Abstract
Objective
During the deconfinement period after the coronavirus disease-2019 (COVID-19) pandemic, the number and characteristics of psychiatric visits changed in our emergency department (ED). We aimed to assess changes in the number of visits and characterize the profiles of these patients.
Methods
In this retrospective observational study, we examined the number of psychiatric ED visits and their proportion among the total number of ED visits. We also evaluated psychiatric visits characteristics during a one-month period after the declaration of deconfinement, and we compared those characteristics to characteristics observed during the same month over the previous 4 years.
Results
The number of psychiatric visits to our emergency department during deconfinement was similar to the number observed in the same month of previous years. However, the proportion of psychiatric visits to our emergency department among all visits to the ED rose during deconfinement to a level never before observed. The mean proportion of psychiatric admissions to all ED admissions rose from 3.5% in past years to 5.3% during deconfinement (p = 0.013). Moreover, during deconfinement, more visits (80%) were without an acute intoxication compared to past years (58.5%; p = 0.031). Also, in the deconfinement period, more visits lacked a follow-up consultation organized at discharge (40%) compared to the historical period (25%, p = 0.036).
Conclusions
The deconfinement period after the first wave COVID-19 changed the number and type of psychiatric emergency medicine consultations at our hospital, suggesting a psychiatric impact of confinement during this pandemic. These findings will be of interest to practitioners and politicians in the coming months.
Keywords: Psychiatric, Deconfinement, Emergency, COVID-19
1. Introduction
After the first wave of coronavirus disease-2019 (COVID-19) outbreak, the Belgian government decided that the confinement measures would be de-escalated in successive stages. Deconfinement was announced in Belgium on April 24, 2020, and it was implemented gradually [1]. On May 4, outdoor activities were allowed for a maximum of two people [2]. On May 18, several institutions were reopened, including schools and cultural attractions; the economy was restarted by allowing professions that required close contact to resume activities; and sports and leisure activities were allowed to resume [3]. In the last phase, starting June 3, all activities were allowed to resume, as described by a spokeperson of the Belgian government of the Belgian government: “freedom is the rule, and what is not allowed is the exception” [4].
The COVID-19 pandemic caused a reduction in the number of emergency room visits [5]. This was due, in part, to the fear of contracting the virus as well as to government recommendations [6]. Other studies have shown that, among psychiatric patients, symptoms related to anxiety increased during the pandemic [7]. Moreover, one quarter of these patients showed post-traumatic stress symptoms (PTSS). Indeed, indicators of PTSS and symptoms of depression have increased after the COVID-19 outbreak [8]. These observations were consistent with past reactions observed in populations that experienced quarantine (e.g., 2003 SARS or Ebola) [9]. The world is expected to change with an economic recession, and the rise in unemployment is expected to be associated with a rise in the suicide rate [10].
In our emergency department (ED), during the month of May, the authors hypothesized that deconfinement might have led to changes in the number and profiles of psychiatric visits. The present retrospective observational study was conducted to test two main hypotheses. First, we hypothesized that the number of psychiatric visits to our ED would increase. Second, we hypothesized that the characteristics of these visits would be different.
2. Methods
2.1. Study design and setting
This retrospective observational single-center study analyzed psychiatric visits to the ED of a university hospital on the outskirts of a city of 200,000 inhabitants. We performed a retrospective chart review. We compared our observations during a 31-day period in May 2020 to past observations in May of the previous 4 years. We chose the month of May, because it corresponded to the time when confinement restrictions were lifted (deconfinement) in Belgium. We decided to end the study period on the 31st of May, because, on one hand, we were not sure how to define a clear stopping point for the deconfinement; and on the other hand, in this special healthcare period during the pandemic, the abstractors had time to perform the analyses in June. Therefore, in view of the seasonal character of psychiatric consultations [11], we compared current observations to averaged observations for the one-month period in May of the 4 preceding years (historical period).
2.2. Selection of participants
After gaining approval from the Ethics Committee, data were obtained by searching our medical records to identify visits to our ED for a reason encoded as psychiatric. Every patient that had an emergency consultation in our ED was administratively categorized at admission as psychiatric, medical, surgical, or pediatric. Additionally, we noted the total number of non-psychiatric visits made during the study period, by searching the database established for the emergency department.
Of the 259 psychiatric visits included in the study, 9 were excluded, due to: encoding errors, declined examination and specific requests for child psychiatry. In some instances, there were several consultations for the same patient and they have all been encoded. These re-visits were scattered over time and were not the specific fact of the deconfinement period.
2.3. Data collection
Two authors (JF and NS) abstracted the data. They were trained to perform abstraction and used a standardized abstraction form. Before starting the extraction of data, they completed a trial process, with each abstractor performing separately, and then, performing together. They collected data on psychiatric visit characteristics, including age, sex, current and past domiciles, co-habitants at home and any eventual conflicts with co-habitants, psychological or psychiatric medical history. They also collected data on the characteristics of the visits, including the main symptom justifying the ED visit, psychiatric medications, acute intoxication, follow-up appointments before and after emergency discharge, diagnosis, and destination after the visit. The use of psychiatric drugs was defined as the use of antipsychotics, antidepressants, hypnotics, sedatives, or anxiolytics. Acute intoxication was defined as excess consumption of alcohol or stronger drugs on the day or the day before of the visit. Diagnoses were classified according to the 8 most common conditions noted in psychiatry textbooks and the conditions identified in our previous study. This classification represented a simplification of the Diagnostic and Statistical Manual of Mental Disorders (DSM 5) system [12], and it was meant to facilitate classifications for the emergency physicians [13,14].
-
•
Adolescent disorder: a change in the behavior of a young patient that is not within the norm for the human environment.
-
•
Organic mental disorder: a dysfunction of the brain that is not due to a psychiatric disorder.
-
•
Toxic consumption disorder: a toxic consumption problem that is presented as the main problem, not as a consequence.
-
•
Schizophrenia: a mental disorder due to an abnormal interpretation of reality.
-
•
Mood disorder: a disturbance that is mainly manifested in mood features.
-
•
Anxiety disorder: the presence of significant anxiety and fear.
-
•
Somatoform disorder: a mental disorder, where bodily symptoms are the main reason for the visit.
-
•
Adjustment disorder: an inadequate reaction to a stressful event.
-
•Others: conditions that cannot be classified as any of the diagnoses described above.
- The authors held periodic meetings with the chart abstractors during the data collection period to monitor and ensure their performances. The abstractors were not blinded to the hypotheses, because they were present when this study was conceived, and we did not have sufficient manpower to invite other abstractors. Inter-rater reliability between abstractors was calculated with a sample of 15% of patients. The minimum kappa value was 0.68 and the maximum was 1.
2.4. Outcomes
The main objective was to identify a possible rebound in psychiatric consultations after lifting the lockdown due to COVID-19. Therefore, the primary outcome was the proportion of psychiatric visits to the ED during deconfinement (the month of May 2020) compared to the historical proportion during the historical group (control period without an epidemic: May in 2016–2019). Other outcomes included characteristics of admission to the ED.
2.5. Statistical analysis
For group comparisons, we performed the student's statistical t-test to compare the average numbers of visits/day admitted for psychiatric reasons, and we performed the statistical chi-square test to compare the proportions of visits for psychiatric reasons.
We checked the main symptom justifying the psychiatric visits to the ED during deconfinement compared to historical reasons for psychiatric visits to our ED. We compared differences between groups in terms of the characteristics of the psychiatric emergency visits. We performed the chi-square test to compare the proportions of each characteristic between the historical period and the deconfinement period. Missing data were encoded as “Non Available” and omitted from the analyses.
All analyses were performed with R4.0.1 (R Foundation for Statistical Computing, Vienna).
3. Results
3.1. Number of visits
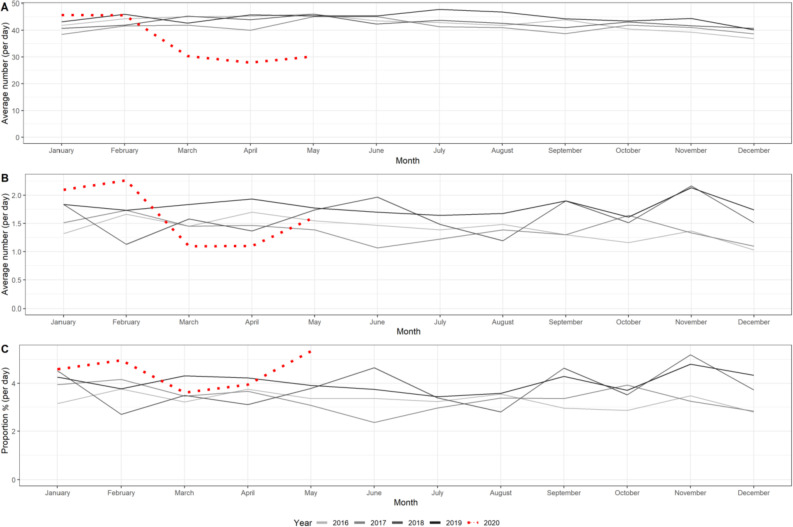
The average number of visits to the ED was low during the deconfinement period compared to the mean number of visits in previous years (from a mean of 45.6 admissions/day historically to a mean of 30.2 during deconfinement, p < 0.0001). However, the number of visits for psychiatric reasons were the same during the deconfinement period and the historical period (mean 50 patients per month). Thus, the proportion of visits for psychiatric reasons increased during the deconfinement (5.3%), compared to previous years (3.5%; p = 0.013) (Fig. 1 ).
Fig. 1.
Numbers and proportions of visits per day in the emergency department before (solid lines) and after (red dots) COVID-19 lockdown. A: All visits. B: Psychiatric emergency visits. C: Proportions of psychiatric visits among all visits. Deconfinement period was the month of May, 2020.
To contextualize these results, it is interesting to compare these changes with those of the first confinement itself. The changes of the number of ED visits is consistent with the previously knew effect of the Emergency state declaration on the number of all ED visits [5], who decreased in our hospital in the beginning of 2020 in March (30.4 admissions/day during march 2020 to a mean of 43.7 during the months of March of the 4 previous years) and April (27.9 admissions/day during april 2020 to a mean of 43.7 during the months of April of the 4 previous years). This decrease was also found in terms of psychiatric visits (34 admissions during March 2020 to a mean of 49 during the months of March of the 4 previous year; 33 during April 2020 to a mean of 51 during the months of April of the 4 previous years).
3.2. Characteristics of visits
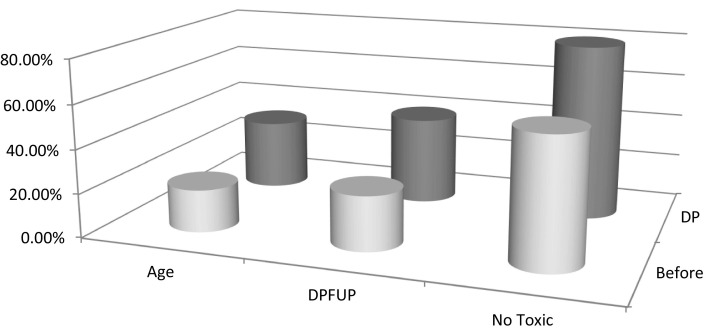
There were two significant differences in the characteristics between the groups. First, more visits in the deconfinement group were without acute intoxication (80% were not intoxicated at admission) compared to those in the historical group (58.5%, p = 0.031; Fig. 2 ). Second, more visits in the deconfinement group did not have a follow-up consultation organized at discharge (40% did not require follow-up), compared to the historical group (25%, p = 0.036).
Fig. 2.
Main interesting changes in the characteristics of patients admitted for psychiatric reasons, before and after the COVID-19 lockdown. Abbreviations: Age, patient's age during the visit; DPFUP, discharge without psychiatric follow Up; No Toxic, no acute intoxication; Before, values for the month of May, averaged over the preceding 4 years; DP, deconfinement period.
The age difference between groups was borderline significant. In the deconfinement group, a larger proportion of visits was with patients under 30 years old (32%) than in the historical group (19.5%, p = 0.056).
There were no statistical differences between the two groups in the other variables. The proportion of females was the same in the two groups (42% for both, p = 1); the majority of visits were from patients who lived in a house or an apartment (94.5% historically; 92% during deconfinement, p = 0.646), and came from their domicile (88.5% historically; 86% during deconfinement, p = 0.627), rather than an institution or a public space. The two groups were also similar for: visits from patients with past psychiatric/psychologic follow ups (39.5% historically; 38% during deconfinement, p = 0.512), visits from patients with psychiatric medical histories (19% historically; 14% during deconfinement period, p = 0.297), and visits from patients taking regular psychiatric drugs (28% historically; 24% during deconfinement, p = 0.481). In addition, in both groups, most visits were from patients who did not receive psychiatric drugs during the emergency visit (73.5% historically; 76% during deconfinement, p = 0.718), did not live alone or have conflicts with co-habitants (62% historically; 68% during deconfinement, p = 0.713), returned home after the visit (65% historically; 68% during deconfinement, p = 0.751), and were unlikely to receive psychiatric drug treatment at discharge (70.5% historically; 58% during deconfinement, p = 0.081).
The main symptoms justifying ED visits were not significantly different between groups. These reasons included depressive symptoms (29% historically;32% during deconfinement, p = 0.663), suicide attempt (20% historically;24% during deconfinement, p = 0.521), anxiety (14%, both historically and during deconfinement, p = 1), and a personality/comportment disorder (19% historically,12% during deconfinement, p = 0.234).
The final diagnoses were not significantly different between the two groups. The most common diagnosis was mood disorder (33% historically;40% during deconfinement, p = 0.359). The second most common diagnosis was adjustment disorder (17% historically;10% during deconfinement, p = 0.216). These were followed by: toxic consumption disorder (14.5% historically;8% during deconfinement, p = 0.219), schizophrenia (11% historically;8% during deconfinement, p = 0.526), anxiety disorder (11% historically;8% during deconfinement, p = 0.708), adolescent disorder (4% historically;10% during deconfinement, p = 0.089), somatoform disorder (4% historically;8% during deconfinement, p = 0.240), organic mental disorder (1% historically;4% during deconfinement, p = 0.132), and others (4% historically;4% during deconfinement, p = 1).
4. Discussion/summary
With deconfinement, psychiatric emergency activity rapidly returned to the usual level of activity, when considering only the number of consultations. However, when we compared this activity to the total activity in the ED, the proportion of psychiatric admissions among all admissions rose to a level never before observed. In our knowledge, this is the first publication to note this. This main result was explained by the low surgical and medical activity during deconfinement. This finding is consistent with observations from other ED showing a lesser to no decline of psychiatric visits compared to other conditions [[15], [16], [17]]. It seemed unlikely that the fear of hospital admission and the associated risk of contracting COVID-19 might have subsided among psychiatric patients more rapidly than among medical and surgical patients. Therefore, one hypothesis is that the COVID-19 outbreak indirectly generated a new type of psychiatric visit. This new type was with younger patients less likely to be acutely intoxicated. The trends of an increase of visits with younger patients is consistent with other findings around the world showing the fragility of this group possibly related to the social and economic repercussions of isolation [18,19]. The finding of fewer visits with acutely intoxicated patients was suprinsing for the authors. An increase in consultations with acutely intoxicated patients was rather expected and would have been correlated with some findings like in the US were an increase in alcohol sales and drug overdose have been documented [20].
Curiously, these new visits with patients who did not require psychiatric and/or psychological follow-up at discharge. One explanation might be that the patients concerning these visits actually did need follow-up, but we might not have identified follow-up plans, because they were not included in the records that we analyzed. Probably, follow-ups could have been systematically organized by the general practitioner.
This study had some limitations. The small sample size and the observational nature of this study could have introduced some bias. The unicentric character of the study should be kept in mind. Consequently, our results might not be generalizable to other populations.
In summary, based on our findings, we suggest that the COVID19 pandemic has changed the nature of psychiatric emergency consultations, at least in the short term during the deconfinement of the first COVID-19 wave in our ED. This finding remains to be confirmed with more data. As others around the world have written [21], we would add our voice to the call for preserving emergency care for psychiatric disorders, because these disorders might change or grow over time.
Data statement
The research data are confidential and fully available for investigators on a protected computer.
Grant/Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Supports, grants and ethics
This publication did not receive any specific grant or support from funding agencies in the public, commercial, or not-for-profit sectors.
The article has never been presented to an organization.
Credit Author Statement
Flament Julien, Scius Nathan, Zdanowicz Nicolas, Regnier Maxime, De Cannière Louis, Thonon Henri
JF conceived the study, ask for the ethics committee approval, drafted the manuscript and JF takes responsibility for the paper as a whole. JF and NS supervised the data collection. MR and HT provided statistical advice on study design and analyzed the data. NZ and LDC participated in the design of the study. All authors contributed substantially to manuscript revision.
Declaration of Competing Interest
The authors have no competing interests to declare.
Acknowledgements
Editorial assistance was provided by San Francisco Edit.
References
- 1.Federal Public Service (FPS) Chancellery of the Prime Minister News Website. 2021. https://news.belgium.be/en/corona#security; [accessed 22 March 2021]
- 2.Federal Public Service (FPS) Health, Food Chain Safety and Environment Coronavirus COVID-19 information website. 2003. https://www.info-coronavirus.be/en/news/nsc-24-04/; [accessed 22 March 2021]
- 3.Federal Public Service (FPS) Health, Food Chain Safety and Environment Coronavirus COVID-19 information website. 2003. https://www.info-coronavirus.be/en/news/nsc-13-05/; [accessed 22 March 2021]
- 4.Federal Public Service (FPS) Health, Food Chain Safety and Environment Coronavirus COVID-19 information website. 2003. https://www.info-coronavirus.be/en/news/nsc-0306/; [accessed 22 March 2021]
- 5.Westgard B., Morgan M., Vazquez-Benitez G., Erickson L.O., Zwank M.D. An analysis of changes in emergency department visits after a state declaration during the time of COVID-19. Ann Emerg Med. 2020 doi: 10.1016/j.annemergmed.2020.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wong L.E., Hawkins J.E., Langness S., Murell K.L., Iris P., Sammann A. Where are all the patients? Addressing Covid-19 fear to encourage sick patients to seek emergency care. NEJM Catal Innov Care Deliv. 2020 doi: 10.1056/CAT.20.0193. [DOI] [Google Scholar]
- 7.Rajkumar R.P. COVID-19 and lmental health: a review of the existing literature. Asian J Psychiatr. 2020 Aug;52:102066. doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. 2020 doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McIntyre R.S., Lee Y. Preventing suicide in the context of the COVID-19 pandemic. World Psychiatry. 2020;19:250–251. doi: 10.1002/wps.20767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Patten S.B., Williams J.V., Lavorato D.H., Bulloch A.G.M., Fiest K.M., Wang J.L., et al. Seasonal variation in major depressive episode prevalence in Canada. Epidemiol Psychiatr Sci. 2017;26(2):169–176. doi: 10.1017/S2045796015001183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American Psychiatric Association . 5th ed. American Psychiatric Publishing; Arlingon, VA: 2013. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- 13.De Clercq M. De Boeck université; Paris: 1997. Urgences psychiatriques et interventions de crise. [Google Scholar]
- 14.Zdanowicz N., Janne P., Reynard C. La dépression insuffisamment traitée par les généralistes? La revue Française de Psychiatrie et de Psychologie Médicale. 1998;19:94–97. [Google Scholar]
- 15.Giannouchos T.V., Biskupiak J., Moss M.J., Brixner D., Andreyeva E., Ukert B. Trends in outpatient emergency department visits during the COVID-19 pandemic at a large, urban, academic hospital system. Am J Emerg Med. 2021 Feb;40:20–26. doi: 10.1016/j.ajem.2020.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lucero A.D., Lee A., Hyun J., Lee C., Kahwaji C., Miller G., et al. Underutilization of the emergency department during the COVID-19 pandemic. West J Emerg Med. 2020 Sep 24;21(6):15–23. doi: 10.5811/westjem.2020.8.48632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alwood S., Musso M.W., Jones G.N., Mosley J., Wippel B., Theriot L., et al. The impact of the COVID-19 pandemic and governor mandated stay at home order on emergency department super utilizers. Am J Emerg Med. 2021 Apr 20;48:114–119. doi: 10.1016/j.ajem.2021.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu C.H., Zhang E., Wong G.T.F., Hyun S., Hahm H.C. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Res. 2020 Aug;290:113172. doi: 10.1016/j.psychres.2020.113172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liang L., Ren H., Cao R., Hu Y., Qin Z., Li C., et al. The effect of COVID-19 on youth mental health. Psychiatry Q. 2020 Sep;91(3):841–852. doi: 10.1007/s11126-020-09744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moutier C. Suicide prevention in the COVID-19 era: transforming threat into opportunity. JAMA Psychiat. 2021;78(4):433–438. doi: 10.1001/jamapsychiatry.2020.3746. [DOI] [PubMed] [Google Scholar]
- 21.Moreno C., Wykes T., Galderisi S., Nordentoft M., Crossley N., Jones N. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry. 2020;7(9):813–824. doi: 10.1016/S2215-0366(20)30307-2. [DOI] [PMC free article] [PubMed] [Google Scholar]