Abstract
The WHO Model List of Essential Medicines (MLEM) has since 1977 helped prioritize and ensure availability of medicines especially in low- and middle-income countries. The MLEM consists mainly of generic medicines, though recent trends point towards listing expensive on-patent medicines and increasing global support for medicines against non-communicable diseases. However, the implications of such changes for national essential medicines list (NEML) updates for access to essential medicines has received relatively little attention. This study examined how government agencies and other actors in Kenya, Uganda and Tanzania participate in and influence the NEML update process and subsequent availability of prioritized medicines; and the alignment of these processes to WHO guidance. A mixed study design was used, with qualitative documentary review, key informant interviews and thematic data analysis. Results show that NEML updating processes were similar amongst the three countries and aligned to WHO guidelines, albeit conducted irregularly, with tendency to reprioritization during procurement stages, and were not always accompanied by revision of clinical guidelines. Variations were noted in the inclusion of medicines against cancer and hepatitis C, and the utilization of health technology assessment (HTA). For medicines against diseases with high global engagement, such as HIV/AIDS and TB, national stakeholders had more limited inputs in prioritization and funding. Furthermore, national actors were not influenced by the pharmaceutical industry during the NEML update process, nor were any conflicting agendas identified between health, trade and industrial policies. Hence, the study suggests that more attention should be paid to the combination of HTAs and NEMLs, particularly as countries work towards universal health coverage, in addition to heightened awareness of how global disease-specific initiatives may confound national implementation of the NEML. The study concludes with a call to strengthen country-level policy and procedural coherence around the process of prioritizing and ensuring availability of essential medicines.
Keywords: Model list of essential medicines, national essential medicines list, health policy, actors, Uganda, Kenya, Tanzania, access to medicines
KEY MESSAGES.
Evidence around governance issues on access to medicines remains scarce, relative to what is available on breakthroughs in biomedical technologies. The WHO Model List of Essential Medicines (MLEM) and national essential medicine list development, update and implementation is one such policy and governance issue. The process for the essential medicines list development and implementation takes place within a national policy space in which national key stakeholders deliberate and choose their policy options to determine availability and access to medicines at point of care.
The national policy-level analysis of essential medicines lists development suggest that prioritization and availability are two sides of the same coin and benefit from being analysed as such and essential medicines lists represents an important interface between demand, and supply-side factors, however, this interface varies according to medicines that come into play with new and more expensive medicines tampering the balance between demand and supply. The differences in content of Essential Medicines Lists amongst countries are a constellation of actors and elements within the process.
Introduction
Evidence around governance issues regarding access to medicines remains scarce, relative to what is known about breakthroughs in biomedical technologies (Simao et al., 2018), and yet medicines account for a large proportion of national health expenditure (WHO, 2011). The concept of essential medicines advanced by the World Health Organization (WHO) in 1977 has been adopted as a global practice (Laing et al., 2003). Essential medicines are defined as those meeting priority health care needs of the population (WHO, 2002). However, considerations of essential medicines also include evidence of efficacy and safety, and both comparative costs and cost-effectiveness (Magrini et al., 2015). WHO revises the model list of essential medicines (MLEM) biennially, providing additional guidance for developing and implementing NEML (Magrini et al., 2015). The usefulness of the list has been tagged to its adaptation by member states as they develop national lists (Laing et al., 2003). The governance aspects of updating national essential medicines lists (NEML) is subject to limited systematic comparison, and especially in low- and middle-income countries (LMICs) (Mori et al., 2014). A common assumption that needs to be critiqued, is that once a select list of medicines is prioritized, e.g. through the NEML, there is improved access, higher quality of care, and rational and safe use of such medicines (WHO, 2002; Mugiraneza, 2009). Even though essential medicines policies are found to be associated with quality use of medicines, there is a stated need for better data about the co-implementation of medicine-related policies as well as the interaction between public and private sectors (Holloway et al., 2020). The national policy space and discourse where key domestic stakeholders deliberate and choose their policy options, often in collaboration with international partners, is a key determinant related to the availability and access to medicines at point of care (Mugiraneza, 2009). Therefore, more attention needs to be paid to how governance and financing at both global and national levels affect the availability of essential medicines (Bernstein and Cashore, 2012; Shaffer and Ginsburg, 2017). Greater engagement of health policy and systems research actors on issues of access to medicines in LMICs is necessary to fill current gaps in published literature (Adam et al., 2011).
The WHO MLEM mainly includes off-patent medicines, which are generally affordable for most countries. However, in 2001, the WHO Executive Board (EB) indicated that absolute treatment cost should not disqualify a proposed addition to the model list, as long as a particular medicine meets the criteria for benefit and public health relevance. The issue of affordability, the EB argued, should be considered as a consequence to be managed after the list is developed (Magrini et al., 2015). Subsequently, in the past 15 years, the inclusion of these on-patent medicines on the MLEM has fuelled discussions within the global health community and among countries about what should be regarded as an ‘essential’ or ‘cost-effective’ product (Laing et al., 2003). Following the 2015 revision of MLEM, many new or relatively new and expensive medicines to treat cancer, hepatitis C and multidrug-resistant tuberculosis were added to the list (Magrini et al., 2015). The extent to which these aforementioned medicines become part of the access norm, through inclusion in revised editions of NEMLs, remains to be established (Ferrario et al., 2018).
In addition to the increasing number of expensive on-patent medicines to the MLEM and specific guidance by WHO on the update process, the last two decades have witnessed changes in pharmaceutical markets with increasing importance of emerging country manufacturers, together with a growing density of global health governance arrangements designed to assist LMIC in adopting and delivering at point of care medicines against key infectious diseases, particularly HIV/AIDS and tuberculosis (WHO 2001a; Laing et al., 2003; Bigdeli et al., 2013; Hill et al., 2018). As a result, national authorities have to contend with increasing number of actors with interest in the development and implementation of national policies relevant to medicines access. Furthermore, country commitments to the sustainable development goals, which sought to reposition access to quality essential medicines as part of efforts towards universal health coverage (UHC), adds to this complexity (Bigdeli et al., 2015). A rising global concern for increased prevalence of non-communicable diseases and hence the case for equitable access to these medicines points towards the possibility of a more inclusive global agenda. Evidently, however, understanding these dynamics and their implications for the national policy processes requires a broader conceptual view (Bigdeli et al., 2013).
There is limited evidence on how countries manage these governance situations, including coordination of multiple stakeholders, funding sources and procurement organizations, and various supply chains within a single national policy environment to support and facilitate access to essential medicines (Kraiselburd and Yadav, 2013; Simao et al., 2018). Therefore, in this study we sought to examine how government agencies and other actors, including non-state actors and international partners in Kenya, Uganda and Tanzania participate in and influence the process of updating their NEML and making prioritized medicines available. In addition, we examined the extent to which the processes in the three countries were aligned to the WHO guidance, paying particular attention to new addition to the 2015 MLEM with focus on tuberculosis, hepatitis C and cancer medicines. This group of medicines formed the bulked of the new addition to the 2015 MLEM. In balancing a wide scope with small-scale empirical data, the study is suited as an initial building block for exploring policy-options and further paths for inquiry. The comparative design, examining the policy-processes in three settings, further strengthens the methodological approach we adopted.
Methodology
A mixed method case study approach was used, relying mainly on qualitative data, collected using semi-structured interviews and a document review guide. Documents for the review were searched from four electronic databases (Allied and Complementary Medicine, Embase, MEDLINE and PsycINFO). Google scholar and websites of Ministries of Health, National Medicine Regulatory Authorities (NMRAs) and national medicines procurement agencies of Kenya, Uganda and Tanzania were also searched to supplement what was obtained from the above databases. The choice of the study sites was informed largely due to the timeframe and the available resources. However, the data generated, and findings is adequate, and likely the same picture holds for countries of similar contextual environment; the LMIC.
Searching databases involved the use of standard Boolean operators. Search on the databases, Google scholar and websites of NMRAs, Ministries of Health yielded 512 documents. Given time restraints the title and abstract review for the initial screening was completed by one reviewer (EP). The final documents used in the analysis were 42 after limiting to broad relevance to study objectives; and availability of full-length articles. The 42 documents also included the three countries’ NEMLs, national pharmaceutical (medicines/drug) policies, national health strategic plans, national health policies; and WHO MLEM 2013 and 2015. The document review was conducted to provide context and empirical literature on discourses in NEML, as well as facilitate identification of the new medicines added to the WHO 2015 MLEM and of those, which ones the countries added to their national lists.
To complement information from the documentary review, key informant interviews were conducted between May and July 2018. The selected participants were senior officials at national level and had partaken in or had knowledge of the most recent NEML update process. Study participants were from Ministries of Health (MOH), NMRAs, Medical Procurement agencies, WHO country offices, Country offices of The Global Fund and non-governmental organizations. A 45 min in-person interview on average was conducted with each of the 20 purposely selected participants (Uganda 8, Kenya 7 and Tanzania 5). None of the invited study participants declined the invitation for interviews. We did not specifically set out to pilot test the interview guide, the authors (WDO, KIS and YD) discussed and revised the question guide. We also used the first two interviews to highlight additional probes to employ during successive interviews given that the questions were already broad and open ended. Interviews were digitally recorded and subsequently transcribed verbatim. The interviews complemented the documentary review by eliciting perspectives from key stakeholders on main drivers and barriers as countries consider adapting WHO revisions to their NEML (Supplementary data S1: Interview guide). The information from interviews was extracted by two authors; WDO and KIS. Where there were disagreements, it was addressed through discussion and consensus. In addition, eight (n = 8) of the study participants took part in a 2-day validation workshop with members of the research team in Mombasa, Kenya, in March 2019, during which preliminary findings were presented and a focus group discussion on select issues requiring clarification were addressed.
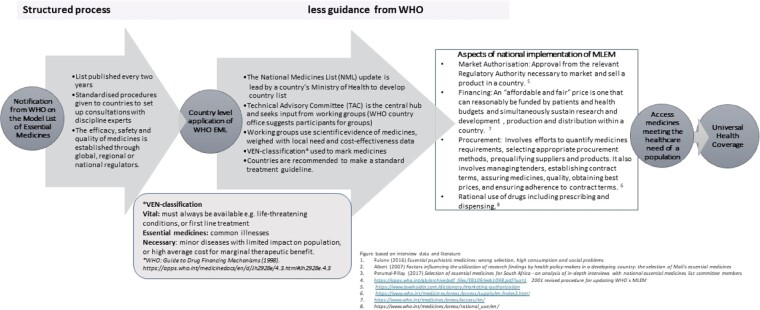
A policy analysis approach adapted from Walt and Gilson’s Policy Triangle Framework guided the analysis. This framework (Walt and Gilson, 1994) posits that policy research needs to consider not just the content of policies (the NEML in this instance), but also the actors, context and process in order to be able to explain outcomes and assess implementation. The analysis was conducted based on preconceived thematic categories of the Policy Triangle Framework. This includes the four categories content (inclusions of the selected medicines on the NEML), actors, the process of updating the list and making medicines available, and finally the context. On the process, we developed a schema of the WHO process in order to examine alignment between the national process and WHO recommendations (Figure 1).
Figure 1.
WHO guidance on the process for updating NEML. Guidance on the process for updating NEML [based on interview data and literature (Fulone et al. 2016; Albert et al. 2007; Perumal-Pillay and Suleman 2017)].
Ethical clearance was obtained from the three countries’ Institutional Review bodies: Kenya’s Kenyatta National Hospital and University of Nairobi Ethics and Research Committee, Tanzania’s National Institute for Medical Research, and Uganda’s Higher Degrees, Research and Ethics Committee at Makerere University School of Public Health. Informed consent of all research participants was obtained, and their confidentiality and privacy observed by anonymizing participants. Only synthesized responses are presented in the results section.
Results
Our survey of selected medicines and interviews with country policy practitioners suggest that the national prioritization of essential medicines is a task that extends beyond the update of the NEML, and is followed by decision-making junctures that are then applied to further down-select the medicines to be provided by the public health system. We found that these decisions play out differently according to medicine groups and contributes to complexity from the health systems perspective. The results are presented thematically according to the elements of the policy triangle framework and summarized in Figure 1 and Tables 1 and 2.
Table 1.
Thematic summary of findings regarding NEML updates in Kenya, Tanzania and Uganda based on the policy triangle framework
| Country | Content | Actors Those involved in the updating and related implementation | Process The interactions between countries new list(s) and the prioritized medicines being available | Context Affecting update process and ensuring the availability or use of the medicines |
|---|---|---|---|---|
|
Kenya Essential Medicines List (KEML) First published 1981; Most recent: 2016 (5th edition) |
|
|
|
These common contextual factors were relevant in all three countries
|
|
Tanzania National Essential Medicines List for Tanzania (NEMLIT) First published 1971a; Most recent: 2017 (5th edition) |
|
|
|
|
|
Uganda Essential Medicines and Health Supplies List for Uganda (EMHSLU) First published 1991; Most recent: 2016 (6th edition) |
|
|
|
The 1977, 1981 and 1986 lists were only drug lists. The NEMLIT &STGs edition started in 1991, then 1997, 2001, 2007, 2013 and 2017.
Table 2.
New tuberculosis, cancer and hepatitis C medicines on the 2015 WHO Model List vis à vis the addition to the latest National EMLs Kenya (2016), Uganda (2016) and Tanzania (2017)
| WHO Model List 2015 Update | Kenya (2016) | Uganda (2016) | Tanzania (2017) |
|---|---|---|---|
| Tuberculosis | |||
|
Bedaquiline Delamanid Linezolid Rifapentine |
Bedaquilinea Capreomycin Cycloserine Delamanida Levofloxacin Linezolida Moxifloxacin p-aminosalicylic acid Prothionamide Rifabutin |
Amikacin Bedaquilinea Capreomycin Clofazimine Cycloserine Ethionamide Kanamycin Levofloxacin Linezolida Moxifloxacin P-Aminosalicylic acid Prothionamide Amoxicillin + Clavulanic Acid |
Bedaquilinea Delamanida Linezolida |
|
| |||
| Cancer | |||
|
| |||
|
All-trans retinoid acid Bendamustine Capecitabine Cisplatin Filgrastim Fludarabine Gemicitabine Imatinib Irinotecan Oxaliplatin Rituximab Trastuzumab Vinorelbine |
Alendronic acidb Anastrozolea Bicalutamidea Capecitabinea Diethylstiboestrolb Docetaxel Filgrastima Gemicitabinea Goserelinb Ifosfamide Imatiniba Irinotecana Melphalanb Mesna Oxaliplatin Paclitaxel Rituximaba Tamoxifen Thalidomide Trastuzumaba Vinorelbine |
Anastrozolea Bicalutamidea Capecitabinea Dactinomycin Filgrastim Fluorouracil Gemicitabinea Goserelin Irinotecan Mesna Oxaliplatina Paclitaxel Thalidomide Vinblastine Rituximab already on the previous national list and retained in 2016 version |
Bicalutamidea Cisplatina Gemcitabinea Imatiniba Irinotecana Oxaliplatina Rituximaba Trastuzumaba |
| Hepatitis C | |||
|
Sofosbuvir Simeprevir Daclatasvir Dasabuvir ledipasvir + sofosbuvir ombitasvir+ paritaprevir + ritonavir |
Pegylated interferon alfa-2a Ribavirin |
Sofosbuvira Ledpasvira Ribavirin |
|
Medicines that were included in the NEMLs from the 2015 update of the WHO Model List.
Medicines not on the 2015 or 2013 WHO MLEM but on the national list.
The process
The process of updating NEMLs can be investigated from the perspective of the stages and interactions during each update, or more broadly, how the practice in each country has developed over time. While this study considers the former, the initial development of a national list and the frequency of updates form a backdrop. Tanzania was the first country of the three to issue an NEML in 1977, updated in 1981 and 1986 (Munishi, 1995); subsequent updates in 1991, 1997, 2007, 2013 and 2017 (Munishi, 1995; Tanzania Ministry of Health, 2017). From 1991, Tanzania NEML (NEMLIT) reviews were conducted concurrently with revisions of the standard treatment guidelines (STG) as recommended by the WHO (WHO 2013). The first edition of the Essential Medicines and Health Supplies List for Uganda (EMHSLU) was published in 1991 with subsequent updates in 1996, 2001, 2007, 2012 and 2016 (Uganda Ministry of Health, 2016). Kenya, on the other hand, developed its first essential medicines list in 1981, with subsequent updates published in 1993, 2003, 2010 and 2016 (Kenya Ministry of Health, 2016). While there is a consistency in how the process is implemented, the intervals vary and have at times been as long as 10 years.
For an NEML update, the WHO recommends the selection of committee members, and the procedure for the structure of interactions and decision-making (WHO 1977, 2001b). Figure 1 summarizes WHO guidance on the process of updating the NEML based on available literature and the interview data. As depicted in Figure 1, WHO guidance is quite prescriptive and structured for the selection and committee processes until the list is in the publication stage. However, it is not explicit on the implementation stage, as the process enters into the broader practice of making the prioritized medicines available.
Examination of the 2016 (Kenya and Uganda) and 2017 (Tanzania) updates, described in the following section, considered factors that influence actors’ coordination, as well as links between the nature of the process and observed outcomes.
The data show that all three NEML update processes were coordinated by national medicines and therapeutic committees (NMTC) anchored at a high level within the Ministries of Health, with input from WHO country offices. The committees had representation from a wide range of stakeholders, or consulted other stakeholders not represented on the committees through technical working groups (TWGs), consultative meetings and written submissions (WHO, 2001a, 2002). The number of meetings varied from 10 to 20. Uganda and Tanzania updated the clinical guidelines (STG) and NEML concurrently. In Kenya, for the update in question, the STG was not concurrently updated with NEML as recommended, reportedly due to funding constraints. None of the interviewees reported any coordination challenges in terms of involving the recommended stakeholders during the update process of the national lists. In all three countries the activities related to updating the NEML, including meetings and workshops were largely funded by development partners. The responsible units at Ministries of Health (MOH) budget for this process, however this usually sits amongst MOH’s unfunded priorities.
The main criteria for inclusion and exclusion of medicines on the lists were efficacy, safety, quality, clinical experience, disease prevalence, cost and cost-effectiveness. It is only Tanzania that incorporated cost-effective criteria using the health technology assessment (HTA) during the update. Uganda and Kenya intended to incorporate cost-effectiveness assessment; however, such methods were not used because HTA had yet to be implemented as a policy tool, and difficulties accessing the relevant data to be used for cost-effectiveness calculations. Neither market authorization, nor status of medicine registration in the country was amongst criteria for inclusion or exclusion in all the three countries.
Once NEMLs are confirmed, the next step is the implementation, initial step being sharing the list with the health system at large. In Uganda and Tanzania, interviewees reported that the NEML was disseminated widely and it is used highly in public and private health facilities. In Kenya, the list has not been disseminated as widely, largely due to limitation in funding. The focus group discussion suggested that the limited dissemination of the list manifests itself as the concept of the essential medicines list not being well understood amongst key stakeholders in both public and private sectors, especially prescribers. On a more general level, the overall demand for and use of the list depends on the general awareness of the essential medicines concept, availability of the list and timely updates.
Following the NEML update and dissemination, interview data show that funding and procurement are additional decision-making points that prioritize which medicines become available. In all the three countries, the procurement of medicines and other health supplies in the public sector are based on the NEML; however, final procurement decisions are influenced by the available budget allocated in the year. To a varying extent among the three countries, global initiatives also support procurement of medicines especially the programmatic medicines for HIV, Malaria and TB. However, they require co-funding arrangements with governments as a mechanism of promoting sustainability, and the co-funding is usually drawn from the same source as for other essential medicines, influencing prioritization of government funds for essential medicines (Uganda Ministry of Health et al., 2012).
Actors
In all the three countries, as mentioned above, the process was led by the NMTC. The WHO recommends inclusion of a wide range of stakeholders to the committee (WHO, 2001a, 2002). Documentation and interviews show that Kenya had the least number of committee members 10, compared with 20 each in Uganda and Tanzania. In Kenya, all the members of the NMTC were from MOH (Kenya Ministry of Health, 2016), while in Uganda and Tanzania the committees had membership from other stakeholder groups (Uganda Ministry of Health, 2016; Tanzania Ministry of Health, 2017). In all countries, the committees established a number of subordinate TWGs with representatives from a number of key stakeholder groups from both public and private sectors, including health professional associations, public and private hospitals, local government representatives, health development partners and the WHO country office. Not all TWG members are also members of the NMTC. Departing from this uniformity is a variation in development partners involved in the process, as is shown in Table 1.
The terms of reference for the NMTCs in the three countries extend beyond coordination of updating of the national medicines list, it includes policy advice on rational use of medicine and clinical guideline development among others. The Committees tended to be inactive between updates, to be reestablished when the List is to be updated. However, in Uganda the NMTC has now been reconstituted into the Appropriate Medicine Use Advisory Group with regular meetings and issuance of guidance as and when required.
With regard to pharmaceutical quality control and procurement, the National Medicines Regulatory Authorities (Kenya Pharmacy and Poisons Board, Uganda National Drugs Authority, and Tanzania Food and Drugs Authority) and the National Medical procurement and supplies agencies [National Medical Stores in Uganda (NMS), Kenya Medicine Supplies Agency (KEMSA) and Medical Stores department (MSD)] are cornerstone actors in all the three countries. These two governmental agencies administer and ensure the actual availability of medicines in the public health system, and are the technical agencies that manage logistics, quality, efficacy and safety of essential medicines. As a result, they bridge funding decisions by Ministries of Finance, global health initiatives, and pharmaceutical manufacturers. For all three countries most of the medicines are imported from Indian pharmaceutical companies, and to a limited extent from China. However, our interview data confirm that these companies or their representatives play no active role in the update process of the EML or further prioritization. The same applies for western multinational pharmaceutical industries. In this way, most of the actors who need to coordinate are firmly positioned within the health (as opposed to trade) sector.
The context
The contextual factors affecting update process and ensuring the availability or use of the medicines in the list are similar in the three countries and are summarized in Table 1. Our interview data suggest two broad categories of contextual drivers: firstly, domestic health system changes, which includes the transition towards UHC and reforms such as devolution of responsibilities from central to district level; and secondly, global health aid funding. Limited information related to changes at the global level and shifting co-financing arrangements challenge governments as they plan medicine procurement budgets. In addition, global initiatives can introduce coordination difficulties if they call for individual medicine updates, initiate parallel procurement and supply chains, or merely conduct negotiations with pharmaceutical industry outside the purview of national stakeholders. Discussion at global level, e.g. between global health financing initiatives and pharmaceutical industries usually do not involve national stakeholders. This has been reportedly so for medicines for TB and HIV/AIDS.
Content
Overall, the latest updates compared with the previous edition indicate there was a net increase of 206 medicines to the 2016 Kenya list (total 687), and 46 to the 2016 Uganda list (total of 674). In Tanzania, the total number of medicines in the list reduced to 400 compared with >500 that were in the 2013 national list (Uganda Ministry of Health, 2012, 2016; Kenya Ministry of Health, 2016). The increase in Kenya was attributed to the push by the specialist groups, especially the oncologists, whereas the reduction in Tanzania has been attributed to use of HTA.
In reviewing how countries aligned their update with the 2015 MLEM, and with a focus of medicines against tuberculosis, cancer and hepatitis C, the most distinct variations among the countries were those medicines for cancer and hepatitis C. Kenya exceeded the additions to the 2015 WHO MLEM regarding treatments for cancer (21 new anticancer medicines were added to the list) (Table 2) (WHO, 2015). One reason, from interview and focus group discussion is that specialist treatment is more developed in the Kenyan health system compared with the other two countries and that clinicians advocate for enhanced access more.
Regarding hepatitis C, Tanzania added three of the new medicines to its essential list, including sofosbuvir. Kenya and Uganda did not add the new drugs included in the 2015 MLEM. The non-inclusion of hepatitis C medicines in Kenya and Uganda lists was reportedly due to limited information on hepatitis C prevalence.
All three countries included new and expensive treatment for MDR TB, Bedaquiline. All countries also included linezolid for treating tuberculosis, while only Tanzania and Kenya included delamanid to their lists. The inclusion of expensive, second line anti-TB medicines is, to an extent, driven by global funding available for these medicines through the global financing initiatives, especially the Global Fund to Fight AIDS, TB and Malaria.
In the three countries, the medicines are classified into sub-groups to facilitate reprioritization during procurement. In the KEML, medicines have been grouped as either core or specialist. In Uganda, a medicine is vital, essential or necessary (VEN) and in Tanzania, for antibiotics, it has been classified as access, watch or reserve. Medicines considered Vital must always be available (for instance against life-threatening conditions, or first line treatment), while the Essential medicines are against common illnesses, and Necessary medicines are those against minor diseases with limited impact on the population, or high average cost for marginal therapeutic benefit (WHO, 1998; Kenya Ministry of Health, 2016; Uganda Ministry of Health, 2016; Tanzania Ministry of Health, 2017). For all the three countries, the lists indicate the level of healthcare facility in which a particular medicine is to be made available (Tanzania Ministry of Health, 2013, 2017; Kenya Ministry of Health, 2016).
Discussion
The three countries’ NEML update processes were similar and showed close alignment to recommended WHO procedures. All countries applied similar criteria for considering changes to the list. However, cost-effectiveness estimations were the most challenging and only Tanzania applied HTA methods through the support of the International Decision Support Initiative (IDSI) (International Decision Support Initiative, 2018). The limited use of HTA in the update process in the region is in line with findings from other studies (Mori et al., 2014; Perumal-Pillay and Suleman, 2016, 2017). Update processes in the studied countries have been largely funded by health development partners, and perhaps the unpredictability that comes with donor funding explains the irregularity in the intervals between updates, ranging from 5 to 10 years.
Another notable feature for the countries included in the study was that many of the medicines have remained on countries NEMLs for a long period of time (Uganda Ministry of Health, 2012; Tanzania Ministry of Health, 2013, 2017; Kenya Ministry of Health, 2016). This is perhaps due to their enduring qualities as safe, efficacious and affordable. However, changes in the local burden of disease and pharmaceutical innovation prompt the need to trade older medicines for new ones, or to consider entire new classes of medicines.
Availability of medicines on the NEML in the public sector rely on government funding allocations to the Ministries of Health (Wirtz et al., 2017). Therefore, financing and affordability are a consideration during the NEML update; whether this is implicitly or explicitly stated. This is reflected in prioritization within the list in terms of medicines classification as either VEN, with available public funding prioritized to vital and essential medicines. As such, even though medicine characteristics and local need represents a potential, its actual availability and accessibility especially in the public sector is inextricably linked to funding.
Further downstream, the link between the updated NEML and procurement planning in the public sector is also the extent to which the Ministry of Health makes the list known to facilities and professionals who procure and prescribe medicines. Once known, its use also depends on it being considered relevant, and not outdated thus requiring the regular updates. However, utilization of the list is likely to work best when the concept of the NEML is integrated as a continuous practice, for instance through professional training, rather than as an implementation or a launch event following each update. Findings by Holloway et al. (2020) indicate that undergraduate training of prescribers in STG is associated with quality use of medicines in comparison to only the biennial updates of the list amongst other NEML implementation enablers.
In developing the NEML, a key objective is that those medicines considered essential will be made available (Laing et al., 2003). Therefore, in the update process, the committee ought to take into account issues of supply chain system including the feasibility of procurement and funding wholesomely. For all of the countries, market authorization was not considered a criterion. According to the WHO, market approval is a regulatory decision on which availability may be conditioned given that it can be a proxy for availability of medicines (WHO, 2002). However, there are regulatory frameworks in the three countries that allow unregistered medicines (non-market authorized) to be brought into the country under special conditions, such as in public health emergencies.
The differences in content of the three countries by way of the essential medicines list updates resulting in a longer or shorter list is likely a constellation of actors and elements within the process. The findings point to a growing dilemma of increasing the number of accessible medicines, for instance against non-communicable diseases such as cancers, and raising the governments’ ability to finance medicines in the public sector. While the process in Kenya appears to have emphasized the former, the introduction of HTA in Tanzania incorporated the latter to a greater extent. However, the present study did not examine the HTA experience in Tanzania beyond publicly available documentation, it cannot detail explicitly how additional economic analyses contributed to the NEML update process outcome (International Decision Support Initiative, 2018). A nascent literature on HTA and priority setting in Africa nevertheless suggests that there is room for discussion as to how economic analysis is carried out, balancing commissioned research with local capacity building (Doherty et al., 2017).
An initial assumption of this study was that coordination between the health and trade sectors at the national policy level represents an obstacle for access to medicines in relation to the NEML. The country perspectives in this study, however, suggest that coordination challenges within the health sector may be more problematic. The reason is the multiple actors within the health sector, especially at the global level with influence or interest at the national level. Apart from the procurement by national medical stores or other national wholesalers, the intersections between national healthcare delivery systems and the pharmaceutical sector occur globally, involving public−private partnerships to incentivize development and introduction of new medicines, conduction of market-shaping activities including bulk procurement, and direct price negotiations. Activities centre around select medicines and may change over time, and country policymakers are poorly represented or rarely directly involved with such initiatives. While these activities of global initiatives may produce substantive gains in terms of access to new and affordable medicines, it conflicts with national ownership, sustainability and the continuation of government funded medicines at the national level (Kusemererwa et al., 2016; Rockers et al., 2018). At the nation level, our finding suggests that there is a window of opportunity to bring in the actors from the trade sector as part of the essential medicine policy development and as a way of engage the sector towards increasing local pharmaceutical production and supplies.
Furthermore, other contextual factors, especially the evolving domestic policies on health systems financing including the establishment of national health insurance schemes and global commitment on UHC influences the process for updating the NEMLs. The way global initiatives support access to medicines varies with disease conditions, yet the update of the NEML is taken as a cross-cutting process at the national level. Therefore, there is a need for better engagement by global health financing initiatives and the country-level stakeholders to ensure smooth introduction of new medicines for programmatic medicines in light of the NEML and associated implementation constraints. Information about the disease prevalence affects inclusion decisions related to medicines on the list, as demonstrated by the case of hepatitis C medicines in the three countries.
Bigdeli et al. (2013) have drawn attention to systemic factors at the national level that influence access, however, their argument largely focuses on going beyond the pharmaceutical sector to other sub-sectors of the health system at all levels; from local to the international. In studying the national policy level—this study suggests that there is still a need to connect demand and supply-side elements within the pharmaceutical area, spanning health and trade sectors. A key limitation of this study is that the exploratory nature of the study combined with modest resources did not allow for a full-fledged systematic review of literature, nor inclusion of additional informants that would be needed for a more in-depth analysis of supply-side factors. Still, the study confirms that by enabling broader representation and perspectives at the national level, the complexity of access becomes apparent, with its priorities, trade-offs, network of global, regional and national stakeholders. This complex system approach is echoed by Ozawa et al. (2019). However, the question remains how this can be best managed. This study suggests that when limited to the specific NEML update process, the three countries are well aligned in following the WHO guidance. In governing the frequency and interlinkages with other policy processes, however, there is a potential for cross-country harmonization and sharing of best practices.
Bigdeli et al. (2013) argue that frameworks for understanding or exploring issue of access to medicines should take into consideration health system dynamics and complexities. For example, when focussing on the health sector, Bigdeli et al. (2013) suggest four constraints on access to medicines, including governance of the pharmaceutical sector (e.g. registration and procurement), prices, overall health sector governance and interaction between private and public services. They also recognize that the international context involves both the market for pharmaceuticals as well as donors’ agenda and funding, but that constraints in this domain is less documented in published literature (Bigdeli et al., 2013). In suggesting that the EML represents an important interface between demand and supply-side factors, this study finds that this interface varies according to medicines that come into play, with new and more expensive medicines tampering with the equilibrium between the two sides. In taking a broader view of health sector governance, one may also see this in relation to the capacity of government to manage actors, networks and institutions, constituting a health sector resilience (Topp, 2020). The remaining question is the extent to which governments are able to steer the engagement of international partners, mobilize own funding and decide on the extent to which new medicines will be offered in the private or public sector.
Conclusions
The present study shows that NEML updates tend to follow a structured process aligned to the WHO guidelines and are influenced by prioritization, the procurement planning, and considerations of demand, funding and cost. The national policy-level analysis of the three countries suggests that the implementation of NEMLs should be subject to heightened attention and systematic analysis, as prioritization and availability are two sides of the same coin and benefit from being analysed as such. Furthermore, STG should inform the NEML, this will make the list relevant to the practitioners and improve its use.
Countries in the region need to ensure that health system financing and pharmaceutical policies at the national level promote the implementation of the Essential Medicines concept through building capacities for substantive coherence to ensure complementarity between policy outcomes. Furthermore, national policymakers need to exert their influence over intersections that are currently outside their own policy domains through enhancing global health diplomacy competencies of government officials involved in global pharmaceutical negotiations. In addition, for future research, it is worth further exploring the consequences of adding on-patent drugs for a variety of diseases on the MLEM and thus NEMLs in terms of access and the function of national EMLs.
Supplementary data
Supplementary data are available at Health Policy and Planning online.
Conflict of interest statement. None declared.
Funding
This work was partly supported by the Research Council of Norway through the Global Health and Vaccination Programme (GLOBVAC Project 234608).
Ethical approval. Ethical clearance was obtained from the Kenya’s Joint Kenyatta National Hospital and University of Nairobi Ethics and Research Committee (P118/03/2018), Tanzania’s National Institute for Medical Research (NIMR/HQ/R.8a/Vol.IX/2726), and Uganda’s Higher Degrees, Research and Ethics Committee at Makerere University School of Public Health (Protocol 543).
Supplementary Material
Acknowledgements
We thank the research assistants; Dr Darlington Muwhezi-Uganda, Ms Ann B. Masese-Kenya and Mr Ernest Nyoni—Tanzania. We also acknowledge the contribution of Trygve Ottersen; the overall project director of the i4C project that supported this study.
Contributor Information
Walter Denis Odoch, East Central and Southern Africa Health Community, Plot 157, Oloirien, Njiro, PO Box 1009, Arusha, Tanzania; African Centre for Health Systems Development, Plot 2703, Block 208, Bombo Rd, Kampala, Uganda.
Yoswa Dambisya, East Central and Southern Africa Health Community, Plot 157, Oloirien, Njiro, PO Box 1009, Arusha, Tanzania.
Elizabeth Peacocke, Fridtjof Nansen Institute, vei 17, 1366 Lysaker, Norway.
Kristin Ingstad Sandberg, Fridtjof Nansen Institute, vei 17, 1366 Lysaker, Norway.
Berit Sofie Hustad Hembre, Norwegian Institute of Public Health, Lovisenberggata 8, 0456 Oslo, Norway; Oslo University Hospital, Sognsvannsveien 20, 0372 Oslo Norway .
References
- Adam T, Ahmad S, Bigdeli M, Ghaffar A, Røttingen J-A. 2011. Trends in health policy and systems research over the past decade: still too little capacity in low-income countries. PLoS One 6: e27263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albert MA, Fretheim A, Maiga D. 2007. Factors influencing the utilization of research findings by health policy-makers in a developing country: the selection of Mali's essential medicines. Health Research Policy and Systems 5: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein S, Cashore B. 2012. Complex global governance and domestic policies: four pathways of influence. International Affairs 88: 585–604. [Google Scholar]
- Bigdeli M, Jacobs B, Tomson G et al. 2013. Access to medicines from a health system perspective. Health Policy and Planning 28: 692–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bigdeli M, Laing R, Tomson G, Babar ZU. 2015. Medicines and universal health coverage: challenges and opportunities. Journal of Pharmaceutical Policy and Practice 8: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doherty J, Wilkinson T, Edoka I, Hofman K. 2017. Strengthening expertise for health technology assessment and priority-setting in Africa. Global Health Action 10: 1370194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrario A, Stephens P, Ross-Degnan D, Wagner A. 2018. Trends in sales volumes of cancer medicines in six Asian countries working toward universal health coverage. Journal of Global Oncology 4: 220s. [Google Scholar]
- Fulone I, Barberato-Filho S, dos Santos MF et al. 2016. Essential psychiatric medicines: wrong selection, high consumption and social problems. BMC Public Health 16: 52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill AM, Barber MJ, Gotham D. 2018. Estimated costs of production and potential prices for the WHO Essential Medicines List. BMJ Global Health 3: e000571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holloway KA, Ivanovska V, Manikandan S et al. 2020. Identifying the most effective essential medicines policies for quality use of medicines: a replicability study using three World Health Organisation data sets. PLoS One 15: e0228201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Decision Support Initiative. 2018. New Treatment Guidelines Launched in Tanzania [Online]. https://www.idsihealth.org/blog/new-treatment-guidelines-launched-in-tanzania/, accessed 2 June 2018.
- Kenya Ministry of Health. 2016. Kenya Essential Medicines List 2016. Nairobi: Kenya Ministry of Health. [Google Scholar]
- Kraiselburd S, Yadav P. 2013. Supply chains and global health: an imperative for bringing operations management scholarship into action. Production and Operations Management 22: 377–381. [Google Scholar]
- Kusemererwa D, Alban A, Obua OT, Trap B. 2016. An exploratory study on equity in funding allocation for essential medicines and health supplies in Uganda's public sector. BMC Health Services Research 16: 453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laing R, Waning B, Gray A, Ford N, Hoen E. 2003. 25 years of the WHO essential medicines lists: progress and challenges. The Lancet 361: 1723–9. [DOI] [PubMed] [Google Scholar]
- Magrini N, Robertson J, Forte G et al. 2015. Tough decisions on essential medicines in 2015. Bulletin of the World Health Organization 93: 283–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mori AT, Kaale EA, Ngalesoni F, Norheim OF, Robberstad B. 2014. The role of evidence in the decision-making process of selecting essential medicines in developing countries: the case of Tanzania. PLoS One 9: e84824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mugiraneza CJ. 2009. Is the World Health Organization Model List of Essential Drugs Relevant to Member States? National Essential Drugs Lists of Selected African Countries in Comparative Perspective. MSc, D’Youville College. [Google Scholar]
- Munishi GK. 1991. The development of the essential drugs program and implications for self-reliance in Tanzania. Journal of Clinical Epidemiology 45:7–14. [DOI] [PubMed] [Google Scholar]
- Ozawa S, Shankar R, Leopold C, Orubu S. 2019. Access to medicines through health systems in low- and middle-income countries. Health Policy and Planning 34: iii1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perumal-Pillay VA, Suleman F. 2016. Quantitative evaluation of essential medicines lists: the South African case study. BMC Health Services Research 16: 687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perumal-Pillay VA, Suleman F. 2017. Selection of essential medicines for South Africa - an analysis of in-depth interviews with national essential medicines list committee members. BMC Health Services Research 17: 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rockers PC, Laing RO, Wirtz VJ. 2018. Equity in access to non-communicable disease medicines: a cross-sectional study in Kenya. BMJ Global Health 3: e000828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer G, Ginsburg T. 2017. The empirical turn in international legal scholarship. American Journal of International Law 106: 1–46. [Google Scholar]
- Simao M, Wirtz VJ, Al-Ansary LA et al. 2018. A global accountability mechanism for access to essential medicines. Lancet (London, England) 392: 2418–2420. [DOI] [PubMed] [Google Scholar]
- Tanzania Ministry of Health. 2013. Standard Treatment Guidelines and Essential Medicines List. Dar es Salaam: Tanzania Ministry of Health.
- Tanzania Ministry of Health. 2017. Standard Treatment Guidelines and National Essential Medicines List Tanzania Mainland. Dar es Salaam: Tanzania Ministry of Health. [Google Scholar]
- Topp SM. 2020. Power and politics: the case for linking resilience to health system governance. BMJ Global Health 5: e002891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uganda Ministry of Health. 2012. Essential Medicines and Health Supplies List for Uganda 2012. Kampala: Uganda Ministry of Health. [Google Scholar]
- Uganda Ministry of Health. 2016. Essential Medicines and Health Supplies List for Uganda. Kampala: Uganda Ministry of Health. [Google Scholar]
- Uganda Ministry of Health, Abt Associations Inc, Makerere University School of Public Health. 2012. Uganda Health Systems Assessment 2011 [Online]. Abt. Associations Inc. http://health.go.ug/docs/hsa.pdf, accessed 12 June 2018.
- Walt G, Gilson L. 1994. Reforming the health sector in developing countries: the central role of policy analysis. Health Policy and Planning 9: 353–70. [DOI] [PubMed] [Google Scholar]
- WHO. 1977. The selection of essential drugs-report of a WHO Expert Committee. WHO Technical Report Series. Geneva: WHO. [PubMed] [Google Scholar]
- WHO. 1998. Guide to Drug Financing Mechanisms [Online]. Geneva: WHO. https://apps.who.int/medicinedocs/en/d/Jh2928e/, accessed 12 May 2018. [Google Scholar]
- WHO. 2001a. EB109/8—Revised procedure for updating WHO’s Model List of Essential Drugs—Report by the Secretariat. WHO Medicines Strategy. Executive Board, 109th Session, 7 December 2001 (Arabic version) [Online]. Geneva: WHO. http://apps.who.int/medicinedocs/en/m/abstract/Js22165ar/, accessed 20 May 2018.
- WHO. 2001b. WHO Medicines Strategy Revised Procedure for Updating. WHO’s Model List of Essential Drugs-Report by the Secretariat.
- WHO. 2002. The Selection of Essential Medicines - WHO Policy Perspectives on Medicines [Online]. Geneva: WHO. https://apps.who.int/iris/bitstream/handle/10665/67375/WHO_EDM_2002.2.pdf; jsessionid=5009FBA4850DE535CDB0B6BCA54B39CA? sequence=1, accessed 19 June 2018.
- WHO. 2011. The World Medicines Situation 2011: MEDICINE EXPENDITURES . Geneva: WHO. [Google Scholar]
- WHO. 2013. WHO Model List of Essential Medicines-18th List. Geneva: WHO. [Google Scholar]
- WHO. 2015. WHO Model List of Essential Medicines. 19th List (April 2015) (Amended November 2015). Geneva: WHO. [Google Scholar]
- Wirtz VJ, Hogerzeil HV, Gray AL et al. 2017. Essential medicines for universal health coverage. The Lancet 389: 403–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.