Abstract
The resistance of negative symptoms to pharmacologic treatment has spurred interest in understanding the psychological factors that contribute to their formation and persistence. However, little is understood about the psychological processes that reinforce and sustain the negative symptoms domain of diminished expression. Prior research has shown that higher levels of diminished expression relate to deficits in metacognitive capacity. We propose a more complex model in which diminished expression occurs when impairments in metacognitive self-reflectivity, alterations in higher-order language structure, and cognitive symptoms interact and thus interfere with persons’ ability to understand and express emotions in ways others can recognize. Individuals with schizophrenia-spectrum disorders (N = 201) provided personal narratives detailing their life story and reflections about their mental illness. Self-reflectivity was measured with the Metacognition Assessment Scale-Abbreviated, and situation models were extracted from participants’ personal narratives via Coh-Metrix 3.0, an automated program that calculates language indices. Diminished expression and cognitive symptoms were measured with the Positive and Negative Syndrome Scale. Structural equation models (SEM) examined whether self-reflectivity mediated the impact of cognitive symptoms and situation models on diminished expression. Results of the SEM revealed that self-reflectivity partially mediated the impact of situation models on diminished expression (β = −.073, p = .008, ±95% CI [−0.126, −0.019]). and fully mediated the influence of cognitive symptoms in diminished expression (β = 0.099, p = .001, ±95% CI [0.038, 0.160]). In conclusion, results suggest that self-reflectivity, linguistic cohesion, and cognitive symptoms may be useful targets for intervention in efforts to treat diminished expression in psychosis.
Keywords: Self-reflectivity, Psychosis, Negative symptoms, Expressive deficit, Metacognition, Schizophrenia
1. Introduction
Negative symptomatology is a core feature of schizophrenia that is resistant to treatment and more persistent than other symptoms (Galderisi et al., 2018; Savill et al., 2015). Extensive empirical evidence supports dividing negative symptoms into two domains: avolition/apathy or experiential symptoms and diminished expression or expressive symptoms (Galderisi et al., 2018; Kaiser et al., 2017; Marder and Galderisi, 2017). The experiential domain refers to a reduction in motivation and interest whereas diminished expression refers to impoverished facial and emotional expression, reduced reactivity, as well as poverty of speech (Horan et al., 2011; Kaiser et al., 2017; Kirkpatrick, 2014; Krynicki et al., 2018; Marder and Galderisi, 2017; Messinger et al., 2011). Thus, experiential symptoms reflect impoverished mental states whereas diminished expression reflects a general deficit in capacity to communicate with others about one’s own mental states.
While each domain of negative symptoms may uniquely impact function, to date most research on psychological factors which underpin or sustain negative symptoms has focused on the experiential domain (Kaiser et al., 2017). Regarding the diminished expression domain, research has examined some of the individual aspects of expressive symptoms. Blunted affect, for example, has been suggested to be linked with abnormalities in emotion perception (Lepage et al., 2011) and disorganization of semantic memory (Sumiyoshi et al., 2005). However, there is currently no comprehensive model for diminished expression accounting for the complex interactions between cognitive, affective, and linguistic functions (Kaiser et al., 2017). Building such a model to understand diminished expression may contribute to the design of new treatments or the tailoring of existing treatments to target the debilitating negative symptoms of schizophrenia.
Based on previous research, we propose a three-fold model in which cognitive symptoms, impaired self-reflectivity, and higher-order language disturbances relate to diminished expression in schizophrenia. The first possible set of factors that we propose contribute to diminished expression in schizophrenia are cognitive symptoms. Observable deficits in functions such as attention, abstract and organization of thinking, and cognitive rigidity have been observed to be fundamental in the experience of schizophrenia (Hasson-Ohayon et al., 2018; Minor and Lysaker, 2014), affecting function and disease-course (Metsänen et al., 2006; Rocca et al., 2018). Indeed, they have been linked with negative symptoms (Bora et al., 2009; Torniainen et al., 2012), and following the cognitive resource limitation model (Cohen et al., 2014), they may uniquely contribute to diminished expression. This model proposes that speech production in social interactions is complex and relies upon spontaneously responding to open-ended questions, thus placing high demands on cognitive processes. If such cognitive processes are impaired, individuals may exhibit symptoms of diminished expression through decreased speech production, such as lower word counts, greater pause lengths, and less semantically and lexically intact speech (Chang et al., 2018; Foussias et al., 2014).
A second possible contributing factor to diminished expression in schizophrenia are deficits in self-reflectivity, a domain of metacognition (Semerari et al., 2003). Metacognition refers to a spectrum of mental activities which can range from discrete processes involving noticing specific thoughts and feelings to more synthetic acts in which information is integrated into complex representations of the self and others, enabling individuals to recognize and respond to life challenges (Lysaker et al., 2019). People with schizophrenia have shown impairments in metacognition as compared to controls (Hasson-Ohayon et al., 2015; Lysaker et al., 2014) and these findings have been replicated in people with first episode psychosis (Trauelsen et al., 2016). Central to the proposed model, impairments in the self-reflectivity domain of metacognition have been shown to predict higher concurrent and prospective negative symptoms in schizophrenia (Lysaker et al., 2015, 2020; Mcleod et al., 2014). Self-reflectivity may be uniquely related to diminished expression for several reasons. With low levels of self-reflectivity, persons may not understand how to label and express a given emotion. They may struggle to differentiate inner experience (i.e., thoughts and feelings) from the context in which it emerges and be relatively unable to find ways to understand why and how it has emerged. Accordingly, with deficits in self-reflectivity, any understanding of the reasons for expressing emotions or ways to express emotions so that others might understand may wane, leaving others unable to detect those emotions.
Third, diminished expression may be explained by disturbances in higher-order language structure, which have been commonly reported in schizophrenia (Cohen et al., 2014; DeLisi, 2001). One form of these higher-order structures is referred to as the situation model, which refer specifically to disturbances in causal, intentional, and temporal cohesion of the language. Disturbances in situation models result in a failure of creating a mental representation of the situation expressed in the speech, leading to a lack of comprehension of the situation for the listener. Situation models are discourse markers that reflect the presence of linguistic structures that aid comprehension of the plot and meaning of mental states and actions of persons included in a narrative episode and play an important role in understanding, remembering, and making inferences about life events (van Dijk and Kintsch, 1983; Zwaan, 2016). Decreased incidence of meaningful connections in speech intended to establish temporal, causal, and intentional links across events, emotions, and thoughts ultimately results in reduced cohesion. Situation models can be inferred from people’s speech using recently developed automated analysis methodologies such as the Coh-Metrix tool (McNamara et al., 2014), which can efficiently estimate deep meanings of language processing that are unlikely to be detected using traditional methodologies (e.g. trained raters). In broad support of the present model, studies have found relationships between disorganized semantic associations and negative symptoms, such as alogia (Sumiyoshi et al., 2005). While minimal research has investigated the relationship between situation models and negative symptoms, we predicted that disruptions in the ability to represent complex social interactions in coherent narratives would relate to difficulties expressing information about one’s inner states.
In order to test our three-fold model, the current study explored the relationship between measures of metacognitive self-reflectivity, cognitive symptoms, and situation models and their relationship to diminished expression in schizophrenia. We formed two major hypotheses. First, we hypothesized that the self-reflectivity domain of metacognition would mediate the relationship between cognitive symptoms and diminished expression. Cognitive symptoms have shown consistent associations with lower self-reflectivity capacity, with one interpretation being that basic cognitive abilities facilitate the integration of thoughts and emotion (Lysaker et al., 2008). Additionally, prior studies have found lower metacognition to predict higher levels of negative symptoms, even after controlling for variables such as neurocognition, social functioning, and demographic factors (Lysaker et al., 2015; Mcleod et al., 2014). Another study detected a similar association between self-reflectivity (but not other components of metacognition) and diminished expression but not with experiential symptoms in first-episode psychosis (Austin et al., 2019). Lastly, a recent study found that the ability to use different perspectives when reflecting about the self and others was a mediator of negative symptom severity (García-Mieres et al., 2020).
Second, we hypothesized two significant relationships between situation models and the other constructs in our model. First, we expected that situation models would inversely correlate with cognitive symptoms, as research has suggested that cognitive symptoms are associated with impaired higher-order language construction and verbal processing (O’Leary et al., 2000). Second, we expected that situation models would relate to diminished expression through a mediating pathway of self-reflectivity in schizophrenia. If individuals are unable to form logical, ordered, and complex narratives (i.e., impaired situation models), they may have difficulty making nuanced reflections about their thoughts and affect (i.e., decreased self-reflectivity) and consequently fail to produce emotional and speech expression that may be meaningfully identified by others (i.e., diminished expression). Recent empirical evidence supporting this hypothesis includes findings that individuals with schizophrenia exhibited decreased use of situation models compared to controls (Willits et al., 2018), and lower self-reflectivity was associated with decreased causal and intentional situation models in schizophrenia (Lundin et al., 2020). Thus, the present work moves one step forward by switching the focus from language disturbances and metacognitive process to clinical symptoms and behavior (i.e., diminished expression).
1.1. Aims of the study
We tested whether diminished expression is a reflection of disrupted self-experience. We specifically predicted that self-reflectivity would mediate the relationship of cognitive symptoms and situation models with diminished expression in individuals with schizophrenia.
2. Methods
2.1. Participants
Participants were 201 outpatient adults in a Midwestern Veterans Affair Medical Center with diagnoses of schizophrenia or schizoaffective disorder (see Table 1). All participants were in a post-acute phase of the illness. All participants were recruited from a series of studies exploring the effects of vocational rehabilitation. Common exclusion criteria across all studies included current hospitalization, changes in medication or housing within the past 30 days, current substance dependence, and diagnosis of an intellectual disability.
Table 1.
Demographic and clinical features of participants (N = 201).
| Variable | n | % |
|---|---|---|
| Diagnosis | ||
| Schizophrenia | 135 | 67.2 |
| Schizoaffective disorder | 66 | 32.8 |
| Gender | ||
| Male | 178 | 88.6 |
| Female | 23 | 11.4 |
| Marital status | ||
| Never married | 100 | 49.8 |
| Married | 22 | 10.9 |
| Divorced | 79 | 39.3 |
| Race | ||
| White/Caucasian | 85 | 42.3 |
| Black/African | 113 | 56.2 |
| Hispanic/Latino | 2 | 1.0 |
| Asian | 1 | 0.5 |
| Variable | M(SD) | Range |
| Age | 47.5 (10.6) | 20–71 |
| Years of education | 12.6 (1.97) | 5–20 |
| PANSS Experiential symptoms | 5.80 (1.96) | 2–10 |
| PANSS Diminished Expression | 8.15 (2.69) | 3–15 |
| PANSS Cognitive | 18.2 (4.33) | 8–29 |
| MAS-A Self-reflectivity | 4.22 (1.33) | 1.5–8 |
| Causal Cohesion | 0.474 (0.316) | 0.026–2.46 |
| Intentional cohesion | 0.813 (0.480) | 0.071–3.67 |
| Temporal cohesion | 0.880 (0.032) | 0.795–0.964 |
Note: PANSS, Positive and Negative Symptoms Scale, MAS-A, Metacognition Assessment Scale Abbreviated.
2.2. Measures
Positive symptoms.
Positive symptoms were measured using the Bell et al. (1994) Positive component of the Positive and Negative Syndrome Scale (PANSS; Kay et al., 1987). This positive factor was composed of five PANSS items: unusual thoughts, delusions, suspiciousness, grandiosity, and hallucinations (Bell et al., 1994).
Negative symptoms.
Diminished expression and experiential negative symptoms were measured using the Khan et al. (2017) factor scores for the PANSS. The diminished expression domain was composed of four PANSS items: blunted affect, lack of spontaneity and flow in conversation, poor rapport, and motor retardation. The experiential domain was composed of three PANSS items: apathetic social withdrawal, emotional withdrawal, and active social avoidance.
Cognitive symptoms.
Cognitive symptoms were measured using the Bell et al. (1994) Cognitive component of the PANSS. This domain was composed of seven PANSS items: difficulty in abstract thinking, stereotyped thinking, conceptual disorganization, lack of judgment and insight, poor attention, tension, and mannerisms and posturing (Bell et al., 1994).
Situation models.
Situation models were quantified by conducting automated analysis on speech generated in response to the Indiana Psychiatric Illness Interview (IPII; Lysaker et al., 2002). The IPII is a semi-structured interview that elicits narratives about one’s life and mental illness. It has an open-ended nature that facilitates participants to speak freely with little influence from examiners. IPII interviews usually last 30–60 min in length. Each interview was recorded and transcribed, removing examiner speech prior to linguistic analysis.
Automated analysis was performed using Coh-Metrix 3.0 (McNamara et al., 2014). This discourse processing tool measures coherence and cohesion in speech samples. Its utility has been demonstrated by studies showing that Coh-Metrix cohesion indices predict reader comprehension (Dempsey et al., 2005) and age-appropriate reading level of texts (Dufty et al., 2006). Important to the present study, Coh-Metrix has detected disruptions in language cohesion in individuals with schizophrenia (Willits et al., 2018) and in young persons at ultra-high risk for psychosis (Gupta et al., 2018) compared to a non-psychiatric control group. Further, this tool has shown to be able to differentiate high and low levels of language organization in healthy adults (McNamara et al., 2006). Coh-Metrix produces 108 indices in 11 categories that provide a comprehensive account of language features, ranging from basic to complex processes. Complex indices measure organization within sentences, between sentences, and across paragraphs. For this study, we selected indices that measure three dimensions of situation models, including temporal cohesion, causal cohesion, and intentional cohesion. These indices detect the degree to which meaningful links are present across speech that help others form a deep understanding of the temporal, causal, and goal-driven actions produced within the participants’ narratives, while also controlling for word-length of the narrative. A comprehensive description of these indices appears in Table 1. Coh-Metrix uses WordNet (Miller, 1995a, 1995b) to classify verbs into the categories of causal and intentional verbs.
Self-reflectivity.
The ability for self-reflection was coded using the self-reflectivity subscale of the Metacognitive Assessment Scale – Abbreviated (MAS-A; Lysaker et al., 2005). This scale was adapted from the original Metacognitive Assessment Scale (MAS; Semerari et al., 2003) for its use in schizophrenia and transformed into a scale which estimates the extent to which participants’ ideas about themselves exists along a continuum from fragmentation to integration. This scale is scored from 0 to 9, with higher scores indicating greater integration and capacity for self-reflection. MAS-A scores were made upon the basis of IPII transcripts.
2.3. Procedure
Participants provided written informed consent to study procedures that were approved by Veterans Affairs Institutional Review Boards. A clinical psychologist administered the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID; First et al., 2002) to confirm participant diagnoses of schizophrenia or schizoaffective disorder. Research assistants with a Bachelor’s degree or higher in a field related to psychology administered the IPIIs and PANSS interviews. IPII transcripts were later used to assess metacognition by raters’ blind to PANSS scores. All assessments were part of baseline assessments and performed prior to any intervention.
2.4. Analyses
Descriptive and correlational analyses were computed with Jamovi version 1.0 (jamovi project, 2019). Structural equation modeling (SEM) and mediation analyses were performed with the lavaan package (Oberski, 2014) for the R software (R Development Core Team, 2008). We conducted the statistical analyses in five stages. First, we computed normalized scores of all variables using Bloom’s formula. Second, we obtained descriptive statistics for sociodemographic and clinical measures. Third, we conducted a Pearson correlational analysis for the negative symptom domains of diminished expression and experiential deficits with all other variables as a preliminary exploration of our hypotheses. We also explored correlations between psychotic symptoms and potential demographic covariates such as age and education. Fourth, we constructed latent variables for situation model indices that strongly correlated with one another.
Finally, we conducted SEM to test the proposed model. We only included the Coh-Metrix situation model indices that showed a significant correlation with our variables of interest. The confidence intervals (CI) and standard errors were derived through bootstrapping. Missing data were handled with Full Maximum Likelihood Estimation. Post-hoc model modifications were subsequently formed by examining path coefficients and eliminating non-significant paths that did not contribute to model fit, when theoretically reasonable. This procedure helped to identify better-fitting, and more parsimonious models. Potential mediations were also tested.
In mediation analyses, we explored whether self-reflectivity was a mediator of cognitive symptoms and situation models on diminished expression. When models were significant, we planned to replicate them controlling for potential covariates that reached statistical significance in the correlational analyses. Squared multiple correlations were extracted to get an estimate of the variance explained by the models. We evaluated the fit of the model using the following established indices: the chi-square test, the comparative fit index (CFI), the Tucker-Lewis index (TLI), the Root Mean Square Error of Approximation (RMSEA), and the Standardized Root Mean Square Residual (SRMR), the Akaike Information Criteria (AIC), and the sample-size adjusted Bayesian Information Criteria (BIC). For mediational effects, we used the standardized coefficients as a measure of the effect size of the indirect path. Statistical tests were considered significant at a threshold of p < .05.
3. Results
Descriptive statistics of the clinical measures appear in Table 2. Correlations among the study measures are depicted in Table 3. Means of the Coh-Metrix scores were within 1 standard deviation of established norms (see Appendix B from McNamara et al., 2014). Diminished expression but not experiential symptoms were associated with self-reflectivity, cognitive symptoms, causal cohesion, and intentional cohesion. Temporal cohesion did not correlate with diminished expression or any other measure. Causal and intentional cohesion were highly correlated with one another, so they were combined into the latent variable of “situation model” for the posterior structural equation model. Regarding potential covariates, years of education (r = −0.227, p = .001) significantly correlated with diminished expression, while age did not (r = −0.063, p = .372). Positive symptoms correlated with causal cohesion, so it was included as a possible moderator in the subsequent SEM.
Table 2.
Description of Coh-Metrix indices that represent three dimensions of situation models.
| Measure | Description | Example verbs or time representations | Example connectives |
|---|---|---|---|
| Causal cohesion | The ratio of causal connectives (particles) to causal verbs. This index measures how often participants provide connecting phrases to explain actions or events that have a causal mechanism, such as verbs reflecting a change in state (e.g., an earthquake erupting), which may or may not be driven by the goals of people. | break, freeze, impact, hit, move | because, in order to, so |
| Intentional cohesion | The ratio of intentional connectives to intentional verbs. This index measures how often participants provide connecting phrases to explain events or actions taken in pursuit of human goals (e.g., buying groceries, driving to work). Intentional actions include change verbs, contact verbs, competition verbs, and communicate verbs. | contact, drop, buy, drive, walk, talk | in order to, so that, by means of, by |
| Temporal cohesion | The ratio of temporal connectives to temporal shifts. This index measures how often participants provide connecting phrases to explain shifts in temporal tense and aspect throughout the text. | Tense: past, present, future Aspect: in progress, completed | after, before, until, later on, on the previous day |
Note. Further information on Coh-Metrix 3.0 indices are available in McNamara et al. (2014).
Table 3.
Correlations between positive symptoms, domains of negative symptoms, self-reflectivity, cognitive symptoms and dimensions of situation models.
| Positive symptoms | Diminished expression | Experiential deficits | Self-reflectivity | Cognitive symptoms | Causal cohesion | Intentional cohesion | |
|---|---|---|---|---|---|---|---|
| Diminished expression | 0.031 | – | |||||
| Experiential deficits | 0.387 *** | 0.335 *** | – | ||||
| Self-reflectivity | 0.073 | −0.299 *** | −0.023 | – | |||
| Cognitive symptoms | 0.210 ** | 0.260 *** | 0.135 | −0.360 *** | – | ||
| Causal cohesion | 0.144 * | −0.310 *** | 0.021 | 0.335 *** | −0.271 *** | – | |
| Intentional cohesion | 0.081 | −0.238 *** | 0.041 | 0.260 *** | −0.231 ** | 0.822 *** | – |
| Temporal cohesion | −0.065 | 0.059 | −0.018 | −0.069 | −0.070 | −0.111 | −0.084 |
Note.
p < .05,
p < .01,
p < .001.
3.1. Path analysis
We began with a theoretical path model based on our hypothesis that self-reflectivity would mediate the cognitive symptoms-diminished expression and situation models-diminished expression relationships. We then modified the model by examining the path regressions and removing non-significant paths when theoretically plausible. The basic model testing our hypotheses showed excellent fit to the data, (χ2 (3) = 4.208; p = .240; CFI = 0.99; TLI = 0.99; RMSEA = 0.045; SRMR = 0.03, AIC = 2524.12, BIC = 2580.28) and is depicted in Fig. 1. The model explained 13.8% of variance of diminished expression.
Fig. 1.
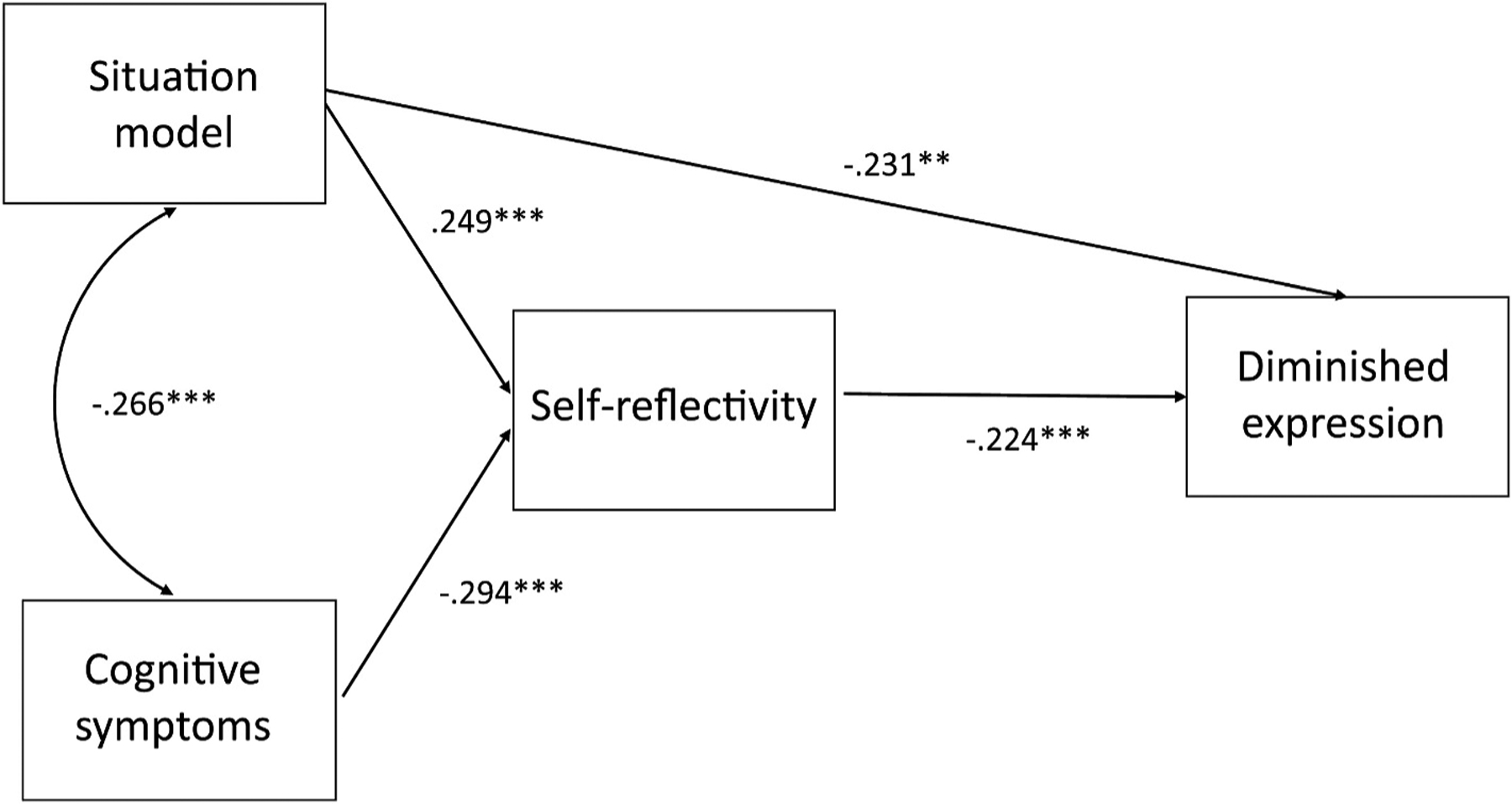
Self-reflectrivity partially mediates the impact of situations models on diminished expression.
Self-reflectivity mediated the relationship between cognitive symptoms and diminished expression (β = .099, p = .001, ±95% CI [0.038, 0.160]). The direct pathway did not remain significant, suggesting full mediation. The paths from cognitive symptoms to self-reflectivity and self-reflectivity to diminished expression both demonstrated significant negative relationships (see Fig. 1). Next, self-reflectivity mediated the relationship between situation models and diminished expression (β = −.073, p = .008, ±95% CI [−0.126, −0.019]). The direct pathway remained significant (β = −0.226, p = .001, ±95% CI [−0.361, −0.090]), suggesting partial mediation. The path from situation models to self-reflectivity had a significant positive association (see Fig. 1). Additionally, situation models and cognitive symptoms showed a significant negative association with one another. Lastly, we tested the model with years of education as a covariate included. Despite the significant influence of years of education on diminished expression in this second model (β = −0.168, p = .017), inclusion of this covariate led to a model with poorer fit to the observed data, (χ2 (7) = 16.31; p = .02; CFI = 0.97; TLI = 0.94; RMSEA = 0.080; SRMR = 0.065, AIC = 3067.34, BIC = 3133.41). Finally, positive symptoms did not act as a significant moderator in any of the pathways of the model. Therefore, our final model did not include years of education or positive symptoms.
4. Discussion
In this study, using a novel methodology we tested the two hypotheses that (i) cognitive symptoms and (ii) reduced situation models in speech would relate to diminished expression through disrupted self-reflectivity. Our findings revealed that the diminished expression domain of negative symptoms, but not the experiential domain, significantly correlated with self-reflectivity, cognitive symptoms, and situation model usage. In support of our central hypotheses, self-reflectivity fully mediated the relationship of cognitive symptoms with diminished expression and partially mediated the association of situation models with diminished expression. Regarding the situation model dimensions, causal and intentional cohesion, but not temporal cohesion significantly correlated with diminished expression.
Cognitive symptoms were related to diminished expression through the pathway of disrupted self-reflectivity. These results may be interpreted as first suggesting that cognitive symptoms may affect a person’s capacity for self-reflection; it seems natural that a basic level of cognitive organization is required for someone to be able to be aware their own mental states. Beyond this basic level, the effects of cognitive symptoms upon diminished expression of emotions and thoughts may be dependent upon a person’s metacognitive capacity for self-reflectivity. It may be, for instance, that deficits in cognition become salient when persons are unable to form awareness and complex knowledge of their own mental states. Other studies have also found that metacognition and cognitive disruptions play a central role in the expression of psychotic symptoms in schizophrenia (Hasson-Ohayon et al., 2018; Minor and Lysaker, 2014).
Next, disturbed language cohesion in causal and intentional relationships partially depended on disrupted self-reflectivity. In other words, the capacity for identification of causal and goal-directed relationships in concrete life events may be a necessary condition to be able to name and form complex ideas about emotional experiences, to connect emotional experiences to interpersonal events, and to express them in ways others can detect. The model also implies that the failure to establish causality and agency in one’s understanding of events may lead more simplistic speech and non-verbal expression that are difficult to understand by others, thus resulting in a failure of expressing thoughts and emotions in a way other people can easily follow. Recent research supports the idea that impairment and disorganization in higher-order levels of language, such as poorer expression of connective threads, may relate to a diminished expression of ideas that are difficult for a listener to understand (Minor et al., 2019).
These findings as a whole are congruent with past research that found greater speech disorganization and greater cognitive disturbances in people with schizophrenia who display poor metacognition (Lysaker et al., 2007; Nicolò et al., 2012). With less capacity for self-reflection, the person may experience their own emotions and thoughts as fragmented and confusing, because pieces of experience appear isolated and disconnected. The person’s inability to understand their own mental states may lead to impoverished speech and poor emotional expression. Overall, these results support Bleuler’s early conception of schizophrenia as a disorder characterized by the fragmentation of previously integrated mental experiences in the three primary areas of psychological function: cognition, emotion, and volition (Bleuler, 1950; Maatz et al., 2015). According to this model, one’s internal states and the surrounding world become confusing when they lose a sense of how thought, emotions, and desires are meaningfully connected to each other. This, in turn, leads to withdrawal.
One unexpected finding was that the temporality dimension of situation models was not significantly related to our variables of interest. It is possible that people with schizophrenia are able to construe events in the order they appear, but they fail to identify how they relate to one another in causal and goal-driven ways. This finding may help to distinguish the complexity of the cognitive and language disturbance present in schizophrenia from the disturbances of other disorders, such as Alzheimer’s, where understanding of temporality can be affected (El Haj and Kapogiannis, 2016). It is also possible that the essential way we ascribe meaning to our life events is by establishing causes and intentions of ourselves and those around us, which implies that people with disrupted cohesion in causal and intentional speech have difficulty perceiving events and the actions of people as interacting dynamically (Noordman and Vonk, 1998). This idea is in line with research that shows that the comprehension of narratives relies more upon understanding the causal relationships relative to the spatial-temporal cues (Magliano et al., 2007) and that the identification of goals within a narrative helps the audience to make more inferences, thus leading to higher comprehension (Costabile, 2016). Alternatively, the temporal cohesion index had low variability in the present sample, which could further explain its non-significant correlations with diminished expression, self-reflectivity, and cognitive symptoms.
Our study has limitations. First, the cross-sectional design of the study prevents drawing conclusions regarding causality. Second, it is unknown whether our results would replicate among individuals with schizophrenia that are younger, female, and those who reject treatment. Third, the IPII narratives were used as speech samples for both situation model analysis and assessment of metacognition. Future studies using separate speech samples at multiple time points should test whether the model results replicate. Fourth, there are some factors, not assessed, that might have influenced the results. Specifically, impairments in emotion recognition, theory of mind, or neurocognition have been largely recognized as playing a role in the expression of negative symptoms (Hartmann-Riemer et al., 2015; Kaiser et al., 2017; Renard et al., 2017). Despite neurocognition having some overlap with cognitive symptoms, this dimension as assessed by the PANSS does not account for specific deficits in executive functioning nor speed of processing (Nielsen et al., 2014). Additionally, we used only one measure to assess expressive and experiential negative symptoms. Future studies are needed that include batteries such as the MATRICS (Nuechterlein et al., 2008) and newer scales to measure negative symptoms such as the CAINS and the BNSS (Lincoln et al., 2017). The model presented in this study represents an advance in the field of understanding diminished expression, but it is conceivable that the limited number of measures employed may have contributed to the small effect size accounted by our model (13.8%). However, at this stage there is no way to determine with certainty whether the variance explained is a fair estimate of the effect or whether more precise measures are needed. Finally, despite the Coh-Metrix tool’s capability to provide comprehensive information about the coherence of language structures, it was developed with an academic text corpus, which may differ from the types of speech used in human conversation.
With replication, these results may have implications for research and clinical practice targeting diminished expression. First, studies using automated analysis for explaining cognitive and clinical processes in schizophrenia are still novel and provide a significant advance in the field. In this sense, previous studies showed that automated analysis for language accounted for more and different variance than traditional clinician-rated measures (Minor et al., 2019). Our findings also support the benefits of implementing a mixed-method approach in research. Second, it should be noted that negative symptoms in general and expressive deficits in particular tend to be persistent (Kelley et al., 2008) and remain a crucial unmet therapeutic need (Galderisi et al., 2018). Interventions which have attempted to tailor treatment towards specific negative symptoms typically focused on the experiential domain (Aleman et al., 2017; Favrod et al., 2019; Nguyen et al., 2016). Experiential deficits are known to be more severe markers of impairment due to their strong influence on the engagement in social meaningful activities and functioning in schizophrenia (Liemburg et al., 2020), with this being the main reason for a stronger research focus on experiential symptoms rather than diminished expression. However, diminished expression may account for specific variability on expressive and conversational skills relevant for social functioning different from experiential deficits, so this domain should not be underestimated. Therefore, our results could contribute to the design of new interventions or the adaptation of existing cognitive interventions to focus on improving diminished expression. For instance, cognitive remediation therapies that target cognitive symptoms and diminished expression may be of benefit to these results, which highlight the importance of metacognitive capacity (Mahmood et al., 2019). In particular, these results support the use of metacognitive interventions that aim to enhance self-reflectivity in schizophrenia, such as Metacognitive Reflection and Insight Therapy (Lysaker et al., 2020; Lysaker and Klion, 2017) or Metacognition Oriented Social Skills Training (Inchausti et al., 2018), a metacognitive intervention with a stronger focus on forming meaningful communicative acts. Following the importance of communication skills, social skills trainings for negative symptoms (Turner et al., 2018) may also be informed by these results, as the mechanisms of change using social skills trainings are still poorly understood (Granholm and Harvey, 2018). The modules of these trainings with a focus on expressive (including appropriate facial expression, verbal content, structure, and amount of speech) and conversational skills may better achieve improvement by incorporating this model into the design of the training when targeting diminished expression in schizophrenia. Such therapies may also assist individuals in crafting complex semantic structures and exercising linguistic abilities, leading to clinical improvement through integration of thoughts and goals (Lundin et al., 2020). Overall, this model aligns with recent holistic and person-centered approaches to treatment of negative symptoms, which are prioritized in current clinical guidelines (e.g., National Institute for Health and Care Excellence, 2014).
Funding
Research supported by grants from The Veterans Rehabilitation Research and Development Service (VA RR&D) D6629R and Indiana University Collaborative Research Grant (Doc # 24787213): Building Statistical Language Processing Algorithms for the Automated Coding of Semi-Structured Interview Data in Clinical Schizophrenia. This research was also supported by a research mobility grant from the Spanish Ministry of Education given to the first author (HGM, grant ref. EST18/0062) the National Institutes of Health United States (NBL, NIMH T32 MH103213), and the National Science Foundation Graduate Research Fellowship Program, United States (NBL, NSF GRFP 1342962).
Footnotes
Data availability statement
Scripts and datasets are available from the authors upon request.
Declaration of competing interest
The authors have no conflicts of interest to declare.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jpsychires.2020.09.008.
References
- Aleman A, Lincoln TM, Bruggeman R, Melle I, Arends J, Arango C, Knegtering H, 2017. Treatment of negative symptoms: where do we stand, and where do we go? Schizophr. Res 186, 55–62. 10.1016/j.schres.2016.05.015. [DOI] [PubMed] [Google Scholar]
- Austin SF, Lysaker PH, Jansen JE, Trauelsen AM, Pedersen MB, Simonsen E, Nielsen H-GL, Pedersen MB, Haahr UH, Simonsen E, 2019. Metacognitive capacity and negative symptoms in first episode psychosis: evidence of a prospective relationship over a 3-year follow-up. J. Exp. Psychopathol 10, 1–11. 10.1177/2043808718821572. [DOI] [Google Scholar]
- Bell MD, Lysaker PH, Beam-Goulet JL, Milstein RM, Lindenmayer J-P, 1994. Five-component model of schizophrenia: assessing the factorial invariance of the positive and negative syndrome scale. Psychiatr. Res 52, 295–303. 10.1016/0165-1781(94)90075-2. [DOI] [PubMed] [Google Scholar]
- Bleuler E, 1950. Dementia Praecox or the Group of Schizophrenias. International Universities Press, New York. [Google Scholar]
- Bora E, Yucel M, Pantelis C, 2009. Cognitive functioning in schizophrenia, schizoaffective disorder and affective psychoses: meta-analytic study. Br. J. Psychiatry 195, 475–482. 10.1192/bjp.bp.108.055731. [DOI] [PubMed] [Google Scholar]
- Chang WC, Kwong VWY, Or Chi Fai P, Lau ESK, Chan GHK, Jim OTT, Hui CLM, Chan SKW, Lee EHM, Chen EYH, 2018. Motivational impairment predicts functional remission in first-episode psychosis: 3-Year follow-up of the randomized controlled trial on extended early intervention. Aust. N. Z. J. Psychiatr 52, 1194–1201. 10.1177/0004867418758918. [DOI] [PubMed] [Google Scholar]
- Cohen AS, McGovern JE, Dinzeo TJ, Covington MA, 2014. Speech deficits in serious mental illness: a cognitive resource issue? Schizophr. Res 160, 173–179. 10.1016/j.schres.2014.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costabile KA, 2016. Narrative construction, social perceptions, and the situation model. Pers. Soc. Psychol. Bull 42, 589–602. 10.1177/0146167216636627. [DOI] [PubMed] [Google Scholar]
- DeLisi LE, 2001. Speech disorder in schizophrenia: review of the literature and exploration of its relation to the uniquely human capacity for language. Schizophr. Bull 27, 481–496. 10.1093/oxfordjournals.schbul.a006889. [DOI] [PubMed] [Google Scholar]
- Dempsey K, McNamara DS, Ozuru Y, Sayroo J, 2005. Effect of text cohesion on comprehension of biology texts. In: Proceedings of the 27th Annual Meeting of the Cognitive Science Society, pp. 1696–1701. [Google Scholar]
- Dufty DF, Graesser AC, Louwerse MM, McNamara DS, 2006. Assigning grade levels to textbooks: is it just readability?. In: Proceedings of the 28th Annual Meeting of the Cognitive Science Society. [Google Scholar]
- El Haj M, Kapogiannis D, 2016. Time distortions in Alzheimer’s disease: a systematic review and theoretical integration. npj Aging Mech. Dis 2 10.1038/npjamd.2016.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Favrod J, Nguyen A, Chaix J, Pellet J, Frobert L, Fankhauser C, Ismailaj A, Brana A, Tamic G, Suter C, Rexhaj S, Golay P, Bonsack C, 2019. Improving pleasure and motivation in schizophrenia: a randomized controlled clinical trial. Psychother. Psychosom 88, 84–95. 10.1159/000496479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First M, Spitzer R, Gibbon M, Williams J, 2002. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. Biometrics Research, New York State Psychiatric Institute, New York, NY. [Google Scholar]
- Foussias G, Agid O, Fervaha G, Remington G, 2014. Negative symptoms of schizophrenia: clinical features, relevance to real world functioning and specificity versus other CNS disorders. Eur. Neuropsychopharmacol 24, 693–709. 10.1016/j.euroneuro.2013.10.017. [DOI] [PubMed] [Google Scholar]
- Galderisi S, Mucci A, Buchanan RW, Arango C, 2018. Negative symptoms of schizophrenia: new developments and unanswered research questions. The Lancet Psychiatry 5, 664–677. 10.1016/S2215-0366(18)30050-6. [DOI] [PubMed] [Google Scholar]
- García-Mieres H, Villaplana A, López-Carrilero R, Grasa E, Barajas A, Pousa E, Feixas G, Ochoa S, 2020. The role of personal identity on positive and negative symptoms in psychosis: a study using the repertory grid technique. Schizophr. Bull 46, 572–580. 10.1093/schbul/sbz082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granholm E, Harvey PD, 2018. Social skills training for negative symptoms of schizophrenia. Schizophr. Bull 44, 472–474. 10.1093/schbul/sbx184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta T, Hespos SJ, Horton WS, Mittal VA, 2018. Automated analysis of written narratives reveals abnormalities in referential cohesion in youth at ultra high risk for psychosis. Schizophr. Res 192, 82–88. 10.1016/j.schres.2017.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartmann-Riemer MN, Hager OM, Kirschner M, Bischof M, Kluge A, Seifritz E, Kaiser S, 2015. The association of neurocognitive impairment with diminished expression and apathy in schizophrenia. Schizophr. Res 169, 427–432. 10.1016/j.schres.2015.10.032. [DOI] [PubMed] [Google Scholar]
- Hasson-Ohayon I, Avidan-Msika M, Mashiach-Eizenberg M, Kravetz S, Rozencwaig S, Shalev H, Lysaker PH, 2015. Metacognitive and social cognition approaches to understanding the impact of schizophrenia on social quality of life. Schizophr. Res 161, 386–391. 10.1016/j.schres.2014.11.008. [DOI] [PubMed] [Google Scholar]
- Hasson-Ohayon I, Goldzweig G, Lavi-Rotenberg A, Luther L, Lysaker PH, 2018. The centrality of cognitive symptoms and metacognition within the interacting network of symptoms, neurocognition, social cognition and metacognition in schizophrenia. Schizophr. Res 202, 260–266. 10.1016/j.schres.2018.07.007. [DOI] [PubMed] [Google Scholar]
- Horan WP, Kring AM, Gur RE, Reise SP, Blanchard JJ, 2011. Development and psychometric validation of the clinical assessment interview for negative symptoms (CAINS). Schizophr. Res 132, 140–145. 10.1016/j.schres.2011.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inchausti F, García-Poveda NV, Ballesteros-Prados A, Ortuño-Sierra J, Sánchez-Reales S, Prado-Abril J, Aldaz-Armendáriz JA, Mole J, Dimaggio G, Ottavi P, Fonseca-Pedrero E, 2018. The effects of metacognition-oriented social skills training on psychosocial outcome in schizophrenia-spectrum disorders: a randomized controlled trial. Schizophr. Bull 44, 1235–1244. 10.1093/schbul/sbx168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- jamovi project, 2019. Jamovi (Version 0.9) [Computer Software]
- Kaiser S, Lyne J, Agartz I, Clarke M, Mørch-Johnsen L, Faerden A, 2017. Individual negative symptoms and domains - relevance for assessment, pathomechanisms and treatment. Schizophr. Res 186, 39–45. 10.1016/j.schres.2016.07.013. [DOI] [PubMed] [Google Scholar]
- Kay SR, Fiszbein A, Opler LA, 1987. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr. Bull 13, 261–276. [DOI] [PubMed] [Google Scholar]
- Kelley ME, Haas GL, van Kammen DP, 2008. Longitudinal progression of negative symptoms in schizophrenia: a new look at an old problem. Schizophr. Res 105, 188–196. 10.1016/j.schres.2008.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan A, Liharska L, Harvey PD, Atkins A, Ulshen D, Keefe RSE, 2017. Negative symptom dimensions of the positive and negative syndrome scale Across geographical regions: implications for social, linguistic, and cultural consistency. Innov. Clin. Neurosci 14, 30–40. 10.1097/01.numa.0000435373.80608.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkpatrick B, 2014. Developing concepts in negative symptoms. J. Clin. Psychiat 75, 3–7. 10.4088/JCP.13049su1c.01. [DOI] [PubMed] [Google Scholar]
- Krynicki CR, Upthegrove R, Deakin JFW, Barnes TRE, 2018. The relationship between negative symptoms and depression in schizophrenia: a systematic review. Acta Psychiatr. Scand 137, 380–390. 10.1111/acps.12873. [DOI] [PubMed] [Google Scholar]
- Lepage M, Sergerie K, Benoit A, Czechowska Y, Dickie E, Armony JL, 2011. Emotional face processing and flat affect in schizophrenia: functional and structural neural correlates. Psychol. Med 41, 1833–1844. 10.1017/S0033291711000031. [DOI] [PubMed] [Google Scholar]
- Liemburg EJ, Enriquez-Geppert S, Wardenaar KJ, Bruggeman R, Aleman A, Castelein S, Knegtering H, Veling W, Alizadeh BZ, van Amelsvoort T, Bartels-Velthuis AA, van Beveren NJ, Bruggeman R, Cahn W, de Haan L, Delespaul P, Luykx JJ, Myin-Germeys I, Kahn RS, Schirmbeck F, Simons CJP, van Haren NE, van Os J, van Winkel R, 2020. Expressive deficits and amotivation as mediators of the associations between cognitive problems and functional outcomes: results from two independent cohorts. Schizophr. Res 218, 283–291. 10.1016/j.schres.2019.12.018. [DOI] [PubMed] [Google Scholar]
- Lincoln TM, Dollfus S, Lyne J, 2017. Current developments and challenges in the assessment of negative symptoms. Schizophr. Res 186, 8–18. 10.1016/j.schres.2016.02.035. [DOI] [PubMed] [Google Scholar]
- Lundin NB, Hochheiser J, Minor KS, Hetrick WP, Lysaker PH, 2020. Piecing together fragments: linguistic cohesion mediates the relationship between executive function and metacognition in schizophrenia. Schizophr. Res 215, 54–60. 10.1016/j.schres.2019.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lysaker PH, Buck KD, Taylor AC, Roe D, 2008. Associations of metacognition and internalized stigma with quantitative assessments of self-experience in narratives of schizophrenia. Psychiatr. Res 157, 31–38. 10.1016/j.psychres.2007.04.023. [DOI] [PubMed] [Google Scholar]
- Lysaker PH, Carcione A, Dimaggio G, Johannesen JK, Nicolo G, Procacci M, Semerari A, 2005. Metacognition amidst narratives of self and illness in schizophrenia: associations with neurocognition, symptoms, insight and quality of life. Acta Psychiatr. Scand 112, 64–71. 10.1111/j.1600-0447.2005.00514.x. [DOI] [PubMed] [Google Scholar]
- Lysaker PH, Clements CA, Plascak-Hallberg CD, Knipscheer SJ, Wright DE, 2002. Insight and personal narratives of illness in schizophrenia. Psychiatry 65, 197–206. 10.1521/psyc.65.3.197.20174. [DOI] [PubMed] [Google Scholar]
- Lysaker PH, Chernov N, Moiseeva T, Sozinova M, Dmitryeva N, Alyoshin V, Faith LA, Karpenko O, Kostyuk G, 2020. Contrasting metacognitive profiles and their association with negative symptoms in groups with schizophrenia, early psychosis and depression in a Russian sample. Psychiatr. Res 10.1016/j.psychres.2020.113177. [DOI] [PubMed] [Google Scholar]
- Lysaker PH, Dimaggio G, Buck KD, Carcione A, Nicolò G, 2007. Metacognition within narratives of schizophrenia: associations with multiple domains of neurocognition. Schizophr. Res 93, 278–287. 10.1016/J.SCHRES.2007.02.016. [DOI] [PubMed] [Google Scholar]
- Lysaker PH, Klion R, 2017. Recovery, Meaning-Making, and Severe Mental Illness: A Comprehensive Guide to Metacognitive Reflection and Insight Therapy, first ed. Routledge, New York. [Google Scholar]
- Lysaker PH, Kukla M, Dubreucq J, Gumley A, Mcleod H, Vohs JL, Buck KD, Minor KS, Luther L, Leonhardt BL, Belanger EA, Popolo R, Dimaggio G, 2015. Metacognitive deficits predict future levels of negative symptoms in schizophrenia controlling for neurocognition, affect recognition, and self-expectation of goal attainment. Schizophr. Res 168, 267–272. 10.1016/j.schres.2015.06.015. [DOI] [PubMed] [Google Scholar]
- Lysaker PH, Minor KS, Lysaker JT, Hasson-Ohayon I, Bonfils K, Hochheiser J, Vohs JL, 2019. Metacognitive function and fragmentation in schizophrenia: relationship to cognition, self-experience and developing treatments, Schizophrenia Research: Cognition. 10.1016/j.scog.2019.100142. [DOI] [PMC free article] [PubMed]
- Lysaker PH, Vohs J, Hamm JA, Kukla M, Minor KS, de Jong S, van Donkersgoed R, Pijnenborg MHM, Kent JS, Matthews SC, Ringer JM, Leonhardt BL, Francis MM, Buck KD, Dimaggio G, 2014. Deficits in metacognitive capacity distinguish patients with schizophrenia from those with prolonged medical adversity. J. Psychiatr. Res 55, 126–132. 10.1016/j.jpsychires.2014.04.011. [DOI] [PubMed] [Google Scholar]
- Maatz A, Hoff P, Angst J, 2015. Eugen Bleuler’s schizophrenia–a modern perspective. Dialogues Clin. Neurosci 17, 43–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magliano JP, Radvansky GA, Copeland DE, 2007. Beyond language comprehension: situation models as a form of autobiographical memory. In: Schmalhofer F, Perfetti CA (Eds.), Higher Level Language Processes in the Brain: Inference and Comprehension Processes. Lawrence Erlbaum Associates Publishers, Mahwah, NJ, US, pp. 379–391. [Google Scholar]
- Mahmood Z, Clark JMR, Twamley EW, 2019. Compensatory Cognitive Training for psychosis: effects on negative symptom subdomains. Schizophr. Res 204, 397–400. 10.1016/j.schres.2018.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marder SR, Galderisi S, 2017. The current conceptualization of negative symptoms in schizophrenia. World Psychiatr. 16, 14–24. 10.1002/wps.20385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mcleod HJ, Gumley AI, Macbeth A, Schwannauer M, Lysaker PH, 2014. Metacognitive functioning predicts positive and negative symptoms over 12 months in first episode psychosis. J. Psychiatr. Res 54, 109–115. 10.1016/j.jpsychires.2014.03.018. [DOI] [PubMed] [Google Scholar]
- McNamara DS, Graesser AC, McCarthy PM, Cai Z, 2014. Automated Evaluation of Text and Discourse with Coh-Metrix. Cambridge University Press., New York, NY. [Google Scholar]
- McNamara DS, Ozuru Y, Graesser AC, Louwerse M, 2006. Validating coh-metrix. In: Sun R, Miyake N (Eds.), Proceedings of the 28th Annual Conference of Cognitive Science Society. Cognitive Science Society, Austin, TX, pp. 573–578. [Google Scholar]
- Messinger JW, Tŕemeau F, Antonius D, Mendelsohn E, Prudent V, Stanford AD, Malaspina D, 2011. Avolition and expressive deficits capture negative symptom phenomenology: implications for DSM-5 and schizophrenia research. Clin. Psychol. Rev 31, 161–168. 10.1016/j.cpr.2010.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metsänen M, Wahlberg K-E, Hakko H, Saarento O, Tienari P, 2006. Thought Disorder Index: a longitudinal study of severity levels and schizophrenia factors. J. Psychiatr. Res 40, 258–266. 10.1016/j.jpsychires.2005.03.004. [DOI] [PubMed] [Google Scholar]
- Miller GA, 1995a. WordNet: a lexical database for English george A. Miller. Commun. ACM 38, 39–41. [Google Scholar]
- Miller GA, 1995b. WordNet: a lexical database for English. Commun. ACM 38, 39–41. [Google Scholar]
- Minor KS, Lysaker PH, 2014. Necessary, but not sufficient: links between neurocognition, social cognition, and metacognition in schizophrenia are moderated by disorganized symptoms. Schizophr. Res 159, 198–204. 10.1016/j.schres.2014.08.005. [DOI] [PubMed] [Google Scholar]
- Minor KS, Willits JA, Marggraf MP, Jones MN, Lysaker PH, 2019. Measuring disorganized speech in schizophrenia: automated analysis explains variance in cognitive deficits beyond clinician-rated scales. Psychol. Med 49, 440–448. 10.1017/S0033291718001046. [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence, 2014. Psychosis and Schizophrenia in Adults: Prevention and Management. [PubMed]
- Nguyen A, Frobert L, McCluskey I, Golay P, Bonsack C, Favrod J, 2016. Development of the positive emotions program for schizophrenia: an intervention to improve pleasure and motivation in schizophrenia. Front. Psychiatr 7 10.3389/fpsyt.2016.00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicolò G, Dimaggio G, Popolo R, Carcione A, Procacci M, Hamm J, Buck KD, Pompili E, Buccione I, Lagrotteria B, Lysaker PH, 2012. Associations of metacognition with symptoms, insight, and neurocognition in clinically stable outpatients with schizophrenia. J. Nerv. Ment. Dis 200, 644–647. 10.1097/NMD.0b013e31825bfb10. [DOI] [PubMed] [Google Scholar]
- Nielsen RE, Lindström E, Telĺeus GK, Levander S, 2014. Is the PANSS cognitive scale measuring cognition? Nord. J. Psychiatry 68, 573–578. 10.3109/08039488.2014.898790. [DOI] [PubMed] [Google Scholar]
- Noordman LGM, Vonk W, 1998. Memory-based processing in understanding causal information. Discourse Process 26, 191–212. 10.1080/01638539809545044. [DOI] [Google Scholar]
- Nuechterlein KH, Green MF, Kern RS, Baade LE, Barch DM, Cohen JD, Essock S, Fenton WS, Frese FJ, Gold JM, Goldberg T, Heaton RK, Keefe RSE, Kraemer H, Mesholam-Gately R, Seidman LJ, Stover E, Weinberger DR, Young AS, Zalcman S, Marder SR, 2008. The MATRICS consensus cognitive battery, Part 1: test selection, reliability, and validity. Am. J. Psychiatr 165, 203–213. 10.1176/appi.ajp.2007.07010042. [DOI] [PubMed] [Google Scholar]
- O’Leary DS, Flaum M, Kesler ML, Flashman LA, Arndt S, Andreasen NC, 2000. Cognitive correlates of the negative, disorganized, and psychotic symptom dimensions of schizophrenia. J. Neuropsychiatry Clin. Neurosci 12, 4–15. 10.1176/jnp.12.1.4. [DOI] [PubMed] [Google Scholar]
- Oberski D, 2014. lavaan.survey: an R package for complex survey analysis of structural equation models. J. Stat. Software 57. 10.18637/jss.v057.i01. [DOI] [Google Scholar]
- R Development Core Team, 2008. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria. [Google Scholar]
- Renard SB, Huntjens RJC, Lysaker PH, Moskowitz A, Aleman A, Pijnenborg GHM, 2017. Unique and overlapping symptoms in schizophrenia spectrum and dissociative disorders in relation to models of psychopathology: a systematic review. Schizophr. Bull 43, 108–121. 10.1093/schbul/sbw063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rocca P, Galderisi S, Rossi A, Bertolino A, Rucci P, Gibertoni D, Montemagni C, Bellino S, Aguglia E, Amore M, Bellomo A, Biondi M, Carpiniello B, Cuomo A, D’Ambrosio E, Dell’Osso L, Girardi P, Marchesi C, Monteleone P, Montemitro C, Oldani L, Pacitti F, Roncone R, Siracusano A, Tenconi E, Vita A, Zeppegno P, Steardo L, Vignapiano A, Maj M, Bracale N, Cardillo S, Brasso C, Andriola I, Romano R, Caforio G, Barlati S, Galluzzo A, Deste G, Pinna F, Lostia di S, Sofia S, Lai A, Signorelli MS, Corbo M, Baroni G, Lupi M, Altamura M, La Montagna M, Malerba S, Murri MB, Corso A, Bugliani M, Pizziconi G, Rossi R, Serrone D, Giusti L, Ussorio D, Salza A, Merlotti E, Piegari G, Patriarca S, Pietrafesa D, de Bartolomeis A, Gramaglia C, Gattoni E, Marangon D, Grottaroli M, Pigoni A, Grassi S, Cremonese C, Meneguzzo P, Collantoni E, Tonna M, Ossola P, Gerra ML, Gesi C, Cremone I, Carpita B, Brugnoli R, Comparelli A, Corigliano V, Di Fabio F, Buzzanca A, Girardi N, Niolu C, Di Lorenzo G, Ribolsi M, Corrivetti G, Bartoli L, Diasco F, Fagiolini A, Bolognesi S, Goracci A, 2018. Disorganization and real-world functioning in schizophrenia: results from the multicenter study of the Italian Network for Research on Psychoses. Schizophr. Res 201, 105–112. 10.1016/j.schres.2018.06.003. [DOI] [PubMed] [Google Scholar]
- Savill M, Banks C, Khanom H, Priebe S, 2015. Do negative symptoms of schizophrenia change over time? A meta-analysis of longitudinal data. Psychol. Med 45, 1613–1627. 10.1017/S0033291714002712. [DOI] [PubMed] [Google Scholar]
- Semerari A, Carcione A, Dimaggio G, Falcone M, Nicolò G, Procacci M, Alleva G, 2003. How to evaluate metacognitive functioning in psychotherapy? The metacognition assessment scale and its applications. Clin. Psychol. Psychother 10, 238–261. 10.1002/cpp.362. [DOI] [Google Scholar]
- Sumiyoshi C, Sumiyoshi T, Nohara S, Yamashita I, Matsui M, Kurachi M, Niwa S, 2005. Disorganization of semantic memory underlies alogia in schizophrenia: an analysis of verbal fluency performance in Japanese subjects. Schizophr. Res 74, 91–100. 10.1016/j.schres.2004.05.011. [DOI] [PubMed] [Google Scholar]
- Torniainen M, Suvisaari J, Partonen T, Castaneda AE, Kuha A, Suokas J, Perälä J, Saarni SI, Lönnqvist J, Tuulio-Henriksson A, 2012. Cognitive impairments in schizophrenia and schizoaffective disorder. J. Nerv. Ment. Dis 200, 316–322. 10.1097/NMD.0b013e31824cb359. [DOI] [PubMed] [Google Scholar]
- Trauelsen AM, Gumley A, Jansen JE, Pedersen MB, Nielsen H-GL, Trier CH, Haahr UH, Simonsen E, 2016. Metacognition in first-episode psychosis and its association with positive and negative symptom profiles. Psychiatr. Res 238, 14–23. 10.1016/j.psychres.2016.02.003. [DOI] [PubMed] [Google Scholar]
- Turner DT, McGlanaghy E, Cuijpers P, van der Gaag M, Karyotaki E, MacBeth A, 2018. A meta-analysis of social skills training and related interventions for psychosis. Schizophr. Bull 44, 475–491. 10.1093/schbul/sbx146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Dijk TA, Kintsch W, 1983. Strategies of Discourse Comprehension. Academic Press, New York, NY. [Google Scholar]
- Willits JA, Rubin T, Jones MN, Minor KS, Lysaker PH, 2018. Evidence of disturbances of deep levels of semantic cohesion within personal narratives in schizophrenia. Schizophr. Res 197, 365–369. 10.1016/j.schres.2017.11.014. [DOI] [PubMed] [Google Scholar]
- Zwaan RA, 2016. Situation models, mental simulations, and abstract concepts in discourse comprehension. Psychon. Bull. Rev 23, 1028–1034. 10.3758/s13423-015-0864-x. [DOI] [PMC free article] [PubMed] [Google Scholar]


