Abstract
Background
Even after potentially curative resection the long-term survival of pancreatic cancer is poor. The local-regional failures are frequent. Previous studies have shown that adjuvant treatment with hyperthermic intra-operative intraperitoneal chemotherapy (HIPEC) may effectively control local disease. The objective of the study is to update the results of the prior publications by integrating data from recently accrued cases. Also, to revisit the clinical and pharmacological rationale for the intraperitoneal administration of chemotherapy in pancreatic cancer patients undergoing potentially curative resection.
Methods
This is a prospective study of pancreatic cancer patients that underwent R0 resection in combination with HIPEC-gemcitabine. Morbidity and mortality were recorded. Survival was calculated and the sites for recurrent disease were recorded.
Results
The updated results for 33 patients that underwent treatment until 2016 and for 6 more patients that were included until 2018 were presented. The hospital mortality and morbidity rate were 5.1% (2 patients), and 28.2% (11 patients) respectively. The median and 5-year survival rate was 17 months and 24% respectively. With a median follow-up time of 13 months 23 patients (59%) were recorded with recurrence. Local regional failures were recorded in 4 patients (10.3%).
Conclusions
HIPEC following R0 resection is a feasible and safe adjuvant treatment for pancreatic cancer. The local-regional failures appear to be significantly decreased and to result in an increased overall survival. Further studies with combined intraperitoneal and systemic perioperative chemotherapy may serve to supplement our data with an increased benefit for patients having pancreas cancer resection.
Keywords: Pancreatic cancer, hyperthermic intra-operative intraperitoneal chemotherapy (HIPEC), gemcitabine, intraperitoneal chemotherapy, perioperative chemotherapy, local recurrence, peritoneal metastases, r0 resection
Introduction
The incidence of pancreatic cancer increases in the Western world and is the 4th most common cause of cancer-related death in USA (1). By 2030 it is expected to be the 2nd most common cause of cancer-related death (2). Despite advances in imaging techniques the incidence of resectable pancreatic tumors does not exceed 10–15% (3-6). The majority of tumors are unresectable either because they infiltrate vital anatomic vessels or because they are associated with liver, retroperitoneal, or peritoneal metastases at the time of initial diagnosis. Five-year survival rate does not usually exceed 10%, although 20–25% has been reported from high volume centers (1,7-11).
The most frequent sites of recurrence after potentially curative resection are the liver in 50–60%, the peritoneal surfaces in 40–50%, and the bed of tumor resection in 50% (12). It is obvious that the incidence of local-regional failures is high and if it could be reduced the overall survival would apparently increase. The pathophysiology of local-regional recurrence remains somewhat an enigma. It may be the result of tumor progression that has originated from undetected pre- or intra-operatively microscopic cancer emboli. It may also be the result of dissemination of cancer emboli that are implanted at the surrounding peritoneal surfaces as a result of surgical trauma during tumor resection (13). Intraperitoneal chemotherapy has shown to be effective by eradicating the microscopic residual tumor in diseases with peritoneal malignancy (14-18) and it could probably be effective in eradicating the residual microscopic cancer emboli after pancreatic surgery. Previous publications have provided evidence that HIPEC following R0 resection of pancreatic carcinomas is quite effective in reducing the local-regional recurrences and increasing long-term survival (19,20).
The purpose of the study is (I) to describe the perioperative intraperitoneal methods of chemotherapy that are in use for the prevention of peritoneal metastases, (II) to update the results of the previously published studies by integrating recent cases into our database, and (III) to present the clinical and pharmacological rationale for the intraperitoneal administration of chemotherapy in patients undergoing potentially curative resection of pancreatic cancer.
Methods
From 2007 to 2018, 39 patients with resectable pancreatic carcinomas underwent R0 resection of the tumor in combination with HIPEC-gemcitabine. The results of 33 of them had been previously analyzed (18) and updated. In the present study 6 more patients were included with the same criteria as before. The study was approved by the Hospital’s Ethical Committee and all patients signed an informed consent.
As has been emphasized only patients with resectable pancreatic adenocarcinomas that did not have distant metastases were included in the study. The preoperative work-up consisted of physical examination, hematological-biochemical examination, tumor markers (CEA, CA 19-9, CA-125), endoscopy combined with endoscopic ultra-sound, CT-abdominal and thoracic scanning, or MRI, and bone-scanning.
Patients older than 16 years of age, with acceptable cardiopulmonary function, performance status >50% (assessed by the Karnofsky performance scale), normal renal function (blood urea level <50 mg/dL, creatinine level <1.5 mg/dL), satisfactory liver function (other than hepatobiliary obstruction), white blood cell count >4,000/mL, and platelet count >150,000/mL were included in the study.
Patients with evidence of distant metastatic disease (liver, osseous, brain, pulmonary or any other distant site), those with poor performance status (Karnofsky performance <50%), those who had been treated with systemic chemotherapy, those patients with prior malignancy at risk for recurrence (except for basal-cell carcinoma or in-situ cervical carcinoma adequately treated), those with psychiatric diseases or addictive disorders, and pregnant women were not included in the study.
Treatments
Patients with cancer of the head of the pancreas underwent subtotal pancreatoduodenectomy (Kausch-Whipple procedure), and those with tumor of the body or tail of the pancreas underwent distal (left) pancreatectomy. HIPEC was performed for 60 min at 42.5–43 °C with 1,000 mg/m2 gemcitabine after tumor resection and before the reconstruction of the gastrointestinal tract with the Coliseum technique (open abdomen). A heater circulation with two roller pumps, one heat exchanger, one reservoir, an extracorporeal system of two inflow and two outflow tubes, and 4 thermal probes was used for HIPEC (Sun-Chip, Gamida Tech, France). A prime solution of 2–3 liters of normal saline was instilled prior to the administration of the cytostatic drug which was given as soon as the mean temperature in the abdominal cavity exceeded 40 °C. Adequate fluids were administered during HIPEC in order to maintain diuresis at 500 mL/h and for 24 hours after surgery.
The reconstruction of the continuity of the gastrointestinal tract was always made after the completion of HIPEC. This was possible with an end-to-side pancreato-jejunal anastomosis, an end-to-side choledocho-jejunal anastomosis in continuity, and a Roux-en-Y gastro-jejunal anastomosis at 60 cm with a second jejunal loop after sub-total pancreatoduodenectomy. After distal pancreatectomy the pancreatic remnant was always sutured with 3.0 silk.
All resected specimens were sent for histopathological examination and staging. The intra-operative and post-operative complications were carefully recorded and treated. Stage III patients were scheduled to receive adjuvant systemic chemotherapy.
Follow-up
All patients were followed-up at 3-month intervals for the first year and at 6-month intervals later with physical examination, hematological-biochemical examinations, tumor markers (CEA, CA 19-9, CA-125), CT-abdominal and thoracic scanning or MRI. Recurrences and the sites of recurrence were recorded.
Statistical analysis
The gender, the anatomic distribution of the tumor, the age, the performance status, the pT, the pN, the pTNM stage, the degree of differentiation, and the use of adjuvant systemic chemotherapy were all correlated to survival. The proportion of patients with a given characteristic was compared by chi square analysis or by Pearson’s test. Differences in the means of continuous measurement were tested by the Student’s t-test. The survival curves were obtained using the Kaplan-Meier method. Cox’s regression model was used for multiple analysis of survival. A two-tailed P value <0.05 was considered statistically significant.
Results
From 2007 to 2018, 39 patients with resectable pancreatic adenocarcinomas were included in the study. There were 19 (48.7%) men, and 20 (51.3%) women. The mean age of the patients was 67.9±10.9 years (range, 38–86 years). The characteristics of the patients are listed in Table 1.
Table 1. Characteristics of 39 patients with pancreatic cancer.
| Characteristics | No. of patients | % |
|---|---|---|
| Performance status | ||
| 90–100% | 29 | 74.4 |
| 70–80% | 9 | 23.1 |
| 50–60% | 1 | 2.6 |
| Anatomic distribution | ||
| Head | 31 | 79.5 |
| Body | 2 | 5.1 |
| Tail | 5 | 12.8 |
| Diffuse | 1 | 2.6 |
| Type of surgery | ||
| Sub-total pancreatoduodenectomy | 30 | 76.9 |
| Distal pancreatectomy | 7 | 17.9 |
| Total pancreatoduodenectomy | 2 | 5.1 |
| pT | ||
| T1 | 2 | 5.1 |
| T2 | 5 | 12.8 |
| T3 | 32 | 82.1 |
| pN | ||
| N0 | 17 | 43.6 |
| N1 | 22 | 56.4 |
| Degree of differentiation | ||
| G1 | 6 | 15.4 |
| G2 | 20 | 51.3 |
| G3 | 13 | 33.3 |
| pTNM | ||
| I | 4 | 10.3 |
| II | 9 | 23.1 |
| III | 26 | 66.7 |
Ductal pancreatic adenocarcinomas were confirmed in all resected specimens and complete staging was possible (Table 1).
During the postoperative period (45 days), 11 patients (28.2%) were recorded with complications which are listed in Table 2. The patient with postoperative bleeding underwent immediate reoperation and hemorrhage was controlled successfully. Two patients with anastomotic leak required reoperation because of choledocho-jejunal anastomosis failure which were successfully controlled with T-tube insertion. The other 2 patients with choledocho-jejunal anastomotic failures were successfully treated conservatively. The rate of reoperation was 5.1%. One patient was recorded with stroke but 6 months after initial treatment was free of neurological symptoms. Two patients were recorded with grade II neutropenia that did not require any specific treatment.
Table 2. Complications of 11 patients with pancreatic cancer.
| Complications | No. of patients | % |
|---|---|---|
| Postoperative bleeding | 1 | 2.6 |
| Pulmonary failure | 2 | 5.2 |
| Anastomotic leak | 4 | 10.3 |
| Sepsis | 1 | 2.6 |
| Grade II neutropenia | 2 | 5.1 |
| Cerebrovascular accident | 1 | 2.6 |
The mean blood loss was 305±205 mL (range, 80–820 mL). The mean operative time was 399±106 min (range, 185–592 min). The mean number of transfused blood units was 2±2 (range, 0–4), and the mean number of transfused FFP’s was 3±1 (range, 0–8). The mean days of hospitalization was 17.7±7 (range, 9–45).
The hospital mortality rate was 5.1% (2 patients). One patient died as a result of sepsis from an unknown site and the other because of pulmonary failure.
Eighteen patients (46.2%) received systemic adjuvant chemotherapy.
The overall 5-year survival rate was 24%. The 1-, 2-, and 3-year survival rate was 64%, 38%, and 28% respectively. The mean and median survival time were 40.3±8.2 months, and 17 months respectively (Figure 1). No variable was found to be related to survival by univariate analysis of survival although the grade of the cancer was of border-line statistical significance (Table 3).
Figure 1.
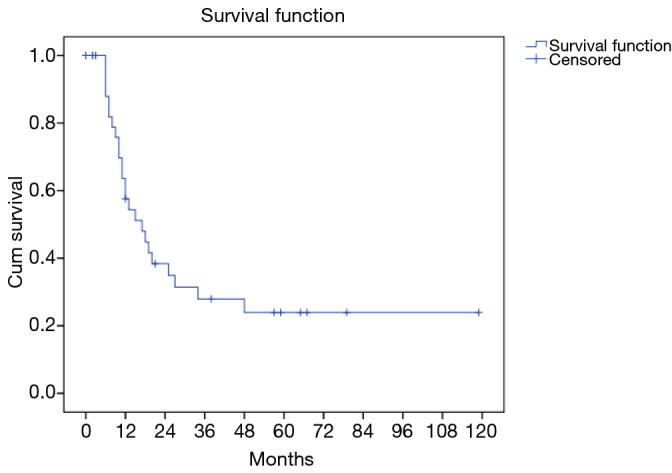
Overall survival of 39 patients with pancreatic cancer undergoing R0 resection and HIPEC.
Table 3. Univariate analysis of survival.
| Variable | P value |
|---|---|
| Gender | 0.758 |
| Anatomic distribution | 0.292 |
| T | 0.409 |
| N | 0.929 |
| TNM | 0.123 |
| G | 0.068 |
| Adjuvant chemotherapy | 0.226 |
One patient with stage II and another one with stage I disease died during the immediate postoperative period. The median follow-up time was 13 months, and the median time to disease progression 11 months. During follow-up 23 patients (59%) were recorded with recurrence. Histopathologically, 2 of them were T2N1, 7 were T3N0, and 14 were T3N1. Nineteen patients (48.7%) were recorded with distant metastatic disease and 4 (10.3%) with local-regional. All patients with local-regional recurrences were T3N1.
Univariate analysis of time to recurrence showed that the degree of differentiation was related to recurrence (P=0.006). The degree of differentiation was prognostic for recurrence (P=0.003, 95% CI: 0.53–0.665).
Currently, 7 patients (17.9%) are alive without evidence of disease, 23 patients (59%) died because of the disease, 8 patients (20.5%) died because of reasons unrelated to disease, and 1 patient (2.6%) is alive with disease. Histopathologically, the disease-free patients are as following: one patient with T1N0, one patient with T2N0, one patient with T3N0, and four patients with T3N1 disease.
Discussion
The best and most effective adjuvant treatment after pancreatic cancer resection has not yet been identified. The Gastrointestinal Study Group trial showed in 1985 that patients receiving chemoradiotherapy were offered significant survival benefit after tumor resection compared to the observation group. The weak point of the trial was the small number of patients studied (21). The next trial (EORTC) that included a large number of patients showed that there was no survival benefit for patients treated with chemoradiation after tumor resection (22). The ESPAC trial showed in patients with pancreatic cancer undergoing potentially curative resection that only systemic chemotherapy offered significant survival benefit. In contrast, chemoradiotherapy or radiotherapy did not offer significant survival benefit (23). Other studies from the USA showed that chemoradiation was more effective than surgery alone (24). A recent retrospective publication including large number of patients showed that adjuvant radiotherapy significantly increased survival in pancreatic cancer patients undergoing surgical resection (25). An even more recent publication showed that adjuvant chemotherapy followed by radiotherapy is a better approach in patients undergoing upfront resection (26). There is evidence from one retrospective study with neo-adjuvant treatment that either chemotherapy or chemoradiotherapy is effective and provides significantly increased survival compared to upfront surgery (27). Another comparative study shows the beneficial effect of preoperative treatment with chemoradiotherapy on both the rate of local-regional and distant metastases without any effect on overall and disease-free survival (28). It is apparent that there is much controversy about the most effective adjuvant treatment. Currently, in the USA chemoradiation is established as the preferred method while in Europe chemotherapy alone based on gemcitabine is the most frequently used popular adjuvant treatment. Newly developed chemotherapeutic regimens have been suggested to be more effective but the prognosis of pancreatic cancer still remains poor (29,30). More aggressive surgical operations (total pancreatectomy, extensive lymph node resection) have not shown to increase overall survival (31,32). The use of IORT (intraoperative radiation therapy) for the control of local disease has not convinced the medical community (33).
It is not possible to precisely determine the pathophysiology of local-regional recurrences. However, a reasonable hypothesis is to incriminate local-regional surgical treatment failure. One must assume that small volume local disease progression occurs in patients who have been left with positive margins of resection. The head of the pancreas, surrounded by vital anatomic structures has extremely narrow limits of resection and the interstitial tissues are frequently traumatized during surgery. The lymphatic vessels must be transected and venous blood is lost during surgical manipulations. As a consequence, cancer emboli disseminate in the peritoneal cavity. During wound healing, these emboli are entrapped in fibrin, inflammatory cells accumulate with local collagen, and this complex is stimulated by growth factors giving rise to recurrent tumor in 2–3 years after initial surgery. The cancer emboli are expected to efficiently implant at the resection site. The implantation of cancer emboli at the bed of resection causes a high-density local recurrence. In addition, distant peritoneal implants are expected to grow (13). Although systemic chemotherapy with gemcitabine has proved to be effective in high-risk patients with pancreatic cancer undergoing potentially curative resection, it has not been shown to be effective in the control of local-regional residual disease (34). The eradication of the residual microscopic tumor is possible with the use of intraperitoneal chemotherapy for those diseases that present with peritoneal carcinomatosis (14-18). Laboratory research has shown that the intraperitoneal administration of gemcitabine may effectively target local-regional control (35). Clinical studies have reconfirmed these same conclusions (19,20,36). The advantage of the intraperitoneal administration of chemotherapy is the high drug level that can be achieved loco-regionally with low systemic exposure (37). Another advantage is its effect on hepatic and lymph node micrometastases. Pharmacologic data have shown that the absorption of the intraperitoneally administered drug is possible in about 90% by the visceral peritoneum (38) and as a consequence the concentration of the drug in the portal circulation appears to be effective on micrometastatic disease. The high rate of distant metastatic disease (48.7% or 19 patients) implies that the intraperitoneal chemotherapy needs to be reinforced with a bolus of systemic chemotherapy. Therefore, we intend to change the protocol. Intravenous 5-FU (400–600 mg/m2) in combination with leucovorin or isovorin (20 mg/m2) during HIPEC will be added in the treatment. Other systemic agents or early postoperative intraperitoneal chemotherapy (EPIC) are also being considered.
Gemcitabine (2, 2-difluorodeoxycitidine) is a pyrimidine analogue. The cytotoxicity of gemcitabine is quite consistent particularly against pancreatic cancer. The pharmacokinetics and tissue distribution of intraperitoneal administration of gemcitabine has been investigated in a rat model and has been shown that the AUC ratio after intraperitoneal administration is favorable for its intraperitoneal use (39). The use of normothermic intraperitoneal gemcitabine in advanced cancer has also been investigated (40-42). Also, a potential indication for heated intraoperative intraperitoneal administration of gemcitabine as an adjuvant to resected advanced pancreatic cancer with high risk of recurrence has been published (36). Although it has not been proved, it is assumed that the open abdominal technique (Coliseum) appears to be the most effective because the surgeon distributes heat and drug uniformly in all peritoneal surfaces, especially the pancreas resection site. In a small number of patients Sugarbaker has used long-term normothermic intraperitoneal chemotherapy (NIPEC-LT) targeting on additional control of the local-regional disease. The method is promising although the distribution of the drug at the peritoneal surfaces is restricted because of the adhesions (43).
Pancreatic cancer resection combined with HIPEC is a safe method, associated with low hematologic toxicity that does not require specific treatment. The preliminary results reported by Sugarbaker have not shown hematologic toxicity (43). There has been no evidence to incriminate HIPEC for the complications. The incidence of complication (28%) of the present study appears to be comparable to the 41–46% complication rate following surgical resection only (19,20,44,45). Delayed gastric emptying and pancreatic leak are very severe and frequent complications after Whipple’s procedure that have not been recorded in the present study. In contrast, biliary leak has been present in 10.3% of our patients, comparable to 9% leak reported after Whipple’s resection without HIPEC (44,45). Intra-abdominal bleeding has been recorded to be 2.6%, comparable to 3% reported in other studies (44,45). Other severe complications are the intra-abdominal abscess 10%, and gastrointestinal bleeding 5%. None of them has been recorded in the present study. In contrast, sepsis of an unknown primary has been present in 2.6%, pulmonary failure in 5.2%, and stroke in 2.6% (Table 2). The hospital mortality of 5.1% is acceptable (19,20,44).
The up-dated results have shown that long-term survival remains high as previously reported and is comparable to survival reported from high-volume centers (10,11). The median follow-up time has been extended from 11 to 13 months. The median survival has also been extended from 13 to 17 months, and the median disease-free survival from 9 to 11 months. The overall survival has remained stable at 24% and the recurrence rate has slightly declined from 60.6% to 59%. In contrast with longer follow-up the rate of local-regional failure has slightly increased from 9.1% to 10.3%. Although these variations are not significant it is important to note that the survival has been stable despite the addition of new patients to our series.
HIPEC with gemcitabine has been used after extensive cytoreduction in 6 patients with peritoneal carcinomatosis of pancreatic cancer. Four of them survived more than 12 months. This limited experience shows that there is probably a group of patients with peritoneal carcinomatosis of pancreatic cancer in which the peritoneal metastases may be adequately eradicated with cytoreduction and HIPEC (46).
Conclusions
There is evidence that HIPEC as an adjuvant after pancreatic cancer resection is a safe and rationale treatment strategy that is effective in improving the local-regional failure. Additionally, HIPEC is probably an effective method in controlling micrometastatic disease. So far, it has been shown that local-regional failure is reduced and the overall survival is high. Building on these positive results, further studies that involve HIPEC-gemcitabine are indicated.
Acknowledgments
Funding: None.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Hospital’s Ethical Committee and all patients signed an informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
Footnotes
Provenance and Peer Review: This article was commissioned by the Guest Editors (Paul H. Sugarbaker and Kurt Van der Speeten) for the focused issue“Intraperitoneal Chemotherapy for Peritoneal Metastases: HIPEC, EPIC, NIPEC, PIPAC and More” published in Journal of Gastrointestinal Oncology. This article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jgo-20-46). The focused issue was sponsored by the Peritoneal Surface Oncology Group International (PSOGI). The author has no other conflicts of interest to declare.
References
- 1.McGuigan A, Kelly P, Turkington RC, et al. Pancreatic cancer: A review of clinical diagnosis, epidemiology, treatment, and outcomes. World J Gastroenterol 2018;24:4846-61. 10.3748/wjg.v24.i43.4846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Siegel RL, Miller KD, Jemal A. Cancer Statistics 2017. CA Cancer J Clin 2017;67:7-30 10.3322/caac.21387 [DOI] [PubMed] [Google Scholar]
- 3.Schneider G, Siveke JT, Eckel F, et al. Pancreatic cancer:basic and clinical aspects. Gastroenterology 2005;128:1606-25. 10.1053/j.gastro.2005.04.001 [DOI] [PubMed] [Google Scholar]
- 4.Geer RJ, Brennan MF, Cameron J, et al. Prognostic indicators for survival after resection of pancreatic adenocarcinoma. Am J Surg 1993;165:68-72; discussion 72-3. 10.1016/S0002-9610(05)80406-4 [DOI] [PubMed] [Google Scholar]
- 5.Nitecki SS, Sarr MG, Colby TV, et al. Long-term survival after resection for ductal adenocarcinoma of the pancreas:is it really improving? Ann Surg 1995;221:59-66. 10.1097/00000658-199501000-00007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Birkmeyer JD, Warshaw AL, Finlayson SRG, et al. Relationship between hospital volume and late survival after pancreaticoduodenectomy. Surgery 1999;126:178-83. 10.1016/S0039-6060(99)70152-2 [DOI] [PubMed] [Google Scholar]
- 7.Bramhall SR, Allum WH, Jones AG, et al. Treatment and survival in 13 560 patients with pancreatic cancer, and incidence of the disease, in the West Midlands: An epidemiological study. Br J Surg 1995;82:111-5. 10.1002/bjs.1800820137 [DOI] [PubMed] [Google Scholar]
- 8.Jemal A, Thomas A, Murray T, et al. Cancer statistics. CA Cancer J Clin 2002;52:23-47. 10.3322/canjclin.52.1.23 [DOI] [PubMed] [Google Scholar]
- 9.Beger HG, Rau B, Gansauge F, et al. Pancreatic cancer-low survival rates. Dtsch Arztebl Int 2008;105:255-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lim JE, Chien MW, Earle CC. Prognostic factors following curative resection for pancreatic adenocarcinoma: A population-based, linked database analysis of 396 patients. Ann Surg 2003;237:74-85. 10.1097/00000658-200301000-00011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cameron JL, Riall TS, Coleman J, et al. One thousand consecutive pancreaticoduodenectomies. Ann Surg 2006;244:10-5. 10.1097/01.sla.0000217673.04165.ea [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Warshaw AL, Fernandez-del Castillo C. Pancreatic carcinoma. N Engl J Med 1992;326:455-65. 10.1056/NEJM199202133260706 [DOI] [PubMed] [Google Scholar]
- 13.Sugarbaker PH. “Observations concerning cancer spread within the peritoneal cavity and concepts supporting an ordered pathophysiology,” in Peritoneal Carcinomatosis: Principles and Practice of Management. Sugarbaker PH (ed). Boston, Mass, USA: Kluwer Academic, 1996: 79-100. [DOI] [PubMed] [Google Scholar]
- 14.Yan TD, Black D, Savady R, et al. A systematic review on the efficacy of cytoreductive surgery and perioperative intraperitoneal chemotherapy for pseudomyxoma peritonei. Ann Surg Oncol 2007;14:484-92. 10.1245/s10434-006-9182-x [DOI] [PubMed] [Google Scholar]
- 15.Yan TD, Welch L, Black D, et al. A systematic review on the efficacy of cytoreductive surgery combined with perioperative intraperitoneasl chemotherapy for diffuse malignant peritoneal mesothelioma. Ann Oncol 2007;18:827-34. 10.1093/annonc/mdl428 [DOI] [PubMed] [Google Scholar]
- 16.Verwaal VJ, van Ruth S, de Bree E, et al. Randomized trial of cytoreduction and hyperthermic intraperitoneal chemotherapy versus systemic chemotherapy and palliative surgery in patients with peritoneal carcinomatosis of colorectal cancer. J Clin Oncol 2003;21:3737-43. 10.1200/JCO.2003.04.187 [DOI] [PubMed] [Google Scholar]
- 17.Tu Y, Tian Y, Fang Z, et al. Cytoreductive surgery combined with hyperthermic intraperitoneal chemoperfusion for the treatment of gastric cancer; A single-centre retrospective study. Int J Hyperthermia 2016;32:587-94. 10.1080/02656736.2016.1190987 [DOI] [PubMed] [Google Scholar]
- 18.van Driel WJ, Koole SN, Sikorska K, et al. Hyperthermic intraperitoneal chemotherapy in ovarian cancer. N Engl J Med 2018;378:230-40. 10.1056/NEJMoa1708618 [DOI] [PubMed] [Google Scholar]
- 19.Tentes AA, Kyziridis D, Kakolyris S, et al. Preliminary results of Hyperthermic intraperitoneal intraoperative chemotherapy as an adjuvant in resectable pancreatic cancer. Gastroenterol Res Pract 2012;2012:506571. 10.1155/2012/506571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tentes AA, Stamou K, Pallas N, et al. The effect of hyperthermic intraoperative intraperitoneal chemotherapy (HIPEC) as an adjuvant in resectable pancreatic cancer. Int J Hyperthermia 2016;32:895-9. 10.1080/02656736.2016.1227094 [DOI] [PubMed] [Google Scholar]
- 21.Kalser MH, Ellenberg SS. Pancreatic cancer. Adjuvant combined radiation and chemotherapy following curative resection. Arch Surg 1985;120:899-903. 10.1001/archsurg.1985.01390320023003 [DOI] [PubMed] [Google Scholar]
- 22.Klinkenbijl JH, Jeekel J, Sahmoud T, et al. Adjuvant radiotherapy and 5-fluorouracil after curative resection of cancer of the pancreas and periampullary region:phase III trial of the EORTC gastrointestinal tract cancer cooperative group. Ann Surg 1999;230:776-82; discussion 782-4. 10.1097/00000658-199912000-00006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Neoptolemos JP, Stocken DD, Friess H, et al. A randomized trial of chemoradiotherapy and chemotherapy after resection of pancreatic cancer. N Engl J Med 2004;350:1200-10. 10.1056/NEJMoa032295 [DOI] [PubMed] [Google Scholar]
- 24.Hsu CC, Herman JM, Corsini MM, et al. Adjuvant chemoradiation for pancreatic adenocarcinoma: The Johns Hopkins hospital-Mayo clinic collaborative study. Ann Surg Oncol 2010;17:981-90. 10.1245/s10434-009-0743-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kamarajah SK, Sonnenday CJ, Cho CS, et al. Association of adjuvant radiotherapy with survival after margin-negative resection of pancreatic ductal adenocarcinoma. Ann Surg 2021;273:587-94. 10.1097/SLA.0000000000003242 [DOI] [PubMed] [Google Scholar]
- 26.Moaven O, Clark CJ, Russell GB, et al. Optimal adjuvant treatment approach after upfront resection of pancreatic cancer: revisiting the role of radiation based on pathologic features. Ann Surg 2020. doi:. 10.1097/SLA.0000000000003770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mokdad AA, Minter RM, Zhu H, et al. Neoadjuvant therapy followed by resection versus upfront resection for resectable pancreatic cancer: A propensity score match analysis. J Clin Oncol 2017;35:515-22. 10.1200/JCO.2016.68.5081 [DOI] [PubMed] [Google Scholar]
- 28.Papavasiliou P, Hoffman JP, Cohen SJ, et al. Impact on preoperative therapy on patterns of recurrence in pancreatic cancer. HPB (Oxford) 2014;16:34-9. 10.1111/hpb.12058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Conroy T, Desseigne F, Ychou M, et al. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med 2011, 364:1817-25. 10.1056/NEJMoa1011923 [DOI] [PubMed] [Google Scholar]
- 30.Von Hoff DP, Ramanathan RK, Borad MJ, et al. Gemcitabine plus nab-paclitaxel is an active regimen in patients with advanced pancreatic cancer: A phase I/II trial. J Clin Oncol 2011;29:4548-54. 10.1200/JCO.2011.36.5742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Koliopanos A, Avgerinos C, Farfaras A, et al. Radical Resection of Pancreatic Cancer. Hepatobiliary Pancreat Dis Int 2008;7:11-8. [PubMed] [Google Scholar]
- 32.Ansari D, Gustafsson A, Andersson R. Update on the management of pancreatic cancer:surgery is no enough. World J Gastroenterol 2015;21:3157-65. 10.3748/wjg.v21.i11.3157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Palta M, Willett C, Czito B. The role of intraoperative radiation therapy in patients with pancreatic cancer. Semin Radiat Oncol 2014;24:126-31. 10.1016/j.semradonc.2013.11.004 [DOI] [PubMed] [Google Scholar]
- 34.Oettle H, Post S, Neuhaus P, et al. Adjuvant chemotherapy with gemcitabine vs observation in patients undergoing curative-intent resection of pancreatic cancer: A randomized controlled trial. JAMA 2007;297:267-77. 10.1001/jama.297.3.267 [DOI] [PubMed] [Google Scholar]
- 35.Ridwelski K, Meyer F, Hribaschek A, et al. Intraoperative and early postoperative chemotherapy into the abdominal cavity using gemcitabine may prevent occurrence of peritoneal carcinomatosis. J Surg Oncol 2002;79:10-6. 10.1002/jso.10000 [DOI] [PubMed] [Google Scholar]
- 36.Sugarbaker PH, Stuart OA, Bijelik L. Intraperitoneal gemcitabine chemotherapy treatment for patients with resected pancreatic cancer: rationale and report of early data. Int J Surg Oncol 2011;2011:161862. 10.1155/2011/161862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dedrick RL. Theoretical and experimental basis of intraperitoneal chemotherapy. Semin Oncol 1985;12:1-6. [PubMed] [Google Scholar]
- 38.Speyer JL, Sugarbaker PH, Collins JM, et al. Portal levels and hepatic clearance of 5-fluorouracil after intraperitoneal administration in humans. Cancer Res 1981;41:1916-22. [PubMed] [Google Scholar]
- 39.Pestieau SR, Stuart OA, Chang D, et al. Pharmacokinetics of intraperitoneal gemcitabine in a rat model. Tumori 1998, 84:706-11. 10.1177/030089169808400619 [DOI] [PubMed] [Google Scholar]
- 40.Sabbatini P, Aghajanian C, Leitao M., et al. Intraperitoneal cisplatin with intraperitoneal gemcitabine in patients with epithelial ovarian cancer: results of a phase I/II Trial. Clin Cancer Res 2004;10:2962-7. 10.1158/1078-0432.CCR-03-0486 [DOI] [PubMed] [Google Scholar]
- 41.Morgan RJ, Jr, Synold TW, Xi B, et al. Phase I trial of intraperitoneal gemcitabine in the treatment of advanced malignancies primarily confined to the peritoneal cavity. Clin Cancer Res 2007;13:1232-7. 10.1158/1078-0432.CCR-06-1735 [DOI] [PubMed] [Google Scholar]
- 42.Gamblin TC, Egorin MJ, Zuhowski EG, et al. Intraperitoneal gemcitabine pharmacokinetics: A pilot and pharmacokinetic study in patients with advanced adenocarcinoma of the pancreas. Cancer Chemother Pharmacol 2008;62:647-53. 10.1007/s00280-007-0647-9 [DOI] [PubMed] [Google Scholar]
- 43.Sugarbaker PH, Stuart OA, Bijelic L. Intraperitoneal gemcitabine chemotherapy as an adjuvant treatment for patients with resected pancreatic cancer:Phase II and pharmacologic studies. Transl Gastrointestin Cancer 2012;1:161-8. [Google Scholar]
- 44.Miedema BW, Sarr MG, van Heerden JA, et al. Complications following pancreaticoduodenectomy. Current management. Arch Surg 1992;127:945-9; discussion 949-50. 10.1001/archsurg.1992.01420080079012 [DOI] [PubMed] [Google Scholar]
- 45.Yeo CJ, Cameron JL, Sohn TA, et al. Six hundred fifty consecutive pancreaticoduodenectomies in the 1990s:pathology, complications, and outcomes. Ann Surg 1997;226:248-57. 10.1097/00000658-199709000-00004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tentes AA, Pallas N, Karamveri C, et al. Cytoreduction and HIPEC for peritoneal carcinomatosis of pancreatic cancer. J BUON 2018;23:482-7. [PubMed] [Google Scholar]


