017).
The nature and impact of ACEs can be best understood by referencing the ACE pyramid (CDC 2020b), which depicts factors influencing exposure to ACEs and how ACEs are connected with poor health outcomes. Positioned at the base of the ACE pyramid is historical trauma, which refers to the notion that the collective traumatic experiences of one generation (e.g., a parent’s own trauma history) can increase predispositions for disease and suboptimal psychological functioning in future generations (Brave Heart and DeBruyn 1998). Historical trauma informs the local context and social conditions (e.g., home environment, socioeconomic resources, neighborhood safety) in which youth maturate, directly effecting the likelihood of exposure and/or direct encounters with ACEs. Upon exposure to ACEs, whether directly (e.g., physical abuse) or indirectly (e.g., witnessing interpersonal violence), youth may experience disruptions in neurodevelopment (e.g., prefrontal brain regions), which can subsequently impair social (e.g., connectedness), emotional (e.g., emotion regulation), and cognitive (e.g., executive functioning) functioning. These impairments, in turn, are shown to heighten risk for the adoption of health risk behaviors (e.g., substance and alcohol use), which subsequently increase risk for poor health outcomes (disease, psychological and physical functioning), and ultimately early death.
Ample research has supported the ACEs pyramid, highlighting the harmful and widespread effects that ACEs can have on health across the lifespan. For instance, research examining the intergenerational transmission of historical trauma has shown that parental ACEs are associated with poorer infant health outcomes (Racine et al. 2018) and later childhood health and health risk behavior (Lê-Scherban et al. 2018). As it relates to the family context, parents with a history of ACEs are also at increased risk for anxiety and depression (Letourneau et al. 2019), have greater difficulty forming secure attachments to their offspring (Iyengar et al. 2014), and are at greater risk to engage in behaviors (e.g., substance use) that impair positive parenting (Meulewaeter et al. 2019). Together, these parental risk factors can foster an ACE prone environment for youth. Upon experiencing ACEs, youth are at greater risk of neurological (e.g., physiological damage), social-emotional (e.g., emotion reactivity), and cognitive impairments (e.g., executive functioning), and are more likely to engage in maladaptive health risk behaviors including substance use and juvenile offenses (Danese and McEwen 2012; Guinosso et al. 2016; Kalmakis and Chandler 2015). ACEs have also been linked with chronic physical health conditions such as cardiovascular disease, respiratory disease, and cancer, especially among those who have experienced multiple ACEs (Bellis et al. 2019; Hughes et al. 2017; Kalmakis and Chandler 2015). The effects of ACEs may be most pronounced in the context of mental health, with literature suggesting that ACEs could account for as much as 30% of cases of anxiety, 40% of cases of depression in North America, and increased rates of suicide (Bellis et al. 2019; Sachs-Ericsson et al. 2016).
ACEs among Black Youth
Unfortunately, significant disparities exist with respect to ACE exposure. Socially disadvantaged groups, and Black youth in particular, are more likely to report multiple ACEs relative to their White counterparts (Bruner 2017; Maguire-Jack et al. 2019; Slopen et al. 2016; Strompolis et al. 2019). This disproportionate exposure may help to explain why Black youth evidence greater health risk behaviors (e.g., conduct problems, substance use) and mental health concerns following exposure to ACEs, compared to youth from other racial and ethnic backgrounds (Fagan and Novak 2018; Lee and Chen 2017; Liu et al. 2018). The psychological burden of ACEs have lasting consequences that continue to disparately plague Black youth as they age into adulthood, and has been linked to increases in symptoms of depression, anxiety, and posttraumatic stress symptoms, as well as increased tobacco, alcohol, and marijuana use (Elkins et al. 2019; Mersky et al. 2013).
Despite the increased mental health risk that Black youth face because of their increased exposure to ACEs, research examining why these disparities exist is scarce. One possible explanation for this lack of research is that the conventional ACEs framework overlooks unique stressors faced by Black youth and youth from other racial and ethnic minority groups (Strompolis et al. 2019; Wang et al. 2019). To this end, scholars have pointed to the necessity of expanding the conceptualization of ACEs to incorporate stressful life experiences of particular relevance to historically disadvantaged and marginalized groups. In a qualitative examination of ACEs within a sample of low-income youth (71% Black), Wade et al. (2014) found that youth spoke about ACEs in ways that extended beyond the traditional conceptualization. Specifically, while some responses aligned with conventional ACEs (e.g., familial substance, physical abuse), youth also described experiences that have not been customarily discussed within ACEs literature including racial discrimination, community violence, poverty, and interactions with juvenile justice and foster care system. As such, the authors concluded that the ACEs framework should be expanded to be more representative of the unique PTEs that youth of color encounter.
In support of this expanded ACEs approach, a study by Cronholm et al. (2015) compared the conventional ACEs framework to an expanded version that included PTEs relevant to experiences of community violence, racial discrimination, foster care placement, and other experiences among a racially diverse adult population. Their findings revealed that racial and ethnic minority adults endorsed more ACEs using their expanded framework, relative to their White counterparts. More recent investigations have yielded similar results finding that Black youth were more likely to report ACEs consistent with the expanded framework (e.g., discrimination and community violence), compared to their White counterparts who were more likely to endorse ACEs that more so aligned with the conventional framework (e.g., exposure to parental drug and alcohol use; Maguire-Jack et al. 2019). Taken together, significant variation exists in the typology of ACEs, which may differ as a function of one’s racial and ethnic background. Despite this evidence, PTEs that disparately occur among youth of color remain on the periphery of scholarly investigations. Integration of culturally-informed PTEs within the broader ACEs framework is an essential first step for understanding and addressing critical gaps in the empirical literature on childhood adversity and traumatic stress.
While several unique PTEs fit within this expanded conceptualization of ACEs, racism-related experiences, and racial discrimination in particular, are among the most chronic and taxing stressors that Black youth negotiate throughout development (Jones et al. 2020; Priest et al. 2013). In cross-sectional and longitudinal studies of Black youth, racism-related experiences have been directly and indirectly associated with greater perceptions of other stressors, increased symptoms of anxiety and depression, hypervigilance, suicidality, lower self-esteem, and emotion and behavioral regulation difficulties (Cave et al. 2020; Himmelstein et al. 2015; Kirkinis et al. 2018; Priest et al. 2013). Indeed, racism has been extensively discussed as key social determinant to ACE exposure and health disparity (Williams and Williams-Morris 2000; Williams et al. 2019; Williams and Collins 2001; Williams and Mohammed 2009), suggesting that racism-related experiences are central to pinpoint when discussing PTEs among Black youth.
Conceptualizing Racial Discrimination as Racial Trauma
Given the enduring and pervasive negative impact of racism on Black youth’s psychological adjustment, scholars have argued that the effects of racism-related encounters (e.g., racial discrimination) should be conceptualized as a distinct form of traumatic stress, otherwise referred to as “racial trauma.” Racial trauma can be defined as “the emotional and psychological response to racism-related incidents that are unexpected, experienced as threatening, and result in significant psychological stress” (Pieterse 2018, p. 205). The concept of racial trauma stems from Carter’s (2007) theory of race-based traumatic stress (Carter 2007), which asserts that racism related experiences can cause emotional and psychological injury which threatens an individual’s sense of safety and security, subsequently triggering a traumatic stress response (e.g., intrusive thoughts, anxiety and depression, avoidance, vigilance).
In support of the notion of racial trauma, scholarship has documented the considerable overlap between the consequences of racial discrimination and traumatic stress sequelae. For example, racial discrimination has been found to predict negative outcomes that strongly parallel post-traumatic stress reactions (Bryant-Davis and Ocampo 2005; Carter et al. 2020). The connection between racism-related experiences and trauma-related symptoms remains even after controlling for general life stressors and other PTEs (Mendez et al. 2020; Pieterse et al. 2010; Polanco-Roman et al. 2016), suggesting that this association may be particularly robust. Thus, it follows that a recent systematic review has implicated racial discrimination as a significant risk factor for trauma symptomatology (Kirkinis et al. 2018).
Given the potentially traumatic implications of racial discrimination, recent literature has taken steps to highlight the developmental implications of racial trauma among Black youth. For example, Jernigan and Daniel (2011) assert that Black youth are particularly vulnerable to racial trauma as they have yet to develop the skills necessary to adaptively process and cope with racism-related encounters. According to Jernigan and Daniel, the school environment is the primary context in which Black youth are repeatedly subjected to racial discrimination by teachers and peers, and without considerable support and advocacy, it may be very difficult to reduce or overcome these traumatic experiences. The Developmental and Ecological Model of Youth Racial Trauma (DEMYth-RT; Saleem et al. 2019) builds upon the work of Jernigan and Daniel by providing a framework to explain how historical trauma, present day interpersonal racism, and ecological factors interact to contribute to posttraumatic stress symptoms among youth of color. Consistent with the intergenerational transmission of stress (Bowers and Yehuda 2016), the DEMYth-RT model asserts that historical trauma (i.e., racial oppression, slavery, parent experiences of racism) informs baseline stress levels, contributing to social and epigenetic dispositions in ways that increase vulnerability to contemporary expressions of racism. Present-day encounters of racial discrimination may further amplify these vulnerabilities and increase risk for traumatic stress responses, with child appraisals, perceptions, and responses to racism-related experiences being further influenced by developmental age and the multiple ecological contexts in which youth are imbedded (e.g., family, community, school).
Although this literature makes a compelling case to suggest that racial trauma represents a pernicious reality for Black youth and other youth of color, it is important to acknowledge that person mediated expressions of racial discrimination represent only a piece of the racism picture (Harrell 1999). Indeed, racism simultaneously operates at the individual (e.g., racial discrimination), institutional (e.g., mass incarceration), and cultural (e.g., stereotypical representations in media) level (Jones 1972) to increase risk for ACEs exposure and health vulnerability among Black youth. Further, racial trauma does not exist in isolation to hinder health trajectories of Black youth. That is, Black youth are not only expected to navigate racism, but also do so while negotiating exposure to other stressors and PTEs that shape physical and psychological outcomes over time. Despite increasing calls to acknowledge the importance of the multilevel nature of racism (Neblett 2019), in addition to how racism-related experiences may interact with other stressors to inform health outcomes (De Coster and Thompson 2017; Peters and Massey 1983), such considerations remain absent within the ACEs literature. As such, a comprehensive conceptual model of childhood adversity that fully acknowledges the pervasive, distinct, and interactive influence of racism on the lived experiences of Black youth is needed.
A Culturally-Informed ACEs Model
Inspired by developmental frameworks elucidating the significance of racial trauma on health among Black youth (Jernigan and Daniel 2011; Saleem et al. 2019), we present a culturally-informed ACEs model, or “C-ACE,” for understanding the pervasive mental health impact of racism on Black youth. This targeted C-ACE model presents racism as a unique sociocultural factor with historical underpinnings that contribute to present day ACE exposure disparities and subsequent stress-related psychopathology among Black youth.
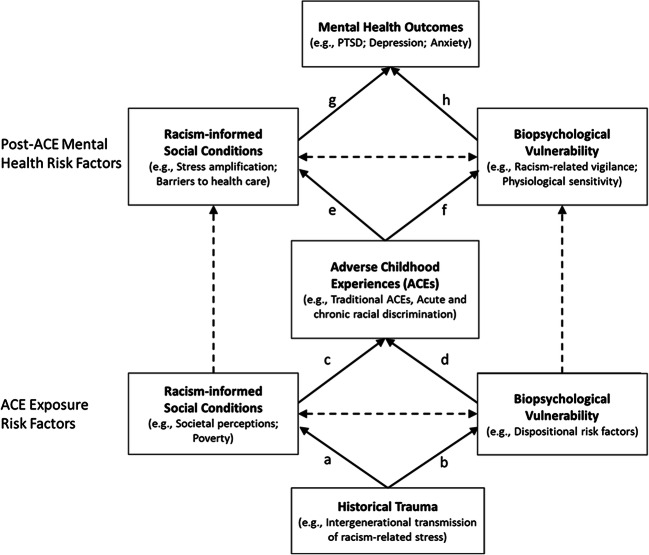
Leveraging the preexisting infrastructure of the ACEs pyramid, the proposed model first recognizes risk factors that increase exposure and vulnerability to ACEs, beginning with historical trauma (see Fig. 1). Unique to the present model is our conceptualization of historical trauma through a historical racism perspective. This allows for the formal recognition of the historical and intergenerational effects of racism, particularly as it pertains to ACE exposure and health disparities that disproportionately impact Black youth. With this historical backdrop serving as the foundation of our C-ACE model, we then present evidence illustrating how historical racism continues to shape present-day social conditions (path a), biological predispositions of Black youth (path b), and overall biopsychosocial vulnerability and risk of ACEs (paths c and d). We next present how contemporary manifestations of racism qualify as ACEs, and how the distinct and stress-amplifying characteristics of racism are influenced by post-ACE risk factors (path e and f) to influence health outcomes (path g and h). Below, we describe the model in detail, discussing relevant pathways where appropriate. The discussion integrates several bodies of empirical literature, content from which is presented in abbreviated fashion to maintain focus on presenting the fundamental components of the C-ACE model.
Fig. 1.
Culturally informed adverse childhood experiences framework for understanding the pervasive mental health impact of racism on black youth
Historical Trauma
As referenced previously, the intergenerational transmission of historical trauma may inform the extent to which youth are exposed to and affected by adverse experiences. The multigenerational nature of historical trauma was initially examined in relation to the Holocaust, with the psychological effects of this mass trauma continuing to be detected in the offspring of Holocaust survivors and even three generations later (Giladi and Bell 2013; Kellerman 2001; Scharf 2007). Building from this compelling evidence, scholars have continued to link historical trauma to contemporary health disparities, particularly among groups who have been subjected to mass trauma as a result of historical colonization, marginalization, genocide, family separation, generational displacement, and other traumatic losses (Brave Heart 2003; Brockie et al. 2015; Mohatt et al. 2014; Sotero 2006). In the United States, historical trauma is especially important to consider for individuals of African descent, with their ancestors being forcefully taken from their homeland, shipped across the Atlantic, and forced into slavery (Harrell 2000).
The atrocities that occurred during American slavery are well-documented and included the abduction and separation of families, sexual exploitation, chronic abuse, and mass murder (Kolchin 2003). Enslaved youth and adults were subjugated to these daily traumatic experiences for generations. The systematic disenfranchisement and persecution of Black Americans continued following the abolishment of slavery at the end of American Civil War, as evidenced by the widespread practice of lynching and eventual institutionalization of Jim Crow laws, which reinforced and maintained the dehumanized and devalued status of Black individuals in America. The historical legacy of racism and slavery in the United States has been linked to the continued marginalization of Black communities within contemporary society, chiefly operating through institutional and structural practices that sustain inequity across multiple sociocultural domains (Williams et al. 2019).
Historical Racism and Current Social Conditions
As noted by Ruef and Fletcher (2003), the enduring effects of historical racism on contemporary social conditions (path a) represents an institutional legacy, or “the reproduction of material-resource and cultural conditions from a social institution despite the fact that the institution has been formally dismantled” (p. 447). That is, while formal practices of chattel slavery, lynchings, and Jim Crow laws may have ended, the ideologies, behaviors, and beliefs that undergirded these practices continue to shape the current cultural context, and serve to maintain economic, educational, and social disadvantage within the Black community (Williams et al. 2019). To this end, the effects of historical racism can be detected within numerous structural systems including housing and lending, residential segregation, education and employment, and access to healthcare (Williams et al. 2019), which in turn, increase risk to ACE exposure and health disparities (path c).
Although there are several ways that historical racism has shaped present day social conditions, perhaps the most influential on the social landscape of the United States is the unequal distribution of wealth, particularly between White and Black households (Thomas et al. 2020). Recent estimates suggest that the medium household income for Black families is only 61% of that of White households, and that this disparity has only marginally improved since 1970 (Pew Research Center 2020). This unequal distribution continues to exist even after accounting for educational attainment and other factors traditionally affiliated with economic mobility, such as home ownership (Darity et al. 2018). This financial disparity may help to explain why Black youth are more likely to live beneath the poverty line compared to youth of any other racial demographic (Bruner 2017), which factors into the maintenance of residential segregation practices, and the disproportionate concentration of Black families within impoverished and high-crime communities (Williams 2018; Williams and Collins 2001). Such, financial disparities and institutional practices increase risk of exposure to ACEs such as community violence, food insecurity, and household instability (Graves et al. 2010).
Moreover, the historical legacy of slavery and racism has fundamentally altered the way broader society perceives Black youth and the Black community as a composite. People, including police officers, are more likely to perceive Black youth as older, less innocent, less intelligent, and more violent compared to youth from other demographic backgrounds (Epstein et al. 2017; Goff et al. 2014). As evidenced by the countless incidents of racial profiling (e.g., stop and frisk, driving while Black) and murders of innocent Black youth and adults by law enforcement and others in the community (e.g., Trayvon Martin, Tamir Rice, Renisha McBride, Ahmuad Arbery, Breoana Taylor, George Floyd), these negative perceptions can have traumatic and potentially lethal consequences. Literature has tied these skewed perceptions of Black individuals to the negative historical depictions and portrayals of Black individuals during and after slavery (Goff et al. 2014; Smiley and Fakunle 2016), which has only continued in modern day media and news (Entman and Rojecki 2001). Such negative depictions and perceptions of Black people may inform, in part, why Black youth are suspended from school, arrested, incarcerated, and more harshly sentenced in the justice system relative to their White peers (Jarvis and Okonofua 2020; Mallett 2018; Morris and Perry 2016), each of which may considerably increase risk for ACEs. This may also help to explain why Black youth in the U.S. are six times more likely to have a parent in jail, compared to White youth (Sykes and Pettit 2014). Although having a parent in prison is currently conceptualized as an ACE, it also increases ACE exposure for youth by reducing the ability of Black families to establish stability and independence, financially support children, and attain social mobility (Harris et al. 2010; Sykes and Pettit 2014).
Historical Racism and Biological Predispositions
Historical trauma also contributes to the biological predisposition of Black youth (path b) in ways that increase risk of ACEs (path d). Behavioral expressions of racism (i.e., racial discrimination) have been shown to compromise health from one generation to the next, particularly through its influence on the prenatal environment of Black women (Alhusen et al. 2016; Dominguez 2008). Racial discrimination has been implicated as a key mechanism to explain why Black mothers face significant disparities in rates of birth complications, preterm births, and low birthweight babies, regardless of sociodemographic characteristics and maternal health behaviors (Alhusen et al. 2016; Giurgescu et al. 2011).
The link between racial discrimination and adverse birth outcomes among Black women has been conceptualized as a result of stress-induced disruptions in immune and inflammatory processes that negatively impact the prenatal environment (Christian 2012). For example, among pregnant Black women, racial discrimination has been associated with abnormal cortisol levels produced by the Hypothalamic-Pituitary-Adrenal (HPA) axis–one of the body’s major neuroendocrine stress response systems. Abnormal cortisol levels have been connected with pregnancy and delivery complications, such as preeclampsia, fetal growth delay, and preterm birth (Davis and Sandman 2006; Nepomnaschy et al. 2006; Reis et al. 1999), all of which are disparately observed within Black women (Giscombé and Lobel 2005; Lu and Halfon 2003; Slaughter-Acey et al. 2019). Maternal experiences of racial discrimination have also been linked to decreased cellular immune function (Christian et al. 2012), which increases risk for infection and birth complications, further compromising the health of Black infants during delivery and postnatally. Finally, experiences of racial discrimination among Black women have been linked to increased cardiovascular reactivity, which has been linked with poor postnatal infant outcomes, such as low birth weight and delays in fetal growth rates (Hilmert et al. 2014). These adverse birth outcomes can have long-term effects on the health Black children, leading to socio-emotional problems (Montagna and Nosarti 2016) and sustained disruption of physiological stress response systems, including diastolic blood pressure and the HPA axis (Arpi and Ferrari 2013; Covelli et al. 2007). Indeed, dysregulation of stress response systems can increase risk for attention and behavioral problems, impulsive behaviors, and socioemotional difficulties, which can further shape exposure and vulnerability to ACEs (Arpi and Ferrari 2013; Heard-Garris et al. 2018).
Interaction of Social and Biopsychological Vulnerability and Risk of ACEs
The joint interplay of social disadvantage and biopsychological predispositions ultimately determines risk for Black youth to be exposed to and affected by ACEs (paths a-d). The interaction of social and biological factors in relation to ACEs aligns with the diathesis-stress model, which asserts that as the degree or number of diatheses (i.e., predispositional vulnerabilities) increase, the stress required to negatively influence well-being decreases (McKeever and Huff 2003). In line with this literature, the proposed C-ACE model postulates that parental experiences of stress and trauma related to and/or compounded by racism-related experiences are passed down to offspring biologically, as well as through negative social conditions that shape the parent-child relationship and the family’s access to resources. Adverse social conditions shaped by historical and institutional racism such as poverty, exposure to community violence, and social marginalization also serve to uniquely affect and conjointly amplify Black youth’s preexisting biopsychological vulnerabilities, disrupting neurological, cognitive, and behavioral development (Blair and Raver 2016; Janusek et al. 2017). Thus, we assert that the interactive and intergenerational nature of social and biological vulnerabilities position Black youth to be particularly susceptible to ACEs and the deleterious health consequences that follow.
Conceptualizing Racial Discrimination as an ACE
In addition to serving as a risk factor for ACE exposure, the trauma conferring potential of direct and vicarious experiences of racism (e.g., racial discrimination) can serve as both a distinct, or time-limited, experience (e.g., being called a racial slur) and as a cumulative stressor (e.g., being treated as less intelligent than non-minority peers). While time-limited or more blatant experiences of racism can certainly reoccur (e.g., repeated exposure to Black individuals being harmed or murdered via social media; Tynes et al. 2019), cumulative or more subtle racism-related experiences such as “microaggressions”– brief behavioral or environmental exchanges that transmit denigrating messages due to their racial or ethnic background (Sue et al. 2007) – are posited to occur more frequently. Nevertheless, blatant and subtle manifestations of racism are equally harmful to mental health (Jones et al. 2016), and can both contribute to short- and long-term mental and physical health problems and disparities (Carter 2007; Cave et al. 2020; Jones et al. 2020). These lasting physical and psychological consequences are believed to result from prolonged activation of biological stress response systems, such as the aforementioned HPA axis, which can have a deleterious “weathering” effect on the body and on cognitive development (Berger and Sarnyai 2015; Geronimus et al. 2006; Matheson et al. 2019).
The biopsychosocial pathways by which racism-related experiences and stressors increase risk for disruptions in neurodevelopment, socio-emotional and cognitive development, health risk behaviors, and mental and physical health outcomes (Clark et al. 1999; Gibbons et al. 2018; Williams and Mohammed 2013), strongly parallel the pathways by which conventional ACEs have been conceptualized to influence health outcomes (Nurius et al. 2016). Specifically, racial discrimination among Black youth has been linked to a cadre of poor outcomes across the ACE pyramid including biological dysregulations (Berger and Sarnyai 2015), executive functioning and socio-emotional concerns (Bair and Steele 2010; Pachter and Coll 2009), substance use and delinquent behaviors (Gibbons et al. 2012; Simons et al. 2003), anxiety and depression (Priest et al. 2013), and increased mortality rates (Assari et al. 2017). In light of this evidence, it is crucial to expand conceptualizations of adversity to include racism-related experiences as an ACE, as this omission may lead to the underestimation of ACEs among ethnic and racial minority communities (Cronholm et al. 2015; Maguire-Jack et al. 2019; Wade et al. 2014).
Racism as Post-ACE Mental Health Risk Factor
In addition to being conceptualized as a risk factor for ACE exposure and as a distinct ACE, it is equally important to consider how racism contributes to post-ACE mental health vulnerability. The historically informed social conditions that increase risk for ACEs among Black youth also increase risk for poor psychological adjustment following ACE exposure. For example, there are clear racial disparities that exist in the quantity and quality of health care that Black and White youth and families receive (Alegria et al. 2010; Williams and Rucker 2000), which has been tied to institutional and structural racism as well as racial inequity in the United States. These disparities are further compounded by the fact that physicians and clinicians are remarkably ill-equipped to effectively discuss, diagnose, or treat issues pertaining to racism-related stress (Alvidrez et al. 2008; Snipes et al. 2011); for instance, Black youth are misdiagnosed as having more severe behavioral problems at higher rates than their White peers (Fadus et al. 2020; Liang et al. 2016), and as such, they are less likely to receive appropriate treatment. With access to quality healthcare and other forms of support being limited following exposure to ACEs, Black youth are at an increased risk for poor mental health outcomes (path g).
In addition to its enduring effects on societal social conditions, the omnipresent nature of racism also continues to confer increased biopsychological vulnerability to future stressors (path f), increasing risk for negative mental health outcomes (path h). Previous experiences of racial discrimination can lead Black youth to become particularly vigilant of their surroundings in efforts to mentally prepare themselves for future discriminatory events (i.e., racism-related vigilance; Clark et al. 2006). While vigilance can serve an important and contextually adaptive function to protect ones mental and physical well-being, the energy needed to sustain a constant state of vigilance can be psychologically and physiologically demanding, leading to increased sleep difficulty, increased physiological and immunology reactivity, and somatic concerns (Clark et al. 2006; Hicken et al. 2013; Williams and Mohammed 2009), thereby increasing stress vulnerability and risk of negative health outcomes (Himmelstein et al. 2015).
The combined biopsychosocial impact of racism following ACEs can contribute to poor mental health outcomes (i.e., trauma-related sequalae) among Black youth in several ways. First, dysregulated biological stress responses, increased cognitive distress, and lack of supportive resources following racism-related incidents may amplify the sensitivity to, and perceived severity of, other stressors that may not appear to on the surface be related to racism-related experiences (Williams 2018)—a process referred to as stress proliferation (Pearlin et al. 2005; Peters and Massey 1983). As an example, racial discrimination has been found to exacerbate the negative impact of other life stressors (including exposure to PTEs), and subsequently increase negative emotional and behavioral functioning such as anger and delinquency among Black youth (De Coster and Thompson 2017). Second, the significant impairment stemming from direct and vicarious racism-related experiences and social conditions may ultimately hamper one’s ability to engage in effective and adaptive coping strategies that assist in stress regulation. This may help to explain why Black youth evidence disparate rates of maladaptive coping strategies, such as substance use (Cooper et al. 2008; Miech et al. 2019), that only further add to stress vulnerability over time. Third, negative racial messages that existed in the pre-ACE environment may be further reinforced in the post-ACE environment due to the continued prevalence of high-profile racism-related incidents that occur and the lack of societal resource to assist in processing and making sense of these events.
Future Research Considerations
It has been established that the lives of Black youth are fundamentally altered by the profound effects of racism. Thus, we join the chorus of literature advocating for the need to account for racism-related stressors when discussing issues of childhood adversity and trauma, and for expanded conceptualizations of adversity to include PTEs that may be predominately relevant among socially disadvantaged communities (Cronholm et al. 2015; Jernigan and Daniel 2011; Saleem et al. 2019; Wade et al. 2014). Integrating racism into adversity research provides a foundation for understanding how best to address ACEs among Black youth from a clinical and public health perspective. Below, we detail several areas of future consideration that build on a culturally-informed, integrated approach to understanding ACEs among Black youth, particularly with respect to assessment, study design, and intervention and prevention programing research.
Assessment
With the recent proliferation of literature establishing the frequency and deleterious implications of childhood trauma, many have determined the prevalence of ACEs to be a public health crisis that warrants immediate attention (Dube 2018). To this end, several assessment tools have been utilized to assess ACEs (Cronholm et al. 2015; Ellis and Dietz 2017; Felitti et al. 1998; Koita et al. 2018; Mersky et al. 2017; Reuben et al. 2016). However, these assessment tools vary in how they categorize and measure ACEs, with only a few including items relevant to experiences of racial discrimination and other culturally relevant stressors (e.g., community violence). The inconsistent evaluation of such experiences makes it difficult to assess ACEs in a reliable and uniform manner and highlights a broader challenge with respect to how ACEs are operationalized and assessed. More specifically scholars have noted that the inconsistent language, measurement, operationalization, and assessment of ACEs makes it difficult to know how or when to systemically intervene (McLaughlin 2016).
As ACE-related data is directly tied to the creation of state and federal funded policies, programs, and initiatives (Strompolis et al. 2019), there is an immediate need to conceptualize adversity in a consistent and inclusive manner to incorporate considerations of racism and racial trauma, and update ACE-related assessment tools to more comprehensively assess PTEs across racial and ethnic groups. At the time that this paper was written, 17 states have active ACE data being collected, primarily through an 11-item module included within the Behavioral Risk Factor Surveillance System (BRFSS), sponsored by the CDC (CDC 2019). The BRFSS is a large-scale state-based surveillance system that gathers information about targetable risk factors for chronic diseases and other leading causes of death. Notably absent from the ACE module within the BRFSS protocol are any items relevant to racism-related experiences or other PTEs documented within previous expanded ACE measures. These omissions make it difficult to ascertain the prevalence and impact of culturally relevant ACEs among racial and ethnic minority communities, and subsequently limits the possibility for clinical researchers to develop prevention and intervention strategies that can effectively address critical needs.
Study Design
While it has been established that ACEs can significantly affect mental health outcomes across the lifespan, scholarship has indicated that the type and developmental timing of an ACE may dictate the severity of subsequent biopsychosocial dysregulation and may have differential effects at different pubertal stages (Herzog and Schmahl 2018; Luby et al. 2019; Schalinski et al. 2016). Interestingly, the impact of racism-related experiences has been found to evidence similar developmental patterns (Cuevas et al. 2019; Gibbons et al. 2018). Thus, additional prospective work is needed to elucidate how racism-related encounters at the interpersonal and institutional level operate in tandem with other ACEs to uniquely and cumulatively impact mental health across critical developmental stages.
Additionally, while Black youth are more likely to be exposed to affected by ACEs, it is equally important for research to incorporate considerations of resilience into scholarly examinations of adversity. Black youth are not monolithic in their responses to adversity, and as such, it is important to understand individual, community, and contextual factors that may shape both risk and resilience over time. Mixed methods and community-based participatory research approaches represent specific techniques that could more precisely locate unique manifestations of ACEs, while also highlighting culturally relevant mechanisms that promote resilience and healing in the context of adversity among Black youth (e.g., racial identity, racial socialization, activism).
Intervention and Prevention
While there are competing philosophies and evidence as to the importance and benefit of modifying psychological treatment based on patient demographics (Castro et al. 2010; Pieterse 2018; Snipes et al. 2011), it is important to recognize that Black youth are less likely to receive mental health treatment (Kilpatrick et al. 2003a). Even when Black youth do receive treatment, literature has found that they evidence lower treatment completion and poorer treatment outcomes compared to their peers (Weiner et al. 2009). Scholars have hypothesized that these disparities may exist, in part, due to the oversight of culturally specific coping strategies that may assist in navigating stressors pertinent to their daily lived experiences such as racism-related stress and trauma (Metzger et al. 2020). Previous literature has connected the minimization of patient experiences of racial discrimination in therapy to weaker therapeutic alliances, lower treatment satisfaction, and higher rates of drop out (Constantine 2007; Sue et al. 2007). These low rates of treatment engagement and retention are further compounded by the lack of adequate training that clinicians receive to comfortably talk about race and racial discrimination within the clinical context (Cardemil and Battle 2003; Sue et al. 2010). Thus, therapeutic spaces conceptually designed to be a place of safety and refuge may actually be perceived by Black youth as a space of invalidation and discomfort.
Despite this concerning data, formal trainings to assist clinicians in their development of the awareness, knowledge, and skills needed to discuss topics of racism-related stress and trauma within the clinical context remain few and far between. However, the present model suggests that clinicians must be made aware of how the historical mistreatment and marginalization of Black communities within the United States has led to the present day skepticism that Black individuals may hold towards the medical field (Kennedy et al. 2007), and how barriers informed by historical trauma may also inform present day racial disparities in the utilization of healthcare services (Gaskin et al. 2012). This includes the history of medical and societal mistreatment (e.g., Tuskegee Syphilis Study, Henrietta Lacks) that Black communities have and continue to be subjected to, which can be directly linked to disparities that continue to occur across various domains of contemporary society (Magaña et al. 2012; Williams and Rucker 2000). Similarly, clinicians need to be prepared to discuss strategies for adaptively navigating racial discrimination and its potentially traumatic consequences (Anderson et al. 2019; Anyiwo et al. 2020; Metzger et al. 2020; Stevenson 2014) as they work to promote positive mental health trajectories among Black youth.
Concluding Remarks
To date, scholarly examinations of the ACEs framework that consider the significance of racism have been limited in number and in scope. In efforts to address this significant limitation, we provide a culturally informed framework centrally focused on demonstrating the harmful effects of racism across the ACEs pyramid to highlight its deleterious biopsychosocial effects among Black youth. As literature continues to shed light on the traumatic implications of racism-related experiences among Black youth (Anderson et al. 2019; Jernigan and Daniel 2011; Saleem et al. 2019), it is imperative that manifestations of racism be appropriately conceptualized as a unique form of adversity that can have acute and long lasting impacts on mental health trajectories. Consistent with stress proliferation literature (Peters and Massey 1983), our model articulates how behavioral manifestations of racism can be conceptualized as a discrete and amplifying form of adversity among Black youth that can lead to the adoption of health risk behaviors that ultimately inform negative mental health outcomes and increased vulnerability to future ACEs. In alignment with recent research (Neblett 2019), we also highlight the necessity of recognizing how institutional and cultural manifestations of racism inform current social conditions to increase and maintain the disparate rates at which Black youth are exposed to and impacted by adverse events.
The ultimate goal in presenting this model is to validate the lived experiences of Black youth through utilization of a framework commonly used to illustrate the effects of childhood trauma and adversity. Formal integration of racism within the ACEs framework is crucial and brings much needed attention to the need to bolster public health efforts to better comprehend and to more comprehensively assess PTEs among Black youth. Gaining a more accurate and nuanced understanding of the prevalence, impact, and typologies of ACEs that disparately influence Black youth can shed light on targetable areas of intervention at the individual (e.g., adaptive coping strategies), contextual (e.g., community initiatives), and institutional (e.g., equitable health care) level that can disrupt the noxious and lasting effects of adversity. It is our hope that this model adds to the scholarly discourse documenting the profound and potentially traumatic impact of racism on Black youth and guides research efforts aimed at clarifying culturally specific mechanisms of risk and resiliency.
Funding Information
The preparation of this manuscript was partially supported by the National Institute on Mental Health (NIMH) Grant T32MH018869 (MPI CK Danielson, D Kilpatrick). All views and opinions expressed herein are those of the authors and do not necessarily reflect those of the funding agencies or respective institutions.
Compliance with Ethical Standards
Conflict of Interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Footnotes
Consistent with previous research, we use the term “Black” to broadly encompass individuals from the African diaspora who reside in the United States.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Alegria M, Vallas M, Pumariega A. Racial and ethnic disparities in pediatric mental health. Child and Adolescent Psychiatric Clinics of North America. 2010;19(4):759–774. doi: 10.1016/j.chc.2010.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alhusen JL, Bower KM, Epstein E, Sharps P. Racial discrimination and adverse birth outcomes: An integrative review. Journal of Midwifery & Women’s Health. 2016;61(6):707–720. doi: 10.1111/jmwh.12490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvidrez J, Snowden LR, Kaiser DM. The experience of stigma among black mental health consumers. Journal of Health Care for the Poor and Underserved. 2008;19(3):874–893. doi: 10.1353/hpu.0.0058. [DOI] [PubMed] [Google Scholar]
- Anderson RE, Stevenson HC. RECASTing racial stress and trauma: Theorizing the healing potential of racial socialization in families. American Psychologist. 2019;74(1):63–75. doi: 10.1037/amp0000392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson RE, McKenny MC, Stevenson HC. EMBRace: Developing a racial socialization intervention to reduce racial stress and enhance racial coping among black parents and adolescents. Family Process. 2019;58(1):53–67. doi: 10.1111/famp.12412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews AR, Jobe-Shields L, López CM, Metzger IW, de Arellano MAR, Saunders B, Kilpatrick G, D. Polyvictimization, income, and ethnic differences in trauma-related mental health during adolescence. Social Psychiatry and Psychiatric Epidemiology. 2015;50(8):1223–1234. doi: 10.1007/s00127-015-1077-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anyiwo N, Palmer GJ, Garrett JM, Starck JG, Hope EC. Racial and political resistance: An examination of the sociopolitical action of racially marginalized youth. Current Opinion in Psychology. 2020;35:86–91. doi: 10.1016/j.copsyc.2020.03.005. [DOI] [PubMed] [Google Scholar]
- Arpi E, Ferrari F. Preterm birth and behaviour problems in infants and preschool-age children: A review of the recent literature. Developmental Medicine & Child Neurology. 2013;55(9):788–796. doi: 10.1111/dmcn.12142. [DOI] [PubMed] [Google Scholar]
- Assari S, Moghani Lankarani M, Caldwell CH. Discrimination increases suicidal ideation in black adolescents regardless of ethnicity and gender. Behavioral Sciences. 2017;7(4):75. doi: 10.3390/bs7040075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bair AN, Steele JR. Examining the consequences of exposure to racism for the executive functioning of black students. Journal of Experimental Social Psychology. 2010;46(1):127–132. doi: 10.1016/j.jesp.2009.08.016. [DOI] [Google Scholar]
- Bellis MA, Hughes K, Ford K, Rodriguez GR, Sethi D, Passmore J. Life course health consequences and associated annual costs of adverse childhood experiences across Europe and North America: A systematic review and meta-analysis. The Lancet Public Health. 2019;4(10):e517–e528. doi: 10.1016/S2468-2667(19)30145-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berger M, Sarnyai Z. “More than skin deep”: Stress neurobiology and mental health consequences of racial discrimination. Stress. 2015;18(1):1–10. doi: 10.3109/10253890.2014.989204. [DOI] [PubMed] [Google Scholar]
- Blair C, Raver CC. Poverty, stress, and brain development: New directions for prevention and intervention. Academic Pediatrics. 2016;16(3, supplement):S30–S36. doi: 10.1016/j.acap.2016.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowers ME, Yehuda R. Intergenerational transmission of stress in humans. Neuropsychopharmacology. 2016;41(1):232–244. doi: 10.1038/npp.2015.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brave Heart MYH. The historical trauma response among natives and its relationship with substance abuse: A Lakota illustration. Journal of Psychoactive Drugs. 2003;35(1):7–13. doi: 10.1080/02791072.2003.10399988. [DOI] [PubMed] [Google Scholar]
- Brave Heart MYH, DeBruyn LM. The American Indian holocaust: Healing historical unresolved grief. American Indian and Alaska Native Mental Health Research. 1998;8(2):56–78. doi: 10.5820/aian.0802.1998.60. [DOI] [PubMed] [Google Scholar]
- Brockie TN, Dana-Sacco G, Wallen GR, Wilcox HC, Campbell JC. The relationship of adverse childhood experiences to PTSD, depression, poly-drug use and suicide attempt in reservation-based Native American adolescents and young adults. American Journal of Community Psychology. 2015;55(3):411–421. doi: 10.1007/s10464-015-9721-3. [DOI] [PubMed] [Google Scholar]
- Bruner C. ACE, place, race, and poverty: Building hope for children. Academic Pediatrics. 2017;17(7):123–129. doi: 10.1016/j.acap.2017.05.009. [DOI] [PubMed] [Google Scholar]
- Bryant-Davis T, Ocampo C. Racist incident–based trauma. The Counseling Psychologist. 2005;33(4):479–500. doi: 10.1177/0011000005276465. [DOI] [Google Scholar]
- Cardemil EV, Battle CL. Guess who’s coming to therapy? Getting comfortable with conversations about race and ethnicity in psychotherapy. Professional Psychology: Research and Practice. 2003;34(3):278–286. doi: 10.1037/0735-7028.34.3.278. [DOI] [Google Scholar]
- Carter RT. Racism and psychological and emotional injury recognizing and assessing race-based traumatic stress. The Counseling Psychologist. 2007;35(1):13–105. doi: 10.1177/0011000006292033. [DOI] [Google Scholar]
- Carter RT, Kirkinis K, Johnson VE. Relationships between trauma symptoms and race-based traumatic stress. Traumatology. 2020;26(1):11–18. doi: 10.1037/trm0000217. [DOI] [Google Scholar]
- Castro FG, Barrera M, Holleran Steiker LK. Issues and challenges in the design of culturally adapted evidence-based interventions. Annual Review of Clinical Psychology. 2010;6:213–239. doi: 10.1146/annurev-clinpsy-033109-132032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cave L, Cooper MN, Zubrick SR, Shepherd CCJ. Racial discrimination and child and adolescent health in longitudinal studies: A systematic review. Social Science & Medicine. 2020;250:112864. doi: 10.1016/j.socscimed.2020.112864. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (November 5, 2019). Behavioral risk factor surveillance system. https://www.cdc.gov/brfss/index.html
- Centers for Disease Control and Prevention (April 3, 2020a). Preventing adverse childhood experiences. https://www.cdc.gov/violenceprevention/acestudy/fastfact.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fviolenceprevention%2Fchildabuseandneglect%2Faces%2Ffastfact.html
- Centers for Disease Control and Prevention . (April 13, 2020b). About the CDC-Kaiser ACE study. https://www.cdc.gov/violenceprevention/acestudy/about.html
- Christian LM. Psychoneuroimmunology in pregnancy: Immune pathways linking stress with maternal health, adverse birth outcomes, and fetal development. Neuroscience & Biobehavioral Reviews. 2012;36(1):350–361. doi: 10.1016/j.neubiorev.2011.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christian LM, Iams JD, Porter K, Glaser R. Epstein-Barr virus reactivation during pregnancy and postpartum: Effects of race and racial discrimination. Brain, Behavior, and Immunity. 2012;26(8):1280–1287. doi: 10.1016/j.bbi.2012.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans: A biopsychosocial model. American Psychologist. 1999;54(10):805–816. doi: 10.1037/0003-066X.54.10.805. [DOI] [PubMed] [Google Scholar]
- Clark R, Benkert RA, Flack JM. Large arterial elasticity varies as a function of gender and racism-related vigilance in black youth. Journal of Adolescent Health. 2006;39(4):562–569. doi: 10.1016/j.jadohealth.2006.02.012. [DOI] [PubMed] [Google Scholar]
- Constantine MG. Racial microaggressions against African American clients in cross-racial counseling relationships. Journal of Counseling Psychology. 2007;54(1):1–16. doi: 10.1037/0022-0167.54.1.1. [DOI] [Google Scholar]
- Cooper ML, Krull JL, Agocha VB, Flanagan ME, Orcutt HK, Grabe S, Dermen KH, Jackson M. Motivational pathways to alcohol use and abuse among black and white adolescents. Journal of Abnormal Psychology. 2008;117(3):485–501. doi: 10.1037/a0012592. [DOI] [PubMed] [Google Scholar]
- Copeland WE, Keeler G, Angold A, Costello EJ. Traumatic events and posttraumatic stress in childhood. Archives of General Psychiatry. 2007;64(5):577–584. doi: 10.1001/archpsyc.64.5.577. [DOI] [PubMed] [Google Scholar]
- Covelli MM, Wood CE, Yarandi HN. The association of low birth weight and physiological risk factors of hypertension in African American adolescents. Journal of Cardiovascular Nursing. 2007;22(6):440–447. doi: 10.1097/01.JCN.0000297380.06379.d0. [DOI] [PubMed] [Google Scholar]
- Cronholm PF, Forke CM, Wade R, Bair-Merritt MH, Davis M, Harkins-Schwarz M, Pachter LM, Fein JA. Adverse childhood experiences: Expanding the concept of adversity. American Journal of Preventive Medicine. 2015;49(3):354–361. doi: 10.1016/j.amepre.2015.02.001. [DOI] [PubMed] [Google Scholar]
- Cuevas, A. G., Ho, T., Rodgers, J., DeNufrio, D., Alley, L., Allen, J., & Williams, D. R. (2019). Developmental timing of initial racial discrimination exposure is associated with cardiovascular health conditions in adulthood. Ethnicity & Health, 1–14. 10.1080/13557858.2019.1613517. [DOI] [PMC free article] [PubMed]
- Danese A, McEwen BS. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiology & Behavior. 2012;106(1):29–39. doi: 10.1016/j.physbeh.2011.08.019. [DOI] [PubMed] [Google Scholar]
- Darity Jr., W., Hamilton, D., Paul, M., Aja, A., Price, A., Moore, A., & Chiopris, C. (2018). What we get wrong about closing the racial wealth gap. Samuel DuBois Cook Center on Social Equity and Insight Center for Community Economic Development, 1–67.
- Davis EP, Sandman CA. Prenatal exposure to stress and stress hormones influences child development. Infants & Young Children. 2006;19(3):246–259. doi: 10.1097/00001163-200607000-00008. [DOI] [Google Scholar]
- De Coster S, Thompson MS. Race and general strain theory: Microaggressions as mundane extreme environmental stresses. Justice Quarterly. 2017;34(5):903–930. doi: 10.1080/07418825.2016.1236204. [DOI] [Google Scholar]
- Dominguez TP. Race, racism, and racial disparities in adverse birth outcomes. Clinical Obstetrics and Gynecology. 2008;51(2):360–370. doi: 10.1097/GRF.0b013e31816f28de. [DOI] [PubMed] [Google Scholar]
- Dube SR. Continuing conversations about adverse childhood experiences (ACEs) screening: A public health perspective. Child Abuse & Neglect. 2018;85:180–184. doi: 10.1016/j.chiabu.2018.03.007. [DOI] [PubMed] [Google Scholar]
- Elkins J, Briggs HE, Miller KM, Kim I, Orellana R, Mowbray O. Racial/ethnic differences in the impact of adverse childhood experiences on posttraumatic stress disorder in a nationally representative sample of adolescents. Child and Adolescent Social Work Journal. 2019;36(5):449–457. doi: 10.1007/s10560-018-0585-x. [DOI] [Google Scholar]
- Ellis WR, Dietz WH. A new framework for addressing adverse childhood and community experiences: The building community resilience model. Academic Pediatrics. 2017;17(7, Supplement):S86–S93. doi: 10.1016/j.acap.2016.12.011. [DOI] [PubMed] [Google Scholar]
- English D, Lambert SF, Tynes BM, Bowleg L, Zea MC, Howard LC. Daily multidimensional racial discrimination among black US American adolescents. Journal of Applied Developmental Psychology. 2020;66:1–12. doi: 10.1016/j.appdev.2019.101068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Entman, R. M., & Rojecki, A. (2001). The black image in the white mind: Media and race in America. University of Chicago Press.
- Epstein, R., Blake, J., & González, T. (2017). Girlhood interrupted: The erasure of black girls’ childhood. Available at SSRN 3000695. 10.2139/ssrn.3000695.
- Fadus MC, Ginsburg KR, Sobowale K, Halliday-Boykins CA, Bryant BE, Gray KM, Squeglia LM. Unconscious bias and the diagnosis of disruptive behavior disorders and ADHD in African American and Hispanic youth. Academic Psychiatry. 2020;44(1):95–102. doi: 10.1007/s40596-019-01127-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagan AA, Novak A. Adverse childhood experiences and adolescent delinquency in a high-risk sample: A comparison of white and black youth. Youth Violence and Juvenile Justice. 2018;16(4):395–417. doi: 10.1177/1541204017735568. [DOI] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. American Journal of Preventive Medicine. 1998;56(4):245–258. doi: 10.1016/S0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Turner HA, Shattuck A, Hamby SL. Violence, crime, and abuse exposure in a national sample of children and youth: An update. JAMA Pediatrics. 2013;167(7):614–621. doi: 10.1001/jamapediatrics.2013.42. [DOI] [PubMed] [Google Scholar]
- Ford, J. D., & Greene, C. A. (2017). Psychological and biological theories of child and adolescent traumatic stress disorders. In M. A. Landolt, M. Cloitre, & U. Schnyder (Eds.), Evidence-based treatments for trauma related disorders in children and adolescents (pp. 97–117). Springer International Publishing. 10.1007/978-3-319-46138-0_5.
- Gaskin DJ, Dinwiddie GY, Chan KS, McCleary R. Residential segregation and disparities in health care services utilization. Medical Care Research and Review. 2012;69(2):158–175. doi: 10.1177/1077558711420263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus AT, Hicken M, Keene D, Bound J. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. American Journal of Public Health. 2006;96(5):826–833. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons FX, O’Hara RE, Stock ML, Gerrard M, Weng C-Y, Wills TA. The erosive effects of racism: Reduced self-control mediates the relation between perceived racial discrimination and substance use in African American adolescents. Journal of Personality and Social Psychology. 2012;102(5):1089–1104. doi: 10.1037/a0027404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons FX, Fleischli ME, Gerrard M, Simons RL. Reports of perceived racial discrimination among African American children predict negative affect and smoking behavior in adulthood: A sensitive period hypothesis. Development and Psychopathology. 2018;30(5):1629–1647. doi: 10.1017/S0954579418001244. [DOI] [PubMed] [Google Scholar]
- Giladi L, Bell TS. Protective factors for intergenerational transmission of trauma among second and third generation holocaust survivors. Psychological Trauma: Theory, Research, Practice, and Policy. 2013;5(4):384. doi: 10.1037/a0028455. [DOI] [Google Scholar]
- Giscombé CL, Lobel M. Explaining disproportionately high rates of adverse birth outcomes among African Americans: The impact of stress, racism, and related factors in pregnancy. Psychological Bulletin. 2005;131(5):662–683. doi: 10.1037/0033-2909.131.5.662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giurgescu C, McFarlin BL, Lomax J, Craddock C, Albrecht A. Racial discrimination and the black-white gap in adverse birth outcomes: A review. Journal of Midwifery & Women’s Health. 2011;56(4):362–370. doi: 10.1111/j.1542-2011.2011.00034.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goff PA, Jackson MC, Di Leone BAL, Culotta CM, DiTomasso NA. The essence of innocence: Consequences of dehumanizing black children. Journal of Personality and Social Psychology. 2014;106(4):526–545. doi: 10.1037/a0035663. [DOI] [PubMed] [Google Scholar]
- Graves KN, Kaslow NJ, Frabutt JM. A culturally-informed approach to trauma, suicidal behavior, and overt aggression in African American adolescents. Aggression and Violent Behavior. 2010;15(1):36–41. doi: 10.1016/j.avb.2009.07.014. [DOI] [Google Scholar]
- Guinosso SA, Johnson SB, Riley AW. Multiple adverse experiences and child cognitive development. Pediatric Research. 2016;79(1):220–226. doi: 10.1038/pr.2015.195. [DOI] [PubMed] [Google Scholar]
- Harrell CJP. Manichean psychology. Washington, DC: Howard University Press; 1999. [Google Scholar]
- Harrell SP. A multidimensional conceptualization of racism-related stress: Implications for the well-being of people of color. American Journal of Orthopsychiatry. 2000;70(1):42–57. doi: 10.1037/h0087722. [DOI] [PubMed] [Google Scholar]
- Harris A, Evans H, Beckett K. Drawing blood from stones: Legal debt and social inequality in the contemporary United States. American Journal of Sociology. 2010;115(6):1753–1799. doi: 10.1086/651940. [DOI] [Google Scholar]
- Heard-Garris NJ, Cale M, Camaj L, Hamati MC, Dominguez TP. Transmitting trauma: A systematic review of vicarious racism and child health. Social Science & Medicine. 2018;199:230–240. doi: 10.1016/j.socscimed.2017.04.018. [DOI] [PubMed] [Google Scholar]
- Herzog, J. I., & Schmahl, C. (2018). Adverse childhood experiences and the consequences on neurobiological, psychosocial, and somatic conditions across the lifespan. Frontiers in Psychiatry, 9. 10.3389/fpsyt.2018.00420. [DOI] [PMC free article] [PubMed]
- Hicken MT, Lee H, Ailshire J, Burgard SA, Williams DR. “Every shut eye, ain’t sleep”: The role of racism-related vigilance in racial/ethnic disparities in sleep difficulty. Race and Social Problems. 2013;5(2):100–112. doi: 10.1007/s12552-013-9095-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilmert CJ, Dominguez TP, Schetter CD, Srinivas SK, Glynn LM, Hobel CJ, Sandman CA. Lifetime racism and blood pressure changes during pregnancy: Implications for fetal growth. Health Psychology. 2014;33(1):43–51. doi: 10.1037/a0031160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Himmelstein MS, Young DM, Sanchez DT, Jackson JS. Vigilance in the discrimination-stress model for black Americans. Psychology & Health. 2015;30(3):253–267. doi: 10.1080/08870446.2014.966104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, Jones L, Dunne MP. The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. The Lancet Public Health. 2017;2(8):e356–e366. doi: 10.1016/S2468-2667(17)30118-4. [DOI] [PubMed] [Google Scholar]
- Iyengar U, Kim S, Martinez S, Fonagy P, Strathearn L. Unresolved trauma in mothers: Intergenerational effects and the role of reorganization. Frontiers in Psychology. 2014;5:5. doi: 10.3389/fpsyg.2014.00966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janusek LW, Tell D, Gaylord-Harden N, Mathews HL. Relationship of childhood adversity and neighborhood violence to a proinflammatory phenotype in emerging adult African American men: An epigenetic link. Brain, Behavior, and Immunity. 2017;60:126–135. doi: 10.1016/j.bbi.2016.10.006. [DOI] [PubMed] [Google Scholar]
- Jarvis SN, Okonofua JA. School deferred: When bias affects school leaders. Social Psychological and Personality Science. 2020;11(4):492–498. doi: 10.1177/1948550619875150. [DOI] [Google Scholar]
- Jernigan MM, Daniel JH. Racial trauma in the lives of black children and adolescents: Challenges and clinical implications. Journal of Child & Adolescent Trauma. 2011;4(2):123–141. doi: 10.1080/19361521.2011.574678. [DOI] [Google Scholar]
- Jones JM. Prejudice and racism. Reading: Addison-Wesley; 1972. [Google Scholar]
- Jones KP, Peddie CI, Gilrane VL, King EB, Gray AL. Not so subtle: A meta-analytic investigation of the correlates of subtle and overt discrimination. Journal of Management. 2016;42(6):1588–1613. doi: 10.1177/0149206313506466. [DOI] [Google Scholar]
- Jones SCT, Anderson RE, Gaskin-Wasson AL, Sawyer BA, Applewhite K, Metzger IW. From “crib to coffin”: Navigating coping from racism-related stress throughout the lifespan of black Americans. American Journal of Orthopsychiatry. 2020;90(2):267–282. doi: 10.1037/ort0000430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalmakis KA, Chandler GE. Health consequences of adverse childhood experiences: A systematic review. Journal of the American Association of Nurse Practitioners. 2015;27(8):457–465. doi: 10.1002/2327-6924.12215. [DOI] [PubMed] [Google Scholar]
- Kellerman NP. Psychopathology in children of holocaust survivors: A review of the research literature. Israel Journal of Psychiatry and Related Sciences. 2001;38(1):36–46. [PubMed] [Google Scholar]
- Kennedy BR, Mathis CC, Woods AK. African Americans and their distrust of the health care system: Healthcare for diverse populations. Journal of Cultural Diversity. 2007;14(2):56–60. [PubMed] [Google Scholar]
- Kilpatrick DG, Ruggiero KJ, Acierno R, Saunders BE, Resnick HS, Best CL. Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: Results from the National Survey of adolescents. Journal of Consulting and Clinical Psychology. 2003;71(4):692–700. doi: 10.1037/0022-006X.71.4.692. [DOI] [PubMed] [Google Scholar]
- Kilpatrick, D. G., Saunders, B. E., & Smith, D. W. (2003b). Youth victimization: Prevalence and implications. Research in brief. Washington, DC: US Department of Justice, Office of Justice Programs.
- Kirkinis, K., Pieterse, A. L., Martin, C., Agiliga, A., & Brownell, A. (2018). Racism, racial discrimination, and trauma: A systematic review of the social science literature. Ethnicity & Health, 1–21. [DOI] [PubMed]
- Koita K, Long D, Hessler D, Benson M, Daley K, Bucci M, Thakur N, Burke Harris N. Development and implementation of a pediatric adverse childhood experiences (ACEs) and other determinants of health questionnaire in the pediatric medical home: A pilot study. PLoS One. 2018;13(12):1–16. doi: 10.1371/journal.pone.0208088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolchin, P. (2003). American slavery: 1619–1877. Macmillan.
- Lee RD, Chen J. Adverse childhood experiences, mental health, and excessive alcohol use: Examination of race/ethnicity and sex differences. Child Abuse & Neglect. 2017;69:40–48. doi: 10.1016/j.chiabu.2017.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lê-Scherban F, Wang X, Boyle-Steed KH, Pachter LM. Intergenerational associations of parent adverse childhood experiences and child health outcomes. Pediatrics. 2018;141(6):e20174274. doi: 10.1542/peds.2017-4274. [DOI] [PubMed] [Google Scholar]
- Letourneau N, Dewey D, Kaplan BJ, Ntanda H, Novick J, Thomas JC, Deane AJ, Leung B, Pon K, Giesbrecht GF, Team, the Ap. S Intergenerational transmission of adverse childhood experiences via maternal depression and anxiety and moderation by child sex. Journal of Developmental Origins of Health and Disease. 2019;10(1):88–99. doi: 10.1017/S2040174418000648. [DOI] [PubMed] [Google Scholar]
- Liang J, Matheson BE, Douglas JM. Mental health diagnostic considerations in racial/ethnic minority youth. Journal of Child and Family Studies. 2016;25(6):1926–1940. doi: 10.1007/s10826-015-0351-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu SR, Kia-Keating M, Nylund-Gibson K. Patterns of adversity and pathways to health among white, black, and Latinx youth. Child Abuse & Neglect. 2018;86:89–99. doi: 10.1016/j.chiabu.2018.09.007. [DOI] [PubMed] [Google Scholar]
- López CM, Andrews AR, Chisolm AM, de Arellano MA, Saunders B, Kilpatrick DG. Racial/ethnic differences in trauma exposure and mental health disorders in adolescents. Cultural Diversity & Ethnic Minority Psychology. 2017;23(3):382–387. doi: 10.1037/cdp0000126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu MC, Halfon N. Racial and ethnic disparities in birth outcomes: A life-course perspective. Maternal and Child Health Journal. 2003;7(1):13–30. doi: 10.1023/A:1022537516969. [DOI] [PubMed] [Google Scholar]
- Luby JL, Tillman R, Barch DM. Association of timing of adverse childhood experiences and caregiver support with regionally specific brain development in adolescents. JAMA Network Open. 2019;2(9):e1911426–e1911426. doi: 10.1001/jamanetworkopen.2019.11426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magaña S, Parish SL, Rose RA, Timberlake M, Swaine JG. Racial and ethnic disparities in quality of health care among children with autism and other developmental disabilities. Intellectual and Developmental Disabilities. 2012;50(4):287–299. doi: 10.1352/1934-9556-50.4.287. [DOI] [PubMed] [Google Scholar]
- Maguire-Jack, K., Lanier, P., & Lombardi, B. (2019). Investigating racial differences in clusters of adverse childhood experiences. American Journal of Orthopsychiatry. [DOI] [PubMed]
- Mallett CA. Disproportionate minority contact in juvenile justice: Today’s, and yesterdays, problems. Criminal Justice Studies. 2018;31(3):230–248. doi: 10.1080/1478601X.2018.1438276. [DOI] [Google Scholar]
- Matheson K, Foster MD, Bombay A, McQuaid RJ, Anisman H. Traumatic experiences, perceived discrimination, and psychological distress among members of various socially marginalized groups. Frontiers in Psychology. 2019;10:1–16. doi: 10.3389/fpsyg.2019.00416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKeever VM, Huff ME. A diathesis-stress model of posttraumatic stress disorder: Ecological, biological, and residual stress pathways. Review of General Psychology. 2003;7(3):237–250. doi: 10.1037/1089-2680.7.3.237. [DOI] [Google Scholar]
- McLaughlin KA. Future directions in childhood adversity and youth psychopathology. Journal of Clinical Child & Adolescent Psychology. 2016;45(3):361–382. doi: 10.1080/15374416.2015.1110823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendez, L., Mozley, M. M., & Kerig, P. K. (2020). Beyond trauma exposure: Discrimination and posttraumatic stress, internalizing, and externalizing problems among detained youth. Journal of Interpersonal Violence. Advanced online publication. 10.1177/0886260520926314 [DOI] [PubMed]
- Mersky JP, Topitzes J, Reynolds AJ. Impacts of adverse childhood experiences on health, mental health, and substance use in early adulthood: A cohort study of an urban, minority sample in the U.S. Child Abuse & Neglect. 2013;37(11):917–925. doi: 10.1016/j.chiabu.2013.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mersky JP, Janczewski CE, Topitzes J. Rethinking the measurement of adversity: Moving toward second-generation research on adverse childhood experiences. Child Maltreatment. 2017;22(1):58–68. doi: 10.1177/1077559516679513. [DOI] [PubMed] [Google Scholar]
- Metzger, I. W., Anderson, R. E., Are, F., & Ritchwood, T. (2020). Healing interpersonal and racial trauma: Integrating racial socialization into trauma-focused cognitive behavioral therapy for African American youth. Child Maltreatment, 1077559520921457. 10.1177/1077559520921457. [DOI] [PMC free article] [PubMed]
- Meulewaeter, F., De Pauw, S. S. W., & Vanderplasschen, W. (2019). Mothering, substance use disorders and intergenerational trauma transmission: An attachment-based perspective. Frontiers in Psychiatry, 10. 10.3389/fpsyt.2019.00728. [DOI] [PMC free article] [PubMed]
- Miech R, Terry-McElrath YM, O’Malley PM, Johnston LD. Increasing marijuana use for black adolescents in the United States: A test of competing explanations. Addictive Behaviors. 2019;93:59–64. doi: 10.1016/j.addbeh.2019.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohatt NV, Thompson AB, Thai ND, Tebes JK. Historical trauma as public narrative: A conceptual review of how history impacts present-day health. Social Science & Medicine. 2014;106:128–136. doi: 10.1016/j.socscimed.2014.01.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montagna A, Nosarti C. Socio-emotional development following very preterm birth: Pathways to psychopathology. Frontiers in Psychology. 2016;7:1–23. doi: 10.3389/fpsyg.2016.00080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris EW, Perry BL. The punishment gap: School suspension and racial disparities in achievement. Social Problems. 2016;63(1):68–86. doi: 10.1093/socpro/spv026. [DOI] [Google Scholar]
- Neblett EW. Racism and health: Challenges and future directions in behavioral and psychological research. Cultural Diversity and Ethnic Minority Psychology. 2019;25(1):12–20. doi: 10.1037/cdp0000253. [DOI] [PubMed] [Google Scholar]
- Nepomnaschy PA, Welch KB, McConnell DS, Low BS, Strassmann BI, England BG. Cortisol levels and very early pregnancy loss in humans. Proceedings of the National Academy of Sciences. 2006;103(10):3938–3942. doi: 10.1073/pnas.0511183103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nurius PS, Green S, Logan-Greene P, Longhi D, Song C. Stress pathways to health inequalities: Embedding ACEs within social and behavioral contexts. International Public Health Journal. 2016;8(2):241–256. [PMC free article] [PubMed] [Google Scholar]
- Pachter LM, Coll CG. Racism and child health: A review of the literature and future directions. Journal of Developmental and Behavioral Pediatrics : JDBP. 2009;30(3):255–263. doi: 10.1097/DBP.0b013e3181a7ed5a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin LI, Schieman S, Fazio EM, Meersman SC. Stress, health, and the life course: Some conceptual perspectives. Journal of Health and Social Behavior. 2005;46(2):205–219. doi: 10.1177/002214650504600206. [DOI] [PubMed] [Google Scholar]
- Peters MF, Massey G. Mundane extreme environmental stress in family stress theories. Marriage & Family Review. 1983;6(1–2):193–218. doi: 10.1300/J002v06n01_10. [DOI] [Google Scholar]
- Pew Research Center. (2020). 6 facts about economic inequality in the U.S. Pew Research Center. https://www.pewresearch.org/fact-tank/2020/02/07/6-facts-about-economic-inequality-in-the-u-s/
- Pieterse AL. Attending to racial trauma in clinical supervision: Enhancing client and supervisee outcomes. The Clinical Supervisor. 2018;37(1):204–220. doi: 10.1080/07325223.2018.1443304. [DOI] [Google Scholar]
- Pieterse AL, Carter RT, Evans SA, Walter RA. An exploratory examination of the associations among racial and ethnic discrimination, racial climate, and trauma-related symptoms in a college student population. Journal of Counseling Psychology. 2010;57(3):255–263. doi: 10.1037/a0020040. [DOI] [PubMed] [Google Scholar]
- Polanco-Roman L, Danies A, Anglin DM. Racial discrimination as race-based trauma, coping strategies and dissociative symptoms among emerging adults. Psychological Trauma : Theory, Research, Practice and Policy. 2016;8(5):609–617. doi: 10.1037/tra0000125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Priest N, Paradies Y, Trenerry B, Truong M, Karlsen S, Kelly Y. A systematic review of studies examining the relationship between reported racism and health and wellbeing for children and young people. Social Science & Medicine. 2013;95:115–127. doi: 10.1016/j.socscimed.2012.11.031. [DOI] [PubMed] [Google Scholar]
- Racine N, Plamondon A, Madigan S, McDonald S, Tough S. Maternal adverse childhood experiences and infant development. Pediatrics. 2018;141(4):e20172495. doi: 10.1542/peds.2017-2495. [DOI] [PubMed] [Google Scholar]
- Reis FM, Fadalti M, Florio P, Petraglia F. Putative role of placental corticotropin-releasing factor in the mechanisms of human parturition. Journal of the Society for Gynecologic Investigation. 1999;6(3):109–119. doi: 10.1177/107155769900600301. [DOI] [PubMed] [Google Scholar]
- Reuben A, Moffitt TE, Caspi A, Belsky DW, Harrington H, Schroeder F, Hogan S, Ramrakha S, Poulton R, Danese A. Lest we forget: Comparing retrospective and prospective assessments of adverse childhood experiences in the prediction of adult health. Journal of Child Psychology and Psychiatry. 2016;57(10):1103–1112. doi: 10.1111/jcpp.12621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruef M, Fletcher B. Legacies of American slavery: Status attainment among southern blacks after emancipation. Social Forces. 2003;82(2):445–480. doi: 10.1353/sof.2004.0024. [DOI] [Google Scholar]
- Sachs-Ericsson NJ, Rushing NC, Stanley IH, Sheffler J. In my end is my beginning: Developmental trajectories of adverse childhood experiences to late-life suicide. Aging & Mental Health. 2016;20(2):139–165. doi: 10.1080/13607863.2015.1063107. [DOI] [PubMed] [Google Scholar]
- Saleem FT, Anderson RE, Williams M. Addressing the “Myth” of racial trauma: Developmental and ecological considerations for youth of color. Clinical Child and Family Psychology Review. 2019;23:1–14. doi: 10.1007/s10567-019-00304-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schalinski I, Teicher MH, Nischk D, Hinderer E, Müller O, Rockstroh B. Type and timing of adverse childhood experiences differentially affect severity of PTSD, dissociative and depressive symptoms in adult inpatients. BMC Psychiatry. 2016;16(1):295. doi: 10.1186/s12888-016-1004-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scharf M. Long-term effects of trauma: Psychosocial functioning of the second and third generation of holocaust survivors. Development and Psychopathology. 2007;19(2):603–622. doi: 10.1017/S0954579407070290. [DOI] [PubMed] [Google Scholar]
- Simons RL, Chen Y-F, Stewart EA, Brody GH. Incidents of discrimination and risk for delinquency: A longitudinal test of strain theory with an African American sample. Justice Quarterly. 2003;20(4):827–854. doi: 10.1080/07418820300095711. [DOI] [Google Scholar]
- Slaughter-Acey JC, Talley LM, Stevenson HC, Misra DP. Personal versus group experiences of racism and risk of delivering a small-for-gestational age infant in African American women: A life course perspective. Journal of Urban Health. 2019;96(2):181–192. doi: 10.1007/s11524-018-0291-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slopen N, Shonkoff JP, Albert MA, Yoshikawa H, Jacobs A, Stoltz R, Williams DR. Racial disparities in child adversity in the U.S.: Interactions with family immigration history and income. American Journal of Preventive Medicine. 2016;50(1):47–56. doi: 10.1016/j.amepre.2015.06.013. [DOI] [PubMed] [Google Scholar]
- Smiley C, Fakunle D. From “brute” to “thug:” the demonization and criminalization of unarmed black male victims in America. Journal of Human Behavior in the Social Environment. 2016;26(3–4):350–366. doi: 10.1080/10911359.2015.1129256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snipes SA, Sellers SL, Tafawa AO, Cooper LA, Fields JC, Bonham VL. Is race medically relevant? A qualitative study of physicians’ attitudes about the role of race in treatment decision-making. BMC Health Services Research. 2011;11(1):183. doi: 10.1186/1472-6963-11-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sotero M. A conceptual model of historical trauma: Implications for public health practice and research. Journal of Health Disparities Research and Practice. 2006;1(1):93–108. doi: 10.1542/peds.2009-1100E. [DOI] [Google Scholar]
- Stevenson, H. (2014). Promoting racial literacy in schools: Differences that make a difference. Teachers College Press.
- Strompolis M, Tucker W, Crouch E, Radcliff E. The intersectionality of adverse childhood experiences, race/ethnicity, and income: Implications for policy. Journal of Prevention & Intervention in the Community. 2019;47(4):310–324. doi: 10.1080/10852352.2019.1617387. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2017). Understanding child trauma [Text]. https://www.samhsa.gov/child-trauma/understanding-child-trauma
- Sue DW, Capodilupo CM, Torino GC, Bucceri JM, Holder AMB, Nadal KL, Esquilin M. Racial microaggressions in everyday life: Implications for clinical practice. American Psychologist. 2007;62(4):271–286. doi: 10.1037/0003-066X.62.4.271. [DOI] [PubMed] [Google Scholar]
- Sue DW, Rivera DP, Capodilupo CM, Lin AI, Torino GC. Racial dialogues and white trainee fears: Implications for education and training. Cultural Diversity and Ethnic Minority Psychology. 2010;16(2):206–214. doi: 10.1037/a0016112. [DOI] [PubMed] [Google Scholar]
- Sykes BL, Pettit B. Mass incarceration, family complexity, and the reproduction of childhood disadvantage. The Annals of the American Academy of Political and Social Science. 2014;654(1):127–149. doi: 10.1177/0002716214526345. [DOI] [Google Scholar]
- Thomas M, Herring C, Horton HD, Semyonov M, Henderson L, Mason PL. Race and the accumulation of wealth: Racial differences in net worth over the life course, 1989–2009. Social Problems. 2020;67(1):20–39. doi: 10.1093/socpro/spz002. [DOI] [Google Scholar]
- Tynes BM, Willis HA, Stewart AM, Hamilton MW. Race-related traumatic events online and mental health among adolescents of color. Journal of Adolescent Health. 2019;65(3):371–377. doi: 10.1016/j.jadohealth.2019.03.006. [DOI] [PubMed] [Google Scholar]
- Wade R, Shea JA, Rubin D, Wood J. Adverse childhood experiences of low-income urban youth. Pediatrics. 2014;134(1):e13–e20. doi: 10.1542/peds.2013-2475. [DOI] [PubMed] [Google Scholar]
- Wamser-Nanney, R., Cherry, K. E., Campbell, C., & Trombetta, E. (2018). Racial differences in children’s trauma symptoms following complex trauma exposure. Journal of Interpersonal Violence, 1–23. 10.1177/0886260518760019. [DOI] [PubMed]
- Wang Y, Nerwen R, Gabris C. Addressing adverse childhood experiences in diverse racial and ethnic settings: A review. Current Opinion in Pediatrics. 2019;31(2):284–289. doi: 10.1097/MOP.0000000000000748. [DOI] [PubMed] [Google Scholar]
- Weiner DA, Schneider A, Lyons JS. Evidence-based treatments for trauma among culturally diverse foster care youth: Treatment retention and outcomes. Children and Youth Services Review. 2009;31(11):1199–1205. doi: 10.1016/j.childyouth.2009.08.013. [DOI] [Google Scholar]
- Williams DR. Stress and the mental health of populations of color: Advancing our understanding of race-related stressors. Journal of Health and Social Behavior. 2018;59(4):466–485. doi: 10.1177/0022146518814251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Collins C. Racial residential segregation: A fundamental cause of racial disparities in health. Public Health Reports. 2001;116(5):404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Mohammed SA. Discrimination and racial disparities in health: Evidence and needed research. Journal of Behavioral Medicine. 2009;32(1):20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Mohammed SA. Racism and health I: Pathways and scientific evidence. American Behavioral Scientist. 2013;57(8):1152–1173. doi: 10.1177/0002764213487340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Rucker TD. Understanding and addressing racial disparities in health care. Health Care Financing Review. 2000;21(4):75–90. [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Williams-Morris R. Racism and mental health: The African American experience. Ethnicity & Health. 2000;5(3–4):243–268. doi: 10.1080/713667453. [DOI] [PubMed] [Google Scholar]
- Williams MT, Metzger IW, Leins C, DeLapp C. Assessing racial trauma within a DSM–5 framework: The UConn racial/ethnic stress & trauma survey. Practice Innovations. 2018;3(4):242–260. doi: 10.1037/pri0000076. [DOI] [Google Scholar]
- Williams DR, Lawrence JA, Davis BA. Racism and health: Evidence and needed research. Annual Review of Public Health. 2019;40:105–125. doi: 10.1146/annurev-publhealth-040218-043750. [DOI] [PMC free article] [PubMed] [Google Scholar]