Abstract
Background
Despite increased emphasis on providing higher-quality patient- and family-centered care in the intensive care unit (ICU), there are no widely accepted definitions of such care in the ICU.
Objectives
To determine (1) aspects of care that patients and families valued during their ICU encounter, (2) outcomes that patients and families prioritized after hospital discharge, and (3) outcomes perceived as equivalent to or worse than death.
Methods
Semistructured interviews (n = 49) of former patients of an urban, academic medical ICU and their family members. Two investigators reviewed all transcripts line by line to identify key concepts. Codes were created and defined in a codebook with decision rules for their application and were analyzed using qualitative content analysis.
Results
Salient themes were identified and grouped into 2 major categories: (1) processes of care within the ICU—communication, patient comfort, and a sense that the medical team was “doing everything” (ie, providing exhaustive medical care) and (2) patient and surrogate outcomes after the ICU—survival, quality of life, physical function, and cognitive function. Several outcomes were deemed worse than death: severe cognitive/physical disability, dependence on medical machinery/equipment, and severe/constant pain.
Conclusion
Although survival was important, most participants qualified this preference. Simple measures of mortality rates may not represent patient- or family-centered outcomes in evaluations of ICU-based interventions, and new measures that incorporate functional outcomes and patients’ and family members’ views of life quality are necessary to promote patient-centered, evidence-based care.
Admission to an intensive care unit (ICU) portends high risks for death, reduced physical and cognitive functioning among survivors, and substantial burdens for family members, including increased rates of depression, posttraumatic stress disorder, and complicated grief.1 As the population of ICU survivors has increased, research has shifted to understanding and improving outcomes of survivors and, in particular, on providing high-quality patient- and family-centered care (PFCC).2–7 Such care is a target for reimbursement through value-based purchasing programs, forms a basis of the National Academy of Medicine’s definition of health care quality, and is prioritized in research funded by the Patient-Centered Outcomes Research Institute.8–10
There is no agreed-upon definition for patient- and family-centered care in the intensive care unit (ICU)
However, there is no agreed-upon definition for PFCC in the ICU, and national, patient-reported quality assessments on hospital care do not specifically ask about ICU experiences.11 As a result, most trials of ICU-based interventions are designed to detect differences in mortality rates, number of ventilator-free days, infection rates, and length of stay (LOS).12 These end points, in fact, may not map with patients’ and families’ values.13,14 Prior efforts to define better outcomes in ICU research have been guided by practitioners and researchers. More recent work has given a voice to patient stakeholders,15–17 including the use of qualitative approaches to study patients’ experiences in the ICU, perspectives on ICU-based palliative care, and services after ICU discharge.18–25 However, perspectives of family caregivers, particularly those of patients who died in the hospital, have rarely been explored.
The central aim of this study was to explore experiences of patients who had been in the ICU and of family caregivers of patients who survived and of those who died. The purpose was to fill existing gaps in the evidence base by identifying (1) ICU processes of care that patients and families valued during their ICU encounter, (2) outcomes that patients and families prioritized after discharge, and (3) participants’ perceptions of outcomes that may be equivalent to or worse than death. We then considered how perspectives map with recent recommendations from Needham et al26 for a core set of post-ICU discharge outcomes, including survival, physical function, cognition, mental health, health-related quality of life, and pain.
Methods
We report this study in accordance with the Consolidated Reporting of Qualitative Research checklist.27 This study was conducted in a closed ICU in an urban, academic medical center from December 2012 through November 2013. The institutional review board at the University of Pennsylvania approved this study.
Study Design
Semistructured interviews analyzed with a qualitative content-analysis approach were used to explore ICU survivors’ and family members’ perspectives on ICU processes of care and postdischarge outcomes.
Participants, Sampling, and Recruitment
We recruited adult, English-speaking patients or patient caregivers with a medical ICU LOS of 4 or more days. This criterion ensured sampling of participants with sufficient experiences of critical care to enable informed perspectives. We purposively selected participants to achieve a diverse patient sample by intentionally recruiting individuals of different age, sex, and race as opposed to random sampling or consecutive sampling of all patients admitted to the ICU for at least 4 days and their family caregivers.28 We excluded patients and caregivers who received direct medical care by study team members.
After receiving attending-physician approval, the research team approached eligible patients for consent to contact after hospital discharge. We sought consent from a surrogate decision-maker for patients without decision-making capacity. For enrolled patients, we also recruited a family caregiver to participate, specifically recruiting the caregiver identified as the patient’s surrogate decision-maker. If a patient declined consent, we did not recruit family. We contacted participants at least 7 days after hospital discharge to schedule an interview. Family members of deceased patients were contacted at least 30 days after the patient’s death to allow time for grieving before recruitment. Participants were considered lost to follow-up if they could not be reached after 3 attempts. Participants who completed an interview were reimbursed $100.
Consistent with recommended qualitative research techniques, we did not set a sample size a priori but continued enrollment until reaching theoretical saturation.29 Theoretical saturation was declared when analysis of completed interviews ceased to yield new information.
Data Collection and Generation
Data were collected via individual hour-long interviews using a semistructured guide asking about ICU experience and life after discharge (see Supplement—available online only at www.ajccon-line.org). Interviews were conducted by the core study team or 1 of 2 trained research assistants. Questions were generated by examination of relevant literature, consensus-building, and consultation with diverse experts in ICU outcomes research. Interviews were conducted in person, with telephone used only if travel distance was prohibitive. Interviews were audio recorded and transcribed verbatim. Participants provided self-defined demographic information.
Data Analysis and Rigor
Two investigators (C.L.A., S.M.L.) conducted line-by-line review of transcripts to identify key concepts. Codes were created and defined in the codebook with decision rules for application. Codes were applied to all transcripts, and 100% of transcripts were double coded. Data were managed using NVivo software (version 10; QSR International). The interrater reliability function in NVivo was used to gauge agreement between coders (κ > 0.7).
We used qualitative content analysis whereby the data generated were analyzed through the systematic classification process of coding and identifying themes or patterns within participants’ perspectives.30,31 A team consisting 2 critical care physicians, a medical anthropologist with a background in nursing, a medical student, and 2 of research assistants met regularly to discuss emerging themes that were organized into 2 groups: (1) ICU processes of care and (2) postdischarge outcomes. After interviews were coded, themes and representative quotes were continually reviewed and interpreted on the basis of consensus.
Intensive care patients and family members participated in qualitative interviews after hospital discharge.
Results
Participant Flow Through Study and Demographics
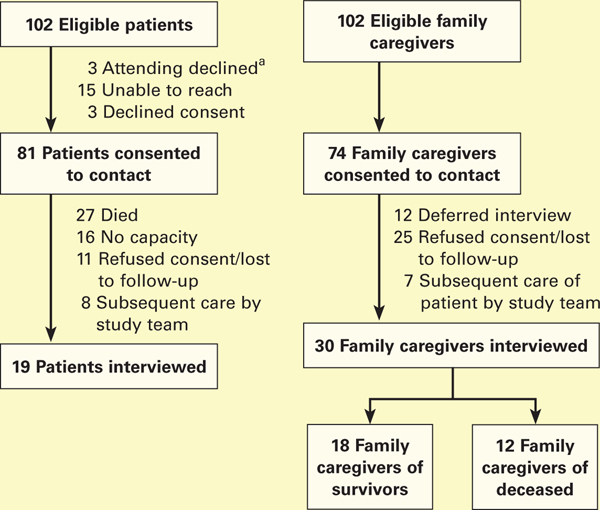
The recruitment flow is presented in the Figure. We identified 102 eligible patients and obtained consent to contact 81 patients (79%). After exclusion of patients subsequently cared for by a team member (10%), those who died (33%) or did not regain decision-making capacity (20%), as well as those who subsequently declined the interview or were lost to follow-up (14%), 19 patients completed interviews. Of the 102 eligible family caregivers, we obtained consent to contact 74 family caregivers (73%). After exclusion of family caregivers whose relative was subsequently cared for by a team member (9%) and those who subsequently declined the interview or were lost to follow-up (34%), 30 family caregivers completed interviews. We did not contact 12 family caregivers because we reached theoretical saturation before their interviews were scheduled. Of the final sample of 30 family members, 18 were family members of survivors and 12 were family members of patients who died. Interviews occurred a median of 18 days (interquartile range, 14–47 days) after hospital discharge for patients and 35 days for family members (interquartile range, 16–48 days).
Figure.
Recruitment of study participants.
a For 3 patients, the attending physician declined recruitment so as not to overburden family members of patients who were actively dying.
Time and effort that providers put into communicating with patients was highly valued and often led patients to feel less alone and afraid.
Participant characteristics are described in Table 1. Patients’ demographic characteristics were similar to those seen in our medical ICU in the year preceding the study with respect to age and race. Most patient participants were women (68%; Table 1). Among patients who completed interviews, the median ICU LOS was 11 days (interquartile range, 7–13 days) and hospital LOS was 23 days (interquartile range, 15–29 days). We grouped themes into 2 major categories: processes of care within the ICU and outcomes after the ICU.
Table 1.
Characteristics of participants interviewed
| Characteristic | All patients with an MICU stay ≥ 4 d in year preceding study (n = 563) | Patients (n = 19) | Family caregivers (n = 30) |
|---|---|---|---|
| Age, mean (SD), y | 58.9 (15.9) | 55.4 (11.8) | 55.3 (10.5) |
| Female, % | 43.7 | 68 | 53 |
| Race other than White, % | 45.5 | 47 | 13 |
| Days in ICU, median (IQR) | 7.6 (5.2–12.3) | 11 (7–13) | NA |
| Days in hospital, median (IQR) | 13.8 (8.5–22.7) | 23 (15–29) | NA |
| Discharge location, % | |||
| Deceased/hospice | 24.7 | 0 | NA |
| Home | 35.6 | 68 | NA |
| Facility | 39.7 | 32 | NA |
| Relationship to patient, % | |||
| Spouse/partner | NA | NA | 57 |
| Sibling | NA | NA | 17 |
| Child | NA | NA | 17 |
| Parent | NA | NA | 10 |
| Patient outcome, % | |||
| Alive | NA | NA | 47 |
| No capacity | NA | NA | 13 |
| Dead | NA | NA | 40 |
Abbreviations: ICU, intensive care unit; IQR, interquartile range; MICU, medical ICU; NA, not applicable.
ICU Processes of Care
Communication.
Both patients and their families prioritized communication. From the patients’ perspective, understanding the medical situation was challenging, but they appreciated when providers would speak directly and clearly. Patients also wanted to feel heard and understood by the medical team. Additional time and effort providers put into communicating with patients was highly valued and often led patients to feel less alone and afraid. Families appreciated being included in communication on rounds and the opportunity to ask questions:
The communication was just crucial, knowing as much, and understanding as much as I could about what was going on with him, and understanding what the medical staff didn’t understand. — Family caregiver (patient survived)
Patient Comfort.
Ensuring patient comfort and avoidance of pain was a priority of patients and family. Patients described not wanting to wait for medication when in pain and appreciated attention to comfort. Among family caregivers of deceased patients, sensing that the patient was comfortable at the end of life was particularly important:
I mean that is one thing the doctors and the nurses kept talking about was his comfort level and whether he was comfortable, feeling okay, as much as possible through all of this. I mean that certainly is what matters to family members. — Family caregiver (patient died)
Exhaustive Medical Care.
Patients and family members frequently wanted to know the medical team was “doing everything.” Feeling a sense that the team was providing exhaustive care was emphasized especially by family caregivers of deceased patients. Believing the medical team had attempted all potentially beneficial treatment strategies seemed to bring a sense of peace to family members whose loved ones died.
You want to make sure that everything is being done that can possibly be done within reason. —Family caregiver (patient died)
Postdischarge Outcomes
Survival, Above All Else.
For approximately 25% of participants, survival was the most important ICU outcome. For these individuals, even prompting deliberation on functional outcomes did not result in more nuanced responses:
The main thing is staying alive. In my book, that’s important. I don’t know what else would be important, I don’t know. That’s it. —Patient
Survival Is Important, But With Qualifications.
For most participants, however, survival alone was inadequate. These individuals either discussed survival in the context of qualifications or described a range of specific functional outcomes that mattered most. Meaningful or satisfactory survival required a minimally acceptable quality of life or evidence the patient was continuing to improve, such that he or she would eventually reach their minimum quality of life:
As long as you have some quality of life, yes, it’s worth it, anything is worth it as long as you have some quality of life. —Patient
Maintaining Physical and Cognitive Functioning.
About 50% of participants specifically mentioned either physical function, with an emphasis on independence and not being a burden to others, or cognitive function, with an emphasis on ability to communicate. Some participants connected physical function and cognition to quality of life. Others focused more on specifics of the abilities they would want to maintain:
I don’t really want to be sitting in a bed somewhere and somebody having to wash me and turn me … that’s not a quality of life to me. —Family caregiver (patient survived)
Well, physical supports you can find those … You don’t even know what quality of life they’re getting at that point if they can’t communicate that to you. So being mentally clear and being able to communicate what they need to me is more important than being able to do it themselves. —Family caregivers (patient survived)
Length of Stay.
We specifically probed participants about ICU LOS and found variable results. Some participants highly valued short ICU stays and would tolerate only very brief trials of critical care, whereas others expressed willingness to accept any duration of ICU stay if there was a chance for survival. Responses varied within and across participant groups, with many family members explicitly noting that their preferences for the duration of the patient’s care may not reflect what the patients would choose:
Six or 7 weeks. Yes. I think that’s enough, especially if you know the person wouldn’t want to live that way. —Family caregiver (patient survived)
No, I want her alive, and if it takes a year, I know she wouldn’t like it. I can guarantee you she wouldn’t like it. She didn’t like 2 weeks or whatever it was in there. I didn’t keep the exact date, but no, I would say yes, you’re going in. —Family caregiver (patient survived)
Outcomes Worse Than Death
We asked participants if there were outcomes of critical care that could be worse than death. For 9 participants, the answer was emphatically no. However, for the majority, there were levels of dysfunction considered as bad as or worse than death.
Inability to Communicate.
The inability to communicate with family or recognize and interact with loved ones was viewed as worse than death for 11 participants. Some participants mentioned coma as being worse than death. When prompted to explain what about being a coma was worse than death, responses aligned with the inability to communicate with family:
If I’m not capable of communicating, no.
I don’t want to live like that. —Patient
Physical Disability.
Severe physical disability was mentioned just as often as the inability to communicate. Descriptions of physical states worse than death included impaired mobility or inability to manage self-care. In discussing the importance of the ability to manage self-care, such as feeding or toileting, the concept of independence seemed to overlap with maintaining dignity:
I think if I couldn’t do anything and there’s no possibility of me getting back to being able to take care of myself, then I don’t think I’d want to go through it. —Family caregiver (patient survived)
Dependence on Machines or Medical Equipment.
Several patients and family caregivers mentioned dependence on machines, specifically the mechanical ventilator. In general, these participants were individuals who had experienced mechanical ventilatory support themselves or had witnessed their family member receiving mechanical ventilatory support:
I think being stuck on a machine would be unacceptable for me. —Family caregiver (patient died)
Severe or Constant Pain.
Finally, 6 participants thought that living with severe or constant pain would be worse than death:Constant, constant pain … I wouldn’t want to live like that. —Patient
Additional representative quotations are included in Table 2; relative frequencies by participant category are presented in Table 3.
Table 2.
Emergent Themes of ICU Processes of Care, Post-Discharge Outcomes, and States Worse than Death with Illustrative Quotations
| Theme | Illustrative quotations | Participant |
|---|---|---|
| ICU processes of care | ||
| Open, transparent, and frequent communication by the medical team | The communication was just crucial, knowing as much, and understanding as much as I could about what was going on with him [the patient], and understanding what the medical staff didn’t understand. | Family caregiver, patient survived |
| They [family members] should be able to question the doctors and get the right answers. Don’ talk to me as if I went to school with you for 12 years, break it down. | Patient | |
| He [one particular physician] was the first one to say give Ms. X a piece of paper. Then I was able to write and communicate. Why didn’ the rest of them [other members of medical team]? … I had all these people, but nobody’s helping me. | Patient | |
| Ensuring patient comfort and avoidance of pain | I mean that is one thing the doctors and the nurses kept talking about was his [the patient’s] comfort level and whether he was comfortable, feeling okay, as much as possible through all of this. I mean that certainly is what matters to family members. | Family caregiver, |
| She [the patient] said she didn’t want to be in that kind of pain and as a sister who loves her dearly knows that you don’t know the feeling … I don’t know what she was going through. I don’t know how the pain was. All I know is I wanted it to be gone, I just wanted it to be gone | Family caregiver, patient died | |
| That’s very difficult to deal with as a family member to see them [the patient] in pain and know you can’t do anything about it. I [had] a lot of questions about how well they are controlling it because we don’t want a narcotic issue where she’s addicted to this or addicted to that, but at the same time you don’t want her sitting there hurting all day long because then she can’t enjoy herself … To me it’s extremely important that she not be in pain and can participate and do things and be comfortable. That’s like top of the line because it has been a very painful year for her. | Family caregiver, patient survived | |
| Sensing that the medical team was providing exhaustive care | Obviously, you always want to see the loved one comes home but you want to make sure that everything is being done that can possibly be done within reason. | Family caregiver, patient died |
| The family was like, “Did you get everything done right?” … and I said, “You know what? We know, we were at the hospital. The doctors did all they could. We asked them to do all they could.” And I believe that they did all they could. | Family caregiver, patient died | |
| If you die there [in the ICU] then you know they’ve done everything they can, or you would hope that they’ve done everything they can, and it’s just your time to go, but at least you’d be around people that tried to take care of you. | Patient | |
| Postdischarge outcomes | ||
| Survival, above all else, is the most important outcome | The main thing is staying alive. In my book, that’s important. I don’t know what else would be important, I don’t know. That’s it. | Patient |
| Well, ultimately the most important thing is that the patient leaves the ICU on their own accord and not in a body bag. That is the most important. | Family caregiver, patient survived | |
| Not dying was the big thing. | Patient | |
| Survival is important, but only if you have an acceptable quality of life | As long as you have some quality of life, yes, it’s worth it, anything is worth it as long as you have some quality of life, where you know who you are; you know who the people are around you and you can experience life events. | Patient |
| Even if they lived what kind of quality of life they had. Was what you did put them in a better position than where they are now. | Family caregiver, patient survived | |
| Some people would rather have their loved ones irregardless and I think it depends on the person. [My husband] would not want irregardless. He would want his quality of life. | Family caregiver, patient died | |
| Maintaining physical function, particularly independence | I don’t really want to be sitting in a bed somewhere and somebody having to wash me and turn me … that’s not a quality of life to me. | Family caregiver, patient survived |
| I would like to live a productive life as long as possible, not necessarily working but just being where I would be productive to keep my facilities, some form of mobility and if I could do those things for as long as I can. | Patient | |
| Your body does have a tendency if you’re not using parts of it not to work right, but she’s [the patient’s] coming back. She’s coming back good … her strength is coming back … Overall she is better, I would say. I would say it is better for her. | Family caregiver, patient survived | |
| Postdischarge outcomes | ||
| Maintaining cognitive function, particularly ability to communicate with others | I like my mental functioning … if you don’t have the mental functioning, you ain’t worth nothing. | Patient |
| Anything is worth it as long as you have some quality of life, where you know who you are, you know who the people are around you, and you can experience life events and know what’s happening and who is around you … You can’t move, so what? As long as you know who you are and what’s going on and who is around you. | Family caregiver, patient died | |
| Well, physical supports you can find those. If the person isn’t mentally clear enough to help you, then there’s really not a lot you can do. You don’t even know what quality of life they’re getting at that point if they can’t communicate that to you. So being mentally clear and being able to communicate what they need to me is more important than being able to do it themselves. | Family caregiver, patient survive | |
| States worse than death | ||
| There is no outcome worse than death | Dying would be the worst thing that could possibly happen … I don’t think there’s anything worse. | Family caregiver, patient survived |
| There is nothing worse than dying. | Family caregiver, patient died | |
| I don’t think so when you weight them side by side. They seem that way at the time but I think when you put them side by side I think given the choice you would take the choice of okay, I have to do this for now if I want to stay alive. | Patient | |
| Inability to communicate with others | If I’m not capable of communicating, no. I don’t want to live like that. | Patient |
| If I was noncommunicative at all, ventilated and if they just come in and look at me and they don’t know whether they are communicating with me or not and whether I can say it or not they don’t know. I think they would say okay, we can put up with it so long. We don’t think this is what he would want, and I have already spelled that out. Then they would let me go. | Patient | |
| If you’re just going to sit there and not know who you are, know who they are, not be able to interact, no. | Family caregiver, patient died | |
| Physical disability | I think if I couldn’t do anything and there’s no possibility of me getting back to being able to take care of myself, then I don’t think I’d want to go through it. | Family caregiver, patient survived |
| I would hate to be where I couldn’t do nothing for myself, like have to depend on somebody to even go to the bathroom; bedridden, I’m not sure I want to live like that. I don’t think I would kill myself, but I would hope I’d go quickly. | Patient | |
| The situation I was in where I was immobilized and can’t help yourself at all and that’s bad. That ain’t good at all. When you’re doing things for yourself and all of a sudden you’re stuck. No, can’t work like that. | Patient | |
| Dependence on machines | I think being stuck on a machine would be unacceptable for me. I think there are many other things that I could live with but I think being required, requiring a machine to help you to breath would not be acceptable to me. I would much rather die in the ICU than that. | Family caregiver, patient died |
| You don’t want to be just kind of there … if you are in the ICU and basically the machines are just keeping you going but you’re not able to enjoy life, then no. | Family caregiver, patient died | |
| I think the worst thing would be to be hooked up to machines to keep you alive but having no quality to your life at all would be the worst thing that could happen … obviously when you are making the decision it’s in the hopes that you are going to get better or somebody that is making it for you has the hope that you will get better. Otherwise, what is the point of hooking you up to all of these machines? And I know that things can go wrong and sometimes you do get worse instead of getting better and to me that would be the worst thing. | Patient | |
| Severe or constant pain | Constant, constant pain…I don’t mean just a pain. I am talking about the piercing type of pain that … that you definitely would have to be drugged in order to … I wouldn’t want to live like that. | Patient |
| I think just if you’re in excruciating pain that is worse. | Family caregiver, patient died | |
| Suffering, just suffering … That’s bad to just watch him scream in pain that it’s unbearable. | Family caregiver, patient survived | |
Abbreviation: ICU, intensive care unit
Table 3.
Frequency of major themes discussed by ICU patients and family caregivers
| No. of participants who
discussed theme |
||||
|---|---|---|---|---|
| Theme | Patients (n = 19) | Family caregiver, patient survived (n = 18) | Family caregiver, patient died (n = 12) | Total (n = 49) |
| ICU processes of care | ||||
| Open, transparent, and frequent communication | 13 | 4 | 2 | 19 |
| Ensuring patient comfort and avoidance of pain | 9 | 5 | 3 | 17 |
| Sensing that the medical team was providing maximal care | 2 | 2 | 6 | 10 |
| Postdischarge outcomes | ||||
| Survival, above all else, is the most important outcome | 6 | 3 | 3 | 12 |
| Survival is important, but only if you have an acceptable quality of life and the patient is improving | 5 | 5 | 5 | 15 |
| Maintaining physical function, particularly independence | 8 | 5 | 1 | 14 |
| Maintaining cognitive function, particularly ability to communicate with others | 4 | 5 | 2 | 11 |
| Outcomes worse than death | ||||
| There is no outcome worse than death | 5 | 2 | 2 | 9 |
| Inability to communicate with others | 6 | 3 | 2 | 11 |
| Physical disability | 4 | 4 | 3 | 11 |
| Dependence on machines | 2 | 4 | 3 | 9 |
| Severe or constant pain | 2 | 3 | 1 | 6 |
Abbreviation: ICU, intensive care unit.
Discussion
In this qualitative study of patients with ICU experience and family members, we identified key themes categorized within ICU processes of care and discharge outcomes. Communication, patient comfort, and sensing the medical team provided exhaustive care emerged as essential aspects of the ICU experience indicative of quality care. As primary bedside providers, nurses are especially well suited to influence patients’ and family’s perceptions of communication and patient comfort. Participants consistently identified survival, quality of life, physical functioning, and cognitive functioning as key postdischarge outcomes. Notably, although some participants described survival as the most important outcome, most qualified survival or described additional functional outcomes as being equally or more important. Participants described a set of potential outcomes of critical illness considered worse than death, namely an inability to communicate with others, dependence on machines, severe physical disability, and severe or constant pain.
Although some participants described survival as the most important outcome, most qualified survival or described additional functional outcomes as being equally or more important.
Recently, the patient experience in the ICU has garnered more attention.18–23,25,32 Needham et al26 have proposed a set of patient-centered outcomes including survival, physical function, cognition, mental health, health-related quality of life, and pain as core outcomes to measure after ICU discharge. Our study extends their work in several key ways. First, we incorporated individual interviews with ICU survivors and family members of survivors and of deceased patients. In prior studies, researchers focused primarily on the perspectives of clinicians, rather than those of patients and family members. Others have included only the experiences of survivors and their family members,33–37 which could influence the breadth of perspectives elicited. Furthermore, studies in which patient perspectives on clinical outcomes were incorporated generally were focused on patients admitted to the ICU with a specific disease, such as acute respiratory failure. In contrast, our qualitative interviews included perspectives from a broader population of ICU stakeholders by incorporating family members and additional disease conditions. The themes that emerged from our study align with those identified by Needham et al,26 extending their findings and perhaps broadening the group of patients to whom they apply.
We also identified outcomes described as being as bad as or worse than death. This framing generated different responses from participants than asking about outcome measures or ways to measure success in the ICU, and could serve as a tool for understanding health states that patients and family members would prefer to avoid when considering aggressive medical interventions. The disease states that participants described overlapped with those specifically queried in an earlier survey of hospitalized patients with serious illness.38 By virtue of open-ended probing, findings in this qualitative study may be less susceptible to affective forecasting errors than in the prior survey study. Still, more work is needed to understand whether avoidance of these states, itself, could be used as an important PFCC outcome measure or value-elicitation tool. Perhaps this phrasing could be developed into a tool that bedside nurses could implement to better understand patients’ priorities for postdischarge outcomes.
Several limitations should be considered when interpreting this study. We conducted the study in a single medical ICU that has high mortality rates and high median LOS. Patients in other types of ICUs may express different priorities. Second, because all our interviews were conducted in English, findings may not encompass the views of patients and family members from a more diverse range of cultural backgrounds. Third, interviews of patients were naturally limited to survivors who regained decision-making capacity. An inherent limitation is that these perspectives may not reflect those of patients who died or remain incapacitated. Finally, we were able to interview each patient and family member at only a single time after hospital discharge or patient death and cannot report how perspectives changed over time.
Conclusion
This study provides a qualitative assessment of the experiences of patients and families in the ICU. Communication and patient comfort, 2 processes of care highly dependent on attentive and quality bedside nursing, were especially important during the ICU experience. Building on proposed guidelines for patient-centered ICU outcomes, we examined 2 essential yet underdeveloped constructs: PFCC outcomes after critical illness and outcomes that are no more desirable than death. Work is needed to determine whether ICU interventions should be evaluated on the basis of the degree to which they reduce the frequency of outcomes that critically ill patients and family members consider equal to or worse than death. Conducting larger studies in which the measurability, consistency across, and stability within individuals of such perceptions of states worse than death are assessed could be a next step in determining suitability of such an outcome for ICU trials. Overall, this work underscores the importance of researchers and clinicians embracing a more diverse approach to outcome measurement and continuing to develop PFCC methods for evaluating critical care interventions.
Supplementary Material
ACKNOWLEDGMENTS
We thank the patients and their families who participated in this study. We also thank Saida Kent, BS, for her contribution to data extraction for this project, as well as Cary Hilbert, BS, and Lauren Strelec, BS, for their contributions to the interview process.
FINANCIAL DISCLOSURES
This study was supported by the Doris Duke Charitable Foundation (C.L.A.), the US National Institutes of Health, National Heart, Lung, and Blood Institute (grants 5T32HL098054-09 [C.L.A.] and K99 HL141678 [M.O.H.]), the University of Pennsylvania Health System and the Institute for Translational Medicine and Therapeutics (S.M.L.), and the Otto Haas Charitable Trust (S.D.H.).
Contributor Information
Catherine L. Auriemma, Division of Pulmonary, Allergy, and Critical Care Medicine, Department of Medicine; Palliative and Advanced Illness Research (PAIR) Center; and Leonard Davis Institute of Health Economics, University of Pennsylvania, Philadelphia..
Michael O. Harhay, Department of Biostatistics, Epidemiology and Informatics, Perelman School of Medicine, University of Pennsylvania..
Kimberley J. Haines, Department of Physiotherapy, Western Health; Department of Physiotherapy, The University of Melbourne; and Australian and New Zealand Intensive Care Research Centre, Monash University, Melbourne, Victoria, Australia..
Frances K. Barg, Department of Family Medicine and Community Health, University of Pennsylvania Perelman School of Medicine; and Department of Anthropology, University of Pennsylvania School of Arts and Sciences, Philadelphia..
Scott D. Halpern, Division of Pulmonary, Allergy, and Critical Care Medicine, Department of Medicine; PAIR Center; Leonard Davis Institute of Health Economics; Department of Biostatistics, Epidemiology and Informatics, and Department of Medical Ethics and Health Policy Perelman School of Medicine, University of Pennsylvania..
Sarah M. Lyon, Division of Pulmonary, Allergy, and Critical Care Medicine, University of Pennsylvania; and Department of Medicine, Division of Pulmonary & Critical Care Medicine, Corporal Michael J. Crescenz Veterans Affairs Medical Center, Philadelphia, Pennsylvania..
REFERENCES
- 1.Girard TD, Shintani AK, Jackson JC, et al. Risk factors for post-traumatic stress disorder symptoms following critical illness requiring mechanical ventilation: a prospective cohort study. Crit Care. 2007;11(1):R28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Turnbull AE, Rabiee A, Davis WE, et al. Outcome measurement in ICU survivorship research from 1970 to 2013: a scoping review of 425 publications. Crit Care Med. 2016; 44(7):1267–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yehya N, Harhay MO, Curley MAQ, et al. Reappraisal of ventilator-free days in critical care research. Am J Respir Crit Care Med. 2019;200(7):828–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harhay MO, Ratcliffe SJ, Small DS, et al. Measuring and analyzing length of stay in critical care trials. Med Care. 2019;57(9):e53–e59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McPeake J, Mikkelsen ME, Quasim T, et al. Return to employment following critical illness and its association with psychosocial outcomes: a systematic review and meta-analysis. Ann Am Thorac Soc. 2019;16(10):1304–1311. [DOI] [PubMed] [Google Scholar]
- 6.McPeake J, Hirshberg EL, Christie LM, et al. Models of peer support to remediate post-intensive care syndrome: a report developed by the Society of Critical Care Medicine Thrive International Peer Support Collaborative. Crit Care Med. 2019;47:E21–E27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Haines KJ, McPeake J, Hibbert E, et al. Enablers and barriers to implementing ICU follow-up clinics and peer support groups following critical illness. Crit Care Med. 2019;47(9): 1194–2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Selby JV, Beal AC, Frank L. The Patient-Centered Outcomes Research Institute (PCORI) national priorities for research and initial research agenda. JAMA. 2012;307:1583–1584. [DOI] [PubMed] [Google Scholar]
- 9.D’Arcy LP, Rich EC. From comparative effectiveness researchto patient-centered outcomes research: policy history and future directions. Neurosurg Focus. 2012;33:E7. [DOI] [PubMed] [Google Scholar]
- 10.Weiner SJ, Schwartz A, Sharma G, et al. Patient-centereddecision making and health care outcomes: an observational study. Ann Intern Med. 2013;158(8):573–579. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Medicare & Medicaid Services. HCAHPS: Patients’ Perspectives of Care Survey. 2020. Accessed June 15, 2020. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/HospitalHCAHPS
- 12.Harhay MO, Wagner J, Ratcliffe SJ, et al. Outcomes and statistical power in adult critical care randomized trials. Am J Respir Crit Care Med. 2014;189(12):1469–1478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dinglas VD, Faraone LN, Needham DM. Understanding patient-important outcomes after critical illness: a synthesis of recent qualitative, empirical, and consensus-related studies. Curr Opin Crit Care. 2018;24(5):401–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Keenan SP, Carlet J, Curtis R, et al. Health services research rounds: patient-centered outcomes. J Crit Care. 2002;17(4): 221–234. [DOI] [PubMed] [Google Scholar]
- 15.Gajic O, Ahmad SR, Wilson ME, et al. Outcomes of critical illness: what is meaningful? Curr Opin Crit Care. 2018;24(5): 394–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haines KJ, Kelly P, Fitzgerald P, et al. The untapped potential of patient and family engagement in the organization of critical care. Crit Care Med. 2017;45(5):899–906. [DOI] [PubMed] [Google Scholar]
- 17.Blackwood B, Ringrow S, Clarke M, et al. A core outcome set for critical care ventilation trials. Crit Care Med. 2019; 47(10):1324–1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Simini B Patients’ perceptions of intensive care. Lancet. 1999;354(9178):571–572. [DOI] [PubMed] [Google Scholar]
- 19.Hofhuis JGM, Spronk PE, van Stel HF, et al. Experiences of critically ill patients in the ICU. Intensive Crit Care Nurs. 2008;24(5):300–313. [DOI] [PubMed] [Google Scholar]
- 20.Meriläinen M, Kyngäs H, Ala-Kokko T. Patients’ interactions in an intensive care unit and their memories of intensive care: a mixed method study. Intensive Crit Care Nurs. 2013; 29(2):78–87. [DOI] [PubMed] [Google Scholar]
- 21.Stein-Parbury J, McKinley S. Patients’ experiences of being in an intensive care unit: a select literature review. Am J Crit Care. 2000;9(1):20–27. [PubMed] [Google Scholar]
- 22.Nelson JE, Puntillo KA, Pronovost PJ, et al. In their own words: patients and families define high-quality palliative care in the intensive care unit. Crit Care Med. 2010;38(3): 808–818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Prinjha S, Field K, Rowan K. What patients think about ICU follow-up services: a qualitative study. Crit Care. 2009; 13(2):R46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Auriemma CL, Lyon SM, Strelec LE, et al. Defining the medical intensive care unit in the words of patients and their family members: a freelisting analysis. Am J Crit Care. 2015; 24(4):e47–e55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hashem MD, Nallagangula A, Nalamalapu S, et al. Patient outcomes after critical illness: a systematic review of qualitative studies following hospital discharge. Crit Care. 2016; 20(1):345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Needham DM, Sepulveda KA, Dinglas VD, et al. Core outcome measures for clinical research in acute respiratory failure survivors: an international modified Delphi consensus study. Am J Respir Crit Care Med. 2017;196(9):1122–1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Heal Care. 2007; 19(6):349–357. [DOI] [PubMed] [Google Scholar]
- 28.Curry LA, Nembhard IM, Bradley EH. Qualitative and mixed methods provide unique contributions to outcomes research. Circulation. 2009;119(10):1442–1452. [DOI] [PubMed] [Google Scholar]
- 29.Bradley EH, Curry LA, Devers KJ. Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health Serv Res. 2007;42(4):758–1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moretti F, van Vliet L, Bensing J, et al. A standardized approach to qualitative content analysis of focus group discussions from different countries. Patient Educ Couns. 2011; 82(3):420–428. [DOI] [PubMed] [Google Scholar]
- 31.Cho JY, Lee EH. Reducing confusion about grounded theory and qualitative content analysis: similarities and differences. Qual Rep. 2014;19(32):1–20. [Google Scholar]
- 32.Curley MA. Patient-nurse synergy: optimizing patients’outcomes. Am J Crit Care. 1998;7(1):64–72. [PubMed] [Google Scholar]
- 33.Sawdon V, Woods I, Proctor M. Post-intensive care interviews: implications for future practice. Intensive Crit care Nurs. 1995;11(6):329–332. [DOI] [PubMed] [Google Scholar]
- 34.Czerwonka AI, Herridge MS, Chan L, et al. Changing support needs of survivors of complex critical illness and their family caregivers across the care continuum: a qualitative pilot study of Towards RECOVER. J Crit Care. 2015;30(2): 242–249. [DOI] [PubMed] [Google Scholar]
- 35.Chiang VCL. Surviving a critical illness through mutually being there with each other: a grounded theory study. Intensive Crit Care Nurs. 2011;27(6):317–330. [DOI] [PubMed] [Google Scholar]
- 36.Adamson H, Murgo M, Boyle M, et al. Memories of intensive care and experiences of survivors of a critical illness: an interview study. Intensive Crit Care Nurs. 2004;20(5):257–263. [DOI] [PubMed] [Google Scholar]
- 37.Ågård AS, Egerod I, Tønnesen E, et al. Struggling for independence: a grounded theory study on convalescence of ICU survivors 12 months post ICU discharge. Intensive Crit Care Nurs. 2012;28(2):105–113. [DOI] [PubMed] [Google Scholar]
- 38.Rubin EB, Buehler AE, Halpern SD. States worse than death among hospitalized patients with serious illnesses. JAMA Intern Med. 2016;176(10):1557–1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.