Abstract
Background
Patient-reported outcomes (PROs) are increasingly relevant endpoints in clinical trials, contributing to our understanding of risk–benefit profiles, in addition to efficacy and safety data. We investigated the impact of entrectinib on patient-reported symptoms, functioning, and health-related quality of life.
Patients and methods
STARTRK-2 is a phase II basket study in patients with locally advanced/metastatic neurotrophic receptor tyrosine kinase 1/2/3 (NTRK1/2/3) and ROS proto-oncogene 1 (ROS1) fusion-positive solid tumours. PROs (prespecified secondary endpoint) were evaluated using the European Organization for Research and Treatment of Cancer quality-of-life questionnaire (QLQ-C30), lung cancer module (QLQ-LC13), and colorectal cancer module (QLQ-CR29), and the EuroQoL 5-Dimension 3-Level instruments, completed before cycle 1 day 1 and each subsequent 4-week cycle of entrectinib dosing, and the end of treatment. Adverse events and treatment-related symptoms were assessed in the safety analysis (SA)-PRO population. Tumour-related symptoms, functioning, and global health status were assessed in the efficacy analysis (EA)-PRO population. Data cut-offs: 31 October 2018 NTRK cohort; 01 May 2019 ROS1 cohort.
Results
SA-PRO populations comprised patients with NTRK fusion-positive solid tumours (N = 88) or ROS1 fusion-positive non-small-cell lung cancer (N = 180) who received one or more doses of entrectinib, completed PRO questionnaires on cycle 1 day 1 and answered one or more questions on-study. EA-PRO populations (N = 71) and (N = 145), respectively, comprised SA-PRO patients with measurable baseline disease. Moderate-to-high baseline global health status scores were maintained in EA-PRO populations during treatment. Role and physical functioning scores were moderate-to-high at baseline, with trends towards clinical improvement during treatment. Both cohorts reported low-to-moderate symptom burden at baseline, which was maintained or trended towards clinically meaningful improvement. Symptoms commonly associated with cancer treatment (e.g. nausea, fatigue) remained stable or improved during treatment. All SA-PRO patients experienced one or more adverse events, most frequently constipation or diarrhoea.
Conclusions
PRO findings were consistent with the favourable safety profile of entrectinib, and further reinforce the positive benefit–risk profile of this treatment, indicating minimal overall treatment burden.
Key words: entrectinib, NTRK, patient-reported outcomes, ROS1, tyrosine kinase inhibitor
Highlights
-
•
During treatment, moderate-to-high baseline functioning and health-related quality-of-life scores were improved/maintained.
-
•
Low-to-moderate tumour-related symptom burden remained stable or trended towards clinical improvement, relative to baseline.
-
•
Notably there was a rapid and sustained clinically meaningful improvement in cough in patients with non-small-cell lung cancer.
-
•
Treatment-related symptoms remained stable or improved; common treatment-related symptoms were absent or low severity.
-
•
PRO data reinforce the positive benefit–risk profile of entrectinib and demonstrate a minimal overall treatment burden.
Introduction
Neurotrophic receptor tyrosine kinase (NTRK) and ROS proto-oncogene 1 (ROS1) gene fusions are known oncogenic drivers across a range of tumour types,1 which result in constitutively active kinase activity.2,3 The European Society for Medical Oncology recommends NTRK testing in advanced solid cancers and ROS1 testing in advanced non-squamous non-small-cell lung cancer (NSCLC).4,5 Entrectinib is an orally available, potent inhibitor of tropomyosin receptor kinase A/B/C, ROS1, and anaplastic lymphoma kinase (ALK).6,7 In an integrated analysis of three clinical trials (ALKA-372-001 [EudraCT, 2012–000148–88], STARTRK-1 [NCT2097810], and STARTRK-2 [NCT02568267]), entrectinib demonstrated clinically meaningful efficacy for locally advanced/metastatic NTRK fusion-positive solid tumours [63.5% objective response rate (ORR), N = 74] and ROS1 fusion-positive NSCLC (67.1% ORR, N = 161), with a manageable and favourable safety and tolerability profile.8,9
As a complement to traditional outcomes of efficacy and tolerability, patient-reported outcomes (PROs) regarding symptoms and their functional impact on daily activities and health-related quality of life (HRQoL) are gaining increasing recognition as important clinical trial endpoints.10 Appropriate consideration of PROs allows for a more comprehensive assessment of an agent's benefit–risk profile by more fully integrating patients' perspectives, and ensuring treatment benefit is not outweighed by unacceptable tolerability and reduced HRQoL.11 To provide information on the overall treatment burden associated with entrectinib, we investigated the impact of treatment on patient-reported symptoms, functioning, and HRQoL in the STARTRK-2 study.
PROs were assessed using the core European Organisation for Research and Treatment of Cancer (EORTC) QoL instrument (QLQ-C30),12 which is a widely used HRQoL questionnaire that assesses global health status (GHS), important functioning domains, and common cancer-associated symptoms, as well as two additional supplements, which were EORTC QLQ-LC13 (lung cancer module)13 and EORTC QLQ-CR29 [colorectal cancer (CRC) module].14 The International Consortium for Health Outcomes Measurement has selected EORTC QLQ-C30, QLQ-CR29, and QLQ-LC13 as standard tools for assessing PROs as outcome indicators for patients with cancer, CRC, and lung cancer, respectively.15
Materials and methods
Patients and study design
The design of STARTRK-2, an open-label phase II basket study, has been reported previously,8,9 and is outlined in more detail in the Supplementary Appendix, available at https://doi.org/10.1016/j.esmoop.2021.100113. Briefly, this study included patients with locally advanced/metastatic solid tumours harbouring an NTRK1/2/3, ROS1, or ALK gene fusion who received oral entrectinib 600 mg once daily in 4-week cycles. Patients with ALK fusion-positive solid tumours were enrolled; however, this arm was discontinued and therefore these data are not included in this analysis.
Safety assessments
Safety was assessed by physical examination, laboratory tests, monitoring of adverse events (AEs), and clinic visits. AEs were coded using the Medical Dictionary for Regulatory Activities (version 14.0 or higher for individual studies; version 21.0 for the integrated safety analysis) and graded using the National Cancer Institute Common Terminology Criteria for Adverse Events (version 4.03).
PRO assessments
PROs were prespecified secondary endpoints, evaluated in all enrolled patients who completed questionnaires on electronic devices before entrectinib dosing on day 1 of every 4-week cycle starting at cycle 1, and at the end of treatment. These included the EuroQoL Group 5-Dimension 3-Level version (EQ-5D-3L) (assesses health resource utilisation; results not included in this publication) and QLQ-C30, which includes 30 questions and comprises five functional scales, three symptom scales, a GHS/QoL scale, and six single items. The QLQ-LC13 module includes 13 questions assessing lung cancer-specific symptoms, while the QLQ-CR29 module includes 29 questions assessing CRC-specific symptoms (Supplementary Table S1, available at https://doi.org/10.1016/j.esmoop.2021.100113).
Statistical analysis
The safety analysis (SA) population included all enrolled patients who received one or more doses of entrectinib. The efficacy analysis (EA) population comprised all patients with measurable baseline disease (by investigator) who received one or more doses of entrectinib. The PRO populations comprised all patients in the EA (EA-PRO population) or the SA (SA-PRO population) populations who completed QLQ-C30 on cycle 1 day 1 and answered one or more questions on an on-study time point thereafter. For NSCLC or CRC baskets, the PRO populations included patients who also completed QLQ-LC13 or QLQ-CR29, respectively, on cycle 1 day 1 and answered one or more questions on an on-study time point thereafter, in addition to QLQ-C30. Analyses of QLQ-C30, QLQ-LC13, and QLQ-CR29 scores were conducted in the EA-PRO population to assess common tumour-related symptoms, functioning, and GHS/QoL. Analyses of QLQ-C30 treatment-related symptoms were conducted in the SA-PRO population. The threshold for data evaluation was ≥25% of the SA-PRO or EA-PRO populations remaining enrolled and participating in the PRO questionnaires, in order to optimise the generalisability of the results. PRO data were summarised with descriptive statistics. Select symptom scales (or single items if there is only one item for that scale) were prespecified for analysis based on their relevance to entrectinib treatment and tumour types evaluated.
PROs were scored according to the developers' scoring manual. All scales and single-item measures were linearly transformed to a score range of 0-100. High scores on functional/GHS scales represent a high level of functioning and high HRQoL, respectively. Conversely, high symptom scores represent greater symptomatology severity. PRO scores are also presented here in comparison to EORTC reference data from the general adult population and patients with NSCLC, as appropriate, to define low, moderate, or high categorisation of scores.16 For multi-item subscales, if ≤50% of items were missing at a time point, the multi-item score was calculated on the basis of non-missing items. If >50% of items were missing/a single-item measure was missing, the subscale was considered missing. Interpreting scores was based on the subjective significance questionnaire developed by Osoba et al.17 which assessed patients' perceptions of changes. Patients who reported ‘a little’ change for better or worse on a particular scale had QLQ-C30 changes ~5-10. Those reporting ‘moderate’ change had changes ~10-20, and ‘very much’ corresponded to a change >20. A ≥10-point change in a score was therefore the threshold for clinical meaningfulness.17
Ethical approval and consent to participate
The trial was conducted in accordance with Good Clinical Practice guidelines and the provisions of the Declaration of Helsinki. All patients provided written informed consent. An independent data and safety monitoring committee reviewed safety data regularly. Protocol approval was obtained from an independent ethics committee at each site.
Results
Patients
Enrolment and data cut-offs were 30 April 2018 and 31 October 2018, respectively, for the NTRK fusion-positive cohort and 31 October 2018 and 01 May 2019, respectively, for the ROS1 fusion-positive cohort (STARTRK-2 enrolment ongoing at time of reporting). The SA-PRO population (N = 268) comprised 88 patients with locally advanced/metastatic NTRK fusion-positive solid tumours and 180 patients with locally advanced/metastatic ROS1 fusion-positive NSCLC. The EA-PRO population (N = 216) comprised 71 patients with locally advanced/metastatic NTRK fusion-positive solid tumours and 145 patients with locally advanced/metastatic ROS1 fusion-positive NSCLC (Supplementary Figure S1, available at https://doi.org/10.1016/j.esmoop.2021.100113). Baseline patient characteristics are summarised in Supplementary Tables S2 and S3, available at https://doi.org/10.1016/j.esmoop.2021.100113. A threshold of ≥25% of enrolled patients responding to the questionnaire determined the number of cycles included in subsequent analyses. Questionnaire completion rates, which represent patients providing data amongst those expected to complete the questionnaire at each time point (patients who had progressed were removed from the denominator), were high at baseline for the ROS1 SA-PRO and EA-PRO populations (97.8%-97.9%), and remained high until the latest cycle included in analyses (cycle 18: 90.2%-90.7%). For the NTRK SA-PRO and EA-PRO populations, baseline completion rates were high (85.7%-100.0%) and decreased slightly by the latest cycle included in analyses (cycle 12/13: 68.8%-80.0%).
Using normative scores of the EORTC from the general adult population as a reference,16 patients in the NTRK and ROS1 EA-PRO populations (N = 88, N = 145, respectively) reported moderate-to-high QLQ-C30 GHS/QoL and functioning at baseline, with slightly higher scores for the NTRK EA-PRO population (baseline scores: GHS/QoL 68.6; physical functioning 74.8; role functioning 66.9; cognitive functioning 83.9) versus the ROS1 EA-PRO population (baseline scores: GHS/QoL 56.0; physical functioning 71.5; role functioning 62.4; cognitive functioning 82.8) (Table 1). Baseline treatment-related symptom scores (QLQ-C30) and tumour-related symptom scores (QLQ-LC13) were lower or comparable with normed scores for patients with NSCLC16 (Table 1).
Table 1.
Mean baseline scores and mean change from baseline in global health status, functioning (based on QLQ-C30), and tumour-related symptom severity (based on QLQ-LC13 and QLQ-CR29), in the NTRK EA-PRO population (N = 71) and ROS1 EA-PRO population (N = 145), and treatment-related symptom severity (based on QLQ-C30) in the NTRK SA-PRO population (N = 88) and ROS1 SA-PRO population (N = 180)
| QLQ-C30 functioning scales |
NTRK fusion-positive solid tumours |
ROS1 fusion-positive NSCLC |
||||
|---|---|---|---|---|---|---|
|
NTRK EA-PRO population (N = 71) |
ROS1 EA-PRO population (N = 145) |
|||||
| BL score (n = 65) | Change from BL, C13a (n = 19) | Change from BL, range (C2–13a) | BL score (n = 142) | Change from BL, C18a (n = 37) | Change from BL, range (C2–18a) | |
| GHS/QoL | 68.6 | +5.3 | +5.3 to −4.4 | 56.0 | +4.1 | +11.3 to +3.8 |
| Physical functioning | 74.8 | +6.3 | +7.7 to −0.4 | 71.5 | +5.7 | +8.8 to +1.6 |
| Role functioning | 66.9 | +12.3 | +16.0 to −0.6 | 62.4 | +3.6 | +10.3 to 0.0 |
| Cognitive functioning | 83.9 | 0.00 | +0.8 to −7.6 | 82.8 | −7.7 | −3.8 to −10.8 |
| QLQ-LC13 tumour-related symptom scales |
NTRK NSCLC EA-PRO population (N = 12) |
ROS1 NSCLC EA-PRO population (N = 145) |
||||
|---|---|---|---|---|---|---|
| BL score (n = 12) | Change from BL, C13a (n = 3) | Change from BL, range (C2–13a) | BL score (n = 140) | Change from BL, C18a (n = 36) | Change from BL, range (C2–18a) | |
| Coughing | 38.9 | −11.1 | 0.0 to −16.7 | 38.6 | −24.1 | −13.6 to −24.1 |
| Chest pain | 5.6 | 0.0 | +16.7 to −8.3 | 18.6 | −3.7 | −2.2 to −12.5 |
| Dyspnoea | 26.9 | −7.4 | +9.3 to −7.4 | 32.3 | −6.2 | −3.6 to −10.3 |
| Arm/shoulder pain | 27.8 | −22.2 | −5.6 to −25.9 | 18.6 | −5.6 | −2.3 to −11.6 |
| Pain in other parts | 33.3 | +11.1 | +16.7 to −18.5 | 24.9b | −1.9c | +2.2 to −9.2 |
| Peripheral neuropathy | 13.9 | 0.0 | +22.2 to 0.0 | 14.1 | 0.0 | +8.7 to 0.0 |
| Dysphagia | 2.8 | 0.0 | +12.1 to 0.0 | 7.1 | +5.6 | +10.8 to +5.0 |
| QLQ-CR29 tumour-related symptom scales |
NTRK CRC EA-PRO population (N = 7) |
||
|---|---|---|---|
| BL score (n = 6) | Change from BL, C6a (n = 2) | Change from BL, range (C2–6a) | |
| Abdominal pain | 27.8 | +16.7 | +16.7 to −8.3 |
| Bloating | 33.3 | +50.0 | +50.0 to −16.7 |
| Stool frequency | 13.9 | 0.0 | +12.5 to −4.2 |
| QLQ-C30 treatment-related symptom scales |
NTRK SA-PRO population (N = 88) |
ROS1 SA-PRO population (N = 180) |
||||
|---|---|---|---|---|---|---|
| BL score (n = 82) | Change from BL, C12a (n = 22) | Change from BL, range (C2–12a) | BL score (n = 176) | Change from BL, C18a (n = 49) | Change from BL, range (C2–18a) | |
| Fatigue | 37.8 | −13.6 | +0.2 to −13.6 | 39.0 | −11.8 | −3.1 to −11.8 |
| Nausea/vomiting | 6.9 | −1.5 | +2.6 to −3.8 | 10.8 | −6.8 | −3.2 to −7.5 |
| Insomnia | 28.1 | −9.1 | −4.8 to −14.1 | 32.0 | −15.0 | −11.8 to −20.4 |
| Appetite loss | 21.1 | −18.2 | −10.0 to −18.2 | 28.0 | −15.7 | −14.3 to −22.2 |
| Constipation | 16.3 | −6.1 | +16.7 to −6.1 | 16.7 | +11.6 | +22.2 to +8.3 |
| Diarrhoea | 8.9 | +13.6 | +13.6 to +3.2 | 7.4 | +10.2 | +13.4 to +6.1 |
All scores are mean or mean change from baseline. Scores range from 0 to 100. For functioning and GHS/QoL, higher score = better HRQoL and function (improvement). For a treatment-related or tumour-related symptom scale/item, however, lower score = lower symptom severity (improvement). A ≥10-point change in score is the threshold for clinical meaningfulness.
BL, baseline; C2, cycle 2 day 1; C6, cycle 6 day 1; C13, cycle 13 day 1; C18, cycle 18 day 1; CRC, colorectal cancer; EA, efficacy analysis; GHS, global health status; NSCLC, non-small-cell lung cancer; NTRK, neurotrophic receptor tyrosine kinase; PRO, patient-reported outcomes; QoL, quality of life; ROS1, ROS proto-oncogene 1; SA, safety analysis.
Cycle shown represents when ≥25% of the population (either the EA-PRO or SA-PRO) remained in the study.
n = 139.
n = 35.
PROs in patients with NTRK fusion-positive solid tumours
Median treatment duration in the NTRK EA population (N = 71) was 8.5 months. According to the QLQ-C30, the EA-PRO population maintained a high baseline GHS/QoL [68.6; mean change from baseline range: +5.3 to −4.4 (Table 1; Figure 1A)] as well as a high baseline physical functioning score (74.8; mean change from baseline: +7.7 to −0.4) during treatment (Table 1, Figure 2A). Notably, while there was a moderate baseline role functioning score (66.9), this reached a clinically meaningful improvement by cycle 10 day 1, which was maintained until cycle 13 day 1 [mean change from baseline: +12.3 (Table 1, Figure 2A)]. Cognitive functioning was maintained at or just below the high baseline level of 83.9 [mean change from baseline: +0.8 to −7.6 (Table 1, Figure 2A)].
Figure 1.
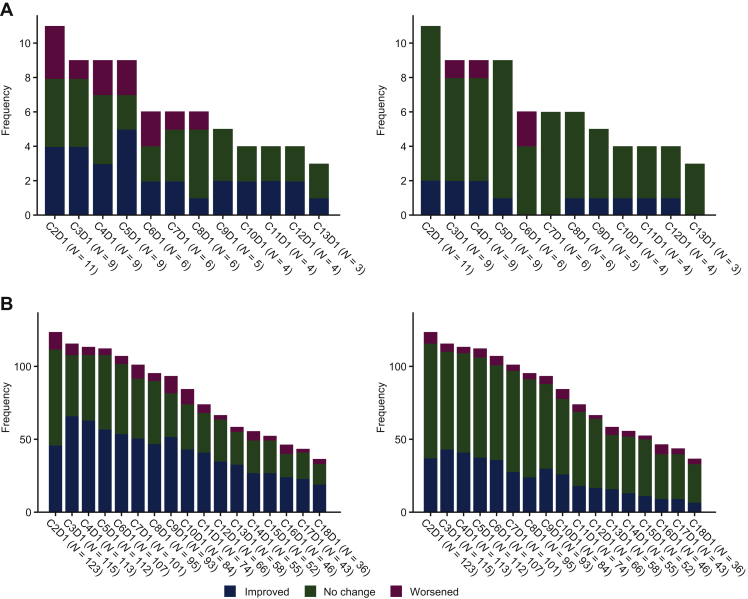
Mean change (with 95% CI) from baseline in global health status (left) and proportion of patients with clinically meaningful change in global health status (right) based on QLQ-C30 in the EA-PRO population with (A) NTRK fusion-positive solid tumours (N = 71) and (B) ROS1 fusion-positive NSCLC (N = 145).
Scores range from 0 to 100. A high score for the GHS/QoL scale represents a high QoL. A ≥10-point change in score is the threshold for clinical meaningfulness. Only visits with three or more patients are included.
C, cycle; CI, confidence interval; D, day; EA, efficacy analysis; GHS, global health status; NSCLC, non-small-cell lung cancer; NTRK, neurotrophic receptor tyrosine kinase; PRO, patient-reported outcomes; QoL, quality of life; ROS1, ROS proto-oncogene 1.
Figure 2.
Mean change from baseline in cognitive, physical, and role functioning scores based on QLQ-C30 in the EA-PRO population with (A) NTRK fusion-positive solid tumours (N = 71) and (B) ROS1 fusion-positive NSCLC (N = 145).
Scores range from 0 to 100. A high score for functional scales represents a high/healthy level of functioning. A ≥10-point change in score is the threshold for clinical meaningfulness. Only visits with three or more patients are included.
C, cycle; D, day; EA, efficacy analysis; NSCLC, non-small-cell lung cancer; NTRK, neurotrophic receptor tyrosine kinase; PRO, patient-reported outcomes; ROS1, ROS proto-oncogene 1.
The NTRK NSCLC EA-PRO population (n = 12) had a median treatment duration of 7.9 months. Based on the QLQ-LC13, a moderate-to-low baseline tumour-related symptom burden was unchanged or improved throughout treatment (Table 1). There was a low mean baseline score for chest pain (5.6) that remained stable (one exception at cycle 6 day 1: +16.7 mean change from baseline), while dyspnoea remained stable throughout, from a low baseline mean score of 26.9. Cough had a moderate baseline mean score (38.9) with clinically meaningful improvements in symptom severity from cycle 3 day 1 (Figure 3A; mean change from baseline: −14.8), which was maintained at cycle 13 day 1 (mean change from baseline: −11.1). The NTRK CRC EA-PRO population (n = 6), had median treatment duration of 4.2 months. Based on the QLQ-CR29, CRC-associated symptom severity (n = 7, including one patient with neuroendocrine colon cancer) generally remained unchanged or improved over time, in particular bloating, blood/mucus in stool, buttock pain, dyspareunia, dysuria, faecal incontinence, and flatulence (data not shown).
Figure 3.
Proportion of patients with clinically meaningful changes from baseline in selected tumour-related symptoms based on QLQ-LC13 in the EA-PRO population with (A) NTRK fusion-positive NSCLC [coughing (left), pain in chest (right); N = 12] and (B) ROS1 fusion-positive NSCLC [coughing (left), pain in chest (right); N = 145].
Scores range from 0 to 100. A high score for a tumour-related symptom scale/item represents a high level of symptomatology. A ≥10-point change in score is the threshold for clinical meaningfulness. Only visits with three or more patients are included.
C, cycle; D, day; EA, efficacy analysis; NSCLC, non-small-cell lung cancer; NTRK, neurotrophic receptor tyrosine kinase; PRO, patient-reported outcomes; ROS1, ROS proto-oncogene 1.
Patients in the NTRK SA-PRO population (N = 88) reported rapid and durable clinically meaningful improvements in some QLQ-C30 treatment-related symptom scores, where improvements exceeded the clinically meaningful threshold at cycle 12 day 1 for both fatigue and appetite loss. With the exception of diarrhoea, other key treatment-related symptoms, including nausea, insomnia, and constipation, remained stable (Table 1). Based on QLQ-C30 and QLQ-LC13, in the NTRK SA-PRO population (N = 88) the high proportion of patients reporting treatment-related symptoms ‘not at all’ in the past week remained stable or increased for most symptoms, with no reports of ‘very much’ for any symptom at cycle 12 day 1. The exception was a trend towards decreased reports in the ‘not at all’ category and increased reports in the ‘a little’ category for diarrhoea, constipation, and peripheral neuropathy (Supplementary Table S4, available at https://doi.org/10.1016/j.esmoop.2021.100113).
PROs in patients with ROS1 fusion-positive NSCLC
Patients in the ROS1 EA population (N = 145) had a median treatment duration of 10.4 months. Based on the QLQ-C30, the EA-PRO population maintained or improved both the moderate baseline GHS/QoL score [56.0; mean change from baseline range: +11.3 to +3.8 (Table 1, Figure 1B)] and moderate baseline role functioning score (62.4; mean change from baseline range: +10.3 to 0.0). A high physical functioning baseline score (71.5) was maintained at most study visits, with a trend towards clinical improvement (Table 1, Figure 2B). A high baseline cognitive functioning score of 82.8 also remained stable throughout, with the exception of cycle 14 [worst mean change score from baseline: −10.8 at cycle 14 day 1 (Table 1, Figure 2B)].
According to the QLQ-LC13, the ROS1 EA-PRO population (N = 145) reported a low-to-moderate tumour-related symptom burden which remained stable or improved throughout. Coughing had a moderate baseline score (38.6), with an immediate clinically meaningful marked improvement (mean change in score from baseline: −13.6 at cycle 2 day 1), sustained throughout [mean change from baseline: −24.1 at cycle 18 day 1 (Table 1, Figure 3B)]. A low baseline chest pain score (18.6) improved or remained stable throughout treatment, including an early clinically meaningful improvement [mean change from baseline: −12.5 at cycle 3 day 1, sustained until cycle 6 day 1: −10.6 (Table 1, Figure 3B)]. Dyspnoea had a moderate baseline score, with a consistent trend towards improvement during treatment, while peripheral neuropathy and dysphagia had low baseline scores, which remained stable with a trend towards worsening in severity (Table 1).
Based on the QLQ-C30, the ROS1 SA-PRO population (N = 180) in general reported a stable or improved low-to-moderate treatment-related symptom burden (Table 1). Fatigue had a moderate baseline score of 39.0, which remained stable with a trend towards improvement. Appetite loss (baseline: 28.0) and insomnia (baseline: 32.0) had immediate marked clinically meaningful improvements (mean changes from baseline: −14.3 and −11.8, respectively, at cycle 2 day 1), which were maintained at cycle 18 day 1 (mean changes from baseline: −15.7 and −15.0, respectively). A low baseline nausea symptom score was maintained during treatment. Constipation (baseline score: 16.7) demonstrated a sustained clinically meaningful worsening over time, while the low baseline diarrhoea score (7.4) remained stable until cycle 9 day 1 before clinically meaningful symptom worsening until cycle 18 day 1 (Table 1). Based on QLQ-C30 and QLQ-LC13, in the ROS1 SA-PRO population (N = 180 and N = 145, respectively), the high proportion of patients at baseline reporting treatment-related symptoms ‘not at all’ in the past week generally remained stable, or increased by cycle 18 day 1 (including appetite loss, nausea, vomiting, trouble sleeping, tingling hands and feet, sore mouth). Reports remained stable or decreased for ‘quite a bit’, and ‘very much’ at cycle 18 day 1 for these symptoms. The exceptions were constipation, diarrhoea, and hair loss, which had decreased reports of ‘not at all’ by cycle 18 day 1 (Supplementary Table S4, available at https://doi.org/10.1016/j.esmoop.2021.100113).
Safety
All patients in the SA-PRO populations experienced at least one AE; the most frequently reported AEs (any grade) associated with QoL impairment were constipation (45.5% of the NTRK SA-PRO population and 52.2% of the ROS1 SA-PRO population), diarrhoea (38.6% and 40.0%, respectively), nausea (25.0% and 31.1%, respectively), and dyspnoea (25.0% and 31.7%, respectively). Treatment-related AEs leading to discontinuations occurred in 4.5% of the NTRK SA-PRO population and 5.6% of the ROS1 SA-PRO population. There were generally no notable differences in the AE profile between the NTRK and ROS1 SA-PRO populations (Table 2).
Table 2.
Summary of safety in the NTRK and ROS1 SA-PRO population
| Patients, n (%) | NTRK fusion-positive solid tumours (N = 88) | ROS1 fusion-positive NSCLC (N = 180) |
|---|---|---|
| Median, months (range) | 14.7 (0.1a-29.7) | 16.8 (0.1a-37.8) |
| Patients with at least one | ||
| AE | 88 (100.0) | 180 (100.0) |
| Grade ≥3 AE | 66 (75.0) | 120 (66.7) |
| Serious AE | 46 (52.3) | 75 (41.7) |
| TRAEs ≥grade 3 | 35 (39.8) | 68 (37.8) |
| TRAEs leading to dose reduction | 28 (31.8) | 54 (30.0) |
| TRAEs leading to discontinuation | 4 (4.5) | 10 (5.6) |
| Study status at data cut-off | ||
| Ongoing/discontinued | 49 (55.7)/39 (44.3) | 108 (60.0)/72 (40.0) |
| Discontinuation due to death | 33 (84.6) | 50 (69.4) |
| Discontinuation due to consent withdrawal | 5 (12.8) | 18 (25.0) |
| Discontinuation due to loss to follow-up | 1 (2.6) | 2 (2.8) |
| Discontinued, other | – | 2 (2.8) |
| AEs associated with QoL impairment (any grade) | ||
| Constipation | 40 (45.5) | 94 (52.2) |
| Diarrhoea | 34 (38.6) | 72 (40.0) |
| Dyspnoea | 22 (25.0) | 57 (31.7) |
| Nausea | 22 (25.0) | 56 (31.1) |
| Vomiting | 17 (19.3) | 41 (22.8) |
| Decreased appetite | 9 (10.2) | 23 (12.8) |
| Dyspnoea exertional | 2 (2.3) | 3 (1.7) |
AE, adverse event; NSCLC, non-small-cell lung cancer; NTRK, neurotrophic receptor tyrosine kinase; PRO, patient-reported outcomes; QoL, quality of life; SA, safety analysis; ROS1, ROS proto-oncogene 1; TRAE, treatment-related AE.
Censored.
Discussion
Here we present PRO data from STARTRK-2, which provide additional evidence to support the association of entrectinib with clinically meaningful benefit in patients with NTRK fusion-positive solid tumours or ROS1 fusion-positive NSCLC.8,9 STARTRK-2 safety data demonstrate entrectinib has a manageable and relatively favourable safety profile. Overall, these PRO data support cumulative safety data, and are consistent with the overall entrectinib benefit–risk assessment. Importantly, patient-reported functioning and HRQoL remained stable or showed a trend towards improvement while on treatment. Patients with ROS1 fusion-positive NSCLC reported moderate-to-low treatment-related and tumour-related symptom burdens throughout, which remained stable or showed a trend towards improvement in most categories, with clinically meaningful improvements in lung-related symptom severity, in particular coughing, as well as some treatment-related symptoms such as appetite loss and trouble sleeping. There were only a few exceptions where there was a trend towards worsening (peripheral neuropathy and dysphagia) or sustained clinically meaningful worsening (constipation and diarrhoea). Patients with NTRK fusion-positive NSCLC or CRC reported moderate-to-low treatment- and tumour-related symptom burdens throughout, with either stable or clinically meaningful improvements in key symptoms. High questionnaire response rates indicate that the data are representative of the overall trial population.
For this analysis, PRO symptoms for evaluation were chosen based on the safety/efficacy profile of entrectinib, which indicated that insomnia, appetite loss, nausea, vomiting, constipation, diarrhoea, peripheral neuropathy, and sore mouth were potentially bothersome. In both SA-PRO populations, reports indicate no notable increase in the severity of these symptoms during treatment. Results of this analysis therefore demonstrate that these symptoms had minimal impact on patients' daily lives and HRQoL, providing further support for the safety and tolerability of entrectinib.
Similar to QLQ-C30 and QLQ-C13 findings for a phase II study of alectinib in patients with ALK fusion-positive advanced NSCLC,18 entrectinib was associated with a trend towards improvement in a number of lung cancer-related symptoms, such as cough, dyspnoea, and chest pain, a sustained high HRQoL, and PRO data were consistent with previously reported safety data. The alectinib study shows that a different tyrosine kinase inhibitor in a similar patient population also demonstrates the capacity to improve GHS/QoL and functioning, as well as alleviate the tumour-related symptom burden, while contributing a minimal treatment-related symptom burden. The value of assessing PROs to generate a more informed benefit–risk profile has also been demonstrated for other targeted therapies. Crizotinib and lorlatinib study PRO assessments demonstrated maintained or improved GHS, global QoL, physical functioning and symptoms, e.g. fatigue, cough, pain, and dyspnoea, but some worsening of specific treatment-related symptoms.19,20
Safety findings demonstrate low discontinuation rates due to treatment-related AEs. Rates of protocol-governed dose reduction were similar in the NTRK and ROS1 SA-PRO populations (31.8% and 30.0%, respectively). However, dose intensity was maintained throughout, with a median dose intensity of 91.4% (NTRK EA population; N = 71) and 92.9% (ROS1 EA population; N = 145), indicating that for the majority of patients, dose modifications were generally short term and did not result in a notable decrease in entrectinib treatment received throughout the study.
Strengths of this entrectinib PRO analysis include the use of multiple validated questionnaires and the high completion rates, as well as alignment with entrectinib's clinical trial efficacy and safety profile. However, some caution may be needed when interpreting results due to the small sample sizes. The single-arm STARTRK-2 trial design and lack of blinding could also potentially create bias in self-reporting, based on patients' treatment expectations.
Conclusions
Entrectinib has a manageable and relatively favourable safety and tolerability profile, which was similar for patients with NTRK fusion-positive solid tumours or ROS1 fusion-positive NSCLC. PRO findings are consistent with this profile, and further reinforce the positive benefit–risk of this treatment. In conclusion, from the patient's perspective, the overall treatment burden is minimal with entrectinib.
Acknowledgements
The authors thank the patients, their families, and the participating study centres. Third-party medical writing assistance, under the direction of the authors, was provided by Alix Biancardi, of Ashfield MedComms, an Ashfield Health company, and was funded by F. Hoffmann-La Roche Ltd. GD acknowledges the support of the Ludwig Center at Harvard and the Pan Mass Challenge (Paul's Posse, Erica's Entourage, and the Sarcoma Cycling Brigade). The authors acknowledge Thomas Karagiannis for contributions to the PRO study design and analysis plan, and Elisabeth Piault-Louis for her contributions to interpretation of the data.
Funding
This study was supported by F. Hoffmann-La Roche Ltd.
Disclosure
LP-A or his relative has received consulting fees from Genentech/F. Hoffmann-La Roche, Loxo Oncology, Bayer, Eli Lilly, AstraZeneca, Pfizer, Merck Sharp & Dohme (MSD), Novartis, Amgen, PharmaMar, Boehringer Ingelheim, Celgene, Servier, Sysmex, Incyte, Ipsen, Adacap, Sanofi, and Blueprint Medicines; sponsored research agreements from Bristol-Myers Squibb (BMS), AstraZeneca, and MSD; travel/accommodation expenses from Roche, AstraZeneca, MSD, BMS, Pfizer, Takeda; serves on the board of Genómica; and has a leadership role at the European Medicines Agency. LP-A is co-founder and sits on the board of Altum sequencing. FB has personal financial interests in AstraZeneca, Bayer, BMS, Boehringer Ingelheim, Eli Lilly Oncology, F Hoffmann-La Roche, Novartis, Merck, MSD, Pierre Fabre, Pfizer, and Takeda; and institutional financial interests in AbbVie, ACEA, Amgen, AstraZeneca, Bayer, BMS, Boehringer Ingelheim, Eisai, Eli Lilly Oncology, F. Hoffmann-La Roche, Genentech, Ipsen, Ignyta, Innate Pharma, Loxo, Novartis, Medimmune, Merck, MSD, Pierre Fabre, Pfizer, Sanofi-Aventis, and Takeda. SS is an advisory board member for Amgen, Bayer, BMS, CheckMab, Celgene, Daiichi Sankyo, Incyte, Merck, Novartis, F. Hoffmann-La Roche, and Seattle Genetics. M-JA has received consultant fees and honoraria from AstraZeneca, Eli Lilly and Company, Takeda, F. Hoffmann-La Roche Ltd, MSD, Merck, Boehringer Ingelheim, Ono Pharmaceutical, BMS, and Alpha Pharmaceutical. AD has received honoraria and consulting fees for advisory boards from Ignyta/F. Hoffmann-La Roche/Genentech, Loxo/Bayer/Eli Lilly, TP Therapeutics, AstraZeneca, Pfizer, Blueprint Medicines, Takeda/Ariad/Millennium, Helsinn, BeiGene, BerGenBio, Hengrui Therapeutics, Exelixis, Tyra Biosciences, Verastem, MORE Health, AbbVie, 14ner/Elevation Oncology, Remedica Ltd, ArcherDX, Monopteros, Novartis, EMD Serono, Liberum, Repare RX, and Melendi; associated research funding paid to institution by Pfizer, Exelixis, Taiho, Teva, GlaxoSmithKline, and PharmaMar; research funding from Foundation Medicine; royalties from Wolters Kluwer; other from Merck, Puma, Merus, and Boehringer Ingelheim; CME honoraria from Medscape, OncLive, PeerVoice, Physicians Education Resources, Targeted Oncology, Research to Practice, Axis, Peerview Institute, Paradigm Medical Communications, WebMD, and MJH Life Sciences. AC received consulting fees from Deciphera, Bayer, Genentech; received research funding from F. Hoffmann-La Roche, Ignyta, Bavarian Nordic, and Nant Pharma. CR is a speaker for MSD, AstraZeneca; has research collaborations with Guardant Health; is an advisory board member for Archer, Inivata, EMD Serono, Novartis and BMS; has received non-financial support from Guardant Health and research grant from LCRF-Pfizer. JW is an advisory board member for Amgen, AstraZeneca, Bayer, Blueprint, BMS, Boehringer Ingelheim, Chugai, Daiichi Sankyo, Ignyta, Janssen, Eli Lilly, Loxo, MSD, Novartis, Pfizer, F. Hoffmann-La Roche, Seattle Genetics, and Takeda; and has conducted research projects sponsored by MSD, Novartis, BMS, Janssen, and Pfizer. TS has received research funding and honoraria from Astellas Pharma, AstraZeneca, Chugai Pharmaceutical, Eli Lilly Japan, Kissei Pharmaceutical, MSD, Nippon Boehringer Ingelheim, Novartis Pharma, Pfizer Japan, Takeda Pharmaceutical; honoraria from BMS, Kyowa Hakko Kirin, Nippon Kayaku, Ono Pharmaceutical, Roche Singapore, Taiho Pharmaceutical, Thermo Fisher Scientific, Yakult Honsha; and research funding from Bayer Yakuhin, Daiichi Sankyo, Eisai, LOXO Oncology, Merck Serono. RD reports advisory boards for: F. Hoffmann-La Roche, Genentech, Bayer, Green Peptide, Blueprint Medicines, Takeda, AstraZeneca and Rain Therapeutics; stock ownership, IP licensing fees and consulting fees from Rain Therapeutics. Licensing fees for biological materials from Genentech, Foundation Medicine, Black Diamond, Pearl River, Voronoi, SeraCare, Ignyta, Loxo, Ariad, GVKbio, and Chugai. AK, SM and SO report employment with F. Hoffmann-La Roche/Genentech DC reports employment with and equity in F. Hoffmann-La Roche. GD received consulting fees from Novartis, Pfizer, EMD-Serono, Sanofi Oncology, Janssen Oncology, Ignyta, Loxo Oncology, Mirati Therapeutics, Epizyme, PharmaMar, Daiichi-Sankyo, WIRB Copernicus Group, Ziopharm, and Polaris Pharmaceuticals; received research support to Dana-Farber from Bayer, Novartis, Pfizer, Janssen Oncology, Ignyta, Loxo Oncology, AbbVie, Epizyme, and Adaptimmune; patent licensed to Novartis from Dana-Farber with royalty paid to Dana-Farber; member, Board of Directors, Blueprint Medicines and Merrimack Pharmaceuticals; member, Scientific Advisory Board with consulting fees and equity, Blueprint Medicines and Translate Bio; consultant, Scientific Advisory Board with consulting fees and equity, G1 Therapeutics, RELAY Therapeutics, CellCarta, Ikena Oncology, Caris Life Sciences, and Champions Oncology; consultant with equity, Bessor Pharmaceuticals. GD was supported in part by the Ludwig Center at Harvard, the Dr Miriam and Sheldon Adelson Medical Research Foundation, and the Pan Mass Challenge (Paul's Posse, Erica's Entourage, and the Sarcoma Cycling Brigade).
Data sharing
Qualified researchers may request access to individual patient level data through the clinical study data request platform (https://vivli.org/). Further details on Roche's criteria for eligible studies are available at https://vivli.org/members/ourmembers/. For further details on Roche's Global Policy on the Sharing of Clinical Information and how to request access to related clinical study documents, see https://www.roche.com/research_and_development/who_we_are_how_we_work/clinical_trials/our_commitment_to_data_sharing.htm.
Supplementary data
References
- 1.Liu D., Offin M., Harnicar S., Li B.T., Alexander Drilon A. Entrectinib: an orally available, selective tyrosine kinase inhibitor for the treatment of NTRK, ROS1, and ALK fusion-positive solid tumors. Ther Clin Risk Manag. 2018;14:1247–1252. doi: 10.2147/TCRM.S147381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vaishnavi A., Le A.T., Doebele R.C. TRKing down an old oncogene in a new era of targeted therapy. Cancer Discov. 2015;5:25–34. doi: 10.1158/2159-8290.CD-14-0765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Davies K.D., Doebele R.C. Molecular pathways: ROS1 fusion proteins in cancer. Clin Cancer Res. 2013;19:4040–4045. doi: 10.1158/1078-0432.CCR-12-2851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Planchard D., Popat S., Kerr K. Metastatic non-small cell lung cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2020;29:iv192–iv237. doi: 10.1093/annonc/mdy275. [DOI] [PubMed] [Google Scholar]
- 5.Marchio C., Scaltriti M., Ladanyi M. ESMO recommendations on the standard methods to detect NTRK fusions in daily practice and clinical research. Ann Oncol. 2019;30:1417–1427. doi: 10.1093/annonc/mdz204. [DOI] [PubMed] [Google Scholar]
- 6.Menichincheri M., Ardini E., Magnaghi P. Discovery of entrectinib: a new 3-aminoindazole as a potent anaplastic lymphoma kinase (ALK), c-ros oncogene 1 kinase (ROS1), and pan-tropomyosin receptor kinases (Pan-TRKs) inhibitor. J Med Chem. 2016;59:3392–3408. doi: 10.1021/acs.jmedchem.6b00064. [DOI] [PubMed] [Google Scholar]
- 7.Ardini E., Menichincheri M., Banfi P. Entrectinib, a pan-TRK, ROS1, and ALK inhibitor with activity in multiple molecularly defined cancer indications. Mol Cancer Ther. 2016;15:628–639. doi: 10.1158/1535-7163.MCT-15-0758. [DOI] [PubMed] [Google Scholar]
- 8.Krebs M.G., De Braud F., Siena S. Efficacy and safety of entrectinib in locally advanced/metastatic ROS1 fusion-positive NSCLC: an updated integrated analysis. Ann Oncol. 2020;31:S831–S833. doi: 10.1200/JCO.20.03025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rolfo C., De Braud F., Doebele R.C. Efficacy and safety of entrectinib in patients with NTRK fusion-positive (NTRK-fp) solid tumors: an updated integrated analysis. J Clin Oncol. 2020;38(15_Suppl) 3065-3065. [Google Scholar]
- 10.Basch E. Patient-reported outcomes: an essential component of oncology drug development and regulatory review. Lancet Oncol. 2018;19:595–597. doi: 10.1016/S1470-2045(18)30141-4. [DOI] [PubMed] [Google Scholar]
- 11.Zagadailov E., Fine M., Shields A. Patient-reported outcomes are changing the landscape in oncology care: challenges and opportunities for payers. Am Health Drug Benefits. 2013;6:264–274. [PMC free article] [PubMed] [Google Scholar]
- 12.Aaronson N.K., Ahmedzai S., Bergman B. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365–376. doi: 10.1093/jnci/85.5.365. [DOI] [PubMed] [Google Scholar]
- 13.Bergman B., Aaronson N.K., Ahmedzai S., Kaasa S., Sullivan M. The EORTC QLQ-LC13: a modular supplement to the EORTC Core Quality of Life Questionnaire (QLQ-C30) for use in lung cancer clinical trials. EORTC Study Group on Quality of Life. Eur J Cancer. 1994;30A:635–642. doi: 10.1016/0959-8049(94)90535-5. [DOI] [PubMed] [Google Scholar]
- 14.Gujral S., Conroy T., Fleissner C. Assessing quality of life in patients with colorectal cancer: an update of the EORTC quality of life questionnaire. Eur J Cancer. 2007;43:1564–1573. doi: 10.1016/j.ejca.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 15.ICHOM International Consortium for Health Outcomes Measurement (ICHOM) 2020. https://connect.ichom.org/standard-sets/ Available at:
- 16.Scott N.W., Fayers P.M., Aaronson N.K. EORTC Quality of Life Group; Brussels, Belgium: 2008. EORTC QLQ-C30 Reference Values. [Google Scholar]
- 17.Osoba D., Rodrigues G., Myles J., Zee B., Pater J. Interpreting the significance of changes in health-related quality-of-life scores. J Clin Oncol. 1998;16:139–144. doi: 10.1200/JCO.1998.16.1.139. [DOI] [PubMed] [Google Scholar]
- 18.Ou S.I., Socinski M.A., Gadgeel S. Patient-reported outcomes in a phase II, North American study of alectinib in patients with ALK-positive, crizotinib-resistant, non-small cell lung cancer. ESMO Open. 2018;3:e000364. doi: 10.1136/esmoopen-2018-000364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Blackhall F., Kim D.W., Besse B. Patient-reported outcomes and quality of life in PROFILE 1007: a randomized trial of crizotinib compared with chemotherapy in previously treated patients with ALK-positive advanced non-small-cell lung cancer. J Thorac Oncol. 2014;9:1625–1633. doi: 10.1097/JTO.0000000000000318. [DOI] [PubMed] [Google Scholar]
- 20.Peters S., Shaw A.T., Besse B. Impact of lorlatinib on patient-reported outcomes (PROs) in patients (pts) with advanced ALK+ or ROS1+ non-small cell lung cancer (NSCLC) Ann Oncol. 2018;29:viii493–viii547. doi: 10.1016/j.lungcan.2020.02.011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.