Abstract
Coronavirus disease 2019 (COVID-19) is likely to have a major impact on society and the economy since the illness is currently infecting a significant number of active workers in the industry and service sectors. The illness can have long-term consequences for patients, affecting their functional capacity and, consequently, their occupational performance. This study analyzed the effects of COVID-19 on occupational health, with a focus on the importance of physical therapy in rehabilitation. An integrative literature review was conducted based on articles retrieved from the PubMed, SciELO, and LILACS databases using the following keywords: COVID-19, physical therapy, rehabilitation, and occupational health. The search retrieved 1,308 studies, 15 of which met inclusion criteria for the review. A thorough assessment of the articles revealed four topics that corresponded to the results of this study: 1) effects of COVID-19 on occupational health; 2) physical therapy in mild and moderate cases without hospitalization; 3) physical therapy in hospitalized patients with COVID-19; 4) physical therapy in post-intensive care unit (ICU) recovery and after hospital discharge. The findings showed that COVID-19 can affect several physiological systems and have both short- and long-term effects on patients, including physical and psychological impairments. Physical therapists must be involved in the battle against this illness to help patients recover their physical function and return to work as quickly, safely, and effectively as possible.
Keywords: physical therapy, COVID-19, rehabilitation, workers’ health
INTRODUCTION
Coronavirus disease 2019 (COVID-19) is an illness caused by infection with the novel coronavirus (severe acute respiratory syndrome coronavirus 2 [SARS-CoV-2]), which was first identified in a December 2019 outbreak in the city of Wuhan, China, before quickly moving on to several countries across the world.1 The rapid global spread of this illness, combined with its high infection and death rates, prompted the World Health Organization (WHO) to deem it a public health emergency of international concern on January 30, 2020, and declare a pandemic on March 11 of the same year.2,3
The SARS-CoV-2 is a single-stranded RNA virus in the Coronaviridae family. The pathogens in this family affect humans and a variety of other animals, causing infections that range from asymptomatic to very severe.4 In humans, the mild or oligosymptomatic form of this virus infection is associated with clinical manifestations such as fever, cough, rhinorrhea, sore throat, anosmia, ageusia, asthenia, mild dyspnea, hyporexia, nausea, diarrhea, and vomiting.5 However, the infection can also progress to severe acute respiratory syndrome (SARS), leading to severe dyspnea, pneumonia, or even death.6
The effects of the coronavirus responsible for COVID-19 can extend far beyond the respiratory system, affecting the cardiovascular, renal, gastrointestinal, endocrine, nervous, and musculoskeletal systems.7,8 Older age and comorbidities such as smoking, obesity, diabetes mellitus, hypertension, heart disease and previous respiratory illnesses also constitute risk factors for more severe disease.9
Furthermore, patients with SARS usually require prolonged hospitalization and mechanical ventilation, which can result in serious side effects and the development of post-intensive care syndrome.10,11 This condition is characterized by physical, cognitive, and psychiatric impairments that affect patients’ quality of life even after hospital discharge.12
The literature shows that patients who developed SARS in a previous outbreak of coronavirus continued to display reduced respiratory capacity and musculoskeletal limitations years after the end of the disease.13,14 Additionally, asymptomatic or even non-infected individuals can experience reduced functional capacity due to a sedentary lifestyle during social distancing; this is especially likely in individuals with pre-existing musculoskeletal diseases.15 These data support the conclusion that COVID-19 can have direct and indirect effects on health, both in the short- and the long term. COVID-19 can undoubtedly have a major impact on society and the economy since the novel coronavirus has infected a significant number of active workers in the industry and service sectors, especially those working in health care settings.16
Physical therapists play an important role in combating the COVID-19 pandemic, as they contribute to the prevention and rehabilitation of impairments caused by the illness,15 in addition to assisting with functional independence and facilitating individuals’ reintegration into society and the job market. This study aimed to analyze the effects of COVID-19 on occupational health, with a focus on the importance of physical therapy in rehabilitation.
METHODS
The goals of this study were achieved through a literature review. The review involved the following steps: topic identification, definition of the research question, methodological design, definition of inclusion and exclusion criteria, data collection and selection, evaluation of included studies, interpretation of the results, and presentation of the review. Articles were identified in the United States National Library of Medicine (PubMed), Scientific Electronic Library Online (SciELO), and Latin American & Caribbean Health Sciences Literature (LILACS) databases in August 2020, using the following Health Sciences Descriptors (DeCS): COVID-19, physical therapy, rehabilitation, and occupational health, in both Portuguese and English. The terms were combined using the Boolean operator “AND” to locate studies that contained all relevant keywords.
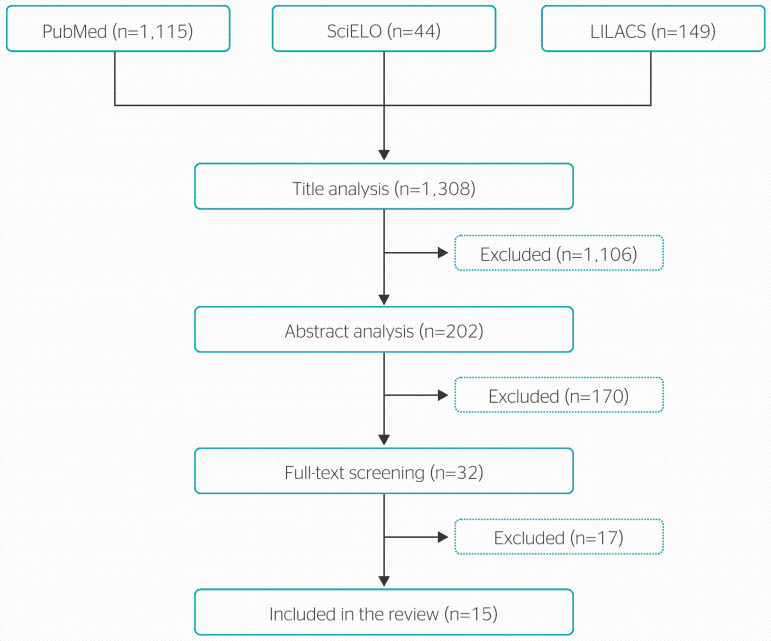
The following inclusion criteria were set for the review: full-text availability; English, Spanish, and/or Portuguese language; having “consequences of COVID-19”, “COVID-19 and physical therapy,” and “COVID-19 and occupational health” as the main topic of study. Duplicate studies and those that did not address the theme of the study were excluded. The reference lists of the main articles included in the review were also hand-searched to identify any relevant studies missed by the electronic search. The search retrieved a total of 1,308 articles across all databases. After title analysis and the application of inclusion criteria, 202 studies were selected for abstract screening. Thirty-two studies were then selected for full-text reading, which led to the exclusion of 12 studies. As a result, the final sample consisted of 15 articles. Figure 1 shows the search and selection strategies used in this review.
Figure 1.
Literature search and study selection flow chart. LILACS = Latin American & Caribbean Health Sciences Literature; PubMed = United States National Library of Medicine; SciELO = Scientific Electronic Library Online.
RESULTS AND DISCUSSION
The 15 articles in the review comprised 7 studies conducted in China, 3 in the United States, 2 in Brazil, 1 in Italy, 1 in England, and 1 multicenter study. Seven studies were descriptive, 2 were literature reviews, 2 were experience reports, 2 were official documents, 1 was a descriptive study and 1 was a quasi-experimental study (Table 1).
Table 1.
Summary of articles reviewed, including authors, country, type of article, objectives, and relation to the theme of this review
| Wang et al.17 | China | Descriptive and exploratory | To evaluate levels of psychological distress, anxiety, depression, and stress in the early stages of the COVID-19 outbreak. | COVID-19 and clinical consequences |
| Iannaccon et al.18 | Italy | Experience report | To identify barriers to functional recovery in patients with COVID-19 and make recommendations for the development of standardized clinical procedures. | COVID-19 and rehabilitation |
| Zhou et al.19 | China | Descriptive and exploratory | To analyze risk factors for hospital death and describe the clinical course of COVID-19 symptoms. | COVID-19 and clinical consequences |
| Rede CoVida20 | Brazil | Literature review | To assess occupational health risks and vulnerabilities during the COVID-19 pandemic. | COVID-19 and occupational health |
| Guan et al.21 | China | Descriptive and exploratory | To analyze the clinical characteristics of COVID-19. | COVID-19 and clinical consequences |
| Baker et al.22 | United States | Descriptive and exploratory | To assess the number and occupational categories of workers exposed to infection and disease at their workplace. | COVID-19 and occupational health |
| Lan et al.23 | United States | Descriptive and exploratory | To identify occupations with a high risk of local transmission of COVID-19. | COVID-19 and occupational health |
| Wu & McGoogan24 | China | Descriptive and exploratory | To analyze all cases diagnosed before February 11, 2020. | COVID-19 and clinical consequences |
| Thomas et al.25 | China | Recommendations | To standardize techniques and procedures for pulmonary rehabilitation. | COVID-19 and rehabilitation |
| PAHO26 | United States | Official document | Considerations and recommendations for rehabilitation. | COVID-19 and rehabilitation |
| Halpin et al.27 | England | Descriptive and exploratory | To examine the impact of COVID-19 on survivors after hospital discharge. | COVID-19 and clinical consequences |
| Liu et al.28 | China | Quasi-experimental | To examine the effects of a 6-week pulmonary rehabilitation program on respiratory function, quality of life, mobility, and psychological functions in older adults with COVID-19. | COVID-19 and rehabilitation |
| Wang et al.29 | China | Literature review | To serve as a guide and starting point for the management of functional impairments and comorbid issues associated with COVID-19. | COVID-19 and rehabilitation |
| Carda et al.30 | Multicenter study | Experience report | To share the experiences and perspectives of clinicians in different rehabilitation centers for COVID-19. | COVID-19, clinical consequences and rehabilitation |
| Brasil31 | Brazil | Epidemiological bulletin | Disclosure of epidemiological data and information on the structure established to combat COVID-19 in Brazil. | COVID-19, clinical consequences and occupational health |
COVID-19 = coronavirus disease 2019; PAHO = Pan-American Health Organization.
The review showed that, despite the wealth of research on COVID-19 published in the past year, few studies have evaluated the effects of this illness on occupational health or the work of physical therapists in the rehabilitation of patients with COVID-19. However, some studies did provide clinical descriptions of patients with COVID-19. This was most frequent in studies performed in China, the epicenter of the disease. Experts, occupational associations, and professional organizations in several countries have also published recommendations for the treatment of these patients. These recommendations were based on the experience of countries that have faced or are facing a large number of COVID-19 cases; on previous research on the treatment of other coronavirus infections; and on studies of SARS not caused by a coronavirus.
After reading the articles, four main themes were identified and used to structure this review: 1) effects of COVID-19 on occupational health; 2) physical therapy in mild and moderate cases without hospitalization; 3) physical therapy in hospitalized patients with COVID-19; and 4) physical therapy in post-intensive care unit (ICU) recovery and after hospital discharge.
EFFECTS OF COVID-19 ON OCCUPATIONAL HEALTH
The clinical presentation of coronavirus infections in humans can vary widely, ranging from a mild cold to severe illnesses such as those associated with the 2002 SARS-CoV epidemic and the Middle East respiratory syndrome coronavirus (MERS-CoV) outbreaks in 2012 and 2015.32 At the end of 2019, a new strain of coronavirus was found to be responsible for outbreaks of respiratory disease in humans. The pathogen was temporarily named the novel coronavirus 2019 (2019-nCoV). Genetic sequencing studies confirmed the existence of a new strain of coronavirus, which was classified as a member of the Betacoronavirus family and named SARS-CoV-2, marking the third instance in which a coronavirus jumps from animals to humans in less than two decades.33,34
Although human infection by SARS-CoV-2 is a recent phenomenon and its clinical features have not been fully defined, the virus is known to be highly pathogenic and cause both upper and lower respiratory tract infections with a risk of lethality.4 The infection is mediated by an affinity with the angiotensin-converting enzyme 2 (ACE2) receptor, which plays a fundamental role in the renin-angiotensin-aldosterone system and influences the regulation of arterial pressure and electrolyte homeostasis.33,35 ACE2 is highly expressed in lung cells and several extrapulmonary tissues, including gastrointestinal, cardiac, endothelial, skin, and smooth muscle tissue, as well as the oral and nasal mucosa.36 When infected, these tissues increase the production of ACE2 and immunosuppressant proteins, as well as the release of inflammatory cytokines.34 Since ACE2 is frequently expressed in type II alveolar cells, the lungs are often compromised in patients with COVID-19. However, the wide distribution of these receptors in other organs allows COVID-19 to affect several organ systems.37
Although patients can have multisystemic infections, the symptoms of COVID-19 can vary between patients, and in most cases, are classified as mild to moderate.19 Yet the infection can become severe, resulting in serious respiratory problems, viral pneumonia, and even death.6 The signs and symptoms of COVID-19 emerge on average 5 to 6 days after infection (mean period of incubation: 5-6 days, range: 1-14 days).38 The course of the illness is divided into two phases: the acute phase involves mostly respiratory symptoms, while the post-acute phase can include symptoms associated with prolonged immobilization, previous respiratory dysfunction, as well as cognitive and emotional disturbances.18
Studies show that older adults and obese individuals, as well as those with heart disease, immunosuppression, and preexisting respiratory problems, are more likely to develop severe forms of the disease.9 Recent studies have noted that, since SARS-CoV-2 binds to host cells through the peptidase domain of ACE2, which facilitates entry and replication,33,35 people treated with angiotensin-converting inhibitors and/or angiotensin II type I receptor blockers, such as patients with diabetes and hypertension, are also more likely to develop severe forms of COVID-19.39
In light of these observations, the impact of COVID-19 on human health is a cause for concern, since the illness affects a significant number of working-age and economically active individuals.20 A study conducted in China on 1,099 people with COVID-19 found that patients had a mean age of47 years.21 Similarly, a meta-analysis of clinical trials of COVID-19 involving 46,959 individuals infected by SARS-CoV-2 observed that patients had a mean age of 46.62 years and that 55.6% of patients were male (95% confidence interval).40.
The literature shows that infection rates were higher in certain occupational categories and that both occupational activities and working conditions could contribute to exposure to the virus and the spread of disease.22,41 At the start of the outbreak, employees and clients of a wet market in Wuhan, China, were among the first to be infected.42 In Singapore, 68% of the first locally transmitted cases were attributed to occupational activities.41 A study that evaluated confirmed cases of COVID-19 in six Asian territories (Hong Kong, Japan, Singapore, Taiwan, Thailand, and Vietnam) found that 14.9% of cases were associated with work and that the sectors most affected by COVID-19 were health care (22%), transportation (18%), services and sales (18%), cleaning and domestic work (9%) and public safety (7%).(.4) These observations were corroborated by Lan et al.23 A report by the Centers for Disease Control and Prevention reported that 55% of hospitalizations and severe cases were reported in non-white people; the vulnerability of this population was attributed to inequalities in health and housing, as well as the nature of their working conditions.43
It is important to note that, in Brazil, underreporting affects both overall case numbers and estimates of the number of professionals on medical leave, infected or dead as a result of COVID-19. The first confirmed case of COVID-19 in Brazil was reported to the Ministry of Health (Ministério da Saúde; MS) on February 26 2020, but it was only on March 31 2020 that the item “occupation” was included in report forms for patients hospitalized with SARS, which are sent to the Influenza Epidemiological Surveillance System (Sistema de Informação de Vigilância da Gripe; SIVEP-Gripe).20,31 Nevertheless, data from the period of January to the first half of April 2020 revealed that occupation was only reported for 1.7% of the 53,733 cases notified to the SIVEP-Gripe.20 This interferes with occupational health surveillance and risk analysis in different professional categories, hindering the development of strategies to combat the illness in work environments. To date, few studies on COVID-19 have addressed working conditions and organization, with most investigations focusing on individual hygiene and social distancing protocols.20,44
Despite underreporting, the 36th Epidemiological Bulletin issued by the Brazilian MS alerted to the large number of SARS cases and deaths among health care workers. According to this document, by October 17 (at which point Brazil placed third in a global ranking of confirmed cases and second in the number of deaths), health care workers accounted for 23.6% (369,260) of reported cases of COVID-19. Although this does not represent the total number of health professionals infected in the country, it reflects the more severe cases in this population.31 Epidemiological reports from other countries also report the number of cases among health care workers as a percentage of total cases.2,24,45.
These data alert to the importance of occupational health, since studies of patients with SARS caused by previous strains of coronavirus or other viruses altogether have shown that patients can continue to experience physical symptoms (reduced cardiorespiratory function, musculoskeletal limitations, and psychological problems) long after the infection subsides, showing that the illness can have short-, medium- and long-term effects on patients.13,14 It is therefore crucial to develop and implement strategies to support workers in the recovery process since the available data already demonstrates a growing demand for specialized rehabilitation services by patients who recover from COVID-19.15,18
PHYSICAL THERAPY IN MILD AND MODERATE CASES WITHOUT HOSPITALIZATION
The severity of COVID-19 can be classified into four levels: mild, moderate, severe and critical.46 According to the MS, most patients (80%) infected with SARS-CoV-2 are categorized as mild to moderate and have symptoms such as discomfort, fever, fatigue, coughing, mild dyspnea, anorexia, sore throat, generalized pain, headaches, nasal congestion, diarrhea, nausea, and vomiting.5,16 Hyposmia/anosmia and ageusia have also been reported.47
In mild cases, patients have influenza-like symptoms and normal radiological findings, which differs from moderate severity cases.46 It is important to note that fever may not always be present, especially in young or older patients, immunosuppressed individuals, or patients taking antipyretic medication.48 The literature shows that these patients can be treated by symptom management,46 and do not usually require hospitalization. However, they must be isolated at home for 14 days after symptom onset, taking care of their health and preventing the spread of disease. In this situation, non-pharmacological strategies can be used to prevent an aggravated clinical course.48,49
Rehabilitation professionals play a crucial role in the self-isolation period, helping patients optimize their functional independence and improve quality of life. Studies show that, during isolation, patients naturally spend more time sitting or lying down, which may contribute to exercise intolerance, reduced muscle strength, musculoskeletal symptoms such as myofascial pain and arthralgia, and an increased risk of deep vein thrombosis.11 The physical therapy protocol for these patients should include low-intensity aerobic exercises, muscle strengthening, balance training, as well as stretching.50 These recommendations are based on scientific evidence of the role of physical exercise in the strengthening of the cardiovascular and immune systems, as well as the physiological functions of the body.51
In patients with respiratory difficulties, physical therapists can help improve respiratory function and determine whether hospitalization is necessary based on the assessment of dyspnea and oxygen saturation through pulse oximetry (SpO2). According to the literature, respiratory exercises should be recommended in mild cases to assist with the improvement of respiratory health and disease prognosis.52 In patients with cough and difficulty expectorating sputum, secretion clearance techniques should be used. However, these are considered high-risk procedures, as they produce and spread microdroplets, which may increase the risk of transmission of SARS-CoV-2. Therefore, procedures and techniques that involve changes in respiratory flow and secretion drainage should only be considered after a careful risk-benefit analysis.53
In an attempt to reduce infections by the novel coronavirus, physical therapy professional organizations in Brazil have allowed their members to use telemedicine, teleconsultation, and telemonitoring to assist and support patients who require physical interventions.54 This allows professionals to limit their physical contact with patients to cases that require a physical examination or specific procedures.
PHYSICAL THERAPY IN HOSPITALIZED PATIENTS WITH COVID-19
Studies show that 80% of patients diagnosed with COVID-19 do not require hospitalization. The remaining 20% of patients are hospitalized with severe (15%) or critical (5%) forms of the disease, and require access to ICUs.55 To date, the most common symptoms in patients hospitalized for COVID-19 include fever, cough, shortness of breath, muscle aches, mental confusion, headaches, sore throat, rhinorrhea, chest pain, diarrhea, nausea, and vomiting.4,56 An analysis of 1,099 people with COVID-19 admitted to hospitals in China found that lymphopenia and ground-glass opacity were present in 83.2 and 56.4% of patients, respectively.21
Patients with severe forms of the illness have impaired respiratory health, with symptoms such as dyspnea, persistent chest tightness, O2 saturation less than 95% in ambient air, PaO2/FiO2 less than 300 mm Hg, cyanosis, and high fever, which characterize SARS.46 In some cases, myalgia, rhinorrhea, headaches, and bilateral pneumonia have also been observed. Patients who experience respiratory complications must be admitted to intensive care and receive mechanical ventilation for respiratory support.4,55
Critical patients, on the other hand, display respiratory failure, septic shock, and multiple organ failure.46,55 Patients in critical condition also have different degrees of muscle dysfunction and cognitive impairment.12,56 A descriptive exploratory analysis of data from the Chinese infectious disease information system revealed a lethality of 49% in critical cases. Patients with comorbidities (cardiovascular disease, diabetes, chronic respiratory illness, hypertension, and cancer) had higher lethality rates (10.5, 7.3, 6.5, 6 and 5.6%, respectively) than those with no comorbidities.24
Therefore, patients with COVID-19, especially those with fragile health, must be rehabilitated by a multidisciplinary team.18,57 Physical therapists have been highly demanded in hospital settings during the novel coronavirus pandemic since these professionals make important contributions to treatment and recovery in both the early and late stages of illness for hospitalized patients with COVID-19.15
Patients admitted with moderate symptoms can also benefit from physical therapy as a means to prevent symptom aggravation; in these cases, physical therapists also perform a constant assessment of the need for respiratory physical therapy.53 In patients with a productive cough, which according to the literature, account for 34% of cases,21 respiratory training should be prescribed to increase airway permeability and prevent the accumulation of bronchial secretions.25,53 These techniques are thought to improve respiratory mechanics by increasing dynamic lung compliance.58 Such treatments are essential, especially for patients with preexisting comorbidities that can lead to hypersecretion or ineffective coughing, such as neuromuscular or respiratory disease, or cystic fibrosis.25
However, the role of the physical therapist is not restricted to the respiratory system: these professionals play a crucial role for hospitalized patients in the acute stages of illness, as they help minimize or neutralize the negative effects of immobility during hospitalization.15 In these cases, physical therapists perform exercises to increase peripheral muscle strength, change patient positions and promote physical movement to keep the patient active and minimize musculoskeletal complications. However, this type of activity should only be carried out if the patient’s clinical condition allows it;50 there is, as such, a need for continuous monitoring, especially of SpO2 values, to guarantee the safety of the intervention.53
In severe cases, physical therapy is a crucial part of intensive care. Physical therapists are part of the team responsible for the operation of ICUs since they play a crucial role in the management of patients with severe disease who require respiratory support. Their role extends from the early stages of preparation and adjustment of the ventilator, until intubation, weaning, and extubation.59,60 Physical therapists also develop procedures to prevent and/or treat common complications observed in ICU patients, such as neuropathy, myopathy, contractures, thrombosis, and postural instability.10,11
According to Wujtewicz et al.,61 patients with severe disease tend to develop pneumonia, and rapidly progress to acute hypoxemic respiratory failure and severe acute respiratory distress syndrome, requiring supplementary oxygenation. Previous studies have also reported on patients with spontaneous ventilation who suddenly went on to require intubation and mechanical ventilation. Therefore, most if not all patients with severe cases of COVID-19 require oxygen therapy or invasive mechanical ventilation (IMV), which in turn demands intensive physical therapy.59
IMV has been associated with several complications, such as baro/volutrauma, conditioned extinction of upper airway defense mechanisms, need for sedoanalgesia, and increased likelihood of infection. Furthermore, many patients do not tolerate noninvasive mechanical ventilation (NIMV) and develop issues such as skin lesions, eye irritation, dry mucosa, claustrophobia, and lung injury caused by excess oxygen.62,63 These data are concerning, as a study of 302 patients with MERS showed that most (92%) patients who received NIMV required intubation and IMV.64 A study performed by Arabi et al.65 also demonstrated that the time taken to initiate invasive ventilation may have contributed to the high number of deaths. Nevertheless, some studies have found that the high tolerability and comfort of NIMV is associated with the masking of more severe situations and the delayed provision of adequate ventilatory support.62 Since these treatments have both risks and contraindications, they should be performed by trained professionals; only a highly experienced team can manage the particularities of COVID-19 patients and minimize the risks of these procedures.66 Physical therapy interventions such as early mobilization must also be implemented to reduce the severity of the muscle atrophy incurred during intensive care, promote rapid functional recovery and improve independence for activities of daily living. According to several authors, the loss of mobility in patients treated in ICUs can harm several structures and systems, including the respiratory and cardiovascular systems, the muscles, as well as the skin and bones, with impairments beginning within 72 hours of admission.67 In the first 7 days of strict bed rest, muscle strength can decrease by up to 30%, with further decreases of 20% observed in each subsequent week. This restriction leads to alterations in muscle fibers, as well as peripheral and respiratory muscle atrophy, which can hinder extubation, prolonging the need for MV.68
For these reasons, the demand for physical therapists in hospital settings has steadily increased during the COVID-19 pandemic. The work of these professionals in the treatment and recovery of individuals with COVID-19 admitted to health care services, in both the early and late stages of the disease, promotes faster recovery and hospital discharge.15 It is crucial that these treatments be offered to patients, especially those who must return to their occupations as soon as possible. Furthermore, studies show that most patients infected with COVID-19 are actively employed: according to epidemiological studies, the symptoms of COVID-19 are less severe in children than in adults, and only a small share of individuals younger than 19 years develop severe (2.5%) or critical (0.2%) forms of the disease.38
PHYSICAL THERAPY IN POST-ICU RECOVERY AND AFTER HOSPITAL DISCHARGE
Although little is known of the clinical consequences of COVID-19, experts have drawn attention to the long-term effects of ICU admission. ICU survivors with critical illnesses can develop what is known as “post-intensive care syndrome” or “post-ICU syndrome.”11 This condition is characterized by physical, cognitive, and psychological alterations that can reduce quality of life and interfere with the return to work.69
Myhren et al.70demonstrated that 55% of previously active ICU survivors who recover from severe illness return to work or school in the year after discharge. Kamdar et al.71 also demonstrated that, in a sample of 922 survivors of acute respiratory distress syndrome (ARDS) in 43 American hospitals, 44% of patients were unemployed after one year of hospital discharge. The study also noted a 71% reduction in patients’ financial earnings, while the variables most closely associated with unemployment were age and length of hospitalization. According to Simpson and Robinson,11 prolonged immobility is associated with cardiorespiratory deconditioning, postural instability, venous thromboembolism, muscle shortening, as well as myogenic, neurogenic and arthrogenic contractures.
It has also been established that interactions between comorbidities, preexisting chronic illnesses, and complications of acute illness, such as hypotension, hypoxia, hypo- or hyperglycemia, and polyneuromyopathy can contribute to the occurrence of symptoms associated with post-intensive care syndrome in ICU survivors.72 In some clinical groups, up to 100% of ICU survivors experience some degree of cognitive impairment which persists after hospital discharge.73 Surviving acute critical illness does not necessarily imply a return to baseline quality of life after hospital discharge.
These findings have resulted in growing concern regarding COVID-19 survivors who required prolonged hospitalization and ICU admission. Though there is still limited information on the nature and prevalence of post-ICU symptoms experienced by patients with COVID-19, some studies have identified deleterious consequences of prolonged hospitalization in these patients, including cognitive alterations, depression, anxiety, changes in mobility, and delirium, in addition to cardiovascular and pulmonary alterations.26,74
A 2-year retrospective observational study performed in the ICU of a hospital in Portugal demonstrated that most patients with ARDS go on to have severe clinical disease and require prolonged hospitalization. The same study found that 27.5% of cases of ARDS were associated with in-hospital complications, the most frequent of which were ventilation-associated pneumonia, pneumothorax, and ICU-acquired myopathy.75 Furthermore, studies of ARDS survivors, regardless of cause, have confirmed that these patients continue to have compromised health, functional impairments, reduced quality of life, and high health care costs even after ICU discharge.69,76
Evidence of long-term consequences in COVID-19 survivors continues to emerge in the literature. A prospective cohort study performed in Wuhan, China, examined the clinical outcomes of 131 patients (aged 18 to 88) who were discharged from hospital after having COVID-19 (severe and non-severe). The study found that 40.46% of patients had symptoms such as cough, fatigue, expectoration, tightness in the chest, dyspnea, dizziness, palpitations, and lymphopenia. Observational follow-up concluded that 48.09% of patients still had one or more of these symptoms in the first to second week post-discharge. This figure decreased to 13.74% by weeks 3 and 4, but many patients still presented with cough (9.16%), dyspnea (1.53%), pharyngeal pain (1.53%), and nausea (0.76%).77 Halpin et al.27 performed a study of 100 COVID-19 survivors discharged from a large teaching hospital in England (the Leeds Teaching Hospitals NHS Trust) and found that at 4 and 8 weeks post-discharge, patients continued to experience symptoms, the most common of which were muscle fatigue (72% in the ICU group and 60.3% in the ward group), shortness of breath (65.6% in the ICU group and 42.6% in the ward group) and psychological distress (46.9% in the ICU and 23.5% in the ward group).
This is a cause for concern since a follow-up study of SARS survivors revealed that lung damage and functional impairment showed the greatest recovery after 2 years of rehabilitation. The same study also observed using computed tomography that lung and femoral head damage could still be observed in some patients 15 years after hospital discharge.78 As a result, many authors believe that rehabilitation will constitute the second stage of recovery for COVID-19 survivors, with physical and occupational therapists playing a crucial role in the process.15,74
On a similar note, a study of COVID-19 survivors demonstrated that those who participated in a 6-week rehabilitation program showed improvements in lung function, functional capacity, and quality of life relative to a control group.28 Furthermore, a document titled “Rehabilitation consideration during the COVID-19 outbreak,” published by the Pan-American Health Organization, clarified the role of rehabilitation in the long-term management of patients with COVID-19.26
It is therefore crucial that rehabilitation professionals provide continued follow-up to patients infected with SARS-CoV-2, especially those who required intensive care and prolonged hospitalization, since, as the literature shows, COVID-19 can have short-, medium- and long-term effects on functioning, thereby interfering with the return-to-work process.
The present study revealed that COVID-19 affects a significant proportion of the active working population, and can have physical, psychological, and cognitive consequences that result in functional disability, especially for individuals who require prolonged hospitalization and intensive care. The literature has shown that patients with SARS, whether or not it is caused by the novel coronavirus, require physical therapy to prevent and recover from issues that can persist in the short, medium, and long term. Physical therapists must be involved in the battle against this illness to help patients recover their physical function and return to work as quickly, safely, and effectively as possible. Furthermore, though a large number of studies have examined occupational health in association with COVID-19, few have described patients’ occupational activities, which may result in the underreporting of cases and an ineffective analysis of the impact of the illness on different occupational classes.
Footnotes
Funding: None
Conflicts of interest: None
REFERENCES
- 1.Velavan TP, Meyer CG. The COVID-19 epidemic. Trop Med Int Health. 2020;25(3):278–280. doi: 10.1111/tmi.13383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team Vital surveillances: the epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) - China, 2020. China CDC Weekly. 2020;2(8):113–122. [PMC free article] [PubMed] [Google Scholar]
- 3.Garcia LP, Duarte E. Intervenções não farmacológicas para o enfrentamento à epidemia da COVID-19 no Brasil. Epidemiol Serv Saude. 2020;29(2):e2020222. doi: 10.5123/S1679-49742020000200009. [DOI] [PubMed] [Google Scholar]
- 4.Brasil. Ministério da Saúde . Protocolo de Manejo Clínico para o Novo Coronavírus (2019-nCoV) Brasília: Ministério da Saúde; 2020. [Google Scholar]
- 5.Iser BPM, Sliva I, Raymundo VT, Poleto MB, Schuelter-Trevisol F, Bobinski F. Definição de caso suspeito da COVID-19: uma revisão narrativa dos sinais e sintomas mais frequentes entre os casos confirmados. Epidemiol Serv Saude. 2020;29(3):e2020233. doi: 10.5123/S1679-49742020000300018. [DOI] [PubMed] [Google Scholar]
- 6.Driggin E, Madhavan MV, Bikdeli B, Chuich T, Laracy J, Biondi-Zoccai G, et al. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J Am Coll Cardiol. 2020;75(18):2352–2371. doi: 10.1016/j.jacc.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Inciardi RM, Lupi L, Zaccone G, Italia L, Raffo M, Tomasoni D, et al. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5(7):819–824. doi: 10.1001/jamacardio.2020.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Loureiro CMC, Serra JPC, Loureiro BMC, Souza TDM, Góes TM, Neto JSA, et al. Alterações pulmonares na COVID-19. Rev Cient HSI. 2020;4(2):89–99. [Google Scholar]
- 9.Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91–95. doi: 10.1016/j.ijid.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Falvey JR, Krafft C, Kornetti D. The essential role of home- and community-based physical therapists during the COVID-19 pandemic. Phys Ther. 2020;100(7):1058–1061. doi: 10.1093/ptj/pzaa069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Simpson R, Robinson L. Rehabilitation after critical illness in people with COVID-19 infection. Am J Phys Med Rehabil. 2020;99(6):470–474. doi: 10.1097/PHM.0000000000001443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Robinson CC, Rosa RG, Kochhann R, Schneider D, Sganzerla D, Dietrich C, et al. Qualidade de vida pós-unidades de terapia intensiva: protocolo de estudo de coorte multicêntrico para avaliação de desfechos em longo prazo em sobreviventes de internação em unidades de terapia intensiva brasileiras. Rev Bras Ter Intensiva. 2018;30(4):405–413. doi: 10.5935/0103-507X.20180063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lau HM, Lee EW, Wong CN, Ng GY, Jones AY, Hui DS. The impact of severe acute respiratory syndrome on the physical profile and quality of life. Arch Phys Med Rehabil. 2005;86(6):1134–1140. doi: 10.1016/j.apmr.2004.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hui DSC, Wong KT, Antonio GE, Tong M, Chan DP, Sung JJY. Long-term sequelae of SARS: physical, neuropsychiatric, and quality-of-life assessment. Hong Kong Med J. 2009;15(Suppl 8):21–23. [PubMed] [Google Scholar]
- 15.Silva RMV, Sousa AVC. Fase crônica da COVID-19: desafios do fisioterapeuta diante das disfunções musculoesqueléticas. Fisioter Mov. 2020;33:e0033002 [Google Scholar]
- 16.Brasil. Secretaria de Vigilância em Saúde, Ministério da Saúde . Boletim Epidemiológico 08 - Doença pelo novo coronavírus 2019. Brasília: Ministério da Saúde; 2020. [17 fev. 2021]. Disponível em: http://www.cofen.gov.br/wp-content/uploads/2020/04/be-covid-08-final.pdf.pdf. [Google Scholar]
- 17.Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in china. Int J Environ Res Public Health. 2020;17(5):1729–1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Iannaccone S, Castellazzi P, Tettamanti A, Houdayer E, Brugliera L, de Blasio F, et al. Role of rehabilitation department for adult individuals with covid-19: the experience of the San Raffaele Hospital of Milan. Arch Phys Med Rehabil. 2020;101(9):1656–1661. doi: 10.1016/j.apmr.2020.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rede CoVida . Saúde do trabalhador na pandemia de Covid-19: riscos e vulnerabilidades. Salvador: Rede CoVida; 2020. [17 fev. 2021]. Disponível em: https://www.cidadessaudaveis.org.br/cepedoc/wp-content/uploads/2020/06/Relatorio-Saude-do-Trabalhador.pdf. [Google Scholar]
- 21.Guan W, Ni Z, Hu Y, Liang W, Ou C, He J, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baker MG, Peckham TK, Seixas NS. Estimating the burden of United States workers exposed to infection or disease: a key factor in containing risk of COVID-19 infection. PLoS One. 2020;15(4):e0232452. doi: 10.1371/journal.pone.0232452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lan F-Y, Wei C-F, Hsu Y-T, Christiani DC, Kales SN. Work-related COVID-19 transmission in six Asian countries/areas: a follow-up study. PLoS One. 2020;15(5):e0233588. doi: 10.1371/journal.pone.0233588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (covid-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 25.Thomas P, Baldwin C, Bissett B, Boden I, Gosselink R, Granger CL, et al. Physiotherapy management for COVID-19 in the acute hospital setting: clinical practice recommendations. J Physiother. 2020;66(2):73–82. doi: 10.1016/j.jphys.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pan American Health Organization (PAHO) Rehabilitation considerations during the COVID-19 outbreak. Washington, DC: PAHO; 2020. [2021 Feb. 17]. Available from: https://iris.paho.org/bitstream/handle/10665.2/52035/NMHMHCOVID19200010_eng.pdf?sequence=6&isAllowed=y. [Google Scholar]
- 27.Halpin SJ, McIvor C, Whyatt G, Adams A, Harvey O, McLean L, et al. Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: a cross-sectional evaluation. J Med Virol. 2021;93(2):1013–1022. doi: 10.1002/jmv.26368. [DOI] [PubMed] [Google Scholar]
- 28.Liu K, Zhang W, Yang Y, Zhang J, Li Y, Chen Y. Respiratory rehabilitation in elderly patients with COVID-19: A randomized controlled study. Complement Ther Clin Pract. 2020;39:101166–101166. doi: 10.1016/j.ctcp.2020.101166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang TJ, Chau B, Lui M, Lam G-T, Lin N, Humbert S. Physical medicine and rehabilitation and pulmonary rehabilitation for COVID-19. Am J Phys Med Rehabil. 2020;99(9):769–774. doi: 10.1097/PHM.0000000000001505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Carda S, Invernizzi M, Bavikatte G, Bensmaïl D, Bianchi F, Deltombe T, et al. Covid-19 pandemic. What should physical and rehabilitation medicine specialists do? A clinician's perspective. Eur J Phys Rehabil Med. 2020;56(4):515–524. doi: 10.23736/S1973-9087.20.06317-0. [DOI] [PubMed] [Google Scholar]
- 31.Brasil. Secretaria de Vigilância em Saúde. Ministério da Saúde . Boletim Epidemiológico Especial 36 - Doença pelo novo Coronavírus 2019. Brasília: Ministério da Saúde; 2020. [17 fev. 2021]. Disponível em: https://www.gov.br/saude/pt-br/media/pdf/2020/outubro/23/boletim_epidemiologico_covid_36_final.pdf. [Google Scholar]
- 32.Wong G, Liu W, Liu Y, Zhou B, Bi Y, Gao GF. MERS, SARS, and Ebola: the role of super-spreaders in infectious disease. Cell Host Microbe. 2015;18(4):398–401. doi: 10.1016/j.chom.2015.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang H, Penninger JM, Li Y, Zhong N, Slutsky AS. Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: molecular mechanisms and potential therapeutic target. Intensive Care Med. 2020;46:586–590. doi: 10.1007/s00134-020-05985-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gorbalenya AE, Baker SC, Baric RS, Groot RJ, Drosten C, Gulyaeva AA, et al. The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020;5:536–544. doi: 10.1038/s41564-020-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bourgonje AR, Abdulle AE, Timens W, Hillebrands JL, Navis GJ, Gordijn SJ, et al. Angiotensin-converting enzyme 2 (ACE2), SARS-CoV-2 and the pathophysiology of coronavirus disease 2019 (COVID-19) J Pathol. 2020;251(3):228–248. doi: 10.1002/path.5471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hamming I, Timens W, Bulthuis ML, Lely AT, Navis G, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203(2):631–637. doi: 10.1002/path.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.He F, Deng Y, Li W. Coronavirus disease 2019: what we know? J Med Virol. 2020;92(7):719–725. doi: 10.1002/jmv.25766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.World Health Organization (WHO) Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19) Geneva: WHO; 2020. [2021 Feb. 17]. Available from: https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf. [Google Scholar]
- 39.Fang L, Karakiulakis G, Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection. Lancet Respir Med. 2020;8(4):e21. doi: 10.1016/S2213-2600(20)30116-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cao Y, Liu X, Xiong L, Cai K. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2: a systematic review and meta-analysis. J Med Virol. 2020;92(9):1449–1459. doi: 10.1002/jmv.25822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Koh D. Occupational risks for COVID-19 infection. Occup Med (Lond) 2020;70(1):3–5. doi: 10.1093/occmed/kqaa036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Center for Disease Control and Prevention (CDC) COVID-19 in racial and ethnic minority groups. Atlanta: CDC; 2020. [2021 Feb. 17]. Available from: https://www.hsdl.org/?view&did=837299. [Google Scholar]
- 44.Fiho JMJ, Assunção AA, Algranti E, Garcia EG, Saito CA, Maeno M. A saúde do trabalhador e o enfrentamento da COVID-19. Rev Bras Saude Ocup. 2020;45:e14 [Google Scholar]
- 45.European Centre for Disease Prevention and Control (ECDC) Rapid risk assessment: coronavirus disease 2019 (COVID-19) in the EU/EEA and the UK - ninth update. Stockholm: ECDC; 2020. [2021 Feb. 17]. Available from: https://www.ecdc.europa.eu/en/publications-data/rapid-risk-assessment-coronavirus-disease-2019-covid-19-pandemic-ninth-update. [Google Scholar]
- 46.Wang Y, Wang Y, Chen Y, Qin Q. Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures. J Med Virol. 2020;92(6):568–576. doi: 10.1002/jmv.25748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bagheri SH, Asghari A, Farhadi M, Shamshiri AR, Kabir A, Kamrava SK, et al. Coincidence of COVID-19 epidemic and olfactory dysfunction outbreak in Iran. Med J Islam Repub Iran. 2020;34:62–62. doi: 10.34171/mjiri.34.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Brasil. Secretaria de Vigilância em Saúde. Ministério da Saúde . Boletim Epidemiológico 05 - Doença pelo novo coronavírus 2019: ampliação da vigilância, medidas não farmacológicas e descentralização do diagnóstico laboratorial. Brasília: Ministério da Saúde; 2020. Disponível em: https://www.sbmfc.org.br/wp-content/uploads/2020/03/2020_03_13_Boletim-Epidemiologico-05-1.pdf.pdf. [Google Scholar]
- 49.Razai MS, Doerholt K, Ladhani S, Oakeshott P. Coronavirus disease 2019 (covid-19): a guide for UK GPs. BMJ. 2020;368:m800–m800. doi: 10.1136/bmj.m800. [DOI] [PubMed] [Google Scholar]
- 50.Saraiva ACL, Bomfim IS, Alcanfor TAF, Furlanetto KC. Recursos terapêuticos para pacientes com sintomas leves da Covid-19. ASSOBRAFIR Cienc. 2020;11(Suppl 1):65–71. [Google Scholar]
- 51.Sahu A, Naqvi WM. Quarantine exercises in the time of Covid-19 - a review. J Evolution Med Dent Sci. 2020;9(26):1922–1927. [Google Scholar]
- 52.Elias B, Shen C, Bar-Yam Y. Respiratory health for better Covid-19 outcomes. Cambridge: New England Complex Systems Institute; 2020. [2021 Feb. 17]. Available from: https://static1.squarespace.com/static/5b68a4e4a2772c2a206180a1/t/5e6fd1c1fa0fef6906396318/1584386498324/Breathing_for_COVID_19-4.pdf. [Google Scholar]
- 53.Arbillaga A, Pardàs M, Escudero R, Rodríguez R, Alcaraz V, Llanes S, et al. Fisioterapia respiratoria en el manejo del paciente con COVID-19: recomendaciones generales. Barcelona: Sociedad Española de Neumologia e Cirurgía Torácia; 2020. [17 feb. 2021]. Disponible en: http://svmefr.com/wp-content/uploads/2020/03/COVID19-SEPAR-26_03_20.pdf. [Google Scholar]
- 54.Brasil. Conselho Federal de Fisioterapia e Terapia Ocupacional . Resolução no 516, de 20 de março de 2020. Dispõe sobre a suspensão temporária do Artigo 15, inciso II e Artigo 39 da Resolução COFFITO nº 424/2013 e Artigo 15, inciso II e Artigo 39 da Resolução COFFITO nº 425/2013 e estabelece outras providências durante o enfrentamento da crise provocada pela Pandemia do COVID-19. Brasília: Diário Oficial da União; 2020. [17 fev. 2021]. Disponível em: https://www.coffito.gov.br/nsite/?p=15825. [Google Scholar]
- 55.World Health Organization (WHO) Oxygen sources and distribution for COVID-19 treatment centres: interim guidance, 4 April 2020. Geneva: WHO; 2020. [2021 Feb. 17]. Available from: https://apps.who.int/iris/bitstream/handle/10665/331746/WHO-2019-nCoV-Oxygen_sources-2020.1-eng.pdf?sequence=1&isAllowed=y. [Google Scholar]
- 56.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ceravolo MG, de Sire A, Andrenelli E, Negrini F, Negrini S. Systematic rapid "living" review on rehabilitation needs due to COVID-19: update to March 31st, 2020. Eur J Phys Rehabil Med. 2020;56(3):347–353. doi: 10.23736/S1973-9087.20.06329-7. [DOI] [PubMed] [Google Scholar]
- 58.Rosa FK, Roese CA, Savi A, Dias AS, Monteiro MB. Comportamento da mecânica pulmonar após a aplicação de protocolo de fisioterapia respiratória e aspiração traqueal em pacientes com ventilação mecânica invasiva. Rev Bras Ter Intensiva. 2007;19(2):170–175. [PubMed] [Google Scholar]
- 59.Guimarães F. Atuação do fisioterapeuta em unidades de terapia intensiva no contexto da pandemia de COVID-19. Fisioter Mov. 2020;33:e0033001 [Google Scholar]
- 60.Rotta BP, Silva JM, Fu C, Goulardins JB, Pires-Neto RC, Tanaka C. Relação entre a disponibilidade de serviços de fisioterapia e custos de UTI. J Bras Pneumol. 2018;44(3):184–189. doi: 10.1590/S1806-37562017000000196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wujtewicz M, Dylczyk-Sommer A, Aszkielowicz A, Zdanowski S, Piwowarczyk S, Owczuk R. COVID-19 - what should anaethesiologists and intensivists know about it. Anaesthesiol Intensive Ther. 2020;52(1):34–41. doi: 10.5114/ait.2020.93756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pires P, Marques C, Masip J. Cânulas nasais de alto fluxo: uma alternativa de oxigenoterapia na insuficiência respiratória aguda. Med Int. 2018;25(2):123–133. [Google Scholar]
- 63.Silva VZM, Neves LMT, Forgiarini Jr LA. Recomendações para a utilização de oxigênio suplementar (oxigenoterapia) em pacientes com COVID-19. ASSOBRAFIR Cienc. 2020;11(Suppl 1):87–91. [Google Scholar]
- 64.Alraddadi BM, Qushmaq I, Al-Hameed FM, Mandourah Y, Almekhlafi GA, Jose J, et al. Noninvasive ventilation in critically ill patients with the Middle East respiratory syndrome. Influenza Other Respir Viruses. 2019;13(4):382–390. doi: 10.1111/irv.12635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Arabi YM, Arifi AA, Balkhy HH, Najm H, Aldawood AS, Ghabashi A, et al. Clinical course and outcomes of critically ill patients with Middle East respiratory syndrome coronavirus infection. Ann Intern Med. 2014;160(6):389–397. doi: 10.7326/M13-2486. [DOI] [PubMed] [Google Scholar]
- 66.Borges DL, Rapello GVG, Deponti GN, Andre FMD. Posição prona no tratamento da insuficiência respiratória aguda na COVID-19. ASSOBRAFIR Cienc. 2020;11(Suppl 1):111–120. [Google Scholar]
- 67.Castro AAM, Holstein JM. Benefícios e métodos da mobilização precoce em UTI: uma revisão sistemática. Lifestyle J. 2019;6(2):7–22. [Google Scholar]
- 68.Rodrigues GS, Gonzaga DB, Modesto ES, Santos FDO, Silva BB, Bastos VPD. Mobilização precoce para pacientes internados em unidade de terapia intensiva: revisão integrativa. Rev Inspir Mov Saude. 2017;42(13):27–31. [Google Scholar]
- 69.Herridge MS, Moss M, Hough CL, Hopkins RO, Rice TW, Bienvenu OJ, et al. Recovery and outcomes after the acute respiratory distress syndrome (ARDS) in patients and their family caregivers. Intensive Care Med. 2016;42(5):725–738. doi: 10.1007/s00134-016-4321-8. [DOI] [PubMed] [Google Scholar]
- 70.Myhren H, Ekeberg Ø, Stokland O. Health-related quality of life and return to work after critical illness in general intensive care unit patients: a 1-year follow-up study. Crit Care Med. 2010;38(7):1554–1561. doi: 10.1097/CCM.0b013e3181e2c8b1. [DOI] [PubMed] [Google Scholar]
- 71.Kamdar BB, Huang M, Dinglas VD, Colantuoni E, von Wachter TM, Hopkins RO, et al. Joblessness and lost earnings after acute respiratory distress syndrome in a 1-year national multicenter study. Am J Respir Crit Care Med. 2017;196(8):1012–1020. doi: 10.1164/rccm.201611-2327OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Azoulay E, Vincent JL, Angus DC, Arabi YM, Brochard L, Brett SJ, et al. Recovery after critical illness: putting the puzzle together-a consensus of 29. Crit Care. 2017;21(1):296–296. doi: 10.1186/s13054-017-1887-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wilcox ME, Brummel NE, Archer K, Ely EW, Jackson JC, Hopkins RO. Cognitive dysfunction in ICU patients: risk factors, predictors, and rehabilitation interventions. Crit Care Med. 2013;41(9 Suppl 1):S81–S98. doi: 10.1097/CCM.0b013e3182a16946. [DOI] [PubMed] [Google Scholar]
- 74.Orsin M, Nascimento JSF, Azizi MAA, Reis CHM, Nunes NSM, Nascimento JKF, et al. Danos psíquicos durante pandemia por COVID-19 no Brasil. Enferm Bras. 2020;19(3):196–201. [Google Scholar]
- 75.Taborda L, Barros F, Fonseca V, Irimia M, Carvalho R, Diogo C, et al. Síndrome de dificuldade respiratória aguda: casuística de dois anos numa unidade de cuidados intensivos. Acta Med Port. 2014;27(2):211–217. [PubMed] [Google Scholar]
- 76.Ruhl AP, Huang M, Colantuoni E, Lord RK, Dinglas VD, Chong A, et al. Healthcare resource use and costs in long-term survivors of acute respiratory distress syndrome: a 5-year longitudinal cohort study. Crit Care Med. 2017;45(2):196–204. doi: 10.1097/CCM.0000000000002088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wang B, Li R, Lu Z, Huang Y. Does comorbidity increase the risk of patients with COVID-19: evidence from meta-analysis. Aging (Albany NY) 2020;12(7):6049–6057. doi: 10.18632/aging.103000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zhang P, Li J, Liu H, Han N, Ju J, Kou Y, et al. Long-term bone and lung consequences associated with hospital-acquired severe acute respiratory syndrome: a 15-year follow-up from a prospective cohort study. Bone Res. 2020;8:8–8. doi: 10.1038/s41413-020-0084-5. [DOI] [PMC free article] [PubMed] [Google Scholar]