Abstract
Objective:
Uncontrolled hypertension is driven by clinical uncertainty around blood pressure data. This research sought to determine whether decision support—in the form of enhanced data visualization—could improve judgments about hypertension control.
Methods:
Participants (Internet sample of patients with hypertension) in three studies (N=209) viewed graphs depicting blood pressure data for fictitious patients. For each graph, participants rated hypertension control, need for medication change, and perceived risk of heart attack and stroke. In Study 3, participants also recalled the percentage of blood pressure measurements outside of the goal range. The graphs varied by systolic blood pressure mean and standard deviation, change in blood pressure values over time, and data visualization type.
Results:
In all three studies, data visualization type significantly impacted judgments of hypertension control. In Study 1 and 2, perceived hypertension control was lower while perceived need for medication change and subjective perceptions of stroke and heart attack risk were higher for raw data displays compared with enhanced visualization that employed a smoothing function generated by the LOWESS algorithm. In general, perceptions of hypertension control were more closely aligned with clinical guidelines when data visualization included a smoothing function. However, conclusions were mixed when comparing tabular presentations of data to graphical presentations of data in Study 3. Hypertension was perceived to be less well controlled when data was presented in a graph rather than a table, but recall was more accurate.
Conclusion:
Enhancing data visualization with the use of a smoothing function to minimize the variability present in raw BP data significantly improved judgments about hypertension control. More research is needed to determine the contexts in which graphs are superior to data tables.
Keywords: hypertension, data visualization, decision support, risk perception, chronic disease management
Introduction
Prevalence of Hypertension
In the United States alone, over 78 million adults have been diagnosed with hypertension (1). Uncontrolled hypertension is a significant public health problem because it is a major risk factor for morbidity and mortality and it contributes to the risk of heart disease, stroke, and chronic kidney disease. However, there exist multiple drugs that have been shown to effectively treat hypertension. Despite this advance in clinical care, hypertension remains uncontrolled in 47% of these patients. In the Hypertension Clinical Action Model, Kerr and colleagues identified four factors that predict uncontrolled hypertension: 1) Clinical uncertainty; 2) Competing demands and prioritization; 3) Medication-related factors (e.g. side effects); and 4) Organizational factors (2).
Development of Shared Data Visualization
This research was conducted as part of a larger project to develop and test a shared data visualization tool designed for hypertension to be jointly viewed by the provider and patient during a clinic visit. Data visualization for hypertension is not part of the current standard of care for Electronic Health Records (EHRs); current practice tends to be heterogeneous with respect to how home and clinic blood pressure data is reviewed and discussed. However, given the recent proliferation of home measurement devices for health monitoring, EHRs and primary care providers will likely be inundated with home blood pressure data and will need to find methods for employing its use in clinical practice. This data visualization tool was designed with this future wealth of data in mind, which will likely contribute to the clinical uncertainty associated with hypertension management. This tool is designed to address the issue of clinical uncertainty, which arises when patients’ blood pressure data varies by time (e.g., between and within clinic visits) and location (e.g. clinic, home, acute care setting). The shared data visualization tool will summarize home, clinic, and ambulatory blood pressures with the goal of reducing uncertainty—for both the patient and the clinician—about whether a patient’s hypertension is controlled.
In the process of developing this data visualization tool, we conducted a rapid prototyping process in which candidate visualizations were iteratively refined based upon regular feedback from both patients and physicians (3). While working on the prototype displays, we also conducted a series of web studies designed to better understand how characteristics of blood pressure data, such as variability and change over time, affect patient judgments about hypertension control (4). These studies demonstrated that perceived hypertension control is negatively related to variability (i.e., standard deviation) and outliers in the blood pressure data. This is concerning because outliers and variability are not important predictors of hypertension-related health outcomes (e.g., heart attack and stroke) (5). Rather, the single strongest indictor of heart attack and stroke risk was the average blood pressure. Variability, which is inherent in blood pressure measurement, distracts from detection of the mean blood pressure value and masks the presence of data trends, which are more important clinical indicators.
Present Research
The goal of the present research was to examine whether enhanced data visualization techniques can improve patient judgments about hypertension control by reducing their overreliance on blood pressure variation. In Study 1 and 2, we compared participant judgments about hypertension control when the data were presented using a standard raw data display to judgments made viewing enhanced displays featuring a data smoothing line generated by the LOWESS (locally weighted scatterplot smoothing) algorithm (6). This function employs a local regression technique to “smooth” the data by presenting an average value within a given interval size. In Study 3, we compared tabular data displays to graphical data displays. Across three studies, we examined the effect of visualization type on judgments about hypertension control.
Study 1 Method
Materials and Procedure
An Internet sample of patients with hypertension completed a web survey featuring several brief vignettes. Each vignette described a fictitious patient being treated for hypertension and included a graph of the patient’s blood pressure data over the past 2 years. Study 1 employed a 2 (Systolic Blood Pressure [SBP] mean: 130 or 145 mmHg) × 2 (SBP standard deviation: 15 or 25) × 3 (data visualization type: raw data, raw + smoothed, or smoothed only) factorial design resulting in 12 unique vignettes. This was a within-subjects design, where participants reviewed all vignettes, with blocks (raw, raw + smoothed, or smoothed only) presented in random order, and provided judgments about the degree of hypertension control for every patient/vignette.
The goal of this study was to examine whether adding the smoothing line to the raw data (raw + smoothed data display) or providing only the smoothing line without the raw data (data display with smoothing line only) would reduce the influence of blood pressure variability on patients’ judgments about hypertension control. See Appendix A for samples of the three types of data visualization displays used in Study 1.
The mean SBP values were chosen to represent either controlled (mean of 130) or uncontrolled (mean of 145) cases of hypertension according to the 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults from the panel members appointed to the Eighth Joint National Committee (JNC8) (7). The SBP standard deviations were chosen to represent moderate (standard deviation = 15) and large (standard deviation = 25) mean variability according to published SBP values (5).
Outcomes
Primary outcomes were: 1) perceived hypertension control; 2) need for medication change; 3) subjective risk of heart attack; and 4) subjective risk of stroke for each vignette. Perceived hypertension control and need for medication change were assessed using agree-disagree Likert-scales (0–100), while subjective likelihood of heart attack and stroke were measured using unlikely-likely Likert scales (1–10); see Table 2 for item wording. In Study 1, we also asked participants to report which of the three data displays (raw, raw + smoothed, or smoothed only) they found the most useful, helpful, and trustworthy, as well as which display they would be most likely to use and which display they preferred overall.
Table 2.
Participant Characteristicsa
| Participant Characteristics | Study 1 | Study 2 | Study 3 |
|---|---|---|---|
| N | 50 | 81 | 78 |
| Sex, male | 17 (34) | 18 (22) | 30 (38) |
| Age, mean (SD), y | 44.64 (14.74) | 48.00 (13.92) | 57.17 (14.02) |
| Age range, y | 20–76 | 18–77 | 25–80 |
| Race/ethnicity | |||
| White/Caucasian | 39 (78) | 64 (79) | 58 (74) |
| Black/African American | 4 (8) | 11 (14) | 9 (12) |
| Asian/Pacific Islander | 3 (6) | 2 (3) | 2 (3) |
| American Indian/Alaskan Native | 0 (0) | 0 (0) | 2 (3) |
| Hispanic or Latino/a | 4 (8) | 3 (4) | 5 (6) |
| Other | 0 (0) | 1 (1) | 2 (3) |
| Single Item Literacy Screener for health literacy, mean (SD) | 1.82 (0.9) | 1.72 (0.87) | 2.23 (1.13) |
| Subjective Numeracy Scale low health literacy | 11 (22) | 11 (14) | 28 (36) |
| Education | |||
| Some high school | 0 (0) | 0 (0) | 3 (4) |
| High school graduate | 10 (20) | 22 (27) | 17 (22) |
| Some college | 13 (26) | 21 (26) | 15 (19) |
| Vocational training | 2 (4) | 3 (4) | 7 (9) |
| Associate’s degree | 8 (16) | 12 (15) | 9 (12) |
| Bachelor’s degree | 15 (30) | 15 (19) | 15 (19) |
| Master’s degree | 2 (2) | 3 (4) | 9 (12) |
| Professional degree | 1 (2) | 3 (4) | 2 (3) |
| Doctoral degree | 0 (0) | 2 (2) | 1 (1) |
| Income (US dollars) | |||
| Less than $10,000 | 4 (8) | 3 (4) | 3 (4) |
| $10,000–$19,000 | 3 (6) | 7 (9) | 14 (18) |
| $20,000–$29,000 | 5 (10) | 16 (20) | 14 (18) |
| $30,000–$39,000 | 8 (16) | 4 (5) | 12 (15) |
| $40,000–$49,000 | 5 (10) | 8 (10) | 8 (10) |
| $50,000–$59,000 | 5 (10) | 10 (12) | 3 (4) |
| $60,000–$69,000 | 1 (2) | 8 (10) | 7 (9) |
| $70,000–$79,000 | 6 (12) | 7 (9) | 6 (8) |
| $80,000–$89,000 | 3 (6) | 6 (7) | 2 (3) |
| $90,000–$99,000 | 1 (2) | 4 (5) | 0 (0) |
| $100,000–$149,000 | 6 (12) | 7 (9) | 7 (9) |
| Above $149,000 | 3 (6) | 1 (1) | 2 (3) |
| How often do you monitor your BP at home? | |||
| Never | 4 (8) | 14 (17) | 16 (210 |
| Annually | 8 (16) | 7 (9) | 4 (5) |
| Monthly | 14 (28) | 20 (25) | 20 (26) |
| Weekly | 17 (34) | 23 (28) | 29 (37) |
| Daily | 7 (14) | 17 (21) | 9 (12) |
| How often do you graph your home BP measurements? | |||
| Never | 40 (80) | 58 (72) | 56 (72) |
| Annually | 3 (6) | 4 (5) | 2 (3) |
| Monthly | 3 (6) | 6 (7) | 7 (9) |
| Weekly | 3 (6) | 8 (10) | 9 (12) |
| Daily | 1 (2) | 5 (6) | 4 (5) |
BP, blood pressure.
Values are presented as number (%) unless otherwise indicated.
After evaluating all vignettes, participants completed the Subjective Numeracy Scale (SNS) (8) and a Single Item Literacy Screener for health literacy (SILS) (9). Participants also provided demographic information (age, gender, race/ethnicity, education, and income) and responded to two additional items about how often they monitor and graph their own BP.
Power and Statistical Analyses
We planned to recruit 50 patients with hypertension for Study 1. Sample size was determined a priori using G-Power (10, 11) with the following data characteristics: 80% power to detect a significant medium-sized effect (Cohen’s f =0.25) at an alpha level of .05, with a minimum correlation of .50 between repeated measures. All outcomes were treated as continuous variables. We examined the effects of data visualization on our primary outcomes by conducting a series of analysis of variance (ANOVA) tests for repeated measures. Predictors included type of data visualization, mean SBP, and SBP standard deviation. Demographic information, health literacy, and subjective numeracy were not included as predictors in these models because the studies were not powered for their inclusion. All tests were conducted in R version 3.5.3 (12) and were considered statistically significant when P < .05.
Study 1 Results
Participants with hypertension (N=50) were recruited by Qualtrics®, a survey company that maintains an opt-in demographically diverse Internet panel of participants, using a single self-reported measure: ‘Has your doctor ever diagnosed you with hypertension, also known as high blood pressure?’. Similar self-report items have been used to identify patients with hypertension in other epidemiologic studies (13, 14). See Table 1 for complete participant characteristics.
Table 1.
Study 1: Mean (SD)
| Raw | Raw + Smoothed | Smoothed | |
|---|---|---|---|
| This patient’s blood pressure is well controlled. | |||
| (0 = strongly disagree to 100 = strongly agree) | |||
| SBP mean 130 | |||
| SD 15 | 52.30 (4.13) | 67.90 (3.80) | 74.46 (3.37) |
| SD 25 | 27.80 (3.63) | 47.98 (4.31) | 69.00 (3.73) |
| SBP mean 145 | |||
| SD 15 | 26.80 (3.12) | 38.24 (3.90) | 50.30 (4.43) |
| SD 25 | 17.22 (3.13) | 23.16 (3.99) | 20.06 (3.17) |
| This patient needs to change their medication. | |||
| (0 = strongly disagree to 100 = strongly agree) | |||
| SBP mean 130 | |||
| SD 15 | 53.54 (4.32) | 37.76 (4.00) | 31.32 (3.98) |
| SD 25 | 73.84 (3.59) | 56.44 (4.26) | 34.98 (4.17) |
| SBP mean 145 | |||
| SD 15 | 76.02 (3.05) | 61.36 (4.09) | 57.84 (4.29) |
| SD 25 | 85.16 (2.88) | 84.62 (3.23) | 78.78 (3.20) |
| Likelihood of heart attack in the next 10 years. | |||
| (1 = extremely unlikely to 10 = extremely likely) | |||
| SBP mean 130 | |||
| SD15 | 5.12 (0.32) | 4.32 (0.31) | 3.72 (0.31) |
| SD 25 | 7.42 (0.29) | 5.78 (0.33) | 3.94 (0.32) |
| SBP mean 145 | |||
| SD 15 | 7.22 (0.23) | 6.06 (0.28) | 5.52 (0.33) |
| SD 25 | 8.02 (0.28) | 7.84 (0.30) | 7.24 (0.31) |
| Likelihood of stroke in the next 10 years. | |||
| (1 = extremely unlikely to 10 = extremely likely) | |||
| SBP mean 130 | |||
| SD 15 | 5.00 (0.34) | 4.32 (0.32) | 3.56 (0.31) |
| SD 25 | 7.30 (0.33) | 5.78 (5.07) | 4.08 (0.32) |
| SBP mean 145 | |||
| SD 15 | 7.32 (0.26) | 6.04 (0.31) | 5.44 (0.35) |
| SD 25 | 8.10 (0.29) | 7.72 (0.31) | 7.34 (0.32) |
SBP, systolic blood pressure.
We observed a significant main effect of data visualization type on judgments of hypertension control, F (2, 98) = 33.19, p < .001, η2G = .11. Generally, hypertension was perceived to be less controlled when the data visualization included only the raw data and more controlled when the display included the smoothing line only. However, this was qualified by a significant 3-way interaction (SBP mean × SBP standard deviation × data visualization type), F (2, 98) = 13.60, p < .001, η2G = .03. As seen in Figure 1, the pattern described above (perceived hypertension control greater with smoothing line) exists in all cases except when SBP mean was 145 and SBP standard deviation was 25. In this case, hypertension was uncontrolled and variability was maximal and all data visualizations yielded similar judgments. Figure 1 displays the frequency distributions for perceived hypertension control ratings for all 12 data visualizations, which illustrates how the entire distribution of responses is altered by different methods of visualizing the same data. Table 2 displays the means and standard deviations of all four primary outcome measures for each of the 12 data visualizations.
Figure 1.
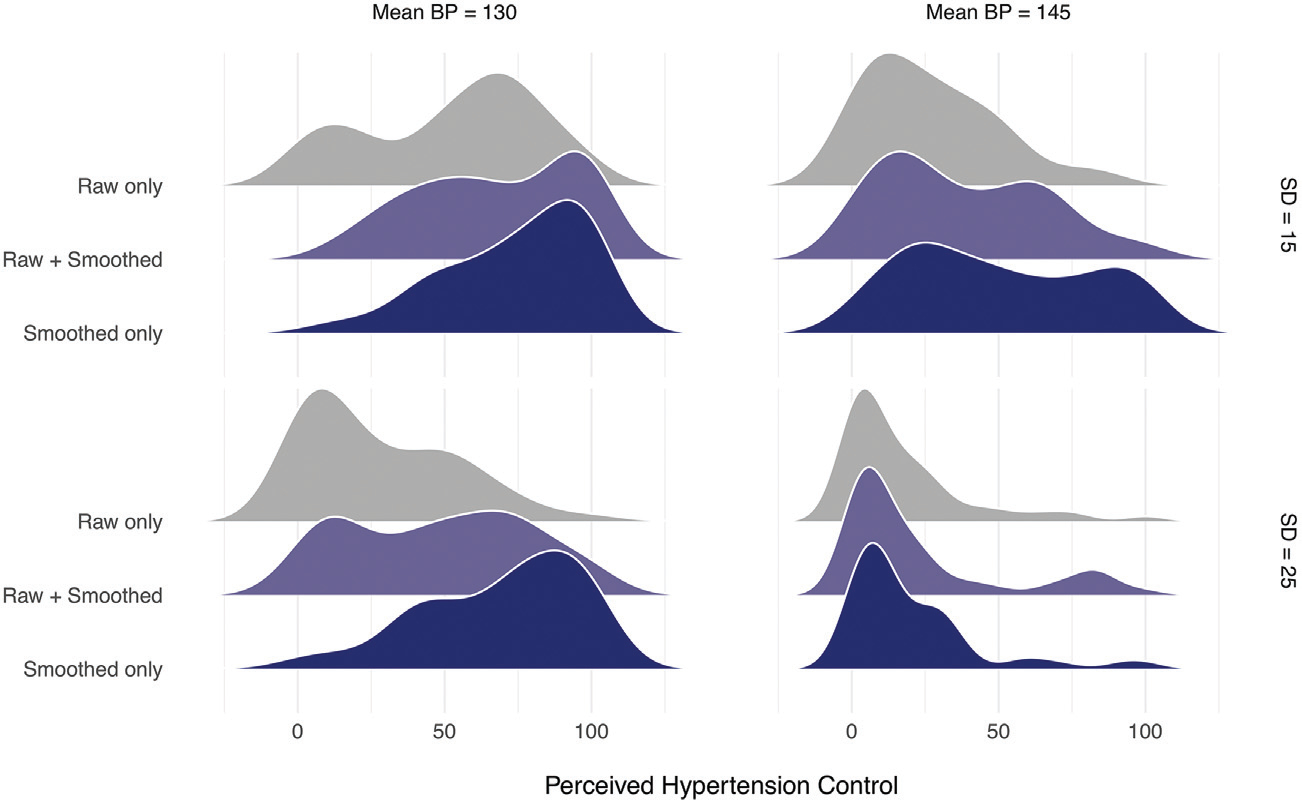
Frequency distributions of perceived hypertension control in Study 1
The same pattern of results exists for the three additional outcome measures. There were significant main effects of data visualization type on perceived need for medication change—F (2, 98) = 28.37p < .001, η2G = .10, heart attack risk—F (2, 98) = 32.34, p < .001, η2G = .09, and stroke risk—F (2, 98) = 32.48, p < .001, η2G = .08. These findings were also qualified by significant 3-way interactions (SBP mean × SBP standard deviation × data visualization type) on perceived need for medication change, F (2, 98) = 5.87, p = .003, η2G = .01, heart attack risk—F (2, 98) = 11.72, p < .001, η2G = .02, and stroke risk—F (2, 98) = 10.60, p < .001, η2G = .02. Again, perceived need for medication change and subjective heart attack and stroke risk were greatest when the data visualization included only the raw data and least when the display included the smoothing line only, with the exception of the case where SBP mean was 145 and the SBP standard deviation was 25 (i.e., uncontrolled hypertension with maximal variability). In this case, judgments were similar across data visualizations.
In addition, we asked about preferences between the three data displays. The raw + smoothed data display was chosen as the most preferred graph overall by 54% of participants; it was also rated as most useful (52%), helpful (56%), and trustworthy (60%) by a majority of the participants. Participants also reported being most likely to use the raw + smoothed display (54%).
Study 2 Methods
Study 2 employed the same procedure as Study 1. We used a 2 (SBP mean: 130 or 145 mmHg) × 3 (absolute value of the slope: 0, 0.50, or 1.0) × 2 (data visualization type: raw or smoothed) factorial design resulting in 12 new vignettes; SBP standard deviation was held constant at 15 mmHg across all vignettes. Slope refers to the change in blood pressure values over time, where slopes of greater magnitude indicate greater change over time. When SBP mean was 130, the slopes were positive, showing blood pressure measurements increasing over time. When SBP mean was 145, the slopes were negative, showing blood pressure measurements that decreased over time. See Appendix B for samples of the data displays used in Study 2. The purpose of this study was to examine whether providing the smoothing line would allow trends in hypertension over time (either increases or decreases) to become more visible to patients, thereby influencing their judgments about hypertension control. We again utilized a within-subjects design, and we chose to compare only the raw data with the smoothed data to minimize response burden on participants.
Study 2 used the same primary outcomes as Study 1 (perceived hypertension control, need for medication change, perceived heart attack risk, and perceived stroke risk) with the same response scales. After evaluating all vignettes, participants also completed the SNS and the SILS and provided the same demographic information as Study 1. Sample size calculations, determined a priori using G-Power (10, 11), indicated that a minimum sample size of 50 would yield 80% power to detect a significant effect at a medium effect size (Cohen’s f =0.25), with type I error rate of .05, and a minimum correlation of .50 between repeated measures.
To examine the impact of SBP mean, SBP slope, and data visualization on our primary outcomes, we conducted a series of analysis of variance (ANOVA) tests for repeated measures. All tests were conducted in R version 3.5.3 (12) and were considered statistically significant when P < .05.
Study 2 Results
Participants (N=81) with hypertension were recruited by Qualtrics using the same method as Study 1. See Table 1 for complete participant characteristics.
Consistent with Study 1, hypertension was perceived to be less controlled when the data was displayed in the raw format compared to when participants viewed the displays with only the smoothing line, F (1, 80) = 45.59, p < .001, η2G = .04. However, there was also a significant 3-way interaction (SBP mean × absolute slope magnitude × data visualization type), F (1, 80) = 6.22, p = .003, η2G = .01. Figure 2 displays frequency distributions for perceived hypertension control, demonstrating that there was a greater discrepancy between perceived hypertension control in the raw and smoothed displays when the SBP mean was 130, controlled hypertension according to clinical guidelines, than when the SBP mean was 145, uncontrolled hypertension.
Figure 2.
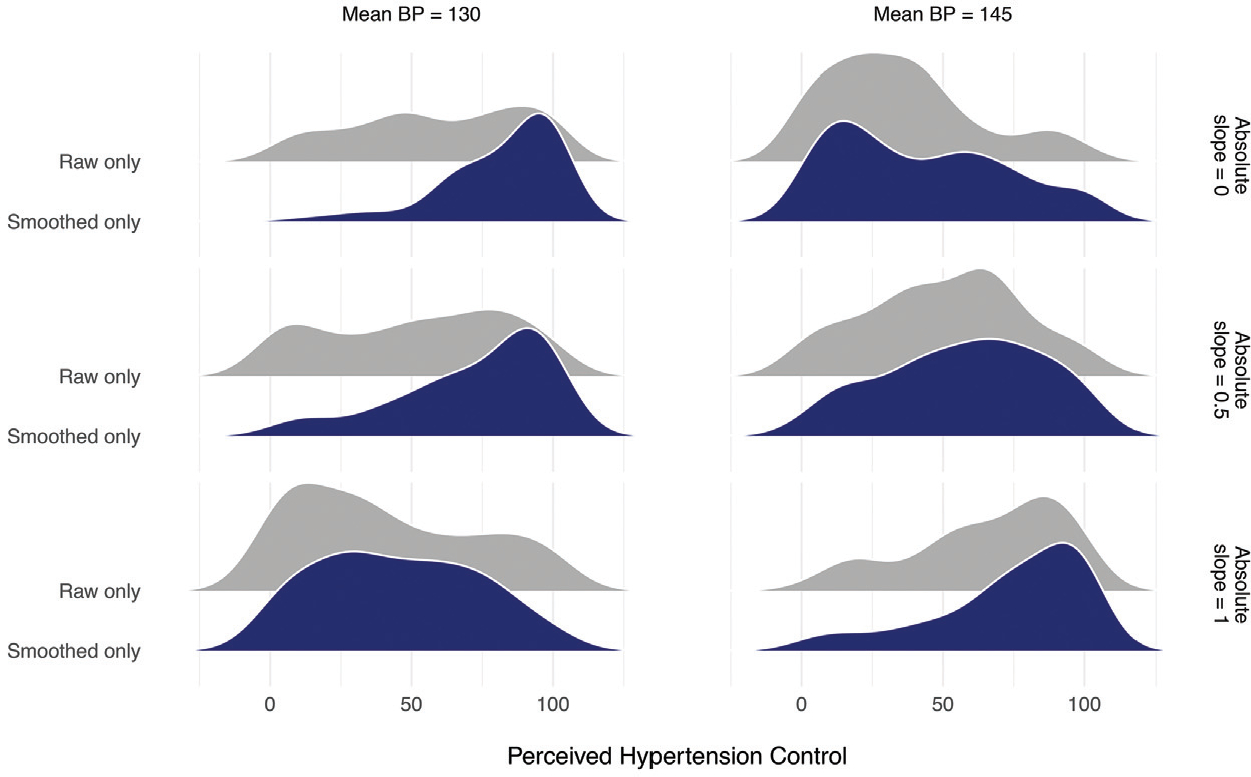
Frequency distributions of perceived hypertension control in Study 2
Perceived hypertension control was also sensitive to change over time (i.e., slope). While there was no main effect of slope, F (2, 160) = 1.55, p = .22, η2G =.002, there was a significant 3-way interaction (SBP mean × absolute slope magnitude × data visualization type), F (2, 160) = 6.23, p = .003, η2G = .01. For vignettes depicting controlled hypertension—when the SBP mean was 130—perception of hypertension control decreased as the slope increased. However, this decrease was sharper for the smoothed data displays than the raw data displays. In contrast, for vignettes with uncontrolled hypertension—when the SBP mean was 145, there was a parallel linear relationship between slope and perceptions of hypertension control for the raw and smoothed data displays. See Table 3 for means and standard deviations.
Table 3.
Study 2: Mean (SD)
| Raw | Smoothed | |
|---|---|---|
| This patient’s blood pressure is well controlled. | ||
| (0 = strongly disagree to 100 = strongly agree) | ||
| SBP mean 130 | ||
| Slope 0 | 58.81 (29.81) | 81.46 (20.97) |
| Slope 0.5 increasing | 51.32 (31.48) | 71.53 (26.51) |
| Slope 1.0 increasing | 41.06 (31.43) | 44.82 (27.63) |
| SBP mean 145 | ||
| Slope 0 | 35.42 (26.30) | 42.18 (29.69) |
| Slope 0.5 decreasing | 49.84 (26.75) | 57.23 (27.74) |
| Slope 1.0 decreasing | 65.13 (26.74) | 72.76 (26.94) |
| This patient needs to change their medication. | ||
| (0 = strongly disagree to 100 = strongly agree) | ||
| SBP mean 130 | ||
| Slope 0 | 47.76 (34.38) | 26.19 (27.41) |
| Slope 0.5 increasing | 52.24 (32.16) | 38.29 (31.81) |
| Slope 1.0 increasing | 72.40 (29.51) | 65.93 (28.29) |
| SBP mean 145 | ||
| Slope 0 | 69.20 (27.12) | 67.68 (27.82) |
| Slope 0.5 decreasing | 60.93 (29.24) | 56.38 (30.10) |
| Slope 1.0 decreasing | 43.39 (31.60) | 34.11 (30.80) |
| Likelihood of heart attack in the next 10 years. | ||
| (1 = extremely unlikely to 10 = extremely likely) | ||
| SBP mean 130 | ||
| Slope 0 | 4.68 (2.66) | 3.28 (2.26) |
| Slope 0.5 increasing | 5.14 (2.63) | 3.93 (2.42) |
| Slope 1.0 increasing | 6.31 (2.56) | 5.67 (2.32) |
| SBP mean 145 | ||
| Slope 0 | 6.42 (2.20) | 5.91 (2.41) |
| Slope 0.5 decreasing | 5.54 (2.05) | 5.16 (2.41) |
| Slope 1.0 decreasing | 4.65 (2.53) | 3.98 (2.43) |
| Likelihood of stroke in the next 10 years. | ||
| (1 = extremely unlikely to 10 = extremely likely) | ||
| SBP mean 130 | ||
| Slope 0 | 4.83 (2.70) | 3.30 (2.23) |
| Slope 0.5 increasing | 5.26 (2.62) | 3.91 (2.34) |
| Slope 1.0 increasing | 6.37 (2.61) | 5.75 (2.34) |
| SBP mean 145 | ||
| Slope 0 | 6.56 (2.15) | 5.97 (2.41) |
| Slope 0.5 decreasing | 5.74 (2.31) | 5.49 (2.49) |
| Slope 1.0 decreasing | 4.78 (2.64) | 3.98 (2.44) |
SBP, systolic blood pressure.
The general patterns were the same for the three additional outcome measures. There were significant 3-way interactions (SBP mean × absolute slope magnitude × data visualization type) for perceived need for medication change—F (2, 164) = 6.29, p = .002, η2G = .01, and stroke risk—F (2, 164) = 3.37, p = .03, η2G = .003, but not for perceived heart attack risk—F (2, 164) = 1.91, p = .15, η2G = .002. However, the important conclusions remain the same. For heart attack risk (along with all other outcomes), the risk was perceived to be greater with the raw data displays compared to the smoothed data displays—F (1, 80) = 27.96, p < .001, η2G = .03.
Study 3 Method
Using the same approach as the two prior studies, Study 3 employed a 2 (SBP mean: 130 or 145 mmHg) × 2 (SBP standard deviation: 15 or 25) × 4 (data visualization type: data table, data table with summary statistics, graph depicting raw data and smoothing line, and graph depicting raw data and smoothing line with an additional linguistic summary) factorial design, resulting in 16 new vignettes. See Appendix C for samples of the data visualization displays used in Study 3. In this study, we compared the effects of displaying blood pressure data in tables versus graphic displays. We tested two different types of data tables: 1) a table that displays all of the individual blood pressure measurements and 2) a table that contains all of the individual measurements and includes a summary table with range of values and mean value for the data displayed in the table. These were compared with two types of graphs: 1) a line graph showing the raw data and the smoothing line and 2) the same line graph with an additional linguistic summary. The linguistic summary includes a sentence that summarizes the display and a sentence that provides direction to the patient about how to proceed. For example, when the display shows blood pressure measurements that are controlled, the linguistic summary reads: “Overall blood pressure is within the healthy goal range. Continue your current treatment plan”. Alternatively, when hypertension is uncontrolled, the linguistic summary reads: “Overall blood pressure is outside of the healthy goal range. Contact your healthcare team.” This data visualization type examines the effect of the presence of these types of summaries, which can be automatically generated with algorithmic and fuzzy logic computational techniques to provide a text summary of numeric data and trends in that data.
In Study 3, we again employed a within-subjects design. To reduce participant response burden, we chose to use only a single data visualization, one that included both the raw data and the smoothing function. Since we opted to use only one type of graph (either with or without the linguistic summary), we chose this visualization type because it included both data elements of interest.
Study 3 employed the same primary outcomes using the same response scales. Additionally, in Study 3, we asked participants to estimate the proportion of SBP values out of range for each vignette [‘What percentage of the patient’s systolic blood pressure values (i.e., top number) would you estimate to be out of the goal range?’]. After evaluating all vignettes, participants also completed the SNS and the SILS and provided the same demographic information as Study 1. Sample size calculations, determined a priori using G-Power (10, 11), indicated that a minimum sample size of 50 would yield 80% power to detect a significant effect at a medium effect size (Cohen’s f =0.25), with type I error rate of .05, and a minimum correlation of .50 between repeated measures.
To examine the impact of SBP mean, SBP SD, and data visualization on our primary outcomes, we conducted a series of analysis of variance (ANOVA) tests for repeated measures. All tests were conducted in R version 3.5.3 (12) and were considered statistically significant when P < .05.
Study 3 Results
Replicating Study 1 and Study 2, perceived hypertension control was lower with higher mean SBP and greater variability. Specifically, in Study 3 we observed a main effect of SBP mean on perceived hypertension control—F (1, 77) = 90.28, p < .001, η2G = 0.09, need for medication change—F (1, 77) = 95.30, p < .001, η2G = 0.11, heart attack risk—F (1, 77) =88.13, p < .001, η2G = 0.08, and stroke risk—F (1, 77) =96.20, p < .001, η2G = 0.07. We also observed a main effect of SBP SD on perceived hypertension control—F (1, 77) = 50.74, p < .001, η2G = 0.02, need for medication change—F (1, 77) = 69.35, p < .001, η2G = 0.02, heart attack risk—F (1, 77) = 53.20, p < .001, η2G = 0.02, and stroke risk—F (1, 77) =51.37, p < .001, η2G = 0.02. In Study 3, we also measured recall for the percentage of SBP values that were out of range. Main effects of SBP Mean—F (1, 77) = 69.21, p < .001, η2G = 0.06—and SD— F (1, 77) = 36.98, p < .001, η2G = 0.01 were observed. Participants correctly recalled that a greater percentage of SBP values were out of range when SBP mean and SD were larger.
Most importantly, there were also significant differences in perception of hypertension control when viewing the different forms of data visualization. Patients judged the same blood pressure data presented in graphical form as less controlled—F (3, 231) = 14.08, p < .001, η2G = 0.03, at greater 10-year risk for heart attack—F (3, 231) = 11.86, p < .001, η2G = 0.02—and stroke—F (3, 231) = 12.26, p < .001, η2G = 0.02, and in greater need of medication change—F (3, 231) = 10.07, p < .001, η2G = 0.02, compared to data presented in tabular form; see Table 4. There was also a main effect of data visualization on recall for the percentage of SBP values out of range, F (3, 231) = 4.62, p = .004, η2G = 0.01. However, recall was actually most accurate after viewing graphical representations and worst after viewing tabular representations. Figure 3 depicts the difference between the recalled percentage of SBP values out of range and the actual number of SBP values out of range. When the recalled value is greater than the actual value, the difference is positive; however, when the recalled value is less than the actual value, the difference is negative. Unlike Study 1 and 2, there were no significant 3-way interactions observed between SBP Mean, SD, and data visualization type for any of the outcome measures, P > .05.
Table 4.
Study 3: Mean (SD)
| Data Table | Data Table + Statistics | Line Graph | Line Graph + Summary | |
|---|---|---|---|---|
| This patient’s blood pressure is well controlled. | ||||
| (0 = strongly disagree to 100 = strongly agree) | ||||
| SBP mean 130 | ||||
| SD 15 | 63.62 (27.67) | 64.38 (29.01) | 58.59 (27.30) | 63.32 (27.89) |
| SD 25 | 54.31 (28.51) | 60.77 (28.97) | 42.35 (29.52) | 44.60 (31.19) |
| SBP mean 145 | ||||
| SD 15 | 38.99 (28.39) | 48.73 (27.41) | 35.24 (27.25) | 35.81 (29.04) |
| SD 25 | 37.31 (29.20) | 44.77 (30.60) | 28.58 (29.73) | 29.81 (28.80) |
| This patient needs to change their medication. | ||||
| (0 = strongly disagree to 100 = strongly agree) | ||||
| SBP mean 130 | ||||
| SD 15 | 41.67 (30.51) | 37.59 (31.12) | 45.37 (30.81) | 41.26 (31.05) |
| SD 25 | 50.74 (29.26) | 45.12 (31.91) | 58.91 (31.67) | 57.10 (32.96) |
| SBP mean 145 | ||||
| SD 15 | 67.64 (24.16) | 55.68 (29.03) | 65.24 (26.20) | 68.77 (26.47) |
| SD 25 | 68.49 (26.77) | 59.63 (29.69) | 76.79 (26.10) | 78.33 (22.90) |
| Likelihood of heart attack in the next 10 years. | ||||
| (1 = extremely unlikely to 10 = extremely likely) | ||||
| SBP mean 130 | ||||
| SD 15 | 4.49 (2.32) | 4.24 (2.35) | 4.87 (2.37) | 4.62 (2.39) |
| SD 25 | 5.06 (2.40) | 4.65 (2.35) | 5.91 (2.43) | 5.53 (2.55) |
| SBP mean 145 | ||||
| SD 15 | 6.19 (2.20) | 5.53 (2.23) | 6.21 (2.20) | 6.14 (2.27) |
| SD 25 | 6.47 (2.27) | 5.73 (2.37) | 7.23 (2.24) | 7.03 (2.17) |
| Likelihood of stroke in the next 10 years. | ||||
| (1 = extremely unlikely to 10 = extremely likely) | ||||
| SBP mean 130 | ||||
| SD 15 | 4.51 (2.40) | 4.49 (2.53) | 5.06 (2.51) | 4.64 (2.47) |
| SD 25 | 5.23 (2.55) | 4.76 (2.49) | 6.03 (2.49) | 5.64 (2.59) |
| SBP mean 145 | ||||
| SD 15 | 6.31 (2.16) | 5.54 (2.34) | 6.33 (2.31) | 6.36 (2.41) |
| SD 25 | 6.55 (2.36) | 5.86 (2.38) | 7.36 (2.27) | 7.17 (2.20) |
SBP, systolic blood pressure.
Figure 3.
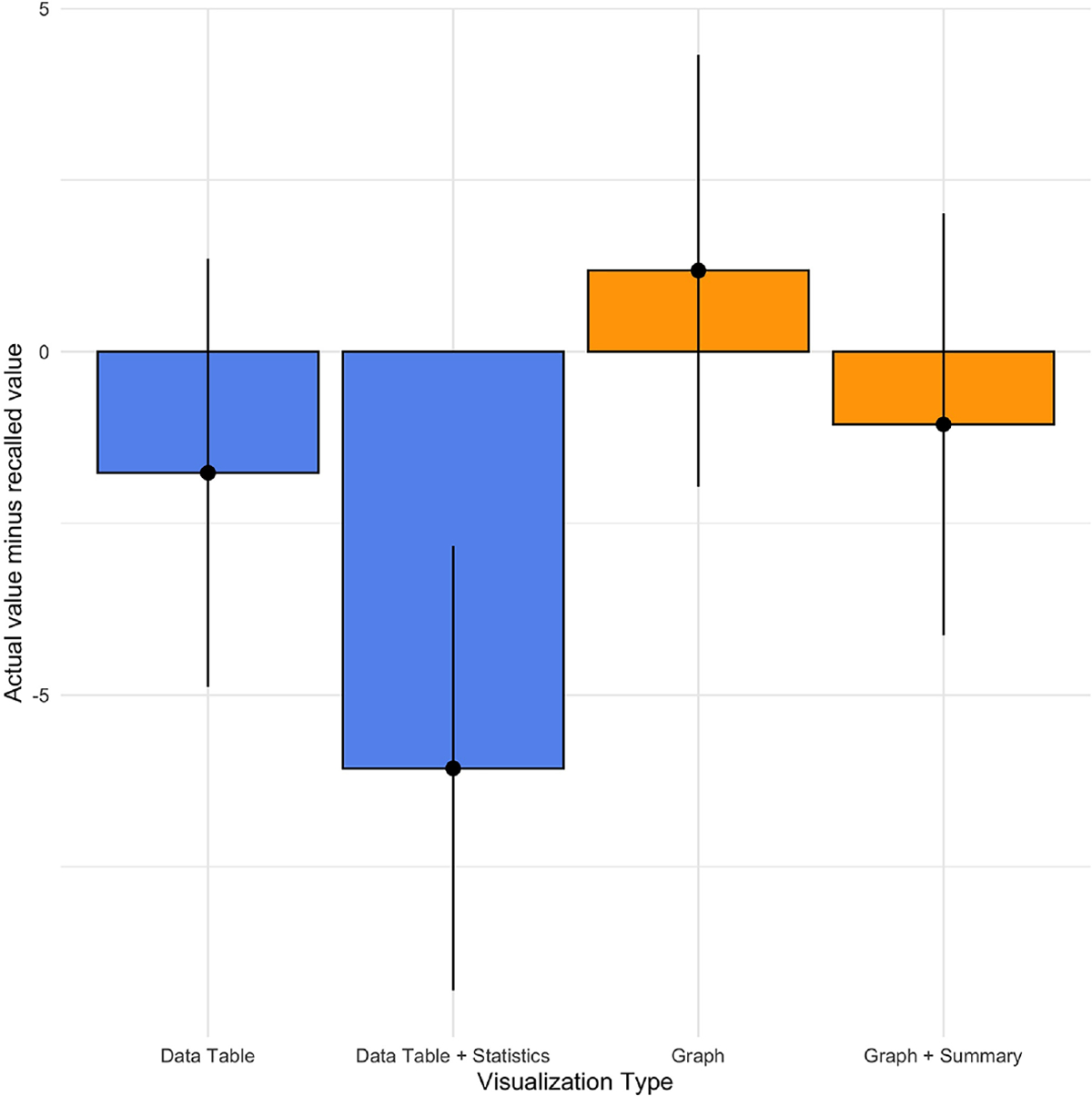
Recall accuracy (actual value – recalled value) by data visualization type, Study 3.
Discussion
To examine whether enhanced data visualization techniques can improve patient judgments by reducing their overreliance on blood pressure variation, we compared judgments about hypertension control when the data were presented using a standard raw data display to judgments made viewing enhanced displays. In Study 1 and Study 2, we compared raw data displays with visualizations that feature a data smoothing line generated by the LOWESS algorithm. In both studies, participants perceived greater hypertension control with displays employing the smoothing function than with raw data displays. The discrepancy between the two displays was greatest when the patient’s hypertension was controlled.
It is of great interest to understand not only how different data visualizations change perceptions of hypertension control but also whether this change results in perceptions that are more or less accurate. In general, we considered judgments about hypertension control to be accurate when they align with published guidelines, e.g. the 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults from the panel members appointed to the Eighth Joint National Committee (JNC8) (7). Based on these guidelines, an SBP mean value of 130 would typically be considered controlled. As seen in Table 2, participants judged hypertension to be uncontrolled for the vignettes with a mean SBP of 130 when the view the raw data displays. By contrast, when participants view the same data with the smoothing function, they perceive hypertension control to be much greater. These latter perceptions align more closely to the JNC-8 guidelines. Therefore, we conclude that the smoothing line produces more “accurate” judgments because participant judgments of hypertension control are more aligned with the judgments made by the clinical experts on our research team and with the JNC-8 guidelines.
Additionally, in Study 2, participants were more sensitive to increases in SBP readings over time when the smoothing function was employed. Given the natural variability inherent in blood pressure measurements, which is due to both measurement error and behavioral factors (e.g. diet, smoking, stress), important increases in blood pressure may not be visible when looking only at the raw data. Therefore, enhanced data visualization with a smoothing function can help reduce focus on variation due to “noise” and make important trends more noticeable.
In Study 3, we examined the effect of data visualization type on patient judgments of hypertension control, comparing two types of graphical displays with two types of data tables. Results about the superiority of given data presentation method were mixed. Patients judged blood pressure data presented in a graphical form as less controlled and at increased heart attack and stroke risk compared to data presented in tabular form. Judgments based on data tables were generally more closely aligned with clinical guidelines in that perceived hypertension control was greater with tables than graphs in the cases where hypertension was in fact controlled (e.g. SBP mean=130). While Study 1 and 2 did not include a data table condition, the differences in findings may also be due to the fact that Study 3 only employed a visualization that included both the raw data and the smoothing function. However, recall for the percentage of SBP values out of target range was more accurate with graphical representations than tabular representations. Therefore, choice of graphical versus tabular display may be dependent upon clinical goals. Future research is needed to understand the contexts in which data tables may be superior to graphical visualizations.
Together, these three studies suggest that visualizing blood pressure data via graphical representations with smoothing functions may improve judgments about hypertension control. The smoothing line minimizes the effect of blood pressure variability on judgments of hypertension control, which is in line with clinical research suggesting than mean blood pressure values are the most important predictors of negative health outcomes (5). Further, these enhanced displays can make important trends more visible. Reducing uncertainly about the state of blood pressure control through graphical representation may help patients and their physicians overcome at least one of the barriers to blood pressure control in Kerr’s model (2).
The smoothing line effectively masks extreme variability which can capture the attention of patients and clinicians without meaningfully improving judgments of hypertension control. Another potential approach to improving correspondence between patient judgments and clinical guidelines would be to simply direct patients to attend to the average blood pressure values and to ignore any extreme values. Although this is a more parsimonious approach than developing sophisticated data visualization tools, there is a rich history of research in judgment and decision making showing that these type of informational correction strategies are fairly ineffective at debiasing (15, 16). However, this remains an empirical question in this specific context; therefore, future research should compare the effects of information correction strategies and other patient education efforts with enhanced data visualizations on judgments of hypertension control.
More work is needed to understand when data tables may provide greater benefit than graphical visualizations. In Study 3, perceptions of hypertension control were more closely aligned with clinical guidelines (i.e. hypertension control was deemed greater when the SBP mean was within the “normal” range) when participants viewed blood pressure data in tabular form. However, recall for the percentage of values outside the goal range was more accurate with the use of graphs. Tabular presentations may promote more informed judgments, although more research is needed to compare tables to visualizations without raw data. Alternatively, graphical representations—more than tabular displays—may promote a greater willingness to intensify medication by highlighting the number of times that blood pressure measurements exceeded the recommended goal range.
Limitations
There are some limitations to these studies that potentially minimize their ability to inform clinical encounters. The primary limitations are the use of Internet patient samples and vignette-based studies. Patient judgments were made without a physician guiding their interpretation; interactions within a clinic visit may alter patient responses. Additionally, participants in this study were asked to make judgments about hypertension control for other patients, not themselves. Given the literature on self-other differences (e.g., 17), these findings may not generalize when patients make judgments about their own data. Further, we focused only on patients in these studies, which represent only one half of the dyad. Future research should examine the effect of data visualization on physicians’ judgments about hypertension control, as well as the effect on shared patient-physician decisions. It is likely that physician judgments will be similar to patients because we are examining judgments that stem from common perceptual and cognitive processes (18, 19).
Conclusions
This work has important implications for the design of data displays in the Electronic Medical Record and patient portal platforms. The format of data visualization significantly impacts judgments of hypertension control. The traditional raw data displays may be less effective in communicating about hypertension control to patients. A smoothing function that visually minimizes the inherent variability in blood pressure data can drive more accurate perceptions of hypertension control, which may help to overcome the clinical inertia documented in the management of hypertension (2). Enhanced data visualization has the potential to improve patient and physician understanding of hypertension control, enhance the shared decision making process, and encourage intensification of anti-hypertensive therapy as needed.
Supplementary Material
Acknowledgments
This research was presented at the 2017 and 2018 Annual Meetings of the Society for Medical Decision Making. This project was supported by grant number R01HS023328 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.1
Footnotes
Financial support for these studies was provided entirely by a grant from the Agency for Health Care Research and Quality. The funding agreement ensured the authors’ independence in designing the study, interpreting the data, writing, and publishing the report.
Contributor Information
Victoria A Shaffer, Department of Psychological Sciences, University of Missouri, USA.
Pete Wegier, Temmy Latner Centre for Palliative Care, Sinai Health System & University of Toronto, CA.
KD Valentine, Health Decision Sciences Center, Massachusetts General Hospital & Harvard Medical School, USA.
Mihail Popescu, Department of Health Management and Informatics, University of Missouri, USA.
Linsey M Steege, School of Nursing, University of Wisconsin-Madison, USA.
Akshay Jain, Department of Electrical and Computer Engineering, University of Missouri, USA.
Richelle J Koopman, Department of Family and Community Medicine, University of Missouri, USA.
References
- 1.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, et al. Executive summary: heart disease and stroke statistics—2013 update: A report from the American Heart Association. Circulation. 2013;127(1):143–52. [DOI] [PubMed] [Google Scholar]
- 2.Kerr EA, Zikmund-Fisher BJ, Klamerus ML, Subramanian U, Hogan MM, Hofer TP. The role of clinical uncertainty in treatment decisions for diabetic patients with uncontrolled blood pressure. Annals of Internal Medicine. 2008;148(10):717–27. [DOI] [PubMed] [Google Scholar]
- 3.Wegier P, Belden JL, Canfield SM, Patil SJ, Shaffer VA, Steege LM, et al. Designinig data visualizations to support shared decision making about blood pressure. Annual Meeting of the Society for Medical Decision Making; Vancouver, CA2016. [Google Scholar]
- 4.Shaffer VA, Wegier P, Valentine K, Belden JL, Canfield SM, Patil SJ, et al. Patient judgments about hypertension control: The role of variability, trends, and outliers in visualized blood pressure sata. Journal of Medical Internet Research. 2019;21(3):e11366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hansen TW, Thijs L, Li Y, Boggia J, Kikuya M, Björklund-Bodegård K, et al. Prognostic value of reading-to-reading blood pressure variability over 24 hours in 8938 subjects from 11 populations. Hypertension. 2010;55(4):1049–57. [DOI] [PubMed] [Google Scholar]
- 6.Cleveland WS, Devlin SJ. Locally weighted regression: An approach to regression analysis by local fitting. Journal of American Statistical Association. 1988;83(403):596–610. [Google Scholar]
- 7.James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507–20. [DOI] [PubMed] [Google Scholar]
- 8.Fagerlin A, Zikmund-Fisher BJ, Ubel PA, Jankovic A, Derry HA, Smith DM. Measuring numeracy without a math test: Development of the subjective numeracy scale. Medical Decision Making. 2007;27(5):672–80. [DOI] [PubMed] [Google Scholar]
- 9.Morris NS, MacLean CD, Chew LD, Littenberg B. The Single Item Literacy Screener: Evaluation of a brief instrument to identify limited reading ability. BMC Family Practice. 2006;7(1):21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Faul F, Erdfelder E, Buchner A, Lang A-G. Statistical power analyses using G* Power 3.1: Tests for correlation and regression analyses. Behavior Research Methods. 2009;41(4):1149–60. [DOI] [PubMed] [Google Scholar]
- 11.Faul F, Erdfelder E, Lang A-G, Buchner A. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods. 2007;39(2):175–91. [DOI] [PubMed] [Google Scholar]
- 12.Team RC. R: A language environment for statistical computing. In: Team RC, editor. Vienna, Austria: R Foundation for Statistical Computing; 2018. [Google Scholar]
- 13.Centers for Disease Control and Prevention. Vital signs: awareness and treatment of uncontrolled hypertension among adults--United States, 2003–2010. 2012. Report No.: 1545–861X. [PubMed] [Google Scholar]
- 14.Diaz VA, Mainous AG, Koopman RJ, Geesey ME. Undiagnosed obesity: implications for undiagnosed hypertension, diabetes, and hypercholesterolemia. Family Medicine. 2004;36:639–44. [PubMed] [Google Scholar]
- 15.Arkes HR. Costs and benefits of judgment errors: Implications for debiasing. Psychological Bulletin. 1991;110(3):486. [Google Scholar]
- 16.Wilson TD, Brekke N. Mental contamination and mental correction: unwanted influences on judgments and evaluations. Psychological Bulletin. 1994;116(1):117. [DOI] [PubMed] [Google Scholar]
- 17.Zikmund‐Fisher BJ, Sarr B, Fagerlin A, Ubel PA. A matter of perspective: choosing for others differs from choosing for yourself in making treatment decisions. Journal of General Internal Medicine. 2006;21(6):618–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Belden JL, Patel J, Lowrance N, Plaisant C, Koopman RJ, Moore J, et al. Inspired EHRs: Designing for Clinicians 2014. Available from: http://inspiredehrs.org/designing-for-clinicians/e-prescribing.php.
- 19.Ware C. Visual queries: The foundation of visual thinking: Springer; 2005. 27–35 p. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


