Abstract
Objectives
Burnout among health care workers is highly prevalent and has profound impact on quality of care. Hospital on‐duty schedules lead to long working hours and short sleeping hours; both are common factors associated with burnout. We examined the dose‐response relationship and the potential mediating role of sleeping hours on the association between working hours and burnout among health care workers.
Methods
We collected data on the burnout status, using the Mandarin version of the Copenhagen Burnout Inventory (subscales measure work‐related and personal burnouts), working hours, sleeping hours, and relevant measures for 2081 health care personnel who underwent a routine health examination in a medical center in Taiwan during 2016‐2017. Four subgroups were compared: physicians (n = 369), nurses (n = 973), technicians (n = 391), and administrators (n = 348).
Results
Average weekly working hours are associated with burnout scores in a non‐linear dose‐response manner. Compared with a work week of 40 hours, the odds ratio of work‐related burnout doubled when hours exceeded 60, tripled when hours exceeded 74, and quadrupled when hours exceeded 84. Physicians’ burnout is less susceptible to incremental increases in working hours, compared to the situations in other health care workers. The proportions eliminated by reducing sleeping hours were 25%‐73% for physicians and 7%‐29% for nurses respectively.
Conclusions
Our findings suggest that working hours are associated with burnout, and the association was partially mediated by sleeping hours.
Keywords: burnout, health care workers, mediation analysis, sleeping hours, working hours
1. INTRODUCTION
Burnout among health care workers was first reported in the United States in 1974, 1 nearly a half‐century ago. Since then, the condition has become prevalent worldwide, with reported aggregate prevalence of 44% in medical students, 2 51% in residents, 3 80% in physicians, 4 and 15%‐60% in nurses. 5 Burnout is characterized by feelings of emotional exhaustion, depersonalization, and reduced personal accomplishment. 6 It not only affects health care workers’ personal health 7 but also is associated with perceived competence, medical performance, and medical errors. 8 , 9 Increasing concern over burnout among health care workers has led to new attention to policies and solutions for burnout prevention—that is, to eliminate causes of burnout. 10 , 11 Epidemiological studies contribute to identifying several predictive factors of burnout, such as female gender, low reported job satisfaction, and long working hours, 12 and offering solution options to prevention strategies. Among predictive factors of burnout across the literature, working hours can be measured and controlled more objectively.
Burnout caused by long working hours among health care workers has commanded considerable attention in recent years, 11 , 13 especially policies to restrict long working hours. For example, the United States implemented a limit of up to 80 hours per week for medical residents in 2011. 14 A cohort study of internal medicine resident physicians at three academic institutions indicated the proportion of working hours >70 per week decreased by 5% after 2011 and burnout prevalence and incidence decreased by 8%‐13%, although these changes did not reach statistical significance. 15 The policy was stricter in Europe; for example, the German policy, following the European Working Time Directive, limited hospital physicians’ working hours at a limit of up to 48 hours per week. 16 A follow‐up of 328 physicians in Hamburg indicated a significant decrease in weekly working hours by 4.5, but the rate of burnout was higher. These inconsistent results trigger our first research question: whether the shape of the dose‐response relationship differs among health care workers who work 80 hours or less per week? To answer this question, we should depict a dose‐response relationship between working hours and burnout, and examine whether they are linear or non‐linear. A study that includes a group of health care workers whose hours of work range at least from 48 to 80 or more could supply this information.
However, reducing working hours might be a challenge during the COVID‐19 pandemic when health care workers are struggling with long working hours. 17 , 18 Therefore, the identification of other modifiable risk factors of burnout and the development of effective intervention strategies for managing and mitigating population vulnerabilities to burnout are crucial. Multiple pathways linking the long working hours to burnout, such as sleep deprivation, 19 may also contribute to explain the inconsistency. Long working hours imply that people are spending more time at work, and, thus, when hours of work increase, hours available for sleep may be reduced. 20 It has been well‐documented that people who sleep less than 6 hours per day are at higher risk of developing clinically defined burnout. 21 The main purpose of sleep is for the body to restore energy and autonomic response function. 22 , 23 The mechanism linking sleep deprivation and burnout includes the increased activity of 2 neuroendocrine stress systems—the autonomic sympathoadrenal system and the hypothalamic‐pituitary‐adrenal axis. 24 Although workers’ burnout differs between working hours, sleeping hours (a predictor of burnout) of workers with different working hours may be also different. Thus, we assumed that there were conditional relationships between working hours and burnout in different sleeping hours. While sleep duration and sleep quality have been recognized as a mediator to explain the association between job stress, sleep problems, and burnout in non‐health care workers, 25 , 26 previous studies of health care workers treated working hours and sleeping hours as independent variables when estimating their association with burnout. 27 , 28 The lack of considering the potential role of sleeping hours as a mediator among the association triggers our second research question: what is the proportion of the effect of working hours on burnout mediated through sleeping hours?
While most aforementioned studies reported burnout situations for physicians and nurses, a Taiwanese study compared burnout levels of physicians and nurses with those of other medical professions, such as medical technicians and administrative staff. 29 Nurses had the highest prevalence of personal and work‐related burnout (66%‐73%), while the prevalence of burnout among physicians, medical technicians, and administrative staff was unexpectedly similar—ranging from 32% to 46%. 29 During the COVID‐19 pandemic, all levels of health care workers, especially administrative staff, reported high levels of burnout. 30 These results triggered our interest in answering the above two research questions for not only physicians and nurses but also medical technicians and administrators.
We hypothesize that jobs characterized by long working hours (e.g., physicians) best fit this theory of sleep deprivation. Thus, the objectives of our study were to depict the dose‐response relationship between working hours and burnout, estimate the proportion of working hour‐related burnout that could be eliminated by resolving insufficient sleeping hours through a hypothetical intervention, and compare differences among physicians, nurses, and other health care workers within the same health care center.
2. MATERIALS AND METHODS
2.1. Study design and setting
According to the Regulations of Labor Health Protection of Taiwan, employees are subject to compliance with health examination in the following frequency: once every 5 years for people aged <40, once every 3 years for people aged ≥40 to <65, and once per year for those aged 65 or older. The China Medical University Hospital (CMUH), a medical center located in central Taiwan, provided its workers more frequent health examinations than the regulation—ie every year. Health care workers who complete personal health examinations at CMUH are asked to complete a self‐administrated questionnaire that includes questions about working hours, sleeping hours, and burnout. They may complete the questionnaire before, at or after their examination. Figure 1 shows the design of our cross‐sectional study and our timeline for data collection from each participant and how variables were analyzed in the mediation analysis.
FIGURE 1.
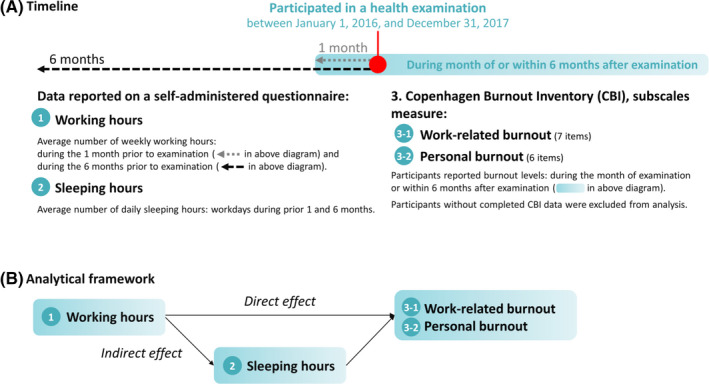
Timeline and conceptual diagram
2.2. Study period and participants
Figure 2 outlines participant recruitment, eligibility, and classification. Our main study groups of interest are physicians, nurses, and technicians. However, the workplace context of these studied group may not have to be similar to other health care workers outside this medical center or even to the general public. A reference group can help us understand the norm with a specific context. We can rely on the reference group to understand the norm of the association between working hours and burnout in the medical center. A group within the medical center more similar to the general public is the administrators. Thus, health care workers of this study included physicians, nurses, technicians, and administrators.
FIGURE 2.
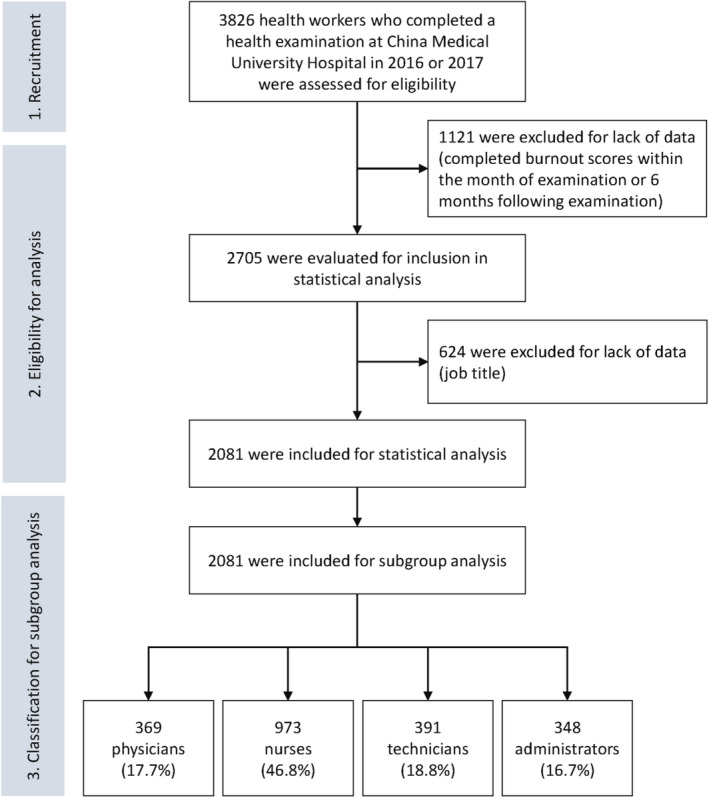
Participant recruitment, eligibility, and classification
2.3. Variables
In the questionnaire, working hours are measured in two‐dimensions: (a) average number of weekly working hours during the 1 month prior to the date of health examination, and (b) average number of weekly working hours during the 6 months prior to the date of health examination. Sleeping hours are defined as the average number of daily sleeping hours on workdays during the aforementioned two time periods, ie during the 1 and 6 months prior to the date of health examination. Both working hours and sleeping hours were self‐reported using open‐ended questions. The short‐term and long‐term measurements of both working hours and sleeping hours could be used to assess consistency and reduce potential recall bias. Alcohol and smoking data were also obtained from the questionnaire with four answer options—namely “never,” “sometimes,” “always,” and “former.” In our statistical analysis, we treated alcohol and smoking as a binary variable by combining “never” and “former” into a group and combining “sometimes” and “always” into another group.
The questionnaire also measures burnout using the Mandarin version of the Copenhagen Burnout Inventory, which consists of two subscales that assess work‐related burnout (7 items; eg Is your work emotionally exhausting?) and personal burnout (6 items; eg, How often do you feel tired?) and has been validated. 31 , 32 Each question was based on a 5‐point scale that ranged from 0 (never/almost never) to 25 (seldom), 50 (sometimes), 75 (often), and 100 (always). We calculated the average scores of the seven items for work‐related burnout and the average scores of the six items for personal burnout. Participants who completed fewer than four questions regarding work‐related burnout or fewer than three questions regarding personal burnout were classified as nonresponders. Based on these scores, work‐related burnout status was defined as high (average score ≥60), moderate (average score 46‐59), or low (average score ≤45). Similarly, personal burnout status was defined as high (average score ≥70), moderate (average score 51‐69), or low (average score ≤50). 33 In our statistical analysis, we treated each type of burnout as a dichotomous variable. Subjects with work‐related burnout scored >45 were classified as the high‐risk group and scores ≤45 as the low‐risk group. A similar dichotomous classification was applied to personal burnout with a cut‐off point at 50, i.e., >50 as the high‐risk group and ≤50 as the low‐risk group.
2.4. Data management, bias, and study size
A total of 3826 health care workers at the medical center who completed a health examination between January 1, 2016, and December 31, 2017, and also consented their data to be recorded on the hospital’s Clinical Research Data Repository, were considered eligible participants. Since burnout score was the outcome indicator of interest, we collected data on burnout scores from questionnaires completed during the month of a participant’s examination or up to 6 months after the examination (Figure 1A). We excluded 1121 participants who did not complete their questionnaire during that time period and thus lacked burnout scores. Among the 2705 participants with complete burnout scores, we collected the reported number of working hours and sleeping hours. We further excluded 624 participants who did not report job titles from the statistical analysis. The final study population for the statistical analysis comprised 2081 participants. For the subgroup analysis, we further classified participants into four groups based on their job titles: physicians (including residents), nurses, technicians (including pharmacists), and administrators (including researchers).
2.5. Quantitative variables and statistical methods
Continuous variables were expressed as mean with standard deviation (SD) and median with interquartile range (IQR), and categorical variables were expressed as frequency (percentage). To test between‐group differences, we used the nonparametric Kruskal‐Wallis test and the chi‐squared test for continuous and categorical variables respectively. We treated burnout as continuous and categorical (high, moderate, and low) variables and used linear regression models and logistic regression models, respectively, to examine the associations between working hours, sleeping hours, and burnout. We also applied the restricted cubic spline model with three knots located at the 10th, 50th, and 90th percentiles of the overall distribution for working hours to detect the possible dose‐response relationship between working hours and burnout. All models were adjusted for age, gender, body mass index, cigarette smoking, alcohol consumption, hypertension, and diabetes.
For the mediation analysis, we applied the method proposed by Lange et al. to assess the effect mediated by sleeping hours in the potential causal pathway between working hours and burnout. 34 Lange et al.’s method relies on a counterfactual framework approximated by inverse probability weighting and provides estimates of both the direct effects of working hours on burnout and the indirect effects of sleeping hours, as depicted in Figure 1B. We performed Lange’s method based on the logistic regression as our outcome was a binary variable. Moreover, as we did not observe the significant interaction between the association of the exposure and the mediator on the outcome (P > .05), all direct effects are equal (ie, control direct effect vs natural direct effect). 35 The causal interpretations in the mediation analysis are valid if the following assumptions are met: (a) there are no unmeasured confounders in the causal pathways between sleeping hours and burnout, between working hours and sleeping hours, and between working hours and burnout; (b) there is no confounder in the pathway between sleeping hours and burnout that is affected by working hours.
We applied aforementioned analyses to overall participants and also to each subgroup to investigate whether the main result remain robust. All statistical analyses were performed in SAS version 9.4 (SAS Institute, Cary), and R version 3.2.3 (R Foundation for Statistical Computing). The statistical significance level was set at α = 0.05 based on a two‐sided test.
3. RESULTS
The mean age of all participants (N = 2081) was 39.9 years; 73.7% were female and 26.3% were male (Table 1). On average, the participants had been at their current job title for 7 years. Across all participants, average weekly working hours were 46.9 hours over the past 1 month and 47.1 hours over the past 6 months. Average daily sleeping hours on workdays was 6.7 hours. The prevalence of moderate and high levels of work‐related burnout was 41.5%, while the prevalence of moderate and high levels of personal burnout was 25.3%. The percentage of high burnout was higher in people who worked ≥60 hours per week, followed by those working 41‐59 hours and ≤40 hours (Appendix Table S1).
TABLE 1.
Participant Characteristics
| Characteristics | All participants (N = 2081) | Participant groups | |||
|---|---|---|---|---|---|
| Physicians (n = 369) | Nurses (n = 973) | Technicians (n = 391) | Administrators (n = 348) | ||
| Age in years | |||||
| Mean (SD) | 39.9 (8.9) | 37.3 (9.7) | 31.0 (7.5) | 35.0 (8.8) | 37.4 (9.0) |
| Median (IQR) | 32.3 (26.8, 38.9) | 34.5 (29.8, 41.1) | 29.2 (24.9, 35.9) | 32.9 (27.9, 40.7) | 37.6 (29.9, 43.0) |
| Gender, n (%) | |||||
| Male | 548 (26.3) | 261 (70.7) | 44 (4.5) | 124 (31.7) | 119 (34.2) |
| Female | 1533 (73.7) | 108 (29.3) | 929 (95.5) | 267 (68.3) | 229 (65.8) |
| Smokes cigarettes, N (%) | 53 (2.6) | 3 (0.8) | 16 (1.6) | 15 (3.8) | 19 (5.5) |
| Drinks alcohol, N (%) | 703 (33.8) | 184 (49.9) | 255 (26.2) | 140 (35.8) | 124 (35.6) |
| Body mass index | |||||
| Mean (SD) | 23.3 (4.3) | 24.6 (4.0) | 22.7 (4.5) | 23.2 (4.0) | 23.9 (4.2) |
| Median (IQR) | 22.6 (20.1, 25.7) | 24.3 (21.6, 26.7) | 21.6 (19.5, 24.8) | 22.5 (20.3, 25.2) | 23.3 (20.6, 26.3) |
| Hypertension, N (%) | 92 (4.4) | 29 (7.9) | 23 (2.4) | 15 (3.8) | 25 (7.2) |
| Diabetes mellitus, N (%) | 33 (1.6) | 10 (2.7) | 4 (0.4) | 7 (1.8) | 12 (3.5) |
| Years in current job title | |||||
| Mean (SD) | 7.0 (7.2) | 7.0 (7.4) | 6.1 (6.5) | 7.9 (7.9) | 8.4 (7.8) |
| Median (IQR) | 4.0 (1.4, 10.6) | 4.1 (1.4, 10.0) | 3.6 (1.3, 9.5) | 4.7 (1.3, 12.5) | 6.4 (1.6, 13.0) |
| Average weekly working hours, past 1 month | |||||
| Mean (SD) | 46.9 (13.7) | 64.2 (20.8) | 43.6 (8.0) | 42.6 (6.2) | 42.7 (7.9) |
| Median (IQR) | 44 (40, 48) | 60 (48, 80) | 40 (40, 48) | 40 (40, 45) | 40 (40, 45) |
| Average weekly working hours, past 6 months | |||||
| Mean (SD) | 47.1 (13.7) | 64.6 (20.3) | 43.7 (8.0) | 42.4 (6.9) | 42.9 (7.6) |
| Median (IQR) | 44 (40, 50) | 60 (48, 80) | 42 (40, 48) | 40 (40, 45) | 40 (40, 45) |
| Average daily sleeping hours, workdays | |||||
| Mean (SD) | 6.7 (1.0) | 6.2 (0.9) | 6.8 (1.1) | 6.7 (0.9) | 6.7 (1.0) |
| Median (IQR) | 7 (6, 7) | 6 (6, 7) | 7 (6, 7) | 7 (6, 7) | 7 (6, 7) |
| Burnout, work‐related | |||||
| Score, mean (SD) | 43.4 (12.5) | 43.4 (13.6) | 45.3 (13.0) | 41.2 (9.9) | 40.7 (11.4) |
| Score, median (IQR) | 42.9 (35.7, 50.0) | 39.3 (35.7, 50.0) | 46.4 (35.7, 50.0) | 39.3 (35.7, 46.4) | 39.3 (32.1, 46.4) |
| Level: low, number (%) | 1218 (58.5) | 231 (62.6) | 483 (49.6) | 264 (67.5) | 240 (69.0) |
| Level: moderate, number (%) | 670 (32.2) | 99 (26.8) | 377 (38.8) | 105 (26.9) | 89 (25.6) |
| Level: high, number (%) | 193 (9.3) | 39 (10.6) | 113 (11.6) | 22 (5.6) | 19 (5.4) |
| Burnout, personal | |||||
| Score, mean (SD) | 44.7 (15.6) | 45.1 (16.9) | 47.1 (16.0) | 41.4 (13.5) | 41.2 (14.1) |
| Score, median (IQR) | 41.7 (33.3, 54.2) | 41.7 (33.3, 54.2) | 45.8 (33.3, 54.2) | 37.5 (29.2, 50.0) | 37.5 (29.2, 50.0) |
| Level: low, n (%) | 1555 (74.7) | 265 (71.8) | 678 (69.7) | 319 (81.6) | 293 (84.2) |
| Level: moderate, n (%) | 352 (16.9) | 67 (18.2) | 197 (20.2) | 54 (13.8) | 34 (9.8) |
| Level: high, n (%) | 174 (8.4) | 37 (10.0) | 98 (10.1) | 18 (4.6) | 21 (6.0) |
Abbreviations: IQR, interquartile range; SD, standard deviation
We observed significantly increased odds ratio (OR) estimates of burnout when the average number of weekly working hours in the past 1 month exceeded 40 hours (black lines in Figure 3; Appendix Figure S1 shows each dose‐response curve with 95% confidence interval), with a nonlinear dose‐response relationship between working hours and OR of burnout. For work‐related burnout, the ORs doubled when average working hours exceeded 59 hours over 1 month (Figure 3A) or 61 hours over 6 months (Figure 3B), tripled when hours exceeded 73 or 75 hours, and quadrupled when hours exceeded 84 hours. For personal burnout (Figure 3C,D), the ORs doubled when working hours exceeded 59 hours over 1 month (Figure 3C) or 71 hours over 6 months (Figure 3D), tripled when hours exceeded 76 or 86 hours, and quadrupled when hours exceeded 88 or 96 hours. In general, the change in ORs with an increase in average working hours was faster for short‐term averages of working hours compared to long‐term averages, as well as faster for work‐related burnout compared to personal burnout.
FIGURE 3.
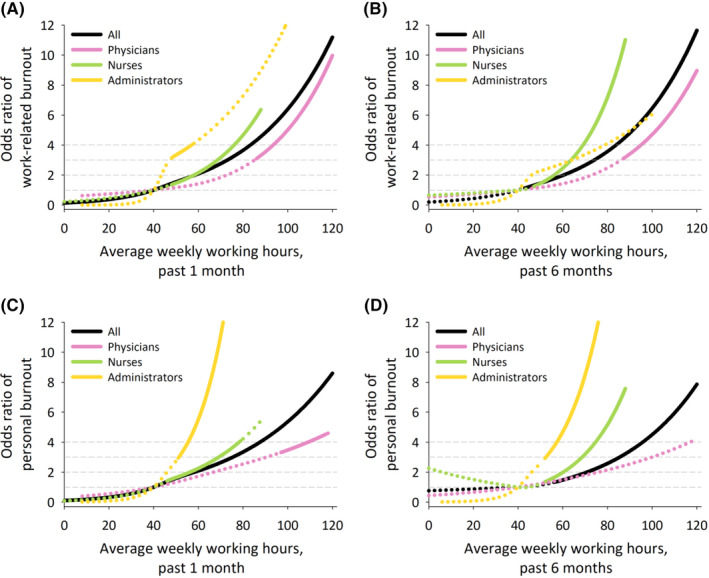
Dose‐response relationships between working hours and odds ratios of burnout. Solid lines represent odds ratios that reach statistical significance at P < .05. Dotted lines represent odds ratios that do not reach statistical significance
The number of working hours was found to be positively associated with work‐related and personal burnout, but also negatively associated with average number of sleeping hours (Appendix Table S2). By regressing both working hours and sleeping hours on burnout, we found that average sleeping hours is also significantly associated with burnout; however, the parameter estimates for the association between working hours and burnout is then reduced (Appendix Table S3). Our mediation analysis indicates that the proportion of working‐hour‐related burnout (12%‐28%) could be eliminated if sleeping hours reached six hours or more among health workers (Table 2).
TABLE 2.
Estimated total and direct effects of working hours on burnout and the effect mediated by sleeping hours
| Odds ratio (95% confidence interval) | Proportion eliminated | |||
|---|---|---|---|---|
| Total effect | Direct effect | Indirect effect | ||
| A. All participants | ||||
| Burnout, work‐related | ||||
| Average weekly working hours, past 1 month | ||||
| ≤40 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | — |
| 41‐59 | 1.50 (1.23, 1.83) | 1.44 (1.17, 1.77) | 1.02 (1.01, 1.03) | 12.0% |
| ≥60 | 1.90 (1.28, 2.80) | 1.67 (1.11, 2.50) | 1.08 (1.03, 1.13) | 25.6% |
| Average weekly working hours, past 6 months | ||||
| ≤40 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | — |
| 41‐59 | 1.42 (1.16, 1.73) | 1.37 (1.12, 1.68) | 1.02 (1.01, 1.03) | 11.9% |
| ≥60 | 1.80 (1.22, 2.64) | 1.63 (1.10, 2.41) | 1.06 (1.02, 1.11) | 21.3% |
| Burnout, personal | ||||
| Average weekly working hours, past 1 month | ||||
| ≤40 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | — |
| 41‐59 | 1.52 (1.21, 1.91) | 1.42 (1.12, 1.79) | 1.03 (1.02, 1.04) | 19.2% |
| ≥60 | 2.44 (1.61, 3.71) | 2.04 (1.30, 3.20) | 1.13 (1.07, 1.19) | 27.8% |
| Average weekly working hours, past 6 months | ||||
| ≤40 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | — |
| 41‐59 | 1.44 (1.15, 1.81) | 1.37 (1.08, 1.72) | 1.03 (1.02, 1.04) | 15.9% |
| ≥60 | 2.27 (1.51, 3.42) | 1.96 (1.27, 3.04) | 1.11 (1.06, 1.16) | 24.4% |
| B. Physicians | ||||
| Burnout, work‐related | ||||
| Average weekly working hours, past 1 month | ||||
| ≤40 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | — |
| 41‐59 | 0.92 (0.42, 2.02) | 0.90 (0.41, 1.97) | 0.99 (0.97, 1.00) | NA |
| ≥60 | 1.24 (0.59, 2.58) | 1.09 (0.53, 2.23) | 1.10 (1.01, 1.20) | 62.5% |
| Average weekly working hours, past 6 months | ||||
| ≤40 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | — |
| 41‐59 | 1.15 (0.51, 2.60) | 1.04 (0.46, 2.39) | 1.01 (1.00, 1.02) | 73.3% |
| ≥60 | 1.42 (0.66, 3.08) | 1.20 (0.55, 2.60) | 1.11 (1.01, 1.21) | 52.4% |
| Burnout, personal | ||||
| Average weekly working hours, past 1 month | ||||
| ≤40 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | — |
| 41‐59 | 1.42 (0.57, 3.55) | 1.39 (0.56, 3.44) | 0.98 (0.97, 1.00) | 7.1% |
| ≥60 | 1.95 (0.83, 4.59) | 1.71 (0.73, 4.03) | 1.13 (1.03, 1.25) | 25.3% |
| Average weekly working hours, past 6 months | ||||
| ≤40 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | — |
| 41‐59 | 1.27 (0.51, 3.18) | 1.09 (0.45, 2.69) | 1.02 (1.00, 1.03) | 66.7% |
| ≥60 | 1.62 (0.68, 3.85) | 1.30 (0.55, 3.07) | 1.13 (1.02, 1.25) | 51.6% |
| C. Nurses | ||||
| Burnout, work‐related | ||||
| Average weekly working hours, past 1 month | ||||
| ≤40 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | — |
| 41‐59 | 1.40 (1.07, 1.83) | 1.36 (1.04, 1.78) | 1.02 (1.00, 1.04) | 10.0% |
| ≥60 | 1.58 (0.73, 3.42) | 1.47 (0.67, 3.25) | 1.05 (1.01, 1.08) | 19.0% |
| Average weekly working hours, past 6 months | ||||
| ≤40 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | — |
| 41‐59 | 1.26 (0.97, 1.64) | 1.24 (0.95, 1.61) | 1.02 (1.00, 1.03) | 7.7% |
| ≥60 | 1.84 (0.90, 3.79) | 1.78 (0.86, 3.67) | 1.03 (1.00, 1.05) | 7.1% |
| Burnout, personal | ||||
| Average weekly working hours, past 1 month | ||||
| ≤40 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | — |
| 41‐59 | 1.51 (1.13, 2.02) | 1.44 (1.07, 1.92) | 1.03 (1.01, 1.06) | 13.7% |
| ≥60 | 1.52 (0.68, 3.41) | 1.37 (0.58, 3.22) | 1.06 (1.02, 1.11) | 28.8% |
| Average weekly working hours, past 6 months | ||||
| ≤40 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | — |
| 41‐59 | 1.34 (1.00, 1.79) | 1.30 (0.97, 1.74) | 1.02 (1.01, 1.04) | 11.8% |
| ≥60 | 1.86 (0.91, 3.83) | 1.78 (0.85, 3.73) | 1.04 (1.01, 1.06) | 9.3% |
| D. Technicians | ||||
| Burnout, work‐related | ||||
| Average weekly working hours, past 1 month | ||||
| ≤40 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | — |
| 41‐59 | 1.33 (0.84, 2.11) | 1.30 (0.82, 2.08) | 1.00 (0.97, 1.04) | 9.1% |
| ≥60 | 3.87 (0.63, 23.69) | 4.72 (0.59, 37.80) | 1.01 (0.92, 1.12) | NA |
| Average weekly working hours, past 6 months | ||||
| ≤40 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | — |
| 41‐59 | 1.34 (0.85, 2.11) | 1.33 (0.84, 2.12) | 1.00 (0.95, 1.06) | 2.9% |
| ≥60 | 3.05 (0.46, 20.40) | 3.85 (0.40, 36.81) | 1.00 (0.88, 1.14) | NA |
| Burnout, personal | ||||
| Average weekly working hours, past 1 month | ||||
| ≤40 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | — |
| 41‐59 | 1.27 (0.74, 2.19) | 1.16 (0.67, 2.01) | 1.04 (0.99, 1.10) | 40.7% |
| ≥60 | 1.91 (0.31, 11.808) | 1.87 (0.24, 14.30) | 1.14 (0.99, 1.31) | 4.4% |
| Average weekly working hours, past 6 months | ||||
| ≤40 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | — |
| 41‐59 | 1.37 (0.80, 2.37) | 1.29 (0.73, 2.29) | 1.06 (0.98, 1.14) | 21.6% |
| ≥60 | 3.05 (0.45, 20.68) | 3.10 (0.37, 25.92) | 1.14 (0.95, 1.36) | NA |
| E. Administrators | ||||
| Burnout, work‐related | ||||
| Average weekly working hours, past 1 month | ||||
| ≤40 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | — |
| 41‐59 | 2.78 (1.68, 4.62) | 2.79 (1.68, 4.65) | 1.00 (0.96, 1.05) | NA |
| ≥60 | 2.78 (0.71, 10.95) | 2.88 (0.70, 11.87) | 1.00 (0.96, 1.04) | NA |
| Average weekly working hours, past 6 months | ||||
| ≤40 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | — |
| 41‐59 | 2.51 (1.52, 4.14) | 2.49 (1.50, 4.14) | 1.01 (0.97, 1.04) | 1.3% |
| ≥60 | 1.45 (0.35, 5.91) | 1.44 (0.35, 5.94) | 1.01 (0.98, 1.04) | 2.2% |
| Burnout, personal | ||||
| Average weekly working hours, past 1 month | ||||
| ≤40 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | — |
| 41‐59 | 2.35 (1.23, 4.52) | 2.39 (1.25, 4.56) | 1.00 (0.94, 1.06) | NA |
| ≥60 | 10.31 (2.52, 42.24) | 11.02 (2.89, 42.0) | 1.00 (0.95, 1.05) | NA |
| Average weekly working hours, past 6 months | ||||
| ≤40 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | — |
| 41‐59 | 2.33 (1.22, 4.45) | 2.31 (1.21, 4.41) | 1.01 (0.96, 1.06) | 1.5% |
| ≥60 | 5.42 (1.37, 21.38) | 5.40 (1.52, 19.19) | 1.01 (0.97, 1.05) | 0.5% |
Estimates adjusted for age, gender, body mass index, seniority (years) in job, cigarettes, alcohol, job type, hypertension, and diabetes mellitus.
3.1. Subgroup analysis
After classifying participants based on job titles and excluding those who did not provide job titles, 2081 participants were included in the subgroup analysis. The majority were nurses (46.8%), and the remaining proportion was broadly balanced between physicians (17.7%), technicians (18.8%), and administrators (16.7%; Figure 2). The mean ages were 31.0 years for nurses, 35.0 years for technicians, 37.3 years for physicians, and 37.4 years for administrators (Table 1). The subgroup of physicians had 70.7% males; the other subgroups had much higher proportions of females than males (nurses: 4.5% male; technicians, 31.7% male; and administrators: 34.2% male). Participants’ average years of experience at their current job were, from low to high, 6.1 years for nurses, 7.0 years for physicians, 7.9 years for technicians, and 8.4 years for administrators.
Average weekly working hours over the past 1 and 6 months were about 20‐22 hours higher among physicians (64.2 and 64.6 hours) compared to the other groups (42.4‐43.7 hours average across groups and time periods). Average daily sleeping hours on workdays were slightly lower among physicians (6.2 hours) compared to the other groups (6.7‐6.8 hours). Nurses had the highest prevalence of both work‐related burnout (50.4%) and personal burnout (30.3%), followed by physicians (37.4% work‐related, 28.2% personal), technicians (32.5% work‐related, 18.4% personal), and administrators (31.0% work‐related, 15.8% personal).
Consistent dose‐response relationships between working hours and OR of burnout were observed among physicians (pink lines in Figure 3), nurses (green lines in Figure 3), and administrators (yellow lines in Figure 3), except for technicians. After confirming that working hours were significantly associated with burnout and for the number of sleeping hours for aforementioned three groups (Appendix Table S4), we also found sleeping hours to be a significant mediator for the relationship between working hours and burnout among physicians and nurses (Table 2). The estimated proportions of the total association of working hours with burnout that could be reduced by resolving insufficient sleeping hours were 25.3% to 73.3% and 7.1% to 28.8% for physicians and nurses respectively.
4. DISCUSSION
Our findings show clear dose‐response relationships between short‐term and long‐term working hours and work‐related burnout among health care workers. Using 40 working hours per week as a reference level, health care workers who worked approximately 60 hours or more per week had a higher OR of work‐related burnout by twofold. The OR increased to three times with average workweeks of 74 hours or more, and increased to four times when working hours exceeded 84 hours per week. Long working hours were also associated with personal burnout, although to a milder degree. Among the above relationships, the increase in sleeping hours explains 7% to 73% of the reduction in working hour‐related burnout in physicians and nurses. Our subgroup analysis indicates that compared with other groups, physicians’ burnout is less susceptible to incremental increases in working hours but more likely to be mediated by sleeping hours.
The nonlinear relationship between working hours and burnout, measured for averages of 40‐120 working hours per week, indicated that ORs of burnout increased faster when working hours were already high, and particularly when the weekly average exceeded 80 hours. Supposing that average weekly working hours could be reduced from 80 to 70 hours among all health care workers, we could expect the OR of burnout to be reduced by about 25% (from OR 3.6–3.7 to OR 2.7‐2.8). A reduction from 80 to 60 hours per week could almost halve the OR, from OR 3.6‐3.7 to OR 2.0‐2.1. Therefore, any level of reduction of average working hours may help protect health care workers from burnout.
Setting up action levels at which to take preventive measures and caps for working hours is important, too. By taking the minimum levels of working hours that showed significant OR (see Figure 3), we can suggest action levels at which to take preventive measures: 46 hours for nurses; 48 hours for administrators; and 86 hours for physicians. Supposing that an OR of 4 (by rounding OR of burnout when average weekly working hours reached 80 hours for all participants) were determined to be an unacceptable level, we can suggest a cap of working hours at 70 hours for nurses; 56 hours for administrators; and 94 hours for physicians.
The rationale for collecting two dimensions of average weekly working hours—the average of the past 1 month and the average of the past 6 months—followed the governmental recognition criteria for overwork‐related diseases established in Taiwan. 36 The national governments have officially included the average number of working hours over the past 6 months as a key factor for developing overwork‐related cardiovascular diseases and listed it as a key criterion in the recognition guidelines for occupational diseases. 36 Our findings show that average working hours over the past 6 months is as important as average hours over the past 1 month in terms of work‐related burnout, which is in alignment with the government recognition guidelines. Preventive actions for burnout should consider the preventing long working hours for a long run.
We also observed differences in the dose‐response relationship based on job title. Per‐unit (ie, per‐hour) increases in working hours are associated with a higher OR of burnout among administrators, followed by nurses and physicians. Physicians’ burnout status is less susceptible to increases or decreases in working hours. Job title can also be a proxy indicator for job demands and controls. High job demands, low job control, and low workplace support have been recognized as important factors associated with burnout. 37 , 38 Although physicians, nurses, and administrators all fall into the area of active jobs, 39 people who are able to spend more time on the activities that are most meaningful to them have reported lower rates of burnout. 40 One survey reported that physicians’ most meaningful work consisted of patient care (68%), followed by research (19%), education (9%), and administration (3%). 40 This could help explain our findings that physicians are less susceptible to burnout at high levels of working hours, if they are doing direct patient care.
We have estimated that the proportion of the effect of working hours on burnout that could be eliminated by intervening on sleeping hours was 25%‐73% in physicians and 7%‐29% in nurses. One previous study of Taiwanese nurses also documented sleeping hours and burnout in a dose‐response manner. 41 Another study from Taiwan indicated that weekend catch‐up sleep was associated with lower burnout status in health care workers who slept less than 7 hours on workdays. 29 One previous study reported that working more than 55 hours a week was associated with sleep disturbance, such as shortened sleeping hours or difficulty falling asleep, compared with working 35‐40 hours a week. 20 Our findings add to existing knowledge by testing the hypothesis that interventions to ameliorate sleeping hours is more apparent in jobs characterized by longer working hours (physicians: 64 hours per week; other groups: <45 hours per week). This may be because extremely long working hours directly reduce the time available for sleep. For those groups working long hours but fewer hours than physicians, sleeping hours accounted for less of the indirect effect on burnout. In these cases, it might be the working hours themselves that contributed to burnout. Longer working hours represent longer exposure time to work‐related factors associated with burnout, such as job stress. Our findings thus suggest the following recommendations for preventing burnout among health care workers: (a) promote sufficient sleep duration for those working longer hours, and (b) reduce working hours as the ultimate solution.
4.1. Limitations
There are several limitations to this study we should address. First, this is a cross‐sectional study, which limits our ability to make causal inferences. There are cumulative risk factors that may cause burnout, and this warrants longitudinal data collection on potential causes and a time‐series analysis. High levels of burnout may also be the risk factors of sleep problem. 23 The bi‐directional effect between sleeping hours and burnout necessities a cohort to examine longitudinal changes. This kind of longitudinal study may also contribute to estimating burnout‐associated costs and turnovers across different job titles as well as bi‐directional effect between sleeping hours and burnout. 23 , 42 , 43 Second, the study setting is a medical center in central Taiwan. This medical center runs multiple departments, such as internal medicine, surgery, children’s hospital, obstetrics and gynecology, Chinese medicine, and international medicine. The number of health care professionals in this medical center accounts for about 8% of the total registered health care professionals of all medical centers in Taiwan. Recruiting participants from a single hospital meant that we could avoid organization‐level variance in burnout or factors associated burnout, 44 but may limit the generalizability of findings to health care workers outside this one health care management system. A third limitation is posed by the several potential factors associated burnout that were not measured by our study. For example, experience of mistreatment (eg, discrimination, harassment, and abuse) is associated with the degree of burnout and has been reported to be two to three times higher among women than men. 45 For the purposes of this study, we assumed that exposure to such factors would be in proportion to hours spent at work, and thus that working hours would act as a variable relevant to these unmeasured variables. A separate analysis incorporating prior known factors related to burnout, such as shift‐work schedules, sleep interruptions, and sleep quality, 46 , 47 may contribute to explore the pathway between working hours, sleeping hours, and burnout.
5. CONCLUSIONS
Our findings showed significant positive associations between working hours and burnout among health care workers and potential interventions to increase sleeping hours could reduce the risk of burnout attributable to working hours. The current shortage of health care professionals, especially frontline health care workers amid the COVID‐19 pandemic, 30 means that reducing working hours might be a challenge in the short‐term. Several intervention strategies, including strengthening the awareness that health care workers need basic healthy lifestyles, have been recommended to support their mental health. 48 Our findings support the suggestion of alternative way to prevent burnout among physicians—promoting sufficient sleep.
DISCLOSURE
Ethical approval: This study was approved by the Big Data Center and the Research Ethical Committee/Institutional Review Board of China Medical University Hospital (CMUH105‐REC3‐068, CMUH108‐REC2‐022). Informed consent: All participants who completed personal health examinations, based on the Regulations of Labor Health Protection of Taiwan, were informed and could decide whether their data to be recorded on the hospital’s Clinical Research Data Repository. Only consented data were analyzed in this study. Registry and the Registration No. of the study/Trial: N/A. Animal Studies: N/A. Conflict of interest: Authors declare no conflict of interest.
AUTHOR CONTRIBUTIONS
R.T.L. contributed to idea formulation, data interpretation, and writing of the manuscript. Y.T.L. contributed to data analysis, reporting results, and data interpretation. Y.F.H. contributed to data collection and data analysis. C.C.K. contributed to data collection and data interpretation. All authors participated in commenting on subsequent drafts, approved the final manuscript, and agreed to submit for publication. R.T.L. and Y.T.L. are the guarantors. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Supporting information
Appendix S1
ACKNOWLEDGMENT
We appreciate the data exploration, statistical analysis, manuscript preparation, and the support of the iHi Clinical Research Platform from the Big Data Center of CMUH. We thank the Health and Welfare Data Science Center (HWDC), Ministry of Health Welfare, and Health Data Science Center, China Medical University Hospital for providing administrative, technical, and funding support. We thank the editors at Tandem Editing LLC for their careful copyediting.
Lin R‐T, Lin Y‐T, Hsia Y‐F, Kuo C‐C. Long working hours and burnout in health care workers: Non‐linear dose‐response relationship and the effect mediated by sleeping hours—A cross‐sectional study. J Occup Health. 2021;63:e12228. 10.1002/1348-9585.12228
Ro‐Ting Lin and Yu‐Ting Lin contributed equally to this work.
Funding information
This research is supported by the Ministry of Science and Technology, Taiwan (grant numbers: MOST 107‐2314‐B‐039‐062‐MY3, MOST 108‐2314‐B‐039‐038‐MY3, and MOST 109‐2321‐B‐468‐001) and the China Medical University, Taiwan (grant numbers: CMU109‐MF‐30 and CMU109‐S‐30). The funders played no role in study design, data collection, data analysis, data interpretation, or reporting.
REFERENCES
- 1. Freudenberger HJ. Staff burn‐out. J Soc Issues. 1974;30:159–165. 10.1111/j.1540-4560.1974.tb00706.x [DOI] [Google Scholar]
- 2. Frajerman A, Morvan Y, Krebs MO, Gorwood P, Chaumette B. Burnout in medical students before residency: a systematic review and meta‐analysis. Eur Psychiat. 2019;55:36–42. 10.1016/j.eurpsy.2018.08.006 [DOI] [PubMed] [Google Scholar]
- 3. Low ZX, Yeo KA, Sharma VK, et al. Prevalence of burnout in medical and surgical residents: a meta‐analysis. Int J Environ Res Public Health. 2019;16(9):22. 1479. doi:10.3390/ijerph16091479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rotenstein LS, Torre M, Ramos MA, et al. Prevalence of burnout among physicians. A systematic review. JAMA 2018;320(11):1131‐1150. doi:10.1001/jama.2018.12777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Aiken LH, Sloane DM, Clarke S, et al. Importance of work environments on hospital outcomes in nine countries. Int J Qual Health C. 2011;23(4):357–364. 10.1093/intqhc/mzr022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Maslach C, Jackson S, Leiter M. Maslach Burnout Inventory Manual, 3rd ed. Consulting Psychologists Press; 1996. [Google Scholar]
- 7. Salvagioni DAJ, Melanda FN, Mesas AE, Gonzalez AD, Gabani FL, de Andrade SM. Physical, psychological and occupational consequences of job burnout: a systematic review of prospective studies. PLoS One. 2017;12(10):29. e0185781. doi:10.1371/journal.pone.0185781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Thomas NK. Resident burnout. JAMA. 2004;292(23):2880–2889. 10.1001/jama.292.23.2880 [DOI] [PubMed] [Google Scholar]
- 9. Salyers MP, Bonfils KA, Luther L, et al. The relationship between professional burnout and quality and safety in healthcare: a meta‐analysis. J Gen Intern Med. 2017;32:475‐482.10.1007/s11606‐016‐3886‐9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Moss M, Good VS, Gozal D, Kleinpell R, Sessler CN. An official critical care societies collaborative statement: burnout syndrome in critical care health care professionals: a call for action. Am J Crit Care. 2016;25(4):368–376. 10.4037/ajcc2016133 [DOI] [PubMed] [Google Scholar]
- 11. West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta‐analysis. Lancet. 2016;388(10057):2272–2281. 10.1016/s0140-6736(16)31279-x [DOI] [PubMed] [Google Scholar]
- 12. Amoafo E, Hanbali N, Patel A, Singh P. What are the significant factors associated with burnout in doctors? Occup Med. 2015;65(2):117–121. 10.1093/occmed/kqu144 [DOI] [PubMed] [Google Scholar]
- 13. Reith TP. Burnout in United States healthcare professionals: a narrative review. Cureus. 2018;10(12):e3681. doi:10.7759/cureus.3681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Accreditation Council for Graduate Medical Education (ACGME) . Common program requirement. Accessed August 8, 2019. https://www.acgme.org/What‐We‐Do/Accreditation/Common‐Program‐Requirements
- 15. Ripp JA, Bellini L, Fallar R, Bazari H, Katz JT, Korenstein D. The impact of duty hours restrictions on job burnout in internal medicine residents: a three‐institution comparison study. Acad Med. 2015;90(4):494‐499. doi:10.1097/acm.0000000000000641 [DOI] [PubMed] [Google Scholar]
- 16. Richter A, Kostova P, Baur X, Wegner R. Less work: more burnout? A comparison of working conditions and the risk of burnout by German physicians before and after the implementation of the EU working time directive. Int Arch Occup Environ Health. 2014;87(2):205–215. 10.1007/s00420-013-0849-x [DOI] [PubMed] [Google Scholar]
- 17. Liu Q, Luo D, Haase JE, et al. The experiences of health‐care providers during the COVID‐19 crisis in China: a qualitative study. Lancet Glob Health. 2020;8(6):e790–e798. 10.1016/S2214-109X(20)30204-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Koh D, Goh HP. Occupational health responses to COVID‐19: what lessons can we learn from SARS? J Occup Health. 2020;62(1):e12128. 10.1002/1348-9585.12128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bannai A, Tamakoshi A. The association between long working hours and health: a systematic review of epidemiological evidence. Scand J Work Environ Health. 2014;40(1):5–18. 10.5271/sjweh.3388 [DOI] [PubMed] [Google Scholar]
- 20. Virtanen M, Ferrie JE, Gimeno D, et al. Long working hours and sleep disturbances: the Whitehall II prospective cohort study. Sleep. 2009;32(6):737–745. 10.1093/sleep/32.6.737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Soderstrom M, Jeding K, Ekstedt M, Perski A, Akerstedt T. Insufficient sleep predicts clinical burnout. J Occup Health Psychol. 2012;17(2):175–183. 10.1037/a0027518 [DOI] [PubMed] [Google Scholar]
- 22. van der Hulst M. Long workhours and health. Scand J Work Environ Health. 2003;29:171–188. [DOI] [PubMed] [Google Scholar]
- 23. Stewart NH, Arora VM. The impact of sleep and circadian disorders on physician burnout. Chest. 2019;156(5):1022–1030. 10.1016/j.chest.2019.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Meerlo P, Sgoifo A, Suchecki D. Restricted and disrupted sleep: effects on autonomic function, neuroendocrine stress systems and stress responsivity. Sleep Med Rev. 2008;12(3):197–210. 10.1016/j.smrv.2007.07.007 [DOI] [PubMed] [Google Scholar]
- 25. Wolkow AP, Barger LK, O'Brien CS, et al. Associations between sleep disturbances, mental health outcomes and burnout in firefighters, and the mediating role of sleep during overnight work: a cross‐sectional study. J Sleep Res. 2019;28(6):15. UNSP e12869. doi:10.1111/jsr.12869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gluschkoff K, Elovainio M, Kinnunen U, et al. Work stress, poor recovery and burnout in teachers. Occup Med. 2016;66(7):564–570. 10.1093/occmed/kqw086 [DOI] [PubMed] [Google Scholar]
- 27. Mendelsohn D, Despot I, Gooderham PA, Singhal A, Redekop GJ, Toyota BD. Impact of work hours and sleep on well‐being and burnout for physicians‐in‐training: the Resident Activity Tracker Evaluation Study. Med Educ. 2019;53(3):306‐315. doi:10.1111/medu.13757 [DOI] [PubMed] [Google Scholar]
- 28. Lin YL, Chen CH, Chu WM, et al. Modifiable risk factors related to burnout levels in the medical workplace in Taiwan: cross‐sectional study. BMJ Open. 2019;9(11):e032779. doi:10.1136/bmjopen‐2019‐032779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Chou LP, Li CY, Hu SC Job stress and burnout in hospital employees: comparisons of different medical professions in a regional hospital in Taiwan. BMJ Open. 2014;4(2):e004185. doi:10.1136/bmjopen‐2013‐004185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Tan BYQ, Kanneganti A, Lim LJH, et al. Burnout and associated factors among health care workers in Singapore during the COVID‐19 pandemic. J Am Med Dir Assoc. 2020;21(12):1751–1758. 10.1016/j.jamda.2020.09.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kristensen TS, Borritz M, Villadsen E, Christensen KB. The Copenhagen Burnout Inventory: a new tool for the assessment of burnout. Work & Stress. 2005;19(3):192–207. 10.1080/02678370500297720 [DOI] [Google Scholar]
- 32. Yeh WY, Cheng Y, Chen CJ, Hu PY, Kristensen TS. Psychometric properties of the Chinese version of Copenhagen burnout inventory among employees in two companies in Taiwan. Int J Behav Med. 2007;14(3):126–133. 10.1007/bf03000183 [DOI] [PubMed] [Google Scholar]
- 33. Occupational Safety and Health Administration, Ministry of Labor, Taiwan . Announcement of the amended "Preventive Guidelines for Diseases Aggravated by Abnormal Workload", 2nd ed. Accessed Jan 27, 2021. https://www.osha.gov.tw/1106/1113/1115/24989 [Google Scholar]
- 34. Lange T, Vansteelandt S, Bekaert M. A simple unified approach for estimating natural direct and indirect effects. Am J Epidemiol. 2012;176(3):190–195. 10.1093/aje/kwr525 [DOI] [PubMed] [Google Scholar]
- 35. Vander Weele TJ. Policy‐relevant proportions for direct effects. Epidemiology. 2013;24(1):175–176. 10.1097/EDE.0b013e3182781410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Chang HH, Lin RT. Policy changes for preventing and recognizing overwork‐related cardiovascular diseases in Taiwan: an overview. J Occup Health. 2019;61(4):278–287. 10.1002/1348-9585.12046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Aronsson G, Theorell T, Grape T et al. A systematic review including meta‐analysis of work environment and burnout symptoms. BMC Public Health. 2017;17:13. 264. doi:10.1186/s12889‐017‐4153‐7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Cheng Y, Chen IS, Chen CJ, Burr H, Hasselhorn HM. The influence of age on the distribution of self‐rated health, burnout and their associations with psychosocial work conditions. J Psychosom Res. 2013;74(3):213–220. 10.1016/j.jpsychores.2012.12.017 [DOI] [PubMed] [Google Scholar]
- 39. Karasek R, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. The Job Content Questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol. 1998;3(4):322–355. 10.1037//1076-8998.3.4.322 [DOI] [PubMed] [Google Scholar]
- 40. Shanafelt TD, West CP, Sloan JA et al. Career fit and burnout among academic faculty. Arch Intern Med. 2009;169(10):990‐995. doi:10.1001/archinternmed.2009.70 [DOI] [PubMed] [Google Scholar]
- 41. Chin W, Guo YL, Hung YJ, Yang CY, Shiao JS. Short sleep duration is dose‐dependently related to job strain and burnout in nurses: a cross sectional survey. Int J Nurs Stud. 2015;52(1):297–306. 10.1016/j.ijnurstu.2014.09.003 [DOI] [PubMed] [Google Scholar]
- 42. Willard‐Grace R, Knox M, Huang B, Hammer H, Kivlahan C, Grumbach K. Burnout and health care workforce turnover. Ann Fam Med. 2019;17(1):36–41. 10.1370/afm.2338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Han S, Shanafelt TD, Sinsky CA, et al. Estimating the attributable cost of physician burnout in the United States. Ann Intern Med. 2019;170(11):784–790. 10.7326/m18-1422 [DOI] [PubMed] [Google Scholar]
- 44. Montgomery A, Panagopoulou E, Esmail A, Richards T, Maslach C. Burnout in healthcare: the case for organisational change. BMJ. 2019;366:l4774. 10.1136/bmj.l4774 [DOI] [PubMed] [Google Scholar]
- 45. Hu Y‐Y, Ellis RJ, Hewitt DB, et al. Discrimination, abuse, harassment, and burnout in surgical residency training. N Engl J Med. 2019;381(18):1741–1752. 10.1056/NEJMsa1903759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Kancherla BS, Upender R, Collen JF, et al. Sleep, fatigue and burnout among physicians: an American Academy of Sleep Medicine position statement. J Clin Sleep Med. 2020;16(5):803–805. 10.5664/jcsm.8408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Kancherla BS, Upender R, Collen JF, et al. What is the role of sleep in physician burnout? J Clin Sleep Med. 2020;16(5):807–810. 10.5664/jcsm.8412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Pollock A, Campbell P, Cheyne J et al. Interventions to support the resilience and mental health of frontline health and social care professionals during and after a disease outbreak, epidemic or pandemic: a mixed methods systematic review. Cochrane Database Syst Rev. 2020;11:CD013779. doi:10.1002/14651858.Cd013779 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1


