Abstract
Objective:
To investigate risk factors for childbirth-related post-traumatic stress disorder (CR-PTSD) measured 1-month after first childbirth, and the association between CR-PTSD and maternal-infant bonding.
Methods:
In this prospective cohort study 3006 nulliparous women living in Pennsylvania, USA, were asked about CR-PTSD at 1-month postpartum, and maternal-infant bonding at 1, 6 and 12-months postpartum. Multivariable logistic regression models identified risk factors for CR-PTSD and associations between CR-PTSD and maternal-infant bonding at 1, 6 and 12-months postpartum, controlling for confounding variables - including postpartum depression, stress and social support.
Results:
Nearly half (47.5%) of the women reported that during labor and delivery they were afraid that they or their baby might be hurt or die, and 225 women (7.5%) reported experiencing one or more CR-PTSD symptoms at 1-month postpartum. Depression, stress and low social support during pregnancy were associated with CR-PTSD, as well as labor induction, delivery complications, poor pain control, and unplanned cesarean delivery. Women with CR-PTSD reported a less positive childbirth experience, less shared decision-making, and were more likely to score in the bottom third on maternal-infant bonding at 1-month postpartum (adjusted odds ratio [aOR] 2.5, 95% CI 1.8–3.3, p < .001); at 6-months postpartum (aOR 2.1, 95% CI 1.5–2.8, p < .001); and at 12-months postpartum (aOR 2.2, 95% CI 1.6–3.0, p < .001).
Conclusion:
In this large-scale prospective cohort study we found that CR-PTSD was consistently associated with lower levels of maternal-infant bonding over the course of the first year after first childbirth.
Keywords: Birth experience, childbirth, maternal-infant bonding, post-traumatic stress disorder, primiparous
Introduction
Childbirth can be a frightening and distressing experience for women, even if the end result is a healthy mother and child. There are many events that can occur during the labor and delivery process that can lead women to fear that they or their baby might be hurt or die; such as prolonged and painful labor, fetal distress, dystocia resulting in instrumental delivery or emergency cesarean, or other types of potentially serious complications. After such an experience some women develop symptoms of post-traumatic stress disorder (PTSD), which has been described as childbirth-related PTSD, or CR-PTSD [1, 2, 3, 4]. Several studies have reported higher rates of CR-PTSD among women after first childbirth than after a subsequent delivery [5, 6]. This may be because the complication rate is higher at first childbirth than at subsequent births. A recent study of maternal and neonatal morbidity rates in US hospitals reported a complication rate of 12.9% for women having vaginal delivery, 19.7% for women with cesarean delivery, a neonatal complication rate of 20.2%, and higher rates of both maternal and neonatal complications at first childbirth [7]. In addition, women are at substantially higher risk for unplanned or emergency cesarean delivery at first childbirth than at subsequent births [8, 9], which is a well-established risk factor for CR-PTSD [10]. However, few studies of CR-PTSD have focused specifically on women at first childbirth.
Over the past two decades many studies have been conducted on the topic of CR-PTSD, primarily aimed at identifying the prevalence of CR-PTSD and associated risk factors. Estimated prevalence rates for CR-PTSD in recent reviews range from 3.1% to 16.8% [11, 12, 13]. Commonly reported risk factors for CR-PTSD include history of mental health disorders, depression during pregnancy, fear of childbirth, maternal and neonatal complications during childbirth, poor pain control, and unplanned or emergency cesarean delivery [14, 15, 16, 11, 13, 17, 18]. Labor is generally considered to be more painful at first childbirth than at subsequent deliveries [19, 20] - therefore poor pain control could be a particularly important predictor of CR-PTSD for women experiencing first childbirth than for women at subsequent deliveries.
There is growing recognition of the importance of the way that health care professionals interact with mothers during labor and delivery as a factor in the development of CR-PTSD. In qualitative studies of traumatic delivery women described trying unsuccessfully to obtain information and help from hospital staff [21]; and being misinformed, disrespected and objectified by healthcare personnel [22]. In a review of ten qualitative studies of traumatic birth the authors concluded that “Healthcare professionals must recognize women’s need to be involved in decision-making and to be fully informed about all aspects of their labour and birth” [23]. In a mixed-methods study of women who had experienced a traumatic birth, the majority of the women (66.7%) described their interactions with healthcare personnel as the primary traumatic element in the childbirth [24]. It is likely that most women in the U.S. who are expecting their first child have had little experience with the way that labor and delivery units in many hospitals function. Women may be particularly upset if they find little support or empathy from hospital personnel who may be overwhelmed with many patients to take care of, or otherwise unwilling or unable to take the time to provide supportive care and to discuss treatment options with them if needed.
Key components of PTSD are the arousal of negative emotions when reminded of the traumatic event, continued efforts to avoid thinking about the traumatic event, and the avoidance of stimuli that can remind one of the traumatic event [25]. In the case of CR-PTSD, it has been hypothesized that the newborn can become a reminder of the traumatic event, leading to difficulty for the mother to bond with her newborn [17]. In a qualitative study of women after a traumatic childbirth most of the women reported initial feelings of rejection toward their newborn, which faded over time [26]. However, results from quantitative studies have been mixed. Several quantitative survey studies reported no association between CR-PTSD and parent-child bonding [27, 28], while. others reported an association between CR-PTSD and maternal-infant bonding which became non-significant when they controlled for postpartum depression [29, 30, 31, 32]. A study of Japanese mothers reported an association between PTSD and impaired bonding even after controlling for depression at 1-month postpartum, but reported no association with postpartum bonding measured at 4 months postpartum [33]. A cross-sectional study of women 0–13 months after childbirth reported an inverse association such that higher postpartum PTSD was associated with fewer bonding difficulties [3]. Several studies that did not control for maternal depression reported lower postpartum bonding or maternal-child attachment among women reporting CR-PTSD symptoms [34, 35]. Because CR-PTSD is usually highly comorbid with postpartum depression, and postpartum depression has been found to be an important risk factor for impaired maternal-infant bonding [36], it has been difficult for researchers to separate the effects of CR-PTSD and postpartum depression on maternal-infant bonding. Most of the previous studies of the association between CR-PTSD and maternal-infant bonding have had relatively small sample sizes and may not have had the statistical power to determine the independent effect of CR-PTSD on maternal-infant bonding after controlling for postpartum depression. In addition, few of the previous studies measured maternal-infant bonding more than once postpartum, so it is not clear if the relationship between CR-PTSD and maternal-infant bonding changes over the course of time.
The present study aimed to conduct a secondary analysis of a large-scale prospective cohort study of women at first childbirth in order to address the following research questions: 1.) How often during first labor and delivery in the U.S. are women afraid that they or their baby might be hurt or die (thus meeting the A1 criterion for PTSD)? 2.) How often do women develop one or more symptoms of CR-PTSD after first childbirth? 3.) What prenatal and intrapartum factors are associated with the development of CR-PTSD symptoms at first childbirth? 4.) To what extent is CR-PTSD symptomatology associated with maternal-infant bonding after first childbirth while controlling for postpartum depression and other psychosocial factors? and 5.) To what extent is CR-PTSD symptomatology consistently associated with maternal-infant bonding over the course of the first year postpartum?
Method
The First Baby Study (FBS) was a prospective cohort study designed to investigate the association between mode of first childbirth and subsequent childbearing [37, 38]. Inclusion criteria included age 18 to 35 years old at study recruitment, with a singleton pregnancy, English or Spanish speaking, living in Pennsylvania USA, and planning to deliver in a hospital in Pennsylvania. Exclusion criteria included a prior pregnancy of 20 weeks gestation or longer, planning to delivery at home or in a birthing center not associated with a hospital, planning to have a tubal ligation at the time of delivery, planning to have the child adopted, and delivering before 34 weeks gestation. Women who were interviewed during pregnancy but later had a stillbirth, neonatal death or hysterectomy at the time of delivery were not included in the study. Women were recruited from childbirth education classes, hospital tours, low-income clinics, private clinician’s offices, ultrasound centers, hospital intra-net postings, newspaper advertisements and targeted mailings. The study participants were interviewed during their third trimester at 30 weeks gestation or later, and at 1, 6, 12, 18, 24, 30 and 36 months postpartum. There were 3006 women who completed both the baseline and 1-month postpartum interviews. The hospital discharge data and birth certificate data for each delivery were obtained as well. The participants delivered at 78 hospitals in the years 2009 to 2011. The women in the FBS were more likely to be white, college educated and married than women delivering their first child in Pennsylvania as a whole, as we have reported previously [37, 38]. The FBS was approved by the institutional review board (IRB), Penn State University College of Medicine, as well as the IRBs of institutions and organizations involved with participant recruitment.
The participants were interviewed by telephone by trained professional interviewers employed by the Center for Survey Research at Penn State University. As part of the baseline interview conducted in the third trimester before first childbirth participants were asked about their education level, race/ethnicity, current relationship status, whether their pregnancy was intended, history of prior pregnancies, a previous diagnosis of anxiety or depression, plans to breastfeed, fear of childbirth and financial struggles, and the psychosocial measures of depression, social support and stress. Descriptions of these measures and their psychometric properties can be seen in Appendix A.
Data were collected from the hospital discharge and birth certificate data, and the 1-month postpartum interviews to measure labor induction, duration of labor, mode of delivery, Apgar scores, maternal and neonatal complications, and length of hospital stay for the mother and newborn. The participants were also asked about depression, social support, stress, birth experience and maternal-infant bonding in the 1-month postpartum interview. Descriptions of these measures and psychometric properties can be seen in Appendix A. Maternal-infant bonding was measured using a modified and shortened version of the Postpartum Bonding Questionnaire (PBQ) [39], consisting of ten questions. These ten questions and their psychometric properties can be seen in Appendix B. These same questions were asked of the study participants at the 6 and 12-month postpartum interviews as well. We scored this scale such that the higher the score the more positive the maternal-infant bonding.
We measured CR-PTSD at 1-month postpartum using an adapted version of the Trauma Screening Questionnaire (TSQ) [40], which comprised 11 items. We chose this instrument because it is brief, well-validated, and the items are simple and easy to understand. Women were asked to report if they had experienced specific posttraumatic symptoms at least twice in the week prior to the interview, as is done in the TSQ. Six of these symptoms measured Criterion B, persistent re-experiencing of the traumatic event and Criterion D, increased arousal. We also added the item “Trying not to think about the childbirth experience”, as a measure of avoidance (Criterion C). Because the TSQ was designed to measure PTSD symptoms after any type of traumatic event, we adapted the TSQ items to refer to childbirth specifically and developed questions to measure the Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition), (DSM-IV) A1 and A2 criteria [25] in reference to a potentially traumatic event associated with childbirth. DSM-IV was the latest version at the time that we began this study. The A1 criterion specifies that “the person experienced, witnessed, or was confronted with an event or events that involved actual or threatened death or serious injury, or threat to the physical integrity of the self or others” and the A2 criterion specifies that “The person’s response involved intense fear, helplessness or horror” [25]. We conducted focus groups among postpartum women to understand their experiences of childbirth, and pilot studies to evaluate the clarity of the items that we developed for our measure of CR-PTSD and the other study instruments. The items that we developed and/or adapted for our measure of CR-PTSD reflected the experiences that women reported in the focus groups, and the pilot study participants reported that they had no difficulty understanding or answering the questions in this scale. As shown in Figure 1, women who reported that they or their baby might be hurt or die during labor and delivery were then asked about their emotional reaction. Women who reported feeling helpless, terrified or horrified were then asked if they had experienced each of the CR-PTSD symptoms at least twice in the previous week. The 11 items which we used to measure CR-PTSD can be seen in Table 1. The Cronbach’s alpha for these items as a summated scale was 0.82.
Fig. 1.
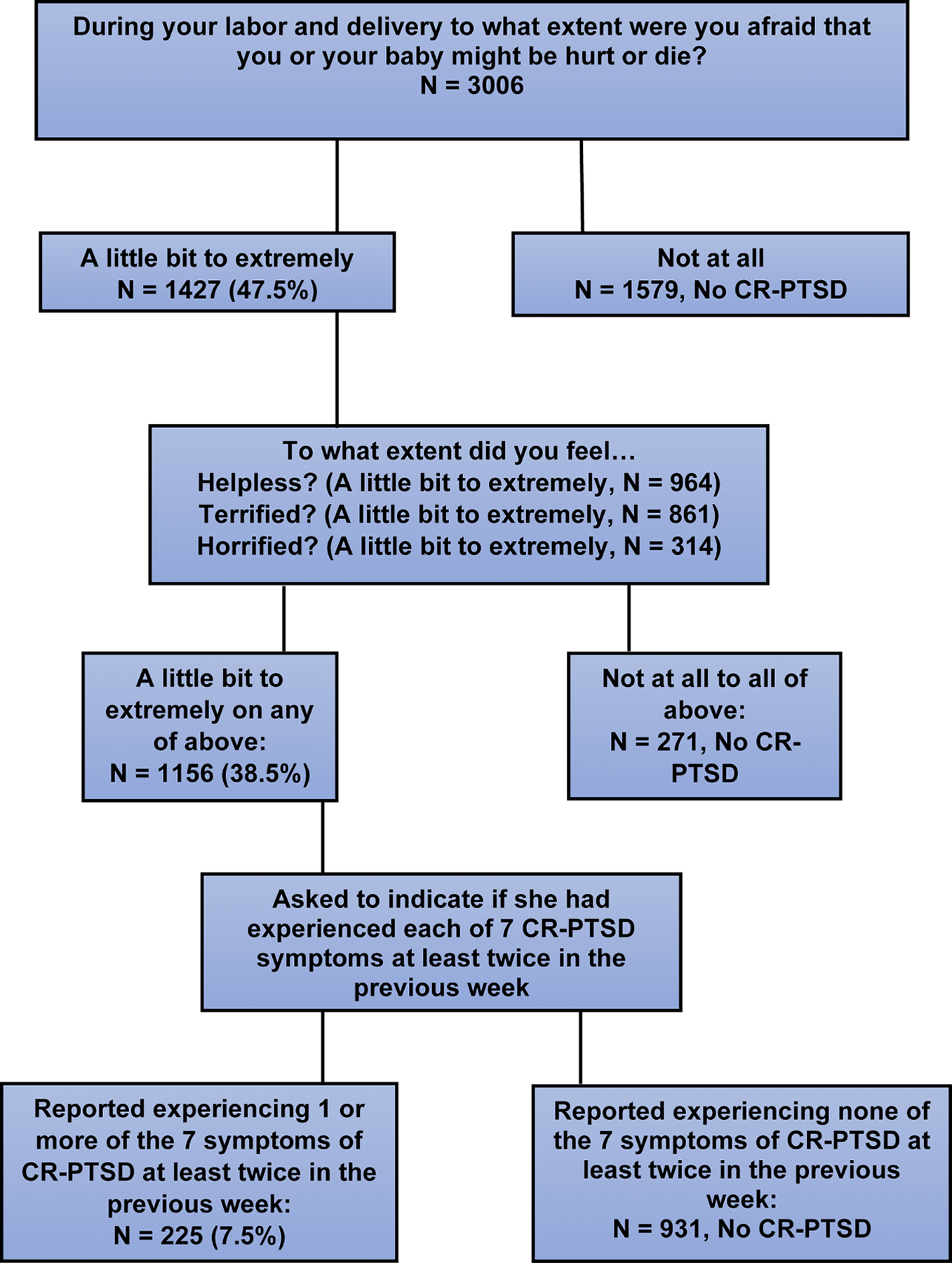
Flow diagram showing process to identify women with CR-PTSD.
Table 1.
Distribution of answers to the questions measuring CR-PTSD, asked at 1-month postpartum (n = 3006).
| n (%) | |
|---|---|
| “During your labor and delivery to what extent were you afraid that you or your baby might be hurt or die?” | |
| Extremely | 97 (3.2) |
| Quite a bit | 139 (4.6) |
| Moderately | 358 (11.9) |
| A little bit | 833 (27.7) |
| Not at all | 1579 (52.5) |
| Women who answered extremely to a little bit to above questions were then asked the following questions: | 1427 (47.5) |
| “To what extent did you feel helpless?” | |
| Extremely | 110 (7.7) |
| Quite a bit | 142 (10.0) |
| Moderately | 269 (18.9) |
| A little bit | 443 (31.0) |
| Not at all | 463 (32.4) |
| “To what extent did you feel terrified?” | |
| Extremely | 120 (8.4) |
| Quite a bit | 99 (6.9) |
| Moderately | 201 (14.1) |
| A little bit | 441 (14.1) |
| Not at all | 566 (39.7) |
| “To what extent did you feel horrified?” | |
| Extremely | 52 (3.6) |
| Quite a bit | 45 (3.2) |
| Moderately | 73 (5.1) |
| A little bit | 144 (10.1) |
| Not at all | 1113 (78.0) |
| Women who answered extremely to a little bit to one or more of above three questions were then asked the following: | 1156 (38.5) |
| “Since the delivery have you experienced any of the following at least twice in the past week?” | |
| “Upsetting thoughts or memories about the childbirth experience that have come into your mind against your will?” | 83 (7.2) |
| “Upsetting dreams about the childbirth experience?” | 14 (1.2) |
| “Acting or feelings as though the childbirth experience were happening again?” | 20 (1.7) |
| “Feeling upset by reminders of the childbirth experience?” | 84 (7.3) |
| “Bodily reactions (such as fast heartbeat, stomach churning, sweatiness, dizziness, etc.) when reminded of the childbirth experience?” | 17 (1.5) |
| “Trying not to think about the childbirth experience?” | 108 (9.3) |
| “Being jumpy or being startled at something unexpected?” | 70 (6.1) |
| Women who reported one or more CR-PTSD symptoms at 1-month | 225 (7.5) |
Statistical analyses were performed using SPSS version 26 statistical program (Chicago, USA). Descriptive statistics were calculated for the independent, dependent and covariate factors. Chi-square analyses were conducted to measure the associations between the independent variables (the vulnerability-related and trauma-related factors) and the presence of one or more CR-PTSD symptoms reported 1-month postpartum. The vulnerability-related and trauma-related variables that were significantly associated with the presence of one or more PTSD symptoms in the bivariate analyses (chi-square and t-test) were included in the initial multivariable logistic regression model. We included the measures of depression, social support and stress from the baseline interview as predictors in this model but we did not include the postpartum measures of depression, social support and stress because they were collinear with the baseline measures. The final more parsimonious model was created by backwards elimination, sequentially removing variables that were not significant one at a time, in order of non-significance, until the model included only variables that were independently associated with the presence of one or more CR-PTSD symptoms at 1-month postpartum.
Three additional multivariable logistic regression models were developed to assess the association between CR-PTSD symptoms reported at 1-month postpartum and maternal-infant bonding at 1, 6, and 12-months postpartum, controlling for maternal age, race, education, marital status, pregnancy intendedness, trouble paying for basic needs, and the 1-month postpartum measures of depression, social support and stress. Because the maternal-infant bonding scores were highly skewed and kurtotic we dichotomized the scores and compared women who scored in the bottom third of the distribution of total scores to those scoring in the top two thirds. Lower scores on the bonding scale indicated less positive maternal-infant bonding.
Results
Nearly half (47.5%) of the 3006 study participants reported that during labor and delivery they were at least a little bit afraid that they or their baby might be hurt or die (Figure 1), among whom 81.0% reported feeling at least a little bit helpless, terrified or horrified. Nearly half of the women reported feeling at least a little bit afraid that they or their baby might be hurt or die during labor and/or delivery, as can be seen in Table 1. Among the 1427 women who were asked the questions addressing the A2 criterion, 8.4% reported feeling extremely terrified. Among the 1156 women who were asked about CR-PTSD symptoms, the most commonly reported symptom was “Trying not to think about the childbirth experience” (9.3%). There were 225 women (7.5% of the total) who reported experiencing one or more CR-PTSD symptoms.
The participants were predominantly non-Hispanic white (83.2%), more than half had college degrees or higher levels of education (56.6%), the majority were married (70.4%) and reported no trouble paying for basic needs (79.2%), as can be seen in Table 2. The vulnerability-related variables that were most strongly associated with the presence of one or more CR-PTSD symptoms at 1-month postpartum in the chi-square analyses were the baseline measures of depression, social support and stress. Among the trauma-related factors that we investigated (Table 3), those that were most strongly related to the presence of CR-PTSD symptoms at 1-month postpartum in the chi-square analyses were maternal-reported complications, unplanned cesarean delivery, and hospital length of stay of four days or more for the mother and the newborn.
Table 2.
Overall characteristics of study participants on the vulnerability-related factors measured during pregnancy, and the bivariate associations between these factors and the presence of one or more CR-PTSD symptoms reported at 1-month postpartum
| Characteristics | Overall N (%) | One or more CR-PTSD symptoms, n (%) |
|---|---|---|
| Overall | 3006 (100) | 225 (7.5) |
| Maternal Age | ||
| 18–24 | 811 (27.0) | 70 (8.6) |
| 25–29 | 1193 (39.7) | 88 (7.4) |
| 30–35 | 1002 (33.3) | 67 (6.7) |
| Education | ||
| HS degree or less | 501 (17.7) | 38 (7.6) |
| Some college or technical school | 804 (26.7) | 66 (8.2) |
| College degree or higher | 1701 (56.6) | 121 (7.1) |
| Race/Ethnicity | ||
| White non-Hispanic | 2502 (83.2) | 177 (7.1) |
| Black non-Hispanic | 221 (7.4) | 24 (10.9) |
| Hispanic | 166 (5.5) | 11 (6.6) |
| Other | 116 (3.9) | 13 (11.2) |
| Insurance coverage | ||
| Private | 2312 (76.9) | 156 (6.7)** |
| Public | 694 (23.1) | 69 (10.0) |
| Marital status | ||
| Married | 2117 (70.4) | 138 (6.5)* |
| Living with partner | 544 (18.1) | 55 (10.1) |
| Partner, not living with | 187 (6.2) | 15 (8.0) |
| No partner | 158 (5.3) | 17 (10.8) |
| Pregnancy intendedness | ||
| Yes | 2022 (67.9) | 136 (6.7)* |
| No | 954 (31.7) | 89 (9.3) |
| Trouble paying for basic needs | ||
| Some or a lot of trouble | 624 (20.8) | 72 (11.6)*** |
| No trouble | 2382 (79.2) | 153 (6.4) |
| History of diagnosed anxiety or depression | ||
| Yes | 688 (22.9) | 74 (10.8)*** |
| No | 2318 (77.1) | 151 (6.5) |
| Previous pregnancy loss | ||
| Yes | 478 (15.9) | 40 (8.4) |
| No | 2528 (84.1) | 185 (7.3) |
| Plan to breastfeed | ||
| Yes | 2772 (92.2) | 210 (7.6) |
| No or don’t know | 234 (7.8) | 15 (6.4) |
| Fear of childbirth in pregnancy | ||
| Low (4–8) | 1025 (34.1) | 52 (5.1)*** |
| Medium (9–12) | 1235 (41.1) | 89 (7.2) |
| High (13–20) | 746 (24.8) | 84 (11.3) |
| Edinburgh depression in pregnancy | ||
| 0–12 | 2816 (93.9) | 187 (6.6)*** |
| 13+ (probable depression) | 182 (6.1) | 37 (20.3) |
| Social support in pregnancy | ||
| Low (5–19) | 510 (17.0) | 63 (12.4)*** |
| Medium (20–23) | 1232 (41.0) | 103 (8.4) |
| High (24–25) | 1261 (42.0) | 58 (4.6) |
| Stress in pregnancy | ||
| Low (12–16) | 1066 (35.5) | 36 (3.4)*** |
| Medium (17–20) | 1123 (37.4) | 95 (8.5) |
| High (21+) | 811 (27.0) | 93 (11.5) |
| High-risk pregnancy | ||
| Yes | 1346 (44.8) | 125 (9.3)*** |
| No | 1660 (55.2) | 100 (6.0) |
significance levels:
p ≤ 0.05
p ≤ 0.01
p ≤ 0.001.
Table 3.
Overall characteristics of study participants on the trauma-related factors and covariates, and the bivariate associations between these factors and the presence of one or more CR-PTSD symptoms reported at 1-month postpartum
| Characteristics | Overall n (%) | One or more CR-PTSD symptoms, n (%) |
|---|---|---|
| Overall | 3006 (100) | 225 (7.5) |
| Labor induced | ||
| Yes | 1017 (33.8) | 105 (10.3)*** |
| No | 1989 (66.2) | 120 (6.0) |
| Long labor duration (19+ hours) | ||
| Yes | 667 (22.2) | 71 (10.6)*** |
| No | 2339 (77.8) | 154 (6.6) |
| Poor pain control during labor and or delivery | ||
| Yes | 1211 (40.3) | 123 (10.2)*** |
| No | 1795 (59.7) | 102 (5.7) |
| Maternal-reported complications from delivery | ||
| Yes | 430 (14.3) | 68 (15.8)*** |
| No | 2575 (85.7) | 157 (6.1) |
| Maternal-reported Infant complications from delivery | ||
| Yes | 435 (14.5) | 56 (12.9)*** |
| No | 2571 (85.5) | 169 (6.6) |
| Maternal morbidities based on ICD-9 codes | ||
| Yes | 818 (27.2) | 77 (9.4)* |
| No | 2188 (72.8) | 148 (6.8) |
| Neonatal morbidities based on ICD-9 codes | ||
| Yes | 397 (13.2) | 47 (11.8)*** |
| No | 2609 (86.8) | 178 (6.8) |
| Mode of delivery | ||
| Spontaneous vaginal | 1876 (62.4) | 89 (4.7)*** |
| Instrumental vaginal | 267 (8.9) | 27 (10.1) |
| Planned cesarean | 160 (5.3) | 9 (5.6) |
| Unplanned cesarean | 703 (23.4) | 100 (14.2) |
| Gestational age (weeks, days) | ||
| Late preterm (34,2 −36,6) | 120 (4.0) | 8 (6.7)* |
| Early term (37,0 – 38,6) | 575 (19.1) | 43 (7.5) |
| Full term (39,0 – 40,6) | 1814 (60.3) | 121 (6.7) |
| Late term (41,0 – 41,6) | 463 (15.4) | 48 (10.4) |
| Post term (42,0 – 43,2) | 34 (1.1) | 5 (14.7) |
| Birthweight | ||
| Low (< 2500 grams) | 93 (3.1) | 11 (11.8) |
| Normal (2500–4000 grams) | 2573 (86.3) | 193 (7.5) |
| High (> 4000 grams) | 316 (10.6) | 19 (6.0) |
| Five-minute Apgar score | ||
| 1–7 | 141 (4.7) | 20 (14.2)** |
| 8–10 | 2840 (95.3) | 202 (7.1) |
| Maternal postpartum hemorrhage | ||
| Yes | 122 (4.1) | 9 (7.4) |
| No | 2884 (95.9) | 216 (7.5) |
| Maternal hospital length of stay (days) | ||
| 0–3 | 2328 (77.4) | 140 (6.0)*** |
| 4+ | 678 (22.6) | 85 (12.5) |
| Infant hospital length of stay (days) | ||
| 0–3 | 2651 (88.2) | 175 (6.6)*** |
| 4+ | 355 (11.8) | 50 (14.1) |
| Shared decision-making during delivery | ||
| Low (0–3) | 244 (8.1) | 59 (24.2)*** |
| Moderate (4–5) | 896 (29.8) | 90 (10.0) |
| High (6) | 1866 (62.1) | 76 (4.1) |
| Childbirth experience (Mean ± SD) | 68.64 ± 6.41 | 61.28 ± 8.70*** |
| Covariates | ||
| Edinburgh depression 1-month | ||
| 0–12 | 2891 (96.3) | 200 (6.9)*** |
| 13+ (probable depression) | 111 (3.7) | 25 (22.5) |
| Social support 1-month | ||
| Low (9–36) | 929 (30.9) | 102 (11.0)*** |
| Medium (37–41) | 906 (30.1) | 78 (8.6) |
| High (42–45) | 1170 (38.9) | 45 (3.8) |
| Stress 1-month | ||
| Low (12–13) | 2116 (70.4) | 107 (5.1)*** |
| Medium (14–15) | 667 (22.2) | 83 (12.4) |
| High (16+) | 222 (7.4) | 35 (15.8) |
| Breastfeeding at 1-month | ||
| Yes | 2094 (69.7) | 149 (7.1) |
| No | 912 (30.3) | 76 (8.3) |
and t-test significance levels:
p ≤ 0.05
p ≤ 0.01
p ≤ 0.001.
In the multivariable logistic regression model to investigate the associations between the vulnerability-related and trauma-related factors and the presence of CR-PTSD, scores on the FBS Birth Experience Scale (Table 4) were strongly associated with CR-PTSD such that women who reported CR-PTSD symptoms were less positive about their childbirth experience than women who did not experience CR-PTSD. Shared decision-making was also strongly associated with CR-PTSD, such that women who reported experiencing CR-PTSD reported lower levels of shared decision-making than women who did not experience CR-PTSD. Fear of childbirth was not significantly associated with CR-PTSD in the regression model most likely because it was moderately associated with childbirth experience (Pearson r = −.245), and childbirth experience was more strongly associated with CR-PTSD. Therefore, when childbirth experience was entered into the regression model fear of childbirth became non-significant.
Table 4.
Adjusted odds ratios (aORs) and 95% confidence intervals (CIs) derived from a multivariable logistic regression model measuring associations between vulnerability-related and trauma-related factors and the presence of one or more CR-PTSD symptoms reported at 1-month postpartum (n = 3006)
| Characteristics | Wald | One or more PTS Symptoms aOR (95% CI)a |
|---|---|---|
| Edinburgh depression in pregnancy of 13+ | 8.99 | 2.08 (1.29–3.36)** |
| Stress in pregnancy | ||
| Low (12–16) (reference category) | ||
| Medium (17–20) | 10.61 | 2.04 (1.33–3.14)*** |
| High (21+) | 8.24 | 1.94 (1.23–3.06) |
| High social support in pregnancy | 5.81 | 0.65 (0.46–0.92)* |
| Labor induction | 3.99 | 1.39 (1.01–1.92)* |
| Poor pain control | 13.33 | 1.80 (1.31–2.47)*** |
| Mode of delivery | ||
| Spontaneous vaginal | 10.76 | 0.55 (0.39–0.79)*** |
| Instrumental vaginal | 0.96 | 0.77 (0.45–1.31) |
| Planned cesarean | 3.84 | 0.44 (0.19–1.00)* |
| Unplanned cesarean (reference category) | ||
| Maternal-reported complications from delivery | 7.70 | 1.67 (1.16–2.39)** |
| Shared decision-making | ||
| Low (0–3) (reference category) | ||
| Medium (4–5) | 1.81 | 0.74 (0.49–1.15) |
| High (6) | 23.87 | 0.33 (0.21–0.52)*** |
| Childbirth experience score | 107.86 | 0.89 (0.88–0.91)*** |
Significance levels:
p ≤ 0.05
p ≤ 0.01
P ≤ 0.001.
Backwards elimination removing non-significant predictors to include only variables independently associated with presence of one or more PTS symptoms.
Women who reported one or more CR-PTSD symptoms were generally about twice as likely to score in the bottom third on the postpartum bonding measure, in comparison to women who did not report CR-PTSD symptoms, even after controlling for maternal age, education, race, marital status, pregnancy intendedness, trouble paying for basic needs, and postpartum depression, stress and social support, as seen in Table 5. The aORs and 95% CI’s to measure the associations between CR-PTSD and maternal-infant bonding across these three time points (1, 6, and 12-months postpartum) were quite similar, indicating a persistent and stable association between CR-PTSD and maternal-infant bonding over the course of the first 12-months after first childbirth.
Table 5.
CR-PTSD symptoms reported at 1-month postpartum in relation to postpartum bonding scores in the bottom third at 1, 6, and 12-months postpartum, multivariable logistic regression models (1-month n = 3005; 6-months n = 2909; 12-months n = 2802)
| Maternal-infant bonding score in bottom third | ||||||
|---|---|---|---|---|---|---|
| 1-month | 6-months | 12-months | ||||
| CR-PTSD symptoms | n (%) | aOR (95% CI)* | n (%) | aOR (95% CI)* | n (%) | aOR (95% CI)* |
| Yes | 135 (60.0) | 2.5 (1.8–3.3)*** | 116 (54.0) | 2.1 (1.5–2.8)*** | 121 (59.0) | 2.2 (1.6–3.0)*** |
| No | 891 (32.1) | Ref | 798 (29.6) | Ref | 866 (33.3) | Ref |
All models controlled for maternal age, education, race, marital status, the intendedness of the pregnancy, trouble paying for basic needs, and the 1-month postpartum measures of depression, stress and social support.
p < 0.001.
Discussion
In this study of first-childbirth related PTSD symptomatology, nearly half of the participants (47.5%) reported feeling at least a little bit afraid that they or their baby might be hurt or die during labor or delivery, and 7.8% reported feeling extremely or quite a bit afraid. Overall, 7.5% of the participants reported experiencing CR-PTSD symptoms. Women with pre-existing vulnerabilities were more likely to report experiencing CR-PTSD symptoms, specifically depression, low social support and high stress during the third trimester before first childbirth. These results are similar to those reported in previous studies [14, 17, 13, 18, 41]. However, contrary to some previous studies [15, 17, 18, 42], fear of childbirth was not associated with CR-PTSD in the multivariable regression model, nor were premature delivery, low birth weight or postpartum hemorrhage. The variables of premature delivery, low birth weight and postpartum hemorrhage were likely non-significant in our model because we had relatively small percentages of women with these conditions in our study. The trauma-related factors associated with CR-PTSD in the multivariable model were labor induction, poor pain control, and having an unplanned cesarean or an instrumental vaginal delivery. Women who had spontaneous vaginal delivery or planned cesarean were the least likely to report CR-PTSD symptoms.
Women with CR-PTSD at 1-month postpartum reported a less positive childbirth experience than women who did not have CR-PTSD symptoms, and less shared decision-making. In addition, these women were more likely to score in the probable depression range on the EDS at 1-month postpartum and to report low social support and high stress at that time. The most commonly reported CR-PTSD symptom was “Trying not to think about the childbirth experience”. Taken together, these results indicate that first childbirth was, for these women, a disturbing, troubling and traumatic experience. The low degree of delivery-related shared decision-making that these women reported indicates that these women felt that their voices were not heard and they were not treated with respect during childbirth. Similar results have been reported in studies of intrapartum factors associated with the development of CR-PTSD [14, 16, 11, 17, 24].
The women in this study who reported CR-PTSD symptoms were considerably less positive about their childbirth experience than the women who did not report CR-PTSD symptoms. These results are in accord with a recent systematic review of CR-PTSD prevalence and risk factors which concluded that “Negative subjective experience of childbirth emerged as the most important predictor.” [13]. Measures of childbirth experience usually ask women to report how they felt right after they had their baby, as we did in our study. The importance of childbirth experience as a predictor of CR-PTSD suggests that the first few moments after childbirth are critical to helping women process the events that occurred in a positive and healthy way. While little research has been conducted to measure how a new mother is treated in the first few moments after childbirth, if she is ignored, or worse – demeaned, she may process the childbirth as a frightening and traumatizing event. On the other hand, if the delivery team provides supportive, respectful and caring attention to new mothers in the first few moments after childbirth, this may help women to view their experience positively and to process it in a healthy way, even if there were frightening and potentially dangerous moments during labor and delivery.
The women in our study who were experiencing CR-PTSD symptoms at 1-month postpartum scored significantly lower on postpartum bonding measured at 1, 6 and 12 months postpartum than the women who did not report CR-PTSD symptoms, even after controlling for relevant confounding variables – including postpartum depression, stress and social support. These results suggest that a traumatic childbirth resulting in CR-PTSD symptoms experienced at 1-month postpartum can have a harmful and potentially enduring effect on new mother’s ability to bond with their newborns. While obstetricians are generally aware of the potential for their patients to experience postpartum depression, there is a lack of awareness about risk for postpartum PTSD [43]. A recent call-to-action commentary published in the journal Obstetrics & Gynecology suggested that obstetricians screen for postpartum PTSD, using the 5-item Primary Care Screen for DSM-5 (PC-PTSD-5) [44], and refer women who screen positive to a mental health professional if possible [43]. However, the PC-PTSD-5 was validated in military veterans, is not specific to childbirth, and has not been used or evaluated among postpartum women. Further research is needed to determine how best to screen and treat women for childbirth-related PTSD. In addition, as previously suggested [45], it is critically important that further research address how to prevent traumatic childbirth in the first place, including studies designed to evaluate the effectiveness of programs to foster caring and respectful treatment of women and their families throughout pregnancy, childbirth and postpartum.
Strengths and limitations
Strengths of this study are that it was a large-scale prospective study with the assessment of important psychosocial predictors of CR-PTSD during and after pregnancy, and the assessment of maternal-infant bonding three times over the course of the first year after first childbirth. However, there are several limitations to consider, as follows: 1.) We did not use a survey instrument that was specifically designed to measure childbirth-related PTSD, but instead adapted an instrument designed to measure general PTSD, which we modified to be specific to childbirth. We chose this route because we had many other outcomes to assess in this study and needed a PTSD measure that was both brief and well-validated. The other publicly available measures of CR-PTSD that we found when we developed our study instruments were considerably longer than the TSQ. However, our 11-item measure of CR-PTSD worked well in this study. The internal consistency reliability of 0.82 was acceptable, and the instrument was associated with vulnerability and trauma related factors as one would expect, as well as the concurrent measures of postpartum depression, social support and stress. In addition, this instrument was a strong and independent predictor of postpartum bonding at 1, 6 and 12 months postpartum. These associations provide evidence of the validity of this 11-item measure of CR-PTSD in our population of U.S. women. 2.) We did not measure CR-PTSD by clinical interview, as some studies have. This would have been prohibitively expensive, given our large sample size. 3.) Several previous studies have noted the importance of prenatal PTSD from exposure to previous trauma as a predictor of CR-PTSD [46, 1], which we did not measure in this study. The primary focus of the First Baby Study was on the health and fertility effects of cesarean delivery [38], with limited interview time to assess such factors as history of previous PTSD. 4.) We measured CR-PTSD following the DSM-IV PTSD criteria, which was the latest DSM version at the time that we began this study. However, new PTSD criteria have been introduced in DSM-5. The DSM-5 PTSD criteria no longer includes the emotional reactions of feeling helpless, terrified or horrified [47]. Had we followed the DSM-5 PTSD criteria we would have asked more women if they were experiencing CR-PTSD symptoms and potentially identified more women experiencing CR-PTSD. 5.) We did not measure CR-PTSD in the fathers/partners. Fathers/partners often play an important role in the labor and delivery process, and may be equally affected by a traumatic delivery [27, 48]. 5.) The women who participated in this study were generally more educated, more likely to be married and to be covered by private insurance than women in the state of Pennsylvania delivering their first child overall [37][38], which limits the generalizability of the study results.
Conclusions
Our study results suggest that the way that women experience, process, react to and remember first childbirth may have long-term effects on the way they relate to their child. For some women in this study childbirth was a frightening and distressing experience that resulted in the development of post-traumatic stress symptoms. The importance of women’s immediate emotional reactions to their childbirth (childbirth experience) and their perception of the extent to which they were involved in the delivery decision-making process suggest areas where obstetric departments may be able to improve the care they provide to women during childbirth and help women to understand and process the delivery in a positive and healthy way.
Highlights.
47.5% were afraid that they or their baby might be hurt or die in labor/delivery.
7.5% experienced childbirth-related post-traumatic stress disorder (CR-PTSD).
A key predictor of CR-PTSD was reporting a less positive birth experience.
CR-PTSD was associated with maternal-infant bonding at 1, 6 and 12-months.
Funding
This study was funded by grant R01-HD052990 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, USA.
Appendix A. Sociodemographic, psychosocial and clinical measures
Prenatal Measures
Age:
As part of the screening process women were asked their age. Age was verified in relation to the maternal age reported the birth certificate record.
Race/Ethnicity:
In the baseline interview women were asked “Do you consider yourself Hispanic or Latina?” and “Do you consider yourself primarily white or Caucasian, Black or African American, Asian, Native Hawaiian or Pacific Islander, American Indian or Alaskan Native, or something else?” If women did not answer one or both of these questions we obtained race/ethnicity information from the birth certificate data.
Education:
In the baseline interview women were asked “What is the highest level of schooling you completed?” If they did not answer this question we obtained this information from the birth certificate data.
Insurance coverage at delivery:
This information was obtained from the hospital discharge data. There were 12 women who were initially classified as self-pay in the discharge data. However, 11 of these 12 women reported at the 6- or 12-month survey that their delivery bills had been covered by Medicaid and were reclassified as insured by Medicaid (public insurance).
Marital status:
In the baseline interview women were asked “Are you married and living with your husband, not married but living with a partner, widowed, divorced, separated or never been married?” If they answered “widowed”, “divorced”, “separated” or “never been married” we then asked “Do you have a partner or significant other (sweetheart)?”. If they answered “No” they were classified as not having a partner. If they answered “yes” we then asked “Do you currently live with this person?” If they answered “no” they were classified as “Partner, not living with”.
Pregnancy intendedness:
In the baseline interview women were asked “Thinking back to just before you got pregnant this time, how did you feel about becoming pregnant?” with response options of “You wanted to be pregnant sooner”, “You wanted to be pregnant later”, “you wanted to be pregnant then” and “You didn’t want to be pregnant then or at any time in the future”. This is a standard question used in the Pregnancy Risk Assessment Monitoring System in the U.S. [49]. If women answered that they wanted to be pregnant later or never, they were classified as having an unintended pregnancy.
Trouble paying for basic needs:
In the baseline interview women were asked “In general do you and your family have a lot of trouble, some trouble, or no trouble at all paying for basic needs such as food, housing, gas and electric bills?” Answers were classified into two categories, “a lot of trouble” or “some trouble” versus “no trouble”.
History of diagnosed anxiety or depression:
In the baseline interview women were asked “Before this pregnancy has a doctor or other health care professional told you that you had any of the following health conditions?” The interviewers read a list of 31 health conditions, including “anxiety or depression”.
Previous pregnancy loss:
In the baseline interview women were asked “How many times have you been pregnant in your life counting your current pregnancy” For each pregnancy that had ended they were asked to report how each pregnancy had ended, including miscarriages and abortions. Because women who had a pregnancy of 20 weeks or longer were excluded, none of the study participants would have had a prior stillbirth.
Plan to breastfeed:
In the baseline interview participants were asked “Do you plan to breastfeed, bottle-feed or both?” Women who answered “breastfeed” or “both” were classified as planning to breastfeed.
High risk pregnancy:
We used the ICD-9 codes in the hospital discharge data to identify women with one or more of a potential of 30 pregnancy complications that would define them as high-risk, such as diabetes, hypertension and heart disease, as described in Korst et al [50].
Depression:
Depression during pregnancy was measured using the 10-item Edinburgh Depression Scale (EDS), with a cut-off score of 13 or higher to indicate probable depression [51]. Total scores could range from 0 (no depression) to 30 (high depression). The Cronbach’s alpha for the EDS was 0.79.
Stress:
Stress was measured using a modified version of the Psychosocial Hassles Scale (PHS) [52] [53]. In the PHS respondents are asked to rate the degree of stress they experienced during the pregnancy due to specific factors such as “Money worries like paying bills” and “Problems with the pregnancy itself”. The response options were “No stress”, “Some stress”, “Moderate stress” and “Severe stress”. Based on pilot testing of the study questionnaires two of the items in the original version of the instrument exhibited poor corrected item-total correlations. These items were “Sexual, emotional or physical abuse” and “Problems with alcohol or drugs”. Based on focus group studies discussing common problems experienced during pregnancy we changed these items to “Fights with partner” and “Fights with other family members”. These new items worked well and exhibited good corrected item-total correlations. Total scores could range from 12 (no stress) to 48 (high stress). The overall Cronbach’s alpha for the scale was 0.76. Total scores were classified into three categories: 12–16 (low stress), 17–20 (medium stress), and 21–48 (high stress).
Social support:
Social support was measured using a 5-item version of the Medical Outcomes Study (MOS) Social Support Scale (the SS-5) [54]. In this measure participants were asked to report how often they have specific types of support available to them, such as “Someone to confide in or talk to about your problems”. Response options were “None of the time”, “A little of the time”, “Some of the time”, “Most of the time” and “All of the time”. Total scores could range from 5 to 25, with higher scores indicating higher social support. Total scores were classified into three categories of social support: 5–19 (low), 20–23 (medium), and 24–25 (high). The Cronbach’s alpha for the SS-5 was 0.88.
Fear of childbirth:
In the baseline interview women were administered the FBS-CAS (First Baby Study Childbirth Anticipation Scale) [55], and were asked to indicate the extent to which they had 10 feelings about the upcoming delivery, using the rating scale of “Extremely”, “Quite a bit”, “Moderately”, “A Little” and “Not at all”. Women’s ratings of the extent to which they were feeling four emotions (nervous, worried, fearful and terrified) were summated to create a total score of fear of childbirth. Total scores could range from 4 (no fear) to 20 (high fear). The Cronbach’s alpha for this scale was .84. Total scores were classified into three categories: 4–8 (low fear), 9–12 (medium fear), and 13–20 (high fear).
Postpartum Measures
Labor induction:
In the 1-month postpartum interview women were asked “Were you in labor when you arrived at the hospital?” and “Did a doctor or nurse in the hospital try to cause your labor to BEGIN by the use of drugs or some other technique?” This is often called trying to induce labor.” Women who answered “no” to the first question and “yes” to the second question were classified as undergoing labor induction. Participants who reported one or more cervical ripening procedures before hospital admission were also classified as having been induced.
Duration of labor:
In the 1-month postpartum interview women were asked “As best as you can remember, about how many hours was it from the time when you first had regular contractions until you delivered your baby? If you are not sure, your best estimate will be fine.” This question was adapted from the “Listening to Mothers” surveys [56].
Maternal morbidities based on ICD-9 codes:
We used the ICD-9 codes in the hospital discharge data to identify women who experienced one or more of 48 possible complications during labor, delivery and postpartum while in the hospital, such as infection, perineal laceration and wound dehiscence, as described in Korst et al [50].
Neonatal morbidities based on ICD-9 codes:
We used the ICD-9 codes in the hospital discharge data to identify newborns who experienced one or more of 63 possible complications during labor, delivery and postnatally while in the hospital, such as birth trauma, hypoxia/asphyxia, or clavicle fracture, as described in Korst et al [50].
Maternal reported complications:
In the 1-month postpartum interview women were asked: “Did you have any complications as a result of the delivery?” and “Did your baby have any complications?”
Mode of delivery:
In the 1-month survey women were asked “Did you have your baby vaginally or by cesarean section?” Maternal self-report of mode of delivery matched 100% with the diagnosis-related group (DRG) code recorded in the hospital discharge data for mode of delivery.
Planned versus unplanned cesarean:
Women who reported that they delivered by cesarean section were then asked “Did you have a planned cesarean section that was scheduled to occur before you went into labor, that is, before regular contractions began, or did you have an unplanned cesarean delivery?” In addition, women were queried extensively about labor, including such questions as: “Were you in labor when you arrived at the hospital?”, “How long had you been in labor when you arrived at the hospital?”, “At some point did your contractions become regular and 5 minutes or less apart? “When you were in labor how painful was it for you during your contractions, before you received any type of pain medication?”, and “As best as you can remember, about how many hours was it from the time when you first had regular contractions until you delivered your baby?”. There were 152 women who reported that they delivered by planned cesarean delivery. For all 152 women their answers to the questions about labor supported their report that they had cesarean delivery before onset of labor. However, among the 711 women who reported that they had unplanned cesarean, we found 8 women who reported that they were not in labor at the time of hospital admission, were not induced, reported no hours in labor and no pain resulting from labor contractions. In addition, none of the indications for cesarean delivery for these 8 women were labor-related. Therefore, we classified these women as having had planned cesarean delivery, for a total of 160 women who had planned cesarean delivery and 703 women who had unplanned cesarean.
Instrumental vaginal:
Women were asked “During your labor and birth, did someone “Use forceps to help get the baby out?” and “During your labor and birth, did someone us a vacuum extractor to help get the baby out?” These questions were from the “Listening to Mothers” surveys [56]. Some women were not certain if they had instrumental delivery, in which case we measured this variable using the birth certificate data.
Spontaneous vaginal:
Women who reported that they delivered vaginally and were not found to have delivered instrumentally were classified as having had spontaneous vaginal delivery.
Gestational age:
We used the obstetrician-estimated gestational age reported in the birth certificate data. We further verified gestational age in relation to the ICD-9 diagnostic codes indicating that the child was born preterm or post-term. Although we also calculated gestational age based on the last menses date reported in the birth certificate data, this later method was generally not in agreement with the obstetrician-estimated gestational age.
Newborn birth weight:
Newborn birth weight was obtained from the birth certificate data.
5-minute Apgar:
The 5-minute Apgar score was obtained from the birth certificate data.
Maternal postpartum hemorrhage:
This variable was measured via the ICD-9 codes 666.0 to 666.3 reported in the hospital discharge data.
Maternal hospital length of stay:
The length of hospital stay for the mother was obtained from the hospital discharge data.
Infant hospital length of stay:
The length of hospital stay for the newborn was obtained from the hospital discharge data.
Breastfeeding at 1-month:
In the 1-month interview women were asked “Have you ever breastfed or tried to breastfeed your baby?” and “Are you still breastfeeding your baby?”
Childbirth Experience:
Participants completed the 16-item FBS Birth Experience Scale (FBS-BES) [55] as part of the 1-month postpartum interview. In this scale participants were asked to think back to right after they had their baby and to report the extent to which they had positive or negative feelings, such as “disappointed”, “delighted”, and “upset”, using the response options of “extremely”, “quite a bit”, “moderately”, “a little bit” and “not at all”. Higher scores indicated a more positive birth experience. Total scores could range from 16 to 80 and the higher the score the more positive the birth experience. The Cronbach’s alpha for the FBS-BES was 0.74.
Poor pain control:
In the 1-month postpartum interview women who received pain medications during labor were asked to rate how helpful the pain medications were, using a four-point scale ranging from “not helpful at all” to “very helpful”, and to rate their degree of pain at delivery, using a 0 to 10 scale ranging from “no pain” to “the worst pain imaginable”. Women who reported that the pain medications they received in labor were not very helpful and/or reported a pain level of 9 or 10 at delivery were classified as experiencing poor pain control.
Shared decision-making:
Shared decision-making was measured using the Delivery Decision-Making Scale (DDMS) [57]. The DDMS has six items, such as “I had an equal say in how my baby was delivered” and “I was treated with respect throughout the delivery process”, and participants answered “true” or “false” to each item. Scores could range from 0 to 6, and we created three categories of shared decision-making: low (0–3), moderate (4–5) or high (6). The internal consistency (Kuder-Richardson) of the DDMS was 0.69.
Postpartum depression:
We used the same 10-item measure of depression in the 1-month postpartum interview as in the baseline interview.
Postpartum stress:
We used the same 12-item measure of psychosocial stress as we did in the baseline interview. However, the item “Problems with the pregnancy itself” was changed to “Problems with the baby”. Total scores could range from 12 to 48 and the Cronbach’s alpha was 0.73.
Postpartum social support:
To measure social support at 1-month postpartum we used the same 5-items as in the baseline interview. However, we added 4 items to measure social support that a new mother might need, to create a 9-item measure of postpartum social support. These new items were “Someone to teach you what you need to know about taking care of a new baby”, “someone to give you advice about breastfeeding if you needed it”, “Someone to help you take care of the baby” and “someone to give you a break taking care of the baby so you can get some rest”. These four new items worked well and the Cronbach’s alpha of this 9-items scale was 0.88. Total scores could range from 9 to 45, with higher scores indicating stronger social support. We created three categories of social support: 9–36 (low), 37–41 (medium) and 42–45 (high).
Appendix B. Maternal-infant bonding measure
Table B1.
Ten items used to measure maternal-infant bonding at 1, 6 and 12 months postpartum and corrected item-total correlations at 1-month postpartum
| Scoring | All of the time | Most of the time | Some of the time | A little of the time | None of the time | Corrected item-total correlation | ||
|---|---|---|---|---|---|---|---|---|
| 1. | I feel close to my baby | Reverse | 1 | 2 | 3 | 4 | 5 | 0.515 |
| 2. | I wish the old days when I had no baby would come back | 1 | 2 | 3 | 4 | 5 | 0.456 | |
| 3. | I feel distant from my baby | 1 | 2 | 3 | 4 | 5 | 0.397 | |
| 4. | I love to cuddle my baby | Reverse | 1 | 2 | 3 | 4 | 5 | 0.429 |
| 5. | I wish that I had never had this baby | 1 | 2 | 3 | 4 | 5 | 0.307 | |
| 6. | I feel happy when my baby looks at me | Reverse | 1 | 2 | 3 | 4 | 5 | 0.295 |
| 7. | My baby cries too much | 1 | 2 | 3 | 4 | 5 | 0.342 | |
| 8. | I love my baby with all my heart | Reverse | 1 | 2 | 3 | 4 | 5 | 0.340 |
| 9. | My baby annoys me | 1 | 2 | 3 | 4 | 5 | 0.470 | |
| 10. | I feel like being a mother is something that I am very good at | Reverse | 1 | 2 | 3 | 4 | 5 | 0.482 |
Items 1, 2, 3, 4, 7 and 9 are from the Postpartum Bonding Questionnaire (PBQ) [39]. Items 5, 6, 8 and 10 are similar to PBQ items, but were reworded, primarily to be more appropriate for American respondents. For example, we changed “I love my baby to bits” to “I love my baby with all my heart”. The first nine items are identical to those in the Shortened Postpartum Bonding Questionnaire (S-PBQ) described in Kinsey et al [58], however we changed the tenth item from “I feel confident when changing my baby’s diapers” to “I feel like being a mother is something that I am good at” because the corrected item-total correlation for the former item was poor (0.175).
Total scores on this scale could range from 10 to 50, with higher scores indicating more positive maternal-infant bonding. The overall Cronbach’s alpha score at 1-month postpartum (n = 3005) was 0.71 and each of the ten items exhibited adequate corrected item-total correlations, as can be seen in Table 1.
The distribution of total scores at 1-month postpartum ranged from 22 to 50, the mean was 47.0, the standard deviation was 2.9, the median was 48.0, the mode was 50.0, skewness was −1.757, and kurtosis was 6.205. Because this variable was both skewed and highly kurtotic, with women generally scoring at the very high end of possible scores, we identified women scoring in the bottom third of the distribution at 1, 6 and 12 months postpartum as those with potentially impaired bonding. The cut off scores for women in the top two-thirds of the distributions were 47 and above at 1-month and 48 and above at 6 and 12-months postpartum.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of interest: none
Conflict of interest
All authors have no competing interests to report.
Contributor Information
Kristen H. Kjerulff, Departments of Public Health Sciences and Obstetrics and Gynecology, College of Medicine, Penn State University, Hershey, Pennsylvania, USA.
Laura B. Attanasio, School of Public Health & Health Sciences, University of Massachusetts Amherst, Amherst, Massachusetts, USA.
Kristin K. Sznajder, Department of Public Health Sciences, College of Medicine, Penn State University, Hershey, Pennsylvania, USA.
Laura H. Brubaker, Department of Obstetrics and Gynecology, Penn State Milton S. Hershey Medical Center, Hershey, Pennsylvania, USA.
REFERENCES
- [1].Verreault N, Da Costa D, Marchand A, Ireland K, Banack H, Dritsa M, Khalifé S, PTSD following childbirth: A prospective study of incidence and risk factors in Canadian women, J. Psychosom. Res (2012). 10.1016/j.jpsychores.2012.07.010. [DOI] [PubMed] [Google Scholar]
- [2].Hairston IS, Handelzalts JE, Assis C, Kovo M, Postpartum bonding difficulties and adult attachment styles: The mediating role of postpartum depressin and childbirth-related PTSD, Infant Ment. Health J (2018). 10.1002/imhj.21695. [DOI] [PubMed] [Google Scholar]
- [3].Handelzalts JE, Hairston IS, Muzik M, Tahar AM, Levy S, A Paradoxical Role of Childbirth-Related Posttraumatic Stress Disorder (PTSD) Symptoms in the Association Between Personality Factors and Mother-Infant Bonding: A Cross-Sectional Study, Psychol. Trauma Theory, Res. Pract. Policy (2019). 10.1037/tra0000521. [DOI] [PubMed] [Google Scholar]
- [4].Dekel S, Ein-Dor T, Dishy GA, Mayopoulos PA, Beyond postpartum depression: posttraumatic stress-depressive response following childbirth, Arch. Womens. Ment. Health (2020). 10.1007/s00737-019-01006-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Wijma K, Söderquist J, Wijma B, Posttraumatic stress disorder after childbirth: A cross sectional study, J. Anxiety Disord (1997). 10.1016/S0887-6185(97)00041-8. [DOI] [PubMed] [Google Scholar]
- [6].Stramrood CAI, Paarlberg KM, E.M.J. Huis In’T Veld, Berger LWAR, Vingerhoets AJJM, Weijmar Schultz WCM, Van Pampus MG, Posttraumatic stress following childbirth in homelike-and hospital settings, J. Psychosom. Obstet. Gynecol (2011). 10.3109/0167482X.2011.569801. [DOI] [PubMed] [Google Scholar]
- [7].Huennekens K, Oot A, Lantos E, Yee LM, Feinglass J, Using Electronic Health Record and Administrative Data to Analyze Maternal and Neonatal Delivery Complications, Jt. Comm. J. Qual. Patient Saf (2020). 10.1016/j.jcjq.2020.08.007. [DOI] [PubMed] [Google Scholar]
- [8].Caughey AB, Cahill AG, Guise JM, Rouse DJ, Safe prevention of the primary cesarean delivery, Obstet. Gynecol. Surv (2014). 10.1016/j.ajog.2014.01.026. [DOI] [PubMed] [Google Scholar]
- [9].Sakala C, Belanoff C, Declercq ER, Factors Associated with Unplanned Primary Cesarean Birth: Secondary Analysis of the Listening to Mothers in California Survey, BMC Pregnancy Childbirth (2020). 10.1186/s12884-020-03095-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Chen Y, Yang X, Guo C, Liao Y, Guo L, Chen W, Chen I, Krewski D, Wen SW, Xie RH, Prevalence of Post-Traumatic Stress Disorder following Caesarean Section: A Systematic Review and Meta-Analysis, J. Women’s Heal (2020). 10.1089/jwh.2019.7750. [DOI] [PubMed] [Google Scholar]
- [11].Grekin R, O’Hara MW, Prevalence and risk factors of postpartum posttraumatic stress disorder: A meta-analysis, Clin. Psychol. Rev (2014). 10.1016/j.cpr.2014.05.003. [DOI] [PubMed] [Google Scholar]
- [12].Yildiz PD, Ayers S, Phillips L, The prevalence of posttraumatic stress disorder in pregnancy and after birth: A systematic review and meta-analysis, J. Affect. Disord (2017). 10.1016/j.jad.2016.10.009. [DOI] [PubMed] [Google Scholar]
- [13].Dekel S, Stuebe C, Dishy G, Childbirth induced posttraumatic stress syndrome: A systematic review of prevalence and risk factors, Front. Psychol (2017). 10.3389/fpsyg.2017.00560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Olde E, Van Der Hart O, Kleber R, Van Son M, Posttraumatic stress following childbirth: A review, Clin. Psychol. Rev (2006). 10.1016/j.cpr.2005.07.002. [DOI] [PubMed] [Google Scholar]
- [15].Furuta M, Sandall J, Bick D, A systematic review of the relationship between severe maternal morbidity and post-traumatic stress disorder, BMC Pregnancy Childbirth (2012). 10.1186/1471-2393-12-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Andersen LB, Melvaer LB, Videbech P, Lamont RF, Joergensen JS, Risk factors for developing post-traumatic stress disorder following childbirth: A systematic review, Acta Obstet. Gynecol. Scand (2012). 10.1111/j.1600-0412.2012.01476.x. [DOI] [PubMed] [Google Scholar]
- [17].Ayers S, Bond R, Bertullies S, Wijma K, The aetiology of post-traumatic stress following childbirth: A meta-analysis and theoretical framework, Psychol. Med 46 (2016) 1121–1134. 10.1017/S0033291715002706. [DOI] [PubMed] [Google Scholar]
- [18].Simpson M, Schmied V, Dickson C, Dahlen HG, Postnatal post-traumatic stress: An integrative review, Women and Birth (2018). 10.1016/j.wombi.2017.12.003. [DOI] [PubMed] [Google Scholar]
- [19].Sheiner E, Sheiner EK, Shoham-Vardi I, The relationship between parity and labor pain, Int. J. Gynecol. Obstet (1998). 10.1016/S0020-7292(98)00164-7. [DOI] [PubMed] [Google Scholar]
- [20].Labor S, Maguire S, Labour is a painful process and is ranked high on the pain rating scale (1), Rev. Pain (2008). [Google Scholar]
- [21].Allen S, A qualitative analysis of the process, mediating variables and impact of traumatic childbirth, J. Reprod. Infant Psychol (1998). 10.1080/02646839808404563. [DOI] [Google Scholar]
- [22].R.-A. J., H.-M. A., R.-A. D., Q.-G. J.M., M.-G. J.M., G.-S. J., Women’s perceptions of living a traumatic childbirth experience and factors related to a birth experience, Int. J. Environ. Res. Public Health (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Elmir R, Schmied V, Wilkes L, Jackson D, Women’s perceptions and experiences of a traumatic birth: A meta-ethnography, J. Adv. Nurs (2010). 10.1111/j.1365-2648.2010.05391.x. [DOI] [PubMed] [Google Scholar]
- [24].Reed R, Sharman R, Inglis C, Women’s descriptions of childbirth trauma relating to care provider actions and interactions, BMC Pregnancy Childbirth (2017). 10.1186/s12884-016-1197-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders, 4th Ed. DSM-IV-TR, 2000. https://doi.org/10.1176/dsm10.1176/appi.books.9780890420249.dsm-iv-tr10.1176/appi.books.9780890420249.dsm-iv-tr . [Google Scholar]
- [26].Ayers S, Eagle A, Waring H, The effects of childbirth-related post-traumatic stress disorder on women and their relationships: A qualitative study, Psychol. Heal. Med (2006). 10.1080/13548500600708409. [DOI] [PubMed] [Google Scholar]
- [27].Ayers S, Wright DB, Wells N, Symptoms of post-traumatic stress disorder in couples after birth: Association with the couple’s relationship and parent-baby bond, J. Reprod. Infant Psychol (2007). 10.1080/02646830601117175. [DOI] [Google Scholar]
- [28].Handelzalts JE, Levy S, Molmen-Lichter M, Ayers S, Krissi H, Wiznitzer A, Peled Y, The association of attachment style, postpartum PTSD and depression with bonding- A longitudinal path analysis model, from childbirth to six months, J. Affect. Disord (2021). 10.1016/j.jad.2020.10.068. [DOI] [PubMed] [Google Scholar]
- [29].McDonald S, Slade P, Spiby H, Iles J, Post-traumatic stress symptoms, parenting stress and mother-child relationships following childbirth and at 2 years postpartum, J. Psychosom. Obstet. Gynecol (2011). 10.3109/0167482X.2011.596962. [DOI] [PubMed] [Google Scholar]
- [30].Seng JS, Sperlich M, Low LK, Ronis DL, Muzik M, Liberzon I, Childhood Abuse History, Posttraumatic Stress Disorder, Postpartum Mental Health, and Bonding: A Prospective Cohort Study, J. Midwifery Women’s Heal (2013). 10.1111/j.1542-2011.2012.00237.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Radoš SN, Matijaš M, Anđelinović M, Čartolovni A, Ayers S, The role of posttraumatic stress and depression symptoms in mother-infant bonding, J. Affect. Disord (2020). 10.1016/j.jad.2020.03.006. [DOI] [PubMed] [Google Scholar]
- [32].Stuijfzand S, Garthus-Niegel S, Horsch A, Parental Birth-Related PTSD Symptoms and Bonding in the Early Postpartum Period: A Prospective Population-Based Cohort Study, Front. Psychiatry (2020). 10.3389/fpsyt.2020.570727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Suetsugu Y, Haruna M, Kamibeppu K, A longitudinal study of bonding failure related to aspects of posttraumatic stress symptoms after childbirth among Japanese mothers, BMC Pregnancy Childbirth (2020). 10.1186/s12884-020-03099-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Davies J, Slade P, Wright I, Stewart P, Posttraumatic stress symptoms following childbirth and mothers’ perceptions of their infants, Infant Ment. Health J (2008). 10.1002/imhj.20197. [DOI] [PubMed] [Google Scholar]
- [35].Dekel S, Thiel F, Dishy G, Ashenfarb AL, Is childbirth-induced PTSD associated with low maternal attachment?, Arch. Womens. Ment. Health (2019). 10.1007/s00737-018-0853-y. [DOI] [PubMed] [Google Scholar]
- [36].Tichelman E, Westerneng M, Witteveen AB, Van Baar AL, Van Der Horst HE, De Jonge A, Berger MY, Schellevis FG, Burger H, Peters LL, Correlates of prenatal and postnatal motherto-infant bonding quality: A systematic review, PLoS One (2019). 10.1371/journal.pone.0222998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Kjerulff KH, Velott DL, Zhu J, Chuang CH, Hillemeier MM, Paul IM, Repke JT, Mode of first delivery and women’s intentions for subsequent childbearing: Findings from the first baby study, Paediatr. Perinat. Epidemiol 27 (2013). 10.1111/ppe.12014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Kjerulff KH, Paul IM, Weisman CS, Hillemeier MM, Wang M, Legro RS, Repke JT, Association Between Mode of First Delivery and Subsequent Fecundity and Fertility, JAMA Netw. Open (2020). 10.1001/jamanetworkopen.2020.3076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Brockington IF, Fraser C, Wilson D, The Postpartum Bonding Questionnaire: A validation, Arch. Womens. Ment. Health 9 (2006) 233–242. 10.1007/s00737-006-0132-1. [DOI] [PubMed] [Google Scholar]
- [40].Brewin CR, Rose S, Andrews B, Green J, Tata P, McEvedy C, Turner S, Foa EB, Brief screening instrument for post-traumatic stress disorder, Br. J. Psychiatry (2002). 10.1017/s0007125000161896. [DOI] [PubMed] [Google Scholar]
- [41].Boorman RJ, Devilly GJ, Gamble J, Creedy DK, Fenwick J, Childbirth and criteria for traumatic events, Midwifery (2014). 10.1016/j.midw.2013.03.001. [DOI] [PubMed] [Google Scholar]
- [42].Zaat TR, van Steijn ME, de Haan-Jebbink JM, Olff M, Stramrood CAI, van Pampus MG, Posttraumatic stress disorder related to postpartum haemorrhage: A systematic review, Eur. J. Obstet. Gynecol. Reprod. Biol (2018). 10.1016/j.ejogrb.2018.04.012. [DOI] [PubMed] [Google Scholar]
- [43].Canfield D, Silver RM, Detection and Prevention of Postpartum Posttraumatic Stress Disorder: A Call to Action, Obstet. Gynecol (2020). 10.1097/AOG.0000000000004093. [DOI] [PubMed] [Google Scholar]
- [44].Prins A, Bovin MJ, Smolenski DJ, Marx BP, Kimerling R, Jenkins-Guarnieri MA, Kaloupek DG, Schnurr PP, Kaiser AP, Leyva YE, Tiet QQ, The Primary Care PTSD Screen for DSM-5 (PC-PTSD-5): Development and Evaluation Within a Veteran Primary Care Sample, J. Gen. Intern. Med (2016). 10.1007/s11606-016-3703-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].de Graaff LF, Honig A, van Pampus MG, Stramrood CAI, Preventing post-traumatic stress disorder following childbirth and traumatic birth experiences: a systematic review, Acta Obstet. Gynecol. Scand (2018). 10.1111/aogs.13291. [DOI] [PubMed] [Google Scholar]
- [46].Alcorn KL, O’Donovan A, Patrick JC, Creedy D, Devilly GJ, A prospective longitudinal study of the prevalence of post-traumatic stress disorder resulting from childbirth events, Psychol. Med (2010). 10.1017/S0033291709992224. [DOI] [PubMed] [Google Scholar]
- [47].A.P. Association, American Psychiatric Association, 2013. Diagnostic and statistical manual of mental disorders (5th ed.), 2013. [Google Scholar]
- [48].Parfitt YM, Ayers S, The effect of post-natal symptoms of post-traumatic stress and depression on the couple’s relationship and parent-baby bond, J. Reprod. Infant Psychol (2009). 10.1080/02646830802350831. [DOI] [Google Scholar]
- [49].Finer LB, Henshaw SK, Disparities in Rates of Unintended Pregnancy In the United States, 1994 and 2001, Perspect. Sex. Reprod. Health (2006). 10.1363/3809006. [DOI] [PubMed] [Google Scholar]
- [50].Korst LM, Fridman M, Lu MC, Mitchell C, Lawton E, Griffin F, Gregory KD, Monitoring childbirth morbidity using hospital discharge data: Further development and application of a composite measure, Am. J. Obstet. Gynecol (2014). 10.1016/j.ajog.2014.03.011. [DOI] [PubMed] [Google Scholar]
- [51].Cox J, Chapman G, Murray D, Jones P, Validation of the Edinburgh Postnatal Depression Scale (EPDS) in non-postnatal women, J. Affect. Disord (1996). http://www.sciencedirect.com/science/article/pii/0165032796000080 (accessed May 10, 2017). [DOI] [PubMed]
- [52].Misra DP, O’Campo P, Strobino D, Testing a sociomedical model for preterm delivery, Paediatr. Perinat. Epidemiol 15 (2001) 110–122. 10.1046/j.1365-3016.2001.00333.x. [DOI] [PubMed] [Google Scholar]
- [53].Phelan AL, DiBenedetto MR, Paul IM, Zhu J, Kjerulff KH, Psychosocial Stress During First Pregnancy Predicts Infant Health Outcomes in the First Postnatal Year, Matern. Child Health J 19 (2015). 10.1007/s10995-015-1777-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].McCarrier K, Bushnell D, Martin M, Paczkowski R, Nelson D, Buesching D, Validation and Psychometric Evaluation of a 5-Item Measure of Perceived Social Support, Value Heal 14 (2011) A148. 10.1016/j.jval.2011.02.824. [DOI] [Google Scholar]
- [55].Elvander C, Cnattingius S, Kjerulff KH, Birth experience in women with low, intermediate or high levels of fear: Findings from the first baby study, Birth 40 (2013) 289–296. 10.1111/birt.12065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Declercq ER, Sakala C, Corry MP, Applebaum S, Listening to Mothers II: Report of the Second National U.S. Survey of Women’s Childbearing Experiences, J. Perinat. Educ 16 (2007) 15–17. 10.1624/105812407X244778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Attanasio LB, Kozhimannil KB, Kjerulff KH, Factors influencing women’s perceptions of shared decision making during labor and delivery: Results from a large-scale cohort study of first childbirth, Patient Educ. Couns (2018). 10.1016/j.pec.2018.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Kinsey CB, Baptiste-Roberts K, Zhu J, Kjerulff KH, Birth-related, psychosocial, and emotional correlates of positive maternal-infant bonding in a cohort of first-time mothers, Midwifery 30 (2014) e188–94. 10.1016/j.midw.2014.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]


